Vesicular monoamine transporter inhibitors versus placebo for antipsychotic‐induced tardive dyskinesia
Abstract
This is a protocol for a Cochrane Review (Intervention). The objectives are as follows:
To report the absolute effects of VMAT2 drugs for people with antipsychotic‐induced tardive dyskinesia.
Background
Description of the condition
Since the 1950s, antipsychotic (otherwise known as neuroleptic) medication has been used extensively to treat people with chronic mental illnesses such as schizophrenia. These medications can effectively control symptoms such as abnormal perceptions (hallucinations), disordered thinking, and fixed false beliefs (delusions). In addition, long‐term therapy with antipsychotic medication is associated with a reduced risk of relapse of schizophrenia (Schooler 1993). Antipsychotic medication, however, has also been associated with a wide range of adverse effects, including movement disorders (Barnes 1993). These movement disorders can be disfiguring, distressing, stigmatising, and are associated with poor compliance to antipsychotic treatment (Barnes 1993; Tarsy 2011).
Tardive dyskinesia (TD) is one such iatrogenic movement disorder. It is characterised by abnormal repetitive and involuntary movements. The clinical features include: tongue protrusion, side‐to‐side or rotatory movement of the jaw, lip smacking, puckering and pursing, and rapid eye blinking (Casey 1999). In some people rapid movements of the arms, legs, and trunk may also occur. TD is a chronic condition of insidious onset, the severity of which fluctuates spontaneously (APA 1992). Although the most frequent cause of TD is the use of antipsychotic medication, it is somewhat counterintuitive that a dose reduction can lead to a temporary exacerbation in symptoms. Conversely, increasing the dose is often associated with a temporary remission (Cavallaro 1993; Smith 1980).
The exact mechanisms underlying the pathophysiology of TD are unknown. Antipsychotic drugs block certain chemical receptor sites in the brain, one such site is specific for dopamine (Casey 1994). One hypothesis explaining the cause of antipsychotic‐induced TD is that chronic blockade of dopamine receptors in specific cells of the brain (i.e. neurones from the nigrostriatum) causes an overgrowth of these receptors (Casey 1994). However, there is some suggestion that the long‐term use of antipsychotics may also cause an abnormal production of highly active atoms and chemical groups (e.g. cytotoxic free radicals), which may damage specific cells in the brain. This, in turn, could be responsible for the appearance of TD (Cadet 1989). This theory is supported by the persistent nature of TD once established (Casey 1994).
TD occurs in more than 20% of people that use first‐generation antipsychotic drugs continually for longer than three months (Tarsy 2011). Every year, 4% to 5% of adults and 25% to 30% of elderly people who continually use these drugs begin to show signs of TD (APA 1992; Correll 2004). Advancing age is a risk factor for both the prevalence and severity of TD, with individuals who are under 60 years of age being three times more likely to spontaneously remit (Smith 1980). Studies on the natural history of TD have reported widely variable remission rates (1% to 62%), depending on the individual's age, psychiatric diagnosis, course of the psychiatric disorder, and duration of therapy (Bergen 1989; Fernandez 2001; Glazer 1990).
When the second‐generation antipsychotic drugs were introduced in the 1990s many hoped that they would not cause TD (Miller 2007; Rosenheck 2007). Although the risk of developing TD with second‐generation antipsychotic drugs does seem to be lower, TD risks ha not been eliminated (Miller 2007; Tarsy 2011). There is even some evidence to indicate that rates of TD do not differ at all between first‐ and second‐generation antipsychotic drugs (Leucht 2009; Rosenheck 2007; Woods 2010). A large, definitive, US, randomised trial of antipsychotic treatments for schizophrenia (CATIE), with a four‐year follow‐up, obtained an incidence rate of TD of around 17% (Miller 2008). Due to the widespread use of second‐generation antipsychotic drugs, increased off‐label use of these agents, and an ageing population, the frequency of TD is likely to be higher than thought (Cloud 2014; Maher 2012) and increasing. The problem will be considerably greater for people in countries where the use of newer drugs is less prevalent (Ballesteros 2000; Martins 2011).
Description of the intervention
1. Vesicular monoamine transporter 2 (VMAT2) inhibitors
This group of drugs acts to reversibly inhibit the vesicular monoamine transporter 2 (VMAT2) protein from carrying out its function of storing monoamine neurotransmitters, primarily dopamine, in vesicles, thus causing levels of dopamine in the synaptic cleft to decrease.
1.1 Deutetrabenazine
Deutetrabenazine (Figure 1), sold as Austedo, was approved by the US Food and Drugs Administration (FDA) on the 30 August 2017 for use in people with tardive dyskinesia. This, the second FDA‐approved drug for the treatment of tardive dyskinesia, is currently distributed exclusively in the USA in the form of oral,coated tablets containing deutetrabenazine at doses of 6 mg, 9 mg, or 12 mg (Martindale 2017a).
![Deutetrabenazine (3R,11bR)‐3‐(2‐methylpropyl)‐9,10‐bis(trideuteriomethoxy)‐1,3,4,6,7,11b‐hexahydrobenzo[a]quinolizin‐2‐one](/cdsr/doi/10.1002/14651858.CD012986/media/CDSR/CD012986/image_n/nCD012986-AFig-FIG01.png)
Deutetrabenazine (3R,11bR)‐3‐(2‐methylpropyl)‐9,10‐bis(trideuteriomethoxy)‐1,3,4,6,7,11b‐hexahydrobenzo[a]quinolizin‐2‐one
1.2 Valbenazine
Valbenazine (Figure 2), sold as Ingressa, was approved by the US FDA in April 2017. This first FDA‐approved drug for treatment of TD is currently distributed exclusively in the USA in the form of oral capsules containing valbenazine at doses of 40 mg and 80 mg (Martindale 2017).
![Valbenazine (2R,3R,11bR)‐3‐isobutyl‐9,10‐dimethoxy‐1,3,4,6,7,11b‐hexahydro‐2H‐pyrido[2,1‐a]isoquinolin‐2‐yl L‐valinate)](/cdsr/doi/10.1002/14651858.CD012986/media/CDSR/CD012986/image_n/nCD012986-AFig-FIG02.png)
Valbenazine (2R,3R,11bR)‐3‐isobutyl‐9,10‐dimethoxy‐1,3,4,6,7,11b‐hexahydro‐2H‐pyrido[2,1‐a]isoquinolin‐2‐yl L‐valinate)
How the intervention might work
Tardive dyskinesia is thought to be caused by dopamine receptor hypersensitivity (Margolese 2005). VMAT2 inhibitors are thought to combat tardive dyskinesia by selectively binding to and inhibiting VMAT2 and preventing it from storing dopamine in synaptic vesicles. This leaves the dopamine vulnerable to metabolism by enzymes. As a result, the reduced level of dopamine in the synaptic cleft means that, while still reacting hyperactively to dopamine, the receptors receive less dopamine and so have a similar response to that of an average receptor. This leads to reduced levels of dopamine in the synaptic cleft as the vesicles do not carry the monoamine neurotransmitters. VMAT2 inhibitors have no significant binding to vesicular monoamine transporter 1 (VMAT1), meaning that there is thought to be no significant adverse or 'off‐target' effects from the reduction of other monoamine neurotransmitters (FDA 2017).
Why it is important to do this review
TD can result in considerable social and physical disability and symptoms are often irreversible (Barnes 1993; Bergen 1989; Fernandez 2001; Gerlach 1988; Glazer 1990). Additionally, TD is frequently associated with a lower quality of life (Ascher‐Svanum 2008), greater mortality rate (Chong 2009), and poor compliance (Barnes 1993). Several antipsychotic medications have been produced in recent decades that claim to cause less or no TD relative to older agents (Lieberman 1996). However, evidence suggests that the thoughtful use of older‐generation drugs is not associated with more TD than newer treatments (Chouinard 2008). In addition, in a global context, it is likely that drugs that are less expensive and morefamiliar than newer‐generation drugs ‐ such as chlorpromazine or haloperidol ‐ will continue to be the mainstay of treatment in people with schizophrenia (WHO Essential List 2010). Use of drugs such as these is associated with emergence of TD and, therefore, this condition is likely to remain a problem for years to come.
Given the high incidence and prevalence of TD among people taking antipsychotic medication, the need for prevention or treatment is clear. Unfortunately, there is sparse evidence to guide clinicians (NICE 2014; Taylor 2009). The recent approval of VMAT2 drugs by the FDA is an indication of hope for the treatment of TD. This review will quantify the best evidence from all relevant randomised controlled trials.
This review is one in a series of Cochrane Reviews (see Table 1) evaluating treatments for antipsychotic‐induced TD. In preparatory consultation with service users with TD for these reviews frustration was expressed by one person concerning this neglected area of research (Figure 3). Informed by these consultations (Bergman 2017), we have included user‐led outcomes in the 'Summary of findings' tables.
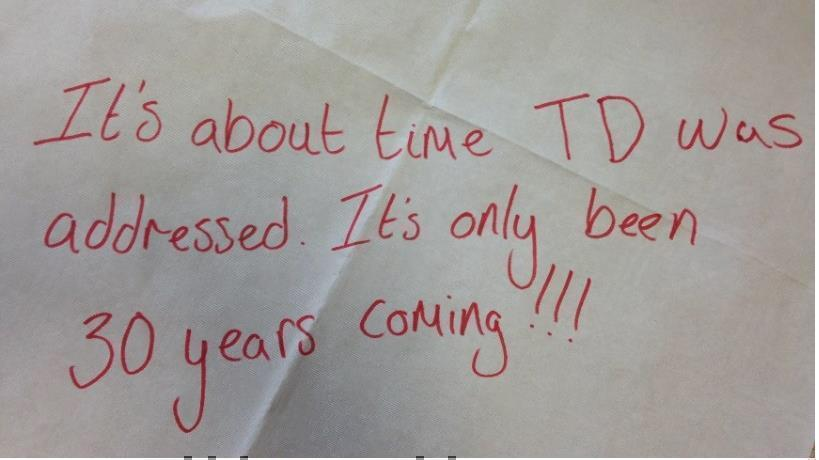
Message from one of the participants in the public and patient involvement consultation of service‐user perspectives on tardive dyskinesia research
| Interventions | Current reference(s) (updates underway) |
| Anticholinergic medication | |
| Benzodiazepines | |
| Calcium‐channel blockers | |
| Cholinergic medication | |
| Gamma‐aminobutyric acid agonists | |
| Miscellaneous treatments | |
| Antipsychotic reduction orcessation, or both, and neuroleptics | |
| Non‐neuroleptic catecholaminergic drugs | |
| Vitamin E |
Objectives
To report the absolute effects of VMAT2 drugs for people with antipsychotic‐induced tardive dyskinesia.
Methods
Criteria for considering studies for this review
Types of studies
We will include all relevant randomised controlled trials. If there are trials that are described as double‐blind, but do not mention whether the study was randomised, we will include them in a sensitivity analysis (see Sensitivity analysis). We will exclude quasi‐randomised studies, such as those allocating participants to different interventions by using alternate days of the week.
Types of participants
We will include people with schizophrenia or any other serious mental illness, diagnosed by any criteria, irrespective of gender, age, or nationality who required the use of antipsychotics for more than three months and who developed TD (diagnosed by any criteria) during antipsychotic treatment, and whom the dose of antipsychotic medication had been stable for one month or more. We will include studies that did not require antipsychotic medication to have been stable for one month prior to randomisation. We feel it important to include these studies as they provide additional important information. However, we will compare the result of these studies with others in a sensitivity analysis primary outcomes and include all together if there no substantive differences.
Types of interventions
1. Vesicular monoamine transporter
1.1 Deutetrabenazine
Any dose suggested as being therapeutic (6 mg/day to 12 mg/day), any means of delivery.
1.2 Valbenazine
Any dose suggested as being therapeutic (40 mg/day to 80 mg/day), any means of delivery.
versus
2. Placebo
Any means of delivery.
Types of outcome measures
We will define clinical efficacy as an improvement in the symptoms of TD of more than 50%, on any scale (please see Data extraction and management for details of the scales we will include). We intend to group outcomes into short term (less than six weeks), medium term (between six weeks and six months) and long term (more than six months).
Primary outcomes
1. Tardive dyskinesia (TD) symptoms
Clinically important change in the TD symptoms of individuals, defined as more than 50% improvement on any TD scale ‐ over any time period
2. Adverse effects
Clinically important extrapyramidal adverse effects ‐ over any time period
Secondary outcomes
1. Tardive dyskinesia (TD) symptoms
1.1 Any change in the symptoms of TD, defined as any change on any TD scale
1.2 Deterioration in the symptoms of TD, defined as any deleterious change on any TD scale
1.3 Average endpoint/change score on any TD scale
2. Mental state
2.1 Relapse (according to any definition)
2.2 Any change in mental state (such as delusions and hallucinations), defined as any change on any scale
2.3 Average endpoint score or change score on mental state scale
2.5 Use of clozapine
3. Leaving the study early (acceptability of treatment)
3.1 Acceptability of the intervention to participants as measured by numbers of people leaving the study early
4. Adverse effects
4.1 Any adverse effect (other than deterioration symptoms of TD or relapse).
4.2 Use of any antiparkinson drugs
4.3 Average endpoint/change score on extrapyramidal adverse effects scale
4.4 Acute dystonia
4.5 Other adverse effects ‐ divided into general and specific
5. Hospital and service utilisation outcomes
5.1 Hospital admission
5.2 Average change in days in hospital
5.3 Improvement in hospital status (e.g. change from formal to informal admission status, use of seclusion, level of observation)
5.4 Improvement in community status (intensity of service utilisation, use of treatment orders)
6. Economic outcomes
6.1 Average change in total cost of medical and mental health care
6.2 Total indirect and direct costs
6.3 Employment
7. Social confidence, social inclusion, social networks, or personalised quality‐of‐life measures
7.1. Clinically important changes in social confidence, social inclusion, social networks, or personalised quality‐of‐life measures in either recipients of care or caregivers
7.2 Average endpoint/change score in social confidence, social inclusion, social networks, or personalised quality‐of‐life measures
7.3 Stigma ‐ however assessed.
8. Behaviour
8.1 Clinically important agitation
8.2 Use of adjunctive medication for sedation
8.3 Aggression to self or others
9. Cognitive state
9.1 Clinically important change
9.2 Any change, general and specific
'Summary of findings' table
We will use the GRADE approach to interpret findings (Schünemann 2011) and use GRADEpro‐GDT to export data from this review to create 'Summary of findings' tables. These tables provide outcome‐specific information concerning the overall quality of evidence from the included studies in the comparison, the magnitude of effects of interventions examined, and the sum of available data on all outcomes rated as important to patient care and decision making. We aim to select the following main outcomes for inclusion in the 'Summary of findings' table.
-
Tardive dyskinesia: clinically important change TD symptoms, defined as more than 50% improvement on any TD scale ‐ over any time period
-
Tardive dyskinesia: deterioration in symptoms of TD, defined as any deleterious change on any TD scale
-
Adverse effects: clinically important extrapyramidal adverse effects ‐ over any time period.
-
Adverse effects: any adverse effect (other than deterioration in symptoms of TD or relapse).
-
Mental state: any change in mental state (such as delusions and hallucinations), defined as any change on any scale.
-
Leaving the study early (acceptability of treatment): acceptability of the intervention to participants as measured by numbers of people leaving the study early.
-
Social confidence, social inclusion, social networks, or personalised quality of‐life measures: clinically important changes in social confidence, social inclusion, social networks, or personalised quality‐of‐life measures in either recipients of care or caregivers.
Search methods for identification of studies
Electronic searches
Cochrane Schizophrenia Group's Study‐Based Register of Trials
The information specialist will search the above register using the following search strategy:
(Deutetrabenazine OR Valbenazine) in Intervention Field of STUDY
In such a study‐based register, searching the major concept retrieves all the synonyms and relevant studies because all the studies have already been organised based on their interventions and linked to the relevant topics (Shokraneh 2018).
This register is compiled by systematic searches of major resources (AMED, BIOSIS, CINAHL, ClinicalTrials.Gov, EMBASE, MEDLINE, PsycINFO, PubMed, WHOICTRP www.who.int/ictrp/en/) and their monthly updates, ProQuest Dissertations and Theses A&I and its quarterly update, Chinese databases (CBM, CNKI, and Wanfang) and their annual updates, hand‐searches, grey literature, and conference proceedings (see Cochrane Schizophrenia Group's Module). There are no language, date, document type, or publication status limitations inclusion of records into the register.
Searching other resources
1. Reference searching
We will inspect the references of all identified studies for further relevant studies.
2. Personal contact
We will contact the first author of each included study for information regarding unpublished trials.
Data collection and analysis
Selection of studies
Review authors BK and CEA will inspect all abstracts and citations of studies identified in the searches and identify potentially relevant reports. SAS will inspect a random 10% sample for reliability. We will resolve disagreement by discussion, or where there is still doubt, we will acquire the full article for further inspection. We will acquire the full articles of all potentially relevant reports/abstracts and carefully inspect them to make a final decision on inclusion based on predetermined criteria (see Criteria for considering studies for this review). Where difficulties or disputes arise, we will ask HB for help. Where it is impossible to decide or if adequate information is not available ‐ even after contacting authors ‐ we will add these studies to those awaiting assessment.
Data extraction and management
1. Extraction
Review authors BK and CEA will independently extract data from all included studies. SAS will extract a random 10% sample for reliability. Again, we will discuss any disagreement and document decisions. We will extract data presented only in graphs and figures whenever possible, but will only include such data if BK and CEA independently the same result. We will attempt to contact study authors through an open‐ended request in order to obtain missing information or for clarification whenever necessary. If studies are multi‐centre, where possible, we will extract data relevant to each component centre separately.
2. Management
2.1 Forms
We will extract data into paper forms.
2.2 Scale‐derived data
We will include continuous data from rating scales only if:
a) the psychometric properties of the measuring instrument have been described in a peer‐reviewed journal (Marshall 2000);
b) the measuring instrument has not been written or modified by one of the trialists for that particular trial; and
c) the instrument should be a global assessment of an area of functioning and not sub‐scores which are not, in themselves, validated or shown to be reliable. However there are exceptions, we will include sub‐scores from mental state scales measuring positive and negative symptoms of schizophrenia.
Ideally the measuring instrument should either be i. a self‐report or ii. completed by an independent rater or relative (not the therapist). We realise that this is not often reported clearly; in 'Description of studies' we will note if this is the case or not.
2.3 Endpoint versus change data
There are advantages of both endpoint and change data: change data can remove a component of between‐person variability from the analysis; however, calculation of change needs two assessments (baseline and endpoint) that can be difficult to obtain in unstable and difficult‐to‐measure conditions such as schizophrenia. We have decided primarily to use endpoint data, and only use change data if the former are not available. If necessary, we will combine endpoint and change data in the analysis, as we prefer to use mean differences (MDs) rather than standardised mean differences (SMDs) throughout (Deeks 2011).
2.4 Skewed data
Continuous data on clinical and social outcomes are often not normally distributed. To avoid the pitfall of applying parametric tests to non‐parametric data, we will apply the following standards to relevant continuous data before inclusion.
For endpoint data from studies including fewer than 200 participants:
a) when a scale starts from the finite number zero, we will subtract the lowest possible value from the mean, and divide this by the standard deviation. If this value is lower than one, it strongly suggests that the data are skewed and we will exclude these data. If this ratio is higher than one but less than two, there is suggestion that the data are skewed: we will enter these data and test whether their inclusion or exclusion would change the results substantially. If such data change results we will enter as 'other data'. Finally, if the ratio is larger than two we will include these data, because it is less likely that they are skewed (Altman 1996; Higgins 2011).
b) if a scale starts from a positive value (such as the Positive and Negative Syndrome Scale (PANSS), which can have values from 30 to 210 (Kay 1986)), we will modify the calculation described above to take the scale starting point into account. In these cases skewed data are present if 2 SD > (S − S min), where S is the mean score and 'S min' is the minimum score.
Please note: we will enter all relevant data from studies of more than 200 participants in the analysis irrespective of the above rules, because skewed data pose less of a problem in large studies. We will also enter all relevant change data, as when continuous data are presented on a scale that includes a possibility of negative values (such as change data), it is difficult to tell whether or not data are skewed.
2.5 Common measure
Where relevant, to facilitate comparison between trials, we plan to convert variables that can be reported in different metrics, such as days in hospital (mean days per year, per week, or per month) to a common metric (e.g. mean days per month).
2.6 Conversion of continuous to binary
Where possible, we plan to convert continuous outcome measures to dichotomous data. This can be done by identifying cutoff points on rating scales and dividing participants accordingly into 'clinically improved' or 'not clinically improved'. It is generally assumed that if there is a 50% reduction in a scale‐derived score such as the Brief Psychiatric Rating Scale (BPRS, Overall 1962) or the PANSS (Kay 1986), this can be considered as a clinically significant response (Leucht 2005a; Leucht 2005b). If data based on these thresholds are not available, we will use the primary cutoff presented by the study authors.
2.7 Direction of graphs
Where possible, we plan to enter data in such a way that the area to the left of the line of no effect indicates a favourable outcome for VMAT2. Where keeping to this makes it impossible to avoid outcome titles with clumsy double‐negatives (e.g. 'not un‐improved') we will present data where the left of the line indicates an unfavourable outcome and note this in the relevant graphs.
Assessment of risk of bias in included studies
BK and CEA will independently assess risk of bias within the included studies by using criteria described in the Cochrane Handbook for Systematic Reviews of Interventions to assess trial quality (Higgins 2011a). This set of criteria is based on evidence of associations between overestimate of effect and high risk of bias the article such as sequence generation, allocation concealment, blinding, incomplete outcome data, and selective reporting.
If the raters disagree, we will make the final rating by consensus, with the involvement of HB. Where inadequate details of randomisation and other characteristics of trials are provided, we will contact authors of the studies in order to obtain further information. If non‐concurrence occurred, we will report this.
We will note the level of risk of bias in the text of the review and in the text and 'Summary of findings' tables.
Measures of treatment effect
1. Binary data
For binary outcomes we will calculate a standard estimation of the risk ratio (RR) and its 95% confidence interval (CI), as it has been shown that RR is more intuitive than odds ratios (Boissel 1999); and that odds ratios tend to be interpreted as RR by clinicians (Deeks 2000). Although the number needed to treat for an additional beneficial outcome (NNTB) and the number needed to treat for an additional harmful outcome (NNTH), with their CIs, are intuitively attractive to clinicians, they are problematic to calculate and interpret in meta‐analyses (Hutton 2009). For binary data presented in the 'Summary of findings' table/s we will, where possible, calculate illustrative comparative risks.
2. Continuous data
For continuous outcomes we will estimate MD between groups. We prefer not to calculate effect size measures (SMD). However if scales of very considerable similarity are used, we will presume there is a small difference in measurement, and we will calculate effect size and transform the effect back to the units of one or more of the specific instruments.
Unit of analysis issues
1. Cluster‐randomised trials
Studies increasingly employ 'cluster randomisation' (such as randomisation by clinician or practice), but the analysis and pooling of clustered data pose problems. First, study authors often fail to account for intraclass correlation in clustered studies, leading to a 'unit of analysis' error (Divine 1992) whereby P values are spuriously low, confidence intervals unduly narrow, and statistical significance overestimated. This causes type I errors (Bland 1997; Gulliford 1999).
If any of the included trials have randomised participants by clusters, and where clustering is not accounted for in primary studies, we will present such data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. In subsequent versions of this review we will seek to contact first authors of studies to obtain intraclass correlation coefficients (ICCs) for their clustered data and to adjust for this by using accepted methods (Gulliford 1999). Where clustering has been incorporated into the analysis of primary studies, we will present these data as if from a non‐cluster‐randomised study, but adjust for the clustering effect.
We have sought statistical advice and have been advised that the binary data as presented in a report should be divided by a 'design effect'. This is calculated using the mean number of participants per cluster (m) and the ICC (design effect = 1 + (m ‐ 1) * ICC) (Donner 2002). If the ICC is not reported we will assume it is 0.1 (Ukoumunne 1999).
If cluster studies are appropriately analysed, taking into account ICCs and relevant data documented in the report, it will be possible to synthesise the results with those of other studies using the generic inverse variance technique.
2. Cross‐over trials
A major concern of cross‐over trials is the carry‐over effect. The carry‐over effect occurs if an effect (e.g. pharmacological, physiological, or psychological) of a treatment in the first phase is carried over to the second phase. As a consequence, on entry to the second phase the participants can differ systematically from their initial state despite a washout phase. For the same reason, cross‐over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both first‐ and second‐phase effects are very likely in individuals with severe mental illness, we will use only data from the first phase of any cross‐over studies.
3. Studies with multiple treatment groups
Where a study involves more than two treatment arms, if relevant, we will present the additional treatment arms in comparisons. If data are binary we will simply add and combine them within a 2 x 2 table. If data are continuous we will combine the data using the formulae in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We will not use data where the additional treatment arms are not relevant.
Dealing with missing data
1. Overall loss of credibility
At some degree of loss to follow‐up, data must lose credibility (Xia 2009). We have decided that, for any particular outcome, should more than 50% of data be unaccounted for we will not reproduce these data or use them within analyses. If, however, more than 50% of those in one arm of a study are lost, but the total loss is less than 50%, we will address this within the 'Summary of findings' tables by downgrading the quality of evidence. We will also downgrade evidence quality within the 'Summary of findings' tables should the loss to follow‐up be 25% to 50% in total.
2. Binary outcomes
Where attrition for a binary outcome is between 0% and 50%, and where these data are not clearly described, we will present data on a 'once‐randomised‐always‐analyse' basis (an intention‐to‐treat (ITT) analysis). We will assume that all those leaving the study early had seen no improvement in TD symptoms. We will undertake a sensitivity analysis, testing how prone the primary outcomes are to change by comparing data only from participants who completed the study to that point to the ITT analysis using the above assumptions.
3. Continuous
3.1 Attrition
We will report and use data where attrition for a continuous outcome is between 0% and 50%, and data only from people who had completed the study to that point are reported.
3.2 Standard deviations
If standard deviations (SDs) are not reported, we will try to obtain the missing values from the authors. If these are not available, where there are missing measures of variance for continuous data, but an exact standard error (SE) and CIs available for group means, and either P value or t value available for differences in mean, we can calculate SDs according to the rules described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). When only the SE is reported, SDs are calculated by the formula SD = SE * √(n). The Cochrane Handbook for Systematic Reviews of Interventions presents detailed formulae for estimating SDs from P, t or F values, CIs, ranges or other statistics (Higgins 2011). If these formulae do not apply, we will calculate the SDs according to a validated imputation method which is based on the SDs of the other included studies (Furukawa 2006). Although some of these imputation strategies can introduce error, the alternative would be to exclude a given study’s outcome and thus to lose information. Nevertheless, we will examine the validity of the imputations in a sensitivity analysis that excludes imputed values.
3.3 Assumptions about participants who left the trials early or were lost to follow‐up
Various methods are available to account for participants who left the trials early or were lost to follow‐up. Some trials just present the results of study completers; others use the method of last observation carried forward (LOCF); while more recently, methods such as multiple imputation or mixed‐effects models for repeated measurements (MMRM) have become more of a standard. While the latter methods seem to be somewhat better than LOCF (Leon 2006), we feel that the high percentage of participants leaving the studies early and differences between groups in their reasons for doing so is often the core problem in randomised schizophrenia trials. We will therefore not exclude studies based on the statistical approach used. However, by preference we will use the more sophisticated approaches, i.e. we will prefer to use MMRM or multiple‐imputation to LOCF, and we will only present completer analyses if some kind of ITT data are not available at all. Moreover, we will address this issue in the item 'Incomplete outcome data' of the 'Risk of bias' tool.
Assessment of heterogeneity
1. Clinical heterogeneity
We will consider all included studies initially, without seeing comparison data, to judge clinical heterogeneity. We will simply inspect all studies for participants who are clearly outliers or situations that we had not predicted would arise and, where found, discuss such situations or participant groups.
2. Methodological heterogeneity
We will consider all included studies initially, without seeing comparison data, to judge methodological heterogeneity. We will simply inspect all studies for clearly outlying methods which we had not predicted would arise and discuss any such methodological outliers.
3. Statistical heterogeneity
3.1 Visual inspection
We will visually inspect graphs to investigate the possibility of statistical heterogeneity.
3.2 Employing the I2 statistic
We will investigate heterogeneity between studies by considering the I² statistic alongside the Chi² P value. The I² statistic provides an estimate of the percentage of inconsistency thought to be due to chance (Higgins 2003). The importance of the observed value of I² depends on the magnitude and direction of effects as well as the strength of evidence for heterogeneity (e.g. P value from Chi²¬test, or a confidence interval for I²). We will interpret an I² estimate greater than or equal to 50% and accompanied by a statistically significant Chi² statistic as evidence of substantial heterogeneity (Chapter 9. Cochrane Handbook for Systematic Reviews of Interventions) (Deeks 2011). When substantial levels of heterogeneity are found in the primary outcome, we will explore reasons for heterogeneity (Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results (Egger 1997). These are described in Chapter 10 of the Cochrane Handbook for Systemic reviews of Interventions (Sterne 2011).
1. Protocol versus full study
We will try to locate protocols of included randomised trials. If the protocol is available, we will compare outcomes in the protocol and in the published report. If the protocol is not available, we will compare outcomes listed in the methods section of the trial report with actually reported results.
2. Funnel plot
We are aware that funnel plots may be useful in investigating reporting biases but are of limited power to detect small‐study effects. We will not use funnel plots for outcomes where there are 10 or fewer studies, or where all studies are of similar size. In other cases, where funnel plots are possible, we will seek statistical advice on their interpretation.
Data synthesis
We understand that there is no closed argument for a preference for the use of fixed‐effect or random‐effects models. The random‐effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This often seems to be true to us and the random‐effects model takes into account differences between studies even if there is no statistically significant heterogeneity. There is, however, a disadvantage to the random‐effects model. It puts added weight onto small studies, which often are the most biased ones. Depending on the direction of effect, these studies can either inflate or deflate the effect size. We will use the fixed‐effect model for analyses.
Subgroup analysis and investigation of heterogeneity
1. Subgroup analyses
1.1 Primary outcomes
We anticipate no subgroup analyses.
1.2 Clinical state, stage, or problem
We propose to undertake this review and provide an overview of the effects of antipsychotic reduction/cessation or specific antipsychotics in people with TD in general. In addition, however, we will try to report data on subgroups of participants in the same clinical state and stage, and with similar problems.
2. Investigation of heterogeneity
We will report where inconsistency is high. First, we will investigate whether data are entered correctly. Second, if data are correct, we will visually inspect the graph and successively remove studies outside of the company of the rest to see if homogeneity is restored. For this review we have decided that, should this occur with data contributing no more than around 10% of the total weighting to the summary finding, we will present these data. If not, we will not pool such data, but will discuss the relevant issues in the text. We know of no supporting research for this 10% cutoff, but are investigating the use of prediction intervals as an alternative to this unsatisfactory state.
When unanticipated clinical or methodological heterogeneity are obvious, we will simply discuss.
Sensitivity analysis
1. Implication of randomisation
If trials are described in some way as to imply randomisation we will undertake a sensitivity analysis of the primary outcomes. We will include these studies in the analyses, and if there is no substantive difference when the implied randomised studies are added to those with a better description of randomisation, we will use relevant data from these studies.
2. Assumptions for lost binary data
Where we have to make assumptions regarding people lost to follow‐up (see Dealing with missing data) we will compare the findings of the primary outcomes when we use our assumption compared with completer data only. If there is a substantial difference, we will report and discuss these results but continue to use our assumption.
Where we have to make assumptions regarding missing SD data (see Dealing with missing data), we will compare the findings of primary outcomes when we use our assumption compared with completer data only. We will undertake a sensitivity analysis, testing how prone the results are to change when completer data only are compared with the imputed data using the above assumption. If there is a substantial difference, we will report and discuss these results but continue to use our assumption.
3. Risk of bias
We will analyse the effects of excluding trials that we judge to be at high risk of bias across one or more of the domains of randomisation (see Assessment of risk of bias in included studies). If the exclusion of trials at high risk of bias does not substantially alter the direction of effect or the precision of the effect estimates, we will include data from these trials in the analyses.
4. Imputed values
If data from cluster‐randomised trials are included, we will undertake a sensitivity analysis to assess the effects of including data from trials where we use imputed values for ICC in calculating the design effect.
If we find substantial differences in the direction or precision of effect estimates in any of the sensitivity analyses listed above, we will not pool data from the excluded trials with the other trials contributing to the outcome, but present them separately.
5. Fixed‐effect and random‐effects models
We will synthesise data using a fixed‐effect model; however, we will also synthesise data for the primary outcome using a random‐effects model to evaluate whether this alters the significance of the results.
6. Studies with stable medication regimens
We anticipate that whereas some studies will keep participants on very stable antipsychotic regimens others may not, and that this could confound the results in a way we are not sure we can predict. We will test, for the primary outcomes, whether removing studies with participants on less‐stable antipsychotic regimens makes any substantive difference to the findings, and where this is not so, will synthesise all data.
![Deutetrabenazine (3R,11bR)‐3‐(2‐methylpropyl)‐9,10‐bis(trideuteriomethoxy)‐1,3,4,6,7,11b‐hexahydrobenzo[a]quinolizin‐2‐one](/es/cdsr/doi/10.1002/14651858.CD012986/media/CDSR/CD012986/image_n/nCD012986-AFig-FIG01.png)
Deutetrabenazine (3R,11bR)‐3‐(2‐methylpropyl)‐9,10‐bis(trideuteriomethoxy)‐1,3,4,6,7,11b‐hexahydrobenzo[a]quinolizin‐2‐one
![Valbenazine (2R,3R,11bR)‐3‐isobutyl‐9,10‐dimethoxy‐1,3,4,6,7,11b‐hexahydro‐2H‐pyrido[2,1‐a]isoquinolin‐2‐yl L‐valinate)](/es/cdsr/doi/10.1002/14651858.CD012986/media/CDSR/CD012986/image_n/nCD012986-AFig-FIG02.png)
Valbenazine (2R,3R,11bR)‐3‐isobutyl‐9,10‐dimethoxy‐1,3,4,6,7,11b‐hexahydro‐2H‐pyrido[2,1‐a]isoquinolin‐2‐yl L‐valinate)

Message from one of the participants in the public and patient involvement consultation of service‐user perspectives on tardive dyskinesia research
| Interventions | Current reference(s) (updates underway) |
| Anticholinergic medication | |
| Benzodiazepines | |
| Calcium‐channel blockers | |
| Cholinergic medication | |
| Gamma‐aminobutyric acid agonists | |
| Miscellaneous treatments | |
| Antipsychotic reduction orcessation, or both, and neuroleptics | |
| Non‐neuroleptic catecholaminergic drugs | |
| Vitamin E |

