Formación de los profesionales de la asistencia sanitaria en la prevención de las úlceras por presión
References
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en curso
Referencias adicionales
Referencias de otras versiones publicadas de esta revisión
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | Study design: 3‐armed RCT Ethics and informed consent: approval gained from each site, written consent obtained from participants Sample size calculation: no ITT analysis: no | |
| Participants | Location: 44 nurses from 2 hospitals and 4 nursing homes in Norway; 81.8% worked in the hospital setting Mean age: not specified Gender: 97.7% F / 2.3% M Years nursing experience: whole group range 0‐32 years; range 0‐2 years n = 5 (16.4%); 3‐5 years n = 12 (27.3%); > 6 years n = 27 (61.4%) Inclusion criteria: registered nurse; employed in acute care hospital or nursing home Exclusion criteria: not specified | |
| Interventions | Aim: to develop and test an e‐learning programme for the assessment of pressure ulcer risk and classification Group A: independent e‐learning module in a computer room using his/her own computer terminal (intervention) (n = 23 nurses) content identical to control group Group B: received 45‐min classroom lecture delivered by an experienced nurse using power point presentation (classroom) (n = 21 nurses) content identical to intervention group Group C: no education (control) ‐ no other details supplied as, quote: "because of massive dropout, we excluded this group and test from the study" Study date: May‐December 2012 | |
| Outcomes | Primary outcomes: knowledge of risk assessment using Braden scale; knowledge of classification using stages 1‐4, DTI and unstageable pressure ulcer categories (NPUAP) Secondary outcomes: none specified Time points: pre‐ and postintervention and 3 months' follow‐up | |
| Notes | Design was 3‐arm RCT but only 2‐arm RCT reported: quote: "because of massive dropout, we excluded this group and test from the study" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "we used block randomization with six in each block to ensure even distribution within the groups" Comment: the method of generating the randomisation sequence was not described |
| Allocation concealment (selection bias) | Low risk | Quote: "a study coordinator prepared the randomization using closed, opaque numbered envelopes to conceal group allocation" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Study protocol (NCT01567410 Clinicaltrials.gov), states that it was a single blind study (participants) but no information given in study report Comment: not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: not reported |
| Incomplete outcome data (attrition bias) | High risk | Quote: "the dropout rate for the three‐month test for the total sample was 59%. The dropout rate was high in both groups" No reasons given by study authors on high dropout rate across both arms; control group not reported upon due to high dropout rate Comment: high level of incomplete outcome data detected |
| Selective reporting (reporting bias) | High risk | Quote: "the study protocol included a third group without additional training and a test six months after training, but because of massive dropout, we excluded this group and test from the study " The study protocol (NCT01567410 Clinicaltrials.gov), also reports a measurement period of 24 weeks but these data were not reported Comment: high level of selective reporting |
| Other bias | Unclear risk | Quote: "we did not ask the nurses about their computer knowledge and preferred learning method" (p 196) Comment: computer proficiency impact upon e‐learning method |
| Methods | Study design: 2‐armed RCT Ethics and informed consent: ethical approval not stated, written consent obtained from participants Sample size calculation: no ITT analysis: yes | |
| Participants | Location: 102 RNs, LPNs and nursing assistants employed within an urban, acute care hospital Mean age: reported whole‐group only: range 20‐69 years; mean 33.3 years; SD 10.3 years Gender: 89.2% F / 10.8% M Years nursing experience: reported whole group only: range 1‐35 years; mean 8.3 years; SD 7.8 years Inclusion criteria: not specified Exclusion criteria: not specified | |
| Interventions | Aim: to determine the effectiveness of a teaching plan designed to increase a hospital nursing staff's knowledge of pressure ulcer risk, assessment, and treatments Group A: received 40‐min, instructional, didactic, teaching intervention of pressure ulcer risk, assessment and treatment strategies (n = 48) Group B: viewed 25‐min video on general aspects of skin care for hospitalised patients (n = 54) Study date: not stated | |
| Outcomes | Primary outcomes: 100‐item true / false knowledge score Secondary outcomes: none measured | |
| Notes | Demographic details not provided by group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "a systematic random sample of subjects" ... "subjects were recruited by letter after random selection from a list of nursing staff employees" ... "assigned randomly to experimental or control groups" Comment: the method of generating the randomisation sequence was not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: participants are unlikely to have known which of the 2 interventions was the 'active' intervention based upon whether they watched the video or took part in the didactic educational session but blinding was not specifically addressed |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: not reported |
| Incomplete outcome data (attrition bias) | Low risk | Comment: full set of outcome data presented for full cohort |
| Selective reporting (reporting bias) | Low risk | Comment: not apparent, all measures reported |
| Other bias | Low risk | None detected |
| Methods | Study design: 3‐group parallel‐RCT with an 18‐month follow‐up period Ethics and informed consent: ethical approval gained and informed consent taken Sample size calculation: yes ITT analysis: yes | |
| Participants | Location: 37 residential homes of 726 residents in North Lincolnshire, UK Mean ages: not reported Patient information: Group A: 0.8% < 65 years; 7.8% 65‐74 years; 91.4% > 75 years: 74% F / 26% M Group B: 0.5% < 65 years; 4.3% 65‐74 years; 95.1% > 75 years: 82% F / 18% M Group C: 1.2% < 65 years; 10.5% 65‐74 years; 88.3% > 75 years: 85% F / 15% M Inclusion criteria: Residential homes were required to:
Residents were required to:
Exclusion criteria: not specified | |
| Interventions | Aim: to examine the effects of introducing a programme of training and monitoring to reduce pressure sores in residential homes Group A: training, monitoring and observation (21 homes; 371 residents) Group B: monitoring and observation (9 homes; 191 residents) Group C: observation only (7 homes; 164 residents) Training: 2‐hour interactive session delivered by a district nurse, quote: "based upon the principles of pressure sore risk assessment using the Norton scale, pressure sore grading, and pressure sore prevention through management of nutrition, continence, mobility and moving and handling". Monitoring: the district nurse, quote: "taught the principles of risk assessment and pressure sore grading only" Observation: quote: "no instruction at all from the district nurse" Study dates: not stated | |
| Outcomes | Primary outcomes: risk assessment using Norton scale and grading using the David classification (grades 1‐4) Secondary outcomes: functional dependency using Barthel Index & quality of life using Euroqol Time points: baseline, 6, 12, and 18 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly selected" ... "randomly allocated into one of three groups" Comment: the method of generating the randomisation sequence was not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not reported |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "it was possible that staff of homes conducting self‐monitoring of risk and pressure sores would reveal their study group by discussion with the research nurse or by asking advice" Comment: not blinded |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "the project therefore progressed without the blinding of research nurses to the home study group" Comment: not blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Comment: unable to assess fully from information presented within the report |
| Selective reporting (reporting bias) | High risk | Comment: not all outcomes reported on e.g. David classification |
| Other bias | Unclear risk | Limited information provided pertaining to the nursing staff participants; potential publication bias |
| Methods | Study design: 2‐group parallel‐RCT using repeated‐measures design Ethics and informed consent: not stated Sample size calculation: yes ITT analysis: yes | |
| Participants | Location: 58 nursing homes in Missouri, USA Inclusion criteria: nursing homes in need of improvement Specifically, homes were required to improve resident outcomes of care as per the minimum data set (MDS) quality improvement scores above the 40th percentile on at least 3 of 4 selected resident outcome measures for 2 consecutive 6‐month periods of MDS data. The 4 selected resident outcome measures were: bowel and bladder incontinence; weight loss; pressure ulcers and decline in activities of daily living. Exclusion criteria: not specified | |
| Interventions | Aim: to test an experimental intervention focused on building organisational capacity to create and sustain improvement in quality of care and improve resident outcomes Group A: multilevel intervention targeted at 3 levels of staff: nursing home owners and administrative staff, nursing, and direct‐care staff (n = 29 nursing homes) Group B: attention control (n = 29 nursing homes) Multilevel intervention included: educational materials comprising a detailed intervention manual, quality improvement tools and two text books provided to leadership of each nursing home. Monthly on‐site consultation from a research nurse of 1‐4 hours duration. Nursing home owners were asked to provide consistent nursing and administrative leadership, to adopt elements of change into their management practices, and to support and encourage the use of team and group processes for (1) decision‐making affecting resident care; (2) use of a quality improvement programme; (3) efforts of staff to focus on care basics including preventing skin breakdown, ambulation, nutrition, hydration, toileting, bowel and pain management. Attention control comprised: educational materials sent to the home on a monthly basis including video‐taped, in‐service training and reading material about ageing and physical assessment of elderly residents alongside monthly telephone support from the co‐principal investigator. Study date: not stated | |
| Outcomes | Primary outcome: odds ratio of pressure ulcer development stage 1‐4 Secondary outcome: none measured Time points: baseline, 1 year post baseline, 2 years post baseline | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "we first randomly assigned owners of facilities in the population of qualified facilities to either intervention or control groups. Then, we randomly contacted qualified facilities to participate and, when they agreed, assigned them to the group designation based on owner. We continued random assignment until the groups were full" (p 61) Comment: the method of generating the randomisation sequence was not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not reported |
| Blinding of participants and personnel (performance bias) | Unclear risk | Comment: not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "collected by an independent nurse observer (blind to the intervention) at baseline and at the end of years 1 and 2 in the intervention group and end of year 2 in the control group" (p 62) Comment: outcome assessment blinded |
| Incomplete outcome data (attrition bias) | High risk | Response rates were low on "Tell us about your Nursing Home" survey (intervention group 71% baseline & 63% study end; control group 65% baseline; 53% control) |
| Selective reporting (reporting bias) | Low risk | Comment: outcomes reported on fully |
| Other bias | Low risk | None detected |
| Methods | Study design: 2‐group cluster‐RCT Ethics and informed consent: ethical approval gained, informed consent not stated Sample size calculation: no ITT analysis: no | |
| Participants | Location: 20 wards from 4 hospitals and 6 nursing homes in the Netherlands Mean age: hospital ward nurses 38 years (SD 10.7 years); nursing home ward nurses 39 years (SD 10.2 years) Gender: hospital ward nurses 89% female; nursing home ward nurses 96% female Inclusion criteria: none specified Exclusion criteria: none specified | |
| Interventions | Aim: to investigate the effect of interactive and tailored education on the knowledge levels of nurses Group A: educational intervention based upon the patient safety programme (n = 5 nursing home wards and n = 5 hospital wards) Group B: no educational intervention (n = 5 nursing home wards and n = 5 hospital wards) Education intervention: each nurse attended a small scale educational meeting lasting approx 1.5 hours based upon guidelines for the prevention of pressure ulcers, urinary tract infections and falls, accessed an educational CD containing theoretical information and feedback test, and attended researcher‐facilitated follow‐up case discussions at ward‐level every 2‐3 months. Appointment of 2 key nurses at each site to champion implementation of intervention and avail of two, 5‐hour outreach visits and periodic contact with the researcher Study date: September 2006‐July 2008 | |
| Outcomes | Primary outcomes: 20‐item knowledge test on pressure ulcers Secondary outcomes: none measured Time points: baseline and 1 year post‐baseline | |
| Notes | As nurses' characteristics differed between hospitals and nursing homes, the data were analysed for hospital wards and nursing home wards separately | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomisation of the wards was stratified for centre and type of ward" Comment: the method of generating the randomisation sequence was not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: not reported |
| Blinding of participants and personnel (performance bias) | High risk | Comment: participants will have known whether they were in the experimental or control group based upon whether they received the educational intervention so blinding unlikely. |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "at each ward, one nurse was responsible for the distribution and collection of the questionnaires" Comment: it is likely that this nurse knew group allocation |
| Incomplete outcome data (attrition bias) | High risk | Low response and high attrition rates noted in study Intervention group of hospital nurses' cohort (80% response rate at baseline; 49% response rate study end) Control group of hospital nurses' cohort (72% response rate at baseline; 87% response rate study end) Intervention group of nursing ward nurses' cohort (66% response rate baseline; 58% response rate study end) Control group of nursing ward nurses' cohort (71% response rate baseline; 56% response rate study end) |
| Selective reporting (reporting bias) | Low risk | Comment: outcomes reported on fully |
| Other bias | Unclear risk | Comment: outcome measured using a non‐standardised assessment measure |
| Recruitment bias (cluster trials only) | Low risk | Quote: "all registered and licensed nurses working within the 20 participating wards were invited to participate in the study" ... "in our study the intervention involved the entire team of nurses and not individual nurses on nursing wards" Comment: recruitment bias unlikely to be a source of bias |
| Baseline imbalance (cluster trials only) | Low risk | Quote: "prior to baseline, randomisation of the wards to an intervention or control group was stratified for centre and type of ward" Comment: potential baseline imbalance accounted for through stratification of clusters |
| Loss of clusters (cluster trials only) | Low risk | No loss of clusters at end point; risk of bias arising from missing outcome data for individuals within clusters appraised as incomplete outcome data (attrition bias) Comment: all clusters remained within the trial |
| Incorrect analysis (cluster trials only) | Low risk | Quote: "the results were analysed for hospitals and nursing homes separately" ... "we used a linear random effects model to analyse the difference in the results on the knowledge test between the intervention and the control wards at follow‐up. This model was used because of the hierarchical structure of the data (nurses were clustered within wards) Comment: statistical analysis took account of clustering |
DTI: deep tissue injury; F: female; ITT: intention‐to‐treat; LPN: licensed practical nurse; M: male; NPUAP:National Pressure Ulcer Advisory Panel; RCT: randomised controlled trial; RN: registered nurse
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| Study design: not a RCT | |
| Study design: not a RCT | |
| Study purpose: educational focus on quality improvement reporting and report interpretation | |
| Study design: invalid comparison. Both cohorts received educational intervention |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Jump to:
| Trial name or title | The effect of pressure ulcer management educational program on the performance of nurses in the care of patients admitted to the intensive care unit |
| Methods | 2 arm RCT |
| Participants | 70 nurses working in intensive care unit |
| Interventions | A pressure ulcer management training programme including a learning workshop, educational leaflet and CD for nurses |
| Outcomes | Primary: nurses' performance. |
| Starting date | Trial registration date October 2017 (IRCT2017080935602N1) apps.who.int/trialsearch |
| Contact information | Estimated end date of recruitment February 2018 |
| Notes |
| Trial name or title | Study protocol of a cluster randomised controlled trial evaluating the efficacy of a comprehensive pressure ulcer prevention programme for private for‐profit nursing homes |
| Methods | Cluster‐RCT |
| Participants | 8 private, for‐profit nursing homes |
| Interventions | A comprehensive pressure ulcer prevention programme defined as including an intensive training course and a pressure ulcer protocol |
| Outcomes | Primary: incidence and prevalence of pressure ulcers. Secondary: care staff's knowledge and skills on pressure ulcer prevention |
| Starting date | Trial registration date October 2014 (NCT02270385) clinicaltrials.gov |
| Contact information | Estimated end date December 2017 |
| Notes |
RCT: randomised controlled trial
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Knowledge hospital group Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1 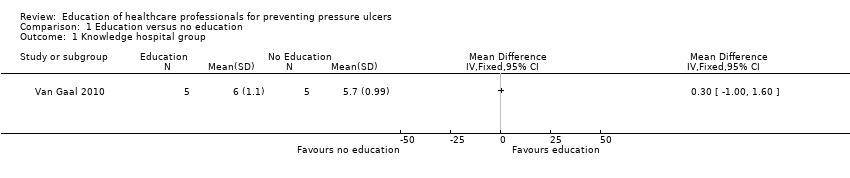 Comparison 1 Education versus no education, Outcome 1 Knowledge hospital group. | ||||
| 2 Knowledge nursing‐home group Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Education versus no education, Outcome 2 Knowledge nursing‐home group. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1  Comparison 2 Training, monitoring and observation vs monitoring and observation, Outcome 1 Pressure ulcer developed. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 Training monitoring and observation vs observation alone, Outcome 1 Pressure ulcer developed. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 4.1  Comparison 4 Monitoring and observation vs observation alone, Outcome 1 Pressure ulcer developed. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Knowledge Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 5.1  Comparison 5 Education via didactic lecture versus video, Outcome 1 Knowledge. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Correct classification of pressure ulcer photographs Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 6.1 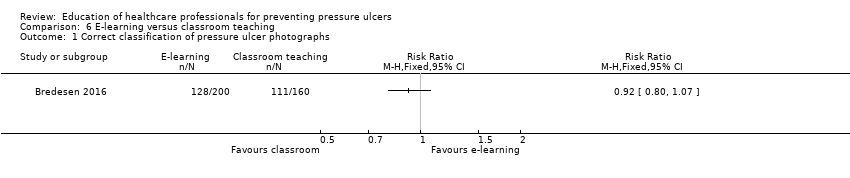 Comparison 6 E‐learning versus classroom teaching, Outcome 1 Correct classification of pressure ulcer photographs. | ||||

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
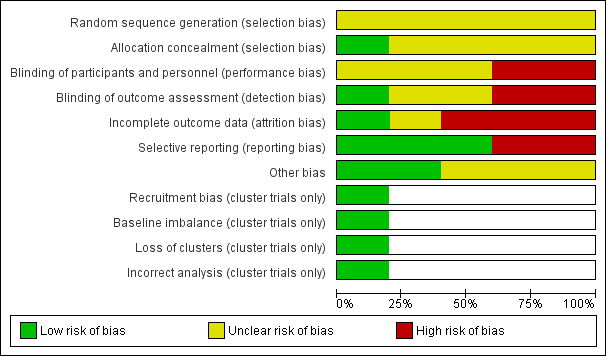
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
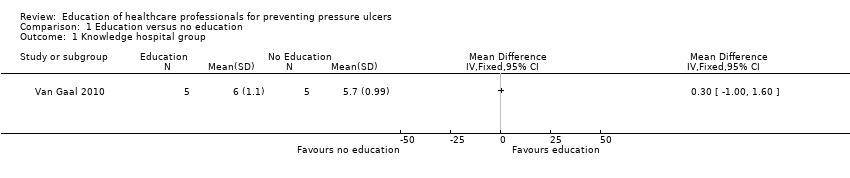
Comparison 1 Education versus no education, Outcome 1 Knowledge hospital group.

Comparison 1 Education versus no education, Outcome 2 Knowledge nursing‐home group.

Comparison 2 Training, monitoring and observation vs monitoring and observation, Outcome 1 Pressure ulcer developed.

Comparison 3 Training monitoring and observation vs observation alone, Outcome 1 Pressure ulcer developed.

Comparison 4 Monitoring and observation vs observation alone, Outcome 1 Pressure ulcer developed.

Comparison 5 Education via didactic lecture versus video, Outcome 1 Knowledge.
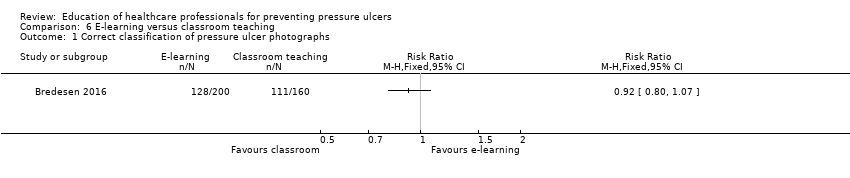
Comparison 6 E‐learning versus classroom teaching, Outcome 1 Correct classification of pressure ulcer photographs.
| Education compared to no education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| No education | Education | |||||
| Knowledge in hospital group | Mean knowledge score with no education was 5.7 | Mean knowledge score was 0.30 units higher (1.0 lower to 1.6 higher) | 10 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in health professionals' knowledge depending on whether they receive education or no education on pressure ulcer prevention | |
| Knowledge in nursing‐home group | Mean knowledge score with no education was 5.1 | Mean knowledge score was 0.30 units higher (0.77 lower to 1.37 higher) | 10 | ⊕⊝⊝⊝ | ||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded four times: serious limitations due to performance bias, detection bias and attrition bias; indirectness due to use of a non validated instrument to assess knowledge; serious imprecision due to a wide confidence interval and small sample size. | ||||||
| Training, monitoring and observation compared to monitoring and observation for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Monitoring and observation | Training, monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 0.63 | 345 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with monitoring and observation | |
| 183 per 1000 | 115 per 1000 | |||||
| Severity of new pressure ulcers | No data were presented by the study author | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Training, monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Training monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.21 | 325 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as training, monitoring and observation compared with observation alone | |
| 94 per 1000 | 114 per 1000 | |||||
| Severity of new pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer‐reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitations due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Monitoring and observation compared to observation alone for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Observation alone | Monitoring and observation | |||||
| Change in health professionals' knowledge | Not reported | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Study population | RR 1.93 | 232 | ⊕⊝⊝⊝ | It is uncertain whether there is a difference in pressure ulcer incidence when using different components of educational intervention such as monitoring and observation compared with observation alone | |
| 94 per 1000 | 182 per 1000 | |||||
| Severity of new pressure ulcers | No data are presented by the study author | |||||
| Patient reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| Carer reported outcomes | Insufficient data within the study report to further interrogate this outcome | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: very serious limitation due to performance, detection and reporting bias; serious imprecision due to wide confidence interval. | ||||||
| Education versus video for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Comparison: didactic lecture | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Didactic education | Video education | |||||
| Change in health professionals' knowledge | Mean knowledge score with didactic education was 84.62 | Mean knowledge score was 4.60 units higher (3.8 units to 6.12 units higher) | 102 | ⊕⊝⊝⊝ | It is uncertain whether education delivered in different formats such as didactic or video‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitation due to unclear risk of selection, performance and detection bias; very serious imprecision due to small sample size and wide confidence intervals. | ||||||
| E‐learning compared with classroom education for preventing pressure ulcers | ||||||
| Patient or population: staff caring for patients at risk of pressure ulcers Settings: hospitals and nursing homes Intervention: e‐learning Comparison: classroom education | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Classroom education | E‐learning | |||||
| Knowledge of pressure ulcer classification | Study population | RR 0.92 (0.80 to 1.07) | 18 participants | very low1 | It is uncertain whether education delivered in different formats such as e‐learning or classroom‐based format makes a difference to health professionals' knowledge of pressure ulcer prevention | |
| 694 per 1000 | 638 per 1000 | |||||
| Change in health professionals' clinical behaviour | Not reported | |||||
| Incidence of new pressure ulcers | Not reported | |||||
| Severity of pressure ulcers | Not reported | |||||
| Patient‐reported outcomes | Not reported | |||||
| Carer‐reported outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
| 1Downgraded three times: serious limitations due to high risk of attrition and selective reporting bias; unclear risk of performance, selection, detection and other bias; serious imprecision due to small sample size and wide confidence intervals. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Knowledge hospital group Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Knowledge nursing‐home group Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Pressure ulcer developed Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Knowledge Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Correct classification of pressure ulcer photographs Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |


