Endovascular treatment for ruptured abdominal aortic aneurysm
Information
- DOI:
- https://doi.org/10.1002/14651858.CD005261.pub4Copy DOI
- Database:
-
- Cochrane Database of Systematic Reviews
- Version published:
-
- 26 May 2017see what's new
- Type:
-
- Intervention
- Stage:
-
- Review
- Cochrane Editorial Group:
-
Cochrane Vascular Group
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Article metrics
Altmetric:
Cited by:
Authors
Contributions of authors
For the current update of this review, Stephen Badger and Rachel Forster performed study selection, quality assessment, and data extraction. Drafting of the review was performed by Rachel Forster with input from Stephen Badger and Denis W Harkin. Paul H Blair, Peter Ellis, and Frank Kee acted as arbitrators in the case of disagreements over inclusion and quality of studies.
For previous versions of this review, Marianne Dillon and Denis W Harkin performed the literature searches, identified all possible trials, considered them for inclusion, and assessed trial quality. Paul H Blair, Peter Ellis, Chris Cardwell, and Frank Kee acted as arbitrators in the case of disagreements over inclusion and quality of studies.
Sources of support
Internal sources
-
No sources of support supplied
External sources
-
Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK.
The Cochrane Vascular editorial base is supported by the Chief Scientist Office.
-
National Institute for Health Research (NIHR), UK.
This project was supported by the NIHR, via Cochrane Incentive Award funding (16/72/05) to Cochrane Vascular. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service (NHS), or the Department of Health.
Declarations of interest
SB: None known.
RF: None known.
PHB: None known.
PE: None known.
FK: None known.
DWH: None known.
Acknowledgements
We would like to thank the members of the Cochrane Vascular editorial board for their guidance and support, and Marianne Dillon and Chris Cardwell for their work on the previous version of this review.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 May 26 | Endovascular treatment for ruptured abdominal aortic aneurysm | Review | Stephen Badger, Rachel Forster, Paul H Blair, Peter Ellis, Frank Kee, Denis W Harkin | |
| 2014 Jul 21 | Endovascular treatment for ruptured abdominal aortic aneurysm | Review | Stephen Badger, Rachel Bedenis, Paul H Blair, Peter Ellis, Frank Kee, Denis W Harkin | |
| 2007 Jan 24 | Endovascular treatment for ruptured abdominal aortic aneurysm | Review | Marianne Dillon, Chris Cardwell, Paul H Blair, Peter Ellis, Frank Kee, Denis W Harkin | |
| 2005 Apr 20 | Endovascular treatment for ruptured abdominal aortic aneurysm | Protocol | Marianne Dillon, P H Blair, C Cardwell, P K Ellis, Denis W Harkin, Frank Kee | |
Differences between protocol and review
In order to reflect the nature of the diagnosis of ruptured abdominal aortic aneurysm, we rephrased 'clinical diagnosis of ruptured abdominal aortic aneurysm' to 'clinical and radiological diagnosis of ruptured abdominal aortic aneurysm'. We also clarified the 'Types of participants' section.
We added a new outcome, 'complications and mortality long term (longer than six months); we sought re‐intervention rates for problems related to the ruptured abdominal aortic aneurysm as well as cause of death with or without re‐intervention, that is device‐related', as we expect these data will become available in the future.
We rephrased the outcome 'aneurysm exclusion' to 'endoleak', as this previously used term was vague and found to be misleading.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- Aortic Aneurysm, Abdominal [mortality, *surgery];
- Aortic Rupture [mortality, *surgery];
- Conversion to Open Surgery [statistics & numerical data];
- Emergency Treatment [*methods, mortality];
- Endoleak [etiology];
- Endovascular Procedures [*methods, mortality];
- Hospital Mortality;
- Intestines [blood supply];
- Ischemia [etiology];
- Kidney Diseases [etiology];
- Myocardial Infarction [etiology];
- Postoperative Complications;
- Quality of Life;
- Randomized Controlled Trials as Topic;
- Respiratory Insufficiency [etiology];
Medical Subject Headings Check Words
Humans;
PICOs

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
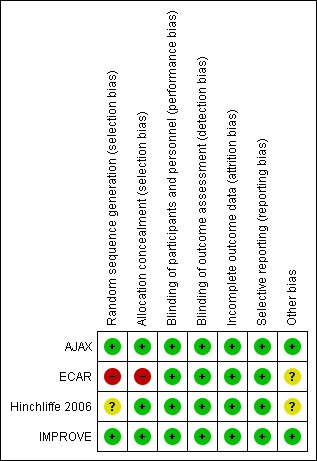
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 1 Short‐term mortality (30‐day or in‐hospital).

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 2 Major complications ‐ 30‐day.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 3 Complication ‐ Myocardial infarction.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 4 Complication ‐ Stroke.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 5 Complication ‐ Cardiac complications (moderate or severe).

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 6 Complication ‐ Renal complications (moderate or severe).

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 7 Complication ‐ Respiratory failure.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 8 Complication ‐ Bowel ischaemia.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 9 Complication ‐ Spinal cord ischaemia.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 10 Complication ‐ Reoperation.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 11 Complication ‐ Amputation.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 12 Mortality ‐ 6 months.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 13 Major complications ‐ 6 months.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 14 Complication ‐ Reoperation ‐ 6 months.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 15 Mortality ‐ 1 year.

Comparison 1 Emergency endovascular aneurysm repair versus open repair, Outcome 16 Cost per patient ‐ 30‐day.
| Emergency endovascular aneurysm repair (eEVAR) compared to conventional open repair for ruptured abdominal aortic aneurysm | |||||
| Patient or population: people diagnosed with RAAA Intervention: eEVAR | |||||
| Outcomes | № of participants | Quality of the evidence | Relative effect | Anticipated absolute effects* (95% CI) | |
| Risk with conventional open repair | Risk difference with eEVAR | ||||
| Short‐term mortality (30‐day or in‐hospital) | 868 | ⊕⊕⊕⊝ | OR 0.88 | Study population | |
| 366 per 1000 | 29 fewer per 1000 | ||||
| Endoleak (30‐day) | 128 | ⊕⊕⊝⊝ | — | A total of 44 endoleak events occurred in 128 participants randomised to eEVAR treatment. As endoleaks are only a result of endovascular repair, meta‐analysis was inappropriate. | |
| Complication: myocardial infarction (30‐day) | 139 | ⊕⊕⊝⊝ | OR 2.38 | Study population | |
| 15 per 1000 | 20 more per 1000 | ||||
| Complication: renal complications (moderate or severe) (30‐day) | 255 | ⊕⊕⊝⊝ | OR 1.07 | Study population | |
| 197 per 1000 | 11 more per 1000 | ||||
| Complication: respiratory failure (30‐day) | 32 | ⊕⊕⊝⊝ | OR 3.62 | Study population | |
| 1 respiratory failure event occurred in 15 participants who were randomised to eEVAR treatment. No respiratory failure events were reported in the open‐repair group. | |||||
| Complication: bowel ischaemia (30‐day) | 223 | ⊕⊕⊝⊝ | OR 0.37 | Study population | |
| 145 per 1000 | 86 fewer per 1000 | ||||
| Mortality (6 months) | 116 | ⊕⊕⊕⊝ | OR 0.89 | Study population | |
| 305 per 1000 | 24 fewer per 1000 | ||||
| *We calculated the assumed risk of the conventional open‐repair group from the average risk in the conventional open‐repair group (i.e. the number of participants with events divided by total number of participants of the conventional open‐repair group included in the meta‐analysis). The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1Downgraded by one level due to imprecision: two of the three studies included in this outcome were underpowered to report on this outcome, as calculated by the study authors. | |||||
| (median, IQR) | (mean, range) | (median, IQR) | (mean, SD) | ||
| Time waiting for procedure | eEVAR | 74 min (39 to 126 min) | 2.9 hours | — | 93 min (± 370) |
| Open repair | 45 min (35 to 70 min) | 1.3 hours | — | 73 min (± 157) | |
| Time in operating theatre | eEVAR | 185 min (160 to 236 min) | — | 160 min (150 to 234 min) | 156 min (± 100) |
| Open repair | 157 min (136 to 194 min) | — | 150 min (141 to 204 min) | 180 min (± 107) | |
| Blood loss during operation | eEVAR | 500 mL (200 to 1375 mL) | Units for transfusion: 6.8 (range 0 to 25.0) | 200 mL (163 to 450 mL) | — |
| Open repair | 3500 mL (1000 to 4600 mL) | Units for transfusion: 10.9 (range 0 to 53.0) | 2100 mL (1150 to 3985 mL) | — | |
| Length of hospital stay | eEVAR | 9 days (4 to 21 days) | 14.3 days (6.0 to 99.0) | 10 days (6 to 28 days) | 9.8 days (± 9.0) |
| Open repair | 13 days (5 to 21 days) | 17.1 days (9.1 to 81.1 ) | 12 days (4 to 52 days) | 12.2 days (± 10.2) | |
| eEVAR: emergency endovascular aneurysm repair | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Short‐term mortality (30‐day or in‐hospital) Show forest plot | 4 | 868 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.66, 1.16] |
| 2 Major complications ‐ 30‐day Show forest plot | 2 | 223 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.42, 1.23] |
| 3 Complication ‐ Myocardial infarction Show forest plot | 2 | 139 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.38 [0.34, 16.53] |
| 4 Complication ‐ Stroke Show forest plot | 2 | 148 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.12, 4.31] |
| 5 Complication ‐ Cardiac complications (moderate or severe) Show forest plot | 3 | 253 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.32, 2.23] |
| 6 Complication ‐ Renal complications (moderate or severe) Show forest plot | 3 | 255 | Odds Ratio (M‐H, Random, 95% CI) | 1.07 [0.21, 5.42] |
| 7 Complication ‐ Respiratory failure Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8 Complication ‐ Bowel ischaemia Show forest plot | 2 | 223 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.14, 0.94] |
| 9 Complication ‐ Spinal cord ischaemia Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10 Complication ‐ Reoperation Show forest plot | 2 | 148 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.39, 2.01] |
| 11 Complication ‐ Amputation Show forest plot | 2 | 223 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.02, 1.32] |
| 12 Mortality ‐ 6 months Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 13 Major complications ‐ 6 months Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 14 Complication ‐ Reoperation ‐ 6 months Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 15 Mortality ‐ 1 year Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 16 Cost per patient ‐ 30‐day Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |


