Apoyo conductual adicional como complemento a la farmacoterapia para el abandono del hábito de fumar
Appendices
Appendix 1. Register Search
Search used in the Cochrane Register of Studies.
-
NRT:TI,AB,KW
-
(nicotine NEAR (replacement OR patch* OR transdermal OR gum OR lozenge* OR sublingual OR inhaler* OR inhalator* OR oral OR nasal OR spray)):TI,AB,KW
-
(bupropion OR zyban OR wellbutrin):TI,AB,KW,MH,EMT
-
(varenicline OR champix OR chantix):TI,AB,KW,MH,EMT
-
combined modality therapy:MH,KW
-
((behavio?r therapy) AND (drug therapy)):KW,MH,EMT,TI,AB
-
((counsel*) AND (*drug therapy)):KW,MH,EMT,TI,AB
-
#1 OR #2 OR #3 OR #4 OR #5
-
#6 OR #7 OR #8
-
#9 AND INREGISTER
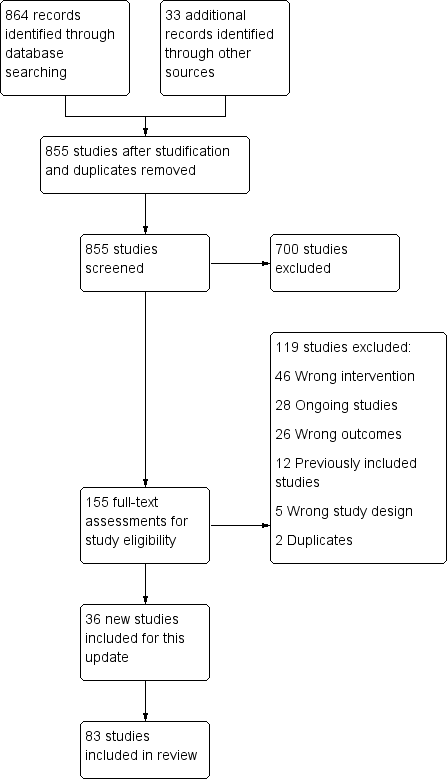
Study flow diagram for 2019 update

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Effect of increasing behavioural support. Abstinence at longest follow‐up.
Subgroups by type of pharmacotherapy
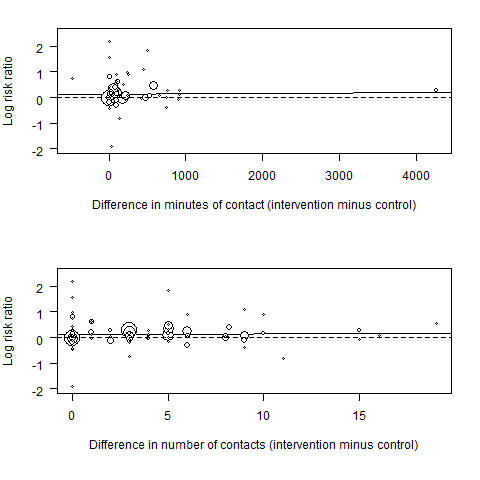
Meta‐regression results (the fitted meta‐regression trend is shown as the solid line)

Funnel plot of comparison: 1 Effect of increasing behavioural support. Abstinence at longest follow‐up, outcome: 1.1 Subgroups by type of pharmacotherapy.

Comparison 1 Effect of increasing behavioural support. Abstinence at longest follow‐up, Outcome 1 Subgroups by type of pharmacotherapy.

Comparison 1 Effect of increasing behavioural support. Abstinence at longest follow‐up, Outcome 2 Subgroups by contrast in number of contacts between intervention & control.
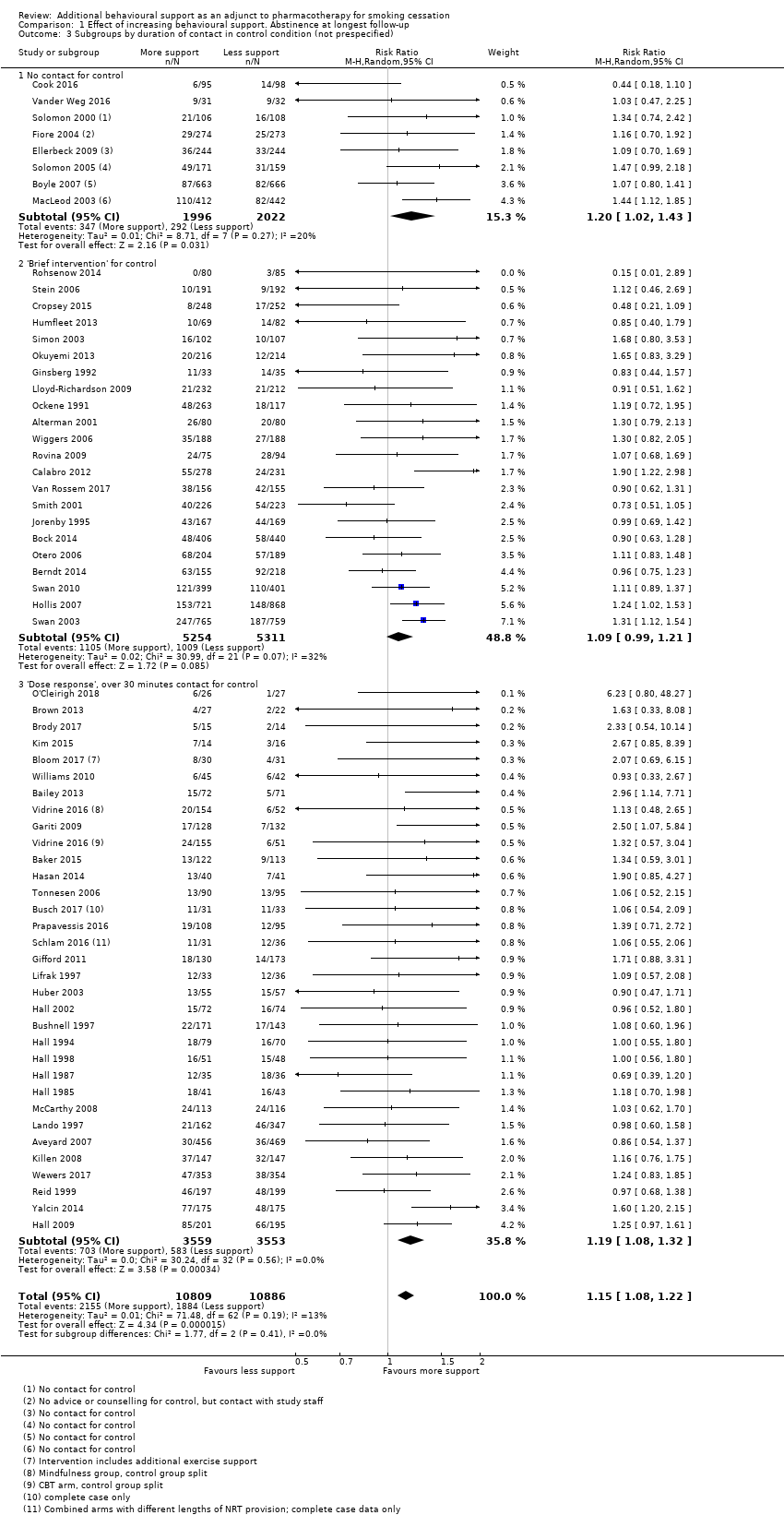
Comparison 1 Effect of increasing behavioural support. Abstinence at longest follow‐up, Outcome 3 Subgroups by duration of contact in control condition (not prespecified).
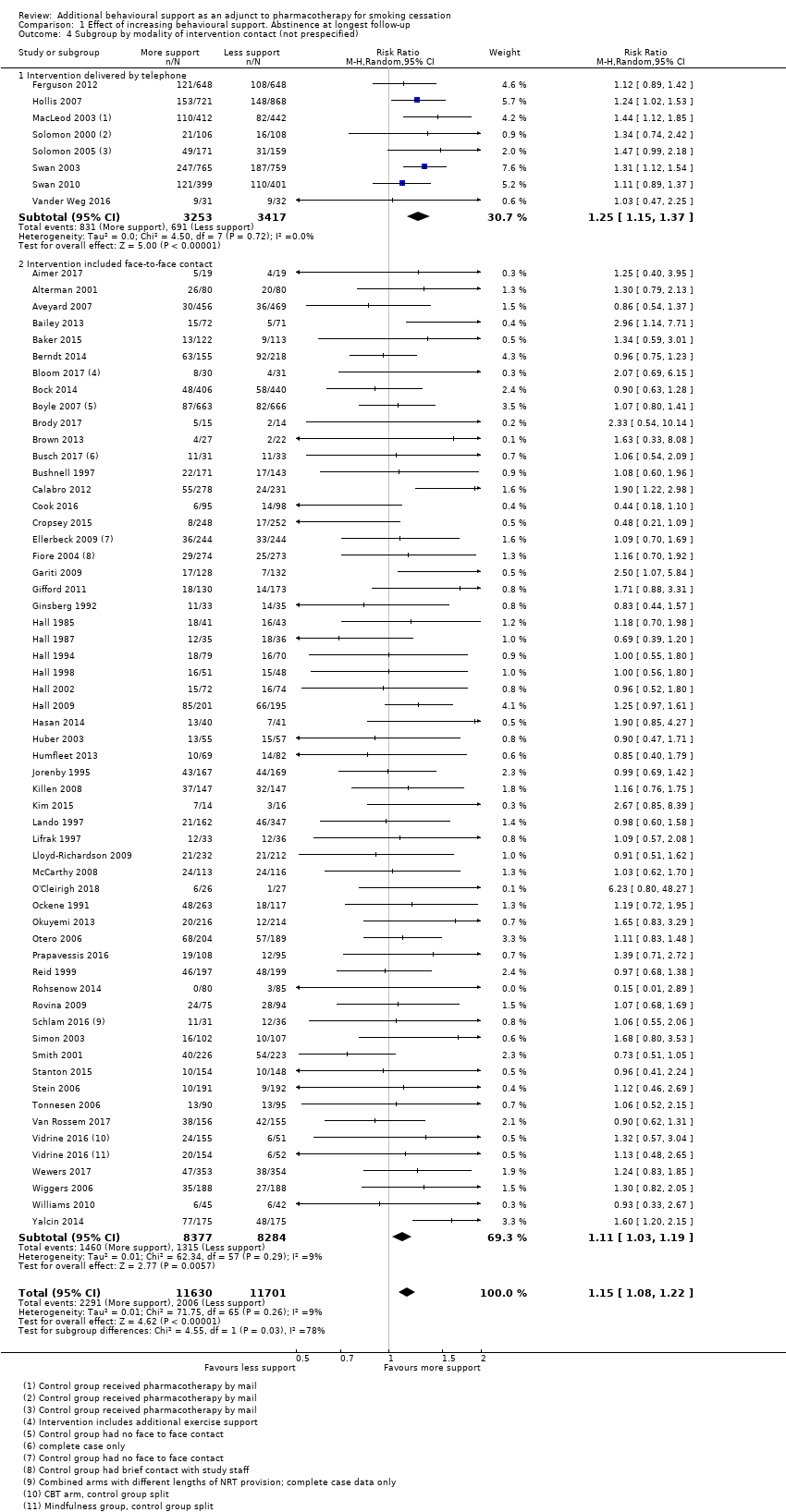
Comparison 1 Effect of increasing behavioural support. Abstinence at longest follow‐up, Outcome 4 Subgroup by modality of intervention contact (not prespecified).
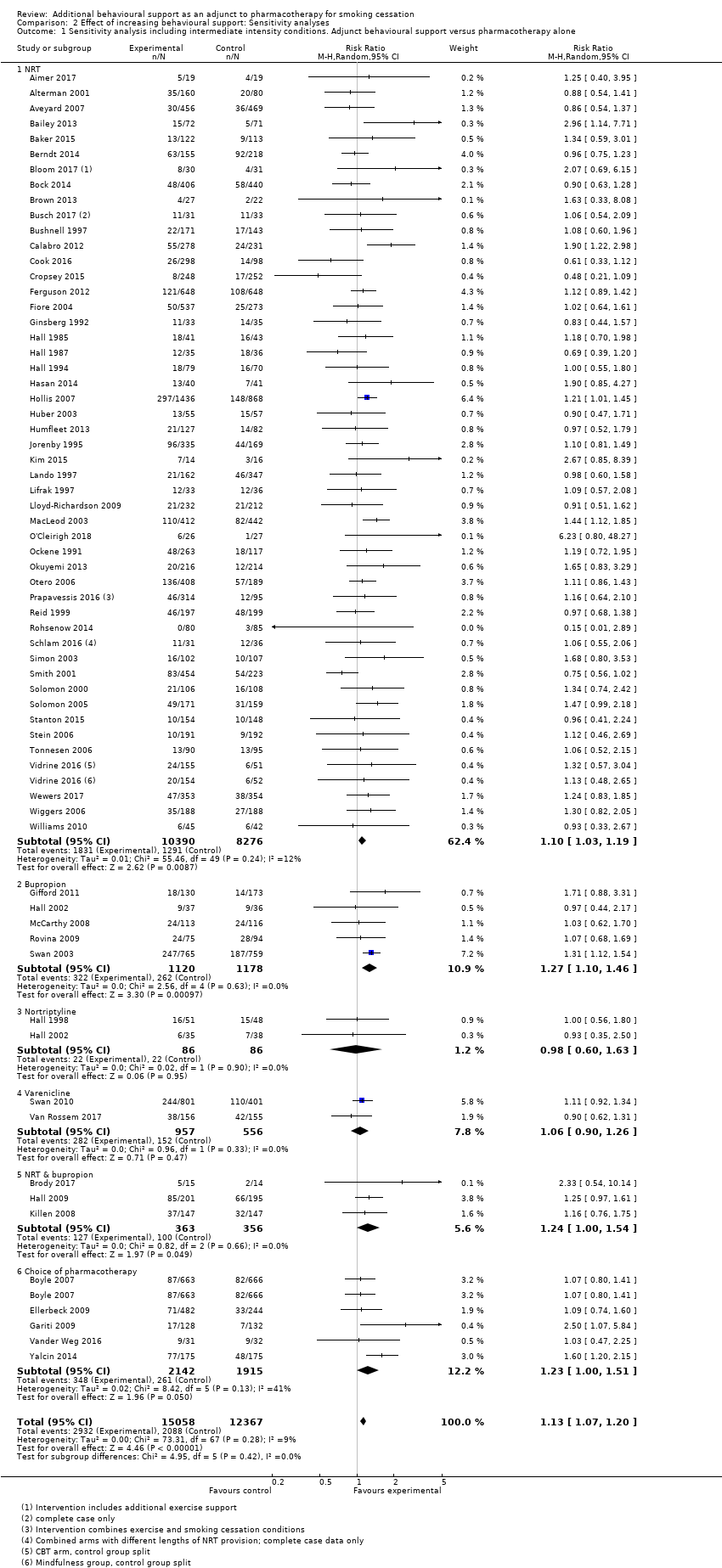
Comparison 2 Effect of increasing behavioural support: Sensitivity analyses, Outcome 1 Sensitivity analysis including intermediate intensity conditions. Adjunct behavioural support versus pharmacotherapy alone.
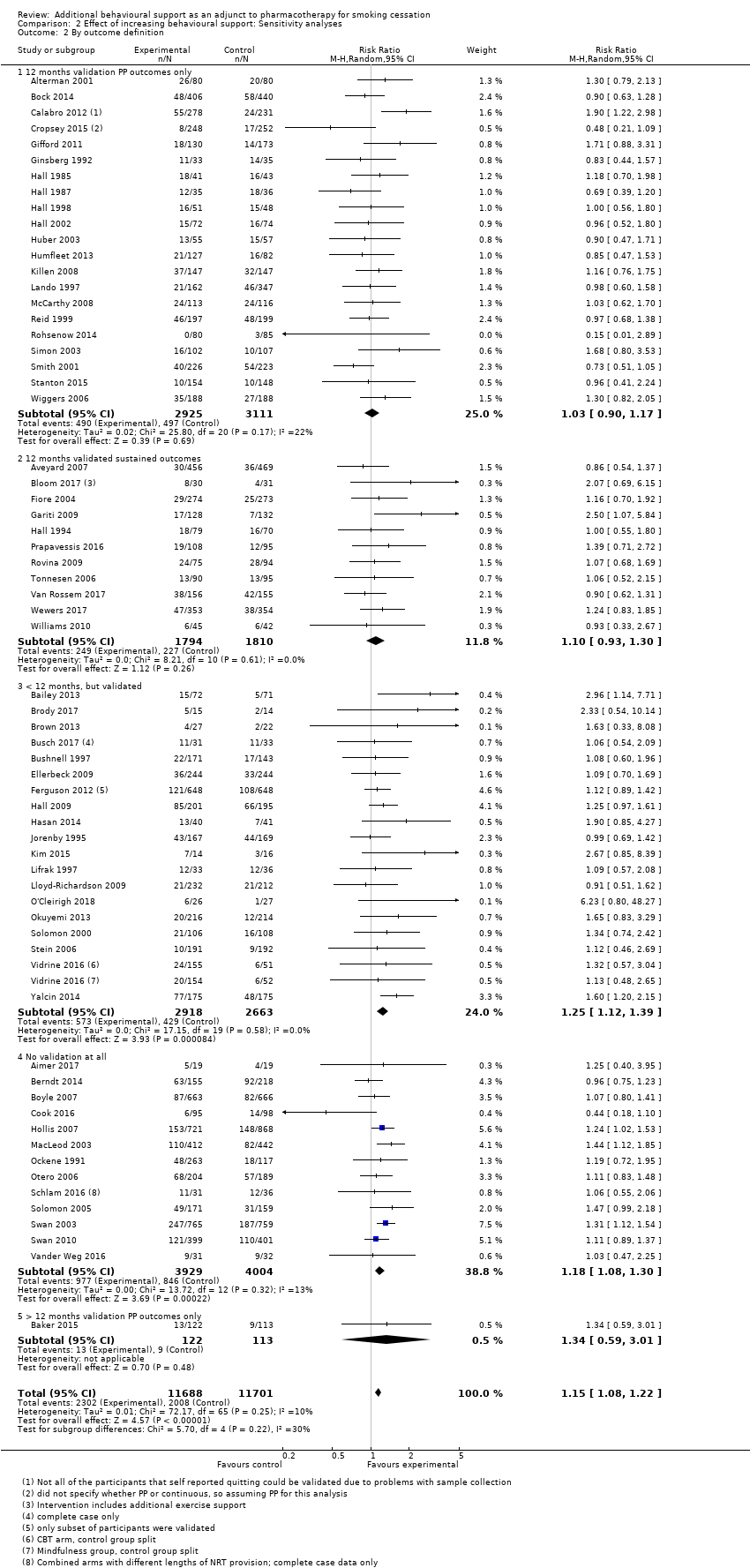
Comparison 2 Effect of increasing behavioural support: Sensitivity analyses, Outcome 2 By outcome definition.

Comparison 3 Studies matched for contact time. Abstinence at longest follow‐up point, Outcome 1 Abstinence at longest follow‐up.
| Behavioural interventions as adjuncts to pharmacotherapy for smoking cessation | ||||||
| Patient or population: People using smoking cessation pharmacotherapy | ||||||
| Outcomes | Illustrative absolute effects* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed successful quitters without intervention | Estimated quitters with intervention | |||||
| Pharmacotherapy (with variable level of behavioural support) | Additional behavioural support (in addition to pharmacotherapy) | |||||
| Smoking cessation at longest follow‐up | Study population1 | RR 1.15 | 23,331 | ⊕⊕⊕⊕ | Effect very stable over time: updates of this analysis (15 new studies added 2015; 18 new studies added 2019) have had minimal impact on the effect estimate. Little evidence of differences in effect based on amount of support or type of pharmacotherapy provided. | |
| 171 per 1000 | 197 per 1000 | |||||
| The estimated rate of quitting with behavioural intervention (and its 95% confidence interval) is based on the assumed quit rate in the control group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Based on the control group crude average 2Sensitivity analysis removing studies at high risk of bias yielded results consistent with those from the overall analysis. A funnel plot was inconclusive but suggested there may have been slightly more small studies with large effect sizes than with small effect sizes. However, asymmetry was not clear and we did not downgrade on this basis; given the large number of included studies and the degree of homogeneity between them, it is unlikely that smaller unpublished studies showing no effect, if they existed, would significantly alter our results. | ||||||
| Intervention | Control | ||||||
| Study ID | Pharmacotherapy | Modality (included face‐to‐face/ telephone only) | Number of contacts | Total duration (minutes) | Number of contacts | Total duration (minutes) | Comments |
| NRT | Face‐to‐face | 6 | 120 | 6 | 120 | ||
| NRT | Face‐to‐face | 4 | Unclear | Unclear | Unclear | ||
| NRT | Face‐to‐face | 16 | 4290 | 1 | 30 | Multiple arms ‐ highest vs lowest intensity | |
| NRT | Face‐to‐face | 7 | 140 | 4 | 80 | ||
| NRT | Face‐to‐face | 19 | 950 | 10 | 500 | ||
| NRT | Face‐to‐face | 17 | 1050 | 17 | 290 | ||
| NRT | Telephone | 5 | 100 | 5 | 100 | ||
| NRT | Face‐to‐face | 7 | 112 | 7 | 112 | ||
| NRT | Face‐to‐face | 7 | 285 | 7 | 105 | ||
| NRT | Face‐to‐face | 20 | 400 | 20 | 880 | Exercise sessions/time excluded | |
| NRT | Face‐to‐face | 3 | Unclear | 1 | Unclear | ||
| Choice | Face‐to‐face | 9 | Unclear | 0 | 0 | ||
| NRT | Telephone | 5 | 90 | 5 | 90 | ||
| NRT & Bupropion | Face‐to‐face | 22 | 970 | 12 | 720 | ||
| NRT | Face‐to‐face | Unclear | Unclear | Unclear | Unclear | ||
| NRT | Face‐to‐face | 6 | 220 | 6 | 87.5 | ||
| NRT | Face‐to‐face | 8 | 480 | 4 | 240 | ||
| NRT | Face‐to‐face | 2 | 120 | 1 | 5 | Intervention also had "access to 5 web‐based booster sessions" | |
| NRT | Face‐to‐face | 11 | 130 | 0 | 0 | Multifactorial ‐ highest vs lowest intensity | |
| NRT | Face‐to‐face | 4 | 100 | 1 | Unclear | ||
| Choice | Face‐to‐face | 6 | Unclear | 0 | 0 | Multiple arms ‐ highest vs lowest intensity | |
| NRT | Telephone | 6 | Unclear | Unclear | Unclear | ||
| NRT | Face‐to‐face | 5 | Unclear | 0 | 0 | Multiple arms ‐ highest vs lowest intensity | |
| Choice | Face‐to‐face | 10 | 125 | 4 | 30 | ||
| Bupropion | Face‐to‐face | 20 | Unclear | 1 | 60 | ||
| NRT | Face‐to‐face | 5 | Unclear | 2 | Unclear | ||
| NRT | Face‐to‐face | 14 | 1050 | 4 | Unclear | ||
| NRT | Face‐to‐face | 14 | 1050 | 5 | 300 | ||
| NRT | Face‐to‐face | 10 | 1200 | 5 | 450 | ||
| Nortriptyline | Face‐to‐face | 10 | 1200 | 5 | 450 | ||
| Bupropion/Nortriptyline | Face‐to‐face | 5 | 450 | 4 | 30 | ||
| NRT & Bupropion | Face‐to‐face | 11 | 330 | 5 | Unclear | Multifactorial study design | |
| NRT | Face‐to‐face | 7 | 195 | 6 | 105 | ||
| NRT | Telephone | 4 | 100 | 1 | 15 | Multiple arms ‐ highest vs lowest intensity | |
| NRT | Face‐to‐face | 5 | 450 | 5 | 225 | ||
| NRT | Face‐to‐face | 6 | 300 | 1 | 'Brief' | Multiple arms ‐ highest vs lowest intensity | |
| NRT | Face‐to‐face | 8 | 480 | 0 | 0 | Multiple arms ‐ highest vs lowest intensity | |
| NRT | Face‐to‐face | 6 | 210 | 6 | 210 | ||
| NRT & Bupropion | Face‐to‐face | 10 | 300 | 10 | 200 | ||
| NRT | Face‐to‐face | 8 | 320 | 8 | 80 | ||
| NRT | Face‐to‐face | 7 | 420 | 7 | 420 | ||
| NRT | Face‐to‐face | 4 | 48 | 0 | 0 | Multiple arms ‐ highest vs lowest intensity | |
| NRT | Face‐to‐face | 20 | 736.5 | 4 | 82.5 | ||
| NRT | Face‐to‐face | 5 | Unclear | 2 | Unclear | ||
| NRT | Telephone | 5 | 60 | 0 | 0 | ||
| NRT | Face‐to‐face | 8 | 480 | 8 | 480 | ||
| NRT | Face‐to‐face | 6 | 540 | 6 | 540 | ||
| Bupropion | Face‐to‐face | 13 | Unclear | 13 | Unclear | Control received 80 minutes less contact than intervention | |
| NRT & Varenicline | Face‐to‐face | 9 | Unclear | 5 | Unclear | ||
| NRT | Face‐to‐face | 5 | 45 | 2 | 15 | ||
| NRT | Face‐to‐face | 10 | 600 | 5 | 100 | ||
| NRT | Face‐to‐face | 6 | 105 | 1 | 12.5 | ||
| NRT | Face‐to‐face | 4 | 240 | 1 | 20 | Multiple arms ‐ highest vs lowest intensity | |
| NRT | Face‐to‐face | 36 | 1080 | 36 | 1080 | Intervention group: "exercise counselling delivered while the participant was engaged in exercise" ‐ have left this time in as also counselling | |
| NRT | Face‐to‐face | 64 | 1985 | 59 | 1860 | Multiple arms ‐ highest vs lowest intensity | |
| NRT | Face‐to‐face | 6 | Unclear | 3 | 45 | ||
| NRT | Face‐to‐face | 3 | 65 | 3 | 35 | ||
| Bupropion | Face‐to‐face | 9 | 540 | 1 | 15 | Multiple arms ‐ highest vs lowest intensity | |
| NRT | Face‐to‐face | 12 | 320 | 4 | 200 | Multifactorial study design | |
| Bupropion | Face‐to‐face | 7 | 420 | 7 | 420 | ||
| NRT | Face‐to‐face | 6 | 195 | 1 | 10 | ||
| NRT | Face‐to‐face | 6 | 90 | 0 | 0 | Multiple arms ‐ highest vs lowest intensity | |
| NRT | Telephone | 4 | 67 | 4 | 60 | Exact duration of contact not recorded, but averages given, intervention: 67.0 (± 25.8), control: 60.1 (± 23.9) | |
| Varenicline | Face‐to‐face | 5 | Unclear | 5 | Unclear | Comparing culturally‐tailored with standard counselling ‐ duration of sessions not stated | |
| NRT | Telephone | See note | See note | 0 | 0 | Control = "access to quitline"; intervention = "up to 12 calls" ‐ averaged 7 calls at 9 minutes each | |
| NRT | Telephone | 8.2 | 80 | 0 | 0 | Intervention numbers based on average number/duration of calls | |
| NRT | Face‐to‐face | 7 | Unclear | 3 | Unclear | ||
| NRT | Face‐to‐face | 3 | 65 | 2 | 5 | Control offered "up to 2 visits", intervention only offered 3rd visit if ready to quit | |
| Bupropion | Face‐to‐face | 12 | 1440 | 12 | 1440 | ||
| Bupropion | Telephone | 4 | Unclear | 1 | 7.5 | Multiple arms ‐ highest vs lowest intensity | |
| Varenicline | Telephone | 5 | 67 | 0 | 0 | ||
| NRT | Face‐to‐face | 12 | 270 | 10 | 150 | ||
| Varenicline | Face‐to‐face | 10 | 120 | 1 | 20 | Duration of sessions not stipulated, but maximum amounts recorded in paper. Intervention: 120, control: 20 | |
| Choice | Telephone | 6 | 150 | 0 | 0 | Intervention sessions listed as 20 to 30 minutes ‐ control was referral to a quitline, but there were no mandated sessions, so contact listed as 0 | |
| Vidrine 2016 (CBT) | NRT | Face‐to‐face | 8 | 960 | 4 | 40 | Vidrine study intervention 2 (control split) |
| Vidrine 2016 (MBAT) | NRT | Face‐to‐face | 8 | 960 | 4 | 40 | Vidrine study intervention 1 (control split) |
| NRT | Face‐to‐face | 12 | Unclear | 12 | Unclear | Sessions' duration not reported | |
| NRT | Face‐to‐face | 1 | 5 | 1 | 5 | ||
| NRT | Face‐to‐face | 9 | 945 | 9 | 945 | Exact duration not listed, but approximate range given | |
| NRT | Face‐to‐face | 7 | 210 | 6 | 180 | Compared 2 interventions, less intensive counted as control | |
| NRT | Face‐to‐face | 3 | Unclear | 1 | Unclear | ||
| NRT | Face‐to‐face | 24 | 1080 | 9 | 180 | ||
| NRT | Face‐to‐face | 4 | 240 | 4 | 240 | ||
| Choice | Face‐to‐face | 14 | 730 | 9 | 150 | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Subgroups by type of pharmacotherapy Show forest plot | 65 | 23331 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.08, 1.22] |
| 1.1 NRT | 49 | 16541 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [1.04, 1.21] |
| 1.2 Bupropion | 5 | 2298 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [1.10, 1.46] |
| 1.3 Nortriptyline | 2 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.60, 1.63] |
| 1.4 Varenicline | 2 | 1111 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.87, 1.27] |
| 1.5 NRT & bupropion | 3 | 719 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [1.00, 1.54] |
| 1.6 Choice of pharmacotherapy | 5 | 2490 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.00, 1.68] |
| 2 Subgroups by contrast in number of contacts between intervention & control Show forest plot | 63 | 21997 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.08, 1.22] |
| 2.1 4 to 8 or > 8 contacts versus no contact | 8 | 4018 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.02, 1.43] |
| 2.2 More than 8 contacts versus 1 to 3 contacts | 4 | 1063 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.70, 1.57] |
| 2.3 4 to 8 contacts versus 1 to 3 contacts | 18 | 9579 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.01, 1.19] |
| 2.4 More than 8 contacts versus 4 to 8 contacts | 12 | 1737 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.98, 1.33] |
| 2.5 Intervention & control in same contact category | 21 | 5600 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.16, 1.50] |
| 3 Subgroups by duration of contact in control condition (not prespecified) Show forest plot | 62 | 21695 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.08, 1.22] |
| 3.1 No contact for control | 8 | 4018 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.02, 1.43] |
| 3.2 'Brief intervention' for control | 22 | 10565 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.99, 1.21] |
| 3.3 'Dose response', over 30 minutes contact for control | 32 | 7112 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [1.08, 1.32] |
| 4 Subgroup by modality of intervention contact (not prespecified) Show forest plot | 65 | 23331 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.08, 1.22] |
| 4.1 Intervention delivered by telephone | 8 | 6670 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [1.15, 1.37] |
| 4.2 Intervention included face‐to‐face contact | 57 | 16661 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [1.03, 1.19] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Sensitivity analysis including intermediate intensity conditions. Adjunct behavioural support versus pharmacotherapy alone Show forest plot | 65 | 27425 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [1.07, 1.20] |
| 1.1 NRT | 49 | 18666 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.03, 1.19] |
| 1.2 Bupropion | 5 | 2298 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [1.10, 1.46] |
| 1.3 Nortriptyline | 2 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.60, 1.63] |
| 1.4 Varenicline | 2 | 1513 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.90, 1.26] |
| 1.5 NRT & bupropion | 3 | 719 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [1.00, 1.54] |
| 1.6 Choice of pharmacotherapy | 5 | 4057 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.00, 1.51] |
| 2 By outcome definition Show forest plot | 65 | 23389 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.08, 1.22] |
| 2.1 12 months validation PP outcomes only | 21 | 6036 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.90, 1.17] |
| 2.2 12 months validated sustained outcomes | 11 | 3604 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.93, 1.30] |
| 2.3 < 12 months, but validated | 19 | 5581 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [1.12, 1.39] |
| 2.4 No validation at all | 13 | 7933 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [1.08, 1.30] |
| 2.5 > 12 months validation PP outcomes only | 1 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.59, 3.01] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Abstinence at longest follow‐up Show forest plot | 15 | 4138 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.84, 1.25] |
| 1.1 Family support versus usual care telephone counselling | 1 | 471 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.72, 1.45] |
| 1.2 Face‐to‐face, tests attentional training v placebo training | 1 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.48, 2.50] |
| 1.3 ACT versus CBT telephone counselling | 1 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.74, 2.46] |
| 1.4 Positive psychotherapy versus usual care (face‐to‐face) | 1 | 77 | Risk Ratio (M‐H, Random, 95% CI) | 8.78 [0.49, 157.62] |
| 1.5 Couples treatment versus individual treatment (face‐to‐face) | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.37, 1.43] |
| 1.6 Behavioural activation versus standard treatment (face‐to‐face) | 1 | 68 | Risk Ratio (M‐H, Random, 95% CI) | 4.72 [0.24, 94.85] |
| 1.7 Culturally tailored versus standard (face‐to‐face) | 4 | 929 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.68, 1.92] |
| 1.8 Exercise counselling versus health education (face‐to‐face) | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.23, 1.89] |
| 1.9 Adherence counselling versus standard care (telephone) | 1 | 987 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.83, 1.15] |
| 1.10 MIndfulness versus CBT (face‐to‐face) | 1 | 309 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.48, 1.45] |
| 1.11 Quitline facilitation session versus brief advice (telephone) | 1 | 600 | Risk Ratio (M‐H, Random, 95% CI) | 1.57 [0.62, 4.00] |
| 1.12 Motivational interviewing versus health education | 1 | 378 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.33, 0.94] |

