Venepuncture versus heel lance for blood sampling in term neonates
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Randomized controlled trial. | |
| Participants | Healthy full term infants undergoing metabolic screening blood test (n = 60). | |
| Interventions | Venepuncture (n=30) versus heel lance (n=30). | |
| Outcomes | Pain assessments were made using the duration of cry within the first 3 minutes after the skin puncture, the Premature Infant Pain Profile (PIPP) score and by changes in the heart rate. | |
| Notes | Infants were randomized using a block randomization technique with sealed envelopes into one of the four groups ‐ HL and VP with and without oral administration of 1 ml of 30% glucose. Data on HL and VP group without the administration of glucose are included for this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomized controlled trial. | |
| Participants | Healthy full term infants undergoing PKU screening (n = 90). | |
| Interventions | Venepuncture with large caliber needle (n = 30) (results not reported). Small caliber venepuncture needle (n = 30; 5 infants excluded) versus heel lance (n = 30; 1 infant excluded). | |
| Outcomes | NIPS (Neonatal Infant Pain Scale) reported at the beginning of each minute, the first minute starting at the moment of puncture. All infants were observed for a minimum of 5 minutes. Number of punctures were also noted. | |
| Notes | Infants were randomized using consecutively numbered envelopes. No envelope was taken out of sequence. Data for the large caliber venepuncture needle group were not presented as in 33% of the infants the venepuncture was unsuccessful. 5 infants in the small caliber venepuncture needle group and 1 infant in the heel lance group were excluded from the analyses because more than two skin punctures were required | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomized controlled trial. | |
| Participants | Healthy term infants undergoing blood testing for phenylketonuria (n=120). Small lancet group: n = 47. Large lancet group: n = 20. | |
| Interventions | Venepuncture (n=50). | |
| Outcomes | Pain assessments were made using Neonatal Facial Action Coding System (NFCS) and cry [latency (cry within 60 seconds of the skin puncture) and duration of first cry and total duration of cry]. Audiotapes were reviewed to determine the latency to cry from the skin puncture, duration of first cry and total time the infant cried during the procedure. Cry was defined as high‐pitched vocalization. | |
| Notes | Infants were randomized using envelopes to receive VP, HL using a small lancet (SL) [three later excluded (one was a preterm infant and two infants screamed prior to heel lance)] or a large lancet (LL). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | Randomized controlled trial. | |
| Participants | Healthy neonates of > =37 weeks gestational age (n=27). Venepuncture group: | |
| Interventions | Venepuncture (n=13) | |
| Outcomes | Pain assessments were made using Neonatal Infant Pain Scale (NIPS). | |
| Notes | Randomization was computer generated. Allocation was by sealed envelopes. One investigator (well‐trained pediatrician) performed all procedures. One of the reviewers (V. Shah) for this systematic review is the primary author of this paper. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Not a randomized controlled trial. |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Need for more than one skin puncture Show forest plot | 3 | 204 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.18, 0.49] |
| Analysis 1.1  Comparison 1 Venepuncture vs. heel lance, Outcome 1 Need for more than one skin puncture. | ||||
| 2 Pain response using NIPS score Show forest plot | 2 | 81 | Mean Difference (IV, Fixed, 95% CI) | ‐1.84 [‐2.61, ‐1.06] |
| Analysis 1.2  Comparison 1 Venepuncture vs. heel lance, Outcome 2 Pain response using NIPS score. | ||||
| 3 Maternal anxiety score prior to the procedure Show forest plot | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [0.34, 1.26] |
| Analysis 1.3  Comparison 1 Venepuncture vs. heel lance, Outcome 3 Maternal anxiety score prior to the procedure. | ||||
| 4 Infant's pain score as rated by the mother Show forest plot | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐1.18, ‐0.42] |
| Analysis 1.4  Comparison 1 Venepuncture vs. heel lance, Outcome 4 Infant's pain score as rated by the mother. | ||||
| 5 Cry within 60 seconds of the skin puncture Show forest plot | 1 | 117 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.41, 0.81] |
| Analysis 1.5  Comparison 1 Venepuncture vs. heel lance, Outcome 5 Cry within 60 seconds of the skin puncture. | ||||
| 6 PIPP‐score Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.46 [‐4.29, ‐0.63] |
| Analysis 1.6  Comparison 1 Venepuncture vs. heel lance, Outcome 6 PIPP‐score. | ||||
| 7 Sampling time (seconds) Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 57.5 [‐23.64, 138.64] |
| Analysis 1.7  Comparison 1 Venepuncture vs. heel lance, Outcome 7 Sampling time (seconds). | ||||
| 8 Need for more than two skin punctures Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.62, 40.28] |
| Analysis 1.8  Comparison 1 Venepuncture vs. heel lance, Outcome 8 Need for more than two skin punctures. | ||||

Comparison 1 Venepuncture vs. heel lance, Outcome 1 Need for more than one skin puncture.

Comparison 1 Venepuncture vs. heel lance, Outcome 2 Pain response using NIPS score.

Comparison 1 Venepuncture vs. heel lance, Outcome 3 Maternal anxiety score prior to the procedure.
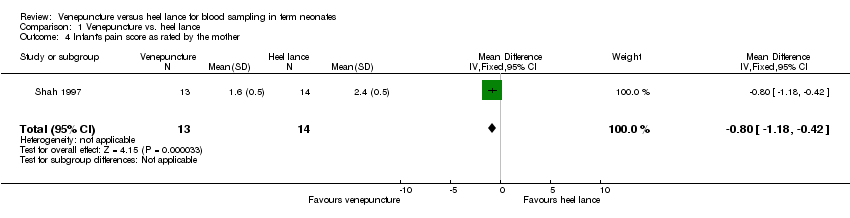
Comparison 1 Venepuncture vs. heel lance, Outcome 4 Infant's pain score as rated by the mother.

Comparison 1 Venepuncture vs. heel lance, Outcome 5 Cry within 60 seconds of the skin puncture.

Comparison 1 Venepuncture vs. heel lance, Outcome 6 PIPP‐score.

Comparison 1 Venepuncture vs. heel lance, Outcome 7 Sampling time (seconds).
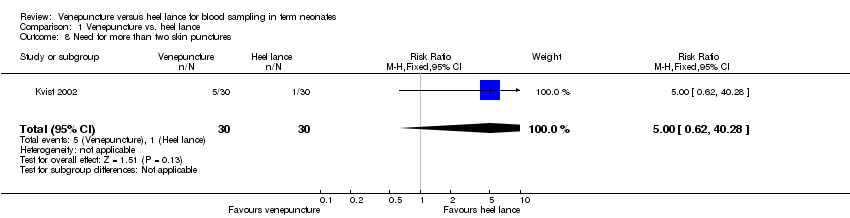
Comparison 1 Venepuncture vs. heel lance, Outcome 8 Need for more than two skin punctures.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Need for more than one skin puncture Show forest plot | 3 | 204 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.18, 0.49] |
| 2 Pain response using NIPS score Show forest plot | 2 | 81 | Mean Difference (IV, Fixed, 95% CI) | ‐1.84 [‐2.61, ‐1.06] |
| 3 Maternal anxiety score prior to the procedure Show forest plot | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [0.34, 1.26] |
| 4 Infant's pain score as rated by the mother Show forest plot | 1 | 27 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐1.18, ‐0.42] |
| 5 Cry within 60 seconds of the skin puncture Show forest plot | 1 | 117 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.41, 0.81] |
| 6 PIPP‐score Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐2.46 [‐4.29, ‐0.63] |
| 7 Sampling time (seconds) Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 57.5 [‐23.64, 138.64] |
| 8 Need for more than two skin punctures Show forest plot | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.62, 40.28] |

