Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT | |
| Participants | Workers (33 males and 12 females) disabled and not working due to low‐back pain for at least 3 month duration, with or without referred pain, mean age 39.91(8.91). | |
| Interventions | Intervention 1 : Standard treatment programme was a in‐patient, multidisciplinary approach to assisting workers in returning to function, that included twice daily sessions of physical therapy and daily aerobic fitness training to increase activity tolerance levels. Daily education classes on mechanisms of pain and group support were also added. Vocational rehabilitation was included through group and individual educational sessions. In addition, patients' medication intake was monitored (n =24). Intervention 2 : Psychological programme included in addition to the standard treatment programme an operant conditioning component involving daily charting of exercise behaviour, with contingent verbal praise, daily relaxation and biofeedback sessions. Group and individual training sessions to teach cognitive behavioural coping skills such as reconceptualisation of pain as an experience were also included. In addition, patients completed daily home work exercises that were reviewed with them on a daily basis (n = 21). Programme duration: three weeks. | |
| Outcomes | Outcome assessed at 6 months after treatment. Return to employment (conservative ie full employment at same job; and liberal measures ie if full time on light duties or part‐time work or training) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Does not state |
| Allocation concealment (selection bias) | Unclear risk | Does not state |
| Blinding (performance bias and detection bias) | High risk | Does not state |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care provider aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | All subjects recorded follow‐up data |
| Incomplete outcome data (attrition bias) | High risk | 21 subjects in each group analysed (there was 2 workers in psychological group) |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | no statistical significant differences between groups in terms of demographic differences |
| Co‐interventions avoided or similar? | Low risk | no co‐interventions mentioned |
| Compliance acceptable? | Unclear risk | measured, but not reported what was considered non‐compliant |
| Timing of the outcome assessment similar? | Low risk | all measurements post‐treatment programme at 6 months |
| Methods | RCT | |
| Participants | workers (28 males and 66 females) with low‐back pain with or without radiation for over 6 months. 78% not working or on suitable duties. | |
| Interventions | Intervention 1(A1) : A combination of 3 modalities was offered: 1. Intensive physical training including aerobic capacity, coordination, muscle strength, and endurance, flexibility, stretching exercises, work hardening, ergonomic training and recreation including ball games, swimming for 5 hrs/day. 2. Psychological pain management that included relaxation and biofeedback for 2 hours a day guided by the clinical psychologist. 3. Patient education of 1 hour/day on a variety of topics led by physicians, therapists, psychologists, social worker and nutritionist (n = 50). Programme duration: a full day (eight hour) programme every weekday for three consecutive weeks followed by a full day per week during the following three weeks (Total: 135 hours). Control: CAU: consisted of no treatment offered, but patients could receive treatment elsewhere. 80% reported seeking treatment elsewhere mostly traditional physical therapy with passive modalities (61%) and manipulation by chiropractor (35%). | |
| Outcomes | Outcome assessed at 12 months. 1. Ability to work (5 categories); 2. contacts with healthcare system; 3. number of sick leave days; 4. back pain (scale of 0‐10); 5. leg pain (scale 0‐10); 6. activities of daily living (scale 0‐30) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Does not state |
| Allocation concealment (selection bias) | High risk | Does not state |
| Blinding (performance bias and detection bias) | Low risk | The project was blinded in that the physician who saw the the patients for the initial examination and the 4‐month follow‐up did not know which group each patient was in. The same physician saw all the patients in both groups throughout the study. The blinding was broken in about 10% of the cases. |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 2 before the treatment programme, 7 during the programme |
| Incomplete outcome data (attrition bias) | High risk | dropouts not analysed at follow‐up |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | no significant differences |
| Co‐interventions avoided or similar? | High risk | intervention group had significantly less contacts with healthcare system than control group |
| Compliance acceptable? | Low risk | except for the dropouts. |
| Timing of the outcome assessment similar? | Low risk | all workers were analysed at baseline and after 4 months |
| Methods | RCT | |
| Participants | Workers (28 males and 75 females) with chronic low‐back pain for over 6 months, and 73% not working or on suitable duties. | |
| Interventions | Intervention 1(B1): A combination of 3 modalities was offered: 1. Intensive physical training including aerobic capacity, coordination, muscle strength, and endurance, flexibility, stretching exercises, work hardening, ergonomic training and recreation including ball games, swimming for 5 hrs/day. 2. Psychological pain management that included relaxation and biofeedback for 2 hours a day guided by the clinical psychologist. 3. Patient education of 1 hour/day on a variety of topics led by physicians, therapists, psychologists, social worker and nutritionist (n = 50). Programme duration: a full day (eight hour) programme every week day for three consecutive weeks followed by a full day per week during the following three weeks (Total: 135 hours). Intervention 2 (B2): Outpatient programme for small group (7‐8) people receiving physical training: 45 min aerobics and 45 min progressive resistance training, twice a week for 6 weeks. One hour of theoretical back school lessons every second day. Intervention 3 (B3): Outpatient programme for small group (7‐8) people receiving 45 min physical training and 75 min psychological pain management. Twice a week for 6 weeks. | |
| Outcomes | Measurement at 1 year after randomization. 1. Ability to work (5 categories); 2. Contacts with healthcare system; 3. Number of sick leave days; 4. Back pain (scale 0‐10); 5. Leg pain (scale 0‐10); 6. Activities of daily living (scale 0‐30); 7. Use of prescription medication (%); 8. Sports activity (%); 9. Overall assessment (scale 1‐5) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | randomization procedure followed minimization principle |
| Allocation concealment (selection bias) | High risk | Does not state |
| Blinding (performance bias and detection bias) | Unclear risk | physician was blinded to treatment allocation, but the blinding was broken by patients in about 10% of cases. Unsure regarding RTW outcomes |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 14 out of 123 patients dropped out |
| Incomplete outcome data (attrition bias) | High risk | dropouts not analysed at follow‐up |
| Selective reporting (reporting bias) | Low risk | No suggestion found |
| Similarity of baseline characteristics? | Low risk | No differences found |
| Co‐interventions avoided or similar? | High risk | All groups had contact with other health professionals before follow‐up |
| Compliance acceptable? | Low risk | 14 out of 123 did not complete programme |
| Timing of the outcome assessment similar? | Low risk | all subjects follow‐up at 1 year after completion of programme |
| Methods | RCT | |
| Participants | 138 workers with chronic low‐back pain from Copenhagen Back Center of which 54% were sick listed; mean age 40, 32% men | |
| Interventions | Intervention: Function Restoration programme, including aerobics, strengthening excercises, occupational therapy, pain management/ group therapy or individual psychological sessions, stretching, theory/back school classes and recreational activities. 3 week schedule full time (8hrs per day) Control: Outpatient intensive physical training including aerobics and strenghtening exercises for 3x1, 5 hr for 8 weeks | |
| Outcomes | Measurement at 1 year after treatment: work capability, number of sick leave days | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | stratification by minimization |
| Allocation concealment (selection bias) | Unclear risk | does not state |
| Blinding (performance bias and detection bias) | Low risk | at 1 year follow‐up evaluation a few queries were discussed with the physician, who was blinded to treatment each specific patient had undergone. This blinding was successful for approx 80% of the patients, but relevant for less than half of the patients because most of them had filled out their quesitonnaire before their meeting with physician |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 21 out of 127 dropped out |
| Incomplete outcome data (attrition bias) | High risk | intention‐to‐treat data were analysed but provided data were per protocol |
| Selective reporting (reporting bias) | Low risk | No suggestion found |
| Similarity of baseline characteristics? | High risk | not regarding sick leave; work capability better for FR group |
| Co‐interventions avoided or similar? | Unclear risk | no other interventions mentioned |
| Compliance acceptable? | Unclear risk | does not state |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 1 year |
| Methods | cluster RCT | |
| Participants | 236 patients with MSDs resulting in severe restriction of work ability and who requested rehabilitation. Inclusion criteria were at least 12 weeks of sick leave in the year before rehabilitation OR subjective expectation of long‐term restrictions affecting occupational duties OR health‐related unemployment | |
| Interventions | Multimodal work hardening: a three week inpatient group programme for 6‐10 patients with 6 modules: work and health; occupational competence; exercise; aquatic exercise; functional capacity training; relaxation. Conventional musculoskeletal rehabilitation: 3 weeks inpatients therapy including exercises, patient education, and psychosocial interventions. | |
| Outcomes | Work status at 6 and 12 months defined as positive if the patient was working and had <6 or <12 (after 12 months) weeks of sick leave. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated random numbers blocked to two sequences of 16 numbers |
| Allocation concealment (selection bias) | Low risk | Performed externally by the method centre of the Rehabilitation Research Association of Berlin‐Brandenburg‐Saxony |
| Blinding (performance bias and detection bias) | Unclear risk | no report |
| Blinding (performance bias and detection bias) | High risk | patients were aware of their treatment |
| Blinding (performance bias and detection bias) | High risk | care providers were not blinded |
| Incomplete outcome data (attrition bias) | High risk | questionnaires after 6 and 12 months follow‐up were completed and returned by 169 (71.6%) and 146 (61.9%) patients, respectively |
| Incomplete outcome data (attrition bias) | Low risk | intention‐to‐treat analysis regardless of premature dropout |
| Selective reporting (reporting bias) | Low risk | No suggestion found |
| Similarity of baseline characteristics? | Low risk | two differences in parameters at baseline were considered as covariates in the analyses |
| Co‐interventions avoided or similar? | Unclear risk | no report |
| Compliance acceptable? | Low risk | treatment was completed according to protocol in 5 out of 6 modules for 91.5% of the MWH participants |
| Timing of the outcome assessment similar? | Low risk | at 6 and 12 months follow‐up |
| Methods | RCT | |
| Participants | 214 workers, with work related soft tissue injury and off work between 3 to 6 months. More than 50% had low‐back pain. | |
| Interventions | Intervention 1: Functional restoration approach: active physical therapy including stretching, strengthening and endurance building; work hardening; education and counselling to address pain related disability issues, attitudinal barriers to recovery, job satisfaction and entitlements, depression, anger and anxiety, medication reduction, sleep disruption, family problems and pain behaviours. Patients were also taught active pain management strategies, stress management and problem solving techniques, relaxation and guided imagery techniques as well as a multidimensional theory of pain. The emphasis was on acquisition of active strategies rather than reliance on passive methods to manage pain (n = 74). Programme duration: maximum of thirty five days at 6.5 hours per day. Intervention 2: Contol group: patients were discharged back to their treating physicians with a note re assessment findings, and recommendation for pro‐active management, including advice to limit narcotic medication and encourage activity despite pain (n = 64). | |
| Outcomes | Outcome assessed at 18 months. 1. Self‐reported work status (dichotomous, 2 versions, %); 2. Pain rating (scale 0‐10); 3. Sleep rating (scale 1‐3); 4. Mean reported narcotic intake (pills/week). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "following intake, the claimant was randomly assigned to a treatment of usual care condition by an employee of the WCB, who was blind to the results of the intake assessment" |
| Allocation concealment (selection bias) | Low risk | Adequate |
| Blinding (performance bias and detection bias) | Low risk | outcome assessor had no familiarity with the patients or the programme and was blind as to the patients group status |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | High risk | 26% for treatment and 36% for control dropped out, which could have led to substantial bias according to the authors |
| Incomplete outcome data (attrition bias) | High risk | "only 74% and 64% in each group respectively were available for analysis" |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | subjects were screened in order to make sure all workers were similar in terms of prognostic indicators |
| Co‐interventions avoided or similar? | Unclear risk | does not state |
| Compliance acceptable? | Unclear risk | does not state |
| Timing of the outcome assessment similar? | High risk | 17 months ‐ 18.9 months |
| Methods | RCT | |
| Participants | 363 workers (240 males and 123 females) aged 16‐65 (mean age 36) with acute (< 3 weeks) pain radiating above knee who consulted their GP for back pain. 64% of workers had reported full sick leave at study entry. | |
| Interventions | Intervention 1: 20 minutes of individual instruction from a physiotherapist, consisting of 8 exercises and 7 pieces of advice applying to daily life, including work. Exercises (in supine) were: semi‐fowler resting position, knees on chest, limbering exercise, stretching of iliopsoas, pelvic flexion, isometric abdominal exercises. The patients were taught anatomy, and were given instructions on how to stand, bend, lift, and carry objects. Work Work difficulties and problems performing the exercises were discussed, and attempts were made, together with the patient, to find solutions in order to maximise compliance. Patients received an audiotape, as well as a book with complete instructions (n = 96). Programme duration: five weeks, twice weekly. Intervention 2: (usual care): information given by GP regarding cause and course of back pain. The role of GP was to exclude other specific causes of back pain, emphasise the importance of heat, movement and short‐lasting bed rest to deal with back pain, and the requirement of return visits by the patient to the GP for follow up (n = 94). | |
| Outcomes | Measurement at 12 months after treatment. 1. Sickness absence during the follow‐up period (% of N; several levels); 2. Absence during back pain (% of N) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | block randomization ( blocks of 6) |
| Allocation concealment (selection bias) | Low risk | Adequate; patients were given sealed envelopes containing treatment group handled by nurse |
| Blinding (performance bias and detection bias) | Low risk | blinded general practitioner |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | exercise group 30 out of 122 dropouts; placebo 11out of 119 dropouts |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis for all available data |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | Low risk | no other interventions noted |
| Compliance acceptable? | Unclear risk | exercise group; 92 out of 122 met criteria for 'on treatment', and 40 patients had a good compliance; placebo group108 out of 119 met criteria for 'on treatment' |
| Timing of the outcome assessment similar? | Low risk | all workers followed up after 2 and weeks and then every months until 12 months |
| Methods | RCT | |
| Participants | 124 workers from orthopaedic practices with acute low‐back pain and decreased ability to perform normal job requirements because of pain for about 3.8 weeks. Mean age was 38.2 and 65% was male. | |
| Interventions | Intervention: a functional restoration early intervention of 3 weeks which consisted of four major components‐pscyhology, physical therapy, occupational therapy and case‐management. Contents were 3 physical evaluations, 1 physician evaluation, 18 physical therapy sessions (individual and group) 9 biofeedback/pain management sessions, 9 group didactic sessions, 9 case manager/occupational therapy sessions and 3 interdisciplinary team conferences. The number of sessions administered to patients was tailored to their specific needs, with most patients not needing all of the aforementioned number of sessions. Control: non‐intervention, care as usual | |
| Outcomes | measured at 1 year after first evaluation: % return‐to‐work | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | urn randomization procedure |
| Allocation concealment (selection bias) | Unclear risk | not stated |
| Blinding (performance bias and detection bias) | Low risk | 'by raters blind to study hypotheses' |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | no dropouts |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | 'these three groups matched for age, gender, race, and time since original injury based upon and urn randomization procedure' |
| Co‐interventions avoided or similar? | High risk | control group received various types of treatment initiated by themselves |
| Compliance acceptable? | Unclear risk | not stated |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 3, 6, 9, 12 months |
| Methods | RCT | |
| Participants | 299 workers with subacute LBP and sick leave between 3 and 6 weeks. Mean age 40.3, 79% male. 98 in high intensity back school, 98 in Low intensity back school, 103 in usual care group | |
| Interventions | Intervention 1: High‐Intensity Back School. This back school was conducted twice a week, for 8 weeks. It consisted of 16 sessions, each lasting 1 hour, supervised by a physiotherapist. Principles of cognitive‐behavioural therapy were applied throughout the back school programme. The physiotherapist promoted a timecontingent increase in the level of activity. The first two sessions consisted of individual exercises simulating the activities the worker experienced as the most problematic at the workplace. Work‐simulating and strength training exercises during subsequent sessions were performed with gradually increasing resistance. The workers were also given home exercises during the time they were participating in the back school programme. Intevention 2: Low‐Intensity Back School. This back school was based on the Swedish model and consisted of four group sessions once a week for 4 consecutive weeks. Each session was divided into an educational (30 minutes) and a practical part (90 minutes) and guided by written information and a standardized exercise programme. Workers were told that functional activities, like working, could be continued despite back pain. During the educational sessions, the physiotherapist discussed the workplace situation. Not only the most problematic activities experienced by the worker because of the low‐back pain will be discussed, workers also received information on how to cope with these activities. The practical part comprised of a standardized exercise programme consisting of strength training and home exercises. The strength training involved progressive resistance training as well as functional exercises. Workers were instructed to perform exercises at home twice a day, and again if they had any recurrences of back complaints. Control: usual cary by occupational physician according to Dutch guidelines for management of low‐back pain | |
| Outcomes | number of sick leave days at 3 and 6 months follow‐up | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | sealed opaque envelopes, coded according to a computerized random number generator, workers were randomly allocated |
| Allocation concealment (selection bias) | Low risk | done by non‐involved researcher |
| Blinding (performance bias and detection bias) | Low risk | comment by author: researcher was unaware of the randomization scheme |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 44 (15%) workers withdrew from the study |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis performed |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | no significant differences noted at baseline |
| Co‐interventions avoided or similar? | High risk | workers in the control group had free access and used other interventions |
| Compliance acceptable? | Low risk | of the 103 workers in the usual care group, 88 (85%) returned the diaries containing information about the content of their treatments. Of the 98 workers allocated to the low‐intensity back school, 75 (77%) completed all treatment sessions. In the high‐intensity back school group, 70 (71%) workers completed all treatments |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up 3 and 6 months |
| Methods | RCT | |
| Participants | 208 workers with non‐specific spinal pain, sick listed for at least 1 month. Mean age 43.5, 45% male | |
| Interventions | Intervention: 4 weeks in groups of 4‐8 workers with 6 didactic sessions addressing psychological aspects of chronic pain, ergonomics and medical aspects of chronic pain, visits to the workplace; work managers and rehabilitation officials were invited to participate in the discharge session at which a rehabilitation plan was agreed upon. 6 booster sessions were held over a period of 1 year after the treatment. A combination of Behaviour‐oriented therapy (PT) for 20 hrs per week. Aimed at enhancing the physical functioning and facilitate a lasting behaviour change of the individual. And cognitive behaviour therapy (CBT) for 13‐14 hrs per week. Aimed at improving the subjects’ ability to manage their pain and resume a normal level of activity. Programme included activity planning, goal setting, problem solving, applied relaxation, cognitive coping techniques, activity pacing , the role of vicious circles and how to break them, the role of significant others and assertion training. Individually tailored homework assignments were given at the end of each session. Control 1: only behaviour oriented therapy (PT) Control 2: only cognitive behaviour therapy (CBT) Control 3: care as usual (usual routines in health care) | |
| Outcomes | Measured at 18 and 36 months after rehabilitation: absence from work for more than 14 days | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | group randomization via blocks |
| Allocation concealment (selection bias) | Low risk | 'screening personnel were blinded to the results of the randomisation' |
| Blinding (performance bias and detection bias) | Low risk | information from author |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 28 workers dropped out of treatment |
| Incomplete outcome data (attrition bias) | Low risk | both PP and ITT analysis |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | pg 66 (Jensen 2001) |
| Co‐interventions avoided or similar? | High risk | control group could seek other medical advice or therapy |
| Compliance acceptable? | Low risk | 56%‐70% adherence to treatment plan |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up post‐treatment at 6 and 12 months |
| Methods | RCT | |
| Participants | 351 patients between 16 to 60 years, partly or fully sick‐listed from work for 4 to 12 weeks because of LBP | |
| Interventions | Intervention 1: brief clinical intervention: standard clinical LBP examination by a physician, relevant imaging and examinations were ordered and treatment options were discussed. Patients were informed about cause, prognosis and treatment options. Furthermore, they were informed about exercise being beneficial, medical pain management, and they were advised to resume work when possible. Physiotherapy examination, with advise about exercise, and general advise about increasing physical activity and exercise. Coordination between stakeholders was ensured. Follow‐up visit at physiotherapist after 2 weeks, and physician if necessary. Intervention 2: brief clinical intervention and case management. This included an interview with a case‐manager within 2‐3 days; with questions about work history, private life, pain and disability perception. The case manager and the participant made a tailored rehabilitaion plan aiming at full or partial RTW. Each case was discussed several times by the entire multidisciplinary team including the rehabilitation physician, a specialist in clinical social medicine, a physiotherapist, a social worker, and a occupational therapist. | |
| Outcomes | return to work defined as the first 4 week period within the first year after inclusion, during which the participant received no social transfer payments. Follow‐up was 1 year. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated block randomization |
| Allocation concealment (selection bias) | Low risk | Performed by a secretary |
| Blinding (performance bias and detection bias) | Low risk | data analyses were carried out by researchers outside the hospital |
| Blinding (performance bias and detection bias) | High risk | patients were aware of the result of the randomization |
| Blinding (performance bias and detection bias) | High risk | at the follow‐up consultation caregivers were aware of the result of the randomization |
| Incomplete outcome data (attrition bias) | Low risk | For primary outcome no dropouts |
| Incomplete outcome data (attrition bias) | Low risk | 100% follow‐up |
| Selective reporting (reporting bias) | Low risk | no suggestions found |
| Similarity of baseline characteristics? | Low risk | Adequate correction for any differences at baseline |
| Co‐interventions avoided or similar? | Unclear risk | not described |
| Compliance acceptable? | Unclear risk | no information |
| Timing of the outcome assessment similar? | Low risk | yes |
| Methods | RCT | |
| Participants | 107 workers with subacute low‐back pain which made working difficult for > 4 weeks and < 3 months. Mean age 44, % female 58.7 | |
| Interventions | Intervention 1: Mini‐Intervention Group (A) (60 min). Interview and examination of patient, discussion of working conditions and result of clinical examination were explained. The main aim was to reduce the patients’ concerns about their back pain by providing accurate information and to encourage physical activity. Back straining activities were appraised and special movements required at the patient’s work were trained if necessary. No more than five exercises for improving the function of deep abdominal muscles and establishing symmetric use of the back. Other daily exercises were planned feasible enough for the patient to commit to and execute them. The aim was to increase body control and exercising in everyday life. Feedback to the patient’s GP included recommendations on further diagnostic tests, treatment, work, and sick leave. The GP at the patient’s local health care center subsequently coordinated the recommended treatment in his/her usual manner at the health care centre. Intervention 2: Work Site Visit Group (B). Identical to mini‐intervention plus a visit of the physiotherapist to the patient’s work site. The patient’s work supervisor and company nurse, physiotherapist, and physician were asked to join in the session to ensure that the patient had adapted to the information and practical instructions of appropriate ways of using the back at work and to encourage their cooperation. Control: usual care group received a leaflet on back pain and were treated by their GP in the usual manner | |
| Outcomes | Measurement at 1 and 2 year after randomization: back pain related sick leave | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | research nurse randomized each patient into 1 out of 3 study groups using four piles of sealed envelopes. the randomization was done in blocks of 15. |
| Allocation concealment (selection bias) | Low risk | a biostatistician had prepared the order from a random number table. A secretary unconnected with the patients had numbered the envelopes sequentially to prevent their rearrangement. Research nurse and researchers were not aware of block size and therefore could not predict the group assignments |
| Blinding (performance bias and detection bias) | Low risk | was not aware |
| Blinding (performance bias and detection bias) | Low risk | until the end of intervention at the FIOH. The work site visit made the difference at the end |
| Blinding (performance bias and detection bias) | Low risk | until the end of intervention at the FIOH. The work site visit made the difference at the end |
| Incomplete outcome data (attrition bias) | Low risk | 1 dropout |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | nu suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences at baseline |
| Co‐interventions avoided or similar? | High risk | control group were free to go seek help and went to more physiotherapists and spent more money on diagnostic tests |
| Compliance acceptable? | Low risk | high follow‐up percentages (94‐100%) in each group |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 3,6,12 months |
| Methods | RCT | |
| Participants | 174 workers with subacute LBP and sick leave of > 6 weeks in last half year. mean age 42, 79% male | |
| Interventions | Intervention: Function‐Centered Treatment for 6 days a week for 3 weeks. The FCT was based on work hardening and functional restoration programmes. Treatment activities were chosen based on a patient’s required capacities, as identified in the work‐related assessment. Treatment consisted of work simulation, strength and endurance training through isokinetic exercise, cardiovascular training performed by walking and aqua‐aerobics, sports therapy, and self‐exercise. Patients were told that increasing activity might cause more pain because the body had to adjust to the activity again. All team members emphasized that patients should continue therapeutic activities even if their pain increased. The treatment protocol did not contain massage, hot packs, and other passive treatments because we did not believe that they facilitate an increase in activity and self‐efficacy, nor has the research literature shown them to be effective. Control: Pain‐Centered Treatment. The primary goal in the PCT group was to reduce pain. The secondary goal was to increase strength and decrease disability. The physical therapist examined the patients to identify painful movements and limitations in mobility, strength, and muscle length in the lumbar region and lower extremities. Treatment was for 2.5 hours a day and consisted of individually selected passive and active mobilization, stretching, strength training, and a mini back school. Unlike with the FCT group, patients in the PCT group were told to stop activities when pain increased. Passive pain modulating treatments such as hot packs, electrotherapy, or massage were used daily. Low‐intensity movement therapy in the pool and progressive muscle relaxation further enhanced relaxation. Progressive muscle relaxation used systematic contraction and relaxation of specific muscle groups. Patients were encouraged to incorporate relaxation techniques into daily living as a coping skill to reduce stress, muscle tension, and pain. | |
| Outcomes | Measured at 1 year after treatment: number of calender work days, the rate of patients receiving unemployment benefits or permanent benefits. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | an independent and blinded research assistant performed concealed randomisation within these 4 strata using a randomisation schedule with blocks of 2 generated on a computer by an independent researcher |
| Allocation concealment (selection bias) | Low risk | see above |
| Blinding (performance bias and detection bias) | Low risk | days at work and other work‐related outcomes were assessed with a questionnaire sent to employers and the patients' primary physicians, who were blinded to the patients' group assignment |
| Blinding (performance bias and detection bias) | High risk | patients aware intervention content, but not of other treatment |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 1 dropout |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no such suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | High risk | subjects used other health care providers between 3 and 12 months |
| Compliance acceptable? | Low risk | all patients attended at least 90% of the scheduled treatments |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up post treatment and at 3 months |
| Methods | RCT | |
| Participants | 134 adults aged 18‐65 years sick listed for at least 12 weeks owing to low back pain | |
| Interventions | Integrated care: consisted of a workplace intervention based on participatory ergonomics, involving a supervisor, and a graded activity programme based on cognitive behavioural principles. Coordination was done by a clinical occupational physician. Usual care: Usual treatment by medical specialist, occupational physician, general practitioner and/or allied health professional | |
| Outcomes | return‐to‐work defined as duration of sick leave due to low back pain in calendar days from the day of randomisation until full return‐to‐work in own or other work with equal earnings for at least four weeks without recurrence, partial or full. Measured at 3,6,9, and 12 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomization of four allocations, using a computer generated random sequence table |
| Allocation concealment (selection bias) | Low risk | For every stratum, an independent statistician carried out the block randomization. A research assistant prepared opaque, sequentially numbered and sealed coded envelopes for each stratum, containing a referral for either the integrated care group or the usual care group. |
| Blinding (performance bias and detection bias) | Low risk | All patients received a code according to which a research assistant entered all data in the computer. This ensured blinded analysis of the data by the researcher. |
| Blinding (performance bias and detection bias) | High risk | Patients were not blinded for treatment allocation |
| Blinding (performance bias and detection bias) | High risk | Care providers were also not blinded |
| Incomplete outcome data (attrition bias) | Low risk | 7% loss to follow‐up |
| Incomplete outcome data (attrition bias) | Low risk | intention‐to‐treat (ITT) analysis |
| Selective reporting (reporting bias) | Low risk | No suggestion found |
| Similarity of baseline characteristics? | Low risk | No significant differences at baseline. |
| Co‐interventions avoided or similar? | High risk | More co‐interventions in the control group. |
| Compliance acceptable? | Unclear risk | 5 participants did not participate in the integrated care interention. 12 participants received only two elements of the integrated care. |
| Timing of the outcome assessment similar? | Low risk | Yes, at 3, 6, 9, and 12 months follow up |
| Methods | RCT | |
| Participants | 103 patients (71 males and 32 females), aged between 19‐64 years, sick listed for at least 6 weeks because of any low‐back pain diagnosis. | |
| Interventions | Intervention 1 : the graded activity programme consisted of: 1. Measurement of functional capacity,including mobility strength and fitness. 2. A work place visit, 3. back school education 4. 5. Individual, submaximal, gradually increased, exercise programme, with an operant conditioning behavioural approach. The operant conditioning method was aimed to teach the patients that it was safe to move while regaining function (N = 51). Programme duration: three times per week until return‐to‐work was achieved. Intervention 2 = CAU: traditional care recommended by their physicians, general rest, analgesics and prescription of unspecific physical treatment modalities(n = 52). | |
| Outcomes | Measurement at 1 and 2 years after randomisation. mean days of sick leave | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | block randomisation procedure |
| Allocation concealment (selection bias) | High risk | does not state |
| Blinding (performance bias and detection bias) | Low risk | assessors blind to sick leave data until conclusion of study |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 2 out of 51 dropped out of activity group, 3 out of 52 dropped out of control group |
| Incomplete outcome data (attrition bias) | Unclear risk | does not state |
| Selective reporting (reporting bias) | Low risk | no suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | High risk | control group were not prevented from getting information from intervention programme, and traditional care was given to them which could include anything |
| Compliance acceptable? | Low risk | 96% of patients followed interventions |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 12 months |
| Methods | RCT; cluster randomisation design was used by the generation of 50 random numbers by a computer, each number being placed in a sealed envelope | |
| Participants | 104 (62 males and 42 females), aged between 18‐65 years, with thoracic or lumbar pain incurred at work, not working or on suitable duties for more than 6 weeks | |
| Interventions | Clinical intervention/full intervention Intervention 1 (CI): Clinical intervention: after 8 weeks of absence included a visit to a back pain specialist and a school for back care education and after 12 weeks absence a multidisciplinary work rehabilitation intervention (functional rehabilitation therapy) was proposed that included fitness development and work hardening with cognitive‐behavioural approach. The programme ended with a progressive return‐to‐work (therapeutic return‐to‐work), that consisted of alternating days at the original job and days receiving functional therapy (N = 31). Programme duration: twelve months from the initial absence from work. Intervention 2 (FI): Full intervention: Clinical and occupational intervention combined. Occupational intervention (OI): (after 6 weeks of absence from work) included visits to an occupational physician (who could recommend investigation or treatment or set up light duties to help patient RTW) and a participatory ergonomic evaluation conducted by an ergonomist (to determine the need for job modifications). After observation of the worker's tasks, a meeting between ergonomist, injured worker, supervisor, management and union representatives was organised to come up with a "specific" ergonomic diagnosis and precise solutions to improve the work site to be presented to management (n = 25).Programme duration: twelve months from the initial absence from work. Clinical intervention/unspecified intervention Intervention 1 (CI): Clinical intervention: after 8 weeks of absence included a visit to a back pain specialist and a school for back care education and after 12 weeks absence a multidisciplinary work rehabilitation intervention (functional rehabilitation therapy) was proposed that included fitness development and work hardening with cognitive‐behavioural approach. The programme ended with a progressive return‐to‐work (therapeutic return‐to‐work), that consisted of alternating days at the original job and days receiving functional therapy (n = 31). Programme duration: 12 months from the initial absence from work. Intervention 2 (UC): patients in this group received care from their attending physician who was free to prescribe any test, treatment or specialist referral (n = 26) | |
| Outcomes | Measurement at 12 months after enrolment: Number days out of regular work; Number of days out of all work; Functional status (Oswestry questionnaire); Pain Level (McGill‐Melzack questionnaire) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | cluster randomisation on workplace; random number generated by computer |
| Allocation concealment (selection bias) | Low risk | random numbers generated by computer and sealed envelopes |
| Blinding (performance bias and detection bias) | Low risk | assessor blinded to subjects randomisation status |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 9% did not respond to follow‐up visit |
| Incomplete outcome data (attrition bias) | High risk | those 9% were not included in analysis |
| Selective reporting (reporting bias) | Low risk | no suggestions found |
| Similarity of baseline characteristics? | High risk | not for age, comorbidity frequency, % women |
| Co‐interventions avoided or similar? | High risk | all groups were free to seek additional treatment in the community |
| Compliance acceptable? | Unclear risk | does not state adherence to protocol |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 4 weeks accumulated absence from work, and at 1 year after initial absence from work |
| Methods | RCT | |
| Participants | 33 workers with chronic non‐specific musculoskeletal disorders with sick leave of at least 2 months or 50% work incapacity from a full‐time job over 3 months. mean age 43 years, 70% male | |
| Interventions | Intervention: called work rehabilitation programme, lasted 8 weeks, 3.5 hours per day, 5 days per week. The work rehabilitation programme aimed to increase functional capacity and improve the patient’s self‐efficacy using an operant behavioural therapy approach. The approach was interdisciplinary and involved rehabilitation physicians, a psychologist, a social worker, occupational and physiotherapists. Every patient had a therapist as a case manager to ensure that goals of the rehabilitation are adapted weekly and coordination between all members in the interdisciplinary team were guaranteed. The programme contained work‐specific exercises, progressive exercise therapy with training devices, education in ergonomics, learning strategies to cope with pain and to increase self‐efficacy, a group intervention with the psychologist, sports activities for recreation and a workplace visit to develop appropriate workload related exercises for the programme [24?26]. The uptake of work was designed to be gradual and started 4 weeks after the programme began. Control: The physician who referred the patient to the hospital administered the control treatment, called progressive exercise therapy. This physician had received specific recommendations concerning work reintegration, medication and training. 3 times a week for 8 weeks progressive exercises in a physiotherapy practice. | |
| Outcomes | Measured at 8 weeks post‐rehabilitation: The ability to work in % of a full‐time job, and the actual performed work status in % of a full‐time job | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | an independent person conducted random allocation by using a minimization procedure and a random number table. After the patients inclusion, a concealed letter concerning the result of the randomisation was given to the therapist to allocated the patient to the respective group. |
| Allocation concealment (selection bias) | Low risk | see above |
| Blinding (performance bias and detection bias) | Low risk | assessor was blinded regarding treatment allocation |
| Blinding (performance bias and detection bias) | Low risk | patients knew about the common aim of the study and control treatment, namely the return‐to‐work, but were blinded concerning the two treatments. This meant they were told that they would undergo a fitness programme, but did not know what the exact content of the two treatments was until they started the treatment. |
| Blinding (performance bias and detection bias) | High risk | provider was aware of treatment allocation |
| Incomplete outcome data (attrition bias) | Low risk | 2 dropouts |
| Incomplete outcome data (attrition bias) | Low risk | according to author |
| Selective reporting (reporting bias) | Low risk | no suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | Low risk | none of the intervention groups received co‐interventions |
| Compliance acceptable? | Low risk | page 70 |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 8 weeks post rehab assessment and at 32 weeks |
| Methods | RCT | |
| Participants | 542 patients (386 males and 156 females), age not stated, with chronic pain caused by low back injury for at least 90 days, with or without radiating pain and off work. | |
| Interventions | Intervention: functional restoration programme consisting of an active exercise programme (sports medicine approach). The programme had two parts, physical exercise and functional simulation programme developed in an occupational gymnasium. Circuit equipment used in this exercise component was designed to work specific muscle groups in sequence to diminish fatigue and to achieve mobility and strengthening of various muscle groups. Work related tasks included were: lifting station, working above head board, stair‐climbing, carrying weights and lifting while twisting. In addition, behavioural and cognitive therapy was included which consisted of education classes, relaxation therapy, biofeedback, individual and group counselling (n = 271). Programme duration: 8 to 12 weeks (40 treatment days ‐ seven hours per day, five days per week). Control: CAU: medical management left entirely in the hands of the GP and included a wide range of treatment methods such as physiotherapy, medication, manipulation, acupuncture, work hardening, back schools, and active exercise programmes using the sports medicine approach (n = 271). | |
| Outcomes | Measurement at 12 months after the treatment. 1. Return to full time work; 2. Cost per workers' compensation claim; 3. Days lost from work | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | does not state |
| Allocation concealment (selection bias) | Unclear risk | does not state |
| Blinding (performance bias and detection bias) | Unclear risk | does not state who was outcome assessor and he was blinded |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | High risk | does not state dropout rate |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis reported |
| Selective reporting (reporting bias) | Low risk | no such suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | High risk | control group could use any consultant of facility that existed in the community |
| Compliance acceptable? | Unclear risk | does not state |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up monthly for 12 months in relation to RTW |
| Methods | RCT | |
| Participants | 132 workers with chronic low‐back pain and on sick leave or at risk of work disability for more than 3 months. Mean age 39.8, 65.1% men | |
| Interventions | Intervention: Functional restoration programme: 5 weeks, 6 hrs a day The group performed exercises supervised by a physiotherapist who adjusted the exercise intensity to each participant every week. Patients performed work simulations during occupational therapy sessions. They were referred to the psychologist at least once in the first week and for further treatment if requested. Dietary advice was given. The schedule of interventions was standardized for all patients. Control: Active individual therapy: 5 weeks 3x1 hr a week. only active exercises supervised directly by the physiotherapist. The last week focused on functional exercises and endurance training. The programme included 50 minutes of individual home exercises 2 days a week (these could include stretching, jogging, and swimming). In both groups, patients were off work during the 5 weeks of treatment. | |
| Outcomes | Measurement directly after treatment: % self perceived ability to return to work, % return‐to‐work, % full‐time return‐to‐work | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | block randomisation using an 8 element permutation table |
| Allocation concealment (selection bias) | High risk | according to author |
| Blinding (performance bias and detection bias) | High risk | according to author |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | return‐to‐work data missing on 1 subject from each group |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no such suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | Unclear risk | according do author |
| Compliance acceptable? | Unclear risk | according to author |
| Timing of the outcome assessment similar? | Low risk | all subjects assessed at the end of treatment period of 5 weeks |
| Methods | RCT | |
| Participants | 211 chronic low‐back pain patients of which 90% were on sick leave and 10% had been sick listed at least 2 months per year for last 2 years. Mean age 43.5, % male 35 | |
| Interventions | Intervention: light multidisciplinary treatment consisting of 3‐4 hours of evaluation, consultation and lecture at the start of intervention period with encouragement to gradually increase activity level. Topics were exercise, lifestyle, and fear avoidance. Intervention: extensive multidisciplinary treatment consisting of 4 wks of 6 hr per day group sessions with education, exercises, and occasional workplace interventions. | |
| Outcomes | Measurement after 12, 18 and 24 months after treatment: information on sick leave status via National Health Insurance | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | random by means of a sequence of pre‐labelled cards contained in sealed envelopes; block randomisation |
| Allocation concealment (selection bias) | Low risk | prepared beforehand by physician outside clinic |
| Blinding (performance bias and detection bias) | Low risk | data from national health insurance register |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 3 patients dropped out (out of 195) |
| Incomplete outcome data (attrition bias) | Low risk | all subjects analysed (in terms of return‐to‐work) in the group to which they were allocated |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | only age and gender provided |
| Co‐interventions avoided or similar? | Low risk | control group could seek other medical advice via GP |
| Compliance acceptable? | Low risk | only 3 patients did not comply with treatment programme |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up once a month during the 26 follow‐up period |
| Methods | RCT | |
| Participants | 134 employees from Schiphol Airport in the Netherlands with low‐back pain of at least 4 weeks. mean age of 38 and 94% men: 67 in intervention group, 67 in control group; all workers were on full or partial sick leave between 6‐14 weeks. | |
| Interventions | Intervention: Graded activity intervention supervised by a physiotherapist along with usual guidance from the OP about work‐related problems and barriers to return to work. Including: physical examination, 1 hour exercise twice a week until complete RTW or 3 months, both generally and individually tailored exercises, proposal of a date for full return‐to‐work, modified hours and duties with a gradually increasing quota of exercises, time‐contingent management Control: care as usual being usual guidance and advice from occupational health physician | |
| Outcomes | Measurement at 100 days and 1 year after randomisation: total number of days absent from work because of low‐back pain. Full return‐to‐work was defined as any full return to regular work with a minimum duration of 4 weeks. After 3 years numbers of workers that were still disabled for work. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | block randomisation after pre stratification for the organizational unit in the workplace from which they were recruited and for the severity of pain symptoms |
| Allocation concealment (selection bias) | Low risk | group allocation in sealed envelopes |
| Blinding (performance bias and detection bias) | Low risk | outcome assessor not aware |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 13 withdrawals of which 3 did not adhere to intervention protocol. 10% dropout |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no such suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences |
| Co‐interventions avoided or similar? | Low risk | no co‐interventions noted. In usual care subjects were allowed to seek any sort of intervention |
| Compliance acceptable? | Low risk | yes, only 3 did not adhere to protocol |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 3 and 6 months post‐randomisation and continuously (days away from work) |
| Methods | RCT | |
| Participants | 112 workers from the Netherlands with low‐back pain. mean age 42 years, 41% men. On sick leave for more than 8 weeks. 55 workers intervention group, 57 workers control group. | |
| Interventions | Intervention: Graded activity programme consisting of 26 one‐hour sessions maximally, with a frequency of two sessions a week. The first session took half an hour more since taking the patients history and a physical examination were part of this session. The programme ended as soon as a full RTW had been established, according to an earlier agreed upon individual schedule . During the programme the worker had an active role in RTW and the physiotherapist (PT) acted as a coach and supervisor, using a hands‐off approach. Control: care as usual including usual guidance by the occupational health physician | |
| Outcomes | Measurement at 6 months and 1 year after first day of sick leave: lasting return to own or equal work, calculated as duration of work absenteeism in calender days from the first day of sick leave to full RTW | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | an independent researcher performed randomisation using a list of random numbers |
| Allocation concealment (selection bias) | Low risk | |
| Blinding (performance bias and detection bias) | Low risk | information from first author: data from automated databases, rest of data from questionnaires |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | all subjects included in follow‐up analysis |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis reported |
| Selective reporting (reporting bias) | Low risk | yes, no suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences |
| Co‐interventions avoided or similar? | Low risk | workers could seek other help e.g. physio, manual therapy, chiropractor, neurologist, orthopedic surgeon |
| Compliance acceptable? | High risk | 19 out of 55 = 35% from graded activity group did not comply |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up for primary outcome during first 12 months (continuously), secondary outcomes at 12, 26 and 52 weeks post‐treatment |
| Methods | RCT | |
| Participants | 93 workers from Local Insurance Offices, and from 2 GPs with LBP and sick listed between 8‐12 weeks. Mean age 41, 48% male. 34 in Cognitive group, 30 in Exercise group, 29 in Control group | |
| Interventions | Both interventions: Routine back examination, X‐rays and CTscans and general encouragement to resume daily activities and work. Intervention 1: Intensive group training: 15 weeks of 2‐3 times a week1 hour exercise, following the Norwegian Aerobic Fitness Model, which is based on both exercise physiology and ergonomic principles, and designed to increase overall fitness and functional capacity. A physical therapist led the programme with focus on ergonomic principles and functional tasks, no pain focus, it is safe to move focus, the whole programme is accompanied by music. Intervention 2: cognitive intervention: 2 consultations between 30‐60 minutes. Including:explanation of pain mechanisms, questionnaire discussion, functional examination with individual feedback and advice, instruction in activation of deep stabilizing muscles and advice on how to use it actively in functional and demanding tasks of daily life, Instruction in the squat technique when lifting is required, How to cope with new attacks, Reassure and emphasize that it is safe to move, 2 consultations 30‐60 minutes. Control: Treated by their GP with to restrictions of treatments or referrals | |
| Outcomes | Measurement at 18 weeks after inclusion: mean days of sick leave | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization was conducted by an engineer working at the hospital who was not involved in the trial. Codes were kept locked in the engineers office. Sealed opaque envelope were handed to workers. |
| Allocation concealment (selection bias) | Low risk | subjects drew sealed envelopes with disclosure of randomisation |
| Blinding (performance bias and detection bias) | Low risk | data collected from data registry and self reported questionnaires |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | Described: 18% loss of patients to follow‐up. Dropout was higher in exercise group. |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no suggestion found |
| Similarity of baseline characteristics? | Low risk | No differences between groups, except a shorter mean time since first LBP episode for the control group |
| Co‐interventions avoided or similar? | Unclear risk | Not clear what control group used for co‐interventions |
| Compliance acceptable? | Low risk | 17 people dropped out (2 from cognitive, 9 from exercise and 6 from control group). Mean adherence to group training classes was 80.4% for people who didn't dropout. One fifth of people in cognitive group came back for more than the 2 recommended consultations. |
| Timing of the outcome assessment similar? | Low risk | yes, all subjects followed up 18 weeks after inclusion |
| Methods | RCT | |
| Participants | 138 workers with back pain. Selected from a rehabilitation centre from the Netherlands. 67% had chronic back pain, 28% subacute back pain. Sick leave between 7.4‐10 weeks. | |
| Interventions | GAPS: graded activity programme and group education with cognitive behavioural therapy focusing on problem solving. GAGE: graded activity programme and group education | |
| Outcomes | Measurement at 6 months and 1 year after treatment: number of workers with 100% return‐to‐work; number of workers with part‐time return‐to‐work; number of workers with no return‐to‐work; mean days of sick leave first half year and mean days of sick leave second half year after treatment | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | randomisation scheme was computer generated, and only known by logistics planner of the rehabilitation centre |
| Allocation concealment (selection bias) | Low risk | see above |
| Blinding (performance bias and detection bias) | Low risk | researchers obtaining data from data bases were blinded to group allocation |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 108 workers randomized; 84 followed up; 22% dropout |
| Incomplete outcome data (attrition bias) | Unclear risk | no clear information found, looks like PP analysis |
| Selective reporting (reporting bias) | Low risk | no such suggestion found |
| Similarity of baseline characteristics? | Low risk | except for RDQ scores and treatment credibility |
| Co‐interventions avoided or similar? | Unclear risk | does not state whether subjects attended other care providers between end of treatment and follow‐up |
| Compliance acceptable? | Unclear risk | 31 of 108 dropped out before start of treatment, another 8 dropped out between treatment and follow up. It does not mention compliance (adherence) to treatment protocol for those that didn't dropout |
| Timing of the outcome assessment similar? | Low risk | both groups measured pre‐treatment and 6, 12 months after treatment stop |
| Methods | RCT | |
| Participants | 80 workers with acute or subacute back pain. Median time off work 20 days, mean age 41, 21% women. 43 workers in intervention and 37 in control group | |
| Interventions | Intervention: Back book + simple, practical advise on how to modify physical activities specific to the individual’s work situation + one treatment from senior physiotherapist depending on assessment findings + 3x1 hr group exercises for 2 weeks Control: back book + GP + additionally, simple, practical advise on how to modify physical activities specific to the individuals work situation was discussed | |
| Outcomes | Measured at 2 months after study entry: rate of return‐to‐work, average number of days off work, light duties at study entry (were not included for analysis), percentage of patients changing from light duties to full duties | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | using a computer programme |
| Allocation concealment (selection bias) | Low risk | a sealed envelope containing the randomized group number was given to the patient to open |
| Blinding (performance bias and detection bias) | Unclear risk | does not state who is assessor and if blinded |
| Blinding (performance bias and detection bias) | High risk | patients aware of allocation and intervention content |
| Blinding (performance bias and detection bias) | High risk | care providers aware of allocation and intervention content |
| Incomplete outcome data (attrition bias) | Low risk | 10 out of 56 dropped out in group 1 and 5 out of 50 in group 2 |
| Incomplete outcome data (attrition bias) | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Low risk | no such suggestions found |
| Similarity of baseline characteristics? | Low risk | no significant differences found |
| Co‐interventions avoided or similar? | High risk | control group could seek other interventions via GP |
| Compliance acceptable? | Unclear risk | does not state |
| Timing of the outcome assessment similar? | Low risk | all subjects followed up at 1 and 2 months |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| no stated relationship between intervention and functional job demands | |
| no stated relationship between intervention and functional job demands | |
| no stated relationship between intervention and functional job demands | |
| physical conditioning was not a structural part of the intervention | |
| outcome measure was not sickness absence | |
| no stated relationship between intervention and functional job demands | |
| no stated relationship between intervention and functional job demands | |
| no stated relationship between intervention and functional job demands | |
| no stated relationship between intervention and functional job demands | |
| no stated relationship between intervention and functional job demands | |
| No existing work disability or sickness absence at baseline | |
| no stated relationship between intervention and functional job demands | |
| no stated relationship between intervention and functional job demands | |
| no stated relationship between intervention and functional job demands | |
| at baseline majority of participants were not on sickleave | |
| outcome measure was not related to sickness absence or return‐to‐work | |
| no stated relationship between intervention and functional job demands | |
| no stated relationship between intervention and functional job demands | |
| at baseline majority of participants were not on sickleave |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Not yet assessed |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Not yet assessed |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Not yet assessed |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion off work Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 Light physical conditioning programme (PCP) + backbook versus backbook intervention only, acute pain, Outcome 1 Proportion off work. | ||||
| 1.1 3 months fu | 1 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work long term follow up Show forest plot | 1 | 190 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.30, 0.27] |
| Analysis 2.1  Comparison 2 Light physical conditioning programme (PCP) versus care as usual (CaU), acute pain, Outcome 1 Time to return to work long term follow up. | ||||
| 1.1 12 months fu | 1 | 190 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.30, 0.27] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion off work long term follow up Show forest plot | 1 | 70 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.05, 1.06] |
| Analysis 3.1  Comparison 3 Intense physical conditioning programme (PCP) versus care as usual (CaU), acute pain, Outcome 1 Proportion off work long term follow up. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.1  Comparison 4 Light physical conditioning programme (PCP) + care as usual (CaU) versus CaU, subacute pain, Outcome 1 Time to return to work. | ||||
| 1.1 6 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 12 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 24 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 1 | 351 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.21 [0.00, 0.42] |
| Analysis 5.1  Comparison 5 Light physical conditioning programme (PCP) + brief clinical intervention (CI) versus brief CI only, subacute pain, Outcome 1 Time to return to work. | ||||
| 1.1 12 months fu | 1 | 351 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.21 [0.00, 0.42] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 5 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 6.1  Comparison 6 Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, subacute pain, Outcome 1 Time to return to work. | ||||
| 1.1 6 months fu | 3 | 447 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.22, 0.15] |
| 1.2 12 months fu | 4 | 395 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.39, 0.01] |
| 2 Time to return to work very long term follow up Show forest plot | 2 | Std. Mean Difference (Fixed, 95% CI) | ‐0.39 [‐0.76, ‐0.02] | |
| Analysis 6.2  Comparison 6 Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, subacute pain, Outcome 2 Time to return to work very long term follow up. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 7.1  Comparison 7 Intense physical conditioning programme (PCP) versus light PCP, subacute pain, Outcome 1 Time to return to work. | ||||
| 1.1 6 months fu | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work short term follow up Show forest plot | 1 | 64 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.59, 0.40] |
| Analysis 8.1  Comparison 8 Intense physical conditioning programme (PCP) versus cognitive intervention, subacute pain, Outcome 1 Time to return to work short term follow up. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐7.20 [‐43.64, 29.24] |
| Analysis 9.1  Comparison 9 Intense physical conditioning programme (PCP) versus care as usual (CaU), subacute pain, Outcome 1 Time to return to work. | ||||
| 1.1 3 months fu | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐7.20 [‐43.64, 29.24] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion off work short term follow up Show forest plot | 2 | 623 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.42, 0.80] |
| Analysis 10.1  Comparison 10 Intense physical conditioning programme (PCP) versus multidisciplinary exercise treatment, subacute pain, Outcome 1 Proportion off work short term follow up. | ||||
| 1.1 3 months fu | 1 | 173 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.22, 0.78] |
| 1.2 6 months fu | 1 | 149 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.38, 1.38] |
| 1.3 12 months fu | 2 | 301 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.40, 0.99] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 11.1  Comparison 11 Light physical conditioning programme (PCP) versus care as usual (CaU), chronic pain, Outcome 1 Time to return to work. | ||||
| 1.1 12 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 24 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to Return to Work Show forest plot | 1 | Std. Mean Difference (Fixed, 95% CI) | ‐4.42 [‐5.06, ‐3.79] | |
| Analysis 12.1  Comparison 12 Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, chronic pain, Outcome 1 Time to Return to Work. | ||||
| 1.1 12 months fu | 1 | Std. Mean Difference (Fixed, 95% CI) | ‐4.42 [‐5.06, ‐3.79] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 5 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| Analysis 13.1  Comparison 13 Intense physical conditioning programme (PCP) versus care as usual (CaU), chronic pain, Outcome 1 Time to return to work. | ||||
| 1.1 3 months fu | 1 | Std. Mean Difference (Random, 95% CI) | ‐1.01 [‐2.11, 0.09] | |
| 1.2 12 months fu | 5 | Std. Mean Difference (Random, 95% CI) | ‐0.23 [‐0.42, ‐0.03] | |
| 1.3 24 months fu | 3 | Std. Mean Difference (Random, 95% CI) | ‐0.26 [‐0.61, 0.10] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion off work short term follow up Show forest plot | 1 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.37, 2.70] |
| Analysis 14.1  Comparison 14 Intense physical conditioning programme (PCP) versus exercise program, chronic pain, Outcome 1 Proportion off work short term follow up. | ||||
| 2 Time to return to work Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 14.2  Comparison 14 Intense physical conditioning programme (PCP) versus exercise program, chronic pain, Outcome 2 Time to return to work. | ||||
| 2.1 6 months fu | 2 | 114 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.63, 0.24] |
| 2.2 12 months fu | 3 | 256 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.96, 0.04] |
| 2.3 24 months fu | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐1.21, ‐0.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 3 | Std. Mean Difference (Fixed, 95% CI) | Subtotals only | |
| Analysis 15.1  Comparison 15 Intense physical conditioning programme (PCP) versus intense PCP + cognitive behavioural therapy (CBT), chronic pain, Outcome 1 Time to return to work. | ||||
| 1.1 6 months fu | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.26 [‐0.50, 1.03] | |
| 1.2 12 months fu | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.05 [‐0.30, 0.40] | |
| 1.3 24 months fu | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.19 [‐0.18, 0.56] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 2 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| Analysis 16.1  Comparison 16 Intense physical conditioning programme (PCP) versus cognitive behavioural therapy (CBT) for workers with chronic back pain, Outcome 1 Time to return to work. | ||||
| 1.1 12 months fu | 2 | Std. Mean Difference (Random, 95% CI) | ‐1.75 [‐4.45, 0.95] | |
| 1.2 24 months fu | 2 | Std. Mean Difference (Random, 95% CI) | ‐0.47 [‐1.36, 0.42] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 17.1  Comparison 17 Intense physical conditioning programme (PCP) versus light PCP, chronic back pain, Outcome 1 Time to return to work. | ||||
| 1.1 12 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 24 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
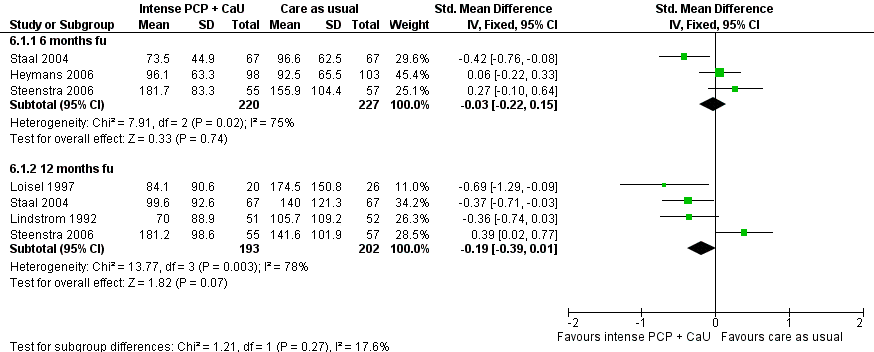
Forest plot of comparison: 7 Intense PC + CaU versus CaU only, subacute pain, outcome: 7.3 Time to return‐to‐work.
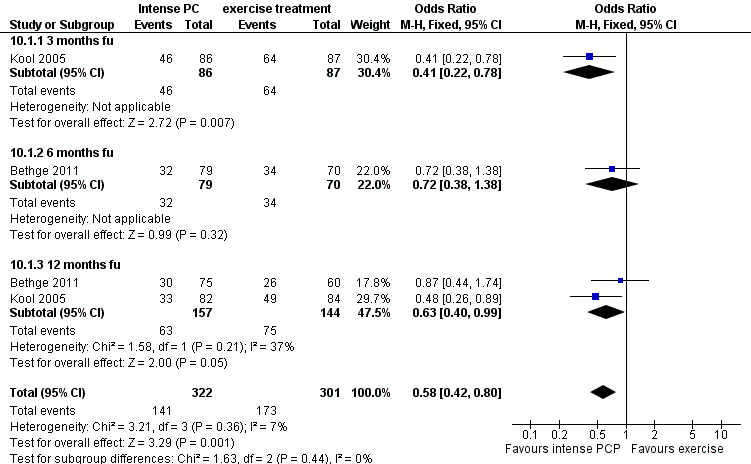
Forest plot of comparison: 11 Intense PC versus multidisciplinary exercise treatment, subacute pain, outcome: 11.1 Proportion off work short‐term follow‐up.
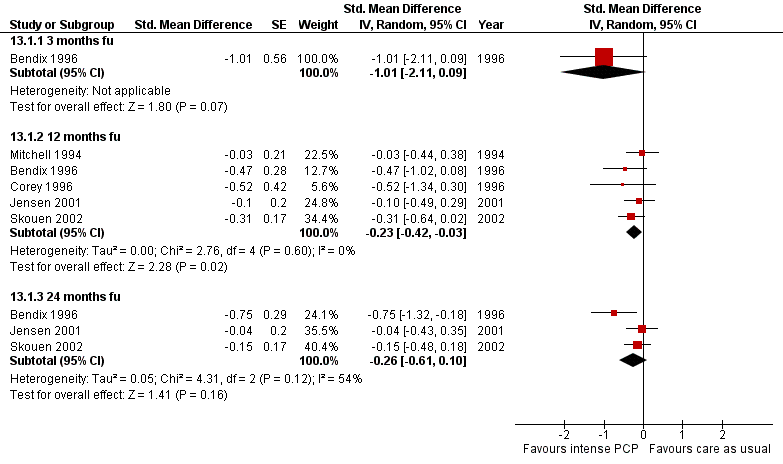
Forest plot of comparison: Intense PCP versus care as usual for workers with chronic back pain, outcome: Time to return‐to‐work at long‐term follow‐up

Forest plot of comparison: Intense PCP versus exercise programme for workers with chronic back pain, outcome: Time to return‐to‐work at intermediate‐term follow‐up.
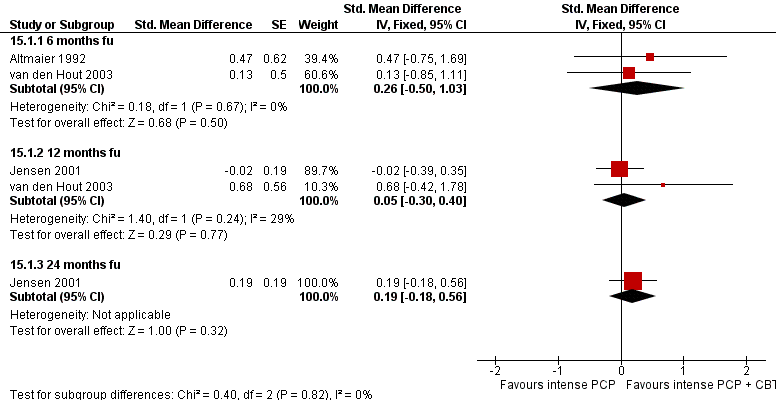
Forest plot of comparison: Intense PCP versus intense PCP with CBT for workers with chronic back pain, outcome: Time to return‐to‐work at long‐term follow‐up.
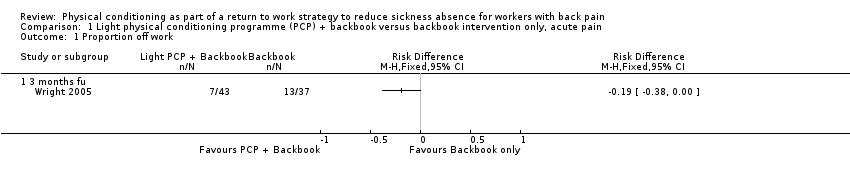
Comparison 1 Light physical conditioning programme (PCP) + backbook versus backbook intervention only, acute pain, Outcome 1 Proportion off work.

Comparison 2 Light physical conditioning programme (PCP) versus care as usual (CaU), acute pain, Outcome 1 Time to return to work long term follow up.

Comparison 3 Intense physical conditioning programme (PCP) versus care as usual (CaU), acute pain, Outcome 1 Proportion off work long term follow up.
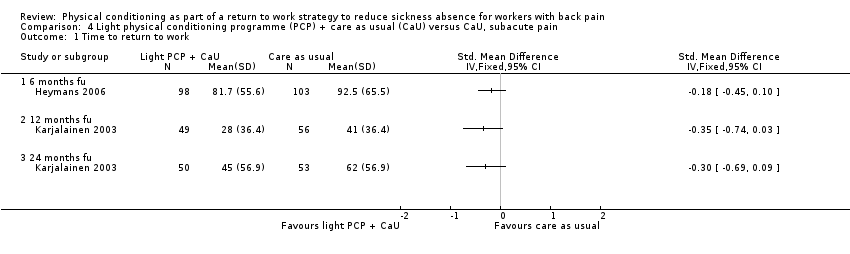
Comparison 4 Light physical conditioning programme (PCP) + care as usual (CaU) versus CaU, subacute pain, Outcome 1 Time to return to work.

Comparison 5 Light physical conditioning programme (PCP) + brief clinical intervention (CI) versus brief CI only, subacute pain, Outcome 1 Time to return to work.

Comparison 6 Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, subacute pain, Outcome 1 Time to return to work.
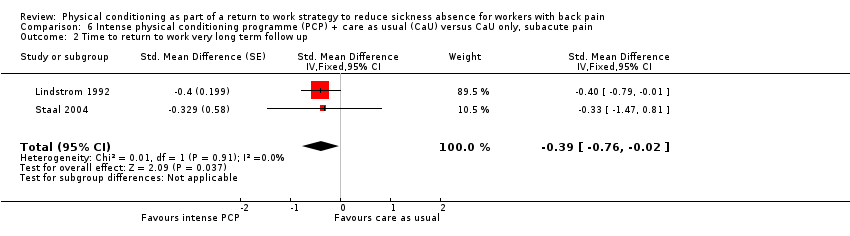
Comparison 6 Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, subacute pain, Outcome 2 Time to return to work very long term follow up.

Comparison 7 Intense physical conditioning programme (PCP) versus light PCP, subacute pain, Outcome 1 Time to return to work.

Comparison 8 Intense physical conditioning programme (PCP) versus cognitive intervention, subacute pain, Outcome 1 Time to return to work short term follow up.

Comparison 9 Intense physical conditioning programme (PCP) versus care as usual (CaU), subacute pain, Outcome 1 Time to return to work.

Comparison 10 Intense physical conditioning programme (PCP) versus multidisciplinary exercise treatment, subacute pain, Outcome 1 Proportion off work short term follow up.

Comparison 11 Light physical conditioning programme (PCP) versus care as usual (CaU), chronic pain, Outcome 1 Time to return to work.

Comparison 12 Intense physical conditioning programme (PCP) + care as usual (CaU) versus CaU only, chronic pain, Outcome 1 Time to Return to Work.

Comparison 13 Intense physical conditioning programme (PCP) versus care as usual (CaU), chronic pain, Outcome 1 Time to return to work.

Comparison 14 Intense physical conditioning programme (PCP) versus exercise program, chronic pain, Outcome 1 Proportion off work short term follow up.
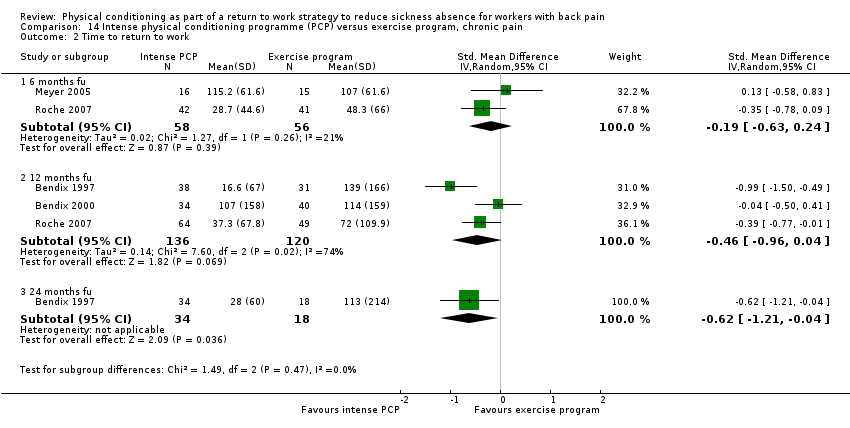
Comparison 14 Intense physical conditioning programme (PCP) versus exercise program, chronic pain, Outcome 2 Time to return to work.

Comparison 15 Intense physical conditioning programme (PCP) versus intense PCP + cognitive behavioural therapy (CBT), chronic pain, Outcome 1 Time to return to work.
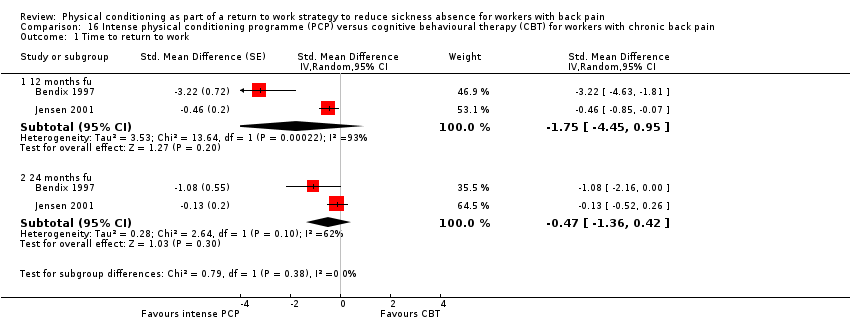
Comparison 16 Intense physical conditioning programme (PCP) versus cognitive behavioural therapy (CBT) for workers with chronic back pain, Outcome 1 Time to return to work.

Comparison 17 Intense physical conditioning programme (PCP) versus light PCP, chronic back pain, Outcome 1 Time to return to work.
| Time span of training | 5 wks | 4 wks | 18 weeks median duration | na | na | 2 wks |
| Number of sessions | 2 per week | 1 per week | after the interview, the participant was seen at least once, and four times on average | 2 | approx. 4 hrs at the start + 6 follow up or individual sessions over a period of 1 year | 1 examination + treatment initially then 3 per week |
| Length of sessions | 20 min | 120 min | 1‐2 hrs | 1‐1,5 hr | unclear | 1 hr |
| Full time | no | no | no | no | no | no |
| group or individual | individual | group | individual | individual | both | both |
| exercises | yes | yes | yes in advice | yes | yes, advice and programme | yes |
| work related exercises | yes | yes | yes in advice | yes | yes in advice | yes |
| operant conditioning behavioural approach | no | no | no | no, although intervention was based on graded activity programme | no | no |
| pain coping/ management | no | no | yes | no | no | no |
| back pain education | no | yes | yes | no | no | no |
| ergonomic advice or occupational training | no | yes | no | no | no | advice on how to modify physical activities specific to the individual's work situation |
| return‐to‐work advice | no | yes | yes | no | no | no |
| workplace visit | no | no | yes | yes | no (not for all individuals) | no |
| therapists involved | physiotherapist | physiotherapist, occupational physician | rehabilitation physician, specialist in clinical social medicine, physiotherapist, social worker, occupational therapist, case manager | physiotherapist, physician | physio therapist, nurse, psychologist | physiotherapist |
| other aspects | written compliance contract | CAU | brief clinical examination | CAU | no | CAU being a back book and advice on how to modify physical activities specific to the indivual's work situation |
| comparison | CAU | CAU/ intense PCP | brief clinical examination only | CAU | CAU / intense PCP | CAU being a back book and advice on how to modify physical activities specific to the individual's work situation ‐ only |
| Time span of training | 3 wks | 3 wks | 6 wks | 3 wks | 3 wks | 33 days | 3 wks | 8 wks |
| Number of sessions | 2 per day | 39 hrs per week + 3x6 hrs follow up | 135 hr in total | 39 hours per week + 3x6 hrs follow‐up | total of 82.2 hours of therapy | 6.5 hr per day | up to 41 | 2 per week |
| Length of sessions | ? | na | na | na | 1‐1.5 hrs | na | 15 min‐1hr | 1 hr |
| Full time | no | yes | yes | yes | yes | yes | no | no |
| group or individual | both | group | group | group | group | both | both | individual |
| exercises | yes | yes | yes | yes | yes | yes | yes | yes |
| work related exercises | yes | yes | yes | yes | yes | yes | yes | yes |
| operant conditioning behavioural approach | yes | yes | yes | yes | yes | yes | not clear | yes |
| pain coping/ management | yes | yes | yes | yes | unclear | yes | yes | no |
| back pain education | yes | yes | yes | yes | yes | yes | no | no |
| ergonomic advice or occupational training | no | occupational therapy and ergonomic training | occupational therapy and ergonomic training | occupational therapy and ergonomic training | no | no | occupational therapy | yes |
| return‐to‐work advice | no | no | no | no | yes | no | no | yes |
| workplace visit | no | no | no | no | no | no | no | no |
| therapists involved | multidisciplinary | multidisciplinary | multidisciplinary including physician, psychologist | occupational therapist, physician, psychologist,physical therapist, social worker | physician, social worker, psychologist, physical therapist | interdisciplinary programme | physiotherapist, occupational therapist, nurse, physician | physiotherapist |
| other aspects | vocational rehabilitation | recreation activities | aerobics, recreational activities | recreation activities | no | no | no | CAU |
| comparison | PCP + CBT | CAU | exercise therapy / pain management | outpatient intensive physical training | inpatient conventional musculoskeletal rehabilitation | CAU | CAU | CAU‐only/ light PCP |
| Time span of training | 4 wks | 3 wks | 12 wks | until RTW | 13 wks | 8 wks | 8 wks | 5 wks |
| Number of sessions | 6 sessions + 20 hrs exercise + 6 booster sessions | 4 hrs per day / 6 days a week | varying | approx. 11 with physical therapist, approx 10 self training sessions (3 per week) | 3,5 hr per day, 5 days a week | 6 hrs per day, 5 days a week | ||
| Lenght of sessions | ||||||||
| Full time | no | almost | no | no | unclear | almost | yes | yes |
| group or individual | both | group | individual | individual | unclear | both | group | group |
| exercises | yes | yes | yes | yes | yes | yes | yes | yes |
| work related exercises | yes | yes | yes | yes | yes | yes | yes | yes |
| operant conditioning behavioural approach | yes | no | yes | yes | yes | yes | yes | no |
| pain coping/ management | 2 didactic sessions on psychological aspects of pain + 2 sessions on medical aspects of pain | no | no | no | no | yes | no | no |
| back pain education | yes | no | no | yes | yes | no | yes | no |
| ergonomic advice or occupational training | 2 sessions on ergonomics | work simulation | yes | no | yes, participatory ergonomics evaluation | education in ergonomics | no | occupational therapy |
| return‐to‐work advice | yes, workplace visit + rehabilitation plan | no | yes | yes | yes | yes | no | no |
| workplace visit | yes | no | yes | yes | yes | yes | no | no |
| therapists involved | physician, physical therapist, psychologist, | rheumatologist, physical and occupational therapist, sports therapist, social worker, nurse | clinical occupational physician, medical specialist, physiotherapist | physical therapist | back pain specialist; multidisciplinary medical, ergonomic and rehabilitation staff | interdisciplinary:rehabilitation physicians, psychologist, social worker, occupational therapist, physiotherapist | unclear | specialist in physical medicine, physiotherapist, psychologist |
| other aspects | no | no | CAU | CAU | CAU | case‐manager recreational activities | no | no |
| comparison | CAU / CBT PCP + CBT | pain centred treatment | CAU‐only | CAU‐only | CAU‐only | exercise therapy | CAU | active individual therapy |
| Time span of training | 4 wks | max 3 months | 13 wks | 15 wks | 8 wks |
| Number of sessions | 5 per week for 4 weeks + follow‐up as in LMT | 2 per week until RTW | 2 per week 26 in total | 2‐3 per week | 28 |
| Lenght of sessions | 6 hr | 1 hr | 1 hr | 1 hr | 30‐90 min |
| Full time | almost | no | no | no | no |
| group or individual | both | individual | individual | group | both |
| exercises | yes | yes | yes | yes | yes |
| work related exercises | yes | yes | yes | not clear | yes |
| operant conditioning behavioural approach | yes | yes | yes | no | yes |
| pain/ coping management | no | no | no | no | no |
| back pain education | yes | no | no | no | yes |
| ergonomic advice or occupational training | yes | no | no | yes, training had a focus on ergonomic principles and functional tasks | yes, training by occupational therapist |
| return‐to‐work advice | no | yes | yes | no | yes |
| Workplace visit | no, occasional workplace intervention | no, but intervention was at workplace | no | no | yes, if necessary |
| therapists involved | physio therapist, nurse, psychologist | physiotherapist, occupational physician | physiotherapist, occupational physician | physical therapist | physiotherapist, occupational therapist, psychologist, occupational physician |
| other aspects | no | CAU/gradually increasing exercise, GP or occupational physician if workers wanted to | CAU/gradually increasing exercise | exercises accompanied by music | contact with patients' supervisor |
| comparison | CAU/ light PCP | CAU‐only | CAU‐only | CAU/ cognitive intervention | PCP + CBT |
| Study ID | 1 | 2 | 3 | 4 | 5 |
| + | ‐ | + | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | + | + | + | |
| + | + | + | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | ‐ | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | + | + | + | |
| + | + | + | + | + | |
| + | + | + | + | + | |
| + | + | + | + | + | |
| + | + | + | + | + | |
| + | + | + | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | + | + | + | |
| + | + | + | ‐ | + | |
| + | + | ‐ | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | + | ‐ | + | |
| + | + | + | ‐ | + |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion off work Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 3 months fu | 1 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work long term follow up Show forest plot | 1 | 190 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.30, 0.27] |
| 1.1 12 months fu | 1 | 190 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.30, 0.27] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion off work long term follow up Show forest plot | 1 | 70 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.05, 1.06] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 2 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 6 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 12 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 24 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 1 | 351 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.21 [0.00, 0.42] |
| 1.1 12 months fu | 1 | 351 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.21 [0.00, 0.42] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 5 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months fu | 3 | 447 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.22, 0.15] |
| 1.2 12 months fu | 4 | 395 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.39, 0.01] |
| 2 Time to return to work very long term follow up Show forest plot | 2 | Std. Mean Difference (Fixed, 95% CI) | ‐0.39 [‐0.76, ‐0.02] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 6 months fu | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work short term follow up Show forest plot | 1 | 64 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.59, 0.40] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐7.20 [‐43.64, 29.24] |
| 1.1 3 months fu | 1 | 59 | Mean Difference (IV, Fixed, 95% CI) | ‐7.20 [‐43.64, 29.24] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion off work short term follow up Show forest plot | 2 | 623 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.42, 0.80] |
| 1.1 3 months fu | 1 | 173 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.22, 0.78] |
| 1.2 6 months fu | 1 | 149 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.38, 1.38] |
| 1.3 12 months fu | 2 | 301 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.40, 0.99] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 12 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 24 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to Return to Work Show forest plot | 1 | Std. Mean Difference (Fixed, 95% CI) | ‐4.42 [‐5.06, ‐3.79] | |
| 1.1 12 months fu | 1 | Std. Mean Difference (Fixed, 95% CI) | ‐4.42 [‐5.06, ‐3.79] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 5 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 1.1 3 months fu | 1 | Std. Mean Difference (Random, 95% CI) | ‐1.01 [‐2.11, 0.09] | |
| 1.2 12 months fu | 5 | Std. Mean Difference (Random, 95% CI) | ‐0.23 [‐0.42, ‐0.03] | |
| 1.3 24 months fu | 3 | Std. Mean Difference (Random, 95% CI) | ‐0.26 [‐0.61, 0.10] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Proportion off work short term follow up Show forest plot | 1 | 136 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.37, 2.70] |
| 2 Time to return to work Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 6 months fu | 2 | 114 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.63, 0.24] |
| 2.2 12 months fu | 3 | 256 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.96, 0.04] |
| 2.3 24 months fu | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐1.21, ‐0.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 3 | Std. Mean Difference (Fixed, 95% CI) | Subtotals only | |
| 1.1 6 months fu | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.26 [‐0.50, 1.03] | |
| 1.2 12 months fu | 2 | Std. Mean Difference (Fixed, 95% CI) | 0.05 [‐0.30, 0.40] | |
| 1.3 24 months fu | 1 | Std. Mean Difference (Fixed, 95% CI) | 0.19 [‐0.18, 0.56] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 2 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 1.1 12 months fu | 2 | Std. Mean Difference (Random, 95% CI) | ‐1.75 [‐4.45, 0.95] | |
| 1.2 24 months fu | 2 | Std. Mean Difference (Random, 95% CI) | ‐0.47 [‐1.36, 0.42] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Time to return to work Show forest plot | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 12 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 24 months fu | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |


