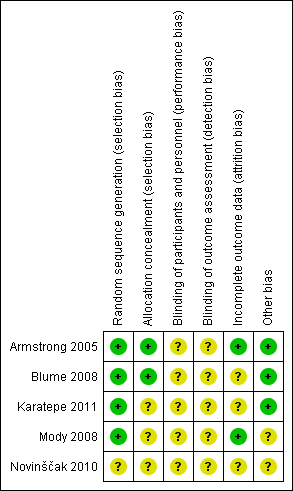
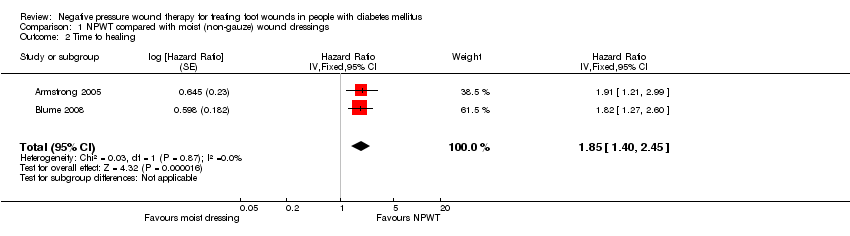
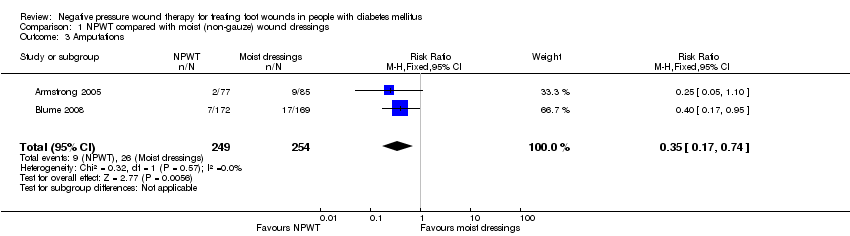
| Armstrong 2005 | 16 weeks | Diabetic foot amputation to trans‐metatarsal level | Group A: moist wound therapy with alginates, hydrocolloid, foam or hydrogel dressings (n = 85) Group B: NPWT (VAC system, dressing changes every 48 h. Treatment conducted until wound closure or completion of 112‐day assessment (n = 77) | Number of wounds completely healed Group A: 33/85 (38.8%) Group B: 43/77 (55.8%) Of healed wounds —healed by secondary intention (without primary/surgical wound closure) Group A: 25/33 (75.8%) Group B: 31/43 (72.1%) Remaining wounds were closed following surgery. Time to wound healing median time to healing Group A: 77 days (IQR 40 to 122) Group B: 56 days (IQR 26 to 92) Log rank = p = 0.005 Amputation Number of participants undergoing further amputation Group A: 9/85 (10.6%) Major = 5/Minor = 4 Group B: 2/77 (2.3%) Major = 0/Minor = 2 There was no difference noted in time to healing for acute or chronic wounds. | Adverse events Participants who had one or more adverse events Group A: 46/85 (54.1%) Group B: 40/77 (51.9%) Participants who had one or more treatment‐related adverse events Group A: 11/85 (12.9%) 5 classified as serious Group B: 9/77 (11.7%) 1 classified serious Resource use Average total cost per participant Group A: USD 36,887 Group B: USD26,972 Average total direct cost per participants for those treated for 8 weeks or longer Group A: USD 36,096 Group B: USD 27,270 Average per participant cost to achieve 100% healing Group A: USD 38,806 Group B: USD 25,954 |
| Blume 2008 | 16 weeks | Ulceration of the foot in people with diabetes | Group A: advanced moist wound therapy dressings used according to guidelines/local protocols (n = 169) Group B: NPWT (VAC system), applied according to manufacturer’s instructions. (n = 172) | Number of wounds completely healed (six participants excluded in paper as did not receive treatment, added back into denominator here) Group A: 48/169 (28.4%) Group B: 73/172 (42.4%) Proportion of wounds closed using surgery (unclear if considered part of healed group) Group A: 14/169 (8.3%) Group B: 16/172 (9.3%) Time to wound healing median time to healing Group A: could not be estimated Group B: 96 days (95% CI 75.0 to 114.0) Log rank taken as P value 0.001 Amputation Number of participants undergoing amputation* Group A: 17/169 (10.1%) Major = 4; minor = 13 Group B: 7/172 (4.1%) Major = 5; minor = 2 | Adverse events Limited data: not extracted Resource use – taken from conference abstract that we think is related to this main publication. Mean estimated total costs of inpatient services per participant Group A: USD 8570 (95%CI USD 5922 to USD 11,432) Group B: USD 5206 (95%CI USD 3172 to USD 7561) |
| Karatepe 2011 | Not specified. Last assessment one month after healing | Diabetic foot ulcers | Group A: conventional wound care treatment: based on text in report taken to be dry gauze (n = 37) Group B: NPWT (VAC system) (n = 30) | Time to healing Median time to healing Group A: 4.4 weeks Group B: 3.9 weeks Mean value presented but not extracted. No specific P value presented | Health‐related quality of life SF‐36: Data not presented. |
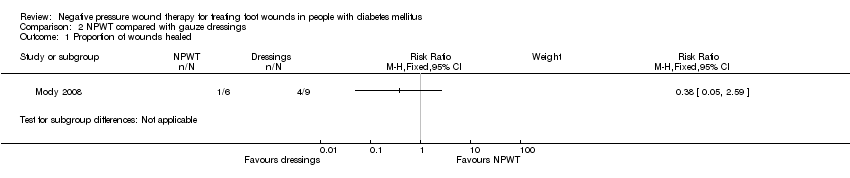
| Mody 2008 | Not specified: until healing or loss to follow‐up | Diabetic foot ulcers | Group A: wet‐to‐dry gauze (n = 9) Group B: locally‐constructed NPWT (n = 6) | Number of wounds completely healed By secondary intention: Group A: 1/9 (11.0%) Group B: 1/6 (16.6%) By delayed primary closure: Group A: 3/9 (33%) Group B: 0/6 (0%) | |
| Novinščak 2010 | 2 months | Complicated diabetic foot ulcers | Group A: classic gauze (n = 8) Group B: dressings (moist) (n = 12)
Group C: NPWT (n = 7) | Healing rate (percentage with wound closure – defined by author on contact) Group A: 4/8* (50%) Group B: 9/12* (75%) Group C: * could not be calculated (90%) *Figure calculated by review author as only proportions obtained from study author | |