Acupuntura o acupresión para el tratamiento del dolor durante el trabajo de parto
Resumen
Antecedentes
A muchas mujeres les gustaría evitar los métodos farmacológicos o invasivos para el manejo del dolor durante el trabajo de parto, lo que puede contribuir a la popularidad de los métodos complementarios para el manejo del dolor. Esta revisión examinó la evidencia que apoya el uso de la acupuntura y la acupresión para el tratamiento del dolor durante el trabajo de parto. Esta es una actualización de una revisión publicada por última vez en 2011.
Objetivos
Examinar los efectos de la acupuntura y la acupresión para el tratamiento del dolor durante el trabajo de parto.
Métodos de búsqueda
Para esta actualización se hicieron búsquedas en el Registro Cochrane de Ensayos de Embarazo y Parto (Cochrane Pregnancy and Childbirth's Trials Register), (25 de febrero 2019), en el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (the Cochrane Library 2019, Número 1), MEDLINE (1966 hasta febrero 2019), CINAHL (1980 hasta febrero 2019), ClinicalTrials.gov (febrero 2019), la WHO International Clinical Trials Registry Platform (ICTRP) (febrero 2019) y las listas de referencias de los estudios incluidos.
Criterios de selección
Ensayos controlados aleatorizados (ECA) publicados y no publicados que compararon acupuntura y acupresión con placebo, ningún tratamiento u otras formas no farmacológicas para el tratamiento del dolor durante el trabajo de parto. Se incluyeron todas las mujeres primíparas o multíparas en trabajo de parto espontáneo o inducido.
Se incluyeron los estudios informados como resúmenes si tenían suficiente información para permitir la evaluación del riesgo de sesgo. Los ensayos que utilizaron un diseño de ECA grupal fueron elegibles para su inclusión, no así los cuasialeatorizados o los estudios cruzados (cross‐over).
Obtención y análisis de los datos
Dos autores de la revisión evaluaron de forma independiente los ensayos para la inclusión y el riesgo de sesgo, extrajeron los datos y verificaron su exactitud. La certeza de la evidencia se evaluó mediante los criterios GRADE.
Resultados principales
Se incluyeron 28 ensayos que informaron datos sobre 3960 mujeres. Trece ensayos informaron sobre la acupuntura y 15 sobre la acupresión. Ningún estudio tuvo bajo riesgo de sesgo en todos los dominios. En general la intensidad del dolor se midió con una escala analógica visual (EAV) de 0 a 10 o de 0 a 100, en la que las puntuaciones bajas indicaron menos dolor.
Acupuntura versus acupuntura simulada
La acupuntura puede hacer poca o ninguna diferencia en cuanto a la intensidad del dolor que sienten las mujeres, en comparación con la acupuntura simulada (diferencia de medias [DM] ‐4,42, intervalo de confianza [IC] del 95%: ‐12,94 a 4,09, dos ensayos, 325 mujeres, evidencia de certeza baja). La acupuntura puede aumentar la satisfacción con el alivio del dolor en comparación con la acupuntura simulada (riesgo relativo [RR] 2,38; IC del 95%: 1,78 a 3,19; un ensayo, 150 mujeres, evidencia de certeza moderada) y probablemente reduce la administración de analgesia farmacológica (RR 0,75; IC del 95%: 0,63 a 0,89; dos ensayos, 261 mujeres, evidencia de certeza moderada). Es posible que la acupuntura no tenga efecto sobre el parto vaginal asistido (evidencia de certeza muy baja) y probablemente tiene poco o ningún efecto sobre la cesárea (evidencia de certeza baja).
Acupuntura en comparación con la atención habitual
No se conoce con certeza si la acupuntura reduce la intensidad del dolor en comparación con la atención habitual porque se encontró que la evidencia es de certeza muy baja (diferencia de medias estandarizada [DME ‐1,31; IC del 95%: ‐2,14 a ‐0,49; cuatro ensayos; 495 mujeres; I2 = 93%). Es posible que la acupuntura tenga poco o ningún efecto sobre la satisfacción del alivio del dolor (evidencia de certeza baja). No se conoce con certeza si la acupuntura reduce la administración de analgesia farmacológica porque se encontró evidencia de certeza muy baja (RR promedio 0,72; IC del 95%: 0,60 a 0,85; seis ensayos, 1059 mujeres, I2 = 70%). Es probable que la acupuntura tenga poco o ningún efecto sobre el parto vaginal asistido (evidencia de certeza baja) o sobre la cesárea (evidencia de certeza baja).
Acupuntura en comparación con ningún tratamiento
Un ensayo comparó la acupuntura con ningún tratamiento. No se conoce con certeza si la acupuntura reduce la intensidad del dolor (DM ‐1,16; IC del 95%: ‐1,51 a ‐0,81; 163 mujeres, evidencia de certeza muy baja), el parto vaginal asistido o la cesárea porque se encontró evidencia de certeza muy baja.
Acupuntura comparada con la inyección de agua estéril
No se conoce con certeza si la acupuntura tiene algún efecto sobre la administración de analgesia farmacológica, el parto vaginal asistido o la cesárea, porque se encontró evidencia de certeza muy baja.
Acupresión comparada con un control simulado
No se conoce con certeza si la acupresión reduce la intensidad del dolor en el trabajo de parto (DM ‐1,93; IC del 95%: ‐3,31 a ‐0,55; seis ensayos, 472 mujeres) o el parto vaginal asistido porque se encontró evidencia de certeza muy baja. La acupresión puede tener poco o ningún efecto sobre la administración de analgesia farmacológica (evidencia de certeza baja). La acupresión probablemente reduce la tasa de cesáreas (RR 0,44; IC del 95%: 0,27 a 0,71; cuatro ensayos, 313 mujeres, evidencia de certeza moderada).
Acupresión en comparación con la atención habitual
No se conoce con certeza si la acupresión reduce la intensidad del dolor en el trabajo de parto (DME ‐1,07; IC del 95%: ‐1,45 a ‐0,69; ocho ensayos, 620 mujeres) o si aumenta la satisfacción con el alivio del dolor (DME 1,05; IC del 95%: 0,75 a 1,35; un ensayo, 105 mujeres) porque se encontró evidencia de certeza muy baja. La acupresión puede tener poco o ningún efecto sobre la cesárea (evidencia de certeza baja).
Acupresión en comparación con un control combinado
La acupresión probablemente reduce ligeramente la intensidad del dolor durante el trabajo de parto en comparación con un control combinado (medido en una escala de 0 a 10 con puntuaciones bajas que indican menos dolor) (DME ‐0,42; IC del 95%: ‐0,65 a ‐0,18; dos ensayos, 322 mujeres, evidencia de certeza moderada). No se conoce con certeza si la acupresión tiene algún efecto sobre la administración de analgesia farmacológica (RR 0,94, IC del 95%: 0,71 a 1,25, un ensayo, 212 mujeres), la satisfacción con el parto, el parto vaginal asistido o la cesárea, porque la certeza de la evidencia fue muy baja.
No se encontraron estudios que informaran sobre el sentido de control en el trabajo de parto y solo uno informó sobre la satisfacción con la experiencia del parto.
Conclusiones de los autores
La acupuntura, en comparación con la acupuntura simulada, puede aumentar la satisfacción con el tratamiento del dolor y reducir la administración de analgesia farmacológica. La acupresión en comparación con un control combinado y la atención habitual puede reducir la intensidad del dolor. Sin embargo, para otras comparaciones de la acupuntura y la acupresión no se conocen los efectos sobre la intensidad del dolor y la satisfacción con el alivio del dolor, debido a que la evidencia es de certeza muy baja. La acupuntura puede tener poco o ningún efecto sobre las tasas de cesárea o de parto vaginal asistido. La acupresión probablemente reduce la necesidad de una cesárea en comparación con un control simulado. Es necesario realizar estudios de investigación adicionales de alta calidad que incluyan controles simulados y comparaciones con la atención habitual, y que informen sobre los resultados del sentido de control en el trabajo de parto, la satisfacción con la experiencia del parto o la satisfacción con el alivio del dolor.
PICOs
Resumen en términos sencillos
Acupuntura o acupresión para aliviar el dolor durante el trabajo de parto
Se examinó la evidencia de los ensayos controlados aleatorizados sobre el uso de la acupuntura o la acupresión para ayudar a las mujeres a controlar el dolor durante el trabajo de parto. Esta es una actualización de una revisión publicada por última vez en 2011.
¿Cuál es el problema?
El dolor que presentan las mujeres durante el trabajo de parto puede ser intenso, y la tensión corporal, la ansiedad y el miedo lo empeoran. El dolor es causado por las contracciones del útero, la apertura del cuello del útero y, al final del periodo de dilatación y en el periodo expulsivo, por el estiramiento de la vagina y el suelo pélvico a medida que el feto se mueve a través del canal de parto. El tratamiento efectivo y satisfactorio del dolor se debe individualizar para cada mujer. Las mujeres también pueden utilizar estrategias para tratar de romper el ciclo miedo‐tensión‐dolor y trabajar con el dolor. Trabajar con el dolor implica ofrecer a las mujeres apoyo y ánimo, encontrar posiciones cómodas, inmersión en agua y técnicas de autoayuda.
A muchas mujeres les gustaría pasar su trabajo de parto sin necesidad de fármacos. Las mujeres pueden recurrir a la acupuntura o a la acupresión para ayudar a reducir el dolor y mejorar su tratamiento.
¿Por qué es esto importante?
La acupuntura tiene una larga historia de uso en Asia, incluida China, Corea y Japón. Se necesitan habilidades técnicas para aplicar las agujas en los puntos correctos. La acupresión también tiene sus orígenes en la antigua China. Para aplicar la acupresión, el terapeuta utiliza sus manos y dedos para activar los mismos puntos que en la acupuntura. En ocasiones solo se necesitan unos pocos puntos para aliviar el dolor o provocar una sensación de relajación. En otras ocasiones puede ser necesaria una combinación de puntos para lograr un mayor efecto. Algunas formas de acupresión las aplican profesionales sanitarios capacitados, mientras que otras las puede aplicar el propio individuo como una forma de auto‐masaje.
¿Qué evidencia se encontró?
La búsqueda actualizada en febrero 2019 identificó 17 ensayos nuevos.
Esta revisión incluye ahora 28 ensayos que informan sobre 3960 mujeres, y 27 ensayos proporcionan resultados. Los ensayos compararon la acupuntura o la acupresión con un tratamiento simulado como placebo, ningún tratamiento o la atención habitual para el tratamiento del dolor durante el trabajo de parto. Trece ensayos informaron sobre la acupuntura y 15 sobre la acupresión. En 18 de los 27 ensayos las mujeres estaban en trabajo de parto espontáneo. En otros estudios se puede haber inducido el trabajo de parto.
Ocho estudios aplicaron la medicina tradicional china individualizada, mientras que en la mayoría de los estudios se utilizaron puntos de acupuntura establecidos. Se observó una amplia variación en la forma de aplicar la estimulación (manualmente o con electroestimulación), la duración de la punción, el número de puntos utilizados y la profundidad de la punción. No está claro cuán representativos de la acupuntura en la práctica fueron los tratamientos de los ensayos.
La mayoría de las comparaciones indican un pequeño efecto beneficioso de la acupuntura, aunque la evidencia de apoyo fue limitada. No se conoce con certeza si la acupuntura reduce la intensidad del dolor en comparación con la acupuntura simulada (dos ensayos, 325 mujeres), la atención habitual (cuatro ensayos, 495 mujeres) y ningún tratamiento (un ensayo, 163 mujeres). La certeza de la evidencia fue baja o muy baja. La acupuntura puede aumentar la satisfacción con el alivio del dolor en comparación con la acupuntura simulada (un ensayo, evidencia de certeza moderada). Redujo ligeramente la administración de analgesia farmacológica en comparación con la acupuntura simulada (dos ensayos, 261 mujeres, evidencia de certeza moderada). El uso de la acupresión se asoció con una reducción de la intensidad del dolor en el trabajo de parto en comparación con un control combinado (dos ensayos, 322 mujeres, evidencia de certeza moderada). La acupuntura no pareció tener efecto sobre la necesidad de partos vaginales asistidos o sobre los partos por cesárea, pero la acupresión redujo la tasa de cesáreas en comparación con la acupresión simulada.
¿Qué significa esto?
La acupuntura puede aumentar la satisfacción con el alivio del dolor y reducir la administración de alivio farmacológico para el dolor. La acupresión puede ayudar a aliviar el dolor durante el trabajo de parto, aunque es posible que la reducción del dolor no sea grande. Sin embargo, para otras comparaciones de la acupuntura y la acupresión no se conocen los efectos sobre la intensidad del dolor y la satisfacción con el alivio del dolor, debido a que la evidencia es de certeza muy baja. La acupuntura o la acupresión pueden tener poco o ningún efecto sobre el parto vaginal asistido, pero las mujeres que reciben acupresión tienen menos probabilidades de necesitar una cesárea. Se realizaron estudios en diferentes países, lo que puede reflejar los diferentes estilos de aplicación de la acupuntura. Un punto débil que aún presentan varios ensayos es que se midieron muy pocos resultados y no se informaron resultados de seguridad. Se necesitan más estudios de investigación de calidad alta.
Conclusiones de los autores
Summary of findings
| Acupuncture compared to sham control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with sham control | Risk with acupuncture | |||||
| Pain intensity Lower scores indicate less pain intensity | The mean pain intensity ranged across control groups from 52.94 to 91.4 | The mean pain intensity score in the intervention group was 4.42 lower (12.94 lower to 4.09 higher) | 325 | ⊕⊕⊝⊝ | ||
| Satisfaction with pain relief in labour | Study population | RR 2.38 | 150 | ⊕⊕⊕⊝ | ||
| 387 per 1000 | 920 per 1000 | |||||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.75 | 261 | ⊕⊕⊕⊝ | ||
| 767 per 1000 | 576 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.10 | 261 | ⊕⊝⊝⊝ | ||
| 163 per 1000 | 179 per 1000 | |||||
| Caesarean section | Study population | RR 1.11 | 411 | ⊕⊕⊝⊝ | ||
| 49 per 1000 | 54 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: one study high or unclear risk of bias on six domains. 2 Downgraded one level due to serious inconsistency: substantial heterogeneity present I2 = 87% 3 Downgraded one level due to serious imprecision: small sample size (150) 4 Downgraded one level due to serious risk of bias: one study did not blind participants to group allocation. Should not affect sham arm outcome but blinding integrity not reported. 5 Downgraded one level due to serious inconsistency: substantial heterogeneity present I2 = 72% 6 Downgraded one level for imprecision due to small sample size and wide confidence intervals crossing the line of no effect 7 Downgraded one level for imprecision due to small number of events and wide confidence intervals crossing the line of no effect 8 Downgraded one level due to serious risk of bias: one study did not blind participants to group allocation and two studies at high risk of other bias | ||||||
| Acupuncture compared to usual care for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with acupuncture | |||||
| Pain intensity Mix of NRS and VAS scales so analysed using SMD | The mean pain intensity score in the intervention group was 1.31 standard deviations lower (2.14 lower to 0.49 lower) | 495 | ⊕⊝⊝⊝ | |||
| Satisfaction with pain relief in labour | Study population | RR 1.07 | 343 | ⊕⊕⊝⊝ | ||
| 787 per 1000 | 843 per 1000 | |||||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.72 | 1059 | ⊕⊝⊝⊝ | ||
| 833 per 1000 | 600 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 0.93 | 1217 | ⊕⊕⊝⊝ | ||
| 127 per 1000 | 118 per 1000 | |||||
| Caesarean section | Study population | RR 0.72 | 861 | ⊕⊕⊝⊝ | ||
| 116 per 1000 | 83 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels for very serious risk of bias: two of the three studies had high risk of performance bias and this was likely to influence a self‐reported outcome. 2 Downgraded two levels for very serious inconsistency: considerable heterogeneity present (I2 = 93%) not explained by subgroup analysis. 3 Downgraded two levels for very serious risk of bias: both studies had unclear or high risk of bias related to blinding and this was likely to influence a self‐reported outcome 4 Downgraded two levels for very serious risk of bias: all studies had unclear or high risk of performance bias and this was likely to influence the need for additional analgesia. 5 Downgraded one level for serious inconsistency: substantial heterogeneity (I2 = 70%) which is not explained by subgroups. 6 Downgraded one level for serious risk of bias: five of six studies at unclear or high risk of bias in both performance and detection bias. This may have influenced the outcome. 7 Downgraded one level for serious risk of bias: three of four studies at high or unclear risk of bias in both performance and detection bias. This may have influenced the outcome. 8 Downgraded one level for imprecision due to wide confidence intervals. | ||||||
| Acupuncture compared to no treatment for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with no treatment | Risk with acupuncture | |||||
| Pain intensity Lower scores indicate less pain. | The mean pain intensity in the control group was 7.92 | The mean pain intensity score in the intervention groups was 1.16 lower | ‐ | 163 | ⊕⊝⊝⊝ | |
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Assisted vaginal birth | Study population | RR 0.49 | 163 | ⊕⊝⊝⊝ | ||
| 123 per 1000 | 60 per 1000 | |||||
| Caesarean section | Study population | RR 0.76 | 163 | ⊕⊝⊝⊝ | ||
| 160 per 1000 | 122 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded by two levels for very serious risk of bias: high risk of bias in one domain (blinding for a subjective outcome) and unclear risk of bias in four domains. 2 Downgraded one level for serious imprecision due to a single study providing data with a small sample size (163) 3 Downgraded two levels for very serious imprecision due to a single study, with few events, small sample size and wide confidence intervals providing data | ||||||
| Acupuncture compared to water injection for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with water injection | Risk with acupuncture | |||||
| Pain intensity ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.84 | 128 | ⊕⊝⊝⊝ | ||
| 424 per 1000 | 356 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.60 | 128 | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 97 per 1000 | |||||
| Caesarean section | Study population | RR 1.33 | 128 | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 81 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to very serious risk of bias: high or unclear risk of bias in both blinding performance and detection bias 2 Downgraded two levels due to very serious imprecision: small study (128) with few events and wide confidence intervals crossing the line of no effect | ||||||
| Acupressure compared to sham control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with sham control | Risk with acupressure | |||||
| Pain intensity as measured by a 10 cm visual analogue scale. Lower scores indicate less pain | The mean pain intensity in the control groups was 8.35 | The mean pain intensity score in the intervention group was 1.93 lower (3.31 lower to 0.55 lower) | 472 | ⊕⊝⊝⊝ | ||
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.54 | 75 | ⊕⊕⊝⊝ | ||
| 256 per 1000 | 138 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 3.00 | 100 | ⊕⊝⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Caesarean section | Study population | RR 0.44 | 313 | ⊕⊕⊕⊝ | ||
| 308 per 1000 | 136 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level for serious risk of bias: majority of studies have unclear risk of bias in at least three domains. 2 Downgraded two levels for very serious inconsistency: considerable heterogeneity (I2 = 94%) 3 Downgraded two levels for very serious imprecision: very small sample size (75), small number of events and very wide confidence intervals 4 Downgraded one level for serious risk of bias: single study has high risk of performance bias and an unclear risk of allocation bias 5 Downgraded two levels for very serious imprecision: small sample size (100) and very wide confidence interval and small number of events 6 Downgraded one level for serious risk of bias: all studies have unclear risk of bias in at least three domains. Two studies have high or unclear risk of bias relating to performance bias | ||||||
| Acupressure compared to usual care for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with acupressure | |||||
| Pain intensity as measured by numeric rating scale (NRS) and visual analogue scale (VAS). Lower scores indicate less pain. | The mean pain intensity was 8.44 | The mean pain intensity score in the intervention group was 1.07 standard deviations lower (1.45 lower to 0.69 lower). | 620 | ⊕⊝⊝⊝ | The use of acupressure would result in a pain score approximately 2 cm lower on a 10 cm VAS or 2 points on a numeric rating scale compared to usual care. | |
| Satisfaction with pain relief | The mean satisfaction score with pain relief in the control group was 1.6 | The mean satisfaction with pain relief score was 1.05 higher (0.75 higher to 1.35 higher) | 105 | ⊕⊝⊝⊝ | ||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Assisted vaginal birth ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Caesarean section | Study population | RR 0.82 | 391 | ⊕⊕⊝⊝ | ||
| 241 per 1000 | 198 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: majority of included studies have high or unclear risk of bias relating to performance and detection bias 2 Downgraded two levels due to very serious inconsistency: considerable heterogeneity (I2 = 75%) 3 Downgraded two levels due to very serious risk of bias: single study at high risk of bias for selection, performance and detection bias. Very likely to have influenced the outcome 4 Downgraded one level due to serious imprecision: small sample size (105) 5 Downgraded one level due to serious risk of bias: two of the four studies included were at high risk of performance and detection bias, two studies were at high or unclear risk of selection bias and three at high or unclear risk of incomplete outcome data 6 Downgraded one level due to serious imprecision: wide confidence intervals incorporating both benefit and harm | ||||||
| Acupressure compared to combined control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with combined control | Risk with acupressure | |||||
| Pain intensity One study used VAS pain score on scale 1 ‐ 100 mm One study used VAS pain score on scale 1 ‐ 10 mm ‐ the mean | The mean pain intensity score in the intervention group was 0.42 standard deviations lower (0.65 lower to 0.18 lower) | 322 | ⊕⊕⊕⊝ | |||
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth | The mean satisfaction score with childbirth in the control group was 80.2 | The mean satisfaction score in the intervention group was 4.8 higher | ‐ | 212 | ⊕⊝⊝⊝ | |
| Use of pharmacological analgesia | Study population | RR 0.94 | 212 | ⊕⊝⊝⊝ | ||
| 525 per 1000 | 493 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 0.81 | 212 | ⊕⊝⊝⊝ | ||
| 156 per 1000 | 126 per 1000 | |||||
| Caesarean section | Study population | RR 0.48 | 212 | ⊕⊝⊝⊝ | ||
| 206 per 1000 | 99 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: both studies have unclear risk of bias for performance bias, possible effect on this outcome 2 Downgraded one level due to serious risk of bias: single study has unclear risk of performance bias, likely to effect this outcome 3 Downgraded two levels due to very serious imprecision: wide confidence interval greater than 0.25 on either side of the line of no effect and small sample size 4 Downgraded two levels for very serious imprecision: wide confidence interval encompassing both benefit and harm and small sample size | ||||||
Antecedentes
Esta revisión es una de una serie de revisiones Cochrane que examinan el control del dolor en el trabajo de parto. Una versión anterior de esta revisión contribuyó a un resumen de revisiones sistemáticas del tratamiento del dolor en las mujeres en trabajo de parto (Jones 2012) y compartió un protocolo genérico (Jones 2011). Esta revisión es una actualización de una revisión publicada por última vez en 2011 (Smith 2011b).
Descripción de la afección
El trabajo de parto representa un reto fisiológico y psicológico para las mujeres. A medida que el trabajo de parto se hace más inminente, puede ser un momento de emociones conflictivas; el miedo y la aprensión pueden ir acompañados de excitación y felicidad. La tensión, la ansiedad y el miedo son factores que contribuyen a la percepción del dolor por las mujeres y pueden también afectar el trabajo de parto y la experiencia del nacimiento del niño. El dolor asociado con el trabajo de parto se ha descrito como una de las formas de dolor más intensas que se puedan experimentar (Melzack 1984), aunque algunas mujeres no presentan dolor intenso durante el trabajo de parto. El trabajo de parto consiste en tres etapas, relacionadas con la dilatación del cuello uterino, el parto del feto y el alumbramiento de la placenta. La fase latente es la parte inicial del trabajo de parto en la que hay contracciones irregulares y el cuello del útero comienza a ablandarse y dilatarse. El periodo de dilatación del trabajo de parto consiste en contracciones regulares de fuerza y frecuencia crecientes, acompañadas de una dilatación cervical más significativa de al menos 4 a 6 cm. La transición se puede observar entre los 7 y los 8 cm y la dilatación completa. El periodo expulsivo del trabajo de parto comienza desde la dilatación cervical completa y llega hasta el parto del feto. El periodo de alumbramiento consiste en la expulsión de la placenta.
El dolor que presentan las mujeres durante el trabajo de parto es producido por las contracciones uterinas, la dilatación del cuello del útero y al final de la primera etapa y durante la segunda, por la dilatación de la vagina y del piso pélvico para acomodar al feto. Existen diferentes filosofías para el tratamiento del dolor, que implican estrategias para prevenir lo que se ha descrito como el ciclo miedo‐tensión‐dolor (Dick‐Read 2004; Dowswell 2009). Dick‐Read 2004, un partidario del "parto natural", indicó que el temor y la ansiedad pueden producir tensión muscular, lo que da lugar a un aumento de la percepción del dolor. La teoría del control de la puerta del dolor, propuesta por primera vez por Melzack y Wall en 1965, indica que el dolor se puede compensar con otras sensaciones "más grandes" o predominantes, como el roce o la presión sobre una lesión para reducir la sensación de dolor (Melzack 1965). Melzack y colegas propusieron además la teoría de la neuromatriz del dolor, que introduce la noción de que el dolor es multidimensional, y que en la intensidad del dolor influyen muchos factores, incluidos los procesos sensoriales, emocionales y cognitivos, entre ellos las experiencias y la memoria (Melzack 2004). En el trabajo de parto, la teoría del dolor incorpora elementos de la teoría de la puerta de control del dolor, pero también las experiencias anteriores, los factores culturales, el estado emocional, el aporte cognitivo, la regulación del estrés y los sistemas inmunes, así como el aporte sensorial inmediato (Trout 2004). Sin embargo, la eliminación completa del dolor no significa necesariamente que la experiencia del nacimiento sea más satisfactoria para la mujer (Dickenson 2003). Un estudio de seguimiento a los cinco años del parto encontró que las mujeres que recibieron epidurales fueron menos positivas sobre el parto cinco años después (Maimburg 2016). La literatura indica que la satisfacción con el parto está significativamente vinculada con el sentido de agencia y la participación de las mujeres en la toma de decisiones durante el embarazo y el parto (Hodnett 2002; Hollins Martin 2013; Hotelling 2013; Howarth 2010). El control efectivo y satisfactorio del dolor se debe individualizar para cada mujer y pueden influir dos paradigmas, el trabajo de parto con dolor o el alivio del dolor (Leap 2010). El paradigma del trabajo de parto con dolor incluye la creencia de que hay efectos beneficiosos a largo plazo en promover el parto normal, y de que el dolor desempeña una función importante en este proceso. Centrado en la mediación hormonal natural del trabajo de parto de la mujer, el enfoque de trabajar con el dolor ofrece apoyo y aliento a las mujeres, recomienda el uso de la inmersión en agua, posiciones cómodas y técnicas de autoayuda para hacer frente a los dolores normales del trabajo de parto y facilitar las hormonas normales del trabajo de parto. El paradigma del alivio del dolor se caracteriza por la creencia de que ninguna mujer necesita padecer dolor durante el trabajo de parto y a las pacientes se les ofrecen diversos analgésicos.
También es importante tener en cuenta los dos conceptos de eficacia y efectividad al evaluar los resultados de los estudios de investigación para el tratamiento del dolor del trabajo de parto. Los ensayos de eficacia están diseñados para mostrar el grado de eficacia de un tratamiento o componente específico de una intervención en circunstancias experimentales ideales, y a menudo utilizan placebo o una comparación simulada. Con frecuencia, las escalas de dolor se utilizan para evaluar la efectividad de la acupuntura o las intervenciones de acupresión, en especial cuando se evalúan tratamientos que proporcionan "alivio del dolor". La escala más utilizada es la escala analógica visual (EAV), que evalúa la reducción de las puntuaciones de dolor de 10 o 100, en respuesta a la intervención. Sin embargo, los ensayos de efectividad están diseñados para evaluar el efecto de toda la terapia en una población general, y a menudo se comparan con la atención habitual. Cuando se considera el "paradigma de trabajo con el dolor", la efectividad de una intervención se puede indicar mediante una reducción del tratamiento farmacológico para el dolor y de las puntuaciones de satisfacción, y es posible que no se refleje necesariamente en las puntuaciones de dolor (MacPherson 2008).
Descripción de la intervención
La acupuntura tiene una larga historia de uso en Asia, incluidos China, Corea y Japón. La teoría de la Medicina Tradicional China (MCT), donde la acupuntura es una de las formas más importantes, describe que el estado de salud se mantiene a través de un equilibrio de energía en el cuerpo. La acupuntura realizada como parte de la MTC es una intervención compleja que incluye no solo la habilidad técnica para la inserción de agujas, sino el desarrollo de una relación terapéutica, la formulación de un diagnóstico, la asesoría sobre el estilo de vida y a menudo la administración de cointervenciones como gua sha (rascado), tuina (masaje), moxibustión (un tipo de medicina china que incluye quemar una hierba cerca de la piel) o estimulación eléctrica. En la práctica clínica el uso de cointervenciones es bastante frecuente, aunque la acupuntura es el foco primario. La acupuntura se realiza mediante la inserción de agujas finas en diferentes partes del cuerpo para corregir el desequilibrio de energía en el mismo. La MTC y la acupuntura clásica explican la enfermedad y la función fisiológica según los conceptos teóricos del Yin y el Yang y los Cinco Elementos (Beinfield 1991; Hicks 2011; Maciocia 2015). La acupuntura de cinco elementos se basa en los textos clásicos de medicina china y se ha desarrollado para su aplicación en un contexto occidental con protocolos de diagnóstico y tratamiento diferentes a los utilizados en Asia (Hicks 2011). Una aplicación médica occidentalizada de la acupuntura implica el uso de acupuntura mediante puntos gatillo, puntos segmentarios y puntos de fórmula utilizados habitualmente. La terapia auricular, una forma de acupuntura occidental, implica el uso del oído para realizar un diagnóstico y, posteriormente, insertar agujas en puntos del mismo. La acupuntura médica puede consistir en la aplicación de la acupuntura basada en los principios de la neurofisiología y de la anatomía, en lugar de los principios y la filosofía de la MTC. El estilo y el enfoque de la acupuntura caracterizan la selección de los puntos de acupuntura y los parámetros de tratamiento relacionados administrados en la práctica clínica y los estudios de investigación.
La acupresión tiene sus orígenes en la China antigua (Beinfield 1991), y se basa en el mismo paradigma que se describe para la acupuntura. Cuando se aplica la acupresión, el terapeuta utiliza las manos y los dedos para activar los mismos puntos que cuando se aplica la acupuntura. En ocasiones solo es necesario tocar algunos puntos para aliviar el dolor o provocar un sentimiento de relajación. En otras circunstancias se utilizarán combinaciones de puntos para lograr un mayor efecto. Hay varias formas de acupresión que se basan en el mismo conocimiento y sistema filosófico de otras formas de medicina asiática tradicional. Algunos de estos sistemas los aplican profesionales sanitarios capacitados y otros los puede aplicar el propio individuo mediante la presión o la activación de los puntos.
El uso de la medicina complementaria y alternativa (MCA), incluida la acupuntura y la acupresión, se ha hecho popular entre los consumidores de todo el mundo. Los estudios indican que entre el 36% y el 62% de los adultos en los países industrializados utilizan alguna forma de medicina complementaria para prevenir o tratar problemas relacionados con la salud (Barnes 2004). Las mujeres en edad reproductiva son las que más frecuentemente utilizan los tratamientos complementarios; casi la mitad (49%) informa que los utilizan (Eisenberg 1998). En un estudio australiano reciente se informó que las mujeres fueron las que más utilizaron la medicina complementaria y alternativa, y que una proporción significativa de mujeres utilizaron dichas terapias durante el embarazo (Steel 2014). Una revisión reciente de 14 estudios con tamaños de muestra grandes (N > 200) sobre el uso de la MCA en el embarazo identificó una tasa de prevalencia que varió del 1% al 87% (en nueve la tasa estuvo entre el 20% y el 60%) (Adams 2009). La revisión identificó el uso de varios tratamientos complementarios que incluyen la acupuntura y la acupresión, la aromaterapia, el masaje, el yoga, la homeopatía y la atención quiropráctica. La revisión también mostró que muchas embarazadas habían utilizado más de un producto o servicio complementario (Adams 2009). A muchas mujeres les gustaría evitar los métodos farmacológicos o invasivos para aliviar el dolor durante el trabajo de parto, lo que puede contribuir a la popularidad de los métodos complementarios para el control del dolor (Steel 2014). Un estudio australiano reciente también mostró que las mujeres y las parejas a las que se les enseñó una variedad de técnicas de terapia complementaria en una clase de educación prenatal, utilizaron entre tres y cuatro terapias diferentes para el control del dolor durante el trabajo de parto (Levett 2016b).
De qué manera podría funcionar la intervención
La acupuntura se ha utilizado para tratar varias afecciones dolorosas y se han formulado varias teorías sobre cómo puede funcionar. Se ha propuesto que la acupuntura puede modificar la percepción del dolor o alterar las funciones fisiológicas (Stux 1995). La mayoría de los puntos de acupuntura están conectados o localizados cerca de estructuras neurales, lo que indica que la acupuntura estimula el sistema nervioso (Zullo 2017). Desde la perspectiva de la acupuntura occidental, los puntos seleccionados se basan en la inervación del órgano objetivo, p.ej. el útero. La activación de aferentes musculares a este nivel segmentario transmite señales a la médula espinal y al sistema nervioso central. Durante la estimulación con agujas de los puntos habituales de acupuntura para el dolor, las señales se transmiten a la médula espinal y, a través de las vías aferentes, al cerebro medio. La percepción del dolor surge del flujo resultante y de la integración de esta información entre áreas cerebrales específicas a través de cambios neuroquímicos y hormonales, y puede dar lugar a un cambio en la percepción del dolor. Otra teoría indica que la acupuntura estimula al cuerpo para producir endorfinas, que reducen el dolor (Pomeranz 1989). Otras sustancias que alivian el dolor, llamadas opiáceos, pueden ser liberadas dentro del cuerpo durante el tratamiento con acupuntura (Ng 1992). Es probable que en el efecto total de la acupuntura estén involucrados mecanismos segmentarios y centrales de la acupuntura (Stener‐Victorin 2006).
En un meta‐análisis realizado por Chae 2013, los autores revisaron 28 estudios de IRMf (imágenes de resonancia magnética funcional) de acupuntura y estimulación táctil, y encontraron que la estimulación de la acupuntura mostró patrones comunes de activación y desactivación en el cerebro, y que el tacto mostró estos mismos patrones, pero no fue significativo. Los patrones de desactivación observados en los estudios se correlacionaron con áreas del cerebro asociadas a una menor percepción del dolor y la ansiedad, así como a la superposición con el área del cerebro conocida como la "matriz del dolor" en el cerebro. Los estudios de investigación realizados por Anderson 2012 indican que la acupuntura funciona mediante la regulación de la interacción de las dos ramas del sistema nervioso autónomo, el simpático y el parasimpático.
Por qué es importante realizar esta revisión
Las mujeres están interesadas en utilizar formas complementarias de atención que las ayuden a controlar el dolor durante el trabajo de parto. Es importante examinar la eficacia, la efectividad y la seguridad de formas de tratamiento no evaluadas adecuadamente, para permitir que las mujeres, los profesionales sanitarios y los elaboradores de políticas tomen decisiones fundamentadas acerca de la atención. Se han realizado varios ensayos clínicos y un resumen de las revisiones actuales (Levett 2014) para estudiar la eficacia de la acupuntura para el dolor durante el trabajo de parto, aunque aún no está claro si la evidencia existente es suficientemente rigurosa para establecer una conclusión definitiva.
Esta revisión es una de una serie de revisiones Cochrane que examinan el control del dolor en el trabajo de parto. Una versión anterior de esta revisión contribuyó a un resumen de revisiones sistemáticas del tratamiento del dolor en las mujeres en trabajo de parto (Jones 2012) y compartió un protocolo genérico (Jones 2011). Esta revisión es una actualización de una revisión publicada por última vez en 2011 (Smith 2011b).
Objetivos
Examinar los efectos de la acupuntura y la acupresión para el tratamiento del dolor durante el trabajo de parto.
Métodos
Criterios de inclusión de estudios para esta revisión
Tipos de estudios
Solo ensayos controlados aleatorizados (ECA) . Se incluyeron los estudios informados como resúmenes si tenían suficiente información para permitir la evaluación del riesgo de sesgo. Se consideraron elegibles para inclusión los ECA grupales, aunque no se identificaron ensayos de este tipo. Los ensayos cuasialeatorizados y los ensayos cruzados no fueron elegibles para inclusión.
Tipos de participantes
Mujeres en trabajo de parto espontáneo o inducido, independientemente de la paridad y de la edad gestacional. Se incluyeron estudios de mujeres con embarazos únicos o múltiples.
Tipos de intervenciones
La versión anterior de esta revisión (Smith 2011b) contribuyó a un resumen de revisiones sistemáticas de intervenciones para el tratamiento del dolor en el trabajo de parto (Jones 2012), y compartió un protocolo genérico (Jones 2011). Para evitar la duplicación, los diferentes métodos de control del dolor se han listado en un orden específico, del uno al 15. Las revisiones individuales que se centran en intervenciones particulares solo incluyen comparaciones con la intervención por encima de ella en la lista. La lista es la siguiente.
-
Placebo/ningún tratamiento
-
Hipnosis (Madden 2016)
-
Biorretroalimentación (Barragán 2011)
-
Inyección de agua estéril intracutánea o subcutánea (Derry 2012)
-
Inmersión en agua (Cluett 2018)
-
Aromaterapia (Smith 2011a)
-
Técnicas de relajación (yoga, música, audio) (Smith 2018a)
-
Acupuntura o acupresión (esta revisión)
-
Métodos manuales (masaje, reflexología) (Smith 2018b)
-
Neuroestimulación eléctrica transcutánea (TENS) (Dowswell 2009)
-
Analgesia inhalada
-
Opiáceos (Smith 2018c)
-
Fármacos no opiáceos (Othman 2012)
-
Bloqueos nerviosos anestésicos locales
-
Epidural (incluida espinal y epidural combinadas) (Anim‐Somuah 2018; Simmons 2012)
Por lo tanto, esta revisión incluye comparaciones de cualquier tipo de acupuntura o acupresión comparada con otro tipo de acupuntura o acupresión, así como cualquier tipo de acupuntura o acupresión comparada con: 1. placebo/ningún tratamiento; 2. hipnosis; 3. biorretroalimentación; 4. inyección de agua estéril intracutánea o subcutánea; 5. inmersión en agua; 6. aromaterapia; 7. técnicas de relajación (yoga, música, audio).
Tipos de medida de resultado
Resultados primarios
Efectos de las intervenciones
-
Intensidad del dolor (según la definición de los autores de los ensayos)
-
Satisfacción con el alivio del dolor (según la definición de los autores de los ensayos)
-
Sensación de control en el trabajo de parto (según la definición de los autores)
-
Satisfacción con la experiencia del parto
-
Uso de productos farmacológicos para el alivio del dolor
Seguridad de las intervenciones
-
Efecto (negativo) sobre la interacción de la madre y el recién nacido
-
Lactancia materna (en puntos temporales específicos)
-
Parto vaginal asistido
-
Cesárea
-
Efectos secundarios (para la madre y el recién nacido; revisión específica)
-
Ingreso en una unidad de cuidados especiales neonatales / unidad de cuidados intensivos neonatales (como lo definieron los autores del ensayo)
-
Puntuación de Apgar menor a siete a los cinco minutos
-
Resultados infantiles deficientes en el seguimiento a largo plazo (como los definieron los autores de los ensayos)
Otros resultados
-
Coste (según la definición de los autores)
Resultados secundarios
Maternal
Duración del trabajo de parto; modo del parto; necesidad de estimulación con oxitocina; trauma perineal (definido como episiotomía e incidencia de desgarro de segundo o tercer grado); pérdida de sangre materna (hemorragia posparto definida como mayor de 500 ml); relajación; ansiedad.
Neonatales
Necesidad de ventilación mecánica; encefalopatía neonatal.
Métodos de búsqueda para la identificación de los estudios
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Búsquedas electrónicas
For this update, we searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (25 February 2019).
The Register is a database containing over 25,000 reports of controlled trials in the field of pregnancy and childbirth. It represents over 30 years of searching. For full current search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link.
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by their Information Specialist and contains trials identified from:
-
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
-
weekly searches of MEDLINE (Ovid);
-
weekly searches of Embase (Ovid);
-
monthly searches of CINAHL (EBSCO);
-
handsearches of 30 journals and the proceedings of major conferences;
-
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results are screened by two people and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set that has been fully accounted for in the relevant review sections (Included studies; Excluded studies; Studies awaiting classification; Ongoing studies).
In addition, we searched the Cochrane Central Register of Controlled Trials (the Cochrane Library 2019, Issue 1), MEDLINE (1966 to 25 Febriuary 2019), and CINAHL (1980 to 25 February 2019) using a combination of subject headings and text words. See Appendix 1.
We also searched ClinicalTrials.gov (25 February 2019) and the WHO International Clinical Trials Registry Platfory (ICTRP) (25 February 2019) for unpublished, planned and ongoing trial reports using the search methods detailed in Appendix 2.
Búsqueda de otros recursos
We searched the reference lists of all included studies.
We did not apply any language or date restrictions.
Obtención y análisis de los datos
For methods used in the previous version of this review, see Smith 2011b.
For this update, the following methods were used for assessing the 79 reports that were identified as a result of the updated search and we also reassessed the five trial reports in the Studies awaiting classification and the two in Ongoing studies sections of Smith 2011b.
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Selección de los estudios
Two review authors independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion or, if required, we consulted the third review author.
Extracción y manejo de los datos
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third review author. Data were entered into Review Manager software (RevMan 2014) and checked for accuracy.
When information regarding any of the above was unclear, we contacted authors of the original reports to provide further details.
Evaluación del riesgo de sesgo de los estudios incluidos
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreement was resolved by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
-
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
-
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
-
unclear risk of bias when it was unclear, or there was insufficient reporting.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
-
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
-
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
-
unclear risk of bias or there was insufficient reporting.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
-
low, high or unclear risk of bias for participants;
-
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
-
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as:
-
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
-
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
-
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
-
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
-
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
-
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). With reference to (1) to (6) above, we planned to assess the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. In future updates, we will explore the impact of the level of bias through undertaking sensitivity analyses ‐ see Sensitivity analysis.
Assessment of the certainty of the evidence using the GRADE approach
For this update, the certainty of the evidence was assessed using the GRADE approach as outlined in the GRADE Handbook in order to assess the certainty of the body of evidence relating to the following outcomes for the main comparisons: acupuncture compared to sham control; acupuncture compared to usual care; acupuncture compared to no treatment; acupuncture compared to water injection; acupressure compared to sham control; acupressure compared to usual care; acupressure compared to combined control.
-
Pain intensity (as defined by trialists)
-
Satisfaction with pain relief (as defined by trialists)
-
Sense of control in labour (as defined by trialists)
-
Satisfaction with childbirth experience
-
Use of pharmacological pain relief
-
Assisted vaginal birth
-
Caesarean section
These outcomes have been included in our 'Summary of findings' tables (Summary of findings table 1; Summary of findings table 2; Summary of findings table 3; Summary of findings table 4; Summary of findings table 5; Summary of findings table 6; Summary of findings table 7).
We used the GRADEpro Guideline Development Tool to import data from Review Manager 5.3 (RevMan 2014) in order to create 'Summary of findings’ tables. A summary of the intervention effect and a measure of certainty for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the certainty of the body of evidence for each outcome. The evidence can be downgraded from 'high certainty' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Assessment of the quality of the acupuncture intervention delivered
We assessed the quality of the acupuncture or acupressure intervention in published journal articles using the NICMAN scale (Smith 2017). The NICMAN scale was developed to assess the quality of the acupuncture delivered in a clinical trial, and is designed to be used in combination with the STRICTA reporting guidelines (MacPherson 2010). This scale assesses and scores the following: the rationale behind the point selection, the qualifications and experience of the practitioner delivering the intervention, the adequacy of the number of treatment sessions, and the reporting of vital components of the acupuncture practice itself such as needle depth, diameter and stimulation. Higher scores indicate improved quality of the acupuncture intervention delivered, but there is no cut‐off for a 'high' versus 'low' quality score on the NICMAN scale. Each trial was independently scored out of 23 by two review authors (CS, KL, MA). Any discrepancies were resolved by discussion. If this was not reached a third review author (KL, CS or MA) decided on the final score.
Medidas del efecto del tratamiento
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
We used the mean difference if outcomes were measured in the same way between trials. We used the standardised mean difference to combine trials that measured the same outcome, but used different methods.
Cuestiones relativas a la unidad de análisis
Cluster‐randomised trials
If we had identified cluster‐randomised trials, we planned to include them in the analyses along with individually‐randomised trials. If such trials are identified in future updates of the review, we will adjust their sample sizes using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions using an estimate of the intra‐cluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely. We will also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation unit.
Cross‐over trials
Cross‐over trials are not a suitable design for trials looking at interventions in labour and have been excluded.
Other unit of analysis issues
If we had identified trials with multiple arms, we planned that data from both treatment arms would be combined into one group. For studies with a sham control and no treatment control group, the shared intervention was divided evenly between groups and the weighting adjusted as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Manejo de los datos faltantes
For included studies, levels of attrition were noted. In future updates, if more eligible studies are included, the impact of including studies with high levels of missing data in the overall assessment of treatment effect will be explored by using sensitivity analysis.
For all outcomes, analyses were carried out, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Evaluación de la heterogeneidad
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if the I² was greater than 30% and either the Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. In future updates, if we identify substantial heterogeneity (above 30%), we plan to explore it by pre‐specified subgroup analysis.
Evaluación de los sesgos de notificación
In future updates, if there are 10 or more studies in the meta‐analysis we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Síntesis de los datos
We carried out statistical analysis using the Review Manager software (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar.
If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary was treated as the average range of possible treatment effects and we discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we did not combine trials. Where we used random‐effects analyses, the results were presented as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Análisis de subgrupos e investigación de la heterogeneidad
Had we identified substantial heterogeneity, we planned to investigate it using subgroup analyses and sensitivity analyses. However, there were too few data included in any one comparison to carry out meaningful subgroup analysis.
In future updates, if possible we will carry out the following subgroup analyses for primary outcomes.
-
Spontaneous labour versus induced labour
-
Nulliparous versus multiparous
-
Term versus preterm
-
Continuous support in labour versus no continuous support
We will assess subgroup differences by interaction tests available within RevMan. We will report the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
We did carry out subgroup analysis by type of acupuncture: manual acupuncture versus electro‐acupuncture, but there was not enough data in any one subgroup to demonstrate any differential effects.
Análisis de sensibilidad
Where subgroup analysis failed to explain the heterogeneity, we planned to analyse the data using the random‐effects model. A priori, we planned to perform sensitivity analyses on results to look at the possible contribution of: (1) differences in methodological quality, with trials of high quality (low risk of bias) compared to all trials; and (2) publication bias by country. If publication bias was present we planned to undertake a sensitivity analysis excluding trials from countries where there was a greater publication bias.
Results
Description of studies
Results of the search
See Figure 1.

Study flow diagram.
For this update, we assessed 165 new records from the search. We also reassessed five studies that were awaiting classification and three ongoing studies from the previous version of the review. We had 112 records after removal of duplicates. From these, we screened out 33, leaving us with 79 trial reports to assess. Of these, we included 17 new studies (30 reports), added an additional report to an already included study, and excluded 26 (29 reports) Fifteen new studies are awaiting further classification (Studies awaiting classification) and three are ongoing (Ongoing studies).
One study (Ziaei 2006) had been previously included in a previous update (Smith 2011b). In this update it was moved to Studies awaiting classification due to having an unclear risk of bias across all domains and the authors had not responded to requests for further information.
The review included 28 trials of 3960 women, with data contributing to data and analysis from 27 trials of 3930 women.
Included studies
Study design
All studies were parallel design. Eleven studies had two groups (Calik 2014; Hamidzadeh 2012; Hamlaci 2017; Hantoushzadeh 2007; Kashanian 2010; Lee 2004; Martensson 2008; Nesheim 2003; Sehhatie‐Shafaie 2013; Skilnand 2002; Tjung 2008). Fourteen studies had three groups (Borup 2009; Chung 2003; Dabiri 2014; Dong 2015; Hjelmstedt 2010; Kordi 2010; Ma 2011; Mafetoni 2016; Mafetoni 2016a; Mansouri 2018; Ozgoli 2016; Qu 2007; Salehian 2011; Vixner 2014), and three studies had four arms (Huang 2008; Mackenzie 2011; Ramnero 2002). Comparative and control groups varied. Thirteen studies used placebo or sham controls (Chung 2003; Dabiri 2014; Hantoushzadeh 2007; Hjelmstedt 2010; Kashanian 2010; Kordi 2010; Lee 2004; Ma 2011; Mackenzie 2011; Mafetoni 2016; Skilnand 2002; Sehhatie‐Shafaie 2013; Skilnand 2002). Placebo, sham, or minimal acupuncture techniques varied between invasive and non‐invasive techniques. Comparison with usual care comprised of medication used in four studies (Borup 2009; Huang 2008; Tjung 2008; Vixner 2014). Other control groups included unspecified care or usual care in five studies (Dong 2015; Hjelmstedt 2010; Mafetoni 2016a; Nesheim 2003; Ramnero 2002). Huang 2008 used transcutaneous electrical nerve stimulation (TENS) and a breathing group; Martensson 2008 used sterile water injections, and comparison with no intervention was reported in two studies (Calik 2014; Qu 2007). Ozgoli 2016 used two active groups and a usual care group.
Sample sizes
Studies included in the review had sample sizes ranging from 30 (Mafetoni 2016a) to 607 (Borup 2009).
Study location and sources of women
Nine studies were undertaken in Iran (Dabiri 2014; Hamidzadeh 2012; Hantoushzadeh 2007; Kashanian 2010; Kordi 2010; Mansouri 2018; Ozgoli 2016; Salehian 2011; Sehhatie‐Shafaie 2013), four studies were undertaken in China (Dong 2015; Huang 2008; Ma 2011; Qu 2007), three studies undertaken in Sweden (Martensson 2008; Ramnero 2002; Vixner 2014), two each in Norway (Nesheim 2003; Skilnand 2002), Brazil (Mafetoni 2016; Mafetoni 2016a), and Turkey (Calik 2014; Hamlaci 2017), and one study each in Denmark (Borup 2009), India (Hjelmstedt 2010), Korea (Lee 2004) Phillipines (Tjung 2008); Taiwan (Chung 2003) and the UK (Mackenzie 2011).
Participants
Seventeen studies recruited both nulliparous and multiparous women (Borup 2009; Chung 2003; Dabiri 2014; Dong 2015; Hamidzadeh 2012; Hamlaci 2017; Kordi 2010; Lee 2004; Ma 2011; Mafetoni 2016; Mafetoni 2016a; Martensson 2008; Nesheim 2003; Ramnero 2002; Sehhatie‐Shafaie 2013; Skilnand 2002; Vixner 2014). Nulliparous only women were recruited in eight studies (Calik 2014; Hantoushzadeh 2007; Hjelmstedt 2010; Kashanian 2010; Mackenzie 2011; Mansouri 2018; Ozgoli 2016; Salehian 2011). Parous women only were recruited in two studies (Huang 2008; Qu 2007). It was unclear in one study (Tjung 2008). Women were recruited in spontaneous labour in 19 studies (Calik 2014; Chung 2003; Dabiri 2014; Hamidzadeh 2012; Hamlaci 2017; Hantoushzadeh 2007; Kordi 2010; Mafetoni 2016; Mafetoni 2016a; Martensson 2008; Mansouri 2018; Nesheim 2003; Ozgoli 2016; Qu 2007; Ramnero 2002; Sehhatie‐Shafaie 2013; Skilnand 2002; Tjung 2008; Vixner 2014). Two studies recruited women in both spontaneous and induced labour (Borup 2009; Hjelmstedt 2010), and one study reported on only induced labour (Mackenzie 2011). Reporting on the onset of labour was unclear in six studies (Dong 2015; Huang 2008; Kashanian 2010; Lee 2004; Ma 2011; Salehian 2011).
The intervention was administered at term for the majority of trials studies except Huang 2008 where details were not reported. There were no studies specifically for pre‐term labour.
We included labouring women either in spontaneous or induced labour, irrespective of parity and pre‐term or post date status. We included women with singleton or multiple pregnancies.
Types of intervention
Fifteen studies used acupressure (Calik 2014; Chung 2003; Dabiri 2014; Hamidzadeh 2012; Hamlaci 2017; Hjelmstedt 2010; Kashanian 2010; Kordi 2010; Lee 2004; Mafetoni 2016; Mafetoni 2016a; Mansouri 2018; Ozgoli 2016; Salehian 2011; Sehhatie‐Shafaie 2013) and 13 studies used acupuncture (Borup 2009; Dong 2015; Hantoushzadeh 2007; Huang 2008; Ma 2011; Mackenzie 2011; Martensson 2008; Nesheim 2003; Qu 2007; Ramnero 2002; Skilnand 2002; Tjung 2008; Vixner 2014) (includes manual and electro‐acupuncture). Acupuncture and acupressure varied in point selection, frequency of treatment and number of treatments, with commonly used points included SP6, LI4, BL23, BL32, HT7, GB34, LR3, ST36, PC6, BL67. A fixed set of acupuncture points only were administered in four studies (Dong 2015; Ma 2011; Mackenzie 2011; Qu 2007). A fixed set of acupressure points was used in 15 studies (Calik 2014; Chung 2003; Dabiri 2014; Hamidzadeh 2012; Hamlaci 2017; Hjelmstedt 2010; Kashanian 2010; Kordi 2010; Lee 2004; Mafetoni 2016; Mafetoni 2016a; Mansouri 2018; Ozgoli 2016; Salehian 2011; Sehhatie‐Shafaie 2013). Individualised treatment was administered in eight studies (Borup 2009; Hantoushzadeh 2007; Huang 2008; Martensson 2008; Nesheim 2003; Ramnero 2002; Skilnand 2002; Vixner 2014). Auriculotherapy, ear acupressure was used in one trial (Mafetoni 2016a). SeeCharacteristics of included studies.
Outcome measures
Pain intensity during labour was measured by visual analogue scale (VAS) in 25 studies (Borup 2009; Calik 2014; Chung 2003; Dabiri 2014; Dong 2015; Hamidzadeh 2012; Hamlaci 2017; Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Kashanian 2010; Kordi 2010; Lee 2004; Ma 2011; Mackenzie 2011; Mafetoni 2016; Mafetoni 2016a; Martensson 2008; Mansouri 2018; Nesheim 2003; Salehian 2011; Sehhatie‐Shafaie 2013; Skilnand 2002; Tjung 2008;Vixner 2014) and by a 0 to 10 numeric rating scale (NRS) in three studies (Ozgoli 2016; Qu 2007; Ramnero 2002). Two studies (Calik 2014; Vixner 2014) did not report pain intensity outcome data in a format that allowed them to be included in the meta‐analysis, so these were reported narratively. When pain intensity scores were given at multiple time points, the last time point was used. Standardised mean difference (SMD) was used when combining VAS and NRS pain scores. Use of pharmacological analgesia was reported by 26 studies.
Length of labour was reported in eight studies (Dong 2015; Hamidzadeh 2012; Hamlaci 2017; Kashanian 2010; Lee 2004; Ma 2011; Salehian 2011; Vixner 2014), and mode of birth (spontaneous vaginal birth, assisted vaginal birth or caesarean section) was reported by 16 studies (Borup 2009; Calik 2014; Hamidzadeh 2012; Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Kashanian 2010; Mackenzie 2011; Martensson 2008; Mafetoni 2016a; Nesheim 2003; Ozgoli 2016; Ramnero 2002; Skilnand 2002; Tjung 2008; Vixner 2014). Maternal outcomes (satisfaction, sense of control, anxiety, childbirth experience and acceptability of the intervention) were reported in 12 studies (Borup 2009; Chung 2003; Hamidzadeh 2012; Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Lee 2004; Martensson 2008; Ozgoli 2016; Qu 2007; Ramnero 2002; Vixner 2014), and clinical outcomes were reported in the majority of studies, however some are reported narratively as they were presented in a format that was not consistent with the review (Qu 2007).
Satisfaction with pain relief or satisfaction with childbirth was reported either via a Likert scale or via a Yes/No response to a question relating to sufficient pain relief. To provide a dichotomous outcome for satisfaction when recorded via a Likert scale we combined the two most favourable categories (e.g. very satisfied and satisfied or very good and good) as a 'Yes' response, while neutral or negative categories were characterised as a 'No' response.
Dates of trials
The majority of the trials took place between the year 1999 to 2013: Borup 2009 (2002‐2004), Calik 2014 (2009‐2010), Dabiri 2014 (2011‐2012), Dong 2015 (2012‐2013), Hamidzadeh 2012 (2006), Hamlaci 2017 (2012), Hantoushzadeh 2007 (2005), Hjelmstedt 2010 (2007‐2008), Huang 2008 (2004‐2005), Kashanian 2010 (2007), Lee 2004 (2002), Mackenzie 2011 (2005‐2009), Mafetoni 2016 (2013), Ozgoli 2016 (2008), Qu 2007 (2004‐2005), Ramnero 2002 (1999‐2000), Salehian 2011 (2008‐2009), Sehhatie‐Shafaie 2013 (2012), Skilnand 2002 (1998‐1999), Vixner 2014 (2008‐2011), Mansouri 2018 (2017), Tjung 2008 (2007‐2008). Five studies did not report the study duration (Chung 2003; Kordi 2010; Ma 2011; Martensson 2008; Nesheim 2003).
Funding
Twelve studies reported funding sources. Borup 2009 was funded by the Asse and Ejnar Danielsen's Foundation, Kgs, Lyngby, Dnemark; Knowledge and Research Cener for Alternative medicine, Aarhus, Denmark; Sophus Jacobsen Foundation, Capenhagen, Denmar; The Danish Midwifery Organisation, Copenhangen, Denmark; Lundbeck Foundation, Copenhagen, Denmark; Mads Clausens Foundation, Nordborg, Denmark; Hede Nielsen Foundation, Horsens, Denmark; The Research Fund at Aarhus University Hosptial, Aarhus, Denmark; Else and Mogens Wedell‐Wedellsborgs Foundation, Copenhagen, Denmark; and King Christian the 10th Foundation, Copenhagen, Denmark; Hantoushzadeh 2007 was funded by the Vali Asr Research Centre for Reproductive Health; Hjelmstedt 2010 was funded by Osher Center for Integrative Medicine, Karolinska Institutet and the Centre for Health Care Science, Karolinska Institutet; Huang 2008 was funded by the National Traditional Chinese Medicine Administration of Traditional Chinese Medicine Science and Techology Research Special TCM Clinical Research Fund (04‐05LQ04); Kashanian 2010 was funded by Iran University of Medical Sciences; Ma 2011 was funded by the State Administration of Traditional Chinese Medicine; National Science Foundation of China; and E‐institutes of Shanghai Municipal Education Commission. Mackenzie 2011 was funded by a grant from the Oxfordshire Health Services Research Committee and the Uterine Contractility Trust fund, held by the Oxford Radcliffe NHS Trust. Martensson 2008 was funded by grants from Skaraborg Institute for Reseach and Development, Barnets, Lychopenning, The Swedish Association of Midwives, Hegu Svenska AB and the University of Skövde; Qu 2007 was funded by the Innovation Research Foundation by government of Heilongjiang Privince, China; Ramnero 2002 was funded by grants from Örebro Council Research Committee and Centre for Nursing Science, Örebro University Hospital; Sehhatie‐Shafaie 2013 was funded by Tabriz University of Medical Sciences. Vixner 2014 was funded by grants from the Centre for Clinical Research Dalarna, Karolinska Institutet, Uppsala‐Örebro Regional Research Council, University of Skövde, FOU Fyrbodal, Magnus Bergvall. Stiftelse, and Dalarna University, Sweden.
Declarations of interest
Seven studies reported no conflict of interest (Hjelmstedt 2010; Ma 2011; Mackenzie 2011; Mansouri 2018; Ozgoli 2016; Sehhatie‐Shafaie 2013; Vixner 2014). One study (Mackenzie 2011) stated that one trial author provides legal opinion on litigation cases. In the remaining 21 studies, there was no clear conflict of interest reported.
Quality of acupuncture
All 15 studies of acupuncture were assessed using the NICMAN Scale (Smith 2017). The NICMAN Scale uses an 11‐item scale to review the quality of acupuncture studies. We now include this and report on studies of acupuncture using this scale. The items include: clear description of the population; intervention; comparator; outcome; appropriateness of study design for question; inclusion of a differential diagnosis; selection of acupuncture points consistent with treatment principles; description of needles, needling depth, stimulation, and sensation; point location description and justification according to texts; treatments administered; and the qualifications of the person administering the treatments (Table 1).
| Study ID | Total NICMAN Score | P | I | C | O | Study design | Differential diagnosis | Point selection | Needling parameters | Acupuncture point location | Treatment dosage | Therapist qualifications |
| Borup 2009 | 19 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 1 | 1 | 2 | 2 |
| Dong 2015 | 15 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 1 | 2 | 0 |
| Hantoushzadeh 2007 | 20 | 2 | 2 | 2 | 2 | 3 | 1 | 2 | 2 | 2 | 2 | 0 |
| Huang 2008 | 16 | 2 | 2 | 2 | 2 | 3 | 2 | 2 | 0 | 0 | 1 | 0 |
| Ma 2011 | 17 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 2 | 0 |
| MacKenzie 2011 | 19 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 1 | 2 | 1 | 2 |
| Martensson 2008 | 16 | 2 | 2 | 2 | 2 | 3 | 0 | 1 | 1 | 0 | 2 | 1 |
| Nesheim 2003 | 16 | 2 | 2 | 2 | 2 | 3 | 2 | 0 | 2 | 0 | 1 | 0 |
| Qu 2007 | 13 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 0 | 1 | 0 |
| Ramnero 2002 | 17 | 2 | 2 | 2 | 2 | 3 | 1 | 1 | 1 | 2 | 1 | 0 |
| Skilnand 2002 | 18 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 1 | 0 |
| Tjung 2008 | 17 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 2 | 1 | 2 |
| Vixner 2014 | 18 | 2 | 2 | 2 | 2 | 3 | 1 | 2 | 1 | 2 | 1 | 0 |
The studies that ranked the highest on the NICMAN Scale were Borup 2009 and Mackenzie 2011, each with a score of 90.5%. The study that ranked the lowest was Mansouri 2018 with a score of 47%. The other studies received scores between these figures: Hantoushzadeh 2007 received a score of 87.0%; Ma 2011 scored 81%; Ramnero 2002 scored 74%; Skilnand 2002 and Vixner 2014 both scored 78.3%. Dong 2015 received a score of 71.4%, and Huang 2008, Martensson 2008 and Nesheim 2003 each scored 70.0%.
In reviewing individual items on the NICMAN Scale, all studies scored at the highest level (2 out of 2 or 3 out of 3) for reporting of clear description of the population; intervention; comparator; outcome; and appropriateness of study design for question. Seven studies reported on the inclusion of a differential diagnosis, and scored 2 (Huang 2008; Nesheim 2003), 1 (Hantoushzadeh 2007; Skilnand 2002; Vixner 2014) or 0 (Martensson 2008; Skilnand 2002) for selection and justification of acupuncture points consistent with treatment principles, seven studies scored 2 (Borup 2009; Hantoushzadeh 2007; Huang 2008; Ma 2011; Mackenzie 2011; Skilnand 2002; Vixner 2014), two studies scored 1 (Martensson 2008; Ramnero 2002) and three studies scored 0 (Dong 2015; Nesheim 2003; Qu 2007; for description and justification of needles type and consistency, needling depth, stimulation and justification, and sensation, four studies scored 2 (Hantoushzadeh 2007; Ma 2011; Nesheim 2003; Skilnand 2002), eight studies scored 1 (Borup 2009; Dong 2015; Mackenzie 2011; Martensson 2008; Qu 2007; Ramnero 2002; Tjung 2008; Vixner 2014), and two studies scored 0 (Huang 2008; Mansouri 2018); for reporting of point location description and justification according to texts, seven studies scored 2 (Hantoushzadeh 2007; Ma 2011; Mackenzie 2011; Ramnero 2002; Skilnand 2002; Tjung 2008; Vixner 2014), two scored 1 (Borup 2009; Dong 2015) and five scored 0 (Huang 2008; Martensson 2008; Mansouri 2018; Nesheim 2003; Qu 2007; with regard to reporting of treatments administered during labour and justified, five scored 2 Borup 2009; Dong 2015; Hantoushzadeh 2007; Ma 2011; Martensson 2008), nine scored 1 (Huang 2008; Mackenzie 2011; Mansouri 2018; Nesheim 2003; Qu 2007; Ramnero 2002; Skilnand 2002; Tjung 2008; Vixner 2014), and none scored 0; and for qualifications of the person administering the treatments meeting World Health Organization guidelines (generally a member of a recognised acupuncture association or > 200 hours training), three studies scored 2 (Borup 2009; Mackenzie 2011; Tjung 2008), one study scored 1 (Martensson 2008), and the remainder scored 0 (Dong 2015; Hantoushzadeh 2007; Huang 2008; Ma 2011; Mansouri 2018; Nesheim 2003; Qu 2007; Ramnero 2002; Skilnand 2002; Vixner 2014).
Excluded studies
We excluded 34 trials;seeCharacteristics of excluded studies. Many studies did not meet the inclusion criteria based on the criteria for interventions: for example, the use of point injection therapy (Zhang 2000), or ice massage (Hajiamini 2012; Kaviani 2012). We excluded eight studies due to insufficient reporting of randomisation (Aghdam 2012; Bo 2006; Deepak 2013; Li 2006; Peng 2010; Ternov 1998; Wang 1994; Zhu 2013), and we were unable to ascertain true randomisation status from the author. The study design was unclear or did not meet the criteria for inclusion in seven studies (Deen 1985; Kermani 2015; Levett 2016a; Mucuk 2014; Sebastian 2014; Vixner 2017; Wu 2017). No clinically relevant outcomes were measured in nine trials (Asadi 2015; Can 2015; Li 1996; Mollart 2013; Moradi 2014; Nistler 2010; Shalev 1991; Shang 1995). One study was reported as an abstract only, with insufficient reporting to determine inclusion (Park 2003). Seven studies did not assess pain in labour (Alsharnoubi 2015; Haghighi 2016; Liu 2012; Liu 2015a; Liu 2015b; Masoudi 2014; Samadi 2018).
Risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreements by discussion or by involving another review author.
SeeFigure 2 and Figure 3 for a graphical summary of the 'Risk of bias' assessments by authors of the included studies based on the six risk of bias domains. No study was at a low risk of bias on all domains.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
Method of allocation
All trials were assessed in terms of methods by which participants were allocation to intervention and control or sham groups. Seventeen trials reported the sequence was computer generated (Borup 2009; Calik 2014; Hamidzadeh 2012; Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Kashanian 2010; Kordi 2010; Ma 2011; Mackenzie 2011; Mafetoni 2016; Martensson 2008; Nesheim 2003; Ozgoli 2016; Salehian 2011; Sehhatie‐Shafaie 2013; Vixner 2014). The sequence was by lot drawing in six trials (Dabiri 2014; Dong 2015; Hamlaci 2017; Qu 2007; Skilnand 2002; Tjung 2008), coin tossing in one trial (Chung 2003), random number tables in one trial (Lee 2004), and shuffling cards in one trial (Ramnero 2002). The method of allocation generation was unclear in two studies (Mansouri 2018; Mafetoni 2016a).
Allocation concealment
Following adequate allocation to groups, allocation concealment was assessed for all studies. We assessed the methods used to prevent investigators' foreknowledge of group allocation, from evidence from the studies, extracted independently by two review authors. Where it was unclear, or not reported, we contacted the study author for clarification. Allocation concealment was described as low risk in 17 trials. Sealed envelopes were used in 15 trials (Calik 2014; Dabiri 2014; Hamlaci 2017; Hantoushzadeh 2007; Hjelmstedt 2010; Kashanian 2010; Mackenzie 2011; Martensson 2008; Mafetoni 2016a; Mansouri 2018; Nesheim 2003; Ramnero 2002; Salehian 2011; Skilnand 2002; Vixner 2014), central randomisation in one trial (Borup 2009) and sequential numbers in one trial (Chung 2003). One trial was at high risk due to no concealment (Ozgoli 2016). Ten trials were assessed at unclear risk in nine trials mainly due to method of concealment not being described (Dong 2015; Hamidzadeh 2012; Huang 2008; Kordi 2010; Lee 2004; Ma 2011; Mafetoni 2016; Qu 2007; Sehhatie‐Shafaie 2013; Tjung 2008).
Blinding
Blinding of participants and personnel (performance bias)
Participants (both participants and personnel) were largely aware of whether they had been assigned to acupuncture or acupressure or control. Some studies included sham controls, in an attempt to blind participants. Five trials were assessed at a low risk of bias (Lee 2004; Mafetoni 2016;Mafetoni 2016a; Sehhatie‐Shafaie 2013; Skilnand 2002). Blinding was assessed at high risk in 17 trials (Borup 2009, Calik 2014, Dabiri 2014; Dong 2015; Hamidzadeh 2012; Hamlaci 2017; Huang 2008; Kordi 2010; Ma 2011; Mackenzie 2011; Martensson 2008; Nesheim 2003; Ozgoli 2016; Qu 2007; Salehian 2011; Tjung 2008; Vixner 2014). The risk of blinding was unclear in six trials due to poor reporting (Chung 2003; Hantoushzadeh 2007; Hjelmstedt 2010; Kashanian 2010; Mansouri 2018; Ramnero 2002). We contacted study authors to clarify where possible.
Blinding of outcome assessment
We rated trials as having low risk of bias when researchers described blinded assessment of outcomes. Blinding was assessed at high risk, that is, assessment was largely done by the investigator, in seven trials (Borup 2009; Calik 2014; Dong 2015; Hamlaci 2017; Kordi 2010; Ozgoli 2016; Vixner 2014); 11 trials were at a low risk of bias, where assessment was performed by an independent person (Dabiri 2014; Hamidzadeh 2012; Hantoushzadeh 2007; Hjelmstedt 2010; Kashanian 2010; Lee 2004; Mackenzie 2011; Mafetoni 2016; Mafetoni 2016a; Mansouri 2018; Tjung 2008). Ten studies were at unclear risk of bias due to lack of reporting (Chung 2003; Huang 2008; Ma 2011; Martensson 2008; Nesheim 2003; Qu 2007; Ramnero 2002; Salehian 2011; Sehhatie‐Shafaie 2013; Skilnand 2002).
Incomplete outcome data
Outcome reporting, and risk of attrition, was assessed at a low risk of bias in 16 trials (Borup 2009; Chung 2003; Dabiri 2014; Dong 2015; Hamidzadeh 2012; Hamlaci 2017; Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Mansouri 2018; Martensson 2008;; Ozgoli 2016; Qu 2007; Ramnero 2002; Salehian 2011; Skilnand 2002), where missing data were clearly accounted for and dropout rates were low. Nine trials were at unclear risk (Kashanian 2010; Kordi 2010; Lee 2004; Ma 2011; Mackenzie 2011; Mafetoni 2016; Sehhatie‐Shafaie 2013; Tjung 2008; Vixner 2014), and three trials were assessed at high risk (Calik 2014; Mafetoni 2016a; Nesheim 2003) due to imbalance in dropout between groups and high attrition.
Selective reporting
Every effort was made to minimise the impact of reporting biases by undertaking comprehensive searches of multiple sources to identify unpublished material including protocols of randomised trials in English and Chinese. Although the study protocol was not available for most of the included studies, many showed consistency between results and methods sections. However, the risk of bias from selective reporting was determined to be unclear in 23 trials due to the absence of a study protocol, except for two trials assessed at low risk (Sehhatie‐Shafaie 2013; Vixner 2014).
Other potential sources of bias
The risk of bias from other sources of bias was rated as high risk in three trials due to lower pain scores in the control group prior to the commencement of the intervention, (Hantoushzadeh 2007); significant difference in baseline characteristics between groups (Hjelmstedt 2010; Skilnand 2002). Fifteen trials were assessed at, low risk (Borup 2009; Chung 2003; Hamlaci 2017; Kashanian 2010; Lee 2004; Mackenzie 2011; Mafetoni 2016a; Mansouri 2018; Martensson 2008; Nesheim 2003; Ozgoli 2016; Qu 2007; Ramnero 2002; Sehhatie‐Shafaie 2013; Tjung 2008) and unclear reporting in nine trials (Calik 2014; Dabiri 2014; Dong 2015; Hamidzadeh 2012; Huang 2008; Kordi 2010; Ma 2011; Mafetoni 2016; Salehian 2011; Vixner 2014).
Effects of interventions
See: Summary of findings for the main comparison Acupuncture compared to sham control for pain management in labour; Summary of findings 2 Acupuncture compared to usual care for pain management in labour; Summary of findings 3 Acupuncture compared to no treatment for pain management in labour; Summary of findings 4 Acupuncture compared to water injection for pain management in labour; Summary of findings 5 Acupressure compared to sham control for pain management in labour; Summary of findings 6 Acupressure compared to usual care for pain management in labour; Summary of findings 7 Acupressure compared to combined control for pain management in labour
This review included 27 trials of 3930 women in the meta‐analysis.
Data were not reported in a form that could be included in the meta‐analysis from Qu 2007 study and results are reported descriptively.
1) Acupuncture versus sham control
Five trials with 642 women reported on this comparison. No trial reported on the primary outcomes of: sense of control in labour, satisfaction with childbirth.
Primary outcomes
1.1) Outcome: pain intensity
Two trials assessed pain along a visual analogue scale (VAS) scale, a lower score indicated less pain. Data on this outcome were available from two trials and 325 women, (Analysis 1.1). Due to significant heterogeneity a random‐effects model was applied. Acupuncture may have little effect on reducing the intensity of pain felt by women when compared with sham acupuncture, (mean difference (MD) ‐4.42, 95% confidence interval (CI) ‐12.94 to 4.09, low‐certainty evidence).
1.2) Outcome: satisfaction with pain relief in labour
Satisfaction was assessed using a four‐point rating scale from very good to weak. Acupuncture probably improves satisfaction with pain relief in labour compared with control, (risk ratio (RR) 2.38, 95% CI 1.78 to 3.19, 1 trial, 150 women, moderate‐certainty evidence; Analysis 1.2).
1.3) Outcome: use of pharmacological analgesia
There was evidence of reduced use of pharmacological analgesia from manual acupuncture (RR 0.75, 95% CI 0.63 to 0.89, 2 trials, 261 women, moderate‐certainty evidence; Analysis 1.3).
1.4) Outcome: assisted vaginal birth
It is uncertain whether manual acupuncture reduces assisted vaginal birth when compared with sham acupuncture because the certainty of the evidence was found to be very low, with concerns due to imprecision, inconsistency of results and study limitations (RR 1.10, 95% CI 0.41 to 2.97, 2 trials, 261 women, very low‐certainty evidence), there was substantial heterogeneity I2 72% and a random‐effects model was applied; Analysis 1.4).
1.5) Outcome: caesarean section
There was no evidence of an effect for acupuncture in reducing caesarean section when compared with sham acupuncture (RR 1.11, 95% CI 0.49 to 2.48, 3 trials, 411 women, low‐certainty evidence;Analysis 1.5).
1.6) Outcome: Apgar score less than seven at five minutes
Two trials reported on this outcome. In the Mackenzie 2011 trial there were no babies with an Apgar score less than seven at five minutes. Skilnand 2002 reported on one event in the control group. The results are therefore unclear with so little data being provided for this outcome.
Secondary outcomes
1.7) Outcome: length of labour
The findings do not tell us whether acupuncture reduces the length of labour when compared with a sham control because the evidence was assessed to be of low certainty (MD ‐37.41 minutes, 95% CI ‐96.37 to 21.55; 1 trial, 175 women; Analysis 1.7).
1.8) Outcome: spontaneous vaginal birth
There was no evidence of an effect for acupuncture in increasing spontaneous vaginal birth when compared with sham acupuncture based on low‐certainty evidence (average RR 0.98, 95% CI 0.86 to 1.12, 3 trials, 411 women). There was significant heterogeneity between trials I2 = 64% and a random‐effects model was applied (Analysis 1.8).
1.9) Outcome: augmentation with oxytocin
There was significant heterogeneity between trials and so the results from the studies were not combined. The trial by Skilnand 2002 found reduced augmentation with synthetic oxytocin in the acupuncture group (RR 0.40, 95% CI 0.23 to 0.69), Hantoushzadeh 2007 found no evidence of a difference between groups (RR 0.93, 95% CI 0.85 to 1.02). The heterogeneity maybe explained by the length of time that the intervention was delivered which varied from two hours and until the time of delivery.
Subgroup analysis
There were not enough data relating to manual or electro‐acupuncture to demonstrate any differential effect according to type of acupuncture.
2) Acupuncture versus usual care
Ten trials with 1622 women had data suitable for inclusion in the meta‐analysis. One study (Vixner 2014) has outcomes reported narratively. No trial reported on the primary outcomes of: sense of control in labour, satisfaction with childbirth.
Primary outcomes
2.1) Outcome: pain intensity
Four trials, 495 women reported on this outcome (Analysis 2.1). Pain intensity was assessed with VAS or numeric rating scale (NRS): lower scores indicate less pain.
We are uncertain if acupuncture reduces the pain intensity when compared with the control, there was significant heterogeneity and a random‐effects model was applied and the evidence was assessed as being very low certainty (standardised mean difference (SMD) ‐1.31, 95% CI ‐2.14 to ‐0.49, I2 = 93%, very low‐certainty evidence).
Vixner 2014 found that there were no differences between acupuncture groups (manual or electro acupuncture) and usual care when a simple non‐interaction model was used. When an interaction model was used there was evidence of an interaction between time and treatment group (P = 0.03), at 120 minutes manual acupuncture had lower pain scores than electro acupuncture, at 270 minutes manual acupuncture had lower pain scores than electro acupuncture and at 360 minutes usual care had lower pain scores than manual acupuncture.
2.2) Outcome: satisfaction with pain relief in labour
Two trials reported on this outcome assessed as the number who self reported satisfaction with pain relief.
Manual or electro acupuncture may have little effect on satisfaction with pain relief during labour (RR 1.07, 95% CI 0.96 to 1.20, 343 women, low‐certainty evidence; Analysis 2.2).
2.3) Outcome: use of pharmacological analgesia
Six trials and 1059 women reported on this outcome (Analysis 2.3). The findings do not tell us whether acupuncture may reduce use of pharmacological analgesia compared to a control because the evidence was assessed as very low certainty (average RR 0.72, 95% CI 0.60 to 0.85), there was significant heterogeneity (I2 = 70%) and a random‐effects analysis was undertaken.
2.4) Outcome: assisted vaginal birth
Six trials and 1217 women reported on this outcome. Acupuncture may make little difference to reducing assisted vaginal birth (RR 0.93, 95% CI 0.70 to 1.24, low‐certainty evidence;Analysis 2.4) (manual acupuncture (RR 0.87, 95% CI 0.64 to 1.17, 6 trials, 1089 women) or electro‐acupuncture (RR 1.60, 95% CI 0.64 to 4.04, 1 trial, 128 women).
2.5) Outcome: caesarean section
Five trials and 861 women reported on caesarean section. Acupuncture may make little difference to reducing caesarean section (RR 0.72, 95% CI 0.47 to 1.09, low‐certainty evidence; Analysis 2.5) (manual acupuncture (RR 0.78, 95% CI 0.50 to 1.24, 4 trials, 683 women), electro‐acupuncture (RR 0.46, 95% CI 0.16 to 1.28, 2 trials 178 women).
2.6) Outcome: Apgar score less than seven at five minutes
Six trials, 1061 women reported on this outcome. There was no evidence of harm from acupuncture (RR 0.99, 95% CI 0.28 to 3.47, very low‐certainty evidence; Analysis 2.6).
Secondary outcomes
2.7) Outcome: length of labour
Acupuncture may make no difference to reducing the length of labour in minutes (MD ‐13.89, 95% CI ‐28.93, 1.14, 3 trials, 608 women; Analysis 2.7), (manual acupuncture (MD 4.00, 95% CI ‐142.47 to 150.47, 1 trial, 124 women); electro‐acupuncture (MD ‐14.08, 95% CI ‐29.20 to 1.03, 3 trials, 484 women)).
2.8) Outcome: spontaneous vaginal birth
Four trials and 449 women reported on this outcome. Acupuncture probably makes little difference to rates of spontaneous vaginal birth (RR 0.98, 95% CI 0.89 to 1.08; Analysis 2.8), manual acupuncture (RR 0.96, 95% CI 0.85 to 1.10, 3 trials, 271 women), electro‐acupuncture (RR 0.99, 95% CI 0.86 to 1.14, 2 trials, 178 women).
2.9) Outcome: augmentation with oxytocin
Four trials and 813 women reported on this outcome. Acupuncture probably makes little difference to rates of augmentation compared with the control (RR 0.88, 95% CI 0.77 to 1.02; Analysis 2.9), manual acupuncture (RR 0.92, 95% CI 0.78 to 1.09, 3 trials, 635 women), electro‐acupuncture (RR 0.78, 95% CI 0.59 to 1.03, 2 trials, 178 women), although the CIs cross one and so a possible increase cannot be ruled out.
2.10) Outcome: perineal trauma
One trial of 253 women reported on this outcome. The three‐arm study included electro and manual acupuncture and may make little difference to reducing perineal trauma (RR 0.49, 95% CI 0.19 to 1.26; Analysis 2.10).
2.11) Outcome: maternal blood loss > 500 mL
One trial of 253 women reported on this outcome. The three arm study included electro and manual acupuncture and may reduce the rate of postpartum haemorrhage for women receiving the intervention (RR 0.30, 95% CI 0.11 to 0.78; Analysis 2.11).
2.12) Outcome: relaxation
We are uncertain whether manual acupuncture increases relaxation (MD ‐0.90, 95% CI ‐1.62 to ‐0.18, 90 women; Analysis 2.12).
Subgroup analysis
There were not enough data relating to manual or electro‐acupuncture to demonstrate any differential effect according to type of acupuncture.
3 Acupuncture versus no treatment
One trial of 163 women reported on this comparison. No trial reported on the primary outcomes of: sense of control in labour, satisfaction with childbirth and satisfaction with pain relief.
Primary outcomes
3.1) Outcome: pain intensity
One trial of electro‐acupuncture assessed pain along a VAS scale where a lower score indicated less pain. It is uncertain whether electro‐acupuncture reduces pain intensity compared to the control based on a single trial providing very low‐certainty evidence (MD ‐1.16, 95% CI ‐1.51 to ‐0.81, 163 women, very low‐certainty evidence; Analysis 3.1).
Data were not reported in a form that could be included in the meta‐analysis from the Qu 2007 study. The electro‐acupuncture group reported a lower intensity of pain compared with the control group (26 participants, one trial Qu 2007 study (P = 0.018)).
3.2) Outcome: assisted vaginal birth
It is uncertain whether electro‐acupuncture reduces assisted vaginal birth compared to the control based on a single trial providing very low‐certainty evidence (RR 0.49, 95% CI 0.18 to 1.38, 163 women, very low‐certainty evidence; Analysis 3.2).
3.3) Outcome: caesarean section
It is uncertain whether electro‐acupuncture reduces caesarean section compared to the control based on a single trial providing very low‐certainty evidence (RR 0.76, 95% CI 0.35 to 1.63, 163 women, very low‐certainty evidence; Analysis 3.3).
4) Acupuncture versus water injection
One trial of manual acupuncture with 128 women reported on this comparison. No trial reported on the primary outcomes of: pain intensity, sense of control in labour, satisfaction with childbirth.
Primary outcomes
4.1) Outcome: satisfaction with pain relief
Data from Martensson 2008 were not included in the meta‐analysis. This study assessed pain along a VAS scale where a lower score indicated less pain. Acupuncture may improve satisfaction with pain relief in labour (MD 18.60, 95% CI 11.54 to 25.66, 128 women).
4.2) Outcome: use of pharmacological analgesia
It is uncertain whether acupuncture reduces the use of pharmacological analgesia because the evidence was based on a single trial of very low‐certainty evidence (RR 0.84, 95% CI 0.54 to 1.30, 1 trial, 128 women, very low‐certainty evidence; Analysis 4.1).
4.3) Outcome: assisted vaginal birth
It is uncertain whether acupuncture reduces assisted vaginal birth because the evidence was based on a single trial of very low‐certainty evidence (RR 1.60, 95% CI 0.47 to 5.39, 1 trial, 128 women, very low‐certainty evidence; Analysis 4.2).
4.4) Outcome: caesarean section
It is uncertain whether acupuncture reduces caesarean section because the evidence was based on a single trial of very low certainty (RR 1.33, 95% CI 0.37 to 4.73, 1 trial, 128 women, Analysis 4.3).
Secondary outcomes
4.5) Outcome: augmentation with oxytocin
It is uncertain whether acupuncture reduces augmentation because the evidence was based on a single trial of very low‐certainty evidence (RR 1.16, 95% CI 0.85 to 1.58, 1 trial, 128 women; Analysis 4.4).
4.6) Outcome: relaxation
Relaxation was assessed along a VAS scale where a score of 0 indicated totally relaxed and 100 feeling very tense. Acupuncture may improve women's sense of relaxation (MD 12.60, 95% CI 4.75 to 20.45, 1 trial, 128 women; Analysis 4.5).
5) Acupressure versus sham control
Seven trials of 547 women reported on this comparison. No trial reported on the primary outcomes of: sense of control in labour, satisfaction with childbirth and satisfaction with pain relief.
Primary outcome
5.1) Outcome: pain intensity
Pain intensity was assessed using a VAS where a low score indicated less pain. We are uncertain if acupressure reduces pain intensity in labour because there was significant heterogeneity and the evidence was assessed as very low certainty (MD ‐1.93, 95% CI ‐3.31 to ‐0.55, 6 trials, 472 women; Analysis 5.1). The heterogeneity may be explained by the timing of the observation of pain at various stages during the first stage of labour.
5.2) Outcome: use of pharmacological analgesia
Acupressure may make little difference in the use of pharmacological analgesia between groups (RR 0.54, 95% CI 0.20 to 1.43, 1 trial, 75 women, low‐certainty evidence; Analysis 5.2).
5.3) Outcome: assisted vaginal birth
We are uncertain if acupressure reduces assisted vaginal birth because the evidence was assessed as very low certainty (RR 3.00, 95% CI 0.13 to 71.92, 100 women, 1 trial, very low‐certainty evidence; Analysis 5.3).
5.4) Outcome: caesarean section
Acupressure probably reduces the caesarean section rate compared to sham control (RR 0.44, 95% CI 0.27 to 0.71, 4 trials, 313 women, moderate‐certainty evidence; Analysis 5.4).
5.5) Outcome: Apgar scores less than seven at five minutes
Due to the small number of events we are uncertain if acupressure reduces the Apgar score (RR 0.33, 95% CI 0.01 to 7.99, 220 women, 2 trials; Analysis 5.5). Mafetoni 2016a reported Apgar scores as a mean and standard deviation at one and five minutes and there were no differences between groups.
Secondary outcomes
5.6) Length of labour
Acupuressure may reduce the length of labour in the acupressure group (minutes) (SMD ‐0.91, 95% CI ‐1.26 to ‐0.57, 4 trials, 399 women; Analysis 5.6). However, there was significant heterogeneity I2 = 63% and a random‐effects model was applied, which was reduced with the SMD. Data from Mafetoni 2016a were not in a form that could be included in the analysis.
5.7) Outcome: spontaneous vaginal birth
There was no evidence of differences between groups (RR 1.04, 95% CI 0.92 to 1.18, 115 women, 2 trials; Analysis 5.7).
5.8) Outcome: augmentation with oxytocin
Acupressure may reduce augmentation, although the results were based on only two small trials (RR 0.65, 95% CI 0.46 to 0.91, 135 women, 2 trials; Analysis 5.8).
5.9) Anxiety
Acupressure may reduce anxiety, but again the results were based on only one small trial (MD ‐1.40, 95% CI ‐2.51 to ‐0.29, 1 trial, 75 women; Analysis 5.9).
6) Acupressure versus usual care
Nine trials of 995 women reported data suitable for inclusion in the meta‐analysis. Calik 2014 reported data with medians and mean rank and this was reported narratively. No trial reported on the primary outcomes of: sense of control in labour, satisfaction with childbirth and satisfaction with pain relief.
Primary outcomes
6.1) Outcome: pain intensity
Pain was assessed using a VAS or NRS where a low score indicated less pain. We are uncertain if acupressure reduces pain intensity in labour because the evidence was assessed as very low certainty (SMD ‐1.07, 95% CI ‐1.45 to ‐0.69, 8 trials, 620 women, very low‐certainty evidence; Analysis 6.1). There was significant heterogeneity I2 75% explained by the Ozgoli 2016 trial.
Calik 2014 recorded pain intensity measures at five time points and found that there were significant differences between the groups in subjective labour pain scores in favour of acupressure at all time points except time point 4 (P < 0.001).
6.2) Outcome: satisfaction with pain relief
Satisfaction was assessed from women's views indicating a score of 0 was not effective to 3 = very effective. We are uncertain if acupressure increases satisfaction with pain relief because the evidence was assessed as very low certainty (MD 1.05, 95% CI 0.75 to 1.35, 1 trial, 105 women, very low‐certainty evidence).
6.3) Outcome: caesarean section
Acupressure may make little difference to caesarean section (RR 0.82, 95% CI 0.54 to 1.23, 4 trials, 391 women, low‐certainty evidence; Analysis 6.3).
6.4) Apgar scores less than seven at five minutes
Two trials Calik 2014 and Ozgoli 2016 reported data that could not be included in the meta‐analysis.
Secondary outcomes
6.5 Length of labour
Acupressure may make little difference to the length of labour in minutes (MD ‐16.23, 95% CI ‐79.64 to 47.18, 1 trial, 44 women; Analysis 6.4). The data from the Salehian 2011 trial were not included as this reported on the first and second stage of labour only. Data from Calik 2014 were excluded due to the unclear reporting of total duration of labour.
6.6 Spontaneous vaginal birth
Acupressure may make little difference to rates of vaginal birth (RR 1.04, 95% CI 0.90 to 1.21, 3 trials, 220 women; Analysis 6.5).
6.7 Augmentation with oxytocin
There was no evidence of a difference between groups (RR 2.00, 95% CI 0.39 to 10.31, 1 trial, 15 women; Analysis 6.6).
7) Acupressure versus combined control (placebo and no treatment)
Two trials of 322 women reported on this comparison. No trial reported on the primary outcomes of: sense of control in labour and satisfaction with pain relief.
Primary outcomes
7.1) Outcome: pain intensity
Pain was assessed using a VAS scale where a low score indicated less pain. Acupressure probably slightly reduces the intensity of pain during labour compared with the combined control (SMD ‐0.42, 95% CI ‐0.65 to ‐0.18, 2 trials, 322 women, moderate‐certainty evidence; Analysis 7.1).
7.2) Outcome: satisfaction with childbirth
Satisfaction was assessed using a VAS scale with a low score indicating very bad and a high score very good. One trial, 212 women reported on this outcome. The results are very low certainty and so we are uncertain whether acupressure has any effect on satisfaction with childbirth (MD 4.80, 95% CI ‐2.25 to 11.85, 1 trial, 212 women; Analysis 7.2).
7.3) Use of pharmacological analgesia
It is uncertain whether acupressure reduces use of pharmacological analgesia because the evidence was based on a single trial of very low certainty (RR 0.94, 95% CI 0.71 to 1.25, 1 trial, 212 women, very low‐certainty evidence; Analysis 7.3).
7.4) Outcome: assisted vaginal birth
It is uncertain whether acupressure reduces assisted vaginal birth because the evidence was based on a single trial of very low certainty (RR 0.81, 95% CI 0.39 to 1.67, 1 trial, 212 women, very low‐certainty evidence; Analysis 7.4).
7.5) Caesarean section
It is uncertain whether acupressure reduces caesarean section because the evidence was based on a single trial of very low certainty (RR 0.48, 95% CI 0.22 to 1.04, 1 trial, 212 women, very low‐certainty evidence; Analysis 7.5).
Secondary outcomes
7.6) Outcome: augmentation with oxytocin
Acupressure may make little difference to augmentation with oxytocin (RR 1.01, 95% CI 0.77 to 1.31, 1 trial, 212 women, low‐certainty evidence; Analysis 7.6).
Sensitivity analysis
It was proposed to undertake a sensitivity analysis on the results to look at the possible contribution of: (1) differences in methodological quality, with trials of high quality (low risk of bias) compared to all trials; and (2) publication bias by country. This was not done due to the small number of trials overall. There were no trials of high quality; there were also too few trials within comparisons to make comparisons to examine the influence of publication bias. Where there was heterogeneity, we applied a random‐effects model.
Subgroup analysis
We were only able to analyse data according to the subgroup of manual versus electro‐acupuncture, but there were not enough data to demonstrate any differences between these two subgroups. For other pre‐specified subgroups, we did not undertake subgroup analysis, based on insufficient reporting of trials with the variables of interest by outcome.
Discusión
Resumen de los resultados principales
La revisión incluyó 28 ensayos con 3960 mujeres, con datos que contribuyeron a los datos y análisis de 27 ensayos con 3930 mujeres. La evidencia indica un efecto beneficioso limitado de la acupuntura y la acupresión en relación con los resultados primarios de dolor menos intenso, y una mayor satisfacción materna con la acupuntura.
Acupuntura comparada con control simulado
Es posible que la acupuntura haga una diferencia mínima o nula en cuanto a la intensidad del dolor que sienten las mujeres en comparación con la acupuntura simulada (evidencia de certeza baja), pero probablemente aumenta la satisfacción con el alivio del dolor y reduce la administración de analgésicos farmacológicos (evidencia de certeza moderada). Es posible que la acupuntura no tenga efecto sobre el parto vaginal asistido (evidencia de certeza muy baja) y probablemente tiene poco o ningún efecto sobre la cesárea (evidencia de certeza baja).
Acupuntura en comparación con la atención habitual
No existe certeza de que la acupuntura reduce la intensidad del dolor en comparación con la atención habitual. Es posible que la acupuntura tenga poco o ningún efecto sobre la satisfacción del alivio del dolor (evidencia de certeza baja). No se conoce con certeza si la acupuntura reduce la administración de analgesia farmacológica (evidencia de certeza muy baja). Es probable que la acupuntura tenga poco o ningún efecto sobre el parto vaginal asistido (evidencia de certeza baja) o sobre la cesárea (evidencia de certeza baja).
Acupuntura en comparación con ningún tratamiento
Un ensayo comparó la acupuntura con ningún tratamiento. No se conoce con certeza si la acupuntura reduce la intensidad del dolor, el parto vaginal asistido o la cesárea, porque se encontró evidencia de certeza muy baja.
Acupuntura comparada con la inyección de agua estéril
No se conoce con certeza si la acupuntura tiene algún efecto sobre la administración de analgesia farmacológica, el parto vaginal asistido o la cesárea, porque se encontró evidencia de certeza muy baja.
Acupresión en comparación con un control simulado
No se conoce con certeza si la acupresión reduce la intensidad del dolor durante el trabajo de parto (evidencia de certeza muy baja), o el parto vaginal asistido (evidencia de certeza muy baja). La acupresión probablemente reduce la tasa de cesáreas en comparación con el control simulado (evidencia de certeza moderada). La acupresión puede tener poco o ningún efecto sobre la administración de analgesia farmacológica (evidencia de certeza baja).
Acupresión en comparación con la atención habitual
No se conoce con certeza si la acupresión reduce la intensidad del dolor durante el trabajo de parto (evidencia de certeza muy baja) o si aumenta la satisfacción con el alivio del dolor (evidencia de certeza muy baja). La acupresión puede tener poco o ningún efecto sobre la cesárea (evidencia de certeza baja).
Acupresión en comparación con un control combinado
La acupresión probablemente reduce ligeramente la intensidad del dolor durante el trabajo de parto en comparación con el control combinado (evidencia de certeza moderada). No existe certeza de que la acupresión tenga algún efecto sobre la administración de analgesia farmacológica, la satisfacción con el parto, el parto vaginal asistido o la cesárea, porque la certeza de la evidencia fue muy baja.
Actualmente hay un escaso número de ensayos incluidos dentro de cada comparación, lo que limita el poder estadístico de la revisión para detectar diferencias significativas entre los grupos y los análisis, e indica que estos efectos beneficiosos limitados se deben interpretar con precaución.
Para los resultados primarios y para los secundarios la evidencia fue de certeza moderada a muy baja cuando se utilizaron los criterios GRADE, y los resultados fueron heterogéneos. Muchas comparaciones se caracterizan por tener heterogeneidad clínica significativa o heterogeneidad estadística significativa o considerable. Este hecho puede estar relacionado con la intervención, en cuanto a las características de la dosis y la heterogeneidad de los controles. En las comparaciones se presentaron los datos según el modo de estimulación de la acupuntura (manual, electroacupuntura). Aunque no todas las comparaciones entre la acupuntura y los diferentes grupos control son consistentes en sus conclusiones, la mayoría de las comparaciones indican un efecto beneficioso de la acupuntura, aunque existe la posibilidad de sesgo. Debido al número pequeño de estudios identificados no se han podido identificar los parámetros de dosis de los tratamientos que pueden modificar e influir en los resultados del tratamiento.
Las fuentes de sesgo se han destacado en toda la revisión, pero la función de las expectativas de los pacientes y su estado a menudo no cegado también pueden desempeñar un papel. En los ensayos en los que no hubo cegamiento, los efectos de las expectativas pueden ser mayores y contribuir a un mayor efecto placebo. Los ensayos controlados simulados en esta revisión muestran un pequeño efecto beneficioso general de la acupuntura en comparación con este control; sin embargo, hay una gran heterogeneidad y los diferentes controles pueden diferir en cuán inertes o creíbles son, o si hay un efecto placebo. Abordar estas interrogantes es una prioridad para los estudios futuros.
Compleción y aplicabilidad general de las pruebas
Aún hay relativamente pocos ensayos de acupuntura y acupresión que evalúan la función de estas intervenciones en el tratamiento del alivio del dolor durante el trabajo de parto. La completitud y la aplicabilidad de la evidencia de los 28 ensayos incluidos son limitadas, y ningún ensayo tuvo bajo de riesgo de sesgo en todos los dominios. Aún es una debilidad de varios ensayos la inclusión de pocos resultados y la omisión de resultados clínicos de seguridad.
Los ensayos incluyeron mujeres de bajo riesgo nulíparas y primíparas a término, principalmente en trabajo de parto espontáneo. Los estudios se realizaron en países diferentes, lo que representa los diferentes estilos de acupuntura administrados en los estudios. Existen muchos estilos de acupuntura, incluida la medicina tradicional china individualizada, como lo ilustran ocho ensayos que administran un tratamiento individualizado (Borup 2009; Hantoushzadeh 2007; Huang 2008; Martensson 2008; Nesheim 2003; Ramnero 2002; Skilnand 2002; Vixner 2014) y los que utilizan puntos de acupuntura estandarizados, como se utilizan en la mayoría de los ensayos de esta revisión. La revisión sistemática muestra que existe una amplia variación en la modalidad de la estimulación, la duración de la aplicación de las agujas, el número de puntos usados, la profundidad de la inserción de las agujas y la duración del ensayo. No está claro cuán representativos son los protocolos de tratamiento utilizados en los estudios de investigación para generalizarlos a la acupuntura tal como se practica habitualmente. No hubo un informe suficiente de la razón para seleccionar la acupuntura usada en la investigación. La variación también puede representar el contexto en el cual se practica la acupuntura.
Calidad de la evidencia
El riesgo de sesgo (Figura 2; Figura 3) demuestra que la acupuntura no se ha sometido de manera sistemática a protocolos de estudio rigurosos. La calidad de la información fue deficiente en la mayoría de los ensayos. El riesgo de sesgo fue principalmente bajo con respecto a la aleatorización. Ningún ensayo se clasificó como de bajo riesgo de sesgo en todos los dominios. Las tasas de seguimiento fueron altas en la mayoría de los ensayos, y solo pocos ensayos informaron de una pérdida pequeña de pacientes. En muchos estudios no fue posible el cegamiento de las participantes y del profesional sanitario y el informe indicó que los resultados podrían haber estado influenciados por la falta de cegamiento, por lo que se clasificaron como de alto riesgo de sesgo. El escaso número de estudios en las comparaciones y la falta de ensayos de alta calidad indican que aún no hay evidencia suficiente de un efecto consistente del tratamiento con acupuntura. Se estableció contacto con los investigadores principales de algunos estudios para que proporcionaran información metodológica y estadística adicional; sin embargo, solo se obtuvieron pocas respuestas (Chung 2003; Huang 2008; Kashanian 2010).
La calidad de la evidencia estuvo afectada por la heterogeneidad no explicada en algunas comparaciones, que surgió de la heterogeneidad de las intervenciones clínicas y de los diseños de los estudios. El pequeño número de estudios en las comparaciones, los tamaños de muestra pequeños y la falta de ensayos de alta calidad impidieron el análisis adicional de la heterogeneidad y de la repercusión sobre los efectos del tratamiento. La certeza de la evidencia se redujo debido a los altos niveles de heterogeneidad, los estudios pequeños y el alto riesgo de sesgo en uno o más dominios. No fue posible examinar el efecto de la calidad de los estudios mediante un análisis de sensibilidad debido a que pocos estudios tuvieron bajo riesgo de sesgo. La calidad del informe fue deficiente en muchos ensayos.
La certeza de la evidencia en general, cuando se utilizaron los criterios GRADE, fue de muy baja a moderada (Resumen de los hallazgos, tabla 1; Resumen de los hallazgos, tabla 2; Resumen de los hallazgos, tabla 3; Resumen de los hallazgos, tabla 4; Resumen de los hallazgos, tabla 5; Resumen de los hallazgos, tabla 6; Resumen de los hallazgos, tabla 7).
Calidad de la acupuntura
La calidad de la acupuntura que se administró se evaluó mediante la recién publicada "Reliability of the NICMAN Scale: An Instrument to Assess the Quality of Acupuncture Administered in Clinical Trials" (Smith 2017). Todos los estudios de acupuntura se calificaron en una escala de 11 puntos que evaluó las poblaciones y los diseños de estudio informados, así como la calidad del informe de los métodos de acupuntura utilizados, la justificación según los textos y la evidencia, y las calificaciones de quienes administran el tratamiento (véase Descripción de los estudios). La administración de la acupuntura en el contexto del dolor de trabajo de parto se evaluó como una "afección aguda" en la que normalmente se han administrado pocos tratamientos de acupuntura. En este contexto, los estudios obtuvieron una alta puntuación y proporcionaron evidencia para apoyar la evaluación de la calidad. En general, el fundamento de la selección de los puntos estuvo bien justificado. Sin embargo, la información sobre los detalles del acupunturista que administró el tratamiento en general se informó de manera deficiente y se consideró poco clara, o se consideró insuficiente. La variación de la duración, la frecuencia y la selección de los puntos de acupuntura indica que es posible que la acupuntura no haya sido terapéuticamente efectiva y en algunos casos es posible que no represente la mejor práctica clínica.
Sesgos potenciales en el proceso de revisión
Se intentó minimizar el sesgo de publicación. La búsqueda fue exhaustiva y se incluyeron estudios identificados en idiomas diferentes al inglés. Sin embargo, no se puede descartar la posibilidad de que se hayan omitido algunos estudios. Los ensayos cruzados se excluyeron de esta revisión debido a la falta de transparencia con respecto al período apropiado de lavado para los ensayos de acupuntura. Dos autores de la revisión evaluaron la elegibilidad de los estudios, realizaron la extracción de los datos y evaluaron el riesgo de sesgo. Se conoce que parte de la bibliografía sobre la acupuntura tal vez no se haya publicado en las revistas tradicionales y, por lo tanto, posiblemente se haya excluido de las bases de datos principales.
Acuerdos y desacuerdos con otros estudios o revisiones
Hay otra revisión sistemática de acupuntura para el tratamiento del dolor en el trabajo de parto (Cho 2010) que incluyó ensayos para los cuales no fue posible determinar los detalles de la asignación al azar, o se excluyeron porque los ensayos no cumplieron los criterios de elegibilidad. Los hallazgos y conclusiones de la presente revisión en cuanto a la función de la acupuntura para el alivio del dolor durante el trabajo de parto son similares a los de Cho 2010. Los resultados difieren de los presentados en una revisión sistemática de intervenciones no farmacológicas basadas en el mecanismo de acción endógeno y comparadas con la atención habitual (Chaillet 2014). Esta revisión clasificó la acupuntura y la acupresión mediante un control inhibitorio nocivo difuso que estimula una respuesta del sistema endorfinérgico. La revisión detalló diferentes criterios de elegibilidad y no se pueden hacer comparaciones directas, pero encontró que la acupuntura y la acupresión comparadas con la atención habitual se asociaron con un menor aumento de la analgesia epidural, el dolor de trabajo de parto y una mejor experiencia en el parto. Se han realizado varios ensayos clínicos para estudiar la eficacia de la acupuntura para el dolor durante el trabajo de parto, aunque aún no está claro si la evidencia existente es suficientemente rigurosa para establecer una conclusión definitiva. En una revisión narrativa de tres revisiones sistemáticas (Levett 2014), los autores señalan que las preguntas del estudio y los métodos para abordarlas difieren, y se debe prestar atención a la adecuación de la pregunta al diseño del estudio. En general, en las revisiones sistemáticas se comprobó que la acupuntura y la acupresión tuvieron un efecto beneficioso en cuanto a las puntuaciones del dolor, la administración de analgesia farmacológica y la satisfacción cuando se consideraron los diseños de estudio apropiados en el contexto de la pregunta clínica.

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
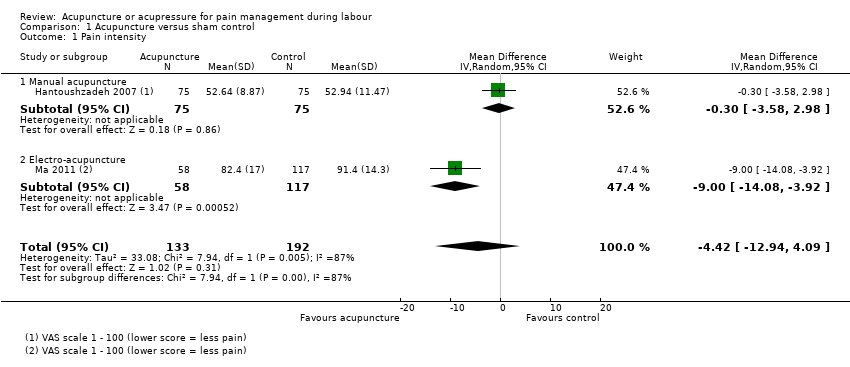
Comparison 1 Acupuncture versus sham control, Outcome 1 Pain intensity.
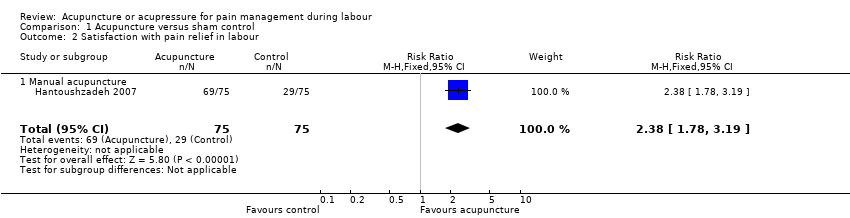
Comparison 1 Acupuncture versus sham control, Outcome 2 Satisfaction with pain relief in labour.
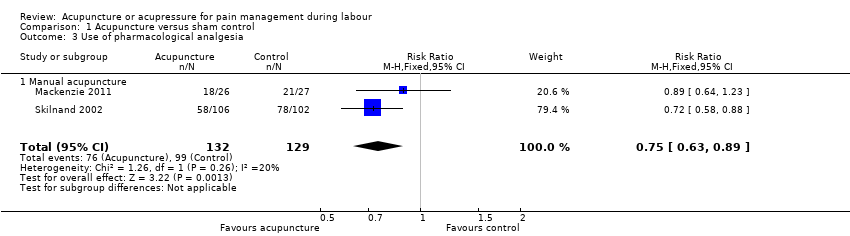
Comparison 1 Acupuncture versus sham control, Outcome 3 Use of pharmacological analgesia.

Comparison 1 Acupuncture versus sham control, Outcome 4 Assisted vaginal birth.

Comparison 1 Acupuncture versus sham control, Outcome 5 Caesarean section.

Comparison 1 Acupuncture versus sham control, Outcome 6 Apgar score < 7 at 5 minutes.
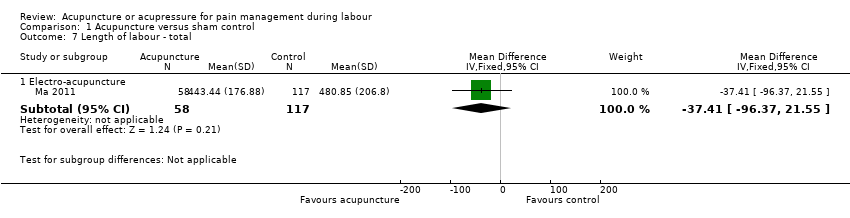
Comparison 1 Acupuncture versus sham control, Outcome 7 Length of labour ‐ total.

Comparison 1 Acupuncture versus sham control, Outcome 8 Spontaneous vaginal birth.
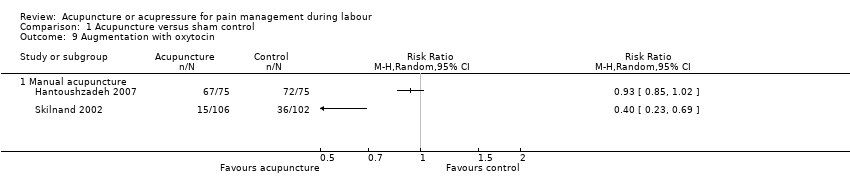
Comparison 1 Acupuncture versus sham control, Outcome 9 Augmentation with oxytocin.

Comparison 2 Acupuncture versus usual care, Outcome 1 Pain intensity.

Comparison 2 Acupuncture versus usual care, Outcome 2 Satisfaction with pain relief in labour.

Comparison 2 Acupuncture versus usual care, Outcome 3 Use of pharmacological analgesia.
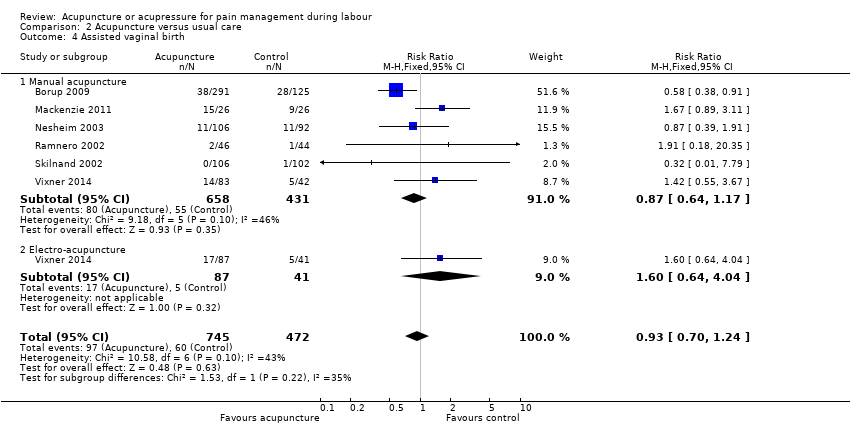
Comparison 2 Acupuncture versus usual care, Outcome 4 Assisted vaginal birth.

Comparison 2 Acupuncture versus usual care, Outcome 5 Caesarean section.
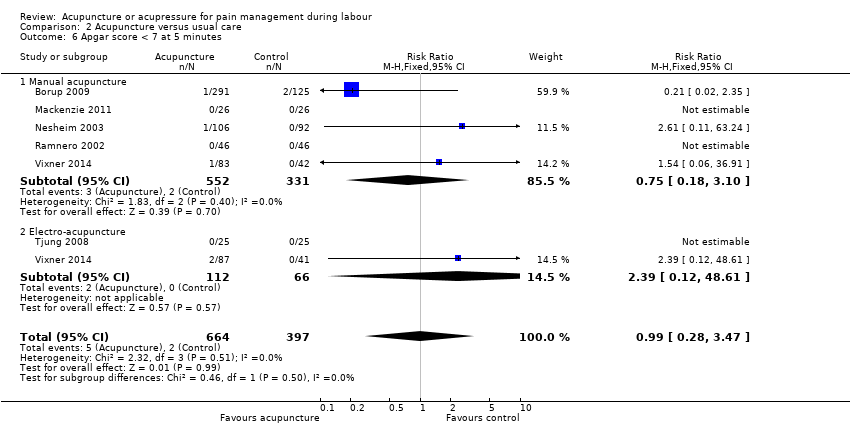
Comparison 2 Acupuncture versus usual care, Outcome 6 Apgar score < 7 at 5 minutes.

Comparison 2 Acupuncture versus usual care, Outcome 7 Length of labour ‐ total.

Comparison 2 Acupuncture versus usual care, Outcome 8 Spontaneous vaginal birth.

Comparison 2 Acupuncture versus usual care, Outcome 9 Augmentation with oxytocin.

Comparison 2 Acupuncture versus usual care, Outcome 10 Perineal trauma.

Comparison 2 Acupuncture versus usual care, Outcome 11 Maternal blood loss > 500 mL.

Comparison 2 Acupuncture versus usual care, Outcome 12 Relaxation.

Comparison 3 Acupuncture versus no treatment, Outcome 1 Pain intensity.
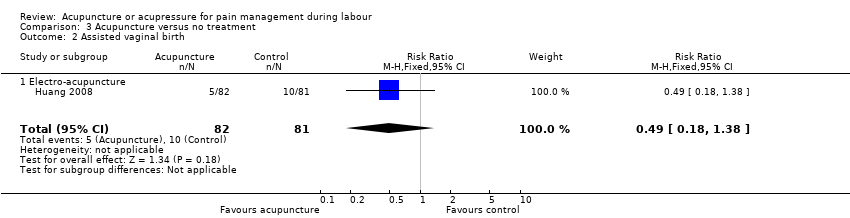
Comparison 3 Acupuncture versus no treatment, Outcome 2 Assisted vaginal birth.
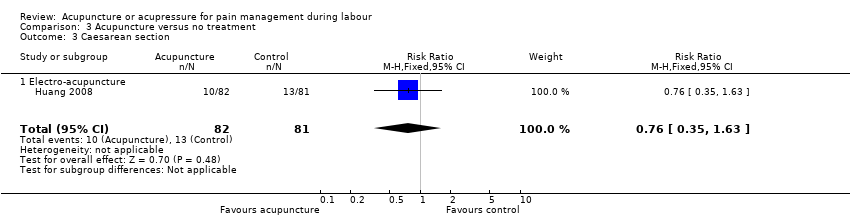
Comparison 3 Acupuncture versus no treatment, Outcome 3 Caesarean section.
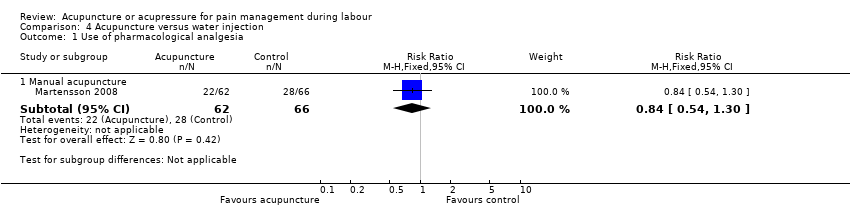
Comparison 4 Acupuncture versus water injection, Outcome 1 Use of pharmacological analgesia.

Comparison 4 Acupuncture versus water injection, Outcome 2 Assisted vaginal birth.
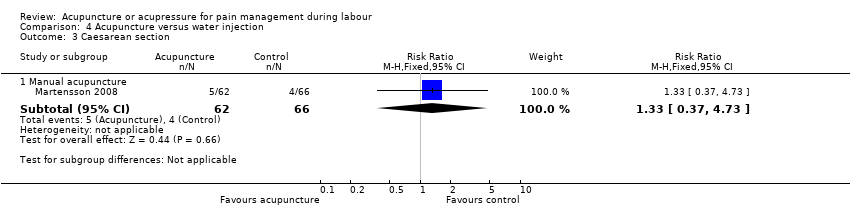
Comparison 4 Acupuncture versus water injection, Outcome 3 Caesarean section.
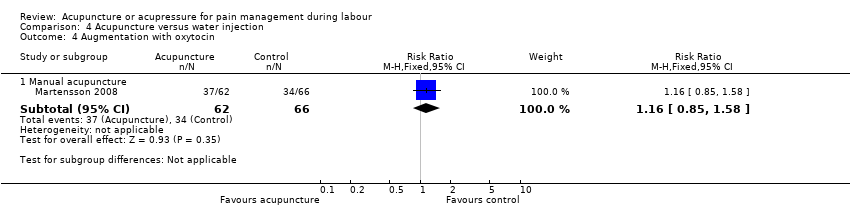
Comparison 4 Acupuncture versus water injection, Outcome 4 Augmentation with oxytocin.

Comparison 4 Acupuncture versus water injection, Outcome 5 Relaxation.

Comparison 5 Acupressure versus sham control, Outcome 1 Pain intensity.

Comparison 5 Acupressure versus sham control, Outcome 2 Use of pharmacological analgesia.

Comparison 5 Acupressure versus sham control, Outcome 3 Assisted vaginal birth.

Comparison 5 Acupressure versus sham control, Outcome 4 Caesarean section.

Comparison 5 Acupressure versus sham control, Outcome 5 Apgar score < 7 at 5 minutes.
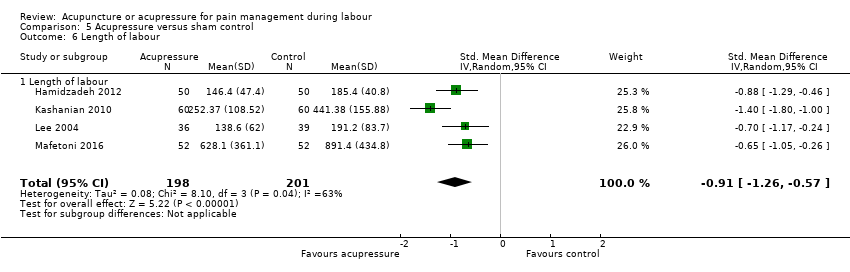
Comparison 5 Acupressure versus sham control, Outcome 6 Length of labour.

Comparison 5 Acupressure versus sham control, Outcome 7 Spontaneous vaginal birth.
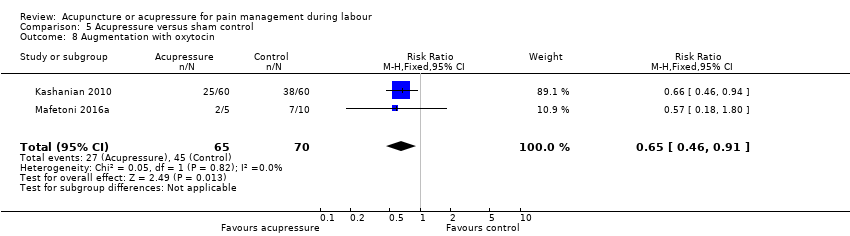
Comparison 5 Acupressure versus sham control, Outcome 8 Augmentation with oxytocin.
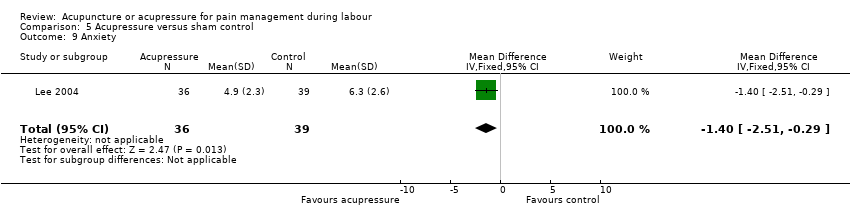
Comparison 5 Acupressure versus sham control, Outcome 9 Anxiety.

Comparison 6 Acupressure versus usual care, Outcome 1 Pain intensity.

Comparison 6 Acupressure versus usual care, Outcome 2 Satisfaction with pain relief.
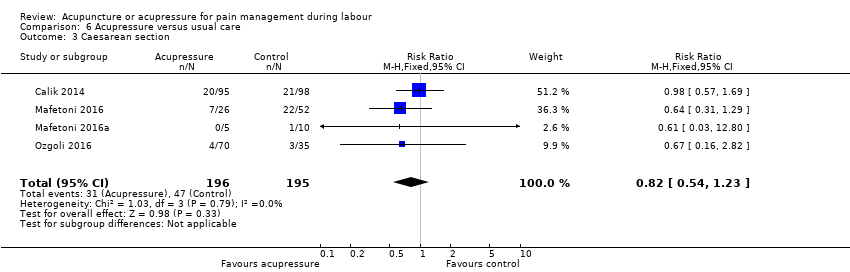
Comparison 6 Acupressure versus usual care, Outcome 3 Caesarean section.

Comparison 6 Acupressure versus usual care, Outcome 4 Length of labour.

Comparison 6 Acupressure versus usual care, Outcome 5 Spontaneous vaginal birth.

Comparison 6 Acupressure versus usual care, Outcome 6 Augmentation with oxytocin.

Comparison 7 Acupressure versus combined control, Outcome 1 Pain intensity.
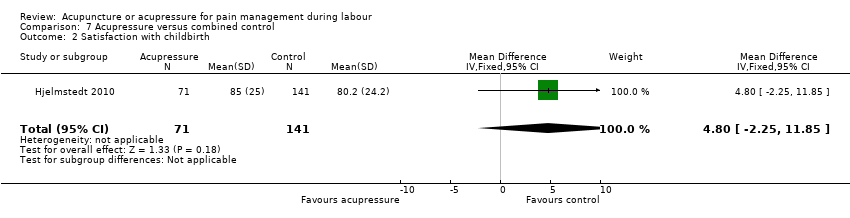
Comparison 7 Acupressure versus combined control, Outcome 2 Satisfaction with childbirth.
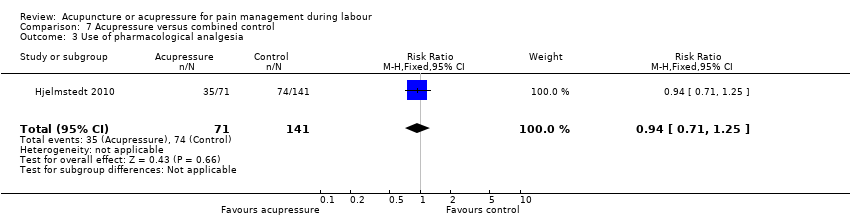
Comparison 7 Acupressure versus combined control, Outcome 3 Use of pharmacological analgesia.

Comparison 7 Acupressure versus combined control, Outcome 4 Assisted vaginal birth.

Comparison 7 Acupressure versus combined control, Outcome 5 Caesarean section.
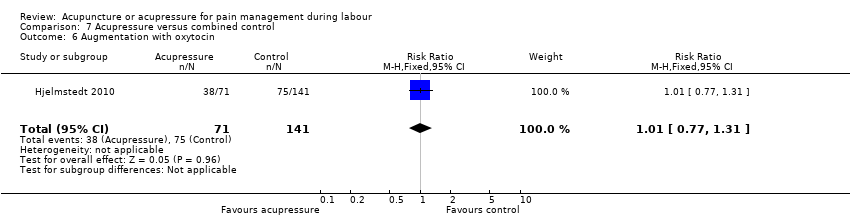
Comparison 7 Acupressure versus combined control, Outcome 6 Augmentation with oxytocin.
| Acupuncture compared to sham control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with sham control | Risk with acupuncture | |||||
| Pain intensity Lower scores indicate less pain intensity | The mean pain intensity ranged across control groups from 52.94 to 91.4 | The mean pain intensity score in the intervention group was 4.42 lower (12.94 lower to 4.09 higher) | 325 | ⊕⊕⊝⊝ | ||
| Satisfaction with pain relief in labour | Study population | RR 2.38 | 150 | ⊕⊕⊕⊝ | ||
| 387 per 1000 | 920 per 1000 | |||||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.75 | 261 | ⊕⊕⊕⊝ | ||
| 767 per 1000 | 576 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.10 | 261 | ⊕⊝⊝⊝ | ||
| 163 per 1000 | 179 per 1000 | |||||
| Caesarean section | Study population | RR 1.11 | 411 | ⊕⊕⊝⊝ | ||
| 49 per 1000 | 54 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: one study high or unclear risk of bias on six domains. 2 Downgraded one level due to serious inconsistency: substantial heterogeneity present I2 = 87% 3 Downgraded one level due to serious imprecision: small sample size (150) 4 Downgraded one level due to serious risk of bias: one study did not blind participants to group allocation. Should not affect sham arm outcome but blinding integrity not reported. 5 Downgraded one level due to serious inconsistency: substantial heterogeneity present I2 = 72% 6 Downgraded one level for imprecision due to small sample size and wide confidence intervals crossing the line of no effect 7 Downgraded one level for imprecision due to small number of events and wide confidence intervals crossing the line of no effect 8 Downgraded one level due to serious risk of bias: one study did not blind participants to group allocation and two studies at high risk of other bias | ||||||
| Acupuncture compared to usual care for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with acupuncture | |||||
| Pain intensity Mix of NRS and VAS scales so analysed using SMD | The mean pain intensity score in the intervention group was 1.31 standard deviations lower (2.14 lower to 0.49 lower) | 495 | ⊕⊝⊝⊝ | |||
| Satisfaction with pain relief in labour | Study population | RR 1.07 | 343 | ⊕⊕⊝⊝ | ||
| 787 per 1000 | 843 per 1000 | |||||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.72 | 1059 | ⊕⊝⊝⊝ | ||
| 833 per 1000 | 600 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 0.93 | 1217 | ⊕⊕⊝⊝ | ||
| 127 per 1000 | 118 per 1000 | |||||
| Caesarean section | Study population | RR 0.72 | 861 | ⊕⊕⊝⊝ | ||
| 116 per 1000 | 83 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels for very serious risk of bias: two of the three studies had high risk of performance bias and this was likely to influence a self‐reported outcome. 2 Downgraded two levels for very serious inconsistency: considerable heterogeneity present (I2 = 93%) not explained by subgroup analysis. 3 Downgraded two levels for very serious risk of bias: both studies had unclear or high risk of bias related to blinding and this was likely to influence a self‐reported outcome 4 Downgraded two levels for very serious risk of bias: all studies had unclear or high risk of performance bias and this was likely to influence the need for additional analgesia. 5 Downgraded one level for serious inconsistency: substantial heterogeneity (I2 = 70%) which is not explained by subgroups. 6 Downgraded one level for serious risk of bias: five of six studies at unclear or high risk of bias in both performance and detection bias. This may have influenced the outcome. 7 Downgraded one level for serious risk of bias: three of four studies at high or unclear risk of bias in both performance and detection bias. This may have influenced the outcome. 8 Downgraded one level for imprecision due to wide confidence intervals. | ||||||
| Acupuncture compared to no treatment for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with no treatment | Risk with acupuncture | |||||
| Pain intensity Lower scores indicate less pain. | The mean pain intensity in the control group was 7.92 | The mean pain intensity score in the intervention groups was 1.16 lower | ‐ | 163 | ⊕⊝⊝⊝ | |
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Assisted vaginal birth | Study population | RR 0.49 | 163 | ⊕⊝⊝⊝ | ||
| 123 per 1000 | 60 per 1000 | |||||
| Caesarean section | Study population | RR 0.76 | 163 | ⊕⊝⊝⊝ | ||
| 160 per 1000 | 122 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded by two levels for very serious risk of bias: high risk of bias in one domain (blinding for a subjective outcome) and unclear risk of bias in four domains. 2 Downgraded one level for serious imprecision due to a single study providing data with a small sample size (163) 3 Downgraded two levels for very serious imprecision due to a single study, with few events, small sample size and wide confidence intervals providing data | ||||||
| Acupuncture compared to water injection for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with water injection | Risk with acupuncture | |||||
| Pain intensity ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.84 | 128 | ⊕⊝⊝⊝ | ||
| 424 per 1000 | 356 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.60 | 128 | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 97 per 1000 | |||||
| Caesarean section | Study population | RR 1.33 | 128 | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 81 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to very serious risk of bias: high or unclear risk of bias in both blinding performance and detection bias 2 Downgraded two levels due to very serious imprecision: small study (128) with few events and wide confidence intervals crossing the line of no effect | ||||||
| Acupressure compared to sham control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with sham control | Risk with acupressure | |||||
| Pain intensity as measured by a 10 cm visual analogue scale. Lower scores indicate less pain | The mean pain intensity in the control groups was 8.35 | The mean pain intensity score in the intervention group was 1.93 lower (3.31 lower to 0.55 lower) | 472 | ⊕⊝⊝⊝ | ||
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.54 | 75 | ⊕⊕⊝⊝ | ||
| 256 per 1000 | 138 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 3.00 | 100 | ⊕⊝⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Caesarean section | Study population | RR 0.44 | 313 | ⊕⊕⊕⊝ | ||
| 308 per 1000 | 136 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level for serious risk of bias: majority of studies have unclear risk of bias in at least three domains. 2 Downgraded two levels for very serious inconsistency: considerable heterogeneity (I2 = 94%) 3 Downgraded two levels for very serious imprecision: very small sample size (75), small number of events and very wide confidence intervals 4 Downgraded one level for serious risk of bias: single study has high risk of performance bias and an unclear risk of allocation bias 5 Downgraded two levels for very serious imprecision: small sample size (100) and very wide confidence interval and small number of events 6 Downgraded one level for serious risk of bias: all studies have unclear risk of bias in at least three domains. Two studies have high or unclear risk of bias relating to performance bias | ||||||
| Acupressure compared to usual care for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with acupressure | |||||
| Pain intensity as measured by numeric rating scale (NRS) and visual analogue scale (VAS). Lower scores indicate less pain. | The mean pain intensity was 8.44 | The mean pain intensity score in the intervention group was 1.07 standard deviations lower (1.45 lower to 0.69 lower). | 620 | ⊕⊝⊝⊝ | The use of acupressure would result in a pain score approximately 2 cm lower on a 10 cm VAS or 2 points on a numeric rating scale compared to usual care. | |
| Satisfaction with pain relief | The mean satisfaction score with pain relief in the control group was 1.6 | The mean satisfaction with pain relief score was 1.05 higher (0.75 higher to 1.35 higher) | 105 | ⊕⊝⊝⊝ | ||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Assisted vaginal birth ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Caesarean section | Study population | RR 0.82 | 391 | ⊕⊕⊝⊝ | ||
| 241 per 1000 | 198 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: majority of included studies have high or unclear risk of bias relating to performance and detection bias 2 Downgraded two levels due to very serious inconsistency: considerable heterogeneity (I2 = 75%) 3 Downgraded two levels due to very serious risk of bias: single study at high risk of bias for selection, performance and detection bias. Very likely to have influenced the outcome 4 Downgraded one level due to serious imprecision: small sample size (105) 5 Downgraded one level due to serious risk of bias: two of the four studies included were at high risk of performance and detection bias, two studies were at high or unclear risk of selection bias and three at high or unclear risk of incomplete outcome data 6 Downgraded one level due to serious imprecision: wide confidence intervals incorporating both benefit and harm | ||||||
| Acupressure compared to combined control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with combined control | Risk with acupressure | |||||
| Pain intensity One study used VAS pain score on scale 1 ‐ 100 mm One study used VAS pain score on scale 1 ‐ 10 mm ‐ the mean | The mean pain intensity score in the intervention group was 0.42 standard deviations lower (0.65 lower to 0.18 lower) | 322 | ⊕⊕⊕⊝ | |||
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth | The mean satisfaction score with childbirth in the control group was 80.2 | The mean satisfaction score in the intervention group was 4.8 higher | ‐ | 212 | ⊕⊝⊝⊝ | |
| Use of pharmacological analgesia | Study population | RR 0.94 | 212 | ⊕⊝⊝⊝ | ||
| 525 per 1000 | 493 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 0.81 | 212 | ⊕⊝⊝⊝ | ||
| 156 per 1000 | 126 per 1000 | |||||
| Caesarean section | Study population | RR 0.48 | 212 | ⊕⊝⊝⊝ | ||
| 206 per 1000 | 99 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: both studies have unclear risk of bias for performance bias, possible effect on this outcome 2 Downgraded one level due to serious risk of bias: single study has unclear risk of performance bias, likely to effect this outcome 3 Downgraded two levels due to very serious imprecision: wide confidence interval greater than 0.25 on either side of the line of no effect and small sample size 4 Downgraded two levels for very serious imprecision: wide confidence interval encompassing both benefit and harm and small sample size | ||||||
| Study ID | Total NICMAN Score | P | I | C | O | Study design | Differential diagnosis | Point selection | Needling parameters | Acupuncture point location | Treatment dosage | Therapist qualifications |
| Borup 2009 | 19 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 1 | 1 | 2 | 2 |
| Dong 2015 | 15 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 1 | 2 | 0 |
| Hantoushzadeh 2007 | 20 | 2 | 2 | 2 | 2 | 3 | 1 | 2 | 2 | 2 | 2 | 0 |
| Huang 2008 | 16 | 2 | 2 | 2 | 2 | 3 | 2 | 2 | 0 | 0 | 1 | 0 |
| Ma 2011 | 17 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 2 | 0 |
| MacKenzie 2011 | 19 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 1 | 2 | 1 | 2 |
| Martensson 2008 | 16 | 2 | 2 | 2 | 2 | 3 | 0 | 1 | 1 | 0 | 2 | 1 |
| Nesheim 2003 | 16 | 2 | 2 | 2 | 2 | 3 | 2 | 0 | 2 | 0 | 1 | 0 |
| Qu 2007 | 13 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 0 | 1 | 0 |
| Ramnero 2002 | 17 | 2 | 2 | 2 | 2 | 3 | 1 | 1 | 1 | 2 | 1 | 0 |
| Skilnand 2002 | 18 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 1 | 0 |
| Tjung 2008 | 17 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 2 | 1 | 2 |
| Vixner 2014 | 18 | 2 | 2 | 2 | 2 | 3 | 1 | 2 | 1 | 2 | 1 | 0 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 2 | 325 | Mean Difference (IV, Random, 95% CI) | ‐4.42 [‐12.94, 4.09] |
| 1.1 Manual acupuncture | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐3.58, 2.98] |
| 1.2 Electro‐acupuncture | 1 | 175 | Mean Difference (IV, Random, 95% CI) | ‐9.0 [‐14.08, ‐3.92] |
| 2 Satisfaction with pain relief in labour Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.38 [1.78, 3.19] |
| 2.1 Manual acupuncture | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.38 [1.78, 3.19] |
| 3 Use of pharmacological analgesia Show forest plot | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.63, 0.89] |
| 3.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.63, 0.89] |
| 4 Assisted vaginal birth Show forest plot | 2 | 261 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.41, 2.97] |
| 4.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.41, 2.97] |
| 5 Caesarean section Show forest plot | 3 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.49, 2.48] |
| 5.1 Manual acupuncture | 3 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.49, 2.48] |
| 6 Apgar score < 7 at 5 minutes Show forest plot | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.79] |
| 6.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.79] |
| 7 Length of labour ‐ total Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Electro‐acupuncture | 1 | 175 | Mean Difference (IV, Fixed, 95% CI) | ‐37.41 [‐96.37, 21.55] |
| 8 Spontaneous vaginal birth Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Manual acupuncture | 3 | 411 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.86, 1.12] |
| 9 Augmentation with oxytocin Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9.1 Manual acupuncture | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 4 | 495 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.31 [‐2.14, ‐0.49] |
| 1.1 Manual acupuncture | 2 | 270 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐2.36, 0.58] |
| 1.2 Electro‐acupuncture | 2 | 225 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.79 [‐3.37, ‐0.21] |
| 2 Satisfaction with pain relief in labour Show forest plot | 2 | 343 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.96, 1.20] |
| 2.1 Manual acupuncture | 2 | 215 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.95, 1.23] |
| 2.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.87, 1.30] |
| 3 Use of pharmacological analgesia Show forest plot | 6 | 1059 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.60, 0.85] |
| 3.1 Manual acupuncture | 5 | 884 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.60, 0.82] |
| 3.2 Electro‐acupuncture | 2 | 175 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.01, 8.16] |
| 4 Assisted vaginal birth Show forest plot | 6 | 1217 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.70, 1.24] |
| 4.1 Manual acupuncture | 6 | 1089 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.64, 1.17] |
| 4.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.64, 4.04] |
| 5 Caesarean section Show forest plot | 5 | 861 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.47, 1.09] |
| 5.1 Manual acupuncture | 4 | 683 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.50, 1.24] |
| 5.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.16, 1.28] |
| 6 Apgar score < 7 at 5 minutes Show forest plot | 6 | 1061 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.28, 3.47] |
| 6.1 Manual acupuncture | 5 | 883 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.18, 3.10] |
| 6.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [0.12, 48.61] |
| 7 Length of labour ‐ total Show forest plot | 3 | 608 | Mean Difference (IV, Fixed, 95% CI) | ‐13.89 [‐28.93, 1.14] |
| 7.1 Manual acupuncture | 1 | 124 | Mean Difference (IV, Fixed, 95% CI) | 4.0 [‐142.47, 150.47] |
| 7.2 Electro‐acupuncture | 3 | 484 | Mean Difference (IV, Fixed, 95% CI) | ‐14.08 [‐29.20, 1.03] |
| 8 Spontaneous vaginal birth Show forest plot | 4 | 449 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.89, 1.08] |
| 8.1 Manual acupuncture | 3 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.85, 1.10] |
| 8.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.86, 1.14] |
| 9 Augmentation with oxytocin Show forest plot | 4 | 813 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.77, 1.02] |
| 9.1 Manual acupuncture | 3 | 635 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.78, 1.09] |
| 9.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.59, 1.03] |
| 10 Perineal trauma Show forest plot | 1 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.19, 1.26] |
| 10.1 Manual acupuncture | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.13, 1.92] |
| 10.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.12, 1.79] |
| 11 Maternal blood loss > 500 mL Show forest plot | 1 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.11, 0.78] |
| 11.1 Manual acupuncture | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.11, 1.43] |
| 11.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.04, 0.93] |
| 12 Relaxation Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 Manual acupuncture | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.62, ‐0.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 1 | 163 | Mean Difference (IV, Fixed, 95% CI) | ‐1.16 [‐1.51, ‐0.81] |
| 1.1 Electro‐acupuncture | 1 | 163 | Mean Difference (IV, Fixed, 95% CI) | ‐1.16 [‐1.51, ‐0.81] |
| 2 Assisted vaginal birth Show forest plot | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.18, 1.38] |
| 2.1 Electro‐acupuncture | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.18, 1.38] |
| 3 Caesarean section Show forest plot | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.35, 1.63] |
| 3.1 Electro‐acupuncture | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.35, 1.63] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Use of pharmacological analgesia Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.30] |
| 2 Assisted vaginal birth Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.47, 5.39] |
| 3 Caesarean section Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.37, 4.73] |
| 4 Augmentation with oxytocin Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.85, 1.58] |
| 5 Relaxation Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Manual acupuncture | 1 | 128 | Mean Difference (IV, Fixed, 95% CI) | 12.60 [4.75, 20.45] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 6 | 472 | Mean Difference (IV, Random, 95% CI) | ‐1.93 [‐3.31, ‐0.55] |
| 2 Use of pharmacological analgesia Show forest plot | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.20, 1.43] |
| 3 Assisted vaginal birth Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 71.92] |
| 4 Caesarean section Show forest plot | 4 | 313 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.27, 0.71] |
| 5 Apgar score < 7 at 5 minutes Show forest plot | 2 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.99] |
| 6 Length of labour Show forest plot | 4 | 399 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.26, ‐0.57] |
| 6.1 Length of labour | 4 | 399 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.26, ‐0.57] |
| 7 Spontaneous vaginal birth Show forest plot | 2 | 115 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.92, 1.18] |
| 8 Augmentation with oxytocin Show forest plot | 2 | 135 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.46, 0.91] |
| 9 Anxiety Show forest plot | 1 | 75 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐2.51, ‐0.29] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 8 | 620 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐1.45, ‐0.69] |
| 2 Satisfaction with pain relief Show forest plot | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 1.05 [0.75, 1.35] |
| 3 Caesarean section Show forest plot | 4 | 391 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.54, 1.23] |
| 4 Length of labour Show forest plot | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐16.23 [‐79.64, 47.18] |
| 5 Spontaneous vaginal birth Show forest plot | 3 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.90, 1.21] |
| 6 Augmentation with oxytocin Show forest plot | 1 | 15 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.39, 10.31] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 2 | 322 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.42 [‐0.65, ‐0.18] |
| 2 Satisfaction with childbirth Show forest plot | 1 | 212 | Mean Difference (IV, Fixed, 95% CI) | 4.80 [‐2.25, 11.85] |
| 3 Use of pharmacological analgesia Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.71, 1.25] |
| 4 Assisted vaginal birth Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.39, 1.67] |
| 5 Caesarean section Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.22, 1.04] |
| 6 Augmentation with oxytocin Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.77, 1.31] |

