Maintenance treatment with antipsychotic drugs for schizophrenia
References
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: chronic schizophrenia (DSM‐IV), at least two years of continuous antipsychotic medication. N = 310. | |
| Interventions | 1. Drug: aripiprazole. Fixed dose of 15 mg/day. N = 155. 2. Placebo: duration of taper (days): n.i. (pre‐trial medication was tapered, when appropriate, before stopping treatment). N = 155. Rescue medication: additional antipsychotic drugs were not allowed. | |
| Outcomes | Examined Relapse: CGI at least minimally worse, a PANSS score of ‐ 5 (moderately severe) on the subscore items of hostility or uncooperativeness on 2 successive days; or a ‐ 20% increase in PANSS total score. Leaving the study early. Service use ‐ number of participants hospitalised (including non psychiatric reasons). Death. Suicide attempts. Adverse effects. Violent/aggressive behaviour. Unable to use/Not included Global state: CGI (no usable data ). Mental state: PANSS, BPRS (no SD/no predefined outcome of interest). Physiological measures: vital signs (pulse rate, systolic and diastolic blood pressure, no data/no predefined outcome of interest), laboratory (haematology, no data; serum chemistries, no data a apart from creatinine phosphate/no predefined outcome of interest) urine tests, ECG (both no data/no predefined outcome of interest) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Correct randomisation assumed, because recent study from industry.. |
| Allocation concealment (selection bias) | Low risk | Correct allocation concealment assumed, because recent study from industry. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | High risk | A high number of participants (62.2%) left the study early, mostly because of relapse (61%), which was more frequent in the placebo group. For other outcomes this could be a problem. For the primary outcome survival analysis was used which was not a full ITT (one post‐baseline/dose) but only few participants were excluded. |
| Selective reporting (reporting bias) | High risk | Only those adverse events that occurred in at least 5% of the participants in either group were reported. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomised, no further details. | |
| Participants | Diagnosis: adolescent patients (13 to 17 years old) with schizophrenia (DSM‐IV‐TR) stabilised on aripiprazole for 7 to 21 weeks before entering the double‐blind phase. N = 146. | |
| Interventions | 1. Drug: aripiprazole. Flexible dose. Allowed dose range: 10 mg/day to 30 mg/day. Mean dose: 19,2 mg/day. N = 98. 2. Placebo: inert placebo. Duration of taper: n.i. N = 48. Rescue medication: not allowed. | |
| Outcomes | Examined Relapse: rating scale based and/or need for hospitalisation and/or clinical judgment. Leaving the study early (any reason, adverse events, inefficacy). Global state‐ number of patients in symptomatic remission (Andreasen criteria, LOCF endpoint cross‐sectional criteria) Global state‐ number of patients in sustained remission (Andreasen criteria, maintained for 6 months) Social functioning: Children´s Global Assessment Scale Adverse events Death. Suicidal ideation: Columbia Suicide Severity Rating Scale. Unable to use/Not included Global state ‐ number of participants improved (no usable data). Mental state: PANSS total score and subscores (no predefined outcome of interest). Quality of life: Pediatric Quality of Life Enjoyment and Satisfaction Questionnaire (no usable data). | |
| Notes | Sponsored by Otzuka Pharmaceutical Development and Commercialization. Adolescent patients subgroup. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised (2:1 ratio), no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | Low risk | The overall attrition rate of 33% could still be acceptable, though higher than 25%, but more participants in the placebo group left the study early, mostly due to relapse. This difference may have biased the results of outcomes other than leaving the study early and relapse, which was assessed using the Kaplan‐Meier survival curve analysis. Data for secondary outcomes were both analysed on an ITT basis (LOCF method) and provided for completers at several time points. |
| Selective reporting (reporting bias) | Low risk | The primary outcome relapse was reported as prespecified; Efficacy and Safety: Quality of Life score not reported completely, but it is not a primary outcome. |
| Other bias | High risk | Terminated early (after 37 relapse events), but it was pre‐planned. |
| Study characteristics | ||
| Methods | Randomisation: sponsor‐prepared computer‐generated randomisation code (2:1 ratio), stratified by region and by last stabilisation dose of study drug. | |
| Participants | Diagnosis: Schizophrenia (DSM‐IV‐TR), diagnosed at least 3 years before. | |
| Interventions | 1. Drug: aripiprazole IM, 1‐month formulation. N = 269 Flexible dose. Mean dose: 396.3 mg/4 weeks. Allowed dose range: either 300 mg or 400 mg/4 weeks. 2. Placebo: duration of taper: depending on the aripiprazole depot half‐life (between 29.9 and 46.5 days). N = 134. Rescue medication: benzodiazepines (maximum 6 mg/day) and anticholinergics (antiparkinson) were permitted, although not within 8 to 12 hours (respectively) of rating scale assessments. | |
| Outcomes | Examined Relapse (rating scale defined and/or need for hospitalisation and/or emergent violent behaviour). Leaving the study early (any cause, adverse events, inefficacy). Global state ‐ Number of participants in sustained remission (Andreasen criteria). Service use ‐ Number of participants hospitalised. Participants´satisfaction with care: Patient Satisfaction with Medication Questionnaire. Social functioning: Personal and Social Performance scale. Adverse effects. Death. Suicide ideation and behaviour: CGI‐SS, Columbia Suicide Severity Rating Scale and Columbia Classification Algorythm of Suicide Assessment. Violent/aggressive behaviour. Unable to use/Not included Global state ‐ number of participants improved (no usable data). Mental state: Positive and Negative Symptoms Scale total scores and subscales (no predefined outcome of interest). Neurocognitive function: Trail Making Test (A), Tower of London, Letter‐Number Span (no predefined outcome of interest). Compliance to treatment: Drug Attitude Inventory Score, Medication Adherence Questionnaire (no predefined outcome of interest). Carer´s satisfaction with care: Investigator´s Assessment Questionnaire (no usable data). | |
| Notes | Sponsored by Otsuka. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sponsor‐prepared computer‐generated randomisation code (2:1 ratio), stratified by region and by last stabilisation dose of study drug |
| Allocation concealment (selection bias) | Low risk | Interactive voice/web response system. |
| Blinding of participants and personnel (performance bias) | Unclear risk | IM trial medications had different appearance (aripiprazole: milky white suspension; placebo: clear solution); they were prepared and administered by an unblinded Trial Drug Manager. |
| Blinding (performance bias and detection bias) | Unclear risk | IM trial medications had different appearance (aripiprazole: milky white suspension; placebo: clear solution); they were prepared and administered by an unblinded Trial Drug Manager. Two participants were unblinded at the site level (one incident with depot dose log, one incidental access to the drug storage cabinet given by the monitor), both withdrawn from the study. |
| Blinding (performance bias and detection bias) | Low risk | IM trial medications had different appearance (aripiprazole: milky white suspension; placebo: clear solution); they were prepared and administered by an unblinded Trial Drug Manager. Two participants were unblinded at the site level (one incident with depot dose log, one incidental access to the drug storage cabinet given by the monitor), both withdrawn from the study. |
| Incomplete outcome data (attrition bias) | High risk | The total attrition rate (35%) was higher than 25% but could still be acceptable. However more participants in the placebo group dropped out, mostly due to relapse (reasons are unbalanced between groups). The primary outcome (relapse) was assessed using the Kaplan‐Meier survival curve analysis. Data for secondary outcomes were analysed on an ITT basis (LOCF). |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | Study terminated early after an interim analysis (64 relapse events), but it was pre‐planned. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (DSM‐IV). N = 386. | |
| Interventions | 1. Drug: asenapine. Fixed dose (same dose as at end of stabilisation phase): mean 17.6 mg/day. N = 194. 2. Placebo: duration of taper: 0 days. N = 192. Rescue medication: benzodiazepines, anticholinergics, antidepressants. | |
| Outcomes | Examined Relapse: CGI‐severity >=4, moderately ill for one week was accompanied by: PANSS total score increase >=20% (a 10 point increase if PANSS was lower than 50), a PANSS item score >=5 on hostility of uncooperativeness or a PANSS item score >=5 and two items of unusual thought content, conceptual disorganisation or hallucinatory behaviour. Relapse was also judged to appear if in the investigator's opinion schizophrenia, risk of violence to self or others, or suicide risk increased so >=1 of the following was required: an additional >=2mg/day lorazepam, compared with the highest open‐label dose for 1 week, addition of antipsychotic, addition or dosage increase of an antidepressant or mood‐stabiliser, increased psychiatric care, arrest or imprisonment, electroconvulsive therapy, or other relevant measures. Suicidal ideation and behaviour. Adverse effects: at least one adverse event, at least one movement disorder, akathisia, sedation, weight gain. Unable to use/Not included Mental state: PANSS (no predefined outcome of interest). Global state: CGI (no usable data ). Leaving the study early (data are unclear). Electrocardiogram (no predefined outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules in taste. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules in taste. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules in taste. |
| Incomplete outcome data (attrition bias) | High risk | High dropout rate, but exact number of dropouts could not be calculated. Dropouts were not clearly enough reported. Survival curve analysis was used for the primary outcome relapse. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: sponsor‐prepared computer‐generated randomisation code (1:1 ratio), assignment of blocks of randomisation numbers to trial centres and individual numbers to patients. | |
| Participants | Diagnosis: Schizophrenia (DSM‐IV‐TR), diagnosed at least 3 years before; stabilised on study drug after resolution of an acute exacerbation. | |
| Interventions | 1. Drug: Brexpiprazole. N = 97 Fixed dose. Mean dose: 3.6 mg/day. Allowed dose range: 1 mg/day to 4 mg/day. 2. Placebo: duration of taper: no. N = 105. Rescue medication: n.i. | |
| Outcomes | Examined Relapse (rating scale defined and/or need for hospitalisation and/or emergent violent/suicidal behaviour). Leaving the study early (any cause, adverse events, inefficacy). Social functioning: Personal and Social Performance scale. Adverse effects Suicidal ideation and behavior: Columbia Suicide Severity Scale Unable to use/Not included Global state ‐ number of participants improved: CGI‐I defined (no usable data). Global state ‐ number of participants in remission: CGI‐S defined (no usable data). Mental state: Positive and Negative Symptoms Scale total score and subscales (no predefined outcome of interest) Affective symptoms: PANSS excited component score, PANSS Marder Anxiety/Depression score (no predefined outcome of interest). Neurocognitive function: Cogstate computerized cognitive test battery (no predefined outcome of interest) Social functioning: Global Assessment of functioning (already used data regarding Personal and Social Performance scale). | |
| Notes | Sponsored by Otsuka. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sponsor‐prepared computer‐generated randomisation code, assignment of blocks of randomisation numbers to trial centres and individual numbers to patients. |
| Allocation concealment (selection bias) | Low risk | Interactive voice/web response system. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. |
| Incomplete outcome data (attrition bias) | High risk | The overall attrition rate of 46% was high, and more participants in the placebo group left the study early, mostly due to relapse. This difference may have biased the results of outcomes other than leaving the study early and relapse, which was assessed using the Kaplan‐Meier survival curve analysis. Data for secondary outcomes were analysed on an ITT basis. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | Terminated early after an interim analysis, but it was pre‐planned. |
| Study characteristics | ||
| Methods | Randomisation: randomised (1:1 ratio), no further details. | |
| Participants | Diagnosis: Schizophrenia (DSM‐IV‐TR), stabilized on treatment for at least 12 weeks before double‐blind phase. | |
| Interventions | 1. Drug: cariprazine. N = 101 Fixed dose. Mean dose: 7.07 mg/day. Allowed dose range: 3 mg/day to 9 mg/day. 2. Placebo: duration of taper: n.i. N = 99. Rescue medication: anticholinergics (antiparkinson), beta‐blocker (akatihsia), lorazepam or oxazepam (anxiety/agitation). | |
| Outcomes | Examined Relapse (clinical judgement and/or need of hospitalisation). Leaving the study early (any reason, inefficacy, adverse events) Global state ‐ number of participants in sustained remission (Andreasen criteria) Social functioning: Personal and Social Performance Scale Adverse events Death Suicide attempts Suicidal ideation: Columbia‐Suicide Severity Rating Scale Unable to use/Not included Mental state: PANSS total score and subscores (no predefined outcome of interest), negative symptoms assessed with NSA‐16 (no predefined outcome of interest). Global state ‐ number of improved participants: CGI‐S and CGI‐I scores (no usable data). | |
| Notes | Sponsored by Forest, Actavis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Low risk | Investigators and patients were blinded to the double‐blind treatment assignment through an interactive web‐response system. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical appearing capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical appearing capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical appearing capsules. |
| Incomplete outcome data (attrition bias) | High risk | The overall attrition rate was high (68%); it was slightly different between the study arms, and reasons were different (more participants in the placebo group left the study early due to relapse). This difference may have biased the results of outcomes other than leaving the study early and relapse, which was assessed using the Kaplan‐Meier survival curve analysis. No full ITT analysis for other outcomes (only patients that had at least one evaluation were included). |
| Selective reporting (reporting bias) | Low risk | No clear evidence of selective reporting. |
| Other bias | High risk | Terminated early, but it was pre‐planned. |
| Study characteristics | ||
| Methods | Randomisation: matched and then randomised by a research assistant. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis), less than 50 years, on chlorpromazine for at least six months, had reached a stable improved state. N = 80. | |
| Interventions | 1. Drug: chlorpromazine. Fixed dose of 200 mg/day. N = 40. 2. Drug: reserpine*. Fixed dose of 2 mg/day. N = 40. 3. Placebo: duration of taper 0 days. N = 40. Rescue medication: not indicated, probably not allowed. | |
| Outcomes | Examined Leaving the study early. Suicide attempts. Unable to use/Not included Mental state: Lorr Multidimensional Scale for Rating Psychiatric Patients (no SD/no predefined outcome of interest). Behaviour: Psychiatric Behaviour Rating Scales (no SD / no predefined outcome of interest). | |
| Notes | *this group was not used in the analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Matched and then randomised by a research assistant. |
| Allocation concealment (selection bias) | Low risk | By a research assistant who carefully guarded the identity of patients and the assigned treatment regimen. Furthermore, medication was assigned by the director of professional services who kept the names for use in case a patient had to be withdrawn from the study. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. |
| Incomplete outcome data (attrition bias) | Low risk | Overall 11% dropped out, most of them due to relapse (88%) in the placebo group. As relapse, dropout and suicide were the only outcomes, this did not produce a risk of bias. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: participants were ranked for morbidity, then matched, then randomised. | |
| Participants | Diagnosis: chronic, long term hospitalised male psychotics (clinical diagnosis), 86 schizophrenia, 6 chronic brain syndrome, 2 personality disorders, 2 n.i.. N = 96. | |
| Interventions | 1. Drug: chlorpromazine ‐ Flexible dose. Allowed dose range: n.i.. Mean dose: n.i.. N = 48. 2. Placebo: duration of taper: 0 days. N = 48. Rescue medication: occasional use of sedatives, antipsychotics were not allowed. | |
| Outcomes | Examined Relapse: condition worsened to such a point that ordinarily a complete change in treatment would be considered. Leaving early due to inefficacy. Unable to use/Not included Behaviour: Lyon’s Behaviour Scale (no SD / no prespecified outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were ranked for morbidity, then matched, then randomised. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Low risk | Double‐blind, identical capsules, each participant was provided medication in individual container. Staff guessed on which medication the participants were but could not guess adequately. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules, each participant was provided medication in individual container. Staff guessed on which medication the participants were but could not guess adequately. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules, each participant was provided medication in individual container. Staff guessed on which medication the participants were but could not guess adequately. |
| Incomplete outcome data (attrition bias) | Unclear risk | It could be that there were participants leaving the study early but this was not clearly reported. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | Blinding was broken once a participant relapsed. |
| Study characteristics | ||
| Methods | Randomisation: "randomly assigned”, no further details. | |
| Participants | Diagnosis: schizophrenia (clinical diagnosis), continuously hospitalised for at least two years. N = 420. | |
| Interventions | 1. Drug: chlorpromazine. Fixed dose of 300 mg/day. N = 208. *2. Drug: chlorpromazine. Fixed dose of 2000 mg/day (titrated within 45 days, dose reduction to 1500 mg/day was possible). N = 208. 3. Placebo: duration of taper: 0 days. N = 212. *4. Routine treatment (any antipsychotic medication, any dose). N = 210. Rescue medication: n.i., but probably not allowed. | |
| Outcomes | Examined Relapse: a patient was considered relapsed if he regressed and had to be returned to known medication before the end of the 24‐week period. Leaving the study early. Global state: number of participants improved. Death. Adverse effects: based on clinical interview. Unable to use/Not included Mental state: Inpatient Multidimensional Psychiatric Scale, Brief Psychiatric Rating Scale (both only P values/no predefined outcome of interest). Global state: number of participants in remission (no usable data, only reported for a subgroup of patients evaluated by the same rater during the trial). Behaviour: Nurses’ Observation Scale for Inpatient Evaluation (no predefined outcome of interest). Readiness for discharge: Discharge‐Readiness Inventory (no predefined outcome of interest). Ophthalmologic examination (no predefined outcome of interest). | |
| Notes | Quote: *We only analysed the low dose group, because the high dose was excessively high (2000mg chlorpromazine per day) and because the conventional treatment group was not double‐blind. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, liquid formulation. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, liquid formulation. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, liquid formulation. |
| Incomplete outcome data (attrition bias) | High risk | Overall 26% dropped out (of which 87% due to relapse). 15% of the participants in the drug group compared to 38% of the participants in the placebo group left the study early. This difference in attrition is a problem for the analysis of other outcomes than relapse. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomly assigned, no further details. | |
| Participants | Diagnosis: schizophrenia (DSM‐II, undifferentiated type 46.3%, paranoid 39%, acute differentiated 8%, schizoid affective 2.7%, other 3.8%), currently hospitalised for less than 2 years. N = 374. | |
| Interventions | Previous medication was gradually shifted to chlorpromazine for two months. 2. Placebo: duration of taper: 0 days. N = 182. Rescue medication: not indicated, but probably not allowed. | |
| Outcomes | Examined Relapse: clinical deterioration of such magnitude that hospitalisation appeared imminent. Service use: number of participants hospitalised. Unable to use/Not included Leaving the study early (numbers not specified for each group separately). Mental state: Brief Psychiatric Rating Scale, Inpatient Multidimensional Psychiatric Scale, Springfield Symptom Index, Hopkin’s Symptom Distress Check List (all no SDs and data only given for subgroups/no predefined outcome of interest). Social behaviour and adjustment: Katz Adjustment Scale, Major Role Adjustment Inventory (no usable data). Number of participants employed (no usable data). | |
| Notes | Half of the participants randomly received major role therapy in addition to chlorpromazine or placebo. For the purpose of this review the four resulting groups were pooled as described above. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules, no further details. |
| Incomplete outcome data (attrition bias) | Low risk | Relatively few participants left the study early due to reasons other than relapse which was the only outcome (n = 31). Although it is unclear in which group they occurred the small percentage does not represent an important risk of bias. |
| Selective reporting (reporting bias) | Low risk | No clear evidence for selective reporting. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: random number table. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis). N = 14. | |
| Interventions | 1. Drug: chlorpromazine ‐ Fixed dose. Allowed dose range n.i.. Mean dose n.i.. N = 7. 2. Placebo: duration of taper: 0 days. N = 7. Rescue medication: benztropine. | |
| Outcomes | Examined Relapse: worsening of psychotic symptoms. Leaving the study early. Unable to use/Not included Behaviour: NOSIE (no data / no prespecified outcome of interest). Extrapyramidal symptoms: clinical and electrophysiological evaluation (no usable data). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table. |
| Allocation concealment (selection bias) | Low risk | All personnel except for the treating psychiatrist remained unaware of the code until the end of the study. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind (patients, scientists, nurses, only the treating psychiatrist knew the treatment). |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind (patients, scientists, nurses, only the treating psychiatrist knew the treatment). |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind (patients, scientists, nurses, only the treating psychiatrist knew the treatment). |
| Incomplete outcome data (attrition bias) | Low risk | One participant in the placebo group left the study prematurely which is an acceptable rate. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomised, no further details. | |
| Participants | Diagnosis: schizophrenia (clinical diagnosis), continuously in hospital for at least 6 years (mean 28 years). | |
| Interventions | 1. Drug: Chlorpromazine ‐ mean dose: 216 mg/day. N = 15. Allowed dose range: the participants were kept on their initial dose. 2. Placebo: duration of taper 0 days. N = 17. Rescue medication: benzodiazepines, anticholinergics. | |
| Outcomes | Examined Relapse (need of antipsychotic medication). Leaving the study early. Unable to use/Not included Behaviour: Ward Behaviour Rating Scale of Wing (no SD / no prespecified outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Low risk | Pharmacists held the key. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. |
| Incomplete outcome data (attrition bias) | Low risk | All participants completed the trial. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No obvious other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (hospital diagnosis, there was an additional evaluation based on research criteria (Kraepelinian), but the results of all participants are presented here), in remission (no positive symptoms, but other symptoms could be present). Patients who were uncooperative in the stabilisation phase were not included in the study. N = 73. | |
| Interventions | 1. Drug: fluphenazine decanoate combined with procyclidine flexible dose of 0.5 mL to 2.0 mL biweekly. Mean dose: n.i.. N = 23. 2. Drug: oral fluphenazine combined with procyclidine. Flexible dose of 5 mg/day to 20 mg/day. Mean dose: n.i.. N = 28. 3. Placebo: duration of taper: 0 days. N = 22. Rescue medication: not clearly indicated, but probably not allowed. Prophylactic antiparkinson medication. | |
| Outcomes | Examined Relapse: substantial deterioration with a potential of marked social impairment. Leaving the study early. Adverse effects: dropout due to specific adverse events. Death. Unable to use/Not included Global state (CGI ‐ no SD, data for relapsed subgroup only). Mental state (Brief Psychiatric Rating Scale ‐ no SD, data for relapsed subgroup only). Employment status (no usable data, unclearly reported). Social adjustment: Katz Adjustment Scale ‐ no SD, only data for relapsed subgroup and a matched but not randomised subsample. Akinesia: Periodic Evaluation Record (no SD, data for relapsed subgroup only). Suicide attempts (unclearly reported, probably not for the global sample). | |
| Notes | * 11 out of 73 patients were then diagnosed as non schizophrenic by the research staff. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Low risk | Double‐dummy technique, procyclidine was added to fluphenazine to avoid unmasking by extrapyramidal side effects. |
| Blinding (performance bias and detection bias) | Low risk | Double‐dummy technique, procyclidine was added to fluphenazine to avoid unmasking by extrapyramidal side effects. |
| Blinding (performance bias and detection bias) | Low risk | Double‐dummy technique, procyclidine was added to fluphenazine to avoid unmasking by extrapyramidal side effects. |
| Incomplete outcome data (attrition bias) | High risk | 67% of the participants discontinued the study due to relapse (41%) or other reasons. More participants in the drug group discontinued due to adverse events, while more participants in the placebo group discontinued due to relapse. This differential attrition can cause bias. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: random 2:1, no further details. | |
| Participants | Diagnosis: schizophrenia (DSM‐II). N = 67. | |
| Interventions | 1. Drug: oral fluphenazine (n = 6) or depot fluphenazine (n = 11). Fixed/flexible dose: unclear. Allowed dose range: unclear. Mean dose: unclear. N = 17. 2. Placebo: duration of taper: 0 days. N = 50. Rescue medication: n.i., but antipsychotics were probably not allowed. | |
| Outcomes | Examined Relapse: rehospitalisation or deterioration in clinical condition which could not be managed within protocol limits (e.g. increased psychological support or adjustment of dosage). Adverse effects: tardive dyskinesia (AIMS). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random 2:1, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether there were participants who left the study early. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: first episode schizophrenia (clinical diagnosis), no evidence of drug abuse or important medical illnesses. When diagnoses were reassessed by Research Diagnostic Criteria, 19 had schizophrenia, 3 had unspecific schizophrenic psychoses, 4 had other psychiatric disorders, one mania with schizotypal features and one depression with schizotypal features. N = 28. | |
| Interventions | 1. Drug: oral fluphenazine ‐ Flexible dose. Allowed dose range: 5‐20 mg/day. Mean dose: n.i.. N = n.i.. 2. Drug: depot fluphenazine ‐ Flexible dose. Allowed dose range: 12.5 mg to 50 mg biweekly. Mean dose: n.i.. N = n.i.. 2. Placebo: duration of taper: 0 days. N = 17. Rescue medication: not indicated. | |
| Outcomes | Examined Relapse: a substantial clinical deterioration with a potential for marked social impairment. Patients were considered dropouts only if they showed no signs of clinical deterioration at the time they left the study. Leaving the study early. Unable to use/Not included Social aspects of premorbid personality: Premorbid Asocial Adjustment Scale (data on placebo group only/no predefined outcome of interest). | |
| Notes | The design was changed during the study in that only non‐compliant patients were randomised to depot fluphenazine or depot placebo, and the randomisation was changed to 2‐1‐1 (placebo, oral fluphenazine, depot fluphenazine). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, all participants received both pills and injections (active or placebo) to maintain double‐blind conditions. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, all participants received both pills and injections (active or placebo) to maintain double‐blind conditions. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, all participants received both pills and injections (active or placebo) to maintain double‐blind conditions. |
| Incomplete outcome data (attrition bias) | High risk | 20 out of 28 participants left the study early, 10 for other reasons than relapse, which was the only outcome apart from leaving the study early. This may present a bias. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Unclear risk | The design was changed during the study in that only non‐compliant patients were randomised to depot fluphenazine or depot placebo, and the randomisation was changed to 2‐1‐1 (placebo, oral fluphenazine, depot fluphenazine). It is unclear whether this biased the results. |
| Study characteristics | ||
| Methods | Randomisation: randomly assigned, no further details. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis), 12 paranoid, 3 hebephrenic, 2 catatonic, 1 simple, 6 chronic undifferentiated, on antipsychotic medication for a mean duration of 2 years. N = 24. | |
| Interventions | 1. Drug: fluphenazine decanoate ‐ Flexible doses. Allowed dose range: 12.5 to 75/mg biweekly. Mean dose: n.i.. N = 13 2. Placebo: sesame oil injections. Duration of taper: 0 days. N = 11. Rescue medication: antiparkinson medication, additional fluphenazine decanoate ‐ but this was considered to be a relapse. | |
| Outcomes | Examined Relapse: clinical deterioration requiring additional antipsychotic drug treatment. Leaving study early. Service use: number of participants hospitalised. Adverse effects (at least one movement disorder). Unable to use / Not included: Global state: 7‐point scale of severity (no usable data for the two study arms ). Mental state: scale published by the authors (no SD/no predefined outcome of interest). Adverse effects: scale published by the authors (no numbers). Physiological measures: ECG, EEG, laboratory (all no data/no predefined outcomes of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, placebo treated participants received injections of sesame oil in a similar amount. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, placebo treated participants received injections of sesame oil in a similar amount. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, placebo treated participants received injections of sesame oil in a similar amount. |
| Incomplete outcome data (attrition bias) | Low risk | No participant left the study early. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | In case of deterioration the participants received additional antipsychotic drugs. This is a problem for the analysis of side effects. |
| Study characteristics | ||
| Methods | Randomisation: randomly allocated by research assistant. | |
| Participants | Diagnosis: chronic schizophrenia (Present State Examination), chronicity defined by at least 2 admissions or 1 admission lasting longer than 6 months, 71 schizophrenic psychosis with delusions or auditory hallucinations, six non affective delusional psychoses, three catatonic schizophrenia. N = 81. | |
| Interventions | 1. Drug ‐ Fixed/flexible dose: allowed dose range: 25 mg/month ‐ no upper limit. Mean dose: 26.4 mg/month. N = 41. 2. Placebo: duration of taper: n.i.. N = 40. Rescue medication: antidepressants, antiparkinson medication | |
| Outcomes | Examined Relapse: deterioration of condition to a degree that participant had to be taken out of the trial to ensure that active medication was prescribed, prescription of oral phenothiazines. Leaving the study early. Service use: number of participants hospitalised. Number of participants employed. Death. Violent/aggressive behaviour. Adverse effects: use of antiparkinson medication. Unable to use/Not included Mental state: Present State Examination (no data/no predefined outcome of interest). Social functioning: Social Performance Schedule, Events Schedule of Bron and Birley (no usable data) Suicidal ideation (no usable data, only reported as referred by the patients´ informants to the study rater). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly allocated by research assistant. |
| Allocation concealment (selection bias) | Low risk | Apart from the research assistant no one knew who was on drug or placebo until the data were analysed. |
| Blinding of participants and personnel (performance bias) | Low risk | Double‐blind, sesame oil injections, unmarked ampoules. Blinding was tested at the end of the trial and it worked. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, sesame oil injections, unmarked ampoules. Blinding was tested at the end of the trial and it worked. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, sesame oil injections, unmarked ampoules. Blinding was tested at the end of the trial and it worked. |
| Incomplete outcome data (attrition bias) | Unclear risk | Overall, 43% of the participants left the study early (no complete ITT for some outcomes). |
| Selective reporting (reporting bias) | Low risk | No evidence for selected reporting. |
| Other bias | Low risk | No evidence of other bias |
| Study characteristics | ||
| Methods | Randomisation: no details (just reported as a "randomised study”). | |
| Participants | Diagnosis: chronic schizophrenia with an acute episode within 6 to 12 months before study entry (no details about diagnostic criteria). N = 20. | |
| Interventions | 1. Drug: fluphenazine depot. Fixed dose: 25 mg or 50 mg/month (long‐acting formulation). Mean dose: n.i.. N = 10 randomised (but data available only for 9 patients who completed the study). 2. Placebo: duration of taper (days): n.i.. N = 10 randomised (but data available only for 7 patients who completed the study). Rescue medication: antiparkinson medication at study entry (and then progressively tapered off, without a prespecified schedule). | |
| Outcomes | Examined Relapse: defined as worsening of clinical status needing an adjunctive new antipsychotic treatment. Leaving the study early. Global state: number of participants improved. Unable to use/Not included Mental state: BPRS (no prespecified outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details (just reported as a "randomised study”). |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind ("patients and authors were not aware of the allocated treatment"). |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind ("patients and authors were not aware of the allocated treatment”). |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind ("patients and authors were not aware of the allocated treatment”). |
| Incomplete outcome data (attrition bias) | Unclear risk | 25% of the participants dropped out, all due to relapse. This may still be acceptable. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: matched then each pair randomised, no further details. | |
| Participants | Diagnosis: probable or definite schizophrenia, any subtype (Research Diagnostic Criteria), in remission for at least 4 weeks or at stable clinical plateau despite vigorous chemotherapy. N = 16. | |
| Interventions | 1. Drug: fluphenazine decanoate ‐ Flexible dose. Allowed dose range: 1.25 mg to 5.0mg biweekly. Mean dose: n.i.. N = 8. 2. Placebo: duration of taper: 0 days, but previously treated with depot medication. N = 8. Rescue medication: minor tranquillisers, additional antipsychotic drugs were not allowed. | |
| Outcomes | Examined Relapse: increase in or re‐emergence of significant symptoms suggesting imminent psychotic relapse. Leaving the study early. Unable to use/Not included Adverse effects (no data). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Matched, then each pair randomised, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | Low risk | Two participants in the drug group (1 relapse, 1 unclear) left the study early, and 7/8 participants in the placebo group dropped out due to relapse. As relapse and dropout were the only outcomes, this did not lead to bias. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomly assigned. | |
| Participants | Diagnosis: chronic schizophrenic outpatients (DSM‐III). N = 31. | |
| Interventions | 1. Drug: fluphenazine decanoate‐ Fixed doses. Allowed dose range: n.i. ‐ same dose as before. Mean dose: n.i.. N = 14. | |
| Outcomes | Examined Relapse: clinical judgement. Leaving the study early. Service use: number of participants hospitalised. Social functioning: Global Assessment Scale (GAS). Unable to use/Not included Community adjustment: Weissman Social Adjustment scale (no usable data) Depression: SADS (no mean, no SD/no prespecified outcome of interest). Adverse effects: tardive diskinesia (no usable data). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, placebo injection. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, placebo injection. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, placebo injection. |
| Incomplete outcome data (attrition bias) | Low risk | 3 out of 30 participants (10%) left the study early which is an acceptable rate, irrespective of the statistical analysis (completer analysis). |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: participants were matched for age, sex, duration of illness, and severity of symptoms in the preceding episode and then assigned based on a randomised schedule. | |
| Participants | Diagnosis: schizophrenia (ICD‐9 and Present State Examination), with two or more episodes and several first rank symptoms in previous episode, free of psychopathology for at least 12 months, on fluphenazine decanoate for at least 2 years. N = 70. | |
| Interventions | 1. Drug: fluphenazine decanoate. Fixed dose of 50 mg IM four/eight weekly. N = 35. 2. Placebo: vitamin B complex IM. Duration of taper: 0 days. N = 35. Rescue medication: nitrazepam for sleep and benzhexol for extrapyramidal side‐effects; additional antipsychotic drugs were not allowed. | |
| Outcomes | Examined Relapse (re‐emergence of definite schizophrenic psychopathology necessitating hospital admission or other major treatment change). Leaving the study early. Death. Adverse effects: tardive dyskinesia (Aquired Involuntary Movements Scale). Unable to use/Not included Mental state: BPRS (no mean, no SD/no predefined outcome of interest). Adverse effects: extrapyramidal symptoms ‐ use of antiparkinson medication (combined with nitrazepam), use of additional nitrazepam for sleep (combined with use of antiparkinson medication). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were matched for age, sex, duration of illness, and severity of symptoms in the preceding episode and then assigned based on a randomised schedule. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | High risk | Double‐blind, evaluating psychiatrist and participants were unaware of the contents of their injections. It seems that treating psychiatrist was aware of the treatment. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, evaluating psychiatrist and participants were unaware of the contents of their injections. It seems that treating psychiatrist was aware of the treatment. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, evaluating psychiatrist and participants were unaware of the contents of their injections. It seems that treating psychiatrist was aware of the treatment. |
| Incomplete outcome data (attrition bias) | High risk | Overall dropout rate drug 40% versus placebo 66%, most due to relapse. This poses a risk for bias for other outcomes. Completer analysis. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for other sources of bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: chronic schizophrenia (Research Diagnostic Criteria), stable for at least 5 years (absence of clinical deterioration and/or an increase of neuroleptic medication, retrospectively and in addition prospectively for at least 12 months), all on fluphenazine decanoate. N = 24. | |
| Interventions | 1. Drug: fluphenazine decanoate.Fixed dose: mean 50.4 mg/4 weeks. N = 12. 2. Placebo: duration of taper: 0 days, but all participants were on depot medication before the study. N = 12. Rescue medication: n.i., but probably not allowed. | |
| Outcomes | Examined Relapse: at least 25% increase of BPRS total score and judgement of by nurse according to Psychotic Inpatient Profile. Unable to us /Not included Mental state: BPRS total, Psychotic Inpatient Profile (for both scales means for subgroups only / no predefined outcome of interest). Physiological measures: prolactin levels (no SD’s/no predefined outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, placebo was sesame oil of identical volume and identical in physical appearance, |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, placebo was sesame oil of identical volume and identical in physical appearance. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, placebo was sesame oil of identical volume and identical in physical appearance. |
| Incomplete outcome data (attrition bias) | Unclear risk | There is no statement on participants leaving the study early. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | There was a baseline imbalance in terms of gender and in terms of baseline fluphenazine dose. |
| Study characteristics | ||
| Methods | Randomisation: unclear, randomisation assumed due to double‐blinding. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis), all had previously responded to haloperidol and were adequately maintained on it. N = 49. | |
| Interventions | 1. Drug: haloperidol tablets.* Flexible dose. Allowed dose range: n.i.. Mean dose: mean 8.8mg/day. N = 17. 2. Drug: haloperidol liquid.* Flexible dose. Allowed dose range: n.i.. Mean dose: 10.4 mg/day. N = 16. 3. Placebo: duration of taper: 0 days. N = 16. Rescue medication: antiparkinson medication was allowed. | |
| Outcomes | Examined Relapse: deterioration of global state. Leaving the study early. Global state ‐ number of participants improved. Adverse effects (movement disorders). Suicide ideation. Unable to use/Not included Mental state: Brief Psychiatric Rating Scale (no SD/no predefined outcome of interest). Global state: Clinical Global Impression of Severity (no SD/no predefined outcome of interest). Behaviour: Nurses Observation Scale for Inpatient Evalutation (NOSIE) (no SD/no predefined outcome of interest). Adverse effects: laboratory (insufficient data/no predefined outcome of interest), vital signs (insufficient data/no predefined outcome of interest). | |
| Notes | *Groups 1 and 2 were pooled for the purpose of this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear, randomisation assumed due to double‐blinding. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, all participants received both (placebo) tablets and (placebo) liquid, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, all participants received both (placebo) tablets and (placebo) liquid, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, all participants received both (placebo) tablets and (placebo) liquid, no further details. |
| Incomplete outcome data (attrition bias) | Low risk | Acceptable dropout rate (10%), which should not affect other outcomes (completer analysis). |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (DSM‐III), not dangerous to themselves, no hospitalisation in the last year. N = 23. | |
| Interventions | Before randomisation all participants were put on haloperidol for one month or until they were considered stable. 1. Drug: haloperidol. Fixed dose (dose before randomisation was maintained). Mean dose: n.i.. N = 11. 2. Placebo: duration of taper: 14 days. N = 12. Rescue medication: n.i., but probably not allowed. | |
| Outcomes | Examined Relapse: significant clinical design defined by either reoccurrence of symptoms or worsening of existing symptoms or prodromals signs such as sleep problems or anxiety. Leaving the study early. Service use: number of participants hospitalised. Death. Unable to use/Not included Mental state: BPRS (no data for each group/no predefined outcome of interest). Quality of life: Heinrich Scale (no data for each group). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, "participants and investigators were blind to treatment", no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, "participants and investigators were blind to treatment”, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, "participants and investigators were blind to treatment”, no further details. |
| Incomplete outcome data (attrition bias) | Unclear risk | 47% of the participants left the study early, most of them due to a relapse (55%). This attrition can be a source of bias for other outcomes than relapse. |
| Selective reporting (reporting bias) | High risk | Data on quality of life were not reported. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomly assigned according to pre‐established randomisation code. | |
| Participants | Diagnosis: chronic schizophrenia (Feighner’s criteria), treated with antipsychotic drugs for at least 2 years and currently under control. N = 32. | |
| Interventions | 1. Drug: haloperidol decanoate. Flexible dose. Allowed dose range: starting dose 1.5 mL (= 150 mg) four‐weekly, maximum 3 mL (= 300 mg) four‐weekly. Median dose 1.5 mL four‐weekly. N = 16. 2. Placebo: duration of taper: 0 days. N = 16. Rescue medication: antiparkinson medication, oral haloperidol, but this was considered to be a relapse. | |
| Outcomes | Examined Relapse: addition of oral haloperidol. Leaving the study early. Global state: number of participants improved. Unable to use/Not included Mental state: Brief Psychiatric Rating Scale (no SD/no predefined outcome of interest). Behaviour: NOSIE (no SD/no predefined outcome of interest). Adverse effects (no usable data). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned according to pre‐established randomisation code. |
| Allocation concealment (selection bias) | Low risk | Randomisation code was unknown to the evaluating investigators. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, administered by a particular nurse. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, administered by a particular nurse. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, administered by a particular nurse. |
| Incomplete outcome data (attrition bias) | Low risk | 12 out of 16 participants in the placebo group compared to 0 out of 16 in the haloperidol group were withdrawn from the trial due to inefficacy of treatment. As the only outcomes were relapse, number of participants improved and leaving the study early this should not have been a problem. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (Research Diagnostic Criteria), requiring neuroleptic maintenance treatment to prevent relapse. N = 43. | |
| Interventions | 1. Drug: haloperidol decanoate 60 mg/4 weeks. Fixed dose. N = 20. 2. Placebo: duration of taper: 0 days, but all on depot medication before study. N = 23. Rescue medication: anticholinergics and sedation. | |
| Outcomes | Examined Relapse: clinical judgement. Leaving the study early. Unable to use/Not included Mental state: Comprehensive Psychopathological Rating Scale (no mean, no SD/no prespecified outcome of interest). Adverse effects: extrapyramidal side‐effects, tardive dyskinesia (no mean, no SD/continuous side‐effect results were not among the prespecified outcomes). Physiological measures: laboratory (prolactin and haloperidol levels, no mean/SD/no prespecified outcomes of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, placebo injections, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, placebo injections, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, placebo injections, no further details. |
| Incomplete outcome data (attrition bias) | High risk | A considerable number of participants (42%) left the study early. The number was clearly higher in the placebo group and the reasons differed. Data were analysed on an ITT basis. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: computer‐generated random sequence (1:1 ratio). | |
| Participants | Diagnosis: Schizophrenia (DSM‐IV), not hospitalised ar the time of screening, then stabilised on iloperidone for at least 12 weeks before the relapse‐prevention phase. | |
| Interventions | 1. Drug: Iloperidone. N = 153 Flexible dose. Mean dose: 15 mg/day. Allowed dose range: 8 mg/day to 24 mg/day. 2. Placebo: duration of taper: n.i. N = 150. Rescue medication: anticholinergics (antiparkinson medication), lorazepam (agitation, severe restlessness, insomnia), zolpidem (insomnia). | |
| Outcomes | Examined Relapse (rating scale based and/or clinical judgement and/or need for hospitalisation or increase in the level of psychiatric care). Leaving the study early ‐ due to adverse events. Social functioning: Sheehan Disability Scale. Adverse effects Death Unable to use/Not included Leaving the study early ‐ due to any cause/inefficacy (no usable data, no crude numbers for relapse are available, subjects withdrawn due to early termination counted as dropouts). Global state‐ Number of participants improved (no usable data) Global state ‐ Number of participants in remission (no usable data, CGI‐I not reported). Mental state: PANSS change in total score, BPRS change in total score (no predefined outcomes of interest) | |
| Notes | Sponsored by Vanda Pharma. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random sequence. |
| Allocation concealment (selection bias) | Low risk | Centralised, interactive voice response system. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical appearing capsules |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical appearing capsules |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical appearing capsules |
| Incomplete outcome data (attrition bias) | High risk | The overall attrition rate (57%) was high, and more participants in the placebo group left the study early due to relapse. This difference may have biased the results of outcomes other than leaving the study early and relapse, which was assessed using the Kaplan‐Meier survival curve analysis. Data for secondary outcomes were analysed on an ITT basis (not full ITT, because only participants who received at least one dose of study medication were included) . |
| Selective reporting (reporting bias) | Unclear risk | Some secondary efficacy outcomes are reported incompletely so that they cannot be entered in the meta‐analysis (e.g. CGI‐I scores). |
| Other bias | High risk | Terminated early, but it was pre‐planned. |
| Study characteristics | ||
| Methods | Randomisation: computer‐generated randomisation scheme (1:1 ratio). | |
| Participants | Diagnosis: Schizophrenia (DSM‐IV‐TR), stabilised on study drug (after experiencing an acute exacerbation) for at least 12 weeks before randomisation. 87% paranoid type, 8% undifferentiated type, 4.9% disorganised type. | |
| Interventions | 1. Drug: Lurasidone. N = 144 Flexible dose. Mean dose: 78.9 mg/day. Allowed dose range: 40 mg/day to 80 mg/day. 2. Placebo: duration of taper: no taper. N = 141. Rescue medication: anticholinergics (antiparkinson), benzodiazepines (insomnia, anxiety/agitation ‐ with restrictions). Limited use of psychotropic medications (including antipsychotics other than lurasidone) immediately prior to study discontinuation was permitted. | |
| Outcomes | Examined Relapse (rating scale based and/or clinical judgement and/or need for hospitalisation or increase in the level of psychiatric care). Leaving the study early (any cause,adverse events, inefficacy). Service use ‐ Number of participants hospitalised. Participants´satisfaction with care: Health Economics Exit Questionnaire. Quality of life: EuroQol 5 Dimensions, Visual Analog Scale (EQ‐VAS). Social functioning: Specific Levels of Functioning, modified. Adverse effects. Death. Suicidal ideation and behaviour: Columbia Suicide Severity Rating Scale. Unable to use/Not included Global state: CGI‐S change scores (no usable data). Mental state: Positive and Negative Syndrome Scale total score and subscores (no predefined outcomes of interest). Depressive symptoms: Montgomery Asberg Depression Rating Scale (no predefined outcome of interest). Compliance to treatment: Brief Adherence Rating Scale (no predefined outcome of interest). Service use: Health Services Utilization Questionnaire (no usable data). Quality of life: Short Form‐12v2 Health Survey (SF‐12) (no usable data, available only for the Physical Component score, subscore of the scale. Chose the EuroQol data over these data) Smoking attitude (no predefined outcome of interest). | |
| Notes | Sponsored by Sunovion, Takeda. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random sequence generation, |
| Allocation concealment (selection bias) | Low risk | Interactive Voice/Web Response System. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identically‐matched placebo. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identically‐matched placebo. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identically‐matched placebo. |
| Incomplete outcome data (attrition bias) | Unclear risk | The overall attrition rate (54%) was high, substantially similar between the two groups. Only slightly more participants in the placebo group left the study early due to inefficacy/relapse. The primary efficacy outcome (relapse) was assessed using the Kaplan‐Meier survival curve analysis. Data for secondary outcomes were all analysed on an ITT basis (MMRM). |
| Selective reporting (reporting bias) | Unclear risk | Many secondary efficacy outcomes (but not the primary outcome) are reported incompletely so that they could not be entered in a meta‐analysis. |
| Other bias | Unclear risk | Following the end of the subject’s participation in the study, the PI or an authorized delegate had to report SAEs. |
| Study characteristics | ||
| Methods | Randomisation: randomly assigned (1:1), no further details. | |
| Participants | Diagnosis: schizophrenia (DSM‐IV), received clozapine for a minimum of 4 weeks before entering the study, had to undergo an elective discontinuation of clozapine (49% due to patient inconvenience, 37% due to adverse events, 13% due to partial response). N = 106. | |
| Interventions | 1. Drug: olanzapine. Fixed dose, 10 mg/day. N = 53. 2. Placebo: inert placebo. duration of taper 2 to 12 days. N = 53. Rescue medication: only benzodiazepines (for agitation) and anticholinergic (for evident EPS). Patients who relapsed could be removed from the double‐blind treatment and enter and optional open‐label cross‐over treatment (clozapine+olanzapine). | |
| Outcomes | Examined Relapse: worsening on at least one of the following COSTART events: schizophrenic reaction, hallucinations, delusions, thinking abnormal. Leaving the study early (any reason, inefficacy) Unable to use/Not included Global state: CGI‐S mean change (no usable data). Mental state: PANSS (no predefined outcome of interest). Depressive symptoms: Montgomery Asberg Depression Rating Scale (no predefined outcome of interest). Performance tests: MiniMental State Examination (no predefined outcome of interest). Adverse events: no usable data. Suicidality: no usable data. | |
| Notes | Not explicitly stated, probably sponsored (EliLilly) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned (1:1), no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | Low risk | The overall attrition rate of 10% was acceptable, but more participants in the placebo group than in the olanzapine group left the study early due to inefficacy. This may be a source of bias for outcomes other than relapse and leaving the study early, but data on such other outcomes are not available. Analyses were all done on an ITT basis. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Unclear risk | Very short follow‐up (3 to 5 days, difficult to discriminate between withdrawal symptoms and illness recurrence); 13% of the randomised patients had partial response to clozapine. |
| Study characteristics | ||
| Methods | Randomisation: randomised, 2:1 ratio, by an interactive voice response system. | |
| Participants | Diagnosis: schizophrenia (n = 266) or schizoaffective disorder (n = 60, DSM‐IV). BPRS total score < 36, positive symptoms at most mild, Global Assessment of Functioning at least 40, currently on maintenance antipsychotic medication. N = 326. | |
| Interventions | Participants were first converted to olanzapine and then stabilised for 8 weeks before randomisation. 1. Drug: olanzapine ‐ Fixed dose of either 10, 15 mg/day or 20 mg/day. Mean dose 13.4 mg/day. N = 224. 2. Placebo: duration of taper: 0 days. N = 102. Rescue medication: a one‐time increase of the same medication (olanzapine or placebo) was allowed. Furthermore, antiparkinson medication and benzodiazepines were allowed. | |
| Outcomes | Examined Relapse: any BPRS positive item > 4, absolute increase of a positive item or of the positive subscore, hospitalisation due to positive symptoms, suicide or suicide attempt. Leaving the study early. Adverse effects. Death, Suicide attempts. Violent/aggressive behaviour Quality of life: Heinrich Carpenter Quality of Life Scale (QLS). Service use ‐ number of participants hospitalised. Unable to use/Not included Mental state: PANSS (no prespecified outcome of interest). Adverse effects: adverse effects with an incidence < 10% (no data), laboratory, EPS‐scales (in part no data/no prespecified outcome of interest), EPS‐scales (no SD/continuous side‐effect results were not among the prespecified outcomes). Physiological measures: vital signs (no prespecified outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised, 2:1 ratio, by an interactive voice response system. |
| Allocation concealment (selection bias) | Low risk | Interactive voice response system. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | High risk | The overall attrition of 26% was acceptable, but many more participants in the placebo group than in the olanzapine group left the study early. Kaplan‐Meier survival analysis was used for the analysis of relapse, ANOVA based on LOCF was used for continuous outcomes. |
| Selective reporting (reporting bias) | High risk | Only those adverse events with a frequency of at least 10% were reported. Use of antiparkinson medication has not been reported. |
| Other bias | High risk | The study was terminated early when there was a sufficient difference, but this was preplanned. |
| Study characteristics | ||
| Methods | Randomisation: randomised, computerised randomisation and stratification scheme. | |
| Participants | Diagnosis: schizophrenia (DSM‐IV), 80% paranoid subtype, 14% undifferentiated subtype, initially with acute exacerbation, then 8 weeks run in and 6 weeks stabilisation phase. N = 207. | |
| Interventions | 1. Drug: paliperidone‐ Flexible doses. Allowed dose range: 3 mg/day to 15 mg/day Mean dose: 10.8 mg/day. N = 105. 2. Placebo: duration of taper: 0 days. N = 102. Rescue medication: benzodiazepines, antiparkinson medication, propanolol, antidepressants when the dose was stable for at least 3 months before the study. | |
| Outcomes | Examined Relapse: (a) psychiatric hospitalisation (involuntary or voluntary admission); b) increase in PANSS total score by 25% for 2 consecutive days for patients who scored more than 40 at randomisation or a 10‐point increase for patients who scored 40 or below at randomisation; c) increase in the Clinical Global Impression‐Severity (CGI‐S) score to at least 4, for patients who scored 3 or below at randomisation, or to at least 5, for patients whose CGI‐S scores were 4 at randomisation, for 2 consecutive days; d) deliberate self‐injury or aggressive behavior, or suicidal or homicidal ideation and aggressive behavior that was clinically significant; e) increase in prespecified individual PANSS item scores to at least 5, for patients whose scores were 3 or below at randomisation, or to at least 6, for patients whose scores were 4 at randomisation, for 2 consecutive days). Leaving the study early. Global state ‐ number of participants improved. Global state ‐ number of participants in remission (CGI‐based). Service use: number of participants hospitalised. Quality of life: Schizophrenia Quality‐of‐Life Scale (SQLS) Social functioning: Personal and Social Performance scale. Adverse effects. Violent/aggressive behaviour. Death; Suicide attempts. Unable to use/Not included Mental state: PANSS (no predefined outcome of interest). Physiological measures: laboratory (except for metabolic problems no data), vital signs, ECG, prolactin (all no data/no predefined outcomes of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised, computerised randomisation and stratification scheme. |
| Allocation concealment (selection bias) | Low risk | Interactive voice‐response system. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | High risk | Only 28 out of 207 participants left the study prematurely for another reason than relapse. Therefore, missing outcomes may not pose a problem for the primary outcome which was assessed with the Kaplan‐Meier method. Nevertheless, high discontinuations due to relapse (75/207) which were much more frequent in the placebo group than in the drug group pose a major problem for secondary outcomes. No full ITT (participants had to receive at least one dose post‐baseline) but only two participants were excluded on this basis. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | Study was terminated after an interim analysis showed a clear advantage of paliperidone. |
| Study characteristics | ||
| Methods | Randomisation: computer‐based randomisation (1:1 ratio). | |
| Participants | Diagnosis: schizophrenia (DSM‐IV‐TR), stabilised on paliperidone before double‐blind phase. | |
| Interventions | .1. Drug: Paliperidone ER N = 65 Fixed dose. Mean dose: 9.5 mg/day. Allowed dose range: 3 mg/day to 12 mg/day. 2. Placebo: duration of taper: n.i. N = 71. Rescue medication: benzodiazepines (anxiety, agitation), antiparkinson medication (anticholinergics). | |
| Outcomes | Examined Relapse (rating scale based and/or clinical judgement and/or need for hospitalisation or increase in the level of psychiatric care) Leaving the study early (any reason, adverse events, inefficacy). Global state ‐ number of participants in remission (CGI‐S defined). Service use ‐ number of patients hospitalised Social functioning: Personal and Social Performance scale. Adverse effects Death Suicidal ideation and behavior: Columbia Suicide Severity Rating Scale. Violent/aggressive behaviour Unable to use/Not included Global state ‐ number of participants improved (no usable data). Mental state: PANSS total score and subscores (no predefined outcomes of interest) Depressive symptoms: PANSS Marder Anxiety/Depression (no predefined outcome of interest). Subjective sleep measures: Sleep Visual Analog scale (no predefined outcome of interest) | |
| Notes | Sponsored by Janssen Research & Development, LLC. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐based randomisation. |
| Allocation concealment (selection bias) | Low risk | Interactive web/voice response system. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, matching placebo. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, matching placebo. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, matching placebo. |
| Incomplete outcome data (attrition bias) | High risk | The overall attrition rate of 67% was high, and more participants in the placebo group left the study early, mostly due to relapse. This difference may have biased the results of outcomes other than leaving the study early and relapse, which was assessed using the Kaplan‐Meier survival curve analysis. Data for secondary outcomes were analysed on an ITT basis. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | Terminated early after an interim analysis, but it was pre‐planned. |
| Study characteristics | ||
| Methods | Randomisation: patients were randomised in a 1 to 1 ratio (via a sponsor prepared, computer generated randomisation scheme, assigned by an interactive voice system). | |
| Participants | Diagnosis: schizophrenia (DSM‐IV‐TR). N = 410. | |
| Interventions | 1. Drug: paliperidone palmitate depot ‐ Fixed dose: originally 25 mg, 50 mg or 100 mg/4 weeks; this dose was maintained. Mean dose: n.i.. N = 206. 2. Placebo: duration of taper: 0 days. N = 204. Rescue medication: n.i.. | |
| Outcomes | Examined Relapse: psychiatric rehospitalisation, deliberate self‐injury or violent behaviour, suicidal or homicidal ideation, certain predefined PANSS score. Leaving the study early. Rehospitalisation. Global state ‐ number of participants in sustained remission (Andreasen criteria). Quality of life: Schizophrenia Quality of Life Scale (SQLS) Social functioning: Personal and Social Performance scale (PSP). Suicidal ideation and attempts. Violent/aggressive behaviour. Death. Adverse effects. Unable to use/Not included Mental state: PANSS (no predefined outcome of interest). Prolactin levels (no predefined outcome of interest). | |
| Notes | The study was stopped early after a significant interim analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Patients were randomised in a 1 to 1 ratio (via a sponsor prepared, computer‐generated randomisation scheme, assigned by an interactive voice system). |
| Allocation concealment (selection bias) | Low risk | Interactive voice system. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | High risk | Overall high dropout rate (45%). Clearly more participants in the placebo group (95) than in the drug group (31) left the study early due to relapse. This imbalance may have biased the results of other outcomes such as adverse events. Kaplan‐Meier survival curve analysis was used for the primary outcome relapse. |
| Selective reporting (reporting bias) | Low risk | Those adverse events that occurred in at least 2% of the participants and severe adverse events were presented. We feel that is acceptable. |
| Other bias | High risk | Study was stopped early after an interim analysis. |
| Study characteristics | ||
| Methods | Randomisation: sponsor‐prepared computer‐generated randomisation scheme (stratified by absence or presence of mood stabilisers or antidepressants and study centre). | |
| Participants | Diagnosis: schizoaffective disorder (Structured Clinical Interview for DSM‐IV Axis I Disorders). | |
| Interventions | 1. Drug: Paliperidone palmitate depot (1‐month formulation). N = 164 Fixed dose. Mean dose: 114.3 mg eq/month. Allowed dose range: 50 mg to 150 mg eq/month. 2. Placebo: duration of taper: depending on the long elimination half‐life of paliperidone depot. N = 170 Rescue medication: anticholinergics (antiparkinson medication); benzodiazepines not allowed within 8 hours prior to efficacy assessments, further antipsychotics or initiation of antidepressants or mood stabilizers were not allowed. | |
| Outcomes | Examined Relapse (rating scale based and/or clinical judgement and/or need for hospitalisation or increase in the level of psychiatric care) Leaving the study early (any reason, inefficacy, adverse events). Global state ‐ number of participants improved (CGI‐S‐SCA defined, as reported by the authors) Global state ‐ number of participants in sustained remission (at least 'mildly ill' at CGI‐S‐SCA evaluation). Patient´s satisfaction with care: Medication Satisfaction Questionnaire. Service use ‐ number of participants hospitalised: Resource Utilization Questionnaire Social functioning: Personal and Social Performance Scale. Number of participants employed Adverse effects (clinical judgement and rating scale based) Suicidal ideation: Columbia‐ Suicide Severity Rating Scale. Violent/aggressive behaviour Death Unable to use/Not included Mental state:PANSS total score and subscores (no predefined outcomes of interest). Affective symptoms: Hamilton Depression Rating Scale, Young Mania Rating Scale (no predefined outcomes of interest). | |
| Notes | Sponsored by Janssen Research & Development, LLC. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sponsor‐prepared computer‐generated stratified randomisation scheme |
| Allocation concealment (selection bias) | Low risk | Central, interactive voice/web response system. |
| Blinding of participants and personnel (performance bias) | Low risk | Double‐blind, matching placebo injections, administered by a person distinct from other study personnel |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, matching placebo injections, administered by a person distinct from other study personnel |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, matching placebo injections, administered by a person distinct from other study personnel |
| Incomplete outcome data (attrition bias) | High risk | The total attrition rate was high (51%), and differed substantially among study arms (drug arm: 39% versus placebo arm: 61%); almost double participants in the placebo group left the study early due to relapse. This may be a source of bias for outcomes other than dropouts and relapse, which was assessed using the Kaplan Mayer survival´s curve analysis. Data for secondary outcomes were analysed on an ITT basis (LOCF method). |
| Selective reporting (reporting bias) | Low risk | No clear evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for bias. |
| Study characteristics | ||
| Methods | Randomisation: sponsor‐prepared computer‐generated randomisation scheme, balanced using permuted blocks across the treatment groups and stratified by study centre to ensure balance of treatment allocation within a centre. | |
| Participants | Diagnosis: Schizophrenia (DSM‐IV‐TR), symptomatically stable when enrolled, then stabilised on paliperidone LAI for at least 12 weeks before randomisation. | |
| Interventions | 1. Drug: Paliperidone palmitate depot (3‐month formulation). N = 160 Fixed dose. Mean dose: 402 mg eq/3 months. Allowed dose range: 175 mg to 525 mg eq/3 months. 2. Placebo: duration of taper: depending on the elimination half‐life of paliperidone depot (between 84 and 139 days) N = 145. Rescue medication: anticholinergics (antiparkinson), beta‐blocker (akathisia), lorazepam (anxiety/agitation), zolpidem (sleep disturbances). | |
| Outcomes | Examined Relapse (rating scale based and/or clinical judgement and/or need for hospitalisation or increase in the level of psychiatric care) Leaving the study early (any reason, inefficacy, adverse events). Social functioning: Personal and Social Performance Scale. Adverse effects (clinical judgement and rating scale based). Violent/aggressive behaviour. Death. Suicide ideation: Columbia Suicide Severity Rating scale based. Unable to use/Not included Global state ‐ number of participants improved (no usable data). Global state ‐ number of participants in remission (no usable data, only available for a subgroup of patients in remission at baseline, reported as change in remitter status, PANSS defined). Mental state: PANSS total score and subscores (no predefined outcomes of interest). Depressive symptoms: PANSS Marder factors (no predefined outcome of interest). | |
| Notes | Sponsored by Janssen Research & Development, LLC. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sponsor‐prepared computer‐generated randomisation scheme, balanced using permuted blocks across the treatment groups and stratified by study centre to ensure balance of treatment allocation within a centre. |
| Allocation concealment (selection bias) | Low risk | Interactive voice/web response system. |
| Blinding of participants and personnel (performance bias) | Low risk | Double‐blind, identical appearing capsules, administered by a person distinct from other study personnel. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical appearing capsules, administered by a person distinct from other study personnel. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical appearing capsules, administered by a person distinct from other study personnel. |
| Incomplete outcome data (attrition bias) | High risk | The overall attrition rate of 30% could still be acceptable, though higher than 25%, but three times as many participants in the placebo group left the study early due to relapse. This difference may have biased the results of outcomes other than leaving the study early and relapse, which was assessed using the Kaplan‐Meier survival curve analysis. Data for secondary outcomes were analysed on an ITT basis. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. All the outcomes have been reported in the protocol‐specified way. |
| Other bias | High risk | Study terminated early after an interim analysis, but this was pre‐planned. |
| Study characteristics | ||
| Methods | Randomisation: matched pairs were formed and then randomised, no further details. | |
| Participants | Diagnosis: chronic psychotic hospitalised patients mainly with schizophrenic and paranoid behaviour patterns, suspected of relapsing after withdrawal of medication (clinical diagnosis). | |
| Interventions | 1. Drug: penfluridol once weekly ‐ Fixed dose, mean dose: n.i., range 10 mg to 40 mg/weekly. N = 13. 2. Placebo: duration of taper: 0 days. N = 13. Rescue medication: sedative neuroleptics allowed for 2 weeks, dexbenzitide. | |
| Outcomes | Examined Relapse: need of medication as decided by two psychiatrists. Leaving the study early Unable to use/Not included Global state ‐ number of participants improved (no usable data). Mental state: Psychiatric Evaluation Scale (no predefined outcome of interest). Adverse effects: movement disorders (Factor Construct Outcome Scale, no data for randomised phase/continuous side‐effect results were not among the prespecified outcomes of interest), neurologic effects (graphometric and tapping test, no data for randomised phase/no prespecified outcomes of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Matched pairs were formed and then randomised, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, indistinguishable placebo. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, indistinguishable placebo. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, indistinguishable placebo. |
| Incomplete outcome data (attrition bias) | Low risk | Apart from those participants who relapsed, no participant left the study early and relapse was the only outcome. |
| Selective reporting (reporting bias) | High risk | Adverse events were not reported for the double‐blind phase. |
| Other bias | Low risk | No obvious other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: severely ill, chronically hospitalised people with schizophrenia (clinical diagnosis). N = 50. | |
| Interventions | 1. Drug: penfluridol once weekly. Fixed dose. Allowed dose range: 40 mg to 160 mg/week. Mean dose: n.i.. N = 25. 2. Placebo: duration of taper: 0 days. N = 25. Rescue medication: antiparkinson medication. | |
| Outcomes | Examined Relapse: worsening of global state. Leaving the study early. Global state: number of participants improved (CGI based). Adverse effects: extrapyramidal side effects. Unable to use/Not included Mental state: BPRS (no mean, no SD/no prespecified outcome of interest). Behaviour: NOSIE (no mean, no SD/no prespecified outcome of interest). Physiological measures: laboratory, ECG, photosensitivity tests, ophthalmologic examinations, vital signs (no clear data/no prespecified outcomes of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | High risk | It is not entirely clear, whether there were dropouts in addition to 18 participants (7 drug, 11 placebo, 36%) who left the study early due to relapse. However, the 36% dropout rate can be a problem for other outcomes. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: divided into two comparable groups by an unbiased statistician. | |
| Participants | Diagnosis: chronic psychotic inpatients (clinical diagnosis), 13 schizophrenia, 1 dementia, 1 paranoia. N = 15. | |
| Interventions | 1. Drug: penfluridol. Fixed/flexible dose: unclear, but different doses according to pretrial medication. Allowed dose range: unclear, but all participants received 40 mg/week. Mean dose: 40 mg/week. N = 7. 2. Placebo: duration of taper: 0 days. N = 8. Rescue medication: | |
| Outcomes | Examined Relapse: need of additional antipsychotic medication. Leaving the study early. Unable to use/Not included Mental state: Zwanikken Scale (no mean, no SD / no predefined outcome of interest). Behaviour: Zwanikken Scale (no mean, no SD / no predefined outcome of interest). Adverse effects: interview (no data). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Divided into two comparable groups by an unbiased statistician. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not explained. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. |
| Incomplete outcome data (attrition bias) | Low risk | No participant left the study early. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomised, no further details. | |
| Participants | Diagnosis: chronic schizophrenia (DSM‐II), catatonic type (n = 2), residual type (n = 15), hebephrenic type (n = 1), simple type (n = 2), paranoid type (n = 1). N = 21. | |
| Interventions | 1. Drug: penfluridol. Fixed dose, mean 43 mg/week. N = 10. 2. Placebo: duration of taper: 0 days. N = 11. Rescue medication: antiparkinson medication, haloperidol, but this was considered to be a sign of relapse. | |
| Outcomes | Examined Relapse: use of additional haloperidol. Leaving the study early. Unable to use/Not included Mental state: Zwanikken scale (no data/no predefined outcome of interest). Adverse effects: Zwanikken scale (no data / continuous side‐effect results were not among the predefined outcomes of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. |
| Incomplete outcome data (attrition bias) | Low risk | No participant left the study prematurely. |
| Selective reporting (reporting bias) | High risk | Data on side effects and the mental state were not reported. |
| Other bias | Low risk | No evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis). N = 35. | |
| Interventions | 1. Drug: penfluridol ‐ Flexible dose. Allowed dose range: 20 mg to 120 mg/week. Mean dose:n.i.. N = 18. 2. Placebo: duration of taper: 0 days. N = 17. Rescue medication: antiparkinson medication, it seems that haloperidol was not allowed in the double‐blind phase. | |
| Outcomes | Examined Relapse: psychiatric decompensation that could not be controlled by dose increase. Leaving the study early. Adverse effects (at least one movement disorder). Unable to use/Not included Global state: Clinical Global Impression Scale (no usable data for remission). Mental state: BPRS (no numbers/no predefined outcomes of interest). Behaviour: NNOSIE (no numbers/no predefined outcomes of interest). Physiological measures: vital signs (weight, pulse, blood pressure, respiratory frequency, temperature ‐ no numbers/no predefined outcomes of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. |
| Incomplete outcome data (attrition bias) | High risk | 12 of 35 participants left the study early (34%), 11 of them were in the placebo group. As all participants in the placebo group discontinued due to relapse, the primary outcome is not affected. But the results of all other outcomes are biased by this effect. |
| Selective reporting (reporting bias) | Low risk | Results on rating scales have not been reported, but these were not outcomes of interest in our review. |
| Other bias | Low risk | No clear other bias |
| Study characteristics | ||
| Methods | Randomisation: n.i., but double‐blind study. | |
| Participants | Diagnosis: chronic schizophrenia (DSM‐III), all on maintenance medication for control of continuous symptoms, all stable for at least 6 months. N = 30. | |
| Interventions | 1. Drug: penfluridol. Fixed dose of 55 mg/week. N = 15. 2. Placebo: duration of taper: 0 days. N = 15. Rescue medication: antiparkinson medication and haloperidol, but this was considered to be a relapse. | |
| Outcomes | Examined Relapse (need of additional haloperidol medication). Leaving the study early. Unable to use/Not included Mental state (Scale for the Assessment of Positive Symptoms and Negative Symptoms ‐ no data /no predefined outcome of interest). Adverse effects: extrapyramidal side‐effects (Simpson Angus Scale (SAS) ‐ no data / continuous side‐effect results were not among the prespecified outcomes). Physiological measures: mean body weight, pulse rate, blood pressure, laboratory (all no data/no prespecified outcomes of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | N.i., but double‐blind study. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double, identical capsules. |
| Incomplete outcome data (attrition bias) | Low risk | Only study completers were used in the final analysis, but as there were only two dropouts (one in each group) this was not necessarily a problem. |
| Selective reporting (reporting bias) | Low risk | Rating scale results were not reported, but these were not of interest for the review. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: arbitrarily allocated. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis by at least two psychiatrists), all with paranoid condition, two additionally catatonic tendencies and one hebephrenic features, six were leucotomised. N = 26. | |
| Interventions | 1. Drug: perphenazine liquid. Fixed dose (same dose as before the start of the study) two 12 mg three times, one 20 mg three times, all other 8mg three times and most less. Mean dose: see above. N = 13. 2. Placebo. duration of taper: 0 days. N = 13. 3. No medication*. duration of taper: 0 days. N = 13. Rescue medication: not allowed apart from antiparkinson medication. | |
| Outcomes | Examined Relapse: "major relapse" = replaced on active medication. Violent/aggressive behaviour. Unable to use/Not included Mental state: self‐developed psychiatric rating scale ‐ unpublished scale (no predefined outcome of interest). Behaviour: Fergus Falls Behaviour Rating Scale (no predefined outcome of interest). | |
| Notes | *This group was not used for the review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Arbitrarily allocated. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Low risk | Double‐blind ‐ only the pharmacist knew which bottles were active. Participants were asked whether they were aware of the medication, but only one realised a change in taste. Nurses were also asked, but did not guess the correct medication better than by chance alone. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind ‐ only the pharmacist knew which bottles were active. Participants were asked whether they were aware of the medication, but only one realised a change in taste. Nurses were also asked, but did not guess the correct medication better than by chance alone. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind ‐ only the pharmacist knew which bottles were active. Participants were asked whether they were aware of the medication, but only one realised a change in taste. Nurses were also asked, but did not guess the correct medication better than by chance alone. |
| Incomplete outcome data (attrition bias) | Unclear risk | Dropouts were not reported. It is not clear, whether there really no dropouts. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomised, no further details. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis), receiving maintenance treatment. | |
| Interventions | 1. Drug: Pimozide. N = 10 Flexible dose. Mean dose: 40 mg/day. 2. Placebo: duration of taper: abrupt withdrawal. N = 10. Rescue medication: n.i. | |
| Outcomes | Examined Leaving the study early. Global state ‐ number of participants improved (CGI‐I defined). Global state ‐ number of participants in remission (CGI‐S defined). Adverse events. Unable to use/Not included Mental state: BPRS (no predefined outcome of interest) Behavior: NOSIE (no predefined outcome of interest). | |
| Notes | Sponsored by McNeil Laboratories. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | Low risk | Only study completers were used in the final analysis, but as there was only one dropout (in the drug arm, before receiving the first dose of medication) this was not necessarily a problem. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | The pimozide doses (40 mg/day) were very high for current standards. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: residual schizophrenia (DSM‐II), chronic, currently treated with antipsychotic drugs. N = 40. | |
| Interventions | 1. Drug: pimozide. Flexible dose. Allowed dose range: n.i.. Mean dose: n.i.. N = 20. 2. Placebo: duration of taper: 0 days. N = 20. Rescue medication: not allowed, only dose increase of pimozide or placebo‐pimozide was possible. Additional use of haloperidol meant relapse. | |
| Outcomes | Examined Relapse: need of additional haloperidol) Leaving the study early. Adverse effects: number of participants with at least one movement disorder, rigor and tremor. Death. Violent/aggressive behaviour. Unable to use/Not included Mental state: Overall Factor Construct Scale (no mean, no SD/no prespecified outcome of interest) Behaviour: ‘Psychiatric Evaluation Scale’ (no mean, no SD/no prespecified outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. |
| Incomplete outcome data (attrition bias) | Low risk | 2 (5%) of the participants left the study early which is an acceptable rate. Both participants were included in the endpoint analysis. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (DSM‐IV), duration ill at least 2 years, Positive and Negative Syndrome Scale total score < 60 before randomised phase, Clinical Global Impression Severity Scale not more than moderately ill. N = 197. | |
| Interventions | 1. Drug: quetiapine XR. Flexible dose 400 mg to 800 mg/day. Mean dose: 669 mg/day. N = 94. 2. Placebo: duration of taper: 4 days.N = 103. Rescue medication: anticholinergic medication, sleep medication, lorazepam, no additional antipsychotic drugs. | |
| Outcomes | Examined Relapse: increase of PANSS by at least 30 percent from baseline, Clinical Global Impression Scale much or very much worse, need for additional antipsychotic medication. Leaving the study early. Global state: number of participants in symptomatic remission (Andreasen criteria). Global state: number of participants in sustained remission (Andreasen criteria, maintained for at least 6 months). Adverse events: open interviews. Death. Extrapyramidal side‐effects: use of antiparkinson medication, Barnes Akathisia Scale, SAS, Aquired Involuntary Movements Scale. Unable to use/Not included Global state: number of participants improved (no usable data). Service use ‐ number of participants hospitalised (unclearly reported). Mental state: PANSS/no predefined outcome of interest. Laboratory: haematology, chemistry, glucose, Hba1c, insulin, lipids, urine analysis, thyroid function), ECG, vital signs, mean weight gain (all no predefined outcomes of interest). Compliance (pill count/no predefined outcome of interest). | |
| Notes | No participant terminated the preplanned study duration of one year. The authors reported that data after 6 months are not reliable because only a few patients were left. Therefore, relapse data after 6 months were not extracted. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Correct randomisation assumed, because recent study from industry. |
| Allocation concealment (selection bias) | Low risk | Correct allocation concealment assumed, because recent study from industry. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. |
| Incomplete outcome data (attrition bias) | High risk | Overall drop‐out rate was 41%, most of them due to relapse (76%), which occurred much more frequently in the placebo group. This difference in attrition may have biased the results of other outcomes than relapse. Kaplan‐Meier survival curve analysis was used for the primary outcome relapse. |
| Selective reporting (reporting bias) | High risk | Only adverse events with a frequency of at least 5% were reported. |
| Other bias | High risk | The study was terminated early after an interim analysis showed a clear superiority of quetiapine; there were certain baseline discrepancies in terms of mean age, duration ill and number of previous episodes. |
| Study characteristics | ||
| Methods | Randomisation: randomised (1:1:1 ratio) to bifeprunox, quetiapine or placebo, no further detail. | |
| Participants | Diagnosis: Schizophrenia (DSM‐IV‐TR), in the maintenance phase (no acute exacerbation and medication unchanged for at least 4 weeks). | |
| Interventions | 1. Drug: Quetiapine. N = 76 Fixed dose. Mean dose: 600 mg/day. 2. Placebo: duration of taper: 21 days, N = 68. Rescue medication: n.i. | |
| Outcomes | Examined Quality of life: Schizophrenia Quality of Life (S‐QoL) scale. Social functioning: Personal and Social Performance scale. Death Unable to use/Not included Relapse (no usable data) Leaving the study early (no usable data, available only for the whole study duration) Global state ‐ number of participants in remission/improved: CGI‐S, CGI‐I (no usable data) Mental state: PANSS total score and subscores (no predefined outcomes of interest) Depressive symptoms: Calgary Depression Scale for Schizophrenia (no predefined outcome of interest) Service use ‐ number of participants hospitalised (no usable data) Social functioning: Global Assessment of Functioning (PSP data used) Adverse effects (no usable data) | |
| Notes | Sponsored by Lundbeck. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only stated randomised, no further detail. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, encapsulated tablets. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, encapsulated tablets. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, encapsulated tablets. |
| Incomplete outcome data (attrition bias) | Unclear risk | Global and per‐arm attrition rate are not reported for the randomised placebo‐controlled period, but only for the total duration of the study. Efficacy and safety were assessed on a ITT base. |
| Selective reporting (reporting bias) | Unclear risk | Relapse was not a pre‐specified outcome. several efficacy outcomes cited as assessed but not reported throughout the text. |
| Other bias | High risk | Terminated early for negative efficacy results after a pooled interim analysis. |
| Study characteristics | ||
| Methods | Randomisation: randomised (1:1:1 ratio) to bifeprunox, quetiapine or placebo, no further detail. | |
| Participants | Diagnosis: Schizophrenia (DSM‐IV‐TR), in the maintenance phase (no acute exacerbation and medication unchanged for at least 4 weeks). | |
| Interventions | 1. Drug: Quetiapine. N = 116. Fixed dose. Mean dose: 600 mg/day. 2. Placebo: Duration of taper: 21 days, N = 119. Rescue medication: n.i. | |
| Outcomes | Examined Quality of life: Schizophrenia Quality of Life (S‐QoL) scale. Social functioning: Personal and Social Performance scale. Death Unable to use/Not included Relapse (no usable data) Leaving the study early (no usable data, available only for the whole study duration) Global state ‐ number of participants in remission/improved: CGI‐S, CGI‐I (no usable data, available data on "at least much improved") Mental state: PANSS total score and subscores (no predefined outcomes of interest) Depressive symptoms: Calgary Depression Scale for Schizophrenia (no predefined outcome of interest) Service use ‐ number of participants hospitalised (no usable data) Social functioning: Global Assessment of Functioning (PSP data used) Adverse effects (no usable data) Suicide attempts (no usable data). | |
| Notes | Sponsored by Lundbeck. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Only stated randomised, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, encapsulated tablets. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, encapsulated tablets. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, encapsulated tablets. |
| Incomplete outcome data (attrition bias) | Unclear risk | Global and per‐arm attrition rate are not reported for the randomised placebo‐controlled period, but only for the total duration of the study. Efficacy and safety were assessed on an ITT base. |
| Selective reporting (reporting bias) | Unclear risk | Relapse was not a pre‐specified outcome. several efficacy outcomes cited as assessed but not reported throughout the text. |
| Other bias | High risk | Terminated early for negative outcome data after a pooled interim analysis. 8 patients in the quetiapine arm and 11 patients in the placebo arm either continued taking or started concomitant new antipsychotic treatment during the study. |
| Study characteristics | ||
| Methods | Randomisation: sequence by computer, fixed block size of four without stratification. | |
| Participants | Diagnosis: schizophrenia and related psychoses (DSM‐IV), all first episode, all well remitted, all had remained well on maintenance medication for 1 year. N = 178. | |
| Interventions | 1. Drug: quetiapine. Fixed dose of 400 mg/day. N = 89. 2. Placebo: duration of taper (days): 35. N = 89. Rescue medication: antipsychotics not allowed. | |
| Outcomes | Examined Relapse: (i) an increase in at least one of the following PANSS psychotic symptom items to a threshold score (delusion, hallucinatory behaviour, conceptual disorganisation, unusual thought content, suspiciousness; (ii) Clinical Global Impression Severity of Illness 3 or above and (iii) CGI change 5 or above). Leaving the study early. Rehospitalisation. Suicide attempts. Adverse effects: akathisia, tardive dyskinesia, tremor, sedation, weight gain. Open employment status. | |
| Notes | Supported by investigator initiated trial award from AstraZeneca. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence by computer, fixed block size of four without stratification. |
| Allocation concealment (selection bias) | Low risk | AstraZeneca prepared individually numbered sets of study drugs, packed them according to the randomisation sequence and then shipped them to the study team in numbered but apparently identical capsules. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Identical capsules, "investigators, patients and all research staff were blind to the study drugs and the block size". |
| Blinding (performance bias and detection bias) | Unclear risk | Identical capsules, "investigators, patients and all research staff were blind to the study drugs and the block size". |
| Blinding (performance bias and detection bias) | Low risk | Identical capsules, "investigators, patients and all research staff were blind to the study drugs and the block size". |
| Incomplete outcome data (attrition bias) | High risk | 72% of the participants left the study early. As most participants dropped out after relapse this outcome was not affected, but it is a source of bias for other outcomes. Survival analysis for the primary outcome relapse. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomised, no further details. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis), hospitalised for at least 2 years. Gender: n.i.. | |
| Interventions | 1. Drug: high‐dose trifluoperazine. Fixed dose of 80 mg/day (reached within 35 days). N = 117. 2. Drug: low‐dose trifluoperazine. Fixed dose of 15 mg/day. N = 113. 3. Placebo: duration of taper: 0 days. N = 111. Rescue medication: not indicated, but probably not allowed. | |
| Outcomes | Examined Relapse: worsening of global state. Leaving the study early. Global state: number of participants improved. Service use; number of participants discharged. Adverse effects: clinical interview based on 40 items checklist. Unable to use/Not included Mental state: Inpatient Multidimensional Psychiatric Scale, BPRS (both only P values/no predefined outcome of interest). Behaviour: NOSIE (only P values/no predefined outcome of interest). Ophthalmologic examination (no predefined outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. Whether blinding was successful was not assessed, although in one group high doses associated with a lot of side effects were administered. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind identical capsules. Whether blinding was successful was not assessed, although in one group high doses associated with a lot of side effects were administered. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. Whether blinding was successful was not assessed, although in one group high doses associated with a lot of side effects were administered. |
| Incomplete outcome data (attrition bias) | High risk | The overall attrition was considerable (33%) and clearly more participants discontinued the study early in the placebo group (53%) than in the two drug groups (23%), mainly due to inefficacy, which can be a problem for other outcomes than relapse. Not all participants were included in the final analysis. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | The high‐dose group used too high doses (80 mg/day) for current standards, even the low‐dose would nowadays be considered to be quite high (15 mg/day). |
| Study characteristics | ||
| Methods | Randomisation: randomised, no further details. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis), >70% of them with extrapyramidal side effects after long treatment with phenothiazines. N = 63. | |
| Interventions | 1. Drug: trifluoperazine ‐ Fixed dose (maintaining the initial dose, necessity of dose increase was considered to be a relapse). Mean dose: 17 mg/day. N = 31. 2. Placebo: duration of taper: 0 days. N = 32. Rescue medication: n.i.. | |
| Outcomes | Examined Relapse: deterioration of participant’s condition to such a degree that additional antipsychotic medication was necessary. Leaving the study early. Death. Unable to use/Not included Adverse effects: movement disorders (no randomised data). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Low risk | Capsules dispensed by the hospital pharmacist who was the only person who knew what the capsules were and to whom they were given. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, placebo capsules, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, placebo capsules, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, placebo capsules, no further details. |
| Incomplete outcome data (attrition bias) | Low risk | 16% left the study early, all but one due to relapse. This appears acceptable. relapse and death were the only outcomes. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | Participants with a relapse were probably removed from the study and the blind broken. Study was probably terminated early. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: chronic psychotic patients (mainly schizophrenia, clinical diagnosis). N = 144. | |
| Interventions | 1. Drug: continuation of antipsychotic taken before the study ‐ Fixed/flexible dose: unclear. Allowed dose range: unclear. Mean dose: n.i.. N = 46. 2. Placebo: duration of taper: "4 weeks to five months, usually 2 months”. N = 98. Rescue medication: n.i.. | |
| Outcomes | Examined Relapse: clinical diagnosis. Unable to use/Not included Social adjustment: (not reported for the randomised participants). Rehospitalisation (unclear numbers). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, unidentifiable capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, unidentifiable capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, unidentifiable capsules. |
| Incomplete outcome data (attrition bias) | Unclear risk | Whether participants left the study early is unclear. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | In case of relapse the blind was broken. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (clinical diagnosis), all withdrawn of subject to periodic disturbances, all needed supervision or management. N = 80. | |
| Interventions | 1. Drug: chlorpromazine; flexible dose; allowed dose range 200 mg/day to 1000 mg/day; mean dose: 894 mg/day (here mean maximum dose); N = 20 2. Drug: trifluoperazine; flexible dose; allowed dose range 10 to 50 mg/day; mean dose: 29 mg/day (here mean maximum dose); N=20 3. Drug: thioridazine; flexible dose; allowed dose range 200 mg/day to 1000 mg/day; mean dose: 958 mg/day (here mean maximum dose); N = 20 4. Placebo: duration of taper: 0 days; N = 20 Rescue medication: phenobarbital and bentropine methansulfonate, no additional antipsychotic drugs | |
| Outcomes | Examined Relapse: worsening of global state Leaving the study early. Global state ‐ number of participants improved (clinical judgement, categories comparable to CGI). Adverse effects: clinical interview, number of participants receiving antiparkinson medication Unable to use/Not included Behaviour: Manifest Behaviour Scale (no SD/no predefined outcome of interest) Personality traits: Minnesota Multiphasic Personality Inventory (MMPI) (no SD/no predefined outcome of interest) | |
| Notes | The results of all drug groups were pooled. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details |
| Allocation concealment (selection bias) | Low risk | Only the hospital pharmacist had the code on what medication the patient was on |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules, each participant had his own container. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules, each participant had his own container. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules, each participant had his own container. |
| Incomplete outcome data (attrition bias) | Low risk | Only 3 out of 80 participants left the study early and the reasons were well described. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
| Other bias | Low risk | No evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomly selected and then assigned. | |
| Participants | Diagnosis: chronically mentally ill, 67% to 83% schizophrenia (clinical diagnosis), in hospital and apparently treated with antipsychotic drugs for the last 18 months. N = 60. | |
| Interventions | 1. Drug: chlorpromazine or thioridazine. Fixed/flexible dose: n.i.. Allowed dose range: n.i.. Mean dose: n.i.. N = 30. 2. Placebo: duration of taper: 0 days. N = 30. Rescue medication: not indicated. | |
| Outcomes | Examined Relapse: attrition because of behavioural upset. Unable to use/Not included Behaviour: various scales (no data reported/no predefined outcome of interest). | |
| Notes | There were several study phases (alternation between drug and placebo). Only the first phase was of interest for the review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly selected and then assigned. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Identical pink capsules. Nurses, raters and patients were blind to the procedure. Treating physician was led to believe that half of the patients were on placebo, the other half on drug. |
| Blinding (performance bias and detection bias) | Unclear risk | Identical pink capsules. Nurses, raters and patients were blind to the procedure. Treating physician was led to believe that half of the patients were on placebo, the other half on drug. |
| Blinding (performance bias and detection bias) | Low risk | Identical pink capsules. Nurses, raters and patients were blind to the procedure. Treating physician was led to believe that half of the patients were on placebo, the other half on drug. |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear how many participants left the study during the first month. |
| Selective reporting (reporting bias) | High risk | Data on behaviour scales were not reported, including aggressive behaviour which was an outcome in our review. |
| Other bias | Low risk | No evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomised, no further details. | |
| Participants | Diagnosis: schizophrenia without positive symptoms (clinical diagnosis). N = 43. | |
| Interventions | 1. Drug: various phenothiazines, mainly chlorpromazine. Fixed/flexible dose: flexible. Allowed dose range: not limited, but complete discontinuation was not allowed. Mean dose: 150 mg/day to 200 mg/day chlorpromazine. N = 24. 2. Placebo: duration of taper: 0 days. N = 19. Rescue medication: not allowed. | |
| Outcomes | Examined Relapse: clinical judgement. Service use: number of participants rehospitalised. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Low risk | Psychiatrist without contact to the participants held the key and filled the medication containers. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, exact placebo replicas. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, exact placebo replicas. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, exact placebo replicas. |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear ‐ whether participants discontinued the study prematurely was not reported. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | Some placebo participants continued to take medication, study terminated early. |
| Study characteristics | ||
| Methods | Randomisation: randomised, no further details. | |
| Participants | Diagnosis: schizophrenia (clinical diagnosis), one third paranoid subtype, without central nervous system disease, without lobotomy. N = 259. | |
| Interventions | 1. Drug: chlorpromazine or thioridazine.* Fixed dose, continuation of the dose given in the stabilisation phase. Mean dose: chlorpromazine mean 400 mg/day, thioridazine mean 350 mg/day. N = 88. 2. Placebo: duration of taper: 1 ‐ 8 days. N = 171. Rescue medication: not indicated. | |
| Outcomes | Examined Relapse: definitive worsening of the condition and medication again necessary, usually joint decision of treatment team. Unable to use/Not included Mental state: Inpatient Multidimensional Psychiatric Scale (IMPS) (no prespecified outcome of interest). Behaviour: Psychotic Reaction Profile Scale (no prespecified outcome of interest). | |
| Notes | * There was another group which received half the original dose. It was not considered in this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | High risk | Double‐blind, identical tablets. However, placebo dose reduction group received medication only every other day. Therefore, blinding was not fully maintained. |
| Blinding (performance bias and detection bias) | High risk | Double,‐blind identical tablets. However, placebo dose reduction group received medication only every other day. Therefore, blinding was not fully maintained. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical tablets. However, placebo dose reduction group received medication only every other day. Therefore, blinding was not fully maintained. |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether there were dropouts or whether the authors analysed only study completers. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Unclear risk | 22 participants who had relapsed in the first 8 weeks were entered in the study again. As the number is small, it is unclear whether they affected the results. |
| Study characteristics | ||
| Methods | Randomisation: randomly assigned. | |
| Participants | Diagnosis: chronic psychotic patients, treatment resistive in closed wards. No seizures, no antidepressants, no candidates for discharge. N = 88. | |
| Interventions | 1. Drug: trifluoperazine (10 mg/day to 90 mg/day), chlorprothixene (50 mg/day to 450 mg/day), same medication (various drugs). Flexible doses. Allowed dose range: n.i.. Mean dose: n.i.. N = 54. | |
| Outcomes | Examined Relapse: clinical judgement. Leaving the study early. Adverse effects. Unable to use/Not included Ward behaviour: unpublished rating scale (no predefined outcome of interest). Urinary excretion (no predefined outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, different colours. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, different colours. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, different colours. |
| Incomplete outcome data (attrition bias) | Low risk | Dropouts 10 out of 88 is acceptable (11%), although only completers were analysed. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: matched in three groups according to age and hospitalisation, then randomised using a table of random numbers. | |
| Participants | Diagnosis: schizophrenia (clinical diagnosis), undifferentiated type (N = 10), hebephrenic (N = 6), catatonic (5), paranoid (5), acute undifferentiated (N = 1). N = 27. | |
| Interventions | 1. Drug: remained on previous antipsychotic medication (chlorpromazine, thioridazine, trifluoperazine, perphenazine, prochlorperazine). Fixed/flexible dose: not clear, but probably fixed. Allowed dose range: n.i.. Mean dose: n.i., because it is unclear which patients were allocated to which group. N = 9. 2. Placebo: duration of taper: 7 days. N = 9**. Rescue medication: tranquilliser (= benzodiazepine). | |
| Outcomes | Examined Relapse: worsening by three points on the factor scores of the Inpatient Multidimensional Psychiatric Scale (IMPS) or withdrawn due to being worse. Leaving the study early. Global state: improvement by three points on the factor scores of the IMPS or withdrawn due to being ready for discharge. Service use: number of participants discharged. Unable to use/Not included Mental state: IMPS (no data/no prespecified outcome of interest). Behaviour: Psychotic Reaction Profile (no data / no prespecified outcome of interest). | |
| Notes | ** a second placebo group that was referred to a specialised ward was not used in our calculations (N = 9). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Matched in three groups according to age and hospitalisation, then randomised using a table of random numbers. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | High risk | There was a considerable number of participants leaving the study early (28%). The approach how missing data were handled is not specified. |
| Selective reporting (reporting bias) | Low risk | Only two factors of the IMPS were presented, but this was no outcome of interest. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (clinical diagnosis), paranoid schizophrenia (N = 19), undifferentiated schizophrenia (N = 8), catatonic schizophrenia (N = 8), hebephrenic schizophrenia (N = 4), acute schizophrenic reaction (N = 1). N = 40. | |
| Interventions | 1. Drug: chlorpromazine (N = 6) or thioridazine (N = 14). Flexible dose. Allowed dose range: 100 mg/day to 600 mg/day. Mean dose: n.i.. N = 20. 2. Placebo: duration of taper (days): 0 days. N = 20. Rescue medication: n.i.. | |
| Outcomes | Examined Relapse: symptoms similar to those which had characterized the patient’s illness prior to successful treatment by phenothiazines. Unable to use/Not included Withdrawal symptoms (no numbers for each group separately/no predefined outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, "the staff, patients and investigators were not aware of which patients were to receive placebo instead of their medication”. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, "the staff, patients and investigators were not aware of which patients were to receive placebo instead of their medication”. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, "the staff, patients and investigators were not aware of which patients were to receive placebo instead of their medication”. |
| Incomplete outcome data (attrition bias) | Unclear risk | It was not reported whether participants left the study early, but it is well possible that there were not any, because it was a relatively short inpatient study. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis by two psychiatrists). N = 40. | |
| Interventions | 1. Drug: chlorpromazine or trifluoperazine. Fixed/flexible dose: n.i.. Allowed dose range: n.i.. Mean dose: n.i.. N = 20. 2. Placebo: duration of taper: 0 days. N = 20. Rescue medication: n.i.. | |
| Outcomes | Examined Relapse: worsening of global state. Global state: number of participants improved. Adverse effects. Unable to use/Not included Mental state: Wing Scale (no SD/no predefined outcome of interest). Behaviour: Wing Scale (no SD/no predefined outcome of interest). Leaving the study early (no data). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Low risk | The hospital pharmacist was responsible for supplying placebo and active drugs to the ward, no one concerned with the care of patients knew which patients were started on placebo. |
| Blinding of participants and personnel (performance bias) | High risk | Double‐blind, identical tablets, but in most cases nurses made correct forecasts on who was on drug and who was on placebo. |
| Blinding (performance bias and detection bias) | High risk | Double‐blind, identical tablets, but in most cases nurses made correct forecasts on who was on drug and who was on placebo. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical tablets, but in most cases nurses made correct forecasts on who was on drug and who was on placebo. |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether there were dropouts. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | Blinding was broken when a participant relapsed. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (Present State Examination (PSE)), recently recovered from an acute episode, 32 florid schizophrenia, 3 delusional psychosis. N = 35. | |
| Interventions | 1. Drug: trifluoperazine or chlorpromazine (depending on the previous medication so that so far as the patient was concerned there was no apparent change in medication). Flexible dose. Allowed dose range: trifluoperazine 5 mg/day to 25 mg/day, chlorpromazine 100 mg/day to 500 mg/day. Mean dose: chlorpromazine 157.1 mg/day, trifluoperazine 12.3 mg/day. N = 20. 2. Placebo: duration of taper: not indicated, probably 0 days. N = 15. Rescue medication: antiparkinson medication, antidepressants, no antipsychotics (doctors received a letter asking them not to prescribe other medication). | |
| Outcomes | Examined Relapse: physician was sufficiently concerned about the patient’s status to want to be certain that he was on active drug. Leaving the study early. Service use: number of participants hospitalised. Adverse effects. Death. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Low risk | Trial medication was held by the unit secretary and dispensed to Julian Leff who gave it to the treating consultant. Only the unit secretary knew which pills were active drug and which were placebo. |
| Blinding of participants and personnel (performance bias) | Low risk | Double‐blind, no further details. But side‐effects were not troublesome in any patient and therefore doctors concerned probably received no clues about whether a patient was on active drug or not. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. But side‐effects were not troublesome in any patient and therefore doctors concerned probably received no clues about whether a patient was on active drug or not. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. But side‐effects were not troublesome in any patient and therefore doctors concerned probably received no clues about whether a patient was on active drug or not. |
| Incomplete outcome data (attrition bias) | High risk | Overall dropout rate was 60%, almost all due to relapse which occurred much more frequently in the placebo group. This poses a problem for other outcomes than relapse. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear other bias. |
| Study characteristics | ||
| Methods | Randomisation: randomised, no further details. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis) with positive or negative symptoms, responsive to treatment with antipsychotic drugs, all so ill that they required continuous treatment with antipsychotic medication for at least 3 months. N = 61. | |
| Interventions | 1. Drug: pimozide ‐ Flexible dose. Allowed dose range: 2 mg/day to 12 mg/day. Mean dose: 6.3 mg/day. N = 21. 2. Drug: trifluoperazine. Flexible dose. Allowed dose range: 5 mg/day to 30 mg/day. Mean dose: 17.5 mg/day. N = 20. 3. Placebo: duration of taper: 21 days. N = 20. Rescue medication: chloralhydrate, antiparkinson medication. | |
| Outcomes | Examined Relapse: at least minimally worse on CGI. Leaving the study early. Global state: number of participants improved (CGI defined). Unable to use/Not included Mental state: BPRS (no predefined outcome of interest). Global state: number of participants in remission (no usable data). Social activity: Family Rating Form (no SD/no predefined outcome of interest). Social adjustment: Harbor View House Residents Rating Report (no SD/no predefined outcome of interest). Adverse effects: open interview (no data). Physiological measures: vital signs, laboratory (both no data/no predefined outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. |
| Incomplete outcome data (attrition bias) | High risk | The overall number of participants leaving the study early (41%) was considerable, with a higher dropout rate in the placebo group. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, in blocks of eight, stratified for age, duration ill and time since last admission. | |
| Participants | Diagnosis: chronic schizophrenia (clinical diagnosis), 22 undifferentiated, 7 paranoid, 1 schizoaffective, no severe other psychiatric or somatic illnesses, no severely ill participants. N = 40. | |
| Interventions | 1. Drug: pimozide.* Flexible dose. Allowed dose range: 2 mg/day to 20 mg/day. Mean dose: 5.3 mg/day. N = 15. 2. Drug: thioridazine.* Flexible dose. Allowed dose range: 75 mg/day to 750 mg/day. Mean dose: 189 mg/day. N = 15. 3. Placebo: duration of taper: 0 days. N = 10. Rescue medication: antiparkinson medication, bedside sedation. | |
| Outcomes | Examined Relapse (worsening of global state). Leaving the study early. Global state: number of participants improved (CGI based). Global state ‐ number of participants in remission (CGI based) Adverse effects: binary outcomes ‐ open interview. Unable to use/Not included Mental state: BPRS (no SD/no prespecified outcome of interest). Functioning: Katz Lyerly Scale of Social Adjustment, Patient Rating Form, Family Rating Form (no data available ) Physiological measures: biological parameters (temperature, mean weight, pulse, blood pressure, all no data/all no prespecified outcomes of interest), laboratory (blood count, urine analysis, liver enzymes, blood sugar, protein bound iodine, all no prespecified outcomes of interest). | |
| Notes | * The results of pimozide and thioridazine were combined in the analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random, in blocks of eight, stratified for age, duration ill and time since last admission. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules, each participant had an individual stock bottle. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules, each participant had an individual stock bottle. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules, each participant had an individual stock bottle. |
| Incomplete outcome data (attrition bias) | High risk | Overall 36% left the study early. The specific reasons why the participants dropped out were not indicated by group. |
| Selective reporting (reporting bias) | Low risk | No clear source for selective reporting. |
| Other bias | Low risk | No clear other sources of bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (clinical diagnosis). N = 45. | |
| Interventions | 1. Drug: prochlorpromazine, perphenazine, chlorpromazine, promazine or trifluoperazine. Fixed doses continued with the same drug and dose taken before the study. Mean dose: n.i. N = 30. 2. Placebo: duration of taper: 0 days. N = 15*. Rescue medication: not allowed. | |
| Outcomes | Examined Relapse (need of medication or deterioration of state or transfer to closed ward) Leaving the study early. Global state ‐ number of participants improved Service use ‐ number of participants hospitalised/discharged. Unable to use/Not included Behaviour: Patient Adjustment Report (no prespecified outcome of interest). Mental state: Taylor Manifest Anxiety Scale (no prespecified outcome of interest). | |
| Notes | * Another 15 participants were treated only for 8 weeks with placebo and then switched back to their initial antipsychotic drug. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | High risk | Double‐blind, thiamine chloride used as placebo, participants and nurses were told that a new medication was given, but nurses soon knew that this was a placebo. |
| Blinding (performance bias and detection bias) | High risk | Double‐blind, thiamine chloride used as placebo, participants and nurses were told that a new medication was given, but nurses soon knew that this was a placebo. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, thiamine chloride used as placebo, participants and nurses were told that a new medication was given, but nurses soon knew that this was a placebo. |
| Incomplete outcome data (attrition bias) | Low risk | Only completers were included in the statistical analysis, but because the drop‐out rate was only 13% we did not consider this a source of bias. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear other risk of bias. |
| Study characteristics | ||
| Methods | Randomisation: randomly in group of 15 each, no further details. | |
| Participants | Diagnosis: schizophrenia (mainly Schneiderian first‐rank symptoms), last relapse 30 to 60 months ago, fully remitted since and maintained on antipsychotic drugs. N = 30. | |
| Interventions | 1. Drug: switched to various antipsychotic drugs with similar profile as the previous one. Fixed/flexible dose: probably flexible. Allowed dose range: n.i.. Mean dose: n.i.. N = 15. 2. Placebo: benzodiazepine (‘active placebo’). Duration of taper 0 days. N = 15. Rescue medication: n.i.. | |
| Outcomes | Examined Relapse: recurrence of symptoms definitely of schizophrenic type, or symptoms not diagnostic of schizophrenia (e.g. sleep problems) which could not be controlled with other measures than antipsychotic drugs or ECT. Leaving the study early. Quality of life: subjective distress (Symptom Questionnaire of Kellner and Sheffield, SQKS). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly in group of 15 each, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | High risk | 12 participants left the study early (40%), among those 10 from the placebo group and 8 for relapse. Outcomes other than relapse and leaving early are clearly prone to bias due to this difference in leaving the study early. |
| Selective reporting (reporting bias) | Low risk | Use of benzodiazepines was not indicated, but this was not an outcome of interest in our review. |
| Other bias | Low risk | No evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (according to Bleuler’s concept, with at least three primary symptoms ‐ e.g. autism, disturbance of affects, association and volition ‐ and at least two secondary symptoms ‐ hallucinations, persecution‐), duration ill at least 2 years. N = 41. | |
| Interventions | 1. Drug: fluphenazine depot (most around 12.5 mg to 25 mg/3 weeks, mean 21.42 mg/3 weeks) or flupenthixol depot (most around 20 mg to 40 mg/3 weeks, mean 27.5/3 weeks) ‐ Fixed dose. N = 24. 2. Placebo: duration of taper: 0 days. N = 17. Rescue medication: chloral hydrate, antiparkinson medication, additional antipsychotic drugs were not allowed. | |
| Outcomes | Examined Relapse: psychotic behaviour or increase in six subscales of the Comprehensive Psychopathological Rating Scale. Leaving the study early. Service use: number of participants hospitalised. Adverse effects. Unable to use/Not included Mental state: Comprehensive Psychopathological Rating Scale (no SD/no predefined outcome of interest). Behaviour: NOSIE (no SD/no predefined outcome of interest). Physiological measures: various laboratory tests (no data/no predefined outcome of interest). Life events (Life Event Scale/no predefined outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, placebo sesame oil. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, placebo sesame oil. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, placebo sesame oil. |
| Incomplete outcome data (attrition bias) | Low risk | Overall, 3 (7%) out of 41 participants left the study early. Although only completers were analysed, due to the low rate this is not a problem. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No obvious risk for other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (clinical diagnosis) in remission. N = 30. | |
| Interventions | 1. Drug: chlorpromazine. Fixed dose of 75 mg/day. N = 10. 2. Drug: haloperidol. Fixed dose of 3 mg/day. N = 10. 3. Placebo: duration of taper (days): 0 days. N = 10. Rescue medication: only nitrazepam for sleep and biperiden for extrapyramidal side‐effects, no additional antipsychotic drugs. | |
| Outcomes | Examined Relapse: clinical judgement. Leaving the study early (due to adverse events). Global state ‐ number of participants in sustained remission (study defined). Unable to use/Not included Number of symptom‐free days (no SD’s/no predefined outcome of interest). | |
| Notes | There were also a diazepam and an imipramine group which were not of interest for the current review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, drug appearance was made identical with respect to taste, colour and volume by adding a kind of "stomatics”. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, drug appearance was made identical with respect to taste, colour and volume by adding a kind of "stomatics”. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, drug appearance was made identical with respect to taste, colour and volume by adding a kind of "stomatics”. |
| Incomplete outcome data (attrition bias) | Low risk | No participant left the study early due to other reasons than relapse in the first phase of the study, the only outcome apart from leaving the study early. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | The doses used were very low for Western standards. The study was initially planned as a cross‐over trial, but due to high dropout rates after the first phase only the first treatment phase was analysed. Nevertheless, this did not interfere with the aims of our review. |
| Study characteristics | ||
| Methods | Randomisation: randomised, 3:1 ratio. | |
| Participants | Diagnosis: chronic psychotic outpatients (DSM‐III), schizophrenia (N = 26), mental retardation with psychosis (N = 9), organic brain syndrome (N = 1). N = 36. | |
| Interventions | 1. Drug: various antipsychotic drugs. Fixed dose: keeping the dose of the antipsychotic the participant was on at the beginning of the study. Mean dose: 365 mg/day chlorpromazine equivalents. N = 9. 2. Placebo: duration of taper: 28 days. N = 27. Rescue medication: n.i.. | |
| Outcomes | Examined Relapse: major clinical deterioration. Leaving the study early. Death. Unable to use/Not included Global state: Clinical Global Impression (CGI) (no data for each group separately/no prespecified outcome of interest). Mental state:BPRS, Profile of Mood Symptoms (PRS) (no data for each group separately/no prespecified outcome of interest). Adverse effects: extrapyramidal side‐effects (Abnormal Involuntary Movement Scale (AIMS), Dyskinesia Rating Scale, no data for each group separately/continuous side‐effect results were not among the prespecified outcomes), other adverse effects (Treatment Emergent Symptoms Scale, no data for each group separately/continuous side‐effect results were not among the prespecified outcomes). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised, 3:1 ratio (information obtained from author). |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, ‘matching placebos’ and sesame oil for fluphenazine decanoate treated participants. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, ‘matching placebos’ and sesame oil for fluphenazine decanoate treated participants. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, ‘matching placebos’ and sesame oil for fluphenazine decanoate treated participants. |
| Incomplete outcome data (attrition bias) | Low risk | The differential dropout rate (placebo group 8/27, 0/9 maintenance group, all due to relapse) can have biased other outcomes than relapse and leaving the study early. But data on such other outcomes were not available anyway. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (DSM‐III), in remission or residual state. N = 87. | |
| Interventions | 1. Drug: haloperidol combined with biperidine and nitrazepam. Fixed dose: 1 mg, 3 mg or 6 mg/day.* N = 37. 2. Drug: propericiazine combined with biperidine and nitrazepam. Fixed dose: 10, 30 mg/day or 60 mg/day.* N = 37. 3. Placebo combined with biperidine and nitrazepam. Duration of taper: 0 days. N = 13. Rescue medication: not indicated, probably no additional antipsychotic medication allowed. | |
| Outcomes | Examined Relapse: clinical judgement. Leaving the study early. Global state ‐ number of participants in sustained remission (study defined). Unable to use/Not included Prolactin levels (no predefined outcome of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, drug appearance was made identical with respect to powder, colour, taste and volume by adding a gastric acid. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, drug appearance was made identical with respect to powder, colour, taste and volume by adding a gastric acid. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, drug appearance was made identical with respect to powder, colour, taste and volume by adding a gastric acid. |
| Incomplete outcome data (attrition bias) | Unclear risk | While in the placebo group and in the haloperidol group the rates of participants leaving early due to other reasons were low, 9 out of 12 participants in the propericiazine group discontinued due to overdose. It is questionable whether relapse rates could be accurately measured, because most participants did not reach the endpoint. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: first episode of schizophrenia (Present State Examination). N = 120. | |
| Interventions | 1. Drug: flupenthixol IM, chlorpromazine, haloperidol, pimozide, trifluoperazine Flexible dose. Allowed dose range: no upper limit, but lower limit was flupenthixol IM 40 mg/month, chlorpromazine 200 mg/day, haloperidol 3 mg/day, pimozide 4 mg/day, trifluoperazine 5 mg/day. Mean dose: flupenthixol 84 mg/month (N = 31), chlorpromazine 366 mg/day (N = 3), haloperidol 11.8 mg/day (N = 3), pimozide 7.8 mg/day (N = 5), trifluoperazine 11.5 mg/day (N = 12). N=54. 2. Placebo: duration of taper (days): 30 days on drug, then received half dose for 30 days before they were put on placebo. N = 66. Rescue medication: antiparkinson medication, antidepressants, anxiolytics. | |
| Outcomes | Examined Relapse: rehospitalisation or rehospitalisation thought necessary although not possible or need of medication. Leaving the study early. Unable to use/Not included Hallucinations, delusions (no data/no predefined outcomes of interest). Global state: clinical judgment of patients global state at endpoint (not usable data/no predefined outcome of interest) Death, Suicide attempts (no usable data, only reported for the total sample). Disturbed behaviour/non‐cooperation (no usable data, only reported for the total sample). Use of antiparkinson medication (unclearly reported, probably referred to the baseline intake). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Allocation lists prepared by pharmacy for five antipsychotic drugs mentioned below, concealment is unclear. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | Low risk | No clear bias. overall rate of leaving early of 11% is acceptable. Survival curve analysis was used for the primary outcome relapse. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | Blind was broken when a participant relapsed. |
| Study characteristics | ||
| Methods | Randomisation: random, no further details. | |
| Participants | Diagnosis: schizophrenia (Schedule for Affective Disorder and Schizophrenia, and Research Diagnostic Criteria), all had previously responded to antipsychotic drugs. N = 100. | |
| Interventions | 1. Drug: various antipsychotic drugs. Fixed/flexible dose: probably flexible. Allowed dose range: n.i.. Mean dose: n.i.. N = 36. 2. Placebo: duration of taper 0 days. N = 64. Rescue medication: n.i.. | |
| Outcomes | Examined Relapse: first signs of symptoms according to ward staff and project nurse, full deterioration was not waited for. Unable to use/Not included Performance tests: Rohrschach test, Wechsler Adult Intelligence Scale (all no clear mean’s, n´s, no SD’s / no predefined outcomes of interest). Mental state: BPRS (no clear mean, no number of participants, no SD/no predefined outcome of interest). Thought disorder: Thought Disorder Index, PRS (all no clear mean’s, no SDs/no predefined outcomes of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, no further details. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not explained. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double, placebo matching in kind and dose the previous medication. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, placebo matching in kind and dose the previous medication. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, placebo matching in kind and dose the previous medication. |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear, because these have not been indicated. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Unclear risk | Unclear, baseline data have not been presented for both groups separately. |
| Study characteristics | ||
| Methods | Randomisation: assumed, because study was double‐blind and because the first study phase was randomised (no further details). | |
| Participants | Diagnosis: first episode schizophrenia (Present State Examination, Feighner criteria and Research Diagnostic Criteria). N = 15. | |
| Interventions | 1. Drug: pimozide once weekly or IM flupenthixol. Flexible doses. Allowed dose range: n.i.. Mean dose: n.i.. N = 8. | |
| Outcomes | Examined Relapse: re‐admission. Rehospitalisation. Unable to use/Not included Leaving the study early (no data). Global state ‐ number of participants in remission (no data for withdrawal study). Social adjustment (no data for withdrawal study). Cognition (no data for withdrawal study / no predefined outcome of interest). Adverse effects: parkinsonism, tardive dyskinesia (no data for withdrawal study). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation assumed. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | Unclear risk | It is unclear whether there were missing data. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Unclear risk | Not entirely clear. |
| Study characteristics | ||
| Methods | Randomisation: centrally randomised by a specialised unit using an "adaptive randomisation method”. | |
| Participants | Diagnosis: schizophrenia or schizoaffective disorder (ICD‐9 and Research Diagnostic Criteria). N = 237. | |
| Interventions | 1. Drug: various antipsychotic drugs. Flexible dose, minimum 100 mg/day chlorpromazine equivalent. Allowed dose range: 100 mg ‐ unlimited chlorpromazine equivalents/day. Mean dose: 201 mg/day. N = 122. 2. No treatment (= crisis management, medication was only given in case of a full relapse). Duration of taper: 50% every two weeks, thus after 6 weeks only 12.5% of initial dose left, thus 42 days. Note that participants were not withdrawn after they had received crisis intervention. N = 115. Rescue medication: in the no treatment group additional antipsychotic medication could only be given in case of relapse. | |
| Outcomes | Examined Relapse: BPRS total score ‐ >10 increase, GAS < 20 reduction, deterioration Clinical Global Impression Scale CGI >7. Leaving the study early. Service use: number of participants hospitalised. Unable to use/Not included Global state: CGI (no usable data ). Mental state: BPRS, AMDP system, Paranoid Depression Scale (all no means, no SDs / no predefined outcome of interest). Functioning: Strauss and Carpenter scale, another scale validated by the study group (no usable data) Subjective well‐being (own scale ‐ no mean, no SD/no predefined outcome of interest). Adverse effects: extrapyramidal side‐effects (AIMS ‐ no SD, SAS, Dosage Record and Treatment Emergent Symptoms Scale ‐ all no means, no SDs/continuous side‐effect results were not among the predefined outcomes of interest). Concept of illness (concept of illness scale ‐ no mean, no SD). Compliance: doctors’ assessment (no predefined outcome of interest). Physiological measures: routine laboratory, ECG, EEG (no data/no predefined outcome of interest). | |
| Notes | There was a third group using intermittent treatment which was not of interest for this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Centrally randomised by a specialised unit using an "adaptive randomisation method”. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | High risk | Open, only key rating scales were additionally rated by a second blind assessor. |
| Blinding (performance bias and detection bias) | Unclear risk | Open, only key rating scales were additionally rated by a second blind assessor. |
| Blinding (performance bias and detection bias) | Low risk | Open, only key rating scales were additionally rated by a second blind assessor. |
| Incomplete outcome data (attrition bias) | High risk | High two‐year discontinuation rate of 43.7%. Analysis was ITT based on Kaplan‐Meier survival curve analysis, completer analyses were presented in addition if different. A risk of bias can not be excluded given the high discontinuation rate. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | Low risk | No clear evidence for other bias. |
| Study characteristics | ||
| Methods | Randomisation: an independent rater created randomisation lists stratified for gender with randomly permuted blocks of 4 allocation groups. Allocation: procedure not described. | |
| Participants | Diagnosis: first episode schizophrenia (DSM‐IV). N = 20. | |
| Interventions | 1. Drug: olanzapine, risperidone, quetiapine, zuclopenthixol. Flexible doses. Mean dose: n.i. N = 9. 2. No treatment: duration of taper: 6 to 12 weeks. N = 11. Rescue medication: not indicated. | |
| Outcomes | Examined Relapse: scale defined or need of hospitalisation for any psychiatric indication. Leaving the study early. Rehospitalisation. | |
| Notes | Sponsor: The Netherlands Organisation for Health Research and Development and EliLilly. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent rater created randomisation lists stratified for gender with randomly permuted blocks of 4 allocation groups. |
| Allocation concealment (selection bias) | Unclear risk | Procedure not described. |
| Blinding of participants and personnel (performance bias) | High risk | Open study. |
| Blinding (performance bias and detection bias) | High risk | Open study. |
| Blinding (performance bias and detection bias) | Low risk | Open study. |
| Incomplete outcome data (attrition bias) | Low risk | 5 out of 20 participants left the study early (25%). Probably an acceptable rate, there was no big difference between drug and placebo group. Kaplan‐Meier survival curves were used for the primary outcome relapse. |
| Selective reporting (reporting bias) | Low risk | No evidence for selective reporting. |
| Other bias | High risk | Premature termination after interim analysis. |
| Study characteristics | ||
| Methods | Randomisation: random, computer‐generated randomisation code. | |
| Participants | Diagnosis: chronic, stable schizophrenia (DSM‐III‐R), less than markedly ill on Clinical Global Impression Scale. 56% of the participants had predominantly negative symptoms at baseline. N = 278 (originally 294 were randomised, but 16 were then excluded from all the analyses due to protocol deviations in one centre). | |
| Interventions | 1. Drug: ziprasidone ‐ Fixed doses of 40 mg/day, 80 mg/day or 160 mg/day.** N = 207 (originally 219 randomised). 2. Placebo: duration of taper < 3 days. N = 71 (originally 75 randomised). Rescue medication: anticholinergics, lorazepam, temazepam, no additional antipsychotic medication. | |
| Outcomes | Examined Relapse: (CGI of much worse or more, PANSS items hostility or uncooperativeness > 6, or in need for additional treatment for exacerbation of symptoms). Leaving the study early. Social functioning: Global Assessment of Functioning scale. Adverse events Violent/aggressive behaviour. Death. Suicidal ideation. Unable to use/Not included Mental state: PANSS total score and subscores (no predefined outcome of interest). Global state: Clinical Global Impression Severity Scale (no usable data for remission). Service use ‐ number of participants hospitalised (no usable data, unclearly reported). Subjective well‐being: own scale (no usable data). Concept of illness: Concept of illness scale (no predefined outcome of interest). Adverse effects: extrapyramidal symptoms (SAS, BAS, AIMS ‐ all no SD/continuous side‐effect results were not among the prespecified outcomes of interest). Physiological measures: ECG, vital signs, weight, ophthalmological assessment, lab tests (all no SD, no data/not prespecified outcomes of interest). | |
| Notes | ** The results of the three dose groups were pooled. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised, computer‐generated randomised code. |
| Allocation concealment (selection bias) | Low risk | Drug treatment cards numbered for each participant entering the double‐blind phase; investigator and pharmacist allocated numbers to participants in strict sequence of entry into the study. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, identical capsules. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, identical capsules. |
| Incomplete outcome data (attrition bias) | High risk | 64% of the participants left the study early, most due to relapse. The rate was higher in the placebo group (86%) than in the medication group (~57%). This was probably not a problem for the primary outcome relapse, but for secondary outcomes for which the LOCF method was used. Appropriate survival curve analysis was used for the primary outcome relapse. |
| Selective reporting (reporting bias) | Low risk | No selective reporting. |
| Other bias | Low risk | No obvious other bias. |
| Study characteristics | ||
| Methods | Randomisation: computer‐generated randomisation list. | |
| Participants | Diagnosis: chronic schizophrenia (DSM‐III‐R), at least mildly ill according to CGI, had a history of recurrence in last 18 months, currently maintained on antipsychotic medication. N = 121. | |
| Interventions | 1. Drug: zotepine. Fixed dose of 300 mg/day which could be reduced once to 150 mg/day. Mean dose: n.i.. N = 63. 2. Placebo:duration of taper: 0 days. N = 58. Rescue medication: antipsychotic drugs not allowed, but benzodiazepines. | |
| Outcomes | Examined Relapse: (i) a moderate clinical deterioration from baseline (an increase in CGI severity score of at least 2 points plus an increase of 2 points in at least two positive symptom items on the BPRS persisting for two assessments over 3 days, but not requiring hospitalisation; (ii) deterioration requiring hospitalisation accompanied, on one assessment, by an increase in CGI severity score of at least 2 points plus an increase of 2 points in at least two positive symptom items on the BPRS; and (iii) severe clinical deterioration (an increase in CGI severity score to ‘severely ill’ for 24 hours, or, if in hospital, requiring special observation for suicidal or aggressive behaviour). Leaving the study early. Global state: number of participants improved (CGI based). Global state: number of participants in remission (CGI based). Adverse effects: binary outcomes ‐ open interview. Suicide ideation Unable to use/Not included Mental state: BPRS, SANS (no prespecified outcomes of interest). Adverse effects: extrapyramidal side‐effects (SAS, AIMS, no SD/continuous side‐effect results were not among the prespecified outcomes). Physiological measures: laboratory, vital signs, ECG (all no data/no prespecified outcomes of interest). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list. |
| Allocation concealment (selection bias) | Low risk | Allocation to treatment was on a double‐blind basis, codes were not broken until the time of analysis. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Unclear risk | Double‐blind, no further details. |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind, no further details. |
| Incomplete outcome data (attrition bias) | High risk | The overall rate of participants leaving the study early was very high (76%) and many more participants in the placebo group than in the drug group dropped out due to relapse. Kaplan‐Meier survival analysis was used for primary outcome relapse. No full ITT analysis, only those participants with at least one post‐baseline assessment were included, but only two participants were excluded on this basis. |
| Selective reporting (reporting bias) | High risk | Only those adverse events that were reported on at least four occasions and serious adverse events were reported. |
| Other bias | Low risk | No clear other bias. |
General abbreviations
CNS: central nervous system
CPZ: chlorpromazine
DSM: Diagnostic and Statistical Manual of Mental Disorders
ECG: electrocardiography
ECT: electroconvulsive therapy
EASY: Early Assessment Service for Young People with Psychosis
EEG: electroencephalography
EPS: extrapyramidal symptoms
HbA1c: glycated haemoglobin
ICD: International Statistical Classification of Diseases and Related Health Problems
IM: intramuscular injection
ITT: intention to treat
LAI: long‐acting injectable
LOCF: last observation carried forward
n.i.: not indicated
SD: standard deviation
Rating scales
AIMS: Abnormal Involuntary Movement Scale
AMDP: Arbeitsgemeinschaft für Methodik und Dokumentation in der Psychiatrie
BAS: Barnes Akathisia Scale
BPRS: Brief Psychiatric Rating Scale
CGI: Clinical Global Impression ‐S: severity, ‐I: improvement
GAS: Global Assessment Scale
IMPS: Inpatient Multidimensional Psychiatric Rating Scale
MMPI: Minnesota Multiphasic Personality Inventory
NOSIE: Nurses Observation Scale for Inpatient Evaluation
PANSS: Positive And Negative Syndrome Scale
PRP: Psychotic Reaction Profile
PRS: Psychiatric Rating Scale
PSE: Present State Examination
RDC: Research Diagnostic Criteria
SADS: Schedule for Affective Disorders
SANS: Scale for the Assessment of Negative Symptoms
SAS: Simpson‐Angus Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Allocation: controlled clinical trial, not randomised. | |
| Allocation: randomised. Participants: not stabilised on antipsychotic drugs. | |
| Allocation: randomised. Participants: including only those at clinical high risk for psychosis (CHR). | |
| Allocation: randomised. Participants: clinically stable for at least 4 weeks, treated with risperidone monotherapy at an optimal dose. Intervention: risperidone (baseline dose), risperidone (gradual dose reduction by 50%), no placebo arm. | |
| Allocation: randomised. Participants: not stabilised on antipsychotic drugs. | |
| Allocation: not randomised, matched groups. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: mild‐to‐moderate schizophrenia, unclear clinical stability. Intervention: BI 409306 (inhibitor of phosphodiesterase 9A), not currently approved for schizophrenia, versus placebo. | |
| Allocation: cluster randomised. Participants: first episode of non‐affective psychosis, Intervention: community care compared to NAVIGATE program, which included individual resilience therapy, family education, supported employment and personalised medication management. The specific effect of maintenance therapy with antipsychotic treatment cannot be assumed from this design. | |
| Allocation: randomised. Participants: first episode schizophrenia, stabilised on antipsychotic medication. Intervention: risperidone versus olanzapine versus aripiprazole; participants failing the initially‐assigned antipsychotic were switched to one of the other two. No real placebo or discontinuation arm. | |
| Allocation: randomised,no hint for real maintenance study design. Participants: first episode schizophrenia; inclusion criteria allow acute patients. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: not clinically stable. | |
| Allocation: randomised. Participants: schizophrenia. Intervention: thiothixene alone versus thiothixene plus group therapy versus chlorpromazine alone versus chlorpromazine plus group therapy. | |
| Allocation: randomised. Participants: not stabilised on antipsychotic drugs (discontinued medication for at least 6 months before study entry). | |
| Allocation: not randomised. | |
| Allocation: not randomised. | |
| Allocation: not randomised. | |
| Allocation: not randomised. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: schizophrenia. Intervention: all participants were on neuroleptics and antiparkinson medication at baseline. They were then randomised to neuroleptics plus continuation of antiparkinson medication versus neuroleptics alone. | |
| Allocation: randomised. Participants: acute exacerbation of schizophrenia. | |
| Allocation: randomised. Participants: outpatients with chronic schizophrenia not truly stabilised on antipsychotic drugs. | |
| Allocation: randomised. Participants: schizophrenia, receiving maintenance treatment, stabilised on study drug for at least 8 weeks. Intervention: aripiprazole LAI (400 mg/4 weeks), aripiprazole oral (10 mg/day to 30 mg/day), aripiprazole LAI suboptimal dose (50 mg/4 weeks), no real placebo arm. | |
| Allocation: randomised. Participants: first episode of psychosis, not stable on antipsychotic medication. | |
| Allocation: randomised. Participants: discontinued antipsychotic medication for some weeks, then kept in the study only if showing signs of psychotic exacerbation. | |
| Allocation: randomised. Participants: unclear baseline clinical status and unclear whether they were stabilised on antipsychotic medication. Intervention: I. butaperazine, trifluoperazine, inert placebo; II. trifluperidol, trifluoperazine, phenobarbital. Outcome: no predefined outcome of interest. | |
| Allocation: randomised (no further details). Participants: schizophrenia or schizoaffective disorder, stabilised on the same depot medication for 1 year. Intervention: fluphenazine decanoate, placebo (cross‐over design). Outcome: no usable data for relevant outcomes (data up to the point of first cross‐over are not available). | |
| Allocation: randomised. Participants: schizophrenia or schizoaffective disorder, clinically stable and with stabilised maintenance antipsychotic therapy. Intervention: fluphenazine decanoate, placebo; cross‐over design. Outcome: no usable data (data up to the point of first cross‐over are not available). | |
| Allocation: randomised. Participants: first‐episode psychosis. Intervention: treatment as usual (including antipsychotics) versus multimodal relapse prevention therapy (including antipsychotics and cognitive behavioral therapy/family intervention). | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: schizophrenia. Interventions: chlorpromazine versus placebo. Outcomes: no usable outcomes. | |
| Allocation: randomised. Participants: patients with chronic schizophrenia. Intervention: abrupt versus gradual withdrawal of chlorpromazine, but chlorpromazine was withdrawn from both groups. Thus not appropriate control group. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: schizophrenia, clinically stable for at least 6 months, no florid psychotic symptoms. Intervention: fluphenazine decanoate, placebo. Outcome: no usable data for relevant outcomes. | |
| Allocation: randomised (no further details). Participants: schizophrenia (DSM‐III‐R), clinically stable and receiving maintenance treatment. Intervention: fluphenazine depot, placebo. Outcome: no usable data for relevant outcomes (not presented for the randomised subset). | |
| Allocation: not randomised. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: 50% not diagnosed as with schizophrenia. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: schizophrenia with relevant negative symptoms, unclear clinical stability. Intervention: MIN‐101 (roluperidone), not currently approved, versus placebo. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: participants were acutely ill, not stable. | |
| Allocation: randomised. Participants: not stable, not all on antipsychotics before the study. | |
| Allocation: randomised. Participants: schizophrenia‐related psychotic disorders, under remitted states. Intervention: maintenance therapy with antipsychotics versus guided dose reduction; no real discontinuation or placebo arm. | |
| Allocation: randomised. Participants: participants were not stable, most not on antipsychotics before the study. | |
| Allocation: randomised. Participants: schizophrenia, on maintenance phenotiazine medication Intervention: pimozide, placebo; cross‐over design. Outcome: no usable data for relevant outcomes. | |
| Allocation: randomised. Participants: not clinically stable. | |
| Allocation: randomised. Participants: chronic schizophrenia, stabilised on antipsychotic treatment for at least 6 months before study entry. Intervention: chlorpromazine, placebo; cross‐over design. Outcome: no usable data for relevant outcomes (data up to the point of first cross‐over are not available). | |
| Allocation: randomised. Participants: schizophrenia, not adequately stable. | |
| Allocation: randomised. Participants: men with schizophrenia. Intervention: chlorpromazine versus placebo. Outcome: no usable outcome. | |
| Allocation: not randomised. | |
| Allocation: some of the participants were matched, not randomised. | |
| Allocation: randomised. Participants: schizophrenia spectrum disorders, currently on antipsychotic medication. Intervention: maintenance treatment with antipsychotics versus dose reduction programme; no real discontinuation or placebo arm. | |
| Allocation: randomised. Participants: outpatients diagnosed with schizophrenia, in remission at baseline. Intervention: timiperone, sulpiride, placebo. The placebo arm was only retrospective, derived from data from previous studies. | |
| Allocation: randomised. Participants: first episode of psychosis, not clinically stable. | |
| Allocation: randomised. Participants: 152 state hospital patients with schizophrenia (severely impaired at time of enrollment), 29 ambulatory schizophrenia patients (not acutely ill but recruited only if severe enough to warrant hospitalisation). | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: schizophrenia. Intervention: chlorpromazine versus chlorpromazine plus propranolol. | |
| Allocation: not randomised. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: chronic schizophrenia. Intervention: chlorpromazine, placebo, orphenadrine. Outcome: no relevant outcome, only auditory attention task. | |
| Allocation: randomised. Participants: chronic schizophrenia, unclear clinical status, 30% uncovered Intervention: antipsychotic therapy + family psychoeducational intervention, antipsychotic treatment alone, control group (in which quote: "medication was not encouraged nor discouraged"). | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: chronic schizophrenia. Intervention: fluphenazine elixir plus placebo injection versus fluphenazine enanthate injection plus oral placebo. | |
| Allocation: randomised. Participants: chronic schizophrenia, same antipsychotic treatment for at least one month before study entry. Intervention: pimozide, placebo. Outcome: no usable data for relevant outcomes (data for the double‐blind phase are not avaiable). | |
| Allocation: randomised. Participants: diagnosed with non‐affective psychosis (first episode), receiving antipsychotic treatment for 12 months since clinical stabilisation, at the same dose for at least 4 months. Intervention: continual antipsychotic treatment, treatment discontinuation. Outcome: study not performed (stopped after recruitment of 16 patients), no data available. | |
| Allocation: randomised. Participants: not stable. | |
| Allocation: randomised. Participants: unclear if clinically stable, probabily not taking antipsychotics before study entry. Intervention: thiopropazate, placebo; cross‐over design. Outcome: no usable data for relevant outcomes (data up to the point of first cross‐over are not available). | |
| Allocation: not randomised. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: schizophrenia, not stabilised on antipsychotic drugs, because all had been withdrawn from antipsychotic drugs for 8 to 20 months before study start. | |
| Allocation: randomised. Participants: participants with newly diagnosed schizophrenia spectrum disorder, from the outpatient early intervention program (OPUS), meeting remission criteria for at least 3 months before study entry. Intervention: maintenance treatment with antipsychotics versus tapering/discontinuation; the control arm does not necessarily imply complete discontinuation of antipsychotic medication in all cases. | |
| Allocation: randomised. Participants: schizophrenia, not described as clinically stable in inclusion criteria. | |
| Allocation: randomised. Participants: schizophrenia. Intervention: depot antipsychotics (fluphenazine depot, flupenthixol depot or clopenthixol depot) plus oral dihomo gammalinolenic acid (DHLA) versus oral DHLA plus placebo injections versus DHLA placebo capsules and placebo injections. What is lacking is a depot antipsychotic only group. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: psychotic participants. Intervention: fluphenazine enanthate versus fluphenazine decanoate. | |
| Allocation: randomised. Participants: acute exacerbation of schizophrenia. | |
| Allocation: randomised. Participants: young people with a first episode of affective/non‐affective psychosis (unclear proportion), meeting remission criteria for at least 3 months. Intervention: maintenance treatment with antipsychotic drugs versus dose reduction strategy; no real discontinuation or placebo arm. | |
| Allocation: randomised. Participants: schizophrenia. Intervention: continuation of current antipsychotic versus gradual withdrawal. However, antipsychotic was given again when early warning signs appeared, i.e. intermittent treatment, a design that was excluded a prior by our protocol. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: schizophrenia and related psychotic disorder. Intervention: continuation of current antipsychotic versus gradual withdrawal. However, antipsychotic was given again when early warning signs appeared, i.e. intermittent treatment, a design that was excluded by the protocol. Approximately 50% of participants were never withdrawn. | |
| Allocation: all participants were in hospital. 95 were allocated to placebo (not randomly). Then 81 participants were quote: "selected at random to match” the intervention group. We feel that this is not an appropriate method of randomisation. | |
| Allocation: randomised. Participants: people with schizophrenia, experiencing an acute episode. | |
| Allocation: randomised. Participants: more than 50% had mental retardation, not schizophrenia. |
DSM‐III‐R: Diagnostic and Statistical Manual of Mental Disorders, Third Edition‐Revised
LAI: LAI: long‐acting injectable
Characteristics of studies awaiting classification [ordered by study ID]
| Methods | Allocation: post‐hoc analysis of a 1‐year randomised open‐label trial. |
| Participants | Diagnosis: schizophrenia. |
| Interventions | 1. Switching of antipsychotic medication 2. Discontinuation of antipsychotic therapy |
| Outcomes | Change scores on standard efficacy and tolerability measures (no usable data reported). |
| Notes | The conference abstract did not report any usable data for outcomes of interest in this review. We tried to contact the trials Authors to ask for further data but did not receive any reply. |
| Methods | Allocation: the study is described as double‐blind; no details about random sequence generation and allocation concealment procedure. Cross‐over design. |
| Participants | Diagnosis: schizophrenia. No details about the baseline clinical status. |
| Interventions | 1. Standard antipsychotics 2. Placebo |
| Outcomes | Efficacy, analysis based on the COMT Val108/158Met polymorphism (no usable data reported). |
| Notes | The conference abstract did not report any usable data for outcomes of interest in this review. We tried to contact the trial Authors to ask for further data but did not receive any reply. |
| Methods | Allocation: the study is described as blinded; no details about random sequence generation and allocation concealment. |
| Participants | Diagnosis: schizophrenia or schizoaffective disorder. No details about the baseline clinical status. |
| Interventions | 1. Atypical antipsychotic monotherapy 2. Placebo |
| Outcomes | Cognitive function, positron emission tomography scanning (no predefined outcomes of interest). |
| Notes | The conference abstract did not report any usable data for outcomes of interest in this review. We tried to contact the trial authors to ask for further data but did not receive an informative reply. |
| Methods | Allocation: randomised. Location: multi‐centre. |
| Participants | Diagnosis: stable schizophrenia. |
| Interventions | 1, Bifeprunox (not marketed drug) 2. Quetiapine 3. Placebo |
| Outcomes | Standard efficacy, safety and tolerability measures. |
| Notes | Prematurely ended, no data available. We were not able to find further information. |
| Methods | Allocation: randomised. Setting: inpatients. |
| Participants | Diagnosis: "deteriorated" schizophrenia, on antipsychotic treatment before study entry (no details). |
| Interventions | 1. Standard antipsychotic treatment 2. Discontinuation of antipsychotic treatment |
| Outcomes | Efficacy on negative symptoms (no predefined outcome of interest). |
| Notes | The paper did not report any usable data for outcomes of interest in this review. We tried to contact the trial authors to ask for further data but did not receive an informative reply. |
Characteristics of ongoing studies [ordered by study ID]
| Study name | A multicenter, randomized, double‐blind, placebo‐controlled study to evaluate the efficacy, safety, and tolerability of risperidone extended‐release injectable suspension (TV‐46000) for subcutaneous use as maintenance treatment in adult and adolescent patients with schizophrenia. |
| Methods | Randomised controlled trial. |
| Participants | Individuals diagnosed with schizophrenia, clinically stable and eligible for risperidone treatment. |
| Interventions | Risperidone ER injectable suspension, subcutaneous injections (two different dose regimens) versus placebo. |
| Outcomes | Efficacy, safety and tolerability outcomes (time to impending relapse, number maintaining stability, number acheiving remission, number with adverse events). |
| Starting date | April 2018 |
| Contact information | |
| Notes |
| Study name | Clinical trial evaluating the efficacy, safety and tolerability of cariprazine in a dose‐reduction paradigm in the prevention of relapse in patients with schizophrenia. |
| Methods | Randomised controlled trial. |
| Participants | Schizophrenia, in maintenance/relapse prevention phase. |
| Interventions | Cariprazine (two different dose regimens) versus placebo. |
| Outcomes | Time to impending relapse. |
| Starting date | July 2018 |
| Contact information | |
| Notes |
| Study name | A study to test if TV‐46000 is safe for maintenance treatment of schizophrenia |
| Methods | Randomised controlled trial. |
| Participants | Schizophrenia, in maintenance/relapse prevention phase. |
| Interventions | TV‐46000 (risperidone extended release injectable suspension) versus matching placebo. |
| Outcomes | Number of adverse events, dropouts due to adverse events. |
| Starting date | April 2019 |
| Contact information | |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Relapse: 1. Within pre‐specified time periods Show forest plot | 71 | 19996 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.33, 0.40] |
| Analysis 1.1  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 1: Relapse: 1. Within pre‐specified time periods | ||||
| 1.1.1 up to 3 months | 44 | 6362 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.28, 0.40] |
| 1.1.2 4‐6 months | 49 | 7599 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.31, 0.42] |
| 1.1.3 7‐12 months | 30 | 4249 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.32, 0.45] |
| 1.1.4 > 12 months | 10 | 1786 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.33, 0.64] |
| 1.2 Relapse: 2. Independent of duration Show forest plot | 71 | 8666 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.30, 0.40] |
| Analysis 1.2  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 2: Relapse: 2. Independent of duration | ||||
| 1.3 Leaving the study early: 1. Due to any reason (acceptability of treatment) Show forest plot | 56 | 7001 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.49, 0.61] |
| Analysis 1.3  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 3: Leaving the study early: 1. Due to any reason (acceptability of treatment) | ||||
| 1.3.1 up to 3 months | 11 | 517 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.17, 0.67] |
| 1.3.2 4 to 6 months | 18 | 1792 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.37, 0.65] |
| 1.3.3 7 to 12 months | 24 | 3951 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.48, 0.65] |
| 1.3.4 > 12 months | 5 | 741 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.51, 0.82] |
| 1.4 Leaving the study early: 2. Due to adverse events (overall tolerability) Show forest plot | 53 | 6627 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [0.85, 1.89] |
| Analysis 1.4  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 4: Leaving the study early: 2. Due to adverse events (overall tolerability) | ||||
| 1.4.1 up to 3 months | 10 | 371 | Risk Ratio (M‐H, Random, 95% CI) | 2.84 [0.12, 65.34] |
| 1.4.2 4 to 6 months | 15 | 1852 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.63, 2.28] |
| 1.4.3 7 to 12 months | 23 | 3870 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.69, 1.97] |
| 1.4.4 > 12 months | 5 | 534 | Risk Ratio (M‐H, Random, 95% CI) | 5.70 [1.28, 25.33] |
| 1.5 Leaving the study early: 3. Due to inefficacy Show forest plot | 55 | 6537 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.32, 0.43] |
| Analysis 1.5  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 5: Leaving the study early: 3. Due to inefficacy | ||||
| 1.5.1 up to 3 months | 11 | 421 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.07, 0.64] |
| 1.5.2 4 to 6 months | 16 | 1661 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.31, 0.54] |
| 1.5.3 7 to 12 months | 24 | 3951 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.31, 0.44] |
| 1.5.4 > 12 months | 4 | 504 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.29, 0.64] |
| 1.6 Global state: number of participants improved (at least minimally) Show forest plot | 16 | 1878 | Risk Ratio (M‐H, Random, 95% CI) | 2.12 [1.58, 2.85] |
| Analysis 1.6  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 6: Global state: number of participants improved (at least minimally) | ||||
| 1.6.1 up to 3 months | 3 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 4.76 [1.65, 13.68] |
| 1.6.2 4 to 6 months | 8 | 1037 | Risk Ratio (M‐H, Random, 95% CI) | 2.33 [1.69, 3.21] |
| 1.6.3 7 to 12 months | 4 | 388 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [0.89, 3.13] |
| 1.6.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.88, 2.09] |
| 1.7 Global state: number of participants in symptomatic remission Show forest plot | 7 | 867 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [1.20, 2.48] |
| Analysis 1.7  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 7: Global state: number of participants in symptomatic remission | ||||
| 1.7.1 up to 3 months | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [0.63, 10.00] |
| 1.7.2 4 to 6 months | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.79, 3.87] |
| 1.7.3 7 to 12 months | 5 | 807 | Risk Ratio (M‐H, Random, 95% CI) | 1.70 [1.11, 2.59] |
| 1.8 Global state: number of participants in sustained remission Show forest plot | 8 | 1807 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [1.28, 2.19] |
| Analysis 1.8  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 8: Global state: number of participants in sustained remission | ||||
| 1.8.1 7 to 12 months | 6 | 1443 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.49, 2.25] |
| 1.8.2 >12 months | 2 | 364 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.13, 1.47] |
| 1.9 Service use: number of participants hospitalised Show forest plot | 21 | 3558 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.32, 0.57] |
| Analysis 1.9  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 9: Service use: number of participants hospitalised | ||||
| 1.9.1 up to 3 months | 2 | 55 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.04, 4.06] |
| 1.9.2 4 to 6 months | 4 | 419 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.03, 1.32] |
| 1.9.3 7 to 12 months | 11 | 2119 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.23, 0.56] |
| 1.9.4 > 12 months | 4 | 965 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.44, 0.69] |
| 1.10 Service use: number of participants discharged Show forest plot | 3 | 404 | Risk Ratio (M‐H, Random, 95% CI) | 2.76 [0.69, 11.06] |
| Analysis 1.10  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 10: Service use: number of participants discharged | ||||
| 1.10.1 4 to 6 months | 3 | 404 | Risk Ratio (M‐H, Random, 95% CI) | 2.76 [0.69, 11.06] |
| 1.11 Death: due to any reason Show forest plot | 25 | 5181 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.39, 2.11] |
| Analysis 1.11  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 11: Death: due to any reason | ||||
| 1.11.1 up to 3 months | 3 | 415 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.11.2 4 to 6 months | 6 | 1159 | Risk Ratio (M‐H, Random, 95% CI) | 2.30 [0.59, 8.98] |
| 1.11.3 7 to 12 months | 15 | 3273 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.11, 1.12] |
| 1.11.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 5.18 [0.25, 107.12] |
| 1.12 Death: due to natural causes Show forest plot | 25 | 5226 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.50, 3.60] |
| Analysis 1.12  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 12: Death: due to natural causes | ||||
| 1.12.1 up to 3 months | 2 | 379 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.12.2 4 to 6 months | 6 | 1159 | Risk Ratio (M‐H, Random, 95% CI) | 2.30 [0.59, 8.98] |
| 1.12.3 7 to 12 months | 16 | 3354 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.11, 2.58] |
| 1.12.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 3.11 [0.13, 75.78] |
| 1.13 Death: due to suicide Show forest plot | 19 | 4634 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.12, 2.97] |
| Analysis 1.13  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 13: Death: due to suicide | ||||
| 1.13.1 up to 3 months | 3 | 415 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.13.2 4 to 6 months | 3 | 1033 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.13.3 7 to 12 months | 12 | 2852 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.06, 2.21] |
| 1.13.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 3.11 [0.13, 75.78] |
| 1.14 Number with suicide attempts Show forest plot | 12 | 3123 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.19, 1.99] |
| Analysis 1.14  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 14: Number with suicide attempts | ||||
| 1.14.1 4 to 6 months | 3 | 776 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 71.51] |
| 1.14.2 7 to 12 months | 9 | 2347 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.13, 1.69] |
| 1.15 Number with suicide ideation Show forest plot | 13 | 3255 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.33, 1.16] |
| Analysis 1.15  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 15: Number with suicide ideation | ||||
| 1.15.1 up to 3 months | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.01, 3.88] |
| 1.15.2 4 to 6 months | 1 | 386 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.15.3 7 to 12 months | 10 | 2486 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.24, 1.09] |
| 1.15.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [0.35, 4.74] |
| 1.16 Violent/aggressive behaviour Show forest plot | 12 | 2856 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.24, 0.59] |
| Analysis 1.16  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 16: Violent/aggressive behaviour | ||||
| 1.16.1 up to 3 months | 1 | 26 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.50] |
| 1.16.2 4 to 6 months | 2 | 350 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.20, 1.08] |
| 1.16.3 7 to 12 months | 8 | 2146 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.19, 0.66] |
| 1.16.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.01, 4.28] |
| 1.17 Adverse effects: at least one adverse event Show forest plot | 18 | 4352 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.98, 1.25] |
| Analysis 1.17  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 17: Adverse effects: at least one adverse event | ||||
| 1.17.1 up to 3 months | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.30, 0.93] |
| 1.17.2 4 to 6 months | 4 | 1079 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.85, 1.12] |
| 1.17.3 7 to 12 months | 12 | 2890 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.99, 1.33] |
| 1.17.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [1.24, 2.45] |
| 1.18 Adverse effects: movement disorders: at least one movement disorder Show forest plot | 29 | 5276 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.25, 1.85] |
| Analysis 1.18  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 18: Adverse effects: movement disorders: at least one movement disorder | ||||
| 1.18.1 up to 3 months | 4 | 158 | Risk Ratio (M‐H, Random, 95% CI) | 2.42 [0.70, 8.33] |
| 1.18.2 4 to 6 months | 8 | 1658 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [1.06, 1.99] |
| 1.18.3 7 to 12 months | 16 | 3126 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [1.17, 2.05] |
| 1.18.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.58, 2.54] |
| 1.19 Adverse effects: movement disorders: akathisia Show forest plot | 21 | 4214 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.93, 2.38] |
| Analysis 1.19  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 19: Adverse effects: movement disorders: akathisia | ||||
| 1.19.1 up to 3 months | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 2.68 [0.49, 14.82] |
| 1.19.2 4 to 6 months | 6 | 1191 | Risk Ratio (M‐H, Random, 95% CI) | 2.14 [0.50, 9.11] |
| 1.19.3 7 to 12 months | 12 | 2620 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.71, 1.61] |
| 1.19.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [0.42, 7.11] |
| 1.20 Adverse effects: movement disorders: akinesia Show forest plot | 3 | 397 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.08, 3.42] |
| Analysis 1.20  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 20: Adverse effects: movement disorders: akinesia | ||||
| 1.20.1 up to 3 months | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.09, 9.92] |
| 1.20.2 7 to 12 months | 2 | 348 | Risk Ratio (M‐H, Random, 95% CI) | 0.16 [0.01, 3.98] |
| 1.21 Adverse effects: movement disorders: dyskinesia Show forest plot | 18 | 3200 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.33, 0.91] |
| Analysis 1.21  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 21: Adverse effects: movement disorders: dyskinesia | ||||
| 1.21.1 up to 3 months | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [0.06, 34.91] |
| 1.21.2 4 to 6 months | 3 | 418 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.11, 0.84] |
| 1.21.3 7 to 12 months | 13 | 2399 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.37, 1.27] |
| 1.21.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.04, 3.29] |
| 1.22 Adverse effects: movement disorders: dystonia Show forest plot | 13 | 2767 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.99, 2.70] |
| Analysis 1.22  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 22: Adverse effects: movement disorders: dystonia | ||||
| 1.22.1 up to 3 months | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [0.13, 49.22] |
| 1.22.2 4 to 6 months | 2 | 382 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.94, 3.29] |
| 1.22.3 7 to 12 months | 9 | 2002 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.65, 4.09] |
| 1.22.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.01, 4.28] |
| 1.23 Adverse effects: movement disorders: rigor Show forest plot | 9 | 922 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.70, 2.79] |
| Analysis 1.23  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 23: Adverse effects: movement disorders: rigor | ||||
| 1.23.1 up to 3 months | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.22, 6.62] |
| 1.23.2 4 to 6 months | 3 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 1.98 [0.67, 5.85] |
| 1.23.3 7 to 12 months | 4 | 693 | Risk Ratio (M‐H, Random, 95% CI) | 1.80 [0.29, 11.24] |
| 1.24 Adverse effects: movement disorders: tremor Show forest plot | 18 | 3353 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.95, 1.98] |
| Analysis 1.24  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 24: Adverse effects: movement disorders: tremor | ||||
| 1.24.1 up to 3 months | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.46, 3.16] |
| 1.24.2 4 to 6 months | 3 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.33, 2.61] |
| 1.24.3 7 to 12 months | 12 | 2790 | Risk Ratio (M‐H, Random, 95% CI) | 1.62 [1.04, 2.54] |
| 1.24.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.10, 2.79] |
| 1.25 Adverse effects: movement disorders: use of antiparkinson medication Show forest plot | 13 | 2908 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [1.10, 1.65] |
| Analysis 1.25  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 25: Adverse effects: movement disorders: use of antiparkinson medication | ||||
| 1.25.1 4 to 6 months | 3 | 841 | Risk Ratio (M‐H, Random, 95% CI) | 1.53 [0.90, 2.61] |
| 1.25.2 7 to 12 months | 9 | 1733 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [1.06, 1.78] |
| 1.25.3 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.64, 1.57] |
| 1.26 Adverse effects: sedation Show forest plot | 18 | 4078 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.24, 1.86] |
| Analysis 1.26  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 26: Adverse effects: sedation | ||||
| 1.26.1 up to 3 months | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.01, 3.70] |
| 1.26.2 4 to 6 months | 7 | 1880 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.89, 2.12] |
| 1.26.3 7 to 12 months | 9 | 1844 | Risk Ratio (M‐H, Random, 95% CI) | 1.78 [1.25, 2.53] |
| 1.26.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.15, 7.27] |
| 1.27 Adverse effects: weight gain Show forest plot | 19 | 4767 | Risk Ratio (M‐H, Random, 95% CI) | 1.69 [1.21, 2.35] |
| Analysis 1.27  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 27: Adverse effects: weight gain | ||||
| 1.27.1 4 to 6 months | 4 | 1039 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.81, 2.73] |
| 1.27.2 7 to 12 months | 14 | 3394 | Risk Ratio (M‐H, Random, 95% CI) | 1.80 [1.17, 2.77] |
| 1.27.3 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 2.18 [1.06, 4.48] |
| 1.28 Participant´s satisfaction with care Show forest plot | 2 | 737 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [1.10, 1.33] |
| Analysis 1.28  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 28: Participant´s satisfaction with care | ||||
| 1.28.1 7 to 12 months | 1 | 403 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [1.02, 1.38] |
| 1.28.2 > 12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [1.08, 1.38] |
| 1.29 Quality of life (various scales, different timepoints) Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.29  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 29: Quality of life (various scales, different timepoints) | ||||
| 1.29.1 up to 3 months ‐ Schizophrenia Quality of Life at endpoint (low score=better) | 2 | 379 | Mean Difference (IV, Random, 95% CI) | ‐2.00 [‐5.80, 1.80] |
| 1.29.2 7 to 12 months ‐ Self‐report Quality of Life Scale change from baseline to endpoint (low score=better) | 2 | 595 | Mean Difference (IV, Random, 95% CI) | ‐4.10 [‐6.32, ‐1.88] |
| 1.29.3 7 to 12 months ‐ Heinrichs Carpenter Quality of Life Scale change from baseline to endpoint (low score=better) | 1 | 304 | Mean Difference (IV, Random, 95% CI) | ‐11.36 [‐14.67, ‐8.05] |
| 1.29.4 7 to 12 months ‐ European Quality of Life Visual Analog Scale at endpoint (low score=better) | 1 | 277 | Mean Difference (IV, Random, 95% CI) | ‐6.30 [‐23.41, 10.81] |
| 1.29.5 > 12 months ‐ Symptom Questionnaire of Kellner and Sheffield at endpoint (low score=better) | 1 | 18 | Mean Difference (IV, Random, 95% CI) | ‐4.90 [‐14.33, 4.53] |
| 1.30 Quality of life (across all scales and timepoints) Show forest plot | 7 | 1573 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.57, ‐0.07] |
| Analysis 1.30  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 30: Quality of life (across all scales and timepoints) | ||||
| 1.31 Number of participants in employment Show forest plot | 3 | 593 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.82, 1.41] |
| Analysis 1.31  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 31: Number of participants in employment | ||||
| 1.31.1 7 to 12 months | 2 | 259 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.75, 1.23] |
| 1.31.2 > 12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.97, 2.00] |
| 1.32 Social Functioning (various scales, different timepoints) Show forest plot | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.32  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 32: Social Functioning (various scales, different timepoints) | ||||
| 1.32.1 up to 3 months ‐ Personal and Social Performance at endpoint (low score=better) | 2 | 379 | Mean Difference (IV, Random, 95% CI) | ‐5.66 [‐11.50, 0.18] |
| 1.32.2 up to 3 months ‐ Global Assessment Scale at endpoint (low score=better) | 1 | 120 | Mean Difference (IV, Random, 95% CI) | ‐3.61 [‐4.66, ‐2.56] |
| 1.32.3 4 to 6 months ‐ Sheehan Disability Schedule change from baseline to endpoint (low score=better) | 1 | 270 | Mean Difference (IV, Random, 95% CI) | ‐2.00 [‐3.60, ‐0.40] |
| 1.32.4 7 to 12 months ‐ Personal and Social Performance change from baseline to endpoint (low score=better) | 7 | 1823 | Mean Difference (IV, Random, 95% CI) | ‐4.92 [‐5.96, ‐3.89] |
| 1.32.5 7 to 12 months ‐ Global Assessment of Functioning at endpoint (low score=better) | 1 | 275 | Mean Difference (IV, Random, 95% CI) | ‐8.80 [‐13.22, ‐4.38] |
| 1.32.6 7 to 12 months ‐ Specific Levels of Functioning change from baseline to endpoint (low score=better) | 1 | 246 | Mean Difference (IV, Random, 95% CI) | ‐2.40 [‐4.85, 0.05] |
| 1.32.7 7 to 12 months ‐ Children Global Assessment Scale change from baseline to endpoint (low score=better) | 1 | 146 | Mean Difference (IV, Random, 95% CI) | ‐4.60 [‐9.84, 0.64] |
| 1.32.8 > 12 months ‐ Personal and Social Performance change from baseline to endpoint (low score=better) | 1 | 329 | Mean Difference (IV, Random, 95% CI) | ‐3.60 [‐6.76, ‐0.44] |
| 1.33 Social Functioning (across all scales and timepoints) Show forest plot | 15 | 3588 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.53, ‐0.34] |
| Analysis 1.33  Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 33: Social Functioning (across all scales and timepoints) | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Subgroup analysis: participants with a first episode Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.33, 0.46] |
| Analysis 2.1  Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 1: Subgroup analysis: participants with a first episode | ||||
| 2.1.1 first episode | 8 | 528 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.38, 0.58] |
| 2.1.2 not first episode | 24 | 3585 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.31, 0.46] |
| 2.2 Subgroup analysis: participants in remission at baseline Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.32, 0.46] |
| Analysis 2.2  Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 2: Subgroup analysis: participants in remission at baseline | ||||
| 2.2.1 in remission | 10 | 1050 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.33, 0.60] |
| 2.2.2 not in remission | 19 | 3063 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.30, 0.44] |
| 2.3 Subgroup analysis: various durations of stability before entering the study Show forest plot | 24 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.3  Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 3: Subgroup analysis: various durations of stability before entering the study | ||||
| 2.3.1 stable at least 1 month | 6 | 574 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.20, 0.50] |
| 2.3.2 stable at least 3 months | 10 | 2250 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.26, 0.43] |
| 2.3.3 stable at least 6 months | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 2.69] |
| 2.3.4 stable at least 12 months | 5 | 326 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.17, 0.57] |
| 2.3.5 stable at least 3 to 6 years | 2 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.18, 0.78] |
| 2.4 Subgroup analysis: abrupt withdrawal versus tapering Show forest plot | 29 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.4  Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 4: Subgroup analysis: abrupt withdrawal versus tapering | ||||
| 2.4.1 Abrupt withdrawal | 18 | 2348 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.35, 0.53] |
| 2.4.2 Taper | 11 | 1765 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.24, 0.44] |
| 2.5 Subgroup analysis: single antipsychotic drugs Show forest plot | 29 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.5  Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 5: Subgroup analysis: single antipsychotic drugs | ||||
| 2.5.1 Chlorpromazine | 2 | 406 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.36, 0.55] |
| 2.5.2 Fluphenazine depot | 6 | 296 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.14, 0.39] |
| 2.5.3 Haloperidol depot | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.04, 0.55] |
| 2.5.4 Various, mixed groups of antipsychotic drugs | 10 | 705 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.27, 0.65] |
| 2.5.5 Quetiapine | 1 | 178 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.34, 0.69] |
| 2.5.6 Paliperidone | 4 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.31, 0.44] |
| 2.5.7 Aripiprazole | 2 | 549 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.14, 0.86] |
| 2.5.8 Brexpiprazole | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.23, 0.56] |
| 2.5.9 Ziprasidone | 1 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.39, 0.64] |
| 2.5.10 Cariprazine | 1 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.38, 0.77] |
| 2.6 Subgroup analysis: depot versus oral drugs Show forest plot | 26 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.6  Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 6: Subgroup analysis: depot versus oral drugs | ||||
| 2.6.1 depot | 10 | 1705 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.23, 0.39] |
| 2.6.2 oral | 16 | 2187 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.38, 0.55] |
| 2.7 Subgroup analysis: first‐ versus second‐generation antipsychotic drugs Show forest plot | 29 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.7  Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 7: Subgroup analysis: first‐ versus second‐generation antipsychotic drugs | ||||
| 2.7.1 First‐generation antipsychotic drugs | 18 | 1430 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.25, 0.48] |
| 2.7.2 Second‐generation antipsychotic drugs | 11 | 2683 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.32, 0.48] |
| 2.8 Subgroup analysis: appropriate versus unclear allocation concealment Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.32, 0.46] |
| Analysis 2.8  Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 8: Subgroup analysis: appropriate versus unclear allocation concealment | ||||
| 2.8.1 appropriate allocation concealment | 13 | 2708 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.30, 0.45] |
| 2.8.2 unclear allocation concealment | 16 | 1405 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.30, 0.54] |
| 2.9 Subgroup analysis: blinded versus open trials Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.32, 0.46] |
| Analysis 2.9  Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 9: Subgroup analysis: blinded versus open trials | ||||
| 2.9.1 blinded trials | 27 | 3856 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.33, 0.48] |
| 2.9.2 unblinded trials | 2 | 257 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.17, 0.39] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Exclusion of studies that were not explicitly described as randomised Show forest plot | 28 | 4098 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.33, 0.46] |
| Analysis 3.1  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 1: Exclusion of studies that were not explicitly described as randomised | ||||
| 3.2 Exclusion of non‐double‐blind studies Show forest plot | 27 | 3856 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.33, 0.48] |
| Analysis 3.2  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 2: Exclusion of non‐double‐blind studies | ||||
| 3.3 Fixed‐effects model Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.35, 0.41] |
| Analysis 3.3  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 3: Fixed‐effects model | ||||
| 3.4 Original authors' assumptions on dropouts Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.32, 0.46] |
| Analysis 3.4  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 4: Original authors' assumptions on dropouts | ||||
| 3.5 Inclusion of only large studies (> 200 participants) Show forest plot | 10 | 2950 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.31, 0.45] |
| Analysis 3.5  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 5: Inclusion of only large studies (> 200 participants) | ||||
| 3.6 Exclusion of studies with clinical diagnosis Show forest plot | 22 | 4054 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.34, 0.48] |
| Analysis 3.6  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 6: Exclusion of studies with clinical diagnosis | ||||
| 3.7 Three months stable Show forest plot | 29 | 4622 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.24, 0.42] |
| Analysis 3.7  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 7: Three months stable | ||||
| 3.8 Six months stable Show forest plot | 20 | 2549 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.20, 0.45] |
| Analysis 3.8  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 8: Six months stable | ||||
| 3.9 Nine months stable Show forest plot | 15 | 1806 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.19, 0.52] |
| Analysis 3.9  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 9: Nine months stable | ||||
| 3.10 Exclusion of studies with unclear randomisation method Show forest plot | 11 | 2644 | Risk Ratio (IV, Random, 95% CI) | 0.36 [0.29, 0.43] |
| Analysis 3.10  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 10: Exclusion of studies with unclear randomisation method | ||||
| 3.11 Exclusion of studies with unclear allocation concealment method Show forest plot | 13 | 2708 | Risk Ratio (IV, Random, 95% CI) | 0.37 [0.30, 0.45] |
| Analysis 3.11  Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 11: Exclusion of studies with unclear allocation concealment method | ||||

Study flow diagram (results of the original search)
For the review update in 2018: 3 reports describing the 2 studies originally excluded from quantitative synthesis were moved to excluded studies (no usable data for outcomes of interest); 3 reports on 1 study, originally excluded (short duration of follow‐up), were moved to included studies; one report originally included as independent study was moved as secondary publication of another included study.

Study flow diagram (results of the 2017/2018/2019 update search and combined results of the original search and the update search)

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.

Funnel plot of comparison: 1 Maintenance treatment with antipsychotic drugs versus placebo/no treatment, outcome: Relapse

Meta‐regression on duration of clinical stability before study start (relapse at 12 months)
The size of the bubbles is proportional to the inverse variance of the treatment effect.

Meta‐regression on duration of taper in the placebo group (relapse at 12 months)
The size of the bubbles is proportional to the inverse variance of treatment effect.
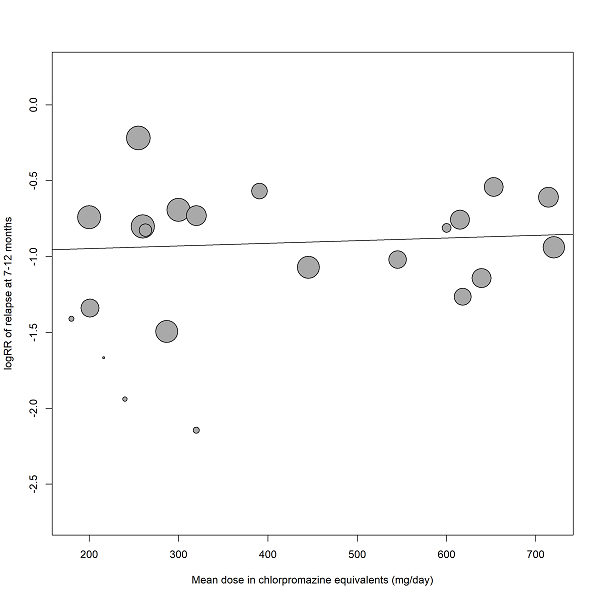
Meta‐regression on mean dose in chlorpromazine equivalents (relapse at 12 months)
The size of the bubbles is proportional to the inverse variance of treatment effect.

Meta‐regression on study duration (relapse, all studies included).
The size of the bubbles is proportional to the inverse variance of treatment effect.

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 1: Relapse: 1. Within pre‐specified time periods

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 2: Relapse: 2. Independent of duration

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 3: Leaving the study early: 1. Due to any reason (acceptability of treatment)

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 4: Leaving the study early: 2. Due to adverse events (overall tolerability)

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 5: Leaving the study early: 3. Due to inefficacy

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 6: Global state: number of participants improved (at least minimally)

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 7: Global state: number of participants in symptomatic remission

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 8: Global state: number of participants in sustained remission

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 9: Service use: number of participants hospitalised

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 10: Service use: number of participants discharged

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 11: Death: due to any reason

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 12: Death: due to natural causes

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 13: Death: due to suicide

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 14: Number with suicide attempts

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 15: Number with suicide ideation

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 16: Violent/aggressive behaviour

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 17: Adverse effects: at least one adverse event

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 18: Adverse effects: movement disorders: at least one movement disorder

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 19: Adverse effects: movement disorders: akathisia

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 20: Adverse effects: movement disorders: akinesia

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 21: Adverse effects: movement disorders: dyskinesia

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 22: Adverse effects: movement disorders: dystonia

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 23: Adverse effects: movement disorders: rigor

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 24: Adverse effects: movement disorders: tremor

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 25: Adverse effects: movement disorders: use of antiparkinson medication

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 26: Adverse effects: sedation

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 27: Adverse effects: weight gain

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 28: Participant´s satisfaction with care

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 29: Quality of life (various scales, different timepoints)

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 30: Quality of life (across all scales and timepoints)

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 31: Number of participants in employment

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 32: Social Functioning (various scales, different timepoints)

Comparison 1: Maintenance treatment with antipsychotic drugs versus placebo/no treatment, Outcome 33: Social Functioning (across all scales and timepoints)

Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 1: Subgroup analysis: participants with a first episode

Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 2: Subgroup analysis: participants in remission at baseline

Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 3: Subgroup analysis: various durations of stability before entering the study

Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 4: Subgroup analysis: abrupt withdrawal versus tapering

Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 5: Subgroup analysis: single antipsychotic drugs

Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 6: Subgroup analysis: depot versus oral drugs

Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 7: Subgroup analysis: first‐ versus second‐generation antipsychotic drugs

Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 8: Subgroup analysis: appropriate versus unclear allocation concealment

Comparison 2: Subgroup analysis (relapse at 12 months), Outcome 9: Subgroup analysis: blinded versus open trials

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 1: Exclusion of studies that were not explicitly described as randomised

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 2: Exclusion of non‐double‐blind studies

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 3: Fixed‐effects model

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 4: Original authors' assumptions on dropouts

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 5: Inclusion of only large studies (> 200 participants)

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 6: Exclusion of studies with clinical diagnosis

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 7: Three months stable

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 8: Six months stable

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 9: Nine months stable

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 10: Exclusion of studies with unclear randomisation method

Comparison 3: Sensitivity analysis (relapse at 12 months), Outcome 11: Exclusion of studies with unclear allocation concealment method
| Methods | Allocation: randomised ‐ clearly described generation of sequence and concealment of allocation |
|---|---|
| Participants | People with schizophrenia or schizophrenia‐like disorder in remission for at least one month |
| Interventions | 1. Any antipsychotic drug (flexible dose within appropriate range) 2. Placebo (after gradual ‐ rather than abrupt ‐ withdrawal of the previous antipsychotic drug) |
| Outcomes | Relapse (primary outcome) Rehospitalisation for psychosis Global state (number of participants improved, in symptomatic and sustained remission) Global state (number of participants in recovery) Leaving the study early (including specific causes) Death (natural and unnatural causes) Violent behaviour Quality of life Satisfaction with care and other measures of subjective well‐being/recovery Side‐effects (well reported) Social functioning, employment and other measures of functioning |
| Maintenance treatment with antipsychotic drugs versus placebo/no treatment for schizophrenia | ||||||
| Patient or population: schizophrenia | ||||||
| Outcomes | Illustrative comparative risks (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Assumed risk | Corresponding risk | |||||
| Control | Maintenance treatment with antipsychotic drugs versus placebo/no treatment | |||||
| Relapse: 7 to 12 months Follow‐up: 7‐12 months | 606 per 1.000 | 230 per 1.000 | RR 0.38 | 4249 | ⊕⊕⊕⊕ | |
| Leaving the study early: due to any reason (acceptability of treatment) Follow‐up: 1‐24 months | 541 per 1.000 | 292 per 1.000 | RR 0.54 | 7001 | ⊕⊕⊕⊕ | |
| Service use: number of participants hospitalised Follow‐up: 1‐36 months | 177 per 1.000 | 76 per 1.000 | RR 0.43 | 3558 | ⊕⊕⊕⊕ | |
| Death: due to suicide Follow‐up: 1‐15 months | 1 per 1.000 | 1 per 1.000 | RR 0.60 | 4634 | ⊕⊕⊝⊝ | |
| Quality of life (various scales; low score=better) Follow‐up: 3‐18 months | The mean quality of life in the intervention group was 0.32 standard deviations lower (from 0.57 to 0.07 standard deviations lower), with lower scores reflecting a better condition. | ‐ | 1573 | ⊕⊕⊝⊝ | SMD ‐0.32 (‐0.57 to ‐0.07) | |
| Number of participants in employment Follow‐up: 9‐15 months | 344 per 1.000 | 372 per 1.000 | RR 1.08 | 593 | ⊕⊕⊝⊝ | |
| Social functioning (various scales; low score=better) Follow‐up: 1‐15 months | The mean social functioning in the intervention group was 0.43 standard deviations lower (from 0.53 to 0.34 standard deviations lower), with lower scores reflecting a better condition. | ‐ | 3588 | ⊕⊕⊕⊝ | SMD ‐0.43 (‐0.53 to ‐0.34) | |
| *The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Publication bias: rated 'undetected' ‐ although the funnel plot was asymmetrical, the trim and fill test did not change the point estimate and the point estimate was also similar when only large studies were included (Analysis 3.5). 2 Risk of bias: rated 'no' ‐ many studies did not report the methods for sequence generation and/or allocation concealment. However, in subgroup analysis (Analysis 2.8) studies reporting high standards of methods showed a similar effect size as compared to studies with unclear methods. Also, in a sensitivity analysis excluding studies with unclear methods (Analysis 3.10 and Analysis 3.11), the effect sizes did not change substantially. Early terminated studies were not judged to contribute substantial weight to this outcome. 3 Inconsistency: rated 'no' ‐ the P value for heterogeneity was statistically significant and the I2 higher than 50%. However, results of individual studies differed rather in magnitude of effect (which could be partly explained by subgroup analyses) rather than in direction of effect. Therefore, this inconsistency does not challenge the overall results. 4 No indirectness was found in terms of study population nor of interventions. In terms of outcome, we followed the original authors definitions of relapse. These definitions used different criteria, but all addressed symptomatic deterioration related to relapse. Therefore, this was not judged to lead to indirectness. 5 Inconsistency: rated 'no' ‐ the P value for heterogeneity was statistically significant and the I‐square higher than 50%. However, results of individual studies differed rather in magnitude of effect than in direction of effect, which was the same in almost all the studies. Therefore, this inconsistency does not challenge the overall results. 6 Publication bias: it is unlikely that a study was unpublished because of unfavourable data in a secondary outcome. As a possible publication bias had no effect on the results for the primary outcome (relapse at 7 to 12 months), we deem that there was no relevant publication bias for this secondary outcome. 7 Indirectness: hospitalisation due to relapse was our primary interest, but in some studies reasons for hospitalisation were unclearly reported. Overall, we do not deem that this uncertainty was an important source of indirectness. 8 Imprecision: rated 'very serious' ‐ only few studies with few events contributed data to this outcome. The CI was wide, ranging from substantial harm to substantial benefit. 9 Risk of bias: rated 'serious' ‐ five out of seven studies were terminated early after interim analyses, possibly leading to overestimation of effect. 10 Indirectness: some rating scales used in the studies have been criticised for eventually not measuring what people understand by quality of life. However, it was decided not to further lower the quality of evidence for this outcome after downgrading for other factors, despite some uncertainty. 11 Imprecise data ‐ only a few studies provided data for this outcome and the confidence interval was large. 12 Indirectness: rated 'serious' ‐ the only three studies included mixed groups of employed and non‐employed participants at baseline, and it is unclear whether employment was supported or competitive employment. 13 Imprecision: rated 'serious' ‐ only three studies contributed to this event which depends on various factors (e.g. the existence of supported employment, rural versus service economy etc). 14 Risk of bias: rated 'serious' ‐ eleven out of fifteen studies were terminated early after interim analyses, possibly leading to overestimation of effects. 15 Indirectness: rated 'no' ‐ different rating scales were used in the studies, but this was not judged to challenge the results. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1.1 Relapse: 1. Within pre‐specified time periods Show forest plot | 71 | 19996 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.33, 0.40] |
| 1.1.1 up to 3 months | 44 | 6362 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.28, 0.40] |
| 1.1.2 4‐6 months | 49 | 7599 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.31, 0.42] |
| 1.1.3 7‐12 months | 30 | 4249 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.32, 0.45] |
| 1.1.4 > 12 months | 10 | 1786 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.33, 0.64] |
| 1.2 Relapse: 2. Independent of duration Show forest plot | 71 | 8666 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.30, 0.40] |
| 1.3 Leaving the study early: 1. Due to any reason (acceptability of treatment) Show forest plot | 56 | 7001 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.49, 0.61] |
| 1.3.1 up to 3 months | 11 | 517 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.17, 0.67] |
| 1.3.2 4 to 6 months | 18 | 1792 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.37, 0.65] |
| 1.3.3 7 to 12 months | 24 | 3951 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.48, 0.65] |
| 1.3.4 > 12 months | 5 | 741 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.51, 0.82] |
| 1.4 Leaving the study early: 2. Due to adverse events (overall tolerability) Show forest plot | 53 | 6627 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [0.85, 1.89] |
| 1.4.1 up to 3 months | 10 | 371 | Risk Ratio (M‐H, Random, 95% CI) | 2.84 [0.12, 65.34] |
| 1.4.2 4 to 6 months | 15 | 1852 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.63, 2.28] |
| 1.4.3 7 to 12 months | 23 | 3870 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.69, 1.97] |
| 1.4.4 > 12 months | 5 | 534 | Risk Ratio (M‐H, Random, 95% CI) | 5.70 [1.28, 25.33] |
| 1.5 Leaving the study early: 3. Due to inefficacy Show forest plot | 55 | 6537 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.32, 0.43] |
| 1.5.1 up to 3 months | 11 | 421 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.07, 0.64] |
| 1.5.2 4 to 6 months | 16 | 1661 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.31, 0.54] |
| 1.5.3 7 to 12 months | 24 | 3951 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.31, 0.44] |
| 1.5.4 > 12 months | 4 | 504 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.29, 0.64] |
| 1.6 Global state: number of participants improved (at least minimally) Show forest plot | 16 | 1878 | Risk Ratio (M‐H, Random, 95% CI) | 2.12 [1.58, 2.85] |
| 1.6.1 up to 3 months | 3 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 4.76 [1.65, 13.68] |
| 1.6.2 4 to 6 months | 8 | 1037 | Risk Ratio (M‐H, Random, 95% CI) | 2.33 [1.69, 3.21] |
| 1.6.3 7 to 12 months | 4 | 388 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [0.89, 3.13] |
| 1.6.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.88, 2.09] |
| 1.7 Global state: number of participants in symptomatic remission Show forest plot | 7 | 867 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [1.20, 2.48] |
| 1.7.1 up to 3 months | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [0.63, 10.00] |
| 1.7.2 4 to 6 months | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.79, 3.87] |
| 1.7.3 7 to 12 months | 5 | 807 | Risk Ratio (M‐H, Random, 95% CI) | 1.70 [1.11, 2.59] |
| 1.8 Global state: number of participants in sustained remission Show forest plot | 8 | 1807 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [1.28, 2.19] |
| 1.8.1 7 to 12 months | 6 | 1443 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.49, 2.25] |
| 1.8.2 >12 months | 2 | 364 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.13, 1.47] |
| 1.9 Service use: number of participants hospitalised Show forest plot | 21 | 3558 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.32, 0.57] |
| 1.9.1 up to 3 months | 2 | 55 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.04, 4.06] |
| 1.9.2 4 to 6 months | 4 | 419 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.03, 1.32] |
| 1.9.3 7 to 12 months | 11 | 2119 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.23, 0.56] |
| 1.9.4 > 12 months | 4 | 965 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.44, 0.69] |
| 1.10 Service use: number of participants discharged Show forest plot | 3 | 404 | Risk Ratio (M‐H, Random, 95% CI) | 2.76 [0.69, 11.06] |
| 1.10.1 4 to 6 months | 3 | 404 | Risk Ratio (M‐H, Random, 95% CI) | 2.76 [0.69, 11.06] |
| 1.11 Death: due to any reason Show forest plot | 25 | 5181 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.39, 2.11] |
| 1.11.1 up to 3 months | 3 | 415 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.11.2 4 to 6 months | 6 | 1159 | Risk Ratio (M‐H, Random, 95% CI) | 2.30 [0.59, 8.98] |
| 1.11.3 7 to 12 months | 15 | 3273 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.11, 1.12] |
| 1.11.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 5.18 [0.25, 107.12] |
| 1.12 Death: due to natural causes Show forest plot | 25 | 5226 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.50, 3.60] |
| 1.12.1 up to 3 months | 2 | 379 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.12.2 4 to 6 months | 6 | 1159 | Risk Ratio (M‐H, Random, 95% CI) | 2.30 [0.59, 8.98] |
| 1.12.3 7 to 12 months | 16 | 3354 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.11, 2.58] |
| 1.12.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 3.11 [0.13, 75.78] |
| 1.13 Death: due to suicide Show forest plot | 19 | 4634 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.12, 2.97] |
| 1.13.1 up to 3 months | 3 | 415 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.13.2 4 to 6 months | 3 | 1033 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.13.3 7 to 12 months | 12 | 2852 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.06, 2.21] |
| 1.13.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 3.11 [0.13, 75.78] |
| 1.14 Number with suicide attempts Show forest plot | 12 | 3123 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.19, 1.99] |
| 1.14.1 4 to 6 months | 3 | 776 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 71.51] |
| 1.14.2 7 to 12 months | 9 | 2347 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.13, 1.69] |
| 1.15 Number with suicide ideation Show forest plot | 13 | 3255 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.33, 1.16] |
| 1.15.1 up to 3 months | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.01, 3.88] |
| 1.15.2 4 to 6 months | 1 | 386 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 1.15.3 7 to 12 months | 10 | 2486 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.24, 1.09] |
| 1.15.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [0.35, 4.74] |
| 1.16 Violent/aggressive behaviour Show forest plot | 12 | 2856 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.24, 0.59] |
| 1.16.1 up to 3 months | 1 | 26 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.50] |
| 1.16.2 4 to 6 months | 2 | 350 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.20, 1.08] |
| 1.16.3 7 to 12 months | 8 | 2146 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.19, 0.66] |
| 1.16.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.01, 4.28] |
| 1.17 Adverse effects: at least one adverse event Show forest plot | 18 | 4352 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.98, 1.25] |
| 1.17.1 up to 3 months | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.30, 0.93] |
| 1.17.2 4 to 6 months | 4 | 1079 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.85, 1.12] |
| 1.17.3 7 to 12 months | 12 | 2890 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.99, 1.33] |
| 1.17.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [1.24, 2.45] |
| 1.18 Adverse effects: movement disorders: at least one movement disorder Show forest plot | 29 | 5276 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.25, 1.85] |
| 1.18.1 up to 3 months | 4 | 158 | Risk Ratio (M‐H, Random, 95% CI) | 2.42 [0.70, 8.33] |
| 1.18.2 4 to 6 months | 8 | 1658 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [1.06, 1.99] |
| 1.18.3 7 to 12 months | 16 | 3126 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [1.17, 2.05] |
| 1.18.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.58, 2.54] |
| 1.19 Adverse effects: movement disorders: akathisia Show forest plot | 21 | 4214 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.93, 2.38] |
| 1.19.1 up to 3 months | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 2.68 [0.49, 14.82] |
| 1.19.2 4 to 6 months | 6 | 1191 | Risk Ratio (M‐H, Random, 95% CI) | 2.14 [0.50, 9.11] |
| 1.19.3 7 to 12 months | 12 | 2620 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.71, 1.61] |
| 1.19.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [0.42, 7.11] |
| 1.20 Adverse effects: movement disorders: akinesia Show forest plot | 3 | 397 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.08, 3.42] |
| 1.20.1 up to 3 months | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.09, 9.92] |
| 1.20.2 7 to 12 months | 2 | 348 | Risk Ratio (M‐H, Random, 95% CI) | 0.16 [0.01, 3.98] |
| 1.21 Adverse effects: movement disorders: dyskinesia Show forest plot | 18 | 3200 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.33, 0.91] |
| 1.21.1 up to 3 months | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [0.06, 34.91] |
| 1.21.2 4 to 6 months | 3 | 418 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.11, 0.84] |
| 1.21.3 7 to 12 months | 13 | 2399 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.37, 1.27] |
| 1.21.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.04, 3.29] |
| 1.22 Adverse effects: movement disorders: dystonia Show forest plot | 13 | 2767 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.99, 2.70] |
| 1.22.1 up to 3 months | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [0.13, 49.22] |
| 1.22.2 4 to 6 months | 2 | 382 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.94, 3.29] |
| 1.22.3 7 to 12 months | 9 | 2002 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.65, 4.09] |
| 1.22.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 0.21 [0.01, 4.28] |
| 1.23 Adverse effects: movement disorders: rigor Show forest plot | 9 | 922 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.70, 2.79] |
| 1.23.1 up to 3 months | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.22, 6.62] |
| 1.23.2 4 to 6 months | 3 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 1.98 [0.67, 5.85] |
| 1.23.3 7 to 12 months | 4 | 693 | Risk Ratio (M‐H, Random, 95% CI) | 1.80 [0.29, 11.24] |
| 1.24 Adverse effects: movement disorders: tremor Show forest plot | 18 | 3353 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.95, 1.98] |
| 1.24.1 up to 3 months | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.46, 3.16] |
| 1.24.2 4 to 6 months | 3 | 160 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.33, 2.61] |
| 1.24.3 7 to 12 months | 12 | 2790 | Risk Ratio (M‐H, Random, 95% CI) | 1.62 [1.04, 2.54] |
| 1.24.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.10, 2.79] |
| 1.25 Adverse effects: movement disorders: use of antiparkinson medication Show forest plot | 13 | 2908 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [1.10, 1.65] |
| 1.25.1 4 to 6 months | 3 | 841 | Risk Ratio (M‐H, Random, 95% CI) | 1.53 [0.90, 2.61] |
| 1.25.2 7 to 12 months | 9 | 1733 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [1.06, 1.78] |
| 1.25.3 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.64, 1.57] |
| 1.26 Adverse effects: sedation Show forest plot | 18 | 4078 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.24, 1.86] |
| 1.26.1 up to 3 months | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.01, 3.70] |
| 1.26.2 4 to 6 months | 7 | 1880 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.89, 2.12] |
| 1.26.3 7 to 12 months | 9 | 1844 | Risk Ratio (M‐H, Random, 95% CI) | 1.78 [1.25, 2.53] |
| 1.26.4 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.15, 7.27] |
| 1.27 Adverse effects: weight gain Show forest plot | 19 | 4767 | Risk Ratio (M‐H, Random, 95% CI) | 1.69 [1.21, 2.35] |
| 1.27.1 4 to 6 months | 4 | 1039 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.81, 2.73] |
| 1.27.2 7 to 12 months | 14 | 3394 | Risk Ratio (M‐H, Random, 95% CI) | 1.80 [1.17, 2.77] |
| 1.27.3 >12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 2.18 [1.06, 4.48] |
| 1.28 Participant´s satisfaction with care Show forest plot | 2 | 737 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [1.10, 1.33] |
| 1.28.1 7 to 12 months | 1 | 403 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [1.02, 1.38] |
| 1.28.2 > 12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [1.08, 1.38] |
| 1.29 Quality of life (various scales, different timepoints) Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.29.1 up to 3 months ‐ Schizophrenia Quality of Life at endpoint (low score=better) | 2 | 379 | Mean Difference (IV, Random, 95% CI) | ‐2.00 [‐5.80, 1.80] |
| 1.29.2 7 to 12 months ‐ Self‐report Quality of Life Scale change from baseline to endpoint (low score=better) | 2 | 595 | Mean Difference (IV, Random, 95% CI) | ‐4.10 [‐6.32, ‐1.88] |
| 1.29.3 7 to 12 months ‐ Heinrichs Carpenter Quality of Life Scale change from baseline to endpoint (low score=better) | 1 | 304 | Mean Difference (IV, Random, 95% CI) | ‐11.36 [‐14.67, ‐8.05] |
| 1.29.4 7 to 12 months ‐ European Quality of Life Visual Analog Scale at endpoint (low score=better) | 1 | 277 | Mean Difference (IV, Random, 95% CI) | ‐6.30 [‐23.41, 10.81] |
| 1.29.5 > 12 months ‐ Symptom Questionnaire of Kellner and Sheffield at endpoint (low score=better) | 1 | 18 | Mean Difference (IV, Random, 95% CI) | ‐4.90 [‐14.33, 4.53] |
| 1.30 Quality of life (across all scales and timepoints) Show forest plot | 7 | 1573 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.57, ‐0.07] |
| 1.31 Number of participants in employment Show forest plot | 3 | 593 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.82, 1.41] |
| 1.31.1 7 to 12 months | 2 | 259 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.75, 1.23] |
| 1.31.2 > 12 months | 1 | 334 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.97, 2.00] |
| 1.32 Social Functioning (various scales, different timepoints) Show forest plot | 15 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.32.1 up to 3 months ‐ Personal and Social Performance at endpoint (low score=better) | 2 | 379 | Mean Difference (IV, Random, 95% CI) | ‐5.66 [‐11.50, 0.18] |
| 1.32.2 up to 3 months ‐ Global Assessment Scale at endpoint (low score=better) | 1 | 120 | Mean Difference (IV, Random, 95% CI) | ‐3.61 [‐4.66, ‐2.56] |
| 1.32.3 4 to 6 months ‐ Sheehan Disability Schedule change from baseline to endpoint (low score=better) | 1 | 270 | Mean Difference (IV, Random, 95% CI) | ‐2.00 [‐3.60, ‐0.40] |
| 1.32.4 7 to 12 months ‐ Personal and Social Performance change from baseline to endpoint (low score=better) | 7 | 1823 | Mean Difference (IV, Random, 95% CI) | ‐4.92 [‐5.96, ‐3.89] |
| 1.32.5 7 to 12 months ‐ Global Assessment of Functioning at endpoint (low score=better) | 1 | 275 | Mean Difference (IV, Random, 95% CI) | ‐8.80 [‐13.22, ‐4.38] |
| 1.32.6 7 to 12 months ‐ Specific Levels of Functioning change from baseline to endpoint (low score=better) | 1 | 246 | Mean Difference (IV, Random, 95% CI) | ‐2.40 [‐4.85, 0.05] |
| 1.32.7 7 to 12 months ‐ Children Global Assessment Scale change from baseline to endpoint (low score=better) | 1 | 146 | Mean Difference (IV, Random, 95% CI) | ‐4.60 [‐9.84, 0.64] |
| 1.32.8 > 12 months ‐ Personal and Social Performance change from baseline to endpoint (low score=better) | 1 | 329 | Mean Difference (IV, Random, 95% CI) | ‐3.60 [‐6.76, ‐0.44] |
| 1.33 Social Functioning (across all scales and timepoints) Show forest plot | 15 | 3588 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.53, ‐0.34] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 2.1 Subgroup analysis: participants with a first episode Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.33, 0.46] |
| 2.1.1 first episode | 8 | 528 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.38, 0.58] |
| 2.1.2 not first episode | 24 | 3585 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.31, 0.46] |
| 2.2 Subgroup analysis: participants in remission at baseline Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.32, 0.46] |
| 2.2.1 in remission | 10 | 1050 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.33, 0.60] |
| 2.2.2 not in remission | 19 | 3063 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.30, 0.44] |
| 2.3 Subgroup analysis: various durations of stability before entering the study Show forest plot | 24 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.3.1 stable at least 1 month | 6 | 574 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.20, 0.50] |
| 2.3.2 stable at least 3 months | 10 | 2250 | Risk Ratio (M‐H, Random, 95% CI) | 0.34 [0.26, 0.43] |
| 2.3.3 stable at least 6 months | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 2.69] |
| 2.3.4 stable at least 12 months | 5 | 326 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.17, 0.57] |
| 2.3.5 stable at least 3 to 6 years | 2 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.38 [0.18, 0.78] |
| 2.4 Subgroup analysis: abrupt withdrawal versus tapering Show forest plot | 29 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.4.1 Abrupt withdrawal | 18 | 2348 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.35, 0.53] |
| 2.4.2 Taper | 11 | 1765 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.24, 0.44] |
| 2.5 Subgroup analysis: single antipsychotic drugs Show forest plot | 29 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.5.1 Chlorpromazine | 2 | 406 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.36, 0.55] |
| 2.5.2 Fluphenazine depot | 6 | 296 | Risk Ratio (M‐H, Random, 95% CI) | 0.23 [0.14, 0.39] |
| 2.5.3 Haloperidol depot | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 0.14 [0.04, 0.55] |
| 2.5.4 Various, mixed groups of antipsychotic drugs | 10 | 705 | Risk Ratio (M‐H, Random, 95% CI) | 0.42 [0.27, 0.65] |
| 2.5.5 Quetiapine | 1 | 178 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.34, 0.69] |
| 2.5.6 Paliperidone | 4 | 1256 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.31, 0.44] |
| 2.5.7 Aripiprazole | 2 | 549 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.14, 0.86] |
| 2.5.8 Brexpiprazole | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 0.36 [0.23, 0.56] |
| 2.5.9 Ziprasidone | 1 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.39, 0.64] |
| 2.5.10 Cariprazine | 1 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.38, 0.77] |
| 2.6 Subgroup analysis: depot versus oral drugs Show forest plot | 26 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.6.1 depot | 10 | 1705 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.23, 0.39] |
| 2.6.2 oral | 16 | 2187 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.38, 0.55] |
| 2.7 Subgroup analysis: first‐ versus second‐generation antipsychotic drugs Show forest plot | 29 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.7.1 First‐generation antipsychotic drugs | 18 | 1430 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.25, 0.48] |
| 2.7.2 Second‐generation antipsychotic drugs | 11 | 2683 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.32, 0.48] |
| 2.8 Subgroup analysis: appropriate versus unclear allocation concealment Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.32, 0.46] |
| 2.8.1 appropriate allocation concealment | 13 | 2708 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.30, 0.45] |
| 2.8.2 unclear allocation concealment | 16 | 1405 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.30, 0.54] |
| 2.9 Subgroup analysis: blinded versus open trials Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.32, 0.46] |
| 2.9.1 blinded trials | 27 | 3856 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.33, 0.48] |
| 2.9.2 unblinded trials | 2 | 257 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.17, 0.39] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 3.1 Exclusion of studies that were not explicitly described as randomised Show forest plot | 28 | 4098 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.33, 0.46] |
| 3.2 Exclusion of non‐double‐blind studies Show forest plot | 27 | 3856 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.33, 0.48] |
| 3.3 Fixed‐effects model Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.35, 0.41] |
| 3.4 Original authors' assumptions on dropouts Show forest plot | 29 | 4113 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.32, 0.46] |
| 3.5 Inclusion of only large studies (> 200 participants) Show forest plot | 10 | 2950 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.31, 0.45] |
| 3.6 Exclusion of studies with clinical diagnosis Show forest plot | 22 | 4054 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.34, 0.48] |
| 3.7 Three months stable Show forest plot | 29 | 4622 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.24, 0.42] |
| 3.8 Six months stable Show forest plot | 20 | 2549 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.20, 0.45] |
| 3.9 Nine months stable Show forest plot | 15 | 1806 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.19, 0.52] |
| 3.10 Exclusion of studies with unclear randomisation method Show forest plot | 11 | 2644 | Risk Ratio (IV, Random, 95% CI) | 0.36 [0.29, 0.43] |
| 3.11 Exclusion of studies with unclear allocation concealment method Show forest plot | 13 | 2708 | Risk Ratio (IV, Random, 95% CI) | 0.37 [0.30, 0.45] |