Asesoramiento conductual individual para el abandono del hábito de fumar
Referencias
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Setting: Community health centre, USA | |
| Participants | 755 African American light smokers (<= 10 cpd) | |
| Interventions | Factorial trial, 2mg nicotine gum/placebo arms collapsed for this review | |
| Outcomes | PP abstinence at 6m (7 day PP) | |
| Notes | New for 2008. Not in main analysis; compares two counselling styles. No significant effect of gum, no evidence of interaction. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Centrally generated blocked scheme, block size 36 |
| Allocation concealment? | Low risk | Sealed envelopes opened sequentially |
| Blinding? | Unclear risk | Staff & participants blind to pharmacotherapy but not to type of counselling |
| Incomplete outcome data addressed? | Low risk | 118 (15.6%) lost to follow‐up included in ITT analysis. HE participants less likely to be lost. Alternative assumptions about losses did not alter conclusions. Low level of cotinine validation. |
| Methods | Setting: Primary care clinic, Spain | |
| Participants | 48 smokers (excludes 6 dropouts) | |
| Interventions | 1. 'Advanced', 4 x30 min over 4 wks, video, cognitive therapy, social influences, relapse prevention | |
| Outcomes | Abstinence at 12m | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Stratified on cigarette consumption & age, block size 4. |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | Staff not blind, unclear for participants |
| Incomplete outcome data addressed? | Low risk | 6 post‐randomization dropouts excluded from ITT analyses. Their inclusion would marginally increase effect size. |
| Methods | Setting: cessation clinic, USA | |
| Participants | 240 smokers of > 1 pack/day | |
| Interventions | All interventions included 8 wks nicotine patch (21 mg with weaning) | |
| Outcomes | Abstinence at 1 yr | |
| Notes | 3 vs 2+1 in intensive versus minimal intervention, but sensitivity analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Urn technique' |
| Allocation concealment? | Unclear risk | No details given. Allocation took place after baseline session common to all conditions |
| Blinding? | Unclear risk | Staff not blind, unclear for participants |
| Incomplete outcome data addressed? | Low risk | 30 (12.5%) lost to follow up included in ITT analysis |
| Methods | Setting: 26 general practices (primary care clinics), UK | |
| Participants | 925 smokers | |
| Interventions | Both interventions included 8 wks 16mg nicotine patch | |
| Outcomes | Abstinence at 12m (sustained at 1, 4, 12, 26 wks) | |
| Notes | New for 2008 update. Not in main analysis; compares higher and lower intensity counselling. Therapists were not full time specialist counsellors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Random number generator |
| Allocation concealment? | Low risk | Numbered sealed envelopes |
| Blinding? | Unclear risk | Staff making follow‐up calls were blind |
| Incomplete outcome data addressed? | Low risk | 288 (31%) lost to follow up, similar across groups, included in ITT analysis |
| Methods | Setting: 12 residential centres for alcohol/drug treatment, USA | |
| Participants | (50 participants in each of 12 sites) | |
| Interventions | 1. 4 x10‐15min sessions. 1st during inpatient stay. 3 by telephone, 8, 12, 16 wks post‐discharge. | |
| Outcomes | Abstinence at 12m post discharge (7 day PP) | |
| Notes | Cluster‐randomized, so individual data not used in primary meta‐analysis. Entered into a secondary analysis using inverse variance method, using adjusted OR 1.02 (CI 0.50 to 2.49) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Matched pairs of centres allocated by coin toss, 2 centres declined participation after allocation |
| Allocation concealment? | High risk | Cluster randomized with participant recruitment (by research team) after centre allocation so potential for selection bias |
| Blinding? | Unclear risk | Staff not blind, unclear for participants |
| Incomplete outcome data addressed? | Low risk | 22% lost to follow up. Including them as smokers made little difference to estimates |
| Methods | Setting: internal medicine practice, USA | |
| Participants | 155 smokers | |
| Interventions | 1. Two 20 min counselling sessions during a periodic health examination (benefits of quitting, assessment of motivation, quit plan, high risk/problem solving) | |
| Outcomes | Abstinence at 18m (sustained from 6‐18m) | |
| Notes | 18m data reported in Secker‐Walker 1990 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomized, method not described |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | Physicians blind, counsellor not blind, participants probably blind, |
| Incomplete outcome data addressed? | Low risk | 20 (13%) not contacted at 6 & 18m, included in ITT analysis. |
| Methods | Setting: Inpatient substance abuse treatment centre, USA | |
| Participants | 39 male veteran inpatients | |
| Interventions | 1. Smoking cessation programme; daily 15 min counselling session and computer‐guided nicotine fading with contingency contract | |
| Outcomes | Abstinence 6m after discharge | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomized, method not described |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | Staff not blind, participants unclear |
| Incomplete outcome data addressed? | Unclear risk | Loss to follow up not reported |
| Methods | Setting: Inpatient Veterans rehabilitation centre, USA | |
| Participants | 150 veteran drug‐ & alcohol‐dependent smokers. | |
| Interventions | All participants were receiving standard substance abuse treatment, smoking banned in building. | |
| Outcomes | Abstinence at 12m (sustained at 1, 3, 6m follow ups) | |
| Notes | 1+2 vs 3 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomized, method not described |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | Staff not blind, participants unclear |
| Incomplete outcome data addressed? | Low risk | 12 (8%) lost to follow up included in ITT analysis |
| Methods | Setting: Hospital inpatients, USA | |
| Participants | 100 MI patients (98% smoked in previous wk) | |
| Interventions | 1. 8 x20 min sessions, 1st during hospitalisation, 7 by phone (<1, 4, 8, 12, 20 & 26 wks post‐discharge). Stage of change model, motivational interviewing, relapse prevention. | |
| Outcomes | Sustained abstinence at 1 yr (no smoking since discharge) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | 'drawing random numbers from an envelope' |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | No information on blinding |
| Incomplete outcome data addressed? | Low risk | 20 (20%) lost to follow up included in ITT analysis |
| Methods | Setting: Primary care patients, 16 clinics, USA | |
| Participants | 961 smokers of >=10 cpd. (A further 908 were allowed to select treatment. Demographic details based on 1869) | |
| Interventions | (Self‐selected group of factorial trial not included in meta‐analysis) | |
| Outcomes | Continuous abstinence at 1 yr (no relapse lasting 7 days), also PP. | |
| Notes | 3 versus 1&2 used in meta‐analysis. More conservative than 3 versus 2. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomized, method not described |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | No information on blinding |
| Incomplete outcome data addressed? | Low risk | Denominators in meta‐analysis based on numbers who collected patches (85%, similar across arms). |
| Methods | Setting: 4 Planned Parenthood clinics, USA | |
| Participants | 1154 female smokers | |
| Interventions | Both groups received 20 sec provider advice. | |
| Outcomes | Abstinence at 6m (for 30 days) | |
| Notes | 26% did not want telephone component, 31% of remainder not reached. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Randomized, block size 4, fixed schedule |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | No details given |
| Incomplete outcome data addressed? | Low risk | 10% loss to follow up included in ITT analysis |
| Methods | Setting: 4 hospitals, USA | |
| Participants | 2095 current smokers | |
| Interventions | 1. Control: modified usual care: smoking cessation booklet in hospital (not used in meta‐analysis). | |
| Outcomes | Abstinence at 12m (7‐day PP). | |
| Notes | New for 2008. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'randomly ordered within blocks of 30 assignments' |
| Allocation concealment? | Unclear risk | Allocation by research assistant, concealment not described |
| Blinding? | Unclear risk | No details given |
| Incomplete outcome data addressed? | Low risk | 78 (3.7%) excluded from ITT analysis due to death or too ill for follow up. 426 (20%) lost to follow up included in ITT analysis; higher loss in treatment than control. |
| Methods | Setting: clinical research centres, USA (2 sites) | |
| Participants | 504 smokers >= 15 cpd | |
| Interventions | Factorial trial; compared 22 mg/day vs 44 mg/day nicotine patch and 3 types of adjuvant treatment. All participants had 8 weekly assessments by research staff | |
| Outcomes | 7 day PP abstinence at 26 wks | |
| Notes | No significant difference in dose‐related outcome and no dose‐counselling interaction at 26 wks reported, so patch arm collapsed in analysis. 2 vs 1, counselling vs NRT alone, Comparison with group counselling covered in Cochrane group therapy review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomized, method not stated |
| Allocation concealment? | Unclear risk | 'In a double blind manner' for NRT, but not specified for counselling |
| Blinding? | Unclear risk | No details given |
| Incomplete outcome data addressed? | Low risk | 16.3% lost to follow up included in ITT analysis, no difference across conditions |
| Methods | Setting: Outpatient clinic, South Korea | |
| Participants | 401 daily smokers, 65% willing to quit within 1m | |
| Interventions | Test of 5As approach. All participants had first been Asked about smoking status & Advised to quit by physicians and told to go to onsite counsellors, who Assessed willingness to quit, and enrolled & randomized patients. | |
| Outcomes | Abstinence at 5m | |
| Notes | New for 2008 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Random list with block size of 6 and 12 allocation strata |
| Allocation concealment? | Low risk | Assignments in sealed opaque envelopes |
| Blinding? | Unclear risk | Outcome assessors were unaware of participants' group |
| Incomplete outcome data addressed? | Low risk | 7 lost to follow up included in ITT analysis |
| Methods | Setting: substance abuse outpatient facility, USA | |
| Participants | 69 smokers | |
| Interventions | Both interventions included use of nicotine patch (24 hr, 10 wks tapered dose) | |
| Outcomes | Abstinence at 12m, 1 wk PP | |
| Notes | Both interventions regarded as counselling, used in comparison of intensity. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Block randomization (block size 10) |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | No details given |
| Incomplete outcome data addressed? | Low risk | 12 administrative drop‐outs/exclusions not included, treatment group not specified. All others included. |
| Methods | Setting: clinic, USA | |
| Participants | 463 smokers | |
| Interventions | Factorial trial. Bupropion/placebo pharmacotherapy arms collapsed. | |
| Outcomes | 7 day PP abstinence at 12m | |
| Notes | New for 2008 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Random number table |
| Allocation concealment? | Low risk | Staff who screened and enrolled participants were unaware of the experimental condition to be assigned |
| Blinding? | Unclear risk | Staff and participants blind to medication but not counselling |
| Incomplete outcome data addressed? | Low risk | 171 (37%) failed to attend quit date visit or lost to follow up, included in ITT analysis |
| Methods | Setting: hospital, UK | |
| Participants | 274 smokers (183 in relevant arms) admitted to medical and surgical wards, smoked in last 28 days | |
| Interventions | 1. Usual Care, no smoking advice | |
| Outcomes | Continuous abstinence at 12m | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'List generated for each centre allocating equally in random permuted blocks of nine.' |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | No details given |
| Incomplete outcome data addressed? | Low risk | 72 (39%) lost to follow up included in ITT analysis |
| Methods | Setting: communities & worksites, Japan | |
| Participants | 977 smokers | |
| Interventions | Intervention: Stage‐base counselling, 1 x40 min, 4 x20‐30 min at 1,2,4,6m. + Phone call if TQD set | |
| Outcomes | Abstinence at 6m, sustained 4 point prevalence at 1,2,4,6m | |
| Notes | New for 2008. Recruited a largely unmotivated population | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Method not stated |
| Allocation concealment? | Unclear risk | No information given |
| Blinding? | Unclear risk | No information given |
| Incomplete outcome data addressed? | Low risk | 54 (5.5%) lost to follow up included in ITT analysis |
| Methods | Setting: cardiac catheterization labs at 3 hospitals, USA | |
| Participants | 267 smokers (256 surviving at 12m follow up) | |
| Interventions | 1. Minimal intervention ‐ 10 min advice and review of an information sheet | |
| Outcomes | Abstinence at 12m (sustained for 6m) | |
| Notes | Average length of contact for intervention was 1.22 hr (20min to > 5hr) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Method not stated |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | Physicians unaware of intervention condition, therapists blinded, participants unclear |
| Incomplete outcome data addressed? | Low risk | No mention of losses to follow up and all survivors included in denominators. |
| Methods | Setting: hospital, Denmark | |
| Participants | 105 smokers | |
| Interventions | 1. Usual care control: in hospital advice to quit + information about NRT + NRT available. | |
| Outcomes | Abstinence at 12 months (point prevalence) | |
| Notes | New for 2008 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomized, method not described |
| Allocation concealment? | Unclear risk | Sealed envelopes, but not stated to be numbered |
| Blinding? | Unclear risk | No information |
| Incomplete outcome data addressed? | Low risk | 10 (9.5%) lost to follow up, included in ITT analysis |
| Methods | Setting: Chest unit, USA | |
| Participants | 74 cigarette smokers | |
| Interventions | 1. Advice to quit | |
| Outcomes | Abstinence at 6m | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Method not described |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | Physicians blinded, therapist not blinded, participants unclear |
| Incomplete outcome data addressed? | Low risk | 8 lost to follow up were reincluded in ITT analysis by reviewers. 8 deaths excluded |
| Methods | Setting: hospital, USA | |
| Participants | 615 smokers or recent quitters (excluding 35 deaths). 37% of intervention and 32% of controls had a current smoking‐related health problem. | |
| Interventions | 1. Usual care | |
| Outcomes | Abstinence at 6m (PP, sustained abstinence reported based on self report) | |
| Notes | Use of validated PP rather than sustained abstinence gives more conservative treatment effect | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Each day's list of eligible smokers put in random order and patients recruited consecutively in this order. Randomized by research assistant |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | Outcome was assessed by blinded interviewer. |
| Incomplete outcome data addressed? | Low risk | 73 (22.4%) lost to follow up included in ITT analysis, no evidence of differential loss. 35 (5.4%) deaths excluded. |
| Methods | Setting: hospital, USA | |
| Participants | Two separate samples recruited: | |
| Interventions | 1. Coping skills, relapse prevention, 6 x1 hr including stress management, homework. | |
| Outcomes | Abstinence at 6m (PP) | |
| Notes | Post‐randomization drop‐outs who did not complete baseline and begin treatment were not included in any data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Randomly assigned', stratified on smoking rate and myocardial infarction status |
| Allocation concealment? | Unclear risk | No details given |
| Blinding? | Unclear risk | No details given |
| Incomplete outcome data addressed? | Low risk | Pretreatment drop outs were excluded, all others included in ITT analysis |
| Methods | Setting: Veterans Administration hospital, USA | |
| Participants | 299 smokers (smoked within 2 wks of admission) (excl 25 deaths) | |
| Interventions | 1. Multicomponent: single counselling session (30‐60 min) prior to discharge (based on social learning theory and stages of change). Video, prescription for nicotine gum if no contraindications. 5 follow‐up counselling calls over 3m | |
| Outcomes | Abstinence at 12m | |
| Notes | 65% of Group 1 and 17% of Group 2 reported using NRT, but use of NRT was not significantly associated with quitting in either group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Random list of assignments' |
| Allocation concealment? | Low risk | 'Sealed opaque envelopes opened on formal enrollment' |
| Blinding? | Unclear risk | Therapists could not have been blind. No information on patients |
| Incomplete outcome data addressed? | Low risk | 25 (8%) lost to follow up included in ITT analysis, 25 (8%) died, excluded from denominator |
| Methods | Setting: Veterans Affairs hospital, USA | |
| Participants | 209 smokers, >= 20 cigs in total in week before hospitalisation, excludes 14 deaths during follow up | |
| Interventions | 1. Intensive counselling: single counselling session (30‐60 min) prior to discharge (based on social learning theory and stages of change), 5 telephone counselling calls < 30 min, 1 & 3 wks, monthly for 3m + S‐H. Recycling encouraged. Nicotine patches begun in hospital, dose based on pre‐hospitalisation smoking rates. 2m supply at discharge. | |
| Outcomes | Abstinence at 12m (7 day PP) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Randomly assigned using computerized algorithm' |
| Allocation concealment? | Unclear risk | No details provided |
| Blinding? | Unclear risk | No details provided; there was an active control |
| Incomplete outcome data addressed? | Low risk | 7 (3%) lost to follow up included in ITT analysis, 14 (6%) died & excluded from denominator |
| Methods | Setting: 2 Health Maintenance Organization hospitals, USA | |
| Participants | 1119 smokers or recent quitters (5%) | |
| Interventions | 1. 20 min counselling session, 12 min video, quit kit, choice of S‐H materials, 1‐2 follow‐up telephone calls, access to hotline, bimonthly newsletter mailings. | |
| Outcomes | Abstinence at 12m (2 PP, 3 & 12m) | |
| Notes | A sensitivity analysis on the effect of exclusion of this non‐random study is reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Not random, intervention alternated between hospitals on a monthly basis in order to avoid contamination |
| Allocation concealment? | High risk | Intervention or control status of hospital known when patients recruited |
| Blinding? | Unclear risk | Patients in control arm were not identified to hospital staff, and were probably unaware of study design. Telephone assessments were by blinded assessors |
| Incomplete outcome data addressed? | Low risk | 6% loss to follow up, no difference by group, included in ITT analysis |
| Methods | Setting: 7 chest clinics, Denmark | |
| Participants | 370 smokers of >1 cpd with COPD | |
| Interventions | Factorial trial. Nicotine sublingual tablet and placebo arms collapsed in meta‐analysis | |
| Outcomes | Sustained abstinence at 12m (validated at all visits from wk 2, PP also reported) | |
| Notes | New for 2008 update. Compares higher and lower intensity counselling. Therapists were not full time specialist counsellors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Block randomization list at each centre |
| Allocation concealment? | Unclear risk | Allocation process not described |
| Blinding? | Unclear risk | Described as double blind, but unclear that this applied to behavioural components |
| Incomplete outcome data addressed? | Low risk | 82 (22%) lost to follow up, included in ITT analysis |
| Methods | Setting: Veterans Administration outpatient clinics, USA | |
| Participants | 466 male smokers | |
| Interventions | 1. Control ‐ pamphlet on hazards of smoking | |
| Outcomes | Abstinence for 1m at 6m (9m for high intensity group, 6m after last contact) | |
| Notes | Using validated quit rates there was no difference between 2 and 3, although self‐reported quitting was greater in 3. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Random number table |
| Allocation concealment? | Low risk | Consecutively numbered envelopes containing treatment assignment. |
| Blinding? | Unclear risk | Therapists not blind, unclear whether participants were |
| Incomplete outcome data addressed? | Low risk | 34 (7.3%) died or lost to follow up included in ITT analysis. More lost in high intensity group. |
| Methods | Setting: Cardiovascular outpatient department, Netherlands | |
| Participants | 385 smokers (8 deaths excluded from outcomes) | |
| Interventions | In both groups, patients planning to quit received 8 wks nicotine patch with instruction from nurse. | |
| Outcomes | Abstinence for 7 days at 12m | |
| Notes | New for 2008. Included on grounds that participants were referred to nurse practitioner for counselling; not part of usual care. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'A computerized balanced randomization programme taking prognostic factors (e.g. clinic attendance, age and gender) into account.' |
| Allocation concealment? | Low risk | 'While patients completed their baseline questionnaire (and signed a written informed consent) nurses randomly assigned ...' |
| Blinding? | Unclear risk | 'Patients were not informed about the behavioural intervention [before enrollment] in order to avoid a Hawthorne effect'. |
| Incomplete outcome data addressed? | Low risk | One withdrawal due to cognitive problems and 8 deaths during follow up not included in analyses. At 12m 45 not reached by mail or phone, included in ITT. More unmarried patients lost. |
| Methods | Setting: University worksite, USA | |
| Participants | 378 smokers | |
| Interventions | All groups received a 10 min session of brief advice | |
| Outcomes | Abstinence at 1 yr (sustained at 6 wks, 6m, 1yr, no more than 2 cigs in period) | |
| Notes | There was no apparent effect of monetary incentives so this arm is collapsed. 4&2 vs 3&1. Number of quitters estimated from graphs | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Computer‐generated assignment |
| Allocation concealment? | Low risk | Sealed numbered envelopes opened after informed consent & baseline questionnaire |
| Blinding? | Unclear risk | Therapists could not be blind, unlikely that participants were |
| Incomplete outcome data addressed? | Low risk | 37 lost to f‐up, included in ITT analysis |
av ‐ average (mean)
CI ‐ confidence interval
CO ‐ carbon monoxide
COHb ‐ carboxyhaemoglobin
COPD ‐ chronic obstructive pulmonary disease
cpd ‐ cigarettes per day
m ‐ month
MA ‐ meta‐analysis
MI ‐ myocardial infarction
min ‐ minute
NRT ‐ Nicotine Replacement Therapy
OR ‐ odds ratio
PP ‐ point prevalence (abstinent at defined period)
ppm ‐ parts per million
S‐H ‐ Self help materials
TQD ‐ Target Quit Date
wk ‐ week
yr ‐ year
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Allocation to behavioural treatment was by clinic attended; each of 3 primary care clinics provided different treatment. | |
| Intervention provided by a nurse as part of usual care, included in Cochrane review of nursing interventions (Rice 2008). | |
| Intervention provided by a nurse during normal duties, included in Cochrane review of nursing interventions (Rice 2008). | |
| Compares Individual to group counselling, see Cochrane review of group based interventions (Stead 2005). | |
| Intervention provided by a nurse, included in Cochrane review of nursing interventions (Rice 2008). | |
| Short follow up (three months). | |
| Data not available for intervention and control groups separately. No significant difference reported. Cessation was a secondary outcome in this trial using motivational interviewing to reduce passive smoke exposure. Participants were not selected by motivation to quit. | |
| Intervention provided by a nurse; included in Cochrane review of nursing interventions (Rice 2008) | |
| Trial of an acceptance & commitment‐based treatment intervention that included multiple group sessions in addition to individual counselling. Comparator was nicotine patch therapy. | |
| Intervention provided by physicians & nurses in usual care setting, not specialist counselling. | |
| Multiple risk factor intervention. | |
| Intervention was multicomponent and included advice/counselling from a physician, nurse and a group programme. Follow up only 5 months. | |
| There was no face‐to‐face contact with counsellors. Contact was by pro‐active telephone calls. | |
| Multiple risk factor intervention enrolling smokers and nonsmokers. | |
| Intervention specifically for pregnant women, see Cochrane review of smoking cessation interventions in pregnancy (Lumley 2004) | |
| Intervention was provided in a self‐help format. | |
| Multiple risk lifestyle intervention. | |
| Short follow up (6 wks). Study added a pharmacotherapy compliance enhancing component to individual counselling using CBT. | |
| All participants received individual counselling; Included in Cochrane NRT review (Stead 2008b). | |
| Intervention combined group and individual counselling with pharmacotherapy. | |
| The health education arm of the trial included a group meeting with didactic lecture, film and discussion, followed by a single individual session with a therapist. We decided that this did not meet the criteria for individual counselling. | |
| Intervention combined the systematic use of NRT with counselling; covered in Cochrane review of worksite interventions (Cahill 2008) | |
| Intervention provided by nurses in a primary care clinic, included in Cochrane review of nursing interventions (Rice 2008) | |
| Short follow up (three months). Compared 2 counselling approaches, no difference detected. | |
| Success was defined as reduction in smoking of over 85%, not complete abstinence. | |
| Primary outcome was not cessation; assessed rates of receiving counselling, referral and treatment. | |
| Motivational interviewing intervention by primary care physician during routine care | |
| Test of motivational interviewing; not all partipants attempted to quit | |
| Intervention providers were respiratory therapists not counsellors. Included in Cochrane review of interventions in hospital inpatients, (Rigotti 2007). | |
| Study targeted multiple risk factors. | |
| Short follow up (three months). |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Positive Paths |
| Methods | RCT |
| Participants | HIV+ smokers |
| Interventions | Brief intervention modeled on PHS guidelines versus a more intensive motivational counselling intervention, with both interventions providing 8 weeks of NRT to those setting a quit date. |
| Outcomes | Smoking cessation |
| Starting date | Completed |
| Contact information | Ray Niaura |
| Notes | NCT00551720 |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking cessation at longest follow‐up Show forest plot | 22 | 9587 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.39 [1.24, 1.57] |
| Analysis 1.1  Comparison 1 Individual counselling compared to minimal contact control, Outcome 1 Smoking cessation at longest follow‐up. | ||||
| 1.1 Counselling versus control (no systematic pharmacotherapy) | 18 | 7855 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [1.25, 1.65] |
| 1.2 Counselling plus NRT versus NRT alone | 4 | 1732 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [1.02, 1.59] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking cessation at longest follow‐up Show forest plot | 5 | 1897 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.74, 1.25] |
| Analysis 2.1  Comparison 2 More intensive versus less intensive counselling, Outcome 1 Smoking cessation at longest follow‐up. | ||||
| 1.1 No pharmacotherapy | 2 | 478 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.53, 2.22] |
| 1.2 Adjunct to pharmacotherapy | 4 | 1419 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.71, 1.25] |
| 2 Sensitivity analyses for Alterman 2001 in intensive versus brief counselling comparison Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.2  Comparison 2 More intensive versus less intensive counselling, Outcome 2 Sensitivity analyses for Alterman 2001 in intensive versus brief counselling comparison. | ||||
| 2.1 Using Alterman high versus low | 5 | 1817 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.81, 1.37] |
| 2.2 Using Alterman high versus moderate | 5 | 1817 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.91, 1.58] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking cessation at longest follow‐up Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.1  Comparison 3 Comparisons between counselling approaches of similar intensity, Outcome 1 Smoking cessation at longest follow‐up. | ||||
| 1.1 Relapse Prevention versus Health Belief model | 1 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.45, 1.98] |
| 1.2 Motivational Interviewing versus Health Education | 1 | 755 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.34, 0.76] |
| 1.3 Counselling versus equal sessions of psychoeducation | 1 | 463 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.62, 1.39] |

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.

Forest plot of comparison: 1 Individual counselling compared to minimal contact control, outcome: 1.1 Smoking cessation at longest follow‐up.
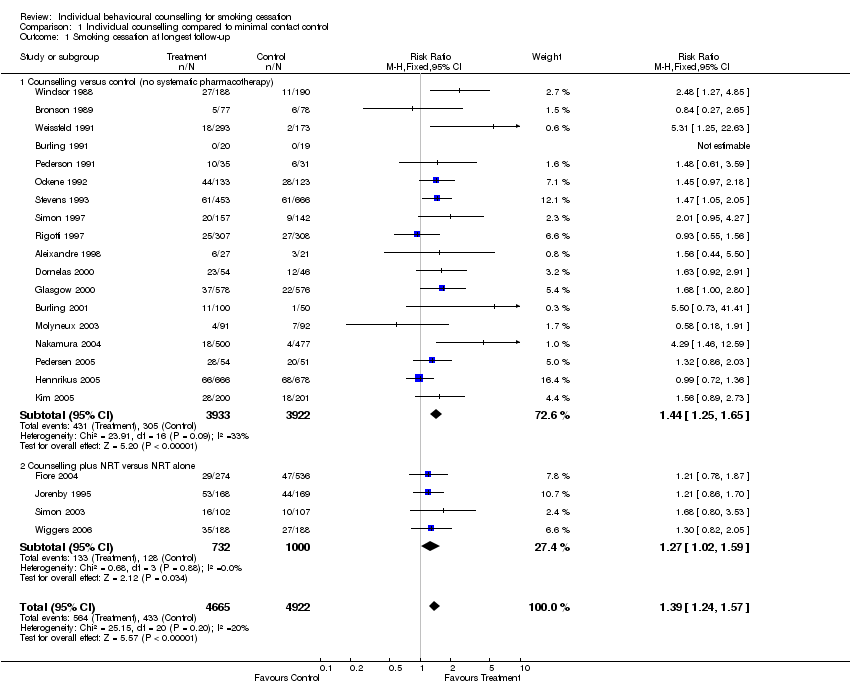
Comparison 1 Individual counselling compared to minimal contact control, Outcome 1 Smoking cessation at longest follow‐up.

Comparison 2 More intensive versus less intensive counselling, Outcome 1 Smoking cessation at longest follow‐up.

Comparison 2 More intensive versus less intensive counselling, Outcome 2 Sensitivity analyses for Alterman 2001 in intensive versus brief counselling comparison.

Comparison 3 Comparisons between counselling approaches of similar intensity, Outcome 1 Smoking cessation at longest follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking cessation at longest follow‐up Show forest plot | 22 | 9587 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.39 [1.24, 1.57] |
| 1.1 Counselling versus control (no systematic pharmacotherapy) | 18 | 7855 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [1.25, 1.65] |
| 1.2 Counselling plus NRT versus NRT alone | 4 | 1732 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [1.02, 1.59] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking cessation at longest follow‐up Show forest plot | 5 | 1897 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.74, 1.25] |
| 1.1 No pharmacotherapy | 2 | 478 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.53, 2.22] |
| 1.2 Adjunct to pharmacotherapy | 4 | 1419 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.71, 1.25] |
| 2 Sensitivity analyses for Alterman 2001 in intensive versus brief counselling comparison Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Using Alterman high versus low | 5 | 1817 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.81, 1.37] |
| 2.2 Using Alterman high versus moderate | 5 | 1817 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.91, 1.58] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking cessation at longest follow‐up Show forest plot | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Relapse Prevention versus Health Belief model | 1 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.45, 1.98] |
| 1.2 Motivational Interviewing versus Health Education | 1 | 755 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.34, 0.76] |
| 1.3 Counselling versus equal sessions of psychoeducation | 1 | 463 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.62, 1.39] |

