Acupuntura o acupresión para el tratamiento del dolor durante el trabajo de parto
References
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised trial of acupuncture, TENS or traditional analgesics. | |
| Participants | 607 healthy, Danish‐speaking women in labour with a normal singleton pregnancy who were giving birth at term (37‐42 completed weeks) and with a fetus in cephalic presentation were eligible for the study. Women were recruited from a university hospital. Women were excluded if they had medical complications, or already received analgesics in labour. | |
| Interventions | Acupuncture group: acupuncture was administered by midwives who had completed a 5‐day course in Western techniques of obstetric acupuncture, and received at least 6 months' clinical training using acupuncture during labour. Treatment was individualised, according to location of pain and woman’s mobility, needles used of 3 depths 0.20 mm x 15 mm, 0.30 mm x 30 mm, 0.35 mm x 50 mm. Duration of needling 30‐120 minutes and could be repeated. Needles removed if woman uncomfortable or if obstetric pathology. Supplementary analgesics provided on request as per control group. Acupuncture points included BL 23, 24, 25, 26, 31‐34, 36, 60, CV20 and sishongong, ear points uterus, shenmen, endocrine, EX‐HN3 yintang, LR3, SP6, SP9, ST36, GB34, HT7, PC6, LI10,11, LU7, LI 4. Control group: traditional analgesics: women randomised to the traditional group could choose among all analgesic methods available (sterile water papules, nitrous oxide, warm tub bath, pethidine, and epidural analgesia). | |
| Outcomes | Need for pharmacological pain relief, pain intensity, overall experience and satisfaction, duration of labour, use of oxytocin, mode of birth, postpartum haemorrhage, Apgar score, umbilical cord pH. | |
| Notes | Study duration: 1 March 2002 to 29 February 2004. Conflicts of interest: none stated. Employment declared in public health and research institutions. Funding: study sponsored by the Asse and Ejnar Danielsen's Foundation, Kgs, Lyngby, Dnemark; Knowledge and Research Cener for Alternative medicine, Aarhus, Denmark; Sophus Jacobsen Foundation, Capenhagen, Denmar; The Danish Midwifery Organisation, Copenhangen, Denmark; Lundbeck Foundation, Copenhagen, Denmark; Mads Clausens Foundation, Nordborg, Denmark; Hede Nielsen Foundation, Horsens, Denmark; The Research Fund at Aarhus University Hosptial, Aarhus, Denmark; Else and Mogens Wedell‐Wedellsborgs Foundation, Copenhagen, Denmark; and King Christian the 10th Foundation, Copenhagen, Denmark. Setting: maternity hospital. Country: Denmark. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence, with randomisation in a ratio of 2:1. |
| Allocation concealment (selection bias) | Low risk | Central randomisation voice response. |
| Blinding of participants and personnel (performance bias) | High risk | Women, midwife acupuncturists were not blinded to their group allocation. Interventions were substantially different and obvious to an observer. |
| Blinding of outcome assessment (detection bias) | High risk | It was unclear if the outcome assessor or analyst was blinded to group allocation. Outcomes would be recorded by staff providing care who would be aware of the intervention. |
| Incomplete outcome data (attrition bias) | Low risk | Data were missing from 8%, with the reasons similar between groups: no project midwife available, did not want the allocated treatment, rapid progression of labour, other reasons. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol is not available but the study reports the expected outcomes. |
| Other bias | Low risk | The study appears free of other biases. |
| Methods | Parallel randomised controlled trial of 193 women. | |
| Participants | Women who would give birth at full term for the first time (between the 37th and 41st week of pregnancy), had 1 fetus with a weight of 2500 g to 4000 g according to ultrasound, had no pregnancy complications, were able to communicate effectively both orally and in written form, were primary school graduates or more, had no systemic or neurological disorder, had an intact membrane, were in the latent phase of labour (cervical opening 2 cm), had no damage, bruises or irritation at the SP6 acupoint, and had similar obstetric histories and socio‐demographic characteristics. | |
| Interventions | 1. The SP6 acupressure was applied 35 times during uterine contractions, 15 times at 2 cm to 3 cm of cervical dilation, and 10 times each at 5 cm to 6 cm and 8 cm to 9 cm of cervical dilation. Acupressure was applied by placing thumbs on both legs at the same time from the beginning to the end of the contraction. 2. Researcher provided the same care for the control group, but without the use of acupressure. | |
| Outcomes | Labour pain and time of labour. Subjective pain was measured using the VAS at 5 time points. | |
| Notes | Study duration: August 2009 to April 2010. Funding: not stated. Conflict of interest: not declared. Setting: maternity hospital. Country: Turkey. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 2 part block randomisation sequence. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes used. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and clinician not blinded. Interventions were substantially different and obvious to an observer. |
| Blinding of outcome assessment (detection bias) | High risk | Assessors unclear, not reported. Outcomes would be recorded by staff providing care who would be aware of the intervention. |
| Incomplete outcome data (attrition bias) | High risk | High attrition rates. 93 women were excluded from the study for the following reasons: 41 women gave birth by caesarean, 19 had a prolonged labour, 9 developed fetal distress, 7 were taken to the obstetric table without 10 cm dilation or wanted to withdraw from the study, 13 women developed complications, and 4 were administered narcotic analgesics No ITT analysis, and data are not able to be re‐included. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available and limited outcomes were included in the study. |
| Other bias | Unclear risk | High attrition rates. No ITT. Unclear if researcher was also outcomes assessor. Researcher provided care for both groups. |
| Methods | Single‐blind, randomised controlled trial of acupressure, effleurage and a control group. It was not feasible for the participant and therapist to be blind to their group allocation. | |
| Participants | 127 women participated in the trial, during their first stage of labour. Participants needed to be between 37 and 42 weeks pregnant, a low‐risk pregnancy, singleton pregnancy and able to speak Chinese. Women who were induced with oxytocin, or received an epidural block or who planned a caesarean section were excluded from the study. The trial was undertaken in Taiwan; no other details were reported. | |
| Interventions | Trained midwives administered the acupressure to women. The intervention lasted 20 minutes, consisting of 5 minutes pressure to points LI4 and BL67. 5 cycles of acupressure were completed in 5 minutes, with each cycle comprising 10 seconds of sustained pressure and 2 seconds of rest without pressure. A protocol was established to control finger pressure, accuracy of points and accuracy of technique. For the effleurage group, the left and right upper arms were massaged for 10 minutes. In the control group, the midwife stayed with the participant for 20 minutes, taking notes or talking with the participant or family members. | |
| Outcomes | A VAS scale was used to measure the intensity of labour pain. This was administered before and after the intervention. Qualitative data were also collected on women's experience of labour pain 1‐2 hours after delivery. The frequency and intensity of uterine contractions were measured from electronic fetal monitors. | |
| Notes | Study duration: unclear. Funding: unclear. Conflict of interest: unclear. Setting: maternity setting. Country: China There was no power analysis. An ITT analysis was not performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin tossing. |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants and clinician not blinded. Interventions were substantially different and obvious to an observer. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The outcome assessors were blinded to women's group allocation but unclear for analyst. |
| Incomplete outcome data (attrition bias) | Low risk | 23 (18%) women withdrew from the study due to a need for a caesarean section, pain medication. The reason for attrition was similar across groups and due to the need for induction or pain relief. |
| Selective reporting (reporting bias) | Unclear risk | Unclear the study protocol was unavailable and limited outcomes were reported. |
| Other bias | Low risk | No other sources of bias detected. |
| Methods | 3‐arm parallel randomised controlled trial of 149 women. | |
| Participants | Singleton pregnant women at a gestational age of 37–42 weeks, cephalic presentation, 4 cm to 5 cm cervical dilatation with spontaneous onset of labour, and with no history of previous high‐risk pregnancy, caesarean section, cephalopelvic disproportion, or narcotic use within the past 8 hours were included in the study. | |
| Interventions | 1. In the acupressure group, a trained and registered midwife, certificated in the acupressure method, performed the treatment. Pressure was applied bilaterally within the contraction on Hegu point (LI4), Prior to applying pressure the patient was asked to take a deep breath then a rotational and vibration pressure was applied for 60 seconds, she then received a 60‐second rest, and pressure was repeated. This cycle continued for 30 minutes. Accurate location of the acupoint was confirmed when the participants felt heaviness, pressure, tingling, or numbness in the area or a pleasant feeling. If the participant reported feeling severe pain at the site of pressure, the pressure was stopped temporarily and commenced after a few minutes. The sign of the intensity of the pressure was partial discolouration of the nail bed to white 2. In the touching group, the same point was touched but with no pressure applied. The 30‐minute intervention time used is based on acupressure theory, which says the time needed to turn the energy in the body’s energy circuits is about 24 minutes. 3. Control. Received usual care | |
| Outcomes | Pain intensity was measured using the VAS. Pain intensity was measured before and several times after the intervention at 30 minutes, 1 hour and every hour after intervention until the end of first stage of labour. | |
| Notes | Study duration: October 2011 to April 2012. Funding: not stated. Conflict of interest: authors declared there are no conflicts of interest. Setting: maternity setting. Country: Iran. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Lot drawing. |
| Allocation concealment (selection bias) | Low risk | Concealed in envelope. |
| Blinding of participants and personnel (performance bias) | High risk | Control group received placebo, usual care not blinded. |
| Blinding of outcome assessment (detection bias) | Low risk | Author clarification that outcome assessor was blinded to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Incomplete data accounted for. ITT analysis included. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available and limited relevant outcomes were reported. |
| Other bias | Unclear risk | Insufficient information to report. |
| Methods | 3‐arm parallel randomised controlled trial of 180 women. | |
| Participants | Women aged 20‐25, with a planned vaginal delivery, singleton pregnancy, 37‐42 weeks gestational age, fetus in vertex presentation, no obstetric or non‐obstetric complications, cervical dilation greater than or equal to 3 cm with regular contractions. | |
| Interventions | 2 experimental groups, 1 control: 1. EX‐B2, 2. SP6, 3. Control. An electro‐acupuncture device (HANS‐100B, China) provides electrical current with intensity range from 5 to 40 mA. The frequency of 100 Hz with a burst frequency of 2 Hz (dense‐dispersed waveform), pulse duration of 0.5 ms (ms) was used. In this study, the intensity of the current was set at 15 mA at the starting point of the active phase of labour and can be adjusted to higher intensity upon request. The device was run by experienced midwives who had been adequately trained in acupuncture before the study. 1. In EX‐B2 (Appointed Jiaji acupoints, approximately 1.7 cm lateral to the posterior median line, from tenth thoracic vertebral to third lumbar vertebral) group, 2 electrodes which connected to the device were attached on the bilateral EX‐B2 acupoints. 2. In SP6 (Sanyinjiao acupoints, 5 cm above medial malleolus in lower leg) group, 2 electrodes were attached on SP6 acupoints of both legs. 3. Routine intrapartum care | |
| Outcomes | Primary: VAS: 0 cm to 10 cm scale. VAS scores were recorded during the last contraction before the intervention and then 30, 60, 120 minutes after the intervention in active phase of labour by the same trained midwife. VAS scores decreased > 3 at the last VAS measurement was considered effective. Secondary: duration of labour – active, second and third phases, oxytocin use, neonatal birthweight, Apgar scores 1 and 5 minutes. | |
| Notes | Study duration: October 2012 to September 2013. Funding: not stated. Conflict of interest: authors state there is no conflicts of interest. Setting: maternity hospital. Country: China. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By lottery method. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and clinician not blinded. Interventions were substantially different and obvious to an observer. |
| Blinding of outcome assessment (detection bias) | High risk | Outcomes assessor was treating clinician. |
| Incomplete outcome data (attrition bias) | Low risk | Describes attrition of participants. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available and limited study outcomes were reported. |
| Other bias | Unclear risk | Not sufficient information reported. |
| Methods | Single‐blind placebo‐controlled trial of 120 women. | |
| Participants | Women have their 1st to 3rd pregnancy, no addiction to drugs, reading and writing literacy, > 37 weeks’ gestation, natural pregnancy, singleton, cephalic presentation, anterior position, spontaneous onset of labour, cervical dilation between 3 cm to 5 cm, 20‐40 years of age, no experience of acupressure, not damage, bruises, sensitivity or irritation at LI4 acupoint, no prior caesarean birth. | |
| Interventions | 1. At the beginning of the active phase of labour (3 cm to 4 cm dilatation of cervix with regular uterine contractions), women in the acupressure group (n = 50) received LI4 acupressure at the onset of the active phase for the duration of each uterine contraction over a period of 20 minutes. At onset of active phase of labour, women in acupressure group received simultaneous acupressure on both hands. 5 pressures on LI4 were applied per minute. Each period included 10 seconds of pressure and 2 seconds of rest. Done during each uterine contraction over a 20‐minute period. The ‘effect’ was confirmed by a feeling by the woman of warmth, weight, swelling and numbness. 2. Women in the control group received a touch on LI4 acupressure point without massage. | |
| Outcomes | Labour pain was measured using the VAS before the intervention, immediately after the intervention, 20 and 60 minutes after, and then every subsequent hour until birth. Satisfaction with labour. Mode of birth. | |
| Notes | Study duration: September 2006 to December 2006. Funding: not stated. Conflict of interest: authors state there are no conflicts of interests. Setting: maternity hospital. Country: Iran. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified randomisation with a block size of 2. Stratified for nulliparous and multiparous women to select 50% each. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and clinician not blinded. Interventions were substantially different and obvious to an observer. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessor was blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Imcomplete data addressed. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol available. Limited study outcomes were reported. |
| Other bias | Unclear risk | Trial seems free of other biases. |
| Methods | Parallel randomised controlled trial of 44 women. | |
| Participants | Pregnant women between 37 and 40 weeks of gestation by ultrasonography, singleton pregnancy, fetal weight of 2500 g to 4000 g according to ultrasonography, had no complications during pregnancy (threatened abortion, hyperemesis gravidarum, etc), had no systemic diseases during pregnancy (gestational diabetes, hypertension, heart disease, etc), spontaneous onset of labour, cervical dilation less than 5 cm, and had planned a vaginal delivery. | |
| Interventions | 1. Study group: Point LI‐4 was located, then acupressure was applied when cervical dilatation reached 4 cm to 5 cm and again when dilation reached 7 cm to 8 cm. In the first and second applications, acupressure was applied to acupoint LI‐4 on both hands at the same time from the beginning to the end of the contraction. Acupressure was applied 16 times during uterine contraction, 8 times at 4 cm to 5 cm of cervical dilatation and 8 times at 7 cm to 8 cm cervical dilatation. Acupressure was applied by placing thumbs on both hands. The mean pressure applied was approximately 3 kg to 5 kg, and this amount was ascertained by the researcher. The first application took approximately 1 hour. The second application took 30 minutes. Acupressure was applied by the researcher in the pregnant woman’s room during labour. It was applied in the active phase of the birth and in the periods of increased labour pain intensity as the most important time for pain management. 2. Control group: pregnant women were given no acupressure or treatment other than routine care. Except for the acupressure practice given to the acupressure group, the researcher gave the participants in both groups equal care throughout the labour. | |
| Outcomes | Pain as measured by VAS. | |
| Notes | Study duration: 1 June 2012 to 30 September 2012. Funding: not stated. Conflict of interest: authors state there are no conflicts of interest. Setting: maternity hospital. Country: Turkey. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Lottery method used. |
| Allocation concealment (selection bias) | Low risk | Sealed envelope. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and clinician not blinded. Interventions were substantially different and obvious to an observer. |
| Blinding of outcome assessment (detection bias) | High risk | Researcher also performed outcome assessment. |
| Incomplete outcome data (attrition bias) | Low risk | All outcome data accounted for. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. Limited study outcomes were reported. |
| Other bias | Low risk | Nil. |
| Methods | Single‐blind randomised controlled trial of acupuncture versus placebo acupuncture using sham needling. Duation: February to September 2005. Setting: government general hospital, Tehran, Iran. | |
| Participants | 150 women with a singleton pregnancy, at term (37 weeks), nulliparous, parturient and in spontaneous active labour. Exclusion criteria: presence of medical or surgical disease, indication for caesarean section, pace‐maker, emphysema, history of anticoagulation, HIV, HCV or HBV infection, pregnancy‐related complications, e.g. chorioamnionitis, placental abruption, placenta praevia and pre‐eclampsia/eclampsia, cervical dilation > 6 cm. | |
| Interventions | The study group received acupuncture administered by the study investigator, who was trained to practice acupuncture. Points were selected bilaterally according to parturient symptoms, and needles were inserted at 45 degree or perpendicularly with a depth that depended on the thickness of the subcutaneous fat. The selection of points was done according to acupuncture principles and was subject to variation from patient to patient. Needles were manually stimulated until the de chi sensation (sensation of warmth, numbness, tingling, or heaviness) was achieved. The needles were not taped and were removed either when delivery occurred or the patient herself asked to do so or when the effect terminated or there was no effect. The following points and there indication were reported as follows: LI4‐ analgesia, BL32‐back pain, BL60 back pain, SP6 severe pain during contractions, ST36 general pain, LR3 analgesia, GB34 cervical rigidity, HT7 anxiety, nervousness. The control group received minimal acupuncture which involved insertion of acupuncture needles away from true acupuncture points. Participants were not asked about de qi and the needles were manually stimulated for about 20 minutes. Both groups received care from health providers, routine analgesia was not available. | |
| Outcomes | Pain scores measured using VAS scale 0‐100, at beginning, 30 minutes, 60 minutes, 120 minutes, then every hour until end of labour. Duration of active labour, amount of oxytocin used, vaginal birth, birthweight, Apgar score at 1 minute, acceptability of acupuncture. | |
| Notes | Study duration: February 2005 to September 2005. Funding: Vali Asr Research Centre for Reproductive Health. Conflict of interest: not stated. Setting: maternity hospital. Country: Iran. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Partcipants blinded to group allocation (assessment of intact blinding not reported), administering clinician unblinded, care provider unclear. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessor blinded. |
| Incomplete outcome data (attrition bias) | Low risk | 5 losses in the acupuncture group: 3 caesarean section, 2 labour stopped. 1 loss in the control group caesarean section. No ITT. |
| Selective reporting (reporting bias) | Unclear risk | Protocol not available. |
| Other bias | High risk | Partcipants in the control group had significantly lower pain scores before intervention commenced. |
| Methods | Parallel randomised controlled trial of acupressure compared with light touch or standard care. | |
| Participants | Public hospital in Trivandrum, India. 212 women randomised to the trial. Inclusion criteria: nulliparous, transferred to labour room, dilation 3 cm to 7 cm, healthy, uncomplicated pregnancy, term, live fetus, cephalic presentation. Exclusion criteria: hypertensive disorder, pre‐eclampsia, diabetes, neuropathic pain, multiparous, intrauterine death, multiple fetuses, breech presentation, gestation < 38 or > 42 weeks, dilation < 3 cm or > 7 cm, elective caesarean section, presence of pharmacological pain relief. | |
| Interventions | Group 1: acupressure at acupoint SP6 bilaterally during contractions over a 30‐minute period. Treatment was not repeated after 2 hours if the woman was not in second stage or had not delivered. Intensity of pressure adapted to each woman's pain threshold. Group 2: (TG) receive light touch at SP6 bilaterally during contractions. Group 3: (SCG) standard care. Acupressure and touch was delivered by same person who had undergone 3 days of training by a certified acupressure therapist. | |
| Outcomes | Participant’s self‐assessment of in‐labour pain via VAS pain scores, oxytocin augmentation, pharmacological pain relief, caesarean section, mode of birth, episiotomy, birthweight, birth length, Apgar (5 minutes). Retrospective ratings of labour pain, coping with labour pain and experience of childbirth. | |
| Notes | Trial duration: 1 September 2007 to 30 April 2008. Funding: Osher Center for Integrative Medicine, Karolinska Institutet and the Centre for Health Care Science, Karolinska Institutet. Conflict of interest: the authors state there are no conflicts of interest. Setting: maternity hospital. Country: India. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelope. |
| Blinding of participants and personnel (performance bias) | Unclear risk | It was unclear if the participant was blinded to light touch or acupressure, the clinician was not blinded to group allocation. It would have been and obvious to an observer.re the group 3. |
| Blinding of outcome assessment (detection bias) | Low risk | The outcome assessor was blinded to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | 1 women withdrew from the standard care group. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable. |
| Other bias | High risk | Baseline pain scores were significantly different between APG and SCG, and boarding on significance between APG and TG. Therefore scores were not used for a between group comparison, but were used for a within‐group comparison over time. |
| Methods | Single‐blind randomised controlled trial, 4‐arm study: 1) electro‐acupuncture group N = 82; TENS group N = 82; control group (breathing) N = 81; spinal‐epidural analgesia group N = 79. Unit of randomisation: 1:1:1:1. | |
| Participants | Inclusion criteria: 324 primiparae women aged 22‐34 years, vaginal delivery, monocyesis, not cephalopelvic disproportion, no abnormal fetal position, no serious complications of pregnancy, agreement to labour analgesia. Exclusion criteria: not explicitly stated. | |
| Interventions | 1) Electro‐acupuncture. Shi diagnosis labour pain mainly located in the lumbosacral and with bearing‐down sensation, sturdy body, desiring cold and fearing of warmth, good appetite, normal or dry stool, normal or less yellow urine, good sleep, normal red tongue with thin and whitish or slightly thicker tongue coating, wiry, drooling and strong pulse. Xu diagnosis: labour pain mainly located in the lower abdomen and distending, weak body, seeking warmth and fearing of cold, poor appetite, loose stool, clear abundant urine, increased nocturnal enuresis, worse sleep, easily waken up in the night, fatty and whitish tongue with teeth mark, thicken and greasy coating, deep and thin, weak pulse. Electro‐acupuncture group applied self‐developed acusector on selected acupoints according to syndrome differentiation, and needling and galvanism were combined on the acupoints. Main acupoints were ST36, CV3 and CV4. Additional points for Shi were BL32 and LR3) and for Xu were LI4 and SP6. Radio frequency electrodes (self‐developed, putting auricular needle in the centre of electrode plate with thumb‐tack needle) were inserted and connected to Han's acupoint nerve stimulator. Dilatational wave of 2Hz/100 Hz operated as a stimulator and the strength adjusted to the woman's tolerance level. 2) TENS group used Han's acupoint nerve stimulator and stimulated point with 2/100 Hz of dilatational wave. 3) Spinal‐epidural analgesia group received combined spinal and epidural block anaesthesia. 4) Advice on breathing during contraction and local massage during severe pain. | |
| Outcomes | VAS scores of pain applied at pre‐pain, 30 minutes, 60 minutes, 120 minutes after pain analgesia, at the end of active stage (cervical dilation of 7 cm to 8 cm), complete dilation of cervix, second stage of labour, third stage of labour and 1 day after labour. 0‐no pain, 1‐mild pain, 10‐most severe and intolerable pain. Degree of satisfaction to labour analgesia 2 hours after delivery. Satisfied: pain completely relieved without evident discomfort. Relatively satisfied: pain relieved to some extent without evident discomfort. Unsatisfied: pain not relieved with evident discomfort. Mode of birth, maternal and labour complications. | |
| Notes | Trial duration: April 2004 to February 2005. Funding: National Traditional Chinese Medicine Administration of Traditional Chinese Medicine Science and Techology Research Special TCM Clinical Research Fund (04‐05LQ04). Conflict of interest: not stated. Setting: delivery unit at the Beijing Gynaecology and Obstetrics Hospital. Country: China. Data from electro‐acupuncture and groups 3 and 4 were combined. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and clinician not blinded. Interventions were substantially different and obvious to an observer. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) | Low risk | No participant loss. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable. |
| Other bias | Unclear risk | Insufficient reporting. |
| Methods | Single‐blind randomised controlled trial of acupressure at SP6 or light touch control group. | |
| Participants | 120 women. Inclusion criteria: age: 18‐35 years, nulliparous, singleton, cephalic presentation, gestational age 37‐41 weeks, intact membranes, cervical dilation 3 cm to 4 cm, established contractions (> 3:10 minutes 45‐60 seconds duration). Exclusion criteria: any sedation during labour, abnormal or deceased fetus, fetal distress, meconium passage, previous hysterotomy or uterine scar, any medical or surgical complications of pregnancy, drug use except usual supplements, vaginal bleeding and high‐risk pregnancy. | |
| Interventions | Acupressure, performed by investigator, at SP6 during contractions for a total acupressure time of 30 minutes. Control: touch at SP6, performed by same investigator, for same duration of time. | |
| Outcomes | Severity of pain as measured by VAS, duration of active phase of labour, mode of birth, use of oxytocin, neonatal weight, and Apgar scores. | |
| Notes | Study duration: March to September 2007. Funding: the research was supported by Iran University. Conflict of interest: not stated. Setting: labour ward at Akbaradi teaching hospital, Iran. Country: Iran. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 4 part block randomisation method (seems to be computer generated). |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes. |
| Blinding of participants and personnel (performance bias) | Unclear risk | It was possible to blind participants. Treatment was known and administered by the investigator. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessor was blinded to treatment group. |
| Incomplete outcome data (attrition bias) | Unclear risk | No discussion of loss of participants at data collection points. No discussion of exclusions after randomisation but exclusion criteria of any sedation during labour or any sign of fetal distress could indicate exclusion after randomisation. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was unavailable. |
| Other bias | Low risk | No imbalances at randomisation. |
| Methods | 3‐arm parallel randomised controlled trial of 83 women. | |
| Participants | Women with a gestational age between 38‐42 weeks, single fetus, cephalic presentation, intact membranes, lack of medical and midwifery diseases, cervical dilatation 3 cm to 4 cm. | |
| Interventions | 1. Acupressure at LI4 2. Touch at LI4 3. Usual care No further details available from translation. | |
| Outcomes | VAS scale measuring intensity of labour pain (immediately, 30 minutes, 1 and 2 hours after the intervention during the first stage of labour), duration of uterine contractions (immediately, 30 minutes, 1, 2, 3 and 4 hours after the intervention). | |
| Notes | Study duration: not stated in translated data extraction. Funding: not stated in translated data extraction. Conflict of interest: not stated in translated data extraction. Setting: Omolbanin Maternity hospital Mashhad, Iran. Country: Iran. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) | High risk | Participants were blinded. Personnel were not blinded. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome assessors were not blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. Limited relevant study outcomes were reported. |
| Other bias | Unclear risk | Unclear. |
| Methods | Single‐blind, randomised controlled trial of acupressure or touch control. | |
| Participants | 89 women were randomly allocated to the trial. Inclusion criteria for the study were: greater than 37 weeks pregnant, singleton pregnancy, planning a vaginal delivery and in good health. Women were recruited to the study from publicity materials in the outpatient department of a general hospital in Korea. | |
| Interventions | Women allocated to the intervention group received acupressure at SP6, or to the control group touch at SP6. The acupressure involved pressure at SP6 on both legs during a contraction during a 30‐minute time period during each contraction. The pressure applied was 2150 mmHg. The control group received touch with no pressure from the thumbs. | |
| Outcomes | Pain was measured along a VAS and assessed at entry, before the intervention was administered, after the intervention, and 30 and 60 minutes after the intervention. Other outcomes included duration of labour, use of pain relief, and maternal anxiety. | |
| Notes | Study duration: May 2002 to September 2002. Funding: not stated. Conflict of interest: not stated. Setting: delivery suite at a University Hospital. Country: Korea. No power analysis was reported. An ITT analysis was performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was generated from random‐number tables. |
| Allocation concealment (selection bias) | Unclear risk | Unclear. |
| Blinding of participants and personnel (performance bias) | Low risk | The participants were blinded to group allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded to group allocation. |
| Incomplete outcome data (attrition bias) | Unclear risk | 14 (15%) women did not complete the study. Reasons given were caesarean section, withdrawal or incomplete data. No information was reported by group allocation. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable. All pre‐specified outcomes were reported. |
| Other bias | Low risk | No other bias detected. |
| Methods | 3‐arm placebo‐controlled randomised trial. | |
| Participants | 350 women in labour, aged 24 to 35 years old, with gestational age 38 to 41 completed weeks, who have had a trial labour indication, have never had prior acupuncture treatment, and have regular uterine contraction, cervical dilatation 2 cm to 3 cm and head presentation labour score > 10 were included. | |
| Interventions | Randomly assigned to receive 1. electroacupuncture (EA), 2. sham EA or 3. no acupuncture. Acupuncture was conducted at the end of the latency period of the first labour stage in all participants, when the dilatation of cervix was at 3 cm. Experimental intervention: EA: women received the electroacupuncture at the 1 acupoint, Sanyinjiao (SP6), at the end of the latent phase of the first labour stage (cervical dilation 2 cm to 4 cm). The inserted needle was stimulated with make‐and‐break waves (dense wave at 4Hz and disperse wave at 20Hz) and left for 30 minutes. Analgesia and safety indices were observed at 7 time points including before needle, needle retention for 15 minutes and 30 minutes, 1, 2, 3 and 4 hours after needle withdrawal. Oxytocin was administered when indicated during labour. Caesarean section was performed as needed based on the patient’s labour progression. Control/Comparison intervention: sham EA and no acupuncture. Sham EA: the procedure was identical to that used in the acupuncture group but without needle insertion into the skin. The needle operations were conducted out of the patient’s visual field. The electroacupuncture apparatus was within sight of the parturients, and the blinking of display lamp in the apparatus could lead parturients to believe that they were receiving electroacupuncture. A post‐examination was conducted for the patients blinding by asking whether they received the acupuncture. No acupuncture: for the control group, parturients were treated as regular parturients in labour. | |
| Outcomes | Self‐rated analgesic effect (VAS: 0‐100). The duration and paralysis time of uterine contraction, uterine contraction regularity, degree of cervical extension, presentation of fetal descent, the condition of intrapartum haemorrhage and postpartum haemorrhage, labour manner, lochia, involution of uterus, milk secretion, neonate Apgar score and neonate body height and weight. | |
| Notes | Study duration: not stated. Funding: State Administration of Traditional Chinese Medicine; National Science Foundation of China; and E‐institutes of Shanghai Municipal Education Commission. Conflict of interest: authors state there are no conflicts of interest. Setting: maternity hospital. Country: China. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Unclear risk | Did not describe. |
| Blinding of participants and personnel (performance bias) | High risk | Not reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Does not describe. |
| Incomplete outcome data (attrition bias) | Unclear risk | Does not describe. |
| Selective reporting (reporting bias) | Unclear risk | No protocol provided. |
| Other bias | Unclear risk | No baseline imbalances. |
| Methods | 4‐arm, single‐blind, placebo‐controlled randomised trial. | |
| Participants | Study reports on participants undergoing a medical induction of labour. 105 nulliparous, singleton pregnancy, fetal cephalic presentation, intact membranes, undergoing labour induction using vaginal prostaglandins, low amniotomy for prolonged gestation or mild hypertension. All groups: subsequent pain management including aromatherapy, TENS and parenteral opioids, and regional blockade was provided when requested or recommended by the attending midwife or obstetrician. | |
| Interventions | Experimental intervention Manual acupuncture – needles stimulated by hand for 30 minutes. Electro‐acupuncture – needles attached to an electrical stimulator and stimulated for 30 minutes. Commenced in both groups after medical induction initiated but before painful contractions started. Acupuncture provided by qualified registered acupuncturists. Needles inserted intramuscularly to depth of 15‐20 mm until unusual sensation (de qi) developed, needles remained inserted for 30‐60 minutes. Points used: LI 4, SP6, BL60 and BL67. Control/Comparison intervention Sham acupuncture – manual and electro 1:1 ratio – acupuncture stimulation not provided. Needles inserted adjacent to the specific acupuncture site – insufficient to provoke de qi sensation. Sham manual received no stimulation, sham electro were connected to the electrical stimulator but current not activated. Usual intrapartum care. | |
| Outcomes | Primary outcome: rate of intrapartum epidural anaesthesia. Secondary outcomes: parenteral analgesia requirement, duration of labour, mode of birth, neonatal condition, postpartum haemorrhage. | |
| Notes | Study duration: August 2005 to February 2009. Funding: supported by a grant from the Oxfordshire Health Services Research Committee and the Uterine Contractility Trust fund, held by the Oxford Radcliffe NHS Trust. Conflict of interest: authors state there are no conflicts of interest, except 1 author (IM) who provides legal opinion in litigation cases at the request of claimants and defendants. Setting: John Radcliffe Hospital. Country: UK. Manual and electro‐acupuncture were combined in the analysis due to the reporting of data in the manuscript for some outcomes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers. Variable block sizes used. |
| Allocation concealment (selection bias) | Low risk | Allocation concealment by sealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Participants blinded in 2 groups, except for the usual care group. Interventions were substantially different and obvious to an observer. |
| Blinding of outcome assessment (detection bias) | Low risk | Blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Does not describe. |
| Selective reporting (reporting bias) | Unclear risk | No published protocol. |
| Other bias | Low risk | No baseline imbalances. |
| Methods | 3‐arm randomised controlled single‐blind pragmatic trial. | |
| Participants | Women of any age and parity, from 37 weeks' gestation, in spontaneous, induced, and/or augmented labour and > 4 cm dilated, 2‐3 contractions every 10 minutes, with undamaged skin at the bilateral SP6 point, fetus in cephalic vertex position with good vital signs. | |
| Interventions | Randomised to: 1. Acupressure SP6 (SP6) 2. Touch group ‐ touch at SP6 3. Placebo and control group (CG) | |
| Outcomes | Pain intensity measured using VAS Caesarean section Length of labour | |
| Notes | Study duration: January 2013 to August 2013. Funding: not stated. Conflict of interest: not stated. Setting: tertiary teaching hospital in Sao Paulo, Brazil. Country: Brazil. Data from groups 1 and 2 included in the analysis. Data from group 3 unclear from translation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were allocated through a computer‐generated sequential list of random numbers in blocks of 6, and participants were distributed in 3 groups. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) | Low risk | Participant in SP6G and TG were blinded. Participants in CG not blinded due to nature of trial. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessor was also blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | No losses to follow‐up. Analysis was ITT. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available, limited relevant study outcomes were reported. |
| Other bias | Unclear risk | Baseline imbalance between SP6 group and control group with mean number of pregnancies (P = 0.02). |
| Methods | 3‐ arm randomised controlled trial | |
| Participants | 30 women. Inclusion criteria: any parity, from 37 weeks' gestation, in spontaneous, induced, and/or augmented labour with dilation > 4 cm dilated, 2 or more contractions every 10 minutes, with intact skin in the auricle pavilion, with a living fetus in cephalic presentation with good vital signs. Exclusion criteria: dilation > 7 cm, severe pre‐eclampsia, placenta previa, previous caesarean section, immediate indication for caesarean section. | |
| Interventions | Auriculotherapy with crystal beads on ear points Shenmen, uterus point, neurasthenia and endocrine point pressed for 1 minute. Control groups Auiculotherapy with glass beads placebo not manipulated Control group | |
| Outcomes | Pain intensity measured on a VAS scale Caesarean section Apgar score at 1 and 5 minutes Length of labour Augmentation with oxytocin | |
| Notes | Study duration April 2015 to August 2015 Funding: not reported. Conflict of interest: not reported Setting: tertiary teaching hospital Sao Paulo Country: Brazil | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | List of random numbers stated but method not stated. |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes |
| Blinding of participants and personnel (performance bias) | Low risk | Treatment and placebo group blinded, control group not blind to group allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Assesor was blinded |
| Incomplete outcome data (attrition bias) | High risk | 10 women withdrawn whose delivery took place prior to last observation, 3 in treatment, 5 placebo and 2 control group. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Other bias | Low risk | No baseline differences. |
| Methods | 3‐armed randomised controlled trial of 165 randomised women | |
| Participants | Inclusion criteria: primiparous, gestational age ≥ 37 weeks, age of 18‐35 years, singleton fetus with vertex presentation, fetal weight of 2500 g to 4000 g, spontaneous vaginal delivery (4 cm to 5 cm cervical dilatation with at least 2 contractions of 20 seconds and more within 10 minutes), healthy skin in the pressure areas, no history of medical and obstetric problems, and pain intensity ≥ 50 mm based on VAS on admission. Exclusion criteria: 1) using any analgesics, 2) fast delivery, 3) emergency caesarean section, 4) abnormal fetal heartbeat, 5) lack of progress, and 6) unwillingness of the mother to continue participating in the study. | |
| Interventions | Group 1 Acupressure on bladder points of BL5, BL8, BL9, and GV20. For the first stage of labor, simultaneous with the beginning of uterine contraction the parturient was placed in a semi‐sitting position with the head in body alignment. The researcher placed over the head of parturient and applied a fixed pressure with a thumb for 60 seconds on each of the BL5, BL8, BL9, and GV20 points. Therefore, the parturient felt the tai chi (heaviness, pressure, hotness, tingling, or numbness) at these points. The pressure was completed within 5 4‐minute cycles (i.e. total of 20 minutes) with intervals of 30 minutes. After the first stage of labour (10 cm cervical dilatation), a four‐minute pressure cycle was resumed on the points at the beginning of the second stage of labour (maternal exiting). Group 2 Pressure on gallbladder points of GB8, GB16, GB17, GB18, and GV20 60 sec of pressure was applied on each of the 5 GB8, GB16, GB17, GB18, and GV20 points (5‐min cycle) with the onset of uterine contraction in the first stage of labour. The pressure was carried out as 4 5‐minute cycles with 30‐minute intervals making a total of 20 minutes pressure. At the beginning of the second stage of labor, 60 seconds of pressure was applied to the points (5‐minute cycle). Group 3 Routine care unspecified. | |
| Outcomes | VAS scale. | |
| Notes | Study duration May 2017 to November 2017 Funding: study formed part of a Masters Thesis. Conflict of interest: authors declare there are no conflicts of interest. Setting: Um Al‐Benin Specialized Women's Hospital, Mashad Country: Iran The 2 acupressure groups were combined in the analysis. Data reported at the end of second stage of labour when intervention finished | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women allocate to the 3 groups through random allocation. ‘The first three participants were asked to take the papers randomly. Afterwards, the order of first three people was repeated for the rest of the participants’ |
| Allocation concealment (selection bias) | Low risk | Concealed in an envelope |
| Blinding of participants and personnel (performance bias) | Unclear risk | Similar pressure was applied to the 2 intervention groups. Women on the control group unblinded. |
| Blinding of outcome assessment (detection bias) | Low risk | Binded research assistant collected outcome data. |
| Incomplete outcome data (attrition bias) | Low risk | 12 women were excluded from the analysis. 7 women in the intervention group stopped receiving the acupressure, 3 women had hypertonic contractions, 1 women had fetal distress and 1 women a lack of progress. Control group 1 women stopped receiving the intervention, one received narcotic pain relief. |
| Selective reporting (reporting bias) | Unclear risk | No reference to a protocol, limited study outcomes reported. |
| Other bias | Low risk | No imbalance at randomisation. |
| Methods | Randomised controlled trial of acupuncture compared with sterile water injections. | |
| Participants | 128 women. Inclusion criteria were: 37‐42 weeks' gestation, spontaneous onset of labour, frequency of 3 contractions during 10 minutes and a requirement for pain relief. Exclusion criteria were: no opoid analgesics, acupuncture, TENS, or sterile water injection in the previous 10 hours, or had received paracervical nerve block, epidural or intrathecal analgesia or augmentation of labour. | |
| Interventions | Acupuncture group: all women were treated at GV20, LI4 and SP6. Local acupuncture points were selected individually depending on where the pain was perceived; the midwives could choose 4 to 7 points from BL23‐24, BL54, EX19, GB25‐29 and KI11. The acupuncture points were chosen both from recommendations in the literature and in cooperation with the midwives, the latter in an attempt to imitate normal clinical practice. The needles (Hegu AB, Landsbro, Sweden) were made of stainless steel (0.3030 or 0.3550 mm). After insertion, the needles were stimulated to evoke needle sensation (De Qi), a feeling of heaviness, numbness and distension, reflecting activation of muscle‐nerve afferents. The needles were left in place for 40 minutes, and were stimulated manually, as described, every 10 minutes. The first assessment after treatment took place 30 minutes after all the needles were in place. The treatment was repeated if necessary. Water injection group was given 48 subcutaneous injections of 0.5 mL sterile water. The injections were administered in the area where the woman felt pain; the injections could be repeated if necessary. A 2‐mL plastic syringe (B. Braun Omnifix†) with a thin needle (B. Braun Omnifix†; diameter: 0.40 mm, length: 20 mm) was used. The injections were administered during a contraction. The first assessment after treatment took place 30 minutes after all the injections were given. 40 midwives administered acupuncture and/or injections of sterile water. All midwives were equally trained in administration of acupuncture and injection of sterile water. All protocols were thoroughly standardised. | |
| Outcomes | Pain and relaxation was assessed using a VAS immediately before and 30, 60, 90, 120, 150 and 180 minutes after treatment. The woman was asked to mark her degree of pain and relaxation on the 100‐mm line with the following endpoints: 0 = no pain at all and 100 = worst conceivable pain, and 0 = totally relaxed and 100 = very tense, for pain and relaxation, respectively. Obstetric outcomes were also assessed. After delivery, the woman was asked the extent to which the treatment had provided pain relief and relaxation, and if she would accept the same treatment during a future delivery. | |
| Notes | Study duration: not stated. Funding: grants from Skaraborg Institute for Reseach and Development, Barnets, Lychopenning, The Swedish Association of Midwives, Hegu Svenska AB and the University of Skövde. Conflict of interest: not stated. Setting: labour ward at Kärnsjukhuset in Skövde. Country: Sweden. Stratified by parity, randomisation in blocks of 10. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and clinician not blinded. Interventions were substantially different and obvious to an observer. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) | Low risk | Dropouts defined as events after randomisation leading to no treatment or events after treatment, such as delivery or requirement for other methods of pain relief. Another midwife undertook women's assessment of pain and relaxation. The reasons for dropout were similar between groups; 16 women in the acupuncture group and 11 women in the injection group dropped out (total 17% dropout). |
| Selective reporting (reporting bias) | Unclear risk | Study protocol was not available. |
| Other bias | Low risk | There was a slight imbalance in age, there appears to be no other source of bias. |
| Methods | A single‐blind, controlled trial of acupuncture versus usual care. | |
| Participants | 198 women were enrolled into the trial of acupuncture versus usual care. Women were recruited to the trial who were at term, experiencing regular contractions and had an ability to speak Norwegian. Women were excluded if their labour was induced, planning a caesarean section, a plan to request an epidural block, medical reasons for an epidural, or experiencing any infectious diseases. | |
| Interventions | 8 midwives were educated and trained to practice acupuncture for the trial. All women received other analgesics on demand. The acupuncture points used were selected based on the participants' needs and included points BL32, GV20, BL60, BL62, HT7, LR3, GB34, CV4, LI10, LI11, BL23, BL27, 28, 32, LI4, SP6, PC6,7, ST36. De qi was obtained. Needles were left in place for 10‐20 minutes, or removed after the needling sensation was obtained, or taped and left in place. Women in the control group received conventional care. | |
| Outcomes | Clinical outcomes included use of meperidine, use of other analgesics, duration of labour, mode of birth and Apgar score. Participants also rated their pain relief along a VAS scale and asked to report any side effects from the treatment. | |
| Notes | Study duration: not stated. Funding: not stated. Conflict of interest: not stated. Setting: Ulleval University hospital, Oslo Norway. Country: Norway. A power analysis was undertaken. An ITT analysis was performed. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Adequate, sealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and clinician not blinded. Interventions were substantially different and obvious to an observer. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) | High risk | Inbalance in dropouts between groups; 6 dropouts, 1 dropout from acupuncture group. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol was unavailable. |
| Other bias | Low risk | Demographic baseline characteristics comparable between groups. |
| Methods | Ranomised controlled trial of LI4 and BL32 acupressure compared with usual care. | |
| Participants | 105 primiparous women in active phase of first stage of labour. Inclusion criteria: age range of 19–35 years, term pregnancy (> 37 weeks of gestation), planned vaginal delivery without obstetrical or non‐obstetric complications, fetal vertex presentation, and being in Exclusion criteria: unwillingness to continue taking part in the study. | |
| Interventions | Experimental intervention: Hegu LI4, n = 35 and BL32 acupressure: n = 35 Intervention applied at cervical dilation 4 cm to 5 cm, 6 cm to 7 cm, 8 cm to 10 cm during 6 uterine contractions. Pressure applied by the researcher until nail bed changed colour. Application of pressure stopped at the end of the contraction. Repeated for 6 contractions, following 6th contraction women gave assessment of pain Control group: usual care | |
| Outcomes | Pain assessed by numerical rating scale. Type of delivery, Apgar score. | |
| Notes | Study duration: August to November 2008. Funding: none reported. Conflict of interest: none declared Setting: Shahid Akbarabadi Hospital (Tehran) Country: Iran Data from both acupuncture groups will be combined in the analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated: random allocation software |
| Allocation concealment (selection bias) | High risk | Open list no concealment. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding, open‐label. |
| Blinding of outcome assessment (detection bias) | High risk | Data collected by the researcher administering the intervention |
| Incomplete outcome data (attrition bias) | Low risk | 1 woman in the control group withdrew |
| Selective reporting (reporting bias) | Unclear risk | No protocol available. Dose of oxytocin that was administered in each subject for labour induction, pattern of uterus contractions, Bishop Score, frequency of pethidine administration were also recorded but not reported. |
| Other bias | Low risk | No evidence of other biases. |
| Methods | Randomised controlled trial of electro‐acupuncture or control (no pain relief). | |
| Participants | 36 study participants. Inclusion criteria: primiparous women, with a normal single pregnancy with spontaneous onset of labour, cephalic presentation, cervical dilation < 6 cm at admission, gestational age 37‐42 completed weeks. Exclusion criteria: diabetes, pre‐eclampsia, hypertension, kidney disease, thrombocytopenia, psychological distress or anorexia, infectious blood disease, atopic eczema or psoriasis. | |
| Interventions | Acupuncture group: bilateral acupuncture points stimulation of points LI4 and SP6. Treatment started at beginning of active phase of first stage of labour. When de‐Qi achieved, needles retained for 2 minutes, then connected to electro‐acupuncture stimulator, at a frequency of 2‐100Hz, current: 14‐30mA. Stimulation increased gradually and needles removed after 20 minutes. When dilation reached 7 cm to 8 cm, procedure performed again. Control group: no pain relief. | |
| Outcomes | Assessment of pain intensity and degree of relaxation throughout the labour. (Assessed hourly. Assessment tool 11‐point scale: 0 = painless and well relaxed; 10 = worst pain imaginable and very tense.) | |
| Notes | Study duration: August 2004 to May 2005. Funding: authors are funded by the Innovation Research Foundation by government of Heilongjiang Privince, China. Conflict of interest: not stated. Setting: affiliated hospital of Heilongjiang University of Chinese Medicine. Country: China. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Lot drawing. |
| Allocation concealment (selection bias) | Unclear risk | quote: "Neither the doctors, midwives, nor the primiparas could predict the group allocation.” |
| Blinding of participants and personnel (performance bias) | High risk | Women and the study practitioner was not blind to the study groups. No other details reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) | Low risk | 3 women excluded from the analysis, 2 acupuncture (no pain or relaxation data available), 1 woman from the control group (no spontaneous labour). |
| Selective reporting (reporting bias) | Unclear risk | Study protocol not available. |
| Other bias | Low risk | No imbalances at baselines, the study appears free of other biases. |
| Methods | Parallel single‐blind, randomised controlled trial of acupuncture. The trial was stratified by parity. Women received acupuncture or no acupuncture. | |
| Participants | 100 women were recruited. Randomisation took place in the delivery suite following admission. Inclusion criteria: 37+ weeks' gestation, spontaneous labour, cephalic presentation, cervical dilatation < 7 cm at admission. Exclusion criteria: diabetes, pre‐eclampsia, kidney disease, thrombocytopenia, psychological distress or anorexia, infectious blood disease, atopic eczema or psoriasis. | |
| Interventions | All women had access to conventional analgesia. 11 midwives completed a 4‐day course in acupuncture for labour pain. These midwives administered acupuncture to the treatment group. Acupuncture treatment was individualised with relaxing points combined with local and distal analgesic points. Needles were inserted at 45 or 90 degrees, stimulated manually until de qui (needling sensation) was obtained. Needles were left in situ and removed after 1‐3 hours. | |
| Outcomes | Pain intensity and degree of relaxation was assessed once every hour, prior to any analgesic and 15 minutes after. Other outcomes included the use of analgesics, augmentation of labour with oxytocin, duration of labour, outcome of birth, antepartum haemorrhage, Apgar scores, and infant birthweight. | |
| Notes | Study duration: April 1999 to June 2000. Funding: supported by grants from Örebro Council Research Committee and Centre for Nursing Science, Örebro University Hospital. Conflict of interest: not stated. Setting: recruited from the antenatal clinic. Country: Sweden. No sample‐size calculation was described. An ITT analysis was performed. Stratified for parity. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was generated by shuffling cards. |
| Allocation concealment (selection bias) | Low risk | Adequate, concealed in sealed, opaque envelopes. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Women and the study practitioner were not blinded to the study groups. No other details reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) | Low risk | 10 (10%) were excluded from the analysis after not meeting the inclusion criteria (breech presentation, not in active labour, not in spontaneous labour, missing pain and relaxation data). 5 from each group relating to not in active labour, breech presentation, not in spontaneous labour, emergency caesarean section, no assessment of pain. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable. |
| Other bias | Low risk | Baseline characteristics comparable between groups, no other identifiable source of bias. |
| Methods | 3‐arm randomised controlled trial. | |
| Participants | Primiparous women at the beginning of active phase of labour, gestational age between 38‐42 weeks, single pregnancy, cephalic presentation of the fetus, and in good health, not diagnosed with any specific diseases, dilation 4 cm and 2 or 3 uterine contractions every 10 minutes. | |
| Interventions | 1. Hoku (Hegu) point (LI4) acupressure 2. SanYinJiao (SP6) acupressure 3. Control group ‐ usual care | |
| Outcomes | Labour pain (before and after the intervention at the stages of 4, 6, 8 and 10 cm cervical dilation), length of labour (in 2 stages: from 4 cm cervical dilation to 10 cm cervical dilatation, and 10 cm cervical dilatation to birth). | |
| Notes | Study duration: 2008 to 2009. Funding: not stated. Conflict of interest: not stated. Setting: Iran Hospital, Iranshahr, Iran. Country: Iran. Translated from Persian. Groups 1 and 2 were combined. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Created 2 blocks and assigned sample numbers equally to each group. |
| Allocation concealment (selection bias) | Low risk | Concealed envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | Women and the study practitioner was not blinded to the study groups. No other details reported. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcome assessor blinded according to author clarification. Analyst unclear. |
| Incomplete outcome data (attrition bias) | Low risk | Predefined outcomes in the methods have been reported on. |
| Selective reporting (reporting bias) | Unclear risk | Outcome measures addressed in the protocol has been reported in the paper but protocol has been registered retrospectively (IRCT138804232170N1). |
| Other bias | Unclear risk | Protocol states that this clinical trial was performed on 60 nulliparas women. Baseline differences not reported. |
| Methods | 2‐group parallel randomised controlled trial. | |
| Participants | 18 to 35 years old, gestational age 37 to 42 weeks (according to LMP or ultrasound in less than 12 weeks), singleton pregnancy, at least 4 cm dilation (entering the active phase of labour), viewing the head, intact amniotic sac at examination, or elapse of 6 hours after the rupture of the amniotic sac, spontaneous onset of uterine contraction, low risk pregnancy (such as the absence of chronic disease like heart disease, hypertension, lung disease, diabetes, anaemia, urinary tract infection, thyroid disease, and epilepsy, did not have abortion, dead fetus, bleeding or any abnormality when referring to the hospital), fetal weight of less than 4000 g (based on Johnson formula), absence of cephalopelvic disproportion during vaginal examination, height of more than 145 cm. No lesions in Sanyinjiao (SP6) and Hegu (LI4) points, no disabilities that lead to communication problems for the mother. | |
| Interventions | At 4 cm dilation, with the start of the contraction in the experimental group (SP6 and LI4), the research assistant applied vertical pressure with thumbs on the sanyinjiao (SP6) points of both inner ankles of the patient. With the start of the first contraction, pressure was applied gradually for 30 seconds on the above mentioned points. Then this pressure was slowly intensified to the extent that the patient felt tingling, numbness, heaviness, and strain in the surrounding area. The amount of applied pressure was identified by the research assistant’s thumb nail colour. When the thumb nail turned white the most pressure was applied. At this point the pressure was held for 1 minute and then it was gradually decreased. The points were free of pressure for 30 seconds. Then for 5 minutes the hegu (LI4) points on both hands were pressed during the contractions followed by the pressure on the sanyinjiao (SP6) points on the inner ankle for 5 minutes. This process continued for 20 minutes. Control group: pressure applied on ineffective areas of the legs and hands with the same timing and condition as the above and by the research assistant's thumb. The pressure in the control group was to the extent that the participants felt the first pain. | |
| Outcomes | Primary: intensity of labour pain as assessed using VAS. Secondary: duration of labour. | |
| Notes | Study duration: February 2012 to May 2012. Funding: Tabriz University of Medical Sciences funding. Conflict of interest: authors state there is no conflicts of interest. Setting: delivery room of Alavi and Sabalan Hospitals. Country: Iran. Clinical trials register: Iranian Registry of Clinical Trials IRCT201106143027N5. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated variable block design. |
| Allocation concealment (selection bias) | Unclear risk | Not described, but implied. |
| Blinding of participants and personnel (performance bias) | Low risk | Blinded. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported as detailed on the Clinical trials register: Iranian Registry of Clinical Trials IRCT201106143027N5. No protocol available. |
| Other bias | Low risk | No significant baseline imbalances. |
| Methods | Single‐blind, randomised controlled trial of acupuncture versus minimal acupuncture. | |
| Participants | 210 women were recruited. Women with a singleton pregnancy, cephalic presentation, in spontaneous active labour met the inclusion criteria. 110 women refused to participate in the trial. | |
| Interventions | Real acupuncture followed a treatment protocol. The protocol specified obtaining the de qi sensation, needles were taped and left in place until delivery or until conventional analgesics were required. Acupuncture points included HT7, LU7, ST30, ST29, GB34, ST36, SP8, SP6, KI3, GB41, LR3, GV20, BL34, BL32, LI4, BL67, BL60. Minimal acupuncture involved the same procedure but needles were inserted away from the meridians. Some needles were removed after 20 minutes if insufficient pain relief was provided by the treatment and control interventions. Conventional pain relief was made available. Midwives providing the intervention had received formal training in acupuncture. | |
| Outcomes | Pain was assessed along a 10 cm VAS, recorded at 30 minutes, 1 and 2 hours after treatment, the need for conventional pain relief and use of oxytocin. | |
| Notes | Study duration: 13 months during 1998/1999. Funding: not stated. Conflict of interest: not stated. Setting: maternity ward. Country: Norway. No power analysis was reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was assigned by drawing lots. |
| Allocation concealment (selection bias) | Low risk | Adequate, randomisation concealed in sealed in opaque envelopes. |
| Blinding of participants and personnel (performance bias) | Low risk | Women were blinded to their group allocation and study personnel collecting data were unaware of women's study group allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) | Low risk | 2 women were excluded from the control group because they delivered prior to the intervention being administered. |
| Selective reporting (reporting bias) | Unclear risk | Study protocol unavailable. Limited study outcomes reported. |
| Other bias | High risk | There was an imbalance in parity at baseline. |
| Methods | 2‐arm randomised controlled trial of electro‐acupuncture versus control (no medication). | |
| Participants | 50 women with a normal singleton pregnancy 37 to 42 weeks' gestation, in labour, cephalic presentation, intact membranes with a cervical dilatation of 4 cm to 5 cm, at least 50% effaced, and Universal Pain Assessment Tool (UPAT) score for pain intensity and relaxation of not more than 3. Exclusion criteria: diagnosis of hypertension, cardiovascular, pulmonary, renal, gastrointestinal, and hematological diseases, moderate to severe dermatologic conditions. | |
| Interventions | The acupuncture points used were Hegu (LI‐4) and (SP‐6) bilaterally. Treatment was started at the beginning of the active phase (4‐5 cm cervical dilatation) in the first stage of labour. Stainless steel filiform needles (gauge 32: 0.25 mm diameter by 25 mm long) were inserted into the acupoints to depths of 15 mm (Hegu LI4), and 20 mm (SP6Sanyinjiao) and the needles were retained for 2 minutes. Then, the handles of the needles were connected to the electro‐acupuncture stimulation apparatus, at a frequency of 2‐100 Hz and electric current of 14‐30 mA (tolerable strength) with a dense‐and‐sparse wave form. The stimulation strength was increased gradually. The needles were removed after 20 minutes. All acupuncture procedures were done by the author, a certified acupuncturist with 2 years of training and 7 years in the practice of acupuncture. Conrol: no pain relief at the start of the active phase of labour. In both groups, patients with pain scale of > 7 were given 50 mg meperidine and 25 mg promethazine at 7 cm dilation | |
| Outcomes | Pain score, use and dose of oxytocin. Apgar score and mode of birth. | |
| Notes | Study duration: between February 2007 and March 2008 Funding: not stated Conflict of interest: not stated Setting: Mary Chiles General Hospital Country: Phillipines | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The numbers 1‐50 were selected randomly by drawing of lots to be designated as belonging to Group A or B. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) | High risk | Open‐label trial no blinding of participants |
| Blinding of outcome assessment (detection bias) | Low risk | Independent assessor. An independent observer (same for both groups) was also asked to rate the patient using the same tool. |
| Incomplete outcome data (attrition bias) | Unclear risk | There are data for 50 participants, but there is no mention of missing data or otherwise |
| Selective reporting (reporting bias) | Unclear risk | Not stated – no protocol referenced |
| Other bias | Low risk | None. No significant difference existed in age of patients, age of gestation, parity and birthweight of the baby between the 2 groups. |
| Methods | 3‐armed, randomised controlled trial. | |
| Participants | 303 nulliparas, normal singleton pregnancies, cephalic presentation, 37 + 0 to 41 + 6 gestational age, expressed need for labour pain relief, admitted to delivery ward in active or latent phase of labour, spontaneous onset of labour. Sufficient Swedish for consent. | |
| Interventions | 1. Manual acupuncture: MA group ‐ needles were inserted and stimulated manually until DeQi achieved and thereafter stimulated at 10‐minute intervals. 2. Electro‐acupuncture: EA group, needles were inserted and first stimulated manually until DeQi achieved, then 8 of the local needles were connected to an electrical stimulator which was set at a high frequency (80 Hz) stimulation. The decision regarding which local needles were to be connected to the stimulator was made by the midwife. The woman adjusted the intensity of the electrical stimulation herself to a level just under the pain threshold. The remaining needles were stimulated manually every ten minutes by the midwife until DeQi was achieved. The women in the EA group received a combination of electrical and manual stimulation. MA or EA treatment was repeated after 2 hours, and thereafter made available on request. After the first treatment with acupuncture, women in the MA end EA groups had access to all the other pharmacological and non‐pharmacological methods of pain relief available on the delivery wards. After randomisation and when requesting pain relief, women in the MA and EA groups were treated with 13–21 needles, at 3 bilateral distal points and 4–8 bilateral local points, all within the same somatic area as the cervix and uterus. The local points were chosen with regard to the pain location. The needles were removed after 40 minutes. 3. Control group: usual care: women had access to all forms of pain relief with the exception of acupuncture, and the choice of which pain relief that was used was made by the woman and the midwife together. Pain relief included pharmacological analgesia (NO2, EDB, morphine), SWI, TENS. | |
| Outcomes | Outcomes: primary: women’s self‐assessment of labour pain. Secondary: experience of relaxation, use of epidural analgesia, satisfaction with pain relief. Outcomes reported in trial design paper also include: labour outcomes: mode of birth, pain relief, augmentation of labour, duration of labour and perineal trauma. Negative side effects, experience of midwife support, pro‐inflammatory cytokines (IL‐1, IL‐6, hs‐CRP, TNF‐alpha). Memory of labour and pain and overall childbirth experience. Infant outcomes: Apgar score, pH, BE, neonatal transfer. | |
| Notes | Study duration: November 2008 to October 2011. Funding: funded by grants from the Centre for Clinical Research Dalarna, Karolinska Institutet, Uppsala‐Örebro Regional Research Council, University of Skövde, FOU Fyrbodal, Magnus Bergvall. Stiftelse, and Dalarna University, Sweden. Conflict of interest: authors state there are no conflicts of interest. Setting: delivery wards at 2 Swedish hospitals. Country: Sweden. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation sequence. The randomisation was conducted in blocks with the length of 9, 12 and 15 which varied randomly. |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes. |
| Blinding of participants and personnel (performance bias) | High risk | No blinding. |
| Blinding of outcome assessment (detection bias) | High risk | Not blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | MA group: 99 randomised – 16 did not receive MA; 19 did not receive MA according to study design (3 did not fulfilled inclusion criteria; 13 received < 7 needles; 9 had Rx < 40 minutes). N = 64 received MA according to study design. EA group: 103 randomised ‐ 16 did not receive EA; 35 did not receive MA according to study design (5 did not fulfilled inclusion criteria; 14 received < 7 needles; 16 had Rx < 40 minutes). N = 52 received MA according to study design. SC group: 101 randomised ‐ 18 did not receive SC; 8 did not receive SC according to study design (8 did not fulfilled inclusion criteria). N = 75 received SC according to study design MA group: ITT n = 83; PP n = 64 EA group: ITT n = 87; PP n = 52 SC group: ITT n = 83; PP n = 75 |
| Selective reporting (reporting bias) | Low risk | Trial protocol published. Some outcomes on blood sampling not reported. |
| Other bias | Unclear risk | No baseline imbalances. |
APG: acupressure group
ITT: intention to treat
LMP: last menstrual period
SCG: standard care group
SWI: sterile water injections
TENS: transcutaneous electrical nerve stimulation
TG: touch group
VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| This study was not randomised. | |
| Outcome measures for this study did not match those of the review. No pain measures were recorded. | |
| Reports methods. | |
| We were unable to establish study details to determine details of randomisation, blinding and data completeness. | |
| Study is investigating the effect of ice massage at acupoints. Study design is not consistent with review. | |
| We were unable to establish study details to determine the exact study design. | |
| Study uses a quasi‐experimental study design. | |
| Study assesses the effect of the intervention delivered postpartum. | |
| Study is investigating the effect of ice massage at acupoints. Study design is not consistent with review. | |
| Study is investigating the effect of ice massage at acupoints. Study design is not consistent with review. | |
| Study uses pethidine as control group. | |
| Study uses multiple techniques for pain management. Confounding effect of combination of techniques being evaluated. | |
| We were unable to confirm if the study was a randomised controlled trial following communication with the authors. | |
| This trial evaluated the effect of 2 acupuncture points on the strength and timing of uterine contractions following acupuncture. It did not report on any primary outcomes relevant to this review by study group. | |
| Study is designed for length of labour, not for pain management in labour. | |
| Control group uses epidural analgesia. Confounding effect of control intervention. | |
| Uses sterile water injections at acupoints and then acupuncture. Confounding effect of SWI. | |
| Intervention is care by a doula plus acupuncture. Outcome measure is anxiety not pain. Counfounding effect of other models of care. | |
| Study is for cervical ripening in preparation for labour, not pain management in labour. | |
| Outcome measures are fetal well‐being and anxiety, not pain management. Not consistent with review. | |
| Study uses TENS machine. This is the subject of another review and is not covered by this one. | |
| Study involved osteopathic treatment and is not consistent with acupuncture/acupressure review. | |
| Only abstract published. Insufficient data reported to assess if eligibility criteria met. | |
| Non randomised study. | |
| The trial assessed anxiety during labour. | |
| We were unable to establish the study design quasi‐randomised or a controlled clinical trial. | |
| Twenty‐five women recruited during labour at a maternity hospital in Israel. Thirteen women randomised to receive electroacupuncture and 12 women received no analgesia at the start of the active phase of labour (cervical dilatation 4 cm, effacement 60%). The study reported on beta endorphin levels and did not report on any measures relevant to this review. | |
| In this trial of 161 women, the effect of acupuncture on Hegu point was examined in relation to the length of the second stage of labour and the amount of postpartum bleeding. The study was excluded as it did not examine the effect on pain relief. | |
| We were unable to establish the study design quasi‐random or a controlled clinical trial. | |
| Cohort study | |
| Not a randomised study. | |
| Use of sterile injection confounded effects of the intervention. | |
| The evaluation of point injection therapy did not meet our eligibility criteria. | |
| Study does not use a randomised design. |
SWI: sterile water injections
TENS: transcutaneous electrical nerve stimulation
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | 3‐arm parallel randomised control trial of 150 women. |
| Participants | 18–35 years of age, term pregnancy, singleton pregnancy, and healthy fetal membranes, no history of medical, surgical, or mental problems, no pregnancy complications. The participants’ uterine contractions started spontaneously and, at admission, the contractions occurred every 5–10 minutes and cervical dilatation was 3 cm to 4 cm. |
| Interventions | 1. Acupressure: the participants were located in the appropriate position and BL32 acupoint was pressed. Pressure was applied by the beginning of contractions (3 to 4 cm cervical dilatation) and continued during the transitional phase of labour (7 cm to 8 cm cervical dilatation), up to the end of the first stage. When the contractions began, the point was pressed gently for 30 seconds. The researcher applied pressure by the right and the left thumbs was measured as 1405 and 1277 mmHg, respectively. The pressure was applied by the beginning and stopped at the end of the contractions. 2. Doula/supportive care: the doula (the researcher) was constantly beside the mother from maternity ward admission (beginning of the active phase of labour at 3 cm to 4 cm cervical dilatation) to the end of the second stage of labour. Supportive measures classified into psychological and emotional, educational, and physical categories were offered to the mother. Psychological and emotional support included touching, empathy, compassion, encouraging the mother to continue co‐operation in the labour process, reassurance, taking mother’s hands, maintaining eye contact, creating a sense of trust and confidence, continuous talking, and reduction of fear during labour. Educational support included informing the mother about the natural process of childbirth and answering her questions. Finally, physical support included cooling the mother, satisfying her hunger and thirst, and helping her change the positions in various stages of labour. These positions were as follows: the mothers followed activity positions, such as straddling a chair, leaning, tailor stretching, and lunging for 20 minutes at 3 cm to 8 cm dilatation. Then, they were required to follow relaxing positions, such as semi sitting and side‐lying for 10 minutes. At 8 cm to 10 cm dilatation, the mothers followed fetal head descent positions, such as dangling, squatting, and hands and knees. 3. Routine care. |
| Outcomes | VAS 10‐point scale following 30‐minute intervention, mode of birth. |
| Notes | Location: Iran. Setting: delivery ward. Authors were contacted seeking clarification of methods of randomisation, no response obtained. |
| Methods | 3‐arm parallel randomised control trial of 150 women. |
| Participants | 18–35 years of age, term pregnancy, singleton pregnancy, and healthy fetal membranes, no history of medical, surgical, or mental problems, no pregnancy complications. The participants’ uterine contractions started spontaneously and, at admission, the contractions occurred every 5–10 minutes and cervical dilatation was 3 cm to 4 cm. |
| Interventions | 1. Acupressure: the participants were located in the appropriate position and BL32 acupoint was pressed. Pressure was applied by the beginning of contractions (3 cm to 4 cm cervical dilatation) and continued during the transitional phase of labour (7 cm to 8 cm cervical dilatation) up to the end of the first stage. when the contractions began, the point was pressed gently for 30 seconds. The researcher applied pressure by the right and the left thumbs was measured as 1405 and 1277 mmHg, respectively. The pressure was applied by the beginning and stopped at the end of the contractions. 2. Doula/supportive care: the doula (the researcher) was constantly beside the mother from maternity ward admission (beginning of the active phase of labour at 3 cm to 4 cm cervical dilatation) to the end of the second stage of labour. Supportive measures classified into psychological and emotional, educational, and physical categories were offered to the mother. Psychological and emotional support included touching, empathy, compassion, encouraging the mother to continue cooperation in the labour process, reassurance, taking mother’s hands, maintaining eye contact, creating a sense of trust and confidence, continuous talking, and reduction of fear during labour. Educational support included informing the mother about the natural process of childbirth and answering her questions. Finally, physical support included cooling the mother, satisfying her hunger and thirst, and helping her change the positions in various stages of labour. These positions were as follows: the mothers followed activity positions, such as straddling a chair, leaning, tailor stretching, and lunging for 20 minutes at 3 cm to 8 cm dilatation. Then, they were required to follow relaxing positions, such as semi sitting and side‐lying for 10 minutes. At 8 cm to 10 cm dilatation, the mothers followed fetal head descent positions, such as dangling, squatting, and hands and knees. 3. Routine care. |
| Outcomes | Length of labour, Apgar scores. The Apgar scores are reported as < 8. Not standard reporting. |
| Notes | The authors were contacted for further information on the methodology of the study. To date no response has been received. |
| Methods | Parallel randomised controlled trial of 200 women. |
| Participants | Women undergoing normal labour. |
| Interventions | Electro‐acupuncture with G6805 needles, with 3‐5 volt, 1500–3000 Hz. |
| Outcomes | Pain control, length of labour, Apgar scores. |
| Notes | The authors were contacted for further information on the methodology of the study. To date no response has been received. |
| Methods | Randomised controlled trial of 128 women. |
| Participants | Pregnant women, nulliparous or multiparous (second pregnancy), 37 weeks, cephalic presentation, cervical dilatation of 3 cm, admitted to the hospital. |
| Interventions | 1. 30 minutes of acupressure on SP‐6 point (6 seconds constant pressure on uterine contractions to the point that participants have a little pain at the site and then 2 seconds of rest, moderate to severe pressure, average pressure was measured as pressure of 1600 mmHg of right thumb and 1300 mmHg of the left thumb; severe pressure was measured as pressure of 2000 mmHg of right thumb and 1800 mmHg of the left thumb). 2. 30 minutes of touch on SP‐6 point. |
| Outcomes | Apgar score at 1 minute and 5 minute, labour pain and pain intensity (VAS scale) before intervention, immediately after intervention, 30 minutes after intervention, and then every hour until the end of the first stage of labour. |
| Notes | The authors were contacted for further information on the methodology of the study. To date no response has been received. |
| Methods | Single‐blind parallel randomised controlled trial. |
| Participants | 174 cases of singleton primiparas. |
| Interventions | Moxibustion applied to an acupuncture point versus moxa to a non acupuncture point and no treatment. |
| Outcomes | Length of labour, Apgar scores. |
| Notes |
| Methods | Randomised controlled trial of acupressure versus oxytocin |
| Participants | 100 women recruited from a private hospital in Turkey. Inclusion criteria: singleton pregnancy, primiparous, in active spontaneous labour. |
| Interventions | Acupressure at point SP6 versus oxytocin |
| Outcomes | Labour, pain, anxiety. length of labour. |
| Notes | Awaiting full text, conference abstract of poster findings only |
| Methods | Randomised controlled trial. |
| Participants | Singleton pregnancy, 38‐42 weeks, cephalic presentation, intact membranes, no disease or restrictions to perform acupressure and electrical stimulation of the skin (skin disorders such as eczema and skin infections) and heart disorders. |
| Interventions | 1. Acupressure group: cervical dilation 3 cm to 4 cm at the beginning of uterine contractions, a researcher massaged the SP6 area (4 fingers above the ankle) on both legs for half an hour. The pressure was ended when uterine contraction was finished. 2. TENS group: clinical Tens novin (model: NEWDYNE 40B) was used. In each leg, a pair of electrodes was placed in the SP6 area. In 3 cm to 4 cm cervical dilatation, skin needle‐like flow of electrical stimulation was maintained continuously and up to the patient's tolerance for half an hour (4 Hz frequency and length of 200 metres per second). This flow increased up to her tolerance each time she felt the flow rate reducing. 3. Control group. |
| Outcomes | Pain intensity (3 groups) and satisfaction of technique for its use in the next delivery (2 groups). |
| Notes | The authors were contacted for further information on the methodology of the study. To date no response has been received. |
| Methods | 3‐armed randomised controlled trial. |
| Participants | The participants were 131 pregnant women between 38‐42 weeks of pregnancy and in labour. They were 18 to 35 years old; parity of 1 or 2; not using medications (psychotherapeutics, labour induction medications, chemical or natural pain killers) prior to the study; cervical dilatation of 3 cm to 5 cm; normal uterine contraction (20 seconds repeated every 5 minutes or less); body mass index less than 29; lack of medical or obstetrical problems such as uterine myomas, precancerous lesions, cephalopelvic disproportion, infertility or surgical operation on uterus or cervix, placenta previa, placental abruption, polyhydramnios or oligohydramnios, erythroblastosis fetalis, pre‐eclampsia, gestational diabetes, decreased fetal movements; no use of tobacco (e.g. smoking, hubble bubble, drugs) or alcohol and no verbal, auditory, or mental problems. Exclusion criteria: lack of consent; oxytocin dose in excess of routine requirements and any sign of fetal distress such as a heart rate of over 160 or less than 110 beats/minute, late decelerations, thick meconium staining and prolonged or precipitate labour, newborn weighing less than 2500 g or more than 4000 g. |
| Interventions | Acupressure on SP6 versus light touch at SP6 and usual care. |
| Outcomes | Labour pain intensity, labour duration and mode of birth. |
| Notes | The authors were contacted for further information on the methodology of the study. To date no response has been received. |
| Methods | 4‐arm randomised controlled trial. |
| Participants | Women were full term (38‐42 weeks' gestation), primigravida, with singleton pregnancy, no cervical or obstetric diseases, healthy fetus, no cephalopelvic disproportion, no contraindications to vaginal delivery, no contraindications to spinal analgesia. |
| Interventions | 1. HANS group (group I): acupuncture at ZhiYang point and JiZhong point. Stimulated at 2/100Hz at 6‐second intervals. The stimulation is at 2Hz and 100 Hz for 0.6ms and 0.2ms, respectively. All titrated up to patient tolerance; usually at 8‐12 mA for ZhiYang, and 15‐25mA for JiZhong point. The acupuncture is done hourly for a total of 30 minutes. 2. Placebo + PCEA (group II): intradural inserted at L3‐5 with lidocaine 6 mL; PCA is given at 4 mL per press, and is subsequently locked for 15 minutes; max is 20 mL per hour. Baseline is given at 0.1 mL per hour. 3. HANS + PCEA (group III): acupuncture as per group I and PCEA as per group II. 4. Control; no intervention (group IV): no intervention. |
| Outcomes | Maternal parameters (blood pressure in kPa, heart rate in beats per minute, breathing in breaths per minute): every 30 minutes from start of stage I labour to completion of delivery. SpO2 – oximetry every half‐hourly; if lower than 90%, given oxygen. Uterine contractions and time of labour. Fetal heart rate every 15‐30 minutes measurement. VAS pain scoring of 0 to 10, measured at pre‐intervention, and every half‐hour post intervention. Neonatal Apgar (1 minute, 5 minute). Adverse events: blood pressure decrease, respiratory arrest, nausea, urinary retention, those requiring labour augmentation (Intravenous or surgical caesarean delivery). Volume of PCEA used and number of PCA presses. Postpartum haemorrhage (total during delivery and up to 2 hours after). |
| Notes | Translated from Chinese. |
| Methods | 3‐arm randomised controlled trial ‐ acupressure versus sham acupressure versus control. |
| Participants | 162 pregnant nulliparous women without any symptoms of labour from Shahid Akbar Abadi Hospital in Tehran, 2015. Inclusion criteria: gestational age of 39‐41 weeks ؛ nulliparous women؛ Bishop score < 4. Exclusion criteria: discontinuing of the study by mother request؛ taking chemical or herbal drugs. |
| Interventions | 1. Acupressure Acupressure was performed in the SP6, BL32, and BL60 at 39‐40 weeks of gestation in low‐risk participants. 30 minutes, twice per day. 2. Sham acupressure Pressure was applied to an ineffective point for 30 minutes 2 times a day 3. Control group No details in abstract or clinical trial registry. |
| Outcomes | Use of analgesics and oxytocin |
| Notes | Only English abstract available. Full text in Farsi |
| Methods | 2‐arm randomised controlled trial of acupressure and control (no details provided. |
| Participants | 120 primiparous women in labour 2 cm to 3 cm dilated |
| Interventions | Acupressure to points LI4, SP6, LR3, PC6, BL32, BL33. |
| Outcomes | Pain scores, mode of birth, length of labour. |
| Notes | English only abstract awaiting full text in Chinese. |
| Methods | 3‐arm randomised controlled trial of acupressure and music. |
| Participants | 241 pregnant women recruited from a maternity hospital in China. |
| Interventions | Acupressure versus music versus no treatment. |
| Outcomes | VAS (pain) (1, 4, 8, 16, 24 hours) |
| Notes | The authors have been contacted for details on randomisation and for pain data that are presented in a graphical format only. |
| Methods | 2‐arm randomised controlled trial. |
| Participants | Inpatient hospital setting in Hebei, China. Described as normal labour women. |
| Interventions | 1. HANS + Diazepam group (group I): diazepam 10 mg intramuscular injection when cervical dilation of 3 cm. HANS acupuncture delivery system is used, after diazepam is given: 4 pads, each 5 cm‐square of electrode pads are placed on both sides of the T10 and L1/2 spine. Their position is adjusted again when cervical dilation is at 7 cm to 8 cm. 2. Control/Comparison intervention: diazepam only (group II): 10 mg of Intramuscular injection diazepam given when cervical dilation of 3 cm. |
| Outcomes | Pain score (taken when dilation 3 cm, 7 cm to 8 cm, and during labour):
Serum cortisol (taken when dilation 3 cm, 7 cm to 8 cm, and during labour). Serum Beta‐endorphin (taken when dilation 3 cm, 7 cm to 8 cm, and during labour), neonatal Apgar, neonatal blood gas, postpartum haemorrhage, labour time, caesarean section. |
| Notes | The authors were contacted for further information on the methodology of the study. To date no response has been received. |
| Methods | 4‐arm randomised controlled trial. |
| Participants | Healthy, full‐term pregnancy, singleton, vertex presentation, primigravida, cervical dilation 2 cm to 3 cm. |
| Interventions | 1. Hans Acupoint Nerve stimulation (HANS): 4 cm x 9 cm electrode pads, placed on the Han’s acupoint area located at T10 to L3 region, and another at the S2 ‐ S4 region on the back. Current is 2/100Hz, alternating, and at 14 mA to 30 mA. 2. Diazepam: 10 mg IV (D). 3. Both Hans Acupoint Nerve stimulation (HANS + D). 4. Control group: (pads placed, but without any current); no intervention given. |
| Outcomes | Primary VAS for pain measurement – pre intervention, post intervention (1 hour post), during first stage labour (or at cervical dilation 7 cm to 8 cm), during 2nd stage of labour. Secondary Labour progress time, postpartum haemorrhage, surgical augmentation, oxytocin, fetal heart rate, amniotic fluid testing, Apgar score, umbilical artery pH, neonatal respiratory distress, neonatal apnoea. |
| Notes | The authors were contacted for further information on the methodology of the study. To date no response has been received. |
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | We have been unable to locate full‐text article. |
| Methods | Randomised controlled trial of acupuncture compared with placebo acupuncture and no intervention. |
| Participants | 90 women were recruited from a hospital in Tehran, Iran. Inclusion criteria: were normal singleton pregnancy of 37 weeks or longer and a spontaneous onset of labour, cephalic version, cervical dilatation of 3 cm to 6 cm. |
| Interventions | Acupuncture (30 women): solid titanium needles GV20, Yingtang, ST36, SP6, LI4, CV2, 3. Needle insertion began when pre‐treatment pain score of 3 or higher was reached. A feeling of de qi was obtained. Needles left in place until delivery. Control group 1 (30 women): ‘pretend’ acupuncture, solid titanium needles of same type as intervention, inserted at 6 points normally used for vaccinations and other injections. Control group 2 (30 women): no intervention. |
| Outcomes | Pain intensity, relaxation, duration of labour, need for augmentation by oxytocin, caesarean section. |
| Notes | The authors were contacted for further information on the methodology of the study as randomisation status was unclear. To date (September 2017) no response has been received. |
PCEA: patient‐controlled epidural analgesia
SpO2: capillary oxygen saturation
TENS: transcutaneous electrical nerve stimulation
VAS: visual analogue scale
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Comparing the effect of auricular and body acupressure on the pain and duration of the first stage of labour |
| Methods | |
| Participants | Primigravida women aged 19‐35 years. Low‐risk pregnancy: gestational age between 37‐42 weeks; singleton pregnancy; cephalic presentation; no prior medical or surgical complication; height more than 150 cm. Having 3 cm to 4 cm cervical dilatation. Exclusion criteria: having analgesic drugs 3 hours prior to or during intervention Induction or augmentation of labour |
| Interventions | 1‐ Auricular acupressure 2‐ body acupressure 3‐ control with routine care |
| Outcomes | Duration of first stage of labour, labour pain |
| Starting date | 11/3/2018 |
| Contact information | Zainab Alimoradi email [email protected] |
| Notes | Trial is recruiting |
| Trial name or title | The effect of pressure on bile duct 21 on labour pain in primiparous women |
| Methods | Randomised controlled trial |
| Participants | Inclusion criteria: primiparous; age 18‐35 years; cephalic presentation; gestational age 37‐41 weeks; singleton; ability to read and write; tendency to use analgesia; active phase of labour. Exclusion criteria: not having willingness to work with researcher, planned caesarean section |
| Interventions | Pressure group on GB 21 Control group: pressure group on sham point |
| Outcomes | Severity of labour pain. Satisfaction of the treatment course |
| Starting date | 21/1/2018 |
| Contact information | Hamideh Torkiyan Shahid Beheshti University of Medical Sciences, [email protected] |
| Notes | Trial has completed recruitment but is unpublished. |
| Trial name or title | The effect of LI4, H7 and SP6, Neima acupressure on the pain severity and duration of delivery in nulliparous women |
| Methods | Randomised controlled trial. |
| Participants | 144 pregnant women aged 19 to 35 years old, nulliparous gestational age between 42‐37 weeks, singleton and low‐risk pregnancies. Exclusion criteria: oxytocin administration for induction of labour, use of analgesic medications, unreliable embryonic cardiac rhythm. |
| Interventions | Acupressure applied to point SP6 in early labour, and from 8 cm, the points are changed to H7 and LI4 points. Control usual care plus aromatherapy. |
| Outcomes | Pain in labour. |
| Starting date | 21/1/2018. |
| Contact information | Fatemeh Ranjkesh email: [email protected] |
| Notes | Trial recruiting |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 2 | 325 | Mean Difference (IV, Random, 95% CI) | ‐4.42 [‐12.94, 4.09] |
| Analysis 1.1 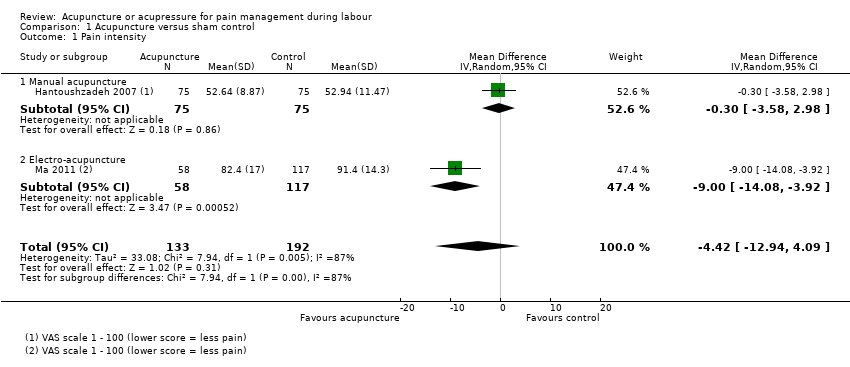 Comparison 1 Acupuncture versus sham control, Outcome 1 Pain intensity. | ||||
| 1.1 Manual acupuncture | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐3.58, 2.98] |
| 1.2 Electro‐acupuncture | 1 | 175 | Mean Difference (IV, Random, 95% CI) | ‐9.0 [‐14.08, ‐3.92] |
| 2 Satisfaction with pain relief in labour Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.38 [1.78, 3.19] |
| Analysis 1.2 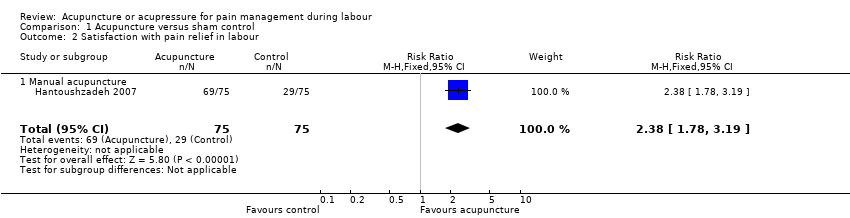 Comparison 1 Acupuncture versus sham control, Outcome 2 Satisfaction with pain relief in labour. | ||||
| 2.1 Manual acupuncture | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.38 [1.78, 3.19] |
| 3 Use of pharmacological analgesia Show forest plot | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.63, 0.89] |
| Analysis 1.3 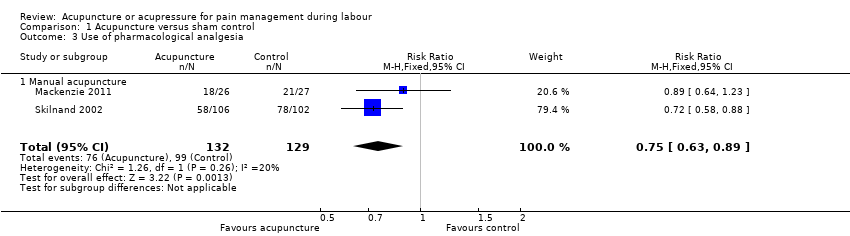 Comparison 1 Acupuncture versus sham control, Outcome 3 Use of pharmacological analgesia. | ||||
| 3.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.63, 0.89] |
| 4 Assisted vaginal birth Show forest plot | 2 | 261 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.41, 2.97] |
| Analysis 1.4  Comparison 1 Acupuncture versus sham control, Outcome 4 Assisted vaginal birth. | ||||
| 4.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.41, 2.97] |
| 5 Caesarean section Show forest plot | 3 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.49, 2.48] |
| Analysis 1.5  Comparison 1 Acupuncture versus sham control, Outcome 5 Caesarean section. | ||||
| 5.1 Manual acupuncture | 3 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.49, 2.48] |
| 6 Apgar score < 7 at 5 minutes Show forest plot | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.79] |
| Analysis 1.6  Comparison 1 Acupuncture versus sham control, Outcome 6 Apgar score < 7 at 5 minutes. | ||||
| 6.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.79] |
| 7 Length of labour ‐ total Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 1.7 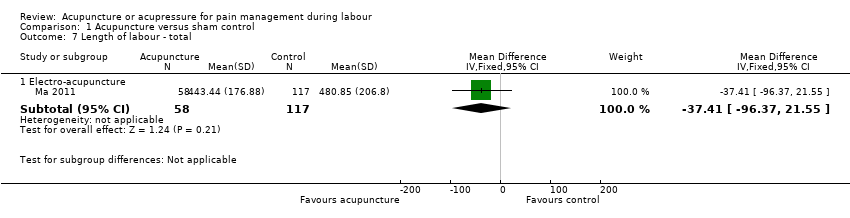 Comparison 1 Acupuncture versus sham control, Outcome 7 Length of labour ‐ total. | ||||
| 7.1 Electro‐acupuncture | 1 | 175 | Mean Difference (IV, Fixed, 95% CI) | ‐37.41 [‐96.37, 21.55] |
| 8 Spontaneous vaginal birth Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.8  Comparison 1 Acupuncture versus sham control, Outcome 8 Spontaneous vaginal birth. | ||||
| 8.1 Manual acupuncture | 3 | 411 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.86, 1.12] |
| 9 Augmentation with oxytocin Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.9 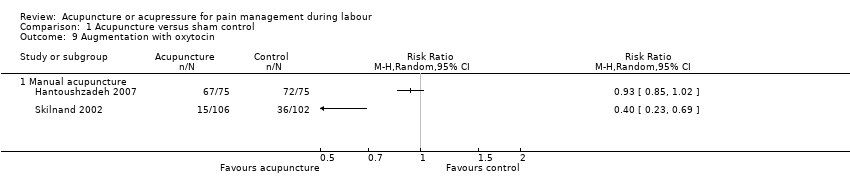 Comparison 1 Acupuncture versus sham control, Outcome 9 Augmentation with oxytocin. | ||||
| 9.1 Manual acupuncture | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 4 | 495 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.31 [‐2.14, ‐0.49] |
| Analysis 2.1  Comparison 2 Acupuncture versus usual care, Outcome 1 Pain intensity. | ||||
| 1.1 Manual acupuncture | 2 | 270 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐2.36, 0.58] |
| 1.2 Electro‐acupuncture | 2 | 225 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.79 [‐3.37, ‐0.21] |
| 2 Satisfaction with pain relief in labour Show forest plot | 2 | 343 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.96, 1.20] |
| Analysis 2.2  Comparison 2 Acupuncture versus usual care, Outcome 2 Satisfaction with pain relief in labour. | ||||
| 2.1 Manual acupuncture | 2 | 215 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.95, 1.23] |
| 2.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.87, 1.30] |
| 3 Use of pharmacological analgesia Show forest plot | 6 | 1059 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.60, 0.85] |
| Analysis 2.3  Comparison 2 Acupuncture versus usual care, Outcome 3 Use of pharmacological analgesia. | ||||
| 3.1 Manual acupuncture | 5 | 884 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.60, 0.82] |
| 3.2 Electro‐acupuncture | 2 | 175 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.01, 8.16] |
| 4 Assisted vaginal birth Show forest plot | 6 | 1217 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.70, 1.24] |
| Analysis 2.4 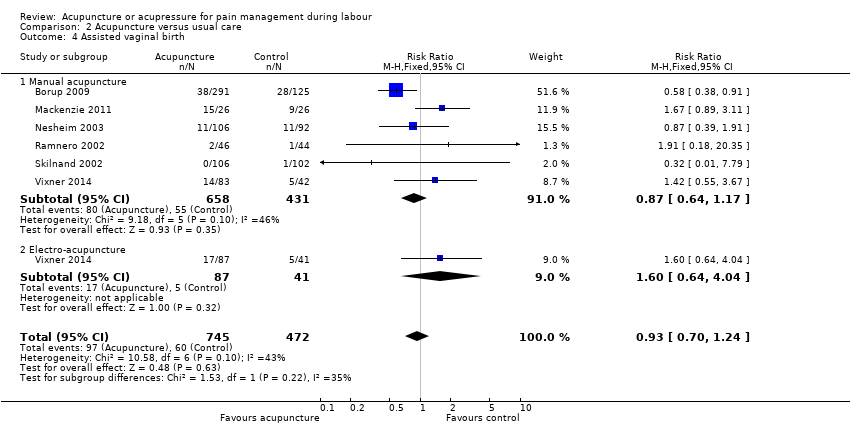 Comparison 2 Acupuncture versus usual care, Outcome 4 Assisted vaginal birth. | ||||
| 4.1 Manual acupuncture | 6 | 1089 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.64, 1.17] |
| 4.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.64, 4.04] |
| 5 Caesarean section Show forest plot | 5 | 861 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.47, 1.09] |
| Analysis 2.5  Comparison 2 Acupuncture versus usual care, Outcome 5 Caesarean section. | ||||
| 5.1 Manual acupuncture | 4 | 683 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.50, 1.24] |
| 5.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.16, 1.28] |
| 6 Apgar score < 7 at 5 minutes Show forest plot | 6 | 1061 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.28, 3.47] |
| Analysis 2.6 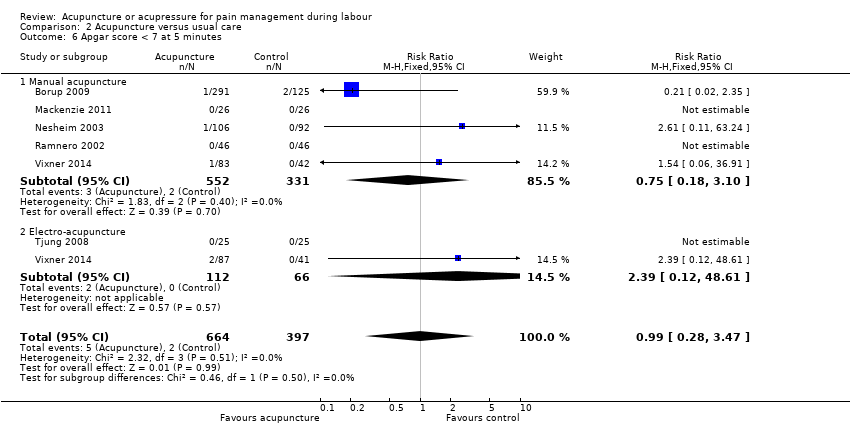 Comparison 2 Acupuncture versus usual care, Outcome 6 Apgar score < 7 at 5 minutes. | ||||
| 6.1 Manual acupuncture | 5 | 883 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.18, 3.10] |
| 6.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [0.12, 48.61] |
| 7 Length of labour ‐ total Show forest plot | 3 | 608 | Mean Difference (IV, Fixed, 95% CI) | ‐13.89 [‐28.93, 1.14] |
| Analysis 2.7  Comparison 2 Acupuncture versus usual care, Outcome 7 Length of labour ‐ total. | ||||
| 7.1 Manual acupuncture | 1 | 124 | Mean Difference (IV, Fixed, 95% CI) | 4.0 [‐142.47, 150.47] |
| 7.2 Electro‐acupuncture | 3 | 484 | Mean Difference (IV, Fixed, 95% CI) | ‐14.08 [‐29.20, 1.03] |
| 8 Spontaneous vaginal birth Show forest plot | 4 | 449 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.89, 1.08] |
| Analysis 2.8  Comparison 2 Acupuncture versus usual care, Outcome 8 Spontaneous vaginal birth. | ||||
| 8.1 Manual acupuncture | 3 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.85, 1.10] |
| 8.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.86, 1.14] |
| 9 Augmentation with oxytocin Show forest plot | 4 | 813 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.77, 1.02] |
| Analysis 2.9  Comparison 2 Acupuncture versus usual care, Outcome 9 Augmentation with oxytocin. | ||||
| 9.1 Manual acupuncture | 3 | 635 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.78, 1.09] |
| 9.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.59, 1.03] |
| 10 Perineal trauma Show forest plot | 1 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.19, 1.26] |
| Analysis 2.10  Comparison 2 Acupuncture versus usual care, Outcome 10 Perineal trauma. | ||||
| 10.1 Manual acupuncture | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.13, 1.92] |
| 10.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.12, 1.79] |
| 11 Maternal blood loss > 500 mL Show forest plot | 1 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.11, 0.78] |
| Analysis 2.11  Comparison 2 Acupuncture versus usual care, Outcome 11 Maternal blood loss > 500 mL. | ||||
| 11.1 Manual acupuncture | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.11, 1.43] |
| 11.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.04, 0.93] |
| 12 Relaxation Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 2.12  Comparison 2 Acupuncture versus usual care, Outcome 12 Relaxation. | ||||
| 12.1 Manual acupuncture | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.62, ‐0.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 1 | 163 | Mean Difference (IV, Fixed, 95% CI) | ‐1.16 [‐1.51, ‐0.81] |
| Analysis 3.1  Comparison 3 Acupuncture versus no treatment, Outcome 1 Pain intensity. | ||||
| 1.1 Electro‐acupuncture | 1 | 163 | Mean Difference (IV, Fixed, 95% CI) | ‐1.16 [‐1.51, ‐0.81] |
| 2 Assisted vaginal birth Show forest plot | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.18, 1.38] |
| Analysis 3.2 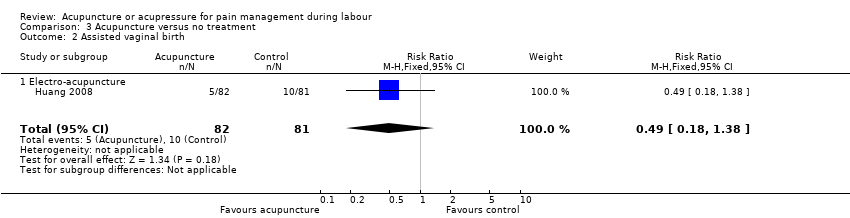 Comparison 3 Acupuncture versus no treatment, Outcome 2 Assisted vaginal birth. | ||||
| 2.1 Electro‐acupuncture | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.18, 1.38] |
| 3 Caesarean section Show forest plot | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.35, 1.63] |
| Analysis 3.3 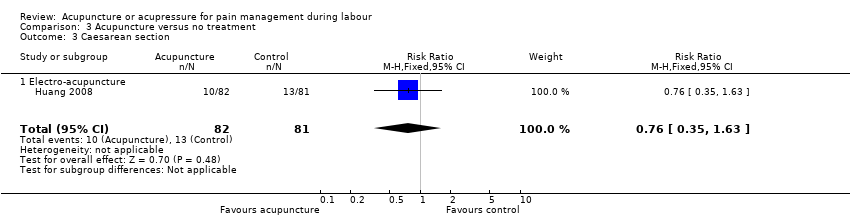 Comparison 3 Acupuncture versus no treatment, Outcome 3 Caesarean section. | ||||
| 3.1 Electro‐acupuncture | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.35, 1.63] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Use of pharmacological analgesia Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.1 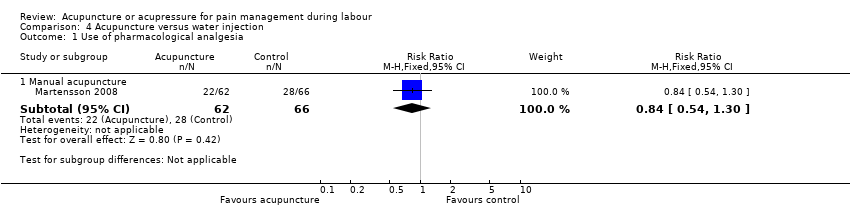 Comparison 4 Acupuncture versus water injection, Outcome 1 Use of pharmacological analgesia. | ||||
| 1.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.30] |
| 2 Assisted vaginal birth Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.2  Comparison 4 Acupuncture versus water injection, Outcome 2 Assisted vaginal birth. | ||||
| 2.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.47, 5.39] |
| 3 Caesarean section Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.3 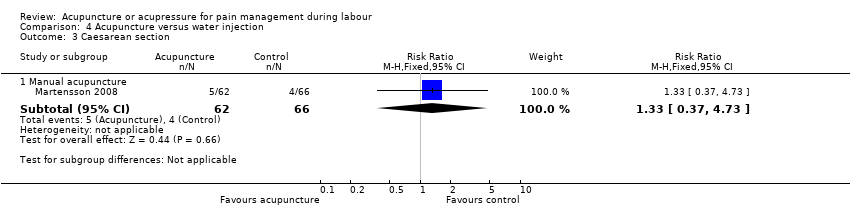 Comparison 4 Acupuncture versus water injection, Outcome 3 Caesarean section. | ||||
| 3.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.37, 4.73] |
| 4 Augmentation with oxytocin Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.4 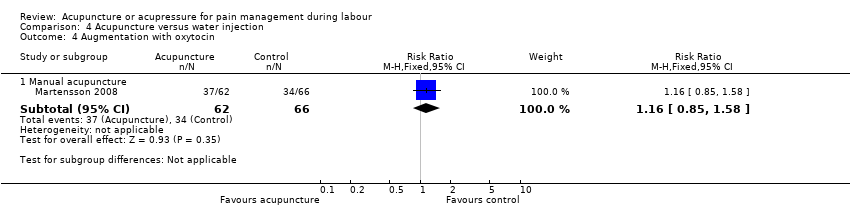 Comparison 4 Acupuncture versus water injection, Outcome 4 Augmentation with oxytocin. | ||||
| 4.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.85, 1.58] |
| 5 Relaxation Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 4.5  Comparison 4 Acupuncture versus water injection, Outcome 5 Relaxation. | ||||
| 5.1 Manual acupuncture | 1 | 128 | Mean Difference (IV, Fixed, 95% CI) | 12.60 [4.75, 20.45] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 6 | 472 | Mean Difference (IV, Random, 95% CI) | ‐1.93 [‐3.31, ‐0.55] |
| Analysis 5.1  Comparison 5 Acupressure versus sham control, Outcome 1 Pain intensity. | ||||
| 2 Use of pharmacological analgesia Show forest plot | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.20, 1.43] |
| Analysis 5.2  Comparison 5 Acupressure versus sham control, Outcome 2 Use of pharmacological analgesia. | ||||
| 3 Assisted vaginal birth Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 71.92] |
| Analysis 5.3  Comparison 5 Acupressure versus sham control, Outcome 3 Assisted vaginal birth. | ||||
| 4 Caesarean section Show forest plot | 4 | 313 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.27, 0.71] |
| Analysis 5.4  Comparison 5 Acupressure versus sham control, Outcome 4 Caesarean section. | ||||
| 5 Apgar score < 7 at 5 minutes Show forest plot | 2 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.99] |
| Analysis 5.5  Comparison 5 Acupressure versus sham control, Outcome 5 Apgar score < 7 at 5 minutes. | ||||
| 6 Length of labour Show forest plot | 4 | 399 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.26, ‐0.57] |
| Analysis 5.6 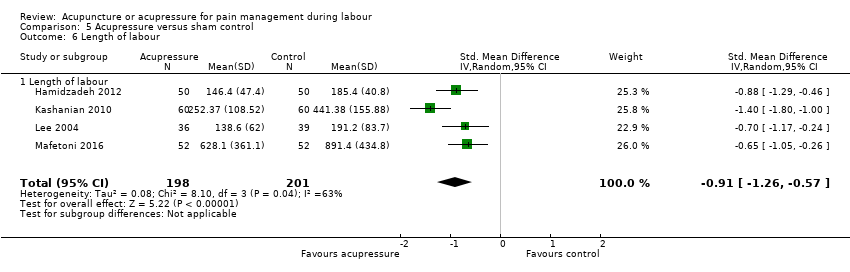 Comparison 5 Acupressure versus sham control, Outcome 6 Length of labour. | ||||
| 6.1 Length of labour | 4 | 399 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.26, ‐0.57] |
| 7 Spontaneous vaginal birth Show forest plot | 2 | 115 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.92, 1.18] |
| Analysis 5.7  Comparison 5 Acupressure versus sham control, Outcome 7 Spontaneous vaginal birth. | ||||
| 8 Augmentation with oxytocin Show forest plot | 2 | 135 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.46, 0.91] |
| Analysis 5.8 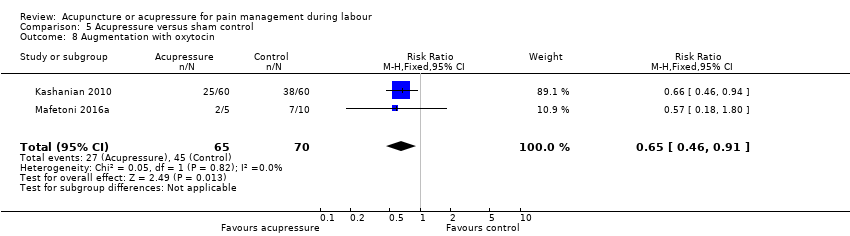 Comparison 5 Acupressure versus sham control, Outcome 8 Augmentation with oxytocin. | ||||
| 9 Anxiety Show forest plot | 1 | 75 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐2.51, ‐0.29] |
| Analysis 5.9 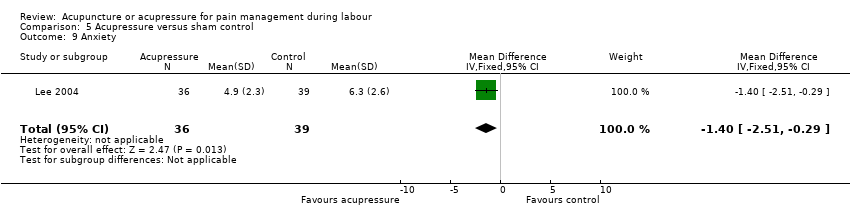 Comparison 5 Acupressure versus sham control, Outcome 9 Anxiety. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 8 | 620 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐1.45, ‐0.69] |
| Analysis 6.1  Comparison 6 Acupressure versus usual care, Outcome 1 Pain intensity. | ||||
| 2 Satisfaction with pain relief Show forest plot | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 1.05 [0.75, 1.35] |
| Analysis 6.2  Comparison 6 Acupressure versus usual care, Outcome 2 Satisfaction with pain relief. | ||||
| 3 Caesarean section Show forest plot | 4 | 391 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.54, 1.23] |
| Analysis 6.3 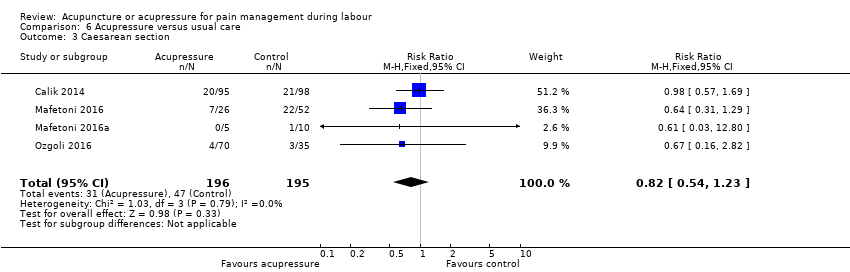 Comparison 6 Acupressure versus usual care, Outcome 3 Caesarean section. | ||||
| 4 Length of labour Show forest plot | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐16.23 [‐79.64, 47.18] |
| Analysis 6.4  Comparison 6 Acupressure versus usual care, Outcome 4 Length of labour. | ||||
| 5 Spontaneous vaginal birth Show forest plot | 3 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.90, 1.21] |
| Analysis 6.5  Comparison 6 Acupressure versus usual care, Outcome 5 Spontaneous vaginal birth. | ||||
| 6 Augmentation with oxytocin Show forest plot | 1 | 15 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.39, 10.31] |
| Analysis 6.6  Comparison 6 Acupressure versus usual care, Outcome 6 Augmentation with oxytocin. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 2 | 322 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.42 [‐0.65, ‐0.18] |
| Analysis 7.1  Comparison 7 Acupressure versus combined control, Outcome 1 Pain intensity. | ||||
| 2 Satisfaction with childbirth Show forest plot | 1 | 212 | Mean Difference (IV, Fixed, 95% CI) | 4.80 [‐2.25, 11.85] |
| Analysis 7.2 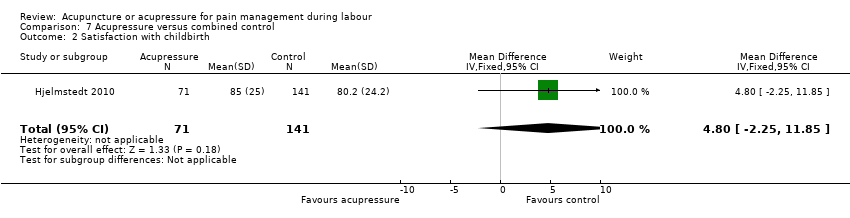 Comparison 7 Acupressure versus combined control, Outcome 2 Satisfaction with childbirth. | ||||
| 3 Use of pharmacological analgesia Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.71, 1.25] |
| Analysis 7.3 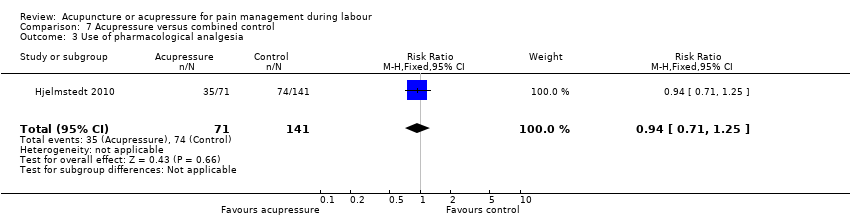 Comparison 7 Acupressure versus combined control, Outcome 3 Use of pharmacological analgesia. | ||||
| 4 Assisted vaginal birth Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.39, 1.67] |
| Analysis 7.4  Comparison 7 Acupressure versus combined control, Outcome 4 Assisted vaginal birth. | ||||
| 5 Caesarean section Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.22, 1.04] |
| Analysis 7.5  Comparison 7 Acupressure versus combined control, Outcome 5 Caesarean section. | ||||
| 6 Augmentation with oxytocin Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.77, 1.31] |
| Analysis 7.6 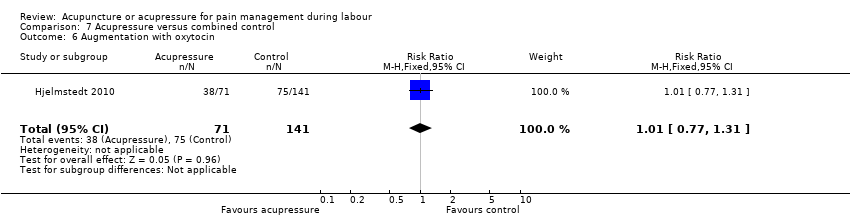 Comparison 7 Acupressure versus combined control, Outcome 6 Augmentation with oxytocin. | ||||

Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
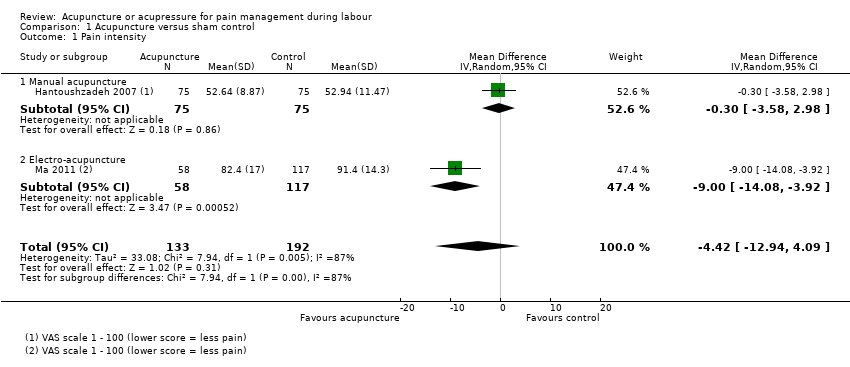
Comparison 1 Acupuncture versus sham control, Outcome 1 Pain intensity.
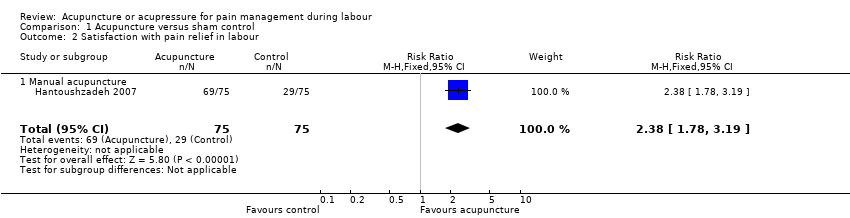
Comparison 1 Acupuncture versus sham control, Outcome 2 Satisfaction with pain relief in labour.
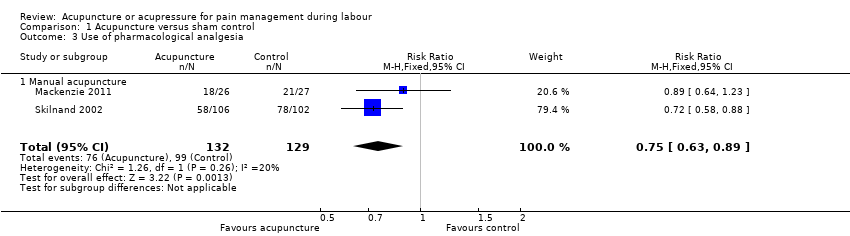
Comparison 1 Acupuncture versus sham control, Outcome 3 Use of pharmacological analgesia.

Comparison 1 Acupuncture versus sham control, Outcome 4 Assisted vaginal birth.

Comparison 1 Acupuncture versus sham control, Outcome 5 Caesarean section.

Comparison 1 Acupuncture versus sham control, Outcome 6 Apgar score < 7 at 5 minutes.
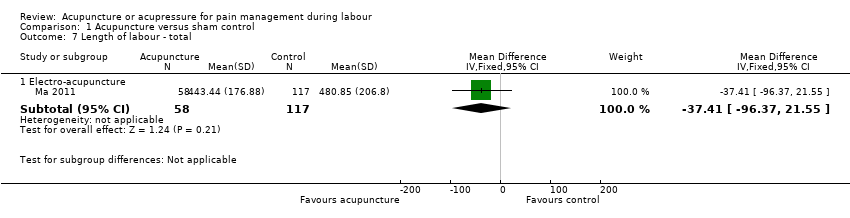
Comparison 1 Acupuncture versus sham control, Outcome 7 Length of labour ‐ total.

Comparison 1 Acupuncture versus sham control, Outcome 8 Spontaneous vaginal birth.
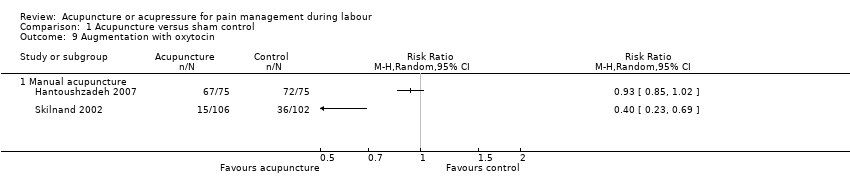
Comparison 1 Acupuncture versus sham control, Outcome 9 Augmentation with oxytocin.

Comparison 2 Acupuncture versus usual care, Outcome 1 Pain intensity.

Comparison 2 Acupuncture versus usual care, Outcome 2 Satisfaction with pain relief in labour.

Comparison 2 Acupuncture versus usual care, Outcome 3 Use of pharmacological analgesia.
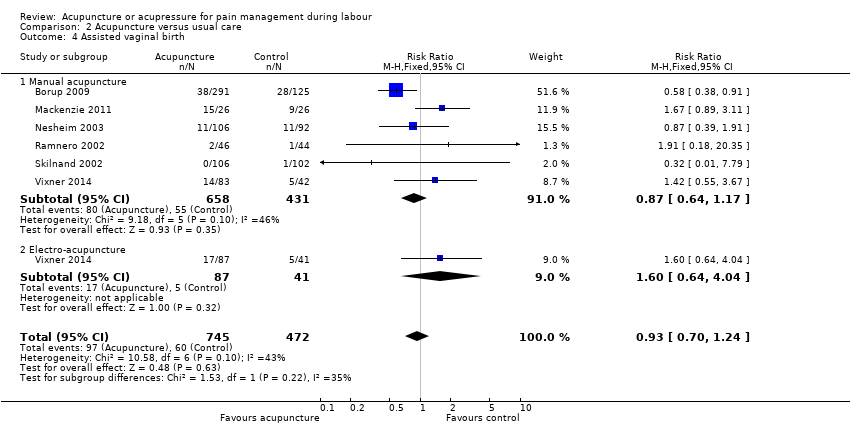
Comparison 2 Acupuncture versus usual care, Outcome 4 Assisted vaginal birth.

Comparison 2 Acupuncture versus usual care, Outcome 5 Caesarean section.
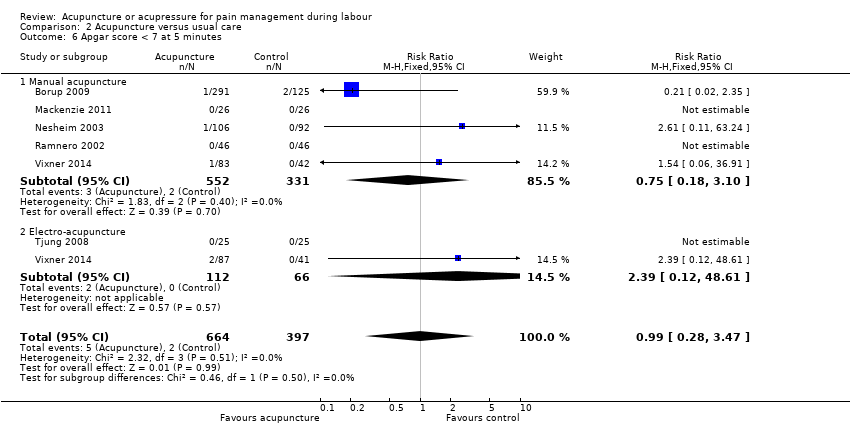
Comparison 2 Acupuncture versus usual care, Outcome 6 Apgar score < 7 at 5 minutes.

Comparison 2 Acupuncture versus usual care, Outcome 7 Length of labour ‐ total.

Comparison 2 Acupuncture versus usual care, Outcome 8 Spontaneous vaginal birth.

Comparison 2 Acupuncture versus usual care, Outcome 9 Augmentation with oxytocin.

Comparison 2 Acupuncture versus usual care, Outcome 10 Perineal trauma.

Comparison 2 Acupuncture versus usual care, Outcome 11 Maternal blood loss > 500 mL.

Comparison 2 Acupuncture versus usual care, Outcome 12 Relaxation.

Comparison 3 Acupuncture versus no treatment, Outcome 1 Pain intensity.
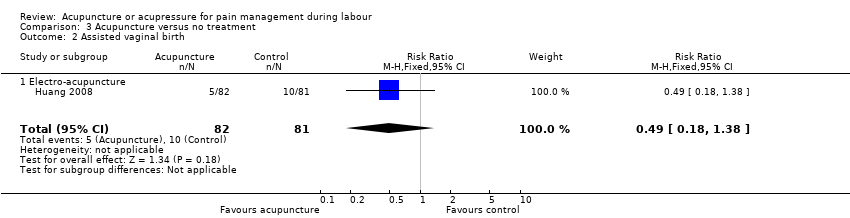
Comparison 3 Acupuncture versus no treatment, Outcome 2 Assisted vaginal birth.
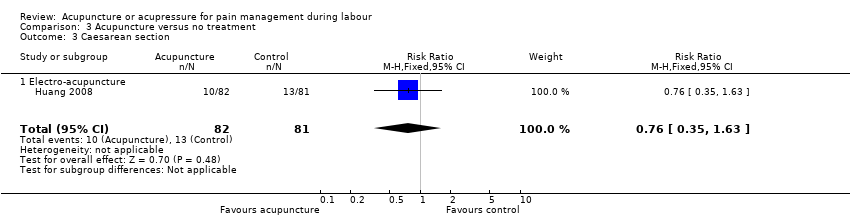
Comparison 3 Acupuncture versus no treatment, Outcome 3 Caesarean section.
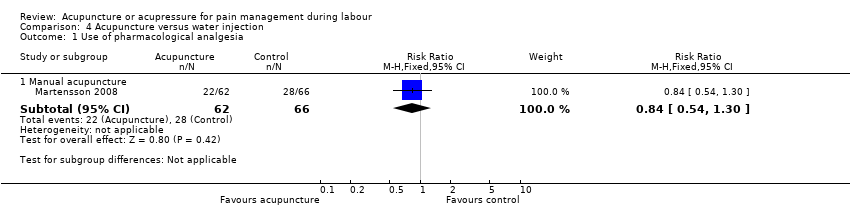
Comparison 4 Acupuncture versus water injection, Outcome 1 Use of pharmacological analgesia.

Comparison 4 Acupuncture versus water injection, Outcome 2 Assisted vaginal birth.
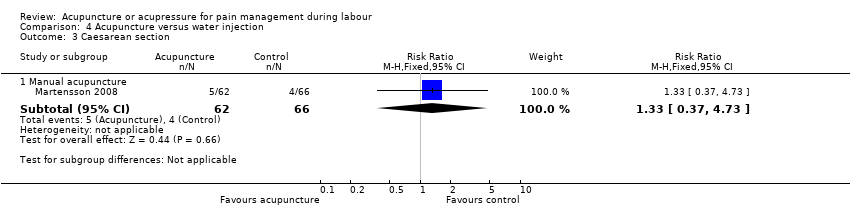
Comparison 4 Acupuncture versus water injection, Outcome 3 Caesarean section.
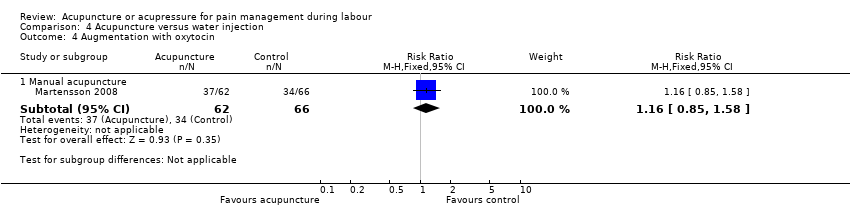
Comparison 4 Acupuncture versus water injection, Outcome 4 Augmentation with oxytocin.

Comparison 4 Acupuncture versus water injection, Outcome 5 Relaxation.

Comparison 5 Acupressure versus sham control, Outcome 1 Pain intensity.

Comparison 5 Acupressure versus sham control, Outcome 2 Use of pharmacological analgesia.

Comparison 5 Acupressure versus sham control, Outcome 3 Assisted vaginal birth.

Comparison 5 Acupressure versus sham control, Outcome 4 Caesarean section.

Comparison 5 Acupressure versus sham control, Outcome 5 Apgar score < 7 at 5 minutes.
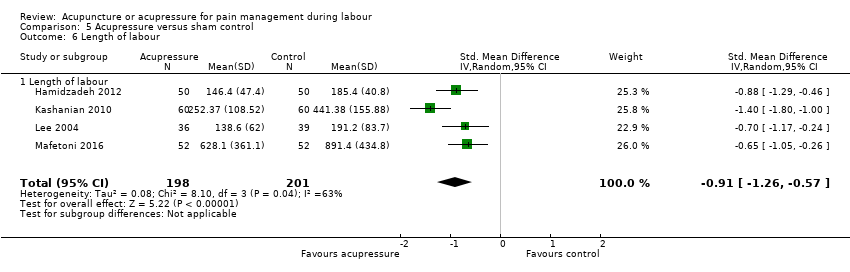
Comparison 5 Acupressure versus sham control, Outcome 6 Length of labour.

Comparison 5 Acupressure versus sham control, Outcome 7 Spontaneous vaginal birth.
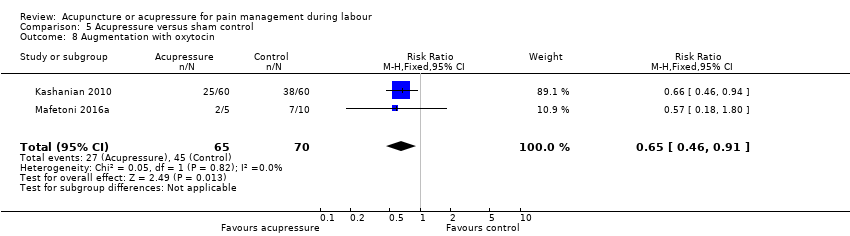
Comparison 5 Acupressure versus sham control, Outcome 8 Augmentation with oxytocin.
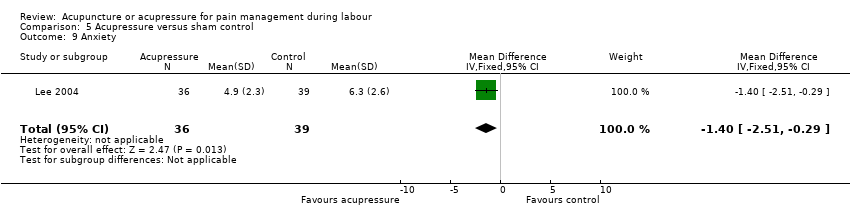
Comparison 5 Acupressure versus sham control, Outcome 9 Anxiety.

Comparison 6 Acupressure versus usual care, Outcome 1 Pain intensity.

Comparison 6 Acupressure versus usual care, Outcome 2 Satisfaction with pain relief.
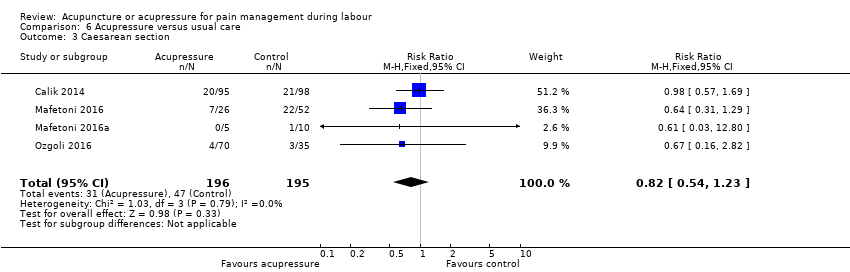
Comparison 6 Acupressure versus usual care, Outcome 3 Caesarean section.

Comparison 6 Acupressure versus usual care, Outcome 4 Length of labour.

Comparison 6 Acupressure versus usual care, Outcome 5 Spontaneous vaginal birth.

Comparison 6 Acupressure versus usual care, Outcome 6 Augmentation with oxytocin.

Comparison 7 Acupressure versus combined control, Outcome 1 Pain intensity.
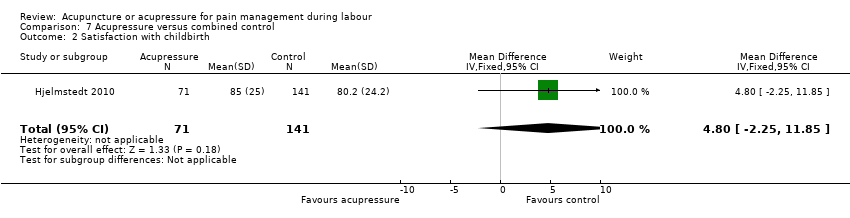
Comparison 7 Acupressure versus combined control, Outcome 2 Satisfaction with childbirth.
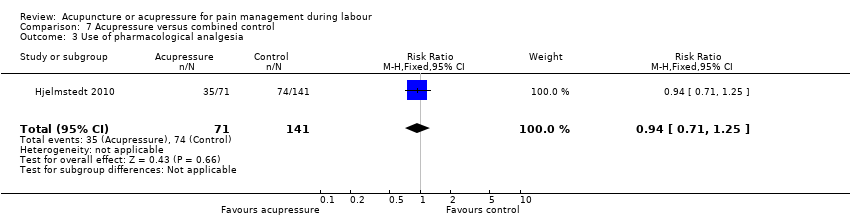
Comparison 7 Acupressure versus combined control, Outcome 3 Use of pharmacological analgesia.

Comparison 7 Acupressure versus combined control, Outcome 4 Assisted vaginal birth.

Comparison 7 Acupressure versus combined control, Outcome 5 Caesarean section.
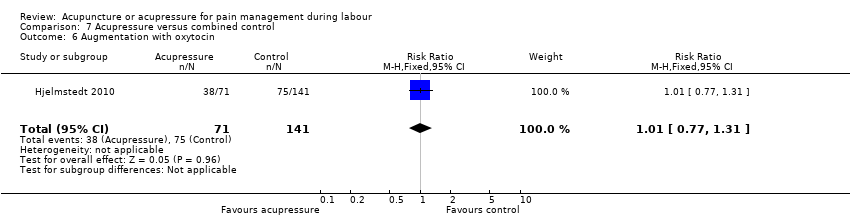
Comparison 7 Acupressure versus combined control, Outcome 6 Augmentation with oxytocin.
| Acupuncture compared to sham control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with sham control | Risk with acupuncture | |||||
| Pain intensity Lower scores indicate less pain intensity | The mean pain intensity ranged across control groups from 52.94 to 91.4 | The mean pain intensity score in the intervention group was 4.42 lower (12.94 lower to 4.09 higher) | 325 | ⊕⊕⊝⊝ | ||
| Satisfaction with pain relief in labour | Study population | RR 2.38 | 150 | ⊕⊕⊕⊝ | ||
| 387 per 1000 | 920 per 1000 | |||||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.75 | 261 | ⊕⊕⊕⊝ | ||
| 767 per 1000 | 576 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.10 | 261 | ⊕⊝⊝⊝ | ||
| 163 per 1000 | 179 per 1000 | |||||
| Caesarean section | Study population | RR 1.11 | 411 | ⊕⊕⊝⊝ | ||
| 49 per 1000 | 54 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: one study high or unclear risk of bias on six domains. 2 Downgraded one level due to serious inconsistency: substantial heterogeneity present I2 = 87% 3 Downgraded one level due to serious imprecision: small sample size (150) 4 Downgraded one level due to serious risk of bias: one study did not blind participants to group allocation. Should not affect sham arm outcome but blinding integrity not reported. 5 Downgraded one level due to serious inconsistency: substantial heterogeneity present I2 = 72% 6 Downgraded one level for imprecision due to small sample size and wide confidence intervals crossing the line of no effect 7 Downgraded one level for imprecision due to small number of events and wide confidence intervals crossing the line of no effect 8 Downgraded one level due to serious risk of bias: one study did not blind participants to group allocation and two studies at high risk of other bias | ||||||
| Acupuncture compared to usual care for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with acupuncture | |||||
| Pain intensity Mix of NRS and VAS scales so analysed using SMD | The mean pain intensity score in the intervention group was 1.31 standard deviations lower (2.14 lower to 0.49 lower) | 495 | ⊕⊝⊝⊝ | |||
| Satisfaction with pain relief in labour | Study population | RR 1.07 | 343 | ⊕⊕⊝⊝ | ||
| 787 per 1000 | 843 per 1000 | |||||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.72 | 1059 | ⊕⊝⊝⊝ | ||
| 833 per 1000 | 600 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 0.93 | 1217 | ⊕⊕⊝⊝ | ||
| 127 per 1000 | 118 per 1000 | |||||
| Caesarean section | Study population | RR 0.72 | 861 | ⊕⊕⊝⊝ | ||
| 116 per 1000 | 83 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels for very serious risk of bias: two of the three studies had high risk of performance bias and this was likely to influence a self‐reported outcome. 2 Downgraded two levels for very serious inconsistency: considerable heterogeneity present (I2 = 93%) not explained by subgroup analysis. 3 Downgraded two levels for very serious risk of bias: both studies had unclear or high risk of bias related to blinding and this was likely to influence a self‐reported outcome 4 Downgraded two levels for very serious risk of bias: all studies had unclear or high risk of performance bias and this was likely to influence the need for additional analgesia. 5 Downgraded one level for serious inconsistency: substantial heterogeneity (I2 = 70%) which is not explained by subgroups. 6 Downgraded one level for serious risk of bias: five of six studies at unclear or high risk of bias in both performance and detection bias. This may have influenced the outcome. 7 Downgraded one level for serious risk of bias: three of four studies at high or unclear risk of bias in both performance and detection bias. This may have influenced the outcome. 8 Downgraded one level for imprecision due to wide confidence intervals. | ||||||
| Acupuncture compared to no treatment for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with no treatment | Risk with acupuncture | |||||
| Pain intensity Lower scores indicate less pain. | The mean pain intensity in the control group was 7.92 | The mean pain intensity score in the intervention groups was 1.16 lower | ‐ | 163 | ⊕⊝⊝⊝ | |
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Assisted vaginal birth | Study population | RR 0.49 | 163 | ⊕⊝⊝⊝ | ||
| 123 per 1000 | 60 per 1000 | |||||
| Caesarean section | Study population | RR 0.76 | 163 | ⊕⊝⊝⊝ | ||
| 160 per 1000 | 122 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded by two levels for very serious risk of bias: high risk of bias in one domain (blinding for a subjective outcome) and unclear risk of bias in four domains. 2 Downgraded one level for serious imprecision due to a single study providing data with a small sample size (163) 3 Downgraded two levels for very serious imprecision due to a single study, with few events, small sample size and wide confidence intervals providing data | ||||||
| Acupuncture compared to water injection for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with water injection | Risk with acupuncture | |||||
| Pain intensity ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.84 | 128 | ⊕⊝⊝⊝ | ||
| 424 per 1000 | 356 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 1.60 | 128 | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 97 per 1000 | |||||
| Caesarean section | Study population | RR 1.33 | 128 | ⊕⊝⊝⊝ | ||
| 61 per 1000 | 81 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to very serious risk of bias: high or unclear risk of bias in both blinding performance and detection bias 2 Downgraded two levels due to very serious imprecision: small study (128) with few events and wide confidence intervals crossing the line of no effect | ||||||
| Acupressure compared to sham control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with sham control | Risk with acupressure | |||||
| Pain intensity as measured by a 10 cm visual analogue scale. Lower scores indicate less pain | The mean pain intensity in the control groups was 8.35 | The mean pain intensity score in the intervention group was 1.93 lower (3.31 lower to 0.55 lower) | 472 | ⊕⊝⊝⊝ | ||
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological analgesia | Study population | RR 0.54 | 75 | ⊕⊕⊝⊝ | ||
| 256 per 1000 | 138 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 3.00 | 100 | ⊕⊝⊝⊝ | ||
| 0 per 1000 | 0 per 1000 | |||||
| Caesarean section | Study population | RR 0.44 | 313 | ⊕⊕⊕⊝ | ||
| 308 per 1000 | 136 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level for serious risk of bias: majority of studies have unclear risk of bias in at least three domains. 2 Downgraded two levels for very serious inconsistency: considerable heterogeneity (I2 = 94%) 3 Downgraded two levels for very serious imprecision: very small sample size (75), small number of events and very wide confidence intervals 4 Downgraded one level for serious risk of bias: single study has high risk of performance bias and an unclear risk of allocation bias 5 Downgraded two levels for very serious imprecision: small sample size (100) and very wide confidence interval and small number of events 6 Downgraded one level for serious risk of bias: all studies have unclear risk of bias in at least three domains. Two studies have high or unclear risk of bias relating to performance bias | ||||||
| Acupressure compared to usual care for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with usual care | Risk with acupressure | |||||
| Pain intensity as measured by numeric rating scale (NRS) and visual analogue scale (VAS). Lower scores indicate less pain. | The mean pain intensity was 8.44 | The mean pain intensity score in the intervention group was 1.07 standard deviations lower (1.45 lower to 0.69 lower). | 620 | ⊕⊝⊝⊝ | The use of acupressure would result in a pain score approximately 2 cm lower on a 10 cm VAS or 2 points on a numeric rating scale compared to usual care. | |
| Satisfaction with pain relief | The mean satisfaction score with pain relief in the control group was 1.6 | The mean satisfaction with pain relief score was 1.05 higher (0.75 higher to 1.35 higher) | 105 | ⊕⊝⊝⊝ | ||
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth experience ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Use of pharmacological pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Assisted vaginal birth ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Caesarean section | Study population | RR 0.82 | 391 | ⊕⊕⊝⊝ | ||
| 241 per 1000 | 198 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: majority of included studies have high or unclear risk of bias relating to performance and detection bias 2 Downgraded two levels due to very serious inconsistency: considerable heterogeneity (I2 = 75%) 3 Downgraded two levels due to very serious risk of bias: single study at high risk of bias for selection, performance and detection bias. Very likely to have influenced the outcome 4 Downgraded one level due to serious imprecision: small sample size (105) 5 Downgraded one level due to serious risk of bias: two of the four studies included were at high risk of performance and detection bias, two studies were at high or unclear risk of selection bias and three at high or unclear risk of incomplete outcome data 6 Downgraded one level due to serious imprecision: wide confidence intervals incorporating both benefit and harm | ||||||
| Acupressure compared to combined control for pain management in labour | ||||||
| Patient or population: pain management in labour | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with combined control | Risk with acupressure | |||||
| Pain intensity One study used VAS pain score on scale 1 ‐ 100 mm One study used VAS pain score on scale 1 ‐ 10 mm ‐ the mean | The mean pain intensity score in the intervention group was 0.42 standard deviations lower (0.65 lower to 0.18 lower) | 322 | ⊕⊕⊕⊝ | |||
| Satisfaction with pain relief ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Sense of control in labour ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Satisfaction with childbirth | The mean satisfaction score with childbirth in the control group was 80.2 | The mean satisfaction score in the intervention group was 4.8 higher | ‐ | 212 | ⊕⊝⊝⊝ | |
| Use of pharmacological analgesia | Study population | RR 0.94 | 212 | ⊕⊝⊝⊝ | ||
| 525 per 1000 | 493 per 1000 | |||||
| Assisted vaginal birth | Study population | RR 0.81 | 212 | ⊕⊝⊝⊝ | ||
| 156 per 1000 | 126 per 1000 | |||||
| Caesarean section | Study population | RR 0.48 | 212 | ⊕⊝⊝⊝ | ||
| 206 per 1000 | 99 per 1000 | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded one level due to serious risk of bias: both studies have unclear risk of bias for performance bias, possible effect on this outcome 2 Downgraded one level due to serious risk of bias: single study has unclear risk of performance bias, likely to effect this outcome 3 Downgraded two levels due to very serious imprecision: wide confidence interval greater than 0.25 on either side of the line of no effect and small sample size 4 Downgraded two levels for very serious imprecision: wide confidence interval encompassing both benefit and harm and small sample size | ||||||
| Study ID | Total NICMAN Score | P | I | C | O | Study design | Differential diagnosis | Point selection | Needling parameters | Acupuncture point location | Treatment dosage | Therapist qualifications |
| Borup 2009 | 19 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 1 | 1 | 2 | 2 |
| Dong 2015 | 15 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 1 | 2 | 0 |
| Hantoushzadeh 2007 | 20 | 2 | 2 | 2 | 2 | 3 | 1 | 2 | 2 | 2 | 2 | 0 |
| Huang 2008 | 16 | 2 | 2 | 2 | 2 | 3 | 2 | 2 | 0 | 0 | 1 | 0 |
| Ma 2011 | 17 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 2 | 0 |
| MacKenzie 2011 | 19 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 1 | 2 | 1 | 2 |
| Martensson 2008 | 16 | 2 | 2 | 2 | 2 | 3 | 0 | 1 | 1 | 0 | 2 | 1 |
| Nesheim 2003 | 16 | 2 | 2 | 2 | 2 | 3 | 2 | 0 | 2 | 0 | 1 | 0 |
| Qu 2007 | 13 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 0 | 1 | 0 |
| Ramnero 2002 | 17 | 2 | 2 | 2 | 2 | 3 | 1 | 1 | 1 | 2 | 1 | 0 |
| Skilnand 2002 | 18 | 2 | 2 | 2 | 2 | 3 | 0 | 2 | 2 | 2 | 1 | 0 |
| Tjung 2008 | 17 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 1 | 2 | 1 | 2 |
| Vixner 2014 | 18 | 2 | 2 | 2 | 2 | 3 | 1 | 2 | 1 | 2 | 1 | 0 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 2 | 325 | Mean Difference (IV, Random, 95% CI) | ‐4.42 [‐12.94, 4.09] |
| 1.1 Manual acupuncture | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐3.58, 2.98] |
| 1.2 Electro‐acupuncture | 1 | 175 | Mean Difference (IV, Random, 95% CI) | ‐9.0 [‐14.08, ‐3.92] |
| 2 Satisfaction with pain relief in labour Show forest plot | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.38 [1.78, 3.19] |
| 2.1 Manual acupuncture | 1 | 150 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.38 [1.78, 3.19] |
| 3 Use of pharmacological analgesia Show forest plot | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.63, 0.89] |
| 3.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.63, 0.89] |
| 4 Assisted vaginal birth Show forest plot | 2 | 261 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.41, 2.97] |
| 4.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.41, 2.97] |
| 5 Caesarean section Show forest plot | 3 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.49, 2.48] |
| 5.1 Manual acupuncture | 3 | 411 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.49, 2.48] |
| 6 Apgar score < 7 at 5 minutes Show forest plot | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.79] |
| 6.1 Manual acupuncture | 2 | 261 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.79] |
| 7 Length of labour ‐ total Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Electro‐acupuncture | 1 | 175 | Mean Difference (IV, Fixed, 95% CI) | ‐37.41 [‐96.37, 21.55] |
| 8 Spontaneous vaginal birth Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Manual acupuncture | 3 | 411 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.86, 1.12] |
| 9 Augmentation with oxytocin Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9.1 Manual acupuncture | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 4 | 495 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.31 [‐2.14, ‐0.49] |
| 1.1 Manual acupuncture | 2 | 270 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐2.36, 0.58] |
| 1.2 Electro‐acupuncture | 2 | 225 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.79 [‐3.37, ‐0.21] |
| 2 Satisfaction with pain relief in labour Show forest plot | 2 | 343 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.96, 1.20] |
| 2.1 Manual acupuncture | 2 | 215 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.95, 1.23] |
| 2.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.87, 1.30] |
| 3 Use of pharmacological analgesia Show forest plot | 6 | 1059 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.60, 0.85] |
| 3.1 Manual acupuncture | 5 | 884 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.60, 0.82] |
| 3.2 Electro‐acupuncture | 2 | 175 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.01, 8.16] |
| 4 Assisted vaginal birth Show forest plot | 6 | 1217 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.70, 1.24] |
| 4.1 Manual acupuncture | 6 | 1089 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.64, 1.17] |
| 4.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.64, 4.04] |
| 5 Caesarean section Show forest plot | 5 | 861 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.47, 1.09] |
| 5.1 Manual acupuncture | 4 | 683 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.50, 1.24] |
| 5.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.16, 1.28] |
| 6 Apgar score < 7 at 5 minutes Show forest plot | 6 | 1061 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.28, 3.47] |
| 6.1 Manual acupuncture | 5 | 883 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.18, 3.10] |
| 6.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [0.12, 48.61] |
| 7 Length of labour ‐ total Show forest plot | 3 | 608 | Mean Difference (IV, Fixed, 95% CI) | ‐13.89 [‐28.93, 1.14] |
| 7.1 Manual acupuncture | 1 | 124 | Mean Difference (IV, Fixed, 95% CI) | 4.0 [‐142.47, 150.47] |
| 7.2 Electro‐acupuncture | 3 | 484 | Mean Difference (IV, Fixed, 95% CI) | ‐14.08 [‐29.20, 1.03] |
| 8 Spontaneous vaginal birth Show forest plot | 4 | 449 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.89, 1.08] |
| 8.1 Manual acupuncture | 3 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.85, 1.10] |
| 8.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.86, 1.14] |
| 9 Augmentation with oxytocin Show forest plot | 4 | 813 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.77, 1.02] |
| 9.1 Manual acupuncture | 3 | 635 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.78, 1.09] |
| 9.2 Electro‐acupuncture | 2 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.59, 1.03] |
| 10 Perineal trauma Show forest plot | 1 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.19, 1.26] |
| 10.1 Manual acupuncture | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.13, 1.92] |
| 10.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.12, 1.79] |
| 11 Maternal blood loss > 500 mL Show forest plot | 1 | 253 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.11, 0.78] |
| 11.1 Manual acupuncture | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.11, 1.43] |
| 11.2 Electro‐acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.04, 0.93] |
| 12 Relaxation Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 Manual acupuncture | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.90 [‐1.62, ‐0.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 1 | 163 | Mean Difference (IV, Fixed, 95% CI) | ‐1.16 [‐1.51, ‐0.81] |
| 1.1 Electro‐acupuncture | 1 | 163 | Mean Difference (IV, Fixed, 95% CI) | ‐1.16 [‐1.51, ‐0.81] |
| 2 Assisted vaginal birth Show forest plot | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.18, 1.38] |
| 2.1 Electro‐acupuncture | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.18, 1.38] |
| 3 Caesarean section Show forest plot | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.35, 1.63] |
| 3.1 Electro‐acupuncture | 1 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.35, 1.63] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Use of pharmacological analgesia Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.30] |
| 2 Assisted vaginal birth Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.47, 5.39] |
| 3 Caesarean section Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.37, 4.73] |
| 4 Augmentation with oxytocin Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Manual acupuncture | 1 | 128 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.85, 1.58] |
| 5 Relaxation Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Manual acupuncture | 1 | 128 | Mean Difference (IV, Fixed, 95% CI) | 12.60 [4.75, 20.45] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 6 | 472 | Mean Difference (IV, Random, 95% CI) | ‐1.93 [‐3.31, ‐0.55] |
| 2 Use of pharmacological analgesia Show forest plot | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.20, 1.43] |
| 3 Assisted vaginal birth Show forest plot | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 71.92] |
| 4 Caesarean section Show forest plot | 4 | 313 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.27, 0.71] |
| 5 Apgar score < 7 at 5 minutes Show forest plot | 2 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.99] |
| 6 Length of labour Show forest plot | 4 | 399 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.26, ‐0.57] |
| 6.1 Length of labour | 4 | 399 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.26, ‐0.57] |
| 7 Spontaneous vaginal birth Show forest plot | 2 | 115 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.92, 1.18] |
| 8 Augmentation with oxytocin Show forest plot | 2 | 135 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.46, 0.91] |
| 9 Anxiety Show forest plot | 1 | 75 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐2.51, ‐0.29] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 8 | 620 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐1.45, ‐0.69] |
| 2 Satisfaction with pain relief Show forest plot | 1 | 105 | Mean Difference (IV, Fixed, 95% CI) | 1.05 [0.75, 1.35] |
| 3 Caesarean section Show forest plot | 4 | 391 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.54, 1.23] |
| 4 Length of labour Show forest plot | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐16.23 [‐79.64, 47.18] |
| 5 Spontaneous vaginal birth Show forest plot | 3 | 220 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.90, 1.21] |
| 6 Augmentation with oxytocin Show forest plot | 1 | 15 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.39, 10.31] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pain intensity Show forest plot | 2 | 322 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.42 [‐0.65, ‐0.18] |
| 2 Satisfaction with childbirth Show forest plot | 1 | 212 | Mean Difference (IV, Fixed, 95% CI) | 4.80 [‐2.25, 11.85] |
| 3 Use of pharmacological analgesia Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.71, 1.25] |
| 4 Assisted vaginal birth Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.39, 1.67] |
| 5 Caesarean section Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.22, 1.04] |
| 6 Augmentation with oxytocin Show forest plot | 1 | 212 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.77, 1.31] |


