Antibióticos profilácticos para la inhibición del trabajo de parto prematuro con membranas intactas
Información
- DOI:
- https://doi.org/10.1002/14651858.CD000246.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 05 diciembre 2013see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Embarazo y parto
- Copyright:
-
- Copyright © 2013 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Vicki Flenady compiled the review in consultation with co‐authors. Glenda Halwey worked with Vicki Flenady to assess studies for inclusion and extract data. Owen Stock extracted information on the new studies for this update, assisted in interpretation of the results and editing the review. Nadia Badawi assisted with interpretation of the results. Sara Kenyon provided information on study characteristics of the ORACLE trial and follow‐up study, assisted in interpretation of the findings and editing the review. All authors commented on drafts of the review and approved the final version before submission.
Sources of support
Internal sources
-
Department of Perinatal Medicine, Royal Women's Hospital, Melbourne, Victoria, Australia.
-
Mater Medical Research Institute, Sth Brisbane, Queensland, Australia.
External sources
-
Commonwealth Department of Health and Ageing, Canberra, Australian Capital Territory, Australia.
Declarations of interest
Sara Kenyon led the ORACLE trial and was the CI for the ORACLE Children's Study.
Acknowledgements
We would like to thank Staffan Bergstrom, Susan Cox, Janice French, John Morrison, Karin Norman, Roberto Romero, Jens Svare and Elizabeth Thom and Heather Watts for assistance in providing unpublished data from their clinical trials and for clarifications of other queries.
We would like to acknowledge Linda Murray who assisted with reference management, correspondence and editing in the previous version of the review. We thank James King for his guidance in leading the previous version of this review and Philippa Middleton for advice.
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team) and the Group's Statistical Adviser.
The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Pregnancy and Childbirth Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2013 Dec 05 | Prophylactic antibiotics for inhibiting preterm labour with intact membranes | Review | Vicki Flenady, Glenda Hawley, Owen M Stock, Sara Kenyon, Nadia Badawi | |
| 2002 Oct 21 | Prophylactic antibiotics for inhibiting preterm labour with intact membranes | Review | James F King, Vicki Flenady, Linda Murray | |
Differences between protocol and review
In this update October 2013, primary and secondary outcomes have been defined. Additional outcomes measures are included as primary outcomes. These are: serious maternal adverse outcome related to antibiotic treatment (respiratory arrest, cardiac arrest, death) and a composite measure of death (fetal, neonatal, or later death up to the time of follow‐up) or major long‐term infant neurosensory impairment. Further, the list of outcomes measures included in subgroup analyses are now restricted to those which are considered to be most clinically important. Two additional comparisons were included: Any macrolide antibiotics versus No macrolide antibiotics; and Any beta‐lactam antibiotics versus No beta‐lactam antibiotics. We also removed the exclusion criterion according to attrition rates.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Anti-Bacterial Agents [adverse effects, therapeutic use];
- Antibiotic Prophylaxis [adverse effects, *methods];
- beta-Lactams [adverse effects, therapeutic use];
- Macrolides [adverse effects, therapeutic use];
- Obstetric Labor, Premature [*prevention & control];
- Perinatal Mortality;
- Pregnancy Complications, Infectious [drug therapy];
- Randomized Controlled Trials as Topic;
Medical Subject Headings Check Words
Female; Humans; Pregnancy;
PICO

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
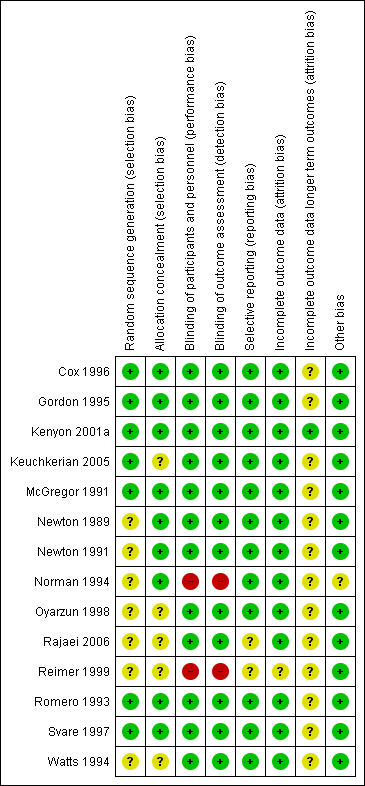
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
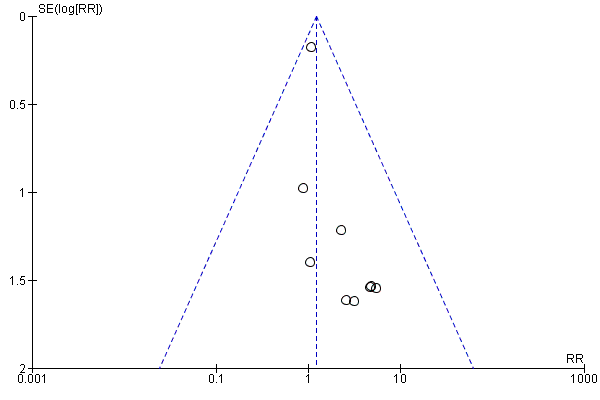
Funnel plot of comparison: 1 Any antibiotics versus no antibiotics, outcome: 1.1 Perinatal mortality.
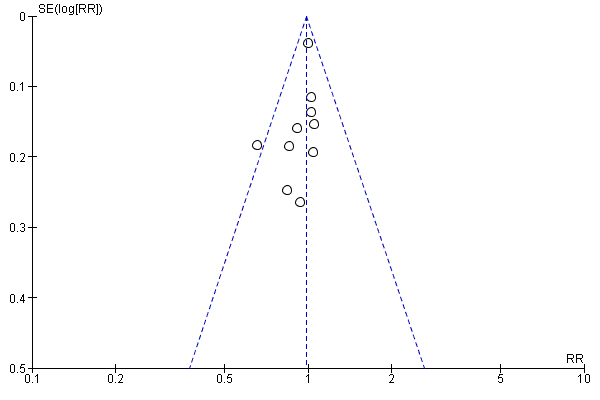
Funnel plot of comparison: 1 Any antibiotics versus no antibiotics, outcome: 1.12 Preterm birth (< 36 or < 37 weeks).
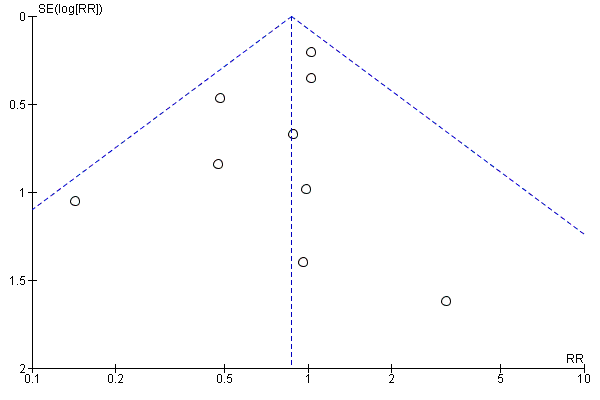
Funnel plot of comparison: 1 Any antibiotics versus no antibiotics, outcome: 1.20 Neonatal sepsis.

Funnel plot of comparison: 1 Any antibiotics versus no antibiotics, outcome: 1.9 Maternal infection.

Comparison 1 Any antibiotics versus no antibiotics, Outcome 1 Perinatal mortality.
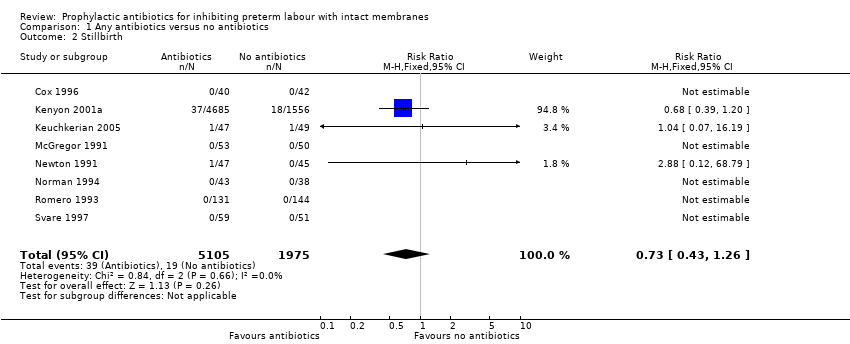
Comparison 1 Any antibiotics versus no antibiotics, Outcome 2 Stillbirth.
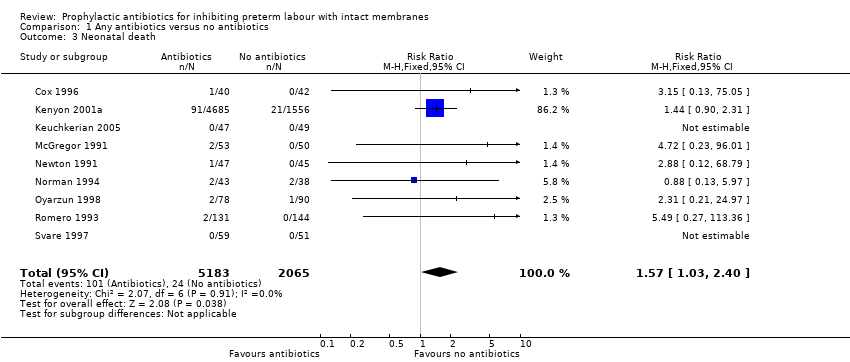
Comparison 1 Any antibiotics versus no antibiotics, Outcome 3 Neonatal death.
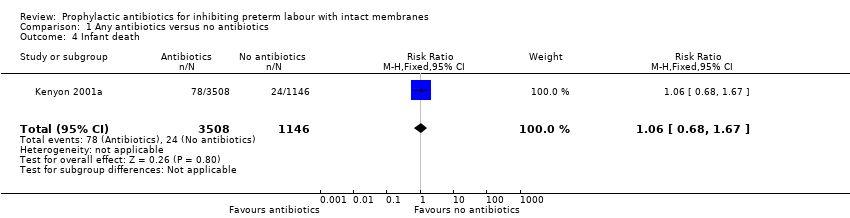
Comparison 1 Any antibiotics versus no antibiotics, Outcome 4 Infant death.

Comparison 1 Any antibiotics versus no antibiotics, Outcome 5 Any functional impairment at 7 years of age..
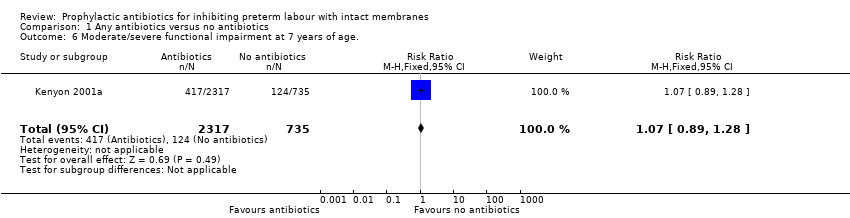
Comparison 1 Any antibiotics versus no antibiotics, Outcome 6 Moderate/severe functional impairment at 7 years of age..

Comparison 1 Any antibiotics versus no antibiotics, Outcome 7 Cerebral palsy at 7 years.
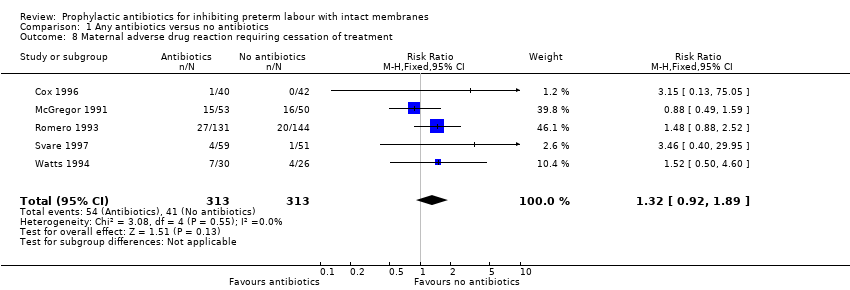
Comparison 1 Any antibiotics versus no antibiotics, Outcome 8 Maternal adverse drug reaction requiring cessation of treatment.

Comparison 1 Any antibiotics versus no antibiotics, Outcome 9 Maternal infection.

Comparison 1 Any antibiotics versus no antibiotics, Outcome 10 Delay in birth (subgrouped by interval).
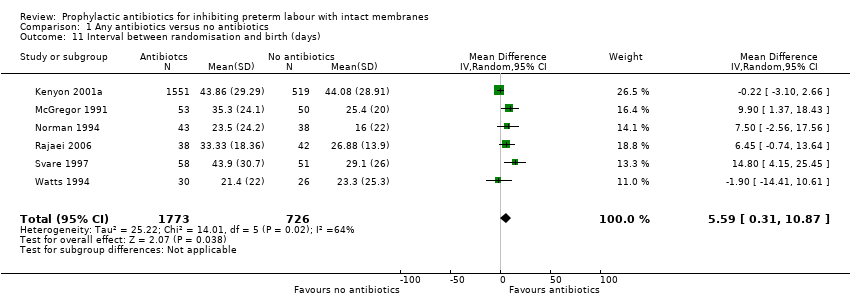
Comparison 1 Any antibiotics versus no antibiotics, Outcome 11 Interval between randomisation and birth (days).

Comparison 1 Any antibiotics versus no antibiotics, Outcome 12 Preterm birth (< 36 or < 37 weeks).
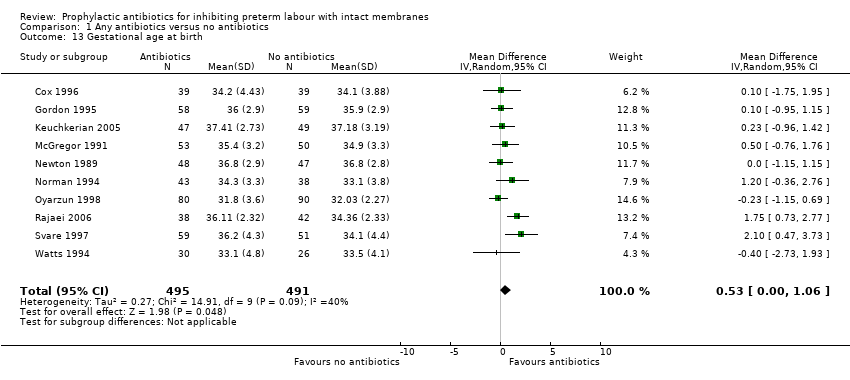
Comparison 1 Any antibiotics versus no antibiotics, Outcome 13 Gestational age at birth.

Comparison 1 Any antibiotics versus no antibiotics, Outcome 14 Birthweight.

Comparison 1 Any antibiotics versus no antibiotics, Outcome 15 Birthweight < 2500 g.
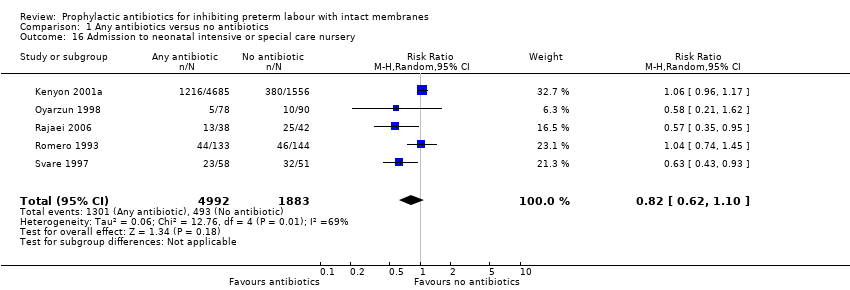
Comparison 1 Any antibiotics versus no antibiotics, Outcome 16 Admission to neonatal intensive or special care nursery.
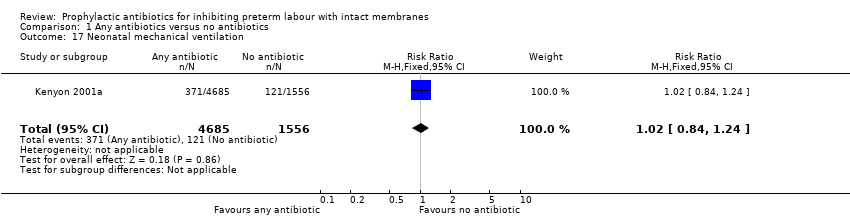
Comparison 1 Any antibiotics versus no antibiotics, Outcome 17 Neonatal mechanical ventilation.

Comparison 1 Any antibiotics versus no antibiotics, Outcome 18 Respiratory distress syndrome.
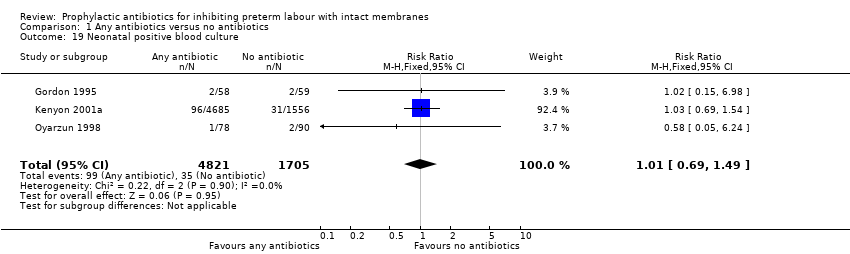
Comparison 1 Any antibiotics versus no antibiotics, Outcome 19 Neonatal positive blood culture.

Comparison 1 Any antibiotics versus no antibiotics, Outcome 20 Neonatal sepsis.
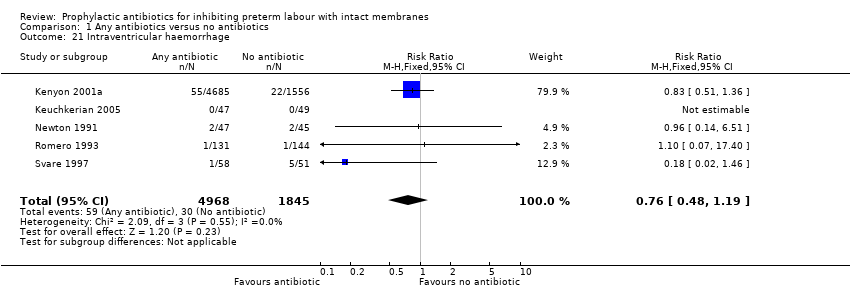
Comparison 1 Any antibiotics versus no antibiotics, Outcome 21 Intraventricular haemorrhage.
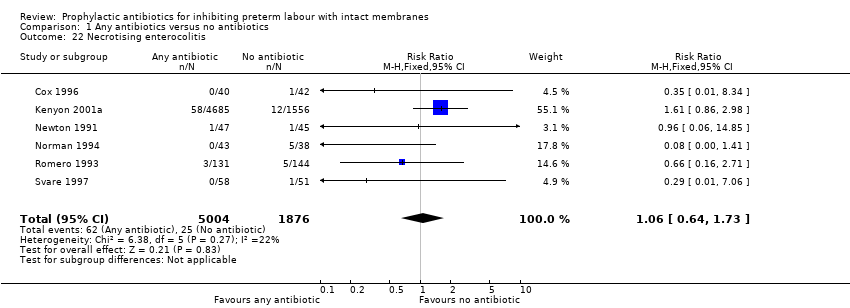
Comparison 1 Any antibiotics versus no antibiotics, Outcome 22 Necrotising enterocolitis.

Comparison 1 Any antibiotics versus no antibiotics, Outcome 23 Major cerebral abnormality.

Comparison 1 Any antibiotics versus no antibiotics, Outcome 24 Chronic neonatal lung disease.

Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 1 Perinatal mortality.
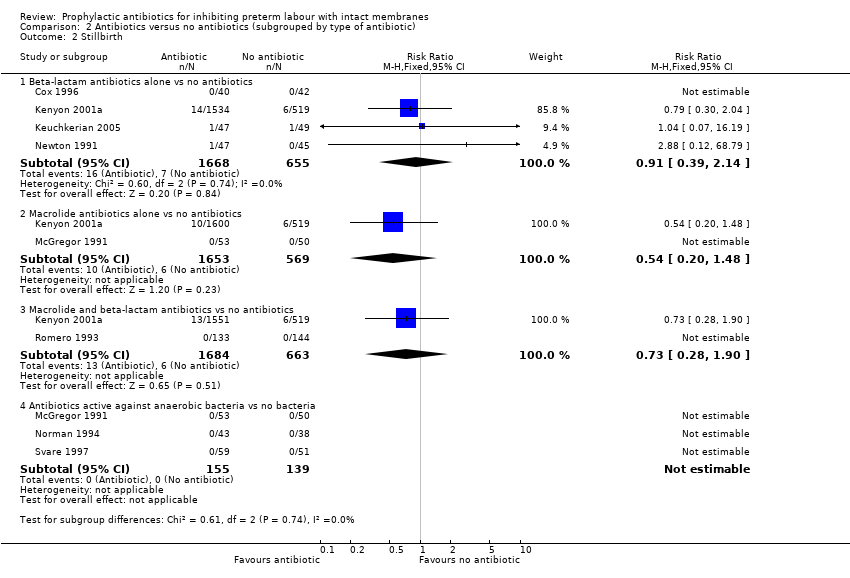
Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 2 Stillbirth.

Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 3 Neonatal death.
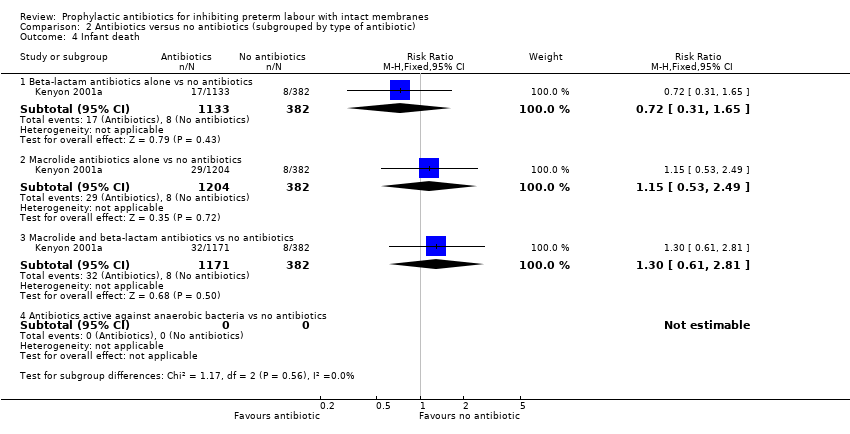
Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 4 Infant death.

Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 5 Any functional impairment at 7 years of age..
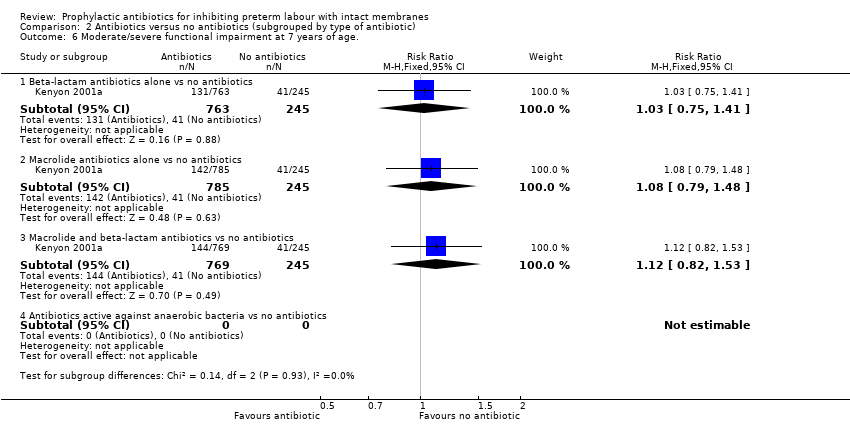
Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 6 Moderate/severe functional impairment at 7 years of age..

Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 7 Cerebral palsy at 7 years of age.

Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 8 Maternal adverse drug reaction requiring cessation of treatment.

Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 9 Maternal infection.

Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 10 Birth within 48 hours of randomisation.

Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 11 Interval between randomisation and birth (days).
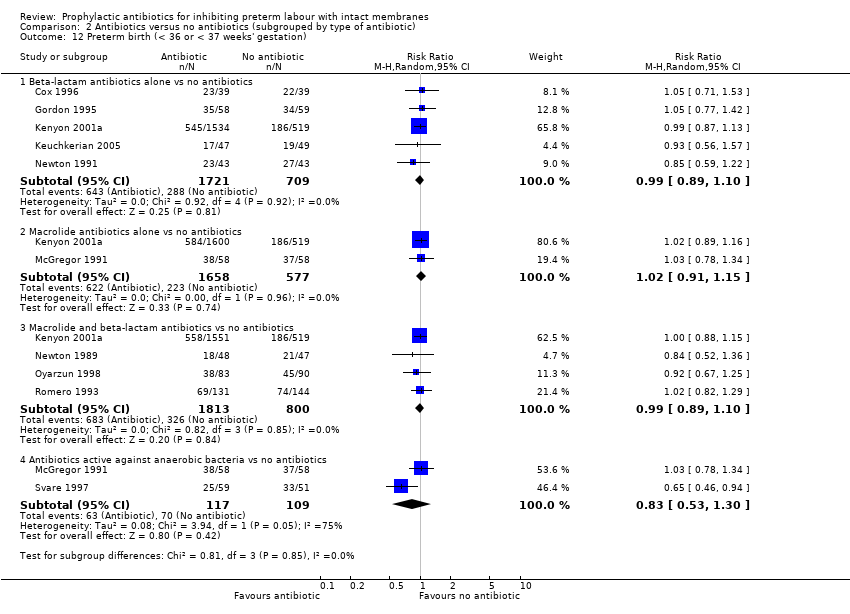
Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 12 Preterm birth (< 36 or < 37 weeks' gestation).

Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 13 Respiratory distress syndrome.
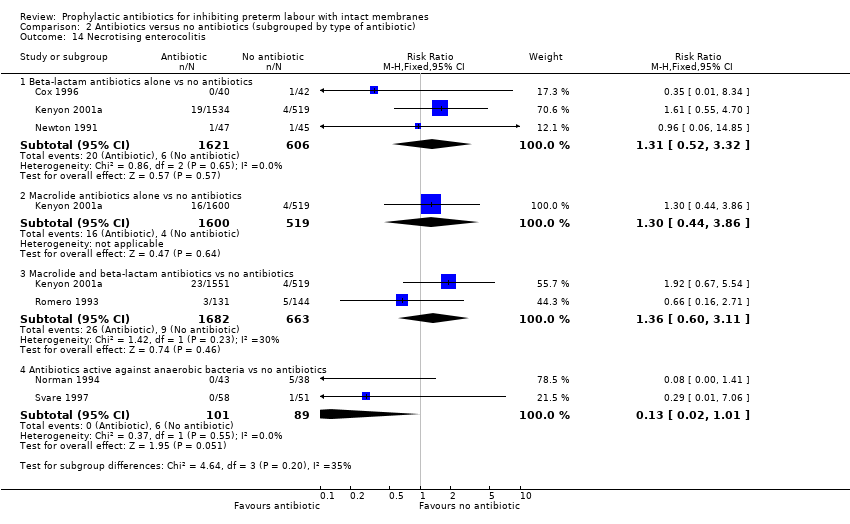
Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 14 Necrotising enterocolitis.

Comparison 2 Antibiotics versus no antibiotics (subgrouped by type of antibiotic), Outcome 15 Intraventricular haemorrhage.

Comparison 3 Any macrolide versus no macrolide, Outcome 1 Perinatal mortality.

Comparison 3 Any macrolide versus no macrolide, Outcome 2 Stillbirth.
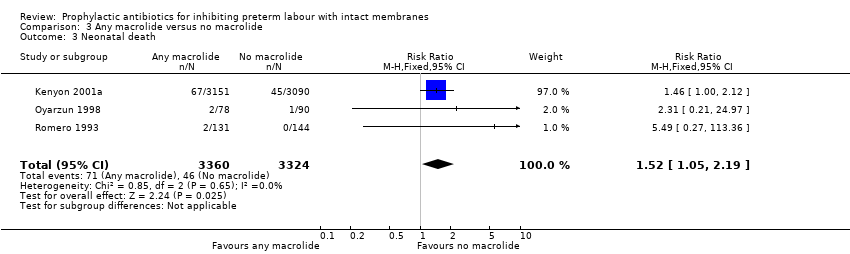
Comparison 3 Any macrolide versus no macrolide, Outcome 3 Neonatal death.
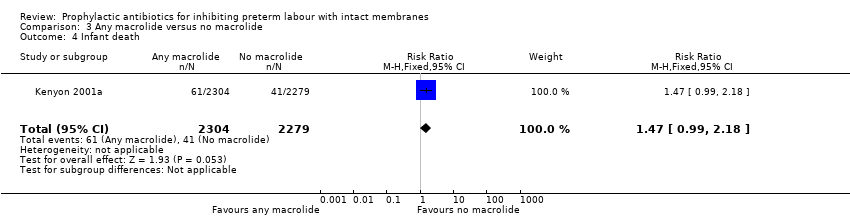
Comparison 3 Any macrolide versus no macrolide, Outcome 4 Infant death.
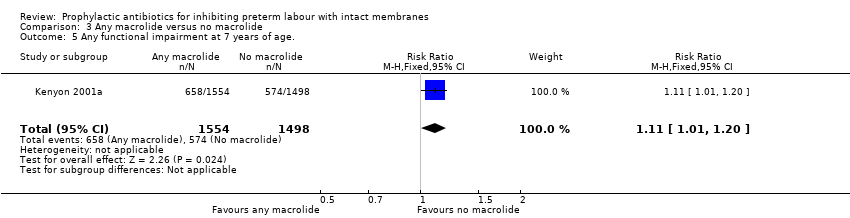
Comparison 3 Any macrolide versus no macrolide, Outcome 5 Any functional impairment at 7 years of age..

Comparison 3 Any macrolide versus no macrolide, Outcome 6 Moderate/severe functional impairment at 7 years of age..
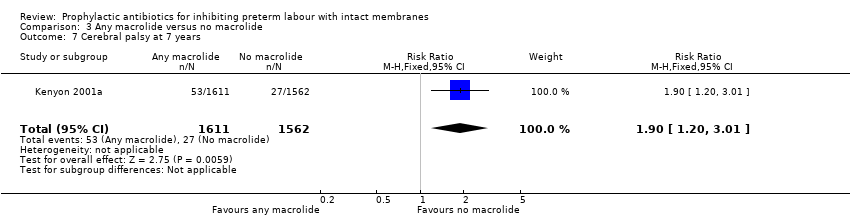
Comparison 3 Any macrolide versus no macrolide, Outcome 7 Cerebral palsy at 7 years.

Comparison 3 Any macrolide versus no macrolide, Outcome 8 Maternal adverse drug reaction requiring cessation of treatment.

Comparison 3 Any macrolide versus no macrolide, Outcome 9 Maternal infection.

Comparison 3 Any macrolide versus no macrolide, Outcome 10 Birth within 48 hours of randomisation.

Comparison 3 Any macrolide versus no macrolide, Outcome 11 Interval between randomisation and birth (days).

Comparison 3 Any macrolide versus no macrolide, Outcome 12 Preterm birth (< 36 or < 37 weeks).
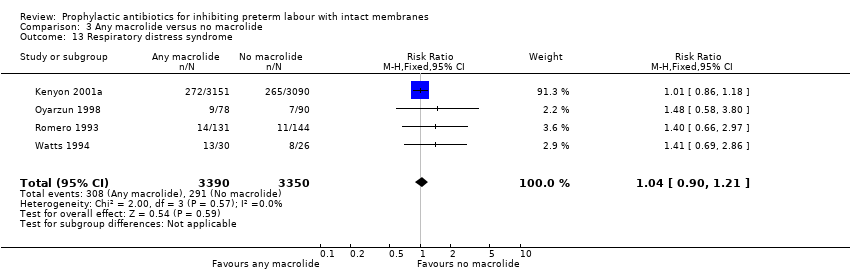
Comparison 3 Any macrolide versus no macrolide, Outcome 13 Respiratory distress syndrome.
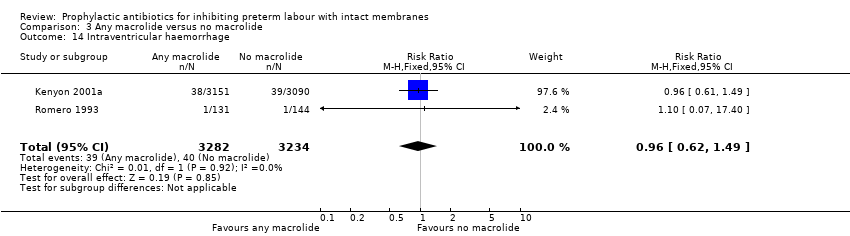
Comparison 3 Any macrolide versus no macrolide, Outcome 14 Intraventricular haemorrhage.
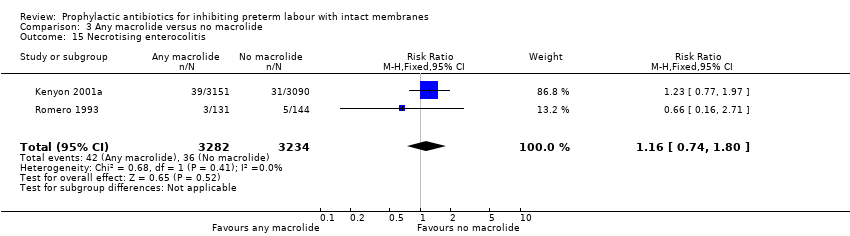
Comparison 3 Any macrolide versus no macrolide, Outcome 15 Necrotising enterocolitis.
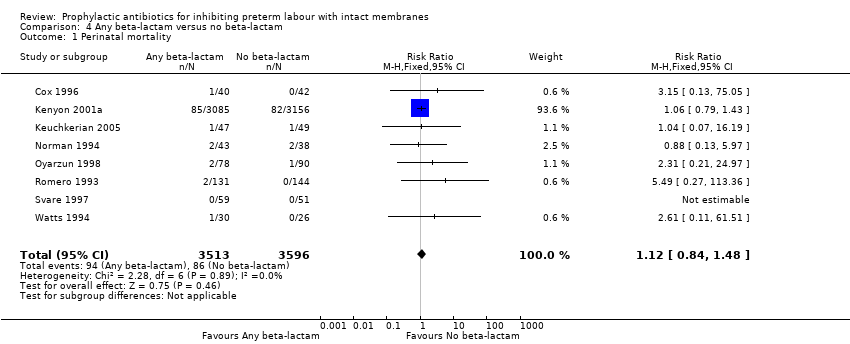
Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 1 Perinatal mortality.

Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 2 Stillbirth.

Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 3 Neonatal death.

Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 4 Infant death.
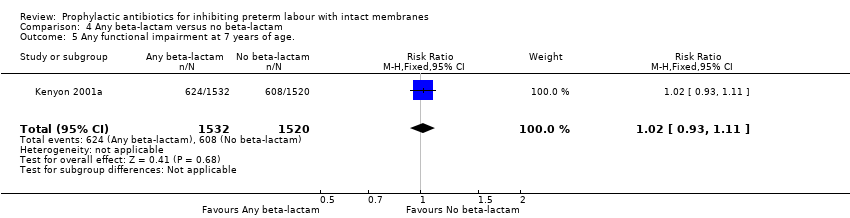
Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 5 Any functional impairment at 7 years of age..
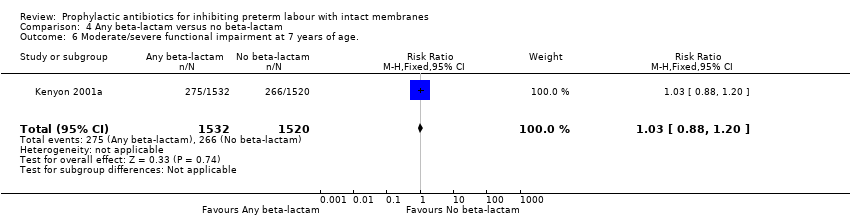
Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 6 Moderate/severe functional impairment at 7 years of age..

Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 7 Cerebral palsy at 7 years.

Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 8 Maternal adverse drug reaction requiring cessation of treatment.

Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 9 Maternal infection.
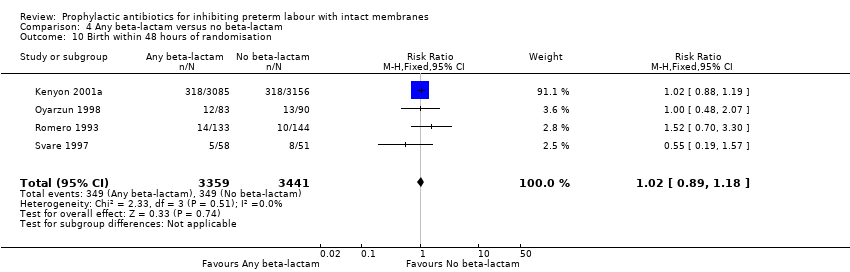
Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 10 Birth within 48 hours of randomisation.

Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 11 Interval between randomisation and birth (days).
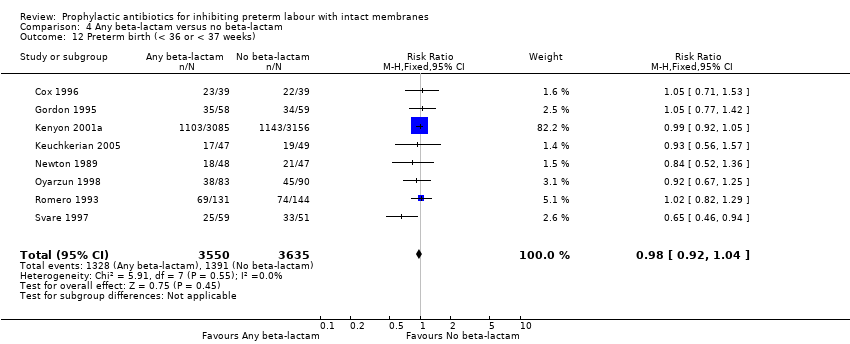
Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 12 Preterm birth (< 36 or < 37 weeks).

Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 13 Respiratory distress syndrome.

Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 14 Intraventricular haemorrhage.

Comparison 4 Any beta‐lactam versus no beta‐lactam, Outcome 15 Necrotising enterocolitis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Perinatal mortality Show forest plot | 10 | 7304 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.88, 1.69] |
| 2 Stillbirth Show forest plot | 8 | 7080 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.43, 1.26] |
| 3 Neonatal death Show forest plot | 9 | 7248 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [1.03, 2.40] |
| 4 Infant death Show forest plot | 1 | 4654 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.68, 1.67] |
| 5 Any functional impairment at 7 years of age. Show forest plot | 1 | 3052 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.99, 1.23] |
| 6 Moderate/severe functional impairment at 7 years of age. Show forest plot | 1 | 3052 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.89, 1.28] |
| 7 Cerebral palsy at 7 years Show forest plot | 1 | 3173 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.82 [0.99, 3.34] |
| 8 Maternal adverse drug reaction requiring cessation of treatment Show forest plot | 5 | 626 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.92, 1.89] |
| 9 Maternal infection Show forest plot | 10 | 7371 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.63, 0.86] |
| 10 Delay in birth (subgrouped by interval) Show forest plot | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Birth within 48 hours | 4 | 6800 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.89, 1.23] |
| 10.2 Birth within 7 days | 8 | 7053 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.87, 1.10] |
| 11 Interval between randomisation and birth (days) Show forest plot | 6 | 2499 | Mean Difference (IV, Random, 95% CI) | 5.59 [0.31, 10.87] |
| 12 Preterm birth (< 36 or < 37 weeks) Show forest plot | 10 | 7387 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.92, 1.05] |
| 13 Gestational age at birth Show forest plot | 10 | 986 | Mean Difference (IV, Random, 95% CI) | 0.53 [0.00, 1.06] |
| 14 Birthweight Show forest plot | 12 | 7531 | Mean Difference (IV, Random, 95% CI) | 58.38 [‐26.24, 143.00] |
| 15 Birthweight < 2500 g Show forest plot | 5 | 6628 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.81, 1.15] |
| 16 Admission to neonatal intensive or special care nursery Show forest plot | 5 | 6875 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.62, 1.10] |
| 17 Neonatal mechanical ventilation Show forest plot | 1 | 6241 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.84, 1.24] |
| 18 Respiratory distress syndrome Show forest plot | 9 | 7200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.84, 1.16] |
| 19 Neonatal positive blood culture Show forest plot | 3 | 6526 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.69, 1.49] |
| 20 Neonatal sepsis Show forest plot | 10 | 7386 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.64, 1.16] |
| 21 Intraventricular haemorrhage Show forest plot | 5 | 6813 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.48, 1.19] |
| 22 Necrotising enterocolitis Show forest plot | 6 | 6880 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.64, 1.73] |
| 23 Major cerebral abnormality Show forest plot | 1 | 6241 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.66, 1.51] |
| 24 Chronic neonatal lung disease Show forest plot | 1 | 6241 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.78, 1.76] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Perinatal mortality Show forest plot | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Beta‐lactam antibiotics alone vs no antibiotics | 4 | 2323 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.64, 2.01] |
| 1.2 Macrolide antibiotics alone vs no antibiotics | 2 | 2222 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.64, 2.11] |
| 1.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 4 | 2569 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.39 [0.79, 2.43] |
| 1.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 3 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.36, 7.39] |
| 2 Stillbirth Show forest plot | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Beta‐lactam antibiotics alone vs no antibiotics | 4 | 2323 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.39, 2.14] |
| 2.2 Macrolide antibiotics alone vs no antibiotics | 2 | 2222 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.20, 1.48] |
| 2.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 2 | 2347 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.28, 1.90] |
| 2.4 Antibiotics active against anaerobic bacteria vs no bacteria | 3 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Neonatal death Show forest plot | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Beta‐lactam antibiotics alone vs no antibiotics | 4 | 2323 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.61, 2.86] |
| 3.2 Macrolide antibiotics alone vs no antibiotics | 2 | 2222 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [0.77, 3.64] |
| 3.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 3 | 2513 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.83 [0.88, 3.82] |
| 3.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 3 | 294 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.63 [0.36, 7.39] |
| 4 Infant death Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Beta‐lactam antibiotics alone vs no antibiotics | 1 | 1515 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.31, 1.65] |
| 4.2 Macrolide antibiotics alone vs no antibiotics | 1 | 1586 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.53, 2.49] |
| 4.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 1 | 1553 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.61, 2.81] |
| 4.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Any functional impairment at 7 years of age. Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Beta‐lactam antibiotics alone vs no antibiotics | 1 | 1008 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.87, 1.25] |
| 5.2 Macrolide antibiotics alone vs no antibiotics | 1 | 1030 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.94, 1.35] |
| 5.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 1 | 1014 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.94, 1.35] |
| 5.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Moderate/severe functional impairment at 7 years of age. Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Beta‐lactam antibiotics alone vs no antibiotics | 1 | 1008 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.75, 1.41] |
| 6.2 Macrolide antibiotics alone vs no antibiotics | 1 | 1030 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.79, 1.48] |
| 6.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 1 | 1014 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.82, 1.53] |
| 6.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Cerebral palsy at 7 years of age Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Beta‐lactam antibiotics alone vs no antibiotics | 1 | 1049 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.41, 3.63] |
| 7.2 Macrolide antibiotics alone vs no antibiotics | 1 | 1073 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.48, 4.15] |
| 7.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 1 | 1052 | Risk Ratio (M‐H, Random, 95% CI) | 2.83 [1.02, 7.88] |
| 7.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Maternal adverse drug reaction requiring cessation of treatment Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 Beta‐lactam antibiotics alone vs no antibiotics | 1 | 82 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.15 [0.13, 75.05] |
| 8.2 Macrolide antibiotics alone vs no antibiotics | 1 | 103 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.49, 1.59] |
| 8.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 2 | 331 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.93, 2.40] |
| 8.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 2 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.59, 1.83] |
| 9 Maternal infection Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1 Beta‐lactam antibiotics alone vs no antibiotics | 4 | 2385 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.56, 0.97] |
| 9.2 Macrolide antibiotics alone vs no antibiotics | 2 | 2222 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.62, 1.08] |
| 9.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 4 | 2563 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.64, 0.98] |
| 9.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 3 | 294 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.11, 3.92] |
| 10 Birth within 48 hours of randomisation Show forest plot | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Beta‐lactam antibiotics alone vs no antibiotics | 1 | 2053 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.75, 1.36] |
| 10.2 Macrolide antibiotics alone vs no antibiotics | 1 | 2119 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.78, 1.42] |
| 10.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 3 | 2520 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.86, 1.45] |
| 10.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 1 | 109 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.19, 1.57] |
| 11 Interval between randomisation and birth (days) Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 Beta‐lactam antibiotics alone vs no antibiotics | 1 | 2053 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐2.96, 2.78] |
| 11.2 Macrolide antibiotics alone vs no antibiotics | 3 | 2302 | Mean Difference (IV, Random, 95% CI) | 4.26 [‐2.88, 11.41] |
| 11.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 3 | 2221 | Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐2.95, 2.41] |
| 11.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 3 | 293 | Mean Difference (IV, Random, 95% CI) | 10.50 [4.95, 16.06] |
| 12 Preterm birth (< 36 or < 37 weeks' gestation) Show forest plot | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 Beta‐lactam antibiotics alone vs no antibiotics | 5 | 2430 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.89, 1.10] |
| 12.2 Macrolide antibiotics alone vs no antibiotics | 2 | 2235 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.91, 1.15] |
| 12.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 4 | 2613 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.89, 1.10] |
| 12.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 2 | 226 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.53, 1.30] |
| 13 Respiratory distress syndrome Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Beta‐lactam antibiotics alone vs no antibiotics | 3 | 3278 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.75, 1.16] |
| 13.2 Macrolide antibiotics alone vs no antibiotics | 1 | 3156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.75, 1.18] |
| 13.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 2 | 3382 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.84, 1.29] |
| 13.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 1 | 109 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.10, 3.37] |
| 14 Necrotising enterocolitis Show forest plot | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 Beta‐lactam antibiotics alone vs no antibiotics | 3 | 2227 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.52, 3.32] |
| 14.2 Macrolide antibiotics alone vs no antibiotics | 1 | 2119 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.44, 3.86] |
| 14.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 2 | 2345 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.36 [0.60, 3.11] |
| 14.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.02, 1.01] |
| 15 Intraventricular haemorrhage Show forest plot | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 Beta‐lactam antibiotics alone vs no antibiotics | 3 | 2241 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.38, 1.87] |
| 15.2 Macrolide antibiotics alone vs no antibiotics | 1 | 2119 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.35, 1.99] |
| 15.3 Macrolide and beta‐lactam antibiotics vs no antibiotics | 2 | 2345 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.43, 2.19] |
| 15.4 Antibiotics active against anaerobic bacteria vs no antibiotics | 1 | 109 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.02, 1.46] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Perinatal mortality Show forest plot | 4 | 6740 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.89, 1.60] |
| 2 Stillbirth Show forest plot | 2 | 6518 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.41, 1.20] |
| 3 Neonatal death Show forest plot | 3 | 6684 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.05, 2.19] |
| 4 Infant death Show forest plot | 1 | 4583 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.99, 2.18] |
| 5 Any functional impairment at 7 years of age. Show forest plot | 1 | 3052 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [1.01, 1.20] |
| 6 Moderate/severe functional impairment at 7 years of age. Show forest plot | 1 | 3052 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.93, 1.26] |
| 7 Cerebral palsy at 7 years Show forest plot | 1 | 3173 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.90 [1.20, 3.01] |
| 8 Maternal adverse drug reaction requiring cessation of treatment Show forest plot | 2 | 331 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.93, 2.40] |
| 9 Maternal infection Show forest plot | 4 | 6745 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.41, 1.07] |
| 10 Birth within 48 hours of randomisation Show forest plot | 3 | 6691 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.94, 1.25] |
| 11 Interval between randomisation and birth (days) Show forest plot | 3 | 6386 | Mean Difference (IV, Random, 95% CI) | 1.07 [‐3.58, 5.72] |
| 12 Preterm birth (< 36 or < 37 weeks) Show forest plot | 4 | 6784 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.95, 1.07] |
| 13 Respiratory distress syndrome Show forest plot | 4 | 6740 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.90, 1.21] |
| 14 Intraventricular haemorrhage Show forest plot | 2 | 6516 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.62, 1.49] |
| 15 Necrotising enterocolitis Show forest plot | 2 | 6516 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.74, 1.80] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Perinatal mortality Show forest plot | 8 | 7109 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.84, 1.48] |
| 2 Stillbirth Show forest plot | 6 | 6887 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.76, 1.58] |
| 3 Neonatal death Show forest plot | 7 | 7053 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.51 [1.06, 2.15] |
| 4 Infant death Show forest plot | 1 | 4654 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.64, 1.38] |
| 5 Any functional impairment at 7 years of age. Show forest plot | 1 | 3052 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.93, 1.11] |
| 6 Moderate/severe functional impairment at 7 years of age. Show forest plot | 1 | 3052 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.88, 1.20] |
| 7 Cerebral palsy at 7 years Show forest plot | 1 | 3173 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [1.06, 2.61] |
| 8 Maternal adverse drug reaction requiring cessation of treatment Show forest plot | 4 | 523 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.61 [1.02, 2.54] |
| 9 Maternal infection Show forest plot | 8 | 7182 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.69, 0.92] |
| 10 Birth within 48 hours of randomisation Show forest plot | 4 | 6800 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.89, 1.18] |
| 11 Interval between randomisation and birth (days) Show forest plot | 3 | 6386 | Mean Difference (IV, Random, 95% CI) | 3.92 [‐5.08, 12.92] |
| 12 Preterm birth (< 36 or < 37 weeks) Show forest plot | 8 | 7185 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.92, 1.04] |
| 13 Respiratory distress syndrome Show forest plot | 8 | 7108 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.88, 1.19] |
| 14 Intraventricular haemorrhage Show forest plot | 4 | 6721 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.56, 1.31] |
| 15 Necrotising enterocolitis Show forest plot | 5 | 6788 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.27, 1.92] |

