Probiotics for vulvovaginal candidiasis in non‐pregnant women
Abstract
Background
Vulvovaginal candidiasis (VVC) is estimated to be the second most common form of infection after bacterial vaginosis. The ability of probiotics in maintaining and recovering the normal vaginal microbiota, and their potential ability to resist Candidas give rise to the concept of using probiotics for the treatment of VVC.
Objectives
To assess the effectiveness and safety of probiotics for the treatment of vulvovaginal candidiasis in non‐pregnant women.
Search methods
We searched the following databases to October 2017: Sexually Transmitted Infections Cochrane Review Group's Specialized Register, CENTRAL, MEDLINE, Embase and eight other databases. We searched in following international resources: World Health Organization International Clinical Trials Registry Platform, ClinicalTrials.gov, Web of Science and OpenGrey. We checked specialty journals, reference lists of published articles and conference proceedings. We collected information from pharmaceutical companies and experts in the field.
Selection criteria
Randomized controlled trials (RCT) using probiotics, alone or as adjuvants to conventional antifungal drugs, to treat VVC in non‐pregnant women. Trials recruiting women with recurrent VVC, coinfection with other vulvovaginal infections, diabetes mellitus, immunosuppressive disorders or taking immunosuppressant medication were ineligible for inclusion. Probiotics were included if they were made from single or multiple species and in any preparation type/dosage/route of administration.
Data collection and analysis
Two review authors independently assessed trials for eligibility and quality and extracted data. We resolved any disagreements through consensus. The quality of the evidence was assessed using the GRADE approach.
Main results
Ten RCTs (1656 participants) met our inclusion criteria, and pharmaceutical industry funded none of these trials. All trials used probiotics as adjuvant therapy to antifungal drugs. Probiotics increased the rate of short‐term clinical cure (risk ratio (RR) 1.14, 95% confidence interval (CI) 1.05 to 1.24, 695 participants, 5 studies, low quality evidence) and mycological cure (RR 1.06, 95% CI 1.02 to 1.10, 969 participants, 7 studies, low quality evidence) and decreased relapse rate at one month (RR 0.34, 95% CI 0.17 to 0.68, 388 participants, 3 studies, very low quality evidence). However, this effect did not translate into a higher frequency of long‐term clinical cure (one month after treatment: RR 1.07, 95% CI 0.86 to 1.33, 172 participants, 1 study, very low quality evidence; three months after treatment: RR 1.30, 95% CI 1.00 to 1.70, 172 participants, one study, very low quality evidence) or mycological cure (one month after treatment: RR 1.26, 95% CI 0.93 to 1.71, 627 participants, 3 studies, very low quality evidence; three months after treatment: RR 1.16, 95% CI 1.00 to 1.35, 172 participants, one study, very low quality evidence). Probiotics use did not increase the frequency of serious (RR 0.80, 95% CI 0.22 to 2.94; 440 participants, 2 studies, low quality evidence). We found no eligible RCTs for outcomes as time to first relapse, need for additional treatment at the end of therapy, patient satisfaction and cost effectiveness.
Authors' conclusions
Low and very low quality evidence shows that, compared with conventional treatment, the use of probiotics as an adjuvant therapy could increases the rate of short‐term clinical and mycological cure and decrease the relapse rate at one month but this did not translate into a higher frequency of long‐term clinical or mycological cure. Probiotics use does not seem to increase the frequency of serious or non‐serious adverse events. There is a need for well‐designed RCTs with standardized methodologies, longer follow‐up and larger sample size.
PICOs
Plain language summary
Probiotics for vulvovaginal candidiasis in non‐pregnant women
Question
In this Cochrane Review, we assessed the effect and safety of probiotics for the treatment of vulvovaginal candidiasis (VVC) in non‐pregnant women compared with conventional antifungal drugs, or probiotics used to change the effects of conventional antifungal drugs.
Background
The condition of VVC occurs because of an imbalance in the normal vaginal microorganism habitat (microbiota). It is characterized by a decrease of a type of bacteria called lactobacilli and a concomitant overgrowth of a fungus called Candida. Although treatments for VVC by conventional antifungal drugs are quite effective at providing clinical cure (no apparent vaginal symptoms), there is an increasing in resistance to the drugs and recurrence of VVC. Conventional antifungal drugs can also cause many side effects. Probiotics are microorganisms that are believed to provide health benefits when consumed. The ability of probiotics in maintaining and recovering the normal vaginal microbiota, and their potential ability to resist Candidas gives rise to the concept of using probiotics for the treatment of VVC. We wanted to find out whether using probiotics could be useful in treating VVC in non‐pregnant women without high risk or side effects.
Study characteristics
We searched evidence up to October 2017 and included 10 clinical trials with 1656 participants. The trials lasted between three months and five years. All trials used at least one laboratory method for diagnosis. Four trials compared vaginal suppository (solid medicine inserted directly into the vagina) or tablet of clotrimazole (antifungal medicine) plus vaginal capsules of probiotics with vaginal suppository or tablet of clotrimazole alone. Three trials compared vaginal suppository of miconazole (antifungal medicine) plus vaginal capsules of probiotics with vaginal suppository of miconazole alone. Two trials compared oral fluconazole (antifungal medicine) plus oral capsules of probiotics with oral fluconazole plus oral capsules of placebo (pretend treatment). One trial compared oral fluconazole and vaginal fenticonazole (antifungal medicines) with oral fluconazole plus vaginal fenticonazole plus probiotic.
Key results
Compared with conventional antifungal drugs used alone, probiotics as adjuvant therapy could enhance their effect in improving the rate of short‐term (within five to 10 days) clinical cure, short‐term mycological cure (no abnormal laboratory results) and relapse at one month (recurrence of problems), but does not seem to influence the rate of long‐term (within one to three months) clinical cure, long‐term mycological cure, serious and non‐serious side events.
However, because of the low quality of evidence available, there is insufficient evidence for the use of probiotics as adjuvants to conventional antifungal medicines or used alone for the treatment of VVC in non‐pregnant women.
Quality of the evidence
The quality of the evidence was low or very low in this review, so we have very little confidence in the results.
Authors' conclusions
Summary of findings
| Probiotics used as adjuvants to conventional antifungal drugs compared with conventional antifungal drugs for the treatment of vulvovaginal candidiasis in non‐pregnant women | |||||||
| Patient or population: non‐pregnant women with vulvovaginal candidiasis Settings: outpatient clinics in Brazil, Bulgaria, Iran and China Intervention: probiotics used as adjuvants to conventional antifungal drugs Comparison: conventional antifungal drugs | |||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | ||
| Assumed risk | Corresponding risk | ||||||
| Conventional antifungal drugs | Probiotics used as adjuvants to conventional antifungal drugs | ||||||
| Clinical cure rate (short‐term) follow‐up: 5‐10 days | Medium risk population | RR 1.14 (1.05 to 1.24) | 695 | ⊕⊕⊝⊝ | ‐ | ||
| 721 per 1000 | 822 per 1000 | ||||||
| Clinical cure rate (long‐term) | 1 month after treatment follow‐up: 1 month | Medium risk population | RR 1.07 (0.86 to 1.33) | 172 | ⊕⊝⊝⊝ | ‐ | |
| 635 per 1000 | 679 per 1000 | ||||||
| 3 months after treatment follow‐up: 3 months | Medium risk population | RR 1.30 (1.00 to 1.70) | 172 | ⊕⊝⊝⊝ | ‐ | ||
| 494 per 1000 | 642 per 1000 | ||||||
| Mycological cure rate (short‐term) follow‐up: 5‐10 days | Medium risk population | RR 1.06 (1.02 to 1.10) | 969 | ⊕⊕⊝⊝ | See 3 in footnotes. | ||
| 880 per 1000 | 933 per 1000 | ||||||
| Mycological cure rate (long‐term) | 1 month after treatment follow‐up: 28‐30 days | Medium risk population | RR 1.26 (0.93 to 1.71) | 627 | ⊕⊝⊝⊝ | See 5 in footnotes. | |
| 706 per 1000 | 890 per 1000 | ||||||
| 3 months after treatment follow‐up: 3 months | Medium risk population | RR 1.16 (1.00 to 1.35) | 172 | ⊕⊝⊝⊝ | ‐ | ||
| 741 per 1000 | 860 per 1000 | ||||||
| Relapse rate follow‐up: 30‐37 days after treatment | Medium risk population | RR 0.34 (0.17 to 0.68) | 388 | ⊕⊝⊝⊝ | ‐ | ||
| 145 per 1000 | 49 per 1000 | ||||||
| Rate of serious adverse events follow‐up: 5‐90 days after treatment | Medium risk population | RR 0.80 (0.22 to 2.94) | 440 | ⊕⊕⊝⊝ | ‐ | ||
| 23 per 1000 | 18 per 1000 | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1Downgraded two levels due to very serious risk of bias: the included studies had a high or unclear risk of bias in at least one key domain i.e. random sequence generation, allocation concealment or blinding. 2Downgraded one level due to serious imprecision: the 95% CI were wide and included null effects. 3A sensitivity analysis that excluded studies with high risk of bias and included only one study showed that the rate of short‐term mycological cure was changed to no significantly difference between two arms. For the heterogeneity and difference in results, we think the reasons may be associated with the small sample of included study, high risk of bias of studies that were excluded for sensitivity analysis. 4Downgraded one level due to inconsistency: there was a substantial heterogeneity between studies. 5There was heterogeneity that may be attributable to differences in route of the administration of probiotics, we undertook a subgroup analysis, the results showed no statistically significant difference between two arms in either subgroup. 6Downgraded one level due to serious imprecision: small sample size and few events. | |||||||
Background
Description of the condition
Epidemiology
Vaginitis is one of the most common reasons for women to seek medical assistance from obstetrician and gynecologists (Nyirjesy 2008). Vulvovaginal candidiasis (VVC) is estimated to be the second most common form of vaginal infection after bacterial vaginosis (Sobel 2007; Martinez 2009a). Data about the incidence of VVC are limited and incomplete, since it is not a reportable disease and is often diagnosed without mycological confirmatory (fungi identified) tests and treated with non‐prescription drugs (Sobel 1998; Nyirjesy 2003). Misdiagnosis is common, and it has been shown that about two‐thirds of all non‐prescription drugs for VVC are used without the disease, and that women who overused non‐prescription antifungal drugs, may increase the risk of resistance to antifungal treatments (Sobel 1998; Sobel 2007; Nyirjesy 2008).
Approximately 70% to 75% of women experience at least one episode of VVC in their lives (Sobel 1998; Sobel 2007). Age appears to be an important factor in the overall incidence of VVC because episodes occur mostly during childbearing years and rarely in premenarchal and postmenopausal years (Sobel 1998; Sobel 2007). Approximately 40% to 45% of women will experience two or more episodes of VVC in one year (Sobel 2007; Nyirjesy 2008). One epidemiological study indicated that the frequency of the first diagnosis of VVC increased rapidly after 17 years of age. By the age of 25 years, 54.7% of female college students experienced at least one episode of physician‐diagnosed VVC (Geiger 1995). Recurrent VVC (RVVC) is defined as four or more episodes in one year, and affects 5% to 8% of adult women (Foxman 1998; Sobel 1998; Falagas 2006; Sobel 2007; Nyirjesy 2008). It is reported that the incidence of VVC almost doubled from 1980 to 1990, based on the number of prescriptions written to treat VVC during that period (Sobel 2007). The annual combined cost of health care and lost productivity due to VVC in the US was estimated to be USD1.8 billion, and is projected to reach USD3.1 billion by 2014 (Foxman 2000).
Pathology
The vaginal microenvironment is a complex microecological system, and Lactobacillus is the most commonly dominant flora (the aggregate of bacteria, fungi or other microorganisms) in the vaginal microecological system (Redondo‐Lopez 1990; Kledanoff 1991; Sobel 2007). In normal conditions, vaginal lactobacilli produce lactic acid, thus acidifying the healthy vagina to a low pH level (4.5 or less), which could inhibit the overgrowth of other pathogenic bacteria or Candida (Redondo‐Lopez 1990; Kledanoff 1991). Many species of Lactobacillus also produce other substances, such as hydrogen peroxide and bacteriocin, which further prevent the overgrowth of the pathogenic microbes (Redondo‐Lopez 1990; Kledanoff 1991; Sobel 1998; Jeavons 2003; Nyirjesy 2003; Sobel 2007).
The condition of VVC occurs as a result of an imbalance in the normal vaginal microbiota (the group of microbe) and is characterized by a decrease or depletion of the lactobacilli species and a concomitant overgrowth of Candida species, epidemiological research has shown that Candida organisms can be found in approximate 20% of asymptomatic healthy women (Sobel 2007). Candida organisms gain access to the vaginal lumen and discharge mainly from the adjacent perianal area, effective anti‐Candida defense in the microenvironment of the vagina allows candidal microbes to persist as an avirulent commensal (Bertholf 1983; Beigi 2004; Sobel 2007; Nyirjesy 2008). There are two potential elements during the development of symptomatic VVC: the first is the Candida species' vaginal colonization, adhesion, invasion and growth, and the second is the transformation from the asymptomatic to the symptomatic phase (Sobel 2007; Nyirjesy 2008). Candida enters the vagina through different sources, including local spread from the perineum (the area in front of the anus extending to the fourchette of the vulva) and gastrointestinal tract, digital introduction and unclean sexual activity (Sobel 2007; Nyirjesy 2008). Estrogen is believed to be crucial in the maintenance of colonization (Hillier 1997). The penetrative ability of hyphae enhances the colonization by the adherence to vaginal epithelial cells (Redondo‐Lopez 1990; Ross 1995; Sobel 2007; Nyirjesy 2008). One study indicated that Candida albicans adheres in significantly higher numbers to vaginal epithelial cells than non‐albicans Candida species (Soll 1989). The Candida strains isolated from the vaginas of women with VVC are mainly Candida albicans, while the rest (range 5% to 15%) are non‐albicans Candida species. Candida glabrata is considered the most common of non‐albicans Candida species (Nyirjesy 2008). However, vulvovaginitis induced by non‐albicans Candida cannot be distinguished clinically from that caused by Candida albicans. RVVC is often caused by non‐albicans Candida, which are frequently more resistant to conventional antifungal treatment (Spinillo 1994; Ross 1995; Sobel 2007; Nyirjesy 2008). Some studies have shown that the widespread and long‐term use of antifungal drugs such as azoles, particularly fluconazole, may lead to a pathogen shift and increase the incidence of the non‐albicans Candida such as Candida glabrata, and the extensive use of azoles may effectively suppress Candida albicans but facilitate the overgrowth of non‐albicans Candida (Sanglard 2002; Hettiarachchi 2010; Mahmoudi 2011). Depressed or reduced protective local immunoregulatory mechanisms, cytokine (any of several non‐antibody proteins, released by a cell population on contact with a specific antigen and act as intercellular mediators, as in the generation of an immune response) elaboration and certain genetic polymorphisms may result in increased susceptibility to RVVC (Giraldo 2007).
The overuse of antibiotics; pregnancy; diabetes mellitus; immunosuppression; frequent and unclean sexual activity; use of oral contraceptives, diaphragms, spermicide and intrauterine devices; and vaginal douching are considered important risk factors for the development of VVC and RVVC (Sobel 1998; Nyirjesy 2003; Sobel 2007; Nyirjesy 2008).
VVC can be classified as uncomplicated VVC and complicated VVC (Sobel 2007; Nyirjesy 2008; CDC 2015).
-
Uncomplicated VVC is defined by:
-
sporadic or infrequent VVC, or
-
mild‐to‐moderate VVC, or
-
likely to be Candida albicans infection, or
-
non‐immunocompromised host.
-
-
Complicated VVC is defined by:
-
four or more episodes of candidiasis per year (RVVC), or
-
severe symptoms or findings (severe VVC), or
-
non‐albicans Candida infection, or
-
abnormal host (e.g. uncontrolled diabetes, debilitation or immunosuppression).
-
Diagnosis
A combination of clinical signs and symptoms, microscopic examination, vaginal culture, or a combination of these is used to diagnose VVC; although acute pruritus and vaginal discharge are the common clinical symptoms of VVC, neither of them is specific (Anderson 2004; Sobel 2007). The typical vaginal discharge has been described as 'cottage‐cheese‐like,' and in practice it could vary from watery to thick (Sobel 2007). Women with VVC may also complain of irritation, soreness, vulvar burning or dyspareunia. Occasionally, VVC can cause external dysuria (difficult or painful urination) by the burning that occurs when urine hits the inflamed vulvar tissues (Eckert 1998). If there is an odor, it is generally insignificant and inoffensive (Sobel 2007). Clinical symptoms may recur or exacerbate in the week before menstruation (Schaaf 1990; Anderson 2004; Sobel 2007). On vulvar examination, women may exhibit erythema (redness of the skin caused by dilation and congestion of the capillaries, often a sign of inflammation or infection), swelling, fissures, or excoriations of the labia and vulva, and vaginal signs of erythema or an adherent curd‐like vaginal discharge may be found (Sobel 1998; Nyirjesy 2003; Sobel 2007; Nyirjesy 2008).
Most women with symptoms of VVC can be easily diagnosed when:
-
saline and 10% potassium hydroxide microscopy examination or Gram stain (63.2% to 65% sensitivity, 97.2% to 100% specificity (Omar 2001; Ilkit 2011)) of vaginal discharge demonstrates Candida species, hyphae or pseudohyphae; or
-
a vaginal culture test yields a Candida species (Sobel 1998; Sobel 2007; Nyirjesy 2008; CDC 2015).
Because Candida vaginitis is associated with a normal vaginal pH (less than 4.5), pH testing is not useful for diagnosis, but the finding of a normal pH helps to exclude bacterial vaginosis, trichomoniasis, atrophic vaginitis or some type of mixed infection (Nyirjesy 2008; CDC 2015).
The 10% potassium hydroxide microscopy examination (50% to 85% sensitivity) should be taken for all women with symptoms or signs of VVC, and women with a positive result should receive treatment (Ilkit 2011; Mylonas 2011). The gold standard for diagnosis is still the growth of the infecting organism in fungal culture on Sabouraud dextrose agar (Ilkit 2011). Up to 50% of women with culture‐positive symptomatic vulvovaginal candidiasis will have negative microscopy (Sobel 2007), so, although routine cultures are not necessary if microscopy is positive, vaginal culture should be performed for women with a negative microscopy result and a normal pH and who are symptomatic (Sobel 2007; CDC 2015). Vaginal culture is useful to identify the species of Candida (Bieber 2006). For women with complicated VVC, vaginal culture can guide the choice of therapy regimen, since non‐albicans species tend to be resistant to the azole drugs (Bieber 2006; Nyirjesy 2008). Table 1 lists species of Candida isolated from the lower genital tract in women with VVC. Candida identified by vaginal culture in the absence of symptoms or signs is not an indication for treatment, because many women harbor Candida species in the vagina. If the 10% potassium hydroxide examination is negative and vaginal culture cannot be performed, an empiric treatment may be considered for symptomatic women with any sign of VVC on examination (CDC 2015).
| Species | Frequency | Response to azoles |
| Candida albicans | 80‐90% | Sensitive |
| Candida glabrata | 5‐10% | Resistant |
| Candida krusei | < 1% | Tends to be resistant |
| Candida lusitaniae | < 1% | Tends to be resistant |
| Candida parapsilosis | < 1% | Tends to be resistant |
| Candida pseudotropicalis | < 1% | Tends to be resistant |
| Candida tropicalis | < 1% | Tends to be resistant |
Source: Bieber 2006.
Although polymerase chain reaction (PCR) testing for Candida species is available, its usefulness is limited because it depends on obtaining PCR for the full spectrum of organisms that can cause VVC, with the associated costs (Trama 2005).
Description of the intervention
The recommended treatments for uncomplicated VVC involve a short course of antifungal drugs (Nurbhai 2007; Pappas 2009; CDC 2015). Table 2 lists the Centers for Disease Control (CDC)‐recommended treatments for uncomplicated VVC (CDC 2015). The oral and topical preparations have similar effects (Pappas 2009; CDC 2015), and treatment with azole drugs results in relief of symptoms and negative cultures in 80% to 90% of women who complete therapy (CDC 2015). The recommended treatments for complicated VVC involve an intensive, longer course of antifungals. Table 3 lists the CDC‐recommended treatments for complicated VVC (CDC 2015).
| Non‐prescription intravaginal agents | Prescription intravaginal agents |
| Butoconazole 2% cream 5 g intravaginally for 3 days OR Clotrimazole 1% cream 5 g intravaginally for 7‐14 days OR Clotrimazole 2% cream 5 g intravaginally for 3 days OR Miconazole 2% cream 5 g intravaginally for 7 days OR Miconazole 4% cream 5 g intravaginally for 3 days OR Miconazole 100 mg vaginal suppository, 1 suppository for 7 days OR Miconazole 200 mg vaginal suppository, 1 suppository for 3 days OR Miconazole 1200 mg vaginal suppository, 1 suppository for 1 day OR Tioconazole 6.5% ointment 5 g intravaginally in a single application | Butoconazole 2% cream (single dose bioadhesive product), 5 g intravaginally for 1 day OR Nystatin 100,000 unit vaginal tablet, 1 tablet for 14 days OR Terconazole 0.4% cream 5 g intravaginally for 7 days OR Terconazole 0.8% cream 5 g intravaginally for 3 days OR Terconazole 80 mg vaginal suppository, 1 suppository for 3 days |
CDC: Centers for Disease Control and Prevention.
Source: CDC 2015.
| Recurrent vulvovaginal candidiasis | |
| Initial regimen: 7‐14 days of any topical azole drug OR Fluconazole 100 mg, 150 mg or 200 mg orally once daily every 3rd day for a total of 3 doses (days 1, 4 and 7) | Maintenance regimen: Fluconazole 100 mg, 150 mg or 200 mg orally once weekly for 6 months |
| Severe vulvovaginal candidiasis | |
| Intravaginally once daily for 7 to 14 days of any topical azole drug OR Fluconazole 150 mg orally once daily in 2 doses (second dose 72 hours after initial dose) | |
| Non‐albicans vulvovaginal candidiasis | |
| Non‐fluconazole azole (oral or topical) 7‐14 days OR Boric acid gelatin capsule Intravaginally once daily for 14 days | |
| Abnormal host | |
| More prolonged (i.e. 7‐14 days) conventional antifungal drugs is necessary | |
CDC: Centers for Disease Control and Prevention.
Source: CDC 2015.
Azole antifungals are a group of fungistatic agents with broad‐spectrum activity in treating systemic and topical fungal infections. They are classified into two groups: triazoles and imidazoles (Nurbhai 2007; CDC 2015). One Cochrane systematic review showed that both imidazole and triazole antifungal treatment (by oral or intravaginal route of administration) achieved clinical cure in over 80% of women (Nurbhai 2007). However, they can cause many adverse effects, including vomiting, diarrhea, abdominal pain, urination, pelvic cramps, paresthesia, rhinorrhea, headache, dizziness, fever, chills, vaginal burning, stinging, itching and irritation (Nurbhai 2007; CDC 2015); more systemic adverse effects are likely to be reported with oral compared with intravaginal antifungal administration (Nurbhai 2007). For the half‐life, duration and any known interactions with other drugs of all azole antifungals for VVC, we recommend following this Merck Manual (www.merckmanuals.com), to reference further information.
Probiotics confer a wide range of effects, and have been used for the prevention and treatment of various medical conditions and to support wellness. Some of their effects against diarrheal diseases, Crohn disease, ulcerative colitis, irritable bowel syndrome, bacterial vaginosis, VVC and urinary tract infections have been validated (Reid 2005; Senok 2005; Doron 2006; Santosa 2006; Sanders 2008; Senok 2008). Probiotics are defined as live microorganisms that, when administered in adequate amounts, exert a health benefit on the host by treating and preventing diseases, they are regulated as dietary supplements and foods, consisting of bacteria or yeast, and they are available as capsules, tablets or powders, and may contain a single microorganism or a mixture of several species (Reid 2003a; Falagas 2006; Othman 2007; Sanders 2008). Table 4 lists common microorganisms used as probiotics (Kopp‐Hoolihan 2001; Senok 2005; Doron 2006; Santosa 2006). Products containing bacteria or yeast are not classified as probiotics, unless they have been shown to be viable and stable at the time of use in sufficient quantity to exert a health benefit. The organisms themselves must be speciated using appropriate molecular methods, and given a designation (Reid 2005; Senok 2005; Doron 2006; Santosa 2006; Vanderhoof 2008).
| Lactobacillus species: Lactobacillus acidophilus Lactobacillus bulgaricus Lactobacillus casei Lactobacillus crispatus Lactobacillus delbrueckii Lactobacillus fermentum Lactobacillus gasseri Lactobacillus johnsonii Lactobacillus lactis Lactobacillus plantarum Lactobacillus reuteri Lactobacillus rhamnosus GG | Streptococcus species: Streptococcus thermophilus
|
| Yeast: Saccharomyces boulardii
| |
| Other species: Bacillus cereus Enterococcus faecalisa Enterococcus faeciuma Escherichia coli Nissle
| |
| Bifidobacterium species: Bifidobacterium adolescentis Bifidobacterium animalis Bifidobacterium bifidum Bifidobacterium breve Bifidobacterium infantis Bifidobacterium lactis Bifidobacterium longum |
Sources: Senok 2005; Doron 2006; Santosa 2006.
Probiotics used in the prevention and treatment of Candida infections include Lactobacillus fermentum RC‐14, Lactobacillus fermentum B‐54, Lactobacillus rhamnosus GR‐1, Lactobacillus rhamnosus GG and Lactobacillus acidophilus (Reid 2001a; Jeavons 2003; Reid 2005; Falagas 2006; Martinez 2009a). Administration of probiotics can be oral, intravaginal or combined (Reid 2004). Probiotics are safe and effective for urogenital infections, with no severe adverse effects (Reid 2003b). The recommended dose is 109 to 1011 colony‐forming units of bacteria, by any route of administration (Reid 2003b; Andreu 2004). Probiotic preparations should not be taken together with bismuth preparations, tannic acid, activated charcoal or tincture. Because of the sensitivity of probiotics to antibiotics, they should not be taken together, to avoid dilution of their effectiveness (Zhang 2008).
How the intervention might work
The concept of treatment with probiotics stems from a belief that modern humans do not consume or replenish the beneficial microbes in their bodies, and that they can do so by taking probiotics (Reid 2005). The normal vaginal microenvironment is predominantly populated by Lactobacillus species, which tend to suppress growth of other bacterial species (Reid 2004). This dominance of lactobacilli and their potential ability to resist VVC gave rise to the concept of oral or vaginal instillation of probiotic Lactobacillus strains to restore the vaginal microbiotic balance. After the live bacteria in probiotic preparations have colonized the vagina, they grow and reproduce, and their metabolic substances can have toxic effects on Candida species (Reid 2001b; Reid 2001c; Reid 2003b). Evidence suggests that oral intake of probiotics leads to transfer of the organisms from the rectum to the vagina, as well as an overall depletion of coliforms and yeasts in the vagina (Reid 2001b; Reid 2001c; Reid 2003b). Certain probiotic strains, including Lactobacillus fermentum RC‐14 and Lactobacillus rhamnosus GR‐1, are able to remain in the vagina for several months after introduction.
The actual mechanism of action of probiotics in the vagina is probably multifactorial; they may block and prevent the Candida species' colonization, adhesion, invasion and growth by lactic acid, hydrogen peroxide and bacteriocin, which are toxic to Candida species (Reid 2003a; Reid 2003c; Reid 2004; Sobel 2007). In addition, probiotics may take the action of competitive exclusion, which is caused by a stronger affinity of Lactobacillus than pathogens to the receptors of the vaginal epithelial cells (Kaewsrichan 2006). The inflammatory temperance effect, provided by stable colonization with probiotics in the vagina, may help to regulate the vaginal immune environment (Fichorova 2011; Rose 2012). It has also been shown that Lactobacillus rhamnosus GR‐1 and Lactobacillus reuteri RC‐14 may directly influence the response of the vaginal epithelial cells to Candida albicans infections (Reid 2003c; Reid 2004; Martinez 2009b). After eliminating most of the Candidas, Lactobacillus could restore and maintain a normal vaginal microenvironment to prevent recurrence (Reid 2003a; Reid 2003c; Reid 2004; Reid 2005).
Why it is important to do this review
A growing number of women are troubled by the high prevalence and recurrence rates of VVC (Martinez 2009a). Although anticandidal agents are quite effective at providing clinical cure for VVC, resistance to the drugs is increasing. In addition, drugs may reduce the normal protective vaginal flora to increase the risk of recurrent infection, and can also cause many adverse effects (Nurbhai 2007; Martinez 2009a; CDC 2015). The increasing availability of probiotic products makes it important that family physicians understand what to look for when making recommendations (Reid 2005). The use of probiotics in augmenting normal bacterial populations is gradually achieving scientific acceptance (Reid 2003c). Probiotics have already been used for treatment of vulvovaginal inflammations in clinical practice (Reid 2001a; Reid 2003a; Reid 2003c; Othman 2007). Some evaluations have shown that probiotics are effective against VVC, and that their adverse effects are minor (Jeavons 2003; Falagas 2006; Martinez 2009a), while others demonstrated no efficacy in VVC (Pirotta 2004; Falagas 2006). There is no consensus on the use of probiotics for treating VVC (Jeavons 2003; Van Kessel 2003). Therefore, it is necessary to conduct a rigorous systematic review of the available clinical trials, to help determine the effectiveness and safety of probiotics for the treatment of VVC, and to identify strategic areas for future research.
Objectives
To assess the effectiveness and safety of probiotics for the treatment of vulvovaginal candidiasis in non‐pregnant women.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCT). We excluded quasi‐randomized trials because such trials produce effects estimates that indicate more extreme benefits when they are compared with RCTs (Higgins 2011). We excluded cross‐over trials because the carry over effect (Higgins 2011).
Types of participants
Non‐pregnant women diagnosed with VVC, regardless of age and race. Diagnosis of VVC was confirmed by the presence of clinical symptoms and signs, and a positive microscopic examination or positive vaginal culture, or both.
We excluded trials of women with RVVC, diabetes mellitus, immunosuppressive disorders; taking immunosuppressant medication; or trials that recruited women with evidence of coinfection with other vulvovaginal infections.
Types of interventions
Any probiotic: single or multiple strains, any preparation type, dosage regimen or route of administration.
-
Used alone versus conventional antifungal drugs.
-
Used as adjuvants to conventional antifungal drugs (before, during or after antifungal treatment) versus conventional antifungal drugs alone.
Conventional antifungal drugs described here refer to the common drugs for VVC treatment, such as azole drugs (triazoles and imidazoles) and nystatin.
Types of outcome measures
Primary outcomes
-
Clinical cure rate (disappearance of symptoms and signs, and no evidence of fungal infection proved by microscopic examination or vaginal culture), split into 'short‐term clinical cure rate' (zero to 14 days after treatment) and 'long‐term clinical cure rate' (one, three and six months after treatment).
-
Mycological cure rate (no evidence of fungal infection proved by microscopic examination or vaginal culture), split into 'short‐term mycological cure rate' (zero to 14 days after treatment)' and 'long‐term mycological cure rate' (one, three and six months after treatment).
-
Relapse rate (symptom recurrence confirmed by microscopic examination or vaginal culture at one, three and six after mycological cure).
-
Rate of serious adverse events (death, internal organ injury, severe skin and mucosal injury).
Secondary outcomes
-
Time to first relapse.
-
Rate of non‐serious adverse events (mild symptoms include vomiting, diarrhea, abdominal pain, abnormal urination, pelvic cramps, paresthesia, rhinorrhea, headache, dizziness, fever, chills, vaginal burning, stinging, itching and irritation).
-
Need for any additional treatment at the end of therapy.
-
Patient satisfaction with treatment.
-
Cost effectiveness.
Search methods for identification of studies
We attempted to identify as many relevant RCTs as possible of "probiotics" for "VVC", regardless of language, publication date or publication status (published, unpublished, in press and in progress). We used both electronic searching in bibliographic databases and handsearching, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Electronic searches
We contacted the Information Specialist of the Cochrane Sexually Transmitted Infections Group to implement a comprehensive search strategy to identify as many relevant RCTs as possible in the electronic databases. The search strategies included a combination of controlled vocabulary (MeSH, EMTREE, DeCS, including exploded terms) and free‐text terms for "probiotics" and "VVC", with field labels (title and abstract), wildcards (truncation), proximity operators (adj) and boolean operators (OR, AND).
We searched the following electronic databases:
-
Sexually Transmitted Infections Cochrane Review Group's Specialized Register (to October 2017);
-
Cochrane Central Register of Controlled Trials (CENTRAL), Ovid (1991 to October 2017);
-
MEDLINE, Ovid (1946 to October 2017);
-
MEDLINE In‐Process & Other Non‐Indexed Citations, Ovid (1946 to October 2017);
-
MEDLINE Daily Update, Ovid (1946 to October 2017);
-
Embase (1947 to October 2017);
-
LILACS, IAHx interface (1982 to October 2017);
-
PsycINFO, Ovid (1946 to October 2017);
-
AMED, Ovid (1946 to October 2017);
-
CBMdisc and CNKI: inception to October 2017.
The search strategies for the STI Specialized Register, CENTRAL, MEDLINE, Embase, AMED, CBMdisc and CNKI, PsycINFO and LILACS can be found in Appendix 1, Appendix 2, Appendix 3, Appendix 4, Appendix 5, Appendix 6, and Appendix 7.
We placed no language restrictions.
Searching other resources
We attempted to identify other published, unpublished and ongoing relevant RCTs by:
-
searching trials registers:
-
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) portal (apps.who.int/trialsearch/);
-
ClinicalTrials.gov (clinicaltrials.gov/);
-
-
searching Web of Science (inception to October 2017);
-
searching grey literature in System for Information on Grey Literature in Europe "OpenGrey" (www.opengrey.eu/) (inception to October 2017);
-
contacting authors of included RCTs and experts in the field to identify any additional published and unpublished materials;
-
contacting pharmaceutical companies producing "probiotics" for "VVC";
-
handsearching the following journals: Anatolian Journal of Obstetrics & Gynecology, Current Medical Literature Gynecology & Obstetrics, Current Obstetrics and Gynecology Reports, ISRN Obstetrics and Gynecology, Journal of South Asian Federation of Obstetrics & Gynecology, Obstetrics and Gynecology International, Obstetrics Gynaecology and Reproductive Medicine and Sexual Science: the newsletter of the Society for the Scientific Study of Sexuality and Sexualities;
-
handsearching the conference proceeding abstracts in the following events:
-
International Society for Sexually Transmitted Diseases Research (ISSTDR) (www.isstdr.org/): 2007, 2009, 2011, 2013 and 2015;
-
British Association for Sexual Health and HIV (BASHH) (www.bashh.org/): 2004, 2006, 2007, 2009, 2010, 2011 and 2014;
-
International Congress on Infectious Diseases (ICID) (www.isid.org/): 2010, 2012 and 2014;
-
International Union against Sexually Transmitted Infections (IUSTI) (www.iusti.org/): 2011, 2012, 2013 and 2014;
-
International Society for Infectious Diseases (ISID) (www.isid.org/): 2011;
-
International Meeting on Emerging Diseases and Surveillance (IMED) (www.isid.org/): 2007, 2009, 2013 and 2014;
-
Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC) (www.icaac.org/): 2011, 2012, 2013, 2014 and 2015;
-
International Federation of Gynecology and Obstetrics (FIGO) (www.figo.org): 2012 and 2015;
-
-
handsearching previous systematic reviews and other relevant publications on the same topic;
-
handsearching reference lists of all RCTs identified by other methods, including available review articles on the topic, and contacting authors of all RCTs identified by other methods.
Data collection and analysis
Selection of studies
Two authors (DW and HC) independently scanned all titles and abstracts from the initial search, to exclude trials that did not meet the inclusion criteria. Multiple reports of the same study were collected and collated so that each study, rather than each report, was used. Two authors (DW and HC) independently assessed the full text of trials that appeared to meet the inclusion criteria. Two authors (DW and HC) contacted the authors of articles if any important information was missing. We resolved any discrepancies through discussion with a third author (HX).
Data extraction and management
Two authors (LM and XW) independently extracted data using a previously designed form for this review. The data extraction form was pilot tested using one of the included studies. We collected the following information.
-
Study characteristics.
-
Year and language of publication.
-
Inclusion and exclusion criteria.
-
Randomization process.
-
Allocation concealment.
-
Blinding.
-
Number of withdrawals (participants excluded from analysis or lost to follow‐up) and reasons.
-
Intention‐to‐treat analysis.
-
Duration of follow‐up.
-
-
Basic participant information.
-
Number.
-
Mean age and age range of the participants.
-
Type of participants (health status, uncomplicated VVC or complicated VVC).
-
-
Intervention.
-
Drug.
-
Type (single or multiple).
-
Preparation.
-
Dosage and route of administration.
-
-
Outcome.
-
Clinical cure rate.
-
Mycological cure rate.
-
Relapse rate.
-
Time to first relapse.
-
-
Adverse events.
-
Serious adverse events.
-
Non‐serious adverse events.
-
-
Cost effectiveness: if the data were mentioned and available.
-
Others.
-
Funding sources reported.
-
Ethical issues: use of signed informed consent and ethics approval.
-
We discussed any disagreements referring back to the trial report until we reached consensus. If data from the trial reports were insufficient or missing, we contacted the trial authors for additional information.
Two authors (LM, XW) entered data into Review Manager 5 (RevMan 2014) and a third author (HX) checked them to ensure data quality. When information regarding any of the above were unclear, we contacted the authors of the studies to ask for further details. For a single randomized controlled clinical trial report, we extracted data directly onto the data extraction form and in case of multiple reports, we extracted data from each report separately and then combined them across the forms. Studies reported a language other than English or Chinese were translated.
Assessment of risk of bias in included studies
Two authors (DW and HC) assessed the methodological quality of each trial using the Cochrane 'Risk of bias' tool. We resolved any disagreements by consensus or by involving a third author (FF). The authors assessing risk of bias were thematic and methodology experts. We assessed the following information which was used for the development of the 'Risk of bias' tables.
-
1. Random sequence generation (checking for possible selection bias). We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups. We assessed the method as: low risk of bias (any truly random process, e.g. random number table, computer random number generator); high risk of bias (any non‐random process, e.g. odd or even date of birth, hospital or clinic record number) or unclear risk of bias.
-
2. Allocation concealment (checking for possible selection bias). We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during, recruitment, or changed after assignment. We assessed the methods as: low risk of bias (e.g. telephone or central randomization, consecutively numbered sealed opaque envelopes); high risk of bias (open random allocation, unsealed or non‐opaque envelopes, alternation, date of birth) or unclear risk of bias.
-
3. Blinding
-
3.1 Blinding of participants and personnel (checking for possible performance bias). We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding would be unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes. We assessed the methods as: low, high or unclear risk of bias for participants; and low, high or unclear risk of bias for personnel.
-
3.2 Blinding of outcome assessment (checking for possible detection bias). We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes. We assessed methods used to blind outcome assessment as low, high or unclear risk of bias.
-
-
4. Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data). We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We reported whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomized participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we reincluded missing data in the analyses that we undertook. We assessed methods as low risk of bias (e.g. no missing outcome data, missing outcome data balanced across groups); high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups, 'as treated' analysis done with substantial departure of intervention received from that assigned at randomization) or unclear risk of bias. We used a cut‐off point of 20% to consider that a study was at low or high risk of bias according to the level of missing data.
-
5. Selective reporting (checking for reporting bias). We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found. We assessed the methods as: low risk of bias (where it was clear that all of the study's prespecified outcomes and all expected outcomes of interest to the review were reported); high risk of bias (where not all the study's prespecified outcomes were reported, one or more reported primary outcomes were not prespecified, outcomes of interest were reported incompletely and so could not be used, study failed to include results of a key outcome that would have been expected to have been reported or unclear risk of bias).
-
6. Other bias (checking for bias due to problems not covered under points 1 to 5 above). We described for each included study any important concerns we had about other possible sources of bias (stopped early due to some data‐dependent process or extreme baseline imbalance or was claimed to be fraudulent or have been sponsored by industry). We assessed whether each study was free of other problems that could put it at risk of bias.
-
7. Overall risk of bias. We made explicit judgments about whether studies are at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). With reference to points 1 to 6 above, we assessed the likely magnitude and direction of the bias and whether we consider it is likely to impact on the findings.
Two authors (DW and HC) independently applied the 'Risk of bias' tool, and resolved differences by discussion or by discussion with a third author (FF). We presented results in a 'Risk of bias' graph. The risk of bias findings were used to inform any meta‐analyses.
Measures of treatment effect
For dichotomous outcomes, we pooled the results in meta‐analyses and presented results as summary risk ratios (RRs) with 95% confidence intervals (CIs). We expressed continuous data as mean differences (MDs) with 95% CIs.
Unit of analysis issues
The primary unit of analysis in meta‐analysis was the participant. For trials that contributed multiple, correlated comparisons, we planned to combine all relevant experimental intervention groups of the trials into a single group and combined all relevant control intervention groups into a single control group so we could create a single pair‐wise comparison (Higgins 2011) when the objective was to compare the experimental branch with any other control group.
Dealing with missing data
Whenever possible, we contacted the original authors to request missing data. We identified levels of attrition for included trials and we performed analyses for all outcomes, as far as possible, on an intention‐to‐treat basis. We attempted to include all participants randomized to each group in the analyses, and all participants were analyzed in the group to which they were allocated, regardless of whether or not they received the allocated intervention. We conducted sensitivity analyses to explore the impact of studies with missing data, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of heterogeneity
If there was obvious heterogeneity (populations, interventions, etc.), we conducted subgroup analyses to investigate potential sources of heterogeneity. We assessed statistical heterogeneity in each meta‐analysis using the T2, I2 and Chi2 statistics. We regarded heterogeneity as substantial if the I² statistic was greater than 40% and either T2 was greater than zero or there was a low P value (less than 0.10) in the Chi2 test for heterogeneity.
Assessment of reporting biases
We planned to assess reporting bias by constructing a funnel plot. If 10 or more original trials were identified, then a funnel plot would be produced in an attempt to identify any publication bias. However, for each outcome, we included fewer than 10 trials in the meta‐analysis, so we did not perform these analyses.
Data synthesis
We performed the statistical analyses by using Review Manager 5 (RevMan 2014). If the trials were judged to be similar, and in the absence of statistical heterogeneity, we pooled the data using a fixed‐effect model, and if statistical heterogeneity was present, we used a random‐effect model. If the outcome data could not be combined, we described the outcome separately. If the data were available, we conducted time‐to‐event analyses for time to recurrence by extracting data from published curves (Parmar 1998). We assessed the quality of the body of evidence.
Because the Chi2 test has low power when sample sizes or number of studies are small, it may fail to detect heterogeneity. In the event of few trials or small samples, we proposed to conduct both a random‐effects and a fixed‐effect meta‐analysis, even if there was no heterogeneity detected.
'Summary of findings' table
We summarized the results for the main comparison in a 'Summary of findings' table. We used the GRADE approach to assess the quality of evidence in relation to each outcome included) and used GRADE profiler (GRADEpro) software to import data from Review Manager 5 (RevMan 2014) to create a 'Summary of findings' table (Higgins 2011).
We produced a 'Summary of findings' table for eight critical outcomes in each type of comparison:
-
clinical cure rate (short‐term);
-
clinical cure rate (long‐term/one month after treatment);
-
clinical cure rate (long‐term/three months after treatment);
-
mycological cure rate (short‐term);
-
mycological cure rate (long‐term/one month after treatment);
-
mycological cure rate (long‐term/three months after treatment);
-
relapse rate;
-
rate of serious adverse events.
For each outcome, quality was categorized into four ratings: high quality (further research is very unlikely to change our confidence in the estimate of effect), moderate quality (further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate), low quality (further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate) and very low quality (we are very uncertain about the estimate) (Higgins 2011).
Subgroup analysis and investigation of heterogeneity
We explored a subgroup analysis in cases of high heterogeneity and assessed the effect of certain subgroups for all outcomes:
-
probiotics: single versus multiple species;
-
route of administration: intravaginal versus oral;
-
different candidal strains: Candida albicans versus non‐albicans;
-
age group of participants: aged less than 18 years versus aged 18 years or greater.
Sensitivity analysis
We planned to perform a sensitivity analysis to explore whether the results of the review were robust, depending on study quality, for each outcome variable. We excluded studies with a high risk of bias, comparing findings within the remainder of the included studies with the original meta‐analysis.
Results
Description of studies
Results of the search
We searched the available literature up to October 2017 and retrieved 2525 references, of which we screened 2481 after we removed duplicates. We excluded 2454 clearly irrelevant references. We screened the full‐text articles of the remaining 27 references. Ten published trials met our inclusion criteria (Zhang 2005; Han 2006; Lin 2006; Ma 2007; Mai 2007; Hua 2008; Martinez 2009; Yang 2009; Nouraei 2012; Kovachev 2015). We excluded 16 studies (see Characteristics of excluded studies table) and one trial is awaiting classification (see the Characteristics of studies awaiting classification table). We presented a PRISMA diagram in Figure 1 to illustrate the study selection process.

Study flow diagram. RCT: randomized controlled trial.
Included studies
We included 10 trials in this review (Zhang 2005; Han 2006; Lin 2006; Ma 2007; Mai 2007; Hua 2008; Martinez 2009; Yang 2009; Nouraei 2012; Kovachev 2015), and included data from 1656 women, with a sample size ranging from 68 to 436 participants. These trials were from China (Zhang 2005; Han 2006; Lin 2006; Ma 2007; Mai 2007; Hua 2008; Yang 2009), Bulgaria (Kovachev 2015), Brazil (Martinez 2009), and Iran (Nouraei 2012). Only one was multicentric trial (Martinez 2009). Seven trials were published in Chinese (Zhang 2005; Han 2006; Lin 2006; Ma 2007; Mai 2007; Hua 2008; Yang 2009), and three trials were published in English (Martinez 2009; Nouraei 2012; Kovachev 2015).
Population
Study populations were heterogeneous. The included trials recruited participants aged between 16 and 50 years. All trials used at least one laboratory method for diagnosis. All the selected trials recruited participants without RVVC, diabetes mellitus, immunosuppressive disorders, taking immunosuppressant medication or evidence of co‐infection with other vulvovaginal infections. One trial implemented an added exclusion criterion related with human papillomavirus infection (Kovachev 2015). Two trials only recruited married participants (Zhang 2005; Nouraei 2012). Three trials required that participants had no sexual activity during treatment and follow‐up (Zhang 2005; Mai 2007; Kovachev 2015), five trials required participants had no sexual activity during treatment and used a condom during follow‐up (Han 2006; Lin 2006; Ma 2007; Hua 2008; Yang 2009), and two trials did not mention the requirement of sexual activity (Martinez 2009; Nouraei 2012).
Interventions
All trials used probiotics as adjuvant therapy to antifungal drugs. Five trials used probiotics of Lactobacillus delbrueckii subsp. Lactis DM8909 (Zhang 2005; Han 2006; Mai 2007; Hua 2008; Yang 2009), two trials used probiotics of Streptococcus faecalis (Lin 2006; Ma 2007), one trial used probiotics of Lactobacillus rhamnosus GR‐1 and Lactobacillus reuteri RC‐14 (Martinez 2009), one trial used probiotics of Lactobacillus acidophilus, Lactobacillus rhamnosus, Streptococcus thermophilus and Lactobacillus delbrueckii subsp. Bulgaricus (Kovachev 2015), and one trial used probiotics contained seven strains of probiotic bacteria (Lactobacillus casei, Lactobacillus rhamnosus, Streptococcus thermophilus, Bifidobacterium breve, Lactobacillus acidophilus, Bifidobacterium longum and Lactobacillus bulgaricus) (Nouraei 2012).
The most frequently used conventional antifungal drug was clotrimazole (Han 2006; Lin 2006; Mai 2007; Yang 2009), three trials used miconazole (Zhang 2005; Ma 2007; Hua 2008), two trials used fluconazole (Martinez 2009; Nouraei 2012), and one trial used fluconazole plus fenticonazole (Kovachev 2015). Table 5 lists a brief summary of interventions in included studies.
| Included study | Intervention groups | Intervention doses and duration | Intervention administration route |
| Clotrimazole + probiotic group | 1 tablet of clotrimazole 500 mg on day 1 and day 4 + 1 capsule of Lactobacillus delbrueckii Subsp. Lactis DM8909 (each capsule contained 0.25 × 106 colony forming units), QD from day 1 to day 10. | Vaginal | |
| Clotrimazole group | 1 tablet of clotrimazole 500 mg on day 1 and day 4. | Vaginal | |
| Miconazole + probiotic group | 1 suppository of miconazole nitrate 400 mg, QD from day 1 to day 6, and then 1 capsule of Lactobacillus delbrueckii subsp. Lactis DM8909 (each capsule contained 0.25 × 106 colony forming units), QD from day 7 to day 16. | Vaginal | |
| Miconazole group | 1 vaginal suppository of Miconazole nitrate (400 mg), QD from day 1 to day 6 | Vaginal | |
| Azole + vaginal probiotic group | Fluconazole 150 mg + 1 globule of fenticonazole 600 mg on the same day; however, 10 applications of probiotics (Lactobacillus acidophilus,Lactobacillus rhamnosus,Streptococcus thermophilus and Lactobacillus delbrueckii subsp. Bulgaricus) were also administered beginning the 5th day after azole treatment. | Fluconazole: oral. Fenticonazole: vaginal Probiotics: vaginal | |
| Azole group | Fluconazole 150 mg + 1 globule of fenticonazole 600 mg on the same day. | Fluconazole: oral Fenticonazole: vaginal | |
| Clotrimazole + probiotic group | 1 suppository of clotrimazole 150 mg, QD from day 1 to day 7, then, 1 capsule of Streptococcus faecalis (each capsule contained 6 × 107 colony forming units), QD from day 8 to day 14. | Vaginal | |
| Clotrimazole group | 1 suppository of clotrimazole 150 mg, QD from day 1 to day 7. | Vaginal | |
| Miconazole + probiotic group | 1 suppository of miconazole nitrate 200 mg, QD from day 1 to day 14, and on day 8, 1 capsule of Streptococcus faecalis (each capsule contained 6 × 107 colony forming units), QD from day 8 to day 14. | Vaginal | |
| Miconazole group | 1 suppository of miconazole nitrate 200 mg, QD from day 1 to day 14. | Vaginal | |
| Clotrimazole + probiotic group | 1 suppository of clotrimazole 150 mg, QN + 1 capsule of Lactobacillus delbrueckii Subsp. Lactis DM8909 (each capsule contained 0.25 × 106 colony forming units), QD from day 1 to day 10. | Vaginal | |
| Clotrimazole group | 1 suppository of clotrimazole 150 mg, QN from day 1 to day 10. | Vaginal | |
| Fluconazole + probiotic group | 1 dose of fluconazole 150 mg + 2 capsules of Lactobacillus rhamnosus GR‐1 and Lactobacillus reuteri RC‐14 (each capsule contained 1 × 109 viable cells of both strains) for 28 days | Oral | |
| Fluconazole + placebo group | 1 dose of fluconazole 150 mg + 2 oral capsules of placebo once daily (every morning) for 28 days. | Oral | |
| Fluconazole + oral protexin group | 1 dose of fluconazole 300 mg (2 × 150 mg) + 2 protexin capsules per day (after meals in the morning and evening) for 3 days. | Oral | |
| Fluconazole + placebo group | 1 dose of fluconazole 300 mg (2 × 150 mg) + 2 placebo capsules daily (after meals in the morning and evening) for 3 days. | Oral | |
| Clotrimazole + probiotic group | 1 tablet of clotrimazole 500 mg on day 1 and day 4 + 1 capsule of Lactobacillus delbrueckii subsp. Lactis DM8909 (each capsule contained 0.25 × 106 colony forming units), QD from day 1 to day 10. | Vaginal | |
| Clotrimazole group | 1 tablet of clotrimazole 500 mg on day 1 and day 4. | Vaginal | |
| Miconazole + probiotic group | 1 suppository of miconazole nitrate 200 mg, QD from day 1 to day 7, and then, 1 capsule of Lactobacillus delbrueckii subsp. Lactis DM8909 (each capsule contained 0.25 × 106 colony forming units), QD from day 8 to day 17. | Vaginal | |
| Miconazole group | 1 suppository of miconazole nitrate 200 mg, QD from day 1 to day 7. | Vaginal |
QD: every day; QN: every night.
Comparison
Four trials compared vaginal suppository or tablet of clotrimazole plus vaginal capsules of probiotics with vaginal suppository or tablet of clotrimazole alone (Han 2006; Lin 2006; Mai 2007; Yang 2009), three trials compared vaginal suppository of miconazole plus vaginal capsules of probiotics with vaginal suppository of miconazole alone (Zhang 2005; Ma 2007; Hua 2008), two trials compared oral fluconazole plus oral capsules of probiotics with oral fluconazole plus oral capsules of placebo (Martinez 2009; Nouraei 2012), and one trial compared oral fluconazole and vaginal globule of fenticonazole plus oral capsules of probiotics with oral fluconazole and vaginal globule of fenticonazole (Kovachev 2015).
Outcomes
All the included trials reported at least one prespecified primary outcome of this review. Five trials reported short‐term clinical cure rate (Han 2006; Ma 2007; Hua 2008; Yang 2009; Nouraei 2012), and only one trial reported long‐term clinical cure rate (Zhang 2005). Seven trials reported short‐term mycological cure rate (Han 2006; Lin 2006; Ma 2007; Mai 2007; Hua 2008; Yang 2009; Nouraei 2012), and three trials reported short‐term mycological cure rate (Zhang 2005; Martinez 2009; Kovachev 2015). Three trials reported the first relapse after treatment (Han 2006; Hua 2008; Yang 2009). Two trials reported the rate of serious adverse events (Zhang 2005; Hua 2008). Seven trials reported the rate of non‐serious adverse events (Zhang 2005; Han 2006; Ma 2007; Hua 2008; Martinez 2009; Yang 2009; Nouraei 2012). We did not obtain any data on the secondary outcomes: time to first relapse, need for any additional treatment at the end of the therapy, patient satisfaction with treatment and cost effectiveness.
Excluded studies
Sixteen trials were initially identified as potentially eligible for inclusion but were subsequently found to be ineligible. The main reason was that they were not RCTs (Ozkinay 2005; Yang 2005; Zhang 2006; Li 2007; Liu 2008; Patel 2008; Anukam 2009; Fu 2009; Ehrstrom 2010; Wang 2010; Song 2011; Fu 2012; Shi 2012; Nagornaya 2013; Wu 2013; Sigridov 2007). The reasons for exclusions are listed in the Characteristics of excluded studies table.
Risk of bias in included studies
We have summarized the 'Risk of bias' assessment in Figure 2 and Figure 3. In addition, we provided additional details of the included trials in the 'Risk of bias' tables of the Characteristics of included studies' table.
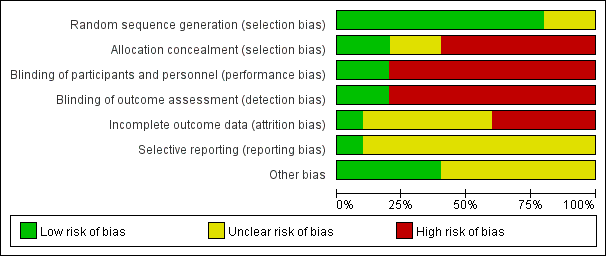
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
Allocation
Random sequence generation (checking for possible selection bias)
Eight studies adequately reported the random sequence generation method by using a Research Randomizer software or a random draw method (All participants were numbered on an individual piece of paper, then took the paper (relevant to participant) out of a container randomly, without being able to see what was written on it; we judged this as a valid method after contacting the original authors.) making selection bias at entry unlikely (Zhang 2005; Han 2006; Lin 2006; Ma 2007; Mai 2007; Hua 2008; Yang 2009; Kovachev 2015). The remaining two studies did not report the random sequence generation methods, making the risk of selection bias at entry unclear (Martinez 2009; Nouraei 2012).
Allocation concealment (checking for possible selection bias)
Two studies had adequate allocation concealment by using codified opaque‐sealed envelopes, and the risk of selection bias related to allocation concealment was low (Mai 2007; Hua 2008). Six studies had a high selection bias as they did not conceal the allocation (Zhang 2005; Han 2006; Lin 2006; Ma 2007; Yang 2009; Kovachev 2015). Two studies had no description regarding concealment allocation disclosed; they were judged with unclear risk of bias for allocation concealment (Martinez 2009; Nouraei 2012).
Blinding
Performance bias
Two studies used double blinding and a placebo‐controlled method; the participants and investigators were blind to the interventions, making performance bias unlikely (Martinez 2009; Nouraei 2012). Six studies were at high performance bias as no blinding was adopted, as the judgment of symptoms and signs were subjectively evaluated; however, in these studies, both participants and investigators knew the allocated interventions during the study and outcomes may be influenced (Zhang 2005; Han 2006; Lin 2006; Ma 2007; Yang 2009; Kovachev 2015). Two studies used single blinding to the investigators, no blinding to participants as lacked a placebo control, and judgment of symptoms and signs by participants may have been influenced, so we also judged the two studies as having high risk of performance bias (Mai 2007; Hua 2008).
Detection bias
Risk of detection bias was low in two studies as the outcome assessors were blinded adequately (Martinez 2009; Nouraei 2012). Six studies had a high detection bias as no blinding was adopted and the judgment of symptoms and signs outcomes by participants may be influenced (Zhang 2005; Han 2006; Lin 2006; Ma 2007; Yang 2009; Kovachev 2015). In two studies, although the outcome assessors were blinded, they still may have been influenced by participants as there was no blinding to participants, so the two studies were judged at high risk of detection bias (Mai 2007; Hua 2008).
Incomplete outcome data
Five studies reported no withdrawals, but these trial did not have enough information for us to judge "yes" or "no" in intention‐to‐treat analyses and as a consequence, we assessed them as at unclear risk of attrition bias (Han 2006; Lin 2006; Ma 2007; Martinez 2009; Yang 2009). Hua 2008 reported a withdrawal rate of 2.1% (less than 20%) during the treatment, Kovachev 2015 reported a withdrawal rate of 4.6% (less than 20%) after the treatment, Mai 2007 reported a withdrawal rate of 6.1% (less than 20%) after the treatment and Zhang 2005 reported a withdrawal rate of 6.5% during the treatment and 7% after the treatment (less than 20%). The results of the four studies were not analyzed on an intention‐to‐treat basis, so we assessed them as at high risk of attrition bias. As Nouraei 2012 reported no attrition or exclusion, we assessed it at low risk of attrition bias.
Selective reporting
We found only one study reporting all the expected outcomes mentioned in their trial protocol (protocols number IRCT201106206807N3); it was clear that the published reports include all prespecified outcomes, so we judged it at low risk of selective reporting bias (Nouraei 2012).
For the other nine studies, the trial protocols were not available and it was unclear if the published reports included all the expected outcomes, including those that were prespecified. The reports had insufficient information to permit judgment of "yes" or "no," so we rated them at unclear risk of bias.
Other potential sources of bias
One study did not mention available data of the baseline characteristics between the two groups to judge the balance, we judged the study as having unclear risk of bias (Kovachev 2015). Although authors of five included studies mentioned there were no significant differences in baseline characteristics, they provided no detailed data; therefore, we judged these studies at unclear risk of bias (Han 2006; Lin 2006; Ma 2007; Hua 2008; Yang 2009). One study mentioned that one author held some patents associated with lactobacilli; however, his input was in protocol design, logistics, student supervision and assistance with the manuscript not in the accumulation of data. In addition, the author was blinded to the results until after the code was broken and findings acquired. We judged that probably this author had a conflict of interest that did not affect the quality of the evidence and there was low risk of bias in this study (Martinez 2009). The remaining studies appeared to be free of other sources of bias (Zhang 2005; Mai 2007; Nouraei 2012).
Effects of interventions
1. Probiotics used alone versus conventional antifungal drugs
None of the included trials analyzed probiotics used alone compared with conventional antifungal drugs.
2. Probiotics used as adjuvants to conventional antifungal drugs (before, during or after antifungal treatment) versus conventional antifungal drugs
All 10 included trials compared probiotics used as adjuvants to conventional antifungal drugs (before, during or after antifungal treatment) with conventional antifungal drugs (Zhang 2005; Han 2006; Lin 2006; Ma 2007; Mai 2007; Hua 2008; Martinez 2009; Yang 2009; Nouraei 2012; Kovachev 2015). Data were available on 1656 outpatients with VVC, they were all non‐pregnant and without RVVC, diabetes mellitus, immunosuppressive disorders, taking immunosuppressant medication or evidence of co‐infection with other vulvovaginal infections.
Primary outcomes
Clinical cure rate: short‐term (zero to 14 days after treatment)
Five trials evaluated 695 participants for short‐term clinical cure rate (Han 2006; Ma 2007; Hua 2008; Yang 2009; Nouraei 2012).
In the probiotics used as adjuvants to conventional antifungal drugs group, clinical cure occurred in 286/347 participants. In the conventional antifungal drugs group, a clinical cure occurred in 251/348 participants. Probiotics as adjuvants therapy was associated with a significantly improved on short‐term clinical cure rate when compared to conventional antifungal drugs alone (combined RR 1.14, 95% CI 1.05 to 1.24; 5 trials, 695 participants, I2 = 28%; Analysis 1.1; Figure 4).

Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.1 Clinical cure rate (short‐term).
A sensitivity analysis excluding the four studies at high risk of bias (Han 2006, Hua 2008, Ma 2007, Yang 2009), only included Nouraei 2012; however, the rate of short‐term clinical cure was still significantly increased in the probiotics used as adjuvants group compared to the conventional antifungal drugs alone group (RR 1.41, 95% CI 1.07 to 1.84; 1 trial, 90 participants; Analysis 1.2).
The GRADE quality of the evidence for this outcome was low due to the limitations of risk of bias (see summary of findings Table for the main comparison for details).
Clinical cure rate: long‐term (one month after treatment)
Only one trial reported the long‐term clinical cure rate at one month after treatment (Zhang 2005). There was no significant improvement associated with probiotics as adjuvant therapy on long‐term clinical cure rate at one month after treatment compared to conventional antifungal drugs alone (RR 1.07, 95% CI 0.86 to 1.33; 1 trial, 172 participants; Analysis 1.4).
The quality of the evidence for this outcome was very low due to the limitations of risk of bias and imprecision (see summary of findings Table for the main comparison for details).
Clinical cure rate: long‐term (three months after treatment)
One trial reported long‐term clinical cure rate at three months after treatment (Zhang 2005). There was no significant improvement associated with probiotics as adjuvant therapy on long‐term clinical cure rate at three months after treatment compared to conventional antifungal drugs alone (RR 1.30, 95% CI 1.00 to 1.70; 1 trial, 172 participants; Analysis 1.5).
The quality of the evidence for this outcome was very low due to the limitations of risk of bias and imprecision (see summary of findings Table for the main comparison for details).
Mycological cure rate: short‐term (zero to 14 days after treatment)
Seven trials with 969 participants evaluated short‐term mycological cure rate (Han 2006; Lin 2006; Ma 2007; Mai 2007; Hua 2008; Yang 2009; Nouraei 2012).
In the probiotics used as adjuvants to conventional antifungal drugs group, mycological cure occurred in 452/485 participants. In the conventional antifungal drugs group, mycological cure occurred in 426/484 participants. Probiotics as adjuvants therapy was associated with a significantly improved short‐term mycological cure rate compared conventional antifungal drugs alone (RR 1.06, 95% CI 1.02 to 1.10; 7 trials, 969 participants, I2 = 0%; Analysis 1.6; Figure 5).
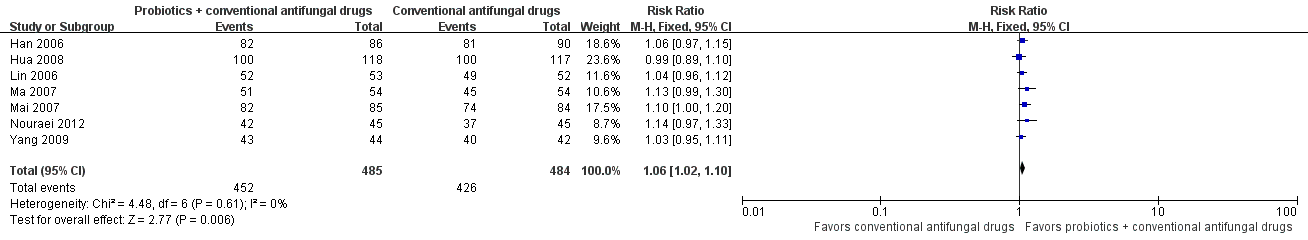
Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.6 Mycological cure rate (short‐term).
A sensitivity analysis excluding the six trials at high risk of bias (Han 2006; Lin 2006; Ma 2007; Mai 2007; Hua 2008; Yang 2009), only included Nouraei 2012; it found the rate of short‐term mycological cure was no longer significantly difference between the groups (RR 1.14, 95% CI 0.97 to 1.33; 1 trial, 90 participants; Analysis 1.7). The result of this sensitivity analysis must be treated and interpreted carefully because of the small sample in Nouraei 2012.
The quality of the evidence for this outcome was low due to the limitations of risk of bias (see summary of findings Table for the main comparison for details).
Mycological cure rate: long‐term (one month after treatment)
Three trials with 627 participants evaluated long‐term mycological cure rate at one month after treatment (Zhang 2005; Martinez 2009; Kovachev 2015).
In the probiotics used as adjuvants to conventional antifungal drugs group, mycological cure occurred in 294/314 participants. In the conventional antifungal drugs group, mycological cure occurred in 221/313 participants. Probiotics as adjuvants therapy was associated with no significant improvement on long‐term mycological cure rate at one month after treatment when compared to conventional antifungal drugs alone (RR 1.26, 95% CI 0.93 to 1.71; 3 trials, 627 participants, I2 = 93%; Analysis 1.10; Figure 6).

Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.10 Mycological cure rate (long‐term/1 month after treatment).
A sensitivity analysis excluding two trials at high risk of bias (Zhang 2005; Kovachev 2015), only included Martinez 2009; however, the rate of long‐term mycological cure rate at one month after treatment was still not significantly difference between probiotics used as adjuvants and conventional antifungal drugs alone (RR 1.32, 95% CI 0.99 to 1.77; 1 trial, 90 participants; Analysis 1.11). This result must be treated and interpreted carefully because of the small sample.
The quality of the evidence for this outcome was very low due to the limitations of risk of bias, imprecision and inconsistency (see summary of findings Table for the main comparison for details).
Mycological cure rate: long‐term (three months after treatment)
Only one trial with 172 participants reported long‐term mycological cure rate at three months after treatment (Zhang 2005). There was no statistically significant difference between probiotics used as adjuvants and conventional antifungal drugs alone in the rate of long‐term mycological cure at three months after treatment (RR 1.16, 95% CI 1.00 to 1.35; 1 trial, 172 participants; Analysis 1.12).
The quality of the evidence for this outcome was very low due to the limitations of risk of bias and imprecision (see summary of findings Table for the main comparison for details).
Relapse rate
Three trials with 388 participants evaluated first relapse after treatment (Han 2006; Hua 2008; Yang 2009). In the probiotics used as adjuvants to conventional antifungal drugs group, relapse occurred in 10/202 participants. In the conventional antifungal drugs group, relapse occurred in 27/186 participants. Probiotic use significantly decreased relapse rate at one month (RR 0.34, 95% CI 0.17 to 0.68; 3 trials, 388 participants, I2 = 0%; Analysis 1.13; Figure 7). No sensitivity analysis or subgroup analyses was done from the available trials.
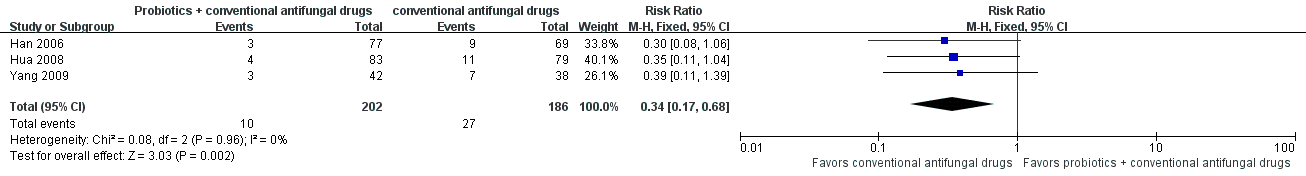
Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.13 Relapse rate.
The quality of the evidence for this outcome was very low due to the limitations of risk of bias and imprecision (see summary of findings Table for the main comparison for details).
Rate of serious adverse events
Two trials with 440 participants evaluated rate of serious adverse events (Zhang 2005; Hua 2008). The reported adverse events included severe vaginal burning, stinging or rash after the first use of miconazole nitrate vaginal suppository. There was no statistically significant difference between probiotics used as adjuvants and conventional antifungal drugs alone in the rate of serious adverse events (RR 0.80, 95% CI 0.22 to 2.94; 2 trials, 440 participants, I2 = 0%; Analysis 1.14). No other serious adverse events were reported.
The quality of the evidence for this outcome was low due to the limitations of risk of bias and imprecision (see summary of findings Table for the main comparison for details).
Secondary outcomes
Time to first relapse
We found no eligible RCTs reporting time to first relapse.
Rate of non‐serious adverse events
Seven trials with 906 participants evaluated rate of non‐serious adverse events (Zhang 2005; Han 2006; Ma 2007; Hua 2008; Martinez 2009; Yang 2009; Nouraei 2012).
The reported adverse events included mild vaginal dryness, burning, stinging, headache, loose stool and nausea. There was no statistically significant difference between probiotics used as adjuvants and conventional antifungal drugs alone in the rate of non‐serious adverse events (RR 0.90, 95% CI 0.48 to 1.70; 7 trials, 906 participants, I2 = 0%; Analysis 1.15; Figure 8).

Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.14 Non‐serious adverse events.
The quality of the evidence for this outcome was low due to the limitations of risk of bias and imprecision (CIs were wide and included null effects).
Need for any additional treatment at the end of the therapy
We found no eligible RCTs reporting need for any additional treatment at the end of the therapy.
Patient satisfaction with treatment
We found no eligible RCTs reporting patient satisfaction with treatment.
Cost effectiveness
We found no eligible RCTs reporting cost effectiveness.
Subgroup analysis and investigation of heterogeneity
We performed subgroup analyses to explore the substantial heterogeneity we found in the analyses "Clinical cure rate: short‐term (zero to 14 days after treatment)." For this analysis, we explored whether differences in species of probiotics and route of administration (intravaginal administration of single species of probiotic or oral administration of multiple species of probiotics). Subgroups did not appear to be different (P = 0.10; Analysis 1.3; Figure 9). The effect of the intervention for this outcome did not change according to these intervention characteristics.

Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.3 Clinical cure rate (short‐term): subgroup analysis.
In the analyses for "mycological cure rate: short‐term (zero to 14 days after treatment)," we explored whether differences in species of probiotics and route of administration (intravaginal administration of single species of probiotic or oral administration of multiple species of probiotics), subgroups did not appear to be different (P = 0.35; Analysis 1.8; Figure 10). The effect of the intervention for this outcome did not change according to these intervention characteristics.

Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.8 Mycological cure rate (short‐term): subgroup analysis.
In addition, we explored the differences between different candidal strains (Candida albicans versus non‐albicans), and found that the subgroup estimates for the different candidal strains did not differ significantly in the oral administration of probiotics (P = 0.88; Analysis 1.9).
In the analyses "mycological cure rate: long‐term (one month after treatment),", we explored the differences between routes of administration (intravaginal or oral administration), subgroups did not appear to be different (P = 0.80; Analysis 1.10). Subgroup analysis did not appear to explain the variability in the overall summary effect measures for the outcome long‐term mycological cure rate, so these findings should be interpreted with caution.
We did not perform the subgroup analysis "age group of participants" because none of the included trials provided information.
Discussion
Summary of main results
Ten RCTs including 1656 participants fulfilled the inclusion criteria and were included. We judged the risk of bias for the included trials to be high. All the 10 included trials were in the comparison of "probiotics used as adjuvants to conventional antifungal drugs versus conventional antifungal drugs alone," and none of the retrieved studies compared "probiotic alone versus conventional treatment."
We found the following results.
-
Compared with conventional antifungal drugs alone, the addition of probiotics could enhance their effect in improving short‐term clinical cure rate (RR 1.14, 95% CI 1.05 to 1.24), regardless of the route of administration, and whether multiple species or single species of probiotics were used. The results did not seem to show a significant improvement between the two groups in long‐term clinical cure rate at one month after treatment (RR 1.07, 95% CI 0.86 to 1.33) and at three months after treatment (RR 1.30, 95% CI 1.00 to 1.70).
-
Compared with conventional antifungal drugs alone, the addition of probiotics could enhance their effect in improving short‐term mycological cure rate (RR 1.06, 95% CI 1.02 to 1.10), but the addition of probiotics did not seem to be different to conventional antifungal drugs used alone in improving the long‐term mycological cure rate at one month after treatment (RR 1.26, 95% CI 0.93 to 1.71) and at three months after treatment (RR 1.16, 95% CI 1.00 to 1.35).
-
Compared with conventional antifungal drugs alone, the addition of probiotics may reduce the first relapse rate at one month after treatment (RR 0.34, 95% CI 0.17 to 0.68). However, this result should be interpreted with caution because of the limitations related to the low quality of primary studies.
-
There appears to be no difference between the addition of probiotics to conventional antifungal drugs and conventional antifungal drugs alone in the rate of serious adverse events (RR 0.80, 95% CI 0.22 to 2.94), the reported adverse events included severe vaginal burning, stinging or rash after the first use of miconazole nitrate vaginal suppository.
-
There was no difference between the addition of probiotics to conventional antifungal drugs and conventional antifungal drugs alone in the rate of non‐serious adverse events (RR 0.90, 95% CI 0.48 to 1.70). The reported adverse events included mild vaginal dryness, burning, stinging, headache, loose stool and nausea.
-
There was no available evidence for evaluating the time to first relapse, need for any additional treatment at the end of therapy, patient satisfaction with treatment and cost effectiveness.
However, all the results found in this review should be interpreted with caution because of the limitations related to the low and very low quality of primary studies.
Overall completeness and applicability of evidence
Although we employed several methods to try to identify all RCTs and included both published and unpublished data in this review, this systematic review included trials at high risk of bias and consequently with very low to low confidence on the estimate of effect (see summary of findings Table for the main comparison). We conducted sensitivity analyses or subgroup analyses (or both) that did not change the results of short‐term clinical cure rate, long‐term clinical cure rate and long‐term mycological cure rate. It strengthened the confidence that could be placed in these results, considering that most of the outcomes were very low or low quality evidence. This review was unable to report on the results of meta‐analysis of long‐term clinical cure rate (at one month and three months after treatment) and long‐term mycological cure rate (three months after treatment), as only one of the included studies offered the relevant data (Zhang 2005). This review was unable to address the issue of whether an oral administration of probiotics used as adjuvants to conventional antifungal drugs could improve the short‐term mycological cure rate, as only one study included with small sample offered the relevant data (Nouraei 2012). For the same reason, it was also unable to address the issue of whether the different candidal strains (Candida albicans versus non‐albicans) could influence the effectiveness of probiotics. For relapse rate, this review estimated the evidence only from studies that used the intravaginal probiotics. This review was also unable to address the issue of whether the different age group of women with VVC could influence the effectiveness of probiotics, because as of 2017, no RCT had focused on these topics. Likewise, none of the included studies assessed time to first relapse, need for any additional treatment at the end of therapy and patient satisfaction with treatment. Finally, this review could provide no evidence for assessing the effectiveness and safety of probiotics used alone versus conventional antifungal drugs, because none of the RCTs focused on these topics.
This review included 10 studies that enrolled 1656 participants. These studies were conducted in China (seven studies), Brazil (one study), Bulgaria (one study) and Iran (one study), and were representative of a relatively wide range of racial, cultural and social groups. However, there was no study investigating the treatment of VVC in resource‐poor settings and this is a limitation to the general applicability of the results. This review focused on non‐pregnant women with VVC, and from the inclusion criteria, the results from this review could not be applied to pregnant women; women with RVVC, diabetes mellitus or immunosuppressive disorders; or women taking immunosuppressant medication. There was a small number of mild adverse events reported, and there were no other serious adverse events reported except severe vaginal burning, stinging or rash after the first use of miconazole nitrate vaginal suppository. It appears that probiotics could be considered safe in general from current limited data.
Quality of the evidence
We considered the 10 included trials to be at high risk of bias, and the confidence in the estimated effect in this review, assessed with the GRADE tool, ranged from very low to low (see Figure 2, Figure 3, and summary of findings Table for the main comparison). There is little confidence in the effect estimates, and the true effect is likely to be substantially different. The confidence is very low due to trial limitations (on risk of bias domain by sequence generation, allocation concealment and blinding of the included studies), inconsistency (substantial heterogeneity between studies and single study in some results) and imprecise results (outcome events with wide CIs, small sample size and few events). We could not evaluate publication bias, because there were too few included trials into each comparison.
Potential biases in the review process
In our review, reporting bias could not be assessed because of the limited numbers of studies for each outcome. Although we undertook several methods to try to identify all trials and included both published and unpublished data in this review, we could not exclude the possibility that studies with negative findings remain unpublished. There was substantial heterogeneity for some outcomes and our investigation of heterogeneity sources (which was based on a small number of trials for each comparison) could have limited value. In addition, the balance in baseline characteristics was not well explained and as confirmed by both published reports and contact authors, there may be unclear risk of bias for the results and conclusions.
Agreements and disagreements with other studies or reviews
We found one systematic review evaluating the effects of miconazole alone and miconazole plus a living preparation of Lactobacillus for the treatment of the uncomplicated VVC (Cui 2010). The authors included only trials using miconazole as the antifungal drug, and methodology details were unavailable. In contrast to our review, it concluded that currently available evidence showed that the effect in the combined group was better and the recurrence rate was lower. However, it did not report adverse events. Although Nouraei 2012, which used an oral administration of probiotics, showed that probiotics used as adjuvants to conventional antifungal drugs performed better at improving the short‐term clinical cure rate, it showed no difference in short‐term mycological cure rate. Likewise, Martinez 2009, which also used an oral administration of probiotics, found no significant difference in long‐term mycological cure rate, but it showed a statistically significant difference in favor of probiotics used as adjuvants to conventional antifungal drugs in enhancing long‐term clinical improvement, which was determined as cure or persistence of Candida species and absence of symptoms. However, this result should be treated with caution as the small size was sample. Ehrstrom 2010 showed that adjunctive treatment of VVC with probiotics led to fewer recurrences and only a few adverse events (single episodes of headache and nausea), but had no impact on short‐term cure rate. However, the large and imbalanced rate of lost to follow‐up and the small sample could influence the result, and, as pointed out in the publication, probiotics were unavailable for women to use as an adjuvant to urogenital care in Nigeria, and even if probiotics were introduced, many of the population could not afford them.

Study flow diagram. RCT: randomized controlled trial.
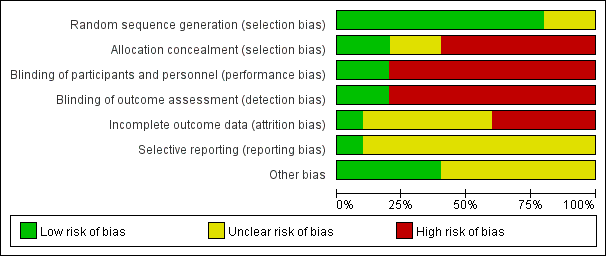
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.

Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.1 Clinical cure rate (short‐term).
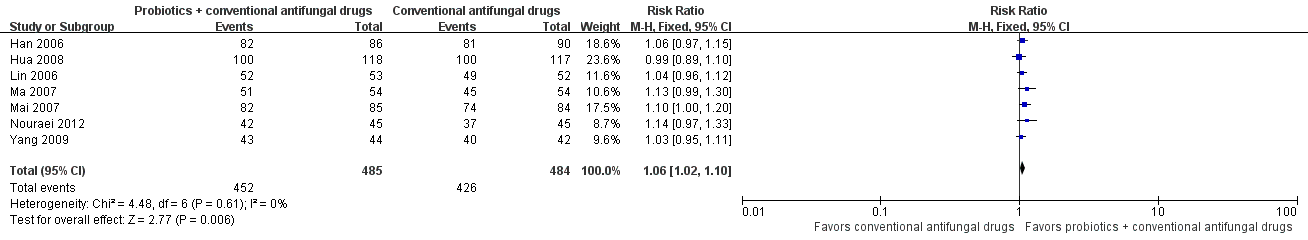
Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.6 Mycological cure rate (short‐term).

Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.10 Mycological cure rate (long‐term/1 month after treatment).
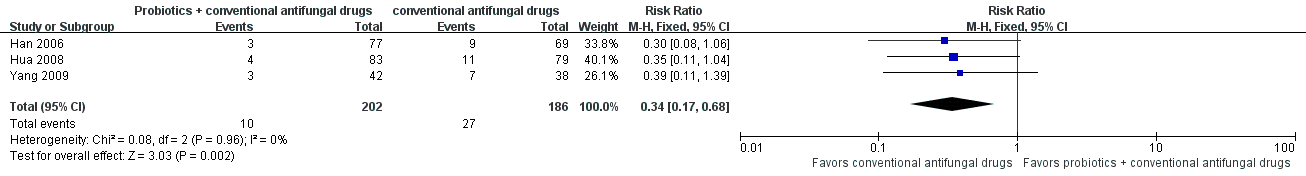
Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.13 Relapse rate.

Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.14 Non‐serious adverse events.

Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.3 Clinical cure rate (short‐term): subgroup analysis.

Forest plot of comparison: 2 Probiotics + conventional antifungal drugs versus conventional antifungal drugs, outcome: 1.8 Mycological cure rate (short‐term): subgroup analysis.

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 1 Clinical cure rate (short‐term).

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 2 Clinical cure rate (short‐term): sensitivity analysis.

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 3 Clinical cure rate (short‐term): subgroup analysis.

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 4 Clinical cure rate (long‐term/1 month after treatment).

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 5 Clinical cure rate (long‐term/3 months after treatment).

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 6 Mycological cure rate (short‐term).

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 7 Mycological cure rate (short‐term): sensitivity analysis.

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 8 Mycological cure rate (short‐term): subgroup analysis.

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 9 Mycological non‐cure (short‐term/Candida albicans versus non‐albicans).
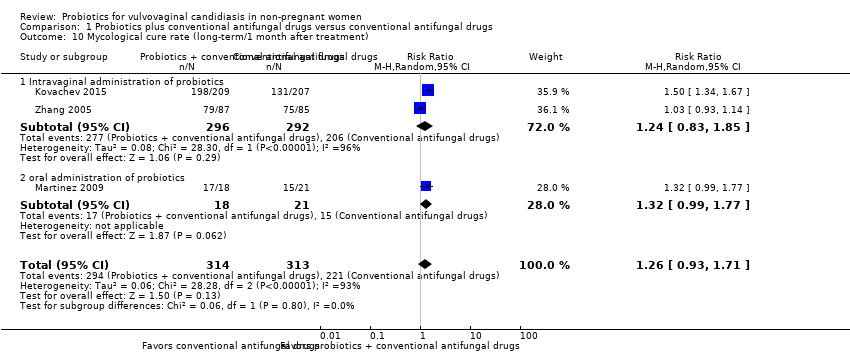
Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 10 Mycological cure rate (long‐term/1 month after treatment).

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 11 Mycological cure rate (long‐term/1 month after treatment): sensitivity analysis.

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 12 Mycological cure rate (long‐term/3 months after treatment).

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 13 Relapse rate.
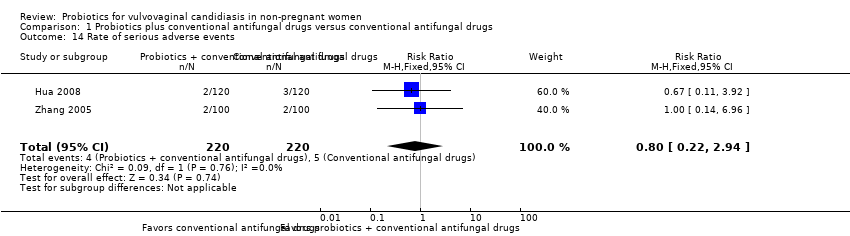
Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 14 Rate of serious adverse events.

Comparison 1 Probiotics plus conventional antifungal drugs versus conventional antifungal drugs, Outcome 15 Rate of non‐serious adverse events.
| Probiotics used as adjuvants to conventional antifungal drugs compared with conventional antifungal drugs for the treatment of vulvovaginal candidiasis in non‐pregnant women | |||||||
| Patient or population: non‐pregnant women with vulvovaginal candidiasis Settings: outpatient clinics in Brazil, Bulgaria, Iran and China Intervention: probiotics used as adjuvants to conventional antifungal drugs Comparison: conventional antifungal drugs | |||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of participants | Quality of the evidence | Comments | ||
| Assumed risk | Corresponding risk | ||||||
| Conventional antifungal drugs | Probiotics used as adjuvants to conventional antifungal drugs | ||||||
| Clinical cure rate (short‐term) follow‐up: 5‐10 days | Medium risk population | RR 1.14 (1.05 to 1.24) | 695 | ⊕⊕⊝⊝ | ‐ | ||
| 721 per 1000 | 822 per 1000 | ||||||
| Clinical cure rate (long‐term) | 1 month after treatment follow‐up: 1 month | Medium risk population | RR 1.07 (0.86 to 1.33) | 172 | ⊕⊝⊝⊝ | ‐ | |
| 635 per 1000 | 679 per 1000 | ||||||
| 3 months after treatment follow‐up: 3 months | Medium risk population | RR 1.30 (1.00 to 1.70) | 172 | ⊕⊝⊝⊝ | ‐ | ||
| 494 per 1000 | 642 per 1000 | ||||||
| Mycological cure rate (short‐term) follow‐up: 5‐10 days | Medium risk population | RR 1.06 (1.02 to 1.10) | 969 | ⊕⊕⊝⊝ | See 3 in footnotes. | ||
| 880 per 1000 | 933 per 1000 | ||||||
| Mycological cure rate (long‐term) | 1 month after treatment follow‐up: 28‐30 days | Medium risk population | RR 1.26 (0.93 to 1.71) | 627 | ⊕⊝⊝⊝ | See 5 in footnotes. | |
| 706 per 1000 | 890 per 1000 | ||||||
| 3 months after treatment follow‐up: 3 months | Medium risk population | RR 1.16 (1.00 to 1.35) | 172 | ⊕⊝⊝⊝ | ‐ | ||
| 741 per 1000 | 860 per 1000 | ||||||
| Relapse rate follow‐up: 30‐37 days after treatment | Medium risk population | RR 0.34 (0.17 to 0.68) | 388 | ⊕⊝⊝⊝ | ‐ | ||
| 145 per 1000 | 49 per 1000 | ||||||
| Rate of serious adverse events follow‐up: 5‐90 days after treatment | Medium risk population | RR 0.80 (0.22 to 2.94) | 440 | ⊕⊕⊝⊝ | ‐ | ||
| 23 per 1000 | 18 per 1000 | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||||
| GRADE Working Group grades of evidence | |||||||
| 1Downgraded two levels due to very serious risk of bias: the included studies had a high or unclear risk of bias in at least one key domain i.e. random sequence generation, allocation concealment or blinding. 2Downgraded one level due to serious imprecision: the 95% CI were wide and included null effects. 3A sensitivity analysis that excluded studies with high risk of bias and included only one study showed that the rate of short‐term mycological cure was changed to no significantly difference between two arms. For the heterogeneity and difference in results, we think the reasons may be associated with the small sample of included study, high risk of bias of studies that were excluded for sensitivity analysis. 4Downgraded one level due to inconsistency: there was a substantial heterogeneity between studies. 5There was heterogeneity that may be attributable to differences in route of the administration of probiotics, we undertook a subgroup analysis, the results showed no statistically significant difference between two arms in either subgroup. 6Downgraded one level due to serious imprecision: small sample size and few events. | |||||||
| Species | Frequency | Response to azoles |
| Candida albicans | 80‐90% | Sensitive |
| Candida glabrata | 5‐10% | Resistant |
| Candida krusei | < 1% | Tends to be resistant |
| Candida lusitaniae | < 1% | Tends to be resistant |
| Candida parapsilosis | < 1% | Tends to be resistant |
| Candida pseudotropicalis | < 1% | Tends to be resistant |
| Candida tropicalis | < 1% | Tends to be resistant |
| Source: Bieber 2006. | ||
| Non‐prescription intravaginal agents | Prescription intravaginal agents |
| Butoconazole 2% cream 5 g intravaginally for 3 days OR Clotrimazole 1% cream 5 g intravaginally for 7‐14 days OR Clotrimazole 2% cream 5 g intravaginally for 3 days OR Miconazole 2% cream 5 g intravaginally for 7 days OR Miconazole 4% cream 5 g intravaginally for 3 days OR Miconazole 100 mg vaginal suppository, 1 suppository for 7 days OR Miconazole 200 mg vaginal suppository, 1 suppository for 3 days OR Miconazole 1200 mg vaginal suppository, 1 suppository for 1 day OR Tioconazole 6.5% ointment 5 g intravaginally in a single application | Butoconazole 2% cream (single dose bioadhesive product), 5 g intravaginally for 1 day OR Nystatin 100,000 unit vaginal tablet, 1 tablet for 14 days OR Terconazole 0.4% cream 5 g intravaginally for 7 days OR Terconazole 0.8% cream 5 g intravaginally for 3 days OR Terconazole 80 mg vaginal suppository, 1 suppository for 3 days |
| CDC: Centers for Disease Control and Prevention. Source: CDC 2015. | |
| Recurrent vulvovaginal candidiasis | |
| Initial regimen: 7‐14 days of any topical azole drug OR Fluconazole 100 mg, 150 mg or 200 mg orally once daily every 3rd day for a total of 3 doses (days 1, 4 and 7) | Maintenance regimen: Fluconazole 100 mg, 150 mg or 200 mg orally once weekly for 6 months |
| Severe vulvovaginal candidiasis | |
| Intravaginally once daily for 7 to 14 days of any topical azole drug OR Fluconazole 150 mg orally once daily in 2 doses (second dose 72 hours after initial dose) | |
| Non‐albicans vulvovaginal candidiasis | |
| Non‐fluconazole azole (oral or topical) 7‐14 days OR Boric acid gelatin capsule Intravaginally once daily for 14 days | |
| Abnormal host | |
| More prolonged (i.e. 7‐14 days) conventional antifungal drugs is necessary | |
| CDC: Centers for Disease Control and Prevention. Source: CDC 2015. | |
| Lactobacillus species: Lactobacillus acidophilus Lactobacillus bulgaricus Lactobacillus casei Lactobacillus crispatus Lactobacillus delbrueckii Lactobacillus fermentum Lactobacillus gasseri Lactobacillus johnsonii Lactobacillus lactis Lactobacillus plantarum Lactobacillus reuteri Lactobacillus rhamnosus GG | Streptococcus species: Streptococcus thermophilus
|
| Yeast: Saccharomyces boulardii
| |
| Other species: Bacillus cereus Enterococcus faecalisa Enterococcus faeciuma Escherichia coli Nissle
| |
| Bifidobacterium species: Bifidobacterium adolescentis Bifidobacterium animalis Bifidobacterium bifidum Bifidobacterium breve Bifidobacterium infantis Bifidobacterium lactis Bifidobacterium longum | |
| Sources: Senok 2005; Doron 2006; Santosa 2006. | |
| Included study | Intervention groups | Intervention doses and duration | Intervention administration route |
| Clotrimazole + probiotic group | 1 tablet of clotrimazole 500 mg on day 1 and day 4 + 1 capsule of Lactobacillus delbrueckii Subsp. Lactis DM8909 (each capsule contained 0.25 × 106 colony forming units), QD from day 1 to day 10. | Vaginal | |
| Clotrimazole group | 1 tablet of clotrimazole 500 mg on day 1 and day 4. | Vaginal | |
| Miconazole + probiotic group | 1 suppository of miconazole nitrate 400 mg, QD from day 1 to day 6, and then 1 capsule of Lactobacillus delbrueckii subsp. Lactis DM8909 (each capsule contained 0.25 × 106 colony forming units), QD from day 7 to day 16. | Vaginal | |
| Miconazole group | 1 vaginal suppository of Miconazole nitrate (400 mg), QD from day 1 to day 6 | Vaginal | |
| Azole + vaginal probiotic group | Fluconazole 150 mg + 1 globule of fenticonazole 600 mg on the same day; however, 10 applications of probiotics (Lactobacillus acidophilus,Lactobacillus rhamnosus,Streptococcus thermophilus and Lactobacillus delbrueckii subsp. Bulgaricus) were also administered beginning the 5th day after azole treatment. | Fluconazole: oral. Fenticonazole: vaginal Probiotics: vaginal | |
| Azole group | Fluconazole 150 mg + 1 globule of fenticonazole 600 mg on the same day. | Fluconazole: oral Fenticonazole: vaginal | |
| Clotrimazole + probiotic group | 1 suppository of clotrimazole 150 mg, QD from day 1 to day 7, then, 1 capsule of Streptococcus faecalis (each capsule contained 6 × 107 colony forming units), QD from day 8 to day 14. | Vaginal | |
| Clotrimazole group | 1 suppository of clotrimazole 150 mg, QD from day 1 to day 7. | Vaginal | |
| Miconazole + probiotic group | 1 suppository of miconazole nitrate 200 mg, QD from day 1 to day 14, and on day 8, 1 capsule of Streptococcus faecalis (each capsule contained 6 × 107 colony forming units), QD from day 8 to day 14. | Vaginal | |
| Miconazole group | 1 suppository of miconazole nitrate 200 mg, QD from day 1 to day 14. | Vaginal | |
| Clotrimazole + probiotic group | 1 suppository of clotrimazole 150 mg, QN + 1 capsule of Lactobacillus delbrueckii Subsp. Lactis DM8909 (each capsule contained 0.25 × 106 colony forming units), QD from day 1 to day 10. | Vaginal | |
| Clotrimazole group | 1 suppository of clotrimazole 150 mg, QN from day 1 to day 10. | Vaginal | |
| Fluconazole + probiotic group | 1 dose of fluconazole 150 mg + 2 capsules of Lactobacillus rhamnosus GR‐1 and Lactobacillus reuteri RC‐14 (each capsule contained 1 × 109 viable cells of both strains) for 28 days | Oral | |
| Fluconazole + placebo group | 1 dose of fluconazole 150 mg + 2 oral capsules of placebo once daily (every morning) for 28 days. | Oral | |
| Fluconazole + oral protexin group | 1 dose of fluconazole 300 mg (2 × 150 mg) + 2 protexin capsules per day (after meals in the morning and evening) for 3 days. | Oral | |
| Fluconazole + placebo group | 1 dose of fluconazole 300 mg (2 × 150 mg) + 2 placebo capsules daily (after meals in the morning and evening) for 3 days. | Oral | |
| Clotrimazole + probiotic group | 1 tablet of clotrimazole 500 mg on day 1 and day 4 + 1 capsule of Lactobacillus delbrueckii subsp. Lactis DM8909 (each capsule contained 0.25 × 106 colony forming units), QD from day 1 to day 10. | Vaginal | |
| Clotrimazole group | 1 tablet of clotrimazole 500 mg on day 1 and day 4. | Vaginal | |
| Miconazole + probiotic group | 1 suppository of miconazole nitrate 200 mg, QD from day 1 to day 7, and then, 1 capsule of Lactobacillus delbrueckii subsp. Lactis DM8909 (each capsule contained 0.25 × 106 colony forming units), QD from day 8 to day 17. | Vaginal | |
| Miconazole group | 1 suppository of miconazole nitrate 200 mg, QD from day 1 to day 7. | Vaginal | |
| QD: every day; QN: every night. | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Clinical cure rate (short‐term) Show forest plot | 5 | 695 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [1.05, 1.24] |
| 2 Clinical cure rate (short‐term): sensitivity analysis Show forest plot | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [1.07, 1.84] |
| 3 Clinical cure rate (short‐term): subgroup analysis Show forest plot | 5 | 695 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [1.05, 1.24] |
| 3.1 Intravaginal administration and single species of probiotics | 4 | 605 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [1.02, 1.21] |
| 3.2 Oral administration and multiple species of probiotics | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [1.07, 1.84] |
| 4 Clinical cure rate (long‐term/1 month after treatment) Show forest plot | 1 | 172 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.86, 1.33] |
| 5 Clinical cure rate (long‐term/3 months after treatment) Show forest plot | 1 | 172 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [1.00, 1.70] |
| 6 Mycological cure rate (short‐term) Show forest plot | 7 | 969 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [1.02, 1.10] |
| 7 Mycological cure rate (short‐term): sensitivity analysis Show forest plot | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.97, 1.33] |
| 8 Mycological cure rate (short‐term): subgroup analysis Show forest plot | 7 | 969 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [1.02, 1.10] |
| 8.1 Intravaginal administration and single species of probiotics | 6 | 879 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [1.01, 1.10] |
| 8.2 Oral administration and multiple species of probiotics | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.97, 1.33] |
| 9 Mycological non‐cure (short‐term/Candida albicans versus non‐albicans) Show forest plot | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.16, 1.30] |
| 9.1 Candida albicans | 1 | 83 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.09, 2.52] |
| 9.2 Non‐albicans | 1 | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.11, 1.53] |
| 10 Mycological cure rate (long‐term/1 month after treatment) Show forest plot | 3 | 627 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.93, 1.71] |
| 10.1 Intravaginal administration of probiotics | 2 | 588 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.83, 1.85] |
| 10.2 oral administration of probiotics | 1 | 39 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [0.99, 1.77] |
| 11 Mycological cure rate (long‐term/1 month after treatment): sensitivity analysis Show forest plot | 1 | 39 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [0.99, 1.77] |
| 12 Mycological cure rate (long‐term/3 months after treatment) Show forest plot | 1 | 172 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [1.00, 1.35] |
| 13 Relapse rate Show forest plot | 3 | 388 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.17, 0.68] |
| 14 Rate of serious adverse events Show forest plot | 2 | 440 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.8 [0.22, 2.94] |
| 15 Rate of non‐serious adverse events Show forest plot | 7 | 906 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.48, 1.70] |

