Acupuntura y técnica de aguja seca para el dolor lumbar
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | ‐Randomized (draw lots). Used sealed opaque envelopes by the acupuncturist. | |
| Participants | 40 patients with acute low‐back pain (less than three days) and no sciatica. Diagnoses: lumbar disc herniation, discopathy and lumbago. Mean age: 44 years old 28 males and 7 females. Working status:? | |
| Interventions | 1) The needles were inserted into SI3 (bilaterally) with Teh Chi sensation, in supine position, and then patients were made to perform back exercise. Needles were left in situ during the back exercise. Insertion depth was 2.5 cm with stainless steel needles (50 mm length, 0.20 mm diameter). Acupuncture treatment was performed once only. 2) Sham needling was performed to SI3 (bilaterally) point in supine position. Acupuncturist mimicked needle insertion: tapped head of needle guide tube and then patients were made to perform back exercise. Gesture of needling was performed during the back exercise. Sham treatment was performed once only. | |
| Outcomes | 1) Pain: Visual Analog Scale (VAS) from 0 to 100 mm; All three outcomes were taken before and immediately after the single session. Costs: not reported Complications: not reported | |
| Notes | The original study was published in abstract only. We obtained additional information from the authors. Language: Japanese For results, see the comparisons: Conclusion: "There is no difference between the effect of acupuncture and that of sham acupuncture" | |
| Methods | see Carlsson 2001 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | see Carlsson 2001 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | ‐ Randomized by computer generated list. A secretarial assistant who was not involved in the study performed the assignments. | |
| Participants | 51 patients with low back pain for six months or longer (mean 9.5 years) without radiation below the knee and normal neurological examination. Diagnoses: 39 muscular origin, 11 severe structural changes on X‐rays. Excluded: trauma, systemic disease, pregnancy and history of acupuncture treatment. Mean age: 50 years 17 males and 33 females. Working status: 20 on sick leave, 17 retired, 12 full time, one unemployed. Previous treatments: corsets, nerve blocks, analgesics, TENS, physiotherapy. Two had undergone surgery. | |
| Interventions | 1) Manual acupuncture: local points (BL24, BL25, BL26, Ex Jiaji) and distal points (LI11, LI4, BL40, BL57 and BL60). "Teh‐Chi" feeling was sought in all instances, mostly at a needle‐tip depth of 2 to 3 cm. The needles were stimulated three times during the 20‐minute treatment sessions to restore Teh Chi feelings. The needles were disposable, stainless steel, with a diameter between 0.3 and 0.32 mm and a length between 30 and 70 mm. 2) In addition to the needles as in the manual acupuncture group, they performed electrical stimulation of four needles (one pair per side in the low back). Frequency: 2 Hz every 2.5 seconds, interrupted by a 15 Hz train for 2.5 seconds. 3) Mock transcutaneous electrical nerve stimulation (TENS) given by an impressive, stationary, but disconnected GRASS (gradient‐recalled acquisition in a steady state) stimulator attached to two large TENS electrodes. The electrodes were placed on the skin over the most intensely painful area in the low back. During stimulation, flashing lamps were displayed and visible to the patient. This group was seen once per week for 8 weeks. | |
| Outcomes | 1) Pain: Visual Analog Scale (VAS) from 0 to 100 mm; measured in the morning and in the evening. Not clear how many patients filled all pain diaries everyday. Outcomes were taken at 1 month, 3 months and 6 months or longer after the end of the 8 sessions. The results of these outcomes at baseline are not reported, except for pain which is slightly different between acupuncture and placebo. Costs: not reported Complications: no complications occurred during treatment or follow‐up period | |
| Notes | Language: English Publication: full paper Additional information from authors: no The authors pooled groups 1 and 2 and compared with group 3. The results for pain are similar in the morning and evening measurements. For results, see the comparisons: Conclusion: "The authors demonstrated a long‐term pain‐relieving effect of needle acupuncture compared with true placebo in some patients with low‐back pain" | |
| Methods | ‐Randomized (table of random numbers). No description of allocation concealment. | |
| Participants | 42 patients with continuous pain for more than 3 months. Normal neurologic exam. No signs of radicular compression. Diagnoses: chronic lumbosacral myofascial pain. Excluded: spinal cord injury, osteoporosis, rheumatic diseases, disk herniation, fibromyalgia, organic diseases, hypertension or obesity. Age: between 30‐50 years old. Mean 42 years old. 30 males and 12 females Working status: ? Previous treatments: none had been treated with acupuncture Co‐morbidity: ? | |
| Interventions | 1) Deep acupuncture: 1.5 cm in the muscle or in the trigger point. Needles: disposable Sedatelec 300um diameter of 3 different lengths: 10 mm, 29 mm and 49 mm. Points: Extra 19, VG6. The following were inserted bilaterally: GB34, UB54, UB62. Plus four trigger points or as second choice in the four most painful muscular tender points found in the lumbar area. Total of eight sessions (total 6 weeks), each session lasted for 20 minutes. 2) Same as described for acupuncture, but the depth of insertion was only 2 mm in the skin. | |
| Outcomes | 1) Pain: verbally using the McGill Pain Questionnaire. They used the number of words chosen and the pain rating index. The pain rating index is the sum of numerical values that has been assigned to each word used to describe the pain. Measured immediately after the end of the sessions and after 3 months. Costs: not reported Complications: not reported | |
| Notes | Language: English Publication: full paper Additional information from authors: we contacted authors, but no response was received. For results, see the comparisons: Conclusions: "Clinical results show that deep stimulation has a better analgesic effect when compared with superficial stimulation" | |
| Methods | ‐Randomized (computer‐generated random sequence). A research assistant confirmed eligibility, collected baseline data and randomised the eligible ones. | |
| Participants | 262 patients who visited a primary care physician for low‐back pain who had persistent pain for at least 6 weeks. Diagnoses: Non‐specific low‐back pain. Excluded: sciatica, acupuncture or massage for back pain, back care from a specialist or CAM provider, clotting disorders or anticoagulant therapy, cardiac pacemakers, systemic or visceral disease, pregnancy, litigation or compensation, inability to speak English, severe or progressive neurologic deficits, previous lumbar surgery, recent vertebral fracture, serious comorbid conditions and bothersomeness of back pain less than 4 (on a 0 to10 scale). Mean age: 44.9 years old 42% males and 58% females Working status: 84% employed or self‐employed Treatments being received at the time of entry in the study: medications (68%), massage (16%), acupuncture (3%), narcotics (10%) Co‐morbidity: see exclusion criteria | |
| Interventions | 1) Acupuncture: Traditional Chinese Medical acupuncture by licensed acupuncturists with at least 3 years of experience; Basic TCM needling techniques, electrical stimulation and manual manipulation of the needles, indirect moxibustion, infrared heat, cupping, and exercise recommendation. 2) Massage by a licensed therapist with at least 3 years of experience. Manipulation of soft tissue: Swedish (71%), movement reeducation (70%), deep‐tissue (65%), neuromuscular (45%), and trigger and pressure point (48%), moist heat or cold (51%). Prohibited: energy techniques (Reiki, therapeutic touch), meridian therapies (acupressure and shiatsu) and approaches deemed too specialized (craniosacral and Rolfing). Massage therapists recommended exercise. They were allowed up to 10 visits over 10 weeks per patient. 3) Self‐care education: high‐quality and inexpensive educational material designed for persons with chronic back pain: a book and 2 professionally produced videotapes. | |
| Outcomes | 1) Pain: bothersomeness of back pain (0 to10), leg pain (0 to10) or numbness or tingling (0 to10). The higher score was used. Outcomes were measured at baseline, 4, 10 and 52 weeks after randomisation Complications: no serious adverse effects were reported by any study participant | |
| Notes | Language: English Publication: full paper For results, see the comparisons: However, the results shown in the table of comparisons are the unadjusted analysis. We based our conclusions on the authors analyses. Conclusions: "Massage is an effective short‐term treatment for chronic low‐back pain, with benefits that persist for at least one year. Self‐care educational materials had little early effect, but by one year were almost as effective as massage. If acupuncture has a positive effect, it seems to be concentrated during the first four weeks because there was little improvement thereafter". | |
| Methods | See Cherkin 2001 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | See Cherkin 2001 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | ‐Randomization was carried out by having prepared in advance a small box with 50 identically‐sized pieces of paper, folded so that they could not be read. 25 had A and 25 had B written on them. The box was shaken and one of the pieces of paper was removed from the box blindly. | |
| Participants | 50 patients recruited via newspapers with low‐back pain for at least 6 months. Diagnoses: Abnormal X‐ray (38/43), Sciatica (27/49), Muscle spasm (36/46) Inclusion criteria: no previous acupuncture treatments, no history of diabetes, infection or cancer, and not more than 2 back surgeries. Mean age: 47 years old (range 18 to 67) 23 males and 27 females Working status:? Previous treatments: back surgery (4) | |
| Interventions | 1) Acupuncture: Classical Oriental meridian theory. Electrical acupuncture in some patients. Selection of acupuncture loci varied. 'Acknowledged acupuncturists'. 10 or more sessions, approximately 10 weeks. Teh chi unclear. 2) Waiting list, no treatment for 15 weeks. Then they received the same acupuncture treatment as above. | |
| Outcomes | 1) Pain: Mean pain scores (0=no pain and 10=worst pain) Results after 10 weeks in acupuncture and after 15 weeks in waiting list group Costs: not reported Complications: not reported | |
| Notes | The authors reported a per protocol analysis. However, because there is individual patient data reported in the article, we were able to recalculate using the intention‐to‐treat principle. Language: English Publication: full paper Additional information from authors: no For results, see the comparisons: Conclusions: "This study demonstrated that acupuncture was a superior form of treatment for these people with low‐back pain, even though they had the condition for an average of 9 years". | |
| Methods | ‐ Randomized (method not described). No mention of concealment of allocation. | |
| Participants | 54 patients with chronic low‐back pain, frequent recurrence, worse during work and relief with rest. Diagnosis: chronic low‐back pain. Excluded: specific pathological entities using lab tests and x‐rays. Mean age: 45 years old in the ancient needling technique and 42 in regular needling technique group (range 19‐68) 40 males and 14 females Working status: ? Previous treatments: ? | |
| Interventions | 1) Ancient needling technique "The turtle exploring the holes". Major points: GV3, Ashi point(s). Supplement points: BL40. Needles 0.38 mm X 75 mm were used for deeper insertion and to different direction in 45 degree angle. Strong Teh chi sensation was obtained. The needles were retained for 40 to 50 minutes. Treatments were given daily up to 10 treatments. 2) Regular needling technique. Needles 0.38 mm X 75 mm were used for deeper perpendicular insertion with twirling or rotating technique was used until strong Teh Chi sensation was acquired. Needle retaining was 20 minutes with 3 to 4 times twirling or rotating stimulation in between. Treatments were given daily for up to 10 days. | |
| Outcomes | 1. Pain on a 4‐point scale: "cure": no pain for 2 months; Measured immediately after and 2 months after the end of the sessions. Costs: Not reported Complications: Not reported | |
| Notes | Language: Chinese Publication: full paper No additional information from authors For results, see the other data table: Conclusions: "An ancient needling technique is better than the regular needling technique in treating chronic low back pain". | |
| Methods | ‐ Randomized (method not described). No mention of concealment of allocation. | |
| Participants | 30 patients with low‐back pain with no improvement after conventional therapy, including bed rest, analgesics, heat and physiotherapy. Patients were felt to have disc disease, which could not be surgically improved. | |
| Interventions | 1) Acupuncture: Manual insertion of 4 sterile needles into traditional acupuncture points (BL 60 and BL 25 bilaterally) until reaching Teh Chi, then electroacupuncture at 3‐10 Hz. 30 minutes, 3 treatments in maximum 2 weeks. Training & experience of acupuncturists unknown. 2) Sham acupuncture, 4 needles placed in areas devoid of classic acupuncture points, no Teh Chi. | |
| Outcomes | 1) Global assessment: subjective improvement of back/leg pain Costs: not reported Complications: not reported | |
| Notes | Number of patients randomised unknown. We only know that 30 were analysed. We classified the patients into "chronic low‐back pain". Language: English Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "There seemed to be no difference in either the subjective or objective changes between the two effects and suggest that much of the improvement in pain syndromes associated with acupuncture may be on the basis of placebo effect". | |
| Methods | ‐Randomized (computer generated four‐tier list). No mention of concealment of allocation. | |
| Participants | 63 patients with acute non radiating low‐back pain, normal neurological examination, absence of tension signs, normal x‐ray, persistent pain despite initial treatment of 4 weeks, being able to localize a point of maximum tenderness (trigger point). Age: mean 38 years old Gender: 41 men and 22 women Working status: not reported Previous treatment: non‐steroidal anti‐inflammatory drugs, hot showers, avoidance of activities that aggravate the pain. No exercise program had been started. | |
| Interventions | 1) Dry‐needling stick with a 21‐gauge needle after an isopropyl alcohol wipe. 1 session. Training & experience of therapists unknown 2) injection with 1.5 ml of 1% lidocaine using a 1.5 inch, 21‐gauge needle after an isopropyl alcohol wipe. 3) injection with 0.75 ml of 1% lidocaine and 0.75 ml of Aristospan (Triamcinolone Hexacetonide) using a 1.5 inch, 21‐gauge needle after an isopropyl alcohol wipe. 4) 10‐second ethyl chloride spray from 6 inches away, followed by 20 second acupressure using the plastic needle guard after an isopropyl alcohol wipe. | |
| Outcomes | 1) global improvement: percentage of not improved or improved. This outcome was measured at 2 weeks after the interventions. Costs: Not reported Complications: | |
| Notes | Intervention is "dry‐needling" Language: English Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "The injected substance apparently is not the critical factor, since direct mechanical stimulus to the trigger‐point seems to give symptomatic relief equal to that of treatment with various types of injected medication". | |
| Methods | see Garvey 1989 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | see Garvey 1989 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | see Garvey 1989 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | ‐Randomized (method not described). Person drew an envelope out of a box with 150 well‐shuffled envelopes, each containing one of three colour codes (50 envelopes per intervention) | |
| Participants | 77 patients with spinal pain for at least 13 weeks (median 6 years). Diagnoses: 82% lower back pain; 42% neck pain and 34% upper back pain. Excluded: nerve root involvement, spinal anomalities, pathology other than mild to moderate osteoarthrosis, previous spinal surgery and leg inequality > 9mm. Median age: 42 years old 30 males and 47 females Working status: 56% blue collar, 26% white collar, 13% academic, 5% retired Previous treatments: 77% drugs, 42% manipulation, 40% physiotherapy and 6% acupuncture Co‐morbidity: not described | |
| Interventions | 1) The treating clinician decided which form of acupuncture to use. 2) Spinal manipulation was performed as judged to be safe and appropriate by the treating chiropractor for the spinal level of involvement only. A high‐velocity, low‐amplitude spinal manipulation was performed. Six treatments applied in a 3 to to 4‐week period. 3) Medication: tenoxican (20 mg/d) and ranitidine (50 mg x 2/ day). Medication was given to the patients for the defined 3 to 4‐week treatment period. Treatment times were standardized by arranging 15 to 20‐minute appointments for all visits to eliminate a potential placebo effect originating from different lengths of exposure to the clinician | |
| Outcomes | 1) Pain: Visual Analog Scale (VAS) from 0 to 10 cm All outcomes were measured immediately after the end of the treatment period Costs: Not reported Complications: No side effects occurred for acupuncture or manipulation. Three medically treated subjects had gastric symptoms | |
| Notes | The results of this study are not used in this review because of the high drop‐out rate in the acupuncture group (52%) that might invalidate the results of this trial. Language: English Publication: full paper No additional information from authors For results, see the comparisons: Study conclusions: "the manipulation group displayed the most substantial improvements that were uniformly found to be significant. In the other intervention groups, not a single significant improvement could be found in any of the outcome measures". | |
| Methods | See Giles 1999 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | See Giles 1999 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | ‐Randomized (method not described). Person drew an envelope out of a box with 150 well‐shuffled envelopes, each containing one of three colour codes (50 envelopes per intervention) | |
| Participants | 109 patients with uncomplicated spinal pain for a minimum of 13 weeks (average duration was 6.4 years) Diagnosis: mechanical spinal pain Excluded: nerve root involvement, spinal anomalies, pathology other than mild to moderate osteoarthrosis, spondylolisthesis exceeding grade 1, previous spinal surgery and leg length inequality >9 mm. Median age: 39 years old 60 males and 49 females Working status: 29% skilled trade, 20% pensioner or unemployed, 20% manager, clerk or sales, 12% professional, 18% other. Previous treatments: not described Co‐morbidity: not described | |
| Interventions | 1) The clinician determined the form of acupuncture technique. The Near and Far technique consists of: needling the trigger point and distal analgesia producing sympatholytic acupuncture points below the elbow or knee. 2) Spinal manipulation. 20‐minute appointment. High‐velocity, low‐amplitude thrust spinal manipulation to a joint was performed as judged to be safe and usual treatment by the treating chiropractor for the spinal level of involvement to mobilize the spinal joints. Two treatments per week up to a maximum of 9 weeks. 3) A medication could be selected that had not already been tried by a patient randomised into the mediation arm of the study. The patients normally were given Celecoxib (200 to 400 mg/day) unless it had previously been tried. The next drug of choice was Rofecoxib (12.5 to 25 mg/day) followed by paracetamol (up to 4 g/day). Doses, left to the sports physician's discretion, were related particularly to the patient's weight, with the severity of symptoms playing a minor role. The treating sports physician also was allocated 20 minutes for follow‐up visits. | |
| Outcomes | 1) Pain: Visual Analog Scale (VAS) from 0 to 10 cm All outcomes were measured immediately after the end of the treatment period Costs: Not reported Complications: Not reported | |
| Notes | Not sure about proportion of patients with lower back pain. The results might be biased by the high and differential drop out rates. Results are presented as medians and 25th and 75th percentiles and were transformed to means and standard deviations. Language: English Publication: full paper No additional information from authors For results, see the comparisons: Study results: "Manipulation yielded the best results over all the main outcome measures except the Neck Disability Index, for which acupuncture achieved a better result than manipulation". "All three therapies showed positive response according to the SF‐36 general health status questionnaire" Conclusions: "In patients with chronic spinal pain, manipulation, if not contraindicated, results in greater short‐term improvement than acupuncture or medication". | |
| Methods | See Giles 2003 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | See Giles 2003 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | ‐ Random numbers were used (method not described) to generate a sequence of sealed envelopes containing the treatment code, the next available envelope being opened on the patient's entry into the trial. | |
| Participants | 60 patients aged 60 years or over, with a complaint of pain of at least 6 months duration. Diagnoses: chronic low‐back pain. Excluded: treatment with anticoagulants, systemic corticosteroids, dementia, previous treatments with acupuncture or TENS, cardiac pacemaker, other severe concomitant disease, inability of patient or therapist to apply TENS machine. Mean age: 73.6 years old 6 males and 54 females Previous treatments: not reported | |
| Interventions | 1) Two sessions of manual acupuncture weekly for 4 weeks, i.e. eight sessions in total. The needles were of a standard size (32 gauge, 1.5 inch length with guide tube). Points were chosen for the individual patient as in routine clinical practice, only using points in the back. Six needles were used on average at each treatment with a minimum of two and a maximum of eight. Treatment sessions lasted for 20 minutes. 2) TENS: Standard machine (TPN 200, Physio‐Med‐Services) using 50 Hz stimulation with the intensity adjusted to suit the patient, again as a routine clinical practice. The patient was given her/his own machine to use at home, and instructed to use it during the day as required for up to 30 minutes per session to a maximum of 6 hours per day. She/he was also seen for 20 minutes, twice weekly, by the physiotherapist, ensuring the same contact with him. At each visit, symptoms were reviewed, treatment discussed and the optimum use of the TENS machine ensured. Co‐interventions: The patients were advised to continue existing medication but not to commence any new analgesics or any additional physical treatments for the duration of the trial. | |
| Outcomes | 1) Pain: visual Analog scale (0 to 200 mm). These outcomes were taken at baseline, 4 days and 3 months after last treatment session. Costs: not reported Complications: 3 acupuncture patients reported dizziness and 3 TENS patients developed skin reactions. (Comparison 07.08) | |
| Notes | The two groups appear different at baseline with respect to the four outcome measures. Patients in the acupuncture group have higher VAS and NHP pain scores, reduced spinal flexion and lower tablet consumption compared to the TENS group. Because the authors had not adjusted for baseline values, no conclusions can be made based on this study. We could try to obtain raw data from authors and run ANCOVA, but the data is also skewed and transformation is not appropriate. Results: Language: English Publication: full paper No additional information from authors Conclusions: "A 4‐week course of either acupuncture or TENS had demonstrable benefits on subjective measures of pain (VAS and NHP score) and allowed them to reduce their consumption of analgesic tablets. The benefits of both treatments remained significant 3 months after completion, with a trend towards further improvement in the acupuncture patients." | |
| Methods | ‐Randomized (randomised blocks, blocks defined by age and operation status; the first subject from each block was assigned to the acupuncture treatment.) | |
| Participants | 56 males with chronic low‐back pain of at least 12 weeks duration, who had 8 weeks of a standard clinic regimen. Diagnoses: disc diseases, low‐back strain, spondylitis, spondylolisthesis, radiculopathy, low‐back contusion, pseudoarthrosis, disc protrusion, prolapsed disc, lumbar disc syndrome, post‐laminectomy syndrome, neuropathy, sciatica, nerve root compression, facet sprain, musculo‐ligamentous strain, compression fracture, interspinous ligament strain, Excluded: Psychosomatic backache. Females. Mean age: 40.6 years old (range 20 to 62 years) Working status: all off work. Previous treatments: some had surgery. | |
| Interventions | 1) Dry‐needling: Standard therapy (physiotherapy, remedial exercises, occupational therapy, industrial assessment) plus dry‐needling on muscle motor points (non‐meridian), 3 to 5 cm needles, direction of the needle perpendicular to the skin, mechanical stimulation by pecking and twirling, low voltage (9V) electrical stimulation interrupted direct current or phasic current. 2) Standard therapy only (physiotherapy, remedial exercises, occupational therapy, industrial assessment). | |
| Outcomes | 1) Global improvement: The above was measured after discharge, 12 weeks after discharge and at the time of writing of the paper. (all these varied) Costs: not reported Complications: not reported | |
| Notes | Intervention is dry‐needling. We dichotomized at 0 versus +/++/+++. Language: English Publication: full paper No additional information from authors For results, see the comparisons: Conclusion: "The group that had been treated with needling was found to be clearly and significantly better than the control group with regard to status at discharge, at 12 weeks, and at final follow‐up". | |
| Methods | ‐Randomized (method not reported). No information about concealment of allocation | |
| Participants | 100 patients with low‐back pain (5 days to 6 months duration), with limited range of motion, and symptoms worse in cold and rainy weather. Excluded: kidney or bone disease confirmed by urine test and X‐ray. Age range: 22 to 79 years old 44 males and 56 females Working status: not reported Previous treatments: not reported | |
| Interventions | 1) Manual acupuncture with moxibustion plus Chinese herbal medicine. Two groups of points: 1) GV 4, BL 22 , Ashi‐points. 2) BL23, GV 3 and Extra 9 (L3‐L4). Moxibustion was used 2 to 3 times on the handle of the needles and needles were retained for 30 minutes. Treatments were given daily up to 10 treatments. Teh Chi sensation was obtained. Herbal formula was given daily. 2) Chinese herbal treatment alone. | |
| Outcomes | 1) Overall assessment that includes pain, physical function, sensitivity to weather change and return to work. The overall assessment was measured one year after the end of the sessions. Costs: not reported Complications: not reported | |
| Notes | We classified the duration as acute/subacute. We dichotomized at a/b/c versus d. Language: Chinese Publication: full paper No additional information from authors For results, see the comparisons: Conclusion: "Manual acupuncture with moxibustion plus Chinese herbal medicine is better (p<0.01) than Chinese herbal medicine alone for treating low‐back pain with cold and dampness, based on TCM diagnosis". | |
| Methods | ‐Randomized (computer generated numbers). Allocation was done by a centralized office using the Internet. | |
| Participants | 27 patients with low back pain of unknown duration who attended the outpatient acupuncture clinic. Excluded: (1) neurological findings, pain or numbness in lower extremity; (2) malignancy, (3) infection or inflammatory disease; (4) fracture; (5) lumbago due to urological problem, gynaecological problem, digestive problem or cardio‐vascular problem; (6) patients who cannot stop other conflicting or ongoing treatments; (7) problem of general condition; (8) dementia; (9) pregnancy. Mean age: 59.6 years old Gender: no information Working status: no information Previous treatments: no information. | |
| Interventions | 1) Real acupuncture: Two needling points were chosen bilaterally from lumbar area (i.e. 4 points in total): BL52 and extra point (yao‐yan: EX‐B7). Needles were inserted to a depth of 20 mm, manipulated by sparrow pecking method for 20 seconds, and then removed. One treatment session was performed. 2) Sham acupuncture: The same two points were chosen. Acupuncturist mimicked needle insertions: tapped head of needle guide tube, then gesture of needling was performed for 20 seconds. One session. | |
| Outcomes | 1) Pain: visual analog scale (VAS) at the most restricted action immediately after the single session. Costs: not reported Complications: not reported | |
| Notes | Language: Japanese Publication: abstract We obtained additional information from authors. For results, see the comparisons: Conclusion: "There was no difference between real needling and sham needling". | |
| Methods | ‐Randomized (computer generated numbers). Allocation was done by a centralized office using the Internet. | |
| Participants | 21 patients with low‐back pain of unknown duration who attended the outpatient acupuncture clinic were included. Excluded: (1) neurological findings, pain or numbness in lower extremity; (2) malignancy, (3) infection or inflammatory disease; (4) fracture; (5) lumbago due to urological problem, gynaecological problem, digestive problem or cardio‐vascular problem; (6) patients who can not stop other conflicting or ongoing treatments; (7) problem of general condition; (8) dementia; (9) pregnancy. Mean age: 55.1 years old Gender: no information Working status: no information Previous treatments: no information. | |
| Interventions | 1) Real acupuncture: One needling point was chosen from lumbar area: most painful locus was detected. Needles were inserted and sparrow‐picking technique was performed for 20 seconds. One session. 2) Sham acupuncture: One needling point was chosen from lumbar area: most painful locus was detected, same as real acupuncture group. Acupuncturist mimicked needle insertion: tapped head of needle guide tube, then gesture of needling was performed for 20 seconds. One session. | |
| Outcomes | 1) Pain: visual analog scale (VAS) at the most restricted action immediately after the single session. Costs: not reported Complications: not reported | |
| Notes | Language: Japanese Publication: abstract We obtained additional information from authors. For results, see the comparisons: Conclusion: "Real needling is superior to sham needling". | |
| Methods | ‐Randomized (computer generated numbers). No information about who performed allocation of patients. | |
| Participants | 60 patients with chronic low‐back pain (> 6 months) with or without leg pain and with no neurologic deficits. Mean duration of pain was 75.8 months. Excluded: age < 18 years old, pregnancy, underlying systemic disorder, rheumatoid arthritis, osteoarthritis of the spine or cancer. Mean age: 41 years old 28 males and 32 females Working status: not reported Previous treatments: not reported | |
| Interventions | 1) Same set of acupoints for everyone, regardless of the distribution of their symptoms: Bl23, Bl25, GB 30, Bl40, Ki3 (all bilateral) and GV4. Eleven needles were used in each session (Seirin acupuncture needles N8, 0.30 x 50 mm, c‐type needle). The needles were inserted until Teh Chi was produced. Position: prone. Duration: 30 minutes. Needles were manually rotated to produce Teh Chi initially and at 10 to 20 minute intervals. Sessions: 6 sessions, over a 6‐week period. 2) Placebo‐TENS: Patients were advised that the treatment was relatively novel and that they should not feel any discomfort with the procedure and, in fact, should not be aware of any sensation at all. They were advised that the treatment had an effect on the nerve‐endings and that it should relieve their symptoms. Patient lying in the prone position for 30 minutes. A non‐functioning TENS machine was attached to 4 electrodes placed over the lumbar spine and the unit was placed in a position to make it difficult to interfere with the apparatus. The investigator monitored the patient's condition after 10 and 20 minutes. Sessions: 6 over a 6‐week period. | |
| Outcomes | 1) Pain (VAS) 4) Global improvement measured at 6 months: "Did you experience pain relief? "Yes" or "No". But only 40 (66.7%) patients were followed up to 6 months Costs: not reported Complications: In the acupuncture group there were 2/23 patients who reported side effects and 2/17 in the placebo group. | |
| Notes | Language: English Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "Although acupuncture showed highly significant differences in all the outcome measures between pre and post‐treatment, the differences between the two groups were not statistically significant". | |
| Methods | ‐ Randomization in blocks of four patients (method not described). No description of who performed the allocation of patients | |
| Participants | 60 patients with acute low‐back pain (lasting less than 10 days). Excluded: Neurologic outcomes, rheumatic illness, malign disease, systemic use of anti‐inflammatory drugs or steroids before inclusion and use of medicine that may interact with anti‐inflammatory drugs. Between 18 and 67 years of age Gender: both sexes Working status: 2/3 on sick leave at time of inclusion | |
| Interventions | 1) First treatment was needling in "lumbago 1 and 3" with medial lumbago, and in "upper lip" with more lateral pain. Later treatments were 5 needles across at level L2, at "Ashi points" (local pain points) and in both ankles. Analgesia was allowed and sick leave provided when necessary. Four treatments within two weeks. 2) Naproxen 500 mg twice daily for ten days | |
| Outcomes | 1) Pain (VAS) measured at baseline, 1 and 2 weeks and 3 and 6 months Costs: not reported | |
| Notes | Language: Norwegian Publication: full paper Asked authors for additional information: no response. For results, see the comparisons: Conclusions: "No difference in reduction of pain or stiffness over a six‐month evaluation" | |
| Methods | ‐Randomized (method not described). No information about concealment of allocation | |
| Participants | 20 patients with lumbar or sacral region pain. Most of patients were between 40 and 50 years old. 10 males and 10 females Working status: Not reported Previous treatments: Not reported | |
| Interventions | 1) Acupuncture: the needles were inserted, and left in situ for 10 minutes, and then removed. Insertion depth was 2 to 4 cm, depending on one's figure. Acupuncture needles used were stainless steel needles (50 mm length, 0.25 mm diameter). Six to eight points in lumbar part were chosen from BL23, 24, 25, 26, 27, 31, 52 and 3 extra channel points by palpation. Abdominal needling was added: needles were inserted to a depth of 1 to 1.5 cm at CV4,13 and ST25 (bilaterally). Acupuncture treatment was performed more than 4 times. 2) Garlic moxibustion in lumbar region: Moxa is placed on top of a slice of garlic. Six to eight points in lumbar area were chosen from BL23, 25, 27, 52 and the other points by palpation. | |
| Outcomes | 1) Pain: 10‐item questionnaire about the specific actions that caused pain. Possible range of this questionnaire is ‐10 to 20 (if patient feels pain at all actions) and higher scores are better. It was measured immediately before second and fourth session Costs: not reported Complications: not reported | |
| Notes | Language: Japanese Publication: full paper No additional information from authors. For results, see the comparisons: Conclusions: "There is no difference between needle retention technique and garlic moxibustion for low‐back pain". | |
| Methods | ‐Randomized (method not described). No information about concealment of allocation | |
| Participants | 20 patients with lumbar or sacral region pain. Most of patients were between 40 and 50 years old. 11 males and 9 females Working status: Not reported Previous treatments: Not reported | |
| Interventions | 1) Acupuncture: the needles were left in situ for 10 minutes, and then removed. Depth was 2 to 4 cm, depending on one's figure. Stainless steel needles (50 mm length, 0.25 mm diameter). Six to eight points in lumbar part were chosen from BL23, 24, 25, 26, 27, 31, 52 and 3 extra channel points by palpation; abdominal needling was added: needles were inserted to a depth of 1 to 1.5 cm at CV4,12 and ST25 (bilaterally). Acupuncture treatment was performed more than 4 times. 2) Other acupuncture technique: needles were removed immediately after insertion. Insertion depth was 2 to 4 cm, depending on one's figure. Stainless steel needles (50 mm length, 0.25 mm diameter). Six to eight points in lumbar part were chosen from BL23, 24, 25, 26, 27, 31, 52 and 3 extra channel points by palpation. Abdominal needling was added: needles were inserted to a depth of 1 to 1.5 cm at CV4,12 and ST25 (bilaterally); needles were left in situ for 10 minutes, and then removed. Acupuncture treatment was performed 3 times. | |
| Outcomes | 1) Pain: 10‐item questionnaire about the specific actions that caused pain. Possible range of this questionnaire is ‐10 to 20 (if patient feels pain at all actions) and higher scores are better. It was measured immediately after the fourth session Costs: not reported Complications: not reported | |
| Notes | Language: Japanese Publication: full paper No additional information from authors. For results, see the comparisons: Conclusions: "Results of needle retention technique is superior to that of simple insertion technique for low‐back pain". | |
| Methods | ‐Block randomisation, blocks defined by prior lumbar surgery (method not reported). No information about concealment of allocation. | |
| Participants | 54 patients screened at orthopaedic clinic with chronic (>3 months) disabling low‐back pain. Excluded: candidates for lumbar surgery, pain less than 3 months, pregnancy, osteomyelitis of the spine, discitis, tumour, ankylosing spondylitis, vertebral fractures and structural scoliosis. Diagnoses: chronic disabling (not working) low‐back pain. Duration of low‐back pain: 48% more than 18 months. Mean age: 39 years old (ranged from 20 to 59) Gender: 33% females. 93% married. Working status: 1/54 was working. 51 were receiving compensation. 33% were involved with litigation. Previous treatments: some had surgery. | |
| Interventions | 1) Electroacupuncture with needles, biphasic wave at 2 to 4 Hz, inner and outer bladder meridian for paravertebral pain. Gall bladder meridian for lateral (sciatic) pain. LI4 points and additional points were stimulated according to the patient's pattern of pain; certified and experienced acupuncturist; twice weekly for 3 weeks. Teh Chi not reported. 2) Real TENS, pulse width of 250/second at 60 Hz, 15 treatments in 3 weeks, sub‐threshold intensity, points of stimulation over the center of pain, experienced physiotherapist. 3) Sham TENS, same as TENS but dead battery. | |
| Outcomes | 1) Peak pain and average pain (VAS) 5) Return to Work after 6 months (from no disability=10 points, to not able to work at all=0 points); Costs: not reported Complications: there were no complications. | |
| Notes | Language: English Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "There were no significant differences between treatment groups with respect to their overall rehabilitation". "The electroacupuncture group demonstrated slightly better results than the other groups." | |
| Methods | ‐Computer‐based randomisation method. | |
| Participants | 150 patients with chronic (> 6 months) non‐radiating low‐back pain. Excluded: Abnormal neurological status, concomitant severe disease, psychiatric illness, current psychotherapy, pathological lumbosacral anterior‐posterior and lateral X‐rays (except for minor degenerative changes), rheumatic inflammatory disease, planned hospitalisation and refusal of participation. Mean age: 48.1 years old Gender: 58% female 76% married Mean BMI: 26.3 Working status: 82% employed Current treatments: 8.4% surgery. 50% analgesics | |
| Interventions | 1) All patients received standardized active physiotherapy of 26 sessions (each 30 minutes) over 12 weeks. It was performed by trained physiotherapists according to the Bruegger‐concept. In addition, 20 sessions (each 30 minutes) by an experienced Taiwanese physician over 12 weeks. In the first 2 weeks, acupuncture was done 5/week, and in the next 10 weeks, 1/week. 2) No additional treatment. Only active physiotherapy (as described above) 3) Sham acupuncture plus physiotherapy. Sham acupuncture received 20 sessions (each 30 minutes) of minimal acupuncture by the same physician over 12 weeks. Sham acupuncture was done following the standards of minimal acupuncture. Needles were inserted superficially, 10 to 20 mm distant to the verum‐acupoints, outside the meridians, and were not stimulated (no Teh Chi). | |
| Outcomes | 1) Pain intensity: 10 cm VAS Costs: not reported Complications: minor, not serious adverse events occurred in three patients in the acupuncture group. | |
| Notes | The use of last observation carried forward usually attenuates the differences between groups. Language: English Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "Acupuncture plus physiotherapy was superior to physiotherapy alone regarding pain intensity, disability and psychological distress at the end of the treatment. Compared to sham acupuncture plus physiotherapy, acupuncture (plus physiotherapy) reduced psychological distress only. At 9 months, the superiority of acupuncture plus physiotherapy compared to physiotherapy alone became less and acupuncture plus physiotherapy was not different from sham plus physiotherapy". | |
| Methods | ‐Randomized (method not reported). | |
| Participants | 156 patients with low‐back pain of varying duration (between 2 days and 8 years) Diagnoses: not reported Excluded: not reported Age between 20 and 71 years old 80 males and 76 females Working status: not reported Previous treatments: not reported | |
| Interventions | 1) Manual acupuncture plus cupping. Teh Chi sensation was obtained and needles were retained for 20 minutes. Major points: BL23, 40. GV 2, 26, LU5. Supplement points: for coldness and dampness: GV3, BL31, 34. For blood stasis: BL17, 18. For kidney deficiency: GV4 and KI 3. Treatment was given every other day (except for acute back pain, which was treated daily) up to 10 treatments. 2) Manual acupuncture alone. Major points: BL23, 40 and GV2. Supplement points: same as treatment group. | |
| Outcomes | 1) Overall assessment (see description in He 1997). Measured immediately after the end of the sessions. Costs: not reported Complications: not reported | |
| Notes | Language: Chinese Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "Manual acupuncture plus cupping technique is better than manual acupuncture alone for treating low‐back pain" | |
| Methods | ‐ Randomization procedure not described. | |
| Participants | 34 male patients from a neurology department. Age: mean 42 years old (ranged from 25 to 52). | |
| Interventions | 1) Acupuncture: 4 needles close to spine, 10 minutes, 4 treatments, 8 days, plus pharmacotherapy. Teh Chi unclear. Training & experience of acupuncturists unknown. 2) Placebo, suggestion, new Swedish method for pain relief, same 4 points echo‐encephalography, 10 minutes, 4 treatments, 8 days, plus pharmacotherapy. | |
| Outcomes | 1) Global improvement (5‐point scale): very good, good, doubtful, unchanged and worsening. Measured after first treatment and after 4 treatments Costs: not reported Complications: not reported | |
| Notes | Very short term follow‐up only. Small sample size. Authors dichotomized at very good + good versus others. We classified the patients as chronic low‐back pain. Language: Polish Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "The therapeutic results were better, both immediately and after a series of acupuncture. The difference in the results of treatment was statistically significant in the patients with longest duration of pains (>3 months)". | |
| Methods | ‐A stratified random process to divide the sexes as equally as possible between the two groups. | |
| Participants | 17 patients referred from orthopaedic or rheumatological departments. Diagnoses: spondylitis, ankylosing spondylitis, degenerative disc lesion, idiopathic, non‐articular rheumatism, osteoarthritis, prolapsed intervertebral disc, arachnoiditis, ligamentous strain and Scheuermann's osteochondritis. Exclusion criteria: not reported Demographics: not reported. But it says "the two groups were comparable in terms of age, duration of pain, mood scores, number of physical signs and severity of pain. | |
| Interventions | 1) Superficial needling: subcutaneous (4 mm) 30‐gauge needle insertion at trigger points. (Number of trigger points unknown). 5 to 20 minutes, maximum of 10 treatments in 10 weeks. Electrical impulses 700µs at 2 Hz if manual stimulation failed. Randomized to this group: 8 2) Placebo transcutaneous electrical stimulation: electrodes connected to dummy apparatus, maximum 10 treatments in 10 weeks. | |
| Outcomes | 1) Pain relief: Costs: not reported Complications: not reported | |
| Notes | Intervention is dry‐needling. Very small sample size, number of treatments unknown, and follow‐up time unknown. Language: English Publication: full paper No additional information from authors Results: Conclusions: "Needling achieved better responses than the placebo in all five measures. Four of the five inter‐group differences were statistically significant." | |
| Methods | ‐Randomized (method not described). Unclear about concealment of allocation. Cross‐over study. | |
| Participants | 95 volunteers with chronic low‐back pain, no compensation or litigation pending, no overt psychiatric disease. Diagnoses: Osteoarthritis, traumatic spondylopathy, disc lesion, sacroiliac joint disorder and backache not specified. Mean age: 54 years old Gender: 37 males and 40 females. Pain duration: 12 years. | |
| Interventions | 1) Traditional Chinese acupuncture by a surgeon trained in Peking; points: B23, 25, 36, 40 and 60. If sciatica: GB 30, 34 and 39. Average 8 needles, manual stimulation until reaching Teh Chi, 30 minutes with no further stimulation, twice weekly, 4 weeks. 2) Sham acupuncture, intradermal injection of 2% lidocaine at non‐acupuncture, non‐tender sites, then acupuncture needles superficially into the infiltrated areas for 30 minutes without stimulation, twice weekly, 4 weeks. | |
| Outcomes | 1) Pain (VAS) 100‐mm scale. Costs: not reported Complications: not reported | |
| Notes | Language: English Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "Patients receiving acupuncture had a greater but not significantly different reduction in pain rating scores compared with those receiving placebo. Similarly, no significant difference was found between the two groups based on self‐assessment of disability". | |
| Methods | ‐Randomized (computer generated random allocation sequence). Serially numbered, sealed, opaque envelopes | |
| Participants | 55 patients with chronic nonspecific low back pain (>12 weeks) and older than 60 years. Excluded: specific cause for low‐back pain, prior use of acupuncture, use of corticosteroids, muscle relaxants, narcotics, anticoagulants. Mean age: 71 years old Gender: 22 male and 33 female Previous treatments: 27 NSAID, 10 analgesics, 1 muscle relaxant and 2 aspirin. Ethnicity: 47 Caucasian, 5 African‐American and 3 Hispanic. Charlson Comorbidity Index: 1.7 (+/‐ 2.0) | |
| Interventions | 1) Acupuncture plus standard therapy: Acupuncture twice a week for 5 weeks. Total 10 sessions. 30‐gauge needles with electrical stimulation (4 to 6 Hz) with a pulse duration of 0.5 ms. Teh Chi response at all points were verified. Between 10 and 14 needles were used per session. Needle retention was 20 minutes. Fixed acupoints: UB23, 24, 25, 28 (bilateral). Du3 and 4. Supplementary acupoints: maximum 4 additional needles: UB36, 54, 37, 40, GB 30, 31. 2) Standard therapy: Primary physician for 5‐week intervention period: NSAID, aspirin, non‐narcotic analgesic. Continue back exercise (physical therapy) or home exercise regimen. Prohibited: narcotics, muscle relaxants, TENS, epidural steroid injections and trigger point injections. | |
| Outcomes | 1) Back specific functional status (modified Roland Disability Questionnaire) These outcomes were measured at 0, 2, 6 and 9 weeks during the trial period, but we only used the measures at 6 weeks (at the end of all sessions) and 9 weeks (3 to 4 weeks after the end of the sessions) . Costs: not reported Complications: no difference in adverse effects. | |
| Notes | Language: English Publication: full paper For results, see the comparisons: Conclusions: "Our data indicate that acupuncture plus standard therapy does decrease back pain and disability in older patients compared with standard therapy alone in a clinically and statistically significant manner" | |
| Methods | ‐Randomized (computer generated) stratified according to pain duration. Central telephone randomisation. | |
| Participants | 186 patients with low‐back pain lasting longer than 6 weeks, with average pain scores greater than 50 mm (max 100 mm) during the last week. Aged between 20 and 60 years old, and speak German. Excluded: sciatica, neurological disorder, disc or spine surgery, bone or joint disorder, previous treatment with acupuncture, psychiatric illness, pregnancy, regular intake of analgesics, off work longer than 6 months, no litigation. Mean age: 50 years old Gender: 97 males and 89 females. Mean duration of pain: 9.9 years. Working status: not reported Previous treatments: not reported | |
| Interventions | 1) Verum acupuncture plus conventional orthopedic therapy. Acupuncture: standard points: BL23, 25, 40 and 60 and GB30 and 34. In addition, up to four points of maximum pain "Ah shi points", which were often close but not necessarily identical to BL 54, 31, 32 were needled. Needle insertion ranged from 1 to 10 cm and needle manipulation was mild to strong. A Teh Chi feeling was always achieved. During the acupuncture treatment, no additional treatment was administered. All patients received 12 verum acupuncture treatments, 3/week, each lasting for 30 minutes. 2) Sham acupuncture plus conventional orthopedic therapy. Sham acupuncture received 12 sham acupuncture treatments, 3/week, each lasting 30 minutes. Sham acupuncture was standardized to ten needles applied superficially (depth of needle insertion was less than 1 cm) at defined non‐acupuncture points of the lumbar region, and five needles on either side of the back. 3) The conventional orthopedic therapy consisted of: daily physiotherapy, physical exercises, back school, mud packs, infrared heat therapy. On demand they received 50 mg diclofenac up to three times a day. Injections or cortisone application of any kind were not allowed. | |
| Outcomes | 1) Pain intensity (VAS) during the last 7 days. All outcomes were taken at the end of the treatment period and 3 months later. Costs: not reported Complications: no side effects or complications occurred in any treatment group | |
| Notes | Language: English Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "Together with conservative orthopedic standard therapy, acupuncture helps to decrease pain intensity directly after treatment, and patients' rating of the acupuncture treatment is significantly better than that of the standard therapy alone. The therapeutic effect lasts for at least 3 months after the end of treatment" | |
| Methods | ‐Randomized (method not described). Sealed envelopes. | |
| Participants | 26 patients with non‐specific low‐back pain of variable duration Excluded: (1) osteoarthritis of lumbar spine, osteoporosis, scoliosis, spondylolysis, spondylolisthesis, herniation of lumbar disc, spinal stenosis or fracture; (2) radiculopathy or neuropathy in the lower extremity; (3) urological problem, gynaecological problem, neurological problem, collagen, diabetes or malignancy; (4) increase of CRP or ESR; (5) medication of corticosteroid, immunosuppressant agent, NSAID or muscle relaxant; (6) problem of general condition; (7) dementia; (8) pregnancy; (9) elderly patient; (10) those who were judged to be inappropriate for the trial by the authors. Mean age: 51 years old Gender: 7 males and 19 females Working status: not reported Previous treatments: not reported | |
| Interventions | 1) Needling points in lumbar area were chosen from BL23, 25, 32, 52 and 2 extra channel points near the spinous process of L4 and L5, and that in lower extremity were chosen from BL37, 40, 57, ST36, GB34 by palpation. Manual acupuncture technique such as needle retention and sparrow pecking technique were performed. Electro‐acupuncture was applied in some cases. Other details in technique not reported. Patients were treated twice a week for two weeks, i.e. four sessions in total. 2) Oral medication, which includes NSAID and/or kampo medicine (Chinese herbs). | |
| Outcomes | 1) Pain relief (VAS) on average on the pervious day, rated by the patient. Higher values are better. Outcomes were measured Immediately at the end of all sessions. Costs: not reported Complications: not reported | |
| Notes | This study reports on two distinct trials, but we used only the data from one trial, which was randomised. The other trial allocated patients using alternation, therefore it was not randomised. Language: Japanese Publication: abstract (and unpublished report). We obtained additional information from authors For results, see the comparisons: Conclusions: "Results of acupuncture are the same as those of medication for low‐back pain" | |
| Methods | ‐Multicentric study. | |
| Participants | 68 patients with low‐back pain (at least 2 weeks) and age 20 years or older. Diagnoses: lumbago (22), lumbar spondylosis (15), discopathy (9), acute low‐back pain (3), spondylolysis (3) , spondylolisthesis (1), sacroiliitis (1) and unclassified (10). Excluded: (1) neurological findings, pain or numbness in lower extremity; (2) malignancy, (3) infection or inflammatory disease; (4) fracture; (5) lumbago due to urological problem, gynaecological problem, digestive problem or cardio‐vascular problem; (6) patients who can not stop other conflicting or ongoing treatments; (7) problem of general condition; (8) dementia; (9) pregnancy; (10) other patients who were judged to be inappropriate for participating in the trial. Mean age: 37 years old Gender: 35 females and 29 males. Working status: not reported Previous treatments: not reported | |
| Interventions | 1) Needling points were chosen by palpation from the part of quadratus lumborum (around BL52) and/or erector spinae (around BL23 and BL26) in the lumbar area. Two points were used bilaterally ‐ in total four points ‐ for each treatment. Patients were treated twice a week for two weeks. 2) TENS: Same points as above. Two points were used bilaterally ‐ in total four points ‐ for each treatment. Patients were treated twice a week for two weeks, i.e. four sessions in total. | |
| Outcomes | 1) JOA (Japan Orthopaedic Association) Score rated by the physician. Subjective symptoms of back pain and restriction of daily activities. Maximum 20 points. Higher values are better. These outcomes were taken after the end of the 4 sessions. Costs: not reported Complications: no adverse event was reported in the electroacupuncture group. In the TENS group: 1 itching and 1 dullness after session. | |
| Notes | Duration of low‐back pain mixed. Language: English and Japanese Publication: full paper We obtained additional information from the authors. For results, see the comparisons: Conclusions: "There was no significant difference between groups in any parameter" | |
| Methods | ‐Randomized (using draws). Stratified by pain duration and gender. Using sealed and numbered envelopes, but the person doing the randomisation was not independent. | |
| Participants | 20 students of acupuncture college who were suffering from lumbago. Excluded: sciatica Duration of pain: Mean 40.4 months in distal group and 81.0 months in local group. Mean age: 26.4 years old in distal group and 35.8 years in local group. Gender: 17 males and 3 females Working status: all students. Previous treatments: not described | |
| Interventions | 1) Distal point technique: At the acupuncture points in lumber area: BL23, 26 and Yao‐yan (extra‐point: EX‐B7), acupuncturist mimicked needle insertion: tapped head of needle guide tube, then gesture of needling was performed. Acupuncture points in lower extremity: BL37, 40 and 58, were needled by real acupuncture needle (40 mm in length and 0.2 mm in diameter). Insertion depth was 1 to 2 cm. Sparrow‐picking technique was performed 5 times, then needles were removed. Participants were treated once a week for 3 weeks. 2) Local points technique: Acupuncture points in lumber area: BL23, 26 and Yo‐gan (extra‐point: EX‐B7), were needled by real acupuncture needle (40 mm in length and 0.2 mm in diameter). Insertion depth was 1 to 2 cm. Sparrow‐picking technique was performed 5 times, then needles were removed. At the acupoints in lower extremity: BL37, 40 and 58, acupuncturist mimicked needle insertion: tapped head of needle guide tube, then gesture of needling was performed. Participants were treated once a week for 3 weeks. | |
| Outcomes | 1) Pain (VAS) All these outcomes were measured immediately before and after the treatment. Costs: not reported Complications: not reported | |
| Notes | Language: Japanese Publication: abstract only We obtained additional information from authors. For results, see the comparisons: Conclusions: "There is no difference between the effects of lumbar area needling and that of distal point needling" | |
| Methods | ‐ Randomized (method not described). No description of concealment of allocation. | |
| Participants | 43 patients from 2 clinics with nociceptive LBP for 6 months or more, restriction of trunk or hip movement due to pain, restriction of ADL, muscle spasm. Excluded: previous surgery, claudication, depression, neurosis, clinical examination not nociceptive. Diagnoses: Osteoarthritis, sacroiliac joint, sciatica, intervertebral disc degeneration, disc prolapse, lumbar strain, osteoporosis Demographics and patients characteristics: not reported, but they say there were no significant differences between the groups. | |
| Interventions | 1) Acupuncture: three different modes of acupuncture: a) manual stimulation, b) low frequency (2 Hz) and c) high frequency (80 Hz) electrical stimulation of needles. Six local points (3 pairs of paraspinal points: UB 23, 25, 26 or 32) and 3 to 4 distal points (SI 6, UB40 or 60, GB 30 or 34 or St36). Insertion 1 to 5 cm, rotation producing Teh Chi, 10 sessions of 30 minutes; 2 registered physiotherapists trained in acupuncture. 2) Waiting list controls, no treatment. | |
| Outcomes | 1) Pain: number of words from chart of 83 words describing pain intensity Outcomes were measured after 6 weeks and 6 months. Costs: not reported Complications: not reported | |
| Notes | Randomization only for comparison acupuncture versus WLC, not for different modes of acupuncture. Language: English Publication: full paper No additional information from authors Results see comparisons: The authors found significant differences for pain outcomes, however, when we entered this data in RevMan (comparison 05.01) this was not significant. Because we did this based on the data extracted from the figure, we decided to follow the author's conclusions. Functional outcomes had to be transformed to effect sizes (comparison 05.07 to be combined with another trial) Conclusions: "After 6 weeks, patients receiving acupuncture were statistically significantly better than the control group on measures of pain, global improvement and mobility. The same results were observed at 6 months, but only for the group that received low frequency electroacupuncture". | |
| Methods | ‐Randomized. Computer‐generated random number were used to make a sequence of sealed envelopes. An independent person prepared an allocation table and sealed envelopes. | |
| Participants | 20 patients with low‐back pain of at least 2 weeks and over 20 years old. Excluded: radiculopathy or neuropathy, fracture, tumour, infection or internal disease, other general heath problem and conflicting or ongoing treatments. Duration of low back pain: acupuncture group=2900 days (+/‐ 1983) and TENS group=3120 days (+/‐ 3306). Mean age: 45 years old Gender: 3 males and 16 females. Working status: not described Previous treatments: acupuncture (4) | |
| Interventions | 1) Acupuncture: Points selected by tenderness and palpable muscle bands detected on the lower back and the buttock. Four points bilaterally (8 in total) were used for each treatment. Points most frequently used were BL23 and BL26. Two types of disposable stainless steel needles were used, depending on stature and fat: 0.20 mm in diameter and 50 mm in length and 0.24 mm in diameter and 60 mm in length. Needles were inserted into the muscles. The average insertion depth was approximately 20 mm. Electrostimulation was applied to the inserted needles with an electronic stimulator with a frequency of 1 Hz for 15 minutes. Press tack needles were inserted after EA at four of the 8 chosen points and left in situ for several days, they are 1.3 mm long projecting from the sticky side of a small round adhesive dressing. 2) TENS: Gel type disposable electrodes of 20x30 mm were used for 8 points. Electro‐stimulation was applied in the same manner as in the acupuncture group. The intensity was adjusted to the maximum comfortable level, and muscle contraction was observed. After each session, a poultice containing methyl salicylic acid, menthol and antihistamine was prescribed to be applied to the low‐back region, at home, in‐between treatments. | |
| Outcomes | 1) Pain (VAS): average pain level on the previous day. These outcomes were measured 3 days after the last session. Costs: not reported Complications: no adverse events reported by the evaluator. The therapists reported transient aggravation of symptoms in the acupuncture group (1), discomfort due to tack needles (1), pain on needle insertion (1) and small subcutaneous bleeding (1). In the TENS group: transient aggravation (1), transient fatigue (1) and itching (1). | |
| Notes | Language: English Publication: full paper For results, see the comparisons: Conclusions: "The results of the present trial showed a significant between‐group difference in pain relief in favour of acupuncture" | |
| Methods | ‐Randomization procedure not described. | |
| Participants | 65 patients from an orthopedic clinic with lumbago and/or ischias, no relief after conventional treatment. Diagnoses: Lombociatalgia (30), low‐back pain (20), LWS Syndrome (10) and Ischialgia (5). Exclusion criteria: neurological problems, scoliosis, concurrent treatment, acute disc prolapse or protrusion, chronic degenerative disorders, infection. Age and gender: not described. Heterogeneous population regarding type, location and duration of disorder. | |
| Interventions | 1) Manual acupuncture, traditional meridian acupuncture or trigger points, rotation, insertion 0.2 to 3 cm, 6 to 12 needles 5 to 20 minutes, 8 treatments. Training & experience of acupuncturists unknown. 2) Sham acupuncture, no traditional acupuncture nor trigger points. | |
| Outcomes | 1) Pain (VAS) | |
| Notes | Language: German Publication: full paper No additional information from authors Results: Conclusions: "The difference in improvement between typically and atypically treated patients was highly significant (p<0.0001)." | |
| Methods | ‐Randomized (method not reported). No description of concealment of allocation. | |
| Participants | 492 patients with low‐back pain of unknown duration. Diagnoses: back pain Exclusion criteria not reported. Gender: 231 males and 261 females. Working status: not reported Previous treatments: not reported | |
| Interventions | 1) Local treatment plus cupping. Teh Chi sensation was obtained and needles were retained for 20 minutes. Points: BL23, 25 and 32. Treatments were given daily up to 10 treatments. 2) Distal treatment plus electrical stimulation. Points: ST36, GB 39, BL60 and LI4. | |
| Outcomes | 1) Overall assessment: a) cure: no pain and normal range of motion, no tenderness upon palpation, and normal life and work status. b) effective: pain is markedly improved, normal lumbar movement, no obvious tenderness upon palpation, and life and work is not affected c) no significant change. Measured 3 months after the sessions. Costs: not reported Complications: not reported | |
| Notes | The authors dichotomized at : Cure+effective versus no change. Language: Chinese Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "Local acupuncture treatment plus cupping is more effective (p<0.05) than the distal treatment plus electrical stimulation." | |
| Methods | See Wu 1991 | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Methods | ‐Randomized (based on odd or even number of the date of patient admission). No mention of concealment of allocation | |
| Participants | 150 patients with acute low‐back pain. Exclusion criteria not described Age between 20 and 55 years old Gender: 105 males and 45 females Working status: not described Previous treatments: not described | |
| Interventions | 1) SI3 point treatment 2) Extra 29 (EX‐UE7) treatment Manual acupuncture technique (no electro‐stimulation) was used. Strong Teh Chi sensation was obtained combined with lumbar spine movement until symptom relieved. No mention of the duration of the treatment. | |
| Outcomes | 1) Global assessment (pain and range of motion). Costs: not reported Complications: not reported | |
| Notes | The authors dichotomized at: Language: Chinese Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "Acupuncture point SI 3 is more effective than the point Yaotongxue." | |
| Methods | ‐Randomized in blocks (method not described). Randomization was blinded. | |
| Participants | 52 patients with chronic low‐back pain (>6 months) with or without radiation. Age between 18 and 75 years. Diagnoses: non‐specific low‐back pain. Excluded: 1. Structural deformity (ankylosing spondylitis, scoliosis) 2. Lower limb fracture 3. Tumours 4. Spinal infection 5. Cauda equina syndrome 6. Pregnancy 7. Spinal cord compression 8. Subjects who were unable to keep the appointments 9. Receiving acupuncture treatment within the past 6 months 10. Receiving physiotherapy treatment within the past 3 months Mean age: 53 years old Gender: 9 males and 43 females Working status: not described Previous treatments: tui na, massage, chiropractor, bone setter or corset. | |
| Interventions | 1) Electro‐acupuncture: 3/week for 4 weeks by a physiotherapist certificated in acupuncture. Points were chosen according to the literature: BL23, BL25, BL40 and SP6. Acupuncture was applied to the side on which patients reported pain. If the reported pain was bilateral, EA was applied to the more painful side. Sterilised disposable needles, number 30 (0.3 mm) 40‐mm long needles were inserted and manipulated until Teh Chi was obtained. Electrical stimulation on needles at a frequency of 2 Hz for 30 minutes. The intensity of the stimulation was set at the level that the patient could tolerate and often with evoked visible muscle contractions. The current had biphasic waveform to the four selected acupoints in two pairs. In addition, all patients also received exercise therapy, the same as in the control group. 2) Standard group exercise program led by the same physiotherapist. | |
| Outcomes | 1) Pain: Numerical rating scale for "average" and for "worst" pain intensity during the last week, by asking the patient to rate perceived level of pain on a scale from 0 to 10, where 0 represents no pain and 10 represents pain as bad as it could be. These outcomes were measured immediately after, 1 month and 3 months after. Costs: not reported Complications: no adverse reaction or complication. | |
| Notes | Language: English Publication: full paper No additional information from authors For results, see the comparisons: Conclusions: "Significantly better scores in the NRS and Aberdeen LBP scale were found in the exercise plus EA group immediately after treatment, at 1‐month follow‐up and at 3‐month follow‐up" | |
Key:
CAM = complementary and alternative medicine
ADL = activities of daily living
WLC = waiting list control
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Sciatica | |
| Acute sciatica of disc origin. | |
| Not randomised | |
| Acupuncture treatment did not involve needling. | |
| Lumbar spinal canal stenosis | |
| Percentage of low‐back pain unknown | |
| Percentage of low‐back pain unknown | |
| Specific causes of low‐back pain | |
| Acupuncture treatment did not involve needling. | |
| Not randomised | |
| No back pain | |
| Sciatica | |
| Sciatica | |
| Sciatica | |
| Not randomised | |
| Lumbar disc herniation | |
| Sciatica | |
| Acupuncture treatment did not involve needling. | |
| Not randomised | |
| Not randomised | |
| No mention of low‐back pain, only musculoskeletal pain. | |
| Not randomised | |
| Not randomised | |
| Not randomised | |
| Lumbar disc surgery | |
| Pregnancy | |
| Sciatica | |
| Not randomised | |
| Back (n=15) and neck (n=8) and it is a preliminary report | |
| Not randomised | |
| Not randomised | |
| Not randomised |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Efficacy of Acupuncture for Chronic Low Back Pain |
| Methods | |
| Participants | Low Back Pain |
| Interventions | Acupuncture |
| Outcomes | |
| Starting date | Funding: National Center for Complementary and Alternative Medicine (NCCAM) |
| Contact information | Janet Erro, RN [email protected] Study chairs or principal investigators Daniel Cherkin, PhD, Study Director, Group Health Cooperative Center for Health Studies Study ID Numbers R01 AT001110‐01 A1 |
| Notes | Source: www.controlled‐trials.com |
| Trial name or title | German Acupuncture Trials |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | http://www.gerac.de/index1.html |
| Notes |
| Trial name or title | Physical CAM Therapies for Chronic Low Back Pain |
| Methods | |
| Participants | Chronic Low Back Pain |
| Interventions | Procedure: massage therapy |
| Outcomes | Study Design: Treatment, Randomized, Open Label, Active Control, Parallel Assignment |
| Starting date | Funding: NIH |
| Contact information | Expected Total Enrollment: 120 More Information |
| Notes | Source: www.controlled‐trials.com |
| Trial name or title | |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes |
| Trial name or title | Randomised controlled single‐blinded trial of deep intra‐muscular stimulation in the treatment of chronic mechanical low back pain. |
| Methods | |
| Participants | Out‐patients between 18 and 65 years old |
| Interventions | |
| Outcomes | |
| Starting date | |
| Contact information | Dr Rajesh Munglani |
| Notes | Source: www.controlled‐trials.com |
| Trial name or title | Longer term clinical and economic benefits of offering acupuncture to patients with chronic low back pain. |
| Methods | |
| Participants | patients with low back pain. Age 20‐65 years with low back pain or sciatica, greater than 4 weeks and less than 12‐months pain this episode |
| Interventions | i) traditional Chinese acupuncture, up to 10 treatments ii) standard care offered by GP only |
| Outcomes | |
| Starting date | Funding: NHS |
| Contact information | Ms Kate Thomas |
| Notes | Source: www.controlled‐trials.com |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (VAS) (lower values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 1 pain (VAS) (lower values are better). | ||||
| 1.1 Immediately after end of sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 functional status (higher scores are better). Generic instrument Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 2 functional status (higher scores are better). Generic instrument. | ||||
| 2.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 physical examination: finger‐floor distance (lower values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 3 physical examination: finger‐floor distance (lower values are better). | ||||
| 3.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 mean difference in pain (final ‐ initial) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 4 mean difference in pain (final ‐ initial). | ||||
| 4.1 Immediately after end of sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 mean difference in functional status (final ‐ initial) Generic instrument Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 5 mean difference in functional status (final ‐ initial) Generic instrument. | ||||
| 5.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 mean difference in physical examination (final ‐ initial): finger‐floor distance Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.6  Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 6 mean difference in physical examination (final ‐ initial): finger‐floor distance. | ||||
| 6.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (VAS): lower values are better Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 acupuncture versus other intervention ((Sub)acute LBP: < 3 months), Outcome 1 pain (VAS): lower values are better. | ||||
| 1.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 global measure (higher values are better) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 acupuncture versus other intervention ((Sub)acute LBP: < 3 months), Outcome 2 global measure (higher values are better). | ||||
| 2.1 Long‐term follow‐up (more than 1 year) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 physical examination (finger floor distance) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 acupuncture versus other intervention ((Sub)acute LBP: < 3 months), Outcome 3 physical examination (finger floor distance). | ||||
| 3.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Side effects / Complications Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 2.4  Comparison 2 acupuncture versus other intervention ((Sub)acute LBP: < 3 months), Outcome 4 Side effects / Complications. | ||||
| 4.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 global measure Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 acupuncture versus acupuncture. ((Sub)acute LBP: < 3 months), Outcome 1 global measure. | ||||
| 1.1 Immediately after the end of the sessions | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (instruments: VAS and number of words) Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 4.1  Comparison 4 acupuncture versus no treatment. (Chronic LBP: > 3 months), Outcome 1 pain (instruments: VAS and number of words). | ||||
| 1.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.73 [‐1.19, ‐0.28] |
| 1.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.78 [‐1.52, ‐0.04] |
| 2 global measure (improvement) Show forest plot | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 4.2  Comparison 4 acupuncture versus no treatment. (Chronic LBP: > 3 months), Outcome 2 global measure (improvement). | ||||
| 2.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 functional status (higher values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.3  Comparison 4 acupuncture versus no treatment. (Chronic LBP: > 3 months), Outcome 3 functional status (higher values are better). | ||||
| 3.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 limitation of activity (higher values are worse) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.4  Comparison 4 acupuncture versus no treatment. (Chronic LBP: > 3 months), Outcome 4 limitation of activity (higher values are worse). | ||||
| 4.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 functional status (standardized measures) Show forest plot | 2 | Effect size (Random, 95% CI) | Subtotals only | |
| Analysis 4.5  Comparison 4 acupuncture versus no treatment. (Chronic LBP: > 3 months), Outcome 5 functional status (standardized measures). | ||||
| 5.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | 90 | Effect size (Random, 95% CI) | 0.63 [0.19, 1.08] |
| 5.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | 40 | Effect size (Random, 95% CI) | 0.03 [‐0.70, 0.76] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 pain (lower values mean better) Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.1  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 1 pain (lower values mean better). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.1 Immediately after the end of the sessions | 4 | 314 | Mean Difference (IV, Random, 95% CI) | ‐10.21 [‐14.99, ‐5.44] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | 138 | Mean Difference (IV, Random, 95% CI) | ‐17.79 [‐25.50, ‐10.07] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.3 Intermediate‐term follow‐up (3 months to 1 year) | 2 | 96 | Mean Difference (IV, Random, 95% CI) | ‐5.74 [‐14.72, 3.25] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.4 Long‐term follow‐up (more than 1 year) | 1 | 27 | Mean Difference (IV, Random, 95% CI) | ‐12.0 [‐41.83, 17.83] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2 global improvement (higher values are better) Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.2  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 2 global improvement (higher values are better). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.1 Immediately after the end of the sessions | 3 | 234 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.04, 1.46] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 3 | 171 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.92, 2.24] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.89, 1.60] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.4 Long‐term follow‐up (more than 1 year) | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 3.29 [0.85, 12.80] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3 pain disability index (lower values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.3  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 3 pain disability index (lower values are better). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4 physical examination (fingertips‐to‐floor distance).( Lower values are better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.4  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 4 physical examination (fingertips‐to‐floor distance).( Lower values are better). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5 improvement in physical examination Show forest plot | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.5  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 5 improvement in physical examination. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6 Sick leave (higher values mean worse) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.6  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 6 Sick leave (higher values mean worse). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6.1 Intermediate‐term follow‐up (3 months to 1 year) | 2 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.22, 1.54] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7 Well being (SF‐36). (Higher values are better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.7  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 7 Well being (SF‐36). (Higher values are better). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8 Side effects / Complications Show forest plot | 3 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.8  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 8 Side effects / Complications. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8.1 Immediately after the end of the sessions | 2 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 8.2 Intermediate‐term follow‐up (3 months to 1 year) | 2 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9 pain (percent of baseline values) Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.9
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 9 pain (percent of baseline values). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9.2 Intermediate‐term follow‐up (3 months to 1 year) | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 9.3 Long‐term follow‐up (more than 1 year) | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10 sick leave Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.10
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 10 sick leave. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 10.1 Long‐term follow‐up | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11 general level of pain (0‐15 points)(more points mean less pain) Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.11
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 11 general level of pain (0‐15 points)(more points mean less pain). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11.1 Immediately after the end of the sessions | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 11.2 Intermediate‐term follow‐up (3 months to 1 year) | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12 pain: difference between within group changes Show forest plot | 1 | differences between (Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.12  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 12 pain: difference between within group changes. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12.1 Immediately after the end of the sessions | 1 | differences between (Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 12.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | differences between (Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13 function: difference between within group changes Show forest plot | 1 | differences between (Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.13  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 13 function: difference between within group changes. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13.1 Immediately after the end of the sessions | 1 | differences between (Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 13.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | differences between (Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14 Pain: percentage of patients with >50% pain reduction Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.14  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 14 Pain: percentage of patients with >50% pain reduction. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 14.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15 spine range of motion: difference between within group changes Show forest plot | 1 | difference between (Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 5.15  Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 15 spine range of motion: difference between within group changes. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15.1 Immediately after the end of the sessions | 1 | difference between (Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 15.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | difference between (Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 pain (lower values are better) Show forest plot | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 6.1  Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 1 pain (lower values are better). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.1 Immediately after the end of the sessions | 5 | 284 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [0.21, 0.75] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | 356 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐2.74, 2.36] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.3 Intermediate‐term follow‐up (3 months to 1 year) | 2 | 356 | Std. Mean Difference (IV, Random, 95% CI) | 2.48 [1.02, 3.94] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2 back specific functional status (lower scores mean better). Ex: RDQ, Oswestry and Aberdeen Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 6.2  Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 2 back specific functional status (lower scores mean better). Ex: RDQ, Oswestry and Aberdeen. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.1 Immediately after the end of the sessions | 4 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.3 Intermediate‐term follow‐up (3 months to 1 year) | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3 return to work (higher values mean better) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 6.3  Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 3 return to work (higher values mean better). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3.1 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4 Side effects / Complications Show forest plot | 7 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 6.4  Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 4 Side effects / Complications. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4.1 Immediately after the end of the sessions | 4 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 4.3 Intermediate‐term follow‐up (3 months to 1 year) | 3 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5 pain and function (adjusted for baseline values) Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 6.5
Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 5 pain and function (adjusted for baseline values). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5.1 Immediately after the end of the sessions | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 5.3 Intermediate‐term follow‐up (3 months to 1 year) | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6 general level of pain (0‐15 points)(more points mean less pain) Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 6.6
Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 6 general level of pain (0‐15 points)(more points mean less pain). | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6.1 Immediately after the end of the sessions | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 6.2 Intermediate‐term follow‐up (3 months to 1 year) | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7 pain: difference between within group changes Show forest plot | 1 | differences between (Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 6.7  Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 7 pain: difference between within group changes. | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 7.1 Immediately after the end of the sessions | 1 | differences between (Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1 pain (lower values mean better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 7.1  Comparison 7 acupuncture versus acupuncture. (Chronic LBP: > 3 months), Outcome 1 pain (lower values mean better). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2 Improvement (higher values are better) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 7.2  Comparison 7 acupuncture versus acupuncture. (Chronic LBP: > 3 months), Outcome 2 Improvement (higher values are better). | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 2.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3 improvement Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Analysis 7.3
Comparison 7 acupuncture versus acupuncture. (Chronic LBP: > 3 months), Outcome 3 improvement. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3.1 Immediately after the end of the sessions | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| 3.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 global measure (higher values are better) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 8.1  Comparison 8 dry‐needling versus other intervention ((Sub)acute LBP < 3 months), Outcome 1 global measure (higher values are better). | ||||
| 1.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 4 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Side effects / Complications Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 8.2  Comparison 8 dry‐needling versus other intervention ((Sub)acute LBP < 3 months), Outcome 2 Side effects / Complications. | ||||
| 2.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (VAS): lower values are better Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 9.1  Comparison 9 acupuncture versus placebo or sham intervention (unknown / mixed duration of low back pain), Outcome 1 pain (VAS): lower values are better. | ||||
| 1.1 Short term (immediately after end of sessions) | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 global measure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 9.2  Comparison 9 acupuncture versus placebo or sham intervention (unknown / mixed duration of low back pain), Outcome 2 global measure. | ||||
| 2.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain score (lower values mean better) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 10.1  Comparison 10 acupuncture versus other intervention (unknown / mixed duration of low back pain), Outcome 1 pain score (lower values mean better). | ||||
| 1.1 Immediately after the end of the sessions | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 pain recovery: higher values are better Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 10.2  Comparison 10 acupuncture versus other intervention (unknown / mixed duration of low back pain), Outcome 2 pain recovery: higher values are better. | ||||
| 2.1 Immediately after the end of the sessions | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 global measure (higher values are better) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 10.3  Comparison 10 acupuncture versus other intervention (unknown / mixed duration of low back pain), Outcome 3 global measure (higher values are better). | ||||
| 3.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 back specific functional status (higher scores are better). Ex: Japan Orthopedic Association Score. Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 10.4  Comparison 10 acupuncture versus other intervention (unknown / mixed duration of low back pain), Outcome 4 back specific functional status (higher scores are better). Ex: Japan Orthopedic Association Score.. | ||||
| 4.1 Immediately after the end of the sessions | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Side effects / Complications Show forest plot | 1 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 10.5  Comparison 10 acupuncture versus other intervention (unknown / mixed duration of low back pain), Outcome 5 Side effects / Complications. | ||||
| 5.1 Immediately after the end of the sessions | 1 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | |||||||||||||||||||||||||||||||||||
| 1 pain (lower values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||
| Analysis 11.1  Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 1 pain (lower values are better). | |||||||||||||||||||||||||||||||||||||||
| 1.1 Short term (immediately after end of sessions) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||
| 2 pain recovery (higher values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||
| Analysis 11.2  Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 2 pain recovery (higher values are better). | |||||||||||||||||||||||||||||||||||||||
| 2.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||
| 3 global measure (higher values are better) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||
| Analysis 11.3  Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 3 global measure (higher values are better). | |||||||||||||||||||||||||||||||||||||||
| 3.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||
| 4 functional status (higher values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||
| Analysis 11.4  Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 4 functional status (higher values are better). | |||||||||||||||||||||||||||||||||||||||
| 4.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||
| 5 physical examination (finger‐floor distance) Higher values are better. Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | ||||||||||||||||||||||||||||||||||||
| Analysis 11.5  Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 5 physical examination (finger‐floor distance) Higher values are better.. | |||||||||||||||||||||||||||||||||||||||
| 5.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | ||||||||||||||||||||||||||||||||||||
| 6 improvement Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||
| Analysis 11.6
Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 6 improvement. | |||||||||||||||||||||||||||||||||||||||
| 6.1 Long‐term follow‐up (more than 1 year) | Other data | No numeric data | |||||||||||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (lower values are better) Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 12.1  Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 1 pain (lower values are better). | ||||
| 1.1 Immediately after the end of the sessions | 4 | 289 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐1.02, ‐0.50] |
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 3 | 182 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.10 [‐1.62, ‐0.58] |
| 1.3 Intermediate‐term follow‐up (3 months to 1 year) | 2 | 115 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐1.14, ‐0.38] |
| 2 pain: difference between within group changes Show forest plot | 2 | differences between (Random, 95% CI) | Subtotals only | |
| Analysis 12.2  Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 2 pain: difference between within group changes. | ||||
| 2.1 Immediately after the end of the sessions | 2 | differences between (Random, 95% CI) | ‐1.07 [‐2.14, ‐0.00] | |
| 2.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | differences between (Random, 95% CI) | ‐0.7 [‐1.33, ‐0.07] | |
| 2.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | differences between (Random, 95% CI) | ‐0.8 [‐1.80, 0.20] | |
| 3 pain disability index (lower values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 12.3  Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 3 pain disability index (lower values are better). | ||||
| 3.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain: percentage of patients with >50% pain reduction Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 12.4  Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 4 Pain: percentage of patients with >50% pain reduction. | ||||
| 4.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 function: difference between within group changes Show forest plot | 2 | differences between (Random, 95% CI) | Subtotals only | |
| Analysis 12.5  Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 5 function: difference between within group changes. | ||||
| 5.1 Immediately after the end of the sessions | 2 | differences between (Random, 95% CI) | ‐6.51 [‐14.99, 1.98] | |
| 5.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | differences between (Random, 95% CI) | ‐3.1 [‐5.26, ‐0.94] | |
| 5.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | differences between (Random, 95% CI) | ‐6.8 [‐12.60, 1.00] | |
| 6 global measure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 12.6  Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 6 global measure. | ||||
| 6.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 back specific functional status (lower scores mean better). Ex: RDQ, Oswestry and Aberdeen Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 12.7  Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 7 back specific functional status (lower scores mean better). Ex: RDQ, Oswestry and Aberdeen. | ||||
| 7.1 Immediately after the end of the sessions | 3 | 173 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.27, ‐0.63] |
| 7.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | 99 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.37, ‐0.54] |
| 7.3 Intermediate‐term follow‐up (3 months to 1 year) | 2 | 115 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.92, ‐0.18] |
| 8 spine range of motion: difference between within group changes Show forest plot | 1 | difference between (Random, 95% CI) | Totals not selected | |
| Analysis 12.8  Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 8 spine range of motion: difference between within group changes. | ||||
| 8.1 Immediately after the end of the sessions | 1 | difference between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | difference between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Side effects / Complications Show forest plot | 2 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 12.9  Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 9 Side effects / Complications. | ||||
| 9.1 Immediately after the end of the sessions | 2 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
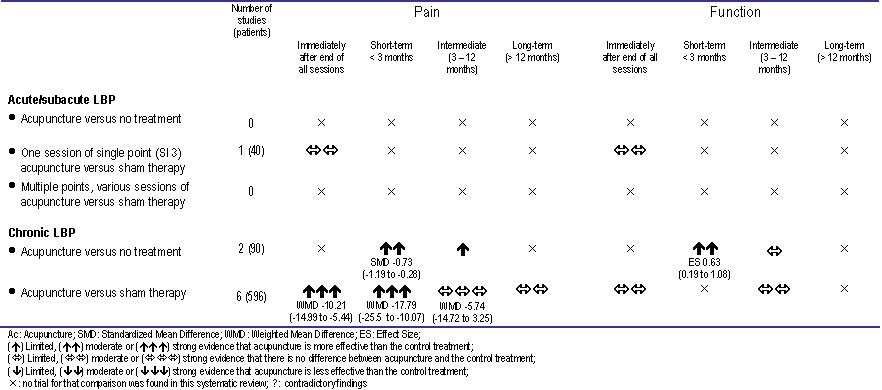
Acupuncture compared to no treatment, placebo or sham therapy

Acupuncture compared to another intervention or added to other interventions

Effects of dry‐needling at trigger points
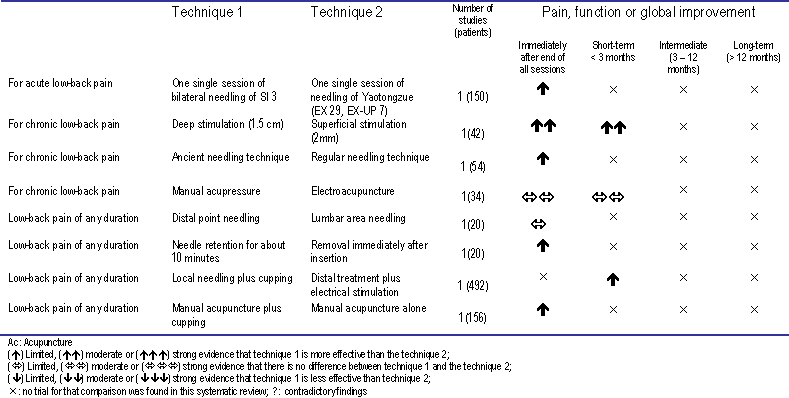
Comparison between two techniques of acupuncture

Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 1 pain (VAS) (lower values are better).

Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 2 functional status (higher scores are better). Generic instrument.

Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 3 physical examination: finger‐floor distance (lower values are better).

Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 4 mean difference in pain (final ‐ initial).

Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 5 mean difference in functional status (final ‐ initial) Generic instrument.

Comparison 1 acupuncture versus placebo or sham intervention ((Sub)acute LBP: < 3 months), Outcome 6 mean difference in physical examination (final ‐ initial): finger‐floor distance.

Comparison 2 acupuncture versus other intervention ((Sub)acute LBP: < 3 months), Outcome 1 pain (VAS): lower values are better.

Comparison 2 acupuncture versus other intervention ((Sub)acute LBP: < 3 months), Outcome 2 global measure (higher values are better).
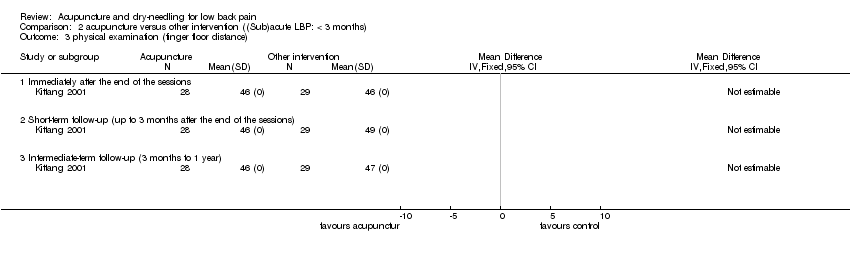
Comparison 2 acupuncture versus other intervention ((Sub)acute LBP: < 3 months), Outcome 3 physical examination (finger floor distance).
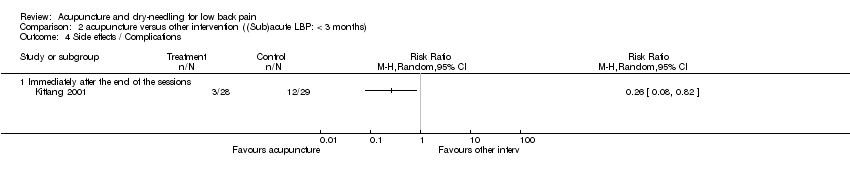
Comparison 2 acupuncture versus other intervention ((Sub)acute LBP: < 3 months), Outcome 4 Side effects / Complications.
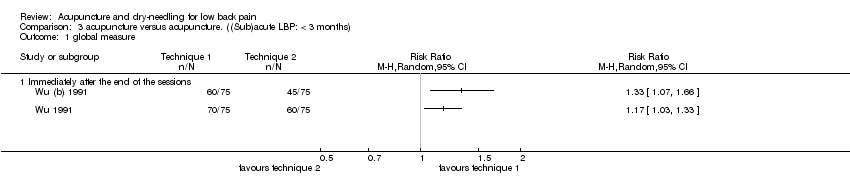
Comparison 3 acupuncture versus acupuncture. ((Sub)acute LBP: < 3 months), Outcome 1 global measure.
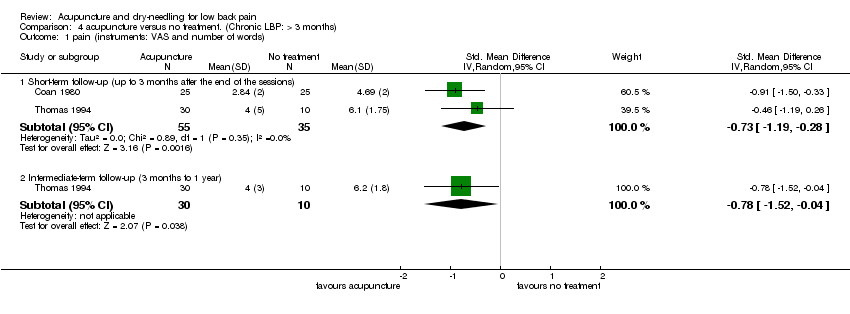
Comparison 4 acupuncture versus no treatment. (Chronic LBP: > 3 months), Outcome 1 pain (instruments: VAS and number of words).
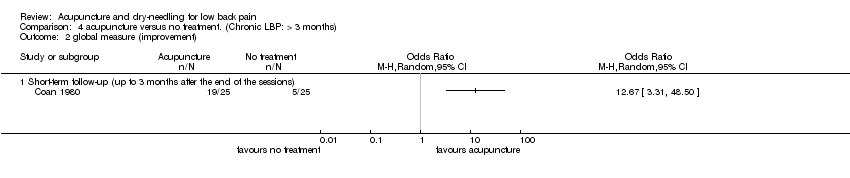
Comparison 4 acupuncture versus no treatment. (Chronic LBP: > 3 months), Outcome 2 global measure (improvement).
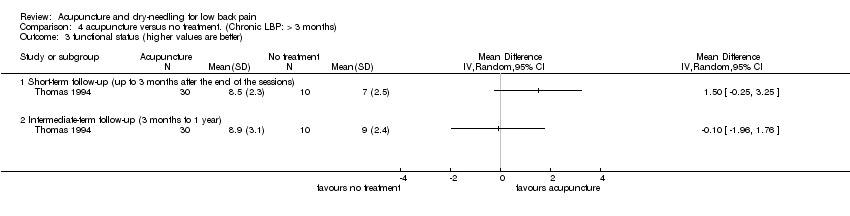
Comparison 4 acupuncture versus no treatment. (Chronic LBP: > 3 months), Outcome 3 functional status (higher values are better).

Comparison 4 acupuncture versus no treatment. (Chronic LBP: > 3 months), Outcome 4 limitation of activity (higher values are worse).
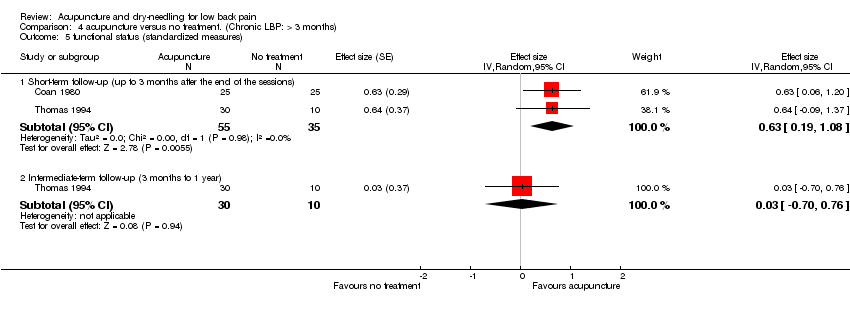
Comparison 4 acupuncture versus no treatment. (Chronic LBP: > 3 months), Outcome 5 functional status (standardized measures).

Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 1 pain (lower values mean better).
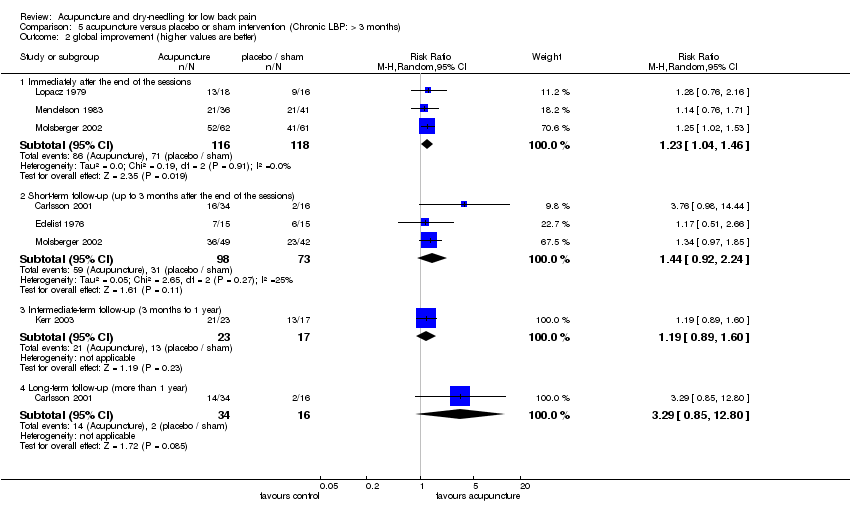
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 2 global improvement (higher values are better).

Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 3 pain disability index (lower values are better).

Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 4 physical examination (fingertips‐to‐floor distance).( Lower values are better).
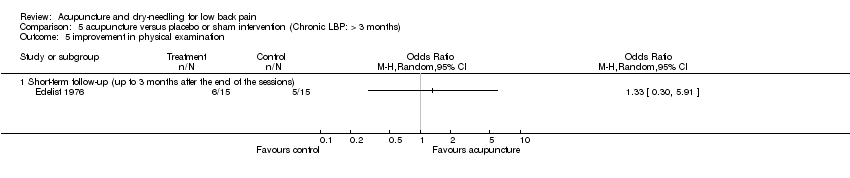
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 5 improvement in physical examination.
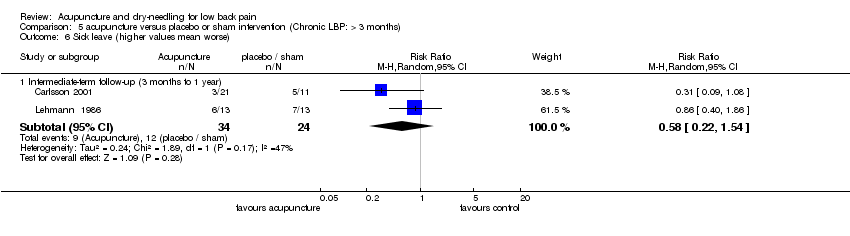
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 6 Sick leave (higher values mean worse).

Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 7 Well being (SF‐36). (Higher values are better).

Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 8 Side effects / Complications.
| Study | Group | Follow‐up | Number of patients | Percent of baseline | Standard Deviation | p value |
| Short‐term follow‐up (up to 3 months after the end of the sessions) | ||||||
| Carlsson (even) | Acupuncture | 1 month | 34 | 87% | 32 | 0.003 |
| Carlsson (even) | Placebo | 1 month | 16 | 123% | 46 | |
| Carlsson (morn) | Acupuncture | 1 month | 34 | 88% | 32 | 0.000 |
| Carlsson (morn) | Placebo | 1 month | 16 | 138% | 40 | |
| Intermediate‐term follow‐up (3 months to 1 year) | ||||||
| Carlsson (even) | Acupuncture | 3 months | 23 | 75% | 34 | 0.007 |
| Carlsson (even) | Placebo | 3 months | 9 | 120% | 50 | |
| Carlsson (morn) | Acupuncture | 3 months | 23 | 76% | 37 | 0.001 |
| Carlsson (morn) | Placebo | 3 months | 9 | 130% | 39 | |
| Long‐term follow‐up (more than 1 year) | ||||||
| Carlsson (even) | Acupuncture | 6 months or longer | 21 | 69% | 31 | 0.056 |
| Carlsson (even) | Placebo | 6 months or longer | 6 | 100% | 48 | |
| Carlsson (morn) | Acupuncture | 6 months or longer | 21 | 76% | 33 | 0.128 |
| Carlsson (morn) | Placebo | 6 months or longer | 6 | 133% | 76 | |
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 9 pain (percent of baseline values).
| Study | Group | Time | Full time work | Sick leave part‐time | Sick leave full time | p value |
| Long‐term follow‐up | ||||||
| Carlsson 2001 | Acupuncture | Baseline | 7 | 6 | 8 | |
| Carlsson 2001 | After 6 months | 11 | 7 | 3 | 0.024 | |
| Carlsson 2001 | Placebo | Baseline | 4 | 2 | 5 | |
| Carlsson 2001 | After 6 months | 5 | 1 | 5 | 0.655 | |
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 10 sick leave.
| Study | Group | Value | p value |
| Immediately after the end of the sessions | |||
| Lehmann 1986 | Acupuncture | 10.59 | F 2,50 = 1.66 (p<0.2) |
| Lehmann 1986 | TENS | 9.16 | |
| Lehmann 1986 | Sham TENS | 9.00 | |
| Intermediate‐term follow‐up (3 months to 1 year) | |||
| Lehmann 1986 | Acupuncture | 11.08 | F 2,41=3.57 |
| Lehmann 1986 | TENS | 8.28 | |
| Lehmann 1986 | Sham TENS | 7.94 | |
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 11 general level of pain (0‐15 points)(more points mean less pain).
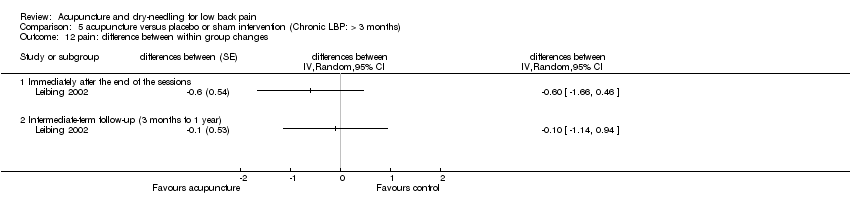
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 12 pain: difference between within group changes.
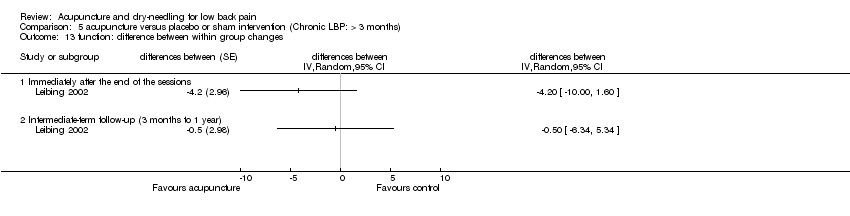
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 13 function: difference between within group changes.
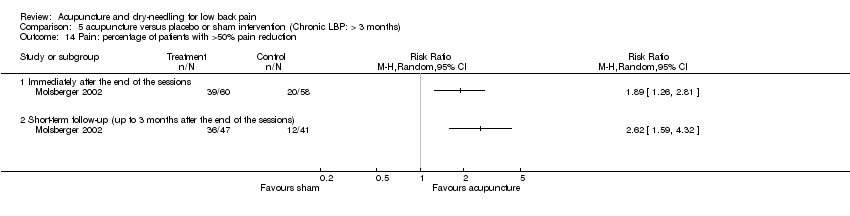
Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 14 Pain: percentage of patients with >50% pain reduction.

Comparison 5 acupuncture versus placebo or sham intervention (Chronic LBP: > 3 months), Outcome 15 spine range of motion: difference between within group changes.
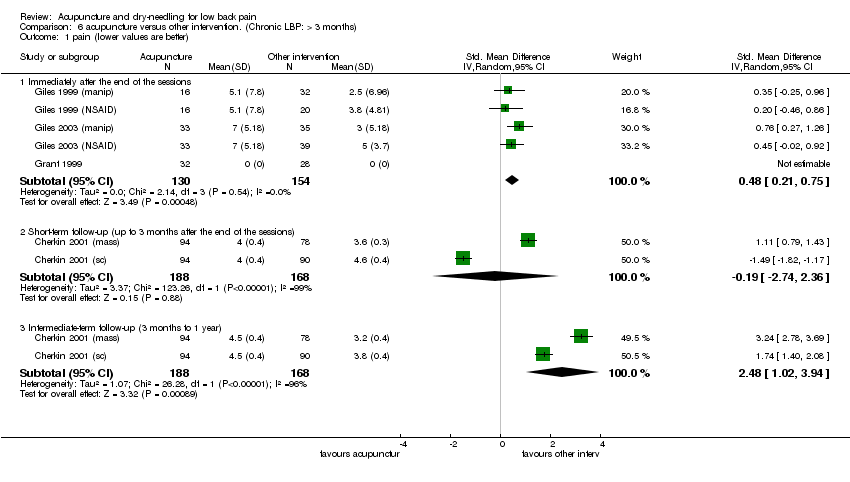
Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 1 pain (lower values are better).
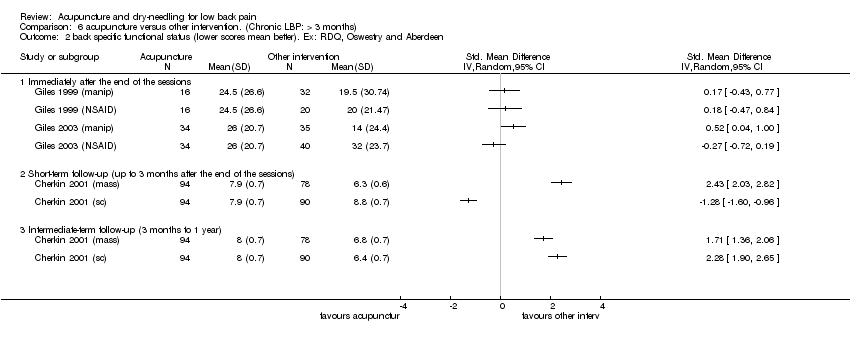
Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 2 back specific functional status (lower scores mean better). Ex: RDQ, Oswestry and Aberdeen.

Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 3 return to work (higher values mean better).
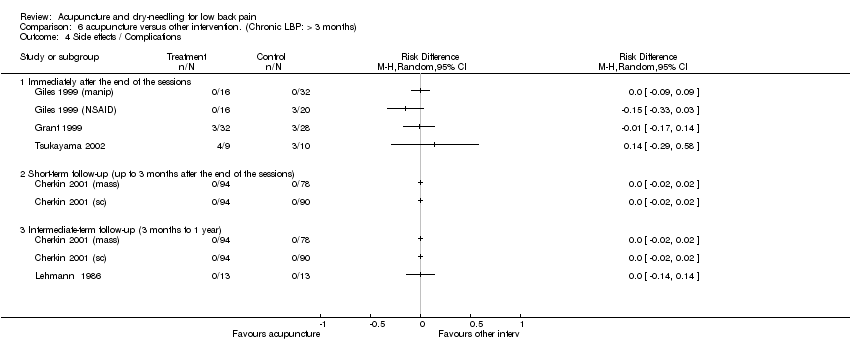
Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 4 Side effects / Complications.
| Study | Comparison | Outcome measure | Timing | p value |
| Immediately after the end of the sessions | ||||
| Tsukayama 2002 | Acupuncture versus TENS | Functional status (JOA): higher scores are better | Immediately after | 0.24 |
| Tsukayama 2002 | ||||
| Short‐term follow‐up (up to 3 months after the end of the sessions) | ||||
| Cherkin 2001 (mass) | Acupuncture versus massage | Pain | 9 weeks | 0.23 |
| Cherkin 2001 (mass) | Function | 9 weeks | 0.01 (massage is better) | |
| Cherkin 2001 (sc) | Acupuncture versus self‐care education | Pain | 9 weeks | 0.55 |
| Cherkin 2001 (sc) | Function | 9 weeks | 0.75 | |
| Intermediate‐term follow‐up (3 months to 1 year) | ||||
| Cherkin 2001 (mass) | Acupuncture versus massage | Pain | 52 weeks | 0.002 (massage is better) |
| Cherkin 2001 (mass) | Function | 52 weeks | 0.05 (massage is better) | |
| Cherkin 2001 (sc) | Acupuncture versus self‐care education | Pain | 52 weeks | 0.10 |
| Cherkin 2001 (sc) | Function | 52 weeks | 0.10 | |
Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 5 pain and function (adjusted for baseline values).
| Study | Group | Value | p value |
| Immediately after the end of the sessions | |||
| Lehmann 1986 | Acupuncture | 10.59 | F 2,50 = 1.66 (p<0.2) |
| Lehmann 1986 | TENS | 9.16 | |
| Lehmann 1986 | Sham TENS | 9.00 | |
| Intermediate‐term follow‐up (3 months to 1 year) | |||
| Lehmann 1986 | Acupuncture | 11.08 | F 2,41=3.57 |
| Lehmann 1986 | TENS | 8.28 | |
| Lehmann 1986 | Sham TENS | 7.94 | |
Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 6 general level of pain (0‐15 points)(more points mean less pain).
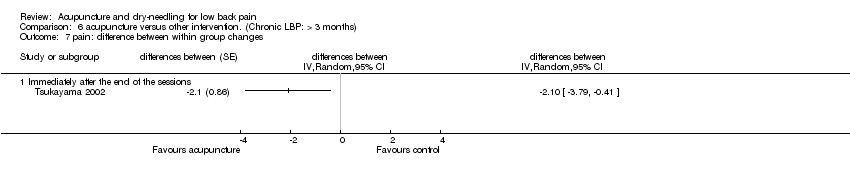
Comparison 6 acupuncture versus other intervention. (Chronic LBP: > 3 months), Outcome 7 pain: difference between within group changes.

Comparison 7 acupuncture versus acupuncture. (Chronic LBP: > 3 months), Outcome 1 pain (lower values mean better).

Comparison 7 acupuncture versus acupuncture. (Chronic LBP: > 3 months), Outcome 2 Improvement (higher values are better).
| Study | Improvement | Technique 1: Regular | Technique 2: Ancient | p value |
| Immediately after the end of the sessions | ||||
| Ding 1998 | Marked effective | 4 | 8 | |
| Ding 1998 | Improved | 6 | 3 | |
| Ding 1998 | No change | 5 | 2 | |
| Ding 1998 | ||||
| Short‐term follow‐up (up to 3 months after the end of the sessions) | ||||
| Ding 1998 | Cure | 4 | 22 | Chi‐square=12.44 |
| Ding 1998 | Marked effective | 4 | 8 | |
| Ding 1998 | Improved | 6 | 3 | |
| Ding 1998 | No change | 5 | 2 | |
Comparison 7 acupuncture versus acupuncture. (Chronic LBP: > 3 months), Outcome 3 improvement.
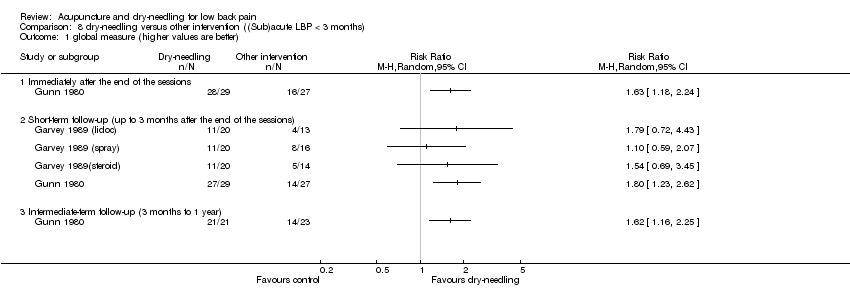
Comparison 8 dry‐needling versus other intervention ((Sub)acute LBP < 3 months), Outcome 1 global measure (higher values are better).
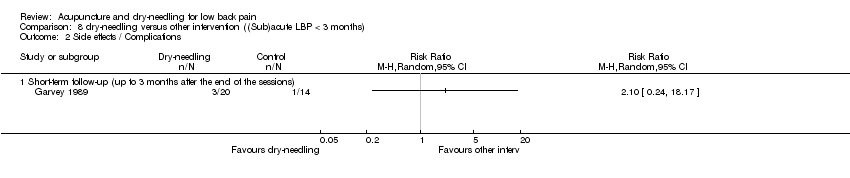
Comparison 8 dry‐needling versus other intervention ((Sub)acute LBP < 3 months), Outcome 2 Side effects / Complications.

Comparison 9 acupuncture versus placebo or sham intervention (unknown / mixed duration of low back pain), Outcome 1 pain (VAS): lower values are better.
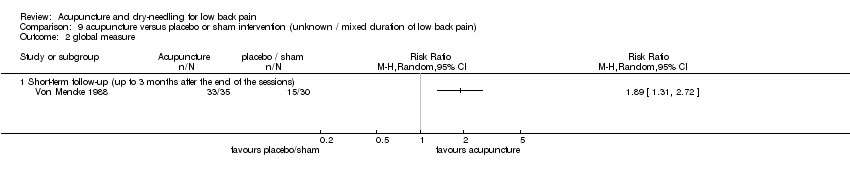
Comparison 9 acupuncture versus placebo or sham intervention (unknown / mixed duration of low back pain), Outcome 2 global measure.

Comparison 10 acupuncture versus other intervention (unknown / mixed duration of low back pain), Outcome 1 pain score (lower values mean better).

Comparison 10 acupuncture versus other intervention (unknown / mixed duration of low back pain), Outcome 2 pain recovery: higher values are better.

Comparison 10 acupuncture versus other intervention (unknown / mixed duration of low back pain), Outcome 3 global measure (higher values are better).

Comparison 10 acupuncture versus other intervention (unknown / mixed duration of low back pain), Outcome 4 back specific functional status (higher scores are better). Ex: Japan Orthopedic Association Score..
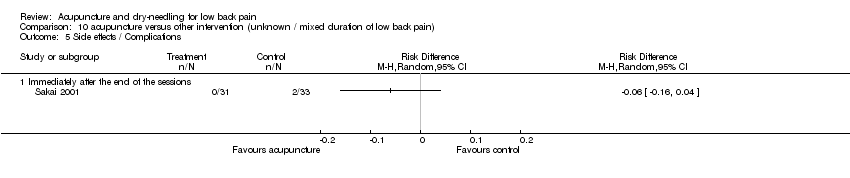
Comparison 10 acupuncture versus other intervention (unknown / mixed duration of low back pain), Outcome 5 Side effects / Complications.
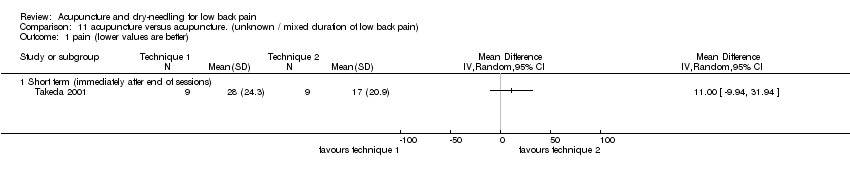
Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 1 pain (lower values are better).
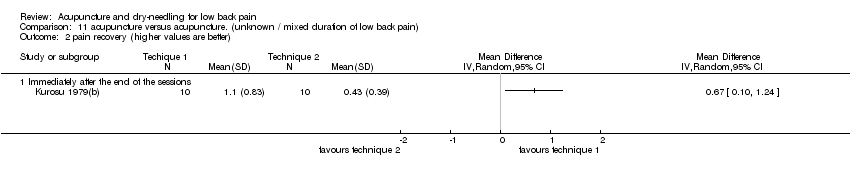
Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 2 pain recovery (higher values are better).

Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 3 global measure (higher values are better).

Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 4 functional status (higher values are better).
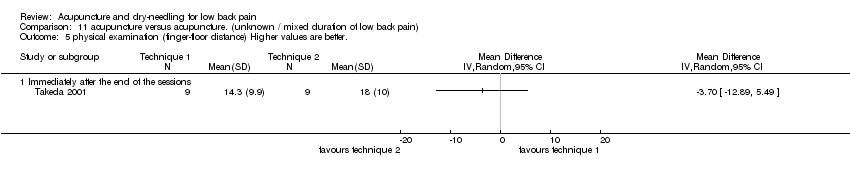
Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 5 physical examination (finger‐floor distance) Higher values are better..
| Study | Improvement | Technique 1: Ac+cupp | Technique 2: Acup | p value |
| Long‐term follow‐up (more than 1 year) | ||||
| Li 1997 | Cure | 33 | 22 | <0.01 |
| Li 1997 | Marked effective | 32 | 28 | |
| Li 1997 | Improved | 13 | 26 | |
| Li 1997 | No change | 0 | 2 | |
Comparison 11 acupuncture versus acupuncture. (unknown / mixed duration of low back pain), Outcome 6 improvement.
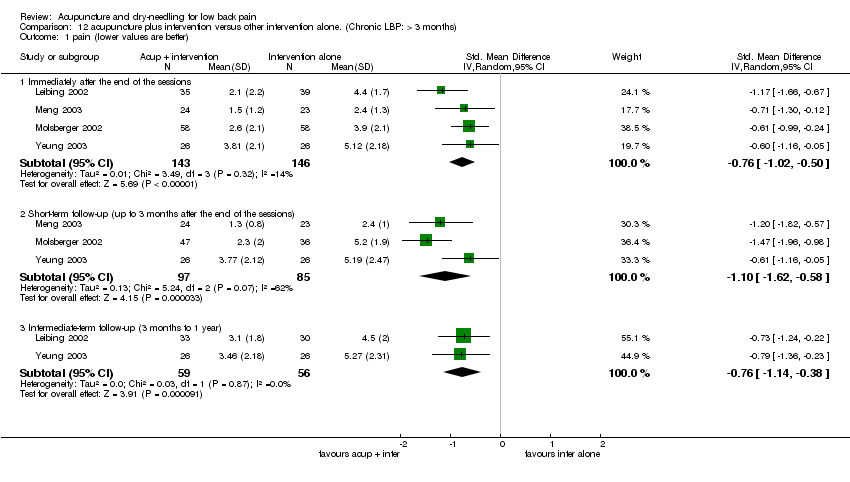
Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 1 pain (lower values are better).
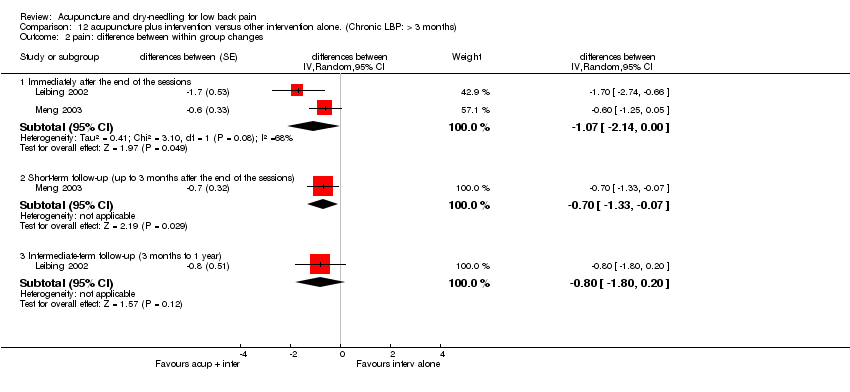
Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 2 pain: difference between within group changes.
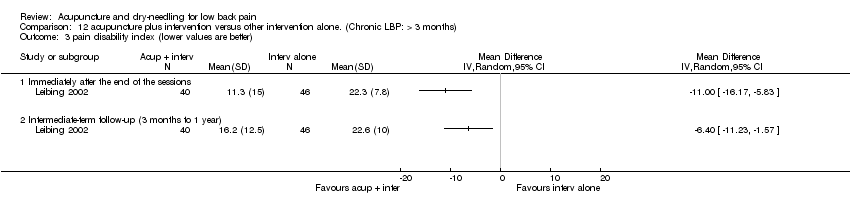
Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 3 pain disability index (lower values are better).

Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 4 Pain: percentage of patients with >50% pain reduction.

Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 5 function: difference between within group changes.
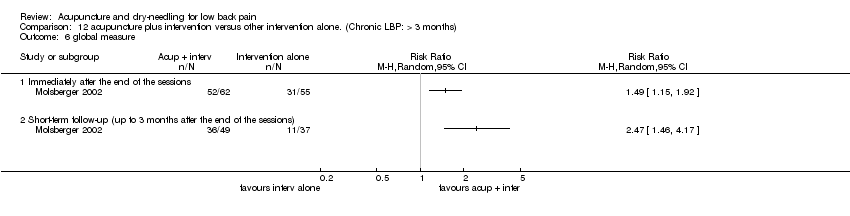
Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 6 global measure.

Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 7 back specific functional status (lower scores mean better). Ex: RDQ, Oswestry and Aberdeen.

Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 8 spine range of motion: difference between within group changes.
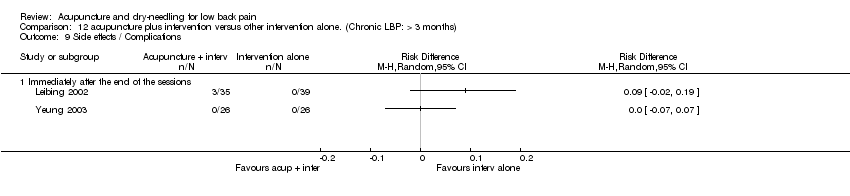
Comparison 12 acupuncture plus intervention versus other intervention alone. (Chronic LBP: > 3 months), Outcome 9 Side effects / Complications.
| Criteria | Operationalization |
| A. Was the method of randomization adequate? | A. A random (unpredictable) assignment sequence. Examples of adequate methods are computer generated random number table and use of sealed opaque envelopes. Methods of allocation using date of birth, date of admission, hospital numbers, or alternation should not be regarded as appropriate. |
| B. Was the treatment allocation concealed? | B. Assignment generated by an independent person not responsible for determining the eligibility of the patients. This person has no information about the persons included in the trial and has no influence on the assignment sequence or on the decision about eligibility of the patient. |
| C. Were the groups similar at baseline regarding the most important prognostic indicators? | C. In order to receive a "yes," groups have to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of patients with neurologic symptoms, and value of main outcome measure(s). |
| D. Was the patient blinded to the intervention? | D. The reviewer determines if enough information about the blinding is given in order to score a "yes." |
| E. Was the care provider blinded to the intervention? | E. The reviewer determines if enough information about the blinding is given in order to score a "yes." |
| F. Was the outcome assessor blinded to the intervention? | F. The reviewer determines if enough information about the blinding is given in order to score a "yes." |
| G. Were cointerventions avoided or similar? | G. Cointerventions should either be avoided in the trial design or similar between the index and control groups. |
| H. Was the compliance acceptable in all groups? | H. The reviewer determines if the compliance to the interventions is acceptable, based on the reported intensity, duration, number and frequency of sessions for both the index intervention and control intervention(s). |
| I. Was the drop‐out rate described and acceptable? | I. The number of participants who were included in the study but did not complete the observation period or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and drop‐outs does not exceed 20% for immediate and short‐term follow‐ups, 30% for intermediate and long‐term follow‐ups and does not lead to substantial bias a "yes" is scored. |
| J. Was the timing of the outcome assessment in all groups similar? | J. Timing of outcome assessment should be identical for all intervention groups and for all important outcome assessments. |
| K. Did the analysis include an intention‐to‐treat analysis? | K. All randomized patients are reported/analyzed in the group they were allocated to by randomization for the most important moments of effect measurement (minus missing values) irrespective of noncompliance and cointerventions. |
| Study | A and B | C | D, E and F | G | H | I | J | K | Comments, flaws, etc |
| Y and Y | Y | Y, N, Y | Y | Y | Y | Y | Y | Score=10 and no serious flaws (High) | |
| Y and Y | DK | Y, N, Y | DK | DK | Y (1 month); N (3 and 6 months) | Y | Y | Score=7 at 1 month (follow‐up=100%), Score=6 at 3 and 6 months (follow‐up=64% and 54% respectively) (High) | |
| Y and DK | Y | DK, N, Y | DK | DK | Y | Y | Y | Score=6. No serious flaws. (High) | |
| Y and DK | Y | N, N, Y | Y | Y | Y | Y | Y | Score=8. No serious flaws (High) | |
| Y and Y | DK | N, N, N | DK | N | N | N | N | Score=2 (Low) | |
| DK and N | DK | Y, N, N | DK | DK | Y | Y | N | Score=3 (Low). Main outcome is very subjective. | |
| DK and DK | DK | Y, N, Y | DK | Y | DK | DK | DK | Score=3 (Low). Main outcome is a subjective measure. Methods poorly described. | |
| Y and DK | DK | Y, N, Y | Y | Y | Y | Y | Y | Score=8. No serious flaws (High). Baseline characteristics are not shown. Groups are very different in size. | |
| DK and Y | DK | N, N, Y | DK | N | N | Y | N | Fatal flaw= 52% drop out during treatment period in the acupuncture group. | |
| Y and Y | Y | N, N, DK | Y | DK | N | Y | Y | Score=6. 39% drop out at 9‐weeks (Low). No adjustment for multiple comparisons | |
| Y and Y | N | N, N, Y | Y | DK | Y | Y | N | Fatal flaw= baseline differences in main outcome measures. VAS (range 0‐200) at baseline in acup group was 140 and in the TENS group was 101. | |
| N and DK | DK | N, N, DK | DK | DK | Y | N | N | Score=1 (Low). Allocation by alternation and not concealed. No mention of blinded assessments. We don't have baseline values for pain. Co‐interventions were allowed and not standardized or monitored. No ITT: this is not a big problem for the 12‐week follow‐up, but maybe for the longer term follow‐up | |
| DK and N | Y | Y, N, N | DK | DK | N | Y | DK | Score=3 (Low). No information about allocation of patients. No description of lost patients. | |
| Y and Y | DK | Y,N, Y | Y | Y | Y | Y | Y | Score=9 (High). We believe there were no losses because the follow‐up was shortly after the single session. | |
| Y and Y | DK | Y,N,Y | Y | Y | Y | Y | Y | Score=9 (High). We believe there were no losses because the follow‐up was shortly after the single session. | |
| Y and DK | DK | Y,N,Y | DK | DK | N | Y | N | Score=4 (Low). Co‐interventions might have influenced the results. Patients followed: 76% in the short and 66.7% in the intermediate follow‐ups. | |
| N and DK | N | DK,DK,Y | Y | Y | Y | Y | Y | Score=6. No serious flaws (High). Baseline differences in three factors (days of sick leave previous year, previous attendance at back schools and use of pain killers) | |
| DK and DK | DK | N, N, DK | DK | Y | DK | Y | DK | Score=2 (Low) | |
| DK and DK | DK | N, N, N | Y | DK | N | Y | N | Score=2 (Low). Follow‐up: 77% immediately after and 61% after 6 months. | |
| Y and Y | Y | Y,N, Y | Y | DK | N | Y | DK | Score=7 (High) However, drop‐out rate: 24% in the short and 37% in the long‐term | |
| DK and N | DK | Y, N, N | DK | DK | N | Y | DK | Score=2 (Low) No information about allocation of patients. No description of lost patients. | |
| DK and DK | DK | N, N, N | Y | DK | Y | Y | Y | Score=4 (Low). No information about randomisation and not blinded. | |
| DK and DK | Y | Y, N, DK | DK | DK | Y | DK | Y | Score=4 (Low). No information about randomisation and timing of follow‐up measures | |
| DK and DK | Y | Y, N, Y | DK | DK | Y | Y | N | Score=5 (Low). Cross over study. | |
| Y and Y | Y (pain); N (Roland) | N, N, N | Y | DK | Y | Y | Y | Score=7 (small difference in baseline in pain outcomes). Score= 6 (important baseline difference in RDQ (acupuncture group: 9.8 and control group: 11.8). (High) | |
| Y and Y | Y | Y, N, Y | DK | Y | Y (immed), N (short) | Y | Y | Score=9 (immediately after) and Score=8 (short‐term: drop‐out rate at 3 months was 34%) (High). Blinding was between verum and sham acupuncture, but not between verum and nothing. | |
| DK and DK | N | N,N,DK | DK | DK | N | N | DK | Score=0 (Low). Methods poorly described. A statistically significant difference was observed in disability score at baseline. ADL was 7.6 in acupuncture group and 10.3 in medication group. Other parameters such as subjective symptom of pain, JOA score, duration of pain, gender were not statistically different at baseline. | |
| Y and Y | Y | N,N, Y | Y | Y | Y | Y | N | Score=8. No serious flaws (High) | |
| Y and DK | DK | Y,N,N | DK | Y | Y | Y | DK | Score=5 (Low) | |
| DK and DK | Y | N,N, DK | N | Y | DK | Y | Y | Score=4 (Low). We get different results when we re‐analysed using the data from the figures. | |
| Y and Y | Y | N, N, Y | Y | Y | Y | Y | Y | Score=9. No serious flaws (High). Outcome assessor was blinded, but patient was not. So it is possible that the blindness was broken, especially because the outcomes are subjective. | |
| DK and DK | DK | Y, N, Y | N | N | N | N | N | Score=2 (Low) | |
| DK and N | DK | Y, N, N | DK | N | N | DK | DK | Score=1 (Low). Not adequately randomised. Doubts about reliability of outcome measures | |
| N and N | DK | Y,N,N | DK | Y | N | Y | DK | Score=3 (Low). Not adequately randomised. Doubts about reliability of outcome measures | |
| DK and Y | Y | N, N, Y | Y | Y | Y | Y | Y | Score=8. No serious flaws (High). Outcome assessor was blinded, but patient was not. So it is possible that the blindness was broken, especially because the outcomes are subjective. One of the few studies that adjusted for confounders in the analysis, but small sample size and did not account for attention effects. | |
| Total "Yes" | 17 14 | 14 | 18, 0, 19 | 15 | 15 | 20 | 28 | 16 | |
| Total "No" | 3 5 | 3 | 15, 34, 10 | 2 | 3 | 12 | 4 | 10 | |
| Total "DK" | 15 16 | 18 | 2, 1, 6 | 18 | 17 | 3 | 3 | 9 |
| Study | Patients | Interventions | Relevant outcomes | Size of effect | Benefits and harms | Serious deficiencies? |
| N | Y | Y | DK | DK | Population is poorly described. Power to detect a difference (alpha 0.05, 2‐tailed) in pain is 12% and in function is 5.1%. | |
| Y | Y | Y | Y | Y | ||
| Y | Y | N | DK | DK | ||
| Y | N | Y | DK | Y | Intervention is individualized to each patient. Pragmatic trial. | |
| Y | N | Y | Y | DK | Intervention is poorly described | |
| Y | N | Y | Y | Y | The strong and deep needling technique may not be practical for all acupuncture settings. | |
| N | Y | N | N | DK | Irrelevant outcomes. | |
| N | Y | N | Y | N | Benefists do not seem to be worth the harms | |
| N | N | Y | Y | DK | Patients and interventions are poorly described | |
| N | Y | Y | DK | DK | Difficult to interpret results due to nature of data presentation. No follow‐up beyond 9 weeks. | |
| N | N | Y | N | N | Population and interventions are poorly described | |
| Y | N | N | Y | DK | We don't know how co‐interventions were applied. We don't have a separate measure for pain. | |
| Y | N | Y | Y | DK | No description of acupuncture points used. Not sure about validity/reliability of outcome measure. | |
| N | Y | DK | N | DK | ||
| N | Y | DK | Y | Y | ||
| N | Y | Y | N | DK | No clinically important effects detected in this study | |
| Y | N | Y | N | DK | ||
| N | Y | N | DK | DK | ||
| Y | N | Y | Y | DK | No description of acupuncture points used. Not sure about validity/reliability of outcome measure. | |
| N | N | N | DK | Y | No description of acupuncture points used. Teh Chi unclear. | |
| Y | Y | Y | DK | N | ||
| N | N | N | DK | DK | Poor description of patients and interventions. | |
| Y | Y | Y | Y | DK | It is not meridian acupuncture and the depth is too superficial. Very small sample size | |
| Y | Y | Y | N | DK | ||
| Y | Y | Y | DK | DK | Size of effect might be biased by small sample size. Harms were assessed, but should be evaluated in larger sample. | |
| Y | Y | Y | Y | DK | ||
| Y | N | Y | DK | DK | Not sure about validity of JOA score. Number of points and sessions too small. | |
| Y | Y | Y | N | DK | Not sure about validity of JOA score. Number of points and sessions too small. | |
| N | Y | Y | N | DK | ||
| N | Y | Y | N | DK | ||
| Y | Y | Y | DK | N | ||
| Y | Y | Y | Y | DK | Teh Chi unclear. | |
| Y | Y | Y | Y | Y | ||
| Y | Y | Y | Y | Y | ||
| Y | Y | Y | Y | Y |
| Comparison group | Acute | Chronic | Unknown / Mixed | |
| Acupuncture | Number of studies | 2 | 16 | 8 |
| Average improvement | 52% | 32% | 51% | |
| Standard deviation | 39% | 24% | 19% | |
| Minimum | 25% | ‐17% | 22% | |
| Maximum | 80% | 62% | 77% | |
| No treatment | Number of studies | 6 | ||
| Average improvement | 6% | |||
| Standard deviation | 25% | |||
| Minimum | ‐33% | |||
| Maximum | 42% | |||
| Sham / placebo | Number of studies | 1 | 6 | 3 |
| Average improvement | 22% | 23% | 25% | |
| Standard deviation | 22% | 17% | ||
| Minimum | ‐19% | 6% | ||
| Maximum | 44% | 37% | ||
| Other treatments | Number of studies | 1 | 6 | 3 |
| Average improvement | 79% | 25% | 99% | |
| Standard deviation | 19% | 73% | ||
| Minimum | 0% | 41% | ||
| Maximum | 50% | 181% | ||
| Study | Choice of acupoints | Number of sessions | Needling technique | Experience | Control group | Comments |
| Adequate because this is acute low‐back pain | Adequate because it is acute low‐back pain | Adequate | Adequate | Appropriate sham acupuncture | But there is no description about credibility of sham acupuncture. | |
| Adequate | Adequate | Adequate | Adequate | Adequate sham TENS | The authors also compared needle acupuncture with electroacupuncture. | |
| Adequate | Adequate | Adequate for the purpose of the study, which was to compare two techniques of acupuncture. | Not reported | Other acupuncture technique | ||
| Individualized points. | Adequate | TCM typically with Teh Chi | Adequate | Other common therapies. | ||
| Not reported | Adequate | Not reported | Not reported | Waiting list. No treatment | Poorly reported, but seems OK (published in 1980). | |
| Adequate | Adequate | Adequate | Adequate | Other acupuncture technique | ||
| Adequate | Few sessions | Adequate | Not reported | Sham acupuncture (but may have some analgesic effect) | The control group used needles placed in areas devoid of classic acupuncture points. | |
| Garvey 1989 (dry needling) | Adequate (dry‐needling) | Adequate | Not reported | Not reported | Three common treatments | |
| Not reported | Adequate | Not reported. | Adequate | Two common treatments: manipulation and drugs | ||
| Not reported | Adequate | Not reported. | Adequate | Two common treatments: manipulation and drugs | ||
| Individualized points. | Adequate | Not reported. | Not reported | Another common treatment: TENS | ||
| Gunn 1980 (dry needling) | Muscle motor points. Not adequate for dry needling. | Adequate | Adequate | Not reported | Standar therapy: physiotherapy, remedial exercises, occupational therapy, industrial assessment. | |
| Adequate | Adequate | Adequate | Not reported | Chinese herbs. | No information about which herbs were used. | |
| Adequate | Adequate for the purpose of the study. | Not reported | Adequate | Sham acupuncture | But there is no description about credibility of sham acupuncture. | |
| Adequate (non meridian) | Adequate for the purpose of the study | Not reported | Not reported | Sham acupuncture | But there is no description about credibility of sham acupuncture. | |
| Adequate | Adequate | Adequate | Not reported | Sham TENS | ||
| Seems adequate | Not reported | Not reported | Not reported | Naproxen: adequate dose and duration of treatment | ||
| Adequate | Adequate for the purpose of the study. | Adequate | Not reported | Garlic moxibustion may be adequate treatment for LBP in some cases | ||
| Adequate | Adequate for the purpose of the study. | Adequate | Not reported | Other acupuncture technique (needle insertion and no retention) | ||
| Choice of meridians is OK | Adequate | Adequate | Adequate | Sham TENS | ||
| Adequate | Adequate | Adequate | Adequate | Sham acupuncture | ||
| Adequate | Adequate | Adequate | Not reported | Manual acupuncture without cupping. | ||
| Not reported | Adequate | Not reported | Not reported | Placebo: to control for attention effect. | ||
| Adequate (not meridian) | Adequate | Adequate for the purpose of the study | Not reported | Sham TENS. | It is easy for patients to perceive that they were receiving different treatments. | |
| Adequate | Adequate | Adequate | Adequate | Maybe not adequate placebo. May have some analgesic effect. | ||
| Adequate | Adequate | Adequate | Adequate | Standard therapy | ||
| Adequate | Adequate | Adequate | Adequate | Sham acupuncture: good placebo. | ||
| Adequate | Adequate for the purpose of the study | Not reported | Not reported | Medication | ||
| Adequate (not meridian) | Adequate for the purpose of the study | Not reported | Not reported | TENS: seems adequate. | But number of sessions too small. | |
| Adequate for the purpose of the study | Adequate | Not reported | Not reported | Other acupuncture technique: local versus distal points. | But there is no description about credibility of sham acupuncture. | |
| Adequate | Adequate | Adequate | Adequate | No treatment | ||
| Adequate | Adequate for the purpose of the study | Adequate | Not reported | TENS | but number of sessions too small. | |
| Adequate | Adequate | Adequate | Not reported | Sham acupuncture | ||
| Adequate | Adequate | Adequate | Adequate | Active acupuncture: distal points | ||
| Adequate (for acute LBP) | Adequate (single session for acute LBP) | Adequate | Adequate | Another active acupuncture treatment | ||
| Adequate | Adequate for the purpose of the study | Adequate | Adequate | Physiotherapy (standard exercises) | Patients in the exercise group did not receive the same attention as in the acupuncture group. |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (VAS) (lower values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Immediately after end of sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 functional status (higher scores are better). Generic instrument Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 physical examination: finger‐floor distance (lower values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 mean difference in pain (final ‐ initial) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Immediately after end of sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 mean difference in functional status (final ‐ initial) Generic instrument Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 mean difference in physical examination (final ‐ initial): finger‐floor distance Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (VAS): lower values are better Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 global measure (higher values are better) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Long‐term follow‐up (more than 1 year) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 physical examination (finger floor distance) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Side effects / Complications Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 global measure Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Immediately after the end of the sessions | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (instruments: VAS and number of words) Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.73 [‐1.19, ‐0.28] |
| 1.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.78 [‐1.52, ‐0.04] |
| 2 global measure (improvement) Show forest plot | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 functional status (higher values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 limitation of activity (higher values are worse) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 functional status (standardized measures) Show forest plot | 2 | Effect size (Random, 95% CI) | Subtotals only | |
| 5.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | 90 | Effect size (Random, 95% CI) | 0.63 [0.19, 1.08] |
| 5.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | 40 | Effect size (Random, 95% CI) | 0.03 [‐0.70, 0.76] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (lower values mean better) Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Immediately after the end of the sessions | 4 | 314 | Mean Difference (IV, Random, 95% CI) | ‐10.21 [‐14.99, ‐5.44] |
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | 138 | Mean Difference (IV, Random, 95% CI) | ‐17.79 [‐25.50, ‐10.07] |
| 1.3 Intermediate‐term follow‐up (3 months to 1 year) | 2 | 96 | Mean Difference (IV, Random, 95% CI) | ‐5.74 [‐14.72, 3.25] |
| 1.4 Long‐term follow‐up (more than 1 year) | 1 | 27 | Mean Difference (IV, Random, 95% CI) | ‐12.0 [‐41.83, 17.83] |
| 2 global improvement (higher values are better) Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Immediately after the end of the sessions | 3 | 234 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.04, 1.46] |
| 2.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 3 | 171 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.92, 2.24] |
| 2.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.89, 1.60] |
| 2.4 Long‐term follow‐up (more than 1 year) | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 3.29 [0.85, 12.80] |
| 3 pain disability index (lower values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 physical examination (fingertips‐to‐floor distance).( Lower values are better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 improvement in physical examination Show forest plot | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Sick leave (higher values mean worse) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Intermediate‐term follow‐up (3 months to 1 year) | 2 | 58 | Risk Ratio (M‐H, Random, 95% CI) | 0.58 [0.22, 1.54] |
| 7 Well being (SF‐36). (Higher values are better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Side effects / Complications Show forest plot | 3 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 Immediately after the end of the sessions | 2 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Intermediate‐term follow‐up (3 months to 1 year) | 2 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 pain (percent of baseline values) Show forest plot | Other data | No numeric data | ||
| 9.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | Other data | No numeric data | ||
| 9.2 Intermediate‐term follow‐up (3 months to 1 year) | Other data | No numeric data | ||
| 9.3 Long‐term follow‐up (more than 1 year) | Other data | No numeric data | ||
| 10 sick leave Show forest plot | Other data | No numeric data | ||
| 10.1 Long‐term follow‐up | Other data | No numeric data | ||
| 11 general level of pain (0‐15 points)(more points mean less pain) Show forest plot | Other data | No numeric data | ||
| 11.1 Immediately after the end of the sessions | Other data | No numeric data | ||
| 11.2 Intermediate‐term follow‐up (3 months to 1 year) | Other data | No numeric data | ||
| 12 pain: difference between within group changes Show forest plot | 1 | differences between (Random, 95% CI) | Totals not selected | |
| 12.1 Immediately after the end of the sessions | 1 | differences between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | differences between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 function: difference between within group changes Show forest plot | 1 | differences between (Random, 95% CI) | Totals not selected | |
| 13.1 Immediately after the end of the sessions | 1 | differences between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | differences between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Pain: percentage of patients with >50% pain reduction Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 14.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 spine range of motion: difference between within group changes Show forest plot | 1 | difference between (Random, 95% CI) | Totals not selected | |
| 15.1 Immediately after the end of the sessions | 1 | difference between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | difference between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (lower values are better) Show forest plot | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Immediately after the end of the sessions | 5 | 284 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [0.21, 0.75] |
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | 356 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐2.74, 2.36] |
| 1.3 Intermediate‐term follow‐up (3 months to 1 year) | 2 | 356 | Std. Mean Difference (IV, Random, 95% CI) | 2.48 [1.02, 3.94] |
| 2 back specific functional status (lower scores mean better). Ex: RDQ, Oswestry and Aberdeen Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Immediately after the end of the sessions | 4 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Intermediate‐term follow‐up (3 months to 1 year) | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 return to work (higher values mean better) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Side effects / Complications Show forest plot | 7 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Immediately after the end of the sessions | 4 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Intermediate‐term follow‐up (3 months to 1 year) | 3 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 pain and function (adjusted for baseline values) Show forest plot | Other data | No numeric data | ||
| 5.1 Immediately after the end of the sessions | Other data | No numeric data | ||
| 5.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | Other data | No numeric data | ||
| 5.3 Intermediate‐term follow‐up (3 months to 1 year) | Other data | No numeric data | ||
| 6 general level of pain (0‐15 points)(more points mean less pain) Show forest plot | Other data | No numeric data | ||
| 6.1 Immediately after the end of the sessions | Other data | No numeric data | ||
| 6.2 Intermediate‐term follow‐up (3 months to 1 year) | Other data | No numeric data | ||
| 7 pain: difference between within group changes Show forest plot | 1 | differences between (Random, 95% CI) | Totals not selected | |
| 7.1 Immediately after the end of the sessions | 1 | differences between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (lower values mean better) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Improvement (higher values are better) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 improvement Show forest plot | Other data | No numeric data | ||
| 3.1 Immediately after the end of the sessions | Other data | No numeric data | ||
| 3.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 global measure (higher values are better) Show forest plot | 4 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 4 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Side effects / Complications Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (VAS): lower values are better Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Short term (immediately after end of sessions) | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 global measure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain score (lower values mean better) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Immediately after the end of the sessions | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 pain recovery: higher values are better Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Immediately after the end of the sessions | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 global measure (higher values are better) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 back specific functional status (higher scores are better). Ex: Japan Orthopedic Association Score. Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Immediately after the end of the sessions | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Side effects / Complications Show forest plot | 1 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 Immediately after the end of the sessions | 1 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (lower values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Short term (immediately after end of sessions) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 pain recovery (higher values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 global measure (higher values are better) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 functional status (higher values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 physical examination (finger‐floor distance) Higher values are better. Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 improvement Show forest plot | Other data | No numeric data | ||
| 6.1 Long‐term follow‐up (more than 1 year) | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 pain (lower values are better) Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Immediately after the end of the sessions | 4 | 289 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐1.02, ‐0.50] |
| 1.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 3 | 182 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.10 [‐1.62, ‐0.58] |
| 1.3 Intermediate‐term follow‐up (3 months to 1 year) | 2 | 115 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐1.14, ‐0.38] |
| 2 pain: difference between within group changes Show forest plot | 2 | differences between (Random, 95% CI) | Subtotals only | |
| 2.1 Immediately after the end of the sessions | 2 | differences between (Random, 95% CI) | ‐1.07 [‐2.14, ‐0.00] | |
| 2.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | differences between (Random, 95% CI) | ‐0.7 [‐1.33, ‐0.07] | |
| 2.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | differences between (Random, 95% CI) | ‐0.8 [‐1.80, 0.20] | |
| 3 pain disability index (lower values are better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Immediately after the end of the sessions | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain: percentage of patients with >50% pain reduction Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 function: difference between within group changes Show forest plot | 2 | differences between (Random, 95% CI) | Subtotals only | |
| 5.1 Immediately after the end of the sessions | 2 | differences between (Random, 95% CI) | ‐6.51 [‐14.99, 1.98] | |
| 5.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | differences between (Random, 95% CI) | ‐3.1 [‐5.26, ‐0.94] | |
| 5.3 Intermediate‐term follow‐up (3 months to 1 year) | 1 | differences between (Random, 95% CI) | ‐6.8 [‐12.60, 1.00] | |
| 6 global measure Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 Immediately after the end of the sessions | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 back specific functional status (lower scores mean better). Ex: RDQ, Oswestry and Aberdeen Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Immediately after the end of the sessions | 3 | 173 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.27, ‐0.63] |
| 7.2 Short‐term follow‐up (up to 3 months after the end of the sessions) | 2 | 99 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.37, ‐0.54] |
| 7.3 Intermediate‐term follow‐up (3 months to 1 year) | 2 | 115 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.92, ‐0.18] |
| 8 spine range of motion: difference between within group changes Show forest plot | 1 | difference between (Random, 95% CI) | Totals not selected | |
| 8.1 Immediately after the end of the sessions | 1 | difference between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Intermediate‐term follow‐up (3 months to 1 year) | 1 | difference between (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Side effects / Complications Show forest plot | 2 | Risk Difference (M‐H, Random, 95% CI) | Totals not selected | |
| 9.1 Immediately after the end of the sessions | 2 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |

