Acupuncture or acupressure for pain management during labour
Abstract
Background
Many women would like to avoid pharmacological or invasive methods of pain management in labour and this may contribute towards the popularity of complementary methods of pain management. This review examined evidence about the use of acupuncture and acupressure for pain management in labour. This is an update of a review last published in 2011.
Objectives
To examine the effects of acupuncture and acupressure for pain management in labour.
Search methods
For this update, we searched Cochrane Pregnancy and Childbirth’s Trials Register, (25 February 2019), the Cochrane Central Register of Controlled Trials (the Cochrane Library 2019, Issue 1), MEDLINE (1966 to February 2019), CINAHL (1980 to February 2019), ClinicalTrials.gov (February 2019), the WHO International Clinical Trials Registry Platfory (ICTRP) (February 2019) and reference lists of included studies.
Selection criteria
Published and unpublished randomised controlled trials (RCTs) comparing acupuncture or acupressure with placebo, no treatment or other non‐pharmacological forms of pain management in labour. We included all women whether nulliparous or multiparous, and in spontaneous or induced labour.
We included studies reported in abstract form if there was sufficient information to permit assessment of risk of bias. Trials using a cluster‐RCT design were eligible for inclusion, but quasi‐RCTs or cross‐over studies were not.
Data collection and analysis
Two review authors independently assessed trials for inclusion and risk of bias, extracted data and checked them for accuracy. We assessed the certainty of the evidence using the GRADE approach.
Main results
We included 28 trials with data reporting on 3960 women. Thirteen trials reported on acupuncture and 15 trials reported on acupressure. No study was at a low risk of bias on all domains. Pain intensity was generally measured on a visual analogue scale (VAS) of 0 to 10 or 0 to 100 with low scores indicating less pain.
Acupuncture versus sham acupuncture
Acupuncture may make little or no difference to the intensity of pain felt by women when compared with sham acupuncture (mean difference (MD) ‐4.42, 95% confidence interval (CI) ‐12.94 to 4.09, 2 trials, 325 women, low‐certainty evidence). Acupuncture may increase satisfaction with pain relief compared to sham acupuncture (risk ratio (RR) 2.38, 95% CI 1.78 to 3.19, 1 trial, 150 women, moderate‐certainty evidence), and probably reduces the use of pharmacological analgesia (RR 0.75, 95% CI 0.63 to 0.89, 2 trials, 261 women, moderate‐certainty evidence). Acupuncture may have no effect on assisted vaginal birth (very low‐certainty evidence), and probably little to no effect on caesarean section (low‐certainty evidence).
Acupuncture compared to usual care
We are uncertain if acupuncture reduces pain intensity compared to usual care because the evidence was found to be very low certainty (standardised mean difference (SMD) ‐1.31, 95% CI ‐2.14 to ‐0.49, 4 trials, 495 women, I2 = 93%). Acupuncture may have little to no effect on satisfaction with pain relief (low‐certainty evidence). We are uncertain if acupuncture reduces the use of pharmacological analgesia because the evidence was found to be very low certainty (average RR 0.72, 95% CI 0.60 to 0.85, 6 trials, 1059 women, I2 = 70%). Acupuncture probably has little to no effect on assisted vaginal birth (low‐certainty evidence) or caesarean section (low‐certainty evidence).
Acupuncture compared to no treatment
One trial compared acupuncture to no treatment. We are uncertain if acupuncture reduces pain intensity (MD ‐1.16, 95% CI ‐1.51 to ‐0.81, 163 women, very low‐certainty evidence), assisted vaginal birth or caesarean section because the evidence was found to be very low certainty.
Acupuncture compared to sterile water injection
We are uncertain if acupuncture has any effect on use of pharmacological analgesia, assisted vaginal birth or caesarean section because the evidence was found to be very low certainty.
Acupressure compared to a sham control
We are uncertain if acupressure reduces pain intensity in labour (MD ‐1.93, 95% CI ‐3.31 to ‐0.55, 6 trials, 472 women) or assisted vaginal birth because the evidence was found to be very low certainty. Acupressure may have little to no effect on use of pharmacological analgesia (low‐certainty evidence). Acupressure probably reduces the caesarean section rate (RR 0.44, 95% CI 0.27 to 0.71, 4 trials, 313 women, moderate‐certainty evidence).
Acupressure compared to usual care
We are uncertain if acupressure reduces pain intensity in labour (SMD ‐1.07, 95% CI ‐1.45 to ‐0.69, 8 trials, 620 women) or increases satisfaction with pain relief (MD 1.05, 95% CI 0.75 to 1.35, 1 trial, 105 women) because the evidence was found to be very low certainty. Acupressure may have little to no effect on caesarean section (low‐certainty evidence).
Acupressure compared to a combined control
Acupressure probably slightly reduces the intensity of pain during labour compared with the combined control (measured on a scale of 0 to 10 with low scores indicating less pain) (SMD ‐0.42, 95% CI ‐0.65 to ‐0.18, 2 trials, 322 women, moderate‐certainty evidence). We are uncertain if acupressure has any effect on the use of pharmacological analgesia (RR 0.94, 95% CI 0.71 to 1.25, 1 trial, 212 women), satisfaction with childbirth, assisted vaginal birth or caesarean section because the certainty of the evidence was all very low.
No studies were found that reported on sense of control in labour and only one reported on satisfaction with the childbirth experience.
Authors' conclusions
Acupuncture in comparison to sham acupuncture may increase satisfaction with pain management and reduce use of pharmacological analgesia. Acupressure in comparison to a combined control and usual care may reduce pain intensity. However, for other comparisons of acupuncture and acupressure, we are uncertain about the effects on pain intensity and satisfaction with pain relief due to very low‐certainty evidence. Acupuncture may have little to no effect on the rates of caesarean or assisted vaginal birth. Acupressure probably reduces the need for caesarean section in comparison to a sham control. There is a need for further high‐quality research that include sham controls and comparisons to usual care and report on the outcomes of sense of control in labour, satisfaction with the childbirth experience or satisfaction with pain relief.
PICOs
Plain language summary
Acupuncture or acupressure for relieving pain during labour
We examined the evidence from randomised controlled trials on the use of acupuncture or acupressure in helping women to manage pain during labour. This is an update of a review last published in 2011.
What is the issue?
The pain women experience during labour can be intense, with body tension, anxiety and fear making it worse. Pain is caused by contractions of the uterus, the opening of the cervix and, in the late first and second stages, by stretching of the vagina and pelvic floor as the baby moves down the birth canal. Effective, satisfactory pain management needs to be individualised for each woman. Women may also use strategies to try to break the fear‐tension‐pain cycle and work with the pain. Working with the pain involves offering women support and encouragement, finding comfortable positions, immersion in water and self‐help techniques.
Many women would like to go through labour without using drugs. Women may turn to acupuncture or acupressure to help reduce their pain and improve management of the pain.
Why is this important?
Acupuncture has a long history of use in Asia, including China, Korea and Japan. Technical needling skills are needed to apply the needles at the correct points. Acupressure also has its origins in early China. To apply acupressure, the therapist uses their hands and fingers to activate the same points as in acupuncture. Sometimes only a few points are needed to alleviate pain or bring about a feeling of relaxation. Other times a combination of points may be required for greater effect. Some forms of acupressure are applied by trained health professionals, while others can be applied by the individual as a form of self‐massage.
What evidence did we find?
Our updated search in February 2019 identified 17 new trials.
This review now includes 28 trials reporting on 3960 women, with 27 trials contributing results. The trials compared acupuncture or acupressure with sham treatment as placebo, no treatment or usual care for pain management during labour. Thirteen trials reported on acupuncture and 15 trials reported on acupressure. For 18 of the 27 trials women were in spontaneous labour. In other studies labour may have been induced.
Eight studies applied individualised traditional Chinese medicine while set acupuncture points were used in the majority of studies. We noted wide variation in how stimulation was applied (manually or with electro‐stimulation), duration of needling, number of points used, and depth of needling. It is unclear how representative the trial treatments were of acupuncture in practice.
Most comparisons suggest a small beneficial effect from acupuncture, though the supporting evidence was limited. We are uncertain if acupuncture reduces the intensity of pain when compared with sham acupuncture (2 trials, 325 women), usual care (4 trials, 495 women) and no treatment (1 trial, 163 women). The certainty of the evidence was low or very low. Acupuncture may increase satisfaction with pain relief compared to sham acupuncture (one trial, moderate‐certainty evidence). It slightly reduced the use of pharmacological analgesia compared to sham acupuncture (2 trials, 261 women, moderate‐certainty evidence). Use of acupressure was associated with a reduction in pain intensity in labour when compared to a combined control (2 trials, 322 women, moderate‐certainty evidence). Acupuncture did not appear to have any effect on the need for assisted vaginal births or caesarean births, but acupressure reduced the rate of caesarean section when compared to sham acupressure.
What does this mean?
Acupuncture may increase satisfaction with pain relief and reduce use of pharmacological pain relief. Acupressure may help relieve pain during labour, although the pain reduction may not be large. However, for other comparisons of acupuncture and acupressure, we are uncertain about the effects on pain intensity and satisfaction with pain relief due to very low‐certainty evidence. Acupuncture or acupressure may have little to no effect on assisted vaginal birth, but women having acupressure maybe less likely to need a caesarean section. Studies were conducted in different countries, which may reflect the different styles of applying acupuncture. A weakness of a number of trials continues to be that very few outcomes were measured and no safety outcomes were reported. More high‐quality research is needed.
Authors' conclusions
Summary of findings
| Acupuncture compared to sham control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with sham control | Risk with acupuncture | |||||
| Pain intensity Lower scores indicate less pain intensity | The mean pain intensity ranged across control groups from 52.94 to 91.4 | The mean pain intensity score in the intervention group was 4.42 lower (12.94 lower to 4.09 higher) | 325 | ⊕⊕⊝⊝ | ||
| Satisfaction with pain relief in labour | Study population | RR 2.38 | 150 | ⊕⊕⊕⊝ | ||
| 387 per 1000 | 920 per 1000 | |||||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.75 | 261 | ⊕⊕⊕⊝ | ||
| 767 per 1000 | 576 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.10 | 261 | ⊕⊝⊝⊝ | ||
| 163 per 1000 | 179 per 1000 | |||||
| Caesarean section | Study population | RR 1.11 | 411 | ⊕⊕⊝⊝ | ||
| 49 per 1000 | 54 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: one study high or unclear risk of bias on six domains. 2 Downgraded one level due to serious inconsistency: substantial heterogeneity present I2 = 87% 3 Downgraded one level due to serious imprecision: small sample size (150) 4 Downgraded one level due to serious risk of bias: one study did not blind participants to group allocation. Should not affect sham arm outcome but blinding integrity not reported. 5 Downgraded one level due to serious inconsistency: substantial heterogeneity present I2 = 72% 6 Downgraded one level for imprecision due to small sample size and wide confidence intervals crossing the line of no effect 7 Downgraded one level for imprecision due to small number of events and wide confidence intervals crossing the line of no effect 8 Downgraded one level due to serious risk of bias: one study did not blind participants to group allocation and two studies at high risk of other bias | ||||||
| Acupuncture compared to usual care for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with acupuncture | |||||
| Pain intensity Mix of NRS and VAS scales so analysed using SMD | The mean pain intensity score in the intervention group was 1.31 standard deviations lower (2.14 lower to 0.49 lower) | 495 | ⊕⊝⊝⊝ | |||
| Satisfaction with pain relief in labour | Study population | RR 1.07 | 343 | ⊕⊕⊝⊝ | ||
| 787 per 1000 | 843 per 1000 | |||||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.72 | 1059 | ⊕⊝⊝⊝ | ||
| 833 per 1000 | 600 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 0.93 | 1217 | ⊕⊕⊝⊝ | ||
| 127 per 1000 | 118 per 1000 | |||||
| Caesarean section | Study population | RR 0.72 | 861 | ⊕⊕⊝⊝ | ||
| 116 per 1000 | 83 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels for very serious risk of bias: two of the three studies had high risk of performance bias and this was likely to influence a self‐reported outcome. 2 Downgraded two levels for very serious inconsistency: considerable heterogeneity present (I2 = 93%) not explained by subgroup analysis. 3 Downgraded two levels for very serious risk of bias: both studies had unclear or high risk of bias related to blinding and this was likely to influence a self‐reported outcome 4 Downgraded two levels for very serious risk of bias: all studies had unclear or high risk of performance bias and this was likely to influence the need for additional analgesia. 5 Downgraded one level for serious inconsistency: substantial heterogeneity (I2 = 70%) which is not explained by subgroups. 6 Downgraded one level for serious risk of bias: five of six studies at unclear or high risk of bias in both performance and detection bias. This may have influenced the outcome. 7 Downgraded one level for serious risk of bias: three of four studies at high or unclear risk of bias in both performance and detection bias. This may have influenced the outcome. 8 Downgraded one level for imprecision due to wide confidence intervals. | ||||||
| Acupuncture compared to no treatment for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with no treatment | Risk with acupuncture | |||||
| Pain intensity Lower scores indicate less pain. | The mean pain intensity in the control group was 7.92 | The mean pain intensity score in the intervention groups was 1.16 lower | ‐ | 163 | ⊕⊝⊝⊝ | |
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Assisted vaginal birth | Study population | RR 0.49 | 163 | ⊕⊝⊝⊝ | ||
| 123 per 1000 | 60 per 1000 | |||||
| Caesarean section | Study population | RR 0.76 | 163 | ⊕⊝⊝⊝ | ||
| 160 per 1000 | 122 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded by two levels for very serious risk of bias: high risk of bias in one domain (blinding for a subjective outcome) and unclear risk of bias in four domains. 2 Downgraded one level for serious imprecision due to a single study providing data with a small sample size (163) 3 Downgraded two levels for very serious imprecision due to a single study, with few events, small sample size and wide confidence intervals providing data | ||||||
| Acupuncture compared to water injection for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with water injection | Risk with acupuncture | |||||
| Pain intensity ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.84 | 128 | ⊕⊝⊝⊝ | ||
| 424 per 1000 | 356 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.60 | 128 | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 97 per 1000 | |||||
| Caesarean section | Study population | RR 1.33 | 128 | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 81 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to very serious risk of bias: high or unclear risk of bias in both blinding performance and detection bias 2 Downgraded two levels due to very serious imprecision: small study (128) with few events and wide confidence intervals crossing the line of no effect | ||||||
| Acupressure compared to sham control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with sham control | Risk with acupressure | |||||
| Pain intensity as measured by a 10 cm visual analogue scale. Lower scores indicate less pain | The mean pain intensity in the control groups was 8.35 | The mean pain intensity score in the intervention group was 1.93 lower (3.31 lower to 0.55 lower) | 472 | ⊕⊝⊝⊝ | ||
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.54 | 75 | ⊕⊕⊝⊝ | ||
| 256 per 1000 | 138 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 3.00 | 100 | ⊕⊝⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Caesarean section | Study population | RR 0.44 | 313 | ⊕⊕⊕⊝ | ||
| 308 per 1000 | 136 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level for serious risk of bias: majority of studies have unclear risk of bias in at least three domains. 2 Downgraded two levels for very serious inconsistency: considerable heterogeneity (I2 = 94%) 3 Downgraded two levels for very serious imprecision: very small sample size (75), small number of events and very wide confidence intervals 4 Downgraded one level for serious risk of bias: single study has high risk of performance bias and an unclear risk of allocation bias 5 Downgraded two levels for very serious imprecision: small sample size (100) and very wide confidence interval and small number of events 6 Downgraded one level for serious risk of bias: all studies have unclear risk of bias in at least three domains. Two studies have high or unclear risk of bias relating to performance bias | ||||||
| Acupressure compared to usual care for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with acupressure | |||||
| Pain intensity as measured by numeric rating scale (NRS) and visual analogue scale (VAS). Lower scores indicate less pain. | The mean pain intensity was 8.44 | The mean pain intensity score in the intervention group was 1.07 standard deviations lower (1.45 lower to 0.69 lower). | 620 | ⊕⊝⊝⊝ | The use of acupressure would result in a pain score approximately 2 cm lower on a 10 cm VAS or 2 points on a numeric rating scale compared to usual care. | |
| Satisfaction with pain relief | The mean satisfaction score with pain relief in the control group was 1.6 | The mean satisfaction with pain relief score was 1.05 higher (0.75 higher to 1.35 higher) | 105 | ⊕⊝⊝⊝ | ||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Assisted vaginal birth ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Caesarean section | Study population | RR 0.82 | 391 | ⊕⊕⊝⊝ | ||
| 241 per 1000 | 198 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: majority of included studies have high or unclear risk of bias relating to performance and detection bias 2 Downgraded two levels due to very serious inconsistency: considerable heterogeneity (I2 = 75%) 3 Downgraded two levels due to very serious risk of bias: single study at high risk of bias for selection, performance and detection bias. Very likely to have influenced the outcome 4 Downgraded one level due to serious imprecision: small sample size (105) 5 Downgraded one level due to serious risk of bias: two of the four studies included were at high risk of performance and detection bias, two studies were at high or unclear risk of selection bias and three at high or unclear risk of incomplete outcome data 6 Downgraded one level due to serious imprecision: wide confidence intervals incorporating both benefit and harm | ||||||
| Acupressure compared to combined control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with combined control | Risk with acupressure | |||||
| Pain intensity One study used VAS pain score on scale 1 ‐ 100 mm One study used VAS pain score on scale 1 ‐ 10 mm ‐ the mean | The mean pain intensity score in the intervention group was 0.42 standard deviations lower (0.65 lower to 0.18 lower) | 322 | ⊕⊕⊕⊝ | |||
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth | The mean satisfaction score with childbirth in the control group was 80.2 | The mean satisfaction score in the intervention group was 4.8 higher | ‐ | 212 | ⊕⊝⊝⊝ | |
| Use of pharmacological analgesia | Study population | RR 0.94 | 212 | ⊕⊝⊝⊝ | ||
| 525 per 1000 | 493 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 0.81 | 212 | ⊕⊝⊝⊝ | ||
| 156 per 1000 | 126 per 1000 | |||||
| Caesarean section | Study population | RR 0.48 | 212 | ⊕⊝⊝⊝ | ||
| 206 per 1000 | 99 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: both studies have unclear risk of bias for performance bias, possible effect on this outcome 2 Downgraded one level due to serious risk of bias: single study has unclear risk of performance bias, likely to effect this outcome 3 Downgraded two levels due to very serious imprecision: wide confidence interval greater than 0.25 on either side of the line of no effect and small sample size 4 Downgraded two levels for very serious imprecision: wide confidence interval encompassing both benefit and harm and small sample size | ||||||
Background
This review is one in a series of Cochrane Reviews examining pain management in labour. An earlier version of this review contributed to an overview of systematic reviews of pain management for women in labour (Jones 2012) and shared a generic protocol (Jones 2011). This review is an update of a review last published in 2011 (Smith 2011b).
Description of the condition
Labour presents a physiological and psychological challenge for women. As labour becomes more imminent, this can be a time of conflicting emotions: fear and apprehension can be coupled with excitement and happiness. Tension, anxiety and fear are factors contributing towards women's perception of pain and may also affect their labour and birth experience. Pain associated with labour has been described as one of the most intense forms of pain that can be experienced (Melzack 1984), although conversely some women do not experience intense pain during labour. Labour involves three stages, relating to dilation of the cervix, birth of the baby and delivery of the placenta. The latent phase is the early part of labour where there are irregular contractions and the cervix is softening and beginning to dilate. The first stage of labour consists of regular contractions with increasing strength and frequency accompanied by more significant cervical dilation of at least 4 cm to 6 cm. Transition may be observable anywhere between 7 cm to 8 cm and full dilation. The second stage of labour commences from full cervical dilation to the birth of the baby. The third stage of labour involves expulsion of the placenta.
Pain experienced by women in labour is caused by uterine contractions, the dilatation of the cervix and, in the late first stage and second stage, by stretching of the vagina and pelvic floor to accommodate the baby. There are different philosophies of pain management, which involve strategies to prevent what has been described as the fear‐tension‐pain cycle (Dick‐Read 2004; Dowswell 2009). Dick‐Read 2004 an advocate of 'natural childbirth', suggested that fear and anxiety can produce muscle tension, resulting in an increased perception of pain. The gate control theory of pain, first proposed by Melzack and Wall in 1965, suggests that pain can be offset by other 'larger' or overriding sensations, such as rubbing or pressing on an injury to reduce pain sensation (Melzack 1965). Melzack and colleagues further proposed the neuromatrix theory of pain, which introduces the notion that pain is multidimensional, and that pain intensity is influenced by many factors, including sensory, emotional and cognitive processes, including experiences and memory (Melzack 2004). In labour, the theory of pain incorporates elements of the gate control theory, but also past experiences, cultural factors, emotional state, cognitive input, stress regulation and immune systems, as well as immediate sensory input (Trout 2004). However, the complete removal of pain does not necessarily mean a more satisfying birth experience for women (Dickenson 2003). A follow‐up study at five years after birth found those women who had epidurals were less positive about the birth five years later (Maimburg 2016). The literature suggests that satisfaction with childbirth is significantly linked with women's sense of agency and participation in decision‐making during pregnancy and birth (Hodnett 2002; Hollins Martin 2013; Hotelling 2013; Howarth 2010). Effective and satisfactory pain management needs to be individualised for each woman, and may be influenced by two paradigms, working with pain, or pain relief (Leap 2010). The working with pain paradigm includes the belief that there are long‐term benefits to promoting normal birth, and that pain and women's agency plays an important role in this process. With a focus on women's natural hormonal mediation of labour, the working with pain approach offers support and encouragement to women, advocates the use of immersion in water, comfortable positions and self‐help techniques to cope with normal labour pain and facilitate the normal hormones of labour. The pain relief paradigm is characterised by the belief that no woman need suffer pain in labour and women are offered a variety of pharmacological pain relief.
The two concepts of efficacy and effectiveness are also important to consider when evaluating research outcomes for labour pain management. Efficacy trials are designed to show the extent to which a specific treatment or component of an intervention is effective under ideal experimental circumstances, and often use a placebo or sham comparison. Commonly, pain scales are used to assess the effectiveness of acupuncture or acupressure interventions, especially when evaluating treatments providing 'pain relief'. The most commonly used scale is the visual analogue scale (VAS), which assesses reduction in pain scores out of 10 or 100, in response to the intervention. However, effectiveness trials are designed to assess the effect of the whole therapy in a general population, and are often compared to usual care. When considering the 'working with pain paradigm', the effectiveness of an intervention may be indicated by a reduction of pharmacological pain medication, and satisfaction scores, and may not necessarily be reflected in pain scores (MacPherson 2008).
Description of the intervention
Acupuncture has a long history of use in Asia, including China, Japan, Korea and Taiwan. Traditional Chinese medicine (TCM), with acupuncture as one of the major modalities, describes a state of health maintained by a balance of energy or Qi in the body. Acupuncture performed within the context of TCM is a complex intervention involving not only technical needling skill but development of a therapeutic relationship, formulation of a diagnosis, provision of lifestyle advice, and often administering co‐interventions such as gua sha (scrapping), tuina (massage), moxibustion (a type of Chinese medicine which involves burning a herb close to the skin) or electrical stimulation. In clinical practice, use of co‐interventions is not uncommon although acupuncture is the primary focus. Acupuncture involves the insertion of fine needles into different parts of the body to correct the imbalance of energy in the body. TCM and classical acupuncture explain disease and physiological function based on theoretical concepts of Yin and Yang and the Five Elements (Beinfield 1991; Hicks 2011; Maciocia 2015). Five element acupuncture is based on the classical Chinese medicine texts and has been developed for application in a Western context with different diagnosis and treatment protocols to those used in Asia (Hicks 2011).A Westernised medical application of acupuncture involves the use of acupuncture using trigger points, segmental points and commonly used formula points. Auricular therapy, a form of Western acupuncture, involves the use of the ear to make a diagnosis and subsequent needling to points on the ear. Medical acupuncture may involve the application of acupuncture based on the principles of neurophysiology and anatomy, rather than TCM principles and philosophy. The style and approach of acupuncture characterises the acupuncture point selection and related treatment parameters administered in clinical practice and research.
Acupressure has its origins in early China (Beinfield 1991), and is based on the same paradigm as described for acupuncture. When acupressure is applied, the therapist uses their hands and fingers to activate the same points as applied by acupuncture. Sometimes only a few points need touch applied to alleviate pain, or bring about a feeling of relaxation. In other circumstances a combinations of points will be used to achieve a greater effect. There are several forms of acupressure, which draw on the same knowledge and philosophical system as other forms of traditional Asian medicine. Some of these systems are applied by trained health professionals and others can be applied by the individual by pressing or activating the points.
The use of complementary and alternative medicine (CAM) including acupuncture and acupressure has become popular with consumers worldwide. Studies suggest that between 36% and 62% of adults in industrialised nations use some form of CAM to prevent or treat health‐related problems (Barnes 2004). Complementary therapies are more commonly used by women of reproductive age, with almost half (49%) reporting use (Eisenberg 1998). In a recent Australian study, women were reported to be the highest users of CAM, and that a significant proportion of women are using these therapies during pregnancy (Steel 2014). A review of 14 studies with large sample sizes (N > 200) on the use of CAM in pregnancy identified a prevalence rate ranging from 1% to 87% (with nine falling between 20% and 60%) (Adams 2009). The review identified use of various complementary therapies including acupuncture and acupressure, aromatherapy, massage, yoga, homeopathy and chiropractic care. The review also showed many pregnant women had used more than one complementary product or service (Adams 2009). Many women would like to avoid pharmacological or invasive methods of pain relief in labour and this may contribute towards the popularity of complementary methods of pain management (Steel 2014). A recent Australian study also showed that women and partners who were taught a variety of complementary therapy techniques in an antenatal education class, used between three and four different therapies for pain management during labour (Levett 2016b).
How the intervention might work
Acupuncture has been used to treat a number of painful conditions, and several theories have been presented as to how acupuncture may work. It has been proposed that acupuncture may modify the perception of pain, or alter physiological functions (Stux 1995). Since the majority of acupuncture points are either connected to, or located near neural structures this suggests that acupuncture stimulates the nervous system (Zullo 2017). From a Western acupuncture perspective, points selected are based according to the innervation of the target organ, e.g. the uterus. Activation of muscle afferents at this segmental level transmits signals in the spinal cord and in the central nervous system. During needle stimulation of common acupuncture points for pain, signals are transmitted to the spinal cord, and via afferent pathways to the midbrain. The perception of pain emerges from the resulting flow and integration of this information among specific brain areas via neurochemical and hormonal changes, and may lead to a change in the perception of pain. Another theory suggests that acupuncture stimulates the body to produce endorphins, which reduce pain (Pomeranz 1989). Other pain‐relieving substances called opioids may be released into the body during acupuncture treatment (Ng 1992). Both segmental and central mechanisms of acupuncture are likely to be involved in the total effect of acupuncture (Stener‐Victorin 2006).
In a meta‐analysis by Chae 2013, authors reviewed 28 fMRI (functional magnetic resonance imaging) studies of acupuncture and touch stimulation, and found that acupuncture stimulation showed common patterns of activation and deactivation in the brain, and that touch showed these same patterns, but was not significant. The deactivation patterns seen in the studies correlated with areas of the brain associated with lower pain and anxiety perception, as well as overlapping with the area of the brain known as the ‘pain matrix’ in the brain. Research by Anderson 2012 suggests that acupuncture works by regulating the interaction of the two branches of the autonomic nervous system, sympathetic and parasympathetic.
Why it is important to do this review
There is interest by women to use additional forms of care to assist with their pain management in labour. It is important to examine the efficacy, effectiveness and safety of under‐evaluated forms of treatment to enable women, health providers and policy makers to make informed decisions about care. A number of clinical trials and a review of current reviews (Levett 2014) have been performed to study the efficacy of acupuncture for pain in labour although it remains uncertain whether the existing evidence is rigorous enough to reach a definitive conclusion.
This review is one in a series of Cochrane Reviews examining pain management in labour. An earlier version of this review contributed to an overview of systematic reviews of pain management for women in labour (Jones 2012) and shared a generic protocol (Jones 2011). This review is an update of a review last published in 2011 (Smith 2011b).
Objectives
To examine the effects of acupuncture and acupressure for pain management in labour.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) only. We included studies reported in abstract form if there was sufficient information to permit assessment of risk of bias. Cluster‐trials were eligible for inclusion, but none were identified. Cross‐over trials and quasi‐randomised trials were not eligible for inclusion.
Types of participants
Labouring women either in spontaneous or induced labour, irrespective of parity and pre‐term or post date status. We included studies of women with singleton or multiple pregnancies.
Types of interventions
The previous version of this review (Smith 2011b) contributed to an overview of systematic reviews of interventions for pain management in labour (Jones 2012), and shared a generic protocol (Jones 2011). To avoid duplication, the different methods of pain management were listed in a specific order, from one to 15. Individual reviews focusing on particular interventions included comparisons with only the intervention above it on the list. The list is as follows.
-
Placebo/no treatment
-
Hypnosis (Madden 2016)
-
Biofeedback (Barragán 2011)
-
Intracutaneous or subcutaneous sterile water injection (Derry 2012)
-
Immersion in water (Cluett 2018)
-
Aromatherapy (Smith 2011a)
-
Relaxation techniques (yoga, music, audio) (Smith 2018a)
-
Acupuncture or acupressure (this review)
-
Manual methods (massage, reflexology) (Smith 2018b)
-
Transcutaneous electrical nerve stimulation (TENS) (Dowswell 2009)
-
Inhaled analgesia
-
Opioids (Smith 2018c)
-
Non‐opioid drugs (Othman 2012)
-
Local anaesthetic nerve blocks
-
Epidural (including combined spinal‐epidural) (Anim‐Somuah 2018; Simmons 2012)
Accordingly, this review includes comparisons of any type of acupuncture or acupressure compared with any other type of acupuncture or acupressure, as well as any type of acupuncture or acupressure compared with: 1. placebo/no treatment; 2. hypnosis; 3. biofeedback; 4. intracutaneous or subcutaneous sterile water injection; 5. immersion in water; 6. aromatherapy; 7. relaxation techniques (yoga, music, audio).
Types of outcome measures
Primary outcomes
Effects of interventions
-
Pain intensity (as defined by trialists)
-
Satisfaction with pain relief (as defined by trialists)
-
Sense of control in labour (as defined by trialists)
-
Satisfaction with childbirth experience
-
Use of pharmacological pain relief
Safety of interventions
-
Effect (negative) on mother/baby interaction
-
Breastfeeding (at specified time points)
-
Assisted vaginal birth
-
Caesarean section
-
Side effects (for mother and baby; review specific)
-
Admission to special care baby unit/neonatal intensive care unit (as defined by trialists)
-
Apgar score less than seven at five minutes
-
Poor infant outcomes at long‐term follow‐up (as defined by trialists)
Other outcomes
-
Cost (as defined by trialists)
Secondary outcomes
Maternal
Length of labour; mode of birth; need for augmentation with oxytocin; perineal trauma (defined as episiotomy and incidence of second‐ or third‐degree tear); maternal blood loss (postpartum haemorrhage defined as greater than 500 mL); relaxation; anxiety.
Neonatal
Need for mechanical ventilation; neonatal encephalopathy.
Search methods for identification of studies
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Electronic searches
For this update, we searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (25 February 2019).
The Register is a database containing over 25,000 reports of controlled trials in the field of pregnancy and childbirth. It represents over 30 years of searching. For full current search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link.
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by their Information Specialist and contains trials identified from:
-
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
-
weekly searches of MEDLINE (Ovid);
-
weekly searches of Embase (Ovid);
-
monthly searches of CINAHL (EBSCO);
-
handsearches of 30 journals and the proceedings of major conferences;
-
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results are screened by two people and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set that has been fully accounted for in the relevant review sections (Included studies; Excluded studies; Studies awaiting classification; Ongoing studies).
In addition, we searched the Cochrane Central Register of Controlled Trials (the Cochrane Library 2019, Issue 1), MEDLINE (1966 to 25 Febriuary 2019), and CINAHL (1980 to 25 February 2019) using a combination of subject headings and text words. See Appendix 1.
We also searched ClinicalTrials.gov (25 February 2019) and the WHO International Clinical Trials Registry Platfory (ICTRP) (25 February 2019) for unpublished, planned and ongoing trial reports using the search methods detailed in Appendix 2.
Searching other resources
We searched the reference lists of all included studies.
We did not apply any language or date restrictions.
Data collection and analysis
For methods used in the previous version of this review, seeSmith 2011b.
For this update, the following methods were used for assessing the 79 reports that were identified as a result of the updated search and we also reassessed the five trial reports in the Studies awaiting classification and the two in Ongoing studies sections of Smith 2011b.
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Selection of studies
Two review authors independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion or, if required, we consulted the third review author.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third review author. Data were entered into Review Manager software (RevMan 2014) and checked for accuracy.
When information regarding any of the above was unclear, we contacted authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreement was resolved by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
-
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
-
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
-
unclear risk of bias when it was unclear, or there was insufficient reporting.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
-
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
-
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
-
unclear risk of bias or there was insufficient reporting.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
-
low, high or unclear risk of bias for participants;
-
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
-
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as:
-
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
-
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
-
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
-
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
-
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
-
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). With reference to (1) to (6) above, we planned to assess the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. In future updates, we will explore the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Assessment of the certainty of the evidence using the GRADE approach
For this update, the certainty of the evidence was assessed using the GRADE approach as outlined in the GRADE Handbook in order to assess the certainty of the body of evidence relating to the following outcomes for the main comparisons: acupuncture compared to sham control; acupuncture compared to usual care; acupuncture compared to no treatment; acupuncture compared to water injection; acupressure compared to sham control; acupressure compared to usual care; acupressure compared to combined control.
-
Pain intensity (as defined by trialists)
-
Satisfaction with pain relief (as defined by trialists)
-
Sense of control in labour (as defined by trialists)
-
Satisfaction with childbirth experience
-
Use of pharmacological pain relief
-
Assisted vaginal birth
-
Caesarean section
These outcomes have been included in our 'Summary of findings' tables (summary of findings Table for the main comparison; summary of findings Table 2; summary of findings Table 3; summary of findings Table 4; summary of findings Table 5; summary of findings Table 6; summary of findings Table 7).
We used the GRADEpro Guideline Development Tool to import data from Review Manager 5.3 (RevMan 2014) in order to create 'Summary of findings’ tables. A summary of the intervention effect and a measure of certainty for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the certainty of the body of evidence for each outcome. The evidence can be downgraded from 'high certainty' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Assessment of the quality of the acupuncture intervention delivered
We assessed the quality of the acupuncture or acupressure intervention in published journal articles using the NICMAN scale (Smith 2017). The NICMAN scale was developed to assess the quality of the acupuncture delivered in a clinical trial, and is designed to be used in combination with the STRICTA reporting guidelines (MacPherson 2010). This scale assesses and scores the following: the rationale behind the point selection, the qualifications and experience of the practitioner delivering the intervention, the adequacy of the number of treatment sessions, and the reporting of vital components of the acupuncture practice itself such as needle depth, diameter and stimulation. Higher scores indicate improved quality of the acupuncture intervention delivered, but there is no cut‐off for a 'high' versus 'low' quality score on the NICMAN scale. Each trial was independently scored out of 23 by two review authors (CS, KL, MA). Any discrepancies were resolved by discussion. If this was not reached a third review author (KL, CS or MA) decided on the final score.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
We used the mean difference if outcomes were measured in the same way between trials. We used the standardised mean difference to combine trials that measured the same outcome, but used different methods.
Unit of analysis issues
Cluster‐randomised trials
If we had identified cluster‐randomised trials, we planned to include them in the analyses along with individually‐randomised trials. If such trials are identified in future updates of the review, we will adjust their sample sizes using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions using an estimate of the intra‐cluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely. We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation unit.
Cross‐over trials
Cross‐over trials are not a suitable design for trials looking at interventions in labour and have been excluded.
Other unit of analysis issues
If we had identified trials with multiple arms, we planned that data from both treatment arms would be combined into one group. For studies with a sham control and no treatment control group, the shared intervention was divided evenly between groups and the weighting adjusted as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Dealing with missing data
For included studies, levels of attrition were noted. In future updates, if more eligible studies are included, the impact of including studies with high levels of missing data in the overall assessment of treatment effect will be explored by using sensitivity analysis.
For all outcomes, analyses were carried out, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if the I² was greater than 30% and either the Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. In future updates, if we identify substantial heterogeneity (above 30%), we plan to explore it by pre‐specified subgroup analysis.
Assessment of reporting biases
In future updates, if there are 10 or more studies in the meta‐analysis we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar.
If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary was treated as the average range of possible treatment effects and we discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we did not combine trials. Where we used random‐effects analyses, the results were presented as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
Had we identified substantial heterogeneity, we planned to investigate it using subgroup analyses and sensitivity analyses. However, there were too few data included in any one comparison to carry out meaningful subgroup analysis.
In future updates, if possible we will carry out the following subgroup analyses for primary outcomes.
-
Spontaneous labour versus induced labour
-
Nulliparous versus multiparous
-
Term versus preterm
-
Continuous support in labour versus no continuous support
We will assess subgroup differences by interaction tests available within RevMan. We will report the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
We did carry out subgroup analysis by type of acupuncture: manual acupuncture versus electro‐acupuncture, but there was not enough data in any one subgroup to demonstrate any differential effects.
Sensitivity analysis
Where subgroup analysis failed to explain the heterogeneity, we planned to analyse the data using the random‐effects model. A priori, we planned to perform sensitivity analyses on results to look at the possible contribution of: (1) differences in methodological quality, with trials of high quality (low risk of bias) compared to all trials; and (2) publication bias by country. If publication bias was present we planned to undertake a sensitivity analysis excluding trials from countries where there was a greater publication bias.
Results
Description of studies
Results of the search
See Figure 1.

Study flow diagram.
For this update, we assessed 165 new records from the search. We also reassessed five studies that were awaiting classification and three ongoing studies from the previous version of the review. We had 112 records after removal of duplicates. From these, we screened out 33, leaving us with 79 trial reports to assess. Of these, we included 17 new studies (30 reports), added an additional report to an already included study, and excluded 26 (29 reports) Fifteen new studies are awaiting further classification (Studies awaiting classification) and three are ongoing (Ongoing studies).
One study (Ziaei 2006) had been previously included in a previous update (Smith 2011b). In this update it was moved to Studies awaiting classification due to having an unclear risk of bias across all domains and the authors had not responded to requests for further information.
The review included 28 trials of 3960 women, with data contributing to data and analysis from 27 trials of 3930 women.
Included studies
Study design
All studies were parallel design. Eleven studies had two groups (Calik 2014; Hamidzadeh 2012; Hamlaci 2017; Hantoushzadeh 2007; Kashanian 2010; Lee 2004; Martensson 2008; Nesheim 2003; Sehhatie‐Shafaie 2013; Skilnand 2002; Tjung 2008). Fourteen studies had three groups (Borup 2009; Chung 2003; Dabiri 2014; Dong 2015; Hjelmstedt 2010; Kordi 2010; Ma 2011; Mafetoni 2016; Mafetoni 2016a; Mansouri 2018; Ozgoli 2016; Qu 2007; Salehian 2011; Vixner 2014), and three studies had four arms (Huang 2008; Mackenzie 2011; Ramnero 2002). Comparative and control groups varied. Thirteen studies used placebo or sham controls (Chung 2003; Dabiri 2014; Hantoushzadeh 2007; Hjelmstedt 2010; Kashanian 2010; Kordi 2010; Lee 2004; Ma 2011; Mackenzie 2011; Mafetoni 2016; Skilnand 2002; Sehhatie‐Shafaie 2013; Skilnand 2002). Placebo, sham, or minimal acupuncture techniques varied between invasive and non‐invasive techniques. Comparison with usual care comprised of medication used in four studies (Borup 2009; Huang 2008; Tjung 2008; Vixner 2014). Other control groups included unspecified care or usual care in five studies (Dong 2015; Hjelmstedt 2010; Mafetoni 2016a; Nesheim 2003; Ramnero 2002). Huang 2008 used transcutaneous electrical nerve stimulation (TENS) and a breathing group; Martensson 2008 used sterile water injections, and comparison with no intervention was reported in two studies (Calik 2014; Qu 2007). Ozgoli 2016 used two active groups and a usual care group.
Sample sizes
Studies included in the review had sample sizes ranging from 30 (Mafetoni 2016a) to 607 (Borup 2009).
Study location and sources of women
Nine studies were undertaken in Iran (Dabiri 2014; Hamidzadeh 2012; Hantoushzadeh 2007; Kashanian 2010; Kordi 2010; Mansouri 2018; Ozgoli 2016; Salehian 2011; Sehhatie‐Shafaie 2013), four studies were undertaken in China (Dong 2015; Huang 2008; Ma 2011; Qu 2007), three studies undertaken in Sweden (Martensson 2008; Ramnero 2002; Vixner 2014), two each in Norway (Nesheim 2003; Skilnand 2002), Brazil (Mafetoni 2016; Mafetoni 2016a), and Turkey (Calik 2014; Hamlaci 2017), and one study each in Denmark (Borup 2009), India (Hjelmstedt 2010), Korea (Lee 2004) Phillipines (Tjung 2008); Taiwan (Chung 2003) and the UK (Mackenzie 2011).
Participants
Seventeen studies recruited both nulliparous and multiparous women (Borup 2009; Chung 2003; Dabiri 2014; Dong 2015; Hamidzadeh 2012; Hamlaci 2017; Kordi 2010; Lee 2004; Ma 2011; Mafetoni 2016; Mafetoni 2016a; Martensson 2008; Nesheim 2003; Ramnero 2002; Sehhatie‐Shafaie 2013; Skilnand 2002; Vixner 2014). Nulliparous only women were recruited in eight studies (Calik 2014; Hantoushzadeh 2007; Hjelmstedt 2010; Kashanian 2010; Mackenzie 2011; Mansouri 2018; Ozgoli 2016; Salehian 2011). Parous women only were recruited in two studies (Huang 2008; Qu 2007). It was unclear in one study (Tjung 2008). Women were recruited in spontaneous labour in 19 studies (Calik 2014; Chung 2003; Dabiri 2014; Hamidzadeh 2012; Hamlaci 2017; Hantoushzadeh 2007; Kordi 2010; Mafetoni 2016; Mafetoni 2016a; Martensson 2008; Mansouri 2018; Nesheim 2003; Ozgoli 2016; Qu 2007; Ramnero 2002; Sehhatie‐Shafaie 2013; Skilnand 2002; Tjung 2008; Vixner 2014). Two studies recruited women in both spontaneous and induced labour (Borup 2009; Hjelmstedt 2010), and one study reported on only induced labour (Mackenzie 2011). Reporting on the onset of labour was unclear in six studies (Dong 2015; Huang 2008; Kashanian 2010; Lee 2004; Ma 2011; Salehian 2011).
The intervention was administered at term for the majority of trials studies except Huang 2008 where details were not reported. There were no studies specifically for pre‐term labour.
We included labouring women either in spontaneous or induced labour, irrespective of parity and pre‐term or post date status. We included women with singleton or multiple pregnancies.
Types of intervention
Fifteen studies used acupressure (Calik 2014; Chung 2003; Dabiri 2014; Hamidzadeh 2012; Hamlaci 2017; Hjelmstedt 2010; Kashanian 2010; Kordi 2010; Lee 2004; Mafetoni 2016; Mafetoni 2016a; Mansouri 2018; Ozgoli 2016; Salehian 2011; Sehhatie‐Shafaie 2013) and 13 studies used acupuncture (Borup 2009; Dong 2015; Hantoushzadeh 2007; Huang 2008; Ma 2011; Mackenzie 2011; Martensson 2008; Nesheim 2003; Qu 2007; Ramnero 2002; Skilnand 2002; Tjung 2008; Vixner 2014) (includes manual and electro‐acupuncture). Acupuncture and acupressure varied in point selection, frequency of treatment and number of treatments, with commonly used points included SP6, LI4, BL23, BL32, HT7, GB34, LR3, ST36, PC6, BL67. A fixed set of acupuncture points only were administered in four studies (Dong 2015; Ma 2011; Mackenzie 2011; Qu 2007). A fixed set of acupressure points was used in 15 studies (Calik 2014; Chung 2003; Dabiri 2014; Hamidzadeh 2012; Hamlaci 2017; Hjelmstedt 2010; Kashanian 2010; Kordi 2010; Lee 2004; Mafetoni 2016; Mafetoni 2016a; Mansouri 2018; Ozgoli 2016; Salehian 2011; Sehhatie‐Shafaie 2013). Individualised treatment was administered in eight studies (Borup 2009; Hantoushzadeh 2007; Huang 2008; Martensson 2008; Nesheim 2003; Ramnero 2002; Skilnand 2002; Vixner 2014). Auriculotherapy, ear acupressure was used in one trial (Mafetoni 2016a). SeeCharacteristics of included studies.
Outcome measures
Pain intensity during labour was measured by visual analogue scale (VAS) in 25 studies (Borup 2009; Calik 2014; Chung 2003; Dabiri 2014; Dong 2015; Hamidzadeh 2012; Hamlaci 2017; Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Kashanian 2010; Kordi 2010; Lee 2004; Ma 2011; Mackenzie 2011; Mafetoni 2016; Mafetoni 2016a; Martensson 2008; Mansouri 2018; Nesheim 2003; Salehian 2011; Sehhatie‐Shafaie 2013; Skilnand 2002; Tjung 2008;Vixner 2014) and by a 0 to 10 numeric rating scale (NRS) in three studies (Ozgoli 2016; Qu 2007; Ramnero 2002). Two studies (Calik 2014; Vixner 2014) did not report pain intensity outcome data in a format that allowed them to be included in the meta‐analysis, so these were reported narratively. When pain intensity scores were given at multiple time points, the last time point was used. Standardised mean difference (SMD) was used when combining VAS and NRS pain scores. Use of pharmacological analgesia was reported by 26 studies.
Length of labour was reported in eight studies (Dong 2015; Hamidzadeh 2012; Hamlaci 2017; Kashanian 2010; Lee 2004; Ma 2011; Salehian 2011; Vixner 2014), and mode of birth (spontaneous vaginal birth, assisted vaginal birth or caesarean section) was reported by 16 studies (Borup 2009; Calik 2014; Hamidzadeh 2012; Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Kashanian 2010; Mackenzie 2011; Martensson 2008; Mafetoni 2016a; Nesheim 2003; Ozgoli 2016; Ramnero 2002; Skilnand 2002; Tjung 2008; Vixner 2014). Maternal outcomes (satisfaction, sense of control, anxiety, childbirth experience and acceptability of the intervention) were reported in 12 studies (Borup 2009; Chung 2003; Hamidzadeh 2012; Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Lee 2004; Martensson 2008; Ozgoli 2016; Qu 2007; Ramnero 2002; Vixner 2014), and clinical outcomes were reported in the majority of studies, however some are reported narratively as they were presented in a format that was not consistent with the review (Qu 2007).
Satisfaction with pain relief or satisfaction with childbirth was reported either via a Likert scale or via a Yes/No response to a question relating to sufficient pain relief. To provide a dichotomous outcome for satisfaction when recorded via a Likert scale we combined the two most favourable categories (e.g. very satisfied and satisfied or very good and good) as a 'Yes' response, while neutral or negative categories were characterised as a 'No' response.
Dates of trials
The majority of the trials took place between the year 1999 to 2013: Borup 2009 (2002‐2004), Calik 2014 (2009‐2010), Dabiri 2014 (2011‐2012), Dong 2015 (2012‐2013), Hamidzadeh 2012 (2006), Hamlaci 2017 (2012), Hantoushzadeh 2007 (2005), Hjelmstedt 2010 (2007‐2008), Huang 2008 (2004‐2005), Kashanian 2010 (2007), Lee 2004 (2002), Mackenzie 2011 (2005‐2009), Mafetoni 2016 (2013), Ozgoli 2016 (2008), Qu 2007 (2004‐2005), Ramnero 2002 (1999‐2000), Salehian 2011 (2008‐2009), Sehhatie‐Shafaie 2013 (2012), Skilnand 2002 (1998‐1999), Vixner 2014 (2008‐2011), Mansouri 2018 (2017), Tjung 2008 (2007‐2008). Five studies did not report the study duration (Chung 2003; Kordi 2010; Ma 2011; Martensson 2008; Nesheim 2003).
Funding
Twelve studies reported funding sources. Borup 2009 was funded by the Asse and Ejnar Danielsen's Foundation, Kgs, Lyngby, Dnemark; Knowledge and Research Cener for Alternative medicine, Aarhus, Denmark; Sophus Jacobsen Foundation, Capenhagen, Denmar; The Danish Midwifery Organisation, Copenhangen, Denmark; Lundbeck Foundation, Copenhagen, Denmark; Mads Clausens Foundation, Nordborg, Denmark; Hede Nielsen Foundation, Horsens, Denmark; The Research Fund at Aarhus University Hosptial, Aarhus, Denmark; Else and Mogens Wedell‐Wedellsborgs Foundation, Copenhagen, Denmark; and King Christian the 10th Foundation, Copenhagen, Denmark; Hantoushzadeh 2007 was funded by the Vali Asr Research Centre for Reproductive Health; Hjelmstedt 2010 was funded by Osher Center for Integrative Medicine, Karolinska Institutet and the Centre for Health Care Science, Karolinska Institutet; Huang 2008 was funded by the National Traditional Chinese Medicine Administration of Traditional Chinese Medicine Science and Techology Research Special TCM Clinical Research Fund (04‐05LQ04); Kashanian 2010 was funded by Iran University of Medical Sciences; Ma 2011 was funded by the State Administration of Traditional Chinese Medicine; National Science Foundation of China; and E‐institutes of Shanghai Municipal Education Commission. Mackenzie 2011 was funded by a grant from the Oxfordshire Health Services Research Committee and the Uterine Contractility Trust fund, held by the Oxford Radcliffe NHS Trust. Martensson 2008 was funded by grants from Skaraborg Institute for Reseach and Development, Barnets, Lychopenning, The Swedish Association of Midwives, Hegu Svenska AB and the University of Skövde; Qu 2007 was funded by the Innovation Research Foundation by government of Heilongjiang Privince, China; Ramnero 2002 was funded by grants from Örebro Council Research Committee and Centre for Nursing Science, Örebro University Hospital; Sehhatie‐Shafaie 2013 was funded by Tabriz University of Medical Sciences. Vixner 2014 was funded by grants from the Centre for Clinical Research Dalarna, Karolinska Institutet, Uppsala‐Örebro Regional Research Council, University of Skövde, FOU Fyrbodal, Magnus Bergvall. Stiftelse, and Dalarna University, Sweden.
Declarations of interest
Seven studies reported no conflict of interest (Hjelmstedt 2010; Ma 2011; Mackenzie 2011; Mansouri 2018; Ozgoli 2016; Sehhatie‐Shafaie 2013; Vixner 2014). One study (Mackenzie 2011) stated that one trial author provides legal opinion on litigation cases. In the remaining 21 studies, there was no clear conflict of interest reported.
Quality of acupuncture
All 15 studies of acupuncture were assessed using the NICMAN Scale (Smith 2017). The NICMAN Scale uses an 11‐item scale to review the quality of acupuncture studies. We now include this and report on studies of acupuncture using this scale. The items include: clear description of the population; intervention; comparator; outcome; appropriateness of study design for question; inclusion of a differential diagnosis; selection of acupuncture points consistent with treatment principles; description of needles, needling depth, stimulation, and sensation; point location description and justification according to texts; treatments administered; and the qualifications of the person administering the treatments (Table 1).
| Study ID | Total NICMAN Score | P | I | C | O | Study design | Differential diagnosis | Point selection | Needling parameters | Acupuncture point location | Treatment dosage | Therapist qualifications |
| Borup 2009 | 19 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 1 | 1 | 2 | 2 |
| Dong 2015 | 15 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 1 | 2 | 0 |
| Hantoushzadeh 2007 | 20 | 2 | 2 | 2 | 2 | 3 | 1 | 2 | 2 | 2 | 2 | 0 |
| Huang 2008 | 16 | 2 | 2 | 2 | 2 | 3 | 2 | 2 | 0 | 0 | 1 | 0 |
| Ma 2011 | 17 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 2 | 0 |
| MacKenzie 2011 | 19 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 1 | 2 | 1 | 2 |
| Martensson 2008 | 16 | 2 | 2 | 2 | 2 | 3 | 0 | 1 | 1 | 0 | 2 | 1 |
| Nesheim 2003 | 16 | 2 | 2 | 2 | 2 | 3 | 2 | 0 | 2 | 0 | 1 | 0 |
| Qu 2007 | 13 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 0 | 1 | 0 |
| Ramnero 2002 | 17 | 2 | 2 | 2 | 2 | 3 | 1 | 1 | 1 | 2 | 1 | 0 |
| Skilnand 2002 | 18 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 1 | 0 |
| Tjung 2008 | 17 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 2 | 1 | 2 |
| Vixner 2014 | 18 | 2 | 2 | 2 | 2 | 3 | 1 | 2 | 1 | 2 | 1 | 0 |
The studies that ranked the highest on the NICMAN Scale were Borup 2009 and Mackenzie 2011, each with a score of 90.5%. The study that ranked the lowest was Mansouri 2018 with a score of 47%. The other studies received scores between these figures: Hantoushzadeh 2007 received a score of 87.0%; Ma 2011 scored 81%; Ramnero 2002 scored 74%; Skilnand 2002 and Vixner 2014 both scored 78.3%. Dong 2015 received a score of 71.4%, and Huang 2008, Martensson 2008 and Nesheim 2003 each scored 70.0%.
In reviewing individual items on the NICMAN Scale, all studies scored at the highest level (2 out of 2 or 3 out of 3) for reporting of clear description of the population; intervention; comparator; outcome; and appropriateness of study design for question. Seven studies reported on the inclusion of a differential diagnosis, and scored 2 (Huang 2008; Nesheim 2003), 1 (Hantoushzadeh 2007; Skilnand 2002; Vixner 2014) or 0 (Martensson 2008; Skilnand 2002) for selection and justification of acupuncture points consistent with treatment principles, seven studies scored 2 (Borup 2009; Hantoushzadeh 2007; Huang 2008; Ma 2011; Mackenzie 2011; Skilnand 2002; Vixner 2014), two studies scored 1 (Martensson 2008; Ramnero 2002) and three studies scored 0 (Dong 2015; Nesheim 2003; Qu 2007; for description and justification of needles type and consistency, needling depth, stimulation and justification, and sensation, four studies scored 2 (Hantoushzadeh 2007; Ma 2011; Nesheim 2003; Skilnand 2002), eight studies scored 1 (Borup 2009; Dong 2015; Mackenzie 2011; Martensson 2008; Qu 2007; Ramnero 2002; Tjung 2008; Vixner 2014), and two studies scored 0 (Huang 2008; Mansouri 2018); for reporting of point location description and justification according to texts, seven studies scored 2 (Hantoushzadeh 2007; Ma 2011; Mackenzie 2011; Ramnero 2002; Skilnand 2002; Tjung 2008; Vixner 2014), two scored 1 (Borup 2009; Dong 2015) and five scored 0 (Huang 2008; Martensson 2008; Mansouri 2018; Nesheim 2003; Qu 2007; with regard to reporting of treatments administered during labour and justified, five scored 2 Borup 2009; Dong 2015; Hantoushzadeh 2007; Ma 2011; Martensson 2008), nine scored 1 (Huang 2008; Mackenzie 2011; Mansouri 2018; Nesheim 2003; Qu 2007; Ramnero 2002; Skilnand 2002; Tjung 2008; Vixner 2014), and none scored 0; and for qualifications of the person administering the treatments meeting World Health Organization guidelines (generally a member of a recognised acupuncture association or > 200 hours training), three studies scored 2 (Borup 2009; Mackenzie 2011; Tjung 2008), one study scored 1 (Martensson 2008), and the remainder scored 0 (Dong 2015; Hantoushzadeh 2007; Huang 2008; Ma 2011; Mansouri 2018; Nesheim 2003; Qu 2007; Ramnero 2002; Skilnand 2002; Vixner 2014).
Excluded studies
We excluded 34 trials;seeCharacteristics of excluded studies. Many studies did not meet the inclusion criteria based on the criteria for interventions: for example, the use of point injection therapy (Zhang 2000), or ice massage (Hajiamini 2012; Kaviani 2012). We excluded eight studies due to insufficient reporting of randomisation (Aghdam 2012; Bo 2006; Deepak 2013; Li 2006; Peng 2010; Ternov 1998; Wang 1994; Zhu 2013), and we were unable to ascertain true randomisation status from the author. The study design was unclear or did not meet the criteria for inclusion in seven studies (Deen 1985; Kermani 2015; Levett 2016a; Mucuk 2014; Sebastian 2014; Vixner 2017; Wu 2017). No clinically relevant outcomes were measured in nine trials (Asadi 2015; Can 2015; Li 1996; Mollart 2013; Moradi 2014; Nistler 2010; Shalev 1991; Shang 1995). One study was reported as an abstract only, with insufficient reporting to determine inclusion (Park 2003). Seven studies did not assess pain in labour (Alsharnoubi 2015; Haghighi 2016; Liu 2012; Liu 2015a; Liu 2015b; Masoudi 2014; Samadi 2018).
Risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreements by discussion or by involving another review author.
SeeFigure 2 and Figure 3 for a graphical summary of the 'Risk of bias' assessments by authors of the included studies based on the six risk of bias domains. No study was at a low risk of bias on all domains.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
Method of allocation
All trials were assessed in terms of methods by which participants were allocation to intervention and control or sham groups. Seventeen trials reported the sequence was computer generated (Borup 2009; Calik 2014; Hamidzadeh 2012; Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Kashanian 2010; Kordi 2010; Ma 2011; Mackenzie 2011; Mafetoni 2016; Martensson 2008; Nesheim 2003; Ozgoli 2016; Salehian 2011; Sehhatie‐Shafaie 2013; Vixner 2014). The sequence was by lot drawing in six trials (Dabiri 2014; Dong 2015; Hamlaci 2017; Qu 2007; Skilnand 2002; Tjung 2008), coin tossing in one trial (Chung 2003), random number tables in one trial (Lee 2004), and shuffling cards in one trial (Ramnero 2002). The method of allocation generation was unclear in two studies (Mansouri 2018; Mafetoni 2016a).
Allocation concealment
Following adequate allocation to groups, allocation concealment was assessed for all studies. We assessed the methods used to prevent investigators' foreknowledge of group allocation, from evidence from the studies, extracted independently by two review authors. Where it was unclear, or not reported, we contacted the study author for clarification. Allocation concealment was described as low risk in 17 trials. Sealed envelopes were used in 15 trials (Calik 2014; Dabiri 2014; Hamlaci 2017; Hantoushzadeh 2007; Hjelmstedt 2010; Kashanian 2010; Mackenzie 2011; Martensson 2008; Mafetoni 2016a; Mansouri 2018; Nesheim 2003; Ramnero 2002; Salehian 2011; Skilnand 2002; Vixner 2014), central randomisation in one trial (Borup 2009) and sequential numbers in one trial (Chung 2003). One trial was at high risk due to no concealment (Ozgoli 2016). Ten trials were assessed at unclear risk in nine trials mainly due to method of concealment not being described (Dong 2015; Hamidzadeh 2012; Huang 2008; Kordi 2010; Lee 2004; Ma 2011; Mafetoni 2016; Qu 2007; Sehhatie‐Shafaie 2013; Tjung 2008).
Blinding
Blinding of participants and personnel (performance bias)
Participants (both participants and personnel) were largely aware of whether they had been assigned to acupuncture or acupressure or control. Some studies included sham controls, in an attempt to blind participants. Five trials were assessed at a low risk of bias (Lee 2004; Mafetoni 2016;Mafetoni 2016a; Sehhatie‐Shafaie 2013; Skilnand 2002). Blinding was assessed at high risk in 17 trials (Borup 2009, Calik 2014, Dabiri 2014; Dong 2015; Hamidzadeh 2012; Hamlaci 2017; Huang 2008; Kordi 2010; Ma 2011; Mackenzie 2011; Martensson 2008; Nesheim 2003; Ozgoli 2016; Qu 2007; Salehian 2011; Tjung 2008; Vixner 2014). The risk of blinding was unclear in six trials due to poor reporting (Chung 2003; Hantoushzadeh 2007; Hjelmstedt 2010; Kashanian 2010; Mansouri 2018; Ramnero 2002). We contacted study authors to clarify where possible.
Blinding of outcome assessment
We rated trials as having low risk of bias when researchers described blinded assessment of outcomes. Blinding was assessed at high risk, that is, assessment was largely done by the investigator, in seven trials (Borup 2009; Calik 2014; Dong 2015; Hamlaci 2017; Kordi 2010; Ozgoli 2016; Vixner 2014); 11 trials were at a low risk of bias, where assessment was performed by an independent person (Dabiri 2014; Hamidzadeh 2012; Hantoushzadeh 2007; Hjelmstedt 2010; Kashanian 2010; Lee 2004; Mackenzie 2011; Mafetoni 2016; Mafetoni 2016a; Mansouri 2018; Tjung 2008). Ten studies were at unclear risk of bias due to lack of reporting (Chung 2003; Huang 2008; Ma 2011; Martensson 2008; Nesheim 2003; Qu 2007; Ramnero 2002; Salehian 2011; Sehhatie‐Shafaie 2013; Skilnand 2002).
Incomplete outcome data
Outcome reporting, and risk of attrition, was assessed at a low risk of bias in 16 trials (Borup 2009; Chung 2003; Dabiri 2014; Dong 2015; Hamidzadeh 2012; Hamlaci 2017; Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Mansouri 2018; Martensson 2008;; Ozgoli 2016; Qu 2007; Ramnero 2002; Salehian 2011; Skilnand 2002), where missing data were clearly accounted for and dropout rates were low. Nine trials were at unclear risk (Kashanian 2010; Kordi 2010; Lee 2004; Ma 2011; Mackenzie 2011; Mafetoni 2016; Sehhatie‐Shafaie 2013; Tjung 2008; Vixner 2014), and three trials were assessed at high risk (Calik 2014; Mafetoni 2016a; Nesheim 2003) due to imbalance in dropout between groups and high attrition.
Selective reporting
Every effort was made to minimise the impact of reporting biases by undertaking comprehensive searches of multiple sources to identify unpublished material including protocols of randomised trials in English and Chinese. Although the study protocol was not available for most of the included studies, many showed consistency between results and methods sections. However, the risk of bias from selective reporting was determined to be unclear in 23 trials due to the absence of a study protocol, except for two trials assessed at low risk (Sehhatie‐Shafaie 2013; Vixner 2014).
Other potential sources of bias
The risk of bias from other sources of bias was rated as high risk in three trials due to lower pain scores in the control group prior to the commencement of the intervention, (Hantoushzadeh 2007); significant difference in baseline characteristics between groups (Hjelmstedt 2010; Skilnand 2002). Fifteen trials were assessed at, low risk (Borup 2009; Chung 2003; Hamlaci 2017; Kashanian 2010; Lee 2004; Mackenzie 2011; Mafetoni 2016a; Mansouri 2018; Martensson 2008; Nesheim 2003; Ozgoli 2016; Qu 2007; Ramnero 2002; Sehhatie‐Shafaie 2013; Tjung 2008) and unclear reporting in nine trials (Calik 2014; Dabiri 2014; Dong 2015; Hamidzadeh 2012; Huang 2008; Kordi 2010; Ma 2011; Mafetoni 2016; Salehian 2011; Vixner 2014).
Effects of interventions
See: Summary of findings for the main comparison Acupuncture compared to sham control for pain management in labour; Summary of findings 2 Acupuncture compared to usual care for pain management in labour; Summary of findings 3 Acupuncture compared to no treatment for pain management in labour; Summary of findings 4 Acupuncture compared to water injection for pain management in labour; Summary of findings 5 Acupressure compared to sham control for pain management in labour; Summary of findings 6 Acupressure compared to usual care for pain management in labour; Summary of findings 7 Acupressure compared to combined control for pain management in labour
This review included 27 trials of 3930 women in the meta‐analysis.
Data were not reported in a form that could be included in the meta‐analysis from Qu 2007 study and results are reported descriptively.
1) Acupuncture versus sham control
Five trials with 642 women reported on this comparison. No trial reported on the primary outcomes of: sense of control in labour, satisfaction with childbirth.
Primary outcomes
1.1) Outcome: pain intensity
Two trials assessed pain along a visual analogue scale (VAS) scale, a lower score indicated less pain. Data on this outcome were available from two trials and 325 women, (Analysis 1.1). Due to significant heterogeneity a random‐effects model was applied. Acupuncture may have little effect on reducing the intensity of pain felt by women when compared with sham acupuncture, (mean difference (MD) ‐4.42, 95% confidence interval (CI) ‐12.94 to 4.09, low‐certainty evidence).
1.2) Outcome: satisfaction with pain relief in labour
Satisfaction was assessed using a four‐point rating scale from very good to weak. Acupuncture probably improves satisfaction with pain relief in labour compared with control, (risk ratio (RR) 2.38, 95% CI 1.78 to 3.19, 1 trial, 150 women, moderate‐certainty evidence; Analysis 1.2).
1.3) Outcome: use of pharmacological analgesia
There was evidence of reduced use of pharmacological analgesia from manual acupuncture (RR 0.75, 95% CI 0.63 to 0.89, 2 trials, 261 women, moderate‐certainty evidence; Analysis 1.3).
1.4) Outcome: assisted vaginal birth
It is uncertain whether manual acupuncture reduces assisted vaginal birth when compared with sham acupuncture because the certainty of the evidence was found to be very low, with concerns due to imprecision, inconsistency of results and study limitations (RR 1.10, 95% CI 0.41 to 2.97, 2 trials, 261 women, very low‐certainty evidence), there was substantial heterogeneity I2 72% and a random‐effects model was applied; Analysis 1.4).
1.5) Outcome: caesarean section
There was no evidence of an effect for acupuncture in reducing caesarean section when compared with sham acupuncture (RR 1.11, 95% CI 0.49 to 2.48, 3 trials, 411 women, low‐certainty evidence;Analysis 1.5).
1.6) Outcome: Apgar score less than seven at five minutes
Two trials reported on this outcome. In the Mackenzie 2011 trial there were no babies with an Apgar score less than seven at five minutes. Skilnand 2002 reported on one event in the control group. The results are therefore unclear with so little data being provided for this outcome.
Secondary outcomes
1.7) Outcome: length of labour
The findings do not tell us whether acupuncture reduces the length of labour when compared with a sham control because the evidence was assessed to be of low certainty (MD ‐37.41 minutes, 95% CI ‐96.37 to 21.55; 1 trial, 175 women; Analysis 1.7).
1.8) Outcome: spontaneous vaginal birth
There was no evidence of an effect for acupuncture in increasing spontaneous vaginal birth when compared with sham acupuncture based on low‐certainty evidence (average RR 0.98, 95% CI 0.86 to 1.12, 3 trials, 411 women). There was significant heterogeneity between trials I2 = 64% and a random‐effects model was applied (Analysis 1.8).
1.9) Outcome: augmentation with oxytocin
There was significant heterogeneity between trials and so the results from the studies were not combined. The trial by Skilnand 2002 found reduced augmentation with synthetic oxytocin in the acupuncture group (RR 0.40, 95% CI 0.23 to 0.69), Hantoushzadeh 2007 found no evidence of a difference between groups (RR 0.93, 95% CI 0.85 to 1.02). The heterogeneity maybe explained by the length of time that the intervention was delivered which varied from two hours and until the time of delivery.
Subgroup analysis
There were not enough data relating to manual or electro‐acupuncture to demonstrate any differential effect according to type of acupuncture.
2) Acupuncture versus usual care
Ten trials with 1622 women had data suitable for inclusion in the meta‐analysis. One study (Vixner 2014) has outcomes reported narratively. No trial reported on the primary outcomes of: sense of control in labour, satisfaction with childbirth.
Primary outcomes
2.1) Outcome: pain intensity
Four trials, 495 women reported on this outcome (Analysis 2.1). Pain intensity was assessed with VAS or numeric rating scale (NRS): lower scores indicate less pain.
We are uncertain if acupuncture reduces the pain intensity when compared with the control, there was significant heterogeneity and a random‐effects model was applied and the evidence was assessed as being very low certainty (standardised mean difference (SMD) ‐1.31, 95% CI ‐2.14 to ‐0.49, I2 = 93%, very low‐certainty evidence).
Vixner 2014 found that there were no differences between acupuncture groups (manual or electro acupuncture) and usual care when a simple non‐interaction model was used. When an interaction model was used there was evidence of an interaction between time and treatment group (P = 0.03), at 120 minutes manual acupuncture had lower pain scores than electro acupuncture, at 270 minutes manual acupuncture had lower pain scores than electro acupuncture and at 360 minutes usual care had lower pain scores than manual acupuncture.
2.2) Outcome: satisfaction with pain relief in labour
Two trials reported on this outcome assessed as the number who self reported satisfaction with pain relief.
Manual or electro acupuncture may have little effect on satisfaction with pain relief during labour (RR 1.07, 95% CI 0.96 to 1.20, 343 women, low‐certainty evidence; Analysis 2.2).
2.3) Outcome: use of pharmacological analgesia
Six trials and 1059 women reported on this outcome (Analysis 2.3). The findings do not tell us whether acupuncture may reduce use of pharmacological analgesia compared to a control because the evidence was assessed as very low certainty (average RR 0.72, 95% CI 0.60 to 0.85), there was significant heterogeneity (I2 = 70%) and a random‐effects analysis was undertaken.
2.4) Outcome: assisted vaginal birth
Six trials and 1217 women reported on this outcome. Acupuncture may make little difference to reducing assisted vaginal birth (RR 0.93, 95% CI 0.70 to 1.24, low‐certainty evidence;Analysis 2.4) (manual acupuncture (RR 0.87, 95% CI 0.64 to 1.17, 6 trials, 1089 women) or electro‐acupuncture (RR 1.60, 95% CI 0.64 to 4.04, 1 trial, 128 women).
2.5) Outcome: caesarean section
Five trials and 861 women reported on caesarean section. Acupuncture may make little difference to reducing caesarean section (RR 0.72, 95% CI 0.47 to 1.09, low‐certainty evidence; Analysis 2.5) (manual acupuncture (RR 0.78, 95% CI 0.50 to 1.24, 4 trials, 683 women), electro‐acupuncture (RR 0.46, 95% CI 0.16 to 1.28, 2 trials 178 women).
2.6) Outcome: Apgar score less than seven at five minutes
Six trials, 1061 women reported on this outcome. There was no evidence of harm from acupuncture (RR 0.99, 95% CI 0.28 to 3.47, very low‐certainty evidence; Analysis 2.6).
Secondary outcomes
2.7) Outcome: length of labour
Acupuncture may make no difference to reducing the length of labour in minutes (MD ‐13.89, 95% CI ‐28.93, 1.14, 3 trials, 608 women; Analysis 2.7), (manual acupuncture (MD 4.00, 95% CI ‐142.47 to 150.47, 1 trial, 124 women); electro‐acupuncture (MD ‐14.08, 95% CI ‐29.20 to 1.03, 3 trials, 484 women)).
2.8) Outcome: spontaneous vaginal birth
Four trials and 449 women reported on this outcome. Acupuncture probably makes little difference to rates of spontaneous vaginal birth (RR 0.98, 95% CI 0.89 to 1.08; Analysis 2.8), manual acupuncture (RR 0.96, 95% CI 0.85 to 1.10, 3 trials, 271 women), electro‐acupuncture (RR 0.99, 95% CI 0.86 to 1.14, 2 trials, 178 women).
2.9) Outcome: augmentation with oxytocin
Four trials and 813 women reported on this outcome. Acupuncture probably makes little difference to rates of augmentation compared with the control (RR 0.88, 95% CI 0.77 to 1.02; Analysis 2.9), manual acupuncture (RR 0.92, 95% CI 0.78 to 1.09, 3 trials, 635 women), electro‐acupuncture (RR 0.78, 95% CI 0.59 to 1.03, 2 trials, 178 women), although the CIs cross one and so a possible increase cannot be ruled out.
2.10) Outcome: perineal trauma
One trial of 253 women reported on this outcome. The three‐arm study included electro and manual acupuncture and may make little difference to reducing perineal trauma (RR 0.49, 95% CI 0.19 to 1.26; Analysis 2.10).
2.11) Outcome: maternal blood loss > 500 mL
One trial of 253 women reported on this outcome. The three arm study included electro and manual acupuncture and may reduce the rate of postpartum haemorrhage for women receiving the intervention (RR 0.30, 95% CI 0.11 to 0.78; Analysis 2.11).
2.12) Outcome: relaxation
We are uncertain whether manual acupuncture increases relaxation (MD ‐0.90, 95% CI ‐1.62 to ‐0.18, 90 women; Analysis 2.12).
Subgroup analysis
There were not enough data relating to manual or electro‐acupuncture to demonstrate any differential effect according to type of acupuncture.
3 Acupuncture versus no treatment
One trial of 163 women reported on this comparison. No trial reported on the primary outcomes of: sense of control in labour, satisfaction with childbirth and satisfaction with pain relief.
Primary outcomes
3.1) Outcome: pain intensity
One trial of electro‐acupuncture assessed pain along a VAS scale where a lower score indicated less pain. It is uncertain whether electro‐acupuncture reduces pain intensity compared to the control based on a single trial providing very low‐certainty evidence (MD ‐1.16, 95% CI ‐1.51 to ‐0.81, 163 women, very low‐certainty evidence; Analysis 3.1).
Data were not reported in a form that could be included in the meta‐analysis from the Qu 2007 study. The electro‐acupuncture group reported a lower intensity of pain compared with the control group (26 participants, one trial Qu 2007 study (P = 0.018)).
3.2) Outcome: assisted vaginal birth
It is uncertain whether electro‐acupuncture reduces assisted vaginal birth compared to the control based on a single trial providing very low‐certainty evidence (RR 0.49, 95% CI 0.18 to 1.38, 163 women, very low‐certainty evidence; Analysis 3.2).
3.3) Outcome: caesarean section
It is uncertain whether electro‐acupuncture reduces caesarean section compared to the control based on a single trial providing very low‐certainty evidence (RR 0.76, 95% CI 0.35 to 1.63, 163 women, very low‐certainty evidence; Analysis 3.3).
4) Acupuncture versus water injection
One trial of manual acupuncture with 128 women reported on this comparison. No trial reported on the primary outcomes of: pain intensity, sense of control in labour, satisfaction with childbirth.
Primary outcomes
4.1) Outcome: satisfaction with pain relief
Data from Martensson 2008 were not included in the meta‐analysis. This study assessed pain along a VAS scale where a lower score indicated less pain. Acupuncture may improve satisfaction with pain relief in labour (MD 18.60, 95% CI 11.54 to 25.66, 128 women).
4.2) Outcome: use of pharmacological analgesia
It is uncertain whether acupuncture reduces the use of pharmacological analgesia because the evidence was based on a single trial of very low‐certainty evidence (RR 0.84, 95% CI 0.54 to 1.30, 1 trial, 128 women, very low‐certainty evidence; Analysis 4.1).
4.3) Outcome: assisted vaginal birth
It is uncertain whether acupuncture reduces assisted vaginal birth because the evidence was based on a single trial of very low‐certainty evidence (RR 1.60, 95% CI 0.47 to 5.39, 1 trial, 128 women, very low‐certainty evidence; Analysis 4.2).
4.4) Outcome: caesarean section
It is uncertain whether acupuncture reduces caesarean section because the evidence was based on a single trial of very low certainty (RR 1.33, 95% CI 0.37 to 4.73, 1 trial, 128 women, Analysis 4.3).
Secondary outcomes
4.5) Outcome: augmentation with oxytocin
It is uncertain whether acupuncture reduces augmentation because the evidence was based on a single trial of very low‐certainty evidence (RR 1.16, 95% CI 0.85 to 1.58, 1 trial, 128 women; Analysis 4.4).
4.6) Outcome: relaxation
Relaxation was assessed along a VAS scale where a score of 0 indicated totally relaxed and 100 feeling very tense. Acupuncture may improve women's sense of relaxation (MD 12.60, 95% CI 4.75 to 20.45, 1 trial, 128 women; Analysis 4.5).
5) Acupressure versus sham control
Seven trials of 547 women reported on this comparison. No trial reported on the primary outcomes of: sense of control in labour, satisfaction with childbirth and satisfaction with pain relief.
Primary outcome
5.1) Outcome: pain intensity
Pain intensity was assessed using a VAS where a low score indicated less pain. We are uncertain if acupressure reduces pain intensity in labour because there was significant heterogeneity and the evidence was assessed as very low certainty (MD ‐1.93, 95% CI ‐3.31 to ‐0.55, 6 trials, 472 women; Analysis 5.1). The heterogeneity may be explained by the timing of the observation of pain at various stages during the first stage of labour.
5.2) Outcome: use of pharmacological analgesia
Acupressure may make little difference in the use of pharmacological analgesia between groups (RR 0.54, 95% CI 0.20 to 1.43, 1 trial, 75 women, low‐certainty evidence; Analysis 5.2).
5.3) Outcome: assisted vaginal birth
We are uncertain if acupressure reduces assisted vaginal birth because the evidence was assessed as very low certainty (RR 3.00, 95% CI 0.13 to 71.92, 100 women, 1 trial, very low‐certainty evidence; Analysis 5.3).
5.4) Outcome: caesarean section
Acupressure probably reduces the caesarean section rate compared to sham control (RR 0.44, 95% CI 0.27 to 0.71, 4 trials, 313 women, moderate‐certainty evidence; Analysis 5.4).
5.5) Outcome: Apgar scores less than seven at five minutes
Due to the small number of events we are uncertain if acupressure reduces the Apgar score (RR 0.33, 95% CI 0.01 to 7.99, 220 women, 2 trials; Analysis 5.5). Mafetoni 2016a reported Apgar scores as a mean and standard deviation at one and five minutes and there were no differences between groups.
Secondary outcomes
5.6) Length of labour
Acupuressure may reduce the length of labour in the acupressure group (minutes) (SMD ‐0.91, 95% CI ‐1.26 to ‐0.57, 4 trials, 399 women; Analysis 5.6). However, there was significant heterogeneity I2 = 63% and a random‐effects model was applied, which was reduced with the SMD. Data from Mafetoni 2016a were not in a form that could be included in the analysis.
5.7) Outcome: spontaneous vaginal birth
There was no evidence of differences between groups (RR 1.04, 95% CI 0.92 to 1.18, 115 women, 2 trials; Analysis 5.7).
5.8) Outcome: augmentation with oxytocin
Acupressure may reduce augmentation, although the results were based on only two small trials (RR 0.65, 95% CI 0.46 to 0.91, 135 women, 2 trials; Analysis 5.8).
5.9) Anxiety
Acupressure may reduce anxiety, but again the results were based on only one small trial (MD ‐1.40, 95% CI ‐2.51 to ‐0.29, 1 trial, 75 women; Analysis 5.9).
6) Acupressure versus usual care
Nine trials of 995 women reported data suitable for inclusion in the meta‐analysis. Calik 2014 reported data with medians and mean rank and this was reported narratively. No trial reported on the primary outcomes of: sense of control in labour, satisfaction with childbirth and satisfaction with pain relief.
Primary outcomes
6.1) Outcome: pain intensity
Pain was assessed using a VAS or NRS where a low score indicated less pain. We are uncertain if acupressure reduces pain intensity in labour because the evidence was assessed as very low certainty (SMD ‐1.07, 95% CI ‐1.45 to ‐0.69, 8 trials, 620 women, very low‐certainty evidence; Analysis 6.1). There was significant heterogeneity I2 75% explained by the Ozgoli 2016 trial.
Calik 2014 recorded pain intensity measures at five time points and found that there were significant differences between the groups in subjective labour pain scores in favour of acupressure at all time points except time point 4 (P < 0.001).
6.2) Outcome: satisfaction with pain relief
Satisfaction was assessed from women's views indicating a score of 0 was not effective to 3 = very effective. We are uncertain if acupressure increases satisfaction with pain relief because the evidence was assessed as very low certainty (MD 1.05, 95% CI 0.75 to 1.35, 1 trial, 105 women, very low‐certainty evidence).
6.3) Outcome: caesarean section
Acupressure may make little difference to caesarean section (RR 0.82, 95% CI 0.54 to 1.23, 4 trials, 391 women, low‐certainty evidence; Analysis 6.3).
6.4) Apgar scores less than seven at five minutes
Two trials Calik 2014 and Ozgoli 2016 reported data that could not be included in the meta‐analysis.
Secondary outcomes
6.5 Length of labour
Acupressure may make little difference to the length of labour in minutes (MD ‐16.23, 95% CI ‐79.64 to 47.18, 1 trial, 44 women; Analysis 6.4). The data from the Salehian 2011 trial were not included as this reported on the first and second stage of labour only. Data from Calik 2014 were excluded due to the unclear reporting of total duration of labour.
6.6 Spontaneous vaginal birth
Acupressure may make little difference to rates of vaginal birth (RR 1.04, 95% CI 0.90 to 1.21, 3 trials, 220 women; Analysis 6.5).
6.7 Augmentation with oxytocin
There was no evidence of a difference between groups (RR 2.00, 95% CI 0.39 to 10.31, 1 trial, 15 women; Analysis 6.6).
7) Acupressure versus combined control (placebo and no treatment)
Two trials of 322 women reported on this comparison. No trial reported on the primary outcomes of: sense of control in labour and satisfaction with pain relief.
Primary outcomes
7.1) Outcome: pain intensity
Pain was assessed using a VAS scale where a low score indicated less pain. Acupressure probably slightly reduces the intensity of pain during labour compared with the combined control (SMD ‐0.42, 95% CI ‐0.65 to ‐0.18, 2 trials, 322 women, moderate‐certainty evidence; Analysis 7.1).
7.2) Outcome: satisfaction with childbirth
Satisfaction was assessed using a VAS scale with a low score indicating very bad and a high score very good. One trial, 212 women reported on this outcome. The results are very low certainty and so we are uncertain whether acupressure has any effect on satisfaction with childbirth (MD 4.80, 95% CI ‐2.25 to 11.85, 1 trial, 212 women; Analysis 7.2).
7.3) Use of pharmacological analgesia
It is uncertain whether acupressure reduces use of pharmacological analgesia because the evidence was based on a single trial of very low certainty (RR 0.94, 95% CI 0.71 to 1.25, 1 trial, 212 women, very low‐certainty evidence; Analysis 7.3).
7.4) Outcome: assisted vaginal birth
It is uncertain whether acupressure reduces assisted vaginal birth because the evidence was based on a single trial of very low certainty (RR 0.81, 95% CI 0.39 to 1.67, 1 trial, 212 women, very low‐certainty evidence; Analysis 7.4).
7.5) Caesarean section
It is uncertain whether acupressure reduces caesarean section because the evidence was based on a single trial of very low certainty (RR 0.48, 95% CI 0.22 to 1.04, 1 trial, 212 women, very low‐certainty evidence; Analysis 7.5).
Secondary outcomes
7.6) Outcome: augmentation with oxytocin
Acupressure may make little difference to augmentation with oxytocin (RR 1.01, 95% CI 0.77 to 1.31, 1 trial, 212 women, low‐certainty evidence; Analysis 7.6).
Sensitivity analysis
It was proposed to undertake a sensitivity analysis on the results to look at the possible contribution of: (1) differences in methodological quality, with trials of high quality (low risk of bias) compared to all trials; and (2) publication bias by country. This was not done due to the small number of trials overall. There were no trials of high quality; there were also too few trials within comparisons to make comparisons to examine the influence of publication bias. Where there was heterogeneity, we applied a random‐effects model.
Subgroup analysis
We were only able to analyse data according to the subgroup of manual versus electro‐acupuncture, but there were not enough data to demonstrate any differences between these two subgroups. For other pre‐specified subgroups, we did not undertake subgroup analysis, based on insufficient reporting of trials with the variables of interest by outcome.
Discussion
Summary of main results
The review included 28 trials of 3960 women, with data contributing to data and analysis from 27 trials of 3930 women. The evidence suggests a limited benefit from acupuncture and acupressure in relation to the primary outcomes of less intense pain, and increased maternal satisfaction from acupuncture.
Acupuncture compared to sham control
Acupuncture may make little or no difference to the intensity of pain felt by women when compared with sham acupuncture (low‐certainty evidence), but probably increases satisfaction with pain relief and probably reduces the use of pharmacological analgesia (moderate‐certainty evidence). Acupuncture may have no effect on assisted vaginal birth (very low‐certainty evidence), and probably little to no effect on caesarean section (low‐certainty evidence).
Acupuncture compared to usual care
We are uncertain if acupuncture reduces pain intensity compared to usual care. Acupuncture may have little to no effect on satisfaction with pain relief (low‐certainty evidence). We are uncertain if acupuncture reduces the use of pharmacological analgesia (very low‐certainty evidence). Acupuncture probably has little to no effect on assisted vaginal birth (low‐certainty evidence) or caesarean section (low‐certainty evidence).
Acupuncture compared to no treatment
One trial compared acupuncture to no treatment. We are uncertain if acupuncture reduces pain intensity, assisted vaginal birth or caesarean section because the evidence was found to be of very low certainty.
Acupuncture compared to sterile water injection
We are uncertain if acupuncture has any effect on use of pharmacological analgesia, assisted vaginal birth or caesarean section because the evidence was found to be of very low certainty.
Acupressure compared to a sham control
We are uncertain if acupressure reduces pain intensity in labour (very low‐certainty evidence), or assisted vaginal birth (very low‐certainty evidence). Acupressure probably reduces the caesarean section rate compared to sham control (moderate‐certainty evidence). Acupressure may have little to no effect on use of pharmacological analgesia (low‐certainty evidence).
Acupressure compared to usual care
We are uncertain if acupressure reduces pain intensity in labour (very low‐certainty evidence) or increases satisfaction with pain relief (very low‐certainty evidence). Acupressure may have little to no effect on caesarean section (low‐certainty evidence).
Acupressure compared to a combined control
Acupressure probably slightly reduces the intensity of pain during labour group compared with the combined control (moderate‐certainty evidence). We are uncertain if acupressure has any effect on the use of pharmacological analgesia, satisfaction with childbirth, assisted vaginal birth or caesarean section because the certainty of the evidence was all very low.
Currently there are a small number of trials included within each comparison, and this limits the power of the review to detect meaningful differences between groups and analyses, suggesting any limited benefits should be interpreted with caution.
For both primary and secondary outcomes the evidence was moderate to very low certainty using the GRADE framework and the results were heterogenous. Many of the comparisons are characterised as having significant clinical and substantial or considerable statistical heterogeneity. This may relate to the intervention regarding dosing characteristics and the heterogeneity of the controls. Within comparisons we presented data by mode of acupuncture stimulation (manual, electro‐acupuncture). Although the comparisons between acupuncture and the different control groups are not all consistent in their findings, most comparisons suggest a beneficial effect from acupuncture, though the potential for bias exists. Due to small numbers of studies we have been unable to identify treatment‐dose parameters that may moderate and influence the treatment outcomes.
Additional sources of bias have been highlighted throughout the review but the role of participants' expectations and their often unblinded status may also play a role. In trials where there was no blinding, the expectation effects may be greater and contribute a larger placebo effect. The sham controlled trials in this review show an overall small benefit from acupuncture compared with this control, however there is high heterogeneity and different controls may differ in the degree of how inert or credible they are, or whether there is a placebo effect. Addressing this is a priority for future studies.
Overall completeness and applicability of evidence
There remain relatively few trials of acupuncture and acupressure that assess the role of these interventions in the management of pain relief in labour. The completeness and applicability of the evidence is limited from the 28 included trials, with no trial at a low risk of bias on all domains. A weakness of a number of trials continues to be the inclusion of few outcomes and omission of safety clinical outcomes.
Trials recruited low‐risk nulliparous and multiparous women at term, mostly in spontaneous labour. Studies were conducted in different countries and consequently this reflects the different styles of acupuncture administered in the studies. There are many styles of acupuncture, including individualised traditional Chinese medicine, as illustrated by eight trials administering individualised treatment (Borup 2009; Hantoushzadeh 2007; Huang 2008; Martensson 2008; Nesheim 2003; Ramnero 2002; Skilnand 2002; Vixner 2014) and those using standardised acupuncture points as used in the majority of trials in this review. The systematic review documented wide variation in the mode of stimulation, duration of needling, number of points used, depth of needling and duration of the trial. It is unclear how representative the treatment protocols used in the research are generalisable to acupuncture as it is usually practiced. There was insufficient reporting of the rationale of the acupuncture used in the research setting. The variation may also reflect the context in which acupuncture is practiced.
Quality of the evidence
The risk of bias (Figure 2; Figure 3) demonstrates that acupuncture has not been consistently subjected to rigorous study protocols. The quality of reporting was poor in the majority of trials. The risk of bias was mostly low in respect to randomisation. No one trial was rated at a low risk of bias on all domains. Rates of follow‐up were high in the majority of trials with only a small number of trials reporting a small loss of participants. For many studies blinding of participants and the practitioner was not possible, and reporting indicated that the outcomes could have been influenced by a lack of blinding and consequently were rated at a high risk of bias. The small number of studies within comparisons and lack of high‐quality trials suggest there remains insufficient evidence of a consistent treatment effect from acupuncture. We contacted the chief investigators of some studies to provide additional methodological and statistical information; however, we obtained only a few responses (Chung 2003; Huang 2008; Kashanian 2010).
The certainty of evidence was affected by unexplained substantial heterogeneity in some comparisons arising from both the heterogeneity of the clinical interventions and study designs. The small number of studies within comparisons, small samples sizes and lack of high‐quality trials prevented further investigation of the heterogeneity and the impact on treatment effects. The certainty of evidence was downgraded due the high levels of heterogeneity, small studies, and high risk of bias on one or more domains. We were unable to examine the effect of study quality using a sensitivity analysis due to few studies at a low risk of bias. The quality of reporting remains poor in many studies.
The certainty of evidence overall using GRADE was very low to moderate (summary of findings Table for the main comparison; summary of findings Table 2; summary of findings Table 3; summary of findings Table 4; summary of findings Table 5; summary of findings Table 6; summary of findings Table 7).
Quality of acupuncture
The quality of acupuncture that was administered was assessed using the newly published 'Reliability of the NICMAN Scale: An Instrument to Assess the Quality of Acupuncture Administered in Clinical Trials' (Smith 2017). All studies of acupuncture were scored on an 11‐point scale that evaluated reported populations and study design, as well as the quality of reporting of the methods of acupuncture used, justification according to texts and evidence, and qualifications of those administering treatment (see Description of studies). The administration of acupuncture in the context of labour pain was assessed as an "acute condition" where few acupuncture treatments would normally be administered. In this context, studies scored high and provided evidence to support the assessment of quality. The rationale for the selection of points was generally well‐justified. However, reporting of details of the acupuncturist delivering the treatment was generally poorly reported and assessed as unclear, or was considered insufficient. The variation in the duration, frequency and selection of acupuncture points suggests that the acupuncture may not have been therapeutically effective and in some cases may not represent best clinical practice.
Potential biases in the review process
We attempted to minimise publication bias. Our search was comprehensive and we included studies identified in languages other than English. However, we cannot rule out the possibility that some studies have been missed. We excluded cross‐over trials from this review owing to lack of clarity regarding the appropriate period of washout for acupuncture trials. Two review authors assessed the eligibility of trials, carried out data extraction and assessed the risk of bias. We are aware that some literature on acupuncture may not be published in mainstream journals and therefore may be excluded from the main databases.
Agreements and disagreements with other studies or reviews
There is one other systematic review of acupuncture to manage pain in labour (Cho 2010) that included trials for which we were unable to ascertain the randomisation details, or we excluded because the trials did not meet the eligibility criteria. Our findings and conclusions concerning the role of acupuncture for pain relief in labour are similar to Cho 2010. Our results differ to those presented in a systematic review of non pharmacological interventions based on endogenous mechanism of action and compared with usual care (Chaillet 2014). This review classified acupuncture and acupressure through a diffuse noxious inhibitory control stimulating an endorphinergic system response. The review detailed different eligibility criteria and direct comparisons can not be made but the review found that acupuncture and acupressure compared to usual care was associated with reduced augmentation of epidural analgesia, labour pain and a better experience with childbirth. A number of clinical trials have been performed to study the efficacy of acupuncture for pain in labour although it remains uncertain whether the existing evidence is rigorous enough to reach a definitive conclusion. In a narrative review of three systematic reviews (Levett 2014), the authors note that the study questions and methods to address these differed, and attention should be paid to the matching of question to study design. Overall, there was evidence of a beneficial effect of acupuncture and acupressure in the systematic reviews in terms of pain scores, use of pharmacological analgesia and satisfaction when appropriate study designs were considered in the context of the clinical question.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
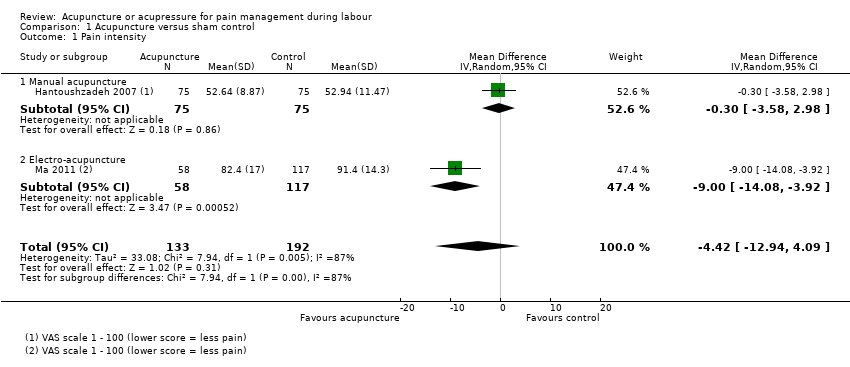
Comparison 1 Acupuncture versus sham control, Outcome 1 Pain intensity.
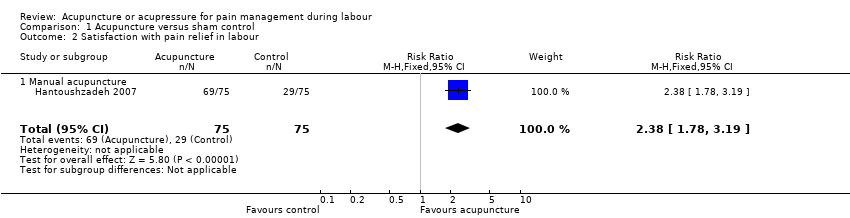
Comparison 1 Acupuncture versus sham control, Outcome 2 Satisfaction with pain relief in labour.
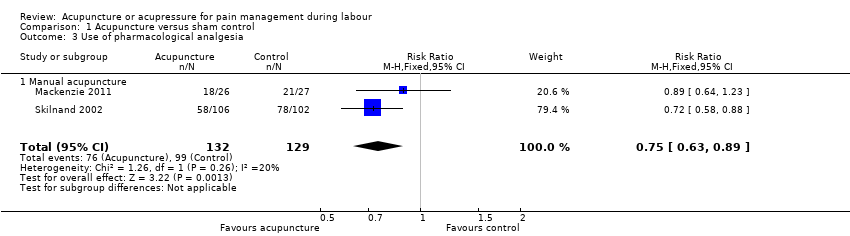
Comparison 1 Acupuncture versus sham control, Outcome 3 Use of pharmacological analgesia.

Comparison 1 Acupuncture versus sham control, Outcome 4 Assisted vaginal birth.

Comparison 1 Acupuncture versus sham control, Outcome 5 Caesarean section.

Comparison 1 Acupuncture versus sham control, Outcome 6 Apgar score < 7 at 5 minutes.
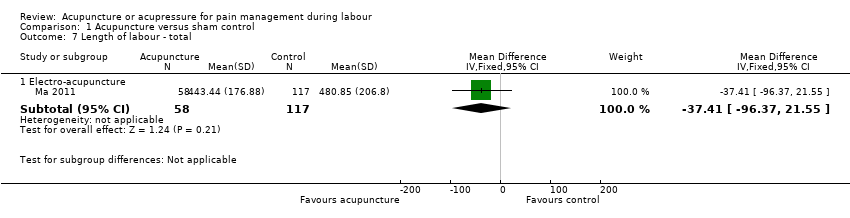
Comparison 1 Acupuncture versus sham control, Outcome 7 Length of labour ‐ total.

Comparison 1 Acupuncture versus sham control, Outcome 8 Spontaneous vaginal birth.
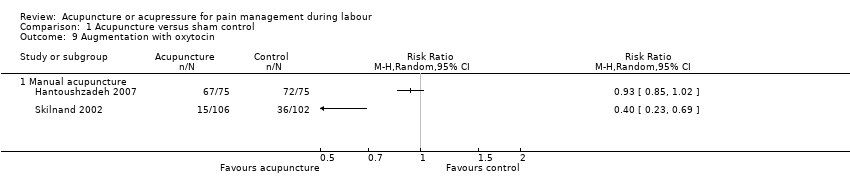
Comparison 1 Acupuncture versus sham control, Outcome 9 Augmentation with oxytocin.

Comparison 2 Acupuncture versus usual care, Outcome 1 Pain intensity.

Comparison 2 Acupuncture versus usual care, Outcome 2 Satisfaction with pain relief in labour.

Comparison 2 Acupuncture versus usual care, Outcome 3 Use of pharmacological analgesia.
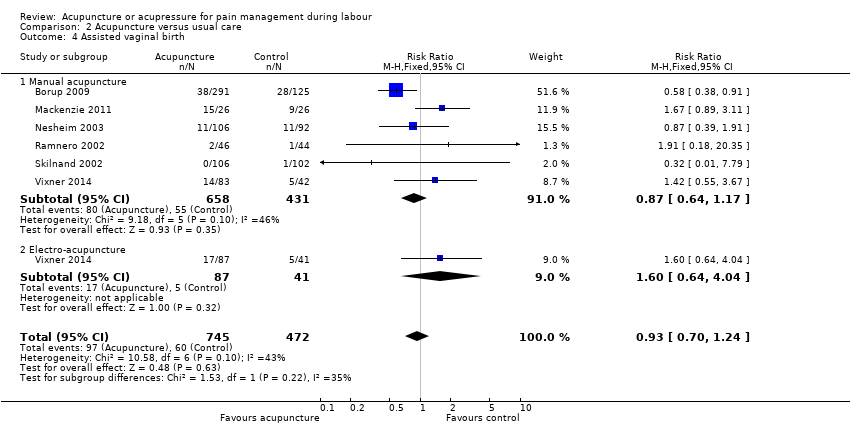
Comparison 2 Acupuncture versus usual care, Outcome 4 Assisted vaginal birth.

Comparison 2 Acupuncture versus usual care, Outcome 5 Caesarean section.
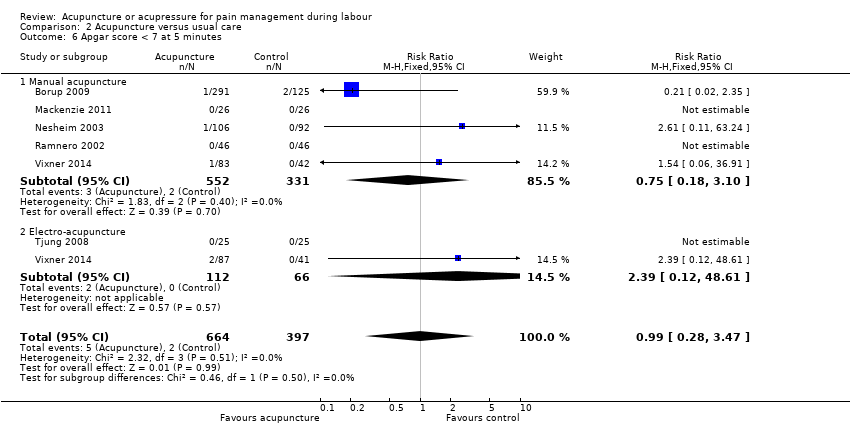
Comparison 2 Acupuncture versus usual care, Outcome 6 Apgar score < 7 at 5 minutes.

Comparison 2 Acupuncture versus usual care, Outcome 7 Length of labour ‐ total.

Comparison 2 Acupuncture versus usual care, Outcome 8 Spontaneous vaginal birth.

Comparison 2 Acupuncture versus usual care, Outcome 9 Augmentation with oxytocin.

Comparison 2 Acupuncture versus usual care, Outcome 10 Perineal trauma.

Comparison 2 Acupuncture versus usual care, Outcome 11 Maternal blood loss > 500 mL.

Comparison 2 Acupuncture versus usual care, Outcome 12 Relaxation.

Comparison 3 Acupuncture versus no treatment, Outcome 1 Pain intensity.
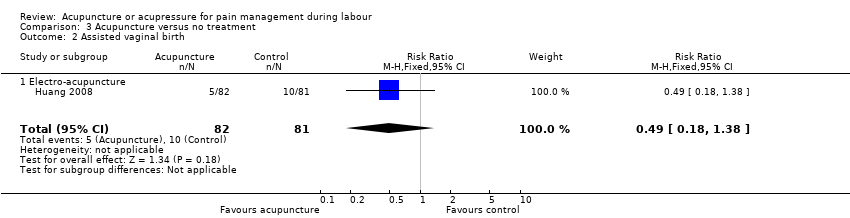
Comparison 3 Acupuncture versus no treatment, Outcome 2 Assisted vaginal birth.
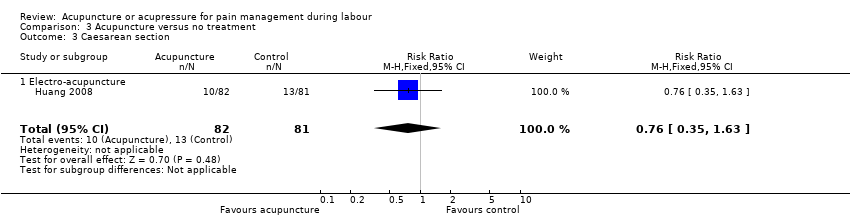
Comparison 3 Acupuncture versus no treatment, Outcome 3 Caesarean section.
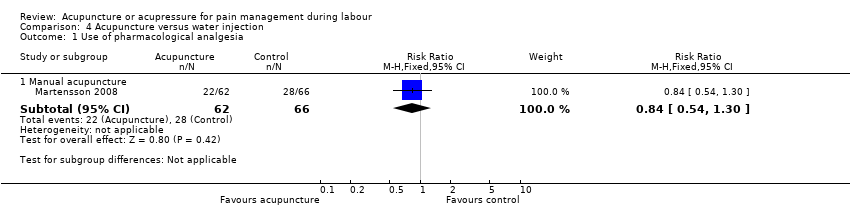
Comparison 4 Acupuncture versus water injection, Outcome 1 Use of pharmacological analgesia.

Comparison 4 Acupuncture versus water injection, Outcome 2 Assisted vaginal birth.
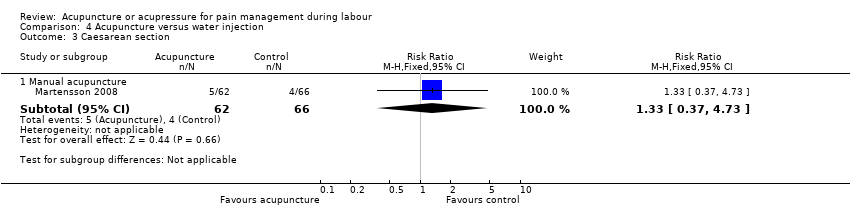
Comparison 4 Acupuncture versus water injection, Outcome 3 Caesarean section.
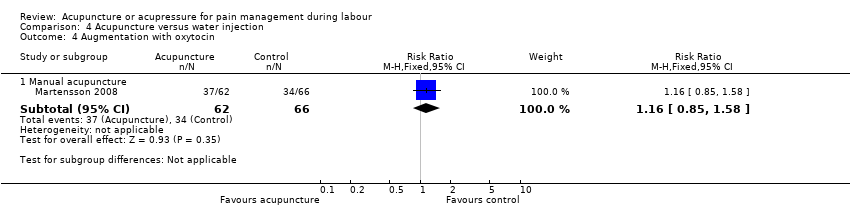
Comparison 4 Acupuncture versus water injection, Outcome 4 Augmentation with oxytocin.

Comparison 4 Acupuncture versus water injection, Outcome 5 Relaxation.

Comparison 5 Acupressure versus sham control, Outcome 1 Pain intensity.

Comparison 5 Acupressure versus sham control, Outcome 2 Use of pharmacological analgesia.

Comparison 5 Acupressure versus sham control, Outcome 3 Assisted vaginal birth.

Comparison 5 Acupressure versus sham control, Outcome 4 Caesarean section.

Comparison 5 Acupressure versus sham control, Outcome 5 Apgar score < 7 at 5 minutes.
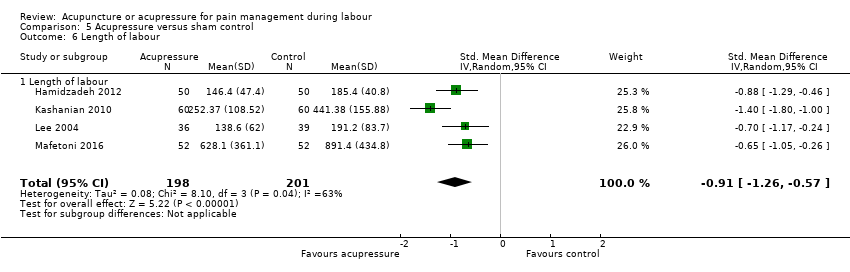
Comparison 5 Acupressure versus sham control, Outcome 6 Length of labour.

Comparison 5 Acupressure versus sham control, Outcome 7 Spontaneous vaginal birth.
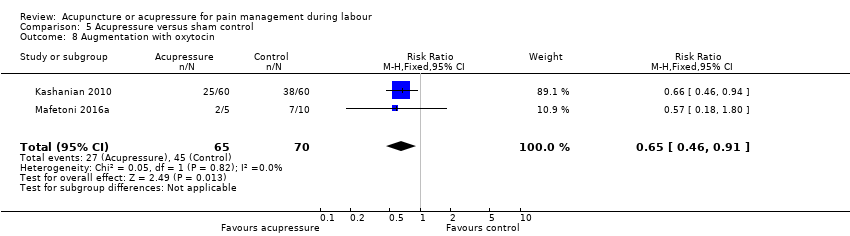
Comparison 5 Acupressure versus sham control, Outcome 8 Augmentation with oxytocin.
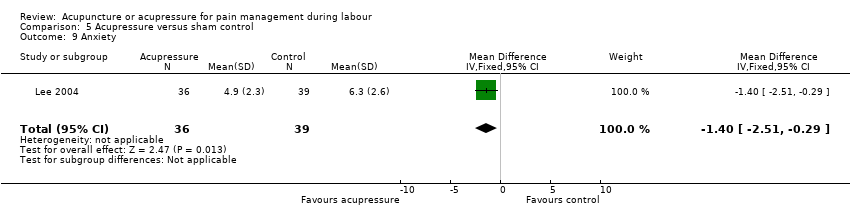
Comparison 5 Acupressure versus sham control, Outcome 9 Anxiety.

Comparison 6 Acupressure versus usual care, Outcome 1 Pain intensity.

Comparison 6 Acupressure versus usual care, Outcome 2 Satisfaction with pain relief.
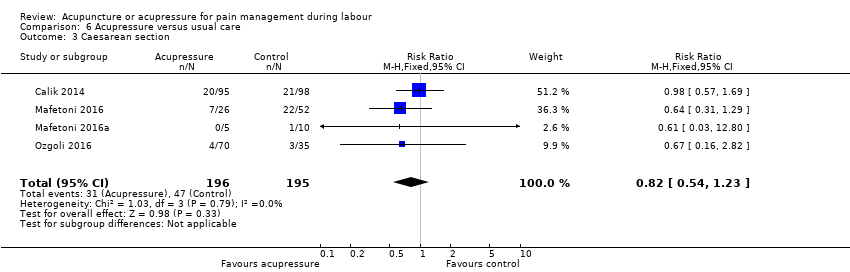
Comparison 6 Acupressure versus usual care, Outcome 3 Caesarean section.

Comparison 6 Acupressure versus usual care, Outcome 4 Length of labour.

Comparison 6 Acupressure versus usual care, Outcome 5 Spontaneous vaginal birth.

Comparison 6 Acupressure versus usual care, Outcome 6 Augmentation with oxytocin.

Comparison 7 Acupressure versus combined control, Outcome 1 Pain intensity.
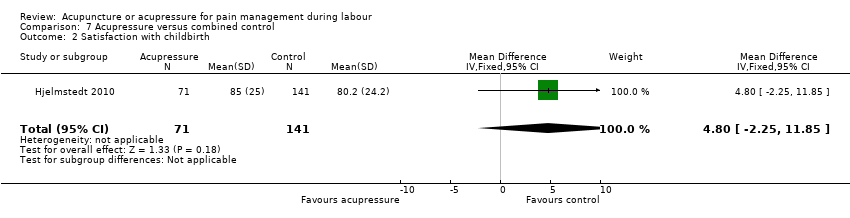
Comparison 7 Acupressure versus combined control, Outcome 2 Satisfaction with childbirth.
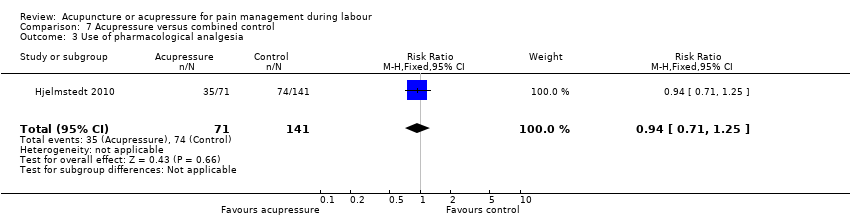
Comparison 7 Acupressure versus combined control, Outcome 3 Use of pharmacological analgesia.

Comparison 7 Acupressure versus combined control, Outcome 4 Assisted vaginal birth.

Comparison 7 Acupressure versus combined control, Outcome 5 Caesarean section.
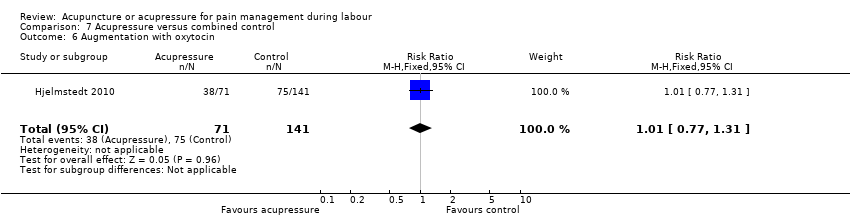
Comparison 7 Acupressure versus combined control, Outcome 6 Augmentation with oxytocin.
| Acupuncture compared to sham control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with sham control | Risk with acupuncture | |||||
| Pain intensity Lower scores indicate less pain intensity | The mean pain intensity ranged across control groups from 52.94 to 91.4 | The mean pain intensity score in the intervention group was 4.42 lower (12.94 lower to 4.09 higher) | 325 | ⊕⊕⊝⊝ | ||
| Satisfaction with pain relief in labour | Study population | RR 2.38 | 150 | ⊕⊕⊕⊝ | ||
| 387 per 1000 | 920 per 1000 | |||||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.75 | 261 | ⊕⊕⊕⊝ | ||
| 767 per 1000 | 576 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.10 | 261 | ⊕⊝⊝⊝ | ||
| 163 per 1000 | 179 per 1000 | |||||
| Caesarean section | Study population | RR 1.11 | 411 | ⊕⊕⊝⊝ | ||
| 49 per 1000 | 54 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: one study high or unclear risk of bias on six domains. 2 Downgraded one level due to serious inconsistency: substantial heterogeneity present I2 = 87% 3 Downgraded one level due to serious imprecision: small sample size (150) 4 Downgraded one level due to serious risk of bias: one study did not blind participants to group allocation. Should not affect sham arm outcome but blinding integrity not reported. 5 Downgraded one level due to serious inconsistency: substantial heterogeneity present I2 = 72% 6 Downgraded one level for imprecision due to small sample size and wide confidence intervals crossing the line of no effect 7 Downgraded one level for imprecision due to small number of events and wide confidence intervals crossing the line of no effect 8 Downgraded one level due to serious risk of bias: one study did not blind participants to group allocation and two studies at high risk of other bias | ||||||
| Acupuncture compared to usual care for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with acupuncture | |||||
| Pain intensity Mix of NRS and VAS scales so analysed using SMD | The mean pain intensity score in the intervention group was 1.31 standard deviations lower (2.14 lower to 0.49 lower) | 495 | ⊕⊝⊝⊝ | |||
| Satisfaction with pain relief in labour | Study population | RR 1.07 | 343 | ⊕⊕⊝⊝ | ||
| 787 per 1000 | 843 per 1000 | |||||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.72 | 1059 | ⊕⊝⊝⊝ | ||
| 833 per 1000 | 600 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 0.93 | 1217 | ⊕⊕⊝⊝ | ||
| 127 per 1000 | 118 per 1000 | |||||
| Caesarean section | Study population | RR 0.72 | 861 | ⊕⊕⊝⊝ | ||
| 116 per 1000 | 83 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels for very serious risk of bias: two of the three studies had high risk of performance bias and this was likely to influence a self‐reported outcome. 2 Downgraded two levels for very serious inconsistency: considerable heterogeneity present (I2 = 93%) not explained by subgroup analysis. 3 Downgraded two levels for very serious risk of bias: both studies had unclear or high risk of bias related to blinding and this was likely to influence a self‐reported outcome 4 Downgraded two levels for very serious risk of bias: all studies had unclear or high risk of performance bias and this was likely to influence the need for additional analgesia. 5 Downgraded one level for serious inconsistency: substantial heterogeneity (I2 = 70%) which is not explained by subgroups. 6 Downgraded one level for serious risk of bias: five of six studies at unclear or high risk of bias in both performance and detection bias. This may have influenced the outcome. 7 Downgraded one level for serious risk of bias: three of four studies at high or unclear risk of bias in both performance and detection bias. This may have influenced the outcome. 8 Downgraded one level for imprecision due to wide confidence intervals. | ||||||
| Acupuncture compared to no treatment for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with no treatment | Risk with acupuncture | |||||
| Pain intensity Lower scores indicate less pain. | The mean pain intensity in the control group was 7.92 | The mean pain intensity score in the intervention groups was 1.16 lower | ‐ | 163 | ⊕⊝⊝⊝ | |
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Assisted vaginal birth | Study population | RR 0.49 | 163 | ⊕⊝⊝⊝ | ||
| 123 per 1000 | 60 per 1000 | |||||
| Caesarean section | Study population | RR 0.76 | 163 | ⊕⊝⊝⊝ | ||
| 160 per 1000 | 122 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded by two levels for very serious risk of bias: high risk of bias in one domain (blinding for a subjective outcome) and unclear risk of bias in four domains. 2 Downgraded one level for serious imprecision due to a single study providing data with a small sample size (163) 3 Downgraded two levels for very serious imprecision due to a single study, with few events, small sample size and wide confidence intervals providing data | ||||||
| Acupuncture compared to water injection for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with water injection | Risk with acupuncture | |||||
| Pain intensity ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.84 | 128 | ⊕⊝⊝⊝ | ||
| 424 per 1000 | 356 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.60 | 128 | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 97 per 1000 | |||||
| Caesarean section | Study population | RR 1.33 | 128 | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 81 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to very serious risk of bias: high or unclear risk of bias in both blinding performance and detection bias 2 Downgraded two levels due to very serious imprecision: small study (128) with few events and wide confidence intervals crossing the line of no effect | ||||||
| Acupressure compared to sham control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with sham control | Risk with acupressure | |||||
| Pain intensity as measured by a 10 cm visual analogue scale. Lower scores indicate less pain | The mean pain intensity in the control groups was 8.35 | The mean pain intensity score in the intervention group was 1.93 lower (3.31 lower to 0.55 lower) | 472 | ⊕⊝⊝⊝ | ||
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.54 | 75 | ⊕⊕⊝⊝ | ||
| 256 per 1000 | 138 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 3.00 | 100 | ⊕⊝⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Caesarean section | Study population | RR 0.44 | 313 | ⊕⊕⊕⊝ | ||
| 308 per 1000 | 136 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level for serious risk of bias: majority of studies have unclear risk of bias in at least three domains. 2 Downgraded two levels for very serious inconsistency: considerable heterogeneity (I2 = 94%) 3 Downgraded two levels for very serious imprecision: very small sample size (75), small number of events and very wide confidence intervals 4 Downgraded one level for serious risk of bias: single study has high risk of performance bias and an unclear risk of allocation bias 5 Downgraded two levels for very serious imprecision: small sample size (100) and very wide confidence interval and small number of events 6 Downgraded one level for serious risk of bias: all studies have unclear risk of bias in at least three domains. Two studies have high or unclear risk of bias relating to performance bias | ||||||
| Acupressure compared to usual care for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with acupressure | |||||
| Pain intensity as measured by numeric rating scale (NRS) and visual analogue scale (VAS). Lower scores indicate less pain. | The mean pain intensity was 8.44 | The mean pain intensity score in the intervention group was 1.07 standard deviations lower (1.45 lower to 0.69 lower). | 620 | ⊕⊝⊝⊝ | The use of acupressure would result in a pain score approximately 2 cm lower on a 10 cm VAS or 2 points on a numeric rating scale compared to usual care. | |
| Satisfaction with pain relief | The mean satisfaction score with pain relief in the control group was 1.6 | The mean satisfaction with pain relief score was 1.05 higher (0.75 higher to 1.35 higher) | 105 | ⊕⊝⊝⊝ | ||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Assisted vaginal birth ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Caesarean section | Study population | RR 0.82 | 391 | ⊕⊕⊝⊝ | ||
| 241 per 1000 | 198 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: majority of included studies have high or unclear risk of bias relating to performance and detection bias 2 Downgraded two levels due to very serious inconsistency: considerable heterogeneity (I2 = 75%) 3 Downgraded two levels due to very serious risk of bias: single study at high risk of bias for selection, performance and detection bias. Very likely to have influenced the outcome 4 Downgraded one level due to serious imprecision: small sample size (105) 5 Downgraded one level due to serious risk of bias: two of the four studies included were at high risk of performance and detection bias, two studies were at high or unclear risk of selection bias and three at high or unclear risk of incomplete outcome data 6 Downgraded one level due to serious imprecision: wide confidence intervals incorporating both benefit and harm | ||||||
| Acupressure compared to combined control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with combined control | Risk with acupressure | |||||
| Pain intensity One study used VAS pain score on scale 1 ‐ 100 mm One study used VAS pain score on scale 1 ‐ 10 mm ‐ the mean | The mean pain intensity score in the intervention group was 0.42 standard deviations lower (0.65 lower to 0.18 lower) | 322 | ⊕⊕⊕⊝ | |||
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth | The mean satisfaction score with childbirth in the control group was 80.2 | The mean satisfaction score in the intervention group was 4.8 higher | ‐ | 212 | ⊕⊝⊝⊝ | |
| Use of pharmacological analgesia | Study population | RR 0.94 | 212 | ⊕⊝⊝⊝ | ||
| 525 per 1000 | 493 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 0.81 | 212 | ⊕⊝⊝⊝ | ||
| 156 per 1000 | 126 per 1000 | |||||
| Caesarean section | Study population | RR 0.48 | 212 | ⊕⊝⊝⊝ | ||
| 206 per 1000 | 99 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: both studies have unclear risk of bias for performance bias, possible effect on this outcome 2 Downgraded one level due to serious risk of bias: single study has unclear risk of performance bias, likely to effect this outcome 3 Downgraded two levels due to very serious imprecision: wide confidence interval greater than 0.25 on either side of the line of no effect and small sample size 4 Downgraded two levels for very serious imprecision: wide confidence interval encompassing both benefit and harm and small sample size | ||||||
| Study ID | Total NICMAN Score | P | I | C | O | Study design | Differential diagnosis | Point selection | Needling parameters | Acupuncture point location | Treatment dosage | Therapist qualifications |
| Borup 2009 | 19 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 1 | 1 | 2 | 2 |
| Dong 2015 | 15 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 1 | 2 | 0 |
| Hantoushzadeh 2007 | 20 | 2 | 2 | 2 | 2 | 3 | 1 | 2 | 2 | 2 | 2 | 0 |
| Huang 2008 | 16 | 2 | 2 | 2 | 2 | 3 | 2 | 2 | 0 | 0 | 1 | 0 |
| Ma 2011 | 17 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 2 | 0 |
| MacKenzie 2011 | 19 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 1 | 2 | 1 | 2 |
| Martensson 2008 | 16 | 2 | 2 | 2 | 2 | 3 | 0 | 1 | 1 | 0 | 2 | 1 |
| Nesheim 2003 | 16 | 2 | 2 | 2 | 2 | 3 | 2 | 0 | 2 | 0 | 1 | 0 |
| Qu 2007 | 13 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 0 | 1 | 0 |
| Ramnero 2002 | 17 | 2 | 2 | 2 | 2 | 3 | 1 | 1 | 1 | 2 | 1 | 0 |
| Skilnand 2002 | 18 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 1 | 0 |
| Tjung 2008 | 17 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 2 | 1 | 2 |
| Vixner 2014 | 18 | 2 | 2 | 2 | 2 | 3 | 1 | 2 | 1 | 2 | 1 | 0 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 2 | 325 | Mean Difference (IV, Random, 95% CI) | ‐4.42 [‐12.94, 4.09] |
| 1.1 Manual acupuncture | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐3.58, 2.98] |
| 1.2 Electro‐acupuncture | 1 | 175 | Mean Difference (IV, Random, 95% CI) | ‐9.0 [‐14.08, ‐3.92] |
| 2 Satisfaction with pain relief in labour Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.38 [1.78, 3.19] |
| 2.1 Manual acupuncture | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.38 [1.78, 3.19] |
| 3 Use of pharmacological analgesia Show forest plot | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.63, 0.89] |
| 3.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.63, 0.89] |
| 4 Assisted vaginal birth Show forest plot | 2 | 261 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.41, 2.97] |
| 4.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.41, 2.97] |
| 5 Caesarean section Show forest plot | 3 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.49, 2.48] |
| 5.1 Manual acupuncture | 3 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.49, 2.48] |
| 6 Apgar score < 7 at 5 minutes Show forest plot | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.79] |
| 6.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.79] |
| 7 Length of labour ‐ total Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Electro‐acupuncture | 1 | 175 | Mean Difference (IV, Fixed, 95% CI) | ‐37.41 [‐96.37, 21.55] |
| 8 Spontaneous vaginal birth Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Manual acupuncture | 3 | 411 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.86, 1.12] |
| 9 Augmentation with oxytocin Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9.1 Manual acupuncture | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 4 | 495 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.31 [‐2.14, ‐0.49] |
| 1.1 Manual acupuncture | 2 | 270 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐2.36, 0.58] |
| 1.2 Electro‐acupuncture | 2 | 225 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.79 [‐3.37, ‐0.21] |
| 2 Satisfaction with pain relief in labour Show forest plot | 2 | 343 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.96, 1.20] |
| 2.1 Manual acupuncture | 2 | 215 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.95, 1.23] |
| 2.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.87, 1.30] |
| 3 Use of pharmacological analgesia Show forest plot | 6 | 1059 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.60, 0.85] |
| 3.1 Manual acupuncture | 5 | 884 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.60, 0.82] |
| 3.2 Electro‐acupuncture | 2 | 175 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.01, 8.16] |
| 4 Assisted vaginal birth Show forest plot | 6 | 1217 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.70, 1.24] |
| 4.1 Manual acupuncture | 6 | 1089 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.64, 1.17] |
| 4.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.64, 4.04] |
| 5 Caesarean section Show forest plot | 5 | 861 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.47, 1.09] |
| 5.1 Manual acupuncture | 4 | 683 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.50, 1.24] |
| 5.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.16, 1.28] |
| 6 Apgar score < 7 at 5 minutes Show forest plot | 6 | 1061 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.28, 3.47] |
| 6.1 Manual acupuncture | 5 | 883 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.18, 3.10] |
| 6.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [0.12, 48.61] |
| 7 Length of labour ‐ total Show forest plot | 3 | 608 | Mean Difference (IV, Fixed, 95% CI) | ‐13.89 [‐28.93, 1.14] |
| 7.1 Manual acupuncture | 1 | 124 | Mean Difference (IV, Fixed, 95% CI) | 4.0 [‐142.47, 150.47] |
| 7.2 Electro‐acupuncture | 3 | 484 | Mean Difference (IV, Fixed, 95% CI) | ‐14.08 [‐29.20, 1.03] |
| 8 Spontaneous vaginal birth Show forest plot | 4 | 449 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.89, 1.08] |
| 8.1 Manual acupuncture | 3 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.85, 1.10] |
| 8.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.86, 1.14] |
| 9 Augmentation with oxytocin Show forest plot | 4 | 813 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.77, 1.02] |
| 9.1 Manual acupuncture | 3 | 635 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.78, 1.09] |
| 9.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.59, 1.03] |
| 10 Perineal trauma Show forest plot | 1 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.19, 1.26] |
| 10.1 Manual acupuncture | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.13, 1.92] |
| 10.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.12, 1.79] |
| 11 Maternal blood loss > 500 mL Show forest plot | 1 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.11, 0.78] |
| 11.1 Manual acupuncture | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.11, 1.43] |
| 11.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.04, 0.93] |
| 12 Relaxation Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 Manual acupuncture | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.62, ‐0.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 1 | 163 | Mean Difference (IV, Fixed, 95% CI) | ‐1.16 [‐1.51, ‐0.81] |
| 1.1 Electro‐acupuncture | 1 | 163 | Mean Difference (IV, Fixed, 95% CI) | ‐1.16 [‐1.51, ‐0.81] |
| 2 Assisted vaginal birth Show forest plot | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.18, 1.38] |
| 2.1 Electro‐acupuncture | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.18, 1.38] |
| 3 Caesarean section Show forest plot | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.35, 1.63] |
| 3.1 Electro‐acupuncture | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.35, 1.63] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Use of pharmacological analgesia Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.30] |
| 2 Assisted vaginal birth Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.47, 5.39] |
| 3 Caesarean section Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.37, 4.73] |
| 4 Augmentation with oxytocin Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.85, 1.58] |
| 5 Relaxation Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Manual acupuncture | 1 | 128 | Mean Difference (IV, Fixed, 95% CI) | 12.60 [4.75, 20.45] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 6 | 472 | Mean Difference (IV, Random, 95% CI) | ‐1.93 [‐3.31, ‐0.55] |
| 2 Use of pharmacological analgesia Show forest plot | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.20, 1.43] |
| 3 Assisted vaginal birth Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 71.92] |
| 4 Caesarean section Show forest plot | 4 | 313 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.27, 0.71] |
| 5 Apgar score < 7 at 5 minutes Show forest plot | 2 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.99] |
| 6 Length of labour Show forest plot | 4 | 399 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.26, ‐0.57] |
| 6.1 Length of labour | 4 | 399 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.26, ‐0.57] |
| 7 Spontaneous vaginal birth Show forest plot | 2 | 115 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.92, 1.18] |
| 8 Augmentation with oxytocin Show forest plot | 2 | 135 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.46, 0.91] |
| 9 Anxiety Show forest plot | 1 | 75 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐2.51, ‐0.29] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 8 | 620 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐1.45, ‐0.69] |
| 2 Satisfaction with pain relief Show forest plot | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 1.05 [0.75, 1.35] |
| 3 Caesarean section Show forest plot | 4 | 391 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.54, 1.23] |
| 4 Length of labour Show forest plot | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐16.23 [‐79.64, 47.18] |
| 5 Spontaneous vaginal birth Show forest plot | 3 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.90, 1.21] |
| 6 Augmentation with oxytocin Show forest plot | 1 | 15 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.39, 10.31] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 2 | 322 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.42 [‐0.65, ‐0.18] |
| 2 Satisfaction with childbirth Show forest plot | 1 | 212 | Mean Difference (IV, Fixed, 95% CI) | 4.80 [‐2.25, 11.85] |
| 3 Use of pharmacological analgesia Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.71, 1.25] |
| 4 Assisted vaginal birth Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.39, 1.67] |
| 5 Caesarean section Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.22, 1.04] |
| 6 Augmentation with oxytocin Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.77, 1.31] |

