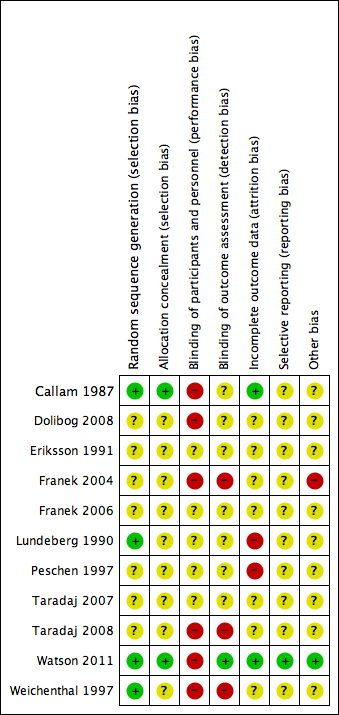
| Study | Intervention and Co‐interventions | Comparison intervention | Participants | Results |
| Callam 1987 5 physiotherapy departments Scotland NB 2 related abstracts say there were 110 participants | US group (n = 52): DIRECT and HIGH FREQUENCY *Lancet paper reports this frequency as 1 mHz. Verified with M Callam in Dec 09 that this should have read 1 MHz. | Standard treatment group (n = 56): cleansing with 1% saline; application of Arachis oil to skin without massage; application of paste bandage (Calaband); application of support bandage (Lestreflex); advice on exercise. Weekly treatment. | Included: patients attending clinics for treatment of chronic leg ulcers Excluded: non consent, allergy to standard treatment, PVD (lack of ankle pulses) | Ulcers completely healed by 12 wks: US: 25/52 (48%) C: 17/56 (30%) Read from graph: Ulcers completely healed at 8 wks: US: 23/52 (45%) C: 14/56 (25%) Ulcers completely healed by 12 wks (complete case): US: 25/41 (61%) C: 17/41 (41%) US treated healed sig more quickly by log rank ;=0.03. this effect persisted even when withdrawals due to pain and deterioration counted as failures. Mean % ulcer unhealed at 12 weeks (no variance): US: 9% C: 27% P<0.05 Withdrawals: US: 11/52 (21%) Allergy 4 Pain 4 DNA/refused 2 Death 2 C: 15/56 (27%) Allergy 6 Pain 3 Refused/DNA 3 Deterioration 2 Arterial disease 1 |
| Dolibog 2008 Poland | US group: 33 participants treated with US, compression (Sigvaris), and drug therapy. INDIRECT and HIGH FREQUENCY | Standard care group (n = 37): compression and drug therapy. Dressings changed daily for 7 weeks. | 70 participants with venous leg ulcers who all had venous surgery, and diagnosed as having venous disease with Duplex scanning. Excluded: diabetes, rheumatoid arthritis Surgery included crossectomy, partial stripping of GSV or LSV, local phlebectomy, ligation of perforators. | Ulcers healed completely: Group 1: 10/33 Group 2: 12/37 Mean area after therapy (SD) Group 1: 13.15 (11.55) Group 2: 13.12 (14.57) |
| Eriksson 1991 Hospital and primary care Sweden | US group: 1.0 W/cm2 at 1 MHz. Enraf Nonius US machine with aquasonic gel. Ultrasound head was 2.8 cm diameter for superficial ulcers and 1.2 cm diameter for deep ulcers. US applied to ulcer surface area and surrounding tissue for 10 minutes twice a week for 8 weeks. DIRECT and HIGH FREQUENCY | Sham US group: cleaned with saline; paste bandage, support bandage plus exercise advice (no further details provided). | Included; people with venous leg ulcers Excluded: allergy to standard treatment, arterial disease, rheumatoid arthritis, diabetic ulcers, traumatic venous ulcer | Ulcers completely healed at 8 wks: US: 6/19 (6/12 completers) C: 4/19 (4/13 completers) Cumulative % healed compared using life table methods. % ulcers completely healed at different times (wks) US:C 2 wks: 8:0 4 wks: 17:8 6 wks: 25:15 8 wks: 41:30 % ulcer area healed at 8 wks (SD): US: 42 (9) C: 48 (13) Withdrawals: US: 7/19 C: 6/19 For allergy: US: 3 C: 2 For pain: US: 2 C: 1 Refusal/DNA: US: 2 C: 3 |
| Franek 2004 Poland Hospital inpatients | US group 1: US at 1 W/cm2 (n = 22) US group 2: US at 0.5 W/cm2 (n = 21) Both groups received pulsed cycle of 1:5, frequency 1 MHz. Cointerventions: saline soaked gauze. Single‐layer elastic compression (Hartmann). INDIRECT and HIGH FREQUENCY | Pharmacotherapy group (n = 22): no US. Local baths of potassium permanganate and wet dressings of 0.1M copper sulphate solution plus compresses of fibrolan, chloramphenicol, colistin, gentamicin. Drugs alternated every few days. Single layer elastic compression (Hartmann). Treatment for 3 weeks. This was problematic as the use of US or not was not the only difference in treatment between the groups i.e. performance bias. Also US groups 1 and 2 were hospitalised in the Dermatology Clinic of Katowice and Group C in the Dermatology Dept of Zabrze. | Included: people with venous ulcers (signs of venous disease) and ABPI > 1.0. Excluded: people with diabetes, advanced sclerosis | Mean (median) area after treatment (cm2): A: 14 (11.14) p = 0.0001 B: 9.29 (3.78) p = 0.00006 C: 20.58 (9.86) p = 0.002 Complete ulcer healing by 3 weeks: A: 1/22 B: 3/21 C: 1/22 |
| Franek 2006 Poland Hospital inpatients | Electrostimulation group: once a day, 50 minutes each session, 6 consecutive days, 4 weeks total (2 weeks cathodic and 2 weeks anodic stimulation), NaCl 0.9% locally (no further details provided) Laser therapy group: 65 mW once a day, 5 consecutive days, duration of each session depending of ulceration area – device was set up to develop 4J/cm2 on average power 65 mW, various pharmacological agents locally, 4 weeks total US group: 0.5 W/cm2 – once a day, duration of each session depending on ulceration area: 5 cm2 received 5 minutes, plus 1 minute more for each 1 cm2 of additional ulcer area, 4 weeks total, 0.9% NaCl locally | Compression therapy provided for all groups. Bandages were removed every time for purposes of physical therapy and then put back on. Compression + pharmacological agents group: 4 weeks total | People with venous leg ulcers | Mean % change in ulcer area (relative to baseline) at 4 weeks: Group 1: ‐55.26%; Group 2: ‐35.97%; Group 3: ‐63.42%; Group 4: ‐30.77% P(Group 3 & Group 4) = 0.007 |
| Lundeberg 1990 Sweden | US. group (n = 22): US: pulsed 1:9 0.5 W/cm2 at 1 MHz US applied to ulcer surface and surrounding tissue for 10 minutes; probe applied for 1 minute per probe head area (no further details provided). Treated 3 x per week for 4 weeks, then 2 x per week for 4 weeks, then once a week for 4 weeks. Plus standard care, which comprised of cleansing with saline; paste bandage; support bandage; exercise instructions. DIRECT and HIGH FREQUENCY | Sham US (no further details provided) + standard treatment group (n = 22): standard care consisted of cleansing with saline; paste bandage; support bandage; exercise instructions. | Patients with VLUs referred from depts. of internal medicine, surgery, primary health care. Exclusion: skin allergy, PVD, RA, DM, traumatic venous ulcer. | Cumulative % (n) healed at 8 weeks: US: 30% (5) C: 20% (3) Cumulative % (n) healed at 12 weeks: US: 59% (10) C: 52% (8) Mean % ulcer area remaining at 8 weeks (SD) in patients completing: US: 47% (8) C: 53% (10) Mean % ulcer area remaining at 12 weeks (SD) in patients completing: US: 39% (5) C: 43% (6) 12/44 patients withdrew (7 placebo group, 5 US group). Placebo: 3 allergy, 1 pain, 3 DNA/refused. US: 2 allergy, 1 pain, 2 DNA/refused |
| Peschen 1997 Germany Outpatient clinic | US group (n = 12): US treatment involved placing legs in footbath of water at 32 °C‐34 °C filled to 10 cm above the ulcer. US sound head transducer immersed in bath and placed in line with ulcer 5 cm away. The continuous US was given for 10 minutes at 30 kHz, 0.1 W/cm2 3 x per week. Standard care was also given. This comprised HCL dressings (Coloplast); compression therapy using “strong‐quality elastic compression bandages (Beiersdorf)” INDIRECT and LOW FREQUENCY | Sham US group (n = 12): sham US plus standard care Sham procedure involved placing legs in footbath of water at 32 °C‐34 °C filled to 10 cm above the ulcer. US sound head transducer immersed in bath and placed in line with ulcer 5 cm away. Sham US for 10 minutes 3 x per week. Standard care consisted of HCL dressings (Coloplast); compression therapy using “strong‐quality elastic compression bandages (Beiersdorf)” | 24 people attending outpatients clinic. Included: people with chronic VLUs at least 2 cm2 and 3 months’ duration. Clinical diagnosis of VLU confirmed by history, Doppler US, light reflection rheography, ABPI of 0.8 or above. Excluded: arterial disease, liver, cardiac or renal insufficiency, heamorrhagic gastroduodenitis, colitis, leukaemia, diabetes, RA, treatment allergy. | Complete ulcer healing at 12 weeks: US: 2/12 C: 0/12 (or 0/10 completers) Mean % decrease in ulcer area 12 weeks: US: 55.4% C: 16.5% No variance data p<0.007 Micro‐bleeding around the ulcer: US: 5 C: 0 Pain: US: 3/12 C: 4/10 pain free Irritation: US: 8/12 C: 0 8 US patients felt tingling sensation during US. After 12 wk treatment phase, standard care continued. At 3 months post treatment: Mean ulcer area: US: 30.6% C: 70.2% Mean change ulcer radius (mm) US: 9.9mm (n = 12) C: 5.3mm (n = 10) (P<0.012) |
| Taradaj 2007 Poland | US group (n = 24): sonotherapy with sonicator 730 device, in water bath, 1 MHZ, 0.5 W/cm2, duration dependent on area of ulceration ‐ e.g. 5 min for ≦ 5 cm2), 6 days/week for 7 weeks plus pharmacotherapy | All participants used moist normal saline dressing, and pharmacotherapy (diosmin 450 mg and hesperidin 50 mg combined as proprietary preparation (Detralex) All patients: treatment duration 7 weeks. Compression group (n = 25): compression plus stocking and pharmacotherapy Standard care group (n = 24): pharmacotherapy | People with venous ulcers who had undergone venous surgery by modified Babcock method. | Mean % change in ulcer area (relative to baseline) at 7 weeks: Group 1: ‐53.6%; Group 2: ‐69.4%; Group 3: ‐62.6% (P > 0.05 for all 3 comparisons between groups). Mean ± SD ulcer area in cm2 at 7 weeks (NB: comparisons are within group vs baseline): Group 1: 14.1 ± 11.7 (P = 0.00002); Group 2: 8.8 ± 10.0 (P = 0.00001); Group 3: 11.4 ± 14.1 (P = 0.00002). |
| Taradaj 2008 Poland | Surgery + US group (n = 21): surgery plus US, compression stockings (Sigvaris, 30 mmHg‐40 mmHg at ankle), drug therapy No surgery + US group: US, compression and drug therapy Drug therapy was flavonoid (450 mg diosmin, 50 mg hesperidin), 2 tabs (one of each) twice daily. Ulcers covered by saline soaks. Dressings changed once day only in clinic. Ultrasound; 0.5 W/cm2 pulsed; impulse 2 mS, interval 8 mS. Frequency 1 MHz. Performed in a bath of water with temp 34 °C. probe head 10 cm2 placed 2 cm above ulcer. An ulcer of 5 cm2 or less had 5 minutes treatment, with 1 minute more for each 1 cm2 by which the ulcer exceeded this size. If larger than 20 cm2 the ulcer was divided in 2. Treatment daily for 6 days/week for 7 weeks. INDIRECT and HIGH FREQUENCY | Surgery ‐ US group (n = 20): surgery plus compression and drug therapy No surgery ‐ US group (n = 20): compression and drug therapy Drug therapy was flavonoid (450 mg diosmin, 50 mg hesperidin), 2 tabs (one of each) twice daily. Ulcers covered by saline soaks. Dressings changed once day only in clinic. | People with venous disease assessed by symptoms and Duplex scanning. All offered venous surgery. Those refusing surgery were randomised to US or no US. | Group 1 vs. Group 2 Group 3 vs. Group 4 Numbers completely healed at 7 weeks: Group 1: 6/21 Group 2: 6/20 Group 3: 6/20 Group 4: 3/20 |
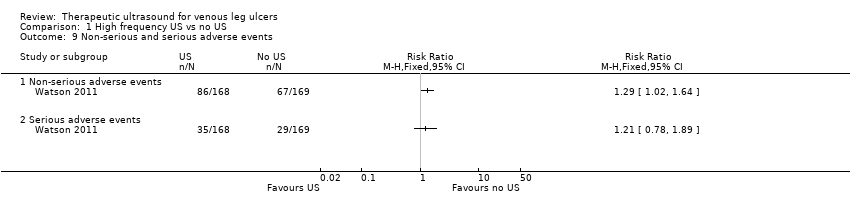
| Watson 2011 UK Community nurse services, community leg ulcer clinics, and hospital outpatient leg ulcer clinics | US group (n = 168): low‐dose (0.5 W/cm2) US, 1 MHz, with a pulsed pattern of 1:4, applied for 5 to 10 minutes to periulcer skin, weekly for up to 12 weeks, plus standard care, then standard care alone. DIRECT and HIGH FREQUENCY | Standard care group (n = 169): simple low‐adherent dressing and high compression (4‐layer bandage), reduced compression or no compression depending on participant tolerance. | 337 patients with hard‐to‐heal venous leg ulcers i.e., ulcer of 6 months’ duration or more and/or area greater than 5 cm2. Considered a venous ulcer if no other obvious causative factor and ulcer appeared clinically venous (moist, shallow, irregular shape, venous eczema, ankle oedema, lipodermatosclerosis, ulcer not confined to the foot). Participants had to have ABPI of 0.8 or greater. Excluded if poorly controlled diabetes, ankle prostheses, thrombophlebitis, active infection including cellulitis, local or metastatic cancer. | Hazard ratio* for US vs. SC 0.99 (0.70 to 1.40), p = 0.969 (NSD). * the analysis adjusted for centre as a random effect, ulcer area (from baseline tracing), ulcer duration and whether or not the patient was treated with high‐compression bandaging. Median time (for all ulcers) to complete healing: US: 365 days (95% CI 224, inestimable) SC: 328 days (95% CI 235, inestimable) P = 0.9051, log rank. Ulcers completely healed/not healed (%) at 8 wks (personal communication): US: 9/168 SC: 15/169 Ulcers completely healed/not healed (%) at 12 wks (personal communication): US: 26/168 SC: 25/169 Ulcers completely healed/not healed (%) at 12 month (personal communication): US: 72/168 SC: 78/169 HRQoL by SF‐12: Mean Baseline PCS (SD): US: 36.55 (11.32); n = 160 SC: 35.33 (11.47); n = 167 3 month PCS (SD): US:33.87 (11.49); n = 143 SC: 34.96 (11.39); n = 142 12 month PCS (SD): US:34.61 (12.09); n = 118 SC: 35.57 (11.39); n = 111 Baseline MCS (SD): US: 46.72 (11.52); n = 160 SC: 47.11 (11.29); n = 167 3 month MCS (SD): US: 45.95 (12.22); n = 143 SC: 46.83 (11.38); n = 142 12 month MCS (SD): US: 47.51 (11.54); n = 118 SC: 45.41 (12.15); n = 111 Serious Adverse Events (SAEs): US: 35/168 patients SC: 29/169 patients Non serious AEs:
US: 86/168 patients SC: 67/169 patients NS using random effects negative binomial regression (p = 0.3904). Using random effects negative binomial regression showed that significantly more non serious AEs in US group (p = 0.0411). For all adverse events in random effects binomial regression, there was a significant effect of treatment (p = 0.0446). Adjusted annual costs ( 95% bias‐corrected CI): US arm 1583.39 (1427.51 to 1728.70) vs. SC arm 1385.51 (1223.84 to 1549.21 |
| Weichenthal 1997 Outpatient clinic Germany | US group: 'experimental' 30 kHz US applicator mounted to footbath. Transducer positioned within 5 cm of ulcer surface. Surface subjected to 30 kHz US at 0.1 W/cm2 for 10 minutes, plus standard care. INDIRECT and LOW FREQUENCY | Conventional therapy group: topical fibrinolytic agents, antibiotics or other antiseptics and occlusive dressings. Eczema of surrounding skin could be treated with topical steroids. Compression with elastic bandages. Dressings changed at least 3 x per week. Participants received foot bathing but participants in US group did not. | Inclusion: presence of ulceration for min. 3 mo. plus evidence of venous incompetence. Excluded: diabetes, arterial disease. | Mean ulcer area at 3 weeks (SD): US: 8.3 (6.4) C: 14.7 (10.4) Mean ulcer area at 8 weeks (SD): US: 6.2 (5.9) C: 13.4 (12.1) Ulcers completely healed at 8 weeks: US: 1/19 C: 0/19 (0/18 completers) US: no/minor complaints about pain with US. Mild to mod erythema often observed with US. |