Les blocs nerveux périphériques pour les fractures de la hanche
Información
- DOI:
- https://doi.org/10.1002/14651858.CD001159.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 11 mayo 2017see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Anestesia
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Joanne Guay: screened abstracts, search websites, checked reference lists for new articles, selected new articles, retrieved relevant articles, graded articles for risk of bias, extracted data, analysed data, interpreted results, rated quality of evidence and drafted the update.
Martyn Parker: reviewed the update for content before submission.
Richard Griifiiths: reviewed the update for content before submission.
Sandra Kopp: screened abstracts, selected new articles, graded articles for risk of bias, extracted data, interpreted results, rated quality of evidence and drafted the update.
Sources of support
Internal sources
-
University of Sherbrooke, Canada.
University of Sherbrooke granted access to electronic databases and to major medical journals.
-
University of Quebec in Abitibi‐Temiscamingue, Canada.
Universiuty of Quebec in Abitibi‐Temiscamingue provided access to electronic databases and medical journals.
-
Cochrane Anaesthesia, Critical and Emergency Care Group, Denmark.
The review authors wish to thank Karen Hovhannisyan, who designed the search strategy for this update.
External sources
-
No sources of support supplied
Declarations of interest
Joanne Guay: has no direct relationship with any pharmaceutical company or equipment manufacturer in the past five years. Has not acted as a witness expert in the past five years. Not an author of any of the included or excluded studies. Does not hold any stock other than mutual funds. Editor of a multi‐author textbook on anaesthesia (including notions on general and regional anaesthesia). Receives fees as associate professor for a course on airway management from University of Quebec in Abitibi‐Temiscamingue.
Martyn Parker: has received expenses and honorarium from several commercial companies and organizations for giving lectures on different aspects of hip fracture treatment. Has received royalties from BBrawn Ltd related to design and development of an implant used for internal fixation of intracapsular hip fractures.
Richard Griffiths: chaired Association of Anaesthetists of Great Britain & Ireland guidelines on proximal femoral fracture. Member of National Institute of Health and Care Excellence 124. Chaired Association of Anaesthetists of Great Britain & Ireland guidelines on surgery in the elderly. Founder of NHS Hip Fracture Perioperative Network.
Sandra Kopp: has no conflicts of interest.
Acknowledgements
The review authors thank Karen Hovhannisyan, who designed the search strategy for this update, as well as the University of Sherbrooke and the University of Quebec in Abitibi‐Temiscamingue for granting access to electronic databases and to medical journals.
We thank Harry Scheinin (Scheinin 2000), Fernando Altermatt (Altermatt 2013), Raquel Ortiz de la Tabla González (De La Tabla 2010), Jochen Gille (Gille 2006), K. Sanem Cakar Turhan (Bölükbasi 2013), Ashok Jadon (Jadon 2014) and Hongling Nie (Nie 2015), who provided additional information for the 2015 update, Karl Sales for traduction of two articles (Segado Jimenez 2009; Segado Jimenez 2010); and Gideon Heinert for translation of Gille 2006.
We would also like to thank Stephan Kettner (Content Editor); Jing Xie (Statistical Editor); Fernanda Fukushima, Pekka Tarkkila, Maya Keplinger, Thomas Fichtner Bendtsen and Thomas Dahl Nielsen (Peer Reviewers); and Patricia Tong (Consumer Referee) for help and editorial advice provided during preparation of this systematic review.
Version history
| Published | Title | Stage | Authors | Version |
| 2020 Nov 25 | Peripheral nerve blocks for hip fractures in adults | Review | Joanne Guay, Sandra Kopp | |
| 2017 May 11 | Peripheral nerve blocks for hip fractures | Review | Joanne Guay, Martyn J Parker, Richard Griffiths, Sandra Kopp | |
| 2002 Jan 21 | Nerve blocks (subcostal, lateral cutaneous, femoral, triple, psoas) for hip fractures | Review | Martyn J Parker, Richard Griffiths, Bal Appadu | |
Notes
For the first update (Issue 1, 2001), we made the following changes.
-
Included study of Chudinov 1999 on psoas compartment blocks.
-
Changed methods score to include item 8.
-
Changed statistical analysis to relative risks.
-
Added a synopsis.
In the second update (Parker 2002), we excluded one newly identified study (Van Leeuwen 2000) and included another (Scheinin 2000a). We have not made changes to the conclusions of the review.
We also updated this review in 2009. At that time, Cochrane updates did not earn a new citation unless they included new review authors or made a change to review conclusions.
For the 2016 update, we made the following changes.
-
Transferred this review to the Anaesthesia, Critical and Emergency Care Group from the Bone, Joint and Muscle Group.
-
Included two new review authors.
-
Updated the search in August 2016.
-
Updated the review and brought the methods up‐to‐date.
-
Excluded from the review studies evaluating neuraxial blocks (epidural/spinal) and wound infiltration as techniques of regional blockade.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Pain Management;
- Anesthetics, Local [administration & dosage, adverse effects];
- Confusion [epidemiology];
- Hip Fractures [mortality, *surgery];
- Movement;
- Myocardial Infarction [epidemiology];
- Nerve Block [adverse effects, *methods];
- Pain Measurement;
- Pain, Postoperative [therapy];
- Peripheral Nerves;
- Pneumonia [epidemiology];
- Randomized Controlled Trials as Topic;
- Time Factors;
Medical Subject Headings Check Words
Aged; Aged, 80 and over; Female; Humans; Male;
PICO
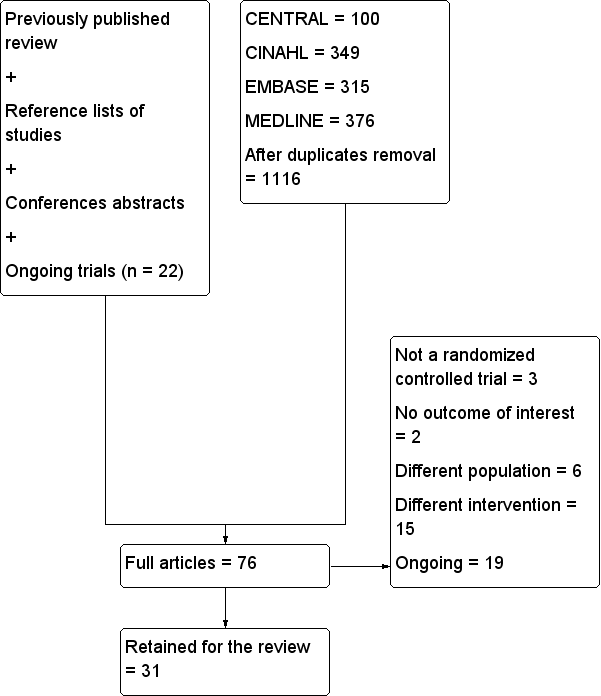
Flow diagram for this update.
n: number.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Pain on movement in participants with hip fracture between 20 and 30 minutes after block placement. The effect size is proportionate to the concentration of local anaesthetic (mg/mL) used in lidocaine equivalent (P < 0.00001).
Local anaesthetic concentration in lidocaine equivalent (calculated as follows: lidocaine = 1, bupivacaine = 4, chloroprocaine = 1.5, dibucaine = 4, etidocaine = 4, levobupivacaine = 3.9, mepivacaine = 0.8, prilocaine = 0.9, procaine = 0.5, ropivacaine = 3 and tetracaine = 4).
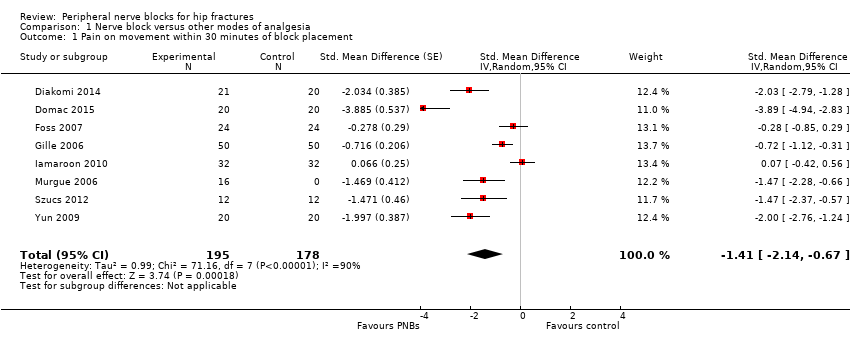
Comparison 1 Nerve block versus other modes of analgesia, Outcome 1 Pain on movement within 30 minutes of block placement.

Comparison 1 Nerve block versus other modes of analgesia, Outcome 2 Pain at rest within 30 minutes after block placement.

Comparison 1 Nerve block versus other modes of analgesia, Outcome 3 Pain at rest at 6 to 8 hours after surgery.

Comparison 1 Nerve block versus other modes of analgesia, Outcome 4 Pain on movement at 24 hours after surgery.

Comparison 1 Nerve block versus other modes of analgesia, Outcome 5 Pain at rest at 24 hours after surgery.
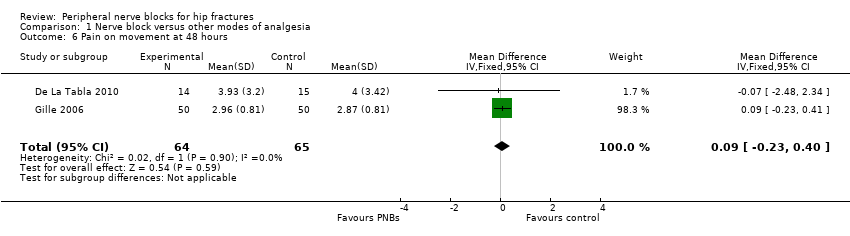
Comparison 1 Nerve block versus other modes of analgesia, Outcome 6 Pain on movement at 48 hours.
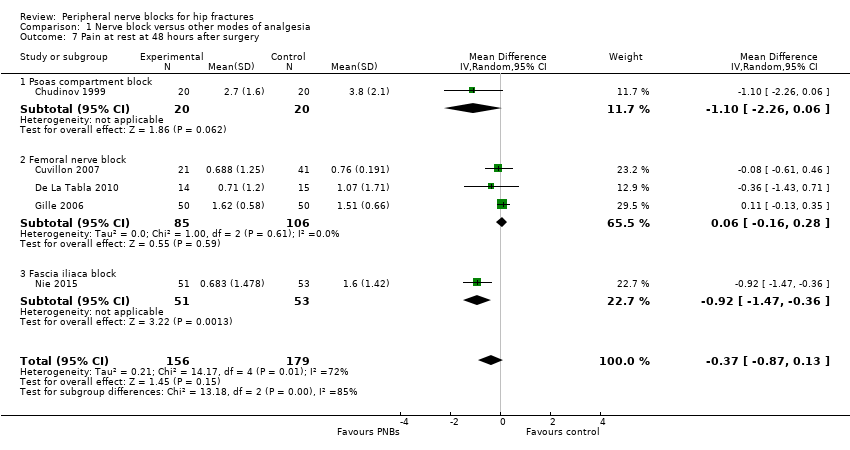
Comparison 1 Nerve block versus other modes of analgesia, Outcome 7 Pain at rest at 48 hours after surgery.
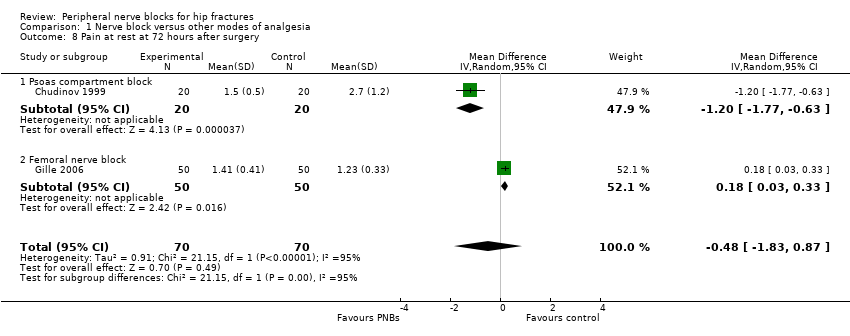
Comparison 1 Nerve block versus other modes of analgesia, Outcome 8 Pain at rest at 72 hours after surgery.
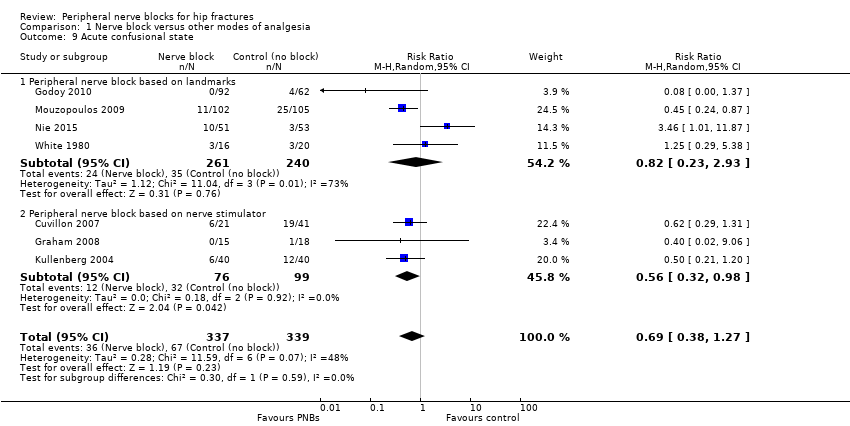
Comparison 1 Nerve block versus other modes of analgesia, Outcome 9 Acute confusional state.
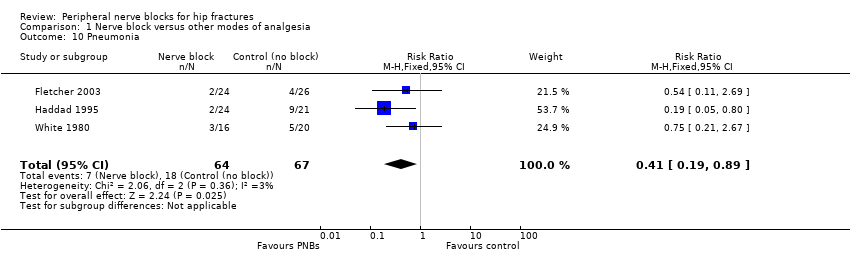
Comparison 1 Nerve block versus other modes of analgesia, Outcome 10 Pneumonia.
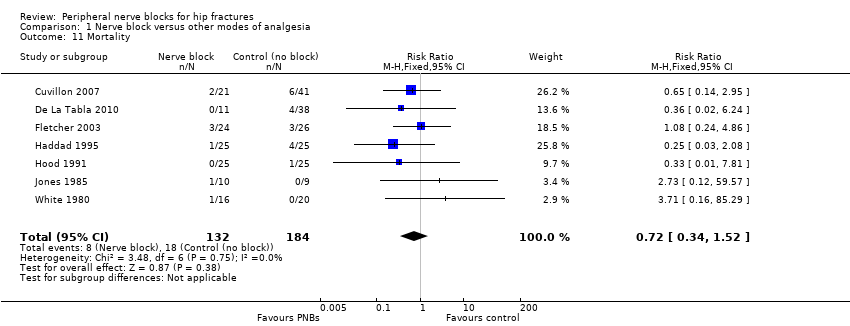
Comparison 1 Nerve block versus other modes of analgesia, Outcome 11 Mortality.

Comparison 1 Nerve block versus other modes of analgesia, Outcome 12 Time to first mobilization.

Comparison 1 Nerve block versus other modes of analgesia, Outcome 13 Costs of analgesic regimens.
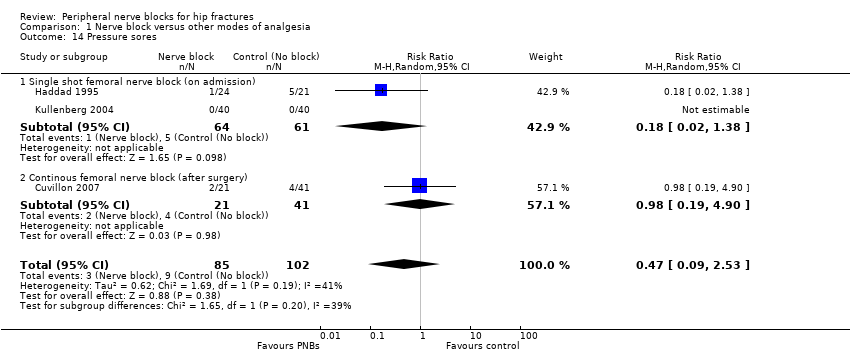
Comparison 1 Nerve block versus other modes of analgesia, Outcome 14 Pressure sores.
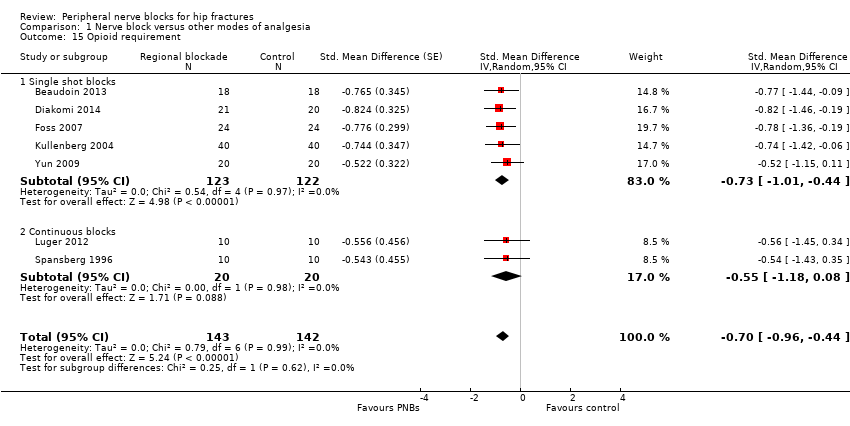
Comparison 1 Nerve block versus other modes of analgesia, Outcome 15 Opioid requirement.

Comparison 1 Nerve block versus other modes of analgesia, Outcome 16 Participant satisfaction.
| Peripheral nerve blocks for hip fracture | ||||||
| Patient or population: patients with hip fracture | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Systemic analgesia | Peripheral nerve blocks | |||||
| Pain on movement at 30 minutes after block placement | Mean pain on movement at 30 minutes after block placement in the intervention groups was | 373 | ⊕⊕⊕⊕ | Equivalent to | ||
| Acute confusional state | Study population | RR 0.69 | 676 | ⊕⊝⊝⊝ | ||
| 198 per 1000 | 136 per 1000 | |||||
| Low | ||||||
| 150 per 1000 | 104 per 1000 | |||||
| High | ||||||
| 250 per 1000 | 172 per 1000 | |||||
| Myocardial ischaemia | Study population | RR 0.2 | 20 | ⊕⊝⊝⊝ | ||
| 500 per 1000 | 100 per 1000 | |||||
| Low | ||||||
| 100 per 1000 | 20 per 1000 | |||||
| High | ||||||
| 500 per 1000 | 100 per 1000 | |||||
| Pneumonia | Study population | RR 0.41 | 131 | ⊕⊕⊕⊝ | ||
| 269 per 1000 | 110 per 1000 | |||||
| Low | ||||||
| 50 per 1000 | 20 per 1000 | |||||
| High | ||||||
| 200 per 1000 | 82 per 1000 | |||||
| Death | Study population | RR 0.72 | 316 | ⊕⊕⊝⊝ | ||
| 98 per 1000 | 70 per 1000 | |||||
| Low | ||||||
| 25 per 1000 | 18 per 1000 | |||||
| High | ||||||
| 150 per 1000 | 108 per 1000 | |||||
| Time to first mobilisation | Mean time to first mobilisation in intervention groups was | 155 | ⊕⊕⊕⊝ | |||
| Cost of analgesic regimens for single shot blocks | Mean cost of analgesic regimens for single shot blocks in intervention groups was | 75 | ⊕⊕⊕⊝ | |||
| The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| a50% or more of studies were rated as having unclear or high risk for allocation concealment or blinding of outcome assessor | ||||||
| Study | Purpose of blockade | Surgical anaesthesia | Block technique | Comparison |
| Preoperative and postoperative analgesia | Unspecified | Continuous lumbar plexus with 0.1% bupivacaine in a patient‐controlled analgesia mode | IV morphine | |
| Postoperative analgesia | Spinal anaesthesia | Continuous femoral nerve block, nerve stimulator, loaded with 18 mL of 0.25% bupivacaine followed by an infusion of 0.125% levobupivacaine at 3‐4 mL/h | IM pethidine | |
| Preoperative analgesia | Unspecified | Ultrasound‐guided femoral nerve block performed by an experienced operator with a 7.5 MHz linear probe, participant in Trendelenburg position, cross‐sectional view, 22 G Whitacre needle in‐plane and 25 mL of bupivacaine 0.5% and distal manual pressure for 5 minutes | IM morphine | |
| Preoperative and postoperative analgesia Surgery for some participants | Treatment group: psoas block alone (3/20) with a sciatic block (5/20), a spinal (11/20) or general anaesthesia (1/20) Control group: neuraxial block (19/20) or general anaesthesia (1/20). | Psoas, loss of resistance, Chayen's technique 0.8 mL/kg of bupivacaine 0.25%, operated side up (1 epidural spread) | IM meperidine and diclofenac | |
| Postoperative analgesia | General anaesthesia for all participants with etomidate, nitrous oxide, enflurane, fentanyl and vecuronium | Lateral cutaneous: 15 mL of 0.5% bupivacaine with epinephrine, Eriksson's technique Femoral (3‐in‐1): 15 mL of 0.5% bupivacaine with epinephrine, Winnie's technique | IM meperidine | |
| Postoperative analgesia | Spinal anaesthesia for all participants | Continuous femoral nerve block. Nerve stimulator 0.3 to 0.5 mA. Non‐stimulating catheter passed 10‐15 cm past the needle tip loaded with 30 mL of 1.5% lidocaine followed by ropivacaine 0.2% at 10 mL/h for 48 hours | SC morphine | |
| Preoperative analgesia | Unspecified | Femoral nerve block under dual guidance (ultrasound and nerve stimulator), catheter loaded with 15 mL of ropivacaine 0.2% followed by an infusion of the same solution at 5 mL/h and 10 mL every 30 minutes | IV metamizole and tramadol | |
| Preoperative analgesia (spinal positioning) | Spinal anaesthesia | Fascia iliaca block, Dalen's technique, landmarks, 40 mL of 0.5% ropivacaine | IV fentanyl | |
| Preoperative analgesia (spinal positioning) plus postoperative analgesia | Spinal anaesthesia | Fascia iliaca block with 15 mL of 0.5% bupivacaine and 15 mL of 2% lidocaine; 2‐3 cm below inguinal ligament at the junction of lateral 1/3 and medial 2/3 of a line from pubis tubercle to anterior iliac spine; 2 pops | IV morphine | |
| Preoperative analgesia | Unspecified | Fermoral (3‐in‐1 nerve block, Wiinie's technique with 20 mL of 0.5% bupivacaine and 5 minutes distal compression) | IV morphine | |
| Preoperative analgesia | Unspecified | Fascia iliaca block based on Dalen's landmarks with a 24 G blunted needle and 40 mL of 1% mepivacaine with epinephrine | IM morphine | |
| Preoperative and postoperative analgesia | Treatment group: spinal anaesthesia for 37/50 and general anaesthesia for 13/50 Control group: spinal anaesthesia for 38/50 and general anaesthesia for 12/50 | Femoral non‐stimulating catheter: needle 18 G, catheter 20 G (Brown‐Perifix‐Plexus Anaesthesia); 0.5 mA and 0.1 msec. Catheters were advanced about 10 cm past the needle tip and fixed. Loading dose was 40 mL of prilocaine 1% followed 2 hours later by ropivacaine 0.2% 30 mL, repeated every 6 hours. Amount (up to 40 mL; n = 5) and intervals (up to every 4 hours; n = 8) or both (n = 6) adjusted on pain scores | IV metamizole plus oral tilidine and naloxone | |
| Preoperative analgesia | Unspecified | Fascia iliaca compartment block, 21G long bevel needle, Dalen's technique with 0.3 mL/kg of 0.25% bupivacaine | IV non‐steroidal anti‐inflammatory drugs | |
| Preoperative analgesia | Unspecified | Femoral (3‐in‐1) nerve block, Winnie's technique, nerve stimulator and 30 mL of bupivacaine 0.5% (not exceeding 3 mg/kg) | IV morphine | |
| Preoperative analgesia | Unspecified | Femoral nerve block with 0.3 mL/kg of bupivacaine 0,25%. Paraesthesia technique with a short bevel needle | IM pethidine, oral co‐dydramol and IM voltarol | |
| Postoperative analgesia | General anaesthesia for all participants with etomidate, nitrous oxide, isoflurane and alfentanil | Femoral nerve block (triple nerve block) with nerve stimulator < 1.0 mA and 35 mL of prilocaine 0.75% and distal digital pressure plus infiltration above the iliac crest with 8 mL of the same solution | IM papaveratum | |
| Preoperative analgesia | Spinal anaesthesia | Femoral nerve block with nerve stimulator (0.2 to 0.4 mA) and 20 mL of bupivacaine 0.5% plus 10 mL of saline | IV fentanyl | |
| Preoperative analgesia | Spinal anaesthesia | Femoral nerve block with nerve stimulator (0.3 to 0.5 mA) and 15 mL of lidocaine 2% plus 5 mL of distilled water | IV fentanyl | |
| Postoperative analgesia | General anaesthesia for all participants with thiopental, nitrous oxide, halothane, fentanyl and alcuronium | Lateral cutaneous nerve block with 15 mL of 0.5% bupivacaine, Eriksson's technique | IM pethidine | |
| Preoperative analgesia | Unspecified | Femoral nerve block with 30 mL of 0.75% ropivacaine. Winnie's approach and nerve stimulator | IM ketobemidon plus tramadol and paracetamol | |
| Preoperative and postoperative analgesia | Spinal anaesthesia | Ultrasound‐guided femoral (3‐in‐1) nerve block (13‐6 MHz linear probe), catheter inserted ≥ 12‐15 cm past the needle tip) loaded with 30 mL of 0.25% bupivacaine followed by an infusion of 0.125% bupivacaine at 6 mL/h (motor blockade not evaluated) or Lumbar epidural analgesia with 0.125% bupivacaine at 8 mL/h | IV/SC piritramide or IV paracetamol | |
| Preoperative analgesia | Spinal anaesthesia | Fascia iliaca block with 20 mL of 1.5% lidocaine | IV fentanyl | |
| Preoperative and postoperative analgesia | Epidural anaesthesia | Fascia iliaca block daily, Dalen's technique with 0.3 mL/kg of bupivacaine (0.25%?) | IV and analgesics | |
| Preoperative analgesia | Unspecified | Femoral nerve block with nerve stimulator and 20 mL of mepivacaine | IV morphine or IV paracetamol and ketoprofen | |
| Postoperative analgesia | General anaesthesia with propofol, remifentanil and atracurium | Fascia iliaca block with landmarks (2‐3 cm below the inguinal ligament); catheter inserted at least 10 cm cranially and loaded with 20 to 30 mL (weight basis) of 0.5% ropivacaine followed by 0.25% bupivacaine at 0.1 mL/kg/h for 48 hours | IV patient‐controlled analgesia with fentanyl and tropisetron | |
| Postoperative analgesia | Spinal anaesthesia | Landmarks. Obturator nerve with 15 mL of bupivacaine with a vasoconstrictive agent, proximal to the obturator orifice. Femoral lateral cutaneous (Brown) with 10 mL of the same solution | IV morphine | |
| Postoperative analgesia | Spinal anaesthesia | Femoral nerve block with nerve stimulator, non‐stimulating catheter advanced 8‐15 cm past needle tip. Inserted just before surgery. Loaded with 0.4 L/kg of bupivacaine 0.5%; continuous infusion with 0.14 mL/kg/h of bupivacaine 0.25% for 16 hours after surgery | IM morphine | |
| Preoperative and postoperative analgesia | Spinal anaesthesia | Non‐stimulating catheter for femoral nerve block, inserted in the emergency department with a nerve stimulator, 0.4 mA and 0.1 msec, space dilated before catheter insertion with 10 mL of 2% lidocaine, catheter advanced 3 cm past the needle tip and 10 mL of 0.5% bupivacaine through the catheter followed by 0.25% bupivacaine infused at | IM morphine | |
| Postoperative analgesia | General anaesthesia for all participants with propofol, nitrous oxide, isoflurane, fentanyl, morphine and atracurium | Femoral (3‐in‐1) nerve block, nerve stimulator 0.1 mA, non‐stimulating catheter advanced 4‐5 cm past the needle tip. Loaded with 30 mL of 2% lidocaine with epinephrine followed by an infusion with bupivacaine 0.125% at 4 mL/h for 48 hours | IV morphine | |
| Intraoperative analgesia | General anaesthesia with thiopental, nitrous oxide, halothane and fentanyl or nitrous oxide and alfaxolone/alfadolone | Psoas block with 30 mL of 2% mepivacaine, side to be blocked uppermost, Chayen's technique or Spinal: 0.6 to 0.8 mL of hyperbaric cinchocaine | Conventional general anaesthesia | |
| Preoperative analgesia | Spinal anaesthesia | Fascia iliaca block, Dalen's technique with 30 mL of 0.375% ropivacaine | IV alfentanil | |
| G: gram h: hour IM: intramuscular mA: milliAmpere mcg/mL: microgram/millilitre mg/kg: milligram/kilogram MHz: megahertz mL: millilitre msec: millisecond n: number SC: subcutaneous | ||||
| Study | Study authors' definition |
| Clinical evaluation "somnolence‐confusion" | |
| "episodes of delirium" | |
| "acute confusional state" | |
| "transient confusion" | |
| "The primary outcome was perioperative delirium. "Daily patient assessments using the MMSE, DRS‐R‐ | |
| "Presurgery cognitive status was estimated using the | |
| "confused" |
| Study | Complications related to regional anaesthesia | Complications related to analgesic technique |
| Not reported | Not reported | |
| No complications such as motor block. local Five participants had accidental removal or the catheter: 4 during the procedure or while the catheter was secured and 1 while in the ward | Not reported | |
| No other adverse events were noted during the study period, and no other adverse events were reported to study investigators | Four‐hour oxygen saturation (%) 96 (93–99) vs (%) 98 (95–99) for regional blockade Adverse events: One participant had an episode of rapid atrial fibrillation requiring diltiazem, but the participant had a history of chronic atrial fibrillation | |
| No major complications were described in group regional blockade. Three participants developed local erythema at the catheter insertion site at the end of the study period No signs of local anaesthetic toxicity were documented One participant developed bilateral blockade (L1‐L3 on the opposite side) | Not reported | |
| No complications related to nerve blocks and no case of prolonged motor blockade | Not reported | |
| Four catheters were prematurely removed: 1 by a confused participant, 2 by nurses (unexplained fever) and 1 by a surgeon (unconfirmed suspicion of local anaesthetic toxicity (ropivacaine blood level < 2 ng/mL)) | More constipation (47% vs 19% for regional blockade) | |
| Not reported | Not reported | |
| Complications such as local anaesthetic toxicity recorded as well (none reported in results section) Nor did complication rates vary between groups | Complications such as hypoventilation (breathing rate < 8 breaths/min) were recorded as well Moreover, the 2 groups did not differ in these parameters at any time point until study completion at 24 hours after surgery. Nor did complication rates vary between groups | |
| Not reported | Not reported | |
| Among study participants, none experienced adverse effects as a result of nerve block administration | No clinically important differences between groups with respect to pulse rate, oxygen saturation or respiratory rate at any time interval. Oxygen saturation 94.87% | |
| No side effects attributable to femoral nerve block were noted in any participants during their hospital stay | More participants (P = 0.05) were sedated in the morphine group at 180 minutes after block placement No difference was noted between groups in nausea and vomiting, with 3 participants in each group having these side effects Tendency toward lower saturation was noted in the opioid group at 60 and 180 minutes after the block despite oxygen supplementation (P = 0.08) | |
| One inadvertent arterial puncture and blood aspiration positive for 3 participants Two transient paraesthesias No catheter site infection Ten catheters accidentally removed | No respiratory depression from systemic analgesia and no allergic reactions All complications were reversible | |
| The only complications were local bruises at the site of injection | Two participants with nausea, and 2 with nausea and vomiting | |
| No immediate complications occurred in either group | No immediate complications were noted in either group | |
| No local or systemic complications of femoral nerve blocks were noted | Not reported | |
| No untoward sequelae were associated with nerve blocks All plasma prilocaine concentrations (maximum 3 pg/mL) were below the suggested threshold for toxicity for prilocaine of 6 pg/mL | Not reported | |
| No adverse systemic toxicity of bupivacaine, such as seizure, arrhythmia or cardiovascular collapse was noted in the femoral nerve block group Neither vascular puncture nor paraesthesia occurred No complications, such as haematoma, infection or persistent paraesthesia, were observed within 24 hours after the operation | No participant in either group had hypoventilation (ventilatory rate < 10/min) or oxygen saturation < 95% | |
| Not reported | In participants of fentanyl group, drowsiness was observed that required the presence of more persons for holding the participant during positioning SpO2 was significantly lower in the fentanyl group (P = 0.001). However, no participant in either group had SpO2 < 90% during the procedure Mean arterial blood pressure was significantly lower in the fentanyl group (P = 0.0019) | |
| No untoward sequelae associated with the nerve block were seen | Not reported | |
| No complications related to the nerve blockade were noted in this study | Not reported | |
| Not reported | Not reported | |
| Not reported | Not reported | |
| No complications of femoral nerve block administrations occurred, except 3 local haematomas developed at the injection site, which resolved spontaneously | Not reported | |
| Not reported | Not reported | |
| No adverse effects, such as pain at the insertion site or paraesthesia, were observed No positive cultures were observed with the fascia iliaca block catheter tip, nor were any signs of infection noted in the current study | Not reported | |
| We did not observe any complications in the realization of regional anaesthetic techniques during or subsequent to the regional anaesthetic techniques | The incidence of side effects (sleepiness, hypotension, constipation, pruritus) was greater in the group with no block than in groups with blocks (P < 0.01) | |
| No haematomas at the site of femoral catheters | Two participants in each group experienced nausea and vomiting | |
| For 1 participant, the elastomeric pump failed, resulting in local anaesthetic administered over less than 54 hours instead of 72 hours, and another participant, suffering from acute confusional state, disconnected his pump after 12 hours | The incidence of nausea/vomiting, pruritus or excessive sedation was similar in the 2 groups | |
| Not reported | Side effects (vomiting and pruritus) were observed significantly more frequently with intravenous analgesia | |
| No participants showed any evidence of local anaesthetic toxicity | Not reported | |
| No adverse systemic toxicity of ropivacaine was noted, and neither vascular puncture nor paraesthesia was elicited No complications, such as haematoma or persistent paraesthesia, were observed in participants with a femoral nerve block within 24 hours after the operation | Hypoventilation (ventilatory rate 6–8/min) or pulse oximetric desaturation (oxygen saturation 88% or 89%) was encountered in 4 participants (20%) in the intravenous analgesia group. This was reverted with assisted manual mask ventilation All participants in the intravenous group experienced mild dizziness, and mild drowsiness was present in 12/20 of them | |
| %: percentage L: litre mg: milligram min: minute ng/mL: nanogram/millilitre pg/mL: picogram/millilitre | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain on movement within 30 minutes of block placement Show forest plot | 8 | 373 | Std. Mean Difference (Random, 95% CI) | ‐1.41 [‐2.14, ‐0.67] |
| 2 Pain at rest within 30 minutes after block placement Show forest plot | 7 | 322 | Std. Mean Difference (Random, 95% CI) | ‐0.80 [‐1.25, ‐0.35] |
| 3 Pain at rest at 6 to 8 hours after surgery Show forest plot | 5 | 286 | Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.70, ‐0.06] |
| 4 Pain on movement at 24 hours after surgery Show forest plot | 4 | 195 | Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐1.08, 0.30] |
| 4.1 Surgical technique unspecified | 3 | 169 | Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.10, 0.29] |
| 4.2 Arthroplasty for 38.4% of participants | 1 | 26 | Mean Difference (IV, Random, 95% CI) | ‐1.94 [‐2.75, ‐1.13] |
| 5 Pain at rest at 24 hours after surgery Show forest plot | 8 | 435 | Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐1.23, ‐0.13] |
| 5.1 Single shot blocks | 2 | 80 | Mean Difference (IV, Random, 95% CI) | ‐0.5 [‐0.90, ‐0.10] |
| 5.2 Continuous blocks | 6 | 355 | Mean Difference (IV, Random, 95% CI) | ‐0.78 [‐1.58, 0.03] |
| 6 Pain on movement at 48 hours Show forest plot | 2 | 129 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.23, 0.40] |
| 7 Pain at rest at 48 hours after surgery Show forest plot | 5 | 335 | Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.87, 0.13] |
| 7.1 Psoas compartment block | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐1.10 [‐2.26, 0.06] |
| 7.2 Femoral nerve block | 3 | 191 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.16, 0.28] |
| 7.3 Fascia iliaca block | 1 | 104 | Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐1.47, ‐0.36] |
| 8 Pain at rest at 72 hours after surgery Show forest plot | 2 | 140 | Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐1.83, 0.87] |
| 8.1 Psoas compartment block | 1 | 40 | Mean Difference (IV, Random, 95% CI) | ‐1.20 [‐1.77, ‐0.63] |
| 8.2 Femoral nerve block | 1 | 100 | Mean Difference (IV, Random, 95% CI) | 0.18 [0.03, 0.33] |
| 9 Acute confusional state Show forest plot | 7 | 676 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.38, 1.27] |
| 9.1 Peripheral nerve block based on landmarks | 4 | 501 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.23, 2.93] |
| 9.2 Peripheral nerve block based on nerve stimulator | 3 | 175 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.32, 0.98] |
| 10 Pneumonia Show forest plot | 3 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.19, 0.89] |
| 11 Mortality Show forest plot | 7 | 316 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.34, 1.52] |
| 12 Time to first mobilization Show forest plot | 2 | 155 | Mean Difference (IV, Random, 95% CI) | ‐11.25 [‐14.34, ‐8.15] |
| 13 Costs of analgesic regimens Show forest plot | 2 | Std. Mean Difference (Random, 95% CI) | Subtotals only | |
| 13.1 Single shot blocks | 1 | 75 | Std. Mean Difference (Random, 95% CI) | ‐3.48 [‐4.23, ‐2.74] |
| 13.2 Continuous blocks | 1 | 62 | Std. Mean Difference (Random, 95% CI) | 0.93 [0.37, 1.48] |
| 14 Pressure sores Show forest plot | 3 | 187 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.09, 2.53] |
| 14.1 Single shot femoral nerve block (on admission) | 2 | 125 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.02, 1.38] |
| 14.2 Continous femoral nerve block (after surgery) | 1 | 62 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.19, 4.90] |
| 15 Opioid requirement Show forest plot | 7 | 285 | Std. Mean Difference (Random, 95% CI) | ‐0.70 [‐0.96, ‐0.44] |
| 15.1 Single shot blocks | 5 | 245 | Std. Mean Difference (Random, 95% CI) | ‐0.73 [‐1.01, ‐0.44] |
| 15.2 Continuous blocks | 2 | 40 | Std. Mean Difference (Random, 95% CI) | ‐0.55 [‐1.18, 0.08] |
| 16 Participant satisfaction Show forest plot | 5 | 237 | Std. Mean Difference (Random, 95% CI) | 0.91 [0.62, 1.20] |

