Zahvati i pokreti za smanjenje bolova u vratu u usporedbi pristupa bez liječenja i drugim oblicima liječenja
Abstract
Background
Manipulation and mobilisation are commonly used to treat neck pain. This is an update of a Cochrane review first published in 2003, and previously updated in 2010.
Objectives
To assess the effects of manipulation or mobilisation alone compared wiith those of an inactive control or another active treatment on pain, function, disability, patient satisfaction, quality of life and global perceived effect in adults experiencing neck pain with or without radicular symptoms and cervicogenic headache (CGH) at immediate‐ to long‐term follow‐up. When appropriate, to assess the influence of treatment characteristics (i.e. technique, dosage), methodological quality, symptom duration and subtypes of neck disorder on treatment outcomes.
Search methods
Review authors searched the following computerised databases to November 2014 to identify additional studies: the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE and the Cumulative Index to Nursing and Allied Health Literature (CINAHL). We also searched ClinicalTrials.gov, checked references, searched citations and contacted study authors to find relevant studies. We updated this search in June 2015, but these results have not yet been incorporated.
Selection criteria
Randomised controlled trials (RCTs) undertaken to assess whether manipulation or mobilisation improves clinical outcomes for adults with acute/subacute/chronic neck pain.
Data collection and analysis
Two review authors independently selected studies, abstracted data, assessed risk of bias and applied Grades of Recommendation, Assessment, Development and Evaluation (GRADE) methods (very low, low, moderate, high quality). We calculated pooled risk ratios (RRs) and standardised mean differences (SMDs).
Main results
We included 51 trials (2920 participants, 18 trials of manipulation/mobilisation versus control; 34 trials of manipulation/mobilisation versus another treatment, 1 trial had two comparisons).
Cervical manipulation versus inactive control:For subacute and chronic neck pain, a single manipulation (three trials, no meta‐analysis, 154 participants, ranged from very low to low quality) relieved pain at immediate‐ but not short‐term follow‐up.
Cervical manipulation versus another active treatment:For acute and chronic neck pain, multiple sessions of cervical manipulation (two trials, 446 participants, ranged from moderate to high quality) produced similar changes in pain, function, quality of life (QoL), global perceived effect (GPE) and patient satisfaction when compared with multiple sessions of cervical mobilisation at immediate‐, short‐ and intermediate‐term follow‐up. For acute and subacute neck pain, multiple sessions of cervical manipulation were more effective than certain medications in improving pain and function at immediate‐ (one trial, 182 participants, moderate quality) and long‐term follow‐up (one trial, 181 participants, moderate quality). These findings are consistent for function at intermediate‐term follow‐up (one trial, 182 participants, moderate quality). For chronic CGH, multiple sessions of cervical manipulation (two trials, 125 participants, low quality) may be more effective than massage in improving pain and function at short/intermediate‐term follow‐up. Multiple sessions of cervical manipulation (one trial, 65 participants, very low quality) may be favoured over transcutaneous electrical nerve stimulation (TENS) for pain reduction at short‐term follow‐up. For acute neck pain, multiple sessions of cervical manipulation (one trial, 20 participants, very low quality) may be more effective than thoracic manipulation in improving pain and function at short/intermediate‐term follow‐up.
Thoracic manipulation versus inactive control: Three trials (150 participants) using a single session were assessed at immediate‐, short‐ and intermediate‐term follow‐up. At short‐term follow‐up, manipulation improved pain in participants with acute and subacute neck pain (five trials, 346 participants, moderate quality, pooled SMD ‐1.26, 95% confidence interval (CI) ‐1.86 to ‐0.66) and improved function (four trials, 258 participants, moderate quality, pooled SMD ‐1.40, 95% CI ‐2.24 to ‐0.55) in participants with acute and chronic neck pain. A funnel plot of these data suggests publication bias. These findings were consistent at intermediate follow‐up for pain/function/quality of life (one trial, 111 participants, low quality).
Thoracic manipulation versus another active treatment: No studies provided sufficient data for statistical analyses. A single session of thoracic manipulation (one trial, 100 participants, moderate quality) was comparable with thoracic mobilisation for pain relief at immediate‐term follow‐up for chronic neck pain.
Mobilisation versus inactive control: Mobilisation as a stand‐alone intervention (two trials, 57 participants, ranged from very low to low quality) may not reduce pain more than an inactive control.
Mobilisation versus another active treatment:For acute and subacute neck pain, anterior‐posterior mobilisation (one trial, 95 participants, very low quality) may favour pain reduction over rotatory or transverse mobilisations at immediate‐term follow‐up. For chronic CGH with temporomandibular joint (TMJ) dysfunction, multiple sessions of TMJ manual therapy (one trial, 38 participants, very low quality) may be more effective than cervical mobilisation in improving pain/function at immediate‐ and intermediate‐term follow‐up. For subacute and chronic neck pain, cervical mobilisation alone (four trials, 165 participants, ranged from low to very low quality) may not be different from ultrasound, TENS, acupuncture and massage in improving pain, function, QoL and participant satisfaction at immediate‐ and intermediate‐term follow‐up. Additionally, combining laser with manipulation may be superior to using manipulation or laser alone (one trial, 56 participants, very low quality).
Authors' conclusions
Although support can be found for use of thoracic manipulation versus control for neck pain, function and QoL, results for cervical manipulation and mobilisation versus control are few and diverse. Publication bias cannot be ruled out. Research designed to protect against various biases is needed.
Findings suggest that manipulation and mobilisation present similar results for every outcome at immediate/short/intermediate‐term follow‐up. Multiple cervical manipulation sessions may provide better pain relief and functional improvement than certain medications at immediate/intermediate/long‐term follow‐up. Since the risk of rare but serious adverse events for manipulation exists, further high‐quality research focusing on mobilisation and comparing mobilisation or manipulation versus other treatment options is needed to guide clinicians in their optimal treatment choices.
PICOs
Laički sažetak
Postupci kiropraktičara ‐ manipulacija i mobilizacija ‐ za liječenje boli u vratu
Istraživačko pitanje
U ovom obnovljenom Cochrane sustavnom pregledu je ispitan učinak manipulacije ili mobilizacije (postupci koje provode kiropraktičari za "namještanje" i "pokretanje" kralježnice) u odnosu na kontrolnu skupinu ili drugi oblik liječenja za bol u vratu, funkciju, poteškoće, zadovoljstvo bolesnika, kvalitetu života i dojam učinka u odraslih s bolnim vratom nezavisno od simptoma u rukama i glavobolje u kratkom i dugom razdoblju praćenja.
Dosadašnje spoznaje
Bolovi u vratu čest su simptom poremećaja mišićnog i koštanog sustava i može uzrokovati različite razine onesposobljenosti. Bolovi se mogu širiti iz vrata u ruke (radikulopatija) ili uzrokovati glavobolju (cervikogena glavobolja). Kiropraktičke metode koje se zovu manipulacija ("podešavanje" kralježnice) i mobilizacija (prisilno pokretanje zglobova i mišića) koristi se zasebno ili zajedno s drugih oblicima fizikalne terapije u osoba koje pate od boli u vratu.
Obilježja studija
Ovaj obnovljeni Cochrane sustavni pregled uključio je 51 kliničku studiju: 18 ispitivanja manipulacije ili mobilizacije u odnosu na placebo tj. nikakvo liječenje; 34 ispitivanja manipulacije ili mobilizacije u odnosu na drugi oblik liječenja (elektroterapija, vježbanje, lijekovi) i različiti drugi postupci ili doze. (Napomena: jedno istraživanje je uključilo dvije usporedne skupine.)
Ključni rezultati
U drugim preglednim člancima koji su se usmjerili na štetne učinke pronađeni su dokazi da je liječenje mobilizacijom sigurno, a da primjena manipulacije može uzrokovati rijetke, ali ozbiljne štetne učinke, primjerice moždani udar, disk hernija ili teški ispadi živčane funkcije. Studije uključene u ovaj sustavni pregled su opisale prolazne i blage štetne učinke, a polovina uključenih studija uopće nije prikazala podatke za štetne učinke.
• Manipulacija ili mobilizacija u usporedbi s neaktivnim liječenjem: Kod subakutnih i kroničnih bolova u vratu, jednokratnom manipulacijom je postignuto privremeno ublažavanje. Međutim, u kratkim studijama koje su primijenile višestruke takve zahvate uočeni su kontradiktorni rezultati. Kratkotrajno i srednje dugo praćenje višekratnih manipulacija kralježnice prsnog koša je pokazalo da je to pristup izbora bolesnika za smanjenje boli, te za poboljšanje funkcije u bolesnika s akutnim i kroničnim bolovima u vratu. Mobilizacija u području kralježnice prsnog koša nije dodatno smanjila bol.
• Manipulacija ili mobilizacija u usporedbi s drugim aktivnim liječenjem: Manipulacija u području vrata dovela je do promjena boli, funkcije, kvalitete života, dojmu učinka i zadovoljstva bolesnika koji su bili usporedivi s onima koji su postignuti mobilizacijom vratne kralježnice tijekom srednje dugog praćenja u bolesnika s bolnim vratom nezavisno od trajanja bolesti. Manipulacija vratne kralježnice kod akutnih i subakutnih bolova imala je bolji učinak u usporedbi s kombinacijama analgetika, miorelaksansa i nesteroidnih protuupalnih lijekova za ublažavanje bolova i poboljšanje funkcije do dugoročnog praćenja. Kod kroničnih cervikogenih glavobolja, manipulacije u području vrata su imale bolji učinak u usporedbi s laganom masažom u smanjenju boli i poboljšanju funkcije u kratkom i srednje dugom praćenju. Za ovu indikaciju je nađeno da su manipulacije u području vrata bolje u odnosu na transkutanu stimulaciju živaca (TENS) u ublažavanju boli u kratkotrajnom praćenju. Za akutnu bol vrata je manipulacija u području vrata učinkovitija nego manipulacija u području kralježnice prsnog koša u ublažavanju boli i poboljšanju funkcije do srednje dugog praćenja. Mobilizacija u području vratne kralježnice za subakutnu i kroničnu bol vrata su po učinku podudarni pulsnom ultrazvuku, TENS‐u, akupunkturi i masaži za ublažavanje boli, poboljšanju funkcije, kvalitete života i zadovoljstva bolesnika do srednje dugog praćenja. Međutim, kombinirana primjena lasera i manipulacije mogla bi biti bolja u odnosu na samu manipulaciju.
Kvaliteta dokaza
U ovom sustavnom pregledu literature nisu nađeni dokazi visoke kvalitete, te stoga ostaje upitno jesu li mobilizacija i manipulacija djelotvorni postupci za liječenje boli vrata. Očekuje se da će daljnja istraživanja dati odgovor na ovo pitanje. Autori ovog sustavnog pregleda uočili su brojne probleme prilikom izrade ovog istraživanja. Primjerice, broj ispitanika u pojedinom istraživanju bio je malen, 80% studija (41/51) je bilo niske i vrlo niske kvalitete te su dokazi za optimalne doze nedostatni.
Authors' conclusions
Summary of findings
| Manipulation (cervical) compared with oral medicine for acute/subacute neck pain | ||||
| Patient or population: patients with acute and subacute neck pain Settings: outpatient clinics, ambulatory care services Intervention: manipulation of cervical region ‐ multiple sessions Comparison: oral medicine ‐ varied combinations of non‐steroidal anti‐inflammatory drugs (NSAIDs), analgesics, opioid analgesics and muscle relaxants | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD ‐0.21 (‐0.5 to 0.08) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD ‐0.32 (‐0.61 to ‐0.02) | 181 | ⊕⊕⊕⊝ Moderatea | Pain reduction favouring manipulation over medication |
| FUNCTION | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD ‐0.30 (‐0.59 to ‐0.00) | 182 | ⊕⊕⊕⊝ Moderatea | Functional improvement favouring manipulation over medication |
| Acute and subacute neck pain Long‐term follow‐up | SMD ‐0.11 (‐0.40 to 0.18)
| 181 | ⊕⊕⊕⊝ Moderatea | No significant difference between groups |
| PARTICIPANT SATISFACTION | ||||
| Acute and subacute neck pain Long‐term follow‐up | Not estimable | 182 | ⊕⊕⊕⊝ Moderatea | Manipulation favoured over medication |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD 0.22 (‐0.07 to 0.51) | 181 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: 0.19 (‐0.10 to 0.49) | 181 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Moderate‐quality evidence suggests that multiple sessions of cervical manipulation are more effective than medication (analgesics and non‐steroidal anti‐inflammatory drugs (NSAIDs)) for improving pain at immediate‐term and long‐term follow‐up (1 trial; 181 participants); function at intermediate term and satisfaction over the long term. Quality of life was similar between groups (1 trial, 182 participants) at intermediate‐ and long‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. | ||||
| aIndirectness: ‐1; a second independent trial is needed to clarify emerging data. | ||||
| Manipulation (thoracic) compared with inactive control for neck pain | ||||
| Patient or population: patients with acute, subacute and chronic neck pain Settings: outpatient clinics, ambulatory care services Intervention: manipulation of thoracic region ‐ multiple sessions Comparison: inactive control | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD pooled ‐1.46 (‐2.20 to ‐0.71) | 242 Fernandez 2004 JWRD; Fernandez 2009; Gonzalez‐Iglesias 2009 JO; | ⊕⊕⊕⊝ Moderatea | Favoured treatment; NNTB: 4 to 7; magnitude of effect: medium |
| Chronic neck pain Intermediate‐term follow‐up | SMD ‐0.64 (‐1.04 to ‐0.25) | 111 | ⊕⊕⊝⊝ Lowb,c | Favoured treatment; NNTB 4; magnitude of effect: small |
| FUNCTION | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD pooled ‐1.73 (‐2.68 to ‐0.78) | 258 | ⊕⊕⊕⊝ Moderatea | Favoured treatment; NNTB 4 to 5; magnitude of effect: medium |
| Chronic neck pain Short‐term follow‐up | SMD ‐0.50 (‐0.89 to ‐0.10) | 111 | ⊕⊕⊝⊝ Lowb,c | Favoured treatment; NNTB 5; magnitude of effect: small |
| Chronic neck pain Intermediate‐term follow‐up | SMD ‐0.38 (‐0.77 to 0.01) | 111 (1 trial; Cheung Lau 2011) | ⊕⊕⊝⊝ Lowb,c | Favoured treatment; NNTB 5; magnitude of effect: small |
| QUALITY OF LIFE (QoL) | ||||
| Chronic neck pain Short‐term follow‐up | SMD ‐0.82 (‐1.23 to ‐0.42) | 111 | ⊕⊕⊝⊝ Lowb,c | Favoured treatment |
| Chronic neck pain Intermediate‐term follow‐up | SMD ‐0.61 (‐1.01 to ‐0.22) | 111 | ⊕⊕⊝⊝ Lowc | Favoured treatment |
| Seven trials (428 participants) using multiple sessions of thoracic manipulation for acute to chronic neck pain were assessed at 3 time intervals. At short‐term follow‐up, moderate‐quality evidence favoured thoracic manipulation for pain reduction among participants with acute/subacute neck pain, and with acute to chronic neck pain, it improved function. These findings were consistent but small at intermediate follow‐up for pain, function and quality of life (low‐quality evidence). | ||||
| GRADE Working Group grades of evidence. | ||||
| bIndirectness: ‐1, immediate post‐treatment data have limited clinical relevance; single trials with only immediate‐ and short‐term follow‐up are downgraded (ceiling effect) because future research is likely to have an important impact on the direction of the reported effect, and a second independent trial is needed to clarify emerging short‐term data. cImprecision: ‐1, small sample size. aInconsistency: P value = 0.002; I² = 84%; sensitivity analysis: Statistical differences led us to explore heterogeneity by the following PICO factors: P: about the same; I: about the same; C: about the same; O: for pain, VAS, NPRS; for disability, NPQ, NDI; RoB: most often low RoB but when the trial of high RoB is removed, pooled SMD increases to ‐2.18 (‐2.71 to ‐1.65) for pain, but these data were derived from trials conducted in the same lab. | ||||
| Manipulation compared with mobilisation for neck pain | ||||
| Patient or population: patients with acute, subacute and chronic neck pain Settings: ambulatory care or outpatient clinic Intervention: manipulation of cervical region ‐ multiple sessions Comparison: mobilisation | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute, subacute and chronic neck pain Intermediate‐term follow‐up | MD pooled ‐0.07 (‐0.72 to 0.59) | 446 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| FUNCTION AND DISABILITY | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD: ‐0.06 (‐0.35 to 0.24) | 176 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| Acute, subacute and chronic neck pain Intermediate‐term follow‐up | SMD pooled: 0.10 (‐0.18 to 0.37)
| 446 | ⊕⊕⊕⊕ High | No significant differences between groups |
| PARTICIPANT SATISFACTION | ||||
| Subacute and chronic neck pain Short‐term follow‐up | SMD: ‐0.02 (‐0.21 to 0.24) | 269 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| GLOBAL PERCEIVED EFFECT | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.06 | 177 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD: 0.08 (‐0.21 to 0.38) | 176 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.06 (‐0.35 to 0.24) | 177 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| Moderate‐ to high‐quality evidence (2 trials, 446 participants) suggests that multiple sessions of cervical manipulation produced similar changes in pain, function, quality of life, global perceived effect and patient satisfaction when compared with multiple sessions of cervical mobilisation at immediate‐, short‐ and intermediate‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. | ||||
| aInconsistency: ‐1. bIndirectness: ‐1. | ||||
| Manipulation compared with exercise for neck pain | ||||
| Patient or population: patients with acute and subacute neck pain Settings: ambulatory care or outpatient clinic setting Intervention: manipulation of cervical region Comparison: exercise | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.16 (‐0.45 to 0.13) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: 0.06 (‐0.23 to 0.35) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| FUNCTION | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.01 (‐0.30 to 0.28)
| 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: ‐0.02 (‐0.31 to 0.27)
| 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| PARTICIPANT SATISFACTION | ||||
| Acute and subacute neck pain Long‐term follow‐up | Not estimable | 182 | ⊕⊕⊕⊝ Moderatea | Improvement in participant satisfaction for manipulation over exercise |
| GLOBAL PERCEIVED EFFECT | ||||
| Acute and subacute neck pain Immediate post‐treatment follow‐up | Not estimable | 182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.05 (‐0.35 to 0.24) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: 0.0 (‐0.29 to 0.29) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Moderate‐quality evidence suggests no differences in pain, function, global perceived effect and quality of life when multiple sessions of cervical manipulation are compared with exercise at immediate‐, intermediate‐ and long‐term follow‐up. Moderate‐quality evidence indicates that use of cervical manipulation led to greater participant satisfaction when compared with an exercise programme at long‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. | ||||
| aIndirectness: ‐1. | ||||
| High dose of manipulation compared with low dose of manipulation for chronic neck pain | ||||
| Patient or population: patients with chronic neck pain with cervicogenic headache (CGH) Settings: ambulatory care or outpatient clinic setting Intervention: manipulation of cervical region Comparison: high dose vs low dose | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Chronic neck pain and CGH Intermediate‐term follow‐up | SMD pooled: ‐0.40 (‐0.96 to 0.16)
| ⊕⊕⊕⊝ Moderatea | Two trials showed no significant differences between groups | |
| FUNCTION | ||||
| Chronic neck pain and CGH Intermediate‐term follow‐up | SMD pooled: ‐0.61 (‐1.38 to 0.17) | ⊕⊕⊕⊝ Moderatea | Two trials showed no significant differences between groups | |
| Moderate‐quality evidence shows that high‐dose (12 to 18 sessions) contrasted against low‐dose (3 to 8 sessions) cervical manipulation produced similar changes in pain and function at intermediate‐term follow‐up for individuals with chronic neck pain with cervicogenic headache. | ||||
| GRADE Working Group grades of evidence. | ||||
| aImprecision: ‐1. | ||||
Background
Description of the condition
Neck disorders are common, disabling to various degrees and costly (Hogg‐Johnson 2008). Most people can expect to have some degree of neck pain within their lifetime. Neck pain with or without symptoms that radiate to the arms or head may involve a variety of pathologies in one or several neurovascular, soft tissue and musculoskeletal structures such as nerves, ganglia, nerve roots, uncovertebral joints, intervertebral joints, discs, bones, periosteum, muscle and ligaments. We included in this review neck pain with cervicogenic headache ‐ a pain that emanates from the neck and suboccipital region and radiates to the forehead, orbital region, temples, vertex or ears and is aggravated by specific neck movements or sustained neck postures.
When examining new episodes of neck pain, we looked at the general population, the workforce and motor vehicle accident (MVA) victims. Every year, an episode of neck pain occurs in 15% to 20% of the general population, in 15% to 60% of the workforce and in 10% to 14% of those involved in traffic collisions (Guzman 2008). Prevalence of neck pain varies from 12% to 72% in the general population and from 27% to 48% among workers (Haldeman 2008). The annual prevalence of activity limitations related to neck pain has been reported as 11% in the UK and 14% in Canada (Côté, 2008). Societal and personal burden from persisting symptoms of postwhiplash injury has been described in up to 50% of those attending an emergency department (Kongsted 2007). Long‐term consequences for individuals and their spouses as detailed by Jennum 2013 include reduced quality of life, mood, ability to cope, social participation, employment rates and job income.
Direct costs attributable to visits to healthcare providers, sick leave and related loss of productive capacity (Borghouts 1998; Côté 2008; Linton 1998; Skargren 1998) are substantive. Mean inflation‐adjusted annual expenditures on medical care for people with back and neck conditions increased from $487 to $950 USD from 1999 to 2008 (Davis 2012). Work‐related claims for neck injury submitted to a Canadian Workers Compensation Board accounted for 5% of all lost time at work (Côté 2008). Indirect costs related to disease‐related work disability or premature mortality were significantly higher in people with neck injury and their spouses when compared with matched controls in a Danish study (Jennum 2013).
Description of the intervention
Manipulation and mobilisation are commonly used treatments for neck pain and may be performed by physical therapists, chiropractors, traditional bone setters, osteopaths, medical doctors and massage therapists. Manipulation consists of a localised force of high velocity and low amplitude directed at specific spinal segments (Basmajian 1993; Grieve 1988). Mobilisations use low‐grade/velocity, small‐ or large‐amplitude passive movement techniques or neuromuscular techniques within the patient's range of motion and within the patient's control (Basmajian 1993; Butler 2000; Grieve 1988). Neuromuscular mobilisation techniques employ the muscular efforts of individuals against a specific force applied by the clinician to more effectively mobilise a joint(s) and related tissues.
Description of the comparison
The methods most commonly compared in trials are inactive controls [placebo (e.g. sham/mock mobilisation or other sham treatment such as sham transcutaneous electrical nerve stimulation (TENS); adjunct treatment (e.g. mobilisation plus a treatment such as ultrasound versus same treatment); and wait list/no treatment)] and other active treatments [one intervention versus another intervention (e.g. manipulation versus exercise); one treatment technique versus another (e.g. rotatory break versus lateral break manipulation); and one dose of treatment versus another dose (e.g. three weeks at nine sessions of manipulation versus four weeks at 12 sessions)].
How the intervention might work
Spinal manipulation or mobilisation appear to have three main proposed underpinning physiological mechanisms. The underlying mechanisms are complex, multifactorial and poorly understood; unravelling these mechanisms continues to have important implications for rehabilitation. First, neurophysiological effects, including analgesic, motor and sympathetic nervous system effects, have been demonstrated (Bialosky 2009; Karason 2003; Perry 2008; Vincenzino 1996); second, mechanical effects, including transient/short‐term to permanent change in length of connective tissue and biomechanical dysfunction, have been revealed (Bialosky 2009; Calloca 2006; Fritz 2011; Martinez‐Segura 2006; Souvlis 2004); and finally, expectations or psychological factors associated with 'manual touch' may produce a placebo effect. The mechanical force of spinal manipulation triggers a chain of neurophysiological reactions that are thought to be the reason for the outcomes seen with spinal manipulation (Bialosky 2009). Proposed neurophysiological effects include pain reduction through inhibition of nociceptors, dorsal horn and descending pathways of the spinal cord (Bialosky 2009; Haavik 2012; Pickar 2002). A manipulation force can stimulate peripheral afferents, altering central mediated/supraspinal input and enhancing motoneuron excitability (Bialosky 2009; Schmid 2008). Increased muscle recruitment after manipulation has impacted spinal stiffness and muscle activity (Fritz 2011). It is difficult to assess to what degree 'hands‐on effects', attention, assessment techniques, other forms of feedback and interaction and communication between the manual therapist and the patient are 'unique' traits of those who provide manual therapy. We acknowledge that these effects may play some role in manual treatment methods.
Why it is important to do this review
Since our 2010 publication (Gross 2010), numerous systematic reviews on similar topics have been published (Boyles 2011; Chaibi 2012; Cross 2011; Furlan 2012; Huisman 2013; Lin 2012; Millan 2012; Posadzki 2011; Racicki 2013; Rodine 2012; Shaw 2010; Thoomes 2013; Vincent 2013; Walser 2009). High‐quality conclusions pertaining to effectiveness or superiority of manipulation or mobilisation over other treatment modalities have NOT been reported. Most evidence pertaining to subacute or chronic neck pain is of moderate to very low quality (Cross 2011; Furlan 2012; Gross 2010), and almost no evidence is available on manipulation or mobilisation as a single stand‐alone therapy for both acute neck disorders (Shaw 2010) or radiculopathy (Boyles 2011; Rodine 2012; Thoomes 2013). An update of this Cochrane systematic review is justified to strengthen our confidence in the evidence.
Objectives
To assess effects of manipulation or mobilisation alone compared wiith those of an inactive control or another active treatment on pain, function, disability, patient satisfaction, quality of life and global perceived effect in adults experiencing neck pain with or without radicular symptoms and cervicogenic headache at immediate‐ to long‐term follow‐up. When appropriate, to assess the influence of treatment characteristics (i.e. technique, dosage), methodological quality, symptom duration and subtypes of neck disorder on treatment outcomes.
Methods
Criteria for considering studies for this review
Types of studies
We included published and unpublished randomised controlled trials (RCTs) or quasi‐RCTs (QRCTs)in full‐text or abstract form. A QRCT uses methods of allocation that are subject to bias in assignment, such as odd‐even numbers, days of the week or patient record or social security number. We applied no restrictions to the methodological quality of RCTs.
Types of participants
Participants were adults (≥ 18 years) with the following.
-
Neck pain without radicular findings, including neck pain without specific cause, whiplash‐associated disorder (WAD) category I and II (Guzman 2008; Spitzer 1987; Spitzer 1995), myofascial pain syndrome and neck pain associated with degenerative changes (Schumacher 1993).
-
Cervicogenic headache (Olesen 1988; Olesen 1997; Sjaastad 1990).
-
Neck disorders with radicular findings (Schumacher 1993), including degenerative joint or disc disease with spinal stenosis, spondylolisthesis or discogenic radiculopathy; WAD category III (Spitzer 1987; Spitzer 1995).
We defined symptom duration as acute (< 30 days), subacute (30 days to 90 days) or chronic (> 90 days).
We excluded studies if they investigated neck disorders with the following specific causes.
-
Definite or possible long tract signs (e.g. myelopathies).
-
Neck pain caused by other pathological entities (Schumacher 1993).
-
Headache not of cervical origin but associated with the neck.
-
Co‐existing headache when neck pain was not dominant, or when the headache was not provoked by neck movements or sustained neck postures.
-
'Mixed' headache, which includes more than one headache classification.
Types of interventions
We included studies using manipulation or mobilisation techniques. Although typically applied to the cervical region, they could be applied to other body regions; the guiding principle was to include a mobilisation or manipulation intervention provided with the intention to treat neck pain. Manipulation involves a localised force of high velocity and low amplitude directed at specific spinal segments. Mobilisations use low‐grade/velocity, small‐ or large‐amplitude passive movement techniques or neuromuscular techniques within the patient's range of motion and within the patient's control. In the included studies, investigators might use these techniques alone or in conjunction with other treatment agents, for example, mobilisation plus ultrasound versus ultrasound. All studies consisted of comparison with an inactive control or with another active treatment as follows.
Inactive control
-
Placebo, for example, sham/mock mobilisation or other sham treatment (e.g. sham TENS).
-
Adjunct treatment, for example, mobilisation plus a treatment (e.g. ultrasound) versus the same treatment (e.g. ultrasound).
-
Wait list or no treatment.
Active treatment for comparison
-
Manipulation or mobilisation versus another intervention (e.g. manipulation versus exercise).
-
One technique of manipulation or mobilisation versus another (e.g. rotatory break versus lateral break manipulation).
-
One dose of manipulation or mobilisation versus another dose (e.g. 3 weeks at 9 sessions manipulation versus 4 weeks at 12 sessions).
Types of outcome measures
Primary outcomes
Primary outcomes of interest included the following.
-
Pain relief.
-
Disability including, but not limited to, self report disability measures such as the Neck Disability Index (NDI), activities of daily living, return to work, sick leave and function.
Secondary outcomes
Secondary outcomes included the following.
-
Global perceived effect.
-
Patient satisfaction.
-
Quality of life.
We set no restrictions on the types of tools used to measure these outcomes, as no universally accepted tools are available, although we found that investigators in several studies did use validated tools. Function and disability could be measured using self report measures or observer‐based physical performance tests (Beattie 2001; Finch 2002). Measures of physical performance require testing the individual's ability to execute a simple activity in a standardised environment using a standardised test and scoring procedure; these measures are concerned with testing a co‐ordinated set of functions needed for purposeful activity (i.e. reaching, walking, driving). Although moderate correlation between self report scales and physical performance tests can be found in the low back literature, it remains unclear whether one is superior to the other (Lee 2001), and in the neck literature, this relationship remains unclear. We excluded tests used during a standard physical examination, such as inspection, range of motion, strength, palpation, provocation, muscular stability, neurological tests and cervical proprioception. We extracted data on adverse effects and costs of treatment. The duration of follow‐up was defined as follows.
-
Immediately post treatment (within one day).
-
Short‐term follow‐up (closest to four weeks; one day to four weeks).
-
Intermediate‐term follow‐up (closest to six months; longer than four weeks to six months).
-
Long‐term follow‐up (closest to 12 months; longer than six months to 12 months).
Search methods for identification of studies
A research librarian searched bibliographic databases, without language restrictions, for medical, chiropractic and allied health literature. All databases were originally searched from their inception. Subject headings (MeSH) and key words included anatomical terms, disorder or syndrome terms, treatment terms and methodological terms consistent with those advised by the Cochrane Back Review Group.
Electronic searches
We searched the following databases from their start to the dates provided:
-
Cochrane Central Register of Controlled Trials (CENTRAL) (Ovid, November 2014; includes the Back Review Group Trials Register).
-
MEDLINE (Ovid, 1950 to November 2014 week 4).
-
EMBASE (Ovid, 1980 to November 2014).
-
Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO, 1982 to November 2014).
-
ClinicalTrials.gov (November 2014).
-
Manual Alternative and Natural Therapy Index System (MANTIS, Ovid, 1980 to May 2014).
-
Index to Chiropractic Literature (ICL) (January 2014).
See Appendix 1 for the search strategies used for CENTRAL, MEDLINE, EMBASE, CINAHL, MANTIS and ICL.
We performed a search update in June 2015. Those results have been added to ‘Studies awaiting classification’ and will be incorporated into the review at the next update.
Searching other resources
We also screened references, personally communicated with identified content experts and checked our own personal files to identify potential references up to November 2014.
Data collection and analysis
Selection of studies
At least two review authors with expertise in medicine, physiotherapy, chiropractic, massage therapy, statistics or clinical epidemiology independently conducted selection at two stages ‐ citation identification (citation posting plus abstract) followed by study selection (full text) ‐ using pre‐piloted forms. The assembled group did not author any of the primary trials. We assessed agreement on study selection using the quadratic weighted Kappa statistic (Kw) and Cicchetti weights (Cicchetti 1976). We consulted a third review author in cases of persisting disagreement.
Data extraction and management
Two review authors independently extracted data on pre‐piloted forms, as per all Cervical Overview Group reviews. We resolved disagreements through consensus. We consulted a neutral third party if consensus was not reached. We contacted study authors to ask for missing information and to clarify data. We used descriptive statistics to provide a summarised description of groups, interventions, outcomes, adverse effects of treatment and costs of care. We extracted data on design (RCT, number analysed/number randomly assigned, intention‐to‐treat analysis, power analysis), participants (disorder subtype, duration of disorder), interventions (treatment characteristics in treatment and comparison groups, dosage/treatment parameters, co‐interventions, treatment schedules, durations of follow‐up) and outcomes (baseline means, end of study means, absolute benefits, reported results, point estimates with 95% confidence intervals (CIs), side effects, costs of care and adverse events). We noted these factors in the Characteristics of included studies table. All results reported were based on the sample size analysed using the 'intention‐to‐treat' principle, in other words, the sample entering the study.
Assessment of risk of bias in included studies
At least two review authors independently assessed risk of bias (Appendix 2; Furlan 2009; Higgins 2011) using pre‐piloted forms. We resolved disagreements through consensus (Graham 2012). The Cervical Overview Group used a calibrated team of assessors, and at least two assessors independently assessed the following characteristics for risk of bias (maximum criteria = 12; low risk of bias = six or more criteria were met versus high risk of bias = five or fewer criteria were met): randomisation; concealment of treatment allocation; blinding of participant, provider and outcome assessor; incomplete data: withdrawal/dropout rate and intention‐to‐treat analysis; selective outcome reporting; and other: similar baseline values, similar co‐interventions, acceptable compliance and similar timing of assessment. We did not exclude studies from further analyses on the basis of results of risk of bias assessments.
Measures of treatment effect
For continuous data, we calculated standardised mean differences with 95% confidence intervals (SMDs; 95% CIs). Standard mean difference was selected over mean difference (MD) because different types of exercises were assessed, and most interventions used different outcome measures and different scales. Mean difference was used for trials reporting the same outcome measure. The Cochrane Back Review Group guidelines (Furlan 2009) were foundational to key estimations of minimum clinically important differences for pain and function/disability. We assumed that the minimum clinically important difference was 10 on a 100‐point pain intensity scale (Cleland 2008; Farrar 2001; Felson 1995; Goldsmith 1993). Similarly, we judged a minimum clinically important difference of 5/50 units, or 10%, to be relevant for the NDI (Stratford 1999); a recent systematic review (MacDermid 2009) reported that the minimal detectable change varied from 5/50 for non‐complicated neck pain to 10/50 for cervical radiculopathy. The clinically important difference varied from 5/50 to 19/50 and was noted to be inconsistent across studies (Cleland 2008; MacDermid 2009). For other outcomes (i.e. global perceived effect and quality of life scales) for which clear guidelines on the size of clinically important effect sizes were lacking, we applied a system commonly used by Cohen 1988: small (0.20), medium (0.50) or large (0.80).
For continuous outcomes reported as medians, we calculated effect sizes (Kendal 1963, page 237).
For dichotomous outcomes, we calculated risk ratios (RRs). A risk ratio less than one represented beneficial treatment. When neither continuous nor dichotomous data were available, we extracted findings and statistical significance as reported by the author(s) of the original study and noted them in the Characteristics of included studies table.
We calculated the number needed to treat for an additional beneficial outcome (NNTB: the number of patients a clinician needs to treat to achieve clinically important improvement in one patient) and treatment advantages (%: clinically important differences or changes in percentage) for primary findings, to give the reader a sense of the magnitude of the treatment effect (Gross 2002a; see Table 1 and Table 2 for operational definition, calculations and results).
| Term | Definiton |
| Per cent treatment advantage (%) | Calculation of the clinically important difference or change in a per cent scale was estimated as follows. Karlberg 1996 data are used in this example. % improvement (control) equals the difference between the change in the control group (1) divided by the control baseline (56), which equals 1.8%. Treatment advantage = 42.6% ‐ 1.8% = 40.8% |
| Number needed to treat (NNTB) | For this example, Karlberg 1996 outcomes measured at short‐term follow‐up are used to derive the data. Number needed to treat is the number of patients a clinician needs to treat to achieve a clinically important improvement in 1. If we assume the minimal clinically important difference to be 10% of the baseline mean in the control group, and the control group mean at baseline is 56, then 10% of 56 is 5.6 The effect is baseline ‐ final value; therefore:
Converting these to standard normal values means that:
NNTB = 1 divided by the difference in areas under the normal curve (experimental group ‐ control group):
|
| Author/Comparison | NNTB | Advantage, % |
| PAIN | ||
| Haas 2004: pain | 12 (clinically important pain reduction) at ST | 23 |
| Haas 2010: pain | 4 (clinically important pain reduction) at IT | 29 |
| Cleland 2005 | 5 (clinically important pain reduction) | 29 |
| Cheung Lau 2011: pain | 4 (clinically important pain reduction) | |
| Fernandez 2004a | Unable to calculate because baseline data not reported | |
| Gonzalez‐Iglesias 2009 | 7 (clinically important pain reduction) | 47 |
| Martinez‐Segura 2006, | 2 (clinically important pain reduction) | 54 |
| Massaracchio 2013: pain | 4 (clinically important pain reduction) | |
| von Piekartz 2011: pain | 2 (clinically important pain reduction) at IT | |
| FUNCTION | ||
| Cheung Lau 2011: function | 5 (clinically important functional improvement) at IT | |
| Gonzalez‐Iglesias 2009 | 5 (clinically important functional improvement) | 41 |
| Haas 2010: function | 5 (clinically important functional improvement) at ST and IT | ST: 41 IT: 39 |
| Massaracchio 2013: function | 4 (clinically important functional improvement) | |
Dealing with missing data
We contacted the primary authors to request missing outcomes. To facilitate analysis, we used data imputation rules when necessary (Appendix 3).
Assessment of heterogeneity
Before calculating a pooled effect measure using RevMan 2014, we assessed the reasonableness of pooling on clinical grounds (Verbeek 2012). Possible sources of heterogeneity considered were symptom duration (acute versus chronic); subtype of neck pain (e.g. WAD); intervention type (e.g. mobilisation versus manipulation); characteristics of treatment (e.g. dosage, technique); and outcomes (pain relief, measures of function and disability, participant satisfaction, quality of life). We tested statistical heterogeneity between studies by using a random‐effects model. In the absence of heterogeneity (P value > 0.1 and I² > 40%), we combined data across studies as pooled SMDs, MDs or RRs using methods available in RevMan 2014.
Assessment of reporting biases
We used a funnel plot to detect reporting bias.
Data synthesis
We combined data across studies as pooled SMDs, MDs or RRs using methods available in RevMan 2014 after we assessed heterogeneity. We assessed the quality of the body of evidence using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach of The Cochrane Collaboration (Guyatt 2010; Higgins 2011; Appendix 4). Domains that may decrease the quality of the evidence include study design, limitations ‐ risk of bias, consistency of results, directness (generalisability), precision (sufficient data) and reporting biases. We defined high‐quality evidence as reported by RCTs with low risk of bias that provided consistent, direct and precise results for the outcome. We reduced the quality of the evidence by one level for each domain not met..
-
High quality: Further research is very unlikely to change our confidence in the estimate of effect. Consistent findings among 75% of RCTs with low risk of bias are generalisable to the population in question. Sufficient data, with narrow confidence intervals, are available. No reporting biases are known or suspected. (All domains are met.)
-
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. (One domain is not met.)
-
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. (Two domains are not met.)
-
Very low quality: We are very uncertain about the estimate. (Three domains are not met.)
-
No evidence: We identified no RCTs that measured the outcome.
We considered various factors to place the results into a larger clinical context: temporality, plausibility, strength of association, dose response, adverse events and costs.
Subgroup analysis and investigation of heterogeneity
Although we planned to perform subgroup analyses to assess the influence of three factors: risk of bias (concealment of allocation, blinding of outcome assessor), duration (acute, subacute, chronic) and subtypes of the disorder (non‐specific, WAD, work‐related, degenerative change‐related, radicular findings, cervicogenic headache), we found that this was not possible. We denoted subgroups to descriptively explore the effects of treatment dosage for manipulation alone or mobilisation alone, as meta‐regression was not possible. We consistently denoted trial risk of bias, quality of the evidence and duration of the disorder.
Sensitivity analysis
We did not perform sensitivity analyses on other factors (i.e. characteristics of the intervention examined, the intervention compared and the outcome (time point); arising analysis factors) nor meta‐regression because data in any one category of mobilisation or manipulation were insufficient. However, we did present data according to body region of manipulation or mobilisation.
Results
Description of studies
This update included 26 new trials for manipulation or mobilisation versus inactive control or another active treatment (Aquino 2009; Bronfort 2012; Cheung Lau 2011; Escortell‐Mayor 2011;Fernandez 2009; Gemmell 2010;Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT; Haas 2010;Leaver 2010;Madson 2010;Martel 2011; Martinez‐Segura 2006a; Masaracchio 2013; Puentedura 2011;Ragonese 2009; Saavedra‐Hernandez 2012CR; Saavedra‐Hernández 2012JO;Saayman 2011; Schomacher 2009;Shin 2006;Sillevis 2010; Sterling 2010; von Piekartz 2011; Youssef 2013; Yurkiw 1996).
Results of the search
Figure 1 describes the flow of studies from our previous updates (1822 citation postings) and from this update (1011 + 1004 + 280 citation postings). From 168 references representing 126 RCTs, we selected 51 RCTs (2910/3294 participants analysed/randomly assigned), and four are pending from our most recent update. Manipulation/Mobilisation versus control represented 18 publications for manipulation or mobilisation performed as a single‐modal application; manipulation/mobilisation versus another treatment represented 34 publications for manipulation or mobilisation performed as a single‐modal application and one publication that compared manipulation/mobilisation versus an inactive control and another active treatment (Saayman 2011); data on multi‐modal approaches that included manual therapy were obtained from this report and were presented separately (D'Sylva 2010; Miller 2010).
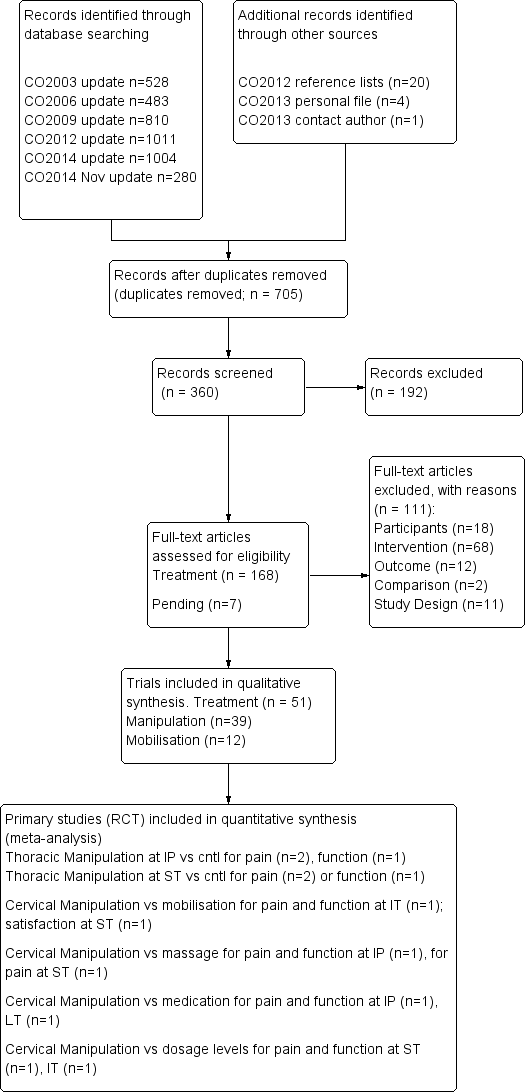
PRISMA diagram for manipulation and mobilisation.
See the reference list for multiple publications per study; the primary trials are depicted here. See Characteristics of included studies for further details on treatment characteristics, co‐interventions, baseline values, absolute benefits, reported results, SMDs, RRs, side effects and costs of care. Agreement between pairs of independent review authors from diverse professional backgrounds for manual therapy was Kw 0.84 (standard error (SE) 0.08).
Included studies
See Characteristics of included studies.
For comparison with various inactive control trials, the following disorder categories emerged.
-
18 studies included individuals with neck pain without radicular findings: acute (Fernandez 2009; Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT); chronic (Bitterli 1977; Cheung Lau 2011; Cleland 2005; Lin 2013; Martel 2011; Saavedra‐Hernandez 2012CR); mixed (Fernandez 2004 JWRD; Howe 1983; Martinez‐Segura 2006a; Masaracchio 2013; Saayman 2011; Sloop 1982; Sterling 2010); and symptom duration not reported (Krauss 2008; Parkin‐Smith 1998).
-
13 studies investigated neck pain: acute (Fernandez 2009; Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT); chronic (Cheung Lau 2011; Cleland 2005; Lin 2013; Martel 2011; Saavedra‐Hernandez 2012CR); mixed (Martinez‐Segura 2006a; Masaracchio 2013; Saayman 2011); and symptom duration not reported (Krauss 2008; Parkin‐Smith 1998).
-
Two investigated whiplash‐associated disorders: mixed (Fernandez 2004 JWRD; Sterling 2010).
-
Two investigated degenerative changes: chronic (Bitterli 1977); and mixed (Sloop 1982).
-
Two investigated cervicogenic headache: chronic (Bitterli 1977); and mixed (Howe 1983).
-
One investigated neck disorders with radicular signs and symptoms: mixed (Howe 1983).
For comparison with active treatment trials, the following disorder categories emerged.
-
34 studies included a comparison group (see Figure 2) (Aquino 2009; Bronfort 2012; Cassidy 1992; Chen 2007; Coppieters 2003; David 1998; Egwu 2008; Escortell‐Mayor 2011; Gemmell 2010; Giles 1999; Haas 2004; Haas 2010; Hurwitz 2002; Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a; Leaver 2010; Lee 2013; Madson 2010; Muller 2005; Nilsson 1997; Puentedura 2011; Ragonese 2009; Saavedra‐Hernández 2012JO; Saayman 2011; Savolainen 2004; Schomacher 2009; Shin 2006; Sillevis 2010; Strunk 2008; van Schalkwyk 2000; von Piekartz 2011; Wood 2001; Youssef 2013; Yurkiw 1996).
-
21 investigated neck pain without radicular findings: subacute (Gemmell 2010; Wood 2001; Yurkiw 1996); chronic (Aquino 2009; Escortell‐Mayor 2011; Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a; Madson 2010;Muller 2005; Saavedra‐Hernández 2012JO; Sillevis 2010); mixed (Bronfort 2012; Cassidy 1992; Coppieters 2003; David 1998; Egwu 2008; Leaver 2010;Saayman 2011; Strunk 2008); and symptom duration not reported (Savolainen 2004; van Schalkwyk 2000).
-
One investigated neck pain with headache: chronic (Nilsson 1997).
-
Two investigated neck pain with or without radicular symptoms: acute (Puentedura 2011); and symptom duration not reported (Fernandez 2004 JWRD).

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
-
One investigated neck pain with radicular signs and symptoms: duration not reported (Ragonese 2009).
-
One investigated neck pain with degenerative changes: chronic (Giles 1999).
-
One investigated a specific neck disorder (herniated disc): chronic (Shin 2006).
-
Three investigated cervicogenic headache: chronic (Haas 2004; Haas 2010; Youssef 2013)
-
One investigated cervicogenic headache with degenerative changes: chronic (Chen 2007)..
-
One investigated cervicogenic headache with or without radicular symptoms: mixed (Hurwitz 2002).
-
One investigated cervicogenic headache with temporomandibular joint (TMJ) dysfunction (von Piekartz 2011).
Ongoing studies
We recognised in this review a total of 13 ongoing studies from 1995 through 2015. With nine of 13 protocols/pilot studies published in 2010 or before, we could not rule out publication bias. See Characteristics of ongoing studies.
Studies awaiting classification
For Moretti 2004 and Cleland 2007, we are awaiting additional data; therefore classification is pending (see Characteristics of studies awaiting classification). For Leonelli 2013, we are awaiting a translation. We retrieved four studies in our most recent (June 2015) update, and they are pending data extraction (Casanova‐Mendez 2014; El Soleny 2014; Izquierdo‐Perez 2014; Karas 2014).
Excluded studies
We excluded 107 RCTs using the PICO (population, intervention, comparison and outcome) format. We excluded 18 trials on the basis of population (i.e. spasmodic torticollis, unable to split data from combined neck and low back trials, normal cervical spine); 68 for interventions (i.e. manual therapy in both treatment and control groups); 10 for design (i.e. mechanistic or multi‐modal trial design); and 11 for outcomes (i.e. range of motion data only).. See Characteristics of excluded studies.
Risk of bias in included studies
Risk of bias of included manipulation/mobilisation versus inactive controls
A total of 18 studies included a control (see Figure 2) (Bitterli 1977; Cheung Lau 2011; Cleland 2005; Fernandez 2004 JWRD; Fernandez 2009; Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT; Howe 1983; Krauss 2008; Lin 2013; Martel 2011; Martinez‐Segura 2006a; Masaracchio 2013; Parkin‐Smith 1998; Saavedra‐Hernandez 2012CR; Saayman 2011; Sloop 1982; Sterling 2010).
-
Researchers failed to describe or use appropriate concealment of allocation (39%, 7/18).
-
Study lacked effective blinding procedures (outcome assessor 83%, 15/18; participant 100%, 18/18; personnel/care provider 100%, 18/18). We acknowledge that it is difficult to blind participants and impossible to blind care providers when manual treatments are provided.
-
Selective outcome reporting bias was seen in 5% (1/18). The Cervical Overview Group has found that very few investigators register their studies with the research database.
-
Co‐intervention was avoided in a small number of studies (28%, 5/18), and compliance was monitored in 44% (8/18).
Risk of bias of included manipulation/mobilisation versus active comparisons
A total of 34 studies included a comparison group (see Figure 2) (Aquino 2009; Bronfort 2012; Cassidy 1992; Chen 2007; Coppieters 2003; David 1998; Egwu 2008; Escortell‐Mayor 2011; Gemmell 2010; Giles 1999; Haas 2004; Haas 2010; Hurwitz 2002; Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a; Leaver 2010; Lee 2013; Madson 2010; Muller 2005; Nilsson 1997; Puentedura 2011; Ragonese 2009; Saavedra‐Hernández 2012JO; Saayman 2011; Savolainen 2004; Schomacher 2009; Shin 2006; Sillevis 2010; Strunk 2008; van Schalkwyk 2000; von Piekartz 2011; Wood 2001; Youssef 2013; Yurkiw 1996). Thirteen studies (13/34, 38%) had low risk of bias and 21 (21/34, 62%) had high risk of bias.
-
Researchers failed to adequately describe or use an appropriate randomisation technique in 13 studies (38%, 13/34).
-
Study authors failed to adequately describe or use appropriate concealment of allocation in 22 studies (65%, 22/34).
-
Effective blinding procedures were lacking in 31 studies regarding the participant (91%, 31/34), in 34 studies regarding the care provider (100%, 34/34) and in 31 studies regarding the outcome assessor (91%, 31/34). We acknowledge that it is difficult to blind the participant and impossible to blind the care provider when manual treatments are provided.
-
Investigators described acceptable dropout rates in 23 studies (68%, 23/34).
-
All randomly assigned participants were reported/analysed in the group to which they were allocated by randomisation in 18 studies (53%, 18/34).
-
Information regarding reporting bias was lacking in 33 studies (97%, 33/34).
-
Groups were similar at baseline regarding the most important prognostic indicators in 20 studies (59%, 20/34).
-
Co‐intervention was avoided or similar between participants in 10 studies (29%, 10/34).
-
Researchers monitored acceptable compliance in 14 studies (41%, 14/34).
-
Timing of the outcome assessment was similar in all groups in 30 studies (88%, 30/34).
Other potential sources of bias
Funnel plot analysis suggests the presence of publication bias (Figure 3).
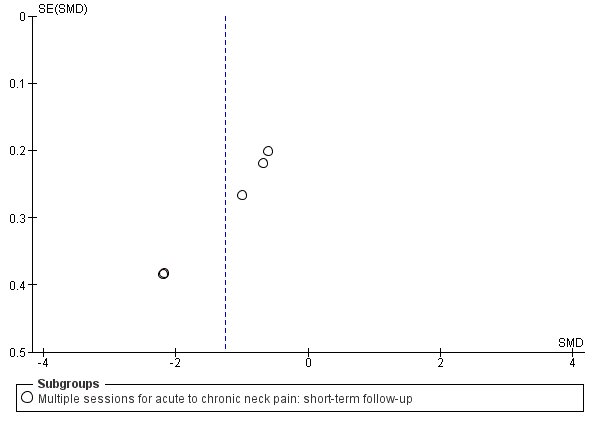
Funnel plot of comparison: manipulation vs control, outcome: FUNNEL PLOT for PAIN: thoracic manipulation vs same treatment in both arms.
Effects of interventions
See: Summary of findings for the main comparison Manipulation (cervical) compared with oral medicine for acute/subacute neck pain; Summary of findings 2 Manipulation (thoracic) compared with inactive control for neck pain; Summary of findings 3 Manipulation compared with mobilisation for neck pain; Summary of findings 4 Manipulation compared with exercise for neck pain; Summary of findings 5 High dose of manipulation compared with low dose of manipulation for chronic neck pain
As data were limited, we were unable to carry out subgroup analyses or meta‐regression for symptom duration, subtype of neck disorder or methodological quality, although we did consistently note them in the text. High‐quality evidence provides greatest certainty about the effectiveness of treatment.
Manipulation alone of cervical region
In all, 24 trials met the inclusion criteria for this section. Twelve of them had low risk of bias (Bronfort 2012; Cassidy 1992; Haas 2004; Haas 2010; Hurwitz 2002; Leaver 2010; Saayman 2011; Sillevis 2010; Sloop 1982; Strunk 2008;Wood 2001; Yurkiw 1996), and 12 had high risk of bias (Bitterli 1977; Chen 2007; Gemmell 2010; Giles 1999; Howe 1983; Martinez‐Segura 2006a; Muller 2005; Nilsson 1997; Puentedura 2011; Saavedra‐Hernández 2012JO; Savolainen 2004; van Schalkwyk 2000). We reported the following observations: (1) results from a single session, which may not depict clinical practice but nevertheless were assessed in clinical trials; and (2) findings of trials using multiple treatment sessions, dose responses and comparison trials.
Manipulation alone of cervical region versus inactive control
Pain
Single session
Three very small RCTs, one at high risk of bias and two at low risk, assessed the effect of a single session of manipulation (see Figure 2): One mock treatment indicated that a single session of manipulation resulted in immediate pain relief (very low quality, number needed to treat for an additional beneficial outcome (NNTB) 2, 71 participants; Martinez‐Segura 2006a) for neck disorders of mixed duration; two trials showed that a single session of manipulation as adjunct treatment to certain medications offered no short‐term benefit for pain relief in chronic neck disorders with radicular findings or headache (very low quality, 29 participants; Howe 1983), nor in subacute and chronic neck disorders with associated cervical spondylosis (low quality, 39 participants; Sloop 1982).
Multiple sessions
Two very small RCTs, one at high and one at low risk of bias, assessed the effects of multiple sessions of manipulation versus a control and provided conflicting evidence. Two trials (low quality, 60 participants; Bitterli 1977; Saayman 2011) that assessed people with subacute and chronic neck pain yielded conflicting results. These results could not be combined because they consisted of different types of data. Six sessions of manipulation over three weeks when added to laser showed pain reduction at short‐term follow‐up (low quality, 40 participants; Saayman 2011). Four sessions over three weeks when compared with an inactive control revealed no evidence of benefit for pain reduction at short‐term follow‐up (low quality, 20 participants; Bitterli 1977).
Manipulation alone of cervical region versus oral medication
Three trials compared cervical manipulation versus use of oral medication.
-
Non‐steroidal anti‐inflammatory drugs (NSAIDs), acetaminophen, opioids and muscle relaxants (moderate quality, 181 participants with acute and subacute neck pain; Bronfort 2012).
-
Tenoxicam with ranitidine (very low quality, 35 participants with chronic neck pain; Giles 1999).
-
Celaconxin, rofecoxib or paracetamol (very low quality, 42 participants with chronic neck pain; Muller 2005).
See summary of findings Table for the main comparison for main results representing evidence of moderate quality.
Pain
For acute/subacute neck pain, manipulation was more effective than use of certain oral medications [non‐steroidal anti‐inflammatory drugs (NSAIDs), acetaminophen, opioids and muscle relaxants] at immediate post treatment (moderate quality, 182 participants, SMD ‐0.34, 95% CI ‐0.64 to ‐0.05; Bronfort 2012) and at long‐term follow‐up (moderate quality, 181 participants, SMD ‐0.32, 95% CI ‐0.61 to ‐0.02; Bronfort 2012) (see Figure 4). Cervical manipulation was found to be no more effective than certain medications at intermediate‐term follow‐up (moderate quality, 216 participants, SMD ‐0.21, 95% CI ‐0.5 to 0.08; Bronfort 2012).

Forest plot of comparison: manipulation vs another treatment, outcome: PAIN: cervical manipulation vs medicine.
For chronic neck pain, manipulation was no different from use of certain medications (see above, per author) at immediate post treatment (very low quality, 35 participants; Giles 1999) and at long‐term follow‐up (very low quality, 42 participants; Muller 2005).
Function and disability
For acute/subacute neck pain, manipulation showed a slight advantage over oral medication (see above) immediate post treatment and at intermediate‐term follow‐up (SMD ‐0.30, 95% CI ‐0.59 to ‐0.00) but not over the long term (SMD ‐0.11, 95% CI ‐0.40 to 0.18, moderate quality, 182 participants; Bronfort 2012).
For chronic neck pain, investigators reported no differences between manipulation and oral medication (see above) at immediate post treatment (very low quality, 30 participants; Giles 1999) and over the long term (very low quality, 42 participants; Muller 2005).
Global perceived effect
Bronfort 2012 (moderate quality, 182 participants) suggested that 12 weeks of manipulation was superior to use of oral medication (see above) for global perceived effect at long‐term follow‐up of participants with acute/subacute neck pain.
Patient satisfication
Bronfort 2012 (moderate quality, 182 participants) suggested that 12 weeks of manipulation was superior to use of oral medication (see above) for satisfaction at long‐term follow‐up among participants with acute/subacute neck pain.
Quality of life
Bronfort 2012 (moderate quality, 182 participants) found no significant results for oral medication (see above) at immediate‐, intermediate‐ and long‐term follow‐up.
Manipulation alone of cervical region versus mobilisation and other manual techniques
Pain
Single session
Two trials assessed the effects of a single session of cervical manipulation versus varied comparisons.
-
A single session of manipulation (low quality, 100 participants; Cassidy 1992) was comparable with a neuromuscular mobilisation approach using muscle energy technique for immediate pain relief in neck disorders of mixed duration.
-
A single session of manipulation (low quality, 28 participants; Yurkiw 1996) showed no significant differences in pain relief when compared with a single session of activator instrument.
None of the above trials showed differences between groups for pain relief at immediate term among individuals with subacute or chronic neck disorders.
Multiple sessions
Ten trials assessed the effects of four to 20 sessions of manipulation conducted over two to 12 weeks against:
-
mobilisations (36 participants, Gemmell 2010; 269 participants, Hurwitz 2002; 177 participants, Leaver 2010);
-
massage ‐ soft tissue treatments (32 participants, Haas 2010; 53 participants, Nilsson 1997);
-
manipulation of the thoracic spine alone (20 participants, Puentedura 2011);
-
combined therapeutic approach including muscle energy provided to the thoracic spine and sacroiliac joint (six participants, Strunk 2008);
-
manipulation of varied dosages (15 participants, Haas 2004; 32 participants, Haas 2010);
-
manipulation of varied techniques (30 participants, van Schalkwyk 2000);
-
mobilisation plus heat; mobilisation plus electronic muscle stimulation (EMS); mobilisation plus heat and EMS (269 participants, Hurwitz 2002); and
-
activator instrument (36 participants, Gemmell 2010; 30 participants, Wood 2001).
Manipulation was no more effective than mobilisation in improving pain at short‐term (SMD ‐0.05, 95% CI ‐0.34 to 0.25; Leaver 2010) and intermediate‐term follow‐up (moderate quality, 446 participants, MD pooled ‐0.07, 95% CI ‐0.72 to 0.59; Hurwitz 2002; Leaver 2010) (see Figure 5; summary of findings Table 3). One trial (of very low quality) assessed the effects of six sessions of manipulation conducted over three weeks compared with six sessions of mobilisation (Gemmell 2010). Despite lack of data, none of these studies showed significant differences between groups for pain relief at immediate‐, short‐, intermediate‐ and long‐term (Gemmell 2010) follow‐up for those with subacute and chronic neck pain. Both Haas 2010 and Nilsson 1997 have concluded that manual therapy was more effective than "light manual therapy" (massage) at short term (low quality, 85 participants, SMD pooled ‐0.5, 95% CI ‐0.93 to ‐0.70) follow‐up. These findings are supported by Haas 2010 at intermediate‐term (low quality, 72 participants, SMD ‐0.79, 95% CI ‐1.47 to ‐0.11) follow‐up. A clinician would have to treat five people (NNTB 5) to achieve this intermediate‐term result in one person.

Forest plot of comparison: manipulation vs another treatment, outcome: PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up.
Puentedura 2011 (very low quality, 20 participants) demonstrated that cervical manipulation was more effective than thoracic manipulation at short‐ (SMD ‐2.43, 95% CI ‐3.64 to ‐1.21, NNTB 12) and intermediate‐term (SMD ‐2.70, 95% CI ‐3.98 to ‐1.42, NNTB 6) follow‐up. Cervical manipulation contrasted against a combined therapeutic approach of thoracic and sacroiliac manipulation (one trial, six participants; Strunk 2008) yielded similar findings for subacute/chronic neck pain at immediate post treatment. Haas 2004 and Haas 2010 reported no significant results regarding the utilisation of 12 sessions of manipulation versus three sessions at short‐ (low quality, 47 participants, SMD pooled ‐0.66, 95% CI ‐1.81 to 0.49) and intermediate‐term (moderate quality, 50 participants, SMD pooled ‐0.40, 95% CI ‐0.96 to 0.16) follow‐up for chronic neck pain with CGH (see summary of findings Table 5). Three trials compared one manipulation technique versus another and found no difference in immediate‐ and short‐term pain relief when a rotary break manipulation was compared with a lateral break manipulation for 10 sessions over four weeks in participants with neck disorder of undefined duration (very low quality; van Schalkwyk 2000); and when manual manipulation was compared with instrumental manipulation (activator) for subacute neck disorder after eight sessions over four weeks (very low quality; Wood 2001) and after six sessions over three weeks (very low quality; Gemmell 2010).
Function and disability
Manipulation was no more effective than mobilisation at short‐ (SMD ‐0.06, 95% CI: ‐0.35 to 0.24; Leaver 2010) and intermediate‐term follow‐up (high quality, 446 participants; Hurwitz 2002; Leaver 2010; SMD pooled 0.10, 95% CI ‐0.18 to 0.37). One additional trial (very low quality, 31 participants; Gemmell 2010) assessed the effects of six sessions of manipulation conducted over three weeks compared with six sessions of mobilisation. Despite lack of data, none of these studies showed significant differences between groups in functional improvement at immediate‐, short‐, intermediate‐ and long‐term follow‐up for those with subacute and chronic neck pain. Haas 2010 (low quality, 36 participants) concluded that manipulation was more effective than "light manual therapy" ‐ massage to improve function at short‐ (low quality, 36 participants; SMD ‐0.87, 95% CI ‐1.60 to ‐0.14) and intermediate‐term (SMD ‐0.72, 95% CI ‐1.39 to ‐0.04) follow‐up. A clinician would have to treat five people (NNTB 5) to achieve this medium advantage (29% treatment advantage) for one person at both time points.
Puentedura 2011 (very low quality, 20 participants) concluded that cervical manipulation was more effective than thoracic manipulation at short‐ (SMD ‐1.01, 95% CI ‐1.96 to ‐0.07; NNTB 5) and intermediate‐term (SMD ‐1.22, 95% CI ‐2.19 to ‐0.24; NNTB 4) follow‐up. Haas 2004 suggested that 12 sessions of manipulation was superior to three sessions for immediate functional improvement in individuals with chronic cervicogenic headache (SMD ‐1.15, 95% CI‐2.27 to ‐0.03). Haas 2004 and Haas 2010 reported no significant results regarding the utilisation of 12 to 16 sessions of manipulation compared with three to eight sessions at short‐ (low quality, 47 participants, SMD pooled ‐0.75, 95% CI ‐1.71 to 0.22) and intermediate‐term (moderate quality, 50 participants, SMD pooled ‐0.61, 95% CI ‐1.38 to 0.17) follow‐up (summary of findings Table 5). One trial assessed the effects of six sessions of manipulation conducted over three weeks compared with six sessions of application of the activator instrument (very low quality, 27 participants; Gemmell 2010); no significant differences between groups were noted in functional improvement at immediate‐, short‐, intermediate‐ and long‐term follow‐up for those with subacute and chronic neck pain.
Global perceived effect
One trial assessed the effects of four sessions of manipulation conducted over two weeks compared with four sessions of mobilisation (moderate quality, 177 participants; Leaver 2010) in individuals with subacute to chronic neck pain. Results showed no differences between groups at immediate‐ (SMD ‐0.18, 95% CI ‐0.47 to 0.12) and intermediate‐term (SMD ‐0.06, 95% CI ‐0.35 to 0.24) follow‐up for global perceived effect. Gemmell 2010 (very low quality, 36 participants) compared the effectiveness of manipulation, mobilisation and the activator instrument. This study showed no significant differences between treatment groups at immediate‐, short‐, intermediate‐ and long‐term follow‐up in global perceived effect for those with subacute neck pain.
Patient satisfication
One trial (moderate quality, 269 participants; Hurwitz 2002) assessed the effect of 12 sessions of manipulation conducted over six weeks compared with mobilisation (SMD ‐0.02, 95% CI ‐0.21 to 0.24). Findings showed no differences in short‐term participant satisfaction among those with subacute and chronic neck pain.
Quality of life
One trial (moderate quality, 176 participants; Leaver 2010) showed no significant differences in quality of life between manipulation and mobilisation at immediate‐, short‐ (SMD 0.08, 95% CI ‐0.21 to 0.38), intermediate‐ (SMD ‐0.06, 95% CI ‐0.35 to 0.24) and long‐term follow‐up for participants with subacute and chronic neck pain. Gemmell 2010 (very low quality, 28 participants) compared the effects of six sessions of manipulation versus application of the activator instrument conducted over three weeks. This trial showed no differences in quality of life between groups at immediate‐, short‐, intermediate‐ and long‐term follow‐up for those with subacute neck pain.
Manipulation alone of cervical region versus exercise or other physical medicine modalities
Pain
Single session
One trial assessed the effects of a single session of cervical manipulation compared with a single use of kinesio‐tape (very low quality, 76 participants; Saavedra‐Hernández 2012JO) and showed no significant differences in pain relief at immediate‐term follow‐up for individuals with subacute or chronic neck disorders.
Multiple sessions
Five trials assessed the effects of manipulation conducted over two to 12 weeks against:
-
exercise (moderate quality, 182 participants; Bronfort 2012);
-
low‐level laser therapy (low quality, 40 participants; Saayman 2011);
-
TENS (very low quality, 70 participants; Chen 2007);
-
acupuncture (very low quality, 43 participants; Muller 2005); and
-
low‐voltage electrical acupuncture (very low quality, 38 participants; Giles 1999).
Cervical manipulation was found to be no more effective than exercise (moderate quality, 216 participants; Bronfort 2012) at immediate‐ (SMD ‐0.13, 95% CI ‐0.43 to 0.16), intermediate‐ (SMD ‐0.16, 95% CI ‐0.45 to 0.13) and long‐term (SMD 0.06, 95% CI ‐0.23 to 0.35) follow‐up. See summary of findings Table 4. One trial (low quality, 40 participants; Saayman 2011) assessed the effects of six sessions of manipulation conducted over three weeks compared with six sessions of low‐level laser therapy at short‐term follow‐up for those with subacute and chronic neck pain; results favoured manipulation plus low‐level laser therapy and showed no differences between manipulation and low‐level laser therapy alone. Chen 2007 (very low quality, 70 participants) demonstrated that manipulation was more effective than TENS for individuals with chronic CGH at short‐term (SMD ‐1.92, 95% CI ‐2.49 to ‐1.35) follow‐up. Manipulation was found to be no different from low‐voltage electrical acupuncture (very low quality, 38 participants; Giles 1999) immediately post treatment or from acupuncture (very low quality, one trial, 43 participants; Muller 2005) in terms of pain relief at long‐term follow‐up.
Function and disability
Single session
One trial (very low quality, 76 participants; Saavedra‐Hernández 2012JO) demonstrated that use of kinesio‐tape for seven days was more effective than performance of two manipulation techniques to improve function immediately after treatment (SMD 0.46, 95% CI 0.01 to 0.92). This difference did not reach the clinically important difference.
Multiple sessions
Manipulation was no more effective than exercise (moderate quality, 182 participants; Bronfort 2012) at immediate‐ (SMD ‐0.21, 95% CI ‐0.50 to 0.08), intermediate‐ (SMD ‐0.01, 95% CI ‐0.30 to 0.28) and long‐term (SMD ‐0.02, 95% CI ‐0.31 to 0.27) follow‐up. Other studies reported no significant differences between groups at any follow‐up time point as follows. No difference in function was noted between low‐voltage electrical acupuncture (very low quality, 38 participants; Giles 1999) immediately post treatment and acupuncture (very low quality, 43 participants; Muller 2005) at long‐term follow‐up. One trial (very low quality, 76 participants; Saayman 2011) assessed the effects of six sessions of manipulation conducted over three weeks versus six sessions of low‐level laser therapy at short‐term follow‐up and showed a significant difference favouring the combination of cervical manipulation plus low‐level laser therapy.
Global perceived effect
Despite the lack of data for statistical analysis, one trial (moderate quality, 182 participants; Bronfort 2012) showed no differences for this outcome between 12 weeks of manipulation and application of a home exercise programme at long‐term follow‐up.
Participant satisfication
Bronfort 2012 (moderate quality, 182 participants) suggested that 12 weeks of cervical manipulation was superior to application of a home exercise programme for participant satisfaction at long‐term follow‐up in participants with acute or subacute neck pain.
Quality of life
One trial (moderate quality, 182 participants; Bronfort 2012) showed no differences (SMD 0.0, 95% CI ‐0.29 to 0.29) between cervical manipulation and a home exercise programme at intermediate‐ and long‐term follow‐up.
Manipulation alone of thoracic region
Twelve trials looked at manipulation alone in the thoracic region.
Manipulation alone of thoracic region versus inactive control
Ten trials (six low risk of bias, four high risk of bias) assessed manipulation alone versus an inactive control in the thoracic region. See summary of findings Table 2.
Pain
Single session
Three RCTs ‐ two with low and one with high risk of bias ‐ assessed the effects of a single session of manipulation. They were clinically heterogeneous owing to disorder type and comparison (see Figure 2). One trial found that manipulation decreased pain when compared with placebo in participants with chronic neck pain (low quality, 36 participants; Cleland 2005). Two trials showed no differences between groups for manipulation when compared with an inactive control (very low, 22 participants; Krauss 2008) and when compared with same treatment in both arms (low quality, 82 participants; Saavedra‐Hernandez 2012CR).
Multiple sessions
Seven RCTs ‐ four with low and three with high risk of bias ‐ assessed the effects of thoracic manipulation provided at multiple sessions at three different follow‐up points (see Figure 2).
-
Immediate follow‐up: Two trials (low quality, 90 participants, pooled SMD ‐3.46, 95% CI ‐4.13 to ‐2.79; Fernandez 2009; Gonzalez‐Iglesias 2009 JO) looked at effects on acute pain and found that results favoured the treatment group. Two trials (low quality, 141 participants, pooled SMD ‐0.23, 95% CI ‐1.15 to 0.69; Cheung Lau 2011; Parkin‐Smith 1998) looked at chronic pain, and the results were heterogeneous (I2 = 81%).
-
Short‐term follow‐up: Four trials (moderate quality, 242 participants; Fernandez 2004 JWRD; Gonzalez‐Iglesias 2009 JO; Gonzalez‐Iglesias 2009 MT; Masaracchio 2013) that looked at acute and subacute neck pain, although assessed to be clinically similar, were statistically heterogeneous (I2 = 84%). Pooled results favoured the experimental group (SMD ‐1.46, ‐2.20 to ‐0.71; NNTB 4 to 7; magnitude of effect: small to medium). For chronic neck pain, one trial (111 participants; Cheung Lau 2011) looked at multiple sessions of thoracic manipulation compared with the same treatment in both arms. Results showed a decrease in pain in the experimental group.
-
Intermediate follow‐up: One trial (low quality, 111 participants; Cheung Lau 2011) favoured the experimental group when compared with the same treatment in both arms.
Function and disability
Six trials investigated the effects of thoracic manipulation when compared with a control.
Single session
One RCT with low risk of bias assessed the effects of single‐session thoracic manipulation (see Figure 2). This trial (low quality, 82 participants; Saavedra‐Hernandez 2012CR) found that thoracic manipulation significantly favoured the experimental group when function was assessed among participants with chronic neck pain.
Multiple sessions
Four RCTs assessed the effects of multiple sessions of thoracic manipulation at three follow‐up periods (see Figure 2).
-
Immediate follow‐up: Two trials (low quality, 141 participants, pooled SMD ‐0.52, 95% CI ‐0.85 to ‐0.18; Cheung Lau 2011; Parkin‐Smith 1998) looked at effects on function/disability and significantly favoured the experimental group for chronic neck pain.
-
Short‐term follow‐up: Four trials (moderate quality, 258 participants; NNTB 5, Cheung Lau 2011; NNTB 5, Gonzalez‐Iglesias 2009 JO; NNTB 5, Gonzalez‐Iglesias 2009 MT; NNTB 4, Masaracchio 2013) looked at the effects of thoracic manipulation among participants with acute, subacute and chronic neck pain. All four trials favoured or significantly favoured the experimental group (pooled SMD ‐1.40, 95% CI ‐2.24 to ‐0.55). The magnitude of effect was small to medium across varied outcome measures.
-
Intermediate follow‐up: One trial (low quality, 111 participants, NNTB 5, magnitude small; Cheung Lau 2011) looked at the effects of thoracic manipulation among participants with chronic neck pain and significantly favoured the experimental group.
Quality of life
One trial investigated the effects of thoracic manipulation when compared with a control.
Multiple sessions
One RCT with low risk of bias assessed the effects of multiple sessions of thoracic manipulation at immediate‐, short‐ and intermediate‐term follow‐up (see Figure 2). This trial (low quality, 111 participants; Cheung Lau 2011) significantly favoured the experimental group for chronic neck pain.
Subgroup analysis
Effects calculated in these meta‐analyses tended to overestimate the intervention effect, as suggested by the asymmetrical appearance of the funnel plots in Figure 3 (pain). Publication bias, a type of reporting bias, was possible and could not be ruled out. When considering disorder subtypes, all trials except one (Fernandez 2004 JWRD) (WAD 2 or 3) discussed neck pain. Therefore, subgroup analysis of this factor could not be formally conductied through meta‐regression. Very low‐quality evidence (one trial, 88 participants; Fernandez 2004 JWRD) supported thoracic manipulation as an adjunct to individualised physiotherapy care for pain reduction in acute/subacute WAD 2 or 3.
Manipulation alone of thoracic region versus mobilisation
Pain
Single session
One trial (moderate quality, 100 participants; Sillevis 2010) rated as having low risk of bias concluded that a single session of thoracic manipulation was comparable with thoracic mobilisation for immediate pain relief among participants with chronic non‐specific neck pain.
Manipulation alone of thoracic region versus mobilisation
Pain
Multiple sessions
One trial (very low quality, 41 participants; Savolainen 2004) with high risk of bias concluded that four sessions of thoracic manipulation over four weeks led to similar pain outcomes when compared with instructed exercise conducted over an undisclosed period for participants with neck pain of undefined duration at long‐term follow‐up.
Mobilisation alone of cervical region
Nine trials ‐ five with low (Coppieters 2003; David 1998; Hurwitz 2002; Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a) and four with high risk of bias (Bitterli 1977; Cassidy 1992; Egwu 2008; Sterling 2001) ‐ met the inclusion criteria.
Mobilisation alone of cervical region versus inactive control
Two trials looked at mobilisation alone of the cervical region versus an inactive control. Both trials had high risk of bias (Bitterli 1977; Sterling 2010).
Pain
One trial (very low quality, 18 participants; Bitterli 1977) reported no additional pain relief when mobilisation was used as an adjunct to manipulation in participants with chronic CGH or degenerative changes immediately following the treatment period. In one trial (low quality, 39 participants; Sterling 2001), results favoured inactive control when compared with manual contact for participants with subacute/chronic neck pain ‐ WAD 2.
Mobilisation alone of cervical region versus medical injection
Pain
Multiple sessions
Lee 2013 (very low quality, 33 participants) concluded that mobilisation using the proprioceptive neuromuscular facilitation technique was more effective than trigger point intramuscular injection of lidocaine (SMD ‐1.05, 95% CI ‐1.96 to ‐0.15) for participants with neck pain with myofascial pain syndrome.
Function
No significant difference in function was found when this mobilisation approach was compared with intramuscular injection in one trial (very low quality, 33 participants; Lee 2013).
Mobilisation alone of cervical region versus mobilisation and other manual techniques
Pain
Single session
Three trials assessed the effect of one session of one mobilisation technique versus another at a randomly chosen segment in participants with chronic neck pain.
-
Mobilisation at most symptomatic segment versus mobilisation at randomly chosen segment (low quality, 48 participants; Aquino 2009).
-
Central posterior‐to‐anterior (PA) passive accessory movement mobilisation technique versus random PAs at the same segment (low quality, 60 participants; Kanlayanaphotporn 2010a).
-
Ipsilateral PAs versus random PAs at the same segment (low quality, 60 participants; Kanlayanaphotporn 2009).
-
Mobilisation perpendicular to the facet plane at the most symptomatic segment versus the same mobilisation three levels above or below (low quality, 126 participants; Schomacher 2009).
None of these studies demonstrated significant differences between groups for reducing neck pain. Two studies compared the effectiveness of one mobilisation technique versus another mobilisation technique in individuals with chronic neck pain (Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a). One study showed no significant differences in pain reduction when an ipsilateral PA mobilisation was compared with one of three randomly selected mobilisation techniques: ipsilateral PA, central PA or contralateral PA (Kanlayanaphotporn 2009). Another study by the same authors demonstrated no significant change in pain when comparing central PA mobilisation versus one of the three random mobilisation techniques (Kanlayanaphotporn 2010a). Although statistically not significant, the mean achieved a minimal clinically important change, and post hoc analysis using an interaction plot favoured PA mobilisations over random mobilisation for neck pain during movement.
Multiple sessions
Seven trials assessed the effects of one mobilisation technique against another manual therapy technique. These studies reported the following varied results.
-
Massage ‐ light manual therapy (very low quality, 22 participants; Madson 2010; 36 participants, Youssef 2013): Youssef 2013 concluded that mobilisation was more effective than a massage regimen consisting of six phases at immediate follow‐up (SMD ‐2.89, 95% CI ‐3.85 to ‐1.93) for chronic CGH, and Madson 2010 noted no difference (SMD ‐0.52, 95% CI ‐1.35 to 0.32) when using effleurage, stroking and pétrissage for chronic neck pain.
-
One technique versus another ‐ anterior‐to‐posterior (AP) accessory movements, PA transverse and cervical rotational oscillatory techniques (low quality, 95 participants; Egwu 2008): Egwu 2008 concluded that use of an AP unilateral pressure technique was more effective for pain relief immediately post treatment when compared with rotation or transverse pressure (RR 0.36, 95% CI 0.18 to 0.72) after multiple sessions of mobilisation given twice a week for a maximum of four weeks.
-
Activator instrument (very low quality, 28 participants; Gemmell 2010): One trial (31 participants; Gemmell 2010) showed no significant difference between mobilisation and the Activator instrument for pain relief at immediate‐, short‐, intermediate‐ and long‐term follow‐up among those with subacute neck pain.
-
Manual therapy to the TMJ (very low quality, 38 participants; von Piekartz 2011): Study authors concluded that manual therapy to the TMJ among individuals with chronic CGH with a minimum of one of the four signs of a TMJ disorder was more effective than manual therapy to the cervical spine immediately post treatment (SMD 2.27, 95% CI 1.43 to 3.10, NNTB 2) and at intermediate‐term (SMD 3.55, 95% CI 2.50 to 4.61, NNTB 2) follow‐up.
-
Various multi‐modal approaches: Hurwitz 2002 (moderate quality, 133 participants) compared the effectiveness of mobilisation versus manipulation as an adjunct treatment to heat, manipulation plus electrical muscular stimulation (EMS) and manipulation plus heat and EMS. This study showed no significant differences in pain relief between treatment groups of participants with subacute or chronic neck pain at intermediate‐term follow‐up. Additionally, Cassidy 1992 (low quality, 100 participants) compared manipulation versus a muscle energy technique and reported no difference in pain measures immediately following the treatment period for chronic neck pain.
Function and disability
Single session
We found no trial.
Multiple sessions
The following four trials assessed the effects of mobilisation against various manual therapy approaches; three suggested no significant results at any time point, and one (von Piekartz 2011) favoured manual therapy to the TMJ.
-
Manual therapy to the TMJ (very low quality, 38 participants; von Piekartz 2011): Investigators found that manual therapy to the TMJ was more effective than manual therapy to the cervical spine immediately post treatment (SMD 1.35, 95% CI 0.64 to 2.06, NNTB 5) and at intermediate‐term (SMD 2.22, 95% CI 1.39 to 3.04, NNTB 4) follow‐up. Participants in this trial had cervicogenic headache with at least one sign or symptom of TMJ disorder.
-
Massage ‐ light manual therapy (very low quality, 23 participants; Madson 2010; 36 participants, Youssef 2013).
-
Activator instrument (very low quality, 31 participants; Gemmell 2010).
Global perceived effect
Two small trials compared the impact of one session of one PA mobilisation technique versus a random mobilisation technique on global perceived effect in individuals with chronic neck pain at immediate follow‐up (low quality, 120 participants; Kanlayanaphotporn 2009; Kanlayanaphotporn 2010a). Researchers reported no significant results for global perceived effect.
Mobilisation alone of cervical region versus exercise and other physical medicine modalities
Pain
Single session
One trial assessed the effect of one session of mobilisation against pulsed ultrasound (low quality, 20 participants; Coppieters 2003). Researchers investigated neural dynamic mobilisation in 20 participants with acute and chronic neck pain and found a non‐significant difference in pain reduction when compared with pulsed ultrasound. Although results were not statistically significant, the mean achieved a minimal clinically important difference (suggesting possible type 2 error).
Multiple sessions
Five trials assessed the effects of mobilisation against:
-
acupuncture (low quality, 51 participants; David 1998): no difference in pain reduction when mobilisation was compared with acupuncture for subacute or chronic neck pain including WAD at long‐term follow‐up;
-
exercise (very low quality, 20 participants; Ragonese 2009): no significant difference for cervical radiculopathy at immediate‐term follow‐up (summary of findings Table 4);
-
TENS (very low quality, 87 participants; Escortell‐Mayor 2011): no significant difference for chronic neck pain.
-
shock wave therapy (very low quality, 33 participants; Lee 2013): cervical neuromuscular mobilisation technique possibly favoured over extracorporeal shock wave therapy at immediate post treatment for myofascial pain in the upper trapezius; and
-
cervical traction (very low quality, 26 participants; Shin 2006): Chuna manual therapy found more effective than cervical traction immediately post treatment for a herniated cervical disc.
Function and disability
None of the following trials (acupuncture: low quality, 51 participants; David 1998; exercise: very low quality, 20 participants; Ragonese 2009; TENS: very low quality, 87 participants; Escortell‐Mayor 2011; shock wave therapy: very low quality, 33 participants; Lee 2013) suggested significant results at any time point.
Patient satisfaction
One study (very low quality, 89 participants; Escortell‐Mayor 2011) assessed the effects of 10 sessions of mobilisation conducted over four weeks compared with utilisation of TENS at the cervical region. Investigators showed no significant results for utilisation of TENS at intermediate‐term (RR 1.09, 95% CI 0.96 to 1.23) follow‐up in terms of patient satisfaction among those with chronic neck pain.
Quality of life
One trial compared the effects of 10 sessions of mobilisation conducted over four weeks versus utilisation of TENS at the cervical region (very low quality, 83 participants; Escortell‐Mayor 2011). Researchers showed no differences at immediate‐ and intermediate‐term follow‐up for quality of life among those with chronic neck pain. David 1998 (low quality, 51 participants) showed no significant results when comparing mobilisation of the cervical region versus acupuncture at intermediate‐term (RR 1.07, 95% CI 0.48 to 2.35) follow‐up.
Other considerations
Adverse events
When researchers looked at mobilisation and manipulation versus an inactive control, they reported the number of participants experiencing side effects in 9.5% (2/18) of trials. One trial (Cheung Lau 2011) reported no side effects, and another trial (Saavedra‐Hernandez 2012CR) reported benign and transient side effects, including increased neck pain (one in the control group) or increased neck fatigue (one in the intervention group). The rate of rare but serious adverse events such as strokes or serious neurological deficits could not be established from our review data; the power to detect any serious events is too low in these RCTs, and strict RCT procedures might prevent occurrence of such serious complications. When investigators contrasted mobilisation and manipulation against another comparison treatment, they noted that 35% (12/34) of participants experienced adverse events. Ten trials reported benign and transient adverse events for manipulation (Bronfort 2012; Cassidy 1992; Chen 2007; Giles 1999; Haas 2004; Hurwitz 2002; Leaver 2010; Puentedura 2011; Saayman 2011; Shin 2006). Among participants receiving manipulation, 22% (105/469 participants) experienced adverse events. Four trials reported benign and transient adverse events for mobilisation (David 1998; Hurwitz 2002; Leaver 2010; Schomacher 2009). Among participants receiving mobilisation, 11% (42/390 participants) experienced adverse events. All adverse events reported for manipulation or mobilisation were benign and transient and were included for both interventions: increased neck pain, soreness, headache, stiffness, dizziness, nausea, paraesthesia, upper limb pain, fatigue, mid‐lower back pain and "unpleasant change in spinal posture".
Cost of care
The 51 trials included in this review reported no direct measures of the cost of care.
Discussion
Summary of main results
The objective of this literature review was to evaluate the effects of manipulation or mobilisation as a single treatment option versus a control intervention or versus other treatment interventions for neck pain. Review authors found support for use of thoracic manipulation versus control for neck pain, function and quality of life. Results for cervical manipulation and mobilisation versus control were few and diverse. We could not rule out publication bias. Findings suggest that manipulation and mobilisation produce similar results. Multiple cervical manipulation sessions provide slightly better improvement over certain medications such as varied combinations of non‐steroidal anti‐inflammatory drugs (NSAIDs), analgesics, opioids and muscle relaxants. In lieu of serious adverse event risk for manipulation and in the light of evidence suggesting that mobilisation and manipulation produce similar results, further high‐quality research exploring mobilisation is needed.
Overall completeness and applicability of evidence
How do we as meta‐analysts reconcile the various models of care? We noted that use of unimodal approaches was not common in clinical practice, although they are essential elements for teasing out which therapeutic item or combination works best. Typical conservative care takes a more holistic clinical approach and includes a treatment continuum (Jovey 2002) ‐ that is, physical, psychological and pharmacological ‐ starting with treatments that are most available, least expensive and least invasive and that produce the fewest side effects. Our review authors have acknowledged these diversities and have noted the following emerging questions.
How do we know when mobilisations will be effective? This remains unclear, as only two additional trials were discovered by this search. Meta‐analyses, subgroup analyses and sensitivity analyses continue to be hampered by the wide spectrum of comparisons, treatment characteristics and dosages. Until the number of high‐quality studies within individual subgroups of neck pain increases, we will not be able to provide strong conclusions about which groups benefit most from manipulation or mobilisation. Cleland 2007 and Puentedura 2012 developed clinical prediction rules for use of thoracic manipulation in the treatment of neck pain. Similar studies investigating clinical prediction rules for other mobilisations or manipulations in varied neck pain populations would help clinicians to determine when to manual therapy should be utilised.
What is the ideal mobilisation or manipulation?Our review showed that one technique was frequently compared with another in head‐to‐head comparisons of single techniques or combined treatment approaches. The answer to this question remains unclear, but evidence suggests that anterior‐posterior (AP) or posterior‐anterior (PA) mobilisations may be more effective for reducing pain than transverse or rotational mobilisations. We believe that continued research is needed to perform head‐to‐head comparisons between the most viable techniques or approaches.
What is the optimal "dosage"? What are the optimal "clinical parameters" for a given technique category? We still do not know how to answer these questions. Data on pain relief gathered to date reveal that the most commonly reported factors were frequency (total number of sessions) and duration (total number of weeks). We noted that levels of these two factors measured at various follow‐up periods were as follows: manipulation to cervical region alone: one to 18 sessions; one day to nine weeks; manipulation of thoracic region alone: one to 15 sessions; one day to three weeks; mobilisation of cervical region alone: one to six sessions; one day to six weeks. The ideal dosage for cervical manipulation, thoracic manipulation or cervical mobilisation for treatment of cervical pain could not be determined when existing controlled trials were evaluated. Pilot studies of mobilisation and manipulation exploring the minimally effective dose and the optimal dose should be conducted before a larger trial is undertaken. These pilot studies would serve a purpose similar to that of the small dose‐finding studies conducted as part of pharmaceutical trials used to establish a minimally effective dose. One such pilot study (Haas 2004) provided preliminary support for a larger trial assessing 12 sessions and nine sessions over three sessions of cervical manipulation.
A systematic review of adverse events (Carlesso 2010) noted that ascertainment bias may compromise the credibility of current studies. More trials are required to report on adverse events if meta‐analysis is to be useful for obtaining a summary estimate of minor adverse events. Two recent randomised trials have noted that transient minor side effects such as increased treatment soreness are common (Paanalahti 2014; Walker 2013). These studies and one systematic review support the theory that the occurrence of catastrophic events is rare (Carlesso 2010). Vertebrobasilar artery stroke following manipulation is a rare event (Cassidy 2008). Nevertheless, craniocervical arterial dissections as sequelae of cervical manipulation occur and should be managed (Albuquerque 2011; Rushton 2012). Conclusive evidence is lacking for a strong association between neck manipulation and stroke (Haynes 2012), and smaller randomised trials are unlikely to detect rare adverse events. From surveys and review articles, the risk of a serious irreversible complication (e.g. stroke) of cervical manipulations has been reported to vary from one adverse event in 3020 to one in 1,000,000 manipulations (Assendelft 1996; Gross 2002b). Reporting of serious adverse events continues to be required. As emerging literature shows that manipulation and mobilisation are valuable additions to patient care options, new trials are necessary to determine economic and risk advantages derived from using manipulation or mobilisation techniques to treat neck pain.
Quality of the evidence
The overarching limitation noted in this review is that only five of the 51 trials included a sample size of more than 100 participants. Many trials were extremely small (20 to 30 participants). The quality of evidence is strongly limited by the large number of small trials.
The randomisation technique was appropriate and was adequately described in 65% (33/51), and allocation concealment was sufficiently detailed and appropriate in 45% (23/51) of studies. These criteria are important for minimising selection bias, so that treatment is applicable to the general population. Without rates of randomisation and allocation concealment, it is unclear whether groups had baseline comparability, and whether study results are applicable to the general patient population.
Many biases (detection and performance biases) are inherent in trials and tend to overestimate the trial effect. A dominant bias in the studies included in this review was lack of blinding of participants (45/51) and therapists (100%). Blinding is difficult to perform in a randomised controlled trial examining manipulation or mobilisation versus control. Blinding of both participants and therapists minimises performance bias as the result of differences in actual treatment provided to groups and expectations of treatment. Given lack of blinding of participants and therapists, it is important to blind outcome assessors to ensure that no detection bias is present; however, only 12% of studies (6/51) blinded the assessor. This occurred in large part because many of the assessors were actually the participants themselves as required by the outcome measures (Neck Disability Index (NDI), visual analogue scale (VAS), Short Form (SF)‐36) used in various trials. Researchers can minimise this bias by integrating observer‐based outcomes, especially those pertaining to function and disability. Many pain trials use self reported outcomes; this makes it hard to protect against detection bias. Similarly, if one is to conclude that treatment effects in fact were due to the intervention, thereby reducing performance bias, it is important to avoid co‐interventions. Thirty‐one per cent (16/51) of the included studies explicitly avoided co‐interventions. Based on the relatively short nature of physiotherapeutic interventions, it would be crucial to avoid co‐interventions that otherwise may confound study results. Timing of outcome assessments is one of the dominant flaws leading to overestimation of the effects of care. In 37% (19/51) of trials, outcomes were assessed for single‐session trials, resulting in overestimation of the treatment effect size.
As this review is examining manipulation or mobilisation versus an inactive control or an active treatment, compliance with treatment must be evaluated if strong conclusions are to be provided. Of the 51 trials included in our review, compliance was monitored and acceptable in 45% (23/51). To ensure compliance, investigators had to track how often the participant came into the clinic to receive manipulation or mobilisation, and whether the participant received any other treatment during the entire length of the study. The most common method of tracking a patient’s treatment schedule is by using a diary. This method was rarely reported in the included trials.
Our group has observed three positive advances in recent years. Trials have become larger, have demonstrated lower risk of bias (20/51) and have used self reported ratings (e.g. pain, disability self report questionnaires, global perceived effect) as primary outcomes on a more consistent basis.
Most of our 51 trials were conducted immediately post treatment. With no long‐term follow‐up studies, it is hard for therapists to make a judgement in terms of using a particular technique in their practice. Single‐session trials using manipulation are few. Many of the benefits of a single manipulation are neurophysiological. Future investigators need to look at the optimal dosage to maximise the effects of manipulation or mobilisation. The very low to low quality of evidence for cervical manipulation and the moderate quality of evidence for thoracic manipulation in treating neck pain can leave a professional therapist with a level of uncertainty. The relevance of the evidence remains in question because (1) participants in manual therapy trials are not blinded as a result of the nature of the intervention being delivered; and (2) primary outcome measures are often self reported (i.e. pain), causing the participant to technically become ‘the outcome assessor’ who is not blinded to previous measures.
Potential biases in the review process
We used two independent review authors who were trained in the process and employed standardised forms. The effectiveness of this strategy was confirmed by strong agreement (kappa analysis) between review authors. We further attempted to limit systematic error by searching for both published and unpublished literature. Randomised controlled trials often go unpublished if they do not yield positive results. Searching the grey literature makes the results of systematic reviews more comprehensive.
Selection bias was avoided for citation screening and full‐text screening, as each phase was conducted in duplicate and with fair to good agreement. Language bias was avoided to the extent of including all languages during study selection; however, we did not search non‐English databases (i.e. Chinese databases). In this update, we captured one non‐English trial (Mansilla‐Ferragud 2008). It is also important to analyse the risks inherent in and the limitations of our systematic review update. A sweeping literature search is important for obtaining the full spectrum of results of applying manipulation or mobilisation for neck pain. Accordingly, it is important that an effort be made to search multiple language‐based databases.
In our grey literature search, one non‐published thesis (Khoury 2002) was uncovered but did not meet our selection criteria. Publication bias cannot be ruled out. The asymmetrical appearance of the funnel plot (see Figure 3) suggests the presence of publication bias. Publication bias was a matter of concern during the systematic review process. Many study authors tend to submit only trials with positive results for publication in peer‐reviewed journals. This can lead to overestimation of results. Fewer than 10 trials were included in each plot, further reducing the meaning of these data. Additionally, nine of 13 trials listed as ongoing trials (those conducted longer than five years ago) conducted during the period from 1995 to 2010 (Groeneweg 2010; Gudavalli 2006;Guerriero 1997; Kjellman 1997;Nagy 2000;Scott‐Dawkins 1997;Shammsuddin 2010; Stokke 1995;Tanaka 1995) may further support the notion of publication bias, especially if a “worse‐case scenario” that all trials are negative is considered. As we know, many negative trials never reach publication. Note that we did search the Internet and databases for all trials included in the ’ongoing’ list, and we wrote to each study author but received no response.
Sources of random error were limited by use of two independent review authors who used a standardised tool during the data extraction process. Reliability of the risk of bias tool was assessed by Graham 2012 for the Cervical Overview Group (COG) and was considered acceptable. Last, we predetermined our primary and secondary outcomes; this limited the random error associated with accepting articles that discussed a broad variety of outcomes.
Future updates of our review could benefit from addressing a diverse range of factors that may help to reduce systematic error. It may be appropriate, for example, to examine the pattern of results based on country of origin, and to explore why this pattern exists. Additional possibilities include examining results on the basis of therapist experience or provision of primary care as opposed to secondary care. Pooling of results according to type of neck disorder and length of injury may or may not be important for the magnitude of effects. Furthermore, risk of time lag bias means that positive trials may be published faster than negative trials. It is important to search the grey literature to find all trials. Future updates will be more informative if review authors can identify a greater number of trials related to the topic under review. Last, in the future, we must scrutinise studies on the basis of conflicts of interest due to funding from donors.
Agreements and disagreements with other studies or reviews
For acute whiplash‐associated disorder (WAD), we retrieved no evidence (0 trials; Shaw 2010). Although we assessed 15 trials on WAD, we found no trials that reported on mobilisation or manipulation provided as a single stand‐alone therapy compared with inactive treatment or other treatment interventions. For subacute WAD, weak evidence favoured manipulation in the short term; concerns regarding the rigor of methods used were noted (weak quality, one trial; Teasell 2010). Our findings are consistent with this evidence.
For cervical radiculopathy, no evidence was found on manipulation or mobilisation compared with inactive treatment. However, we found one trial (Ragonese 2009) suggesting that mobilisation alone is equal to exercise alone at short‐term follow‐up for pain. This very low quality of evidence statement is consistent with findings of the Thoomes 2013 systematic review on all forms of intervention for cervical radiculopathy.
For people with acute, subacute and chronic neck pain, manipulation more effectively reduced pain immediately following treatment when contrasted with inactive treatment (low to moderate quality, four trials; Clar 2014; Furlan 2012). Posadzki 2011 (one trial) compared one osteopathic manipulation versus a sham ultrasound and reported significant longitudinal change for individuals with chronic neck pain. We found eight trials assessing non‐specific neck pain and suggesting that a single manipulation reduces pain more effectively immediately post treatment or in the short term compared with a control. We suggest that evidence continues to be of lowor very lowquality, as trial results could not be pooled. Furthermore, when we compared the effectiveness of several sessions of manipulation versus several sessions of mobilisation, we found high‐ to moderate‐quality evidence showing that these two manual therapy interventions are equally effective in improving pain, function, quality of life, patient satisfaction and global perceived effect. These findings are consistent with those of the Neck Pain Task Force review (Hurwitz 2008) and Furlan 2012 systematic review. We found moderate‐quality evidence suggesting that manipulation is superior to medication (NSAIDs and analgesics) for pain relief at immediate‐, intermediate‐ and long‐term follow‐up based on findings of a large trial (Bronfort 2012) and two smaller trials (Giles 1999; Madson 2010). Our findings contrast with those of Furlan 2012, who concluded that manipulations are similar to medication in providing pain relief at short‐term follow‐up.
We agree with Scholten Peeters 2013 and Walser 2009 that thoracic manipulation is beneficial when contrasted with a placebo intervention, but we noted no differences from other treatment. We found one trial that favoured cervical manipulation over thoracic manipulation (Puentedura 2011) and two trials that showed thoracic manipulation to be equally effective when compared with thoracic mobilisation (Sillevis 2010) and with exercise (Savolainen 2004). The findings of Huisman 2013 were comparable with our own.
For participants with acute/subacute or chronic or mixed non‐specific neck pain, mobilisation reduced pain when contrasted with no treatment (low quality, three trials; Furlan 2012). However, no difference in chronic non‐specific neck pain was noted when mobilisation was contrasted with placebo (low quality, one trial; Furlan 2012). Contrary to this finding, our review found two trials (57 participants) provided low‐ or very low‐quality evidence showing no pain relief. Finally, we found that certain forms of mobilisation (AP) are superior to other forms (rotatory or transversal mobilisation) for providing pain relief at immediate follow‐up. To our knowledge, no other systematic review has reported this very low level of evidence finding.
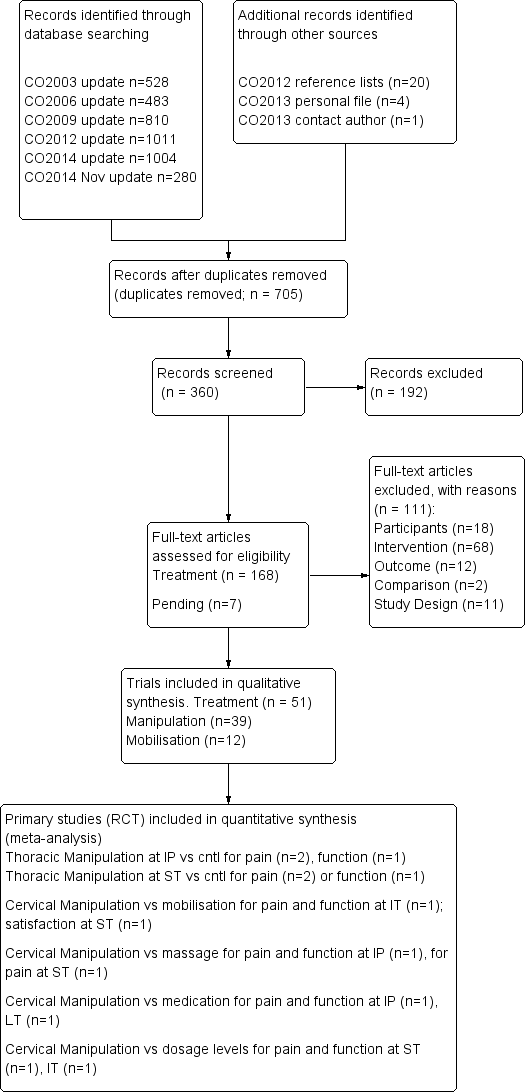
PRISMA diagram for manipulation and mobilisation.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
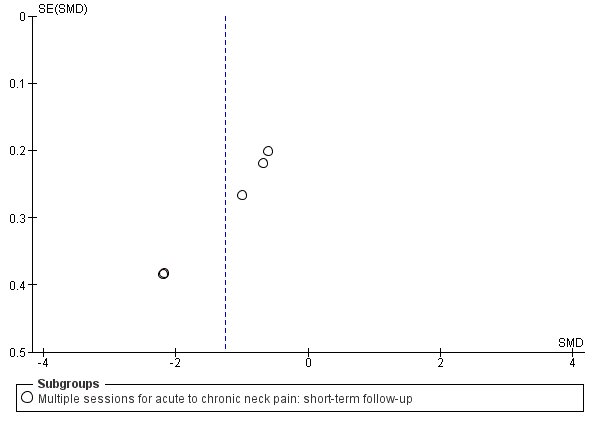
Funnel plot of comparison: manipulation vs control, outcome: FUNNEL PLOT for PAIN: thoracic manipulation vs same treatment in both arms.

Forest plot of comparison: manipulation vs another treatment, outcome: PAIN: cervical manipulation vs medicine.

Forest plot of comparison: manipulation vs another treatment, outcome: PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up.
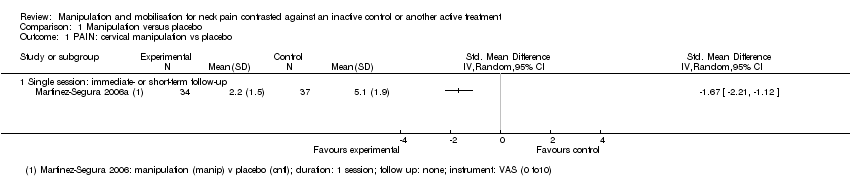
Comparison 1 Manipulation versus placebo, Outcome 1 PAIN: cervical manipulation vs placebo.

Comparison 1 Manipulation versus placebo, Outcome 2 PAIN: thoracic manipulation vs placebo.
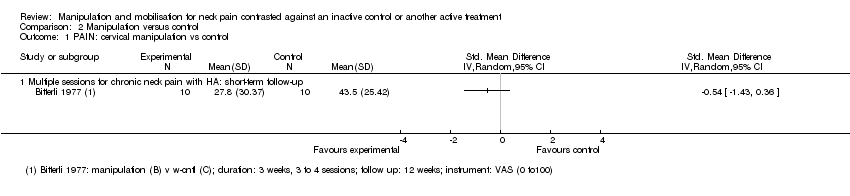
Comparison 2 Manipulation versus control, Outcome 1 PAIN: cervical manipulation vs control.

Comparison 2 Manipulation versus control, Outcome 2 PAIN: cervical manipulation plus treatment vs same treatment in both arms.

Comparison 2 Manipulation versus control, Outcome 3 PAIN: cervical manipulation vs same treatment in both arms.

Comparison 2 Manipulation versus control, Outcome 4 PAIN: thoracic manipulation vs control.

Comparison 2 Manipulation versus control, Outcome 5 PAIN: thoracic manipulation vs same treatment in both arms.
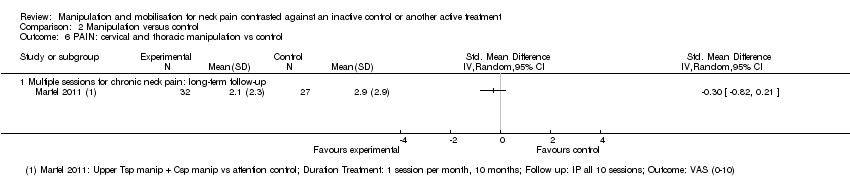
Comparison 2 Manipulation versus control, Outcome 6 PAIN: cervical and thoracic manipulation vs control.

Comparison 2 Manipulation versus control, Outcome 7 FUNCTION: thoracic manipulation vs same treatment in both arms.
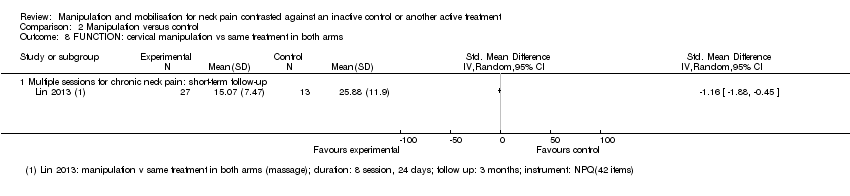
Comparison 2 Manipulation versus control, Outcome 8 FUNCTION: cervical manipulation vs same treatment in both arms.

Comparison 2 Manipulation versus control, Outcome 9 FUNCTION: cervical and thoracic manipulation vs control.

Comparison 2 Manipulation versus control, Outcome 10 QUALITY OF LIFE: thoracic manipulation vs control.

Comparison 2 Manipulation versus control, Outcome 11 FUNNEL PLOT for pain: thoracic manipulation vs same treatment in both arms.
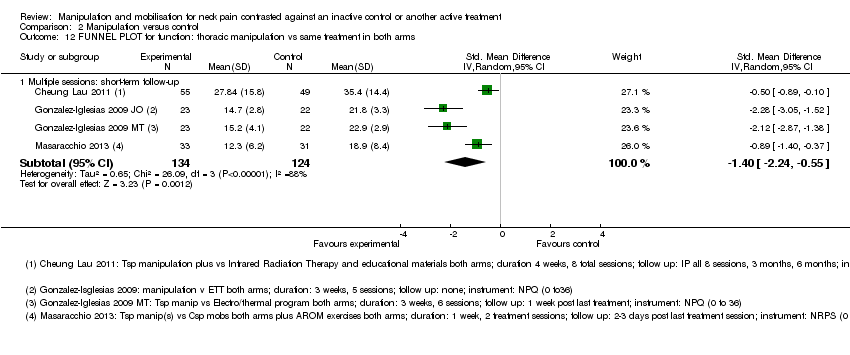
Comparison 2 Manipulation versus control, Outcome 12 FUNNEL PLOT for function: thoracic manipulation vs same treatment in both arms.

Comparison 3 Mobilisation versus control, Outcome 1 PAIN: cervical mobilisation vs control.
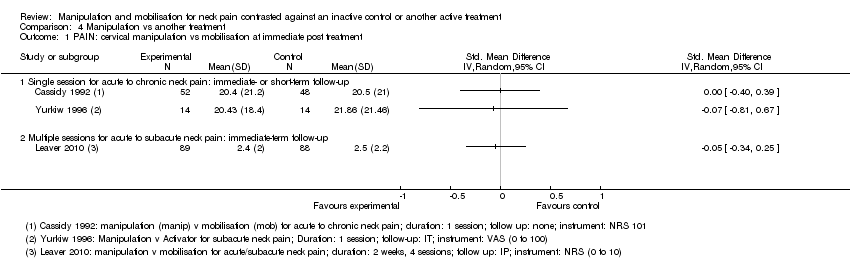
Comparison 4 Manipulation vs another treatment, Outcome 1 PAIN: cervical manipulation vs mobilisation at immediate post treatment.

Comparison 4 Manipulation vs another treatment, Outcome 2 PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up.
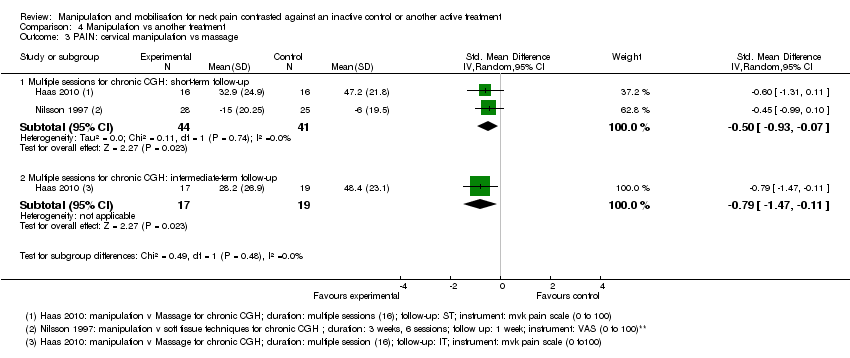
Comparison 4 Manipulation vs another treatment, Outcome 3 PAIN: cervical manipulation vs massage.

Comparison 4 Manipulation vs another treatment, Outcome 4 PAIN: cervical manipulation vs medicine.

Comparison 4 Manipulation vs another treatment, Outcome 5 PAIN: cervical manipulation vs exercise.

Comparison 4 Manipulation vs another treatment, Outcome 6 PAIN: cervical manipulation vs electrotherapy.
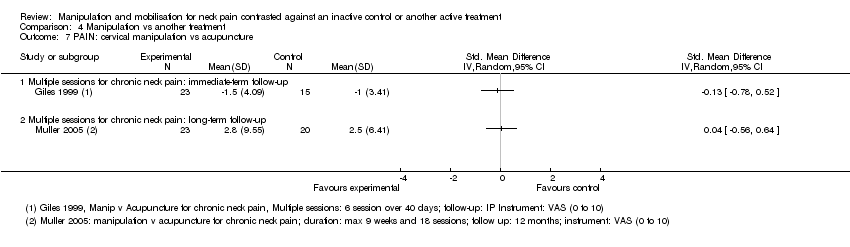
Comparison 4 Manipulation vs another treatment, Outcome 7 PAIN: cervical manipulation vs acupuncture.
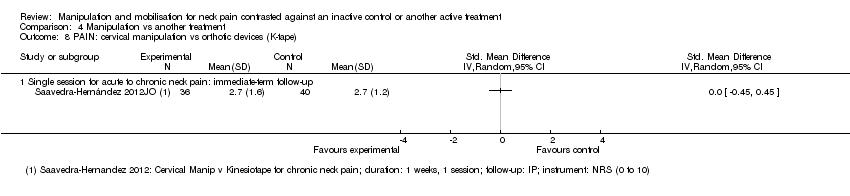
Comparison 4 Manipulation vs another treatment, Outcome 8 PAIN: cervical manipulation vs orthotic devices (K‐tape).
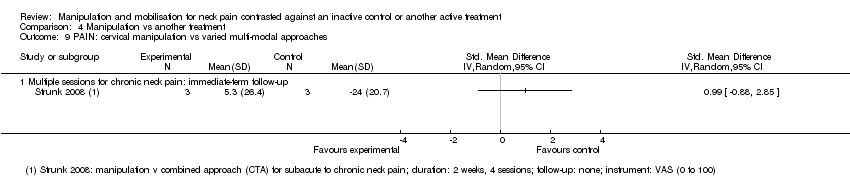
Comparison 4 Manipulation vs another treatment, Outcome 9 PAIN: cervical manipulation vs varied multi‐modal approaches.
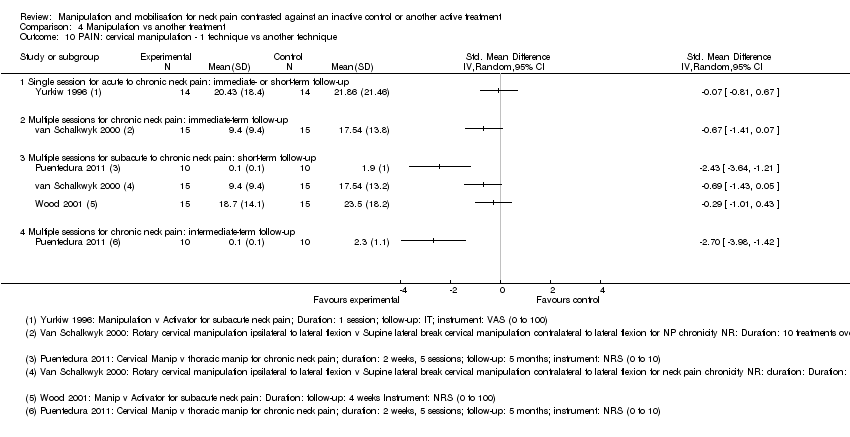
Comparison 4 Manipulation vs another treatment, Outcome 10 PAIN: cervical manipulation ‐ 1 technique vs another technique.
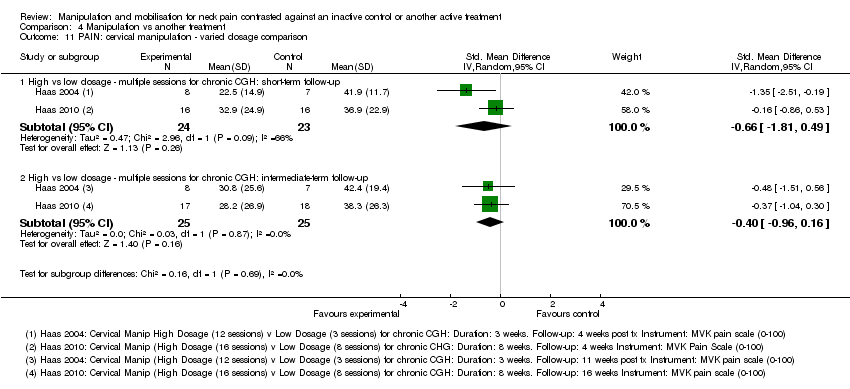
Comparison 4 Manipulation vs another treatment, Outcome 11 PAIN: cervical manipulation ‐ varied dosage comparison.

Comparison 4 Manipulation vs another treatment, Outcome 12 PAIN: thoracic manipulation vs exercise.

Comparison 4 Manipulation vs another treatment, Outcome 13 FUNCTION: cervical manipulation vs mobilisation.
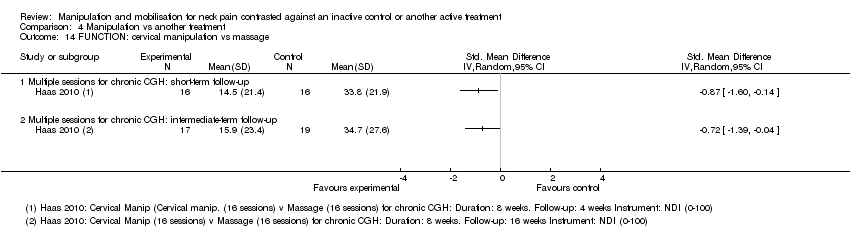
Comparison 4 Manipulation vs another treatment, Outcome 14 FUNCTION: cervical manipulation vs massage.
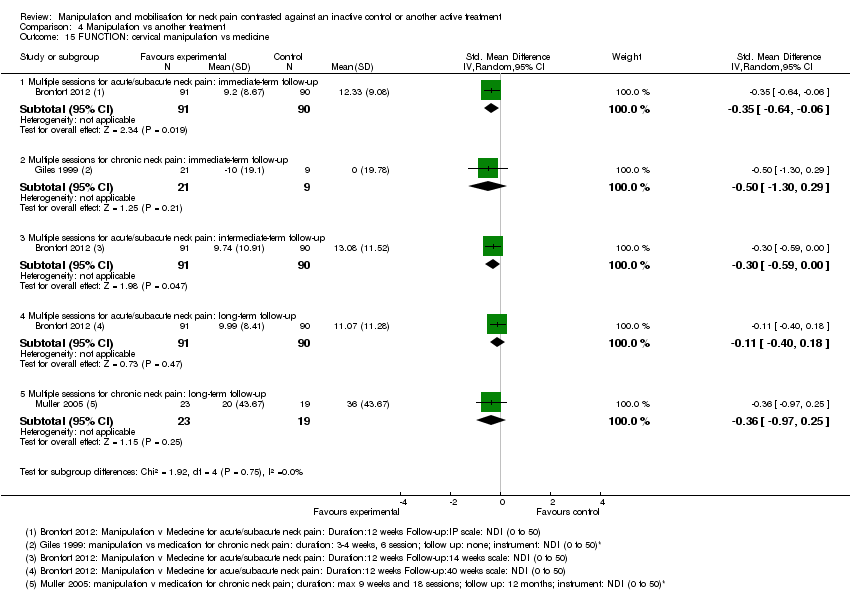
Comparison 4 Manipulation vs another treatment, Outcome 15 FUNCTION: cervical manipulation vs medicine.

Comparison 4 Manipulation vs another treatment, Outcome 16 FUNCTION: cervical manipulation vs exercise.

Comparison 4 Manipulation vs another treatment, Outcome 17 FUNCTION: cervical manipulation vs orthotic devices (K‐taping).

Comparison 4 Manipulation vs another treatment, Outcome 18 FUNCTION: cervical manipulation vs acupuncture.

Comparison 4 Manipulation vs another treatment, Outcome 19 FUNCTION: cervical manipulation vs varied multi‐modal approaches.

Comparison 4 Manipulation vs another treatment, Outcome 20 FUNCTION: cervical manipulation ‐ 1 technique vs another technique.

Comparison 4 Manipulation vs another treatment, Outcome 21 FUNCTION: cervical manipulation ‐ varied dosage comparison.
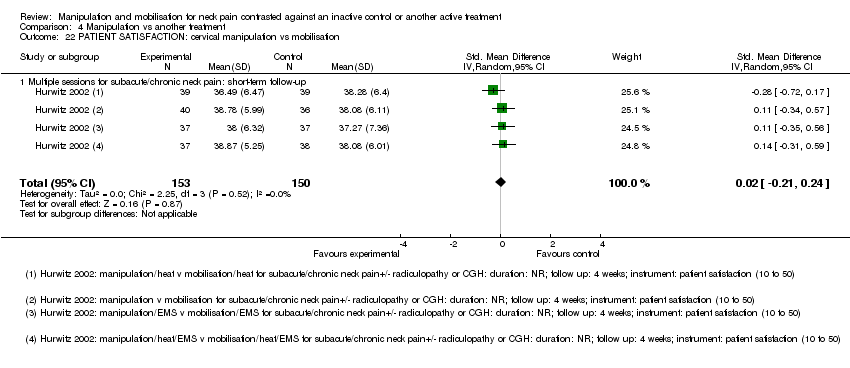
Comparison 4 Manipulation vs another treatment, Outcome 22 PATIENT SATISFACTION: cervical manipulation vs mobilisation.

Comparison 4 Manipulation vs another treatment, Outcome 23 PATIENT SATISFACTION: cervical manipulation vs varied multi‐modal approaches.
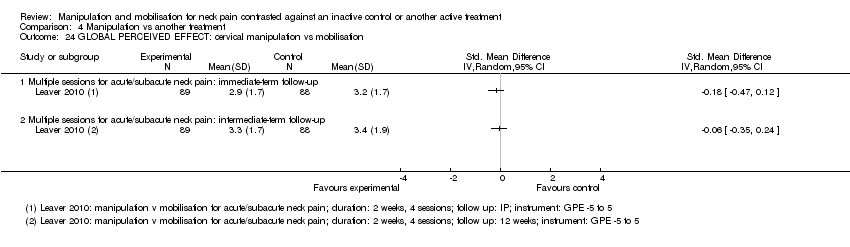
Comparison 4 Manipulation vs another treatment, Outcome 24 GLOBAL PERCEIVED EFFECT: cervical manipulation vs mobilisation.
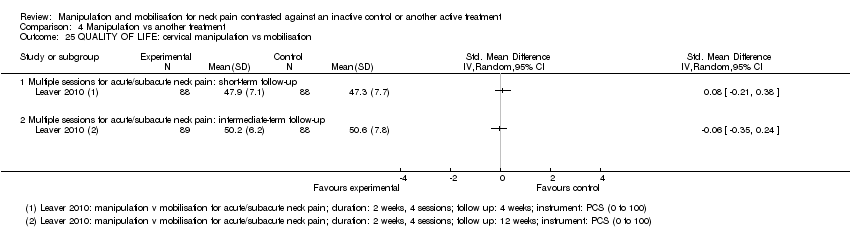
Comparison 4 Manipulation vs another treatment, Outcome 25 QUALITY OF LIFE: cervical manipulation vs mobilisation.

Comparison 4 Manipulation vs another treatment, Outcome 26 QUALITY OF LIFE: cervical manipulation vs medicine.

Comparison 4 Manipulation vs another treatment, Outcome 27 QUALITY OF LIFE: cervical manipulation vs exercise.
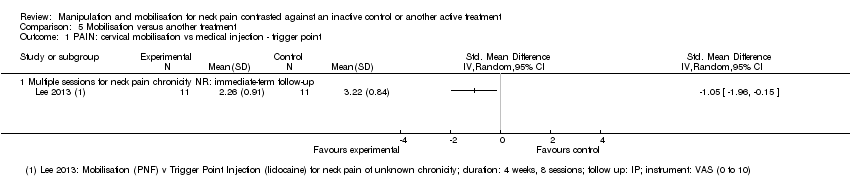
Comparison 5 Mobilisation versus another treatment, Outcome 1 PAIN: cervical mobilisation vs medical injection ‐ trigger point.
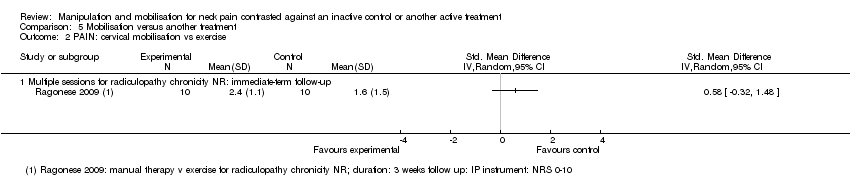
Comparison 5 Mobilisation versus another treatment, Outcome 2 PAIN: cervical mobilisation vs exercise.
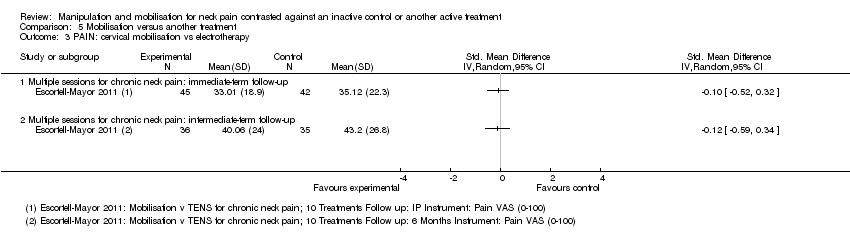
Comparison 5 Mobilisation versus another treatment, Outcome 3 PAIN: cervical mobilisation vs electrotherapy.

Comparison 5 Mobilisation versus another treatment, Outcome 4 PAIN: cervical mobilisation vs sonic devices ‐ ultrasound, shock wave therapy.

Comparison 5 Mobilisation versus another treatment, Outcome 5 PAIN: cervical mobilisation vs mechanical traction.

Comparison 5 Mobilisation versus another treatment, Outcome 6 PAIN: cervical mobilisation vs acupuncture.

Comparison 5 Mobilisation versus another treatment, Outcome 7 PAIN: cervical mobilisation vs varied multi‐modal approaches.

Comparison 5 Mobilisation versus another treatment, Outcome 8 PAIN: cervical mobilisation ‐ 1 technique vs another technique.

Comparison 5 Mobilisation versus another treatment, Outcome 9 PAIN: cervical mobilisation ‐ 1 technique vs another technique.

Comparison 5 Mobilisation versus another treatment, Outcome 10 PAIN: cervical mobilisation vs massage.

Comparison 5 Mobilisation versus another treatment, Outcome 11 FUNCTION: cervical mobilisation vs medical injection ‐ trigger point.

Comparison 5 Mobilisation versus another treatment, Outcome 12 FUNCTION: cervical mobilisation vs exercise.
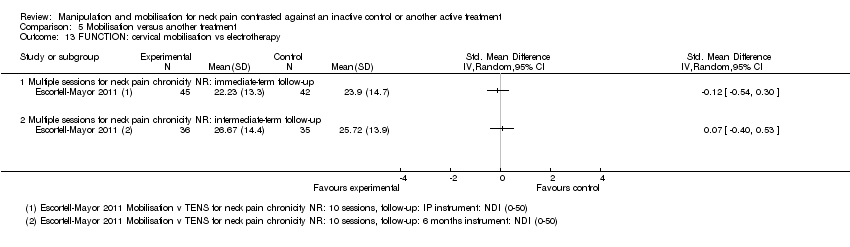
Comparison 5 Mobilisation versus another treatment, Outcome 13 FUNCTION: cervical mobilisation vs electrotherapy.

Comparison 5 Mobilisation versus another treatment, Outcome 14 FUNCTION: cervical mobilisation vs sonic devices ‐ shock wave therapy.

Comparison 5 Mobilisation versus another treatment, Outcome 15 FUNCTION: cervical mobilisation vs acupuncture.

Comparison 5 Mobilisation versus another treatment, Outcome 16 FUNCTION: cervical mobilisation vs varied multi‐modal approaches.

Comparison 5 Mobilisation versus another treatment, Outcome 17 FUNCTION: cervical mobilisation vs massage.

Comparison 5 Mobilisation versus another treatment, Outcome 18 FUNCTION: cervical mobilisation ‐ 1 technique vs another technique.
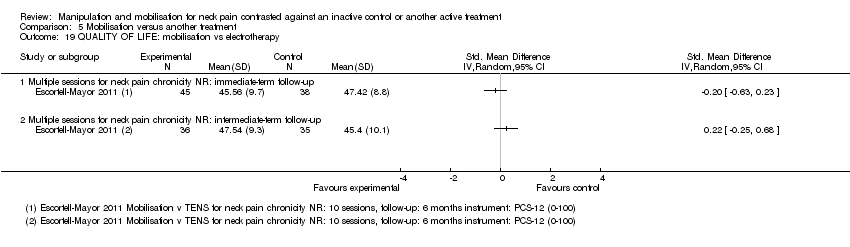
Comparison 5 Mobilisation versus another treatment, Outcome 19 QUALITY OF LIFE: mobilisation vs electrotherapy.

Comparison 5 Mobilisation versus another treatment, Outcome 20 PATIENT SATISFACTION: cervical mobilisation vs varied multi‐modal approaches.
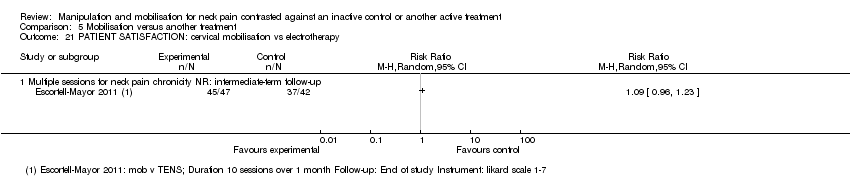
Comparison 5 Mobilisation versus another treatment, Outcome 21 PATIENT SATISFACTION: cervical mobilisation vs electrotherapy.
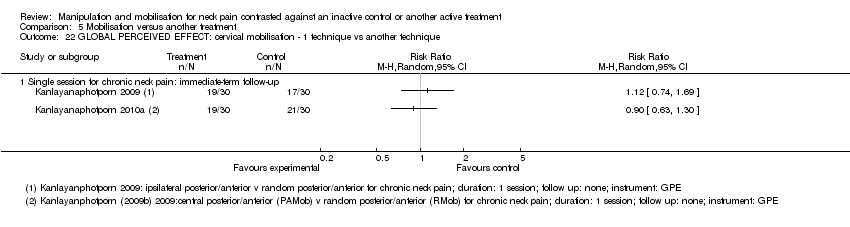
Comparison 5 Mobilisation versus another treatment, Outcome 22 GLOBAL PERCEIVED EFFECT: cervical mobilisation ‐ 1 technique vs another technique.
| Manipulation (cervical) compared with oral medicine for acute/subacute neck pain | ||||
| Patient or population: patients with acute and subacute neck pain Settings: outpatient clinics, ambulatory care services Intervention: manipulation of cervical region ‐ multiple sessions Comparison: oral medicine ‐ varied combinations of non‐steroidal anti‐inflammatory drugs (NSAIDs), analgesics, opioid analgesics and muscle relaxants | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD ‐0.21 (‐0.5 to 0.08) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD ‐0.32 (‐0.61 to ‐0.02) | 181 | ⊕⊕⊕⊝ Moderatea | Pain reduction favouring manipulation over medication |
| FUNCTION | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD ‐0.30 (‐0.59 to ‐0.00) | 182 | ⊕⊕⊕⊝ Moderatea | Functional improvement favouring manipulation over medication |
| Acute and subacute neck pain Long‐term follow‐up | SMD ‐0.11 (‐0.40 to 0.18)
| 181 | ⊕⊕⊕⊝ Moderatea | No significant difference between groups |
| PARTICIPANT SATISFACTION | ||||
| Acute and subacute neck pain Long‐term follow‐up | Not estimable | 182 | ⊕⊕⊕⊝ Moderatea | Manipulation favoured over medication |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD 0.22 (‐0.07 to 0.51) | 181 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: 0.19 (‐0.10 to 0.49) | 181 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Moderate‐quality evidence suggests that multiple sessions of cervical manipulation are more effective than medication (analgesics and non‐steroidal anti‐inflammatory drugs (NSAIDs)) for improving pain at immediate‐term and long‐term follow‐up (1 trial; 181 participants); function at intermediate term and satisfaction over the long term. Quality of life was similar between groups (1 trial, 182 participants) at intermediate‐ and long‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. | ||||
| aIndirectness: ‐1; a second independent trial is needed to clarify emerging data. | ||||
| Manipulation (thoracic) compared with inactive control for neck pain | ||||
| Patient or population: patients with acute, subacute and chronic neck pain Settings: outpatient clinics, ambulatory care services Intervention: manipulation of thoracic region ‐ multiple sessions Comparison: inactive control | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD pooled ‐1.46 (‐2.20 to ‐0.71) | 242 Fernandez 2004 JWRD; Fernandez 2009; Gonzalez‐Iglesias 2009 JO; | ⊕⊕⊕⊝ Moderatea | Favoured treatment; NNTB: 4 to 7; magnitude of effect: medium |
| Chronic neck pain Intermediate‐term follow‐up | SMD ‐0.64 (‐1.04 to ‐0.25) | 111 | ⊕⊕⊝⊝ Lowb,c | Favoured treatment; NNTB 4; magnitude of effect: small |
| FUNCTION | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD pooled ‐1.73 (‐2.68 to ‐0.78) | 258 | ⊕⊕⊕⊝ Moderatea | Favoured treatment; NNTB 4 to 5; magnitude of effect: medium |
| Chronic neck pain Short‐term follow‐up | SMD ‐0.50 (‐0.89 to ‐0.10) | 111 | ⊕⊕⊝⊝ Lowb,c | Favoured treatment; NNTB 5; magnitude of effect: small |
| Chronic neck pain Intermediate‐term follow‐up | SMD ‐0.38 (‐0.77 to 0.01) | 111 (1 trial; Cheung Lau 2011) | ⊕⊕⊝⊝ Lowb,c | Favoured treatment; NNTB 5; magnitude of effect: small |
| QUALITY OF LIFE (QoL) | ||||
| Chronic neck pain Short‐term follow‐up | SMD ‐0.82 (‐1.23 to ‐0.42) | 111 | ⊕⊕⊝⊝ Lowb,c | Favoured treatment |
| Chronic neck pain Intermediate‐term follow‐up | SMD ‐0.61 (‐1.01 to ‐0.22) | 111 | ⊕⊕⊝⊝ Lowc | Favoured treatment |
| Seven trials (428 participants) using multiple sessions of thoracic manipulation for acute to chronic neck pain were assessed at 3 time intervals. At short‐term follow‐up, moderate‐quality evidence favoured thoracic manipulation for pain reduction among participants with acute/subacute neck pain, and with acute to chronic neck pain, it improved function. These findings were consistent but small at intermediate follow‐up for pain, function and quality of life (low‐quality evidence). | ||||
| GRADE Working Group grades of evidence. | ||||
| bIndirectness: ‐1, immediate post‐treatment data have limited clinical relevance; single trials with only immediate‐ and short‐term follow‐up are downgraded (ceiling effect) because future research is likely to have an important impact on the direction of the reported effect, and a second independent trial is needed to clarify emerging short‐term data. cImprecision: ‐1, small sample size. aInconsistency: P value = 0.002; I² = 84%; sensitivity analysis: Statistical differences led us to explore heterogeneity by the following PICO factors: P: about the same; I: about the same; C: about the same; O: for pain, VAS, NPRS; for disability, NPQ, NDI; RoB: most often low RoB but when the trial of high RoB is removed, pooled SMD increases to ‐2.18 (‐2.71 to ‐1.65) for pain, but these data were derived from trials conducted in the same lab. | ||||
| Manipulation compared with mobilisation for neck pain | ||||
| Patient or population: patients with acute, subacute and chronic neck pain Settings: ambulatory care or outpatient clinic Intervention: manipulation of cervical region ‐ multiple sessions Comparison: mobilisation | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute, subacute and chronic neck pain Intermediate‐term follow‐up | MD pooled ‐0.07 (‐0.72 to 0.59) | 446 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| FUNCTION AND DISABILITY | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD: ‐0.06 (‐0.35 to 0.24) | 176 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| Acute, subacute and chronic neck pain Intermediate‐term follow‐up | SMD pooled: 0.10 (‐0.18 to 0.37)
| 446 | ⊕⊕⊕⊕ High | No significant differences between groups |
| PARTICIPANT SATISFACTION | ||||
| Subacute and chronic neck pain Short‐term follow‐up | SMD: ‐0.02 (‐0.21 to 0.24) | 269 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| GLOBAL PERCEIVED EFFECT | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.06 | 177 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD: 0.08 (‐0.21 to 0.38) | 176 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.06 (‐0.35 to 0.24) | 177 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| Moderate‐ to high‐quality evidence (2 trials, 446 participants) suggests that multiple sessions of cervical manipulation produced similar changes in pain, function, quality of life, global perceived effect and patient satisfaction when compared with multiple sessions of cervical mobilisation at immediate‐, short‐ and intermediate‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. | ||||
| aInconsistency: ‐1. bIndirectness: ‐1. | ||||
| Manipulation compared with exercise for neck pain | ||||
| Patient or population: patients with acute and subacute neck pain Settings: ambulatory care or outpatient clinic setting Intervention: manipulation of cervical region Comparison: exercise | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.16 (‐0.45 to 0.13) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: 0.06 (‐0.23 to 0.35) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| FUNCTION | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.01 (‐0.30 to 0.28)
| 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: ‐0.02 (‐0.31 to 0.27)
| 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| PARTICIPANT SATISFACTION | ||||
| Acute and subacute neck pain Long‐term follow‐up | Not estimable | 182 | ⊕⊕⊕⊝ Moderatea | Improvement in participant satisfaction for manipulation over exercise |
| GLOBAL PERCEIVED EFFECT | ||||
| Acute and subacute neck pain Immediate post‐treatment follow‐up | Not estimable | 182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.05 (‐0.35 to 0.24) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: 0.0 (‐0.29 to 0.29) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Moderate‐quality evidence suggests no differences in pain, function, global perceived effect and quality of life when multiple sessions of cervical manipulation are compared with exercise at immediate‐, intermediate‐ and long‐term follow‐up. Moderate‐quality evidence indicates that use of cervical manipulation led to greater participant satisfaction when compared with an exercise programme at long‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. | ||||
| aIndirectness: ‐1. | ||||
| High dose of manipulation compared with low dose of manipulation for chronic neck pain | ||||
| Patient or population: patients with chronic neck pain with cervicogenic headache (CGH) Settings: ambulatory care or outpatient clinic setting Intervention: manipulation of cervical region Comparison: high dose vs low dose | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Chronic neck pain and CGH Intermediate‐term follow‐up | SMD pooled: ‐0.40 (‐0.96 to 0.16)
| ⊕⊕⊕⊝ Moderatea | Two trials showed no significant differences between groups | |
| FUNCTION | ||||
| Chronic neck pain and CGH Intermediate‐term follow‐up | SMD pooled: ‐0.61 (‐1.38 to 0.17) | ⊕⊕⊕⊝ Moderatea | Two trials showed no significant differences between groups | |
| Moderate‐quality evidence shows that high‐dose (12 to 18 sessions) contrasted against low‐dose (3 to 8 sessions) cervical manipulation produced similar changes in pain and function at intermediate‐term follow‐up for individuals with chronic neck pain with cervicogenic headache. | ||||
| GRADE Working Group grades of evidence. | ||||
| aImprecision: ‐1. | ||||
| Term | Definiton |
| Per cent treatment advantage (%) | Calculation of the clinically important difference or change in a per cent scale was estimated as follows. Karlberg 1996 data are used in this example. % improvement (control) equals the difference between the change in the control group (1) divided by the control baseline (56), which equals 1.8%. Treatment advantage = 42.6% ‐ 1.8% = 40.8% |
| Number needed to treat (NNTB) | For this example, Karlberg 1996 outcomes measured at short‐term follow‐up are used to derive the data. Number needed to treat is the number of patients a clinician needs to treat to achieve a clinically important improvement in 1. If we assume the minimal clinically important difference to be 10% of the baseline mean in the control group, and the control group mean at baseline is 56, then 10% of 56 is 5.6 The effect is baseline ‐ final value; therefore:
Converting these to standard normal values means that:
NNTB = 1 divided by the difference in areas under the normal curve (experimental group ‐ control group):
|
| Author/Comparison | NNTB | Advantage, % |
| PAIN | ||
| Haas 2004: pain | 12 (clinically important pain reduction) at ST | 23 |
| Haas 2010: pain | 4 (clinically important pain reduction) at IT | 29 |
| Cleland 2005 | 5 (clinically important pain reduction) | 29 |
| Cheung Lau 2011: pain | 4 (clinically important pain reduction) | |
| Fernandez 2004a | Unable to calculate because baseline data not reported | |
| Gonzalez‐Iglesias 2009 | 7 (clinically important pain reduction) | 47 |
| Martinez‐Segura 2006, | 2 (clinically important pain reduction) | 54 |
| Massaracchio 2013: pain | 4 (clinically important pain reduction) | |
| von Piekartz 2011: pain | 2 (clinically important pain reduction) at IT | |
| FUNCTION | ||
| Cheung Lau 2011: function | 5 (clinically important functional improvement) at IT | |
| Gonzalez‐Iglesias 2009 | 5 (clinically important functional improvement) | 41 |
| Haas 2010: function | 5 (clinically important functional improvement) at ST and IT | ST: 41 IT: 39 |
| Massaracchio 2013: function | 4 (clinically important functional improvement) | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical manipulation vs placebo Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Single session: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: thoracic manipulation vs placebo Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Single session: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Multiple sessions for chronic neck pain with HA: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical manipulation plus treatment vs same treatment in both arms Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Single session for subacute/chronic neck pain: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 PAIN: cervical manipulation vs same treatment in both arms Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Single session for subacute/chronic neck pain with radicular findings and HA: short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 PAIN: thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Single session for neck pain of not reported duration: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: thoracic manipulation vs same treatment in both arms Show forest plot | 8 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Multiple sessions for acute neck pain: immediate‐term follow‐up | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐3.46 [‐4.13, ‐2.79] |
| 5.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐1.15, 0.69] |
| 5.3 Single session for chronic neck pain: short‐term follow‐up | 1 | 82 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.36, 0.51] |
| 5.4 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 4 | 242 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.46 [‐2.20, ‐0.71] |
| 5.5 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐0.99, ‐0.20] |
| 5.6 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.04, ‐0.25] |
| 6 PAIN: cervical and thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 FUNCTION: thoracic manipulation vs same treatment in both arms Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.85, ‐0.18] |
| 7.2 Single session for chronic neck pain: short‐term follow‐up | 1 | 81 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.61, 0.27] |
| 7.3 Multiple sessions for acute neck pain: short‐term follow‐up | 3 | 154 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.73 [‐2.68, ‐0.78] |
| 7.4 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.89, ‐0.10] |
| 7.5 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.77, 0.01] |
| 8 FUNCTION: cervical manipulation vs same treatment in both arms Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 FUNCTION: cervical and thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 QUALITY OF LIFE: thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 FUNNEL PLOT for pain: thoracic manipulation vs same treatment in both arms Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 Multiple sessions for acute to chronic neck pain: short‐term follow‐up | 5 | 346 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.26 [‐1.86, ‐0.66] |
| 12 FUNNEL PLOT for function: thoracic manipulation vs same treatment in both arms Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Multiple sessions: short‐term follow‐up | 4 | 258 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.40 [‐2.24, ‐0.55] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical mobilisation vs control Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Single session: intermediate post treatment | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Multiple sessions: short‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical manipulation vs mobilisation at immediate post treatment Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Single session for acute to chronic neck pain: immediate‐ or short‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Multiple sessions for acute to subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Multiple sessions for acute to chronic neck pain: intermediate‐term follow‐up | 2 | 446 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.72, 0.59] |
| 3 PAIN: cervical manipulation vs massage Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Multiple sessions for chronic CGH: short‐term follow‐up | 2 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.93, ‐0.07] |
| 3.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.47, ‐0.11] |
| 4 PAIN: cervical manipulation vs medicine Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: cervical manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 PAIN: cervical manipulation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Multiple sessions for subacute to chronic CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Multiple sessions for subacute to chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 PAIN: cervical manipulation vs acupuncture Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 PAIN: cervical manipulation vs orthotic devices (K‐tape) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Single session for acute to chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 PAIN: cervical manipulation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 PAIN: cervical manipulation ‐ 1 technique vs another technique Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Single session for acute to chronic neck pain: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Multiple sessions for subacute to chronic neck pain: short‐term follow‐up | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.4 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 PAIN: cervical manipulation ‐ varied dosage comparison Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 High vs low dosage ‐ multiple sessions for chronic CGH: short‐term follow‐up | 2 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.81, 0.49] |
| 11.2 High vs low dosage ‐ multiple sessions for chronic CGH: intermediate‐term follow‐up | 2 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.96, 0.16] |
| 12 PAIN: thoracic manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Multiple sessions for neck pain chronicity NR: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 FUNCTION: cervical manipulation vs mobilisation Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 1 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.35, 0.24] |
| 13.2 Multiple sessions for acute to chronic neck pain: intermediate‐term follow‐up | 2 | 445 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.21, 0.18] |
| 14 FUNCTION: cervical manipulation vs massage Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Multiple sessions for chronic CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 FUNCTION: cervical manipulation vs medicine Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.64, ‐0.06] |
| 15.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.30, 0.29] |
| 15.3 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.59, ‐0.00] |
| 15.4 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.40, 0.18] |
| 15.5 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | 42 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.97, 0.25] |
| 16 FUNCTION: cervical manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 FUNCTION: cervical manipulation vs orthotic devices (K‐taping) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 17.1 Single session for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 FUNCTION: cervical manipulation vs acupuncture Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 18.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 FUNCTION: cervical manipulation vs varied multi‐modal approaches Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 19.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Multiple sessions for subacute/chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 FUNCTION: cervical manipulation ‐ 1 technique vs another technique Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 20.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.3 Multiple sessions for neck pain chronicity NR: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.4 Multiple sessions for acute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 FUNCTION: cervical manipulation ‐ varied dosage comparison Show forest plot | 2 | 97 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.09, ‐0.14] |
| 21.1 High vs low dosage ‐ multiple sessions for chronic CGH: short‐term follow‐up | 2 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.71, 0.22] |
| 21.2 High vs low dosage ‐ multiple sessions for chronic CGH: intermediate‐term follow‐up | 2 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.38, 0.17] |
| 22 PATIENT SATISFACTION: cervical manipulation vs mobilisation Show forest plot | 1 | 303 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.21, 0.24] |
| 22.1 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | 303 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.21, 0.24] |
| 23 PATIENT SATISFACTION: cervical manipulation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 23.1 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 GLOBAL PERCEIVED EFFECT: cervical manipulation vs mobilisation Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 24.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 QUALITY OF LIFE: cervical manipulation vs mobilisation Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 25.1 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 QUALITY OF LIFE: cervical manipulation vs medicine Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 26.1 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.2 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 QUALITY OF LIFE: cervical manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 27.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical mobilisation vs medical injection ‐ trigger point Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical mobilisation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Multiple sessions for radiculopathy chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 PAIN: cervical mobilisation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 PAIN: cervical mobilisation vs sonic devices ‐ ultrasound, shock wave therapy Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Single session for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: cervical mobilisation vs mechanical traction Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 PAIN: cervical mobilisation vs acupuncture Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 PAIN: cervical mobilisation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 PAIN: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Single session for chronic neck pain: immediate‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Single session for chronic neck pain ± radiculopathy: immediate‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 PAIN: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9.1 PA vs other mobilisation for acute/subacute neck pain: multiple sessions: immediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 AP vs other mobilisation: multiple sessions: immediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 PAIN: cervical mobilisation vs massage Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.56 [‐4.15, 1.03] |
| 10.2 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.89 [‐3.85, ‐1.93] |
| 11 FUNCTION: cervical mobilisation vs medical injection ‐ trigger point Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 FUNCTION: cervical mobilisation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Multiple sessions for radiculopathy: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 FUNCTION: cervical mobilisation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 FUNCTION: cervical mobilisation vs sonic devices ‐ shock wave therapy Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 FUNCTION: cervical mobilisation vs acupuncture Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15.1 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 FUNCTION: cervical mobilisation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 FUNCTION: cervical mobilisation vs massage Show forest plot | 2 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.90, 0.84] |
| 17.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | 23 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐1.35, 0.32] |
| 17.2 Multiple sessions for subacute/chronic CGH: immediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.28, 1.04] |
| 18 FUNCTION: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 18.1 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 QUALITY OF LIFE: mobilisation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 19.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 PATIENT SATISFACTION: cervical mobilisation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 20.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 PATIENT SATISFACTION: cervical mobilisation vs electrotherapy Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 21.1 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 GLOBAL PERCEIVED EFFECT: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 22.1 Single session for chronic neck pain: immediate‐term follow‐up | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |

