Colaboración interprofesional para mejorar la práctica profesional y los resultados de la atención sanitaria
Appendices
Appendix 1. CENTRAL search strategy
#1[mh "Interprofessional Relations"] and (collaborat* or team*)
#2 [mh "Patient Care Team"] and (collaborat* or team*)
#3 ((interprofession* or inter‐profession*) next (collaborat* or team*))
#4 ((interdisciplin* or inter‐disciplin*) next (collaborat* or team*))
#5 ((interoccupation* or inter‐occupation*) next (collaborat* or team*))
#6 ((multiprofession* or multi‐profession*) next (collaborat* or team*))
#7 ((multidisciplin* or multi‐disciplin*) next (collaborat* or team*))
#8((multioccupation* or multi‐occupation*) next (collaborat* or team*))
#9((transdisciplin* or trans‐disciplin*) next (collaborat* or team*))
#10(team* next collaborat*)
#11{or #1‐#10}
Appendix 2. MEDLINE search strategy
1 exp Interprofessional Relations/ and (collaborat$ or team$).tw. (8220)
2 exp Patient Care Team/ and (collaborat$ or team$).tw. (13439)
3 ((interprofession$ or inter‐profession$) adj (collaborat$ or team$)).tw. (853)
4 ((interdisciplin$ or inter‐disciplin$) adj (collaborat$ or team$)).tw. (2660)
5 ((interoccupation$ or inter‐occupation$) adj (collaborat$ or team$)).tw. (0)
6 ((multiprofession$ or multi‐profession$) adj (collaborat$ or team$)).tw. (355)
7 ((multidisciplin$ or multi‐disciplin$) adj (collaborat$ or team$)).tw. (7856)
8 ((multioccupation$ or multi‐occupation$) adj (collaborat$ or team$)).tw. (0)
9 ((transdisciplin$ or trans‐disciplin$) adj (collaborat$ or team$)).tw. (105)
10 (team$ adj collaborat$).tw. (158)
11 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 (26183)
12 randomized controlled trial.pt. (276233)
13 controlled clinical trial.pt. (42446)
14 randomized controlled trials/ (83918)
15 random allocation/ (45887)
16 double blind method/ (80591)
17 single blind method/ (16519)
18 12 or 13 or 14 or 15 or 16 or 17 (452549)
19 animals/ not humans/ (1793680)
20 18 not 19 (410246)
21 11 and 20 (954)
22 limit 21 to yr="2007 ‐Current" (595)
Appendix 3. CINAHL search strategy
1 (MH "Interprofessional Relations+") AND TX ((collaborat* or team*))
2 (MH " Multidisciplinary Care Team+") AND TX ((collaborat* or team*))
3 TX ((interprofession* or inter‐profession*) N1 (collaborat* or team*))
4 TX ((interdisciplin* or inter‐disciplin*)) N1 (collaborat* or team*))
5 TX ((interoccupation* or inter‐occupation*) N1 (collaborat* or team*))
6 TX ((multiprofession* or multi‐profession*) N1 (collaborat* or team*))
7 TX ((multidisciplin* or multi‐disciplin*) N1 (collaborat* or team*))
8 TX ((multioccupation* or multi‐occupation*) N1 (collaborat* or team*))
9 TX ((multioccupation* or multi‐occupation*) N1 (collaborat* or team*))
10 TX ((transdisciplin* or trans‐disciplin*) N1 (collaborat* or team*))
11 TX team* N1 collaborat*
12 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11
13 (MH "Clinical Trials+")
14 PT Clinical trial
15 TX ( (trebl* n1 blind*) or (trebl* n1 mask*) )
16 TX ( (tripl* n1 blind*) or (tripl* n1 mask*) )
17 TX ( (doubl* n1 blind*) or (doubl* n1 mask*) )
18 TX ( (singl* n1 blind*) or (singl* n1 mask*) )
19 TX randomi* control* trial*
20 (MH "Random Assignment")
21 TX random* allocat*
22 TX placebo*
23 (MH "Placebos")
24 (MH "Quantitative Studies")
25 TX allocat* random*
26 S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25
27 S12 AND S26
28 S12 AND S26. Limiters ‐ Publication Year: 2007‐2014; Clinical Trial
Appendix 4. ClinicalTrials.gov and ICTRP search strategies
ClinicalTrials.gov search strategy
(collaboration OR team) AND (interdisciplinary OR interprofessional OR multidisciplinary OR multiprofessional)
ICTRP search strategy
#1 collaboration AND interdisciplinary
#2 collaboration AND interprofessional
#3 collaboration AND multidisciplinary
#4 collaboration AND multiprofessional
#5 team AND interdisciplinary
#6 team AND interprofessional
#7 multidisciplinary team
#8 team AND multiprofessional
#9 OR/1‐8

Flow diagram of study selection
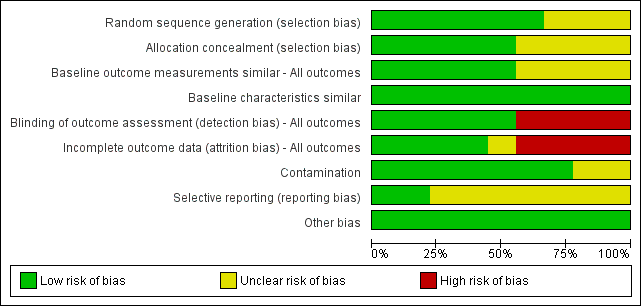
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies, based on EPOC methods.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study, based on EPOC methods.
| Effects of practice‐based interprofessional collaboration (IPC) interventions on professional practice and healthcare outcomes compared to usual care | |||
| Patient or population: health and social care professionals involved in the delivery of health services and patient care | |||
| Outcomes | Impacts | No. of studies (participants) | Certainty of the evidence |
| Patient health outcomes | |||
| Patient functional status | Externally facilitated interprofessional activities may slightly improve stroke patients' functional status (Strasser 2008). | 1 (464) | ⊕⊕⊖⊖ Lowa |
| Patient‐assessed quality of care | It is uncertain if externally facilitated interprofessional activities increases patient‐assessed quality of care because the certainty of this evidence is very low (Black 2013). | 1 (1185) | ⊕⊖⊖⊖ Very lowb |
| Patient mortality, morbidity or complication rates | None of the included studies reported patient mortality, morbidity or complication rates. | ‐‐ | ‐‐ |
| Clinical process or efficiency outcomes | |||
| Adherence to recommended practices | The use of interprofessional activities with an external facilitator or interprofessional meetings may slightly improve adherence to recommended practices and prescription of drugs (Cheater 2005; Deneckere 2013; Schmidt 1998). | 3 (2576) | ⊕⊕⊖⊖ Lowc |
| Continuity of care | It is uncertain if externally facilitated interprofessional activities improves continuity of care because the certainty of this evidence is very low (Strasser 2008). | 1 (464) | ⊕⊖⊖⊖ Very lowd |
| dUse of healthcare resources | Interprofessional checklists (Calland 2011), interprofessional rounds (Curley 1998; Wild 2004) or externally facilitated interprofessional activities (Strasser 2008), may slightly improve overall use of resources, length of hospital stay, or costs. | 4 (1679) | ⊕⊕⊖⊖ Lowe |
| Collaborative behaviour outcomes | |||
| Collaborative working; team communication; team co‐ordination | It is uncertain whether externally facilitated interprofessional activities (Black 2013; Calland 2011; Cheater 2005; Deneckere 2013) improve collaborative working, team communication, and co‐ordination because the certainty of this evidence is very low. | 4 (1936) | ⊕⊖⊖⊖ Very lowf |
| GRADE Working Group grades of evidence | |||
| a We assessed the certainty of the evidence as low because of high risk of bias (no blinding of outcome assessment). b We assessed the certainty of the evidence as very low because of the risk of bias (high risk of attrition and detection bias; details about allocation sequence generation and concealment were not reported). c We assessed the certainty of the evidence as low due to potential indirectness (both studies were conducted in one country and the outcomes may not be transferable to other settings), and risk of bias (high risk of attrition, unclear selection and reporting risk). d We assessed the certainty of the evidence as very low because of risk of bias (high risk of attrition and detection bias, and unclear risk of selection bias). e We assessed the certainty of evidence as low because of high risk of bias (attrition and detection), and unclear risk of bias (selection, reporting, and contamination). f We assessed the certainty of the evidence as very low due to high risk of bias (selection, attrition, and detection) or unclear risk of bias (reporting and contamination). | |||
| Effects of practice‐based interprofessional collaboration (IPC) interventions on professional practice and healthcare outcomes compared with alternative IPC intervention | |||
| Patient or population: health and social care professionals involved in the delivery of health services and patient care Settings: two hospitals in Australia Intervention: multidisciplinary video conferencing Comparison: multidisciplinary audio conferencing | |||
| Outcomes | Impacts | No. of | Certainty of the evidence (GRADE) |
| Patient health outcomes | The study did not report patient health outcomes. | ‐ | ‐ |
| Clinical process or efficiency outcomes | Video conferencing may reduce the average length of treatment, compared to audio conferencing and may improve process/efficiency outcomes by reducing the number of multidisciplinary conferences needed per patient and patient length of stay. | 1 (100) | ⊕⊕⊖⊖ Lowa |
| Collaborative behaviour outcomes | There was little or no difference between the interventions in the number of communications between health professionals. | 1 (100) | ⊕⊕⊖⊖ Lowa |
| GRADE Working Group grades of evidence | |||
| a We assessed the certainty of evidence as low because of high risk of bias (attrition and detection) and unclear risk of bias (selection, reporting, and contamination). | |||

