Manipulación y movilización para el dolor de cuello comparadas con un control inactivo u otro tratamiento activo
References
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Type of trial: RCT | |
| Participants | Chronic non‐specific cervical disorder | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Mobilisation randomly chosen at cervical vertebral level (A): technique: posterior‐anterior central vertebral pressure, posterior‐anterior unilateral pressure and transversal vertebral pressure; technique selected at physiotherapist’s discretion, indications by Maitland et al.; timing: at baseline; frequency: 1 session; route: cervical spine CO‐INTERVENTION: not applicable (N/A) Duration of treatment: 1 day, 1 session | |
| Outcomes | PAIN (during most painful movement, 11‐point pain scale, 0 to 10) Baseline mean: A 6.2, B 6.04 End of study mean: A 3.58, B 3.37 Absolute benefit: A 2.62, B 2.67 Reported results: not significant SMD (A vs B): 0.07 (95% CI ‐0.49 to 0.64) FUNCTION: not reported (NR) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not adequately designed; page 96, middle column, paragraph 2 |
| Allocation concealment (selection bias) | Unclear risk | Not adequately designed; page 96, middle column, paragraph 2 |
| Blinding of Participants (performance bias) | Unclear risk | Participant blinding not described but possible |
| Blinding of Personal (performance bias) | High risk | Study authors state that care providers were blinded; however, we believe this was not possible because treatment was provided at the discretion of the therapist |
| Blinding of the Outcome assessor (detection bias) | Unclear risk | Participant is the assessor |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design; Figure 1 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 and Table 3 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
| Methods | Type of trial: quasi‐RCT | |
| Participants | Chronic neck pain with headache or degenerative changes (spondylogenic) | |
| Interventions | INDEX TREATMENT Group B (B): technique: manipulation; frequency: 1 session/wk; dose: mean 7.2 manipulations over 3.8 sessions; route: cervical spine COMPARISON TREATMENT CO‐INTERVENTION: none Duration of treatment: 3 weeks, 3 to 4 sessions | |
| Outcomes | PAIN (VAS, 0 to 100) Baseline mean: A 60.50, B 64.40, C 57.60 End of study mean: A 38.50, B 27.80, C 43.50 Absolute benefit: A 22.0, B 36.6, C 14.1 Reported results: not significant SMD (A vs C): ‐0.18 (95% CI‐1.12 to 0.75) (power 10%) FUNCTION: NR GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: Manipulation and mobilisation were well tolerated, with the customary reaction of minimal benign reaction lasting less than 24 hours (RR 1.34, 95% CI 0.77 to 2.34) COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Draw lots; even chance of getting assigned to 1 of 3 groups |
| Allocation concealment (selection bias) | High risk | Not concealed |
| Blinding of Participants (performance bias) | High risk | VAS pain; not blind to participant |
| Blinding of Personal (performance bias) | High risk | Not blind |
| Blinding of the Outcome assessor (detection bias) | High risk | Participant is outcome assessor for VAS pain |
| Incomplete outcome data (attrition bias) | Low risk | See Table 1, page 260, for complete data |
| Randomized Participants analysed were allocated (attrition bias) | High risk | ITT not reported |
| Selective outcome (reporting bias) | Unclear risk | No previous protocol |
| Similar groups at baseline? | Low risk | Presented in text, page 260, 2nd column, 2nd paragraph. |
| co‐interventions avoided or similar? | Low risk | No co‐intervention was noted |
| Compliance acceptable? | High risk | Not assessed |
| Similar timing of outcome assessment? | Low risk | All groups were measured at similar time points |
| Methods | Type of trial: RCT | |
| Participants | Acute/subacute mechanical neck pain (grade I or II according to Bone and Joint Decade 2000‐2010 Task on Neck Pain and Its Associated Disorders classification) | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Medication (B): technique: NSAID, acetaminophen or both. Second line of therapy for those who did not respond was narcotic medication. Muscle relaxants were also used (choice made by the physician); timing: at baseline; frequency: left to the physician's discretion (mean visits = 4.8); dose: choice made by the physician; duration: 15 to 20 minutes (included brief history and examination); route: oral Home exercise (C): technique: self mobilisation exercise (gentle controlled movement) of the neck and shoulder (neck retraction, rotation, extension, flexion, lateral bending motions and scapular retraction with no resistance); timing: at baseline; frequency: 6 to 8 times per day; dose: 5 to 10 rep/exercise; route: cervical and shoulder joint CO‐INTERVENTION: avoided in trial design: additional treatment for neck pain from non‐study healthcare providers, 4 participants (n = 3 in the medication group and n = 1 in the HEA group) reported to visit other healthcare providers during 12‐week interventions; by week 52, participants in each treatment group sought additional health care after completing the treatment phase (n = 18 in the SMT group, n = 14 in the medication group, n = 17 in the HEA group) Duration of treatment: maximum 12 weeks; number of treatment sessions was left to the discretion of the provider | |
| Outcomes | PAIN (NRS, 0 to 10) Baseline mean: A 5.27, B 4.93, C 5.05 End of study mean: A 1.60, B 2.14, C 1.92 Absolute benefit: A 3.67, B 2.79, C 3.13 Reported results: significant favouring A over B at IP and LT SMD (A vs C): IP ‐0.13 (95% CI ‐0.43 to 0.16), IT ‐0.16 (95% CI ‐0.45 to 0.13), LT 0.06 (95% CI ‐0.23 to 0.35) SMD (A vs B): IP ‐0.34 (95% CI ‐0.64 to ‐0.05), IT ‐0.21 (95% CI ‐0.50 to 0.08), LT ‐0.32 (95% CI ‐0.61 to ‐0.02); NNTB 12 FUNCTION (NDI, 0 to 50) Baseline mean: A 24.22, B 25.12, C 25.12 End of study mean: A 9.99, B 11.07, C 10.20 Absolute benefit: A 14.23, B 14.05, C 14.92 Reported results: significant favouring A over B at IP and IT SMD (A vs C): IP ‐0.21 (95% CI ‐0.50 to 0.08), IT ‐0.01 (95% CI ‐0.30 to 0.28), LT ‐0.02 (95% CI ‐0.31 to 0.27) SMD (A vs B): IP ‐0.35 (95% CI ‐0.64 to ‐0.06), IT ‐0.30 (95% CI ‐0.59 to ‐0.00), LT ‐0.11 (95% CI ‐0.40 to 0.18); NNTB 15 GPE (9‐point scale, 1 to 9) End of study mean: A 2.22, B 2.57, C 2.43 Reported results: significant improvement favouring A over B PATIENT SATISFACTION (7‐point scale, 1 to 7) End of study mean: A 1.67, B 2.48, C 2.06 Reported results: significant improvement favouring A over B QoL (PCS component of SF‐36, 0 to 100) Baseline mean: A 43.36, B 46.27, C 45.31 End of study mean: A 52.51, B 51.13, C 52.48 Absolute benefit: A 9.15, B 4.86, C 7.17 Reported results: not significant SMD (A vs C): IP 0.08 (95% CI ‐0.21 to 0.37), IT ‐0.05 (95% CI ‐0.35 to 0.24), LT 0.00 (95% CI ‐0.29 to 0.29) SMD (A vs B): IP 0.14 (95% CI ‐0.15 to 0.43), IT 0.22 (95% CI ‐0.07 to 0.51), LT 0.19 (95% CI ‐0.10 to 0.49) SIDE EFFECTS Aggravation of pain: A 28/91, B 0/90, C 37/91 Headache: A 5/91, B 0/90, C 3/91 Stiffness: A 5/91, B 0/90, C 4/91 Not specified: A 4/91, B 5/90, C 0/91 Paraesthesia: A 2/91, B 0/90, C 3/91 Nausea: A 1/91, B 5/90, C 1/91 Crepitus: A 0/91, B 0/90, C 3/91 Increased blood pressure: A 0/91, B 1/90, C 0/91 Stress incontinence: A 0/91, B 1/90, C 0/91 Disturbed sleep: A 0/91, B 4/90, C 0/91 Congestion: A 0/91, B 6/90, C 0/91 Rash: A 0/91, B 7/90, C 0/91 Cognitive symptoms: A 0/91, B 10/90, C 0/91 Dry mouth: A 0/91, B 10/90, C 0/91 Gastrointestinal symptoms: A 0/91, B 17/90, C 0/91 Drowsiness: A 0/91, B 18/90, C 0/91 COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 2, left column, at the bottom |
| Allocation concealment (selection bias) | Low risk | Page 2, right column, at the top |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Unclear risk | Study flow diagram is unclear – are long‐term dropouts 31 or 52 (short term + long term). Also, long‐term dropout in medication group is 34.4%. Unclear whether dropouts in each week of diagram are the same participants |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 3, right column, paragraph 3 |
| Selective outcome (reporting bias) | Low risk | Page 2, right column, paragraph 2 – similar to Evans 2003 pilot |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | High risk | Table 2 – Variety of co‐interventions were provided to SMT group; types of other interventions used by each group are not reported |
| Compliance acceptable? | Unclear risk | Unsure whether participants were compliant with home exercises |
| Similar timing of outcome assessment? | Low risk | Page 3, right column, paragraph 2 |
| Methods | Type of trial: RCT | |
| Participants | Acute, subacute, chronic neck pain with varied degenerative changes (spondylosis) | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: none Duration of treatment: 1 session | |
| Outcomes | PAIN (NRS, 0 to 100) Baseline mean: A 37.7, B 31.0 End of study mean: A 20.4, B 20.5 Absolute benefit: A 17.3, B 10.5 Reported results: not significant SMD (A vs B): 0.00 (95% CI ‐0.40 to 0.39) (power 16%) FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: no complications; 3 participants in each group reported more pain after intervention (RR 0.97, 95% CI 0.47 to 2.03) COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Mentioned in letter to editor, 1993, page 279 |
| Allocation concealment (selection bias) | Low risk | Mentioned in letter to editor, 1993, page 279 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No previous protocol found |
| Similar groups at baseline? | High risk | Mentioned in letter to editor, 1993, page 279 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
| Methods | Type of trial: quasi‐RCT | |
| Participants | Chronic cervicogenic headache from degenerative changes | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of therapy period: 10 sessions | |
| Outcomes | PAIN (NRS, 0 to 10) Baseline mean: A 7.45, B 7.86 End of study mean: A 2.31, B 5.26 Absolute benefit: A 5.14, B 2.6 Reported results: significant favouring manipulation SMD (A vs B): ‐1.92 (95% CI ‐2.49 to ‐1.35); NNTB 7 FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: none COST OF CARE: NR | |
| Notes | Chinese translation: Kein Trinh | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Page 404, right column, paragraph 1 |
| Allocation concealment (selection bias) | High risk | Page 404, right column, paragraph 1 |
| Blinding of Participants (performance bias) | High risk | Blinding not mentioned in the paper but really not possible, as 2 treatment methods are very different |
| Blinding of Personal (performance bias) | High risk | Page 404, left column, paragraph 2 |
| Blinding of the Outcome assessor (detection bias) | High risk | Page 404, right column, 1.3 and 1.4 sections. Describe subjective rating system of treatment effectiveness and pain score. Scores are given by participant, so outcome assessor is not blinded |
| Incomplete outcome data (attrition bias) | Low risk | Page 404, right column, lines 5 to 7 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Table 2, page 405 |
| Selective outcome (reporting bias) | Unclear risk | No previous protocol published |
| Similar groups at baseline? | Low risk | Page 405, section 2.1; also Tables 1 and 2, baseline data |
| co‐interventions avoided or similar? | Low risk | Not mentioned |
| Compliance acceptable? | Low risk | Page 405, section 2.1 |
| Similar timing of outcome assessment? | Low risk | Page 404, right column, section 1.4 |
| Methods | Type of trial: RCT Location of study: Hong Kong | |
| Participants | Chronic (> 3 months) mechanical neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of therapy period: 4 weeks | |
| Outcomes | PAIN (NPRS, 0 to 10) Baseline mean: manip plus cntl 5.02, cntl 5.05 End of study mean: manip plus cntl 2.98, cntl 4.24 Absolute benefit: manip plus cntl 2.04, cntl 0.81 Reported results: significant favouring manipulation SMD (6 months): ‐0.64 (95% CI ‐1.04 to ‐0.25); NNTB 4 FUNCTION: NPQ, 0 to 100% Baseline mean: manip plus cntl 39.15, cntl 41.86 End of study mean: manip plus cntl 28.77, cntl 34.80 Absolute benefit: manip plus cntl 10.38, cntl 7.06 Reported results: significant favouring manipulation SMD: ‐0.38 (95% CI ‐0.77 to 0.01); NNTB 5 PARTICIPANT SATISFACTION: NR GPE: NR QoL: SF‐36 PCS and MCS PCS Baseline mean: manip plus cntl 38.35, cntl 35.35 End of study mean: manip plus cntl 41.24, cntl 35.67 Absolute benefit: manip plus cntl 2.89, cntl 0.32 Reported results: significant favouring manipulation SMD: ‐0.64 (95% CI ‐1.02 to ‐0.26) SIDE EFFECTS: none COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 142, left column, paragraphs 3 and 4 |
| Allocation concealment (selection bias) | Low risk | Page 142, left column, paragraphs 3 and 4 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to intervention |
| Blinding of Personal (performance bias) | High risk | Not possible owing to intervention |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to intervention |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Figure 1 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Home exercise compliance not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, immediate, 3 months, 6 months. Figure 1; page 142, right column, paragraph 4 |
| Methods | Type of trial: RCT | |
| Participants | Chronic neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT COINTERVENTION: NR Duration of therapy period: 1 session | |
| Outcomes | PAIN (VAS, 0 to 100) Baseline mean: manip 41.6, placebo 47.7 End of study mean: manip 26.1, cntl 43.5 Absolute benefit: manip 15.5, cntl 4.2 Reported results: significant favouring manipulation SMD: ‐0.93 (95% CI ‐1.62 to ‐0.24); NNTB 2; treatment advantage 29% FUNCTION: NR PARTICIPANT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: none COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 129, column 1, paragraph 3 |
| Allocation concealment (selection bias) | Low risk | Page 129, column 1, paragraph 3 |
| Blinding of Participants (performance bias) | Low risk | Page 130, column 2, paragraph 2 |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Page 130, column 2, paragraph 2 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Not reported |
| Selective outcome (reporting bias) | Low risk | Protocol available |
| Similar groups at baseline? | Low risk | Table 1, page 131 |
| co‐interventions avoided or similar? | Low risk | Table 1, page 131 |
| Compliance acceptable? | Low risk | Pre‐test/Post‐test design |
| Similar timing of outcome assessment? | Low risk | Pre‐test/Post‐test design |
| Methods | Type of trial: RCT | |
| Participants | Subacute/chronic neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of therapy period: 1 session | |
| Outcomes | PAIN (NRS, 0 to 10) Baseline mean: A 7.3, B 7.7 End of study mean: A 5.8, B 7.4 Absolute benefit: A 1.5, B 0.3 Reported results: positive immediate effect favouring mobilisations: SMD (A vs B) ‐0.78, 95% CI‐1.70 to 0.13 (power 58%) FUNCTION: NR PARTICIPANT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation technique not specified |
| Allocation concealment (selection bias) | Unclear risk | Opaque sealed envelopes, not numbered |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No protocol published |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
| Methods | Type of trial: RCT | |
| Participants | Subacute, chronic neck pain with degenerative changes (i.e. cervical spondylosis), whiplash‐associated disorder (WAD) | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 6 weeks, 6 sessions maximum | |
| Outcomes | PAIN (VAS, 0 to 100) Baseline mean: A 51, B 51 End of study mean: A 22, B 28 Absolute benefit: A 29, B 23 Reported results: not significant SMD (A vs B): ‐0.33 (95% CI ‐0.89 to 0.23) (power 24%) FUNCTION (NPQ, 0 to 36) Baseline mean: A 36, B 36 End of study mean: A 22, B 25 Absolute benefit: A 14, B 11 Reported results: not significant SMD (A vs B): ‐0.16 (95% CI ‐0.72 to 0.39) (power 15%) PARTICIPANT SATISFACTION: NR GPE: NR QoL (GHQ 28, 0 to 28) Reported results: not significant RR (A vs B): 1.07 (95% CI 0.48 to 2.35) SIDE EFFECTS: no side effects with acupuncture COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation technique not specified |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to study design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to study design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to study design |
| Incomplete outcome data (attrition bias) | High risk | Page 1119, right column 2, dropout not described and exceeds 30% long term |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Table 1: Numbers do not add up |
| Selective outcome (reporting bias) | Unclear risk | No published protocol |
| Similar groups at baseline? | Low risk | Figures 1, 2 and 3 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 6 weeks, 6 months |
| Methods | Type of trial: quasi‐RCT | |
| Participants | Acute or subacute neck pain with degenerative changes ‐ cervical spondylosis of C5/6 | |
| Interventions | INDEX TREATMENT GROUPS Anterior‐posterior‐unilateral pressure (B): technique: anterior‐posterior oscillatory pressure on the side of symptoms (Maitland); frequency: 3 times/wk; dose: 10 oscillations in 60 seconds; route: transverse processes of C5/6 Cervical oscillatory rotation (C): technique: rotation oscillation by turning head and neck to the opposite side from the pain until pain is just elicited and then oscillations are given (Maitland); frequency: 3 times/wk; dose: 10 oscillations in 60 seconds; route: rotation performed with hands on jaw and occiput Transverse oscillatory pressure (D): technique: transverse oscillation produced by a push‐relax sequence on the spinous process using the thumbs to produce movement (Maitland); frequency: 3 times/wk; dose: 10 oscillations in 60 seconds; route: spinous processes of C5/6 CO‐INTERVENTION: NR Duration of treatment: 4 weeks or until pain was absent, 12 sessions maximum | |
| Outcomes | PAIN STATUS (5 categories, pain free to worse) Reported results: NR RR (B vs A): 0.60 (95% CI 0.16 to 2.23) RR (B vs C): 0.29 (95% CI 0.09 to 0.91) RR (B vs D): 0.30 (95% CI 0.09 to 0.96) RR (A vs C): 0.48 (95% CI 0.19 to 1.19) RR (A vs D): 0.50 (95% CI 0.20 to 1.25) RR (A vs B): 1.67 (95% CI 0.45 to 6.21) MEAN TREATMENT TIME (minutes) Mean: A 161, B 130, C 201, D 221 Reported results: not significant RELAPSE AFTER 3 MONTHS (number reported) A 0, B 0, C 3, D 2 Reported results: NR FUNCTION: NR GPE: NR PARTICIPANT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sequential ordering into groups, page 104 |
| Allocation concealment (selection bias) | High risk | Not possible with consecutive allocation. |
| Blinding of Participants (performance bias) | High risk | Not described as blinded in paper |
| Blinding of Personal (performance bias) | High risk | Not described as blinded in paper |
| Blinding of the Outcome assessor (detection bias) | High risk | Not described as blinded in paper |
| Incomplete outcome data (attrition bias) | High risk | Page 106, 13 dropouts were not described |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | 13 dropouts were not described, but Table 1 seems to include all participants |
| Selective outcome (reporting bias) | Unclear risk | No protocol available |
| Similar groups at baseline? | Unclear risk | Data other than age not given |
| co‐interventions avoided or similar? | Unclear risk | Not stated |
| Compliance acceptable? | Unclear risk | Not mentioned |
| Similar timing of outcome assessment? | Unclear risk | Not clear when outcomes were taken |
| Methods | Type of trial: RCT | |
| Participants | Chronic non‐specific cervical disorder | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: not avoided: medication; avoided in trial design: other health professionals Duration of treatment: 1 month, 10 sessions | |
| Outcomes | PAIN (VAS, 0 to 100 mm) Baseline mean: A 54.91, B 56.45 End of study mean: A 33.01, B 35.12 Absolute benefit: A 21.90, B 21.33 Reported results: not significant SMD (A vs B): IP ‐0.10 (95% CI ‐0.52 to 0.32), IT ‐0.12 (95% CI ‐0.59 to 0.34) FUNCTION (NDI, 0 to 50) Baseline mean: A 31.63, B 34.38 End of the study mean: A 22.23, B 23.90 Absolute benefit: A 9.40, B 10.48 Reported results: not significant SMD (A vs B): IP ‐0.12 (95% CI ‐0.54 to 0.30), IT 0.07 (95% CI ‐0.40 to 0.53) PATIENT SATISFACTION (Likert scale, 1 to 7) End of the study mean: unsatisfied: A 2, B 3, indifferent: A 0, B 2, satisfied: A 45, B 37 Reported results: not significant RR (A vs B): 1.09 (95% CI 0.96 to 1.23) GPE: NR QoL (PCS component of the SF‐12, 0 to 100) Baseline mean: A 43.26, B 42.66 End of the study mean: A 45.56, B 47.42 Absolute benefit: A 2.30, B 4.76 Reported results: not significant SMD (A vs B): IP ‐0.20 (95% CI ‐0.63 to 0.23), IT 0.22 (95% CI ‐0.25 to 0.68) SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of block randomisation is not clearly stated; it is not clear whether complete blocks were done at each centre |
| Allocation concealment (selection bias) | Unclear risk | Envelopes were not numbered |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 69, paragraph 2 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Home exercise compliance not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 1 month, 6 months |
| Methods | Type of trial: RCT | |
| Participants | Acute, subacute neck pain ‐ WAD II or III | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 15 sessions | |
| Outcomes | PAIN (VAS, 0 to 10) Baseline mean: NR End of study mean: NR Absolute benefit: A 2.27, B 1.66 Reported results: significant favouring group A SMD:‐0.68 (95% CI ‐1.11 to ‐0.25); NNTB can calculate no baseline values FUNCTION: NR PARTICIPANT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Page 59, paragraph 3 |
| Allocation concealment (selection bias) | High risk | Not reported |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Page 56 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 59, paragraph 3 |
| Selective outcome (reporting bias) | Unclear risk | No protocol reported |
| Similar groups at baseline? | High risk | Reported only male/female and mean age |
| co‐interventions avoided or similar? | High risk | Not reported |
| Compliance acceptable? | Low risk | Short‐term follow‐up |
| Similar timing of outcome assessment? | Low risk | Baseline, 3 weeks |
| Methods | Type of trial: RCT | |
| Participants | Acute mechanical neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 5 sessions | |
| Outcomes | PAIN (VAS, 0 to 100) Baseline mean: group A 54.7, group B 52.7 End of study mean: group A 20.2, group B 44.7 Absolute benefit: group A 24.5, group B 8 Reported results: significant favouring group A SMD: ‐3.48 (95% CI ‐4.43 to ‐2.53); NNTB 4 FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 155, column 3, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 155, column 3, paragraph 2 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of Personal (performance bias) | High risk | Not possible |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences between interventions |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1, page 157, middle of paragraph 2 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | No dropouts |
| Selective outcome (reporting bias) | High risk | No reporting of Norwick follow‐up scores but measured at baseline |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | Page 156, column 3, paragraph 1 |
| Similar timing of outcome assessment? | Low risk | No dropouts |
| Methods | Type of trial: RCT | |
| Participants | Subacute mechanical neck pain | |
| Interventions | INDEX TREATMENT Mobilisation (B): technique: posterior‐anterior and transverse oscillations to the articular pillar and spinous process; timing: at baseline; frequency: 2 treatments/wk for 3 weeks; dose: grade III mobilisation; duration: 10 to 15 minutes; route: 1 or more restricted upper thoracic or cervical spine segments COMPARISON TREATMENT Activator instrument (C): technique: application of the instrument over the articular pillar in line with the facet joint, with the patient prone and with a setting of 1 for the Atlas and 2 for the cervical and upper thoracic segments; timing: at baseline; frequency: 2 treatments/wk for 3 weeks; dose: 1 thrust; duration: 10 to 15 minutes; route: 1 or more restricted upper thoracic or cervical spine segments CO‐INTERVENTION: not avoided: medication (specify: paracetamol 500 mg was allowed as rescue medication); avoided in trial design: other health professional (specify: Participant agreed not to take medication or receive other treatment for neck pain during the course of the study); comparable between index and control groups: package of care (specify: trigger point pressure release to active trigger points; post‐isometric relaxation stretching; exercise and ergonomic advice, use of rescue medication) Duration of treatment: 3 weeks or until symptom free, 6 sessions maximum | |
| Outcomes | PAIN (11‐point pain scale, 0 to 10) Reported results (as reported in the article): no significant differences between groups at any follow‐up points FUNCTION (Neck Bournemouth Questionnaire, 0 to 70) Reported results (as reported in the article): no significant differences between groups at any follow‐up points PATIENT SATISFACTION: NR GPE (PGIC, 7‐point scale) Reported results (as reported in the article): no significant differences between groups for any follow‐up points QoL (PCS component of SF‐36, 0 to 100) Reported results (as reported in the article): no significant differences between groups at any follow‐up points SIDE EFFECTS Mildly increased neck pain: A 4/16, B 2/15, C 7/16 Mild radiating pain: A 2/16, B 1/15, C 5/16 Mild arm weakness: A 0/16, B 0/15, C 1/16 Mild arm numbness: A 0/16, B 0/15, C 1/16 Mild headache: A 3/16, B 4/15, C 3/16 Mild fatigue: A 3/16, B 0/15, C 3/16 Mild dizziness: A 1/16, B 1/15, C 1/16 Mild muscle twitching: A 1/16, B 0/15, C 0/16 COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 3, left column, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 3, left column, paragraph 2 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to perceptible differences between interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to perceptible differences between interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to perceptible differences between interventions |
| Incomplete outcome data (attrition bias) | Unclear risk | Not adequately described |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 5, left column, paragraph 2 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | High risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 3, 6, 12 months |
| Methods | Type of trial: RCT | |
| Participants | Chronic neck pain with degenerative changes | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Medication (C): tenoxicam (NSAID) with ranitidine, median 15 days CO‐INTERVENTION: NR Duration of treatment: 3 to 4 weeks, 6 sessions | |
| Outcomes | PAIN (neck pain change scores, VAS, 0 to 10) Baseline median: A 4.5, B 2.0, C 4.0 Absolute benefit: A 1.5, B 1.0, C 0.5 Reported results: not clear SMD (A vs C): ‐0.19 (95% CI ‐0.89 to 0.51) FUNCTION (NDI, 0 to 50) Baseline median: A 32, B 40, C 28 Absolute benefit: A 10.0, B 6.0, C 0.0 Reported results: not clear SMD (A vs C): ‐0.50 (95% CI ‐1.30 to 0.29) PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: no side effects seen with acupuncture or manipulation COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 377, left column, paragraph 3 |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | High risk | Page 378, left column, paragraph 2 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Numbers in Table 1 and Table 2 do not add up |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | High risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 4 weeks |
| Methods | Type of trial: RCT Protocol: The protocol for this study was approved by the Human Research Committee of the Escuela de Osteopatía de Madrid | |
| Participants | Acute neck pain | |
| Interventions | INDEX TREATMENT Electrothermal therapy (ETT): type: infrared lamp and TENS; frequency: 2 sessions/wk; dose: infrared 250 W for 15 minutes, TENS 100 Hz for 20 minutes; route: infrared lamp 50 cm from the participant's neck, TENS applied to each side of C7 COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 5 sessions | |
| Outcomes | PAIN (intensity at rest change score, VAS, 0 to 100) Baseline mean: TSM + ETT 54.7, ETT 52.7 IP treatment mean: TSM + ETT 20.2, ETT 44.7 2‐Week follow‐up mean: TSM + ETT 26.4, ETT 41.2 4‐Week follow‐up mean: TSM + ETT 21.5, ETT 42.2 Reported results: significant for comparisons at all time points IP treatment SMD (TSM + ETT vs ETT): ‐3.43 (95% CI ‐4.38 to ‐2.49) 4‐Week follow‐up SMD (TSM + ETT vs ETT): ‐2.19 (95% CI‐2.94 to ‐1.44); NNTB 7 FUNCTION (Northwich Park Pain Questionnaire, 0 to 36) Baseline mean: TSM + ETT 27.9, ETT 27.0 IP treatment mean: TSM + ETT 15.2, ETT 23.1 2‐Week follow‐up mean: TSM + ETT 14.7, ETT 21.8 Reported results: significant for comparisons at all time points IP treatment SMD (TSM + ETT vs ETT): ‐2.17 (95% CI ‐2.92 to ‐1.42) 2‐Week follow‐up SMD (TSM + ETT vs ETT): ‐2.28 (95% CI ‐3.05 to ‐1.52); NNTB 5 4‐Week follow‐up: not collected GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | For 4‐week disability (NPPQ) data: "We only collected changes in disability up to the 2‐week follow‐up period. It would have been beneficial to see if these benefits remain at 1‐month, similar to the improvements in pain" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 21, column 3, paragraph 3 |
| Allocation concealment (selection bias) | Low risk | Page 21, column 3, paragraph 3 |
| Blinding of Participants (performance bias) | High risk | Participants in control did not receive sham or placebo |
| Blinding of Personal (performance bias) | High risk | Not possible owing to intervention |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible as participant was assessor of pain |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | No dropouts |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | |
| co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Unclear risk | Not mentioned |
| Similar timing of outcome assessment? | Low risk | |
| Methods | Type of trial: RCT Location of study: Spain | |
| Participants | Acute mechanical neck pain | |
| Interventions | INDEX TREATMENT Electrothermal therapy (ETT): type: infrared lamp and TENS; frequency: 2 sessions/wk for 3 weeks; dose: infrared 250 W for 15 minutes, TENS 100 Hz for 20 minutes; route: infrared lamp 50 cm from the participant's neck, TENS applied bilaterally to spinous process of C7 COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 6 sessions | |
| Outcomes | PAIN INTENSITY NRPS (0 to 10) Baseline mean: EG 5.6, CG 5.37 End of study mean: EG 2.3, CG 4.3 Absolute benefit: EG 3.3, CG 1.07 Reported results: significant favouring EG SMD: ‐2.16 (95% CI ‐2.91 to ‐1.42); NNTB 5 FUNCTION (NPQ, 0 to 36) Baseline mean: EG 27.8, CG 27.1 End of study mean: EG 15.2, CG 22.9 Absolute benefit: EG 12.6, CG 4.2 Reported results: significant favouring EG SMD: ‐2.12 (95% CI ‐2.87 to ‐1.38); NNTB 4 PATIENT SATISFACTION: NR QoL: NR GPE: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 308, column 1, paragraph 4 |
| Allocation concealment (selection bias) | Low risk | Page 308, column 1, paragraph 4 |
| Blinding of Participants (performance bias) | Low risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Low risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Page 309, Figure 2 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 309, Figure 2 |
| Selective outcome (reporting bias) | Unclear risk | Not reported |
| Similar groups at baseline? | Low risk | Page 310, Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Baseline, 1 week after discharge |
| Methods | Type of trial: RCT | |
| Participants | Chronic neck pain with headache | |
| Interventions | INDEX TREATMENT Group 3 sessions/wk (9s): technique: manipulation: high‐velocity low‐amplitude manipulation; frequency: 3 sessions/wk; route: cervical spine COMPARISON TREATMENT CO‐INTERVENTION: comparable between groups: heat, soft tissue therapy with massage, trigger point therapy, education (modification of ADLs), rehabilitation exercises Duration of treatment: 3 weeks, 9 to 12 sessions | |
| Outcomes | PAIN (neck pain, modified von Korff scale, 0 to 100) FUNCTION (neck disability modified von Korff scale, 0 to 100) SMD (12s vs 3s): IT ‐1.15 (95% CI ‐2.27 to ‐0.03) PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: none COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 548, under design |
| Allocation concealment (selection bias) | Unclear risk | Opaque sealed envelopes, not numbered |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Page 550, compliance and dropout |
| Randomized Participants analysed were allocated (attrition bias) | High risk | One participant lost for analysis |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | High risk | Table 2 |
| co‐interventions avoided or similar? | High risk | Table 3 |
| Compliance acceptable? | Low risk | Page 550, right column, paragraph 2 |
| Similar timing of outcome assessment? | Low risk | Baseline, 4 weeks, 12 weeks |
| Methods | Type of trial: RCT | |
| Participants | Chronic cervicogenic headache (migraine + tension type concomitant) | |
| Interventions | INDEX TREATMENT Manipulation 16 treatments (B): technique: high‐velocity low‐amplitude spinal manipulation with light massage (2 minutes) before treatment; timing: at baseline; frequency: 2×/wk for 8 weeks; duration: 10 minutes; route: cervical spine and upper thoracic COMPARISON TREATMENT Massage 8 treatments (C): technique: low‐intensity manual therapy consisting of gentle effleurage (gliding) and gentle pétrissage (kneading); timing: at baseline; frequency: 1×/wk for 8 weeks (+ 1 assessment/wk); duration: 10 minutes; route: neck and shoulder muscles Massage 16 treatments (D): technique: low‐intensity manual therapy consisting of gentle effleurage (gliding) and gentle pétrissage (kneading); timing: at baseline; frequency: 2×/wk for 8 weeks; duration: 10 minutes; route: neck and shoulder muscles CO‐INTERVENTION Not avoided: alternative health care avoided in inclusion criteria, but 10 participants had recourse to other professionals during treatment (outside care visits were balanced across groups and were not correlated with pain improvement at between four and 24 weeks); comparable between index and control groups: palliative drug use, application of heat pack (5 minutes) before treatment Duration of treatment: 8 weeks, maximum 16 sessions | |
| Outcomes | PAIN (VAS, 0 to 100) SMD (B vs A): ST ‐0.16 (95% CI ‐0.86 to 0.53), IT ‐0.37 (95% CI ‐1.04 to 0.30) SMD (B vs D): ST ‐0.60 (95% CI ‐1.31 to 0.11), IT ‐0.79 (95% CI ‐1.47 to ‐0.11); NNTB 5, treatment advantage 29% FUNCTION (neck pain, modified von Korff scale, 0 to 100) Baseline mean: A 46.3, B 36.2, C 48.5, D 41.6 SMD (B vs A): ST ‐0.35 (95% CI ‐1.05 to 0.35), IT ‐0.32 (95% CI ‐0.98 to 0.35) SMD (B vs D): ST ‐0.87 (95% CI ‐1.60 to ‐0.14), NNTB 5; treatment advantage 29% SMD (B vs D): IT ‐0.72 (95% CI ‐1.39 to ‐0.04); NNTB 5, treatment advantage 39% GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 118, right column, paragraph 4 |
| Allocation concealment (selection bias) | Low risk | Page 118, right column, paragraph 4 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1, page 121, right column, paragraph 1 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Tables 2 and 3 legends |
| Selective outcome (reporting bias) | Unclear risk | No protocol available |
| Similar groups at baseline? | High risk | Disabilities for CGH and neck pain were clinically different |
| co‐interventions avoided or similar? | Low risk | Page 122, left column, paragraph 1 |
| Compliance acceptable? | Low risk | Page 118, right column, paragraph 5 |
| Similar timing of outcome assessment? | Low risk | Abstract |
| Methods | Type of trial: RCT | |
| Participants | Subacute, chronic neck pain with radicular findings and headache | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENTS CO‐INTERVENTION: 2 participants in manipulation group had lignocaine‐hydrocortisone injections Duration of treatment: 1 session | |
| Outcomes | PAIN (count, neck/shoulder/arm/hand pain and headache present) FUNCTION: NR PARTICIPANT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 574, column 2, paragraph 3 |
| Allocation concealment (selection bias) | Low risk | Page 574, column 2, paragraph 3 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Low risk | Page 574, column 2, paragraph 3 |
| Incomplete outcome data (attrition bias) | High risk | Page 578, Table 4 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Not reported |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | High risk | Page 575, Table 2 |
| co‐interventions avoided or similar? | High risk | Not reported |
| Compliance acceptable? | High risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 1 week, 3 weeks |
| Methods | Type of trial: RCT (2 × 2 × 2 factorial design) | |
| Participants | Subacute chronic neck pain with or without radicular symptoms and headache | |
| Interventions | INDEX TREATMENTS Manipulation with heat (Manip + H): 10‐minute moist heat application before manipulation Manipulation with EMS (Manip + EMS): 10‐minute application of this modality before manipulation; parameters NR Mobilisation (Mob): technique: low‐velocity variable‐amplitude movements applied within the individual's passive range of motion directed to 1 or more restricted upper thoracic or cervical spine joint segments; frequency: NR; route: cervical spine and thoracic spine Mobilisation with heat (Mob + H): 10‐minute moist heat application before mobilisation Mobilisation with EMS (Mob + EMS): 10‐minute application of this modality before mobilisation; parameters NR COMPARISON TREATMENTS CO‐INTERVENTION: All participants received information on posture and body mechanics and 1 or more of the following ‐ stretching, flexibility or strengthening exercises ‐ and advice about ergonomic and workplace modifications. Duration of treatment: NR | |
| Outcomes | PAIN INTENSITY (average pain during previous week, most severe pain, NRS, 0 to 10) SMD (Manip + EMS vs Mob + EMS): 0.32 (95% CI ‐0.16 to 0.8) SMD (Manip + EMS + H vs Mob + EMS + H): ‐0.62 (95% CI ‐1.12 to ‐0.11) SMD (Manip + H vs Mob + H): ‐0.17 (95% CI ‐0.64 to 0.31) FUNCTION (NDI, 0 to 50) SMD (Manip + EMS + H vs Mob + EMS + H): ‐0.28 (95% CI ‐0.77 to 0.22) SMD (Manip + EMS vs Mob + EMS): 0.37 (95% CI ‐0.10 to 0.85) SMD (Manip + H vs Mob + H): ‐0.18 (95% CI ‐0.66 to 0.29) SATISFACTION (10 to 50 scale; at 4w of care) SMD (Manip + EMS vs Mob + EMS): 0.11 (95% CI ‐0.35 to 0.56) SMD (Manip + H vs Mob + H): ‐0.28 (95% CI ‐0.72 to 0.17) GPE: NR QoL: NR PATIENT SATISFACTION: NR SIDE EFFECTS: interviewed at 4 weeks of care, no known study‐related adverse events; manipulation group had statistically significant more transient minor discomfort (16%) vs mobilisation group (8.7%) COST OF CARE: number of disability days not significantly different between groups | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 1634, middle column, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 1634, middle column, paragraph 2 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences in treatment methods |
| Blinding of Personal (performance bias) | High risk | Not possible |
| Blinding of the Outcome assessor (detection bias) | High risk | Subjective rating of pain |
| Incomplete outcome data (attrition bias) | Low risk | Page 1636, paragraph 2 |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | Intention‐to‐treat not described |
| Selective outcome (reporting bias) | Unclear risk | Not described |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 2 weeks, 6 weeks, 3 months, 6 months |
| Methods | Type of trial: RCT | |
| Participants | Chronic neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 1 session | |
| Outcomes | PAIN (intensity with most painful movement, VAS, 0 to 100) FUNCTION: NR GPE (1 to 7) PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 189, right column, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 189, right column, paragraph 2 |
| Blinding of Participants (performance bias) | Low risk | Different treatments were not perceptually different to participants |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Low risk | Participant is the assessor and is blinded |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No pilot study available |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post study, no opportunity for co‐intervention |
| Compliance acceptable? | Low risk | Pre‐post study |
| Similar timing of outcome assessment? | Low risk | Pre‐post study |
| Methods | Type of trial: RCT | |
| Participants | Chronic neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 1 session | |
| Outcomes | PAIN (intensity with most painful movement change score, VAS, 0 to 100) FUNCTION: NR GPE (1 to 7) PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 624, right column, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 624, right column, paragraph 2 |
| Blinding of Participants (performance bias) | Low risk | Page 624, right column, paragraphs 3 and 4 |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Low risk | Page 624, right column, paragraphs 3 and 4 |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol available |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
| Methods | Type of trial: RCT | |
| Participants | Neck pain (duration of symptoms NR) | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 1 session | |
| Outcomes | PAIN (intensity with left rotation, 9 point faces pain scale) PAIN (intensity with right rotation, 9 point faces pain scale) FUNCTION: NR GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Page 95, left column, paragraph 4 |
| Allocation concealment (selection bias) | High risk | Unsure whether envelopes were opaque, questions about allocation numbers |
| Blinding of Participants (performance bias) | High risk | Not possible owing to intervention |
| Blinding of Personal (performance bias) | High risk | Not possible owing to intervention |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to intervention |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No protocol reported |
| Similar groups at baseline? | High risk | Not enough baseline data available |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
| Methods | Type of trial: RCT | |
| Participants | Acute/subacute non‐specific cervical disorder | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Mobilisation (B): technique: low‐velocity oscillating passive movement, particular technique according to clinical judgement; timing: at baseline; frequency: 4 treatments over 2 weeks; route: cervical spine CO‐INTERVENTION Not avoided: possibility of other treatment during follow‐up, option to continue existing exercise programme during treatment, use of other manipulations or mobilisation at different body locations during treatment not constrained Duration of treatment: 2 weeks, 4 sessions | |
| Outcomes | PAIN (NRS, 0 to 10) SMD (A vs B): IP ‐0.05 (95% CI ‐0.34 to 0.25), IT 0.11 (‐0.19 to 0.40) FUNCTION (NDI, 0 to 50) Baseline mean: A 16.1, B 14.8 SMD (A vs B): ST ‐0.06 (95% CI ‐0.35 to 0.24), IT ‐0.03 (95% CI ‐0.33 to 0.26) GPE (5‐point scale, ‐5 to 5) End of study mean: A 3.3, B 3.4 SMD (A vs B): IP ‐0.18 (95% CI ‐0.47 to 0.12), IT ‐0.06 (95% CI ‐0.35 to 0.24) PATIENT SATISFACTION: NR QoL (PCS component of the SF‐12, 0 to 100) Baseline mean: A 42.9, B 43.6 SMD (A vs B): ST 0.08 (95% CI ‐0.21 to 0.38), IT ‐0.06 (95% CI ‐0.35 to 0.24) SIDE EFFECTS Additional neck pain: A 28/91, B 24/91 Headache: A 22/91, B 17/91 Dizziness/vertigo: A 7/91, B 6/91 Nausea: A 4/91, B 7/91 Paraesthesia: A 8/91, B 5/91 Other (upper limb pain, neck stiffness, fatigue, mid‐lower back pain, unpleasant change in spinal posture): A 7/91, B 3/91 COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 1314, right column, paragraph 2 and page 1315, right column |
| Allocation concealment (selection bias) | Low risk | Page 1314, right column, paragraph 2 and page 1315, right column |
| Blinding of Participants (performance bias) | High risk | Not possible |
| Blinding of Personal (performance bias) | High risk | Not possible |
| Blinding of the Outcome assessor (detection bias) | High risk | Participant is the assessor |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | 5 participants not analysed in secondary analysis |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Co‐interventions not reported |
| Compliance acceptable? | Low risk | Page 1315, left column |
| Similar timing of outcome assessment? | Low risk | Baseline, 2, 4, 12 weeks |
| Methods | Type of trial: RCT | |
| Participants | Non‐specific cervical disorder (myofascial pain syndrome of the upper trapezius), duration NR | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT EWST (B): technique: extracorporeal shock wave therapy applied to trigger points with 17‐mm gun and low power; timing: at baseline; frequency: 2 sessions/wk for 4 weeks; dose: 1000 impulsions, 5 Hz; route: upper trapezius TPI (C): technique: trigger point injection of 0.2 mL of 0.3% lidocaine (Travell method); timing: at baseline; frequency: 2 sessions/wk for 4 weeks; dose: 1 injection/trigger point; route: upper trapezius CO‐INTERVENTION Comparable between index and control groups: Each participant received hot pack therapy for 20 minutes and US for 5 minutes Duration of treatment: 4 weeks, 8 sessions | |
| Outcomes | PAIN (NRS, 0 to 10) SMD (A vs B): IP ‐1.01 (95% CI ‐1.91 to ‐0.11) SMD (A vs C): IP ‐1.05 (95% CI ‐1.96 to ‐0.15) FUNCTION (NDI, 0 to 50) Baseline mean: A 24.45, B 28.00, C 26.73 SMD (A vs B): IP 0.69 (95% CI ‐0.18 to 1.55) SMD (A vs C): IP 0.76 (95% CI ‐0.11 to 1.63) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences in interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to differences in interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences in interventions |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | No dropouts |
| Selective outcome (reporting bias) | Unclear risk | No protocol or registration |
| Similar groups at baseline? | Low risk | Tables 1 and 2 |
| co‐interventions avoided or similar? | Unclear risk | P343L medication may have increased effects of specific techniques |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Unclear risk | Baseline, 4 weeks for intervention but no description of when follow‐up was performed |
| Methods | Type of trial: RCT | |
| Participants | Chronic mechanical neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Traditional Chinese massage (B): technique: massage technique such as stroking, rubbing, shaking, pinching, plucking, clapping and acupressure; frequency: 8‐ to 20‐minute sessions, 1 session every 3 days for 24 days; route: cervical spine CO‐INTERVENTION Duration of treatment: 24 days, 8 sessions | |
| Outcomes | PAIN (NPRS, 0 to 10 mm) End of study mean: A 2.06, B 4.54 SMD (A vs B): ‐1.30 (‐2.02 to ‐0.57) FUNCTION (NPQ, 42 items) Baseline mean: A 35.44, B 36.14 SMD (A vs B): ‐1.16 (‐1.88 to ‐0.45) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 310, column 2, paragraph 1 |
| Allocation concealment (selection bias) | Low risk | Page 310, column 2, paragraph 1 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | High risk | Figure 2 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Figure 2 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 3‐month follow‐up |
| Methods | Type of trial: RCT | |
| Participants | Chronic non‐specific cervical disorder | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Massage (B): technique: effleurage, stroking and pétrissage; timing: at baseline; frequency: 2 or 3 treatments/wk for 4 weeks; duration: 30 minutes; route: neck and upper back muscles CO‐INTERVENTION Not avoided: Participants were allowed to continue taking prescribed pain medication; avoided in trial design: other therapeutic interventions and modalities; comparable between groups: application of moist heat packs to the neck and upper back for 20 to 30 minutes before treatment Duration of treatment: 4 weeks, maximum 12 sessions | |
| Outcomes | PAIN (VAS, 0 to 100 mm) SMD (A vs B): ‐0.25 (95% CI ‐1.09 to 0.59) FUNCTION (NDI, 0 to 50) Baseline mean: A 13.54, B 12.75 SMD (A vs B): ‐0.52 (95% CI ‐1.35 to 0.32) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 645, right column |
| Allocation concealment (selection bias) | Low risk | Page 645, right column |
| Blinding of Participants (performance bias) | High risk | Not possible |
| Blinding of Personal (performance bias) | High risk | Not possible |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1 – no dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | No dropouts |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | High risk | Table 1, Table 2 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Exercise compliance not reported. |
| Similar timing of outcome assessment? | Low risk | Page 648, left column, paragraph 1 |
| Methods | Type of trial: RCT | |
| Participants | Chronic (> 3 months) mechanical neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT 10‐Month attention‐control group (AC); frequency: participants attended the clinic once every 2 months for 20 to 30 minutes for 10 months, 5 sessions in total CO‐INTERVENTION: NR Duration of therapy period: 10 months | |
| Outcomes | PAIN (VAS, 0 to 10 cm) FUNCTION (NDI, 0 to 50) Baseline mean: AC 26.1, SMT 21.5 PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: none COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 2, left column |
| Allocation concealment (selection bias) | Low risk | Page 3, left column |
| Blinding of Participants (performance bias) | High risk | Not possible owing to intervention |
| Blinding of Personal (performance bias) | High risk | Not possible owing to intervention |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to intervention |
| Incomplete outcome data (attrition bias) | Low risk | Figure 1 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Not all randomly assigned participants were included; Figure 1 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | High risk | Page 7, right column |
| Compliance acceptable? | High risk | Page 7, left column |
| Similar timing of outcome assessment? | Low risk | Baseline, 12 months; mid‐trial data unclear; however, we believe long‐term follow‐up data are more important |
| Methods | Type of trial: RCT | |
| Participants | Subacute chronic neck pain, no radiculopathy | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 1 session | |
| Outcomes | PAIN INTENSITY (VAS, 0 to 10 cm) FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not reported |
| Allocation concealment (selection bias) | High risk | Not reported |
| Blinding of Participants (performance bias) | High risk | Not reported |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Page 513, Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
| Methods | Type of trial: RCT Location of study: USA | |
| Participants | Mechanical neck pain < 3 months (acute and subacute) | |
| Interventions | INDEX TREATMEAT Experimental group (EG): thoracic spine manipulations plus cervical non‐thrust manipulations plus cervical spine active range of motion exercises (thoracic spine manip plus control vs control): technique: 2 upper thoracic spine thrust manipulations and 2 middle thoracic spine thrust manipulations plus cervical spine posterior‐anterior non‐thrust manipulations; frequency: 10 reps for non‐thrust manip; dose: 1 to 2 attempts for thrust manip; duration: 2 treatment sessions; routes: T1‐3 and T4‐7 and C2‐7; duration of follow‐up: 1 week, 2 to 3 days following last treatment session COMPARISON TREATMENT Comparison group (CG): cervical posterior‐anterior non‐thrust manipulation to the segment spinous processes plus cervical active range of motion exercises; frequency: 10 reps followed by 10‐second rest between segments; dose: grade 3; duration: 2 treatment sessions; route: spinous process of C2‐C7; duration of follow‐up: 1 week, 2 to 3 days following last treatment session CO‐INTERVENTION: NR Duration of therapy period: 1 week | |
| Outcomes | PAIN INTENSITY (NPRS, 0 to 10) FUNCTION (NDI, 0 to 50) PATIENT SATISFACTION: NR QoL: NR GPE: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 120, column 3, paragraph 2 |
| Allocation concealment (selection bias) | Unclear risk | Did not follow adequate level of allocation concealment |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Figure 5, page 122 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 122, column 2, paragraph 1 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Page 123, Table 2 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 1 week |
| Methods | Type of trial: RCT | |
| Participants | Chronic neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Acupuncture (C): technique: 8 to 10 needles placed in local paraspinal and intramuscular pain areas, 5 needles placed in distal point meridians; frequency: 2 sessions/wk until asymptomatic or acceptable pain relief achieved; dose: 20 minutes with turning or flicking needles every 5 minutes if tolerated; route: sterile HWATO Chinese acupuncture guide tube needles (50 mm length, 0.25 mm gauge) CO‐INTERVENTION: not avoided Duration of treatment: 9 weeks or until asymptomatic, maximum 18 sessions | |
| Outcomes | PAIN (intensity, VAS, 0 to 10) Absolute benefit: A 3.2, B ‐0.7, C 4.5 FUNCTION (NDI, 0 to 50) Absolute benefit: A 8, B 6, C 12 GPE: NR PATIENT SATISFACTION: NR QoL: NR for neck group alone SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation technique not adequate |
| Allocation concealment (selection bias) | Unclear risk | Envelopes not sequentially numbered |
| Blinding of Participants (performance bias) | High risk | Not possible owing to study design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to study design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to study design |
| Incomplete outcome data (attrition bias) | High risk | Dropout rate > 50%, only compliers used |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Page 6 ‐ improper Intention‐to‐treat technique; only responders included |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Unclear risk | NDI and Oswestry data not given; data for only 62 participants given |
| co‐interventions avoided or similar? | High risk | Page 8, left column, paragraph 2 |
| Compliance acceptable? | High risk | Page 8, left column, paragraph 2 |
| Similar timing of outcome assessment? | Low risk | Baseline, 12‐month follow‐up |
| Methods | Type of trial: RCT | |
| Participants | Chronic neck pain with headache | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 6 sessions | |
| Outcomes | PAIN (headache intensity per episode; VAS, 0 to 100) FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 327, right column, paragraph 1 |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Page 328, left column, paragraph 1 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | One participant lost for analysis |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Tables 2 and 3 |
| co‐interventions avoided or similar? | High risk | Unsure whether co‐interventions were similar between groups |
| Compliance acceptable? | Unclear risk | Diary described, but no data on compliance with treatment |
| Similar timing of outcome assessment? | Low risk | Figure 1 |
| Methods | Type of trial: RCT | |
| Participants | Neck pain, duration not reported (NR) | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: not specified Duration of treatment: 3 weeks, 6 sessions | |
| Outcomes | PAIN INTENSITY (NRS‐101, 0 to 100) FUNCTION (NDI, 0 to 50) PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Not reported |
| Allocation concealment (selection bias) | High risk | Not reported |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | High risk | Not reported |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Not reported |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Page 329, Table 21 |
| co‐interventions avoided or similar? | High risk | Not reported |
| Compliance acceptable? | High risk | Not Reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 4 weeks |
| Methods | Type of trial: RCT | |
| Participants | Acute mechanical neck pain (with or without unilateral upper extremity symptoms) | |
| Interventions | INDEX TREATMENT Cervical thrust manipulation (A): technique: during first 2 sessions: mid‐range high‐velocity low‐amplitude thrust into rotation to both sides of cervical segment directed up towards the participant's contralateral eye (participant in supine position with cervical spine rotation and side bending); timing: at baseline; frequency: 3× for first week and 2× during second week, 5 treatment sessions; dose: maximum of 2 thrusts for each manipulation technique; route: cervical spine COMPARISON TREATMENT Thoracic thrust manipulation (B): technique: application of 3 different thoracic spine manipulation techniques during first 2 sessions; mid‐range high‐velocity upward distraction thrust to lower thoracic spine (participant in a sitting position) and end‐range high‐velocity low‐amplitude anterior‐posterior thrust to mid‐thoracic and lower thoracic spines with cervicothoracic flexion (participant in supine position); timing: at baseline; frequency: 3× for the first week and 2× during the second week, 5 treatment sessions; dose: maximum 2 thrusts for each manipulation technique; route : thoracic spine CO‐INTERVENTION: comparable between groups: during last 3 therapy sessions, participants from both groups performed a standardised exercise programme to improve ROM and strength (3 times 10 reps, 3 to 4×/d) and did not receive further manipulation Duration of treatment: 2 weeks, 5 sessions | |
| Outcomes | PAIN (NRS, 0 to 10) SMD (A vs B): ST ‐2.43 (95% CI ‐3.64 to ‐1.21); NNTB 12 FUNCTION (NDI, 0 to 50) Baseline mean: A 13.4, B 12.6 SMD (A vs B): ST ‐1.01 (95% CI ‐1.96 to ‐0.07); NNTB 5 GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: reported A 1/14 reported minor increased neck pain after first treatment COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 210, right column, paragraph 1 |
| Allocation concealment (selection bias) | Unclear risk | Envelopes not numbered |
| Blinding of Participants (performance bias) | High risk | Interventions perceptibly different |
| Blinding of Personal (performance bias) | High risk | Interventions perceptibly different |
| Blinding of the Outcome assessor (detection bias) | High risk | Interventions perceptibly different |
| Incomplete outcome data (attrition bias) | High risk | High dropout rate in cervical manipulation group; all dropouts were in this group |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Page 212, middle column, paragraph 2 and Figure 5 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Unclear risk | Duration different between groups, see page 217 for study author comments on this |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 1 week, 4 weeks, 6 months |
| Methods | Type of trial: RCT | |
| Participants | Neck disorder with radiculopathy (radicular symptoms or signs), duration NR | |
| Interventions | INDEX TREATMENT Manual therapy (A): technique: cervical lateral glide in supine position of all cervical segments (C2 to C7), PAs in prone position of hypomobile segment of the thoracic spine and sliding neural dynamic technique of the median nerve (as described by Butler); timing: at baseline; frequency: 3 times/wk for 3 weeks; dose: grade III to IV oscillatory movements as described by Maitland for cervical glide and thoracic mobilisation and unknown for the neural dynamic technique; route: cervical spine, thoracic spine and upper extremity of the affected side COMPARISON TREATMENT Exercises (B): technique: deep neck flexor strengthening in supine position, lower and middle trapezius strengthening in prone position and serratus anterior strengthening in standing position. No home programme was prescribed; timing: at baseline; frequency: 3 times/wk for 3 weeks; dose: 10 × 10 seconds for neck flexor, 2 × 15 reps (with or without dumbbells) for trapezius and serratus anterior; route: cervical spine, thoracic spine and upper extremity of affected side CO‐INTERVENTION: NR Duration of treatment: 3 weeks, 9 sessions | |
| Outcomes | PAIN (NRS, 0 to 0) SMD (A vs B): 0.58 (95% CI ‐0.32 to 1.48) FUNCTION (NDI, 0 to 50) Baseline mean: A 39.6, B 28.7 SMD (A vs B): 0.76 (95% CI ‐0.16 to 1.67) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear for sequence |
| Allocation concealment (selection bias) | Unclear risk | Unclear for sequence |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Unclear risk | Not reported |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Table 4 |
| Selective outcome (reporting bias) | Unclear risk | Not reported |
| Similar groups at baseline? | High risk | Tables 2 and 3, initial NDI difference |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Unclear risk | Not clear when outcomes were performed each week |
| Methods | Type of trial: RCT | |
| Participants | Chronic mechanical neck pain | |
| Interventions | INDEX TREATMENT Full manipulation group (A): technique: high‐velocity low‐amplitude thrust, (1) cervical spine: manipulation directed upward and medially in the direction of the participant's contralateral eye, participant in supine position with the cervical spine in a neutral position, (2) cervicothoracic junction: thrust applied toward the participant's right or left side, thrust applied bilaterally, participant prone with head and neck rotated, (3) upper thoracic spine: distraction thrust manipulation directed in an upward direction, participant in supine position with arms crossed; timing: at baseline; frequency: 1 session; dose: 1 to 2 thrusts per area; route: cervical spine, cervicothoracic junction, upper thoracic spine, symptomatic level COMPARISON TREATMENT Cervical manipulation group (B): technique: high‐velocity low‐amplitude thrust manipulation directed upward and medially in the direction of the participant's contralateral eye, participant in supine position with the cervical spine in a neutral position; timing: at baseline; frequency: 1 treatment session; dose: 1 to 2 thrusts; route: cervical spine, symptomatic level CO‐INTERVENTION: N/A Duration of treatment: 1 day, 1 session | |
| Outcomes | PAIN (NPRS, 0 to 10) SMD: 0.08 (95% CI ‐0.36 to 0.51) FUNCTION (NDI, 0 to 50) Baseline mean: A 22.2, B 23.7 SMD: ‐0.17 (95% CI ‐0.61 to 0.27) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: reported Minor increase in neck pain or fatigue after manipulation(s): A 1/41, B 1/40 COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 3, column 2, paragraph 1 |
| Allocation concealment (selection bias) | Low risk | Page 3, column 2, paragraph 1 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Figure 4, page 4 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Figure 4, page 4 |
| Selective outcome (reporting bias) | Unclear risk | Not reported |
| Similar groups at baseline? | Low risk | Table 1, page 5 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Low risk | Short‐term follow‐up |
| Similar timing of outcome assessment? | Low risk | Baseline, 7‐day follow‐up |
| Methods | Type of trial: RCT | |
| Participants | Chronic mechanical neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Kinesio‐tape (B): technique: tape with width of 5 cm and thickness of 0.5 mm. Each tail of the first strip (blue Y‐strip, 2‐tailed) was applied with the participant's neck in a position of cervical contralateral side bending and rotation. Tape was first placed from T1‐T2 to C1‐C2. Overlying strip (black) was a space‐tape (opening) placed perpendicular to the Y‐strip, over C3‐C6, with the participant's cervical spine in flexion to apply tension to posterior structures; timing: at baseline; duration: tape worn for 7 days; route: thoracic spine and cervical spine CO‐INTERVENTION: N/A Duration of treatment: 1 day, 1 session | |
| Outcomes | PAIN (NPRS, 0 to 10) SMD (A vs B): 0.00 (95% CI ‐0.45 to 0.45) FUNCTION (NDI, 0 to 50) Baseline mean: A 22.5, B 21.4 SMD (A vs B): 0.46 (95% CI 0.01 to 0.92) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: reported Minor increase in neck pain or fatigue after manipulation: A 3/36, B 0/40 COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pages 725 to 726 |
| Allocation concealment (selection bias) | Low risk | Pages 725 to 726 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to intervention |
| Blinding of Personal (performance bias) | High risk | Not possible owing to intervention |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to intervention |
| Incomplete outcome data (attrition bias) | Low risk | Figure 4 |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | Unclear whether ITT was properly performed – see manipulation group numbers in Table 1 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported whether participants in kinesiotape group kept it on for 7 days |
| Similar timing of outcome assessment? | Low risk | Baseline, 7 days |
| Methods | Type of trial: RCT | |
| Participants | Subacute/chronic mechanical neck pain (facet joint dysfunction/syndrome) | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Low‐level laser therapy (B): technique: use of a Uni‐Laser 201 830‐nm gallium Combination of CMT and LLLT (C): technique: combination of the 2 interventions mentioned before. Manipulative procedures completed first. Protocols were the same; timing: at baseline; frequency: 6 sessions over 3 weeks; duration: 30 minutes; see groups A and B for other dosage parameters CO‐INTERVENTION: avoided in trial design: participants requested not to take analgesic or NSAID or any other form of physical treatment to the neck, nor to partake in activities that would exacerbate the pain for the duration of the study Duration of treatment: 3 weeks, 6 sessions | |
| Outcomes | PAIN (NRS, 0 to 10) FUNCTION (NDI, 0 to 50, converted in 100%) Baseline mean: A 24, B 23.5, C 26 GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: reported: no adverse serious effects in any study groups COST OF CARE: NR | |
| Notes | Wrote study author in 2015 to request additional data (SD) for week 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 154, right column, paragraph 4 |
| Allocation concealment (selection bias) | Low risk | Page 154, right column, paragraph 4 |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences between interventions |
| Incomplete outcome data (attrition bias) | Low risk | Figure 3 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Figure 3 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Unclear risk | Co‐interventions not reported |
| Compliance acceptable? | Unclear risk | Compliance not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 2 weeks, 3 weeks, 4 weeks (see abstract) |
| Methods | Type of trial: RCT | |
| Participants | Neck pain, duration NR | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 4 weeks for manipulation group, unknown for control group | |
| Outcomes | PAIN (neck pain intensity (pain right now); VAS, 0 to 10) FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to study design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to study design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to study design |
| Incomplete outcome data (attrition bias) | High risk | Table 1 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Table 1 |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Tables 1 and 2 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 6 weeks, 12 months |
| Methods | Type of trial: RCT | |
| Participants | Neck disorder ± radicular symptoms or signs (inclusion criteria; patient with or without irradiation into the arm(s) that changed with movements between C2 and C7), duration NR | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Mobilisation 3 levels below or above (B): technique: intermittent translatoric (perpendicular to the facet plane) traction 3 levels below or above the most painful joint between C2 and C7; timing: at baseline; frequency: 1 session; dose: grade II, 6 to 7 Hz and changed as needed at 30 seconds; duration: 4 minutes; route: cervical spine CO‐INTERVENTION: not specified. Duration of treatment: 1 day, 1 session | |
| Outcomes | PAIN (NRS, 0 to 10) SMD (A vs B): ‐0.13 (95% CI ‐0.48 to 0.22) FUNCTION: NR GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS Allodynia: A 1/59, B 1/67 COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not adequately described |
| Blinding of Participants (performance bias) | Low risk | Our group believes that the participant would not be able to perceive differences between the 2 interventions |
| Blinding of Personal (performance bias) | High risk | Page 103, middle column, paragraph 1 and page 107, left column, paragraph 2 |
| Blinding of the Outcome assessor (detection bias) | Low risk | Participant is the assessor |
| Incomplete outcome data (attrition bias) | Low risk | Only 2 dropouts due to allodynia |
| Randomized Participants analysed were allocated (attrition bias) | High risk | 2 dropouts not analysed |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Page 104 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
| Methods | Type of trial: RCT | |
| Participants | Specific cervical disorder: herniated cervical disc (MRI diagnosis), duration NR | |
| Interventions | INDEX TREATMENT Chuna manual therapy (A): technique: soft tissue manipulation and thrust technique analogous to chiropractic manipulation, in which the practitioner’s hands apply focused and forceful movements to various areas of the body; timing: at baseline; frequency : 1 session/d for 2 weeks; duration: 20 minutes; route: various areas of the body COMPARISON TREATMENT Traction (B): technique: cervical traction treatment; timing: at baseline; CO‐INTERVENTION: not specified Duration of treatment: 2 weeks, 12 sessions | |
| Outcomes | PAIN (VAS, 0 to 10) SMD (A vs B): ‐0.94 (95% CI ‐1.75 to ‐0.12) FUNCTION: NR GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: reported (no adverse effects occurred) COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not adequately described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences between interventions |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | No dropouts |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Unclear risk | Data were given only for age and pain; missing for other characteristics |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Low risk | Table 1 – appears that all received 12 treatments. |
| Similar timing of outcome assessment? | Low risk | Baseline, 2 weeks |
| Methods | Type of trial: RCT | |
| Participants | Chronic non‐specific neck pain | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT Thoracic mobilisation (B): technique: described by Cleland et al. Practitioner’s flat hand placed under T4 segment, participant in the same position as described in group A. Application of a light 3‐second compression of the participant's arm to the chest; timing: at baseline; frequency: 1 treatment session; dose: 1 mobilisation; route: thoracic spine (T3 to T4) CO‐INTERVENTION: avoided in trial design; no medication that alters the functioning of the autonomic nervous system less than 24 hours before the study, and no caffeinated drinks, smoke or food less than 12 hours before the study Duration of treatment: 1 day, 1 session | |
| Outcomes | PAIN (VAS, 0 to 100) FUNCTION: NR GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 184, left column, paragraph 2 |
| Allocation concealment (selection bias) | Low risk | Page 184, left column, paragraph 2 |
| Blinding of Participants (performance bias) | Unclear risk | Unsure whether control was a true sham manipulation |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Unclear risk | Unsure whether control was a true sham manipulation |
| Incomplete outcome data (attrition bias) | Low risk | 1 dropout |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Figure 3 and Table 1 do not add up to 101 analysed |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 1 |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
| Methods | Type of trial: RCT cross‐over design | |
| Participants | Subacute chronic neck pain with variable degenerative changes (cervical spondylosis) | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: "other medical management was not restricted during the study" Duration of treatment: 1 session | |
| Outcomes | PAIN (neck pain intensity; VAS, 0 to 100) FUNCTION (selected daily activities; VAS, 0 to 100) PATIENT SATISFACTION: NR QoL: NR GPE [patient perceived effect, 0 (completely well) to 8 (worst possible), collapsed to dichotomous response (improved/not improved) SIDE EFFECTS: 2 people had superficial phlebitis following diazepam injection and recovered uneventfully; 2 people in the manipulation group reported new discomfort in their neck followed by improvement in their chronic neck pain COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 533, column 1, paragraph 1 |
| Allocation concealment (selection bias) | Low risk | Page 533, column 2, paragraph 2 |
| Blinding of Participants (performance bias) | Low risk | Cross‐over design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | Low risk | Page 533, column 2, paragraph 3 |
| Incomplete outcome data (attrition bias) | Low risk | Page 534, column 1, paragraph 1 |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Cross‐over design |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Page 533, column 1, paragraph 5 |
| co‐interventions avoided or similar? | High risk | Not reported |
| Compliance acceptable? | Low risk | Cross‐over design |
| Similar timing of outcome assessment? | Low risk | Baseline, 3 weeks, 12 weeks |
| Methods | Type of trial: RCT | |
| Participants | Subacute chronic neck pain > 3 months WAD II | |
| Interventions | INDEX TREATMENT frequency of treatment: 1 session Dose of treatment: 3 sets of 1 minute; 5 minutes total: 3 minutes of treatment with 1 minute rest between sets Duration of treatment: 1 session Route: C5/6 CONTROL TREATMENT CO‐INTERVENTION: avoided in trial designs | |
| Outcomes | PAIN (neck pain intensity; VAS, 0 to 10) Baseline mean: SMT 6.2, cntl 4.5 End of study mean: SMT 5.8, cntl 3.6 FUNCTION: NR PATIENT SATISFACTION: NR QoL: NR GPE: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Page 151, left column, paragraph 2 |
| Allocation concealment (selection bias) | Unclear risk | Page 151, left column, paragraph 2 |
| Blinding of Participants (performance bias) | High risk | Stated participant not blinded, page 153, left column, paragraph 3 |
| Blinding of Personal (performance bias) | High risk | Not possible |
| Blinding of the Outcome assessor (detection bias) | High risk | Stated participant not blinded, page 153, left column, paragraph 3 |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | High risk | ITT not done for NFR |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | High risk | VAS different between groups |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
| Methods | Type of trial: RCT | |
| Participants | Subacute or chronic neck pain | |
| Interventions | INDEX TREATMENT Cervical manipulation (A): technique: high‐velocity low‐amplitude manipulation of hypomobile segment of the cervical spine; frequency: 2 sessions/wk; dose: grade 5 manipulation; route: hypomobile segments identified from C0 to C7 COMPARISON TREATMENT Thoracic and sacroiliac manipulation + muscle energy technique (B): For thoracic spine and sacroiliac joint manipulation: technique: high‐velocity low‐amplitude spinal manipulation; frequency: 2 sessions/wk; dose: grade 5 manipulation; route: thoracic spine and sacroiliac joint. Muscle energy: technique: post‐isometric relaxation technique to hypertonic muscles according to Lewis procedures; frequency: 2 sessions/wk; dose: 2 sets of 3 reps; route: left or right scalenes, upper fibres of trapezius, levator scapulae, suboccipital muscles based on assessment findings CO‐INTERVENTION: NR Duration of treatment: 2 weeks, 4 sessions | |
| Outcomes | PAIN (VAS, 0 to 100) Absolute benefit: A 2, B ‐30 FUNCTION (NDI, 0 to 100%) Absolute benefit: A 4, B 8 GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 3, left and right columns |
| Allocation concealment (selection bias) | Low risk | Page 3, left and right columns |
| Blinding of Participants (performance bias) | High risk | Not possible owing to study design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to study design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to study design |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Table 2, no dropouts |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | High risk | NDI scores different between groups |
| co‐interventions avoided or similar? | Unclear risk | No data available for measurement |
| Compliance acceptable? | Low risk | Page 5, right column, paragraph 2 |
| Similar timing of outcome assessment? | Low risk | Baseline, 2 weeks |
| Methods | Type of trial: quasi‐RCT | |
| Participants | Neck pain, duration NR | |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION: NR Duration of treatment: 4 weeks, 10 sessions | |
| Outcomes | PAIN INTENSITY (NRS, 0 to 100) SMD (A vs B): IP ‐0.67 (95% CI ‐1.41 to 0.07), ST SMD (A vs B): ‐0.69 (95% CI ‐1.43 to 0.05) FUNCTION (NDI, 0 to 50) PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 327, right column, paragraph 1 |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | Not described |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Table 14 |
| co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Unclear risk | Unclear description, page 328, left column, paragraph 3 |
| Methods | Type of trial: RCT | |
| Participants | Chronic cervicogenic headache (diagnosed according to ICDH‐II); | |
| Interventions | INDEX TREATMENT Manual therapy to cervical spine (A): technique: manual therapy, therapist decision; timing: at baseline; frequency: depended on therapist decision; dose: 6 treatments; duration: 30 minutes; route: cervical spine COMPARISON TREATMENT Manual therapy to the TMJ (B): technique: accessory (translatory) movements of the temporomandibular region and/or masticatory muscle techniques (tender‐trigger point treatment and muscle stretching), active and passive movement of cranial nerve tissue, co‐ordination exercises, home exercises and treatment of the cervical region when necessary; timing: at baseline; frequency: depended on therapist decision; dose: 6 sessions; duration: 30 minutes; route: TM region and cervical spine CO‐INTERVENTION: not specified Duration of treatment: minimum 21 and maximum 42 days, 6 sessions | |
| Outcomes | PAIN (CGH pain, CAS, 0 to 10) SMD (A vs B): IP 2.27 (95% CI 1.43 to 3.10); NNTB 2, IT 3.55 (95% CI 2.50 to 4.61); NNTB 2 FUNCTION (NDI, 0 to 50) Baseline mean: A 15.4, B 15.6 Reported results: significantfavouring B SMD (A vs B): IP 1.35 (95% CI 0.64 to 2.06); NNTB 5, IT 2.22 (95% CI 1.39 to 3.04); NNTB 4 GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 3, left column, paragraph 1 |
| Allocation concealment (selection bias) | Unclear risk | Concealment not described |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to differences between interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences between interventions |
| Incomplete outcome data (attrition bias) | Low risk | Page 5, right column, paragraph 3 |
| Randomized Participants analysed were allocated (attrition bias) | High risk | Intention‐to‐treat not done; Figure 1 shows numbers; page 5, right column, paragraph 3 |
| Selective outcome (reporting bias) | Unclear risk | No protocol |
| Similar groups at baseline? | Low risk | Table 3 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Home exercise compliance not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 3 months, 6 months |
| Methods | Type of trial: quasi‐RCT | |
| Participants | Subacute neck pain | |
| Interventions | INDEX TREATMENT COMPARISON Manipulation with Activator II (B): technique: manipulation using Activator II adjusting Instrument, mechanical force, manually assisted; frequency: 2 to 3 sessions/wk; route: cervical spine CO‐INTERVENTION: no medication ≥ 1 month; no other treatment modalities, exercises or education prescribed Duration of treatment: 4 weeks, 8 sessions | |
| Outcomes | PAIN INTENSITY (NRS, 0 to 100) FUNCTION (NDI, 0 to 50) PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 261, right column, paragraph 1 |
| Allocation concealment (selection bias) | Unclear risk | Unsure whether opaque and sealed envelopes were used |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Unclear risk | Not described |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | Not described |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Low risk | Table 5 |
| co‐interventions avoided or similar? | Unclear risk | Not described in Results section |
| Compliance acceptable? | Unclear risk | Not described |
| Similar timing of outcome assessment? | Low risk | Baseline, 4 weeks, 8 weeks |
| Methods | Type of trial: RCT | |
| Participants | Subacute/Chronic cervicogenic headache with neck pain | |
| Interventions | INDEX TREATMENT Mobilisation (A): technique: low‐velocity high‐amplitude passive spinal mobilisation (posterior‐anterior central vertebral pressure; unilateral and bilateral posterior‐anterior vertebral pressure; transverse vertebral pressure); timing: at baseline; frequency: 2 sessions/wk for 6 weeks; duration: 30 to 40 minutes; route: C1 to C3 cervical segment COMPARISON TREATMENT Massage (B): technique: massage regimen consisted of 6 phases: warm‐up, myofascial release, manual cervical traction, trigger point therapy procedure, facilitated stretching techniques and session closure; timing: at baseline; frequency: 2 sessions/wk for 6 weeks; duration: 30 to 40 minutes; route: C‐spine and upper limb/cervical musculature CO‐INTERVENTION: avoided in trial design: therapeutic treatment for neck pain or headache during previous 6 months; comparable between index and control groups: All participants underwent active neck range of motion, isometric and dynamic strengthening and endurance exercises in 2 sessions/wk for 6 weeks Duration of treatment: 6 weeks, 12 sessions | |
| Outcomes | PAIN (CGH pain, NRS, 0 to 10) SMD (A vs B): IP ‐2.89 (95% CI ‐3.85 to ‐1.93) FUNCTION (NDI, 0 to 50) Baseline mean: A 46.7, B 48.3 Reported results: not significant SMD (A vs B): IP 0.38 (95% CI ‐0.28 to 1.04) GPE: NR PATIENT SATISFACTION: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated |
| Allocation concealment (selection bias) | Unclear risk | Envelopes not numbered |
| Blinding of Participants (performance bias) | High risk | Not possible owing to differences in interventions |
| Blinding of Personal (performance bias) | High risk | Not possible owing to differences in interventions |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to differences in interventions |
| Incomplete outcome data (attrition bias) | Low risk | Page 19, left column, paragraph 2 |
| Randomized Participants analysed were allocated (attrition bias) | Unclear risk | 2 dropouts apparently not analysed, but unclear |
| Selective outcome (reporting bias) | Unclear risk | No protocol or registration |
| Similar groups at baseline? | Low risk | Table 4 |
| co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Similar timing of outcome assessment? | Low risk | Baseline, 7 weeks |
| Methods | Type of trial: RCT | |
| Participants | Subacute neck pain | |
| Interventions | INDEX TREATMENT COMPARISON CO‐INTERVENTION: avoided Duration of treatment: 1 session | |
| Outcomes | PAIN INTENSITY (VAS, 0 to 100) FUNCTION: NR PATIENT SATISFACTION: NR GPE: NR QoL: NR SIDE EFFECTS: NR COST OF CARE: NR | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Page 158, left column, paragraph 4 |
| Allocation concealment (selection bias) | High risk | Page 158, left column, paragraph 4, considered high risk of bias according to scale |
| Blinding of Participants (performance bias) | High risk | Not possible owing to design |
| Blinding of Personal (performance bias) | High risk | Not possible owing to design |
| Blinding of the Outcome assessor (detection bias) | High risk | Not possible owing to design |
| Incomplete outcome data (attrition bias) | Low risk | Pre‐post design |
| Randomized Participants analysed were allocated (attrition bias) | Low risk | Pre‐post design |
| Selective outcome (reporting bias) | Unclear risk | No reported protocol |
| Similar groups at baseline? | Unclear risk | Page 259, statistical analysis section |
| co‐interventions avoided or similar? | Low risk | Pre‐post design |
| Compliance acceptable? | Low risk | Pre‐post design |
| Similar timing of outcome assessment? | Low risk | Pre‐post design |
-
Record of personal communications/Unpublished data.
-
Allison 2001 provided an early manuscript and data clarification.
-
Brodin 1985 provided additional raw data to facilitate study selection and calculation of effect measures.
-
Bronfort 2000 provided his manuscript before publication in Spine and included raw data on range, muscle strength and endurance.
-
Coppieter 2001 provided 2 early manuscripts and raw data.
-
Hoving 2002 provided an early manuscript and clarification of data.
-
Hurwitz 2002 provided an early manuscript.
-
Jull 2001 provided an early manuscript and additional unpublished data.
-
Koes 1992 provided additional raw data on the neck disorder subgroup to facilitate calculation of effect measures.
-
Sloop 1982 communicated that additional information on raw data was not available.
-
-
Definitions of terms.
-
-
Acute ≤ 30 days (1 month, 4 weeks).
-
Subacute = 30 days (1 month, 4 weeks) to 90 days (3 months, 12 weeks).
-
Chronic ≥ 90 days (3 months, 12 weeks).
-
-
Timing of outcomes.
-
IP = immediate post‐treatment follow‐up < 1 dayIT = intermediate‐term follow‐up ≥ 3 months and < 1 year.
-
LT = long‐term follow‐up ≥ 1 year.
-
ST = short‐term follow‐up ≥ 1 day and < 3 months.
-
-
Types of controls.
-
AC = attention control.
-
cntl = control group.
-
Manual therapy placebo.
-
Non‐manual therapy placebo.
-
NT = no treatment control.
-
Same other treatment control.
-
Sham.
-
Wait list control.
-
-
-
Short forms commonly used in text.
-
Clinical terms.
-
AROM = active range of motion.
-
CGH = cervicogenic headache.
-
DT = drug therapy.
-
ED = education.
-
EMS = electrical muscle stimulation.
-
ETT = electrothermal therapy.
-
H = heat.
-
Kinesio‐tape = an elastic therapeutic sports taping product applied to the neck, thorax and shoulder placed on the skin.
-
manip = manipulation.
-
MNP = mechanical neck pain.
-
mob = mobilisation.
-
MT = manual therapy
-
PEMT = pulsed electromagnetic therapy.
-
PMM = physical medicine methods.
-
PROM = passive range of motion.
-
PSWD = pulsed short‐wave diathermy.
-
SMT = spinal manipulation therapy.
-
-
-
TENS = transcutaneous electrical nerve stimulation.
-
TSM = thoracic spinal thrust manipulation.
-
TTM = thoracic thrust manipulation.
-
-
-
US = ultrasound
-
W = watts.
-
-
-
-
Outcome measures.
-
-
-
-
EuroQ = Euro Quality of Life scale, 0 to 100‐point scale.
-
GHQ 28 = General Health Questionnaire 28.
-
GPE = global perceived effect.
-
GRC = global rating of change.
-
MCID = minimal clinically important difference.
-
MDC = minimal detectable change.
-
NDI = Neck Disability Index.
-
NPQ = Northwick Park neck pain Questionnaire.
-
NPRS = Numerical Pain Rating Scale.
-
NRS‐101 = Numerical Rating Scale 101, 0 to 100‐point scale.
-
PCS = physical component score.
-
PPT = pain pressure threshold, measured by algometry.
-
QoL = quality of life measures.
-
SF‐12 = Short‐Form 12, short form with 12 questions, yielding an 8‐scale health profile.
-
SF‐36 = Short‐Form 36, short form with 36 questions yielding an 8‐scale health profil
-
VAS = visual analogue scale.
-
WHYMPI = West Haven‐Yale Multidimensional Pain Inventory (subscale of pain severity).
-
-
Statistical terms.
-
ANCOVA = analysis of co‐variance.
-
ANOVA = analysis of variance.
-
95% CI = 95% confidence interval.
-
IQR = interquartile range.
-
ITT = intention‐to‐treat analysis.
-
MANOVA = multi‐variate analysis of variance.
-
MD = mean difference.
-
NNTB = number needed to treat for an additional beneficial outcome.
-
-
-
-
-
RR = risk ratio.
-
SD = standard deviation.
-
SE = standard error.
-
SMD = standard mean difference.
-
-
-
-
Other.
-
m = months.
-
N/A = not applicable.
-
NR = not reported.
-
RCT = randomised controlled trial.
-
v = versus.
-
w = weeks.
-
y = years.
-
-
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Intervention: manipulation received in all arms | |
| Intervention: multi‐modal approach | |
| Design: quasi‐RCT sequential allocation cohort | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: mechanical traction | |
| Population: study included only children | |
| Intervention: behavioural exercise programme vs manual therapy | |
| Design: this was a secondary analysis in which participants were not randomly assigned | |
| Intervention: intervention technique was not mobilisation nor manipulation | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: participants received mechanical traction using the Tru‐Trac series 92B machine under the supervision of a physiotherapist | |
| Design: not an RCT | |
| Intervention: aimed at therapist, not at study population | |
| Intervention: manipulation and exercise | |
| Intervention: multi‐modal | |
| Design: article is a systematic review, not an RCT | |
| Intervention: both groups underwent manual therapy | |
| Population: tenstion ‐type headache and migraine | |
| Population: tension‐type headache | |
| Intervention: manipulation was used in combination with ibuprofen as a control | |
| Outcome: outcome measure used was not clearly stated | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Population: cervical vertigo | |
| Intervention: multi‐modal approach | |
| Population: asymptomatic individuals | |
| Population: unsure, sample not adequately described (query whiplash‐associated neck disorder) | |
| Intervention: ischaemic compression and trigger point pressure release on neck pain | |
| Intervention: multi‐modal approach | |
| Population: unable to split spinal data. Attempts to contact study author resulted in no response | |
| Intervention: manual therapy in active and control groups | |
| Population: did not meet review inclusion criteria | |
| Intervention: Control treatment was individualised care (acupuncture, massage, mobs, hot pack, TENS, US, exercise), and we were not able to elucidate the exact treatment mix for the "treat as usual" group | |
| Design: phase IV diagnostic trial, not an efficacy trial | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: did not consist of mobilisation nor manipulation | |
| Outcome: included only measures of blood flow | |
| Intervention: multi‐modal approach | |
| Outcomes: excluded on basis of outcomes | |
| Outcome: psychosocial outcome measure | |
| Population: no sample with neck disorder meeting inclusion criteria (torticollis) | |
| Intervention: multi‐modal approach | |
| Intervention: no manual therapy intervention | |
| Design: observational study | |
| Intervention: manual/mechanical traction | |
| Intervention: Shiatsu type of manipulation | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: co‐intervention inconsistencies Design: quasi‐RCT | |
| Intervention: Control group performed craniocervical flexor exercises Design: method of randomisation unclear | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Interventions: no manual therapy | |
| Population: mixed headache | |
| Intervention: Mobilisations were combined with exercises | |
| Population: no sample with neck disorder meeting inclusion criteria (repetitive strain injury of upper limb) | |
| Design: case study (not an RCT) | |
| Intervention: manual therapy in treatment and control groups | |
| Population: canal spinal stenosis unclear; long tract signs Intervention: local point traction manipulation | |
| Population: unable to split data into neck pain‐only group | |
| Population: unable to split data into neck pain‐only group | |
| Outcome: PPT was not an outcome of interest in this review | |
| Intervention: manipulation plus exercise | |
| Population: seniors | |
| Intervention: no manual therapy included | |
| Outcome was PPT and mouth ROM | |
| Outcome: PPT was not an outcome of interest in this review | |
| Population: asymptomatic cervical spine; outcomes: no outcomes measuring cervical spine or related disability | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Outcome: Muscle strength measure was not part of our inclusion outcomes | |
| Design: unsure RCT | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach including myofascial trigger point and mobilisation techniques | |
| Intervention: integrated neuromuscular inhibition technique (INIT) | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: behavioural exercise programme | |
| Intervention: behavioural exercise programme | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: mobilisation plus exercise | |
| Design: not a randomised controlled trial | |
| Population: rat study; not human study | |
| Population: no sample with neck disorder meeting inclusion criteria (normal cervical spine) | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Population: Study population did not meet inclusion criteria for the review | |
| Design: a mechanistic trial | |
| Design: not an RCT but a single‐group study | |
| Population: individuals with migraine | |
| Intervention: multi‐modal approach | |
| Outcome: PPT was not an outcome of interest in this review | |
| Intervention: multi‐modal Outcome: adverse effects | |
| Outcome: range of motion data only; study does not meet our inclusion criteria | |
| Outcome: outcomes for neck and back pain combined | |
| Intervention: injection‐type manipulation | |
| Intervention: multi‐modal approach | |
| Intervention: multi‐modal approach | |
| Intervention: traction + MT/Ex vs MT/Ex | |
| Intervention: multi‐modal approach ‐ traditional bone setting ‐ mobilisation and manipulation | |
| Intervention: acupuncture |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT |
| Participants | Chronic non‐specific neck pain |
| Interventions | Dog technique vs toggle‐recoil technique |
| Outcomes | Self reported neck pain (visual analogue scale); neck mobility (cervical range of motion); pressure pain threshold at cervical and thoracic levels (C4 and T4 spinous process) and over the site described for location of tense bands of the upper trapezius muscle |
| Notes |
| Methods | RCT |
| Participants | Primarily neck pain with and without upper extremity symptoms |
| Interventions | Thrust vs non‐thrust manipulation/Mobilisation |
| Outcomes | NDI, NRS, fear avoidance |
| Notes | Clarify population |
| Methods | RCT |
| Participants | Patients with cervical spine disorders |
| Interventions | SNAGs group vs manipulation group vs exercise group |
| Outcomes | Cervical range of motion (CROM) was measured using CROM device, with pain assessed using the visual analogue scale (VAS), and grade of functional recovery measured using the Neck Disability Index (NDI) |
| Notes |
| Methods | RCT |
| Participants | Chronic neck pain |
| Interventions | High velocity low amplitude (HVLA) vs mobilisation (Mob) vs sustained natural apophyseal glide (SNAG) |
| Outcomes | Visual analogue scale (VAS), Neck Disability Index (NDI), Global Rating of Change (GROC) and cervical range of motion (CROM) |
| Notes |
| Methods | RCT |
| Participants | Cervical spine pain |
| Interventions | Seated thoracic manipulation vs targeted supine thoracic manipulation group |
| Outcomes | Pain and flexion ROM measures |
| Notes |
| Methods | RCT |
| Participants | Radiculopathy |
| Interventions | Neurodynamic technique |
| Outcomes | Pain, NDI |
| Notes | Spanish translation needed |
| Methods | RCT |
| Participants | Benign cervicobrachialgia of mechanical origin |
| Interventions | Manipulative therapy |
| Outcomes | Pain |
| Notes | Interlibrary loan ordered ‐ access to article pending |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Comparison of the Effectiveness of Manual Therapy and Physical Therapy in Patients with Neck Pain |
| Methods | RCT |
| Participants | Patients with chronic neck pain |
| Interventions | Exercice + manual therapy; Exercise + physical therapy; Exercise |
| Outcomes | Pain (VAS) Function (NDI) Quality of life (SF‐36) Global perceived effect |
| Starting date | Unknown |
| Contact information | None |
| Notes |
| Trial name or title | Effectiveness and Cost Evaluation of Manual Therapy and Physical Therapy in Patients with Subacute and Chronic Non‐specific Neck Pain: Rationale and Design of a Randomised Controlled Trial (RCT) |
| Methods | Type of trial: RCT protocol intention‐to‐treat analysis: calculated Power analysis: calculated 80% pre‐hoc (specify beta value per comparison: 0.2) |
| Participants | Subacute/Chronic non‐specific cervical; patients may have received radiation to the elbow and may have CGH (inclusion criteria) |
| Interventions | INDEX TREATMENT COMPARISON TREATMENT CO‐INTERVENTION Not avoided: Participants are free to use medication prescribed by a physician or of their own choice; avoided in trial design: Participant will not receive treatment other than treatments allocated in the trial Duration of treatment: 6 weeks, maximum 6 (UMT) and 9 (PT) treatment sessions |
| Outcomes | Pain (NRS), function (NDI), GPE (7‐point ordinal scale) and QoL (PCS and MCS components of SF‐36) |
| Starting date | 2008 |
| Contact information | The Netherlands |
| Notes |
| Trial name or title | Randomised Clinical Trial Comparing Non‐operative Conservative Medical Care, Chiropractic Cervical Distraction and a Combination of Both for Chronic Neck Pain |
| Methods | RCT |
| Participants | Chronic neck pain with or without associated arm symptoms or headache |
| Interventions | Non‐operative conservative medical care ‐ active exercise programme to stabilise neck muscles and decrease anterior head carriage |
| Outcomes | NDI, VAS pain intensity over previous week |
| Starting date | Study is currently in manuscript phase |
| Contact information | Palmer Center for Chiropractic Research |
| Notes |
| Trial name or title | Comparative Effects of Manipulation and Physical Therapy on Motion in the Cervical Spine |
| Methods | RCT |
| Participants | Chronic neck pain |
| Interventions | Cervical spine manipulation vs sham treatment vs cervical spine manipulation, ischaemic compression of myofascial trigger points, PNF, interferential therapy |
| Outcomes | Cervical ROM |
| Starting date | |
| Contact information | Palmer Institute of Graduate Studies and Research, Davenport, Iowa. |
| Notes |
| Trial name or title | Comparison of Treatment of Neck Pain |
| Methods | RCT |
| Participants | Neck pain |
| Interventions | Not specified |
| Outcomes | Not specified |
| Starting date | |
| Contact information | Department of Neuroscience and Locomotion, Physiotherapy, Faculty of Health Sciences, Linkopings Universitet, Sweden |
| Notes |
| Trial name or title | Cervical Radiculopathy: Study Protocol of a Randomised Clinical Trial Evaluating the Effects of |
| Methods | RCT |
| Participants | Cervical radiculopathy |
| Interventions | One group will receive a 4‐week rehabilitation programme targeting opening of the intervertebral foramen; the |
| Outcomes | Primary outcome measure will be the validated Neck Disability Index questionnaire. Secondary outcome measures will include the short version of the Disabilities of the Arm, Shoulder and Hand Questionnaire, a numerical pain rating scale, cervicothoracic mobility and participants' perceived global rating of change |
| Starting date | 2012 |
| Contact information | |
| Notes |
| Trial name or title | Randomised Placebo Controlled Trial for Cervicobrachial Pain Syndrome Using Manual Therapy |
| Methods | RCT |
| Participants | Cervicobrachial pain syndrome |
| Interventions | Manipulative therapy vs placebo physiotherapy vs control |
| Outcomes | EMG muscle onset, pain, functional disability |
| Starting date | |
| Contact information | B Nagy, |
| Notes |
| Trial name or title | Comparative Effectiveness of Adjustments vs Mobilisation in Chronic Mechanical Neck Pain |
| Methods | RCT |
| Participants | Chronic mechanical neck pain |
| Interventions | Adjustments (diversified) vs mobilisation (muscle energy technique) |
| Outcomes | Cervical ROM, NRS, short form McGill Pain Questionnaire, NDI |
| Starting date | |
| Contact information | Technikon Natal College of Chiropractic, Durban, South Africa |
| Notes |
| Trial name or title | Effectiveness of Thoracic Spine Manipulation on Pain and Disability in Patients with Neck Pain: A Pilot Randomised Clinical Trial |
| Methods | Participants were randomly assigned to receive MNP only or MNP + TTM for a maximum of 12 sessions 2×/wk. Primary outcomes were an 11‐point Numerical Pain Rating Scale (NPS), the Neck Disability Index (NDI), and a 15‐point Global Rating of Change (GRC) scale to measure perceived change in health status. Neck active range of motion (AROM) was a secondary outcome. Outcomes were collected at baseline and at 2, 4 and 6 weeks (GRC was not collected at baseline). As the goal of the study was to prepare parameter estimates, hypothesis testing was not done. We determined clinically important changes by comparing point estimates of within‐participant changes for NPS and NDI vs their established minimal clinically important differences (MCIDs). MCIDs for NPS and NDI are 2 points and 10% change, respectively. We calculated the percentage of participants in each group who reported moderate or higher improvement on the GRC at each follow‐up. For neck AROM, changes greater than published values of minimal detectable change (MDC) were considered noticeable changes. Between‐group differences at 6 weeks in primary outcomes were used to estimate sample size |
| Participants | Mechanical neck pain |
| Interventions | Multi‐modal neck programme (MNP) that includes electrothermal modalities, active exercises and some form of manual therapy (commonly non‐thrust) directed at the cervical spine vs thoracic thrust manipulation (TTM) |
| Outcomes | Pain, disability, AROM, global rating of improvement |
| Starting date | 2010 |
| Contact information | Shamsuddin Khoja, Samannaaz, Daliman, Daniel, Regina Sara, Piva |
| Notes |
| Trial name or title | Dose Optimisations for Spinal Treatment Effectiveness (the Dose Study): Higher Applied Mobilisation Force Associated with Reduced Pain and Spinal Stiffness in Patients with Chronic Neck Pain |
| Methods | RCT |
| Participants | Chronic non‐specific neck pain |
| Interventions | Posterior‐to‐anterior mobilisation vs placebo (de‐tuned laser) |
| Outcomes | Pain, PPT, ROM and spinal stiffness |
| Starting date | |
| Contact information | Australia |
| Notes |
| Trial name or title | Randomised Comparison of Chiropractic and Physiotherapy Treatment for Neck Pain of Functional (Mechanical) Origins. A Controlled Clinical Trial |
| Methods | RCT |
| Participants | Neck pain, neck and head pain, neck and shoulder pain |
| Interventions | Chiropractic spinal manipulation vs physiotherapy vs medication |
| Outcomes | NDI, pain intensity VAS |
| Starting date | |
| Contact information | Institute of Community Medicine, School of Medicine, University of Tromso, 9037 Tromso, Norway |
| Notes |
| Trial name or title | Chiropractic Therapy Compared to Medical Therapy for Chronic Cervical Pain |
| Methods | RCT |
| Participants | Chronic cervical spine pain |
| Interventions | Chiropractic care: (lateral flexion) manipulation, exercise plus heat vs medical care: heat, exercise, acetaminophen |
| Outcomes | McGill Pain Questionnaire, NDI, cervical ROM, cervical muscle strength (Cybex), SF‐36 |
| Starting date | Start: November 1994 |
| Contact information | Colorado Prevention Centre, Denver, Colorado, USA |
| Notes |
| Trial name or title | Short‐Term Treatment vs Long‐Term Management of Neck and Back Disability in Older |
| Methods | RCT |
| Participants | Back and neck disability |
| Interventions | 12 weeks SMT + SRE or 36 weeks SMT + SRE |
| Outcomes | Self report questionnaires administered at 2 baseline visits and at 4, 12, 24, 36, 52 and 78 weeks |
| Starting date | 2014 |
| Contact information | Northwestern Health Sciences University, Wolfe‐Harris Center for Clinical |
| Notes |
We have attempted to find most of these study authors over the Internet; however, we have not been able to make contact with many of them, especially authors of older trials.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical manipulation vs placebo Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.1 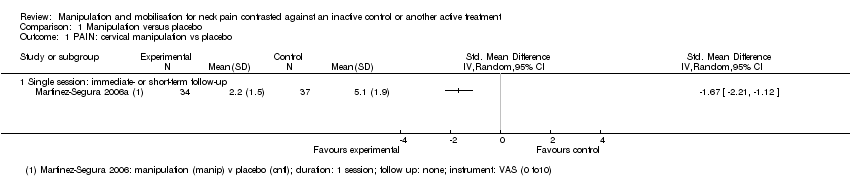 Comparison 1 Manipulation versus placebo, Outcome 1 PAIN: cervical manipulation vs placebo. | ||||
| 1.1 Single session: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: thoracic manipulation vs placebo Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Manipulation versus placebo, Outcome 2 PAIN: thoracic manipulation vs placebo. | ||||
| 2.1 Single session: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.1 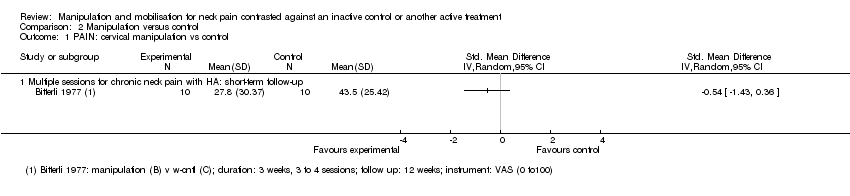 Comparison 2 Manipulation versus control, Outcome 1 PAIN: cervical manipulation vs control. | ||||
| 1.1 Multiple sessions for chronic neck pain with HA: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical manipulation plus treatment vs same treatment in both arms Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 Manipulation versus control, Outcome 2 PAIN: cervical manipulation plus treatment vs same treatment in both arms. | ||||
| 2.1 Single session for subacute/chronic neck pain: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 PAIN: cervical manipulation vs same treatment in both arms Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 Manipulation versus control, Outcome 3 PAIN: cervical manipulation vs same treatment in both arms. | ||||
| 3.1 Single session for subacute/chronic neck pain with radicular findings and HA: short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 PAIN: thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.4  Comparison 2 Manipulation versus control, Outcome 4 PAIN: thoracic manipulation vs control. | ||||
| 4.1 Single session for neck pain of not reported duration: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: thoracic manipulation vs same treatment in both arms Show forest plot | 8 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.5  Comparison 2 Manipulation versus control, Outcome 5 PAIN: thoracic manipulation vs same treatment in both arms. | ||||
| 5.1 Multiple sessions for acute neck pain: immediate‐term follow‐up | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐3.46 [‐4.13, ‐2.79] |
| 5.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐1.15, 0.69] |
| 5.3 Single session for chronic neck pain: short‐term follow‐up | 1 | 82 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.36, 0.51] |
| 5.4 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 4 | 242 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.46 [‐2.20, ‐0.71] |
| 5.5 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐0.99, ‐0.20] |
| 5.6 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.04, ‐0.25] |
| 6 PAIN: cervical and thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.6 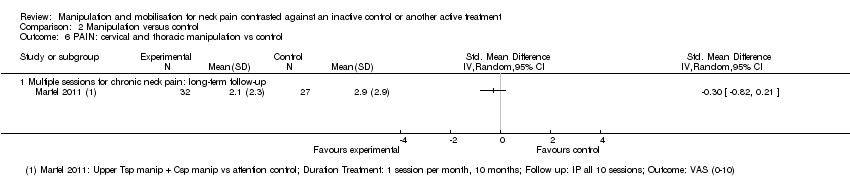 Comparison 2 Manipulation versus control, Outcome 6 PAIN: cervical and thoracic manipulation vs control. | ||||
| 6.1 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 FUNCTION: thoracic manipulation vs same treatment in both arms Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.7  Comparison 2 Manipulation versus control, Outcome 7 FUNCTION: thoracic manipulation vs same treatment in both arms. | ||||
| 7.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.85, ‐0.18] |
| 7.2 Single session for chronic neck pain: short‐term follow‐up | 1 | 81 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.61, 0.27] |
| 7.3 Multiple sessions for acute neck pain: short‐term follow‐up | 3 | 154 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.73 [‐2.68, ‐0.78] |
| 7.4 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.89, ‐0.10] |
| 7.5 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.77, 0.01] |
| 8 FUNCTION: cervical manipulation vs same treatment in both arms Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.8 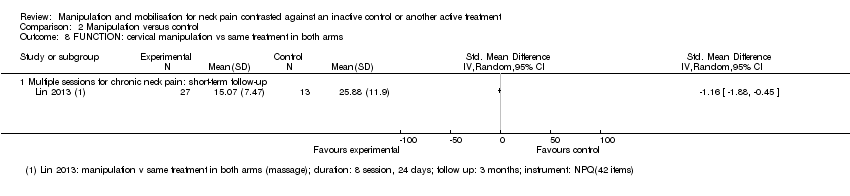 Comparison 2 Manipulation versus control, Outcome 8 FUNCTION: cervical manipulation vs same treatment in both arms. | ||||
| 8.1 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 FUNCTION: cervical and thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.9  Comparison 2 Manipulation versus control, Outcome 9 FUNCTION: cervical and thoracic manipulation vs control. | ||||
| 9.1 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 QUALITY OF LIFE: thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.10  Comparison 2 Manipulation versus control, Outcome 10 QUALITY OF LIFE: thoracic manipulation vs control. | ||||
| 10.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 FUNNEL PLOT for pain: thoracic manipulation vs same treatment in both arms Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.11  Comparison 2 Manipulation versus control, Outcome 11 FUNNEL PLOT for pain: thoracic manipulation vs same treatment in both arms. | ||||
| 11.1 Multiple sessions for acute to chronic neck pain: short‐term follow‐up | 5 | 346 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.26 [‐1.86, ‐0.66] |
| 12 FUNNEL PLOT for function: thoracic manipulation vs same treatment in both arms Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.12 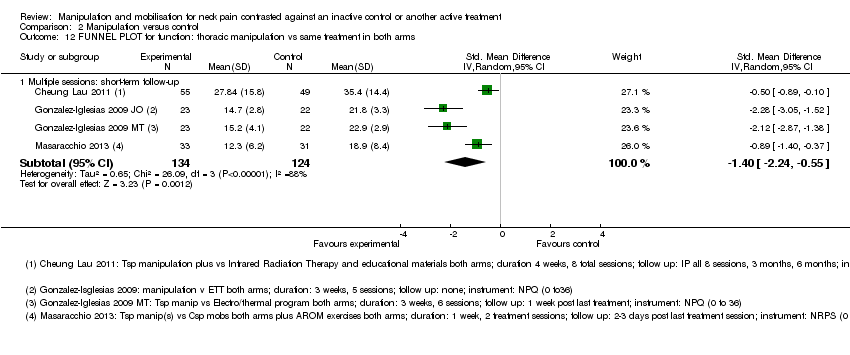 Comparison 2 Manipulation versus control, Outcome 12 FUNNEL PLOT for function: thoracic manipulation vs same treatment in both arms. | ||||
| 12.1 Multiple sessions: short‐term follow‐up | 4 | 258 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.40 [‐2.24, ‐0.55] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical mobilisation vs control Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 3.1  Comparison 3 Mobilisation versus control, Outcome 1 PAIN: cervical mobilisation vs control. | ||||
| 1.1 Single session: intermediate post treatment | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Multiple sessions: short‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical manipulation vs mobilisation at immediate post treatment Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.1 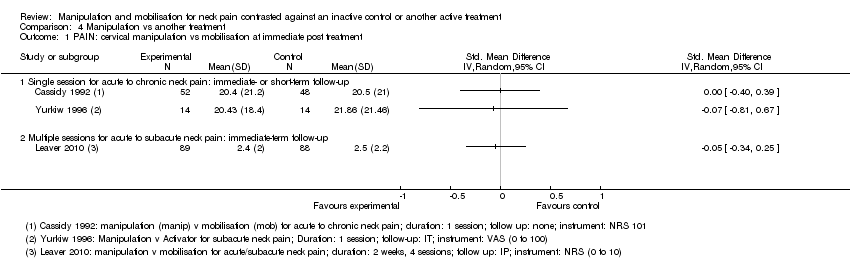 Comparison 4 Manipulation vs another treatment, Outcome 1 PAIN: cervical manipulation vs mobilisation at immediate post treatment. | ||||
| 1.1 Single session for acute to chronic neck pain: immediate‐ or short‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Multiple sessions for acute to subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 4.2  Comparison 4 Manipulation vs another treatment, Outcome 2 PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up. | ||||
| 2.1 Multiple sessions for acute to chronic neck pain: intermediate‐term follow‐up | 2 | 446 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.72, 0.59] |
| 3 PAIN: cervical manipulation vs massage Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 4.3 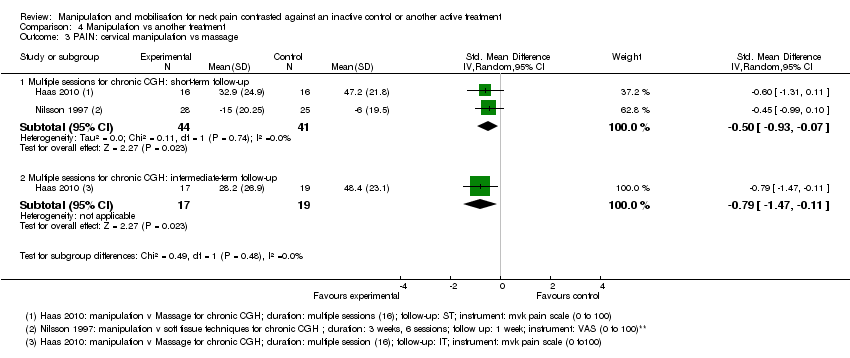 Comparison 4 Manipulation vs another treatment, Outcome 3 PAIN: cervical manipulation vs massage. | ||||
| 3.1 Multiple sessions for chronic CGH: short‐term follow‐up | 2 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.93, ‐0.07] |
| 3.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.47, ‐0.11] |
| 4 PAIN: cervical manipulation vs medicine Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.4  Comparison 4 Manipulation vs another treatment, Outcome 4 PAIN: cervical manipulation vs medicine. | ||||
| 4.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: cervical manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.5  Comparison 4 Manipulation vs another treatment, Outcome 5 PAIN: cervical manipulation vs exercise. | ||||
| 5.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 PAIN: cervical manipulation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.6  Comparison 4 Manipulation vs another treatment, Outcome 6 PAIN: cervical manipulation vs electrotherapy. | ||||
| 6.1 Multiple sessions for subacute to chronic CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Multiple sessions for subacute to chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 PAIN: cervical manipulation vs acupuncture Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.7 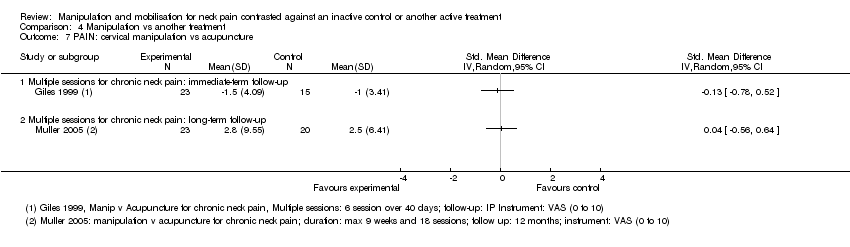 Comparison 4 Manipulation vs another treatment, Outcome 7 PAIN: cervical manipulation vs acupuncture. | ||||
| 7.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 PAIN: cervical manipulation vs orthotic devices (K‐tape) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.8 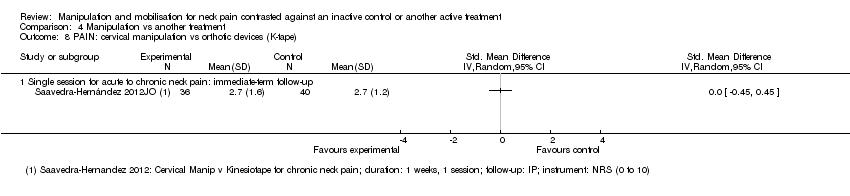 Comparison 4 Manipulation vs another treatment, Outcome 8 PAIN: cervical manipulation vs orthotic devices (K‐tape). | ||||
| 8.1 Single session for acute to chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 PAIN: cervical manipulation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.9 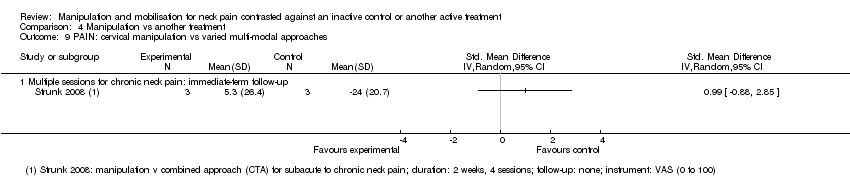 Comparison 4 Manipulation vs another treatment, Outcome 9 PAIN: cervical manipulation vs varied multi‐modal approaches. | ||||
| 9.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 PAIN: cervical manipulation ‐ 1 technique vs another technique Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.10 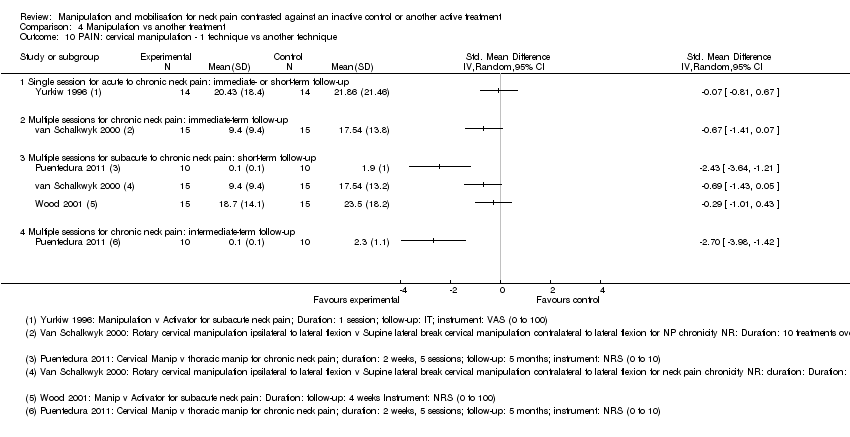 Comparison 4 Manipulation vs another treatment, Outcome 10 PAIN: cervical manipulation ‐ 1 technique vs another technique. | ||||
| 10.1 Single session for acute to chronic neck pain: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Multiple sessions for subacute to chronic neck pain: short‐term follow‐up | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.4 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 PAIN: cervical manipulation ‐ varied dosage comparison Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 4.11 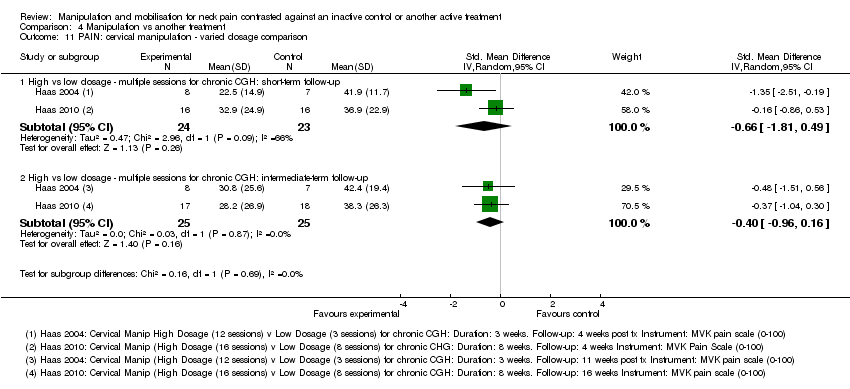 Comparison 4 Manipulation vs another treatment, Outcome 11 PAIN: cervical manipulation ‐ varied dosage comparison. | ||||
| 11.1 High vs low dosage ‐ multiple sessions for chronic CGH: short‐term follow‐up | 2 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.81, 0.49] |
| 11.2 High vs low dosage ‐ multiple sessions for chronic CGH: intermediate‐term follow‐up | 2 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.96, 0.16] |
| 12 PAIN: thoracic manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.12  Comparison 4 Manipulation vs another treatment, Outcome 12 PAIN: thoracic manipulation vs exercise. | ||||
| 12.1 Multiple sessions for neck pain chronicity NR: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 FUNCTION: cervical manipulation vs mobilisation Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 4.13  Comparison 4 Manipulation vs another treatment, Outcome 13 FUNCTION: cervical manipulation vs mobilisation. | ||||
| 13.1 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 1 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.35, 0.24] |
| 13.2 Multiple sessions for acute to chronic neck pain: intermediate‐term follow‐up | 2 | 445 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.21, 0.18] |
| 14 FUNCTION: cervical manipulation vs massage Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.14 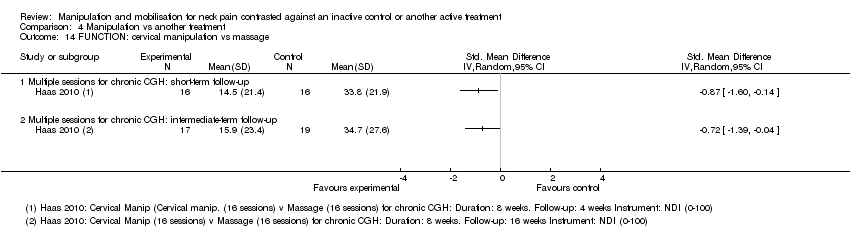 Comparison 4 Manipulation vs another treatment, Outcome 14 FUNCTION: cervical manipulation vs massage. | ||||
| 14.1 Multiple sessions for chronic CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 FUNCTION: cervical manipulation vs medicine Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 4.15 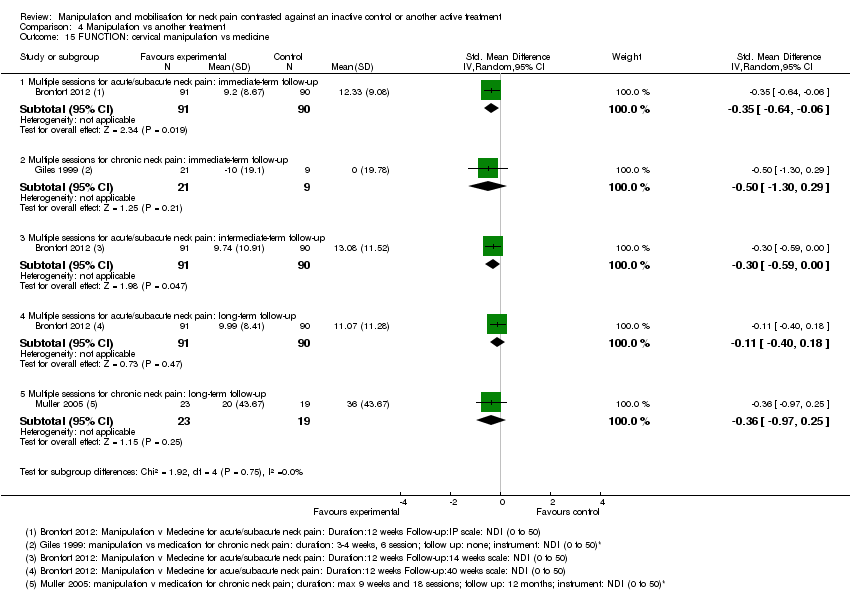 Comparison 4 Manipulation vs another treatment, Outcome 15 FUNCTION: cervical manipulation vs medicine. | ||||
| 15.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.64, ‐0.06] |
| 15.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.30, 0.29] |
| 15.3 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.59, ‐0.00] |
| 15.4 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.40, 0.18] |
| 15.5 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | 42 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.97, 0.25] |
| 16 FUNCTION: cervical manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.16  Comparison 4 Manipulation vs another treatment, Outcome 16 FUNCTION: cervical manipulation vs exercise. | ||||
| 16.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 FUNCTION: cervical manipulation vs orthotic devices (K‐taping) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.17  Comparison 4 Manipulation vs another treatment, Outcome 17 FUNCTION: cervical manipulation vs orthotic devices (K‐taping). | ||||
| 17.1 Single session for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 FUNCTION: cervical manipulation vs acupuncture Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.18  Comparison 4 Manipulation vs another treatment, Outcome 18 FUNCTION: cervical manipulation vs acupuncture. | ||||
| 18.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 FUNCTION: cervical manipulation vs varied multi‐modal approaches Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.19  Comparison 4 Manipulation vs another treatment, Outcome 19 FUNCTION: cervical manipulation vs varied multi‐modal approaches. | ||||
| 19.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Multiple sessions for subacute/chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 FUNCTION: cervical manipulation ‐ 1 technique vs another technique Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.20  Comparison 4 Manipulation vs another treatment, Outcome 20 FUNCTION: cervical manipulation ‐ 1 technique vs another technique. | ||||
| 20.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.3 Multiple sessions for neck pain chronicity NR: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.4 Multiple sessions for acute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 FUNCTION: cervical manipulation ‐ varied dosage comparison Show forest plot | 2 | 97 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.09, ‐0.14] |
| Analysis 4.21  Comparison 4 Manipulation vs another treatment, Outcome 21 FUNCTION: cervical manipulation ‐ varied dosage comparison. | ||||
| 21.1 High vs low dosage ‐ multiple sessions for chronic CGH: short‐term follow‐up | 2 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.71, 0.22] |
| 21.2 High vs low dosage ‐ multiple sessions for chronic CGH: intermediate‐term follow‐up | 2 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.38, 0.17] |
| 22 PATIENT SATISFACTION: cervical manipulation vs mobilisation Show forest plot | 1 | 303 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.21, 0.24] |
| Analysis 4.22 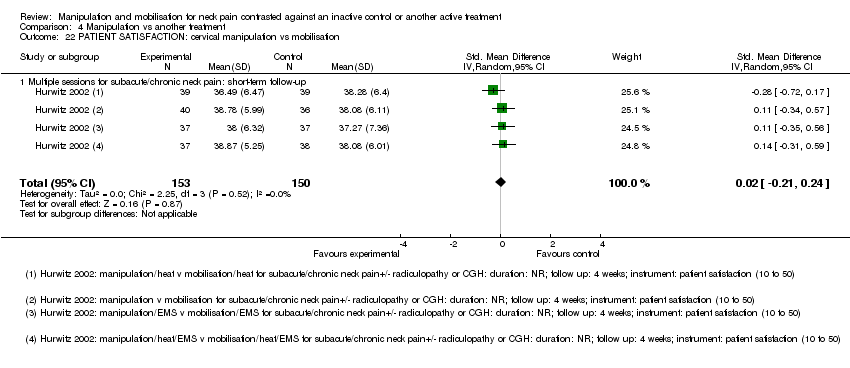 Comparison 4 Manipulation vs another treatment, Outcome 22 PATIENT SATISFACTION: cervical manipulation vs mobilisation. | ||||
| 22.1 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | 303 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.21, 0.24] |
| 23 PATIENT SATISFACTION: cervical manipulation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.23  Comparison 4 Manipulation vs another treatment, Outcome 23 PATIENT SATISFACTION: cervical manipulation vs varied multi‐modal approaches. | ||||
| 23.1 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 GLOBAL PERCEIVED EFFECT: cervical manipulation vs mobilisation Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.24 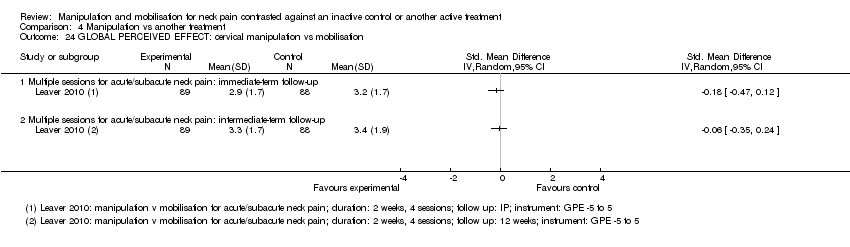 Comparison 4 Manipulation vs another treatment, Outcome 24 GLOBAL PERCEIVED EFFECT: cervical manipulation vs mobilisation. | ||||
| 24.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 QUALITY OF LIFE: cervical manipulation vs mobilisation Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.25 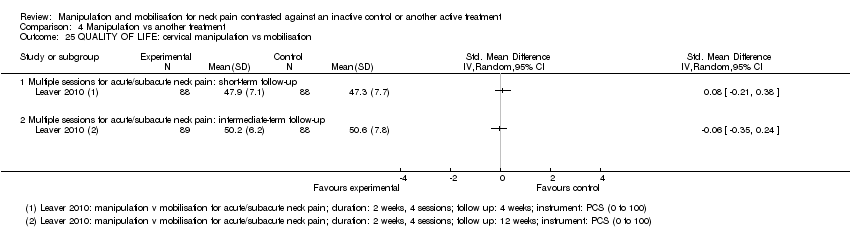 Comparison 4 Manipulation vs another treatment, Outcome 25 QUALITY OF LIFE: cervical manipulation vs mobilisation. | ||||
| 25.1 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 QUALITY OF LIFE: cervical manipulation vs medicine Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.26  Comparison 4 Manipulation vs another treatment, Outcome 26 QUALITY OF LIFE: cervical manipulation vs medicine. | ||||
| 26.1 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.2 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 QUALITY OF LIFE: cervical manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 4.27  Comparison 4 Manipulation vs another treatment, Outcome 27 QUALITY OF LIFE: cervical manipulation vs exercise. | ||||
| 27.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical mobilisation vs medical injection ‐ trigger point Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.1 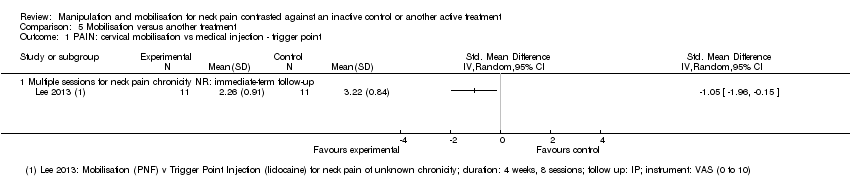 Comparison 5 Mobilisation versus another treatment, Outcome 1 PAIN: cervical mobilisation vs medical injection ‐ trigger point. | ||||
| 1.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical mobilisation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.2 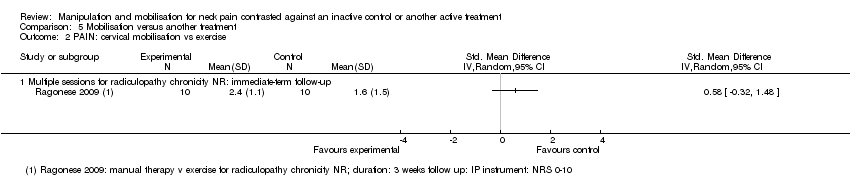 Comparison 5 Mobilisation versus another treatment, Outcome 2 PAIN: cervical mobilisation vs exercise. | ||||
| 2.1 Multiple sessions for radiculopathy chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 PAIN: cervical mobilisation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.3 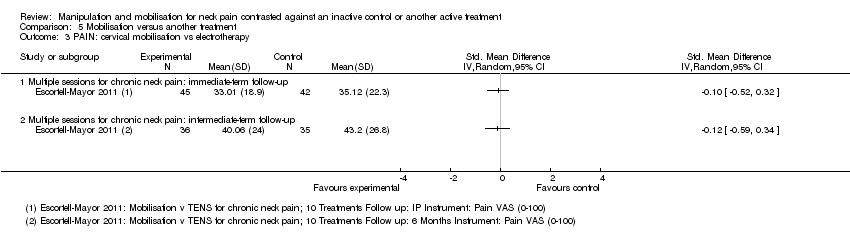 Comparison 5 Mobilisation versus another treatment, Outcome 3 PAIN: cervical mobilisation vs electrotherapy. | ||||
| 3.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 PAIN: cervical mobilisation vs sonic devices ‐ ultrasound, shock wave therapy Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.4  Comparison 5 Mobilisation versus another treatment, Outcome 4 PAIN: cervical mobilisation vs sonic devices ‐ ultrasound, shock wave therapy. | ||||
| 4.1 Single session for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: cervical mobilisation vs mechanical traction Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.5  Comparison 5 Mobilisation versus another treatment, Outcome 5 PAIN: cervical mobilisation vs mechanical traction. | ||||
| 5.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 PAIN: cervical mobilisation vs acupuncture Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.6  Comparison 5 Mobilisation versus another treatment, Outcome 6 PAIN: cervical mobilisation vs acupuncture. | ||||
| 6.1 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 PAIN: cervical mobilisation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.7  Comparison 5 Mobilisation versus another treatment, Outcome 7 PAIN: cervical mobilisation vs varied multi‐modal approaches. | ||||
| 7.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 PAIN: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.8  Comparison 5 Mobilisation versus another treatment, Outcome 8 PAIN: cervical mobilisation ‐ 1 technique vs another technique. | ||||
| 8.1 Single session for chronic neck pain: immediate‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Single session for chronic neck pain ± radiculopathy: immediate‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 PAIN: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 5.9  Comparison 5 Mobilisation versus another treatment, Outcome 9 PAIN: cervical mobilisation ‐ 1 technique vs another technique. | ||||
| 9.1 PA vs other mobilisation for acute/subacute neck pain: multiple sessions: immediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 AP vs other mobilisation: multiple sessions: immediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 PAIN: cervical mobilisation vs massage Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 5.10  Comparison 5 Mobilisation versus another treatment, Outcome 10 PAIN: cervical mobilisation vs massage. | ||||
| 10.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.56 [‐4.15, 1.03] |
| 10.2 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.89 [‐3.85, ‐1.93] |
| 11 FUNCTION: cervical mobilisation vs medical injection ‐ trigger point Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.11  Comparison 5 Mobilisation versus another treatment, Outcome 11 FUNCTION: cervical mobilisation vs medical injection ‐ trigger point. | ||||
| 11.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 FUNCTION: cervical mobilisation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.12  Comparison 5 Mobilisation versus another treatment, Outcome 12 FUNCTION: cervical mobilisation vs exercise. | ||||
| 12.1 Multiple sessions for radiculopathy: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 FUNCTION: cervical mobilisation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.13 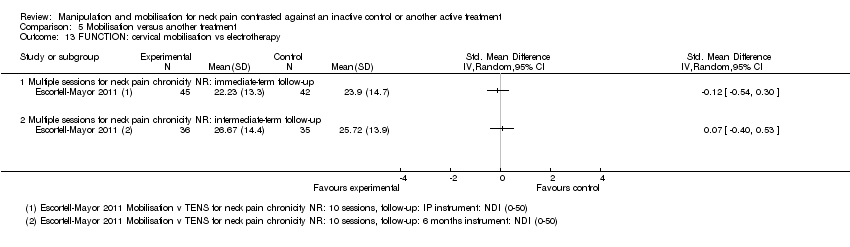 Comparison 5 Mobilisation versus another treatment, Outcome 13 FUNCTION: cervical mobilisation vs electrotherapy. | ||||
| 13.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 FUNCTION: cervical mobilisation vs sonic devices ‐ shock wave therapy Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.14  Comparison 5 Mobilisation versus another treatment, Outcome 14 FUNCTION: cervical mobilisation vs sonic devices ‐ shock wave therapy. | ||||
| 14.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 FUNCTION: cervical mobilisation vs acupuncture Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.15  Comparison 5 Mobilisation versus another treatment, Outcome 15 FUNCTION: cervical mobilisation vs acupuncture. | ||||
| 15.1 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 FUNCTION: cervical mobilisation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.16  Comparison 5 Mobilisation versus another treatment, Outcome 16 FUNCTION: cervical mobilisation vs varied multi‐modal approaches. | ||||
| 16.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 FUNCTION: cervical mobilisation vs massage Show forest plot | 2 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.90, 0.84] |
| Analysis 5.17  Comparison 5 Mobilisation versus another treatment, Outcome 17 FUNCTION: cervical mobilisation vs massage. | ||||
| 17.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | 23 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐1.35, 0.32] |
| 17.2 Multiple sessions for subacute/chronic CGH: immediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.28, 1.04] |
| 18 FUNCTION: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.18  Comparison 5 Mobilisation versus another treatment, Outcome 18 FUNCTION: cervical mobilisation ‐ 1 technique vs another technique. | ||||
| 18.1 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 QUALITY OF LIFE: mobilisation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.19 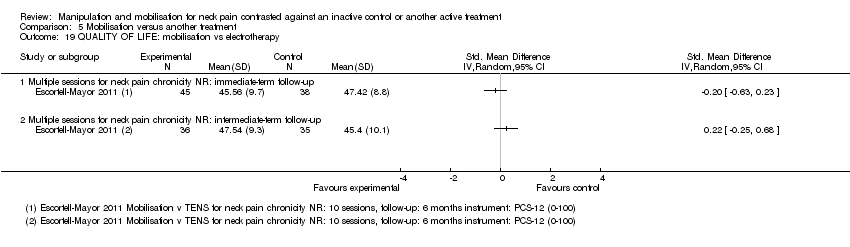 Comparison 5 Mobilisation versus another treatment, Outcome 19 QUALITY OF LIFE: mobilisation vs electrotherapy. | ||||
| 19.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 PATIENT SATISFACTION: cervical mobilisation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 5.20  Comparison 5 Mobilisation versus another treatment, Outcome 20 PATIENT SATISFACTION: cervical mobilisation vs varied multi‐modal approaches. | ||||
| 20.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 PATIENT SATISFACTION: cervical mobilisation vs electrotherapy Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 5.21 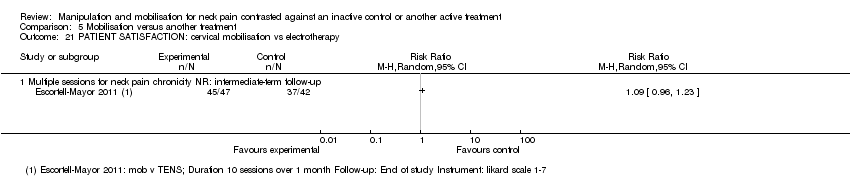 Comparison 5 Mobilisation versus another treatment, Outcome 21 PATIENT SATISFACTION: cervical mobilisation vs electrotherapy. | ||||
| 21.1 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 GLOBAL PERCEIVED EFFECT: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 5.22 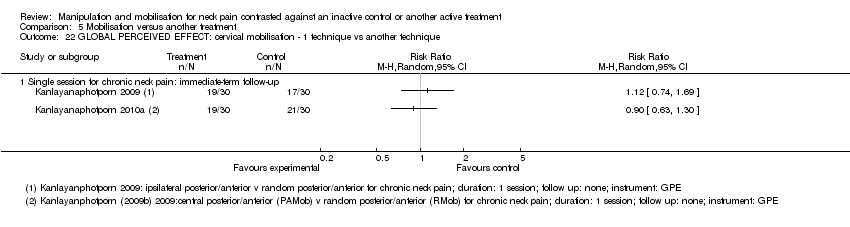 Comparison 5 Mobilisation versus another treatment, Outcome 22 GLOBAL PERCEIVED EFFECT: cervical mobilisation ‐ 1 technique vs another technique. | ||||
| 22.1 Single session for chronic neck pain: immediate‐term follow‐up | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
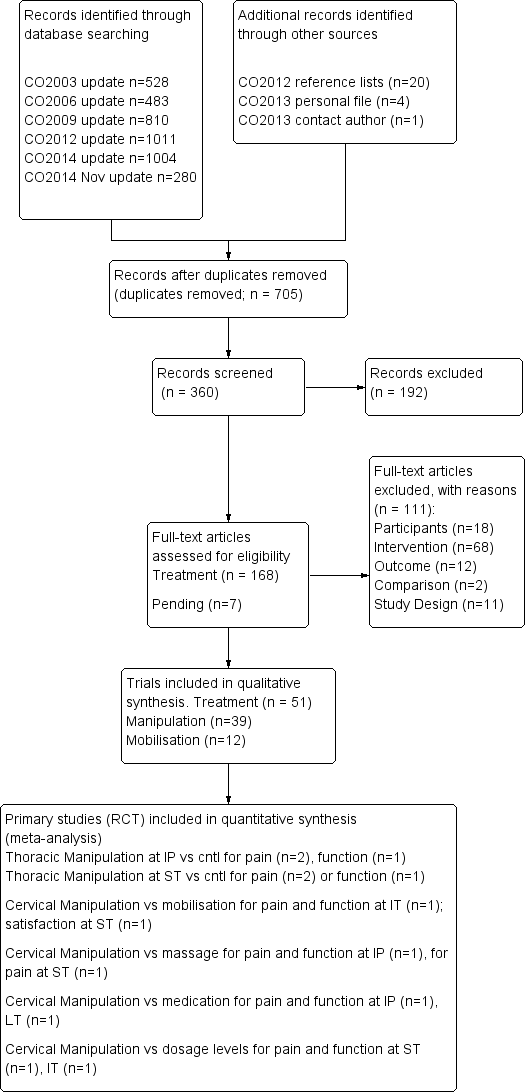
PRISMA diagram for manipulation and mobilisation.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
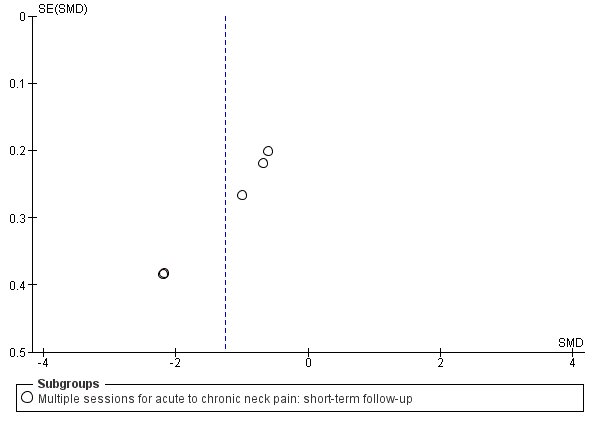
Funnel plot of comparison: manipulation vs control, outcome: FUNNEL PLOT for PAIN: thoracic manipulation vs same treatment in both arms.

Forest plot of comparison: manipulation vs another treatment, outcome: PAIN: cervical manipulation vs medicine.

Forest plot of comparison: manipulation vs another treatment, outcome: PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up.
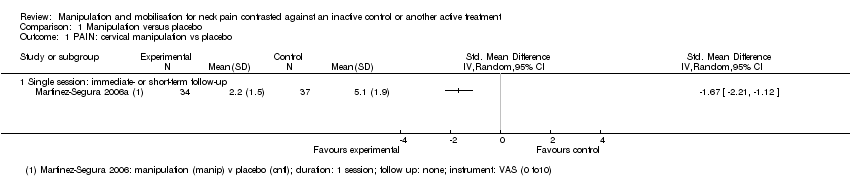
Comparison 1 Manipulation versus placebo, Outcome 1 PAIN: cervical manipulation vs placebo.

Comparison 1 Manipulation versus placebo, Outcome 2 PAIN: thoracic manipulation vs placebo.
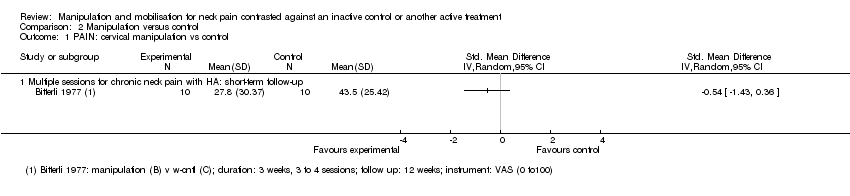
Comparison 2 Manipulation versus control, Outcome 1 PAIN: cervical manipulation vs control.

Comparison 2 Manipulation versus control, Outcome 2 PAIN: cervical manipulation plus treatment vs same treatment in both arms.

Comparison 2 Manipulation versus control, Outcome 3 PAIN: cervical manipulation vs same treatment in both arms.

Comparison 2 Manipulation versus control, Outcome 4 PAIN: thoracic manipulation vs control.

Comparison 2 Manipulation versus control, Outcome 5 PAIN: thoracic manipulation vs same treatment in both arms.
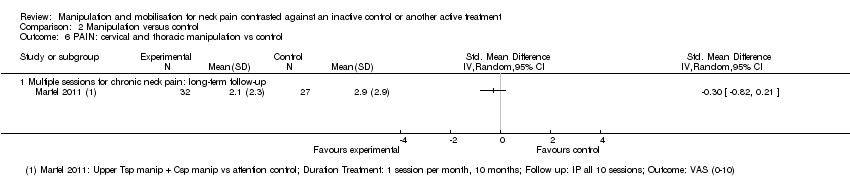
Comparison 2 Manipulation versus control, Outcome 6 PAIN: cervical and thoracic manipulation vs control.

Comparison 2 Manipulation versus control, Outcome 7 FUNCTION: thoracic manipulation vs same treatment in both arms.
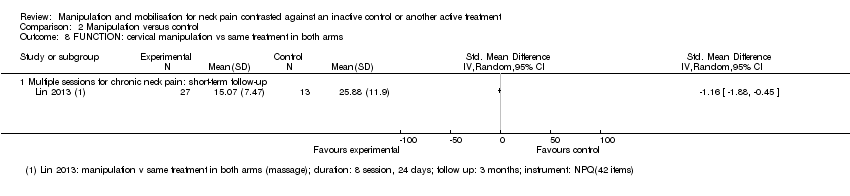
Comparison 2 Manipulation versus control, Outcome 8 FUNCTION: cervical manipulation vs same treatment in both arms.

Comparison 2 Manipulation versus control, Outcome 9 FUNCTION: cervical and thoracic manipulation vs control.

Comparison 2 Manipulation versus control, Outcome 10 QUALITY OF LIFE: thoracic manipulation vs control.

Comparison 2 Manipulation versus control, Outcome 11 FUNNEL PLOT for pain: thoracic manipulation vs same treatment in both arms.
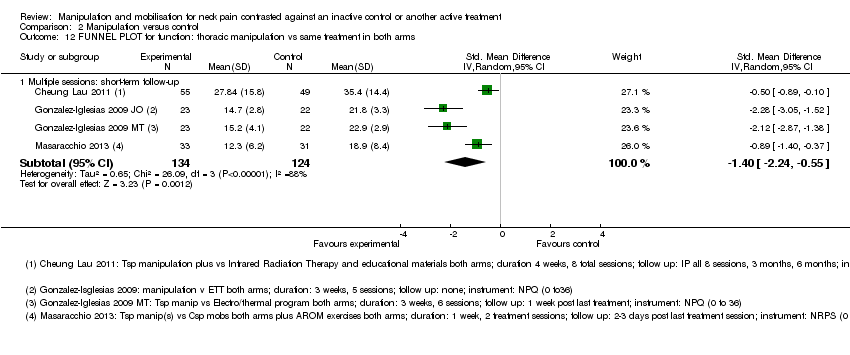
Comparison 2 Manipulation versus control, Outcome 12 FUNNEL PLOT for function: thoracic manipulation vs same treatment in both arms.

Comparison 3 Mobilisation versus control, Outcome 1 PAIN: cervical mobilisation vs control.
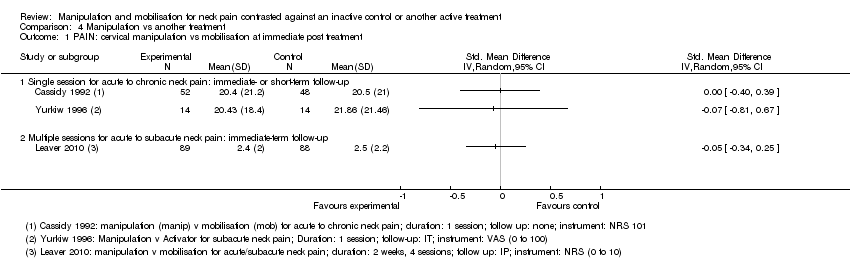
Comparison 4 Manipulation vs another treatment, Outcome 1 PAIN: cervical manipulation vs mobilisation at immediate post treatment.

Comparison 4 Manipulation vs another treatment, Outcome 2 PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up.
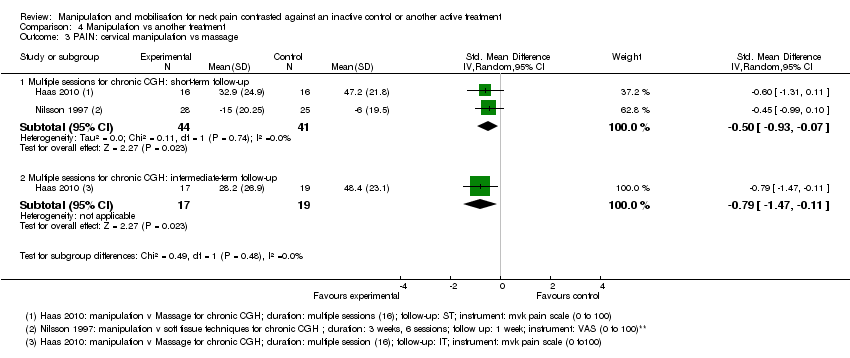
Comparison 4 Manipulation vs another treatment, Outcome 3 PAIN: cervical manipulation vs massage.

Comparison 4 Manipulation vs another treatment, Outcome 4 PAIN: cervical manipulation vs medicine.

Comparison 4 Manipulation vs another treatment, Outcome 5 PAIN: cervical manipulation vs exercise.

Comparison 4 Manipulation vs another treatment, Outcome 6 PAIN: cervical manipulation vs electrotherapy.
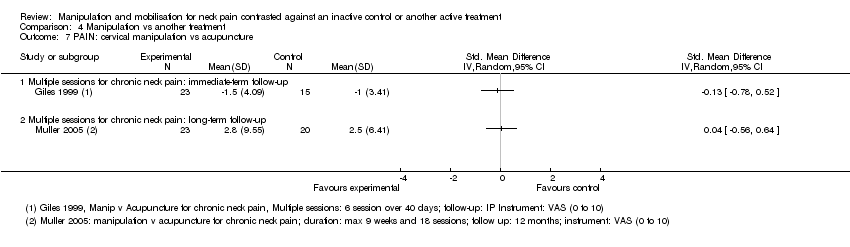
Comparison 4 Manipulation vs another treatment, Outcome 7 PAIN: cervical manipulation vs acupuncture.
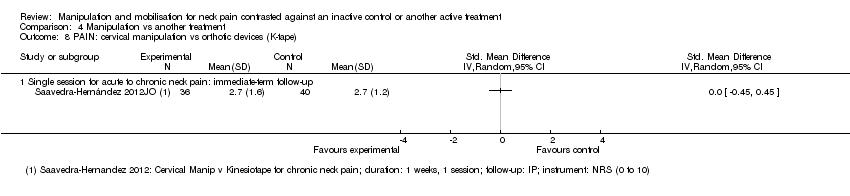
Comparison 4 Manipulation vs another treatment, Outcome 8 PAIN: cervical manipulation vs orthotic devices (K‐tape).
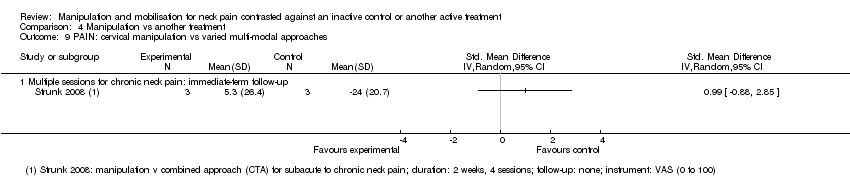
Comparison 4 Manipulation vs another treatment, Outcome 9 PAIN: cervical manipulation vs varied multi‐modal approaches.
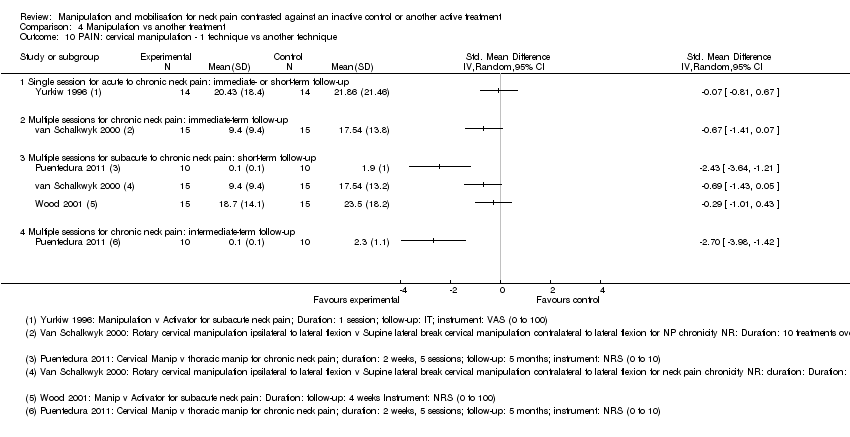
Comparison 4 Manipulation vs another treatment, Outcome 10 PAIN: cervical manipulation ‐ 1 technique vs another technique.
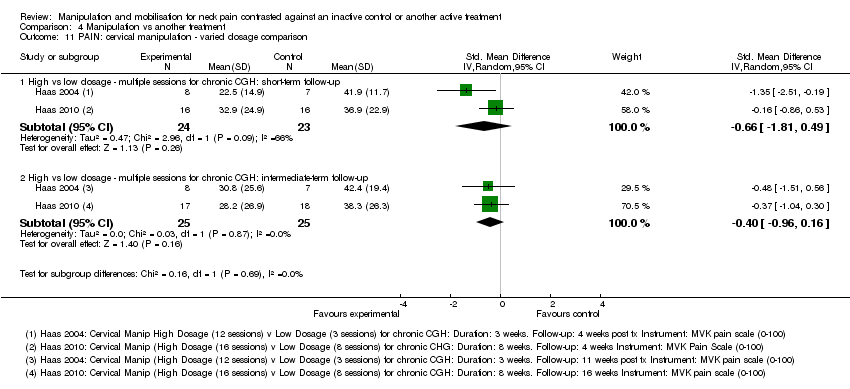
Comparison 4 Manipulation vs another treatment, Outcome 11 PAIN: cervical manipulation ‐ varied dosage comparison.

Comparison 4 Manipulation vs another treatment, Outcome 12 PAIN: thoracic manipulation vs exercise.

Comparison 4 Manipulation vs another treatment, Outcome 13 FUNCTION: cervical manipulation vs mobilisation.
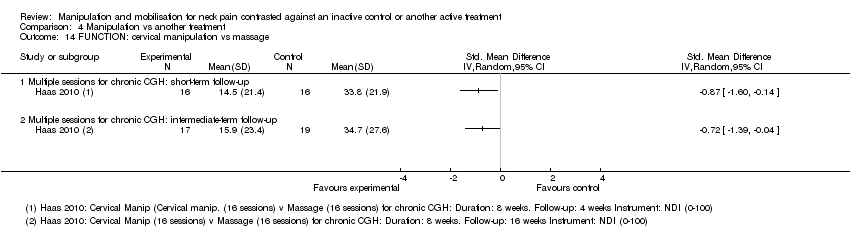
Comparison 4 Manipulation vs another treatment, Outcome 14 FUNCTION: cervical manipulation vs massage.
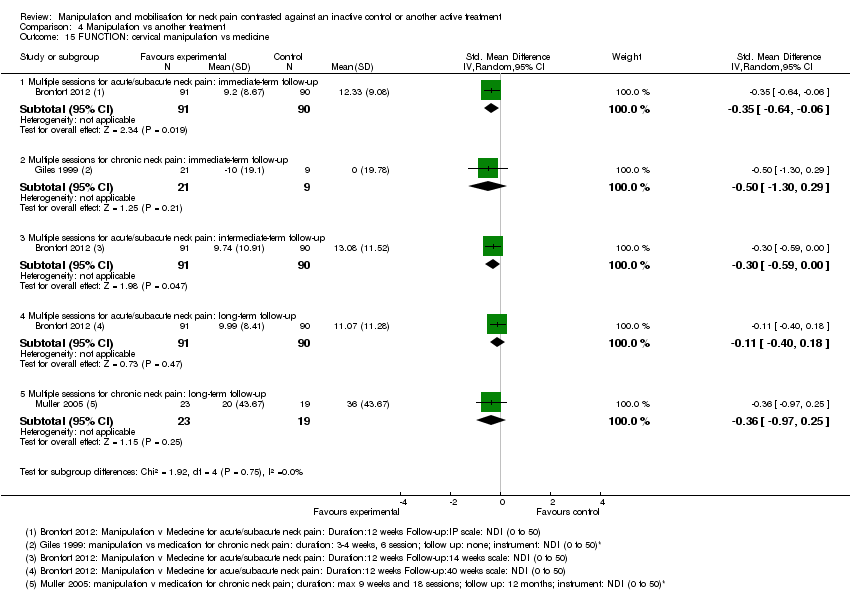
Comparison 4 Manipulation vs another treatment, Outcome 15 FUNCTION: cervical manipulation vs medicine.

Comparison 4 Manipulation vs another treatment, Outcome 16 FUNCTION: cervical manipulation vs exercise.

Comparison 4 Manipulation vs another treatment, Outcome 17 FUNCTION: cervical manipulation vs orthotic devices (K‐taping).

Comparison 4 Manipulation vs another treatment, Outcome 18 FUNCTION: cervical manipulation vs acupuncture.

Comparison 4 Manipulation vs another treatment, Outcome 19 FUNCTION: cervical manipulation vs varied multi‐modal approaches.

Comparison 4 Manipulation vs another treatment, Outcome 20 FUNCTION: cervical manipulation ‐ 1 technique vs another technique.

Comparison 4 Manipulation vs another treatment, Outcome 21 FUNCTION: cervical manipulation ‐ varied dosage comparison.
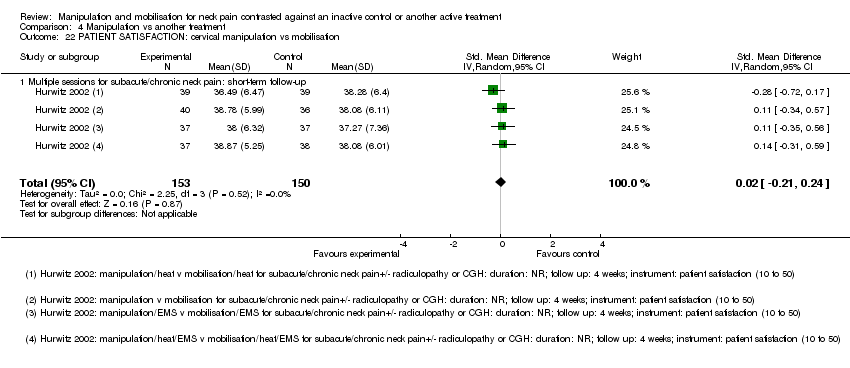
Comparison 4 Manipulation vs another treatment, Outcome 22 PATIENT SATISFACTION: cervical manipulation vs mobilisation.

Comparison 4 Manipulation vs another treatment, Outcome 23 PATIENT SATISFACTION: cervical manipulation vs varied multi‐modal approaches.
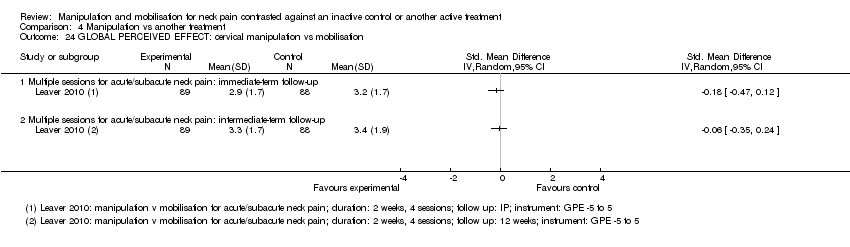
Comparison 4 Manipulation vs another treatment, Outcome 24 GLOBAL PERCEIVED EFFECT: cervical manipulation vs mobilisation.
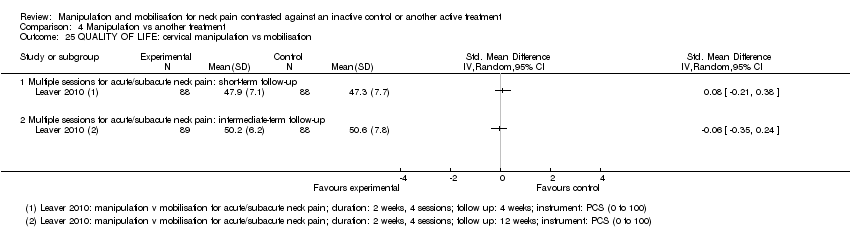
Comparison 4 Manipulation vs another treatment, Outcome 25 QUALITY OF LIFE: cervical manipulation vs mobilisation.

Comparison 4 Manipulation vs another treatment, Outcome 26 QUALITY OF LIFE: cervical manipulation vs medicine.

Comparison 4 Manipulation vs another treatment, Outcome 27 QUALITY OF LIFE: cervical manipulation vs exercise.
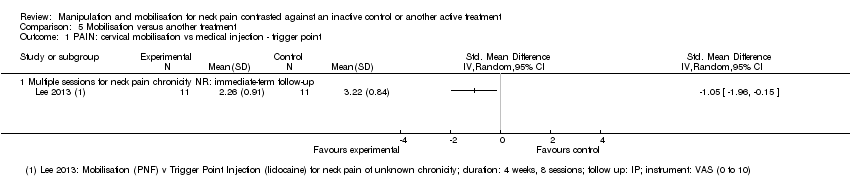
Comparison 5 Mobilisation versus another treatment, Outcome 1 PAIN: cervical mobilisation vs medical injection ‐ trigger point.
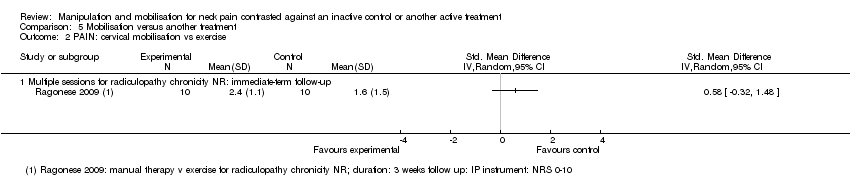
Comparison 5 Mobilisation versus another treatment, Outcome 2 PAIN: cervical mobilisation vs exercise.
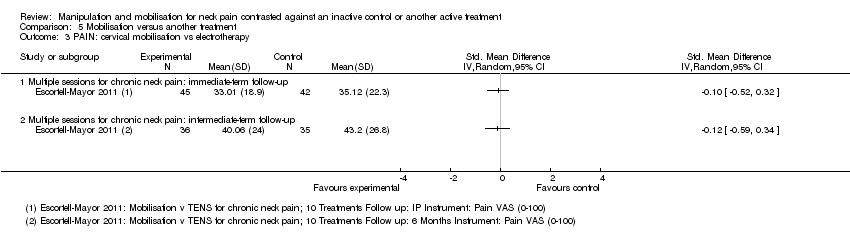
Comparison 5 Mobilisation versus another treatment, Outcome 3 PAIN: cervical mobilisation vs electrotherapy.

Comparison 5 Mobilisation versus another treatment, Outcome 4 PAIN: cervical mobilisation vs sonic devices ‐ ultrasound, shock wave therapy.

Comparison 5 Mobilisation versus another treatment, Outcome 5 PAIN: cervical mobilisation vs mechanical traction.

Comparison 5 Mobilisation versus another treatment, Outcome 6 PAIN: cervical mobilisation vs acupuncture.

Comparison 5 Mobilisation versus another treatment, Outcome 7 PAIN: cervical mobilisation vs varied multi‐modal approaches.

Comparison 5 Mobilisation versus another treatment, Outcome 8 PAIN: cervical mobilisation ‐ 1 technique vs another technique.

Comparison 5 Mobilisation versus another treatment, Outcome 9 PAIN: cervical mobilisation ‐ 1 technique vs another technique.

Comparison 5 Mobilisation versus another treatment, Outcome 10 PAIN: cervical mobilisation vs massage.

Comparison 5 Mobilisation versus another treatment, Outcome 11 FUNCTION: cervical mobilisation vs medical injection ‐ trigger point.

Comparison 5 Mobilisation versus another treatment, Outcome 12 FUNCTION: cervical mobilisation vs exercise.
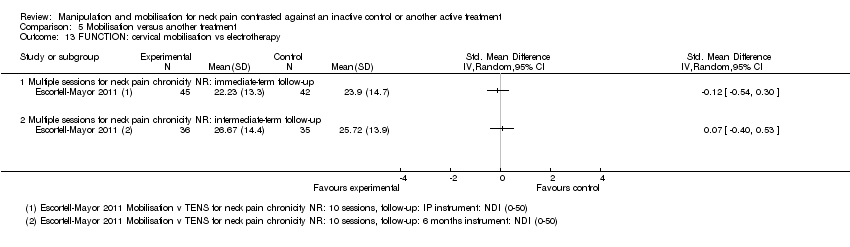
Comparison 5 Mobilisation versus another treatment, Outcome 13 FUNCTION: cervical mobilisation vs electrotherapy.

Comparison 5 Mobilisation versus another treatment, Outcome 14 FUNCTION: cervical mobilisation vs sonic devices ‐ shock wave therapy.

Comparison 5 Mobilisation versus another treatment, Outcome 15 FUNCTION: cervical mobilisation vs acupuncture.

Comparison 5 Mobilisation versus another treatment, Outcome 16 FUNCTION: cervical mobilisation vs varied multi‐modal approaches.

Comparison 5 Mobilisation versus another treatment, Outcome 17 FUNCTION: cervical mobilisation vs massage.

Comparison 5 Mobilisation versus another treatment, Outcome 18 FUNCTION: cervical mobilisation ‐ 1 technique vs another technique.
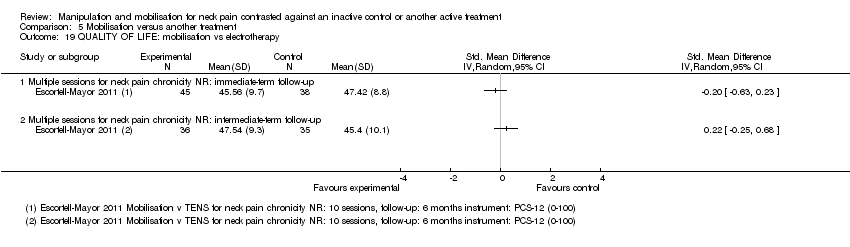
Comparison 5 Mobilisation versus another treatment, Outcome 19 QUALITY OF LIFE: mobilisation vs electrotherapy.

Comparison 5 Mobilisation versus another treatment, Outcome 20 PATIENT SATISFACTION: cervical mobilisation vs varied multi‐modal approaches.
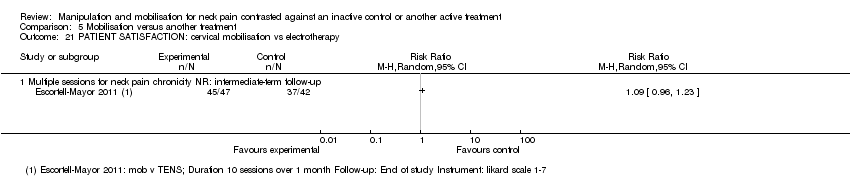
Comparison 5 Mobilisation versus another treatment, Outcome 21 PATIENT SATISFACTION: cervical mobilisation vs electrotherapy.
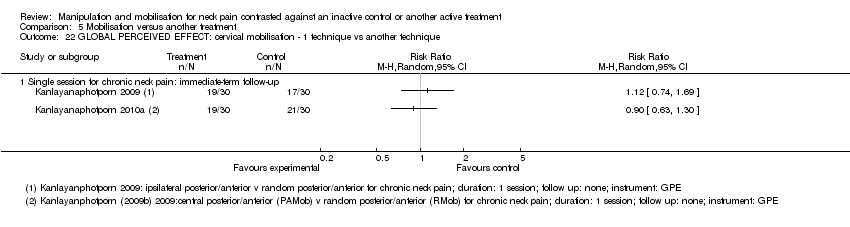
Comparison 5 Mobilisation versus another treatment, Outcome 22 GLOBAL PERCEIVED EFFECT: cervical mobilisation ‐ 1 technique vs another technique.
| Manipulation (cervical) compared with oral medicine for acute/subacute neck pain | ||||
| Patient or population: patients with acute and subacute neck pain Settings: outpatient clinics, ambulatory care services Intervention: manipulation of cervical region ‐ multiple sessions Comparison: oral medicine ‐ varied combinations of non‐steroidal anti‐inflammatory drugs (NSAIDs), analgesics, opioid analgesics and muscle relaxants | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD ‐0.21 (‐0.5 to 0.08) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD ‐0.32 (‐0.61 to ‐0.02) | 181 | ⊕⊕⊕⊝ Moderatea | Pain reduction favouring manipulation over medication |
| FUNCTION | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD ‐0.30 (‐0.59 to ‐0.00) | 182 | ⊕⊕⊕⊝ Moderatea | Functional improvement favouring manipulation over medication |
| Acute and subacute neck pain Long‐term follow‐up | SMD ‐0.11 (‐0.40 to 0.18)
| 181 | ⊕⊕⊕⊝ Moderatea | No significant difference between groups |
| PARTICIPANT SATISFACTION | ||||
| Acute and subacute neck pain Long‐term follow‐up | Not estimable | 182 | ⊕⊕⊕⊝ Moderatea | Manipulation favoured over medication |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD 0.22 (‐0.07 to 0.51) | 181 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: 0.19 (‐0.10 to 0.49) | 181 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Moderate‐quality evidence suggests that multiple sessions of cervical manipulation are more effective than medication (analgesics and non‐steroidal anti‐inflammatory drugs (NSAIDs)) for improving pain at immediate‐term and long‐term follow‐up (1 trial; 181 participants); function at intermediate term and satisfaction over the long term. Quality of life was similar between groups (1 trial, 182 participants) at intermediate‐ and long‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. | ||||
| aIndirectness: ‐1; a second independent trial is needed to clarify emerging data. | ||||
| Manipulation (thoracic) compared with inactive control for neck pain | ||||
| Patient or population: patients with acute, subacute and chronic neck pain Settings: outpatient clinics, ambulatory care services Intervention: manipulation of thoracic region ‐ multiple sessions Comparison: inactive control | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD pooled ‐1.46 (‐2.20 to ‐0.71) | 242 Fernandez 2004 JWRD; Fernandez 2009; Gonzalez‐Iglesias 2009 JO; | ⊕⊕⊕⊝ Moderatea | Favoured treatment; NNTB: 4 to 7; magnitude of effect: medium |
| Chronic neck pain Intermediate‐term follow‐up | SMD ‐0.64 (‐1.04 to ‐0.25) | 111 | ⊕⊕⊝⊝ Lowb,c | Favoured treatment; NNTB 4; magnitude of effect: small |
| FUNCTION | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD pooled ‐1.73 (‐2.68 to ‐0.78) | 258 | ⊕⊕⊕⊝ Moderatea | Favoured treatment; NNTB 4 to 5; magnitude of effect: medium |
| Chronic neck pain Short‐term follow‐up | SMD ‐0.50 (‐0.89 to ‐0.10) | 111 | ⊕⊕⊝⊝ Lowb,c | Favoured treatment; NNTB 5; magnitude of effect: small |
| Chronic neck pain Intermediate‐term follow‐up | SMD ‐0.38 (‐0.77 to 0.01) | 111 (1 trial; Cheung Lau 2011) | ⊕⊕⊝⊝ Lowb,c | Favoured treatment; NNTB 5; magnitude of effect: small |
| QUALITY OF LIFE (QoL) | ||||
| Chronic neck pain Short‐term follow‐up | SMD ‐0.82 (‐1.23 to ‐0.42) | 111 | ⊕⊕⊝⊝ Lowb,c | Favoured treatment |
| Chronic neck pain Intermediate‐term follow‐up | SMD ‐0.61 (‐1.01 to ‐0.22) | 111 | ⊕⊕⊝⊝ Lowc | Favoured treatment |
| Seven trials (428 participants) using multiple sessions of thoracic manipulation for acute to chronic neck pain were assessed at 3 time intervals. At short‐term follow‐up, moderate‐quality evidence favoured thoracic manipulation for pain reduction among participants with acute/subacute neck pain, and with acute to chronic neck pain, it improved function. These findings were consistent but small at intermediate follow‐up for pain, function and quality of life (low‐quality evidence). | ||||
| GRADE Working Group grades of evidence. | ||||
| bIndirectness: ‐1, immediate post‐treatment data have limited clinical relevance; single trials with only immediate‐ and short‐term follow‐up are downgraded (ceiling effect) because future research is likely to have an important impact on the direction of the reported effect, and a second independent trial is needed to clarify emerging short‐term data. cImprecision: ‐1, small sample size. aInconsistency: P value = 0.002; I² = 84%; sensitivity analysis: Statistical differences led us to explore heterogeneity by the following PICO factors: P: about the same; I: about the same; C: about the same; O: for pain, VAS, NPRS; for disability, NPQ, NDI; RoB: most often low RoB but when the trial of high RoB is removed, pooled SMD increases to ‐2.18 (‐2.71 to ‐1.65) for pain, but these data were derived from trials conducted in the same lab. | ||||
| Manipulation compared with mobilisation for neck pain | ||||
| Patient or population: patients with acute, subacute and chronic neck pain Settings: ambulatory care or outpatient clinic Intervention: manipulation of cervical region ‐ multiple sessions Comparison: mobilisation | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute, subacute and chronic neck pain Intermediate‐term follow‐up | MD pooled ‐0.07 (‐0.72 to 0.59) | 446 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| FUNCTION AND DISABILITY | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD: ‐0.06 (‐0.35 to 0.24) | 176 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| Acute, subacute and chronic neck pain Intermediate‐term follow‐up | SMD pooled: 0.10 (‐0.18 to 0.37)
| 446 | ⊕⊕⊕⊕ High | No significant differences between groups |
| PARTICIPANT SATISFACTION | ||||
| Subacute and chronic neck pain Short‐term follow‐up | SMD: ‐0.02 (‐0.21 to 0.24) | 269 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| GLOBAL PERCEIVED EFFECT | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.06 | 177 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Short‐term follow‐up | SMD: 0.08 (‐0.21 to 0.38) | 176 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.06 (‐0.35 to 0.24) | 177 | ⊕⊕⊕⊝ Moderateb | No significant differences between groups |
| Moderate‐ to high‐quality evidence (2 trials, 446 participants) suggests that multiple sessions of cervical manipulation produced similar changes in pain, function, quality of life, global perceived effect and patient satisfaction when compared with multiple sessions of cervical mobilisation at immediate‐, short‐ and intermediate‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. | ||||
| aInconsistency: ‐1. bIndirectness: ‐1. | ||||
| Manipulation compared with exercise for neck pain | ||||
| Patient or population: patients with acute and subacute neck pain Settings: ambulatory care or outpatient clinic setting Intervention: manipulation of cervical region Comparison: exercise | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.16 (‐0.45 to 0.13) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: 0.06 (‐0.23 to 0.35) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| FUNCTION | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.01 (‐0.30 to 0.28)
| 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: ‐0.02 (‐0.31 to 0.27)
| 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| PARTICIPANT SATISFACTION | ||||
| Acute and subacute neck pain Long‐term follow‐up | Not estimable | 182 | ⊕⊕⊕⊝ Moderatea | Improvement in participant satisfaction for manipulation over exercise |
| GLOBAL PERCEIVED EFFECT | ||||
| Acute and subacute neck pain Immediate post‐treatment follow‐up | Not estimable | 182 (1 trial; Bronfort 2012) | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| QUALITY OF LIFE | ||||
| Acute and subacute neck pain Intermediate‐term follow‐up | SMD: ‐0.05 (‐0.35 to 0.24) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Acute and subacute neck pain Long‐term follow‐up | SMD: 0.0 (‐0.29 to 0.29) | 182 | ⊕⊕⊕⊝ Moderatea | No significant differences between groups |
| Moderate‐quality evidence suggests no differences in pain, function, global perceived effect and quality of life when multiple sessions of cervical manipulation are compared with exercise at immediate‐, intermediate‐ and long‐term follow‐up. Moderate‐quality evidence indicates that use of cervical manipulation led to greater participant satisfaction when compared with an exercise programme at long‐term follow‐up. | ||||
| GRADE Working Group grades of evidence. | ||||
| aIndirectness: ‐1. | ||||
| High dose of manipulation compared with low dose of manipulation for chronic neck pain | ||||
| Patient or population: patients with chronic neck pain with cervicogenic headache (CGH) Settings: ambulatory care or outpatient clinic setting Intervention: manipulation of cervical region Comparison: high dose vs low dose | ||||
| Outcomes | Relative effect | Number of participants | Quality of the evidence | Comments |
| PAIN | ||||
| Chronic neck pain and CGH Intermediate‐term follow‐up | SMD pooled: ‐0.40 (‐0.96 to 0.16)
| ⊕⊕⊕⊝ Moderatea | Two trials showed no significant differences between groups | |
| FUNCTION | ||||
| Chronic neck pain and CGH Intermediate‐term follow‐up | SMD pooled: ‐0.61 (‐1.38 to 0.17) | ⊕⊕⊕⊝ Moderatea | Two trials showed no significant differences between groups | |
| Moderate‐quality evidence shows that high‐dose (12 to 18 sessions) contrasted against low‐dose (3 to 8 sessions) cervical manipulation produced similar changes in pain and function at intermediate‐term follow‐up for individuals with chronic neck pain with cervicogenic headache. | ||||
| GRADE Working Group grades of evidence. | ||||
| aImprecision: ‐1. | ||||
| Term | Definiton |
| Per cent treatment advantage (%) | Calculation of the clinically important difference or change in a per cent scale was estimated as follows. Karlberg 1996 data are used in this example. % improvement (control) equals the difference between the change in the control group (1) divided by the control baseline (56), which equals 1.8%. Treatment advantage = 42.6% ‐ 1.8% = 40.8% |
| Number needed to treat (NNTB) | For this example, Karlberg 1996 outcomes measured at short‐term follow‐up are used to derive the data. Number needed to treat is the number of patients a clinician needs to treat to achieve a clinically important improvement in 1. If we assume the minimal clinically important difference to be 10% of the baseline mean in the control group, and the control group mean at baseline is 56, then 10% of 56 is 5.6 The effect is baseline ‐ final value; therefore:
Converting these to standard normal values means that:
NNTB = 1 divided by the difference in areas under the normal curve (experimental group ‐ control group):
|
| Author/Comparison | NNTB | Advantage, % |
| PAIN | ||
| Haas 2004: pain | 12 (clinically important pain reduction) at ST | 23 |
| Haas 2010: pain | 4 (clinically important pain reduction) at IT | 29 |
| Cleland 2005 | 5 (clinically important pain reduction) | 29 |
| Cheung Lau 2011: pain | 4 (clinically important pain reduction) | |
| Fernandez 2004a | Unable to calculate because baseline data not reported | |
| Gonzalez‐Iglesias 2009 | 7 (clinically important pain reduction) | 47 |
| Martinez‐Segura 2006, | 2 (clinically important pain reduction) | 54 |
| Massaracchio 2013: pain | 4 (clinically important pain reduction) | |
| von Piekartz 2011: pain | 2 (clinically important pain reduction) at IT | |
| FUNCTION | ||
| Cheung Lau 2011: function | 5 (clinically important functional improvement) at IT | |
| Gonzalez‐Iglesias 2009 | 5 (clinically important functional improvement) | 41 |
| Haas 2010: function | 5 (clinically important functional improvement) at ST and IT | ST: 41 IT: 39 |
| Massaracchio 2013: function | 4 (clinically important functional improvement) | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical manipulation vs placebo Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Single session: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: thoracic manipulation vs placebo Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Single session: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Multiple sessions for chronic neck pain with HA: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical manipulation plus treatment vs same treatment in both arms Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Single session for subacute/chronic neck pain: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 PAIN: cervical manipulation vs same treatment in both arms Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 Single session for subacute/chronic neck pain with radicular findings and HA: short‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 PAIN: thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Single session for neck pain of not reported duration: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: thoracic manipulation vs same treatment in both arms Show forest plot | 8 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Multiple sessions for acute neck pain: immediate‐term follow‐up | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐3.46 [‐4.13, ‐2.79] |
| 5.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐1.15, 0.69] |
| 5.3 Single session for chronic neck pain: short‐term follow‐up | 1 | 82 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.36, 0.51] |
| 5.4 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 4 | 242 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.46 [‐2.20, ‐0.71] |
| 5.5 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐0.99, ‐0.20] |
| 5.6 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐1.04, ‐0.25] |
| 6 PAIN: cervical and thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 FUNCTION: thoracic manipulation vs same treatment in both arms Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 141 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.85, ‐0.18] |
| 7.2 Single session for chronic neck pain: short‐term follow‐up | 1 | 81 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.61, 0.27] |
| 7.3 Multiple sessions for acute neck pain: short‐term follow‐up | 3 | 154 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.73 [‐2.68, ‐0.78] |
| 7.4 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.89, ‐0.10] |
| 7.5 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.77, 0.01] |
| 8 FUNCTION: cervical manipulation vs same treatment in both arms Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 FUNCTION: cervical and thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 QUALITY OF LIFE: thoracic manipulation vs control Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Multiple sessions for chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 FUNNEL PLOT for pain: thoracic manipulation vs same treatment in both arms Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 Multiple sessions for acute to chronic neck pain: short‐term follow‐up | 5 | 346 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.26 [‐1.86, ‐0.66] |
| 12 FUNNEL PLOT for function: thoracic manipulation vs same treatment in both arms Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Multiple sessions: short‐term follow‐up | 4 | 258 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.40 [‐2.24, ‐0.55] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical mobilisation vs control Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Single session: intermediate post treatment | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Multiple sessions: short‐term follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical manipulation vs mobilisation at immediate post treatment Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Single session for acute to chronic neck pain: immediate‐ or short‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Multiple sessions for acute to subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical manipulation vs mobilisation at intermediate‐term follow‐up Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Multiple sessions for acute to chronic neck pain: intermediate‐term follow‐up | 2 | 446 | Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.72, 0.59] |
| 3 PAIN: cervical manipulation vs massage Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Multiple sessions for chronic CGH: short‐term follow‐up | 2 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.93, ‐0.07] |
| 3.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.47, ‐0.11] |
| 4 PAIN: cervical manipulation vs medicine Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.4 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.5 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: cervical manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 PAIN: cervical manipulation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Multiple sessions for subacute to chronic CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 Multiple sessions for subacute to chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 PAIN: cervical manipulation vs acupuncture Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 PAIN: cervical manipulation vs orthotic devices (K‐tape) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Single session for acute to chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 PAIN: cervical manipulation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 PAIN: cervical manipulation ‐ 1 technique vs another technique Show forest plot | 4 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 Single session for acute to chronic neck pain: immediate‐ or short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Multiple sessions for subacute to chronic neck pain: short‐term follow‐up | 3 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.4 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 PAIN: cervical manipulation ‐ varied dosage comparison Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 High vs low dosage ‐ multiple sessions for chronic CGH: short‐term follow‐up | 2 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.81, 0.49] |
| 11.2 High vs low dosage ‐ multiple sessions for chronic CGH: intermediate‐term follow‐up | 2 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.96, 0.16] |
| 12 PAIN: thoracic manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Multiple sessions for neck pain chronicity NR: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 FUNCTION: cervical manipulation vs mobilisation Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 1 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.35, 0.24] |
| 13.2 Multiple sessions for acute to chronic neck pain: intermediate‐term follow‐up | 2 | 445 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.21, 0.18] |
| 14 FUNCTION: cervical manipulation vs massage Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Multiple sessions for chronic CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 FUNCTION: cervical manipulation vs medicine Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.64, ‐0.06] |
| 15.2 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.30, 0.29] |
| 15.3 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.59, ‐0.00] |
| 15.4 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | 181 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.40, 0.18] |
| 15.5 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | 42 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.97, 0.25] |
| 16 FUNCTION: cervical manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 FUNCTION: cervical manipulation vs orthotic devices (K‐taping) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 17.1 Single session for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 FUNCTION: cervical manipulation vs acupuncture Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 18.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Multiple sessions for chronic neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 FUNCTION: cervical manipulation vs varied multi‐modal approaches Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 19.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Multiple sessions for subacute/chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 FUNCTION: cervical manipulation ‐ 1 technique vs another technique Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 20.1 Multiple sessions for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.3 Multiple sessions for neck pain chronicity NR: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.4 Multiple sessions for acute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 FUNCTION: cervical manipulation ‐ varied dosage comparison Show forest plot | 2 | 97 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.09, ‐0.14] |
| 21.1 High vs low dosage ‐ multiple sessions for chronic CGH: short‐term follow‐up | 2 | 47 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.75 [‐1.71, 0.22] |
| 21.2 High vs low dosage ‐ multiple sessions for chronic CGH: intermediate‐term follow‐up | 2 | 50 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐1.38, 0.17] |
| 22 PATIENT SATISFACTION: cervical manipulation vs mobilisation Show forest plot | 1 | 303 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.21, 0.24] |
| 22.1 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | 303 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.21, 0.24] |
| 23 PATIENT SATISFACTION: cervical manipulation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 23.1 Multiple sessions for subacute/chronic neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24 GLOBAL PERCEIVED EFFECT: cervical manipulation vs mobilisation Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 24.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 24.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25 QUALITY OF LIFE: cervical manipulation vs mobilisation Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 25.1 Multiple sessions for acute/subacute neck pain: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 25.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26 QUALITY OF LIFE: cervical manipulation vs medicine Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 26.1 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 26.2 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27 QUALITY OF LIFE: cervical manipulation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 27.1 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27.2 Multiple sessions for acute/subacute neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 27.3 Multiple sessions for acute/subacute neck pain: long‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 PAIN: cervical mobilisation vs medical injection ‐ trigger point Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 PAIN: cervical mobilisation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Multiple sessions for radiculopathy chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 PAIN: cervical mobilisation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 PAIN: cervical mobilisation vs sonic devices ‐ ultrasound, shock wave therapy Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Single session for subacute/chronic neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 PAIN: cervical mobilisation vs mechanical traction Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 PAIN: cervical mobilisation vs acupuncture Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 PAIN: cervical mobilisation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 PAIN: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 5 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Single session for chronic neck pain: immediate‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 Single session for chronic neck pain ± radiculopathy: immediate‐term follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.4 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 PAIN: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9.1 PA vs other mobilisation for acute/subacute neck pain: multiple sessions: immediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 AP vs other mobilisation: multiple sessions: immediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 PAIN: cervical mobilisation vs massage Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.56 [‐4.15, 1.03] |
| 10.2 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | ‐2.89 [‐3.85, ‐1.93] |
| 11 FUNCTION: cervical mobilisation vs medical injection ‐ trigger point Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 FUNCTION: cervical mobilisation vs exercise Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 Multiple sessions for radiculopathy: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 FUNCTION: cervical mobilisation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 FUNCTION: cervical mobilisation vs sonic devices ‐ shock wave therapy Show forest plot | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 Multiple sessions for acute/subacute neck pain: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 FUNCTION: cervical mobilisation vs acupuncture Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15.1 Multiple sessions for chronic neck pain: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 FUNCTION: cervical mobilisation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 FUNCTION: cervical mobilisation vs massage Show forest plot | 2 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.90, 0.84] |
| 17.1 Multiple sessions for chronic neck pain: immediate‐term follow‐up | 1 | 23 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐1.35, 0.32] |
| 17.2 Multiple sessions for subacute/chronic CGH: immediate‐term follow‐up | 1 | 36 | Std. Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.28, 1.04] |
| 18 FUNCTION: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 18.1 Multiple sessions for chronic CGH: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 Multiple sessions for chronic CGH: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 QUALITY OF LIFE: mobilisation vs electrotherapy Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 19.1 Multiple sessions for neck pain chronicity NR: immediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 PATIENT SATISFACTION: cervical mobilisation vs varied multi‐modal approaches Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 20.1 Multiple sessions for subacute/chronic neck pain ± radiculopathy or CGH: short‐term follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 21 PATIENT SATISFACTION: cervical mobilisation vs electrotherapy Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 21.1 Multiple sessions for neck pain chronicity NR: intermediate‐term follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 22 GLOBAL PERCEIVED EFFECT: cervical mobilisation ‐ 1 technique vs another technique Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 22.1 Single session for chronic neck pain: immediate‐term follow‐up | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |

