Les interventions dans les médias de masse pour la prévention du tabagisme chez les jeunes
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Design: Controlled clinical trial; nested, cluster (procedures identified probability samples of households within each area screened for adolescent), non‐equivalent control group Country: USA Objective: To evaluate the effectiveness of a mass media campaign to prevent cigarette smoking in adolescents Study site: (schools) Standardised Metropolitan Statistical Areas (SMSAs); Homes in SMSAs in SE USA Method of analysis: Logistic and linear regression (both individual ‐ accounting for unit of allocation ‐ and SMSAs treated as unit of analysis), ANOVA Confounders analyzed: Individual respondents, treatments, sociodemographic status, personality predictors of adolescent smoking | |
| Participants | Age: 12 ‐ 15 yrs Gender: boys and girls (further details not provided) Ethnicity: SMSAs with > 90% whites excluded | |
| Interventions | Programme name: RADIO, RPEER, RTVPEER Theoretical basis: Behavioural science theory and research; Formative media research used to develop TV and radio messages Intervention description 1.) RADIO: 8 x 30‐sec radio messages about 7 expected consequences of smoking that are related to whether young people become regular smoker, relevant to adolescents, broadcast in 2 SMSAs Intervention description 2.) RPEER: Same as RADIO, plus 60‐sec message inviting entry into “I won't smoke “ sweepstake, prize USD 2000, with a USD 20 incentive to recruit 5 (+) entrants, broadcast in 2 SMSAs. Brochures mailed to respondents and recruits encouraging communication with peers to discourage smoking Intervention description 3.) RTVPEER: Same as RPEER plus TV broadcast of sweepstake offer and only 3 expected consequence messages, broadcast in 2 SMSAs Control description: CONTROL: No media intervention Duration/study dates: Expected consequences messages broadcast during Nov 1985, Jan and April 1986. TV sweepstake offer Nov 1985. Brochures mailed Jan 1986 ‐ Feb 1987 Intervention delivery: Messages delivered by adolescent speakers (thoughtful, self‐confident, casually dressed peer, being most appropriate image suggested by formative media research) | |
| Outcomes | Reported outcomes: Validation: alveolar CO and saliva thiocyanate levels Follow‐up: time‐period: 11 ‐ 17 months after broadcasts ended, 2 ‐ 8 months after brochures mailed | |
| Notes | Selection of SMSAs was influenced by cost of advertising, legal restrictions (e.g. sweepstakes illegal in some areas) and need for non‐overlapping broadcast areas Random geographic allocation of SMSAs to treatment conditions; 6 intervention, 4 control Number of participants across SMSAs ranged from 132 to 232 (2534 eligible) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Some randomization was attempted, but methods not described, and 2 of the SMSAs had to be reallocated to different arms of the study |
| Allocation concealment (selection bias) | High risk | No allocation concealment occurred |
| Blinding (performance bias and detection bias) | High risk | No mention of blinding in the study. Blinding not possible due to nature of the intervention |
| Incomplete outcome data (attrition bias) | High risk | Significant departure of follow‐up sample, likely to be related to true outcome (this group are smokers or more likely to be smokers); different recruitment methods resulted in some participants not having data collected |
| Selective reporting (reporting bias) | High risk | Additional data that were collected were not presented in any of the publications; 1000 adolescents excluded from analysis; Roanoke students excluded from analysis due to teacher recruitment |
| Other bias | High risk | Sample sizes too small to even observe a 0.50 significance level; gender, ethnicity and socio‐economic status is not quantified in any of the publications; gender was not asked, but coded as male or female based on first names, producing identification of only 90% of applicants. Authors state that findings could not be generalized to all participants in the mass media to smoking prevention |
| Imbalance of outcome measures at baseline | High risk | Significant differences in smoking rates; once adjustments occurred these differences were even more significant |
| Comparability of intervention and control group characteristics at baseline | High risk | Significant inter‐community variation; significant differences in smoking rates and experimentation between communities; following adjustment for known correlates, the differences were strengthened in every case |
| Protection against contamination | Unclear risk | Unable to determine level of contamination through communities via teachers or students, but it is possible. Also the sweepstakes involved recruiting friends, who would possibly be from the control or other intervention groups. Hence possible contamination, but not confirmed |
| Selective recruitment of participants | High risk | SMSAs were selected based on location and community traits to reduce overlap; students were recruited by phone at random, but selection methods not described; personal contacts were made for 1 intervention group (RPEER) more than any other; participant self‐selection, but partly adjusted for |
| Methods | Design: Interrupted time‐series study Country: USA Objective: To evaluate an intervention to reduce smoking among young adult ‘partiers’ in Oklahoma Study site: Partier crowds who attended night clubs, bars and other popular clubs (n=33) Method of analysis: Chi2 test for categorical variables and Wilcoxon signed rank test for continuous variables; multivariate multinomial regression examined the association between recall of intervention and outcomes of smoking Confounders analyzed: Demographic and attitudinal covariates | |
| Participants | Age: 18 to 26 years (n = 188 between 18 and 20 years; n = 1942 between 21 and 23 years; n = 1218 between 24 and 26 years) Gender: n = 1594 male Ethnicity: n = 2027 white; n = 325 African‐American; n = 469 Hispanic; n = 188 Asian/Pacific Islander; n = 177 American Indian/Alaskan Native; n = 137 other; n = 25 unaccounted for in the full text | |
| Interventions | Programme name: HAVOC Theoretical basis: Social branding intervention Intervention description: The intervention was designed to influence smoking behaviour by associating the smoke‐free HAVOC brand with partiers at social events and build an association between that brand and characteristics valued by partiers (confidence, social success and physical attractiveness); HAVOC included sponsored events, brand ambassadors, social media, direct mail and involved influential DJs, promoters and socialites; social games were used to build an association between being social and living tobacco‐free; signage throughout the clubs included videos and banners reinforcing the tobacco prevention message; social media campaigns (YoTube, Twitter and Facebook) launched in March 2010 and direct mail sustained HAVOC messages following events Control description: Not relevant Duration/study dates: HAVOC events occurred over 3 years (2010 ‐ 2012); by final follow‐up over 17,000 people attended a HAVOC event, > 11,000 likes on the HAVOC Facebook page, with over 17 direct mailings, 38 e‐mails and 41 text messages to the > 2950 unique addresses, 3000 e‐mail addresses and 1850 cell phones; The estimated reach of the campaign was 42,500 ‐ 45,000 individual occasions with almost 85,000 impressions by e‐mail Intervention delivery: HAVOC ambassadors (n > 200) were trained to deliver the messages and top brand ambassadors were hired to staff the HAVOC events and provide feedback | |
| Outcomes | Reported outcomes: Follow‐up time‐period: 2 years (3 time periods) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants were not randomly assigned |
| Allocation concealment (selection bias) | High risk | No allocation concealment occurred |
| Blinding (performance bias and detection bias) | High risk | No blinding occurred |
| Incomplete outcome data (attrition bias) | High risk | 25 participants do not have ethnicity accounted for in the full text; Interrupted time‐series design, hence, individual participant attrition not relevant |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Imbalance of outcome measures at baseline | Unclear risk | Insufficient information to permit judgement |
| Comparability of intervention and control group characteristics at baseline | Unclear risk | No control group |
| Protection against contamination | Unclear risk | Insufficient information to permit judgement |
| Selective recruitment of participants | Unclear risk | Insufficient information to permit judgement |
| Methods | Design: Randomized controlled trial, factorial, nested, cluster, non‐equivalent control group, (multi‐attribute blocking approach) Country: USA Objective: To test the independent and combined effects of a classroom curriculum and TV programming for social resistance skills training, smoking prevention, and smoking cessation Study site: Schools, homes and towns in Los Angeles and San Diego, Southern California Analysis: Regression (accounting for school as unit of allocation and individual as unit of analysis) | |
| Participants | Age: 12 ‐ 14 year olds Gender: At 2‐year follow‐up 47.6% of the overall population were boys Ethnicity: Whole sample population at pre‐test: Hispanic 35.5%, white 33.3%, African‐American 13.9%, other 17.3%; Whole sample population at 2‐year follow‐up: Hispanic 36.1%, 33.3% white, 13.9% African‐American, and 17.3% other | |
| Interventions | Programme name: The Television, School and Family Smoking Prevention and Cessation Project, (TVSFP) Theoretical basis: Social influences approach and communications theory. Diagnostic and formative media research with TV staff to develop scripts Los Angeles: Intervention description 1.) School curriculum +TV: Classwork and homework activities between students and parents for both prevention and cessation in the home, supplemented by TV segments to provide convincing resistance skill models for students and cessation strategies for adults. A workbook identical to that sent from the TV station to requesters was also sent home with students Intervention description 2.) Curriculum‐only: Classwork and homework activities between students and parents for both prevention and cessation in the home. The workbook for the CR‐Only condition made no reference to the TV program, but in all other respects was the same as that of the TV condition Intervention description 3.) TV‐Only: TV segments to provide convincing resistance skill models for students and cessation strategies for adults, with a supplemented workbook identical to that sent from the TV station to requesters Control description 1.) Attention control placebo: A health information‐based attention‐control curriculum. Outcome expectancies that were equivalent to the treatment conditions, but which was not expected to change smoking behaviour. It was thought that a health information‐based programme would increase students’ tobacco and health knowledge without increasing their social‐resistance skills or subsequently decreasing their smoking, thus providing an effective control for expectancy effects. Control description 2.) No‐treatment control: Usual practice San Diego: Intervention description 4.) Curriculum‐only: Social resistance classroom curriculum only Control description 3.) No treatment control: Usual practice Duration/study dates: 6 weeks: weeks 1 and 6, classroom curricula delivered and TV smoking prevention messages broadcast; week 2, TV cessation messages for adults broadcast in same area as TV prevention messages, first commencing in February/March 1986 until 1988 Intervention delivery: Physician host of regular primetime TV health news programme, presented smoking prevention messages based on filmed classroom sessions; Usual classroom teachers for school programme, with parental involvement in homework | |
| Outcomes | Reported outcomes: Expired air samples collected as a 'bogus pipeline' procedure to encourage more accurate self‐reports (No process measures stated) Follow‐up time period: immediately post‐intervention, 1 year, 2 years | |
| Notes | Students in 47 schools (340 classrooms) in 6 school districts | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Graham 1984 randomized multi‐attribute blocking design, but methods of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Schools randomized to conditions which were open‐label, but method of allocation concealment not described |
| Blinding (performance bias and detection bias) | High risk | No allocation concealment occurred |
| Incomplete outcome data (attrition bias) | High risk | Loss of > 50% of the original sample at 2‐year follow‐up. Those more likely to drop out were from Los Angeles, African‐American and had lower school grades; missing data and attrition problems decreased by methods of analysis, but still a concern; coping effort outcome data had fewer responders |
| Selective reporting (reporting bias) | Unclear risk | Insufficient data to determine selective outcome reporting |
| Other bias | High risk | TV programme design issues do not meet research objectives fully; low stability values for results due to length of time between measures and circumstances of an intervention; design issues, as this is an incomplete factorial design, which may introduce bias when entering raw data into generic statistical software analysers; programme poorly executed, sample size too small, ‘floor effects’ could be related to true outcome |
| Imbalance of outcome measures at baseline | High risk | Control group more likely not to start smoking at baseline |
| Comparability of intervention and control group characteristics at baseline | Low risk | No substantial pre‐test differences requiring adjustment |
| Protection against contamination | Low risk | Media controlled for by replicating these conditions in a second metropolitan site (San Diego) |
| Selective recruitment of participants | High risk | n values vary depending on number of participants available for each outcome, i.e. those with data in 1 outcome but not in another will still be included in that 1 outcome |
| Methods | Design: Controlled clinical trial; nested, non‐equivalent control group; interrupted time‐series design Country: USA Objective: To test the effectiveness of mass media interventions to enhance school smoking prevention programmes Study site: Homes with TV and schools in Standardised Metropolitan Statistical Areas (SMSAs), 2 SMSAs in Northeastern USA and 2 in Montana Method of analysis: Logistic regression (unit of allocation community, unit of analysis individual, adjusted for in analysis) Confounders analyzed: Treatment group, gender, grade | |
| Participants | Age: 9 ‐ 17‐year‐olds Gender: Intervention ‐ girls 51.8%, boys 48.2%; Control ‐ girls 47%, boys 53% Ethnicity: Intervention white 97.2%; Control white 95.6% | |
| Interventions | Programme name: Not provided Theoretical basis: Social learning theory and related behaviour change theories. Diagnostic and formative media research with student focus group Intervention description: Specifically designed 30‐ and 60‐second TV and radio spot messages broadcast as a campaign averaging 190 TV broadcasts, 350 cable TV, and 350 radio exposures purchased in each of the 4 years in each of the 2 targeted media SMSAs. Paid media time was increased by 50% by donated media time. Media exposure modified to match changing media use of maturing cohort. Survey data informed the timing and placement of advertisements Control description: Schools‐only programme ‐ grade‐specific educational materials used in 3 ‐ 4 class period with 10 ‐ 15‐year‐olds: information about smoking and health, refusal skills, skills to resist advertising pressures, and awareness of social support for non‐smoking were included Duration/study dates: 4 years between 1986 and 1989 Intervention delivery: Intervention: Diagnostic and formative media research used to identify most appropriate media, time placement and images. Control: Usual class teacher, trained by project staff during 4 annual day‐long teacher‐training workshops | |
| Outcomes | Reported outcomes: Smoking perceptions (perceived norms, adult smoking, peer smoking and sibling smoking) Saliva samples from school group, as a 'bogus pipeline' procedure to encourage more accurate self‐reports Follow‐up time period: annually over 4‐year intervention and 2 years post‐intervention, (6 total) | |
| Notes | School and mass media intervention linked only by educational objectives, intended to be seen as independent sources of information 4 demographically‐matched study communities selected to provide 2 pairs of SMSAs, targeting high‐risk populations indicated by adult educational attainment and income. 50 schools selected from census tracts, indicating higher risk for smoking | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not random selection. Geographical allocation based on census tracts |
| Allocation concealment (selection bias) | High risk | Participants and investigators were aware of student assignment. No randomization occurred |
| Blinding (performance bias and detection bias) | High risk | No outcome assessor or investigator blinding has been mentioned |
| Incomplete outcome data (attrition bias) | High risk | The missing outcome data from the 2918 students whose data were not available for comparison is likely to be related to the true outcome; furthermore, excluded participants had a less stable family environment, which may be related to higher smoking prevalence |
| Selective reporting (reporting bias) | High risk | P828B "A supplemental analysis is presented in which the community is the unit, although the original design was not intended to support this analytic strategy." These primary outcomes were not prespecified |
| Other bias | High risk | Design bias; communities were selected due to high risk, not randomization; baseline imbalance in intervention arm statistically significant, may have affected outcome; and control group had a higher prevalence of smoking; design concern: low statistical power to determine meaningful results |
| Imbalance of outcome measures at baseline | Unclear risk | None of the baseline outcomes differed significantly for the 2 groups, except that the school‐only group reported perceiving more peer smoking. The degree to which this occurred and its significance are unclear |
| Comparability of intervention and control group characteristics at baseline | High risk | Intervention group had a younger population, (P < 0.01) and a larger proportion of girls (P < 0.01) |
| Protection against contamination | Unclear risk | Insufficient information to assess this outcome |
| Selective recruitment of participants | Unclear risk | Insufficient information to assess this outcome |
| Methods | Design: Randomized controlled trial, cluster, cross‐sectional time series Country: USA Objective: Assess the efficacy of mass media interventions to decrease perception of smoking prevalence among young people, increase perceptions of disapproval, increase confidence in ability to refuse cigarettes, decrease positive outcome expectations for smoking, increase negative outcome expectations, and decrease prevalence of self‐reported smoking Study Site: Clustered media campaigns (home) with data collection at school Method of Analysis: General linear mixed models Confounders analyzed: At baseline and completion (grade, gender, race/ethnicity) | |
| Participants | Age: Grades 7 ‐ 12 Gender: Baseline control boys (n = 4765) control girls (n = 5612); intervention boys (n = 4391) intervention girls (n = 5114); Ethnicity: Baseline control African‐American 23.6%; Hispanic/Latino 13.2%; non‐Hispanic white 58.3%; other, unknown 4.9%; intervention African‐American 22.8%; Hispanic/Latino 14.1%; non‐Hispanic white 57.2%; Other, unknown 5.8% | |
| Interventions | Programme name: Not provided Theoretical basis: Social cognitive theory Intervention description: 4 separate media campaigns running simultaneously. 30‐ and 60‐second TV or radio messages were broadcast using purchased time with approximately 3 ‐ 4 exposures a week Approximately 10 messages were chosen for each campaign in 2002. 5 additional messages were developed annually for each campaign in 2003 ‐ 2005 (60 total) Control description: No intervention Duration/study dates: 4 years between 2001 and 2005 Intervention delivery: Media only, (TV, radio, newspapers, billboards and magazines) | |
| Outcomes | Reported outcomes: 30‐day smoking prevalence, 7‐day smoking prevalence; Intentions to smoke; Perceived community smoking prevalence; Peer smoking norms; Confidence in refusing cigarette measures; Negative outcome expectations; positive outcome expectations Follow‐up time period: 4 years | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization mentioned but not described |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment not described |
| Blinding (performance bias and detection bias) | High risk | No allocation concealment occurred |
| Incomplete outcome data (attrition bias) | High risk | No students responded from 1 baseline school at follow‐up |
| Selective reporting (reporting bias) | High risk | Not all analyses were reported, only raw standard deviation estimates presented |
| Other bias | Low risk | No other threats to validity identified |
| Imbalance of outcome measures at baseline | Low risk | No imbalance of outcome measures at baseline evident |
| Comparability of intervention and control group characteristics at baseline | Low risk | Overall distribution by grade, gender and race/ethnicity did not differ between conditions at either survey |
| Protection against contamination | High risk | A large national youth‐focused anti‐tobacco media campaign was initiated in 2000 and was active in all of the intervention and control DMAs at a high level of intensity throughout the intervention The authors note: "The cumulative effects of these changes most likely reduced the magnitude of tobacco control effects that could be achieved by additional media based intervention campaigns" |
| Selective recruitment of participants | Unclear risk | Unable to determine selective recruitment |
| Methods | Design: Controlled clinical trial; cluster; non‐equivalent control group Country: Norway Objective: To evaluate 3 provocative mass media campaigns to prevent adolescents smoking Study site: Homes, communities and cinemas in 2 counties in SE Norway Method of Analysis: Logistic regression (county unit of allocation and individual unit of analysis) Co‐founders analyzed: smoking at baseline and gender | |
| Participants | Age: All students aged 14 ‐ 15 eligible for the study, followed up until aged 17 ‐ 18 Gender: Intervention ‐ girls n = 1457 boys n = 1285; Control ‐ girls n = 1784 boys n = 1654 Ethnicity: South‐eastern part of Norway ‐ same proportion of rural‐urban settlement across groups | |
| Interventions | Programme name: Not provided Theoretical basis: Hypothesis that provocative appeals stimulate discussion, thereby influencing behaviour. Adolescent focus groups identified the key messages used in the campaign Intervention description: 3 different full‐page newspaper advertisements; 1 poster, 1 TV and cinema spot. In each 3‐week period: TV and cinema spots shown 167 times; each of the 3 newspaper advertisements appeared once in each of the 5 newspapers; posters (n = 1140) mailed to all schools, youth organizations and sports clubs Control description: No intervention (not described) Duration/study dates: 3 annual media campaigns of 3 weeks duration, 1992, 1993 and 1994 (the third campaign was launched for 4 weeks) Intervention delivery: Personnel not clear, but media delivery included TV, cinema advertisement, newspaper, posters in schools and youth organizations | |
| Outcomes | Reported outcomes: Smoking behaviour (daily, weekly, occasional and non) number of cigarettes smoked Intentions to smoke Follow‐up time‐period: 1 year post‐3rd campaign (3 years) | |
| Notes | 2 counties matched for size, education level, income, urban‐rural settlement and smoking prevalence and allocated to Intervention and Control Girls targeted for intervention; Intervention messages were aimed to be provocative in order to gain attention, for example: "i.) 'You can't ask girls to decide important matters, they don't even understand the simplest things' ii.) 'The numbers speak for themselves Norwegian boys understand more and more, Norwegian girls less and less' and iii.) 'Teachers should be concentrating on boys. It has been established that girls are not capable of logical thinking'." Hafstad 1997 page 123 of 'Use of provocative emotional appeals in a mass media campaign designed to prevent smoking among adolescents' manuscript | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not randomized |
| Allocation concealment (selection bias) | High risk | Population selected, not randomized |
| Blinding (performance bias and detection bias) | High risk | No mention of blinding, due to nature of intervention, blinding highly unlikely for participants |
| Incomplete outcome data (attrition bias) | High risk | Participant data missing as they did not complete both questionnaires, or some parts of their questionnaires; Non‐responders more likely to be smokers; 5 surveys in intervention county, and only 2 in control county due to financial constraints |
| Selective reporting (reporting bias) | Unclear risk | Study protocol not available, unable to determine selective outcome reporting |
| Other bias | High risk | Generalizability concerns, campaign only targeting girls; validity concerns due to self‐report of smoking behaviour |
| Imbalance of outcome measures at baseline | High risk | Male daily smokers in intervention county higher at baseline than in control |
| Comparability of intervention and control group characteristics at baseline | Unclear risk | Insufficient demographic detail to determine differences at baseline |
| Protection against contamination | Unclear risk | P229C “since local media were used only, the risk of spill‐over of media exposure was minimized.” Minimized but not eradicated |
| Selective recruitment of participants | High risk | Participant cluster site selected by study staff |
| Methods | Design: Randomized controlled trial; cluster; non‐equivalent control group Country: USA Objective: To assess the efficacy of mass media interventions to combat illegal drug use among America's youth by means of an advertising and social marketing programme focusing on the dangers of drug use Study site: High schools and middle‐feeder schools throughout South Dakota Method of analysis: Logistics regression model with baseline covariates for dichotomous data, linear regression used for all other outcomes Confounders analyzed: gender, race/ethnicity (white/non‐white), monthly smoking at baseline, school grades, parental education and monitoring, tobacco use by an important adult, and whether or not the adolescent lives with both biological parents | |
| Participants | Age: between 9 ‐ 18 years, but in 2002 this was narrowed to 11 ‐ 17‐year‐olds Gender: Overall sample population 49.4% girls Ethnicity: Overall sample‐population ‐ Non‐white 11.7% | |
| Interventions | Programme name: Project ALERT (middle‐school) or ALERT Plus (high schools) Theoretical basis: The health belief model (HBM), the self‐efficacy theory of behaviour change, and social influences theory Intervention description 1.) ALERT: School lessons on smoking cessation, designed to appeal to more committed and alienated smokers and to highlight student susceptibility to the negative consequences of use; parent involvement activities; a series of home‐learning activities that encourage parental involvement in substance‐use prevention during 7th and 8th grades, plus exposure to the National Youth Anti‐Drug Media Campaign (NYADMC) with intended degree of campaign exposure of 2.5‐youth orientated ads per week Intervention description 2.) ALERT Plus: Same as for ALERT, with the addition of booster lessons in the 9th and 10th grades which seek to reinforce the middle‐school curriculum while also strengthening norms against high‐risk drug use, enhancing adolescents' capacity to protect themselves against risky drug situations, and helping them develop alternative strategies for coping with stress. Plus exposure to the NYADMC with intended degree of campaign exposure of 2.5‐youth orientated ads per week Control description: Adolescents in the control condition received other prevention curricula already in place at their schools but were not exposed to any part of the ALERT curriculum in any grades Duration/study dates: 6 months for school curriculum; media intervention still running at completion of trial (2 years); intention of 2.5‐youth orientated ads per week. Launched in 1997 continuing through until 2002. Intervention delivery: media: television and other media (not specified), entertainment, and sports industries as well as partnerships with civic, professional, and community groups, teachers through schools and parents | |
| Outcomes | Reported outcomes: ALERT Only ‐ weekly and monthly smoking; Follow‐up time period: 2 years | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear methods of randomization. However, P500A “The full study design randomized 48 clusters. However, assignment of three clusters was restricted to the ALERT or ALERT Plus conditions. Those clusters were not included in this analysis.” |
| Allocation concealment (selection bias) | High risk | No allocation concealment occurred |
| Blinding (performance bias and detection bias) | High risk | Not possible to blind due to the nature of the intervention. There is no mention of blinding attempts for outcome assessors or investigators |
| Incomplete outcome data (attrition bias) | High risk | 3 clusters excluded from analysis due to lack of randomization; adolescents who had missing data were more likely to be smokers or have higher risk factors, even after adjustments; authors were concerned that the imbalance was not eliminated |
| Selective reporting (reporting bias) | Unclear risk | Tobacco data not shown in paper A; protocol not available, unable to determine if any prespecified outcomes are missing; some outcomes not presented stated by authors; 3 clusters excluded from analysis due to lack of randomization |
| Other bias | High risk | Generalizability concerns ‐ more effective with at‐risk girls; outcomes based on self‐report |
| Imbalance of outcome measures at baseline | Low risk | Baseline outcome attrition was equal across groups; adjustments for variance conducted |
| Comparability of intervention and control group characteristics at baseline | Low risk | Participants are reported as being "similar" at baseline |
| Protection against contamination | Unclear risk | Possible contamination due to allocation within media area/community, but not reported in paper |
| Selective recruitment of participants | Unclear risk | Unable to determine selective recruitment. 3 schools were excluded from the analysis due to selection rather than randomization. However, further risk is not clear |
| Methods | Design: Controlled clinical trial, not randomized Country: USA Objective: To evaluate the effectiveness of televised messages to prevent smoking in young adolescents Study site: Rural schools in Vermont county Method of analysis: Repeated measures ANOVA (schools unit of allocation and individuals unit of analysis) Confounders analyzed: Not reported | |
| Participants | Age: 10 ‐ 12‐year‐olds Gender: boys and girls, no further details provided Ethnicity: No details available | |
| Interventions | Programme name: Not stated Theoretical basis: Social learning theory and related behavioural change theories. Diagnostic and formative media research using teenage focus groups Intervention description: Schools in range of a network affiliate TV station. 7 x 30‐second TV smoking prevention messages, placed as paid advertising during after‐school and Saturday morning viewing hours, placed next to the programmes most popular with the target group. TV spots changed in new exposure periods Control description: Adjacent areas out of range of TV signal; No TV messages Duration/study dates: Exposure for 3 x 13‐week periods, no exposure for 2 x 3‐month periods, during an 18‐month period overall. 10 TV spots broadcast weekly; Dates not stated. Intervention delivery: Positive non‐smoking role models, reinforcing positive norms and values by depicting young people who refuse cigarettes and enjoy social benefits in a smoke‐free life style. Image informed by student focus groups; Television broadcasts | |
| Outcomes | Reported outcomes: Recall of media campaign; Perception of friends' approval of smoking; Perception of friends' smoking; Intention to smoke a cigarette if offered by a friend; Smoking behaviour | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Groups selected by investigators |
| Allocation concealment (selection bias) | High risk | Groups selected, not randomized |
| Blinding (performance bias and detection bias) | High risk | Blinding of participants and outcome assessors not mentioned, but due to nature of intervention it is highly unlikely that blinding occurred |
| Incomplete outcome data (attrition bias) | High risk | Attrition not described |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement |
| Other bias | Unclear risk | Insufficient information to permit judgement |
| Imbalance of outcome measures at baseline | Unclear risk | Insufficient information to permit judgement |
| Comparability of intervention and control group characteristics at baseline | High risk | Families in the intervention group had slightly higher education and income levels than the controls |
| Protection against contamination | Unclear risk | Possible contamination, as some students from the control group may have been within range of the TV station's broadcast, or visited people during the intervention period that were within the broadcast range |
| Selective recruitment of participants | Unclear risk | Insufficient information to permit judgement |
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Multicomponent community‐wide smoking prevention intervention, with a mass media component; not young people‐specific, no smoking‐related outcome measures | |
| Describes schools‐based smoking prevention intervention and an information and education campaign which used posters, advertisements in youth media, booklets, buttons, stickers, and free T‐shirts. There were no specific pre‐evaluation measures or post‐evaluation measures, no control group and effects of advertisements in youth media were not independently reported | |
| Besançon smoke‐free project | |
| Iowa Program Against Smoking (IPAS) | |
| "Leave us Clean" prevention campaign in Romagna (Northern Italy), which took place when students were in middle school. However the study population reported on are first contacted in second year high, and as a result there are no baseline data reported | |
| Massachusetts anti‐tobacco media campaign, which included television advertisements produced by public health organizations and by tobacco companies. No control and no baseline data presented | |
| School‐based smoking prevention intervention which used videotaped material for use in individual schools. School‐based smoking prevention programme, not mass media as defined in this review | |
| Smoking cessation campaign targeted at pregnant 15 ‐ 24 year‐olds, mass media used as part of a multicomponent community‐wide intervention. No separate results for mass media component alone | |
| Pawtucket HHP | |
| Minnesota TM (Target Market) campaign ‐ organied around 3 components 1. paid advertising 2. youth organization and 3. website targeted to youth. No control group, no true baseline (evaluation began 2 years into the campaign) | |
| Smoking cessation intervention targeted at black smokers. No smoking‐related results for young people reported | |
| Limited reporting in conference abstract, unlikely to be a randomized controlled trial or controlled clinical trial; appears more as a protocol of what will and is starting to be done rather than a completed study | |
| The American Legacy Foundation's 'Legacy's Truth' campaign. Tobacco countermarketing, examining racial/ethnic differences in association to exposure and subsequently youth's beliefs and attitudes about cigarette companies and their intention to smoke. No control and no baseline data presented | |
| Teenage mass‐media smoking prevention and cessation campaign. No smoking‐related outcomes reported | |
| No baseline data were collected and no control group | |
| National Truth Campaign: 2 arms ‐ 'truth' campaign supplemented with additional advertising compared with comparison markets receiving less than the national average exposure of 'truth' messages. No true control group | |
| Anti‐smoking advertisements in cinemas aimed at young women's perceptions of smoking in movies and their intentions to smoke. Controlled clinical trial, no baseline, control surveyed during week 1 and intervention during week 2 | |
| Multicomponent community‐wide lifestyle intervention: smoking component cessation only | |
| Schools‐based smoking prevention programme using films, videos and poster messages in schools. School‐based, not mass media as defined in this review | |
| Stanford Cardiovascular Disease Prevention Programs: | |
| National 'truth' anti‐smoking campaign: Cohort longitudinal study in 12 ‐ 17‐year‐olds followed up over 3 years. No control group | |
| Previously included study, now excluded due to inadequate comparison between groups. The intervention population was made up of self‐selected schools and the control group contained schools which did not respond to the invitation to participate | |
| Review of mass media campaigns for smoking cessation, prevention excluded: does not report outcomes for young people separately | |
| Chicago Televised Smoking Cessation Programme | |
| Nationwide No Smoking Day evaluated: no separate results for young people | |
| Mass media smoking prevention campaign. No smoking‐related outcomes reported | |
| Paper describes the development of the advertisements, processes of the campaign including media reach but no outcomes related to smoking behaviour | |
| Intervention used interactive computer programmes to provide adolescents with confidential, non‐judgemental health information, behavioural change strategies, sources of referral and social support. Not mass media as defined in this review | |
| Health Education Board for Scotland's anti‐smoking campaign. Countrywide multifaceted smoking cessation intervention. No separate results for young people | |
| No control group, survey of the Horry County media campaign | |
| In‐school anti‐tobacco media campaign in 10 schools, USA. No control | |
| National Youth Anti‐Drug Media Campaign: 3 nationally represented samples of US youth aged 9 ‐ 18 years surveyed at 4 time points; media included television, radio, websites, magazines and movie theatres. No control group | |
| Richmond quits smoking: Multicomponent community‐wide intervention, including use of the mass media; no smoking‐related results given | |
| Advertisements in comics and TV advertising; no smoking‐related outcomes, post‐test measures only | |
| Intervention to increase children’s and parents' awareness and knowledge of substance abuse and prevention. No smoking behaviour or smoking‐related outcomes reported for young people | |
| Primarily a school‐based smoking prevention study using a TV programme. Not mass media as defined in this review | |
| School‐based evaluation of advertisements developed for a mass media campaign; no smoking‐related outcomes reported | |
| Intervention used mass media as part of a multicomponent community‐wide smoking prevention programme for black adolescents, no independent smoking‐related outcomes for mass media component alone | |
| Quit and Win Minnesota: | |
| Evaluation of the "smoke‐free" youth campaign from the Federal Center for Health Education which included mass media (television/cinema spots, advertisement), internet, and face‐to‐face communication, with a focus on school. No comparison control group or multiple time series analysis | |
| Progama Latino para Dejar de Fumar: | |
| Knights Against Tobacco: Students at a high school in Detroit USA received a grant for a multi‐media campaign including anti‐tobacco commercials and posters. No control group, study only conducted in 1 school | |
| Description of a planned national youth anti‐drug media campaign; no evaluation | |
| Multicomponent, including mass media, smoking cessation intervention aimed at Vietnamese men over 18 years of age. No separate results relating to smoking behaviour given for young people | |
| Multicomponent community‐wide intervention, including use of the mass media; no separate results given for young people | |
| Multicomponent community‐wide smoking cessation intervention. No separate results for young people | |
| Minnesota‐Wisconsin Adolescent Tobacco Use Research Project: Multicomponent statewide intervention, including a mass media component; no independent smoking‐related outcome measures for the mass media component alone | |
| Hearbeat Wales: Multicomponent intervention including mass media; no outcomes related to smoking behaviour, no results for mass media component alone | |
| Coeur en sante St‐Henri, Montreal, Canada: Mass media component included in a multicomponent community‐wide intervention; no smoking‐related outcome measures, no results for mass media component alone | |
| A policy mix comprising various structural and behavioural prevention messages in Germany, which included a smoke‐free youth campaign 'rauchfrei'. No comparison control group | |
| Multicomponent countrywide smoking prevention and cessation intervention. No smoking‐related outcome reported | |
| Midwestern Prevention Project (selected papers referenced): | |
| Description of the development of the campaign; no evaluation | |
| Minnesota Heart Health Programme (selected papers referenced): | |
| Quit and Win Australia: Community‐wide multicomponent smoking cessation programme, including use of the mass media; evaluated using before‐and‐after surveys of smoking prevalence, no separate results for young people | |
| Multicomponent smoking cessation campaign, including use of the mass media, encouraging smokers to quit. No separate results for young people | |
| California Tobacco Education Media Campaign | |
| A su salud: | |
| Mirame! [Look at me !]: Multicomponent community‐wide smoking prevention programme; description of intervention, no results reported | |
| Examination of perceived impact of anti‐drug advertising on aspects of youth drug use, no smoking‐related outcomes given | |
| Youth anti‐tobacco campaign. No smoking‐related outcomes | |
| Coronary Risk Factor Study (CORIS): Multicomponent intervention with a mass media component to reduce coronary heart disease in white South African adults living in South‐Western Cape Province; no independent smoking‐related outcome measures reported for the mass media component alone | |
| Mass media campaign aimed at youth aged 12 ‐ 18 to prevent smoking and increase awareness of dangers whilst using positive messages. No control | |
| Randomized controlled trial of in‐school and media‐based efforts aimed at reducing marijuana and alcohol uptake in younger adolescents, eight intervention and eight control schools. Media smoking prevention component small and dependent on person‐to‐person contact | |
| Florida 'truth' anti‐tobacco media evaluation, 4 data collection time points for intervention group and 2 for control. No smoking‐related outcomes reported for control population | |
| Paper investigates involvement of school‐based drug abuse prevention programme on viewing and evaluation of current anti‐drug‐abuse TV programme. No smoking‐related outcomes for young people given | |
| Mass media smoking cessation intervention targeted at smokers; no separate results for young people | |
| Mass‐media anti‐smoking campaign in Israel, randomly targeting adolescents aged 12 ‐ 18 years. No baseline data and no control | |
| Quit and Win Sweden: Multicomponent nationwide anti‐tobacco use intervention aimed at adult cigarette and oral snuff users; mass media used to encourage tobacco users to participate, no separate results for young people | |
| Florida's Truth Campaign: 7 waves of data collection from 2000 to 2004. No control group | |
| Mass media smoking cessation intervention: no separate results for young people | |
| Smokebusters: Mass media used to advertise multicomponent smoking prevention intervention aimed at young people, no smoking‐related outcomes given for mass media component alone | |
| North Karelia Youth Project: | |
| No‐Smoking Class: | |
| Multicomponent community‐wide intervention including use of the mass media; no separate results for young people | |
| Mass media smoking cessation campaign; no separate results for young people, no control group | |
| Community‐wide smoking cessation campaign using self‐help manual. No control group | |
| Stanford 5‐City Project: | |
| Mass media (youth magazines) used to promote anti‐smoking message. No smoking‐related outcomes given | |
| Multicomponent community‐wide anti‐smoking intervention targeted at 11 ‐ 13‐year‐olds, local newspapers and radio provided widespread coverage of the programme; no independent outcome measures for the mass media component |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||||||||||||||||||||||
| 1 Smoking outcomes Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||||||
| Analysis 1.1
Comparison 1 Primary outcomes for Mass media smoking prevention programmes, Outcome 1 Smoking outcomes. | ||||||||||||||||||||||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||||||||||
| 1 Smoking attitudes Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||
| Analysis 2.1
Comparison 2 Intermediate outcomes for Mass media smoking prevention programmes, Outcome 1 Smoking attitudes. | ||||||||||||||||||||||||||||||||
| 2 Smoking intentions Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||
| Analysis 2.2
Comparison 2 Intermediate outcomes for Mass media smoking prevention programmes, Outcome 2 Smoking intentions. | ||||||||||||||||||||||||||||||||
| 3 Smoking knowledge Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||
| Analysis 2.3
Comparison 2 Intermediate outcomes for Mass media smoking prevention programmes, Outcome 3 Smoking knowledge. | ||||||||||||||||||||||||||||||||
| 4 Self‐esteem/self‐efficacy Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||
| Analysis 2.4
Comparison 2 Intermediate outcomes for Mass media smoking prevention programmes, Outcome 4 Self‐esteem/self‐efficacy. | ||||||||||||||||||||||||||||||||
| 5 Smoking perceptions Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||
| Analysis 2.5
Comparison 2 Intermediate outcomes for Mass media smoking prevention programmes, Outcome 5 Smoking perceptions. | ||||||||||||||||||||||||||||||||
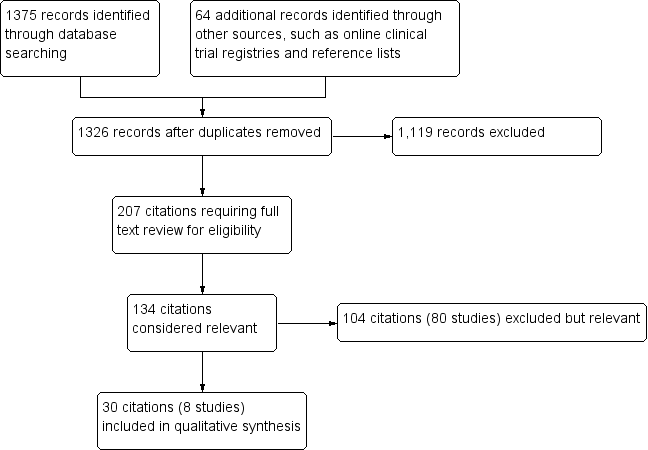
Study flow diagram.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
| Study | Sample size at follow‐up | Outcomes analyzed | Results |
| Bauman 1991 | Clusters n = 2 (SMSAs) Individuals n = 1637 | Weekly and ever‐smoking | Overall outcome ‐ No evidence of an effect Means of all smoking variables changed significantly in the direction of more smoking. No P values are significant (authors state that F > 1.00 in all instances). Data consistent with the conclusion that the campaign did not influence smoking. |
| Fallin 2015 | Clusters n = 33 (nightclubs/bars) Individuals n = 3348 | Daily and non‐daily smoking | Overall outcome ‐ No evidence of an effect Smoking rates did not change across the 3 time periods (P = 0.17), but partiers who recalled the HAVOC intervention had lower daily smoking (OR 0.30, 95% CI 0.10 to 0.95; P < 0.05), compared to those who did not recall the intervention |
| Flay 1995 | Clusters n = 47 (schools) Individuals n = 4134 | Smoker (No quantity) | Overall outcome ‐ No evidence of an effect There were no consistent programme effects on smoking outcomes, suggesting that the treatment was no more or less effective for different groups |
| Flynn 1995 | Clusters n = 2 (communities) Individuals n = 2860 | Daily, weekly and smokeless tobacco | Overall outcome ‐ Favours intervention Significant difference in the school‐and‐media group only within the final 2 years, a consistent trend toward less smoking was noted prior to this. In the 5th year the relative differences for daily smoking was 34% and for weekly smoking 35% between school‐and‐media and school‐only groups. For smokeless tobacco behaviour the 2 groups did not differ significantly, except in the 4th year when the school‐only group was more likely to report use. |
| Flynn 2010 | Clusters n = 98 (schools) Individuals n = 23,246 | Weekly and monthly | Overall outcome ‐ No evidence of an effect The 30‐day smoking rates appeared to decline over the 4‐year interval between baseline and follow‐up surveys for participants in both conditions, but this trend was not significant. Similar results were obtained for 7‐day prevalence. |
| Hafstad 1997 | Clusters n = 2 (counties) Individuals n = 6234 | Daily, weekly, monthly, non‐smoker and smoker (No quantity) | Overall outcome ‐ Favours intervention Among non‐smokers, a significantly lower proportion of adolescents of both genders had started to smoke in the intervention county compared to the proportion in the control county. Among those who were smokers at baseline, significantly more girls in the intervention county had stopped than in the control county, while no significant differences were detected among boys. |
| Longshore 2006 | Clusters n = 100 (schools) Individuals: ALERT n = 4276 ALERT Plus n = 4015 | Weekly and monthly | Overall outcome ‐ Favours intervention ALERT Plus held down current (past month) and regular (weekly) smoking producing a 23% reduction in both measures of use, P < 0.01. Project ALERT curbed current use among the high‐risk experimenters and the even higher‐risk baseline smokers (users) by approximately 20% (P < 0.03), and cut regular (weekly) cigarette use across all 3 groups by anywhere from 19% (P < 0.06) to 39% (P < 0.02). |
| Worden 1983 | Clusters n = 93 (schools) Individuals n = 4005 | Weekly | Overall outcome ‐ No evidence of an effect There were no significant differences in smoking between intervention and control groups. A trend (non‐significant) favouring the intervention group toward a lower level of smoking was noted. P values were not provided. |
Comparison 1 Primary outcomes for Mass media smoking prevention programmes, Outcome 1 Smoking outcomes.
| Study | Sample size at follow‐up | Outcomes analyzed | Results |
| Bauman 1991 | Clusters n = 2 (SMSAs) Individuals n = 1637 | Attitudes toward smoking (total), perceived peer attitudes | Overall outcome ‐ No evidence of an effect No statistically significant post‐campaign differences in attitudes, suggesting that the peer‐involvement component did not impact on those characteristics. |
| Flay 1995 | Clusters n = 47 (schools) Individuals n = 4134 | Disadvantages/negatives (toward parental smoking) | Overall outcome ‐ Favours intervention Marginally significant overall effect (P < 0.06), but there was a significant interaction between television and social resistance conditions at immediate post‐test, (P < 0.03). In San Diego there was more positive change in the social resistance condition, (P < 0.003) toward disapproval of parental smoking (Intervention description 4 in Characteristics of included studies table). |
| Flynn 1995 | Clusters n = 2 (communities) Individuals n = 2860 | Attitude toward smoking (total), advantages/positives, disadvantages/negatives | Overall outcome ‐ Favours intervention A significant difference in change over time was found between girls in the 2 treatment groups with scores increasing less among girls in the media‐school communities, for positive attitudes toward smoking (P < 0.02). |
| Flynn 2010 | Clusters n = 98 (schools) Individuals n = 23,246 | Advantages/positives, disadvantages/negatives | Overall outcome ‐ Favours control Positive outcome expectation scores increased significantly over time in both study groups, an unfavourable change. Negative outcome expectation scores may have decreased in the comparison but not in the intervention group, although this difference was not significant. |
| Longshore 2006 | Clusters n = 100 (schools) Individuals ALERT n = 4276 ALERT Plus n = 4015 | Advantages/positives, disadvantages/negatives, perceived peer attitudes | Overall outcome ‐ No evidence of an effect Neither boys nor girls exhibited significant differences for tobacco cognitions. |
Comparison 2 Intermediate outcomes for Mass media smoking prevention programmes, Outcome 1 Smoking attitudes.
| Study | Sample size at follow‐up | Outcomes analyzed | Results |
| Flay 1995 | Clusters n = 47 (schools) Individuals n = 4134 | Intentions to smoke | Overall outcome ‐ No evidence of an effect There were no significant condition‐related differences at any wave in Los Angeles or San Diego. No consistent programme effects on behaviours |
| Flynn 1995 | Clusters n = 2 (communities) Individuals n = 2860 | Intentions to smoke | Overall outcomes ‐ Favours intervention A significant difference in change over time was found between girls in the 2 treatment groups, with a lower increase among girls in the media‐school communities in intentions to smoke cigarettes (P < 0.01). |
| Flynn 2010 | Clusters n = 98 (schools) Individuals n = 23,246 | Intentions to smoke | Overall outcome ‐ No evidence of an effect Intentions to smoke appeared to decline over the 4‐year interval between baseline and follow‐up surveys for participants in both conditions, but this trend was not significant. |
| Hafstad 1997 | Clusters n = 2 (counties) Individuals n = 6234 | Intentions to smoke | Overall outcomes ‐ Favours intervention A significant difference between the intervention and the control counties was detected regarding expectation of future smoking habits measured in 1995. In the intervention county, 9% expected to be smokers in 3 years, with 13% in the control county (P < 0.01). No significant gender difference was revealed. |
Comparison 2 Intermediate outcomes for Mass media smoking prevention programmes, Outcome 2 Smoking intentions.
| Study | Sample size at follow‐up | Outcomes analyzed | Results |
| Flay 1995 | Clusters n = 47 (schools) Individuals n = 4134 | Tobacco and health knowledge (overall) | Overall outcome ‐ Favours control Tobacco and health knowledge was significantly higher in the attention control group than in any of the other conditions in Los Angeles at the immediate post‐test (P < 0.001), 1‐year follow‐up (P < 0.001) and 2‐year follow‐up (P < 0.001). However, both smokers and non‐smokers in the attention control condition learned more than students in any of the other conditions. Unexpectedly, tobacco and health knowledge also increased in the social resistances programme in San Diego at the immediate post‐test (P < 0.001). However, this effect was not statistically significant at the 1‐ and 2‐year follow‐ups. There were significant differences in the social influences and resistance skills knowledge scale between conditions in Los Angeles at the immediate post‐test (P < 0.001), 1‐year follow‐up (P < 0.001) and 2‐year follow‐up (P < 0.001). The combined television and social resistance condition did not improve as much, relative to the control conditions, as the social resistance condition. |
Comparison 2 Intermediate outcomes for Mass media smoking prevention programmes, Outcome 3 Smoking knowledge.
| Study | Sample size at follow‐up | Outcomes analyzed | Results |
| Flay 1995 | Clusters n = 47 (schools) Individuals n = 4134 (whole sample) n = 2245 for control sample only | Self‐efficacy | Overall outcome ‐ No evidence of an effect Refusal self‐efficacy did not differ significantly between groups for the primary population comparison. In Los Angeles, there were no significant condition‐related effects at any of the waves. In San Diego, refusal/self‐efficacy was unexpectedly improved in the control condition, relative to the social resistance condition, at the immediate post‐test, (P < 0.004). |
| Longshore 2006 | Clusters n=100 (schools) Individuals ALERT n=4276 ALERT Plus n=4015 | Self‐efficacy | Overall outcome ‐ No evidence of an effect Neither group exhibited significant differences for tobacco cognitions. |
Comparison 2 Intermediate outcomes for Mass media smoking prevention programmes, Outcome 4 Self‐esteem/self‐efficacy.
| Study | Sample size at follow‐up | Outcomes analyzed | Results |
| Flay 1995 | Clusters n = 47 (schools) Individuals n = 4134 | Perceived adult smoking, perceived peer smoking | Overall outcome ‐ Favours intervention There were significantly lower prevalence estimates, (peer) for the social resistance, (P < 0.001) and television (P < 0.006) conditions, and at 2 years the main effect of the social resistance conditions remained. However, the presence of a significant interaction between the television and social resistance conditions (P < 0.05) indicated that the lower prevalence estimates of the social resistance condition was increased in the television plus social resistance condition. |
| Flynn 1995 | Clusters n = 2 (communities) Individuals n = 2860 | Perceived norms, perceived adult smoking, perceived peer smoking, perceived sibling smoking. | Overall outcome ‐ Favours intervention A significant difference in change over time was found between girls in the 2 treatment groups with scores increasing less among girls in the media‐school communities, for perceived peer smoking (P < 0.01). This difference was likely due to the slightly older age and greater representation of boys in the school‐only group. A significant difference was evident at grades 5 to 7, that persisted at grades 8 to 10, for perceived norms (P < 0.01). |
| Flynn 2010 | Clusters n = 98 (schools) Individuals n = 23,246 | Perceived norms, perceived peer smoking | Overall outcome ‐ No evidence of an effect Significant favourable changes in both study groups for perceived prevalence and peer norms, but there were no between‐group differences |
| Longshore 2006 | Clusters n = 100 (schools) Individuals ALERT n = 4276 ALERT Plus n = 4015 | Perceived norms | Overall outcome ‐ No evidence of an effect Neither group exhibited significant differences for tobacco cognitions. |
Comparison 2 Intermediate outcomes for Mass media smoking prevention programmes, Outcome 5 Smoking perceptions.
| Mass media interventions for preventing smoking in young people | ||||
| Patient or population: Young people aged less than 25 years Settings: Schools, community groups, television, radio, newspapers, billboards, posters, leaflets or booklets Intervention: Mass media channels of communication intended to reach large numbers of people and which are not dependent on person‐to‐person contact Comparison: Usual care, minimal education, no intervention or co‐interventions | ||||
| Outcomes | Impact | No of Participants | Quality of the evidence | Comments |
| Smoking rates (follow‐up 18 months to 6 years) | 3 (n = 17,385), 1 which compared a mass media intervention to no intervention and 2 which evaluated mass media interventions as adjuncts to school‐based interventions, found that the mass media interventions reduced the smoking behaviour of young people. The remaining 5 studies (n = 72,740) did not detect a significant effect on smoking behaviour. These included 3 studies comparing a mass media intervention with no intervention, 1 study evaluating a mass media intervention as an adjunct to a school‐based intervention, and 1 interrupted time‐series study of a social media intervention. | 90,125 (8 studies) | ⊕⊝⊝⊝ | The 3 campaigns for which a significant effect was detected described a theoretical basis, used formative research in designing the campaign messages, and used message broadcast of reasonable intensity over extensive periods of time. However, some of the campaigns which did not detect an effect also exhibited these characteristics. |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||
| GRADE Working Group grades of evidence | ||||
| 1Downgraded two levels due to serious risk of bias: all included studies were rated high risk of bias in at least four domains. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking outcomes Show forest plot | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Smoking attitudes Show forest plot | Other data | No numeric data | ||
| 2 Smoking intentions Show forest plot | Other data | No numeric data | ||
| 3 Smoking knowledge Show forest plot | Other data | No numeric data | ||
| 4 Self‐esteem/self‐efficacy Show forest plot | Other data | No numeric data | ||
| 5 Smoking perceptions Show forest plot | Other data | No numeric data | ||

