Métodos de cierre del muñón apendicular para complicaciones durante la apendicectomía laparoscópica
Resumen
Antecedentes
La apendicectomía laparoscópica es una de las intervenciones quirúrgicas generales más habituales en el mundo desarrollado. Podría decirse que la parte más crítica de esta intervención es el cierre efectivo del muñón apendicular para prevenir complicaciones intrabdominales catastróficas provocadas por una fuga fecal a la cavidad abdominal.
En todo el mundo se utilizan diferentes métodos de cierre del muñón apendicular; estos pueden dividirse ampliamente en ligaduras tradicionales (como las ligaduras intracorpóreas o extracorpóreas o nudos de Roeder) y dispositivos mecánicos (como grapadoras, clips o dispositivos electrotérmicos). Sin embargo, el método óptimo continúa siendo incierto.
Objetivos
Comparar todas las técnicas quirúrgicas utilizadas actualmente para el cierre del muñón apendicular durante la apendicectomía laparoscópica.
Métodos de búsqueda
En junio 2017, se hicieron búsquedas en el Registro Cochrane Central de Ensayos Controlados (Cochrane Central Register of Controlled Trials) (CENTRAL; 2017, número 6) en la Cochrane Library, MEDLINE Ovid (1946 hasta 14 junio 2017), Embase Ovid (1974 hasta 14 junio 2017), Science Citation Index ‐ Expanded (14 junio 2017), China Biological Medicine Database (CBM), el World Health Organization International Trials Registry Platform search portal, ClinicalTrials.gov, Current Controlled Trials, el Chinese Clinical Trials Register, y en el EU Clinical Trials Register (todos en junio 2017). Se realizaron búsquedas en las listas de referencias de publicaciones relevantes, así como en resúmenes de reuniones y en Conference Proceedings Citation Index para buscar ensayos clínicos relevantes adicionales.
Criterios de selección
Se incluyeron todos los ensayos controlados con asignación aleatoria (ECA) que compararan el cierre mecánico del muñón apendicular (grapadora, clips o dispositivos electrotérmicos) versus ligadura (Endoloop, nudo de Roeder o técnicas de nudo intracorpóreo) para la apendicitis no complicada.
Obtención y análisis de los datos
Dos autores de la revisión identificaron los ensayos para la inclusión, recopilaron los datos y evaluaron el riesgo de sesgo de forma independiente. Se realizó el metanálisis utilizando Review Manager 5. Se calculó el cociente de riesgos (CR) para los resultados dicotómicos y la diferencia de medias (DM) para los resultados continuos con intervalos de confianza (IC) del 95%.
Resultados principales
Se incluyeron ocho estudios aleatorios con 850 participantes. Cinco estudios compararon los clips de titanio versus la ligadura, dos estudios compararon una grapadora endoscópica versus la ligadura y un estudio comparó una grapadora endoscópica, clips de titanio y la ligadura. En este análisis de resultados principales, no se hallaron diferencias en las complicaciones totales (OR 0,97; IC del 95%: 0,27 a 3,50; ocho ECA, evidencia de calidad muy baja), las complicaciones intraoperatorias (OR 0,93; IC del 95%: 0,34 a 2,55; ocho ECA, evidencia de calidad muy baja) ni en las complicaciones posoperatorias (OR 0,80; IC del 95%: 0,21 a 3,13; ocho ECA, evidencia de calidad muy baja) entre la ligadura y todos los tipos de dispositivos mecánicos. Sin embargo, los análisis de resultados secundarios muestran que el uso de dispositivos mecánicos ahorraron aproximadamente nueve minutos del tiempo total de operación al compararlo con el uso de la ligadura (diferencia de medias (DM) ‐9,04 minutos; IC del 95%: ‐12,97 a ‐5,11 minutos; ocho ECA, evidencia de muy baja calidad). No obstante estos hallazgos no se tradujeron en una reducción estadísticamente ni clínicamente significativa en la estancia hospitalaria (DM 0,02 días; IC del 95%: ‐0,12 a 0,17 días; ocho ECA, evidencia de muy baja calidad). La información disponible no fue suficiente para realizar una comparación fiable entre ambas estrategias con respecto a los costes totales hospitalarios y el dolor y la calidad de vida posoperatorios. En general, la evidencia en todos los análisis fue de calidad muy baja, con un importante potencial de factores de confusión. Dadas las limitaciones de todos los estudios en términos de sesgo y dada la baja calidad de la evidencia disponible, no es posible concluir claramente la superioridad de un dispositivo mecánico en concreto con respecto a otro.
Conclusiones de los autores
Actualmente no existe suficiente evidencia para abogar por la omisión del cierre del muñón apendicular basado en la ligadura convencional en favor de un de dispositivo mecánico concreto sobre otro en la apendicitis no complicada.
PICOs
Resumen en términos sencillos
Determinar el método óptimo para cerrar de forma segura la base del apéndice durante la cirugía laparoscópica tras la extracción del apéndice inflamado
Antecedentes
La apendicitis es una inflamación del apéndice. El tratamiento convencional para esta afección implica una operación para extraer el apéndice, llamada apendicectomía. En los últimos años, esta operación se ha realizado cada vez más mediante una apendicectomía laparoscópica o cirugía de ojo de cerradura. En la extracción del apéndice durante una apendicectomía laparoscópica, no está claro cuál es el mejor método de cierre del muñón apendicular restante para evitar una fuga del contenido intestinal. Las estrategias tradicionales han implicado las ligaduras y los nudos. Sin embargo, en los últimos años, algunos cirujanos han escogido utilizar dispositivos mecánicos automatizados en lugar de ligaduras y no está claro si estos dispositivos reducen las complicaciones durante la apendicectomía laparoscópica al compararlos con las ligaduras.
Características de los estudios
Se buscaron todos los ensayos controlados aleatorios relevantes hasta el 14 de junio de 2017. Esta revisión sistemática incluyó ocho ensayos controlados aleatorios que incluyeron un total de 850 participantes. Todos los ensayos compararon dispositivos mecánicos versus ligaduras para el cierre del muñón apendicular. Cinco de los ocho ensayos compararon el uso de clips versus ligadura, dos ensayos compararon una grapadora automatizada versus ligadura y un ensayo comparó los tres métodos.
Resultados clave
El uso de dispositivos mecánicos para cerrar el muñón apendicular durante la apendicectomía laparoscópica no supuso una diferencia significativa en la tasa de complicaciones globales al compararlo con el uso de la ligadura, ni tampoco en la tasa de complicaciones ocurridas durante o después de la apendicectomía. No obstante, los dispositivos mecánicos sí que redujeron la duración de la operación en nueve minutos al compararlos con las ligaduras. Los dispositivos mecánicos no supusieron una diferencia importante en la estancia hospitalaria global. No hubo suficiente información para evaluar de forma fiable los costes hospitalarios, el dolor ni la calidad de vida para ninguna de las comparaciones. Como resultado, no se ha hallado suficiente evidencia en este momento para recomendar firmemente ningún método sobre otro. Deben realizarse más estudios para comparar mejor los nuevos métodos disponibles.
Calidad de la evidencia
La evidencia utilizada para extraer las conclusiones fue, por lo general, de calidad baja. Los estudios incluidos para cada análisis fueron vulnerables a diferentes tipos de sesgo y contenían inconsistencias e imprecisión en sus resultados debido al bajo número de participantes y eventos en cada grupo de estudio incluido. Es probable que la investigación futura cambie sustancialmente las conclusiones; se necesitan más estudios en este campo.
Conclusiones de los autores
Summary of findings
| Mechanical devices vs ligatures for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligatures | Risk with mechanical devices | ||||
| Total complications | 205 per 1000 | 169 per 1000 | OR 0.97 (0.27 to 3.50) | 850 | ⊕⊝⊝⊝ |
| Intraoperative complications | 76 per 1000 | 63 per 1000 | OR 0.93 (0.34 to 2.55) | 850 | ⊕⊝⊝⊝ |
| Postoperative complications | 129 per 1000 | 109 per 1000 | OR 0.80 (0.21 to 3.13) | 850 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 26 per 1000 | 13 per 1000 | OR 0.58 | 850 | ⊕⊝⊝⊝ |
| Postoperative ileus | 41 per 1000 | 20 per 1000 | OR 0.47 | 850 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 14 per 1000 | 12 per 1000 | OR 0.79 | 850 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.6 minutes. | Mean operative time (minutes) in the intervention group was 9.04 minutes shorter (12.97 minutes shorter to 5.11 minutes shorter). | ‐ | 850 | ⊕⊝⊝⊝ |
| Hospital stay (days) | Mean hospital stay was 1.4 days. | Mean hospital stay in the intervention group was 0.02 days longer (0.12 days shorter to 0.17 days longer). | ‐ | 850 | ⊕⊝⊝⊝ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Endoscopic stapler vs ligature for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: endoscopic stapler Comparison: ligature | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligature | Risk with endoscopic stapler | ||||
| Total complications | 421 per 1000 | 198 per 1000 | OR 0.34 (0.05 to 2.41) | 327 | ⊕⊝⊝⊝ |
| Intraoperative complications | 182 per 1000 | 191 per 1000 | OR 1.06 (0.17 to 6.70) | 327 | ⊕⊝⊝⊝ |
| Postoperative complications | 239 per 1000 | 250 per 1000 | OR 0.20 (0.09 to 0.44) | 327 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 44 per 1000 | 47 per 1000 | OR 0.10 (0.01 to 0.84) | 327 | ⊕⊝⊝⊝ |
| Postoperative ileus | 88 per 1000 | 93 per 1000 | OR 0.37 (0.13 to 1.07) | 327 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 31 per 1000 | 33 per 1000 | OR 0.45 (0.10 to 2.08) | 327 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.6 minutes. | Mean operative time in the intervention group was 8.52 minutes lower (15.64 minutes shorter to 1.39 minutes shorter). | 327 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 1.9 days. | Mean hospital stay in the intervention group was 0.02 days longer (0.38 days shorter to 0.34 days longer). | 327 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Clips vs ligatures for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: clips Comparison: ligature | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligature | Risk with clips | ||||
| Total complications | 17 per 1000 | 18 per 1000 | OR 2.03 (0.71 to 5.84) | 553 | ⊕⊝⊝⊝ |
| Intraoperative complications | 21 per 1000 | 22 per 1000 | OR 1.74 (0.33 to 9.04) | 553 | ⊕⊝⊝⊝ |
| Postoperative complications | 17 per 1000 | 18 per 1000 | OR 1.88 (0.63 to 5.64) | 553 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 14 per 1000 | 15 per 1000 | OR 1.25 (0.32 to 4.90) | 553 | ⊕⊝⊝⊝ |
| Postoperative ileus | 10 per 1000 | 11 per 1000 | OR 0.92 (0.15 to 5.64) | 553 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 3 per 1000 | 4 per 1000 | OR 1.75 (0.28 to 10.93) | 553 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.0 minutes. | Mean operative time in the intervention group was 8.14 minutes shorter (11.73 minutes shorter to 4.55 minutes shorter). | 553 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 1.5 days. | Mean hospital stay in the intervention group was 0.03 days shorter (0.16 days shorter to 0.11 days longer). | 553 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Endoscopic stapler vs clips for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: endoscopic stapler Comparison: clips | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with clips | Risk with endoscopic stapler | ||||
| Total complications | 67 per 1000 | 70 per 1000 | OR 1.00 (0.13 to 7.60) | 60 | ⊕⊝⊝⊝ |
| Intraoperative complications | 67 per 1000 | 70 per 1000 | OR 1.00 (0.13 to 7.60) | [60 | ⊕⊝⊝⊝ |
| Postoperative complications | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative superficial infections | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative ileus | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative deep infections | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Operative time (minutes) | Mean operative time was 39.4 minutes. | Mean operative time in the intervention group was 3.46 minutes shorter (6.94 minutes shorter to 0.02 minutes longer). | 60 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 2.0 days. | Mean hospital stay in the intervention group was 0.04 days shorter (0.28 days shorter to 0.20 days longer). | 60 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for single study with limited sample size. bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (the sole included studies had few participants and therefore few events, resulting in wide confidence intervals, which limited the precision of estimates). | |||||
Antecedentes
La apendicitis se refiere a la inflamación del apéndice. La apendicectomía (extracción quirúrgica del apéndice) se realiza como una intervención de urgencia para tratar a pacientes con apendicitis aguda (Andersen 2005).
Descripción de la afección
La apendicitis aguda, descrita por primera vez por Fitz en 1886, es la causa más habitual de dolor abdominal agudo (Andersen 2005; Rehman 2011; Wilms 2011). La incidencia global de apendicitis aguda varía entre 76 y 227 casos por cada 100 000 personas al año (Addiss 1990; Andreu‐Ballester 2009; Buckius 2011; Lee 2010; Pieper 1982). Se ha informado de que el riesgo de padecer apendicitis aguda a lo largo de la vida se sitúa entre el 6% y el 16% (Addiss 1990; Lee 2010). Esta enfermedad afecta a todos los grupos etarios, con una mayor incidencia en la segunda década (Addiss 1990; Wilms 2011).
La causa de la apendicitis aguda es un asunto de debate considerable (Andersen 2005). La apendicitis aguda podría estar asociada con la obstrucción de la luz apendicular (el especio interior de un apéndice), que podría resultar en un aumento de la presión intraluminal con necrosis del tejido transmural (Andersen 2005). La necrosis del tejido va seguida de una invasión bacteriana que da lugar a la inflamación del apéndice (Andersen 2005).
Descripción de la intervención
Los pacientes con apendicitis aguda a menudo necesitan una apendicectomía (sin importar si es con acceso abierto o laparoscópico) para aliviar los síntomas y evitar complicaciones. La apendicectomía laparoscópica se describió por primera vez en 1983 (Schier 1998). Desde entonces, la intervención ha sufrido algunas modificaciones (de cuatro puertos a tres y después a dos) En 1992, Pelosi informó sobre la operación laparoscópica de incisión única, que daba como resultado menos traumatismo superficial al mismo tiempo que proporcionaba un acceso operatorio seguro (Pelosi 1992). Tanto la apendicectomía laparoscópica como la apendicectomía abierta están bien consideradas entre los cirujanos, y los datos clínicos han mostrado ventajas relativas definidas de la apendicectomía laparoscópica, aunque pequeñas en términos absolutos. Un posible inconveniente de la técnica laparoscópica es que presenta una tasa de absceso intrabdominal ligeramente más alta (Sauerland 2010). En este contexto, se ha sugerido que las técnicas de cierre del muñón apendicular desempeñan un papel clave para prevenir las complicaciones infecciosas tras la apendicectomía (Krisher 2001).
De qué manera podría funcionar la intervención
La técnica tradicional para asegurar el muñón apendicular durante la apendicectomía abierta implicaba la transfixión de la base apendicular y la posterior sutura en bolsa de tabaco alrededor de la base del apéndice para invertirla hacia el ciego. Sin embargo, esta sutura es difícil de aplicar durante la apendicectomía laparoscópica (Houben 1998). Por ello, se han introducido otras dos técnicas para la apendicectomía laparoscópica. La primera técnica implica el nudo de Roeder, un lazo corredizo preatado desarrollado por Roeder (un cirujano otorrinolaringólogo alemán) para la amigdalectomía (Röder 1918). Tras la aplicación de uno o más de estos nudos a la base del apéndice, este puede ser extraído. (Beldi 2006; Shimi 1994). La segunda técnica utiliza un dispositivo mecánico como una grapadora para anastomosis gastrointestinal (AG) (Daniell 1991; Klaiber 1994),clips de titanio (Akbiyik 2011; Ates 2012; Delibegovic 2012; Gonenc 2012),o un dispositivo bipolar electrotérmico de sellado de tejido (Sucullu 2009).
La grapadora para AG aplica dos filas de pequeñas grapas para sujetar entre sí los bordes del tejido, de manera que la disección automática puede realizarse entre las dos filas (Beldi 2006). Este dispositivo puede cargarse con diferentes cartuchos de grapas, permitiendo así su aplicación a diferentes tipos de tejidos, como la base apendicular y el mesoapéndice con su arteria. Más recientemente se ha descrito el uso de diferentes tipos de clips de titanio para la apendicectomía laparoscópica (Hanssen 2007; Partecke 2010; Delibegovic 2009), los cuales ofrecen las ventajas de ser fáciles de aplicar y baratos. El LigaSure Vessel Sealing System (Valleylab, Boulder, Colorado, EE. UU.) (Yang 2015) evita la colocación de clips prostéticos mediante una sistema bipolar electrotérmico de sellado de tejido.
Por qué es importante realizar esta revisión
El uso de ligaduras tradicionales (como los nudos intracorpóreos o los nudos de Roeder) y dispositivos mecánicos (como las grapadoras AG, los clips o los dispositivos electrotérmicos) está ampliamente extendido en apendicectomías laparoscópicas en todo el mundo. Actualmente se cree que la principal diferencia entre estas dos estrategias gira en torno a la elección entre el coste o la seguridad. Sin embargo, este concepto no está basado en la evidencia; aunque los dispositivos mecánicos son más caros de utilizar, no está claro si realmente proporcionan un cierre más seguro del muñón apendicular en comparación con su equivalente más barato, las ligaduras. Sin duda alguna, el grado de inflamación local y la experiencia del cirujano desempeñan un papel decisivo en la elección de la técnica quirúrgica. No obstante, hasta la fecha, ninguna revisión Cochrane ha determinado la técnica de preferencia para asegurar el muñón apendicular en la apendicectomía laparoscópica.
Objetivos
Comparar todas las técnicas quirúrgicas utilizadas actualmente para el cierre del muñón apendicular durante la apendicectomía laparoscópica.
Métodos
Criterios de inclusión de estudios para esta revisión
Tipos de estudios
Se incluyeron ensayos controlados con asignación aleatoria (ECA) independientemente de su estado de publicación e idioma, incluidos estudios con asignación aleatoria por grupos. Se excluyeron ensayos cuasialeatorios (en los que la asignación se realizó conforme a una secuencia pseudoaleatoria, por ejemplo: número de ingreso par o impar, fecha de nacimiento, alternancia) y estudios sin asignación aleatoria. (Higgins 2011a). Se incluyeron estudios que informaron únicamente en forma de resumen si los datos completos del estudio estaban disponibles.
Tipos de participantes
Se incluyó a pacientes (sin importar su edad, sexo o raza) a los que se les iba a realizar una apendicectomía laparoscópica.
Tipos de intervenciones
Se examinaron las siguientes comparaciones.
-
Cierre mecánico del muñón apendicular (con grapadora, clips o dispositivo Ligasure) versus ligadura (con Endoloop, nudo Roeder o nudo intracorpóreo).
-
Grapadora versus ligadura (con Endoloop, nudo Roeder o nudo intracorpóreo).
-
Clips versus ligadura (con Endoloop, nudo Roeder o nudo intracorpóreo).
-
Grapadora versus clips
-
Una ligadura versus dos (con Endoloop, nudo Roeder o nudo intracorpóreo).
-
Dispositivo de sellado LigaSure versus otro dispositivo mecánico (grapadora o clips) o versus ligadura (con Endoloop, nudo Roeder o nudo intracorpóreo).
Tipos de medida de resultado
Las medidas de resultado principales se centraron en complicaciones entre las diferentes intervenciones, mientras que las medidas de resultado secundarias examinaron las implicaciones económicas y relacionadas con la salud de las diferentes intervenciones evaluadas.
Resultados primarios
-
Complicaciones totales (definidas como todas las complicaciones, es decir, la suma de complicaciones intraoperatorias y posoperatorias)
-
Complicaciones intraoperatorias:
-
Hemorragia intraoperatoria
-
Rotura intraoperatoria del apéndice
-
Lesión de un órgano/encopresis fecal intraoperatorias
-
lesión visceral relacionada con el acceso
-
-
Complicaciones posoperatorias:
-
Infección del sitio quirúrgico (superficial)
-
Infección profunda
-
Hemorragia posoperatoria
-
Íleo paralítico
-
Peritonitis purulenta
-
Resultados secundarios
-
Duración de la intervención (minutos)
-
Estancia hospitalaria (días)
-
Costes hospitalarios (operación, directos e indirectos)
-
Dolor/calidad de vida, medidos con un instrumento validado (es decir, la escala visual analógica; EVA)
Results
Description of studies
We have presented search results and a flow chart of studies in Figure 2.

*Lange 1993 was not retrievable following a worldwide search because the journal was published and is going out of print (see Results section).
Results of the search
We identified 342 studies from a search of the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE Ovid, Embase Ovid, and Science Citation Index ‐ Expanded. Removal of duplicates yielded 238 studies. One of these studies was not available for screening, as the journal it was published in no longer existed and an online archive could not be located (Lange 1993). A worldwide search commissioned by the Bodleian Library, University of Oxford, could not locate a printed version of this paper for our screening process. After excluding studies from the remaining 237 that did not meet our inclusion criteria, we short‐listed 11 studies for full‐text review and data extraction (Akbiyik 2011; Ates 2012; Beldi 2004; Colak 2013; Delibegovic 2012; Gonenc 2012; Nadeem 2015; Ortega 1995; Shalaby 2001; Sucullu 2009; Yang 2014). Of these, we subsequently excluded three studies from the quantitative meta‐analysis following risk of bias assessment owing to quasi‐randomisation that resulted in an unacceptably high risk of randomisation bias (Ates 2012; Beldi 2004; Sucullu 2009). This resulted in inclusion of eight studies in the final meta‐analysis. All studies were published in the English language, except for Yang 2014, which was published in Chinese and translated by review authors.
Upon re‐running the searches in June 2017, we identified two abstracts (Lv 2016; Sadat‐Safavi 2016). These two abstracts are too recent to have been classified by the publication date of this meta‐analysis, thus we have listed them under Studies awaiting classification and will consider them for inclusion in a future update of this review.
Included studies
Our review included eight randomised controlled trials, with a total of 850 participants (Akbiyik 2011; Colak 2013; Delibegovic 2012; Gonenc 2012; Nadeem 2015; Ortega 1995; Shalaby 2001; Yang 2014). These studies span two decades from Ortega 1995 to Nadeem 2015. One study was reported from the USA (Ortega 1995), three from Turkey (Akbiyik 2011; Colak 2013; Gonenc 2012;), one from Bosnia and Herzegovina (Delibegovic 2012), one from China (Yang 2014), one from Pakistan (Nadeem 2015), and one from Egypt and Saudi Arabia (Shalaby 2001). Six studies compared clips versus a ligatures (Akbiyik 2011; Colak 2013; Delibegovic 2012; Gonenc 2012; Nadeem 2015; Yang 2014), two compared stapler versus ligature (Ortega 1995; Shalaby 2001), and one compared stapler versus clip use (Delibegovic 2012).
We have summarised these studies in the Characteristics of included studies tables. No studies were eligible for inclusion in comparisons that examined the question of one ligature versus two ligatures, or LigaSure sealing device versus other mechanical devices (with stapler or clips) or versus ligation (with Endoloop, Roeder loop, or intracorporeal knot).
Excluded studies
We excluded three trials from the quantitative meta‐analysis following risk of bias assessment, as they used quasi‐randomisation, resulting in an unacceptably high risk of randomisation bias (Ates 2012; Beldi 2004; Sucullu 2009). Of these three quasi‐randomised trials, one study compared titanium clips versus a ligature (Endoloop/intracorporeal knot) (Ates 2012), one compared the LigaSure sealing device versus titanium clips (Sucullu 2009), and one compared one ligature (with Endoloop) versus two ligatures (with Endoloops) (Beldi 2004).
Risk of bias in included studies
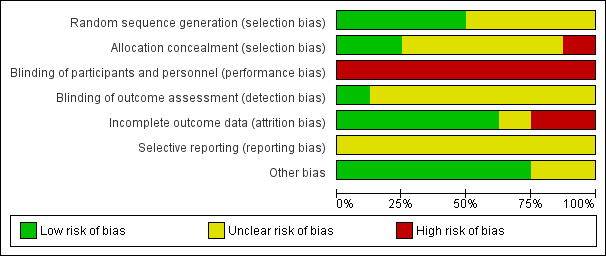
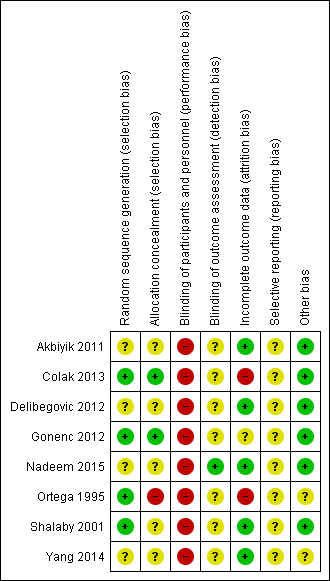
We have presented results of our risk of bias assessment in Figure 3 and Figure 4. We judged the overall risk of bias for all trials across domains as high.
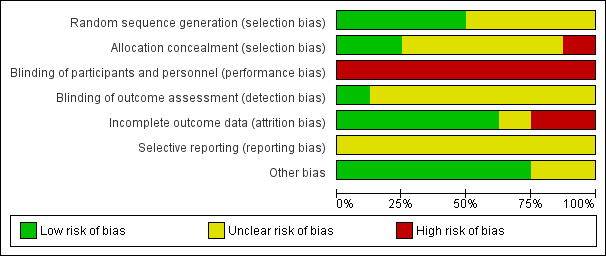
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
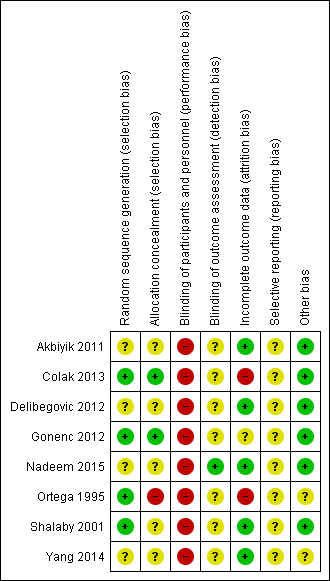
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Details of random sequence generation were unavailable for four of the included trials (Akbiyik 2011; Delibegovic 2012; Nadeem 2015; Yang 2014), in which the only indication of randomisation was seen in variations of the statement, “patients randomly allocated". On this basis, we classified risk of selection bias in these trials as unclear. Trials for which details were available achieved randomisation by using a “computer‐generated randomisation schedule” (Colak 2013), “by the lottery method” (Gonenc 2012), through a “computer‐generated random numbers table” (Ortega 1995), or by using a “table of random numbers” (Shalaby 2001). Colak 2013 recruited a total of 60 participants and excluded four participants postoperatively owing to conversion to open appendectomy, along with three participants owing to loss of follow‐up. Moreover, Ortega 1995 stated that "endoscopic staplers were temporarily unavailable at one point during the study and five patients randomised to endoscopic linear stapler underwent appendectomies with pre‐tied loops" and were subsequently re‐allocated to corresponding groups. We interpreted this as high risk for attrition bias as well as high risk for allocation concealment bias, as it was likely to influence effect estimates.
Blinding
Blinding of performing surgeons to the technique is impossible with this type of intervention, and personnel are likely to be aware of study group allocation from intraoperative and postoperative records. This lack of personnel blinding is an inherent drawback of such surgical intervention trials. We classified all eight trials (Akbiyik 2011; Colak 2013; Delibegovic 2012; Gonenc 2012; Nadeem 2015; Ortega 1995; Shalaby 2001; Yang 2014) as showing high risk of performance bias. Ortega 1995 stated that “data collection was performed in a prospective fashion using two standardised data sheets", and it was unclear whether these data sheets were intended for different arms of the study, or whether they were trial arm‐specific; if so, this would imply complete lack of postoperative blinding of the healthcare team (even those not directly involved in the operation). The remaining studies made no mention of this (Akbiyik 2011; Colak 2013; Delibegovic 2012; Gonenc 2012; Shalaby 2001; Yang 2014).
Nadeem 2015 stated that this was a single‐blinded trial and made efforts to minimise detection bias by ensuring that investigators who collected data were "at the same time blinded for the type of procedure done". However, it was unclear to what extent the operating team could influence the postoperative course outside the remit of data collection. In all studies except Nadeem 2015, it was also unclear whether participants were aware of the method used because no specific reference was made to methods of participant blinding. Studies that described procedures performed by residents had the potential for performance bias (Gonenc 2012; Ortega 1995). Ortega 1995 (n = 253) and Gonenc 2012 (n = 107) contributed some of the largest participant populations to our analysis and were conducted entirely by residents, with attending surgeons experienced in laparoscopic and open surgical techniques present (Ortega 1995). Attendings presumably were holding the camera during these laparoscopic procedures. Trial authors did not refer to the variation in seniority amongst operating residents (although Gonenc 2012 stated that investigators were at least within their second year of residency). The assumption is that all residents were equally skilled and fluent in both randomised methods of appendix stump closure; however, because trial authors did not explicitly state that all residents were trained to equal proficiency in both approaches, we recorded the potential for performance bias as 'unclear'.
Incomplete outcome data
We classified five trials as having low risk of attrition bias, as they were free of postrandomisation exclusions (Akbiyik 2011; Delibegovic 2012; Nadeem 2015; Shalaby 2001; Yang 2014). We classified two trials as having high risk of attrition bias (Colak 2013; Ortega 1995). Colak 2013 recruited a total of 60 participants and excluded four participants postoperatively owing to conversion to open appendectomy and three participants because of loss to follow‐up. Moreover, Ortega 1995 stated that "endoscopic staplers were temporarily unavailable at one point during the study and five patients randomised to endoscopic linear stapler underwent appendectomies with pre‐tied loops" and were subsequently re‐allocated to corresponding groups. We interpreted this as high risk for attrition bias as well as high risk for allocation concealment bias and believed it was likely to influence effect estimates. We classified one trial as having unclear risk of attrition bias (Gonenc 2012). Gonenc 2012 excluded participants with an intraoperative diagnosis of complicated appendicitis and those who had undergone an open appendectomy. However, trial authors provided no information on the number of participants initially recruited to the study before randomisation and how many of these were subsequently excluded, if any. As a result, the level of attrition bias in this study was not clear.
Selective reporting
Similar to the ubiquitous problem of blinding amongst our included studies, we could not identify an a priori publication of intended outcomes from either a published trial protocol or trial registration for any of the studies included in this review. As a result, we considered all studies as having 'unknown' risk of selective reporting bias. In addition, Akbiyik 2011 had a follow‐up period that varied between one week and one year, and no uniform long‐term outcome data were made available for comparison between groups, as this study published only limited data from four‐month follow‐up.
Other potential sources of bias
Postoperative pain constituted one of the primary outcomes in one of our included studies (Ortega 1995), which suffered a combination of attrition and reporting biases because amongst 253 participants randomised at 10 different centres, the comparison of postoperative pain between study arms was undertaken only in a subpopulation of 134 participants from a single centre. It is not clear to what degree participant characteristics at this single centre were similar to or different from those noted in the rest of the study population. We therefore classified Ortega 1995 as having unclear risk of other bias. We classified Yang 2014 as having unclear risk of other potential sources of bias, as only limited methodological information was provided in its published manuscript.
Effects of interventions
See: Summary of findings for the main comparison Mechanical devices versus ligature for appendix stump closure during laparoscopic appendectomy; Summary of findings 2 Endoscopic stapler versus ligature for appendix stump closure during laparoscopic appendectomy; Summary of findings 3 Clips versus ligature for appendix stump closure during laparoscopic appendectomy; Summary of findings 4 Endoscopic stapler versus clips for appendix stump closure during laparoscopic appendectomy
We present the following results for our a priori primary and secondary outcomes for outlined comparisons.
1. Mechanical appendix stump closure (with stapler, clips, or LigaSure device) versus ligation (with Endoloop, Roeder loop, or intracorporeal knot)
1.1 Primary outcomes
1.1.1 Total complications
The composite comparison of 850 participants from eight randomised studies (Akbiyik 2011; Colak 2013; Delibegovic 2012; Gonenc 2012; Nadeem 2015; Ortega 1995; Shalaby 2001; Yang 2014) of all types of mechanical devices versus ligature (or Endoloop, Roeder loop, or intracorporeal knot) for appendix stump closure during laparoscopic appendectomy showed no significant differences in overall complications (odds ratio (OR) 0.97, 95% confidence interval (CI) 0.27 to 3.50) (Analysis 1.1). However, it should be noted that the wide 95% confidence intervals in this analysis might actually represent imprecision of the estimate, rather than no true difference. This analysis was subject to a high degree of heterogeneity (I2 = 84%); therefore GRADE should be downgraded further by one level to very low quality (i.e. owing to inconsistency), largely because of the addition of the two most recent trials (Nadeem 2015; Yang 2014).
1.1.2 Intraoperative complications
Data show no differences in intraoperative complications from the use of any mechanical device when compared with ligature (OR 0.93, 95% CI 0.34 to 2.55; I2 = 25%) (Analysis 1.2).
1.1.3 Postoperative complications
Similar to our analysis of intraoperative complications, we found no substantial differences in postoperative complications between the use of any mechanical device versus any ligature‐based appendix stump closure technique (OR 0.80, 95% CI 0.21 to 3.13) (Analysis 1.3). This analysis was subject to substantial heterogeneity (I2 = 83%). More detailed examination by type of postoperative complication helped to reduce heterogeneity but still showed no significant differences between mechanical devices and ligature. Data show no differences in postoperative superficial infection rates (OR 0.58, 95% CI 0.18 to 1.93; I2 = 8%) (Analysis 1.6), deep infection rates (OR 0.79, 95% CI 0.24 to 2.53; I2 = 0%) (Analysis 1.7), and postoperative ileus rates (OR 0.47, 95% CI 0.19 to 1.18; I2 = 0%) (Analysis 1.8), when any mechanical device was compared with ligature.
Quality of the evidence
We judged the overall quality of evidence for the primary outcomes for this comparison as very low owing to high risk of bias, imprecision, small sample sizes, lack of long‐term follow‐up, and heterogeneity amongst included studies (summary of findings Table for the main comparison).
1.2 Secondary outcomes
The evidence upon which our secondary outcome analyses were based had a GRADE rating of very low quality for three main reasons: (1) methodological limitations amongst the included studies listed above, (2) the more general subjective nature of using hospital stay as an outcome measure, which can be confounded by a number of factors unaccounted for in the included studies, and (3) the paucity of pain and quality of life‐related outcome measures amongst included studies.
1.2.1 Operative time
Results show a significant reduction in operative time with mechanical devices compared with ligature‐based techniques, with saving of approximately nine minutes on average across all studies (mean difference (MD) ‐9.04 minutes, 95% CI ‐12.97 to ‐5.11 minutes; I2 = 87%) (Analysis 1.4).
1.2.2 Duration of hospital stay
We noted no significant differences in reduction in hospital stay with mechanical devices compared with ligature‐based techniques (MD 0.02 days, 95% CI ‐0.12 to 0.17 days; I2 = 30%) (Analysis 1.5).
1.2.3 Hospital cost
Only four of the included trials commented on the consumable cost of the method used in each comparison arm, with mechanical devices costing at least three‐fold more than ligature‐based methods (Akbiyik 2011; Delibegovic 2012; Nadeem 2015; Shalaby 2001). None of the included studies evaluated total health economic costs such as whether any additional costs in staff time were required for device setup, maintenance, and disposal; or whether the observed reduction in operating time translated into additional emergency operations per day.
1.2.4 Pain/Quality of life
Only Ortega 1995 evaluated postoperative pain and reported showed no significant differences between use of the endoscopic stapler and ligature use. However, the published description suggests that the method used to ascertain this might have been subject to methodological confounding (see section Other potential sources of bias). No other studies evaluated quality of life postoperatively.
Quality of the evidence
We judged the overall quality of evidence for secondary outcomes for this comparison to be very low owing to high risk of bias, imprecision, small sample sizes, lack of long‐term follow‐up, and heterogeneity amongst included studies (summary of findings Table for the main comparison).
2. Stapler versus ligation (with Endoloop, Roeder loop, or intracorporeal knot)
2.1 Primary outcomes
2.1.1 Total complications
Analysis of the comparison of endoscopic stapler device versus ligature amongst 327 participants randomised in three studies showed that the endoscopic stapler device resulted in no substantial differences in overall complications compared with the ligature (Delibegovic 2012; Ortega 1995; Shalaby 2001) (OR 0.34, 95% CI 0.05 to 2.41; I2 = 60%) (Analysis 2.1).
2.1.2 Intraoperative complications
Data show no differences in intraoperative complications in our comparison of endoscopic stapler device versus ligature technique for appendix stump closure (OR 1.06, 95% CI 0.17 to 6.70; I2 = 45%) (Analysis 2.2).
2.1.3 Postoperative complications
Results show a significant reduction in postoperative complications with use of the stapler device compared with ligature (OR 0.20, 95% CI 0.09 to 0.44; I2 = 0%) (Analysis 2.3); this was masked in the analysis of overall complications by no differences amongst intraoperative complications in this comparison (OR 1.06, 95% CI 0.17 to 6.70; I2 = 45%) (Analysis 2.2). Exploration of this reduction in postoperative complications revealed that it was chiefly driven by a reduction in postoperative superficial wound infections in the endoscopic stapler arm when compared with the ligature arm (OR 0.10, 95% CI 0.01 to 0.84; I2 = 0%) (Analysis 2.6). We noted no significant differences in postoperative deep infection (OR 0.45, 95% CI 0.10 to 2.08; I2 = 0%) (Analysis 2.7) or postoperative ileus (OR 0.37, 95% CI 0.13 to 1.07; I2 = 0%) (Analysis 2.8) between the two groups. No studies reported postoperative bleeding, appendix stump rupture, or purulent peritonitis in either comparison group.
Quality of the evidence
We judged overall quality of evidence for the primary outcomes for this comparison to be very low owing to high risk of bias, imprecision, and substantial heterogeneity amongst included studies (summary of findings Table 2).
2.2 Secondary outcomes
The evidence upon which our secondary outcome analyses were based also had a very low GRADE quality rating for the same three main reasons as for the primary outcome analyses, with the addition of subjective reporting of hospital stay as an outcome measure, which can be confounded by several factors unaccounted for in the included studies, and the paucity of pain and quality of life‐related outcomes measures amongst included studies.
2.2.1 Operative time
Data show a significant reduction in operative time with use of the endoscopic stapler device versus the ligature‐based technique (MD ‐8.52 minutes, 95% CI ‐15.64 to ‐1.39 minutes; I2 = 91%) (Analysis 2.4).
2.2.2 Duration of hospital stay
We noted no significant reduction in differences in hospital stay with use of the endoscopic stapler compared with ligature‐based techniques (MD ‐0.02 days, 95% CI ‐0.38 to 0.34 days; I2 = 66%) (Analysis 2.5).
2.2.3 Hospital cost
Two of the three studies included in this subanalysis commented on the consumable cost of the method used in each comparison arm (Delibegovic 2012; Shalaby 2001). Delibegovic 2012 commented that the cost per 45‐mm stapler used was EUR 230.7, whereas the cost per ligature (Endoloop) was EUR 28.85 (with two loops generally used). Shalaby 2001 commented that the cost per Endo GIA stapler (Ethicon Endo‐Surgery, Cincinnati, Ohio, USA) was USD 100 (EUR 86.00), whereas the cost per ligature (Endoloop) was USD 30 (EUR 25.80). No studies commented on indirect costs.
2.2.4 Pain/Quality of life
As described in Section 1.2.4, only one study evaluated postoperative pain (Ortega 1995), showing no significant differences between use of the endoscopic stapler and ligature use. However, the published description suggests that the method used to ascertain might have been subject to methodological confounding (see section Other potential sources of bias). No other studies evaluated quality of life postoperatively.
Quality of the evidence
We judged the overall quality of evidence for secondary outcomes for this comparison to be very low owing to high risk of bias, imprecision, and substantial heterogeneity amongst included studies (summary of findings Table 2).
3. Clips versus ligation (with Endoloop, Roeder loop, or intracorporeal knot)
3.1 Primary outcomes
3.1.1 Total complications
Similarly, data show no significant differences in overall complications between use of clips versus ligature placement (OR 2.03, 95% CI 0.71 to 5.84; I2 = 61%) (Analysis 3.1) amongst 553 participants from six studies (Akbiyik 2011; Colak 2013; Delibegovic 2012; Gonenc 2012; Nadeem 2015; Yang 2014). This analysis was subject to high heterogeneity (I2 = 61%), and, similar to the composite analyses in Analysis 1.1, much of this heterogeneity was contributed by inclusion of a more recent study (Yang 2014).
3.1.2 Intraoperative complications
We noted no differences in intraoperative complications in our comparison of endoscopic clip placement versus ligature (OR 1.74, 95% CI 0.33 to 9.04; I2 = 19%) (Analysis 3.2).
3.1.3 Postoperative complications
Results show no substantial differences in postoperative complications between endoscopic clip placement and ligature placement for appendix stump closure (OR 1.74, 95% CI 0.33 to 9.04; I2 = 19%) (Analysis 3.3).
Quality of the evidence
We judged the overall quality of evidence for the primary outcomes for this comparison as very low owing to high risk of bias, imprecision, and heterogeneity amongst included studies (summary of findings Table 3).
3.2 Secondary outcomes
The evidence upon which our secondary outcome analyses were based also had a very low GRADE quality rating for the same three main reasons as for the primary outcome analyses.
3.2.1 Operative time
Data show a significant reduction in operative time with use of endoscopic clips versus a ligature‐based technique (MD ‐8.14 minutes, 95% CI ‐11.73 to ‐4.55 minutes; I2 = 66%) (Analysis 3.4).
3.2.2 Duration of hospital stay
We noted no significant difference in reduction in hospital stay with endoscopic clip use compared with ligature‐based techniques (MD ‐0.03 days, 95% CI ‐0.16 to 0.11 days; I2 = 0%) (Analysis 3.5).
3.2.3 Hospital cost
Three of the six included studies commented on the consumable cost of the method used in each comparison arm (Akbiyik 2011; Delibegovic 2012; Nadeem 2015). Akbiyik 2011 commented that the cost per Endo GIA (Ethicon Endo‐Surgery, Cincinnati, Ohio, USA) stapler was USD 100, whereas the cost per ligature (Endoloop) was USD 60.75 (with two loops generally used). Delibegovic 2012 commented that the cost per one Hem‐o‐lok clip (non‐absorbable polymeric clips) was EUR 4.75 (USD 5.52) but did not comment on the cost of the endoscopic clipping device. Delibegovic 2012 commented that the cost per ligature (Endoloop) was EUR 28.85 (USD 33.55)(with two loops generally used). Nadeem 2015 commented that total cost for the metallic endoclip arm was USD 800, whereas the cost per loop in the ligature arm was USD 200. However, Nadeem 2015 did not provide a justification for these costs. None of the included studies specifically listed indirect costs associated with each comparison arm.
3.2.4 Pain/Quality of life
None of the included studies evaluated pain or quality of life postoperatively.
Quality of the evidence
We judged the overall quality of evidence for secondary outcomes for this comparison to be very low owing to high risk of bias, imprecision, and heterogeneity amongst included studies (summary of findings Table 3).
4. Stapler versus clips
4.1 Primary outcomes
Only one study with 60 participants directly compared endoscopic staplers versus endoscopic clips (Delibegovic 2012).
4.1.1 Total complications
Only one study reported complications (Delibegovic 2012), noting no significant differences in overall complications (OR 1.00, 95% CI 0.13 to 7.60) (Analysis 4.1).
4.1.2 Intraoperative complications
Data show no differences in intraoperative complications in our comparison of endoscopic stapler versus clips (OR 1.00, 95% CI 0.13 to 7.60).
4.1.3 Postoperative complications
We noted no postoperative complications in either comparison arm in this study.
Quality of the evidence
We graded the quality of evidence for the primary outcomes of this comparison as very low owing to high risk of bias, limited sample size, and lack of longer‐term follow‐up (summary of findings Table 4).
4.2 Secondary outcomes
The evidence upon which our secondary outcome analyses were based also had a very low GRADE quality rating for the same three main reasons as for the primary outcome analysis, and because investigators did not examine the paucity of pain and quality of life‐related outcomes measures in sufficient detail.
4.2.1 Operative time
Data show no significant differences in reduction in operative time with endoscopic stapler use compared with use of endoscopic clips (MD ‐3.46 minutes, 95% CI ‐6.94 to 0.02) (Analysis 4.4).
4.2.2 Duration of hospital stay
We noted no significant differences in reduction in hospital stay with endoscopic stapler use compared with use of endoscopic clips (MD ‐0.04 days, 95% CI ‐0.28 to 0.20 days) (Analysis 4.5).
4.2.3 Hospital cost
Delibegovic 2012 commented that the cost per 45‐mm stapler was EUR 230.7, whereas the cost per ligature (Endoloop) was EUR 28.85 (with two loops generally used), and that the cost per one Hem‐o‐lok clip (non‐absorbable polymeric clips) was EUR 4.75; however, investigators did not comment on the cost of the endoscopic clipping device and did not describe indirect costs associated with each comparison arm.
4.2.4 Pain/Quality of life
Data show no evaluation of postoperative pain or quality of life.
Quality of the evidence
We graded the quality of evidence for secondary outcomes of this comparison as very low owing to high risk of bias, limited sample size, and lack of longer‐term follow‐up (summary of findings Table 4).
5. One versus two ligatures (with Endoloop, Roeder loop, or intracorporeal knot)
We found no eligible randomised trials comparing one ligature versus two ligatures for appendix stump closure. Beldi 2004 evaluated this question bycomparing one versus two Endoloops, but we excluded this study from meta‐analysis on the basis of a quasi‐randomised approach to allocating participants to each study arm based on the date of surgery. On odd days, investigators performed the operation using one and on even days two Endoloops to the appendix stump. In total, 208 participants received one Endoloop (n = 109) and 99 participants received two Endoloops to the appendix base. This study found no significant differences in postoperative complications between use of one Endoloop and use of two Endoloops, with each arm reporting five postoperative complications. However, this study was underpowered to demonstrate equivalence between the two arms; therefore the evidence upon which the question of whether one or two Endoloops are appropriate is of very low quality overall.
6. LigaSure sealing device versus other mechanical devices (with stapler or clips) or versus ligation (with Endoloop, Roeder loop, or intracorporeal knot)
We found no eligible randomised trials comparing the LigaSure sealing device versus other mechanical devices (with stapler or clips) or versus ligation (with Endoloop, Roeder loop, or intracorporeal knot).
7. Sensitivity analyses
We have provided in Table 1 a detailed description of all complications seen amongst included studies, and in Table 2 a summary of our sensitivity analysis of primary and secondary outcomes across all comparisons. Our presented results did not vary substantially by any of the a priori defined factors listed in the Methods section. We could not perform our planned sensitivity analysis with exclusion of trials at high risk of bias because all trials were at high risk of overall bias.
| Study ID | Intervention arms | Total no. with complications | Total no. without complications | Intraoperative | Postoperative | |||||||||||
| Bleeding | Intraoperative rupture of appendix | Intraoperative organ injury/ faecal soiling | Access‐related visceral injury | Other | Total | Surgical site infection (superficial) | Deep infection | Bleeding | Paralytic ileus | Purulent peritonitis | Other | Total | ||||
| Ortega 1995 | Endoscopic linear stapler (LAS) | 27 | 51 | 11 | 2 | 5 | 0 | 0 | 18 | 0 | 2 | 0 | 5 | 0 | 2a | 9 |
| 2× catgut ligatures (Endoloops) (LAL) | 62 | 27 | 14 | 4 | 11 | 0 | 0 | 29 | 4 | 4 | 0 | 14 | 0 | 11b | 33 | |
| Open appendectomy (OA) | 44 | 42 | 20 | 5 | 1 | 0 | 0 | 26 | 11 | 0 | 0 | 6 | 0 | 1c | 18 | |
| Akbiyik 2011 | Hem‐o‐lok clip (non‐absorbable polymeric clips) | 0 | 28 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ligaure (Endoloop) | 0 | 21 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Delibegovic 2012 | 45‐mm stapler | 2 | 28 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1 ligature (Endoloop) | 0 | 30 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 1 Hem‐o‐lok clip (non‐absorbable polymeric clips) | 2 | 28 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Beldi 2004 | 1 ligature (Endoloop) only at appendix base (1 other at 6 to 12 mm distally) | 5 | 104 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 2d | 5 |
| 2 ligatures (Endoloops) at base of appendix (1 other at 6 to 12 mm distally) | 5 | 94 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 1e | 5 | |
| Sucullu 2009 | Endodissector and endoclip | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| LigaSure 5 to 10 mm | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Shalaby 2001 | Endo GIA (Ethicon Endo‐Surgery, Cincinnati, Ohio, USA) stapler | 0 | 60 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ligature (Endoloop) | 5 | 35 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 0 | 0 | 0 | 1f | 5 | |
| Extracorporeal laparoscopically assisted appendectomy | 6 | 44 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 4 | |
| Colak 2013 | Hem‐o‐lok (non‐absorbable polymeric clips) | 3 | 23 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 1g | 3 |
| Ligature (Endoloop) | 3 | 24 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1g | 3 | |
| Gonenc 2012 | Titanium endoclip | 4 | 57 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 3 |
| Intracorporeal knotting | 6 | 40 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 2 | 1 | 0 | 4 | |
| Ates 2012 | Titanium endoclip | 8 | 22 | NS | NS | NS | NS | 1h | 7 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Intracorporeal knotting | 7 | 24 | NS | NS | NS | NS | 0 | 4 | 1 | 0 | 0 | 0 | 0 | 2i | 3 | |
| Yang 2014 | Intracorporeal knotting | 5 | 125 | 0 | NS | NS | NS | NS | 0 | NS | 0 | NS | NS | NS | 5j | 5 |
| Titanium hem‐o‐lok | 17 | 69 | 0 | NS | NS | NS | NS | 0 | NS | 0 | NS | NS | NS | 17k | 17 | |
| Nadeem 2015 | Extracorporeal knotting | 5 | 31 | 1 | NS | 0 | NS | NS | 1 | 2 | 0 | NS | 1 | NS | 1 | 4 |
| Metallic endoclip | 10 | 22 | 2 | NS | 1 | NS | NS | 3 | 2 | 2 | NS | 2 | NS | 1l | 7 | |
NS: non‐significant.
aTwo cases of vomiting. bEleven cases of vomiting. cone case of vomiting. dOne case of pulmonary embolism (PE) and one case of persistent port site pain. eOne case of prolonged percutaneous drainage. fOne case of intestinal obstruction. gOne non‐surgical complication. ihTwo open endoclips dropped during procedure and discovered by abdominal X‐ray postoperatively. iOne case of abdominal pain and one case unknown. jThree cases of lower abdominal discomfort, one case of abdominal pain, and two cases of fever. kEight cases of lower abdominal discomfort, three cases of abdominal pain, five cases of fever, and one reoperation. lOne re‐admission occurred in each arm: The re‐admitted participant in the metallic endoclip arm required peritoneal lavage and drain placement.
| Mechanical appendix stump closure (with endoscopic stapler or clip(s)) vs ligation (with Endoloop or intra/extracorporeal knot) | |||||||||
| Odds ratio (95% CI) | Risk ratio (95% CI) | Risk difference (95% CI) | Mean difference (95% CI) | ||||||
| Outcome | Fixed effect | Random effects | Fixed effect | Random effects | Fixed effect | Random effects | Fixed effect | Random effects | |
| Total complications | 0.77 (0.53 to 1.13) | 0.97 (0.27 to 3.50) | 0.83 (0.64 to 1.08) | 1.09 (0.41 to 2.88) | ‐0.03 (‐0.08 to 0.01) | ‐0.02 (‐0.12 to 0.09) | ‐ | ‐ | |
| Intraoperative complications | 0.81 (0.45 to 1.46) | 0.93 (0.34 to 2.55) | 0.85 (0.53 to 1.35) | 0.93 (0.40 to 2.18) | ‐0.01 (‐0.04 to 0.02) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative complications | 0.80 (0.52 to 1.24) | 0.80 (0.21 to 3.13) | 0.83 (0.57 to 1.19) | 0.86 (0.27 to 2.74) | ‐0.02 (‐0.06 to 0.02) | ‐0.02 (‐0.10 to 0.06) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐11.94 (‐13.04 to ‐10.84) | ‐9.04 (‐12.97 to ‐5.11) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.02 (‐0.12 to 0.16) | 0.02 (‐0.12 to 0.17) | |
| Postoperative superficial infections | 0.47 (0.17 to 1.26) | 0.58 (0.18 to 1.93) | 0.48 (0.19 to 1.24) | 0.61 (0.19 to 1.93) | ‐0.02 (‐0.04 to 0.01) | ‐0.01 (‐0.02 to 0.01) | ‐ | ‐ | |
| Postoperative ileus | 0.48 (0.20 to 1.15) | 0.47 (0.19 to 1.18) | 0.51 (0.23 to 1.14) | 0.50 (0.22 to 1.17) | ‐0.02 (‐0.04 to 0.01) | ‐0.01 (‐0.03 to 0.02) | ‐ | ‐ | |
| Postoperative deep infections | 0.86 (0.31 to 2.41) | 0.79 (0.24 to 2.53) | 0.87 (0.32 to 2.35) | 0.79 (0.25 to 2.47) | ‐0.00 (‐0.02 to 0.02) | ‐0.00 (‐0.02 to 0.01) | ‐ | ‐ | |
| Endoscopic stapler vs ligature | |||||||||
| Total complications | 0.26 (0.14 to 0.46) | 0.34 (0.05 to 2.41) | 0.49 (0.35 to 0.68) | 0.51 (0.09 to 2.84) | ‐0.21 (‐0.29 to ‐0.12) | ‐0.13 (‐0.40 to 0.14) | ‐ | ‐ | |
| Intraoperative complications | 0.72 (0.38 to 1.39) | 1.06 (0.17 to 6.70) | 0.79 (0.48 to 1.28) | 1.07 (0.22 to 5.19) | ‐0.04 (‐0.11 to 0.04) | ‐0.00 (‐0.11 to 0.10) | ‐ | ‐ | |
| Postoperative complications | 0.19 (0.09 to 0.41) | 0.20 (0.09 to 0.44) | 0.27 (0.14 to 0.51) | 0.25 (0.08 to 0.75) | ‐0.17 (‐0.24 to ‐0.10) | ‐0.12 (‐0.34 to 0.09) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐12.94 (‐14.35 to ‐11.53) | ‐8.36 (‐15.68 to ‐1.03) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.03 (‐0.14 to 0.20) | ‐0.02 (‐0.38 to 0.34) | |
| Postoperative superficial infections | 0.10 (0.01 to 0.86) | 0.10 (0.01 to 0.84) | 0.11 (0.01 to 0.88) | 0.11 (0.01 to 0.87) | ‐0.05 (‐0.08 to ‐0.01) | ‐0.04 (‐0.08 to 0.00) | ‐ | ‐ | |
| Postoperative ileus | 0.37 (0.13 to 1.07) | 0.37 (0.13 to 1.07) | 0.41 (0.15 to 1.08) | 0.41 (0.15 to 1.08) | ‐0.05 (‐0.10 to 0.00) | ‐0.02 ( ‐0.10 to 0.05) | ‐ | ‐ | |
| Postoperative deep infections | 0.45 (0.10 to 2.02) | 0.45 (0.10 to 2.08) | 0.46 (0.11 to 1.95) | 0.47 (0.11 to 2.04) | ‐0.02 (‐0.05 to 0.02) | ‐0.02 (‐0.05 to 0.02) | ‐ | ‐ | |
| Endoscopic stapler vs clips | |||||||||
| Total complications | 1.00 (0.13 to 7.60) | 1.00 (0.13 to 7.60) | 1.00 (0.15 to 6.64) | 1.00 (0.15 to 6.64) | 0.00 (‐0.13 to 0.13) | 0.00 (‐0.13 to 0.13) | ‐ | ‐ | |
| Intraoperative complications | 1.00 (0.13 to 7.60) | 1.00 (0.13 to 7.60) | 1.00 (0.15 to 6.64) | 1.00 (0.15 to 6.64) | 0.00 (‐0.13 to 0.13) | 0.00 (‐0.13 to 0.13) | ‐ | ‐ | |
| Postoperative complications | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐3.46 (‐6.94 to 0.02) | ‐3.46 (‐6.94 to 0.02) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.04 (‐0.28 to 0.20) | ‐0.04 [‐0.28, 0.20] | |
| Postoperative superficial infections | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Postoperative ileus | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Postoperative deep infections | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Clips vs ligature (Endoloop and intra/extracorporeal knot) | |||||||||
| Total complications | 2.33 (1.31 to 4.13) | 2.03 (0.71 to 5.84) | 2.11 (1.29 to 3.47) | 1.84 (0.73 to 4.62) | 0.08 (0.03 to 0.13) | 0.05 (‐0.03 to 0.13) | ‐ | ‐ | |
| Intraoperative complications | 1.79 (0.49 to 6.56) | 1.74 (0.33 to 9.04) | 1.76 (0.51 to 6.01) | 1.69 (0.35 to 8.19) | 0.01 (‐0.02 to 0.04) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative complications | 2.40 (1.28 to 4.48) | 1.88 (0.63 to 5.64) | 2.20 (1.27 to 3.82) | 1.75 (0.66 to 4.61) | 0.07 (0.02 to 0.12) | 0.03 (‐0.04 to 0.11) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐8.06 (‐9.85 to ‐6.26) | ‐8.14 (‐11.73 to ‐4.55) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.03 (‐0.16 to 0.11) | ‐0.03 (‐0.16 to 0.11) | |
| Postoperative superficial infections | 1.27 (0.33 to 4.86) | 1.25 (0.32 to 4.90) | 1.25 (0.35 to 4.49) | 1.24 (0.34 to 4.56) | 0.00 (‐0.02 to 0.03) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative ileus | 0.92 (0.19 to 4.56) | 0.92 (0.15 to 5.64) | 0.92 (0.20 to 4.21) | 0.93 (0.16 to 5.33) | ‐0.00 (‐0.02 to 0.02) | ‐0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative deep infections | 1.79 (0.37 to 8.58) | 1.75 (0.28 to 10.93) | 1.77 (0.38 to 8.16) | 1.71 (0.28 to 10.28) | 0.01 (‐0.02 to 0.03) | 0.00 (‐0.01 to 0.02) | ‐ | ‐ | |
CI: confidence interval; NE: not estimable; "‐": not applicable.
Discusión
Resumen de los resultados principales
Los autores de la revisión no hallaron ninguna diferencia significativa en los resultados principales de complicaciones totales, complicaciones intraoperatorias y complicaciones posoperatorias entre el uso de dispositivos mecánicos y el uso de técnicas de ligadura para el cierre del muñón apendicular durante la apendicectomía laparoscópica. Una excepción a esto fue que la grapadora dio como resultado una probabilidad reducida de infección posoperatoria superficial de la herida al compararla con la ligadura (odds ratio [OR] 0,10; intervalo de confianza [IC] del 95%: 0,01 a 0,84) (Análisis 2.6). Sin embargo, esta revisión no puede recomendar inequívocamente el uso sistemático de un dispositivo mecánico sobre otro para el cierre del muñón apendicular, debido a que las reducciones de infección superficial posoperatoria y del resultado secundario de duración de la intervención no se tradujeron en una reducción significativa estadística y clínicamente de las complicaciones globales ni de la estancia hospitalaria al compararlas con el uso de ligadura. En cuanto a las comparaciones indirectas de dispositivos mecánicos, los análisis de complicaciones totales asociadas con el uso de una grapadora endoscópica en comparación con la ligadura (OR 0,34; IC del 95%: 0,05 a 2,41) (Análisis 2.1), y asociadas con el uso de clips en comparación con la ligadura (OR 2,03; IC del 95%: 0,71 a 5,84) (Análisis 3.1), presentaron heterogeneidad moderada; el único estudio que comparó directamente dos dispositivos no halló diferencias sustanciales en las complicaciones totales (OR 1,00; IC del 95%: 0,13 a 7,60) (Análisis 4.1) (Delibegovic 2012). Todos los estudios incluidos presentaron limitaciones en forma de sesgos; por lo tanto, no es posible extraer una conclusión clara en vista de la calidad de la evidencia actual.
Aunque estos hallazgos sugieren que el uso de la grapadora endoscópica da lugar a una reducción de la duración de la operación y a un descenso en las tasas de infección superficial posoperatoria en comparación con la colocación de ligadura (o Endoloop), el motivo de la reducción de infección superficial posoperatoria no está totalmente claro. Se debe tener en cuenta que las grapadoras endoscópicas requieren un puerto de 10 a 12 mm, mientras que las ligaduras pueden introducirse a través de un puerto de 5 mm, y las tasas de infección podrías estar relacionadas con el tamaño de la incisión quirúrgica. Una segunda explicación podría basarse en la técnica necesaria para utilizar una grapadora versus la necesaria para colocar una ligadura. La grapadora endoscópica requiere atención a la hora de asegurar que se ha colocado un muñón apendicular viable entre los brazos de la grapadora para permitir márgenes claros de tejido sano cuando se 'dispara' el dispositivo. Una vez se ha colocado correctamente, el cierre del muñón da como resultado poca contaminación de la víscera que lo rodea y poco desplazamiento del dispositivo en la aplicación y la retirada. El resultado podría ser menos contaminación fecal de los tejidos circundantes, puesto que se cierran simultáneamente las luces proximal y distal del apéndice. Por el contrario, los nudos endoscópicos de Roeder o el nudo intracorpóreo requieren mayores habilidades para garantizar una economía de movimiento suficiente para asegurar el nudo y extirpar el apéndice sin una contaminación involuntaria de las puntas de los instrumentos ni de las vísceras circundantes (que podría producir y extender una infección). Los posibles riesgos adicionales de la contaminación fecal y la instrumentación intrabdominal una vez se ha asegurado la ligadura podrían explicar las excesivas tasas de infección superficial posoperatorias del íleo y el tiempo de intervención informado al compararla con dispositivos mecánicos. Cabe destacar que no se observó una diferencia en las tasas de infección posoperatoria profunda ni de íleo, como cabría esperar tras esta explicación. En teoría, esta explicación debería ser igualmente aplicable al uso del clip endoscópico y al de la grapadora endoscópica. Sin embargo, no se observa una reducción de la infección superficial posoperatoria con clips endoscópicos de la misma manera que se observa con el uso de una grapadora endoscópica. Esto podría tener más relación con las limitaciones de evaluación de resultados de los estudios incluidos, especialmente en resultados subjetivos como el íleo posoperatorio (ver Calidad de la evidencia), y podría no ser realmente representativo de la técnica empleada.
Un cirujano debe considerar dos cuestiones claves a la hora de decidir cómo cerrar el muñón apendicular, las cuales son la seguridad del paciente y los costes económicos de salud. La seguridad del paciente podría ampliarse para incluir también los efectos perjudiciales de una anestesia prolongada, entre ellos el retraso en la duración de intervención, el posible daño colateral o lesión iatrogénica por el uso de la intervención y las implicaciones del fracaso para el desenlace deseado de la intervención. Los costes económicos se extienden más allá de los costes de la maquinaria por uso de la intervención e incluyen también las repercusiones económicas de las intervenciones que requieren más tiempo (y reducen el tiempo para otras operaciones), la estancia hospitalaria prolongada y los costes de reintervenciones o seguimiento.
Cualquier reducción de los costes resultantes de menores complicaciones posoperatorias debe compatibilizarse con el coste del dispositivo, especialmente porque una grapadora de media es al menos cuatro veces más cara que una ligadura (en forma de Endoloops). Los estudios incluidos no proporcionaron suficientes datos para permitir un análisis de coste‐beneficio detallado. De manera similar, la información disponible no es suficiente para realizar una comparación cuantitativa de morbilidad entre los dispositivos. Sin embargo, los resultados de la revisión cualitativa no muestran diferencias sustanciales en el dolor ni la calidad de vida asociados con alguna intervención concreta.
Compleción y aplicabilidad general de las pruebas
Esta revisión incluyó ensayos controlados con asignación aleatoria (ECA) de participantes a los que se les realizó una apendicectomía laparoscópica. Dos de los estudios incluidos excluyeron a participantes traspasados a apendicectomía abierta. (Colak 2013; Gonenc 2012). Por lo tanto, los hallazgos de esta revisión son aplicables a pacientes diagnosticados de apendicitis aguda no complicada aptos para una intervención laparoscópica.
Calidad de la evidencia
Para esta revisión, el metanálisis incluyó 850 participantes de ocho estudios aleatorios. La calidad de la evidencia para el resultado principal 'complicaciones totales' de todas las comparaciones se redujo en un nivel por el elevado riesgo de sesgo, en un nivel por inconsistencia debida a la heterogeneidad considerable y en un nivel por imprecisión. La calidad de la evidencia del resto de resultados de todas las comparaciones se calificó de muy baja debido al alto riesgo de sesgo e imprecisión (intervalos de confianza amplios).
Todos los estudios informaron acerca de detalles de las complicaciones intraoperatorias y posoperatorias. No obstantes, ningún estudio proporcionó información sobre el cegamiento del personal ni de los participantes. El cegamiento del personal en estudios con asignación aleatoria que comparan diferentes intervenciones quirúrgicas es complicado, lo cual es un inconveniente habitual de muchos ensayos quirúrgicos. El cegamiento puede afectar a la percepción de los resultados secundarios como el dolor o la calidad de vida. También puede influir en la detección de resultados como el íleo posoperatorio, que, aunque estos resultados muestran que se reduce con dispositivos mecánicos, puede ser difícil de cuantificar objetivamente incluso por un profesional cegado; ninguno de los estudios incluidos especifica claramente si el diagnóstico lo realizó personal cegado. Deberían emplearse todos los esfuerzos posibles en el cegamiento de la evaluación de resultados, puesto que podría contribuir significativamente a reducir el sesgo de detección.
Dos ensayos tuvieron un alto riesgo de sesgo de selección y de deserción por excluir a participantes de manera posoperatoria (Colak 2013) o modificar la asignación de varios participantes del grupo que se había asignado aleatoriamente en inicio a Ortega 1995. Además, dos ensayos tuvieron un riesgo de sesgo de deserción incierto, porque excluyeron a participantes de forma posoperatoria pero no proporcionaron detalles suficientes sobre el proceso de exclusión para permitir una valoración. (Gonenc 2012; Nadeem 2015). Tanto el sesgo de selección como el de deserción podrían haberse reducido mediante la publicación y el registro de un protocolo de ensayo previo y adecuado, así como mediante un informe diligente de resultados predefinidos de todos los participantes asignados al azar según el grupo al que fueron asignados (análisis por intención de tratar).
La calidad de la evidencia podría verse comprometida también como resultado de la heterogeneidad de los cirujanos. Ortega 1995 aportó la mayor población de participantes a este análisis; todas las intervenciones las realizaron residentes y hubo un elevado número informado de complicaciones totales. Esto puede suponer una importante fuente de sesgo en la evaluación de los resultados principales, especialmente sin diferencias significativas en las tasas de complicaciones informadas por otros estudios. Para asegurar una evaluación homogénea, los profesionales a cargo de las intervenciones deberían ser cirujanos expertos con niveles predefinidos de competencia. Los datos disponibles en los estudios incluidos no fueron suficientes para realizar los pretendidos análisis detallados de subgrupo (ver Análisis de subgrupo e investigación de la heterogeneidad). Además, ningún estudio publicado apto para su inclusión permitió realizar los análisis pretendidos de una versus dos ligaduras ni del dispositivo de sellado LigaSure versus otros métodos; esto proporciona un campo de investigación para el futuro (ver Implicaciones para la investigación).
Sesgos potenciales en el proceso de revisión
Se siguió la guía proporcionada en el Manual Cochrane para Revisiones Sistemáticas de Intervenciones (Cochrane Handbook for Systematic Reviews of Interventions) (Higgins 2011a). No se aplicaron restricciones en cuanto al idioma, el estado de publicación ni el tamaño de la muestra. Se minimizó el sesgo en la selección de ensayos y sólo se incluyeron ECA. Puesto que no se aplicó ninguna restricción sobre la fecha de publicación, se incluyeron ensayos realizados antes de la imposición del registro obligatorio de ensayos. Por este motivo, existe la posibilidad de que no se hubiera informado acerca de algunos ensayos debido a la dirección de los resultados (sesgo de publicación). Además, la exclusión de ensayos que no cumplieron con los criterios de selección resultó en ocho estudios para inclusión en el metanálisis cuantitativo, una cantidad que fue insuficiente para generar gráficos de embudo para evaluar el sesgo de informe. (Sterne 2011).
Acuerdos y desacuerdos con otros estudios o revisiones
En los últimos años, diferentes autores han revisado este tema (Kazemier 2006; Sajid 2009; Shaikh 2015). De manera similar a nuestra revisión, las tres revisiones anteriores utilizaron un modelo de efectos aleatorios para metanalizar los estudios incluidos. Sin embargo, los criterios de elegibilidad para cada una de las tres revisiones fueron diferentes, lo cual significa que se incluyeron o excluyeron diferentes estudios en cada revisión. Tanto Kazemier 2006 como Sajid 2009 incluyeron sólo dos de los ocho ECA utilizados en la revisión (Ortega 1995; Shalaby 2001),pero también incluyeron varios estudios que se excluyeron en esta revisión por no proporcionar la solidez metodológica mínima definida por los criterios de elegibilidad; Kazemier 2006 incluyó Beldi 2006, Klima 1998 y Lange 1993, y Sajid 2009 incluyó Klima 1996, Klima 1998 y Lange 1993. Shaikh 2015 incluyó cuatro de los ocho ECA que se utilizaron en la revisión (Akbiyik 2011; Colak 2013; Delibegovic 2012; Gonenc 2012)pero incluyó tres estudios adicionales que no cumplieron los criterios de inclusión (Ates 2012; Delibegovic 2009; Hue 2012). Estas diferencias podrían explicar por qué las conclusiones extraídas por los respectivos autores de la revisión difieren tan radicalmente. Kazemier 2006 concluyó que el uso sistemático de grapadoras endoscópicas era favorable y Shaikh 2015 concluyó que el uso del Endoclip era sencillo, eficaz, seguro y una alternativa rentable, mientras que Sajid 2009 concluyó que, aunque el uso de Endoloop llevó más tiempo que el uso de Endo‐GIA, la duración de la estancia hospitalaria, las tasas de complicación perioperatoria y la incidencia de abscesos intrabdominales fueron iguales. Hasta donde se sabe, esta revisión sistemática es la más extensa en este campo hoy en día y sus resultados muestran que la evidencia actual no es suficiente para apoyar firmemente el uso sistemático de ningún método de cierre de muñón sobre otro durante la apendicectomía laparoscópica.

Data collection form (Microsoft Word).

*Lange 1993 was not retrievable following a worldwide search because the journal was published and is going out of print (see Results section).
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 1 Total complications.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications.
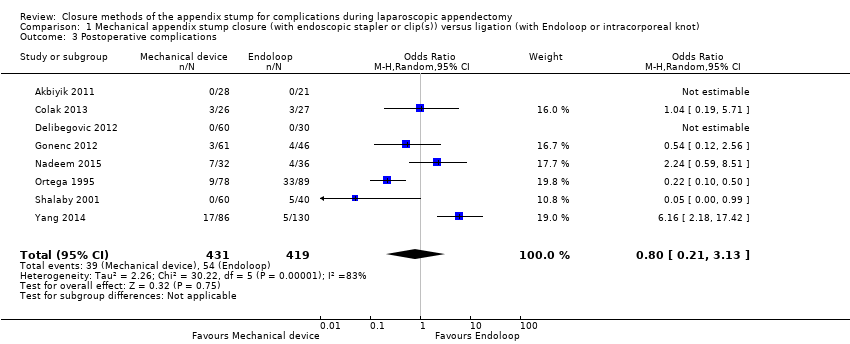
Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 3 Postoperative complications.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between mechanical device and ligature.
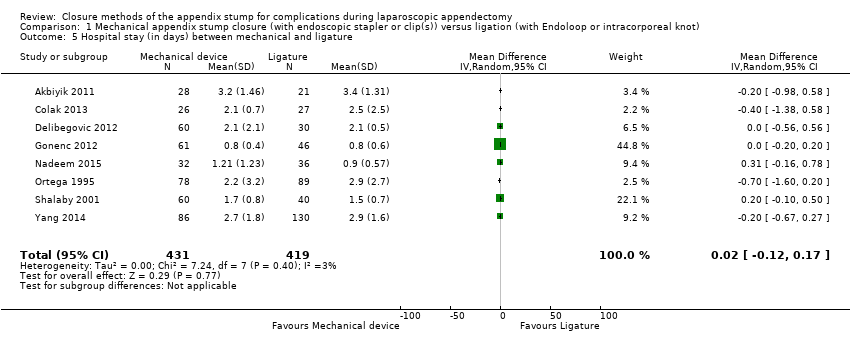
Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 5 Hospital stay (in days) between mechanical and ligature.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections.
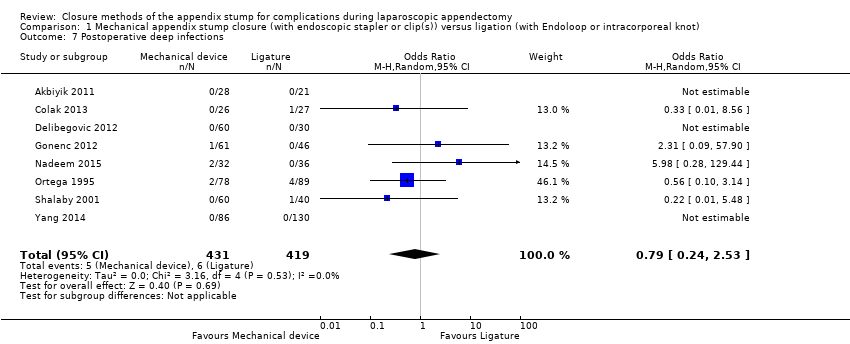
Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus.
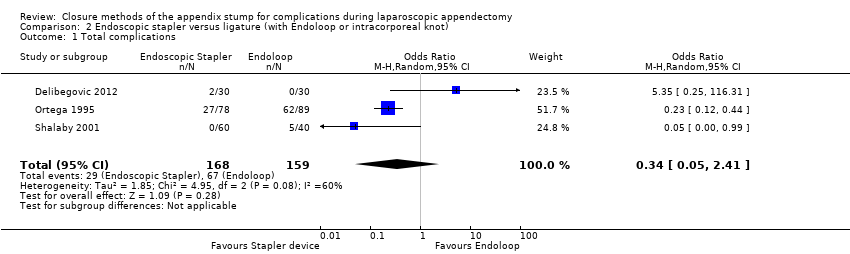
Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 1 Total complications.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 3 Postoperative complications.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between stapler and ligature.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 5 Comparison of hospital stay between stapler and ligature.
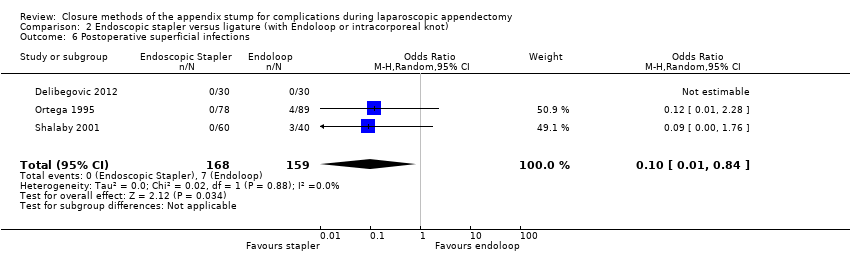
Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections.
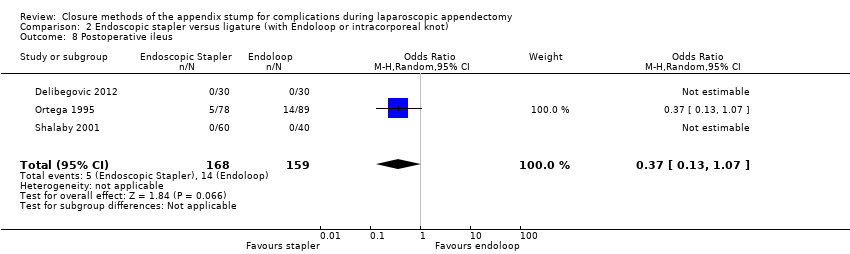
Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 1 Total complications.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications.
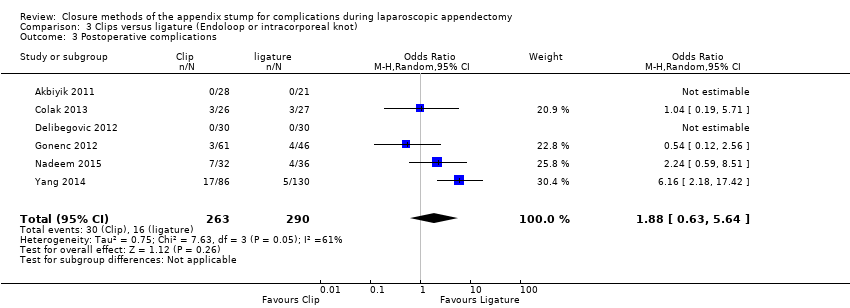
Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 3 Postoperative complications.
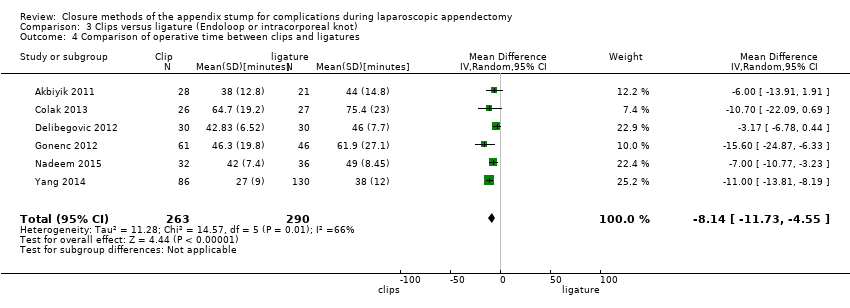
Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between clips and ligatures.
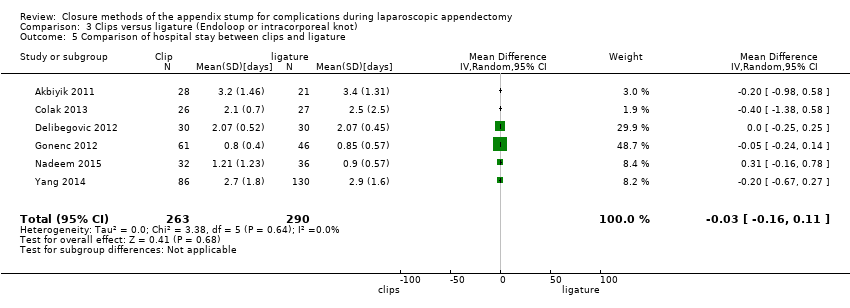
Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 5 Comparison of hospital stay between clips and ligature.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus.

Comparison 4 Endoscopic stapler versus clips, Outcome 1 Total complications.

Comparison 4 Endoscopic stapler versus clips, Outcome 2 Intraoperative complications.

Comparison 4 Endoscopic stapler versus clips, Outcome 3 Postoperative complications.

Comparison 4 Endoscopic stapler versus clips, Outcome 4 Comparison of operative time between stapler and clips.
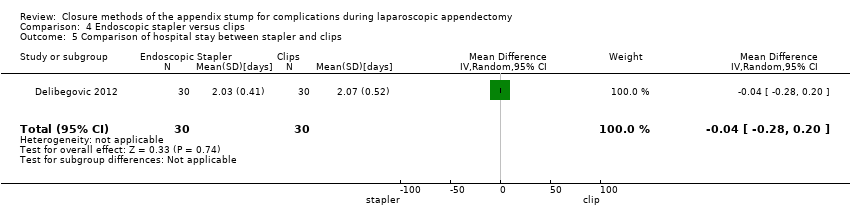
Comparison 4 Endoscopic stapler versus clips, Outcome 5 Comparison of hospital stay between stapler and clips.

Comparison 4 Endoscopic stapler versus clips, Outcome 6 Postoperative superficial infections.

Comparison 4 Endoscopic stapler versus clips, Outcome 7 Postoperative deep infections.
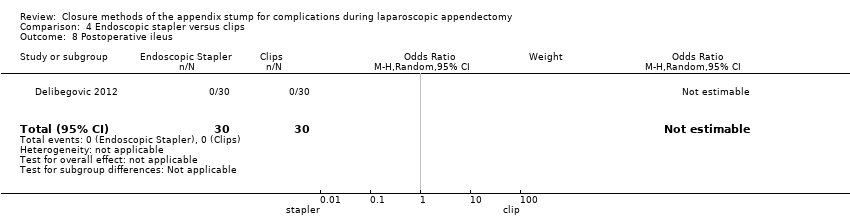
Comparison 4 Endoscopic stapler versus clips, Outcome 8 Postoperative ileus.
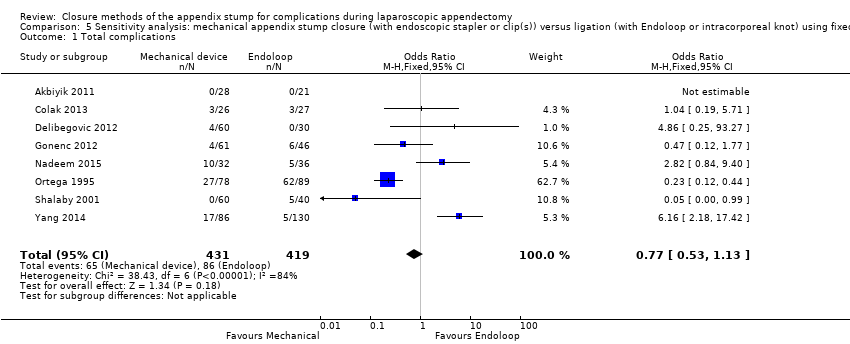
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications.
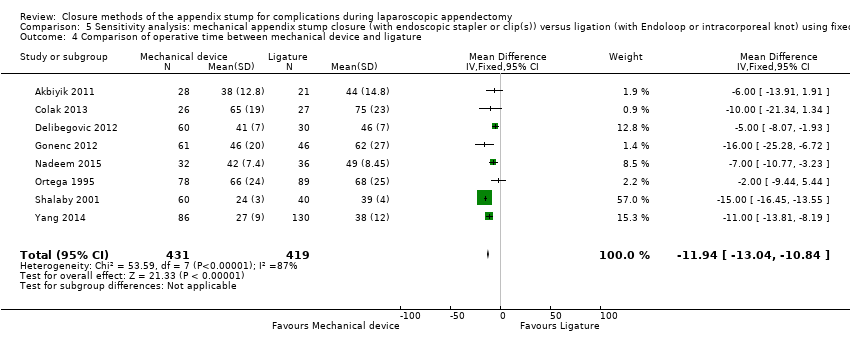
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between mechanical device and ligature.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Hospital stay (in days) between mechanical device and ligature.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections.
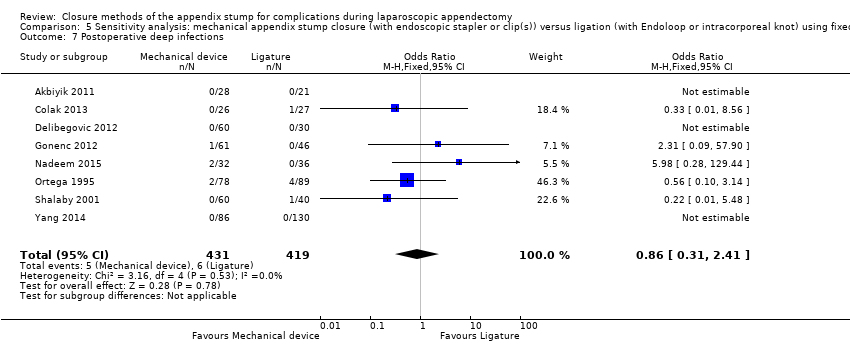
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections.
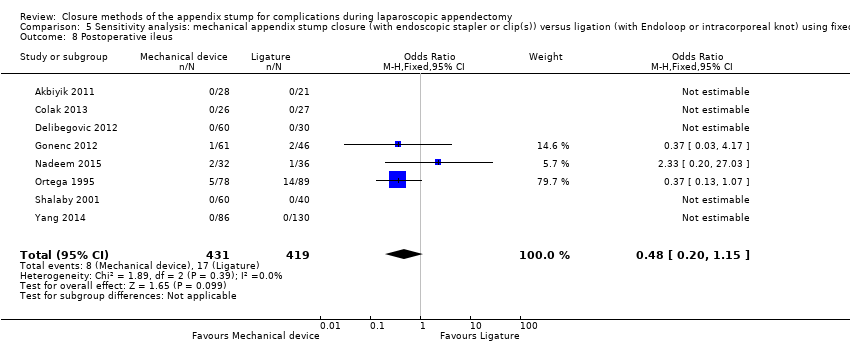
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications.
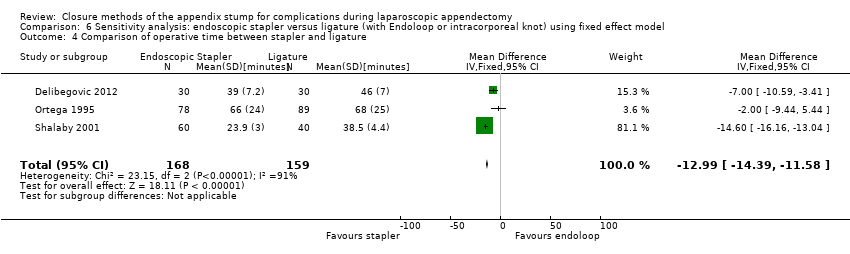
Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between stapler and ligature.
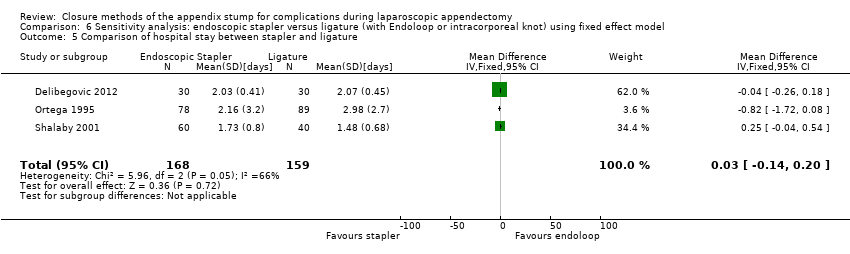
Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Comparison of hospital stay between stapler and ligature.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus.
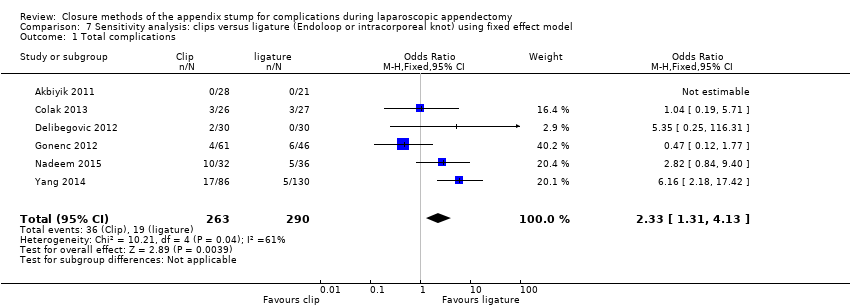
Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications.
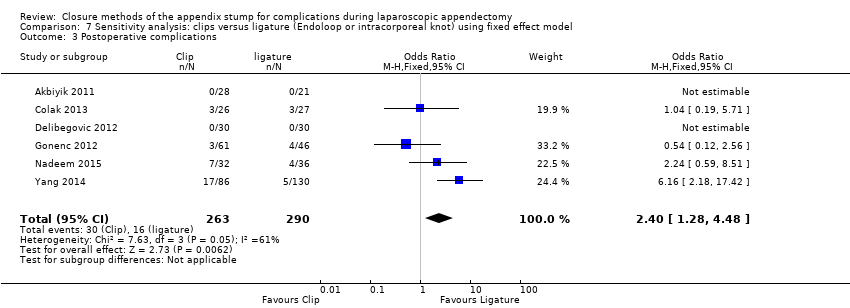
Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between clips and ligature.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Comparison of hospital stay between clips and ligature.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections.
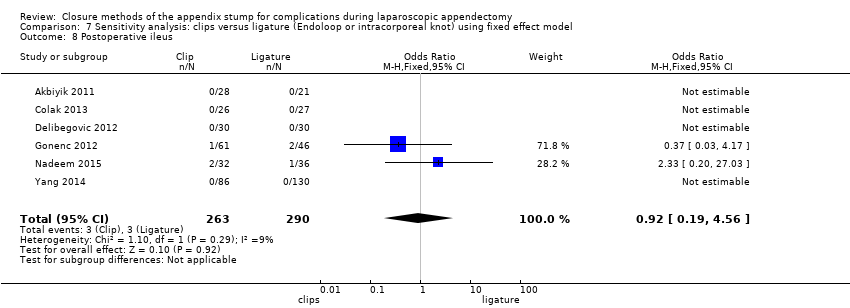
Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 1 Total complications.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 2 Intraoperative complications.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 3 Postoperative complications.
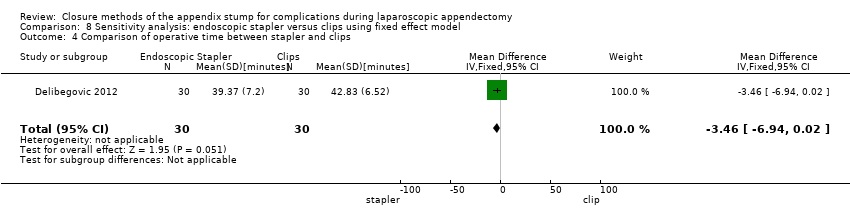
Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 4 Comparison of operative time between stapler and clips.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 5 Comparison of hospital stay between stapler and clips.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 6 Postoperative superficial infections.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 7 Postoperative deep infections.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 8 Postoperative ileus.
| Mechanical devices vs ligatures for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligatures | Risk with mechanical devices | ||||
| Total complications | 205 per 1000 | 169 per 1000 | OR 0.97 (0.27 to 3.50) | 850 | ⊕⊝⊝⊝ |
| Intraoperative complications | 76 per 1000 | 63 per 1000 | OR 0.93 (0.34 to 2.55) | 850 | ⊕⊝⊝⊝ |
| Postoperative complications | 129 per 1000 | 109 per 1000 | OR 0.80 (0.21 to 3.13) | 850 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 26 per 1000 | 13 per 1000 | OR 0.58 | 850 | ⊕⊝⊝⊝ |
| Postoperative ileus | 41 per 1000 | 20 per 1000 | OR 0.47 | 850 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 14 per 1000 | 12 per 1000 | OR 0.79 | 850 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.6 minutes. | Mean operative time (minutes) in the intervention group was 9.04 minutes shorter (12.97 minutes shorter to 5.11 minutes shorter). | ‐ | 850 | ⊕⊝⊝⊝ |
| Hospital stay (days) | Mean hospital stay was 1.4 days. | Mean hospital stay in the intervention group was 0.02 days longer (0.12 days shorter to 0.17 days longer). | ‐ | 850 | ⊕⊝⊝⊝ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Endoscopic stapler vs ligature for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: endoscopic stapler Comparison: ligature | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligature | Risk with endoscopic stapler | ||||
| Total complications | 421 per 1000 | 198 per 1000 | OR 0.34 (0.05 to 2.41) | 327 | ⊕⊝⊝⊝ |
| Intraoperative complications | 182 per 1000 | 191 per 1000 | OR 1.06 (0.17 to 6.70) | 327 | ⊕⊝⊝⊝ |
| Postoperative complications | 239 per 1000 | 250 per 1000 | OR 0.20 (0.09 to 0.44) | 327 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 44 per 1000 | 47 per 1000 | OR 0.10 (0.01 to 0.84) | 327 | ⊕⊝⊝⊝ |
| Postoperative ileus | 88 per 1000 | 93 per 1000 | OR 0.37 (0.13 to 1.07) | 327 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 31 per 1000 | 33 per 1000 | OR 0.45 (0.10 to 2.08) | 327 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.6 minutes. | Mean operative time in the intervention group was 8.52 minutes lower (15.64 minutes shorter to 1.39 minutes shorter). | 327 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 1.9 days. | Mean hospital stay in the intervention group was 0.02 days longer (0.38 days shorter to 0.34 days longer). | 327 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Clips vs ligatures for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: clips Comparison: ligature | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligature | Risk with clips | ||||
| Total complications | 17 per 1000 | 18 per 1000 | OR 2.03 (0.71 to 5.84) | 553 | ⊕⊝⊝⊝ |
| Intraoperative complications | 21 per 1000 | 22 per 1000 | OR 1.74 (0.33 to 9.04) | 553 | ⊕⊝⊝⊝ |
| Postoperative complications | 17 per 1000 | 18 per 1000 | OR 1.88 (0.63 to 5.64) | 553 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 14 per 1000 | 15 per 1000 | OR 1.25 (0.32 to 4.90) | 553 | ⊕⊝⊝⊝ |
| Postoperative ileus | 10 per 1000 | 11 per 1000 | OR 0.92 (0.15 to 5.64) | 553 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 3 per 1000 | 4 per 1000 | OR 1.75 (0.28 to 10.93) | 553 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.0 minutes. | Mean operative time in the intervention group was 8.14 minutes shorter (11.73 minutes shorter to 4.55 minutes shorter). | 553 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 1.5 days. | Mean hospital stay in the intervention group was 0.03 days shorter (0.16 days shorter to 0.11 days longer). | 553 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Endoscopic stapler vs clips for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: endoscopic stapler Comparison: clips | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with clips | Risk with endoscopic stapler | ||||
| Total complications | 67 per 1000 | 70 per 1000 | OR 1.00 (0.13 to 7.60) | 60 | ⊕⊝⊝⊝ |
| Intraoperative complications | 67 per 1000 | 70 per 1000 | OR 1.00 (0.13 to 7.60) | [60 | ⊕⊝⊝⊝ |
| Postoperative complications | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative superficial infections | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative ileus | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative deep infections | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Operative time (minutes) | Mean operative time was 39.4 minutes. | Mean operative time in the intervention group was 3.46 minutes shorter (6.94 minutes shorter to 0.02 minutes longer). | 60 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 2.0 days. | Mean hospital stay in the intervention group was 0.04 days shorter (0.28 days shorter to 0.20 days longer). | 60 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for single study with limited sample size. bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (the sole included studies had few participants and therefore few events, resulting in wide confidence intervals, which limited the precision of estimates). | |||||
| Study ID | Intervention arms | Total no. with complications | Total no. without complications | Intraoperative | Postoperative | |||||||||||
| Bleeding | Intraoperative rupture of appendix | Intraoperative organ injury/ faecal soiling | Access‐related visceral injury | Other | Total | Surgical site infection (superficial) | Deep infection | Bleeding | Paralytic ileus | Purulent peritonitis | Other | Total | ||||
| Ortega 1995 | Endoscopic linear stapler (LAS) | 27 | 51 | 11 | 2 | 5 | 0 | 0 | 18 | 0 | 2 | 0 | 5 | 0 | 2a | 9 |
| 2× catgut ligatures (Endoloops) (LAL) | 62 | 27 | 14 | 4 | 11 | 0 | 0 | 29 | 4 | 4 | 0 | 14 | 0 | 11b | 33 | |
| Open appendectomy (OA) | 44 | 42 | 20 | 5 | 1 | 0 | 0 | 26 | 11 | 0 | 0 | 6 | 0 | 1c | 18 | |
| Akbiyik 2011 | Hem‐o‐lok clip (non‐absorbable polymeric clips) | 0 | 28 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ligaure (Endoloop) | 0 | 21 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Delibegovic 2012 | 45‐mm stapler | 2 | 28 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1 ligature (Endoloop) | 0 | 30 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 1 Hem‐o‐lok clip (non‐absorbable polymeric clips) | 2 | 28 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Beldi 2004 | 1 ligature (Endoloop) only at appendix base (1 other at 6 to 12 mm distally) | 5 | 104 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 2d | 5 |
| 2 ligatures (Endoloops) at base of appendix (1 other at 6 to 12 mm distally) | 5 | 94 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 1e | 5 | |
| Sucullu 2009 | Endodissector and endoclip | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| LigaSure 5 to 10 mm | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Shalaby 2001 | Endo GIA (Ethicon Endo‐Surgery, Cincinnati, Ohio, USA) stapler | 0 | 60 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ligature (Endoloop) | 5 | 35 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 0 | 0 | 0 | 1f | 5 | |
| Extracorporeal laparoscopically assisted appendectomy | 6 | 44 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 4 | |
| Colak 2013 | Hem‐o‐lok (non‐absorbable polymeric clips) | 3 | 23 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 1g | 3 |
| Ligature (Endoloop) | 3 | 24 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1g | 3 | |
| Gonenc 2012 | Titanium endoclip | 4 | 57 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 3 |
| Intracorporeal knotting | 6 | 40 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 2 | 1 | 0 | 4 | |
| Ates 2012 | Titanium endoclip | 8 | 22 | NS | NS | NS | NS | 1h | 7 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Intracorporeal knotting | 7 | 24 | NS | NS | NS | NS | 0 | 4 | 1 | 0 | 0 | 0 | 0 | 2i | 3 | |
| Yang 2014 | Intracorporeal knotting | 5 | 125 | 0 | NS | NS | NS | NS | 0 | NS | 0 | NS | NS | NS | 5j | 5 |
| Titanium hem‐o‐lok | 17 | 69 | 0 | NS | NS | NS | NS | 0 | NS | 0 | NS | NS | NS | 17k | 17 | |
| Nadeem 2015 | Extracorporeal knotting | 5 | 31 | 1 | NS | 0 | NS | NS | 1 | 2 | 0 | NS | 1 | NS | 1 | 4 |
| Metallic endoclip | 10 | 22 | 2 | NS | 1 | NS | NS | 3 | 2 | 2 | NS | 2 | NS | 1l | 7 | |
| NS: non‐significant. | ||||||||||||||||
| Mechanical appendix stump closure (with endoscopic stapler or clip(s)) vs ligation (with Endoloop or intra/extracorporeal knot) | |||||||||
| Odds ratio (95% CI) | Risk ratio (95% CI) | Risk difference (95% CI) | Mean difference (95% CI) | ||||||
| Outcome | Fixed effect | Random effects | Fixed effect | Random effects | Fixed effect | Random effects | Fixed effect | Random effects | |
| Total complications | 0.77 (0.53 to 1.13) | 0.97 (0.27 to 3.50) | 0.83 (0.64 to 1.08) | 1.09 (0.41 to 2.88) | ‐0.03 (‐0.08 to 0.01) | ‐0.02 (‐0.12 to 0.09) | ‐ | ‐ | |
| Intraoperative complications | 0.81 (0.45 to 1.46) | 0.93 (0.34 to 2.55) | 0.85 (0.53 to 1.35) | 0.93 (0.40 to 2.18) | ‐0.01 (‐0.04 to 0.02) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative complications | 0.80 (0.52 to 1.24) | 0.80 (0.21 to 3.13) | 0.83 (0.57 to 1.19) | 0.86 (0.27 to 2.74) | ‐0.02 (‐0.06 to 0.02) | ‐0.02 (‐0.10 to 0.06) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐11.94 (‐13.04 to ‐10.84) | ‐9.04 (‐12.97 to ‐5.11) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.02 (‐0.12 to 0.16) | 0.02 (‐0.12 to 0.17) | |
| Postoperative superficial infections | 0.47 (0.17 to 1.26) | 0.58 (0.18 to 1.93) | 0.48 (0.19 to 1.24) | 0.61 (0.19 to 1.93) | ‐0.02 (‐0.04 to 0.01) | ‐0.01 (‐0.02 to 0.01) | ‐ | ‐ | |
| Postoperative ileus | 0.48 (0.20 to 1.15) | 0.47 (0.19 to 1.18) | 0.51 (0.23 to 1.14) | 0.50 (0.22 to 1.17) | ‐0.02 (‐0.04 to 0.01) | ‐0.01 (‐0.03 to 0.02) | ‐ | ‐ | |
| Postoperative deep infections | 0.86 (0.31 to 2.41) | 0.79 (0.24 to 2.53) | 0.87 (0.32 to 2.35) | 0.79 (0.25 to 2.47) | ‐0.00 (‐0.02 to 0.02) | ‐0.00 (‐0.02 to 0.01) | ‐ | ‐ | |
| Endoscopic stapler vs ligature | |||||||||
| Total complications | 0.26 (0.14 to 0.46) | 0.34 (0.05 to 2.41) | 0.49 (0.35 to 0.68) | 0.51 (0.09 to 2.84) | ‐0.21 (‐0.29 to ‐0.12) | ‐0.13 (‐0.40 to 0.14) | ‐ | ‐ | |
| Intraoperative complications | 0.72 (0.38 to 1.39) | 1.06 (0.17 to 6.70) | 0.79 (0.48 to 1.28) | 1.07 (0.22 to 5.19) | ‐0.04 (‐0.11 to 0.04) | ‐0.00 (‐0.11 to 0.10) | ‐ | ‐ | |
| Postoperative complications | 0.19 (0.09 to 0.41) | 0.20 (0.09 to 0.44) | 0.27 (0.14 to 0.51) | 0.25 (0.08 to 0.75) | ‐0.17 (‐0.24 to ‐0.10) | ‐0.12 (‐0.34 to 0.09) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐12.94 (‐14.35 to ‐11.53) | ‐8.36 (‐15.68 to ‐1.03) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.03 (‐0.14 to 0.20) | ‐0.02 (‐0.38 to 0.34) | |
| Postoperative superficial infections | 0.10 (0.01 to 0.86) | 0.10 (0.01 to 0.84) | 0.11 (0.01 to 0.88) | 0.11 (0.01 to 0.87) | ‐0.05 (‐0.08 to ‐0.01) | ‐0.04 (‐0.08 to 0.00) | ‐ | ‐ | |
| Postoperative ileus | 0.37 (0.13 to 1.07) | 0.37 (0.13 to 1.07) | 0.41 (0.15 to 1.08) | 0.41 (0.15 to 1.08) | ‐0.05 (‐0.10 to 0.00) | ‐0.02 ( ‐0.10 to 0.05) | ‐ | ‐ | |
| Postoperative deep infections | 0.45 (0.10 to 2.02) | 0.45 (0.10 to 2.08) | 0.46 (0.11 to 1.95) | 0.47 (0.11 to 2.04) | ‐0.02 (‐0.05 to 0.02) | ‐0.02 (‐0.05 to 0.02) | ‐ | ‐ | |
| Endoscopic stapler vs clips | |||||||||
| Total complications | 1.00 (0.13 to 7.60) | 1.00 (0.13 to 7.60) | 1.00 (0.15 to 6.64) | 1.00 (0.15 to 6.64) | 0.00 (‐0.13 to 0.13) | 0.00 (‐0.13 to 0.13) | ‐ | ‐ | |
| Intraoperative complications | 1.00 (0.13 to 7.60) | 1.00 (0.13 to 7.60) | 1.00 (0.15 to 6.64) | 1.00 (0.15 to 6.64) | 0.00 (‐0.13 to 0.13) | 0.00 (‐0.13 to 0.13) | ‐ | ‐ | |
| Postoperative complications | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐3.46 (‐6.94 to 0.02) | ‐3.46 (‐6.94 to 0.02) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.04 (‐0.28 to 0.20) | ‐0.04 [‐0.28, 0.20] | |
| Postoperative superficial infections | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Postoperative ileus | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Postoperative deep infections | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Clips vs ligature (Endoloop and intra/extracorporeal knot) | |||||||||
| Total complications | 2.33 (1.31 to 4.13) | 2.03 (0.71 to 5.84) | 2.11 (1.29 to 3.47) | 1.84 (0.73 to 4.62) | 0.08 (0.03 to 0.13) | 0.05 (‐0.03 to 0.13) | ‐ | ‐ | |
| Intraoperative complications | 1.79 (0.49 to 6.56) | 1.74 (0.33 to 9.04) | 1.76 (0.51 to 6.01) | 1.69 (0.35 to 8.19) | 0.01 (‐0.02 to 0.04) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative complications | 2.40 (1.28 to 4.48) | 1.88 (0.63 to 5.64) | 2.20 (1.27 to 3.82) | 1.75 (0.66 to 4.61) | 0.07 (0.02 to 0.12) | 0.03 (‐0.04 to 0.11) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐8.06 (‐9.85 to ‐6.26) | ‐8.14 (‐11.73 to ‐4.55) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.03 (‐0.16 to 0.11) | ‐0.03 (‐0.16 to 0.11) | |
| Postoperative superficial infections | 1.27 (0.33 to 4.86) | 1.25 (0.32 to 4.90) | 1.25 (0.35 to 4.49) | 1.24 (0.34 to 4.56) | 0.00 (‐0.02 to 0.03) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative ileus | 0.92 (0.19 to 4.56) | 0.92 (0.15 to 5.64) | 0.92 (0.20 to 4.21) | 0.93 (0.16 to 5.33) | ‐0.00 (‐0.02 to 0.02) | ‐0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative deep infections | 1.79 (0.37 to 8.58) | 1.75 (0.28 to 10.93) | 1.77 (0.38 to 8.16) | 1.71 (0.28 to 10.28) | 0.01 (‐0.02 to 0.03) | 0.00 (‐0.01 to 0.02) | ‐ | ‐ | |
| CI: confidence interval; NE: not estimable; "‐": not applicable. | |||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.97 [0.27, 3.50] |
| 2 Intraoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.93 [0.34, 2.55] |
| 3 Postoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.80 [0.21, 3.13] |
| 4 Comparison of operative time between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Random, 95% CI) | ‐9.04 [‐12.97, ‐5.11] |
| 5 Hospital stay (in days) between mechanical and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.12, 0.17] |
| 6 Postoperative superficial infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.18, 1.93] |
| 7 Postoperative deep infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.79 [0.24, 2.53] |
| 8 Postoperative ileus Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.47 [0.19, 1.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.34 [0.05, 2.41] |
| 2 Intraoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 1.06 [0.17, 6.70] |
| 3 Postoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.20 [0.09, 0.44] |
| 4 Comparison of operative time between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Random, 95% CI) | ‐8.52 [‐15.64, ‐1.39] |
| 5 Comparison of hospital stay between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.38, 0.34] |
| 6 Postoperative superficial infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.10 [0.01, 0.84] |
| 7 Postoperative deep infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.45 [0.10, 2.08] |
| 8 Postoperative ileus Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.37 [0.13, 1.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 2.03 [0.71, 5.84] |
| 2 Intraoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.74 [0.33, 9.04] |
| 3 Postoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.88 [0.63, 5.64] |
| 4 Comparison of operative time between clips and ligatures Show forest plot | 6 | 553 | Mean Difference (IV, Random, 95% CI) | ‐8.14 [‐11.73, ‐4.55] |
| 5 Comparison of hospital stay between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.16, 0.11] |
| 6 Postoperative superficial infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.25 [0.32, 4.90] |
| 7 Postoperative deep infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.75 [0.28, 10.93] |
| 8 Postoperative ileus Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.15, 5.64] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 1.0 [0.13, 7.60] |
| 2 Intraoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 1.0 [0.13, 7.60] |
| 3 Postoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Comparison of operative time between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐3.46 [‐6.94, 0.02] |
| 5 Comparison of hospital stay between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.28, 0.20] |
| 6 Postoperative superficial infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Postoperative deep infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Postoperative ileus Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.53, 1.13] |
| 2 Intraoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.45, 1.46] |
| 3 Postoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.52, 1.24] |
| 4 Comparison of operative time between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Fixed, 95% CI) | ‐11.94 [‐13.04, ‐10.84] |
| 5 Hospital stay (in days) between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.12, 0.16] |
| 6 Postoperative superficial infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.17, 1.26] |
| 7 Postoperative deep infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.31, 2.41] |
| 8 Postoperative ileus Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.20, 1.15] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.14, 0.46] |
| 2 Intraoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.38, 1.39] |
| 3 Postoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.09, 0.41] |
| 4 Comparison of operative time between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Fixed, 95% CI) | ‐12.99 [‐14.39, ‐11.58] |
| 5 Comparison of hospital stay between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.14, 0.20] |
| 6 Postoperative superficial infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 0.86] |
| 7 Postoperative deep infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.10, 2.02] |
| 8 Postoperative ileus Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.13, 1.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.33 [1.31, 4.13] |
| 2 Intraoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.49, 6.56] |
| 3 Postoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.40 [1.28, 4.48] |
| 4 Comparison of operative time between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Fixed, 95% CI) | ‐8.06 [‐9.85, ‐6.26] |
| 5 Comparison of hospital stay between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.16, 0.11] |
| 6 Postoperative superficial infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.33, 4.86] |
| 7 Postoperative deep infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.37, 8.58] |
| 8 Postoperative ileus Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.19, 4.56] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.13, 7.60] |
| 2 Intraoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.13, 7.60] |
| 3 Postoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Comparison of operative time between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐3.46 [‐6.94, 0.02] |
| 5 Comparison of hospital stay between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.28, 0.20] |
| 6 Postoperative superficial infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Postoperative deep infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Postoperative ileus Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

