Métodos de cierre del muñón apendicular para complicaciones durante la apendicectomía laparoscópica
References
Referencias de los estudios incluidos en esta revisión
Referencias de los estudios excluidos de esta revisión
Referencias de los estudios en espera de evaluación
Referencias adicionales
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Jump to:
| Methods | Randomised controlled trial | |
| Participants | Number of participants: 49 Number of centres: 1 Mean age: not specified (age ranged from 1 to 15 years) Number of males: 32 Number of females: 17 Inclusion criteria: diagnosis of acute or perforated appendicitis between May 2008 and May 2009 Exclusion criteria: NS | |
| Interventions | Intervention arm: hem‐o‐lok clip (non‐absorbable polymeric clips) Control arm: ligature (Endoloop) Antibiotic use: not specified | |
| Outcomes | Primary outcome measures: intraoperative complications, postoperative complications, and postoperative radiological appearance Secondary outcome measures: cost, operative time, and hospital stay | |
| Notes | Level of seniority of operating surgeon: all participants operated on by a single surgeon | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "compared prospectively" Comment: information about the sequence generation process insufficient to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Information insufficient to permit judgement |
| Blinding of participants and personnel (performance bias) | High risk | It is unclear whether participants were aware of the method used. Personnel would likely be aware from operative records. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Personnel would likely be aware which study group participants had been assigned to on the basis of postoperative imaging findings and operative records. |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | Quote: "Patients were followed up for a period of 1 week to 1 year". Comment: Follow‐up period varied from 1 week to 1 year. No uniform longer‐term outcome data were available for comparison between arms. Additionally, no a priori publication of intended outcomes was identified from either a published trial protocol or trial registration. |
| Other bias | Low risk | This study appears to be free of other sources of bias. |
| Methods | Randomised controlled trial | |
| Participants | Number of participants: 53 Number of centres: 1 Mean age: 29 years Number of males: 28 Number of females: 25 Inclusion criteria:diagnosis of acute appendicitis and admission to General Surgery Department of Samsun Education and Research Hospital between September 2010 and July 2011 Exclusion criteria: < 16 years of age, previous major abdominal operations, pregnancy, refusal to consent to participation in the study, and conversion to open appendectomy | |
| Interventions | Intervention arm: hem‐o‐lok (non‐absorbable polymeric clips) Control arm: ligature (Endoloop) Antibiotic use: prophylactic dose of third‐generation cephalosporin given intravenously after GA induction | |
| Outcomes | Primary outcome measures: intraoperative complications Secondary outcome measures: operative time and surgical findings | |
| Notes | Level of seniority of operating surgeon: The same surgical team (level of seniority not specified) performed all operations. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patients randomly allocated" Comment: computer randomisation method used |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was conducted by using a computer‐generated randomisation schedule". Comment: probably done |
| Blinding of participants and personnel (performance bias) | High risk | It is unclear whether participants were aware of the method used. Personnel would likely be aware from operative records. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information insufficent to allow judgement, but personnel would likely be aware from operative records. |
| Incomplete outcome data (attrition bias) | High risk | Four participants excluded postoperatively owing to conversion to open appendectomy, and 3 participants owing to loss of follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No a priori publication of intended outcomes was identified from either a published trial protocol or trial registration. |
| Other bias | Low risk | This study appears to be free of other sources of bias. |
| Methods | Randomised controlled trial | |
| Participants | Number of participants: 90 Number of centres: 1 Mean age: 27 years Number of males: 48 Number of female: 42 Inclusion criteria: diagnosis of acute appendicitis and admission to General Surgery Department of University Clinic Center Tuzla, between January 2010 and May 2011 Exclusion criteria: NS | |
| Interventions | Intervention arm 1: 45‐mm stapler Intervention arm 2: 1 hem‐o‐lok clip (non‐absorbable polymeric clips) Control arm: 1 ligature (Endoloop) Antibiotic use: NS | |
| Outcomes | Primary outcome measures: intraoperative complications and postoperative complications Secondary outcome measures: cost, operative time, and hospital stay | |
| Notes | Level of seniority of operating surgeon not specified | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly divided" Comment: method of randomisation not explicitly specified |
| Allocation concealment (selection bias) | Unclear risk | Not specified, but investigator likely to be aware of allocation pattern |
| Blinding of participants and personnel (performance bias) | High risk | It is unclear whether participants were aware of the method used. Personnel would likely be aware from operative records. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information insufficient to allow judgement, but personnel would likely be aware from operative records. |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | No a priori publication of intended outcomes was identified from either a published trial protocol or trial registration. |
| Other bias | Low risk | This study appears to be free of other sources of bias. |
| Methods | Randomised controlled trial | |
| Participants | Number of participants: 107 Number of centres: 1 Mean age: 27 years Number of males: 61 Number of females: 56 Inclusion criteria: all those given diagnosis of acute appendicitis between December 2010 and May 2011 Exclusion criteria: unwillingness to participate, inability to give informed consent (mental disabilities), age < 15 years, pregnancy, preference for the open procedure, severe sepsis or septic shock on admission, medical or technical contraindication for laparoscopy, American Society of Anesthesiologists class III and IV, intraoperative diagnosis of complicated appendicitis, conversion to an open procedure, and normal appendix at histopathological examination | |
| Interventions | Intervention arm: titanium endoclip Control arm: intracorporeal knotting Antibiotic use: single dose of cefuroxime axetil (1500 mg, intravenously) during GA induction | |
| Outcomes | Primary outcome measures: postoperative complications, including re‐admissions, rehospitalisations, and reoperations Secondary outcome measures: operative time, intraoperative complications, and length of hospital stay | |
| Notes | Level of seniority of operating surgeon: All operations were performed by the residents, who were at least within their second year, under the supervision of the chief resident or the attending surgeon. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was done by the lottery method". Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote: "One of the residents who had no idea about the preoperative data and who would not join the operation was chosen as the card picker". Comment: probably done |
| Blinding of participants and personnel (performance bias) | High risk | It is unclear whether participants were aware of the method used. Personnel would likely be aware from operative records. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information insufficient to allow judgement, but personnel would likely be aware from operative records. |
| Incomplete outcome data (attrition bias) | Unclear risk | Quote: "Patients on intraoperative diagnosis of complicated appendicitis or open appendectomy were excluded from the study". Comment: information on exclusion process insufficient to allow judgement |
| Selective reporting (reporting bias) | Unclear risk | No a priori publication of intended outcomes was identified from either a published trial protocol or trial registration. |
| Other bias | Low risk | This study appears to be free of other sources of bias. |
| Methods | Randomised controlled trial | |
| Participants | Number of participants: 68 Number of centres: 3 Mean age: 24 years Number of males: 37 Number of females: 31 Inclusion criteria: undergoing laparoscopic appendectomy in 3 tertiary care hospitals in Peshawar from 1 June 2013 to 1 June 2014 Exclusion criteria: perforation of appendix, local and diffuse peritonitis, friable appendix base, evidence of pelvic inflammatory disease, conversion to open procedure, and possible other diagnoses | |
| Interventions | Intervention arm: metallic endoclip Control arm: extracorporeal ligature tie Antibiotic use: oral cefixime for 5 to 7 days | |
| Outcomes | Primary outcome measures: bleeding, organ injury, postoperative ileus, intra‐abdominal infection, surgical site infection, re‐admission, and reoperation Secondary outcome measures: cost, operative time, and hospital stay | |
| Notes | Level of seniority of operating surgeon: All participants underwent minimal access surgery performed by certified surgeons with more than 10 years' experience in laparoscopic procedures. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomised controlled trial" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "were divided randomly into two groups" Comment: no information on allocation method available to allow judgement |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "single‐blinded" Comment: This is a drawback of these types of trials, as it is impossible to blind surgeons to the procedure; however, single‐blinded suggests that participants were not aware of the method used. Personnel would likely be aware from operative records. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The residents/intern present at the time of procedure would collect the data on data sheets with no blinded |
| Incomplete outcome data (attrition bias) | Low risk | No participants were lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No a priori publication of intended outcomes was identified from either a published trial protocol or trial registration. |
| Other bias | Low risk | This study appears to be free of other sources of bias. |
| Methods | Randomised controlled trial | |
| Participants | Number of participants: 253 Number of centres: 10 Mean age: 25 years Number of males: 180 Number of females: 73 Inclusion criteria: clinical diagnosis of appendicitis or lower quadrant pain of uncertain etiology and suitable candidates for laparoscopy and laparotomy Exclusion criteria: pregnancy, minors, prisoners, or incapable of providing informed consent | |
| Interventions | Intervention arm 1: endoscopic linear stapler (LAS) Intervention arm 2: open appendectomy (OA) Control arm: 2× catgut ligatures (Endoloops) (LAL) Antibiotic use: NS | |
| Outcomes | Primary outcome measures: intraoperative blood loss, fragmentation of appendix, faecal soilage of abdomen, postoperative abscess, vomiting, ileus, wound infection, and re‐admissions Secondary outcome measures: operative time, pain, length of stay, and resumption of activity | |
| Notes | Level of seniority of operating surgeon: All participants were operated on by residents with attending surgeons experienced in laparoscopic and open surgical techniques. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was executed". Comment: computer randomisation method used |
| Allocation concealment (selection bias) | High risk | Quote: "computer‐generated random numbers table administered centrally via a toll‐free telephone connection" Comment: probably done Quote: "endoscopic staplers were temporarily unavailable (...), 5 patients with LAS underwent appendectomies with pre‐tied loops" Comment: probably done |
| Blinding of participants and personnel (performance bias) | High risk | It is unclear whether participants were aware of the method used. Personnel would likely be aware from operative records. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "Data collection was performed in a prospective fashion using two standardized data sheets". Comment: probably done |
| Incomplete outcome data (attrition bias) | High risk | Quote: "Endoscopic staplers were temporarily unavailable at one point during the study, 5 patients randomised to LAS underwent appendectomies with pre‐tied loops". |
| Selective reporting (reporting bias) | Unclear risk | No a priori publication of intended outcomes was identified from either a published trial protocol or trial registration. |
| Other bias | Unclear risk | Quote: "A subgroup of 134 patients at one institution were evaluated using a visual analogue pain scale" Comment: insufficient rationale that an identified problem will introduce bias |
| Methods | Randomised controlled trial | |
| Participants | Number of participants: 150 Number of centres: 2 Mean age: 10 years Number of males: 67 Number of females: 83 Inclusion criteria: diagnosis of acute appendicitis from October 1997 to October 1999 Exclusion criteria: NS | |
| Interventions | Intervention arm 1: Endo GIA (Ethicon Endo‐Surgery, Cincinnati, Ohio, USA) stapler Intervention arm 2: extracorporeal laparoscopically assisted appendectomy Control arm: ligature (Endoloop) Antibiotic use: 50 mg/kg ceftriaxone preoperatively, then 1 or 2 doses postoperatively. Metronidazole 25 mg/kg to those with suppurative and gangrenous appendicitis | |
| Outcomes | Primary outcome measures: residual abscess, wound infection, bleeding, and intestinal obstruction Secondary outcome measures: cost, operative time, and hospital stay | |
| Notes | Level of seniority of operating surgeon not specified | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomly assigned to one of the groups using a table of random numbers. The randomisation procedure was not restricted". |
| Allocation concealment (selection bias) | Unclear risk | Information insufficient to allow judgement |
| Blinding of participants and personnel (performance bias) | High risk | It is unclear whether participants were aware of the method used. Personnel would likely be aware from operative records. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information insufficient to allow judgement, but personnel would likely be aware from operative records. |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | No a priori publication of intended outcomes was identified from either a published trial protocol or trial registration. |
| Other bias | Low risk | This study appears to be free of other sources of bias. |
| Methods | Randomised controlled trial | |
| Participants | Number of participants: 216 Number of centres: 1 Mean age: NS Number of males: NS Number of females: NS Inclusion criteria: undergoing laparoscopic appendectomy from July 2004 to June 2013 Exclusion criteria: NS | |
| Interventions | Intervention arm: titanium hem‐o‐lok Control arm: extracorporeal knotting Antibiotic use: NS | |
| Outcomes | Primary outcome measures: operation time, amount of bleeding, intestinal function recovery time, and hospital stay after operation and complications Secondary outcome measures: NS | |
| Notes | Published paper translated from Chinese Level of seniority of operating surgeon not specified | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly divided" |
| Allocation concealment (selection bias) | Unclear risk | Information insufficient to allow judgement |
| Blinding of participants and personnel (performance bias) | High risk | Blinding unlikely to have been in place appropriately |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information insufficient to allow judgement |
| Incomplete outcome data (attrition bias) | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | No a priori publication of intended outcomes was identified from either a published trial protocol or trial registration. |
| Other bias | Unclear risk | Information insufficient to allow judgement |
GA: gestational age.
NS: not specified.
Characteristics of excluded studies [ordered by study ID]
Jump to:
| Study | Reason for exclusion |
| Quasi‐randomised trial | |
| Quasi‐randomised trial | |
| Quasi‐randomised trial |
Characteristics of studies awaiting assessment [ordered by study ID]
Jump to:
| Methods | Randomised controlled trial |
| Participants | Number of participants: 1100 Number of centres: 1 Mean age: 37 years Number of males: 505 Number of females: 595 Inclusion criteria: undergoing laparoscopic appendectomy from April 2012 to February 2015 with appendicular base < 12 mm in diameter, and acute appendicitis (except in cases of perforation or a gangrenous base). Patients with malignant appendicular diseases including carcinoid tumours, adenocarcinoma, and mucinous adenocarcinoma (confirmed by pathology) were excluded, and a randomised label given to the next patient. Exclusion criteria: conversion to open surgery or malignant appendicular disease |
| Interventions | Intervention arm: absorbable polymeric surgical clips (Lapro‐Clips) Control arm: non‐absorbable polymeric clips (hem‐o‐lok clips) Antibiotic use: not specified |
| Outcomes | Primary outcome measures 1. Postoperative complications including intra‐abdominal abscess, superficial wound infection, appendicular stump leakage, and postoperative abdominal pain (defined as abdominal complaints after surgery requiring prolonged clinical observation or additional biochemical or radiological tests) 2. Re‐interventions including percutaneous and/or transrectal drainage, reoperation (laparoscopy/laparotomy), and prolonged use of intravenous antibiotics (> 3 to 5 days) 3. Duration of the operation (time from skin incision to skin closure), duration of hospital stay, and re‐admission (duration of a re‐admission was included in the hospital stay calculation) |
| Notes | Level of seniority of operating surgeon not specified, but states, "All surgeons participating in this study could perform appendicular closure with Lapro‐Clips or Hemo‐ |
| Methods | Randomised controlled trial |
| Participants | Number of participants: 76 Number of centres: 1 Mean age: 37 years Number of males: 34 Number of females: 42 Inclusion criteria: undergoing laparoscopic appendectomy between 1 March 2013 and 25 May 2015, after receiving clinical diagnosis of acute appendicitis Exclusion criteria: conversion to open surgery or malignant appendicular disease, pain longer than 4 days, mass in the right lower quadrant area identified during examination, phlegmon in images or peritonitis symptoms, underwent surgery that turned into open laparoscopic owing to adhesion and improper anatomical conditions |
| Interventions | Intervention arm: absorbable polymeric surgical clips (Lapro‐Clips) Control arm: non‐absorbable polymeric clips (Hem‐o‐lok clips) Antibiotic use: not specified |
| Outcomes | Primary outcome measures: operative time (minutes), hospital stay (days), wound infection, surgical site pain, technical complications, stump leak, reoperations |
| Notes | Level of seniority of operating surgeon not specified, but states, "all operations were performed by single surgeon" |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.97 [0.27, 3.50] |
| Analysis 1.1  Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 1 Total complications. | ||||
| 2 Intraoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.93 [0.34, 2.55] |
| Analysis 1.2  Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications. | ||||
| 3 Postoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.80 [0.21, 3.13] |
| Analysis 1.3 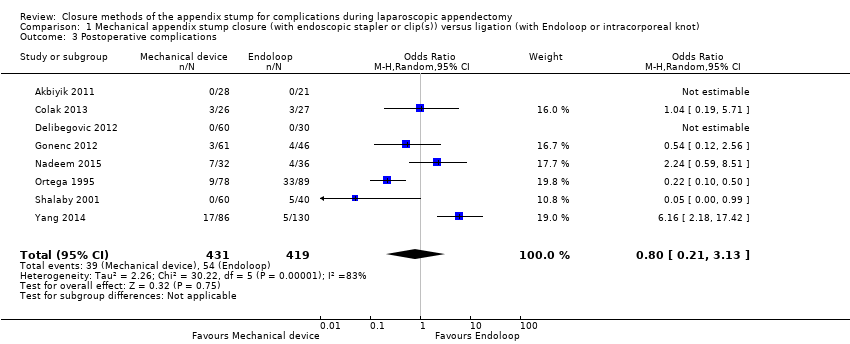 Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 3 Postoperative complications. | ||||
| 4 Comparison of operative time between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Random, 95% CI) | ‐9.04 [‐12.97, ‐5.11] |
| Analysis 1.4  Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between mechanical device and ligature. | ||||
| 5 Hospital stay (in days) between mechanical and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.12, 0.17] |
| Analysis 1.5 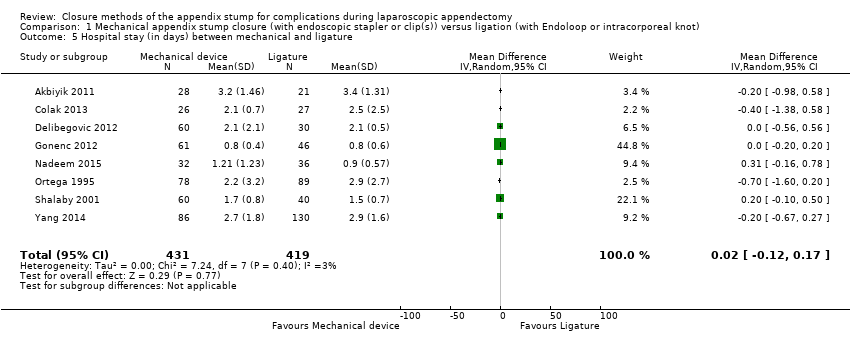 Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 5 Hospital stay (in days) between mechanical and ligature. | ||||
| 6 Postoperative superficial infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.18, 1.93] |
| Analysis 1.6  Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections. | ||||
| 7 Postoperative deep infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.79 [0.24, 2.53] |
| Analysis 1.7 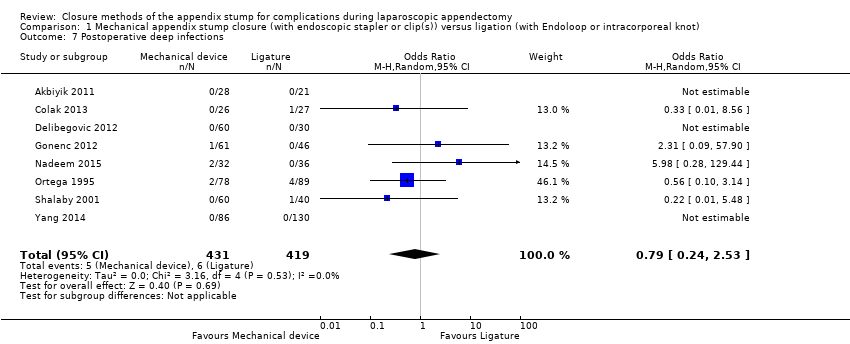 Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections. | ||||
| 8 Postoperative ileus Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.47 [0.19, 1.18] |
| Analysis 1.8  Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.34 [0.05, 2.41] |
| Analysis 2.1 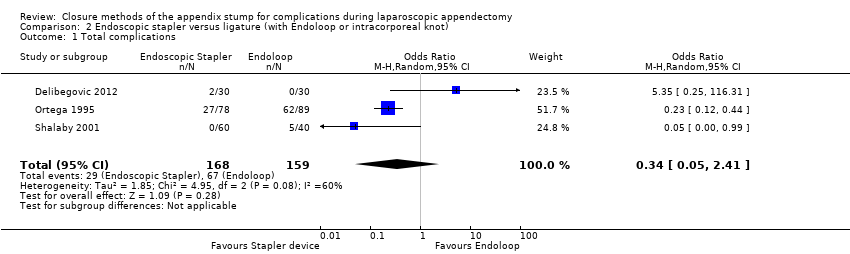 Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 1 Total complications. | ||||
| 2 Intraoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 1.06 [0.17, 6.70] |
| Analysis 2.2  Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications. | ||||
| 3 Postoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.20 [0.09, 0.44] |
| Analysis 2.3  Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 3 Postoperative complications. | ||||
| 4 Comparison of operative time between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Random, 95% CI) | ‐8.52 [‐15.64, ‐1.39] |
| Analysis 2.4  Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between stapler and ligature. | ||||
| 5 Comparison of hospital stay between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.38, 0.34] |
| Analysis 2.5  Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 5 Comparison of hospital stay between stapler and ligature. | ||||
| 6 Postoperative superficial infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.10 [0.01, 0.84] |
| Analysis 2.6 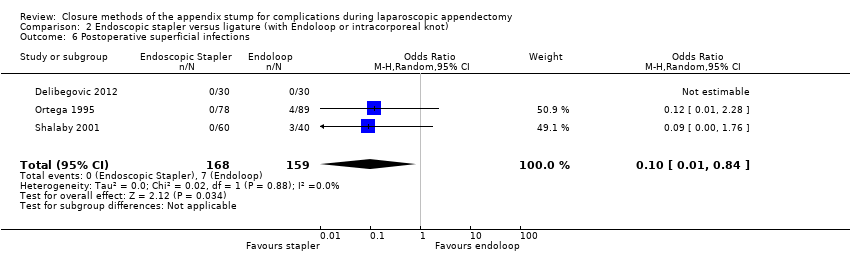 Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections. | ||||
| 7 Postoperative deep infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.45 [0.10, 2.08] |
| Analysis 2.7  Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections. | ||||
| 8 Postoperative ileus Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.37 [0.13, 1.07] |
| Analysis 2.8 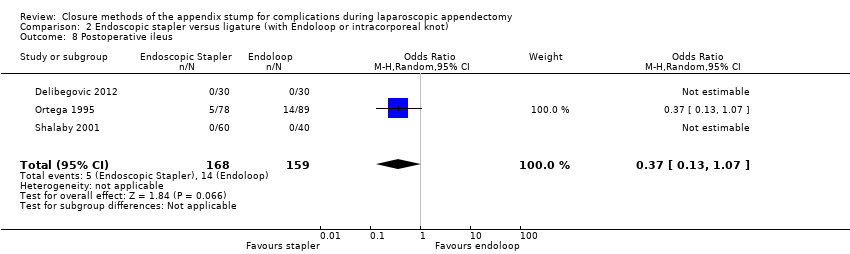 Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 2.03 [0.71, 5.84] |
| Analysis 3.1  Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 1 Total complications. | ||||
| 2 Intraoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.74 [0.33, 9.04] |
| Analysis 3.2  Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications. | ||||
| 3 Postoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.88 [0.63, 5.64] |
| Analysis 3.3 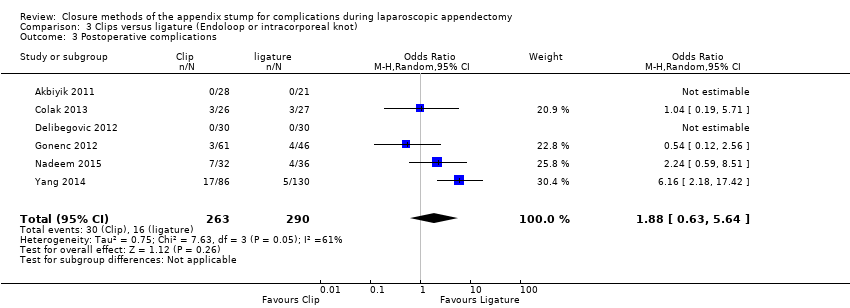 Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 3 Postoperative complications. | ||||
| 4 Comparison of operative time between clips and ligatures Show forest plot | 6 | 553 | Mean Difference (IV, Random, 95% CI) | ‐8.14 [‐11.73, ‐4.55] |
| Analysis 3.4 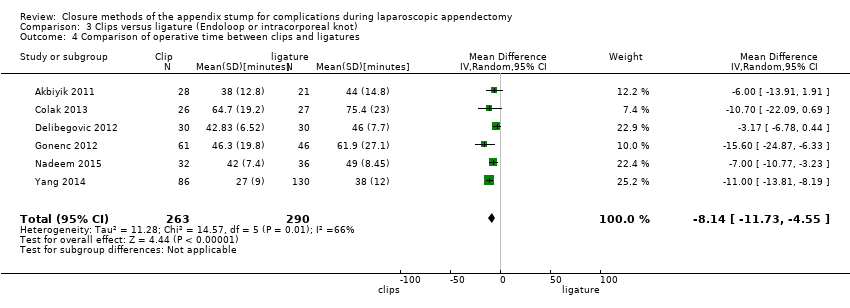 Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between clips and ligatures. | ||||
| 5 Comparison of hospital stay between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.16, 0.11] |
| Analysis 3.5 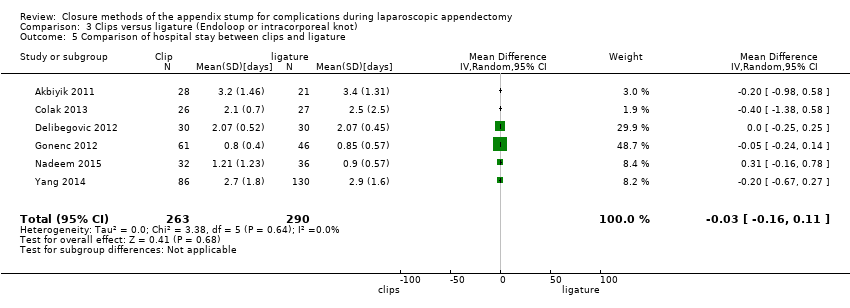 Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 5 Comparison of hospital stay between clips and ligature. | ||||
| 6 Postoperative superficial infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.25 [0.32, 4.90] |
| Analysis 3.6  Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections. | ||||
| 7 Postoperative deep infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.75 [0.28, 10.93] |
| Analysis 3.7  Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections. | ||||
| 8 Postoperative ileus Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.15, 5.64] |
| Analysis 3.8  Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 1.0 [0.13, 7.60] |
| Analysis 4.1  Comparison 4 Endoscopic stapler versus clips, Outcome 1 Total complications. | ||||
| 2 Intraoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 1.0 [0.13, 7.60] |
| Analysis 4.2  Comparison 4 Endoscopic stapler versus clips, Outcome 2 Intraoperative complications. | ||||
| 3 Postoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 4.3  Comparison 4 Endoscopic stapler versus clips, Outcome 3 Postoperative complications. | ||||
| 4 Comparison of operative time between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐3.46 [‐6.94, 0.02] |
| Analysis 4.4  Comparison 4 Endoscopic stapler versus clips, Outcome 4 Comparison of operative time between stapler and clips. | ||||
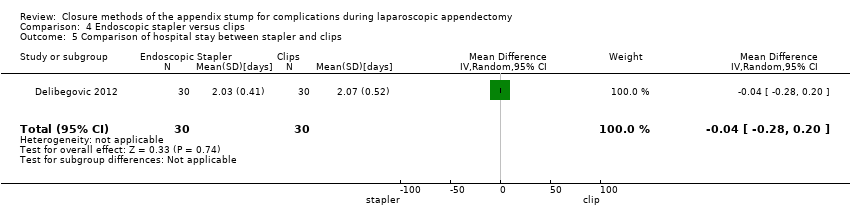
| 5 Comparison of hospital stay between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.28, 0.20] |
| Analysis 4.5 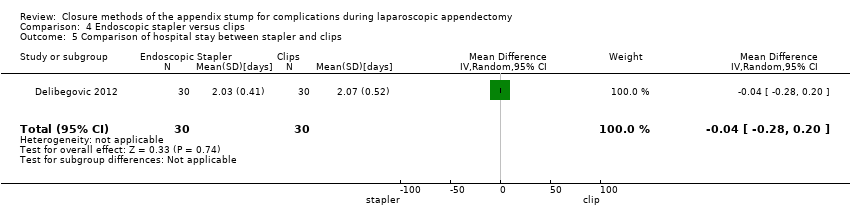 Comparison 4 Endoscopic stapler versus clips, Outcome 5 Comparison of hospital stay between stapler and clips. | ||||
| 6 Postoperative superficial infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 4.6  Comparison 4 Endoscopic stapler versus clips, Outcome 6 Postoperative superficial infections. | ||||
| 7 Postoperative deep infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 4.7  Comparison 4 Endoscopic stapler versus clips, Outcome 7 Postoperative deep infections. | ||||
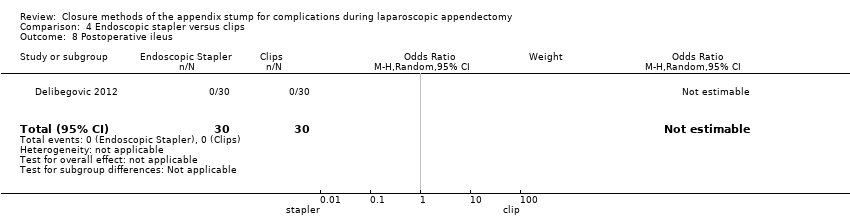
| 8 Postoperative ileus Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 4.8 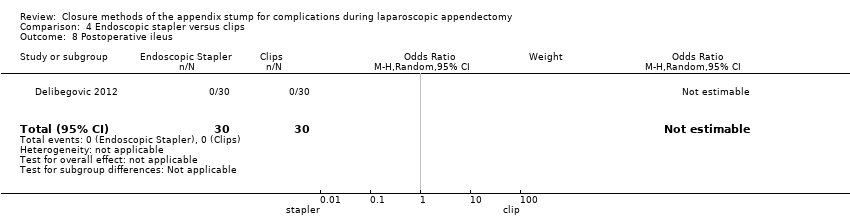 Comparison 4 Endoscopic stapler versus clips, Outcome 8 Postoperative ileus. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.53, 1.13] |
| Analysis 5.1 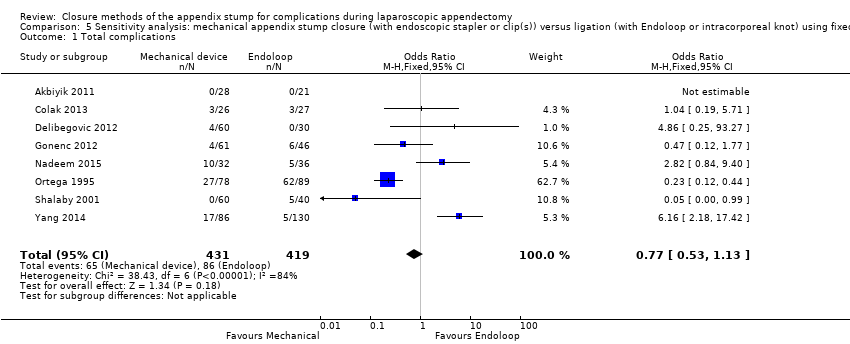 Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications. | ||||
| 2 Intraoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.45, 1.46] |
| Analysis 5.2  Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications. | ||||
| 3 Postoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.52, 1.24] |
| Analysis 5.3  Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications. | ||||
| 4 Comparison of operative time between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Fixed, 95% CI) | ‐11.94 [‐13.04, ‐10.84] |
| Analysis 5.4 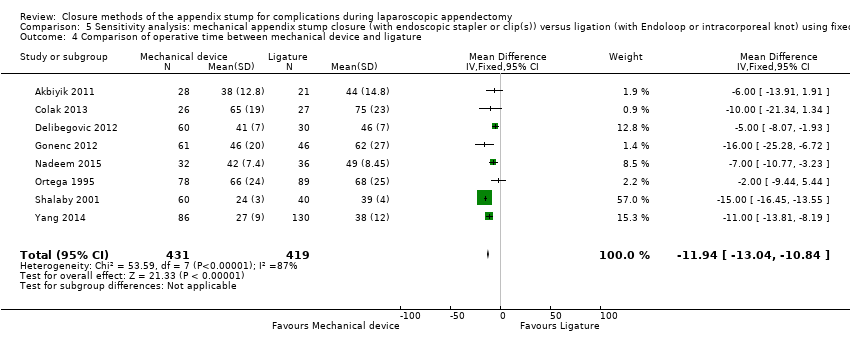 Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between mechanical device and ligature. | ||||
| 5 Hospital stay (in days) between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.12, 0.16] |
| Analysis 5.5  Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Hospital stay (in days) between mechanical device and ligature. | ||||
| 6 Postoperative superficial infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.17, 1.26] |
| Analysis 5.6  Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections. | ||||
| 7 Postoperative deep infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.31, 2.41] |
| Analysis 5.7 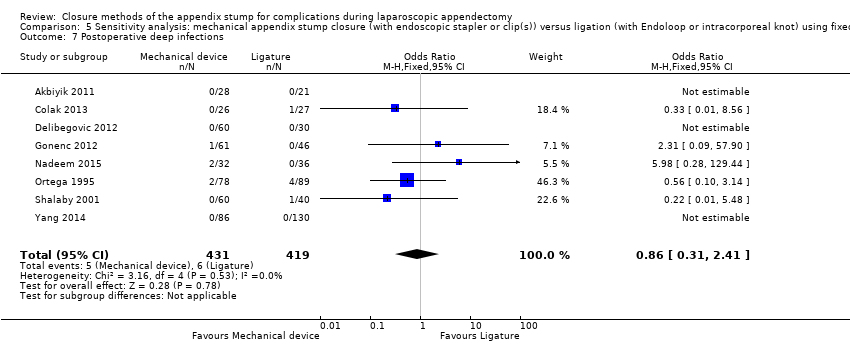 Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections. | ||||
| 8 Postoperative ileus Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.20, 1.15] |
| Analysis 5.8 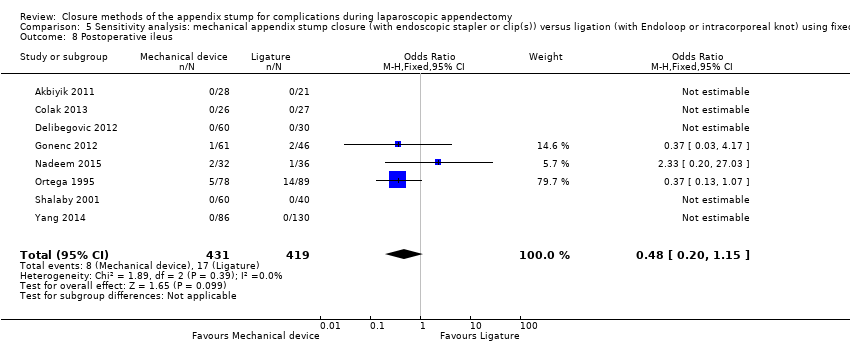 Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.14, 0.46] |
| Analysis 6.1  Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications. | ||||
| 2 Intraoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.38, 1.39] |
| Analysis 6.2  Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications. | ||||
| 3 Postoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.09, 0.41] |
| Analysis 6.3  Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications. | ||||
| 4 Comparison of operative time between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Fixed, 95% CI) | ‐12.99 [‐14.39, ‐11.58] |
| Analysis 6.4 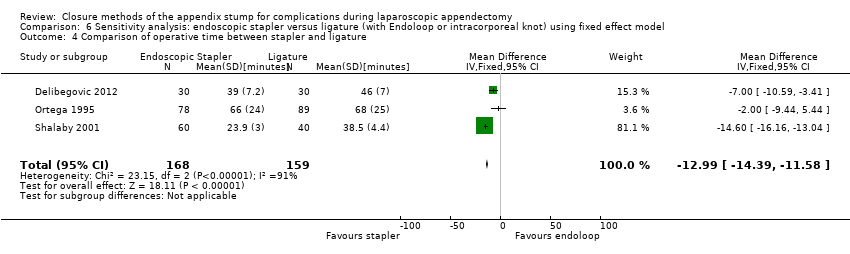 Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between stapler and ligature. | ||||
| 5 Comparison of hospital stay between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.14, 0.20] |
| Analysis 6.5 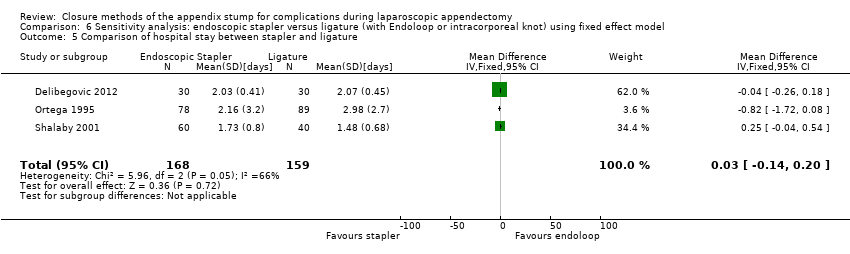 Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Comparison of hospital stay between stapler and ligature. | ||||
| 6 Postoperative superficial infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 0.86] |
| Analysis 6.6  Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections. | ||||
| 7 Postoperative deep infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.10, 2.02] |
| Analysis 6.7  Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections. | ||||
| 8 Postoperative ileus Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.13, 1.07] |
| Analysis 6.8  Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.33 [1.31, 4.13] |
| Analysis 7.1 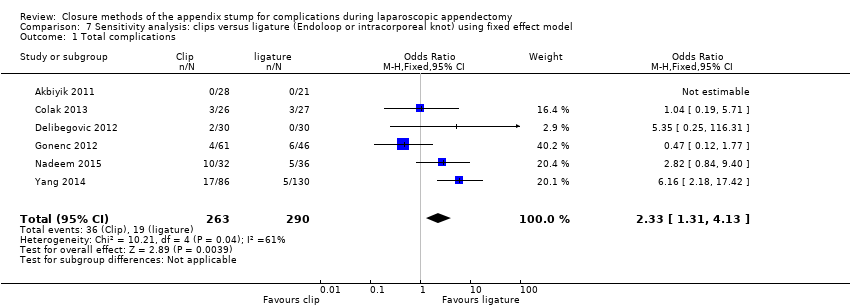 Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications. | ||||
| 2 Intraoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.49, 6.56] |
| Analysis 7.2  Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications. | ||||
| 3 Postoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.40 [1.28, 4.48] |
| Analysis 7.3 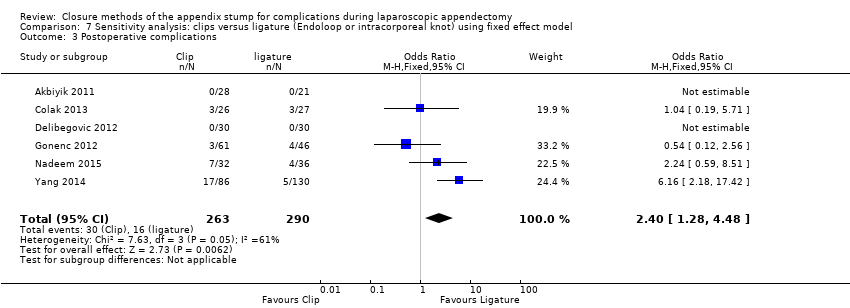 Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications. | ||||
| 4 Comparison of operative time between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Fixed, 95% CI) | ‐8.06 [‐9.85, ‐6.26] |
| Analysis 7.4  Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between clips and ligature. | ||||
| 5 Comparison of hospital stay between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.16, 0.11] |
| Analysis 7.5  Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Comparison of hospital stay between clips and ligature. | ||||
| 6 Postoperative superficial infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.33, 4.86] |
| Analysis 7.6  Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections. | ||||
| 7 Postoperative deep infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.37, 8.58] |
| Analysis 7.7  Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections. | ||||
| 8 Postoperative ileus Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.19, 4.56] |
| Analysis 7.8 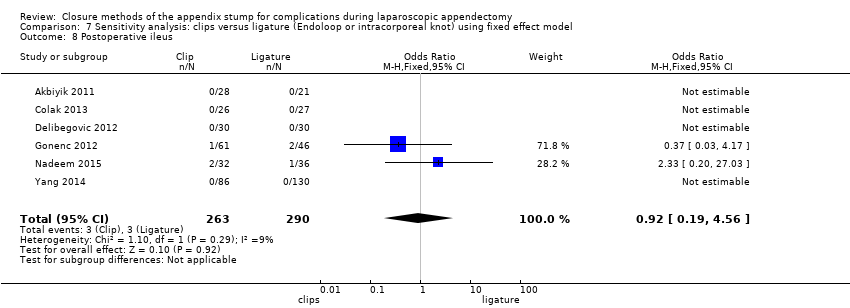 Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.13, 7.60] |
| Analysis 8.1  Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 1 Total complications. | ||||
| 2 Intraoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.13, 7.60] |
| Analysis 8.2  Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 2 Intraoperative complications. | ||||
| 3 Postoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 8.3  Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 3 Postoperative complications. | ||||
| 4 Comparison of operative time between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐3.46 [‐6.94, 0.02] |
| Analysis 8.4 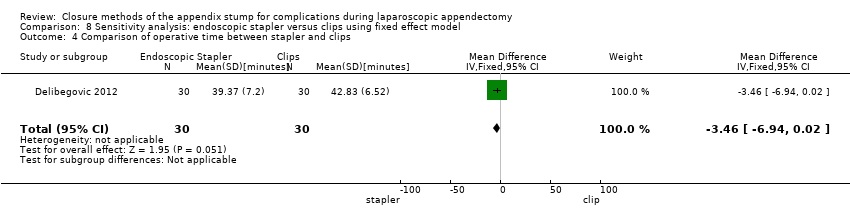 Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 4 Comparison of operative time between stapler and clips. | ||||
| 5 Comparison of hospital stay between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.28, 0.20] |
| Analysis 8.5  Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 5 Comparison of hospital stay between stapler and clips. | ||||
| 6 Postoperative superficial infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 8.6  Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 6 Postoperative superficial infections. | ||||
| 7 Postoperative deep infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 8.7  Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 7 Postoperative deep infections. | ||||
| 8 Postoperative ileus Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| Analysis 8.8  Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 8 Postoperative ileus. | ||||

Data collection form (Microsoft Word).

*Lange 1993 was not retrievable following a worldwide search because the journal was published and is going out of print (see Results section).
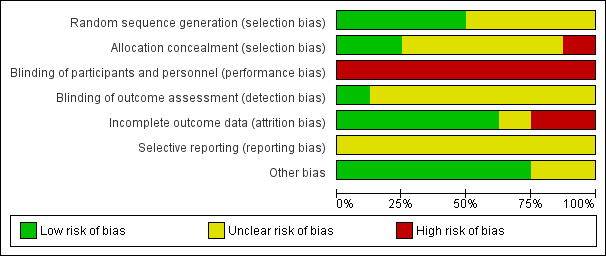
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
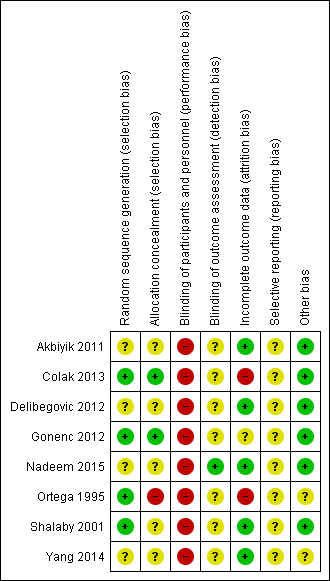
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 1 Total complications.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications.
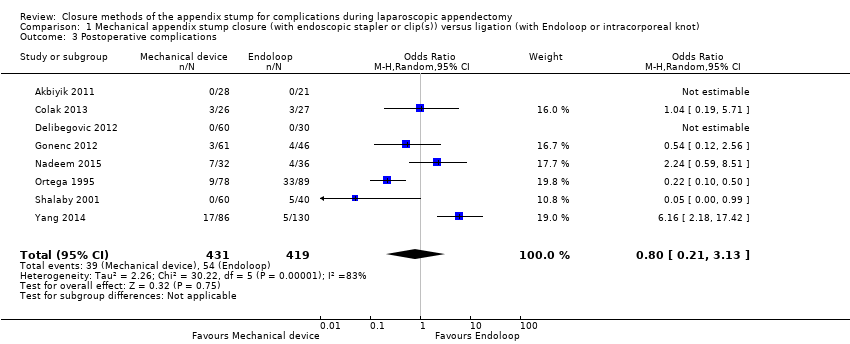
Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 3 Postoperative complications.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between mechanical device and ligature.
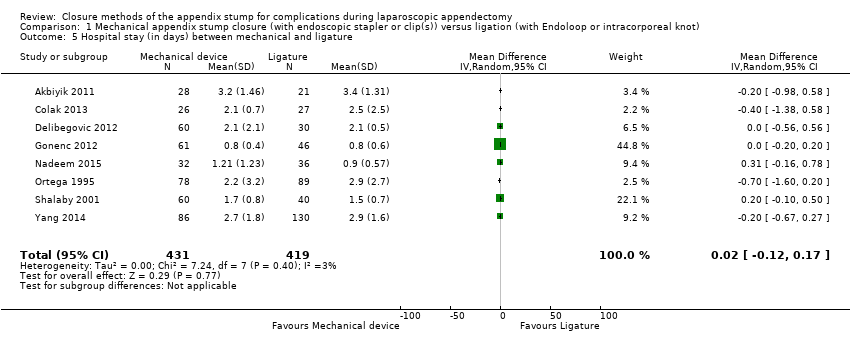
Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 5 Hospital stay (in days) between mechanical and ligature.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections.
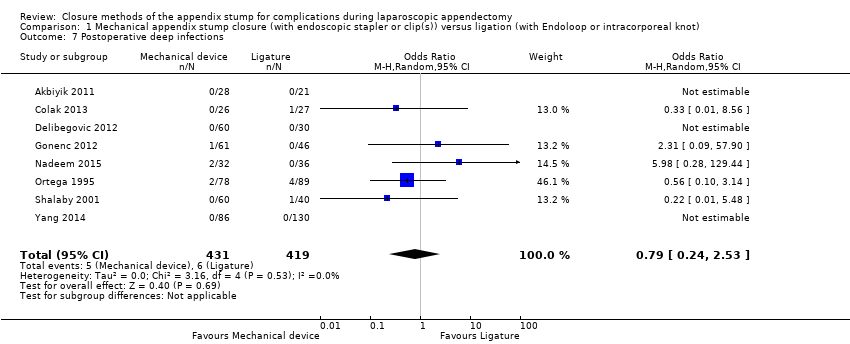
Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections.

Comparison 1 Mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus.
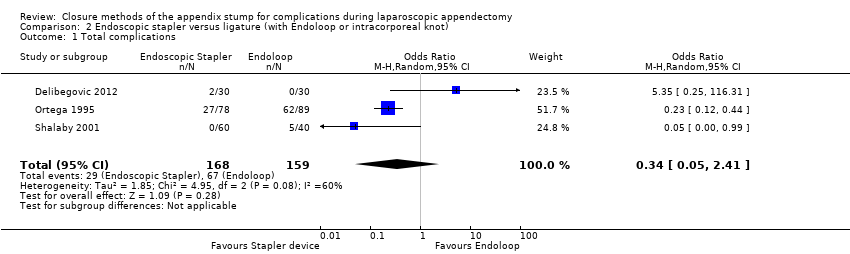
Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 1 Total complications.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 3 Postoperative complications.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between stapler and ligature.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 5 Comparison of hospital stay between stapler and ligature.
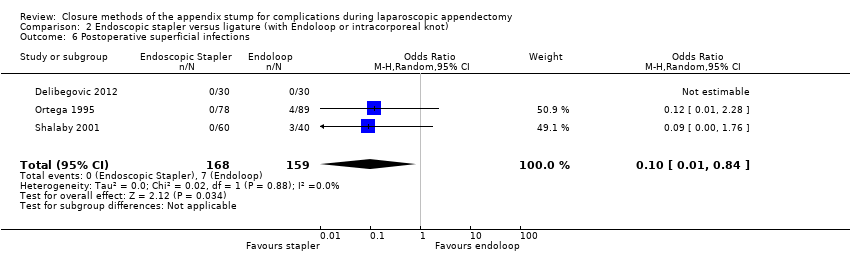
Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections.

Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections.
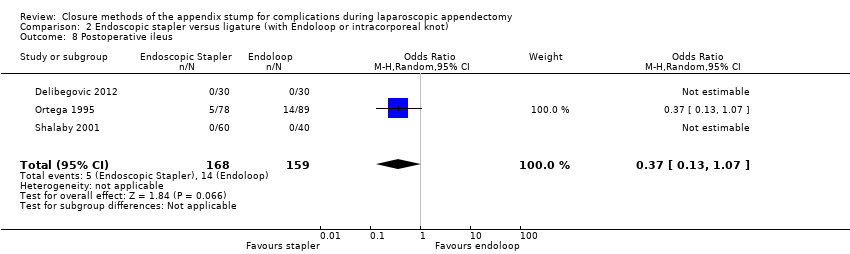
Comparison 2 Endoscopic stapler versus ligature (with Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 1 Total complications.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 2 Intraoperative complications.
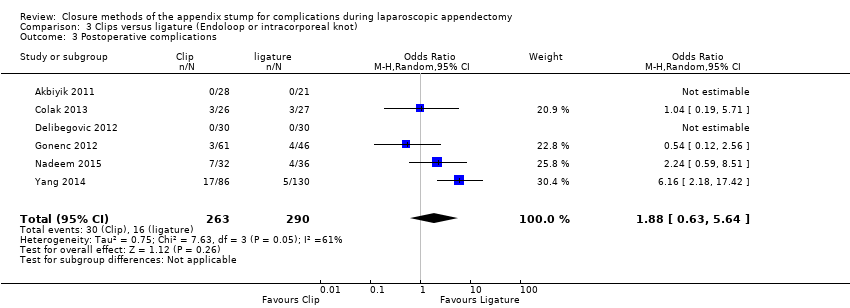
Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 3 Postoperative complications.
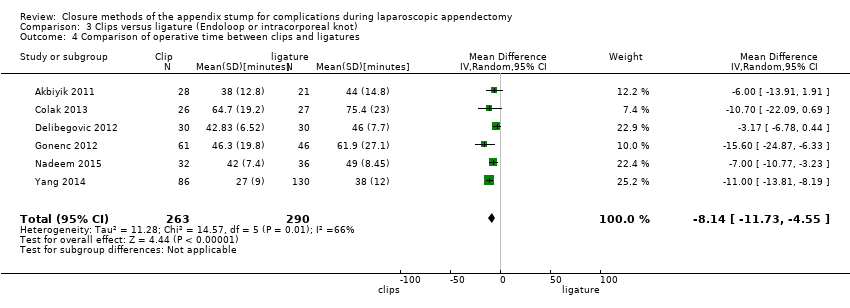
Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 4 Comparison of operative time between clips and ligatures.
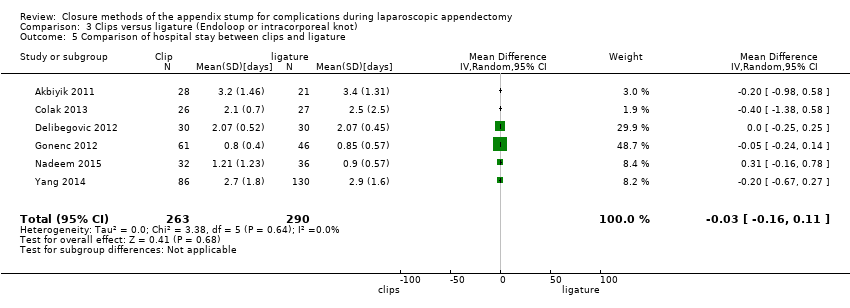
Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 5 Comparison of hospital stay between clips and ligature.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 6 Postoperative superficial infections.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 7 Postoperative deep infections.

Comparison 3 Clips versus ligature (Endoloop or intracorporeal knot), Outcome 8 Postoperative ileus.

Comparison 4 Endoscopic stapler versus clips, Outcome 1 Total complications.

Comparison 4 Endoscopic stapler versus clips, Outcome 2 Intraoperative complications.

Comparison 4 Endoscopic stapler versus clips, Outcome 3 Postoperative complications.

Comparison 4 Endoscopic stapler versus clips, Outcome 4 Comparison of operative time between stapler and clips.
Comparison 4 Endoscopic stapler versus clips, Outcome 5 Comparison of hospital stay between stapler and clips.

Comparison 4 Endoscopic stapler versus clips, Outcome 6 Postoperative superficial infections.

Comparison 4 Endoscopic stapler versus clips, Outcome 7 Postoperative deep infections.
Comparison 4 Endoscopic stapler versus clips, Outcome 8 Postoperative ileus.
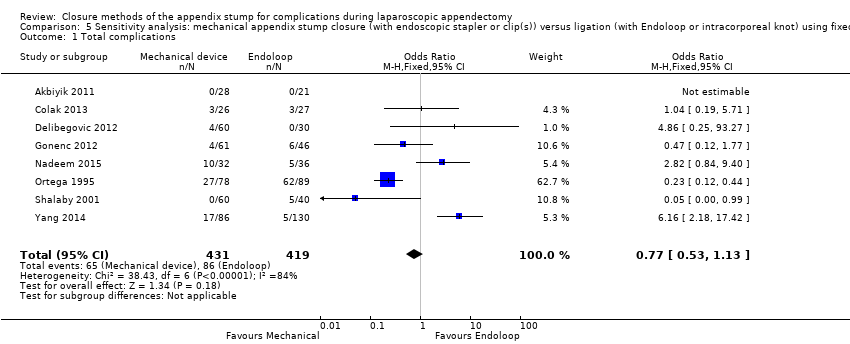
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications.
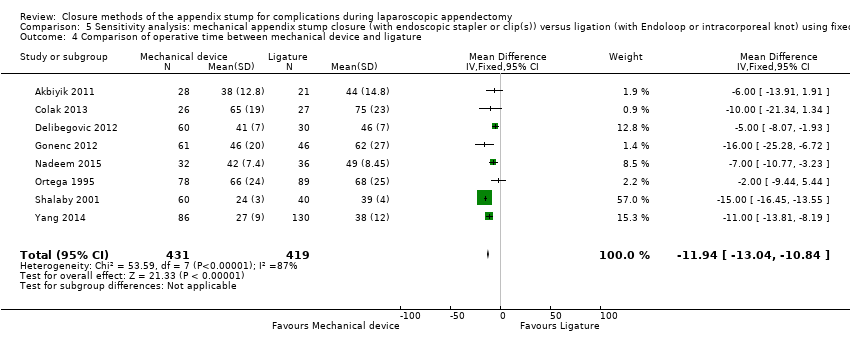
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between mechanical device and ligature.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Hospital stay (in days) between mechanical device and ligature.

Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections.
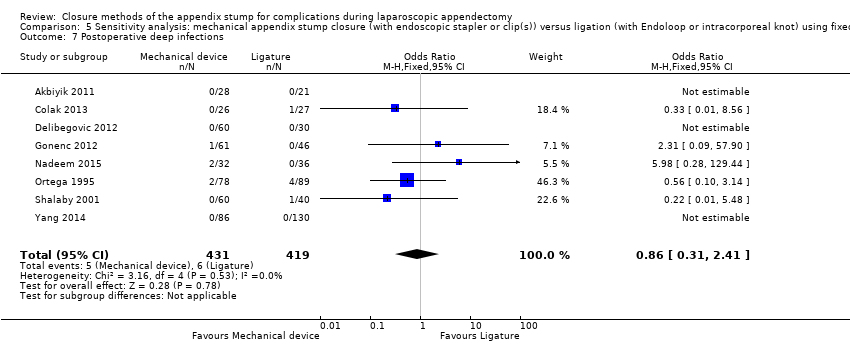
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections.
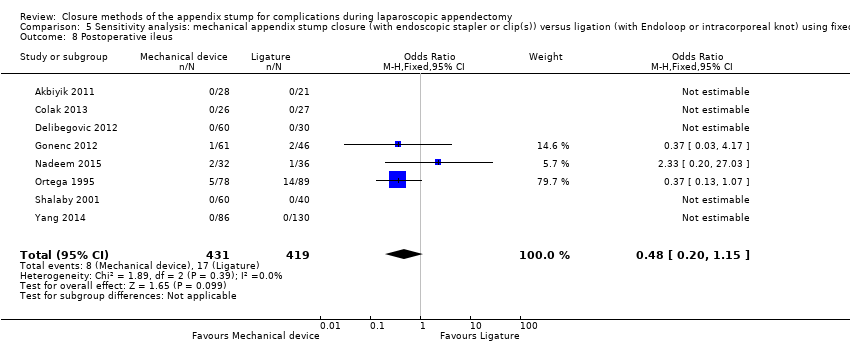
Comparison 5 Sensitivity analysis: mechanical appendix stump closure (with endoscopic stapler or clip(s)) versus ligation (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications.
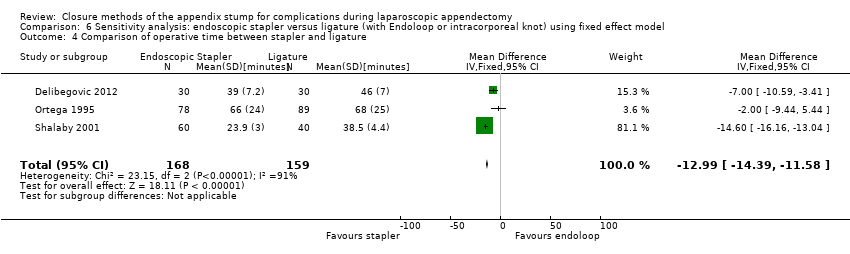
Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between stapler and ligature.
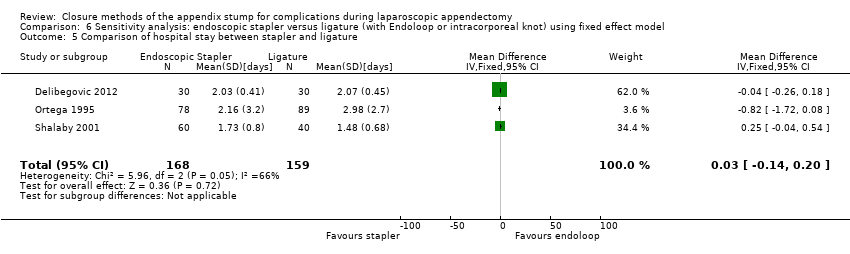
Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Comparison of hospital stay between stapler and ligature.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections.

Comparison 6 Sensitivity analysis: endoscopic stapler versus ligature (with Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus.
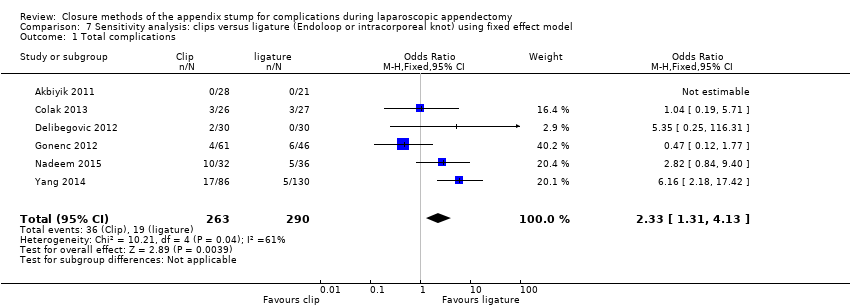
Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 1 Total complications.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 2 Intraoperative complications.
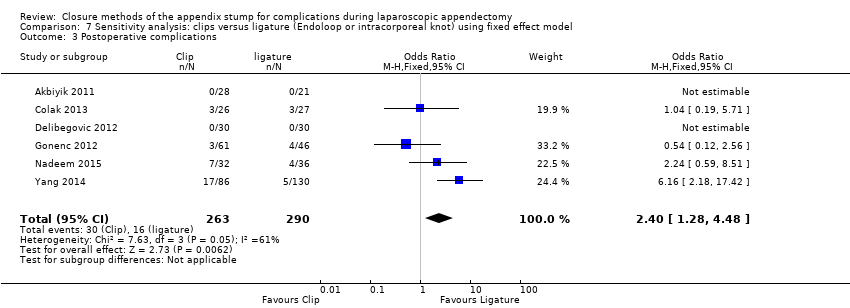
Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 3 Postoperative complications.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 4 Comparison of operative time between clips and ligature.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 5 Comparison of hospital stay between clips and ligature.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 6 Postoperative superficial infections.

Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 7 Postoperative deep infections.
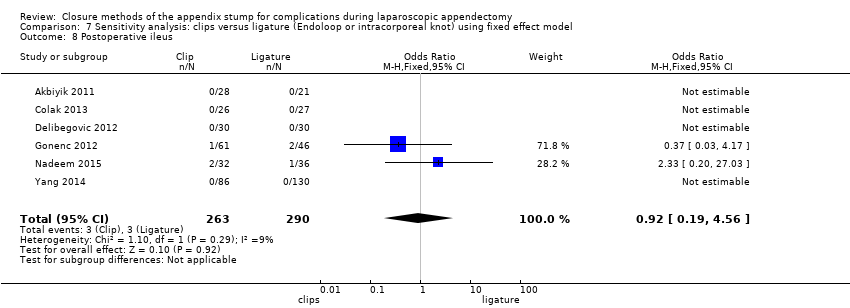
Comparison 7 Sensitivity analysis: clips versus ligature (Endoloop or intracorporeal knot) using fixed effect model, Outcome 8 Postoperative ileus.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 1 Total complications.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 2 Intraoperative complications.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 3 Postoperative complications.
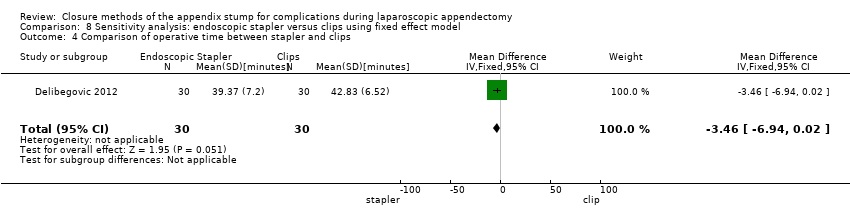
Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 4 Comparison of operative time between stapler and clips.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 5 Comparison of hospital stay between stapler and clips.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 6 Postoperative superficial infections.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 7 Postoperative deep infections.

Comparison 8 Sensitivity analysis: endoscopic stapler versus clips using fixed effect model, Outcome 8 Postoperative ileus.
| Mechanical devices vs ligatures for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligatures | Risk with mechanical devices | ||||
| Total complications | 205 per 1000 | 169 per 1000 | OR 0.97 (0.27 to 3.50) | 850 | ⊕⊝⊝⊝ |
| Intraoperative complications | 76 per 1000 | 63 per 1000 | OR 0.93 (0.34 to 2.55) | 850 | ⊕⊝⊝⊝ |
| Postoperative complications | 129 per 1000 | 109 per 1000 | OR 0.80 (0.21 to 3.13) | 850 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 26 per 1000 | 13 per 1000 | OR 0.58 | 850 | ⊕⊝⊝⊝ |
| Postoperative ileus | 41 per 1000 | 20 per 1000 | OR 0.47 | 850 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 14 per 1000 | 12 per 1000 | OR 0.79 | 850 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.6 minutes. | Mean operative time (minutes) in the intervention group was 9.04 minutes shorter (12.97 minutes shorter to 5.11 minutes shorter). | ‐ | 850 | ⊕⊝⊝⊝ |
| Hospital stay (days) | Mean hospital stay was 1.4 days. | Mean hospital stay in the intervention group was 0.02 days longer (0.12 days shorter to 0.17 days longer). | ‐ | 850 | ⊕⊝⊝⊝ |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Endoscopic stapler vs ligature for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: endoscopic stapler Comparison: ligature | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligature | Risk with endoscopic stapler | ||||
| Total complications | 421 per 1000 | 198 per 1000 | OR 0.34 (0.05 to 2.41) | 327 | ⊕⊝⊝⊝ |
| Intraoperative complications | 182 per 1000 | 191 per 1000 | OR 1.06 (0.17 to 6.70) | 327 | ⊕⊝⊝⊝ |
| Postoperative complications | 239 per 1000 | 250 per 1000 | OR 0.20 (0.09 to 0.44) | 327 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 44 per 1000 | 47 per 1000 | OR 0.10 (0.01 to 0.84) | 327 | ⊕⊝⊝⊝ |
| Postoperative ileus | 88 per 1000 | 93 per 1000 | OR 0.37 (0.13 to 1.07) | 327 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 31 per 1000 | 33 per 1000 | OR 0.45 (0.10 to 2.08) | 327 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.6 minutes. | Mean operative time in the intervention group was 8.52 minutes lower (15.64 minutes shorter to 1.39 minutes shorter). | 327 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 1.9 days. | Mean hospital stay in the intervention group was 0.02 days longer (0.38 days shorter to 0.34 days longer). | 327 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Clips vs ligatures for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: clips Comparison: ligature | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with ligature | Risk with clips | ||||
| Total complications | 17 per 1000 | 18 per 1000 | OR 2.03 (0.71 to 5.84) | 553 | ⊕⊝⊝⊝ |
| Intraoperative complications | 21 per 1000 | 22 per 1000 | OR 1.74 (0.33 to 9.04) | 553 | ⊕⊝⊝⊝ |
| Postoperative complications | 17 per 1000 | 18 per 1000 | OR 1.88 (0.63 to 5.64) | 553 | ⊕⊝⊝⊝ |
| Postoperative superficial infections | 14 per 1000 | 15 per 1000 | OR 1.25 (0.32 to 4.90) | 553 | ⊕⊝⊝⊝ |
| Postoperative ileus | 10 per 1000 | 11 per 1000 | OR 0.92 (0.15 to 5.64) | 553 | ⊕⊝⊝⊝ |
| Postoperative deep infections | 3 per 1000 | 4 per 1000 | OR 1.75 (0.28 to 10.93) | 553 | ⊕⊝⊝⊝ |
| Operative time (minutes) | Mean operative time was 40.0 minutes. | Mean operative time in the intervention group was 8.14 minutes shorter (11.73 minutes shorter to 4.55 minutes shorter). | 553 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 1.5 days. | Mean hospital stay in the intervention group was 0.03 days shorter (0.16 days shorter to 0.11 days longer). | 553 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for inconsistency (substantial heterogeneity). bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (all included studies had few participants and events and thus wide confidence intervals, limiting the precision of estimates). | |||||
| Endoscopic stapler vs clips for appendix stump closure during laparoscopic appendectomy | |||||
| Patient or population: patients undergoing appendix stump closure during laparoscopic appendectomy Settings: hospital Intervention: endoscopic stapler Comparison: clips | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | |
| Risk with clips | Risk with endoscopic stapler | ||||
| Total complications | 67 per 1000 | 70 per 1000 | OR 1.00 (0.13 to 7.60) | 60 | ⊕⊝⊝⊝ |
| Intraoperative complications | 67 per 1000 | 70 per 1000 | OR 1.00 (0.13 to 7.60) | [60 | ⊕⊝⊝⊝ |
| Postoperative complications | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative superficial infections | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative ileus | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Postoperative deep infections | 0 events in both treatment arms | NE | 60 | ⊕⊝⊝⊝ | |
| Operative time (minutes) | Mean operative time was 39.4 minutes. | Mean operative time in the intervention group was 3.46 minutes shorter (6.94 minutes shorter to 0.02 minutes longer). | 60 | ⊕⊝⊝⊝ | |
| Hospital stay (days) | Mean hospital stay was 2.0 days. | Mean hospital stay in the intervention group was 0.04 days shorter (0.28 days shorter to 0.20 days longer). | 60 | ⊕⊝⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence. | |||||
| aDowngraded one level for single study with limited sample size. bDowngraded one level for high risk of bias. cDowngraded one level for imprecision (the sole included studies had few participants and therefore few events, resulting in wide confidence intervals, which limited the precision of estimates). | |||||
| Study ID | Intervention arms | Total no. with complications | Total no. without complications | Intraoperative | Postoperative | |||||||||||
| Bleeding | Intraoperative rupture of appendix | Intraoperative organ injury/ faecal soiling | Access‐related visceral injury | Other | Total | Surgical site infection (superficial) | Deep infection | Bleeding | Paralytic ileus | Purulent peritonitis | Other | Total | ||||
| Ortega 1995 | Endoscopic linear stapler (LAS) | 27 | 51 | 11 | 2 | 5 | 0 | 0 | 18 | 0 | 2 | 0 | 5 | 0 | 2a | 9 |
| 2× catgut ligatures (Endoloops) (LAL) | 62 | 27 | 14 | 4 | 11 | 0 | 0 | 29 | 4 | 4 | 0 | 14 | 0 | 11b | 33 | |
| Open appendectomy (OA) | 44 | 42 | 20 | 5 | 1 | 0 | 0 | 26 | 11 | 0 | 0 | 6 | 0 | 1c | 18 | |
| Akbiyik 2011 | Hem‐o‐lok clip (non‐absorbable polymeric clips) | 0 | 28 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ligaure (Endoloop) | 0 | 21 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Delibegovic 2012 | 45‐mm stapler | 2 | 28 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1 ligature (Endoloop) | 0 | 30 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| 1 Hem‐o‐lok clip (non‐absorbable polymeric clips) | 2 | 28 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Beldi 2004 | 1 ligature (Endoloop) only at appendix base (1 other at 6 to 12 mm distally) | 5 | 104 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 2d | 5 |
| 2 ligatures (Endoloops) at base of appendix (1 other at 6 to 12 mm distally) | 5 | 94 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 1e | 5 | |
| Sucullu 2009 | Endodissector and endoclip | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| LigaSure 5 to 10 mm | 0 | 16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Shalaby 2001 | Endo GIA (Ethicon Endo‐Surgery, Cincinnati, Ohio, USA) stapler | 0 | 60 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Ligature (Endoloop) | 5 | 35 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 0 | 0 | 0 | 1f | 5 | |
| Extracorporeal laparoscopically assisted appendectomy | 6 | 44 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 1 | 1 | 0 | 0 | 0 | 4 | |
| Colak 2013 | Hem‐o‐lok (non‐absorbable polymeric clips) | 3 | 23 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 1g | 3 |
| Ligature (Endoloop) | 3 | 24 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 1g | 3 | |
| Gonenc 2012 | Titanium endoclip | 4 | 57 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 3 |
| Intracorporeal knotting | 6 | 40 | 0 | 0 | 1 | 1 | 0 | 2 | 1 | 0 | 0 | 2 | 1 | 0 | 4 | |
| Ates 2012 | Titanium endoclip | 8 | 22 | NS | NS | NS | NS | 1h | 7 | 0 | 1 | 0 | 0 | 0 | 0 | 1 |
| Intracorporeal knotting | 7 | 24 | NS | NS | NS | NS | 0 | 4 | 1 | 0 | 0 | 0 | 0 | 2i | 3 | |
| Yang 2014 | Intracorporeal knotting | 5 | 125 | 0 | NS | NS | NS | NS | 0 | NS | 0 | NS | NS | NS | 5j | 5 |
| Titanium hem‐o‐lok | 17 | 69 | 0 | NS | NS | NS | NS | 0 | NS | 0 | NS | NS | NS | 17k | 17 | |
| Nadeem 2015 | Extracorporeal knotting | 5 | 31 | 1 | NS | 0 | NS | NS | 1 | 2 | 0 | NS | 1 | NS | 1 | 4 |
| Metallic endoclip | 10 | 22 | 2 | NS | 1 | NS | NS | 3 | 2 | 2 | NS | 2 | NS | 1l | 7 | |
| NS: non‐significant. | ||||||||||||||||
| Mechanical appendix stump closure (with endoscopic stapler or clip(s)) vs ligation (with Endoloop or intra/extracorporeal knot) | |||||||||
| Odds ratio (95% CI) | Risk ratio (95% CI) | Risk difference (95% CI) | Mean difference (95% CI) | ||||||
| Outcome | Fixed effect | Random effects | Fixed effect | Random effects | Fixed effect | Random effects | Fixed effect | Random effects | |
| Total complications | 0.77 (0.53 to 1.13) | 0.97 (0.27 to 3.50) | 0.83 (0.64 to 1.08) | 1.09 (0.41 to 2.88) | ‐0.03 (‐0.08 to 0.01) | ‐0.02 (‐0.12 to 0.09) | ‐ | ‐ | |
| Intraoperative complications | 0.81 (0.45 to 1.46) | 0.93 (0.34 to 2.55) | 0.85 (0.53 to 1.35) | 0.93 (0.40 to 2.18) | ‐0.01 (‐0.04 to 0.02) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative complications | 0.80 (0.52 to 1.24) | 0.80 (0.21 to 3.13) | 0.83 (0.57 to 1.19) | 0.86 (0.27 to 2.74) | ‐0.02 (‐0.06 to 0.02) | ‐0.02 (‐0.10 to 0.06) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐11.94 (‐13.04 to ‐10.84) | ‐9.04 (‐12.97 to ‐5.11) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.02 (‐0.12 to 0.16) | 0.02 (‐0.12 to 0.17) | |
| Postoperative superficial infections | 0.47 (0.17 to 1.26) | 0.58 (0.18 to 1.93) | 0.48 (0.19 to 1.24) | 0.61 (0.19 to 1.93) | ‐0.02 (‐0.04 to 0.01) | ‐0.01 (‐0.02 to 0.01) | ‐ | ‐ | |
| Postoperative ileus | 0.48 (0.20 to 1.15) | 0.47 (0.19 to 1.18) | 0.51 (0.23 to 1.14) | 0.50 (0.22 to 1.17) | ‐0.02 (‐0.04 to 0.01) | ‐0.01 (‐0.03 to 0.02) | ‐ | ‐ | |
| Postoperative deep infections | 0.86 (0.31 to 2.41) | 0.79 (0.24 to 2.53) | 0.87 (0.32 to 2.35) | 0.79 (0.25 to 2.47) | ‐0.00 (‐0.02 to 0.02) | ‐0.00 (‐0.02 to 0.01) | ‐ | ‐ | |
| Endoscopic stapler vs ligature | |||||||||
| Total complications | 0.26 (0.14 to 0.46) | 0.34 (0.05 to 2.41) | 0.49 (0.35 to 0.68) | 0.51 (0.09 to 2.84) | ‐0.21 (‐0.29 to ‐0.12) | ‐0.13 (‐0.40 to 0.14) | ‐ | ‐ | |
| Intraoperative complications | 0.72 (0.38 to 1.39) | 1.06 (0.17 to 6.70) | 0.79 (0.48 to 1.28) | 1.07 (0.22 to 5.19) | ‐0.04 (‐0.11 to 0.04) | ‐0.00 (‐0.11 to 0.10) | ‐ | ‐ | |
| Postoperative complications | 0.19 (0.09 to 0.41) | 0.20 (0.09 to 0.44) | 0.27 (0.14 to 0.51) | 0.25 (0.08 to 0.75) | ‐0.17 (‐0.24 to ‐0.10) | ‐0.12 (‐0.34 to 0.09) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐12.94 (‐14.35 to ‐11.53) | ‐8.36 (‐15.68 to ‐1.03) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 0.03 (‐0.14 to 0.20) | ‐0.02 (‐0.38 to 0.34) | |
| Postoperative superficial infections | 0.10 (0.01 to 0.86) | 0.10 (0.01 to 0.84) | 0.11 (0.01 to 0.88) | 0.11 (0.01 to 0.87) | ‐0.05 (‐0.08 to ‐0.01) | ‐0.04 (‐0.08 to 0.00) | ‐ | ‐ | |
| Postoperative ileus | 0.37 (0.13 to 1.07) | 0.37 (0.13 to 1.07) | 0.41 (0.15 to 1.08) | 0.41 (0.15 to 1.08) | ‐0.05 (‐0.10 to 0.00) | ‐0.02 ( ‐0.10 to 0.05) | ‐ | ‐ | |
| Postoperative deep infections | 0.45 (0.10 to 2.02) | 0.45 (0.10 to 2.08) | 0.46 (0.11 to 1.95) | 0.47 (0.11 to 2.04) | ‐0.02 (‐0.05 to 0.02) | ‐0.02 (‐0.05 to 0.02) | ‐ | ‐ | |
| Endoscopic stapler vs clips | |||||||||
| Total complications | 1.00 (0.13 to 7.60) | 1.00 (0.13 to 7.60) | 1.00 (0.15 to 6.64) | 1.00 (0.15 to 6.64) | 0.00 (‐0.13 to 0.13) | 0.00 (‐0.13 to 0.13) | ‐ | ‐ | |
| Intraoperative complications | 1.00 (0.13 to 7.60) | 1.00 (0.13 to 7.60) | 1.00 (0.15 to 6.64) | 1.00 (0.15 to 6.64) | 0.00 (‐0.13 to 0.13) | 0.00 (‐0.13 to 0.13) | ‐ | ‐ | |
| Postoperative complications | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐3.46 (‐6.94 to 0.02) | ‐3.46 (‐6.94 to 0.02) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.04 (‐0.28 to 0.20) | ‐0.04 [‐0.28, 0.20] | |
| Postoperative superficial infections | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Postoperative ileus | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Postoperative deep infections | NE | NE | NE | NE | 0.00 (‐0.06 to 0.06) | 0.00 (‐0.06 to 0.06) | ‐ | ‐ | |
| Clips vs ligature (Endoloop and intra/extracorporeal knot) | |||||||||
| Total complications | 2.33 (1.31 to 4.13) | 2.03 (0.71 to 5.84) | 2.11 (1.29 to 3.47) | 1.84 (0.73 to 4.62) | 0.08 (0.03 to 0.13) | 0.05 (‐0.03 to 0.13) | ‐ | ‐ | |
| Intraoperative complications | 1.79 (0.49 to 6.56) | 1.74 (0.33 to 9.04) | 1.76 (0.51 to 6.01) | 1.69 (0.35 to 8.19) | 0.01 (‐0.02 to 0.04) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative complications | 2.40 (1.28 to 4.48) | 1.88 (0.63 to 5.64) | 2.20 (1.27 to 3.82) | 1.75 (0.66 to 4.61) | 0.07 (0.02 to 0.12) | 0.03 (‐0.04 to 0.11) | ‐ | ‐ | |
| Operative time (minutes) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐8.06 (‐9.85 to ‐6.26) | ‐8.14 (‐11.73 to ‐4.55) | |
| Hospital stay (days) | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐0.03 (‐0.16 to 0.11) | ‐0.03 (‐0.16 to 0.11) | |
| Postoperative superficial infections | 1.27 (0.33 to 4.86) | 1.25 (0.32 to 4.90) | 1.25 (0.35 to 4.49) | 1.24 (0.34 to 4.56) | 0.00 (‐0.02 to 0.03) | 0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative ileus | 0.92 (0.19 to 4.56) | 0.92 (0.15 to 5.64) | 0.92 (0.20 to 4.21) | 0.93 (0.16 to 5.33) | ‐0.00 (‐0.02 to 0.02) | ‐0.00 (‐0.02 to 0.02) | ‐ | ‐ | |
| Postoperative deep infections | 1.79 (0.37 to 8.58) | 1.75 (0.28 to 10.93) | 1.77 (0.38 to 8.16) | 1.71 (0.28 to 10.28) | 0.01 (‐0.02 to 0.03) | 0.00 (‐0.01 to 0.02) | ‐ | ‐ | |
| CI: confidence interval; NE: not estimable; "‐": not applicable. | |||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.97 [0.27, 3.50] |
| 2 Intraoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.93 [0.34, 2.55] |
| 3 Postoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.80 [0.21, 3.13] |
| 4 Comparison of operative time between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Random, 95% CI) | ‐9.04 [‐12.97, ‐5.11] |
| 5 Hospital stay (in days) between mechanical and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.12, 0.17] |
| 6 Postoperative superficial infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.58 [0.18, 1.93] |
| 7 Postoperative deep infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.79 [0.24, 2.53] |
| 8 Postoperative ileus Show forest plot | 8 | 850 | Odds Ratio (M‐H, Random, 95% CI) | 0.47 [0.19, 1.18] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.34 [0.05, 2.41] |
| 2 Intraoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 1.06 [0.17, 6.70] |
| 3 Postoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.20 [0.09, 0.44] |
| 4 Comparison of operative time between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Random, 95% CI) | ‐8.52 [‐15.64, ‐1.39] |
| 5 Comparison of hospital stay between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.38, 0.34] |
| 6 Postoperative superficial infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.10 [0.01, 0.84] |
| 7 Postoperative deep infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.45 [0.10, 2.08] |
| 8 Postoperative ileus Show forest plot | 3 | 327 | Odds Ratio (M‐H, Random, 95% CI) | 0.37 [0.13, 1.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 2.03 [0.71, 5.84] |
| 2 Intraoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.74 [0.33, 9.04] |
| 3 Postoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.88 [0.63, 5.64] |
| 4 Comparison of operative time between clips and ligatures Show forest plot | 6 | 553 | Mean Difference (IV, Random, 95% CI) | ‐8.14 [‐11.73, ‐4.55] |
| 5 Comparison of hospital stay between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.16, 0.11] |
| 6 Postoperative superficial infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.25 [0.32, 4.90] |
| 7 Postoperative deep infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 1.75 [0.28, 10.93] |
| 8 Postoperative ileus Show forest plot | 6 | 553 | Odds Ratio (M‐H, Random, 95% CI) | 0.92 [0.15, 5.64] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 1.0 [0.13, 7.60] |
| 2 Intraoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 1.0 [0.13, 7.60] |
| 3 Postoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Comparison of operative time between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐3.46 [‐6.94, 0.02] |
| 5 Comparison of hospital stay between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.28, 0.20] |
| 6 Postoperative superficial infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Postoperative deep infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Postoperative ileus Show forest plot | 1 | 60 | Odds Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.53, 1.13] |
| 2 Intraoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.45, 1.46] |
| 3 Postoperative complications Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.52, 1.24] |
| 4 Comparison of operative time between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Fixed, 95% CI) | ‐11.94 [‐13.04, ‐10.84] |
| 5 Hospital stay (in days) between mechanical device and ligature Show forest plot | 8 | 850 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.12, 0.16] |
| 6 Postoperative superficial infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.17, 1.26] |
| 7 Postoperative deep infections Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.31, 2.41] |
| 8 Postoperative ileus Show forest plot | 8 | 850 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.20, 1.15] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.14, 0.46] |
| 2 Intraoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.38, 1.39] |
| 3 Postoperative complications Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.09, 0.41] |
| 4 Comparison of operative time between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Fixed, 95% CI) | ‐12.99 [‐14.39, ‐11.58] |
| 5 Comparison of hospital stay between stapler and ligature Show forest plot | 3 | 327 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.14, 0.20] |
| 6 Postoperative superficial infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 0.86] |
| 7 Postoperative deep infections Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.10, 2.02] |
| 8 Postoperative ileus Show forest plot | 3 | 327 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.13, 1.07] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.33 [1.31, 4.13] |
| 2 Intraoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.49, 6.56] |
| 3 Postoperative complications Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.40 [1.28, 4.48] |
| 4 Comparison of operative time between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Fixed, 95% CI) | ‐8.06 [‐9.85, ‐6.26] |
| 5 Comparison of hospital stay between clips and ligature Show forest plot | 6 | 553 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.16, 0.11] |
| 6 Postoperative superficial infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.33, 4.86] |
| 7 Postoperative deep infections Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.37, 8.58] |
| 8 Postoperative ileus Show forest plot | 6 | 553 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.19, 4.56] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Total complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.13, 7.60] |
| 2 Intraoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.13, 7.60] |
| 3 Postoperative complications Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Comparison of operative time between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐3.46 [‐6.94, 0.02] |
| 5 Comparison of hospital stay between stapler and clips Show forest plot | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.28, 0.20] |
| 6 Postoperative superficial infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Postoperative deep infections Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Postoperative ileus Show forest plot | 1 | 60 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |

