Tratamiento antiplaquetario oral para el accidente cerebrovascular isquémico agudo
Información
- DOI:
- https://doi.org/10.1002/14651858.CD000029.pub3Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 25 marzo 2014see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Accidentes cerebrovasculares
- Copyright:
-
- Copyright © 2019 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
Carl Counsell prepared the original version of this Cochrane review, and has checked the analyses and commented on each subsequent revision. Gord Gubitz performed the literature searches, extracted the data, performed the statistical analyses and re‐redrafted the text for the 1999 update. Mei‐Chiun Tseng did the searches, extracted data, updated the analyses and commented on the text for the 2007 update. Peter Sandercock designed and performed a pre‐Cochrane systematic review in 1993 of trials of antiplatelet agents versus control, which became the basis for this review; for each subsequent update he helped with searches, data extraction, data checking, analysis and drafting of the text, and is the guarantor of the review. For this update Emanuela Cecconi did the searches, updated the text and analyses, and commented on the review.
Sources of support
Internal sources
-
University of Edinburgh, UK.
-
University of Aberdeen, UK.
External sources
-
Wellcome Trust, UK.
-
Medical Research Council, UK.
Declarations of interest
Peter Sandercock was the principal investigator of the International Stroke Trial (IST 1997).
Carl Counsell was on the Steering Committee of IST. He has received from a variety of manufacturers of antiplatelet and anticoagulant drugs (Sanofi, Bristol Meyer Squibb, Sanofi‐Synthelabo, Organon, Boehringer Ingelheim, Janssen) lecture fees and travel expenses for lectures delivered at conferences; consultancy fees; has in the past received research grants from Glaxo‐Wellcome and Boehringer Ingelheim; and the drug supply for the start‐up phase of the IST‐3 trial was donated to his department by Boehringer Ingelheim. However, he does not have any contractual consultancy arrangements with any company, or any current research grants from any company, nor does he hold stock (or hold any other financial interests) in any pharmaceutical company.
Gordon Gubitz: randomised participants in the IST.
Mei‐Chiun Tseng: none known.
Acknowledgements
We would like to thank Professor Bernard Boneu for providing us with Dr Pince's thesis; Dr Helen Massey (Syntex, UK) for providing us with unpublished data from the ticlopidine trials; Boehringer Ingelheim for providing information on the Kaye 1989 trial; Professor Livia Candelise for providing additional data from MAST‐I 1995; Dr Zheng‐Ming Chen and Dr Hongchao Pan for providing additional data from CAST 1997; Dr Colin Baigent and Dr Cathie Sudlow at the Clinical Trials Service Unit in Oxford for providing data from the Antiplatelet Trialists' Collaboration; Hazel Fraser for sending us regular lists of trials identified by the Cochrane Stroke Review Group's search strategy, and Brenda Thomas for help with trial searching.
Ongoing trials
Any clinician who knows of additional trials that we have omitted please write to Peter Sandercock.
Version history
| Published | Title | Stage | Authors | Version |
| 2022 Jan 14 | Oral antiplatelet therapy for acute ischaemic stroke | Review | Jatinder S Minhas, Tamara Chithiramohan, Xia Wang, Sam C Barnes, Rebecca H Clough, Meeriam Kadicheeni, Lucy C Beishon, Thompson Robinson | |
| 2014 Mar 25 | Oral antiplatelet therapy for acute ischaemic stroke | Review | Peter AG Sandercock, Carl Counsell, Mei‐Chiun Tseng, Emanuela Cecconi | |
| 2008 Jul 16 | Antiplatelet therapy for acute ischaemic stroke | Review | Peter AG Sandercock, Carl Counsell, Gordon J Gubitz, Mei‐Chiun Tseng | |
| 2003 Apr 22 | Antiplatelet therapy for acute ischaemic stroke | Review | Peter Sandercock, Gordon J Gubitz, Peter Foley, Carl Counsell | |
Differences between protocol and review
For this update we changed the title of the review to 'Oral antiplatelet therapy for acute ischaemic stroke'. We decided to exclude parenterally administrated antiplatelet agents since some of them, GP IIb/IIIa receptor inhibitors, are the focus of a separate review (Ciccone 2006) which is being updated.
Moreover, we planned to assess the methodological quality of any new trials in the following domains: random sequence generation; allocation concealment; blinding of participants, personnel and outcome assessment; incomplete outcome data; and selective outcome reporting. However, since no new trials were identified we have retained the original assessment of risk of bias and no new sensitivity analyses were performed.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Aspirin [therapeutic use];
- Brain Ischemia [drug therapy, prevention & control];
- Dipyridamole [therapeutic use];
- Platelet Aggregation Inhibitors [adverse effects, *therapeutic use];
- Randomized Controlled Trials as Topic;
- Risk;
- Stroke [*drug therapy, prevention & control];
- Ticlopidine [therapeutic use];
- Time‐to‐Treatment;
Medical Subject Headings Check Words
Humans;
PICO
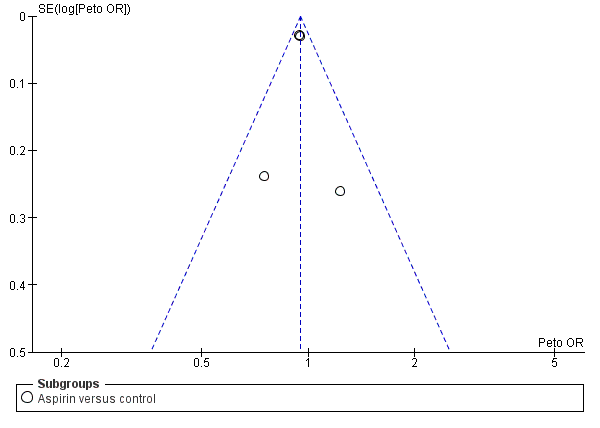
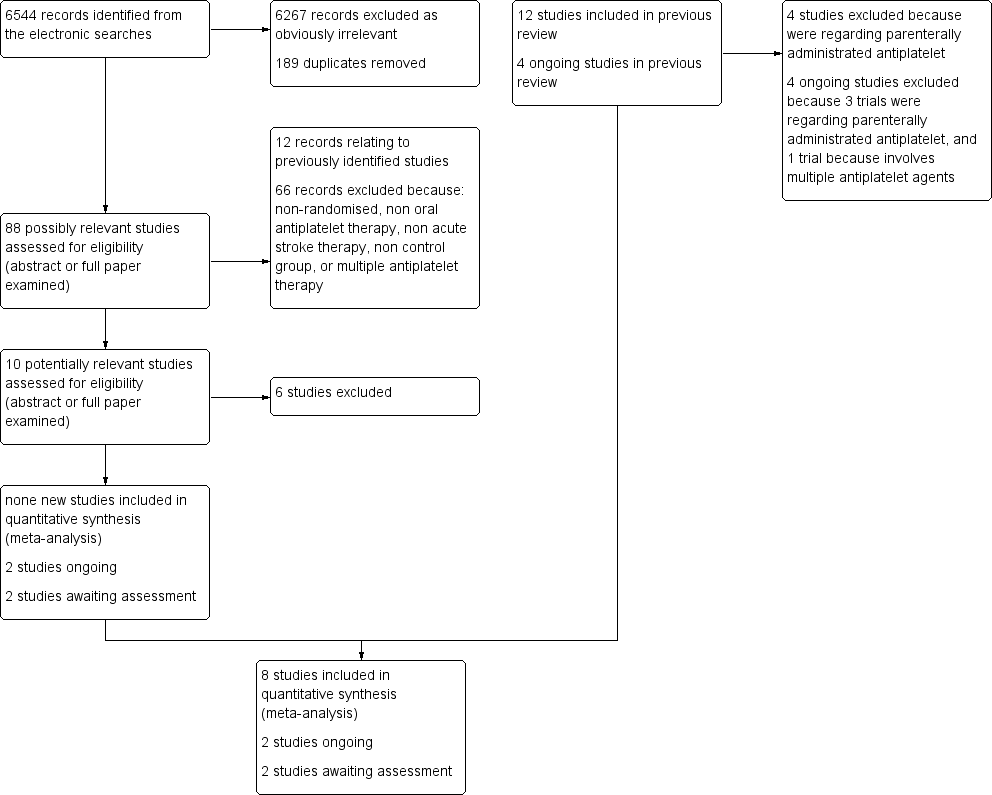
Funnel plot of comparison: 1 Antiplatelet agent versus control in acute presumed ischaemic stroke, outcome: 1.1 Death or dependence at end of follow‐up.

Funnel plot of comparison: 1 Antiplatelet agent versus control in acute presumed ischaemic stroke, outcome: 1.2 Deaths from all causes during treatment period.
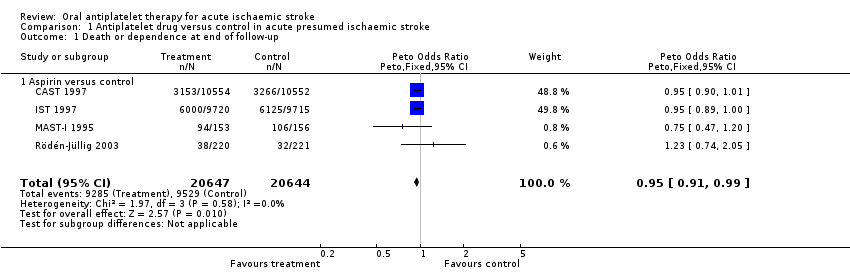
Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 1 Death or dependence at end of follow‐up.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 2 Deaths from all causes during treatment period.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 3 Deaths from all causes during follow‐up.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 4 Deep venous thrombosis during treatment period.
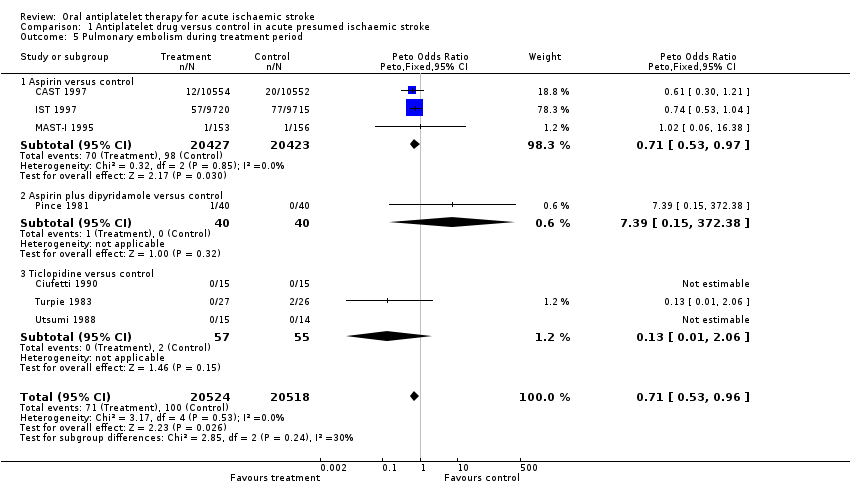
Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 5 Pulmonary embolism during treatment period.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 6 Recurrent ischaemic/unknown stroke during treatment period.
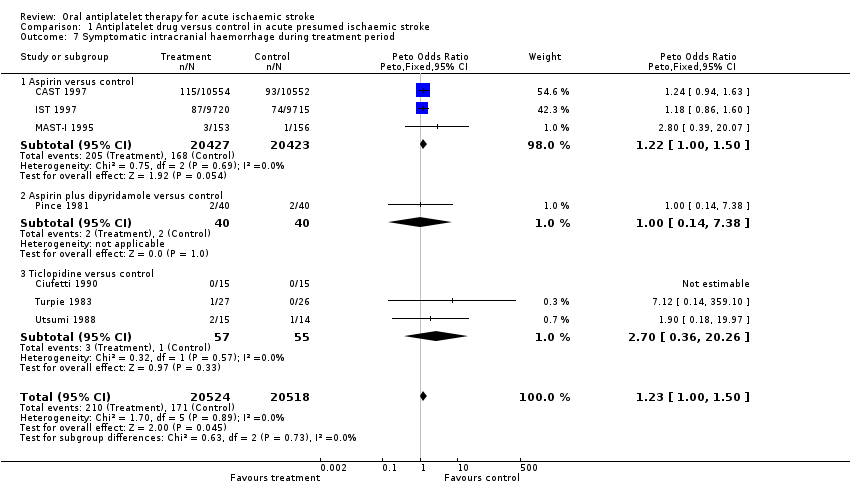
Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 7 Symptomatic intracranial haemorrhage during treatment period.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 8 Any recurrent stroke/intracranial haemorrhage during treatment period.

Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 9 Major extracranial haemorrhage during treatment period.
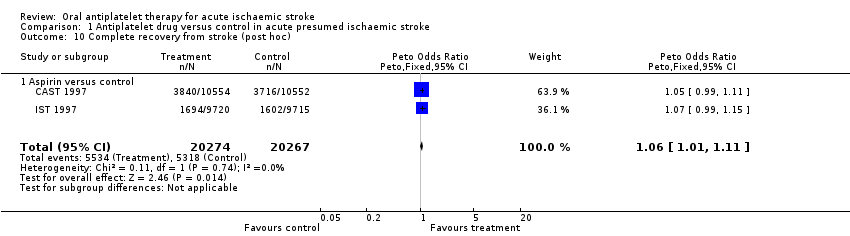
Comparison 1 Antiplatelet drug versus control in acute presumed ischaemic stroke, Outcome 10 Complete recovery from stroke (post hoc).
| Outcome | Control event rate | No of events avoided | NNTB or NNTH |
| Per 1000 people treated (95% CI) | Data are number needed to treat to benefit (NNTB) (95% CI) unless otherwise indicated. NNTH = number needed to treat to harm | ||
| Estimated from the average of the control event rate in the 2 largest trials (CAST 1997 and IST 1997) | Estimated by applying the odds ratio for the outcome for studies of aspirin. Calculator is available at: http://www.dcn.ed.ac.uk/csrg/entity/entity_NNT2.asp | Estimated by applying the odds ratio for the outcome for studies of aspirin. Calculator is available at: http://www.dcn.ed.ac.uk/csrg/entity/entity_NNT2.asp | |
| Death or dependence at end of follow‐up | 0.47 | 13 (3 to 23) | 79 (43 to 400) |
| Deaths from all causes during follow‐up | 0.13 | 9 (2 to 15) | 108 (66 to 436) |
| Pulmonary embolism during treatment period | 0.01 | 1 (0 to 2) | 693 (427 to 6700) |
| Recurrent ischaemic/unknown stroke during treatment period | 0.03 | 7 (4 to 10) | 140 (104 to 248) |
| Symptomatic intracranial haemorrhage during treatment period | 0.01 | ‐2 (i.e. 2 extra) (‐4 to 0) | NNTH 574 (254 to 126 010) |
| Any recurrent stroke/intracranial haemorrhage during treatment | 0.04 | 5 (1 to 8) | 200 (123 to 868) |
| Major extracranial haemorrhage during treatment period | 0.01 | ‐4 (i.e. 4 extra) (‐7 to ‐2) | NNTH 245 (153 to 481) |
| Complete recovery from stroke (post hoc) | 0.26 | 11 (2 to 21) | 89 (49 to 523) |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Death or dependence at end of follow‐up Show forest plot | 4 | 41291 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.95 [0.91, 0.99] |
| 1.1 Aspirin versus control | 4 | 41291 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.95 [0.91, 0.99] |
| 2 Deaths from all causes during treatment period Show forest plot | 8 | 41483 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.92 [0.85, 1.00] |
| 2.1 Aspirin versus control | 4 | 41291 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.92 [0.85, 1.00] |
| 2.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.47 [0.43, 4.99] |
| 2.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.01, 1.20] |
| 3 Deaths from all causes during follow‐up Show forest plot | 8 | 41483 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.92 [0.87, 0.98] |
| 3.1 Aspirin versus control | 4 | 41291 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.92 [0.87, 0.98] |
| 3.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.47 [0.43, 4.99] |
| 3.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.12 [0.02, 0.88] |
| 4 Deep venous thrombosis during treatment period Show forest plot | 2 | 133 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.78 [0.36, 1.67] |
| 4.1 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.35 [0.13, 0.95] |
| 4.2 Ticlopidine versus control | 1 | 53 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.37 [0.72, 7.73] |
| 5 Pulmonary embolism during treatment period Show forest plot | 7 | 41042 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.71 [0.53, 0.96] |
| 5.1 Aspirin versus control | 3 | 40850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.71 [0.53, 0.97] |
| 5.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.39 [0.15, 372.38] |
| 5.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.13 [0.01, 2.06] |
| 6 Recurrent ischaemic/unknown stroke during treatment period Show forest plot | 7 | 41042 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.77 [0.69, 0.87] |
| 6.1 Aspirin versus control | 3 | 40850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.77 [0.69, 0.87] |
| 6.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Symptomatic intracranial haemorrhage during treatment period Show forest plot | 7 | 41042 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.23 [1.00, 1.50] |
| 7.1 Aspirin versus control | 3 | 40850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.22 [1.00, 1.50] |
| 7.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.0 [0.14, 7.38] |
| 7.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.70 [0.36, 20.26] |
| 8 Any recurrent stroke/intracranial haemorrhage during treatment period Show forest plot | 7 | 41042 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.88 [0.79, 0.97] |
| 8.1 Aspirin versus control | 3 | 40850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.87 [0.79, 0.97] |
| 8.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.0 [0.14, 7.38] |
| 8.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 2.70 [0.36, 20.26] |
| 9 Major extracranial haemorrhage during treatment period Show forest plot | 7 | 41042 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.69 [1.35, 2.11] |
| 9.1 Aspirin versus control | 3 | 40850 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.69 [1.35, 2.11] |
| 9.2 Aspirin plus dipyridamole versus control | 1 | 80 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 Ticlopidine versus control | 3 | 112 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Complete recovery from stroke (post hoc) Show forest plot | 2 | 40541 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.06 [1.01, 1.11] |
| 10.1 Aspirin versus control | 2 | 40541 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 1.06 [1.01, 1.11] |