Ecografía para la confirmación de la colocación de la sonda gástrica
Appendices
Appendix 1. Additional characteristics of included studies
| Study ID | Basile 2015 |
| Report ID | 2‐26 |
| Review author name | HT and YK |
| Authors | Basile V, Cresci A, Brondi D, Solinas D, Cei M, Mumoli N |
| Contact address | Department of Internal Medicine, Ospedale Civile Livorno, Livorno, Italy |
| Country of the study | Italy |
| Language of publication | English |
| Participants | |
| Age (mean, median, range) | Unclear |
| Sex (male numbers/%) | Unclear |
| BMI | Unclear |
| Study characteristics | |
| Single or multicentre? | Single |
| Inclusion criteria of participants | Consecutive |
| Total number of participants | 46 |
| Total number of adults | Unclear |
| Total number of children | Unclear |
| Total number of non‐sedated participants | Unclear |
| Total number of intubated participants | Unclear |
| Types of tubes (nasogastric or orogastric) | Nasogastric |
| Diameter of gastric tube | Unclear |
| Reference standard (chest or abdominal X‐ray visualization) | Chest X‐ray |
| Detail reference standard process (if available) | Blind |
| Index test (where was the echo window of the tube?) | Unclear |
| Index test (where the ultrasound test was performed) | Unclear |
| Index test (who performed the test) | Nurses |
| Time gap between index test and reference standard | Unclear |
| Study outcome (number of people) | |
| Correct gastric tube placement and correct visualization by ultrasound (i.e. true‐positive test) | 17 |
| Incorrect gastric tube placement but failure to visualize by ultrasound (i.e. false‐positive test) | 10 |
| Correct gastric tube placement but failure to visualize by ultrasound (i.e. false‐negative test) | 17 |
| Incorrect gastric tube placement and correct visualization by ultrasound (i.e. true‐negative test) | 2 |
| Number of X‐ray misinterpretation | Not reported |
| Additional information | ‐ |
| Conflict of interest | Unclear |
| Study ID | Brun 2012 |
| Report ID | 2‐21 |
| Review author name | Dr Laurie Dontigny‐Duplain, Dr Mbah Okwen Patrick (for data extraction of the French article) |
| Authors | Brun PM, Chenaitia H, Bessereau J, Leyral J, Barberis C, Pradel‐Thierry AL, Stephan J, Benner P, Querellou E, Topin F |
| Contact address | E‐mail: [email protected] |
| Country of the study | France |
| Language of publication | France |
| Participants | |
| Age (mean, median, range) | Mean: 52 years; median: 53.5 years; SD: 23 years |
| Sex (male numbers/%) | 56/58.3% |
| BMI | Not available |
| Study characteristics | |
| Single or multicentre? | Single |
| Inclusion criteria of participants | People intubated by prehospital services that required an NG tube |
| Total number of participants | 96 |
| Total number of adults | 96 |
| Total number of children | 0 |
| Total number of non‐sedated participants | 0 |
| Total number of intubated participants | 96 |
| Types of tubes (nasogastric or orogastric) | NG |
| Diameter of gastric tube | 14 or 16 Fr |
| Reference standard (chest or abdominal X‐ray visualization) | Chest X‐ray on arrival at hospital |
| Detail reference standard process (if available) | ‐ |
| Index test (where was the echo window of the tube?) | Transverse left subcostal |
| Index test (where the ultrasound test was performed) | Prehospital setting |
| Index test (who performed the test) | Prehospital services doctor trained in eFAST examination |
| Time gap between index test and reference standard | Not available |
| Study outcome (number of people) | |
| Correct gastric tube placement and correct visualization by ultrasound (i.e. true‐positive test) | 80 |
| Incorrect gastric tube placement but failure to visualize by ultrasound (i.e. false‐positive test) | 0 |
| Correct gastric tube placement but failure to visualize by ultrasound (i.e. false‐negative test) | 8 |
| Incorrect gastric tube placement and correct visualization by ultrasound (i.e. true‐negative test) | 8 |
| Number of X‐ray misinterpretation | 0 |
| Additional information | ‐ |
| Conflict of interest | None |
| Study ID | Brun 2014 |
| Report ID | 2‐01 |
| Review author name | HT and YK |
| Authors | Brun PM, Chenaitia H, Lablanche C, Pradel AL, Deniel C, Bessereau J, Melaine R |
| Contact address | Department of Emergency Medicine and Intensive Care, Desgenettes Military Hospital, Lyon, France |
| Country of the study | France |
| Language of publication | English |
| Participants | |
| Age (mean, median, range) | mean: 57 years, median: 59 years, range unclear |
| Sex (male numbers/%) | 18/56.3% |
| BMI | Unclear |
| Study characteristics | |
| Single or multicentre? | Single |
| Inclusion criteria of participants | Aged ≥ 18 years receiving prehospital care and requiring GT insertion. Exclusion criteria: aged < 18 years, pregnant, contraindication at GT insertion, interhospital transfers and absence of X‐ray control. |
| Total number of participants | 32 |
| Total number of adults | 32 |
| Total number of children | 0 |
| Total number of non‐sedated participants | 0 |
| Total number of intubated participants | 32 |
| Types of tubes (nasogastric or orogastric) | Either nasogastric or orogastric tubes used |
| Diameter of gastric tube | 14 Fr: 12, 16 Fr: 20 |
| Reference standard (chest or abdominal X‐ray visualization) | X‐ray |
| Detail reference standard process (if available) | Protocol also required final confirmation of GT placement by X‐ray on arrival at hospital, X‐ray was the test method reference to confirm correct GT placement. |
| Index test (where was the echo window of the tube?) | Portable ultrasound system (Titan, Sonosite, Bothell, WA) with a microconvex probe (2‐A MHz). Technique standardized; probe placed transversely on anterior neck just superior to suprasternal notch in midline at level of thyroid gland and focused on visible part of the oesophagus (Figure 1 of publication), with longitudinal and transversal viewing, then probe placed in subxiphoid area and oriented towards left upper abdominal quadrant to visualize stomach (Figure 2 of publication), with transverse and longitudinal viewing. The antrum was imaged in transversal plane in epigastric area using left lobe of liver as an internal landmark, angling the transducer towards left subcostal area to image gastric body. Ultrasound examination was considered as positive when GT was visualized, appearing as an hyperechogenic circle posterior to the thyroid tissue adjacent to the trachea (Figure 1 of publication), and as a hyperechogenic line in stomach (Figure 2 of publication). When GT was seen in oesophagus and not in stomach, 50 mL of air were injected through the GT, if ultrasonography showed dynamic fogging in the stomach, GT was considered in stomach. |
| Index test (where the ultrasound test was performed) | Prehospital setting |
| Index test (who performed the test) | Emergency physician |
| Time gap between index test and reference standard | Unclear |
| Study outcome (number of people) | |
| Correct gastric tube placement and correct visualization by ultrasound (i.e. true‐positive test) | Echo + fogging 28 Echo only 27 |
| Incorrect gastric tube placement but failure to visualize by ultrasound (i.e. false‐positive test) | Echo + fogging 0 Echo only 0 |
| Correct gastric tube placement but failure to visualize by ultrasound (i.e. false‐negative test) | Echo + fogging 0 Echo only 1 |
| Incorrect gastric tube placement and correct visualization by ultrasound (i.e. true‐negative test) | Echo + fogging 4 Echo only 4 |
| Number of X‐ray misinterpretation | 0 |
| Additional information | ‐ |
| Conflict of interest | Unclear |
| Study ID | Chenaitia 2012 |
| Report ID | 2‐05,11 |
| Review author name | HT and YK |
| Authors | Chenaitia H, Brun PM, Querellou E, Leyral J, Bessereaud J, Aimée C, Bouazize R, Georgesf A, Louisf F; WINFOCUS (World Interactive Network Focused On Critical Ultrasound) Group France |
| Contact address | Service de Médecine d'Urgence et de Radiologie, Centre Hospitalier General de Clavary, Grasse, France Tel.: +33 4 91499191; fax: +33 4 91386943 |
| Country of the study | France |
| Language of publication | English |
| Participants | |
| Age (mean, median, range) | Mean ± SD: 55.7 ± 19.8 years |
| Sex (male numbers/%) | 77/59% |
| BMI | Unclear |
| Study characteristics | |
| Single or multicentre? | Multicentre |
| Inclusion criteria of participants | Inclusion criteria: aged ≥ 18 years in prehospital settings and requiring GT insertion Exclusion criteria: aged < 18 years, pregnant, interhospital transfers and absence of X‐ray control |
| Total number of participants | 130 |
| Total number of adults | 130 |
| Total number of children | 0 |
| Total number of non‐sedated participants | 0 |
| Total number of intubated participants | 130 |
| Types of tubes (nasogastric or orogastric) | Both |
| Diameter of gastric tube | 7 × 18‐Fr GTs were inserted and all were visible, 94 × 16‐Fr GTs were inserted and 98% were visible, and 29 × 14‐Fr GTs were inserted and 81% were visible. |
| Reference standard (chest or abdominal X‐ray visualization) | X‐ray |
| Detail reference standard process (if available) | X‐ray on arrival at hospital |
| Index test (where was the echo window of the tube?) | Subxiphoid area |
| Index test (where the ultrasound test was performed) | Prehospital |
| Index test (who performed the test) | 2 emergency physicians who performed ultrasound examination were experienced and certified in emergency ultrasound, had 1‐day of training dedicated to study the specificities of this type of ultrasound examination. |
| Time gap between index test and reference standard | Unclear |
| Study outcome (number of people) | |
| Correct gastric tube placement and correct visualization by ultrasound (i.e. true‐positive test) | 116 |
| Incorrect gastric tube placement but failure to visualize by ultrasound (i.e. false‐positive test) | 0 |
| Correct gastric tube placement but failure to visualize by ultrasound (i.e. false‐negative test) | 2 |
| Incorrect gastric tube placement and correct visualization by ultrasound (i.e. true‐negative test) | 12 |
| Number of X‐ray misinterpretation | 0 |
| Additional information | ‐ |
| Conflict of interest | None |
| Study ID | Gok 2015 |
| Report ID | 2‐06,07,09 |
| Review author name | HT and YK |
| Authors | Gok F, Kilicaslan A, Yosunkaya A |
| Contact address | Necmettin Erbakan University, Meram Faculty of Medicine, Department of Anesthesiology and Email: [email protected] |
| Country of the study | Turkey |
| Language of publication | English |
| Participants | |
| Age (mean, median, range) | Mean ± SD: 48.4 ± 28.9 years |
| Sex (male numbers/%) | 32/57.1% |
| BMI | Mean ± SD: 27.1 ± 6.4 |
| Study characteristics | |
| Single or multicentre? | Single |
| Inclusion criteria of participants | 56 mechanically ventilated participants monitored in the ICU between February and July 2014 who received ultrasound‐guided NG tube placement were included in the study. Exclusion criteria: histories of neck surgery (e.g. tracheotomy), anatomic deformity, nasal fracture or severe coagulopathy. |
| Total number of participants | 56 |
| Total number of adults | 56 (author's reply) |
| Total number of children | 0 (author's reply) |
| Total number of non‐sedated participants | 0 |
| Total number of intubated participants | 56 |
| Types of tubes (nasogastric or orogastric) | Nasogastric, guidewire |
| Diameter of gastric tube | 10‐14 Fr |
| Reference standard (chest or abdominal X‐ray visualization) | After ultrasound‐guided tube insertion, gastric placement of the NG tube tip confirmed with abdominal X‐ray (author's reply). All reference standard results interpreted by a single person (author's reply). Used prespecified criteria of the correct position; i.e. NG tube tip below the diaphragm; should follow straight course down midline of chest to a point below diaphragm (author's reply). |
| Detail reference standard process (if available) | ‐ |
| Index test (where was the echo window of the tube?) | Transversely placed over the suprasternal notch. Images obtained of isthmus and 2 lobes of thyroid gland. By shifting the |
| Index test (where the ultrasound test was performed) | ICU |
| Index test (who performed the test) | Ultrasound examination performed by the same operator, experienced in ultrasonography. |
| Time gap between index test and reference standard | 10 minutes to 1 hour (author's reply) |
| Study outcome (number of people) | |
| Correct gastric tube placement and correct visualization by ultrasound (i.e. true‐positive test) | 52 |
| Incorrect gastric tube placement but failure to visualize by ultrasound (i.e. false‐positive test) | 0 |
| Correct gastric tube placement but failure to visualize by ultrasound (i.e. false‐negative test) | 4 |
| Incorrect gastric tube placement and correct visualization by ultrasound (i.e. true‐negative test) | 0 |
| Number of X‐ray misinterpretation | 0 |
| Additional information | 4 unclear result of ultrasound |
| Conflict of interest | None reported |
| Study ID | Kim 2012 |
| Report ID | 2‐12,13,14 |
| Review author name | HT and YK |
| Authors | Kim HM, So BH, Jeong WJ, Choi SM, Park KN |
| Contact address | Department of Emergency Medicine, College of Medicine, The Catholic Email: [email protected] |
| Country of the study | Korea |
| Language of publication | English |
| Participants | |
| Age (mean, median, range) | Mean ± SD: 57.6 ± 17.2 years |
| Sex (male numbers/%) | 28/59.6% |
| BMI | Unclear |
| Study characteristics | |
| Single or multicentre? | Single |
| Inclusion criteria of participants | Unclear criteria Prospective study performed between May and September 2011 in a local emergency centre. Included participants with low consciousness in whom correct placement of NG tube was ultimately verified by chest X‐ray. Aged > 18 years, undergoing NG tube insertions for reasons including drug overdose, suspicion of gastric bleeding, endotracheal intubation and others. 17 patients with normal levels of consciousness were excluded. 10 participants did not undergo X‐ray examination. |
| Total number of participants | 47 |
| Total number of adults | 47 |
| Total number of children | 0 |
| Total number of non‐sedated participants | 0 |
| Total number of intubated participants | 27 |
| Types of tubes (nasogastric or orogastric) | Nasogastric |
| Diameter of gastric tube | 16 Fr |
| Reference standard (chest or abdominal X‐ray visualization) | Chest X‐ray |
| Detail reference standard process (if available) | Final confirmation of gastric placement of tube by chest X‐ray, i.e. test method reference standard to confirm correct NG tube placement. Chest X‐rays interpreted by emergency medicine specialist who did not perform ultrasound examinations. |
| Index test (where was the echo window of the tube?) | In oesophagogastric junction, NG tube directly visualized with longitudinal and angled scans of the epigastrium. Visualization of NG tube in separate scans of fundus and antrum of stomach. |
| Index test (where the ultrasound test was performed) | EMS |
| Index test (who performed the test) | Ultrasound examinations conducted by 2 emergency medicine specialists. |
| Time gap between index test and reference standard | Unclear |
| Study outcome (number of people) | ‐ |
| Correct gastric tube placement and correct visualization by ultrasound (i.e. true‐positive test) | 38 |
| Incorrect gastric tube placement but failure to visualize by ultrasound (i.e. false‐positive test) | 1 |
| Correct gastric tube placement but failure to visualize by ultrasound (i.e. false‐negative test) | 6 |
| Incorrect gastric tube placement and correct visualization by ultrasound (i.e. true‐negative test) | 2 |
| Number of X‐ray misinterpretation | 0 |
| Additional information | ‐ |
| Conflict of interest | None reported |
| Study ID | Lock 2003 |
| Report ID | 2‐08 |
| Review author name | Ms Katharina Kunzweiler, Dr Matthias Rinderknecht (translation and data extraction of the German article) |
| Authors | Lock G, Reng CM, Köllinger M, Rogler G, Schölmerich J, Schlottmann K |
| Contact address | Medizinische Klinik Albertinenkrankenhaus Süntelstr. 11a, 22457 Hamburg, Germany Tel.: 040/5588‐2262, Email: [email protected] |
| Country of the study | Germany |
| Language of publication | Germany |
| Participants | |
| Age (mean, median, range) | Mean ± SD: 59.2 ± 16.2 years; range: 16‐84 years |
| Sex (male numbers/%) | Not reported |
| BMI | Not reported |
| Study characteristics | |
| Single or multicentre? | Single (internal ICU of a university hospital) |
| Inclusion criteria of participants | Inclusion criteria: people in ICU, endotracheal intubation and ventilation or independent breathing Exclusion criteria: percutaneous endoscopic gastrostomy How were participants' coughs managed: not reported. How were auscultation findings dealt with: auscultation in the epigastrium after insufflation of 50 mL of air by a bladder syringe; localization counted as correct if sound of incoming air in epigastrium could clearly be auscultated. Prior testing: not reported. Presentation: in 50/60 procedures, participants were endotracheally intubated and ventilated; in 10/60 procedures, participants were breathing spontaneously, none had a tracheostomy. In 51/60 procedures, participants were unable to co‐operate; in 8/60 procedures, participants were partly able to co‐operate and in 1 procedure fully able to co‐operate. In 49/60 procedures, tube placed for feeding, in 11/60 procedures, for drainage. |
| Total number of participants | 55 participants with in 60 gastric tube insertions |
| Total number of adults | Not reported |
| Total number of children | Not reported |
| Total number of non‐sedated participants | 9 procedures |
| Total number of intubated participants | Participants were intubated in 50 gastric tube insertions |
| Types of tubes (nasogastric or orogastric) | Nasogastric (in exceptional cases orogastric) |
| Diameter of gastric tube | 58 times soft silicon tube, diameter 14.6 Charrière 2 times drainage tube, diameter not reported |
| Reference standard (chest or abdominal X‐ray visualization) | Reference standard: X‐ray X‐ray of lower thorax or upper abdomen. Incorrect localization of tube defined as localization of tube in oesophagus or lungs. X‐ray usually carried out routinely on next morning after procedure or because of another medical indication. Period between placement of gastric tube and radiological control was within 24 hours. |
| Detail reference standard process (if available) | Not reported |
| Index test (where was the echo window of the tube?) | In ultrasound, correct placement of tip of tube in stomach was ascertained by detecting a 50 mL air jet applied with a syringe via the gastric tube. |
| Index test (where the ultrasound test was performed) | ICU |
| Index test (who performed the test) | Ultrasound performed by 10 experienced examiners/practitioners. |
| Time gap between index test and reference standard | After auscultation in the epigastrium, pH measurement of aspirate or ultrasound, examiner decided, if correct placement of gastric tube was documented by these methods. Period between placement of gastric tube and radiological control always within 24 hours. |
| Study outcome (number of people) | |
| Correct gastric tube placement and correct visualization by ultrasound (i.e. true‐positive test) | 43 |
| Incorrect gastric tube placement but failure to visualize by ultrasound (i.e. false‐positive test) | 0 |
| Correct gastric tube placement but failure to visualize by ultrasound (i.e. false‐negative test) | 15 |
| Incorrect gastric tube placement and correct visualization by ultrasound (i.e. true‐negative test) | 2 |
| Number of X‐ray misinterpretation | ‐ |
| Additional information | ‐ |
| Conflict of interest | Not reported |
| Study ID | Nikandros 2006 |
| Report ID | 3‐01 |
| Review author name | HT and YK |
| Authors | Nikandros M, Skampas N, Theodorakopoulou M, Ioannidou S, Theotokas M, Armaganidis A |
| Contact address | Not reported (we contacted the journal Critical Care and Prof Armaganidis Apostles) |
| Country of the study | Greece |
| Language of publication | English |
| Participants | |
| Age (mean, median, range) | Mean ± SD: 66.3 ± 7.1 years |
| Sex (male numbers/%) | 9/56% |
| BMI | Unclear |
| Study characteristics | |
| Single or multicentre? | Single |
| Inclusion criteria of participants | Unclear |
| Total number of participants | 16 |
| Total number of adults | Unclear |
| Total number of children | Unclear |
| Total number of non‐sedated participants | 0 |
| Total number of intubated participants | 16 |
| Types of tubes (nasogastric or orogastric) | NG tube |
| Diameter of gastric tube | Unclear |
| Reference standard (chest or abdominal X‐ray visualization) | X‐ray |
| Detail reference standard process (if available) | ‐ |
| Index test (where was the echo window of the tube?) | Unclear |
| Index test (where the ultrasound test was performed) | ICU |
| Index test (who performed the test) | Unclear |
| Time gap between index test and reference standard | Unclear |
| Study outcome (number of people) | |
| Correct gastric tube placement and correct visualization by ultrasound (i.e. true‐positive test) | 15 |
| Incorrect gastric tube placement but failure to visualize by ultrasound (i.e. false‐positive test) | 0 |
| Correct gastric tube placement but failure to visualize by ultrasound (i.e. false‐negative test) | 1 |
| Incorrect gastric tube placement and correct visualization by ultrasound (i.e. true‐negative test) | 0 |
| Number of X‐ray misinterpretation | 0 |
| Additional information | ‐ |
| Conflict of interest | Unclear |
| Study ID | Radulescu 2015 |
| Report ID | 2‐27 |
| Review author name | HT and YK |
| Authors | Radulescu V, Ahmad S |
| Contact address | Stony Brook University Hospital, St James, NY |
| Country of the study | US |
| Language of publication | English |
| Participants | |
| Age (mean, median, range) | Unclear |
| Sex (male numbers/%) | Unclear |
| BMI | Unclear |
| Study characteristics | |
| Single or multicentre? | Unclear |
| Inclusion criteria of participants | Unclear |
| Total number of participants | 32 |
| Total number of adults | Unclear |
| Total number of children | Unclear |
| Total number of non‐sedated participants | Unclear |
| Total number of intubated participants | Unclear |
| Types of tubes (nasogastric or orogastric) | Gastric tube |
| Diameter of gastric tube | Unclear |
| Reference standard (chest or abdominal X‐ray visualization) | Chest X‐ray |
| Detail reference standard process (if available) | Unclear |
| Index test (where was the echo window of the tube?) | Anterolateral neck scanned in high frequency to visualize the gastric tube's characteristic echogenic surface with posterior anechoic shadow in oesophagus. Then, right diaphragm location identified by low‐frequency imaging. |
| Index test (where the ultrasound test was performed) | Unclear |
| Index test (who performed the test) | Unclear |
| Time gap between index test and reference standard | Unclear |
| Study outcome (number of people) | |
| Correct gastric tube placement and correct visualization by ultrasound (i.e. true‐positive test) | 28 |
| Incorrect gastric tube placement but failure to visualize by ultrasound (i.e. false‐positive test) | 0 |
| Correct gastric tube placement but failure to visualize by ultrasound (i.e. false‐negative test) | 2 |
| Incorrect gastric tube placement and correct visualization by ultrasound (i.e. true‐negative test) | 2 |
| Number of X‐ray misinterpretation | 0 |
| Additional information | ‐ |
| Conflict of interest | Unclear |
| Study ID | Vigneau 2004 |
| Report ID | 2‐3,28 |
| Review author name | HT and YK |
| Authors | Vigneau C, Baudel JL, Guidet B, Offenstadt G, Maury E |
| Contact address | Service de Reanimation Medicale, Hôpital Saint ‐Antoine, Assistance Publique‐Hôpitaux de Paris, 184 rue du Faubourg Saint‐Antoine, 75571 Paris Cedex 12, France |
| Country of the study | France |
| Language of publication | English |
| Participants | |
| Age (mean, median, range) | Mean ± SD: 62.2 ± 19.8 years |
| Sex (male numbers/%) | 18/54.5% |
| BMI | Mean 24.8 ± 5.8 |
| Study characteristics | |
| Single or multicentre? | Single |
| Inclusion criteria of participants | All consecutive participants during a 2‐month period who received a weighted NG tube (12CH, Cair, France) for enteral feeding between 8:30 a.m. and 8:00 p.m. |
| Total number of participants | 33 |
| Total number of adults | Unclear |
| Total number of children | Unclear |
| Total number of non‐sedated participants | 14 |
| Total number of intubated participants | 26 |
| Types of tubes (nasogastric or orogastric) | NG (weighted‐tip NG tube) |
| Diameter of gastric tube | 12 Fr |
| Reference standard (chest or abdominal X‐ray visualization) | X‐ray |
| Detail reference standard process (if available) | As soon as tube was correctly inserted, radiology department performed confirmatory X‐ray. Times required to obtain the X‐ray and ultrasound results were recorded. |
| Index test (where was the echo window of the tube?) | Epigastric area |
| Index test (where the ultrasound test was performed) | ICU |
| Index test (who performed the test) | Principal investigator (CV) was an intensive care physician who had not graduated in sonography, and who therefore followed a specific 2‐hour training course with a radiologist. |
| Time gap between index test and reference standard | Not recorded |
| Study outcome (number of people) | |
| Correct gastric tube placement and correct visualization by ultrasound (i.e. true‐positive test) | Echo only 26 Echo + saline injection 8 |
| Incorrect gastric tube placement but failure to visualize by ultrasound (i.e. false‐positive test) | 0 |
| Correct gastric tube placement but failure to visualize by ultrasound (i.e. false‐negative test) | 1 unclear result of ultrasound, but successful insertion (author's response) |
| Incorrect gastric tube placement and correct visualization by ultrasound (i.e. true‐negative test) | 0 |
| Number of X‐ray misinterpretation | 0 |
| Additional information | 1 unclear result of ultrasound (gas interposition) |
| Conflict of interest | None (author's response) |
BMI: body mass index; eFAST: extended Focused Assessment with Sonography for Trauma; GT: gastric tube; ICU: intensive care unit; NG: nasogastric; SD: standard deviation.
Appendix 2. CENTRAL search strategy
-
MeSH descriptor: [Ultrasonography] explode all trees
-
(ultrason* or ultrasound* or echotomograph* or echo tomograph* or echograph* or sonograph* or ultra sound or acoustic):ti,ab,kw (Word variations have been searched)
-
#1 or #2
-
MeSH descriptor: [Intubation, Gastrointestinal] explode all trees
-
((stomach or gastric or gastro* or nasogastric or feeding or fine bore or Ryles) near/3 (tube* or intubat*)):ti,ab,kw (Word variations have been searched)
-
#4 or #5
-
#3 and #6
Appendix 3. MEDLINE search strategy
-
exp Ultrasonography/
-
(ultrason* or ultrasound* or echotomograph* or echo tomograph* or echograph* or sonograph* or ultra sound or acoustic).ti,ab,kw.
-
1 or 2
-
exp Intubation, Gastrointestinal/
-
((stomach or gastric or gastro* or nasogastric or feeding or fine bore or Ryles) adj3 (tube* or intubat*)).ti,ab,kw.
-
4 or 5
-
3 and 6
-
animals/ not human/s
-
7 not 8
Appendix 4. Embase search strategy
-
exp ultrasound/
-
(ultrason* or ultrasound* or echotomograph* or echo tomograph* or echograph* or sonograph* or ultra sound or acoustic).ti,ab,kw.
-
1 or 2
-
exp stomach tube/
-
exp nasogastric tube/
-
((stomach or gastric or gastro* or nasogastric or feeding or fine bore or Ryles) adj3 (tube* or intubat*)).ti,ab,kw.
-
4 or 5 or 6
-
3 and 7
-
animal/not human/
-
8 not 9
Appendix 5. Study quality assessment details
Domain 1: participant selection
Risk of bias: could the selection of participants have introduced bias?
Signalling question 1: was a consecutive or random sample of participants enrolled?
Signalling question 2: was a case‐control design avoided?
Signalling question 3: did the study avoid reinsertion of the tube when participants coughed too much?
Signalling question 4: did the study avoid reinsertion of the tube when participants did not make a bubbling sound?
Signalling question 5 and 6: did the study avoid inappropriate exclusions?
Coughing or the absence of bubbling sounds indicates misplacement of tubes into the airway. If participants experience these tests and receive reinsertion based on the results, referral bias is suspected. In addition, anatomical variation of the neck structure (e.g. larynx, pharynx) may make insertion of gastric tubes more difficult (Der Kureghian 2011; Holland 2013). This point may also affect the difficulty of visualizing the tubes by ultrasound. We classified as 'yes' those studies that excluded people who had difficulties with nasogastric tube insertion or visualization, 'no' for those studies where people did not experience such difficulties and 'unclear' where this information was not clear.
Applicability: were there concerns that the included participants and the setting did not match the review question?
The inclusion criteria for this review specified studies in which the participants were considered to require gastric tube insertion (not including transpyloric tube) for any reason. Therefore, we anticipated that all the studies in the review were judged as 'low' concern.
Domain 2: index test
Risk of bias: could the conduct or interpretation of the index test have introduced bias?
Signalling question 1: were the index test results interpreted without knowledge of the results of the reference standard?
We classified the study as 'yes' if ultrasound test results were interpreted without knowledge of the reference standard or if ultrasound test results were interpreted before the X‐ray test, 'no' if the ultrasound tests were interpreted with knowledge of the reference standard results and 'unclear' if this information was not clear.
Applicability: were there concerns that the index test, its conduct or interpretation differed from the review question?
Confirmation of gastric tube placement by ultrasound was an inclusion criterion for this review, so we anticipated that all studies were classified as 'low' concern.
Domain 3: reference standard
Risk of bias: could the reference standard, its conduct or its interpretation have introduced bias?
Signalling question 1: is the reference standard likely to correctly classify the target condition?
Signalling question 2: were the reference standard results interpreted without knowledge of the results of the index test?
Signalling question 3: were the criteria of reference standard for target condition prespecified?
We classified the studies as 'yes' if the criteria for appropriate gastric tube placement were checked by X‐ray visualization, 'no' if the criteria for verification of placement were by any other methods and 'unclear' if this information was not clear. We classified the study as 'yes' if X‐ray visualization results were interpreted without knowledge of the index test, 'no' if the X‐ray visualization was interpreted with knowledge of the index test results and 'unclear' if this information was not clear. We classified the study as 'yes' if the criteria of reference standard for target condition were prespecified, 'no' if the criteria of reference standard for target condition were not prespecified and 'unclear' if this information was not clear.
Applicability: were there concerns that the target condition as defined by the reference standard did not match the review question?
The target condition is the appropriate placement of a gastric tube in the stomach via the nose or mouth, which may be improved by the use of prespecified diagnostic criteria for chest X‐ray interpretation (Lamont 2011). We evaluated those studies that used clear diagnostic criteria for X‐ray visualization interpretation as 'low' concern, those that did not use any criteria or where the interpretation was based on an individual clinician's interpretation as 'high' concern and 'unclear' concern if this information was not clear.
Domain 4: flow and timing
Risk of bias: could the participant flow have introduced bias?
Signalling question 1: did all participants receive the same reference standard?
Signalling question 2: was there an appropriate interval between the index test and reference standard?
Signalling question 3: were all participants included in the analysis?
We classified the study as 'yes' if all participants had the same reference standard, 'no' if the reference standard was different from chest or abdominal X‐ray and 'unclear' if this information was not clear. If a gastric tube was correctly inserted and initial gastric tube placement was confirmed, continual assessment is still required because some routine activities (e.g. vomiting, coughing, retching) may cause tube displacement (Simons 2012). Therefore, any delay in testing may influence results. However, we set an arbitrary time delay between tests in line with the AACCN 2009, which recommends tube location to be checked at four‐hourly intervals (Simons 2012). We classified the study as 'yes' if the delay was less than four hours, 'no' if the delay was four hours or more and 'unclear' if the information was not clear.
Uninterpretable results may be present (e.g. unclear chest X‐ray or ultrasound). Additionally, withdrawals from the study may be present. We classified the study as 'yes' if uninterpretable results were reported and the study had no withdrawals or the withdrawals were unlikely to affect the results, 'no' if uninterpretable results were not reported or there were withdrawals that were likely to affect the results, or both, and 'unclear' if this information was not clear.

Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies.
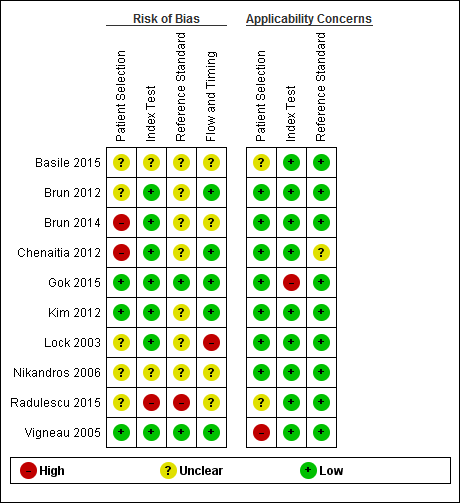
Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study.

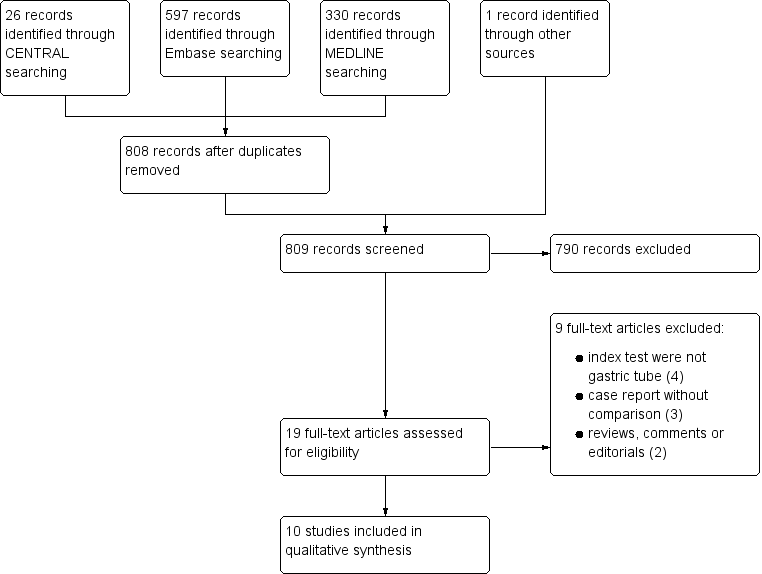
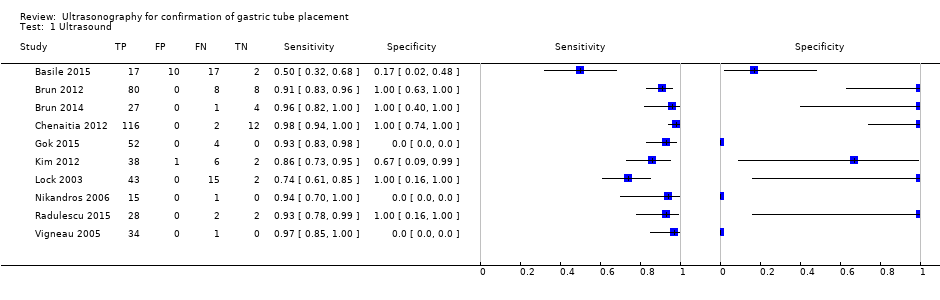
Forest plot of diagnostic accuracy of ultrasound in different ways. Four studies reported the diagnostic accuracy of ultrasound (Brun 2012; Chenaitia 2012; Gok 2015; Radulescu 2015), while the others reported the diagnostic accuracy of ultrasound combined with other methods. Gok 2015 reported the diagnostic accuracy of ultrasound during tube insertion (ultrasound‐guide insertion). We found three visualization methods (echo window) of ultrasound: neck (Gok 2015), epigastric (Brun 2012; Chenaitia 2012; Kim 2012; Lock 2003; Vigneau 2005), and a combination (Brun 2014; Radulescu 2015). Studies used air injection during ultrasound (Basile 2015; Brun 2014), saline injection (Vigneau 2005), both air and saline injection (Kim 2012), and dextrose and air injection (Nikandros 2006). Two studies did not report the echo window (Basile 2015; Nikandros 2006).
| Accuracy of ultrasound for confirmation of gastric tube placement | |||||||||
| Population | Adults in any settings (prehospital, ICU, EMS or unclear) | ||||||||
| Index test | Ultrasound (any methods) | ||||||||
| Reference standard | X‐ray | ||||||||
| Studies | Cross‐sectional study or unclear study designa | ||||||||
| Study ID | TPb | FPb | FNb | TNb | Participants | Sensitivity | Specificity | Methodc | Echo windowc |
| 17 | 10 | 17 | 2 | 46 | 0.50 (0.32 to 0.68) | 0.17 (0.02 to 0.48) | Ultrasound + air injection after insertion | NR | |
| Brun 2012a,d | 80 | 0 | 8 | 8 | 96 | 0.91 (0.83 to 0.96) | 1.00 (0.63 to 1.00) | Ultrasound after insertion | Epigastric |
| 27 | 0 | 1 | 4 | 32 | 0.96 (0.82 to 1.00) | 1.00 (0.40 to 1.00) | Ultrasound + air injection after insertion | Neck + epigastric | |
| 116 | 0 | 2 | 12 | 130 | 0.98 (0.94 to 1.00) | 1.00 (0.74 to 1.00) | Ultrasound after insertion | Epigastric | |
| 52 | 0 | 4 | 0 | 56 | 0.93 (0.83 to 0.98) | Not estimable | Ultrasound during insertion | Neck | |
| 38 | 1 | 6 | 2 | 47 | 0.86 (0.73 to 0.95) | 0.67 (0.09 to 0.99) | Ultrasound + saline and air injection | Neck + epigastric | |
| 43 | 0 | 15 | 2 | 55 (60 measurements)e | 0.74 (0.61 to 0.85) | 1.00 (0.16 to 1.00) | Ultrasound + air injection after insertion | Epigastric | |
| 15 | 0 | 1 | 0 | 16 | 0.94 (0.70 to 1.00) | Not estimable | Ultrasound + dextrose and air injection after insertion | NR | |
| 28 | 0 | 2 | 2 | 32 | 0.93 (0.78 to 0.99) | 1.00 (0.16 to 1.00) | Ultrasound after insertion | Neck + epigastric | |
| 34 | 0 | 1 | 0 | 35 | 0.97 (0.85 to 1.00) | Not estimable | Ultrasound + saline injection after insertion | Epigastric | |
| CI: confidence interval; EMS: emergency medical service; ICU: intensive care unit: FN: false negative; FP: false positive; NR: not reported; TN: true negative; TP: true positive. | |||||||||
| Accuracy of ultrasound for confirmation of gastric tube placement for drainage in settings where X‐ray facilities are not readily available | |||||||||
| Population | Adults underwent gastric tube insertion for drainage in settings where X‐ray facilities are not readily available (prehospital or EMS) | ||||||||
| Index test | Ultrasound (any methods) | ||||||||
| Reference standard | X‐ray | ||||||||
| Studies | Cross‐sectional study or unclear study designa | ||||||||
| Study ID | TPb | FPb | FNb | TNb | Participants | Sensitivity | Specificity | Methodc | Echo windowc |
| Brun 2012c,d | 80 | 0 | 8 | 8 | 96 | 0.91 (0.83 to 0.96) | 1.00 (0.63 to 1.00) | Ultrasound after insertion | Epigastric |
| 27 | 0 | 1 | 4 | 32 | 0.96 (0.82 to 1.00) | 1.00 (0.40 to 1.00) | Ultrasound+ air injection after insertion | Neck + epigastric | |
| 116 | 0 | 2 | 12 | 130 | 0.98 (0.94 to 1.00) | 1.00 (0.74 to 1.00) | Ultrasound after insertion | Epigastric | |
| 38 | 1 | 6 | 2 | 47 | 0.86 (0.73 to 0.95) | 0.67 (0.09 to 0.99) | Ultrasound + saline and air injection | Neck + epigastric | |
| CI: confidence interval; EMS: emergency medical service; FN: false negative; FP: false positive; TN: true negative; TP: true positive. | |||||||||
| Study ID | Male:female | Age | BMI | Children | Non‐sedated | Sedated | Intubated | Diameter | Setting |
| NR | NR | NR | NR | NR | NR | NR | NR | NR | |
| 56:24 | 52 ± 23 | NR | 0 | 0 | 96 | 96 | 14 or 16 | Prehospital | |
| 18:14 | 57 ± 17 | NR | 0 | 22 | 10 | 32 | 14 or 16 | Prehospital | |
| 77:53 | 55.7 ± 19.8 | NR | 0 | 0 | 130 | 130 | 14‐18 | Prehospital | |
| 32:24 | 48.4 ± 28.9 | 27.1 ± 6.4 | 0 | 0 | 56 | 56 | 10‐14 | ICU | |
| 28:19 | 57.6 ± 17.2 | NR | 0 | 0 | 47 | 27 | 16 | EMS | |
| NR | 59.2 ± 16.2 | NR | NR | NR | NR | 50 | 14 or 16 | ICU | |
| 9:7 | 66.3 ± 7.1 | NR | NR | 0 | 16 | 16 | NR | ICU | |
| NR | N/R | NR | NR | NR | NR | NR | NR | NR | |
| 18:16 | 62.2 ± 19.8 | 24.8 ± 5.8 | 0 | 14 | 19 | 26 | 12 | ICU | |
| BMI: body mass index; EMS: emergency medical service; ICU: intensive care unit; NR: not reported; SD: standard deviation. a Reports from the same research group. | |||||||||
| Test | No. of studies | No. of participants |
| 1 Ultrasound Show forest plot | 10 | 550 |