Closure methods of the appendix stump for complications during laparoscopic appendectomy
Information
- DOI:
- https://doi.org/10.1002/14651858.CD006437.pub3Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 13 November 2017see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Colorectal Group
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
Gurdeep S. Mannu coordinated all aspects of the review team and prepared the final manuscript.
Maria Sudul extracted data from published papers, entered data into Review Manager 5, helped carry out the analysis, and helped prepare the final review.
Joao H. Bettencourt‐Silva entered data into Review Manager 5 and helped carry out the analysis.
Elspeth Cumber and Fangfang Kate Li selected which trials were included/excluded and extracted data from included trials.
Allan B Clark provided statistical expertise.
Yoon K Loke helped interpret the analysis within the review and provided methodological expertise.
All review authors agreed on the final version of the manuscript for publication.
Sources of support
Internal sources
-
West China Hospital, Sichuan University, China.
External sources
-
No sources of support supplied
Declarations of interest
None known.
Acknowledgements
We would like to thank the Cochrane Colorectal Cancer Group, the CCCG Editorial Office, and Dr. Henning Keinke Andersen for assisting in development of the protocol, the review, and careful copy editing; Anne Sofie Christensen, who assisted in development of the protocol; Marija Barbateskovic, who developed the search strategies and ran the initial literature searches; and CCCG editors and peer referees Keith Chapple and Brett Doleman. We also would like to thank Nia Roberts, Outreach Librarian at the Bodliean Library, University of Oxford; and Sys Johnsen, Information Specialist at the Cochrane Colorectal Cancer Group; for updating the systematic search. We would like to acknowledge Stefan Sauerland and Geert Kazemier, who had the idea for the review; and Su Peng, Yao Chen, Jin Zhou, Yalin Zhang, Nansheng Cheng, Yun Liao, and Zong‐Guang Zhou, who drafted the review protocol. And finally Dolores Matheews from the Copy Edit Support team.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Nov 13 | Closure methods of the appendix stump for complications during laparoscopic appendectomy | Review | Gurdeep S Mannu, Maria K Sudul, Joao H Bettencourt‐Silva, Elspeth Cumber, Fangfang Li, Allan B Clark, Yoon K Loke | |
| 2012 Dec 12 | Appendix stump closure during laparoscopic appendectomy | Protocol | Su Peng, Yao Cheng, Yalin Zhang, Jin Zhou, Yun Liao, Nansheng Cheng, Geert Kazemier, Stefan Sauerland, Zong‐Guang Zhou | |
| 2007 Apr 18 | Appendix stump closure during laparoscopic appendectomy | Protocol | Stefan Sauerland, Geert Kazemier | |
Differences between protocol and review
We appropriately refined primary comparisons compared with those in the published protocol (Peng 2012) and followed results of the updated systematic search for 'mechanical devices compared to ligature devices' due to paucity of published research on different subtypes of mechanical devices, as discussed in Quality of the evidence and Implications for research. Furthermore, whereas the protocol specified the inclusion of all studies irrespective of length of publication, we decided that in cases when studies were reported solely in abstract form, we would include them in our quantitative synthesis only if full study data were made available to us. In preparation of this review, these refined inclusion criteria did not result in subsequent exclusion of any studies. In light of the type of outcome measures reported amongst included studies, we deemed Peto odds ratio (Peto OR) with 95% confidence intervals to be more appropriate for dichotomous outcomes when compared with relative risk estimates. However, we have presented the results of both in our sensitivity analysis.
Notes
None.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Abdominal Wound Closure Techniques [adverse effects, instrumentation];
- Appendectomy [*adverse effects];
- Appendix [*surgery];
- Intraoperative Complications [epidemiology, prevention & control];
- Laparoscopy;
- Length of Stay;
- Operative Time;
- Postoperative Complications [epidemiology, prevention & control];
- Randomized Controlled Trials as Topic;
- Surgical Instruments [adverse effects];
- Surgical Staplers [adverse effects];
- Sutures [adverse effects];
Medical Subject Headings Check Words
Humans;
PICOs

Data collection form (Microsoft Word).

*Lange 1993 was not retrievable following a worldwide search because the journal was published and is going out of print (see Results section).
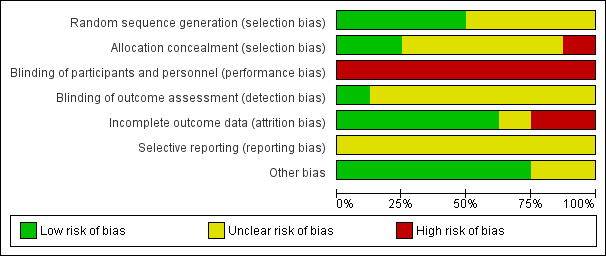
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
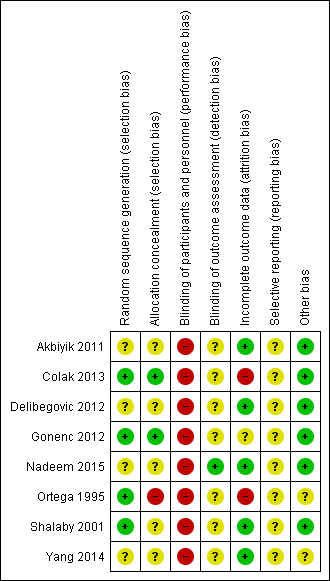
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 1 Total complications.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications.
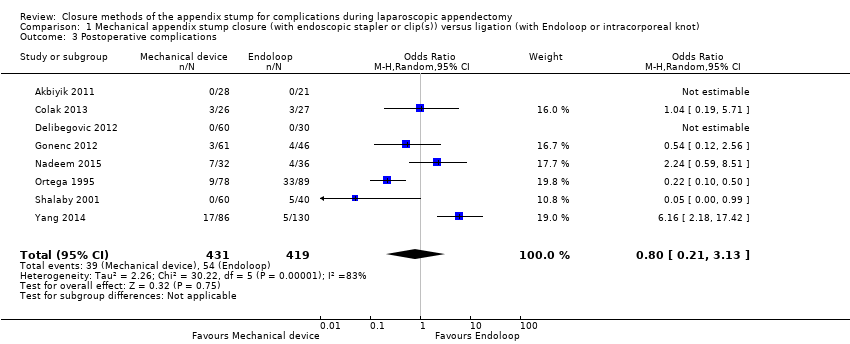
Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 3 Postoperative complications.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between mechanical device and ligature.
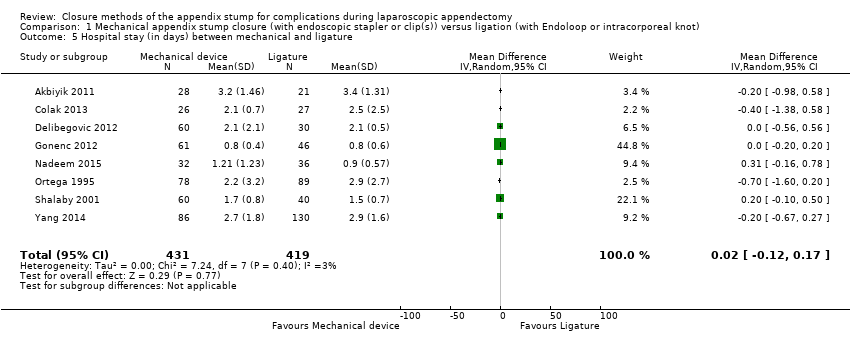
Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 5 Hospital stay (in days) between mechanical and ligature.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections.
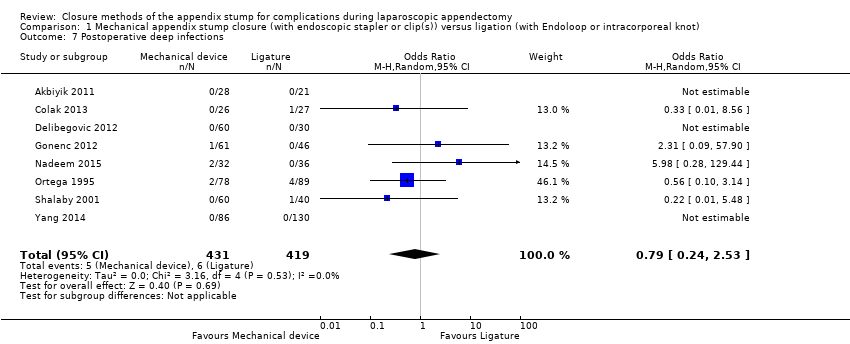
Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus.
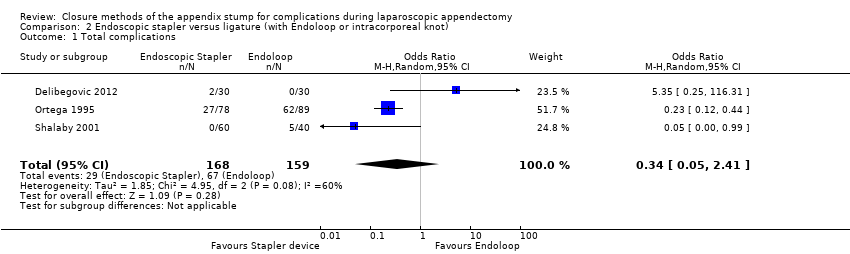
Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 1 Total complications.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 3 Postoperative complications.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between stapler and ligature.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 5 Comparison of hospital stay between stapler and ligature.
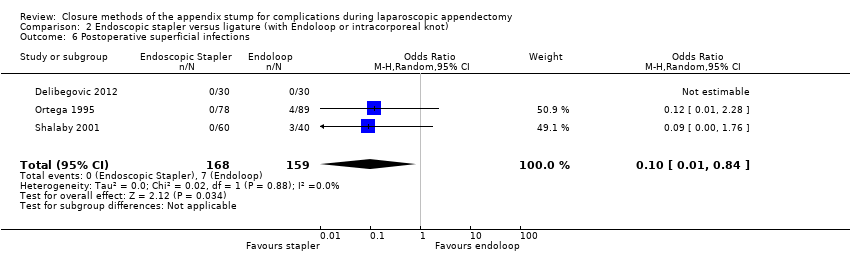
Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections.
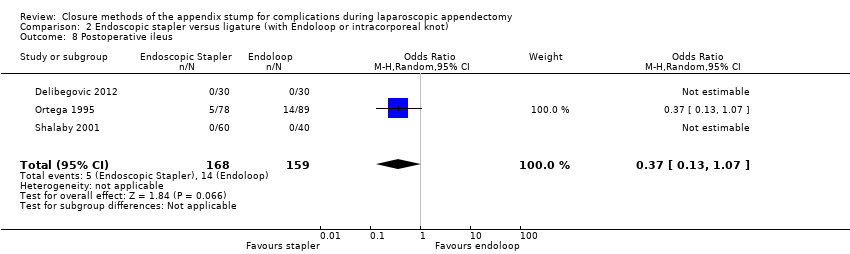
Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 1 Total complications.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications.
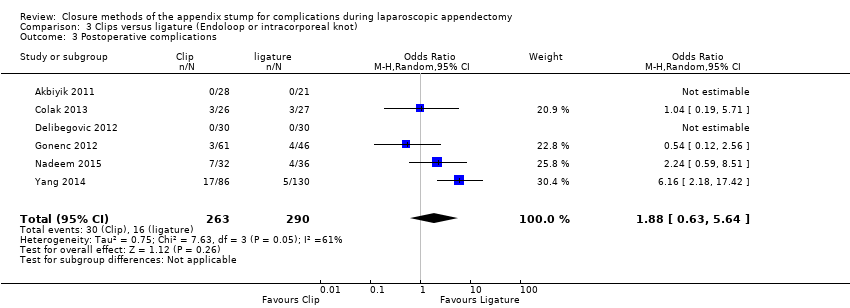
Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 3 Postoperative complications.
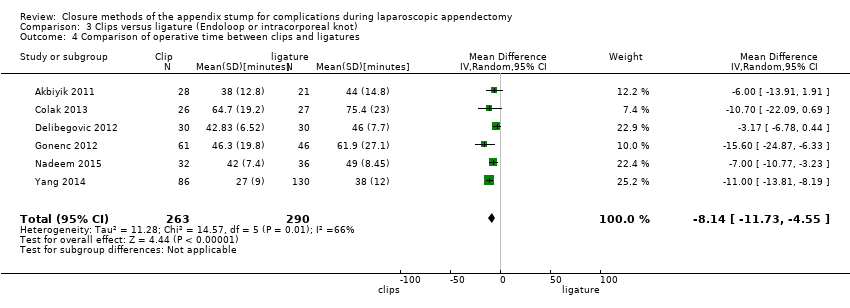
Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between clips and ligatures.
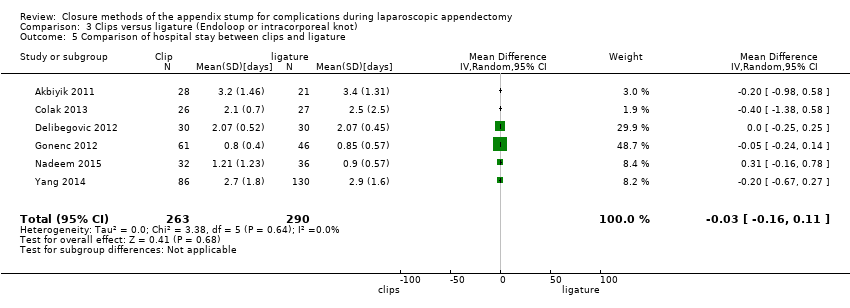
Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 5 Comparison of hospital stay between clips and ligature.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus.

Comparison 4 Endoscopic stapler versus clips, Outcome 1 Total complications.

Comparison 4 Endoscopic stapler versus clips, Outcome 2 Intraoperative complications.

Comparison 4 Endoscopic stapler versus clips, Outcome 3 Postoperative complications.

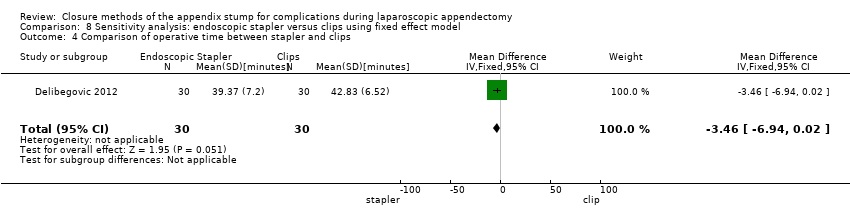
Comparison 4 Endoscopic stapler versus clips, Outcome 4 Comparison of operative time between stapler and clips.
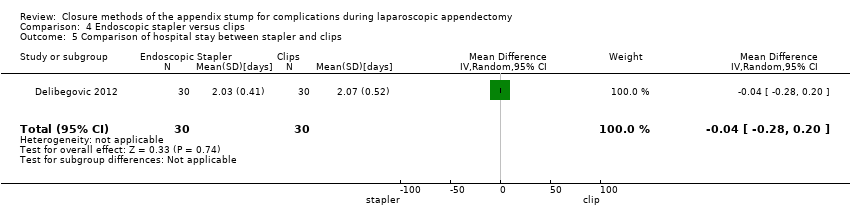
Comparison 4 Endoscopic stapler versus clips, Outcome 5 Comparison of hospital stay between stapler and clips.

Comparison 4 Endoscopic stapler versus clips, Outcome 6 Postoperative superficial infections.

Comparison 4 Endoscopic stapler versus clips, Outcome 7 Postoperative deep infections.
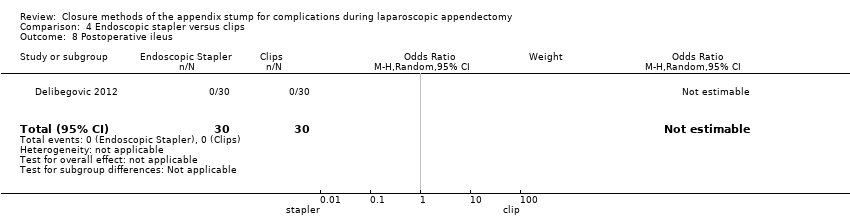
Comparison 4 Endoscopic stapler versus clips, Outcome 8 Postoperative ileus.
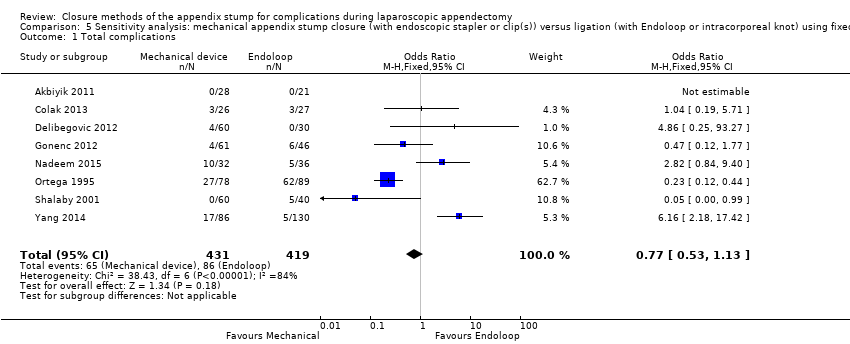
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications.
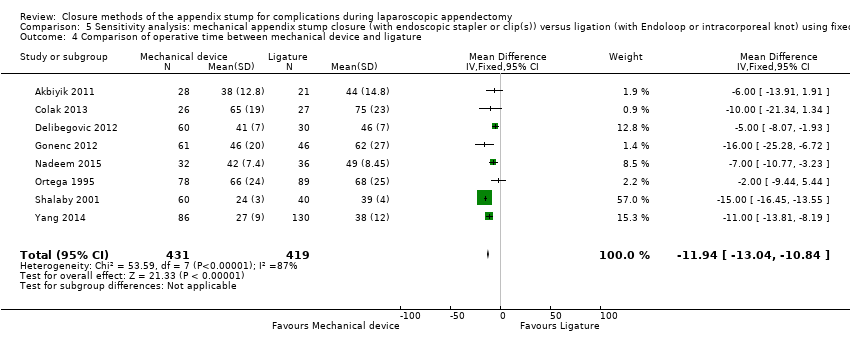
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between mechanical device and ligature.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Hospital stay (in days) between mechanical device and ligature.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections.
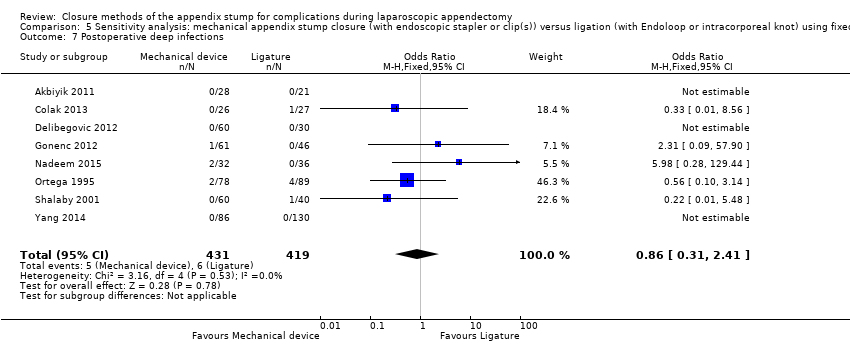
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections.
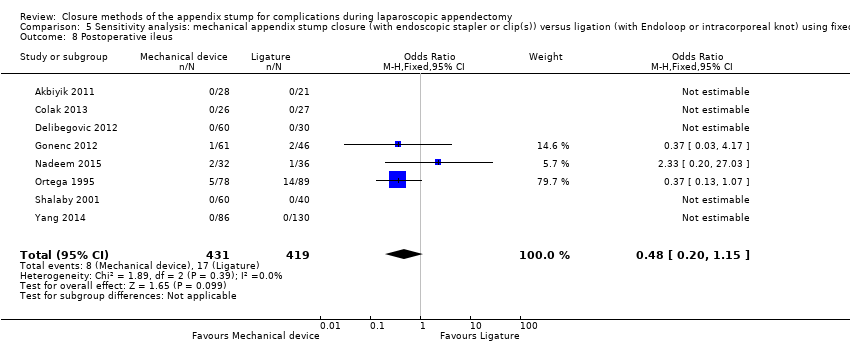
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications.
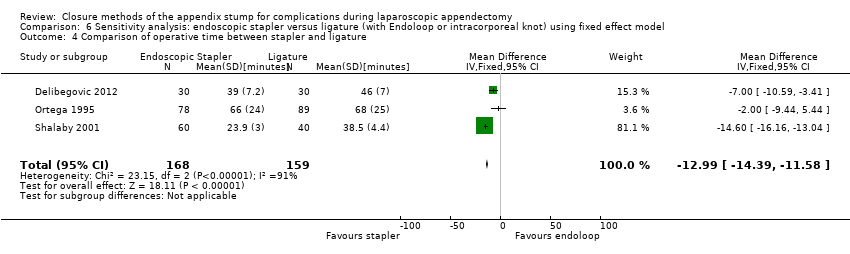
Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between stapler and ligature.
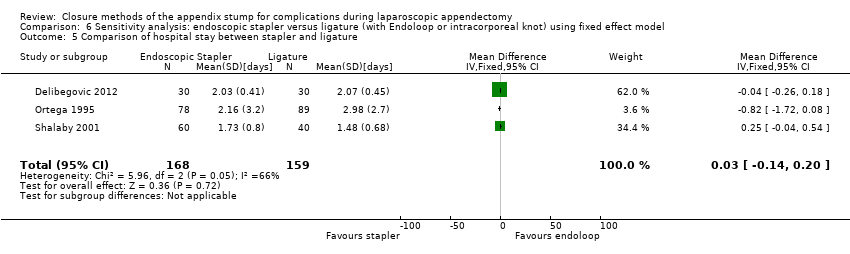
Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Comparison of hospital stay between stapler and ligature.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus.
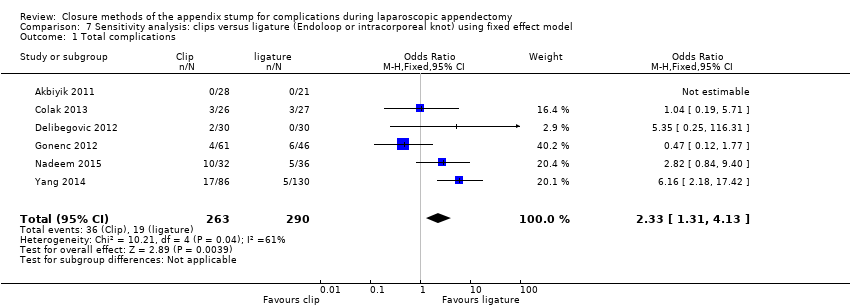
Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications.
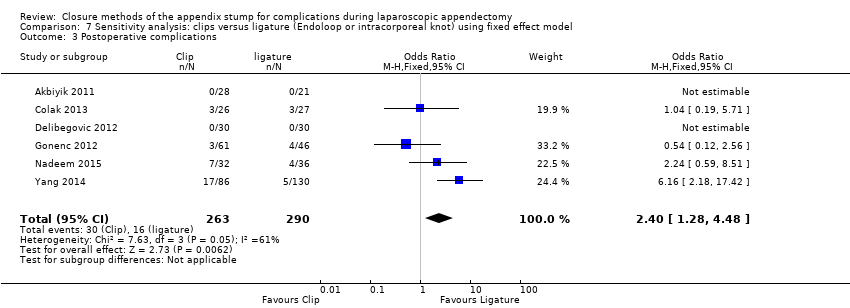
Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between clips and ligature.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Comparison of hospital stay between clips and ligature.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections.
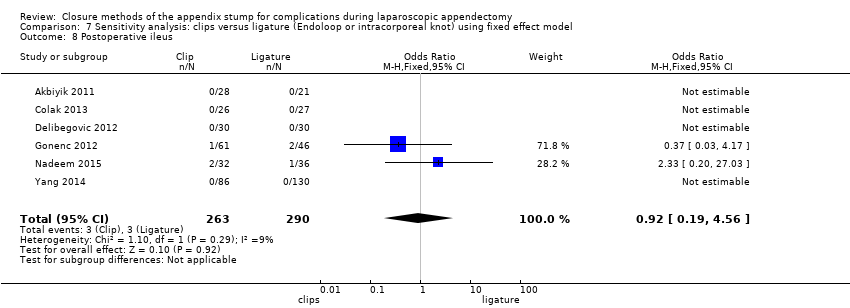
Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 1 Total complications.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 2 Intraoperative complications.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 3 Postoperative complications.
Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 4 Comparison of operative time between stapler and clips.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 5 Comparison of hospital stay between stapler and clips.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 6 Postoperative superficial infections.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 7 Postoperative deep infections.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 8 Postoperative ileus.
| Mechanical devices vs ligatures for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligatures | Risk with mechanical devices | ||||
| Total complications | 205 per 1000 | 169 per 1000 | OR 0.97 (0.27 to 3.50) | 850 | ⊕⊝⊝⊝ |
| Intraoperative complications | 76 per 1000 | 63 per 1000 | OR 0.93 (0.34 to 2.55) | 850 | ⊕⊝⊝⊝ |
| Postoperative complications | 129 per 1000 | 109 per 1000 | OR 0.80 (0.21 to 3.13) | 850 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 26 per 1000 | 13 per 1000 | OR 0.58 | 850 | ⊕⊝⊝⊝ |
| Postoperative ileus | 41 per 1000 | 20 per 1000 | OR 0.47 | 850 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 14 per 1000 | 12 per 1000 | OR 0.79 | 850 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.6 minutes. | Mean operative time (minutes) in the intervention group was 9.04 minutes shorter (12.97 minutes shorter to 5.11 minutes shorter). | ‐ | 850 | ⊕⊝⊝⊝ |
| Hospital stay (days) | Mean hospital stay was 1.4 days. | Mean hospital stay in the intervention group was 0.02 days longer (0.12 days shorter to 0.17 days longer). | ‐ | 850 | ⊕⊝⊝⊝ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Endoscopic stapler vs ligature for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: endoscopic stapler Comparison: ligature | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligature | Risk with endoscopic stapler | ||||
| Total complications | 421 per 1000 | 198 per 1000 | OR 0.34 (0.05 to 2.41) | 327 | ⊕⊝⊝⊝ |
| Intraoperative complications | 182 per 1000 | 191 per 1000 | OR 1.06 (0.17 to 6.70) | 327 | ⊕⊝⊝⊝ |
| Postoperative complications | 239 per 1000 | 250 per 1000 | OR 0.20 (0.09 to 0.44) | 327 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 44 per 1000 | 47 per 1000 | OR 0.10 (0.01 to 0.84) | 327 | ⊕⊝⊝⊝ |
| Postoperative ileus | 88 per 1000 | 93 per 1000 | OR 0.37 (0.13 to 1.07) | 327 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 31 per 1000 | 33 per 1000 | OR 0.45 (0.10 to 2.08) | 327 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.6 minutes. | Mean operative time in the intervention group was 8.52 minutes lower (15.64 minutes shorter to 1.39 minutes shorter). | 327 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 1.9 days. | Mean hospital stay in the intervention group was 0.02 days longer (0.38 days shorter to 0.34 days longer). | 327 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Clips vs ligatures for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: clips Comparison: ligature | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligature | Risk with clips | ||||
| Total complications | 17 per 1000 | 18 per 1000 | OR 2.03 (0.71 to 5.84) | 553 | ⊕⊝⊝⊝ |
| Intraoperative complications | 21 per 1000 | 22 per 1000 | OR 1.74 (0.33 to 9.04) | 553 | ⊕⊝⊝⊝ |
| Postoperative complications | 17 per 1000 | 18 per 1000 | OR 1.88 (0.63 to 5.64) | 553 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 14 per 1000 | 15 per 1000 | OR 1.25 (0.32 to 4.90) | 553 | ⊕⊝⊝⊝ |
| Postoperative ileus | 10 per 1000 | 11 per 1000 | OR 0.92 (0.15 to 5.64) | 553 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 3 per 1000 | 4 per 1000 | OR 1.75 (0.28 to 10.93) | 553 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.0 minutes. | Mean operative time in the intervention group was 8.14 minutes shorter (11.73 minutes shorter to 4.55 minutes shorter). | 553 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 1.5 days. | Mean hospital stay in the intervention group was 0.03 days shorter (0.16 days shorter to 0.11 days longer). | 553 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Endoscopic stapler vs clips for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: endoscopic stapler Comparison: clips | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with clips | Risk with endoscopic stapler | ||||
| Total complications | 67 per 1000 | 70 per 1000 | OR 1.00 (0.13 to 7.60) | 60 | ⊕⊝⊝⊝ |
| Intraoperative complications | 67 per 1000 | 70 per 1000 | OR 1.00 (0.13 to 7.60) | [60 | ⊕⊝⊝⊝ |
| Postoperative complications | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative superficial infections | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative ileus | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative deep infections | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Operative time (minutes) | Mean operative time was 39.4 minutes. | Mean operative time in the intervention group was 3.46 minutes shorter (6.94 minutes shorter to 0.02 minutes longer). | 60 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 2.0 days. | Mean hospital stay in the intervention group was 0.04 days shorter (0.28 days shorter to 0.20 days longer). | 60 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for single study with limited sample size. bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (the sole included studies had few participants and therefore few events, resulting in wide confidence intervals, which limited the precision of estimates). | |||||
| Study ID | Intervention arms | Total no. with complications | Total no. without complications | Intraoperative | Postoperative | |||||||||||
| Bleeding | Intraoperative rupture of appendix | Intraoperative organ injury/ faecal soiling | Access‐related visceral injury | Other | Total | Surgical site infection (superficial) | Deep infection | Bleeding | Paralytic ileus | Purulent peritonitis | Other | Total | ||||
| Ortega 1995 | Endoscopic linear stapler (LAS) | 27 | 51 | 11 | 2 | 5 | 0 | 0 | 18 | 0 | 2 | 0 | 5 | 0 | 2a | 9 |
| 2× catgut ligatures (Endoloops) (LAL) | 62 | 27 | 14 | 4 | 11 | 0 | 0 | 29 | 4 | 4 | 0 | 14 | 0 | 11b | 33 | |
| Open appendectomy (OA) | 44 | 42 | 20 | 5 | 1 | 0 | 0 | 26 | 11 | 0 | 0 | 6 | 0 | 1c | 18 | |
| Akbiyik 2011 | Hem‐o‐lok clip (non‐absorbable polymeric clips) | 0 | 28 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ligaure (Endoloop) | 0 | 21 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Delibegovic 2012 | 45‐mm stapler | 2 | 28 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1 ligature (Endoloop) | 0 | 30 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 1 Hem‐o‐lok clip (non‐absorbable polymeric clips) | 2 | 28 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Beldi 2004 | 1 ligature (Endoloop) only at appendix base (1 other at 6 to 12 mm distally) | 5 | 104 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 2d | 5 |
| 2 ligatures (Endoloops) at base of appendix (1 other at 6 to 12 mm distally) | 5 | 94 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 1e | 5 | |
| Sucullu 2009 | Endodissector and endoclip | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| LigaSure 5 to 10 mm | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Shalaby 2001 | Endo GIA (Ethicon Endo‐Surgery, Cincinnati, Ohio, USA) stapler | 0 | 60 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ligature (Endoloop) | 5 | 35 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 0 | 0 | 0 | 1f | 5 | |
| Extracorporeal laparoscopically assisted appendectomy | 6 | 44 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 4 | |
| Colak 2013 | Hem‐o‐lok (non‐absorbable polymeric clips) | 3 | 23 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 1g | 3 |
| Ligature (Endoloop) | 3 | 24 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1g | 3 | |
| Gonenc 2012 | Titanium endoclip | 4 | 57 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 3 |
| Intracorporeal knotting | 6 | 40 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 2 | 1 | 0 | 4 | |
| Ates 2012 | Titanium endoclip | 8 | 22 | NS | NS | NS | NS | 1h | 7 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Intracorporeal knotting | 7 | 24 | NS | NS | NS | NS | 0 | 4 | 1 | 0 | 0 | 0 | 0 | 2i | 3 | |
| Yang 2014 | Intracorporeal knotting | 5 | 125 | 0 | NS | NS | NS | NS | 0 | NS | 0 | NS | NS | NS | 5j | 5 |
| Titanium hem‐o‐lok | 17 | 69 | 0 | NS | NS | NS | NS | 0 | NS | 0 | NS | NS | NS | 17k | 17 | |
| Nadeem 2015 | Extracorporeal knotting | 5 | 31 | 1 | NS | 0 | NS | NS | 1 | 2 | 0 | NS | 1 | NS | 1 | 4 |
| Metallic endoclip | 10 | 22 | 2 | NS | 1 | NS | NS | 3 | 2 | 2 | NS | 2 | NS | 1l | 7 | |
| NS: non‐significant. | ||||||||||||||||
| Mechanical appendix stump closure (with endoscopic stapler or clip(s)) vs ligation (with Endoloop or intra/extracorporeal knot) | |||||||||
| Odds ratio (95% CI) | Risk ratio (95% CI) | Risk difference (95% CI) | Mean difference (95% CI) | ||||||
| Outcome | Fixed effect | Random effects | Fixed effect | Random effects | Fixed effect | Random effects | Fixed effect | Random effects | |
| Total complications | 0.77 (0.53 to 1.13) | 0.97 (0.27 to 3.50) | 0.83 (0.64 to 1.08) | 1.09 (0.41 to 2.88) | ‐0.03 (‐0.08 to 0.01) | ‐0.02 (‐0.12 to 0.09) | ‐ | ‐ | |
| Intraoperative complications | 0.81 (0.45 to 1.46) | 0.93 (0.34 to 2.55) | 0.85 (0.53 to 1.35) | 0.93 (0.40 to 2.18) | ‐0.01 (‐0.04 to 0.02) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative complications | 0.80 (0.52 to 1.24) | 0.80 (0.21 to 3.13) | 0.83 (0.57 to 1.19) | 0.86 (0.27 to 2.74) | ‐0.02 (‐0.06 to 0.02) | ‐0.02 (‐0.10 to 0.06) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐11.94 (‐13.04 to ‐10.84) | ‐9.04 (‐12.97 to ‐5.11) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.02 (‐0.12 to 0.16) | 0.02 (‐0.12 to 0.17) | |
| Postoperative superficial infections | 0.47 (0.17 to 1.26) | 0.58 (0.18 to 1.93) | 0.48 (0.19 to 1.24) | 0.61 (0.19 to 1.93) | ‐0.02 (‐0.04 to 0.01) | ‐0.01 (‐0.02 to 0.01) | ‐ | ‐ | |
| Postoperative ileus | 0.48 (0.20 to 1.15) | 0.47 (0.19 to 1.18) | 0.51 (0.23 to 1.14) | 0.50 (0.22 to 1.17) | ‐0.02 (‐0.04 to 0.01) | ‐0.01 (‐0.03 to 0.02) | ‐ | ‐ | |
| Postoperative deep infections | 0.86 (0.31 to 2.41) | 0.79 (0.24 to 2.53) | 0.87 (0.32 to 2.35) | 0.79 (0.25 to 2.47) | ‐0.00 (‐0.02 to 0.02) | ‐0.00 (‐0.02 to 0.01) | ‐ | ‐ | |
| Endoscopic stapler vs ligature | |||||||||
| Total complications | 0.26 (0.14 to 0.46) | 0.34 (0.05 to 2.41) | 0.49 (0.35 to 0.68) | 0.51 (0.09 to 2.84) | ‐0.21 (‐0.29 to ‐0.12) | ‐0.13 (‐0.40 to 0.14) | ‐ | ‐ | |
| Intraoperative complications | 0.72 (0.38 to 1.39) | 1.06 (0.17 to 6.70) | 0.79 (0.48 to 1.28) | 1.07 (0.22 to 5.19) | ‐0.04 (‐0.11 to 0.04) | ‐0.00 (‐0.11 to 0.10) | ‐ | ‐ | |
| Postoperative complications | 0.19 (0.09 to 0.41) | 0.20 (0.09 to 0.44) | 0.27 (0.14 to 0.51) | 0.25 (0.08 to 0.75) | ‐0.17 (‐0.24 to ‐0.10) | ‐0.12 (‐0.34 to 0.09) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐12.94 (‐14.35 to ‐11.53) | ‐8.36 (‐15.68 to ‐1.03) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.03 (‐0.14 to 0.20) | ‐0.02 (‐0.38 to 0.34) | |
| Postoperative superficial infections | 0.10 (0.01 to 0.86) | 0.10 (0.01 to 0.84) | 0.11 (0.01 to 0.88) | 0.11 (0.01 to 0.87) | ‐0.05 (‐0.08 to ‐0.01) | ‐0.04 (‐0.08 to 0.00) | ‐ | ‐ | |
| Postoperative ileus | 0.37 (0.13 to 1.07) | 0.37 (0.13 to 1.07) | 0.41 (0.15 to 1.08) | 0.41 (0.15 to 1.08) | ‐0.05 (‐0.10 to 0.00) | ‐0.02 ( ‐0.10 to 0.05) | ‐ | ‐ | |
| Postoperative deep infections | 0.45 (0.10 to 2.02) | 0.45 (0.10 to 2.08) | 0.46 (0.11 to 1.95) | 0.47 (0.11 to 2.04) | ‐0.02 (‐0.05 to 0.02) | ‐0.02 (‐0.05 to 0.02) | ‐ | ‐ | |
| Endoscopic stapler vs clips | |||||||||
| Total complications | 1.00 (0.13 to 7.60) | 1.00 (0.13 to 7.60) | 1.00 (0.15 to 6.64) | 1.00 (0.15 to 6.64) | 0.00 (‐0.13 to 0.13) | 0.00 (‐0.13 to 0.13) | ‐ | ‐ | |
| Intraoperative complications | 1.00 (0.13 to 7.60) | 1.00 (0.13 to 7.60) | 1.00 (0.15 to 6.64) | 1.00 (0.15 to 6.64) | 0.00 (‐0.13 to 0.13) | 0.00 (‐0.13 to 0.13) | ‐ | ‐ | |
| Postoperative complications | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐3.46 (‐6.94 to 0.02) | ‐3.46 (‐6.94 to 0.02) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.04 (‐0.28 to 0.20) | ‐0.04 [‐0.28, 0.20] | |
| Postoperative superficial infections | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Postoperative ileus | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Postoperative deep infections | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Clips vs ligature (Endoloop and intra/extracorporeal knot) | |||||||||
| Total complications | 2.33 (1.31 to 4.13) | 2.03 (0.71 to 5.84) | 2.11 (1.29 to 3.47) | 1.84 (0.73 to 4.62) | 0.08 (0.03 to 0.13) | 0.05 (‐0.03 to 0.13) | ‐ | ‐ | |
| Intraoperative complications | 1.79 (0.49 to 6.56) | 1.74 (0.33 to 9.04) | 1.76 (0.51 to 6.01) | 1.69 (0.35 to 8.19) | 0.01 (‐0.02 to 0.04) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative complications | 2.40 (1.28 to 4.48) | 1.88 (0.63 to 5.64) | 2.20 (1.27 to 3.82) | 1.75 (0.66 to 4.61) | 0.07 (0.02 to 0.12) | 0.03 (‐0.04 to 0.11) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐8.06 (‐9.85 to ‐6.26) | ‐8.14 (‐11.73 to ‐4.55) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.03 (‐0.16 to 0.11) | ‐0.03 (‐0.16 to 0.11) | |
| Postoperative superficial infections | 1.27 (0.33 to 4.86) | 1.25 (0.32 to 4.90) | 1.25 (0.35 to 4.49) | 1.24 (0.34 to 4.56) | 0.00 (‐0.02 to 0.03) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative ileus | 0.92 (0.19 to 4.56) | 0.92 (0.15 to 5.64) | 0.92 (0.20 to 4.21) | 0.93 (0.16 to 5.33) | ‐0.00 (‐0.02 to 0.02) | ‐0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative deep infections | 1.79 (0.37 to 8.58) | 1.75 (0.28 to 10.93) | 1.77 (0.38 to 8.16) | 1.71 (0.28 to 10.28) | 0.01 (‐0.02 to 0.03) | 0.00 (‐0.01 to 0.02) | ‐ | ‐ | |
| CI: confidence interval; NE: not estimable; "‐": not applicable. | |||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.97 [0.27, 3.50] |
| 2 Intraoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.93 [0.34, 2.55] |
| 3 Postoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.80 [0.21, 3.13] |
| 4 Comparison of operative time between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Random, 95% CI) | ‐9.04 [‐12.97, ‐5.11] |
| 5 Hospital stay (in days) between mechanical and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.12, 0.17] |
| 6 Postoperative superficial infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.18, 1.93] |
| 7 Postoperative deep infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.79 [0.24, 2.53] |
| 8 Postoperative ileus Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.47 [0.19, 1.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.34 [0.05, 2.41] |
| 2 Intraoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 1.06 [0.17, 6.70] |
| 3 Postoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.20 [0.09, 0.44] |
| 4 Comparison of operative time between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Random, 95% CI) | ‐8.52 [‐15.64, ‐1.39] |
| 5 Comparison of hospital stay between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.38, 0.34] |
| 6 Postoperative superficial infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.10 [0.01, 0.84] |
| 7 Postoperative deep infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.45 [0.10, 2.08] |
| 8 Postoperative ileus Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.37 [0.13, 1.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 2.03 [0.71, 5.84] |
| 2 Intraoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.74 [0.33, 9.04] |
| 3 Postoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.88 [0.63, 5.64] |
| 4 Comparison of operative time between clips and ligatures Show forest plot | 6 | 553 | Mean Difference (IV, Random, 95% CI) | ‐8.14 [‐11.73, ‐4.55] |
| 5 Comparison of hospital stay between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.16, 0.11] |
| 6 Postoperative superficial infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.25 [0.32, 4.90] |
| 7 Postoperative deep infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.75 [0.28, 10.93] |
| 8 Postoperative ileus Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.15, 5.64] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 1.0 [0.13, 7.60] |
| 2 Intraoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 1.0 [0.13, 7.60] |
| 3 Postoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Comparison of operative time between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐3.46 [‐6.94, 0.02] |
| 5 Comparison of hospital stay between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.28, 0.20] |
| 6 Postoperative superficial infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Postoperative deep infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Postoperative ileus Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.53, 1.13] |
| 2 Intraoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.45, 1.46] |
| 3 Postoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.52, 1.24] |
| 4 Comparison of operative time between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Fixed, 95% CI) | ‐11.94 [‐13.04, ‐10.84] |
| 5 Hospital stay (in days) between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.12, 0.16] |
| 6 Postoperative superficial infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.17, 1.26] |
| 7 Postoperative deep infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.31, 2.41] |
| 8 Postoperative ileus Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.20, 1.15] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.14, 0.46] |
| 2 Intraoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.38, 1.39] |
| 3 Postoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.09, 0.41] |
| 4 Comparison of operative time between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Fixed, 95% CI) | ‐12.99 [‐14.39, ‐11.58] |
| 5 Comparison of hospital stay between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.14, 0.20] |
| 6 Postoperative superficial infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 0.86] |
| 7 Postoperative deep infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.10, 2.02] |
| 8 Postoperative ileus Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.13, 1.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.33 [1.31, 4.13] |
| 2 Intraoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.49, 6.56] |
| 3 Postoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.40 [1.28, 4.48] |
| 4 Comparison of operative time between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Fixed, 95% CI) | ‐8.06 [‐9.85, ‐6.26] |
| 5 Comparison of hospital stay between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.16, 0.11] |
| 6 Postoperative superficial infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.33, 4.86] |
| 7 Postoperative deep infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.37, 8.58] |
| 8 Postoperative ileus Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.19, 4.56] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.13, 7.60] |
| 2 Intraoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.13, 7.60] |
| 3 Postoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Comparison of operative time between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐3.46 [‐6.94, 0.02] |
| 5 Comparison of hospital stay between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.28, 0.20] |
| 6 Postoperative superficial infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Postoperative deep infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Postoperative ileus Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

