Effects of total fat intake on bodyweight in children
Abstract
Background
As part of efforts to prevent childhood overweight and obesity, we need to understand the relationship between total fat intake and body fatness in generally healthy children.
Objectives
To assess the effects of total fat intake on measures of weight and body fatness in children and young people not aiming to lose weight.
Search methods
For this update we revised the previous search strategy and ran it over all years in the Cochrane Library, MEDLINE (Ovid), MEDLINE (PubMed), and Embase (Ovid) (current to 23 May 2017). No language and publication status limits were applied. We searched the World Health Organization International Clinical Trials Registry Platform and ClinicalTrials.gov for ongoing and unpublished studies (5 June 2017).
Selection criteria
We included randomised controlled trials (RCTs) in children aged 24 months to 18 years, with or without risk factors for cardiovascular disease, randomised to a lower fat (30% or less of total energy (TE)) versus usual or moderate‐fat diet (greater than 30%TE), without the intention to reduce weight, and assessed a measure of weight or body fatness after at least six months. We included prospective analytical cohort studies in these children if they related baseline total fat intake to weight or body fatness at least 12 months later. We duplicated inclusion decisions and resolved disagreement by discussion with other authors.
Data collection and analysis
We extracted data on participants, interventions or exposures, controls and outcomes, and trial or cohort quality characteristics, as well as data on potential effect modifiers, and assessed risk of bias for all included studies. We extracted outcome data using the following time point ranges, when available: RCTs: baseline to six months, six to 12 months, one to two years, two to five years and more than five years; cohort studies: baseline to one year, one to two years, two to five years, five to 10 years and more than 10 years. We planned to perform random‐effects meta‐analyses with relevant subgrouping, and sensitivity and funnel plot analyses where data allowed.
Main results
We included 24 studies comprising three parallel‐group RCTs (n = 1054 randomised) and 21 prospective analytical cohort studies (about 25,059 children completed). Twenty‐three were conducted in high‐income countries. No meta‐analyses were possible, since only one RCT reported the same outcome at each time point range for all outcomes, and cohort studies were too heterogeneous.
For the RCTs, concerns about imprecision and poor reporting limited our confidence in our findings. In addition, the inclusion of hypercholesteraemic children in two trials raised concerns about applicability. Lower versus usual or modified total fat intake may have made little or no difference to weight over a six‐ to twelve month period (mean difference (MD) ‐0.50 kg, 95% confidence interval (CI) ‐1.78 to 0.78; 1 RCT; n = 620; low‐quality evidence), nor a two‐ to five‐year period (MD ‐0.60 kg, 95% CI ‐2.39 to 1.19; 1 RCT; n = 612; low‐quality evidence). Compared to controls, lower total fat intake (30% or less TE) probably decreased BMI in children over a one‐ to two‐year period (MD ‐1.5 kg/m2, 95% CI ‐2.45 to ‐0.55; 1 RCT; n = 191; moderate‐quality evidence), with no other differences evident across the other time points (two to five years: MD 0.00 kg/m2, 95% CI ‐0.63 to 0.63; 1 RCT; n = 541; greater than five years; MD ‐0.10 kg/m2, 95% CI ‐0.75 to 0.55; 1 RCT; n = 576; low‐quality evidence). Lower fat intake probably slightly reduced total cholesterol over six to 12 months compared to controls (MD ‐0.15 mmol/L, 95% CI ‐0.24 to ‐0.06; 1 RCT; n = 618; moderate‐quality evidence), but may make little or no difference over longer time periods. Lower fat intake probably slightly decreased low‐density lipoprotein (LDL) cholesterol over six to 12 months (MD ‐0.12 mmol/L, 95% CI ‐0.20 to ‐0.04; 1 RCT; n = 618, moderate‐quality evidence) and over two to five years (MD ‐0.09, 95% CI ‐0.17 to ‐0.01; 1 RCT; n = 623; moderate‐quality evidence), compared to controls. However, lower total fat intake probably made little or no difference to HDL‐C over a six‐ to 12‐month period (MD ‐0.03 mmol/L, 95% CI ‐0.08 to 0.02; 1 RCT; n = 618; moderate‐quality evidence), nor a two‐ to five‐year period (MD ‐0.01 mmol/L, 95% CI ‐0.06 to 0.04; 1 RCT; n = 522; moderate‐quality evidence). Likewise, lower total fat intake probably made little or no difference to triglycerides in children over a six‐ to 12‐month period (MD ‐0.01 mmol/L, 95% CI ‐0.08 to 0.06; 1 RCT; n = 618; moderate‐quality evidence). Lower versus usual or modified fat intake may make little or no difference to height over more than five years (MD ‐0.60 cm, 95% CI ‐2.06 to 0.86; 1 RCT; n = 577; low‐quality evidence).
Over half the cohort analyses that reported on primary outcomes suggested that as total fat intake increases, body fatness measures may move in the same direction. However, heterogeneous methods and reporting across cohort studies, and predominantly very low‐quality evidence, made it difficult to draw firm conclusions and true relationships may be substantially different.
Authors' conclusions
We were unable to reach firm conclusions. Limited evidence from three trials that randomised children to a lower total fat intake (30% or less TE) versus usual or modified fat intake, but with no intention to reduce weight, showed small reductions in body mass index, total‐ and LDL‐cholesterol at some time points with lower fat intake compared to controls, and no consistent differences in effects on weight, high‐density lipoprotein (HDL) cholesterol or height. Associations in cohort studies that related total fat intake to later measures of body fatness in children were inconsistent and the quality of this evidence was mostly very low. Twenty‐three out of 24 included studies were conducted in high‐income countries, and may not be applicable in low‐ and middle‐income settings. High‐quality, longer‐term studies are needed, that include low‐ and middle‐income settings and look at both possible benefits and risks.
PICO
Plain language summary
Effect of cutting down the amount of fat on bodyweight in children
Review question
What is the relationship between the amount of fat a child eats and their weight and body fat?
Background
To try to better prevent people from being overweight and obese, we need to understand what the ideal amount of total fat in our diets should be, and particularly how this is related to bodyweight and fatness. This relationship differs in children compared to adults, because children are still growing and developing.
Study characteristics
This review looked at the effects of eating less fat on bodyweight and fatness in healthy children aged between two and 18 years, who were not aiming to lose weight. We carried out a comprehensive search for studies up to May 2017.
Key results
We found three randomised controlled trials (clinical trials where people are randomly put into one of two or more treatment groups) conducted in 1054 children in high‐income (wealthy) countries, that compared children who consumed a lower total fat intake (30% or less of their total daily energy) to children who consumed a usual or modified fat intake (more than 30% of their total daily energy) for between one and seven years. Some of these results showed that a lower fat intake may reduce body mass index (BMI; a measure of body fatness based on height and weight) and the blood levels of different types of cholesterol (a fat carried in the blood) when compared to a higher fat intake. However, these effects varied over time with some results showing that a lower fat intake may make little or no difference. Evidence from one trial suggested that lower fat intake probably had no effect on blood levels of one type of cholesterol (called HDL‐cholesterol) and may have no effect on height compared to higher fat intakes. This evidence cannot necessarily be applied to all healthy children, as two studies were done in children with raised blood cholesterol levels.
We also looked at 21 studies in approximately 25,059 children that observed and measured the children's intake of fat and their weight, BMI, and other body measures over time (these are called cohort studies). Over half of these cohort studies that reported on body fatness suggested that as total fat intake increases, body fatness may move in the same direction. However, results varied across all these studies and we could not draw any firm conclusions.
Quality of the evidence
We found no high‐quality evidence with which to answer this question. Evidence from the cohort studies was generally of very low quality so we are uncertain about these results and cannot draw conclusions. For the three randomised controlled trials, the results that we were most interested in were generally of moderate‐ or low‐quality evidence. We could not make any conclusions about children in low‐ and middle‐income countries as 23 of the 24 studies were done in high‐income countries. More high‐quality, long‐term studies are required that also include children from low‐ and middle‐income settings.
Authors' conclusions
Summary of findings
| Total fat intake ≤ 30% of total energy compared to usual fat intake for bodyweight in children (RCTs) A comprehensive table including data for all time points for each outcome can be found in Appendix 2 | |||||
| Patient or population: boys and girls aged 24 months to 18 years Setting: paediatric practices, schools and health maintenance organisations in high‐income countries Intervention: lower total fat intake ≤ 30%TE Comparison: usual or modified fat intake | |||||
| Outcomes (at time point ranges where data were reported) | No of participants (No of studies) | Illustrated comparative effect (95% CI) | Quality | What happens | |
| Usual fat intake1 | Effect difference with total fat ≤ 30% of total energy2 | ||||
| Weight‐for‐age z‐score Follow‐up: range 6 to 12 months | 151 (1 RCT) | The mean weight‐for‐age z‐score in control group was 0.29 | MD 0.18 lower | ⊕⊝⊝⊝ | We were uncertain whether lower total fat intake (≤ 30%TE) had an effect on weight‐for‐age in children over a 12‐month period (1 study). |
| Weight (kg) | 620 (1 RCT) | The mean weight (kg) in control group was 38.2 | MD 0.5 lower | ⊕⊕⊝⊝ | Lower total fat intake (≤ 30%TE) may have made little or no difference to weight in children over a 5‐year period (1 study). |
| Follow‐up: range 2 to 5 years | 612 (1 RCT) | The mean weight (kg) in control group was 49.5 | MD 0.6 lower | ⊕⊕⊝⊝ | |
| BMI (kg/m2) | 620 (1 RCT) | The mean BMI (kg/m2) in control group was 18.5 | MD 0.3 lower | ⊕⊕⊝⊝ | Lower total fat intake (≤ 30%TE) may have made little or no difference to BMI in children over a 1‐year period (1 study). |
| Follow‐up: range 1 to 2 years | 191 (1 RCT) | The mean BMI (kg/m2) in control group was 24.8 | MD 1.5 lower | ⊕⊕⊕⊝ | Lower total fat intake (≤ 30%TE) probably reduced BMI in children over a period of 1 to 2 years (1 study). |
| Follow‐up: range 2 to 5 years | 541 (1 RCT) | The mean BMI (kg/m2) in control group was 21.7 | MD 0 | ⊕⊕⊝⊝ | Lower total fat intake (≤ 30%TE) may have made little or no difference to BMI in children over a 2 to 5‐year period and > 5‐years (1 study). Please see Appendix 2 for Data for > 5 years. |
| Total cholesterol (mmol/L) | 618 (1 RCT) | The mean total cholesterol (mmol/L) in control group was 5.1 | MD 0.15 lower | ⊕⊕⊕⊝ | Total fat intake ≤ 30%TE probably slightly reduced total cholesterol in children over a 12‐month period (1 study). |
| Follow‐up: range 2 to 5 years | 522 (1 RCT) | The mean total cholesterol (mmol/L) in control group was 4.6 | MD 0.06 lower | ⊕⊕⊝⊝ | Lower total fat intake (≤ 30%TE) may have made little or no difference to total cholesterol in children over a 2 to 5‐year period and > 5‐years (1 study). Please see Appendix 2 for Data for > 5 years. |
| LDL‐C (mmol/L) | 618 (1 RCT) | The mean LDL‐C (mmol/L) in control group was 3.29 | MD 0.12 lower | ⊕⊕⊕⊝ | Lower total fat intake (≤ 30%TE) probably reduced LDL‐C in children over a 12‐month period (1 study) and over a 2 to 5‐year period (1 study). Please see Appendix 2 for Data for > 5 years. |
| Follow‐up: range 2 to 5 years | 623 (1 RCT) | The mean LDL‐C (mmol/L) in control group was 3.07 | MD 0.09 lower | ⊕⊕⊕⊝ | |
| HDL‐C (mmol/L) | 618 (1 RCT) | The mean HDL‐C (mmol/L) in control group was 1.47 | MD 0.03 lower | ⊕⊕⊕⊝ | Lower total fat intake (≤ 30%TE) probably made little or no difference to HDL‐C in children over a 6 to 12‐month period (1 study) and over a 2 to 5‐year period (1 study). Please see Appendix 2 for Data for > 5 years. |
| Follow‐up: range 2 to 5 years | 522 (1 RCT) | The mean HDL‐C (mmol/L) in control group was 1.32 | MD 0.01 lower | ⊕⊕⊕⊝ | |
| Triglycerides (mmol/L) | 618 (1 RCT) | The mean triglycerides (mmol/L) in control group was 0.98 | MD 0.01 lower | ⊕⊕⊕⊝ | Lower total fat intake (≤ 30%TE) probably made little or no difference to triglycerides in children over a 6 to 12‐month period (1 study). Please see Appendix 2 for Data for > 2 years. |
| Height‐for‐age z‐score Follow‐up: range 6 to 12 months | 151 (1 RCT) | The mean height‐for‐age z‐score in control group was 0.05 | MD 0.05 lower | ⊕⊝⊝⊝ | We were uncertain whether lower total fat intake (≤ 30%TE) reduced height‐for‐age in children over a 12‐month period (1 study). |
| Height (cm) | 642 (1 RCT) | The mean height (cm) in control group was 143.1 | MD 0 | ⊕⊕⊝⊝ | Lower total fat intake (≤ 30%TE) may have made little or no difference to height in children over a period > 5 years (1 study). |
| Follow‐up: range 2 to 5 years | 540 (1 RCT) | The mean height (cm) in control group was 167.4 | MD 0.10 lower | ⊕⊕⊝⊝ | |
| %TE: percentage of total energy; BMI: body mass index; CI: confidence interval; HDL‐C: high‐density lipoprotein cholesterol; LDL‐C: low‐density lipoprotein cholesterol; MD: mean difference; RCT: randomised controlled trial. aNotes: For all outcomes, there were too few studies to assess publication bias. | |||||
| GRADE Working Group grades of evidence | |||||
| 1Mean change observed between baseline and follow‐up in the control group. 2Difference in intervention group (and its 95% confidence interval) was based on the assumed change in the comparison group (and its 95% confidence interval). 3Downgraded by 1 for risk of bias: unclear risk of bias across all domains. 4Only 1 study for this outcome, therefore we could not rate for inconsistency. 5Downgraded by 1 for indirectness: participants were children with raised blood lipids, thus results may not be directly generalisable to all children. 6Downgraded by 1 for imprecision: small sample size and confidence interval included no effect and important benefit or harm. 7Not downgraded for serious risk of bias; a well‐conducted trial (methods in place to minimise risk of selection, performance, detection, attrition and reporting bias). 8Downgraded by 1 for imprecision: confidence interval included no effect and important benefit or harm. 9Downgraded by 1 for risk of bias: allocation concealment not reported. 10Not downgraded for serious imprecision: both bounds of the confidence interval indicate benefit, and calculated optimal information size met (158 patients are required to have a 80% chance of detecting, as significant at the 5% level, an important decrease in BMI of 1.7 kg/m2 (the average of the change across the 50th to 97th percentiles in 12.5 year‐olds, as per BMI‐for‐age tables, Centers of Disease Control & Prevention, 2000). 11Not downgraded for serious imprecision: both bounds of the confidence interval indicate benefit. 12Not downgraded for serious imprecision: precise estimate of no effect. 13Downgraded by 1 for imprecision: small sample size (optimal information size not met). | |||||
| Total fat intake and bodyweightin children (cohort studies) A comprehensive table including data for all time points for each outcome can be found in Appendix 3 | ||||
| Patient or population: boys and girls aged 24 months to 18 years Setting: communities, schools, households, healthcare centres in high‐income countries Exposure: total fat intake | ||||
| Outcomes | No of studies (No of participants) | Impact | Quality | What happens |
| Weight (kg) Follow‐up: 2 to 5 years | 4 cohort studies (13,802) | 2 studies that adjusted for TE intake: After 3 years, "Dairy fat was not a stronger predictor of weight gain than other types of fat, and no fat (dairy, vegetable, or other) intake was significantly associated with weight gain after energy adjustment, nor was total fat intake;" no numerical results reported. After 3 years, for every 1% increase in TE intake from total fat of children, weight will decrease by 0.0011 kg. 2 studies that did not adjust for TE intake: After 4 years, weight of children with low‐fat intake (< 30%TE) will increase by 8.1 kg on average, and by 8.9 kg on average in children with high‐fat intake (> 35%TE). After 2 years, children with low‐fat intake (≤ 30%TE) will gain on average 0.2 kg per year more than children with high‐fat intakes (> 30%TE) | ⊕⊝⊝⊝ | When adjusted for TE, we were uncertain whether fat intake was associated with weight in children over 2 to 5 years. When not adjusted for TE, we were uncertain whether lower fat was associated with weight in children over 2 to 5 years. |
| Follow‐up: 5 to 10 years | 1 cohort study (126) | 1 study that did not adjust for TE intake: After 6 years, weight of children with low‐fat intake (< 30%TE) will increase by 16.8 kg on average, and by 13.9 kg on average in children with high‐fat intake (> 35%TE) | ⊕⊝⊝⊝ | We were uncertain whether fat intake was associated with weight over 5 to 10 years (1 study). |
| BMI (kg/m2, kg/m2 per year, z‐score, percentile) Follow‐up: 2 to 5 years | 7 cohort studies (3143) | 4 studies that adjusted for TE intake: After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.63 z‐score in boys but increase by 0.07 z‐score in girls. "Dietary factors were not associated with BMI across the three study years." After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.00008 kg/m2. After 4 years, increase in the total fat intake, will increase BMI by 0.087 z‐score. The model explained 48% of variance in the change of BMI z‐score. 2 studies that did not adjust for TE intake: After 2.08 years, low‐fat intake (≤ 30%TE) will result in a 0.02 kg/m2 per year greater increase in BMI on average, compared to high‐fat intake (> 30%TE). After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.01 percentile in girls. 1 study where TE adjustment was not applicable, as TE was part of exposure: After 3 years, for every 1 z‐score increase in the energy‐dense, high‐fat and low‐fibre dietary pattern, BMI will increase by 0.03 z‐score in boys and by 0.99 z‐score in girls. After 3 years, the ratio of odds for being overweight/obese was 1.04 greater in boys and 1.02 greater in girls with higher dietary pattern z‐scores, compared to the odds in boys and girls with lower dietary pattern z‐scores. | ⊕⊝⊝⊝ Very low6,7,8 | We were uncertain whether fat intake was associated with BMI in children over 2 to 10 years. |
| Follow‐up: 5 to 10 years | 4 cohort studies (1158) | 3 studies that adjusted for TE intake: After 6 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.011 z‐score in boys but increase by 0.005 z‐score in girls. After 9 years, increase in the total fat intake will increase BMI by 0.122 z‐score. After 10 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.029 kg/m2 in white girls and by 0.012 kg/m2 in black girls. 1 study that did not adjust for TE intake: After 6 years, for every 1 g increases in the fat intake, BMI will increase by 0.01 kg/m2 | ⊕⊝⊝⊝ | |
| LDL‐C (mmol/L) Follow‐up: 2 to 5 years | 1 cohort study (1163) | 1 study where TE adjustment not applicable, as TE was part of exposure: After 3 years, for every 1 z‐score increase in the energy‐dense, high‐fat and low‐fibre dietary pattern, LDL‐C will increase by 0.001 mmol/L in boys and 0.04 mmol/L in girls | ⊕⊝⊝⊝ | We were uncertain whether fat intake was associated with LDL‐C in children over 2 to 5 years (1 study). |
| HDL‐C (mmol/L) Follow‐up: 2 to 5 years | 2 cohort studies (1393) | 1 study that adjusted for TE intake: After 3 years, for every 1% increase in energy intake from total fat, HDL‐C will decrease by 0.21 mmol/L in girls. 1 study where TE adjustment not applicable, as TE was part of exposure: After 3 years, for every 1 z‐score increase in the energy‐dense, high‐fat and low‐fibre dietary pattern, HDL‐C will decrease by 0.002 mmol/L in boys but increase by 0.02 mmol/L in girls. | ⊕⊕⊝⊝ | When adjusted for TE, fat intake may be inversely associated with HDL‐C in girls over 2 to 5 years (1 study). When not adjusted for TE, fat intake may make little or no difference to HDL‐C in girls over 2 to 5 years (1 study). |
| Triglycerides (mmol/L) Follow‐up: 2 to 5 years | 1 cohort study (1163) | 1 study where TE adjustment not applicable, as TE was part of exposure: After 3 years, for every 1 z‐score increase in the energy‐dense, high‐fat and low‐fibre dietary pattern, triglycerides will increase by 1% in either boys or girls. | ⊕⊝⊝⊝ | We were uncertain whether fat intake was associated with triglycerides in children over 2 to 5 years (1 study). |
| Height (cm) Follow‐up: 2 to 5 years | 3 cohort studies (973) | 1 study that adjusted for TE intake: After 3 years, for every 1% increase in energy intake from fat, height in children will decrease by 0.0009 cm on average. 2 studies that did not adjust for TE intake: After 2 years, low‐fat intake (≤ 30%TE) will result in a 0.2 cm per year greater increase in height on average compared to high‐fat intake (> 30%TE). After 4 years, on average children in low‐fat intake (< 30%TE) gain 27.9 cm in height, while children in high‐fat intake (> 35%TE) gain 28.3 cm in height. | ⊕⊝⊝⊝ | We were uncertain whether fat intake was associated with height in children over 2 to 10 years. |
| Follow‐up: 5 to 10 years Age at baseline: 2 years | 1 cohort study (126) | 1 study that did not adjust for TE intake: At 6 years, on average children in low‐fat intake (< 30%TE) gain 44.9 cm in height while children in high‐fat intake (> 35%TE) gain 40.3 cm in height. | ⊕⊝⊝⊝ | |
| BMI: body mass index; HDL‐C: high‐density lipoprotein cholesterol; LDL‐C: low‐density lipoprotein cholesterol; MD: mean difference; TE: total energy. aNotes: Some cohort studies reported more than one eligible analysis for the same outcome (e.g. BMI as continuous or binary outcome) or different measures of exposure (e.g. fat intake as continuous %TE or as binary classification of less‐exposed vs more‐exposed). In these cases, we selected outcomes and exposure measures so as not to use the same study sample of participants more than once per outcome and time point range in the table. For all outcomes, there were too few studies to assess publication bias. | ||||
| GRADE Working Group grades of evidence | ||||
| 1Although, risk of bias was concerning (studies with strong contributions did not adjust for all important prognostic variables), plausible residual confounding would likely reduce the demonstrated effect in the studies that did not adjust for total energy intake; thus we chose not to downgrade for risk of bias. 2Downgraded by 1 for imprecision: in studies reporting variance, the variance included no effect and important benefit or harm. 3Although risk of selection bias (no matching of exposed and non‐exposed groups, or statistical adjustments) and attrition bias (> 50% attrition) was concerning, plausible residual confounding would likely reduce the demonstrated effect as this study did not adjust for total energy; thus we chose not to downgrade for selection bias. 4Only 1 study for this outcome, therefore we could not rate for inconsistency. 5Downgraded by 1 for indirectness: a single study in a high‐income country likely has limited generalisability. 6Imprecision was considered, but we considered a decision would not impact on the rating and thus no judgement was made for imprecision. 7Downgraded by 1 for risk of bias: risk of selection bias: 5 studies did not match exposed and non‐exposed groups or make important statistical adjustments; high risk of detection bias: dietary assessment for 3 studies were not adequately rigorous. 8Downgraded by 1 for inconsistency: some studies reported small to large positive associations between exposure and outcome, while others reported no association or a small to medium inverse association between exposure and outcome. 9Downgraded by 1 for risk of bias: risk of selection bias: 2 studies with strongest contributions, did not adjust for all important prognostic variables; high risk of detection bias: dietary assessment in 1 study was not adequately rigorous. 10Downgraded by 1 for risk of bias: risk of selection bias; no matching of exposed and unexposed groups or adjustment for all important prognostic variables. 11Study was judged to have a lower overall risk of bias; attrition < 50% and satisfactory assessment of exposure. 12Not downgraded for serious imprecision as judged to be precise estimates of no effect in both studies. | ||||
Background
Description and implications of the condition
Childhood obesity is an important global public health problem. The World Health Organization (WHO) defines childhood obesity as the proportion of children with weight‐for‐height z‐score (WHZ) values greater than three standard deviations (SDs) from the WHO growth standard median (de Onis 2007), with slightly different standards being reported by other organisations such as the International Obesity Task Force (IOTF) (Cole 2000). Overweight and obesity levels among infants, children and adolescents are rising globally. The combined prevalence of overweight and obesity in children increased by 47.1% between 1980 and 2013 (Ng 2014). Overweight and obesity affects disadvantaged population groups more, and rising levels are being seen particularly in low‐ and middle‐income countries (LMICs), largely due to the rapid nutrition transition (de Onis 2010; GBD 2017a; WHO 2016). Of all children under five years of age who were overweight in 2016, 49% lived in Asia and 24% in Africa (UNICEF 2017).
Obesity has physical and psychosocial health consequences during childhood that are likely to extend into adulthood. Children who are obese are more at risk of high blood pressure and high cholesterol; impaired glucose tolerance and type 2 diabetes; asthma and musculoskeletal complications (Pollock 2015). It also increases the risk of psychosocial problems such as depression and poor socialisation (Fenner 2016; WHO 2016). Beyond its consequences in children, childhood obesity is an independent risk factor for adult obesity, with the associated health and economic implications for individuals as well as societies (WHO 2016). Overweight and obesity in adulthood are associated with increased risks of many cancers, coronary heart disease and stroke, and were among the top risk factors contributing to disability‐adjusted life years in 2015 (GBD 2017b).
Given the rising global burden of childhood obesity and its far‐reaching consequences, prevention, by addressing modifiable risk factors, is one of the most important actions. Obesity develops from sustained positive energy balance linked to various genetic, biological, behavioural, environmental and socioeconomic factors (Lobstein 2004; WHO 2016). Ethnicity has been linked to risk of obesity, with non‐white ethnicities living in westernised countries being at greater risk. In the USA, the prevalence of overweight among Hispanic and African‐American children rose twice as fast in a 12‐year period compared to white children (Lobstein 2004). Other factors that influence bodyweight measures in children include parental overweight or obesity, due to genetic and lifestyle influences. Lower socioeconomic status is also associated with higher bodyweight (Lobstein 2004; Ng 2014). There are greater absolute numbers of overweight and obese children in LMICs (Ng 2014). In high‐income countries, obesity risk is greater among populations of lower socioeconomic status whereas in developing countries it is more prevalent among wealthier populations (Lobstein 2004; Ng 2014). Rising levels of obesity are also seen among urban populations in developing countries due to westernised diets and the nutrition transition. This association between socioeconomic status and obesity risk is independent of the association between lower education levels and higher bodyweight measures (Lobstein 2004). Markers of maturation, such as age at menarche, stage of puberty or peak height velocity also influence body fatness, with children who mature more rapidly or earlier being at greater risk of obesity (Parsons 1999). Insufficient physical activity and excessive inactivity (e.g. television viewing) are also associated with risk of obesity (LeBlanc 2012; WHO 2004). Dietary risk factors associated with excess weight gain include high intake of sugar‐sweetened drinks or energy‐dense, nutrient‐poor foods (WHO 2004). Among these dietary risk factors is total fat intake, which may have important effects on body fatness measures in children, with international expert panels having debated on the optimal fat intakes (WCRF/AICR 2009), and which is the subject of this review.
Description of the intervention/exposure
The intervention or exposure of interest in this review is a reduced total fat intake in healthy non‐obese children and young people. Reduced fat intake may be achieved through interventions of nutrition education (e.g. counselling), changes in the food environment, peer‐support programmes, food provision or combinations of these.
Importantly, dietary intake is challenging to measure accurately, and any single common method used (such as the 24‐hour dietary recall, dietary record (DR), dietary history, and Food Frequency Questionnaire (FFQ)) provides subjective estimates, with strengths and limitations related to validity (Shim 2014). Although it is well known that the research objective, hypothesis, design, and available resources need to be carefully considered to select the most appropriate dietary assessment method (Shim 2014), the fidelity of application of dietary assessment methods varies widely across research studies, and adherence to nutrition counselling by study participants also varies widely. These factors may introduce a lot of variation into the relationship between estimates of total fat intake and body fatness measures, which is often difficult to quantify accurately and leads to disparate findings and distortion in the estimated measure of association across studies. Additionally, studies usually quantify total fat intake in absolute grams per day, as a percentage of total energy (%TE) intake or both. These different measures are then used in various ways across studies in data analyses, which may add to the heterogeneity in effects and associations being examined. Studies have shown positive associations between proportion of energy intake as fat and bodyweight measures in children, with less clear associations in longitudinal compared to cross‐sectional studies (Johnson 2008; Lobstein 2004; McGloin 2002; Pérez‐Escamilla 2012). A meta‐regression in a systematic review of randomised controlled trials (RCTs) on the effects of step I and II diets of the National Heart, Lung and Blood Institute national cholesterol education programme to reduce the risk of cardiovascular disease in the general population and those at increased cardiovascular risk, respectively, found a strong relation between total fat intake and bodyweight (Yu‐Poth 1999). The German Nutrition Society guidelines state that whereas intervention and cohort studies in adults that have adjusted for energy intake show a probable lack of association between fat intake and risk of obesity, other studies that have not adjusted for energy intake, show a probable association between total fat intake and risk of obesity (Wolfram 2015).
Fat and energy intake can influence body fatness, and fat intake closely correlates with energy intake, which makes it difficult to separate their individual effects on bodyweight (Wolfram 2015). Change in body fatness that occurs with modifying intakes of total fat are mediated via changes in energy intakes. Additionally, differences in total energy intake can result in extraneous variation in nutrient intake because of individual differences in body size, physical activity and metabolic efficiency. Thus, to distinguish the isolated effect of fat intake on bodyweight, the effect of energy intake needs to be adjusted for in analyses (Jakes 2004; Rhee 2014). In observational studies, statistical models that adjust for prognostic variables, such as energy intake, attempt to simulate the comparability of randomised groups in an intervention study (Wolfram 2015). Similarly, in intervention studies where energy intake is ad libitum, it can confound the association between fat intake and weight gain, and isocaloric comparisons can be simulated through statistical modelling, controlling for the effect of energy intake.
Successfully isolating the effect of a single nutrient, such as fat, on weight is challenging given the complex mixture of nutrients and other components that make up our diets, typically characterised by various dietary patterns (different quantities, proportions, variety, and combinations of different foods and beverages) consumed over time. The nutrients provided by dietary patterns also have synergistic, additive or antagonistic effects on health. One review in Asian children on the relationship between dietary patterns as the exposure variable and childhood overweight and obesity as the outcome reported several meaningful, yet inconsistent, associations between dietary patterns and childhood overweight/obesity in children and adolescents, and heterogeneity of studies in terms of measures of dietary patterns and obesity standards (Yang 2012). Thus, carefully considering the way in which diets differ in components other than only total fat is part of better understanding the relationship between fat intake, weight and other health outcomes.
Another factor that can influence observable effects of total fat intake on bodyweight measures is the time‐varying nature of this relationship. Studies have different periods of observation and follow‐up, and different frequencies or intervals of study contacts and measurement. The duration of lower fat intake interventions or the duration of the exposure to lower total fat intake influence potential changes in bodyweight outcomes. It is thus important to consider this factor when examining the relationship between fat intake and weight, particularly in prospective cohort studies and the often secular nature of their data.
Why is it important to do this review?
Existing reviews looking at low‐fat diets included studies where weight loss was a goal of the intervention (Yu‐Poth 1999), which may have overstated any relation because the advice was to lower both fat and energy intake, did not explore the effect of low‐fat diets on weight or other body fatness outcomes (Schwingshackl 2013a), or looked at low‐fat intake as part of a wider health promotion intervention (Ni 2010). Other reviews that assessed body fatness were either limited to the effect of low‐fat dairy versus high‐fat dairy consumption (Benatar 2013), or investigated it as part of looking at overall dietary patterns (Ambrosini 2014), or diet quality (Aljadani 2015).
To examine these issues, a Cochrane Review including RCTs and cohort studies in adults and children was updated in 2015 (Hooper 2015a). With the aim of ensuring all relevant data in children were summarised, the WHO commissioned an expedited update of this systematic review in children only, to aid the understanding of the relation between total fat intake and bodyweight in children, in studies not intending to induce weight loss, with a view to inform the updating of their guidelines on total fat intake. Therefore, the combined review in children and adults (Hooper 2015a) was split into two reviews with the titles, "Effects of total fat intake on bodyweight in adults;" (in preparation) and "Effects of total fat intake on bodyweight in children." The 2015 combined (adults and children) review will be withdrawn with notes to direct readers to the two separate reviews.
Objectives
To assess the effects of total fat intake on measures of weight and body fatness in children and young people not aiming to lose weight.
Methods
Criteria for considering studies for this review
Types of studies
RCTs of children and young people: trials of lower fat intake compared with usual diet or modified fat intake, with no intention to reduce weight (in any groups), continued for at least six months, unconfounded by non‐nutritional interventions and assessing a measure of body fatness at least six months after the intervention was initiated.
We included studies that randomised participants (i.e. parallel‐group design), and cluster randomised trials where at least six groups of children (i.e. clusters) were randomised. We had intended to exclude cross‐over trials (as previous weight gain or weight loss is likely to affect future weight trends) unless the first half of the cross‐over could be used independently, but we did not find any eligible cross‐over trials.
Cohort studies of children and young people: analytical prospective cohort studies that followed participants for at least 12 months after baseline assessment of total fat intake, and related baseline total fat intake to absolute or change in body fatness at least 12 months later. Cohort studies using explanatory models were included, but those that used baseline data to predict later body fatness without empirical data from the later time point (predictive models) were excluded.
Considering the research focus on identifying weight management strategies in overweight and obese children, and the nature of our question that addresses an intervention, we anticipated not finding many longer‐term trials in children not intending to manage weight, and therefore also included cohort studies. Additionally, decision‐makers are required to identify and use the best available evidence in formulating recommendations, and this generally translates into evidence that is of the highest quality as assessed by GRADE, for each important outcome. The fact that we did not know a priori what type of evidence (i.e. from RCTs or observational studies) would be of highest quality was a further rationale for including prospective cohort studies.
Types of participants
We included studies in children and young people (aged 24 months to 18 years) with or without risk factors for cardiovascular disease, for example, a family history of cardiovascular disease, raised blood pressure or raised lipid levels. Participants could be of either sex, but we excluded children who were acutely ill, as well as disease‐ or condition‐specific populations, such as children with cystic fibrosis, autism or diabetes. We excluded intervention studies where the selection of the participants was primarily for raised weight or body mass index (BMI) with the intention to reduce weight.
Studies including a subset of eligible participants (e.g. aged 15 to 24 years) were included if results were reported separately for the eligible subset (e.g. 15 to 18 years). If not, such studies were only included if more than 80% of the baseline sample were aged 24 months to 18 years. We intended to exclude data from these studies in sensitivity analyses to test the robustness of the primary meta‐analyses, but we did not pool data. Birth cohorts were only included if baseline total fat intake was related to absolute or change in body fatness at least 12 months later, and both these time points fell within our eligible age range, in which the earlier time point was regarded as the baseline.
Types of interventions
Interventions
We considered all RCTs of interventions stating an intention to reduce total dietary fat intake (by provision of nutrition education in any form, foods or both), when compared with a usual or modified fat intake.
We considered a lower fat intake to be one where fat intake was 30% or less of total energy (30%TE or less), and energy lost was at least partially replaced with carbohydrates (simple or complex), protein, or fruit and vegetables. We considered a 'usual' fat diet to be one with total fat intake greater than 30%TE, and considered a modified fat diet to be one with greater than 30%TE from fats, and that included higher levels of monounsaturated or polyunsaturated fats than a 'usual' fat diet. Interventions consisting of meals or food items lower in fat were included if they were provided with the intention of reducing fat intake over a period, thus targeting total fat intake.
As we were interested in the effects of total fat intake on bodyweight and fatness in everyday dietary intake over time (rather than in those aiming to reduce their bodyweight in weight‐reducing diets), we excluded studies aiming primarily to reduce the weight of some or all participants, as well as those that included only participants who had recently lost weight, or recruited participants primarily according to a raised bodyweight or BMI.
We excluded multifactorial interventions other than diet or supplementation, unless the effects of diet or supplementation could be separated such that the additional intervention was consistent between the intervention and control groups (e.g. studies that reduced fat and encouraged physical activity in one group and compared this with encouraging physical activity in the control group were included; studies that reduced fat and encouraged physical activity in one group and compared this with no interventions in the control group were excluded; studies that reduced fat and encouraged fruit and vegetables in one group and compared this with no intervention in the control group were included). Studies that selected groups based on a possible prognostic variable other than total fat intake, for example, genotype, were excluded.
We excluded Atkins‐type diets aiming to increase protein and fat intake, as well as studies where fat was reduced by means of a fat substitute (such as Olestra). We excluded studies that included enteral and parenteral feeding, as well as nutritional formula‐based weight‐reducing or other weight‐reducing diets.
Thus, we included all trials that intended to reduce dietary fat to 30%TE or less in one group compared to usual or modified fat intake (greater than 30%TE from fat) in another group regardless of the degree of difference between fat intake in the two groups (i.e. 'dose difference'). We intended to explore the effects of the difference in %TE from fat between control and intervention groups, as well as the effects of fat intake in the control groups and adherence to dietary fat goals in the intervention groups in subgroup analyses, but data did not allow us to perform these.
Exposures
For analytical prospective cohort studies, total dietary fat intake, in grams, as a percentage of total dietary energy intake or as one of the defining characteristics of a dietary pattern, had to be assessed at baseline and related to a measure of body fatness, or change in body fatness, at least one year later.
Types of outcome measures
Primary outcomes
-
Body fatness, including bodyweight (kg), BMI (kg/m2), waist circumference (cm), skinfold thickness (mm) and percentage body fat.
Secondary outcomes
-
Other routine cardiovascular risk factors, namely circulating total low‐density lipoprotein (LDL) and high‐density lipoprotein (HDL) cholesterol and triglyceride concentrations, and systolic (SBP) and diastolic blood pressure (SBP).
-
Height (adverse outcome). It is plausible that reducing total fat intake would reduce total energy and nutrient intake in children, possibly increasing the risk for suboptimal statural growth.
Tertiary outcomes (randomised controlled trials only)
-
Process outcomes, including changes in saturated and total fat intakes, as well as other macronutrients.
This is not a systematic review of the effects of lower fat on these secondary or tertiary outcomes, but we collated the outcomes from included studies to understand whether any effects on weight or body fatness might have been influenced by changes in these outcomes.
Search methods for identification of studies
Electronic searches
For this update in children only, we developed a new search strategy, which was run in the Cochrane library (May 2017, Issue 5) and in MEDLINE (Ovid, 1946 to May 2017), MEDLINE (PubMed, 1946 to May 2017) and Embase (Ovid, 1947 to May 2017) (Appendix 1). We searched comprehensively for all eligible studies, regardless of language and publication status.
Searching other resources
The previous authors (Hooper 2015a) searched the bibliographies of all identified systematic reviews for further trials and cohort studies, including Ajala 2013; Aljadani 2013; Aljadani 2015; Ambrosini 2014; Benatar 2013; Chaput 2014; Gow 2014; Havranek 2011; Hu 2012; Kratz 2013; Ni 2010; Schwingshackl 2013a; Schwingshackl 2013b; and Yang 2013. We searched the bibliographies of all included RCTs in this update. We also searched the tables of included and excluded studies in children in the previous version of this review that included both adults and children (Hooper 2015b).
To identify ongoing and unpublished studies, we searched the WHO International Clinical Trials Registry Platform (inception to 5 June 2017; WHO ICTRP, apps.who.int/trialsearch/) and ClinicalTrials.gov (inception to 5 June 2017; www.clinicaltrials.gov) (5 June 2017) (Appendix 1).
Data collection and analysis
This update was prepared in Review Manager 5 (RevMan 2014).
Selection of studies
One review author (CN) conducted an initial title screen using keywords to remove records that were obviously irrelevant. Keywords used for the title screen included words indicative of animal studies (e.g. 'murine'), ineligible participants (e.g. 'cystic fibrosis,' 'autism,' 'anorexia nervosa') and ineligible interventions (e.g. 'ketogenic,' 'parenteral,' 'olestra'). For quality assurance purposes, a second review author (MV) screened a random selection of 10% of the removed records, yielding a 98% inter‐rater agreement. Thereafter, two review authors independently screened all remaining titles and abstracts using Covidence (Covidence). We obtained the full‐text articles of records identified as potentially eligible, and screened these in duplicate and independently to determine final eligibility. When an abstract could not be rejected with certainty, we obtained the full text of the article for further evaluation. We were careful not to exclude studies based on outcome reporting. We did this by examining the objectives and methods of the study and deciding whether our eligible outcomes were likely to be within the scope of the study (i.e. considering whether one would expect them to be reported in the particular study, or they were measured and results were not reported). We only excluded studies when none of our eligible outcomes were reported and we judged that our eligible outcomes were outside of the scope of the study. We resolved any disagreements through discussion and consultation with two other review authors (CN or AS) when necessary.
Data extraction and management
We extracted data concerning participants, interventions or exposures, controls and outcomes, and trial or cohort quality characteristics onto forms designed and piloted for the review. We extracted data on potential effect modifiers from RCTs (including duration of intervention, control group fat intake, sex, year of first publication, difference in %TE from fat between the intervention and control groups, type of intervention (food or nutrition education provided), the dietary fat goals set for each group, baseline BMI and health at baseline), and from cohort studies (age, sex, energy intake, ethnicity, parental BMI, physical activity (or screen time, or both), pubertal stage and socioeconomic (income and educational) status). Where provided, we collected data on risk factors for cardiovascular disease (secondary and tertiary outcomes). When assessment of fat intake was reported using more than one dietary assessment method for the same outcome in the same participants, we selected the method deemed to be most appropriate and valid (e.g. multiple applications over time were better than a single once‐off application), or most likely to be relevant to answering our question. If different methods were judged to have similar validity, we used multiple food frequencies preferentially, as these were more likely to represent usual dietary intake (Gibson 2005).
We extracted outcome data according to the following time point ranges, when available: RCTs: from baseline to six months, six to 12 months, one to two years, two to five years and more than five years; cohort studies: baseline to one year, one to two years, two to five years, five to 10 years and more than 10 years. When outcome data were reported at more than one point within our time point ranges (e.g. three and five years), we extracted data from the latest point available within each range (five years in this example), unless the data from this time point were judged to be less reliable than the data from the earlier time point, in which case we used the more reliable data with an explanation.
All trial outcomes were continuous and where possible in trials, we extracted change data (change in the outcome from baseline to outcome assessment) with relevant data on variance for intervention and control groups (along with numbers of participants at that time point). Where change data were not available, we extracted data at study end (or other relevant time point) along with the variance and numbers of participants for each group. In the cohort studies, we extracted the most adjusted odds ratio, risk ratio, mean change or mean end values per group, when comparing the most exposed group of participants (highest fat intake) with the least exposed group (lowest fat intake). The most adjusted regression outputs (e.g. beta coefficient and its variance, P value, T value) were extracted when total dietary fat intake was assessed at baseline and related to a measure of body fatness, or change in body fatness, at least one year later. Two review authors extracted all data independently, with discrepancies resolved by another review author.
Assessment of risk of bias in included studies
We carried out 'Risk of bias' assessments independently and in duplicate. We assessed risk of bias in RCTs using the Cochrane tool for assessment of risk of bias (Higgins 2011a). For included RCTs, we also assessed whether trials were free of differences in diet (between intervention and control groups) other than dietary fat intake, as this may also influence differences in weight, body fatness and other related outcomes. We used the category 'other bias' for this assessment, and also to note any further issues of methodological concern.
For cohort studies we assessed the following.
-
Was adequate outcome data available?
-
Was there matching of less‐exposed and more‐exposed participants for prognostic factors associated with outcome, or were relevant statistical adjustments done?
-
Did the exposures between groups differ in components other than only total fat?
-
Could we be confident in the assessment of outcomes?
-
Could we be confident in the assessment of exposure?
-
Could we be confident in the assessment of presence or absence of prognostic factors?
-
Was selection of less‐exposed and more‐exposed groups from the same population? (Cochrane Methods; Guyatt 2011).
Measures of treatment effect
The effect measure of choice for continuous outcomes was the mean difference (MD). Where data allowed, we presented the MD alongside its 95% confidence interval (CI).
Unit of analysis issues
We found no cluster‐randomised or cross‐over trials. Where there was more than one intervention and control group, we selected the most relevant intervention group and most relevant control group for this review. We excluded intervention groups that were not appropriate for this review, or less appropriate than another group.
When primary outcomes were assessed at more than one time point in our time point ranges, we used the data from the latest time point available (in participants in the eligible age range) in general analyses. We also intended to use this data in relevant subgroup analyses, but we could not perform meta‐analyses as the data did not allow this. We were careful not to present the same study sample of participants more than once per outcome and time point range (e.g. summary of findings Table 2), unless the different analyses were from the same study sample were clearly referenced (e.g. Tables 6 to 15).
Dealing with missing data
Where study authors had not reported all relevant statistics per outcome (e.g. SD of change per group for continuous data), we attempted to calculate or estimate the required data from other statistics reported in the study by using relevant formulas from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). If we could not calculate or estimate these statistics with reasonable confidence, we emailed the study authors. Where we did not receive a timely response, or where we received a response for which we lacked confidence, we did not impute the missing values but instead reported the available results in a table. We indicated in the tables where we made use of unpublished data supplied to us by study authors.
Assessment of heterogeneity
We intended to examine heterogeneity per outcome and time point by visual inspection of the forest plots (i.e. we looked at physical overlap of CIs across the included studies). We intended to assess statistical heterogeneity among the intervention effects across the included studies in the meta‐analyses as follows:
-
Chi2 test for heterogeneity;
-
I2 statistic to quantify heterogeneity; and
-
Tau2 statistic to measure the extent of heterogeneity.
In meta‐analyses, we intended to consider heterogeneity as an I2 value of greater than 30% and either a Chi2 of less than 0.1 or Tau2 greater than 0. We planned to perform subgroup analyses to explore heterogeneity, but data did not allow meta‐analyses (see Subgroup analysis and investigation of heterogeneity).
Assessment of reporting biases
Where more than 10 included studies addressed a primary outcome, we intended to used funnel plots to assess the possibility of small‐study effects. For future review updates, in the case of asymmetry, we will consider various explanations such as publication bias, poor study design and the effect of study size.
Data synthesis
We sought to combine data by the inverse variance method in random‐effects meta‐analysis to assess MDs between lower and higher fat intake arms, but data did not allow for any meta‐analyses. Where possible, we converted variables to comparable units to allow pooling of data if appropriate. We planned to conduct separate meta‐analyses of data from RCTs and data from cohort studies, and only where data from separate studies were similar enough to be combined (see Assessment of heterogeneity).
We intended not to use end data in meta‐analysis, where the difference between the intervention and control groups at baseline was greater than the change in that measure between baseline and endpoint in both groups. Instead, we intended to use change data in forest plots but without SDs, so the data did not add to the meta‐analyses but instead provided comparative information. However, this was not relevant in this update as we could not meta‐analyse the data.
'Summary of findings' tables
Based on the methods described in Chapter 11 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2011), we prepared two 'Summary of findings' tables to present the results of the RCTs and cohort studies separately. In both 'Summary of findings' tables we included our primary outcome of body fatness (measured by weight‐for‐age z‐score, weight and BMI), cardiovascular risk factors (total cholesterol, LDL, HDL and triglyceride concentrations), and height (in cm or height‐for‐age z‐score). We deemed these outcomes the most important as guided by our question and the primary purpose of the review. Given the large number of time points examined, we selected time points for inclusion in the tables by considering the influence of:
-
height gain on bodyweight change in children;
-
intervention fidelity over time in RCTs; and
-
the challenges with repeated dietary intake measurements over time in cohort studies.
Summary tables for all time points are presented in Appendix 2 (RCTs) and Appendix 3 (cohort studies).
We used the GRADE system to rank the quality of the evidence using GRADEpro GDT software (GRADEpro GDT). As data were reported heterogeneously, and meta‐analyses were not possible, we presented results in a narrative 'Summary of findings' table for cohort studies (drawing on McNeill 2017 as an example).
Subgroup analysis and investigation of heterogeneity
For this update, we classified all dietary interventions and exposures as lower fat versus usual or modified fat. We intended to compare the intervention effects or associations across the following subgroups, but the available data did not allow us to perform any of these:
-
difference in %TE from fat between lower fat and control groups in RCTs (e.g. up to 5%TE from fat, 5%TE to 10%TE from fat, 10%TE to 15%TE from fat, 15%TE or greater from fat or unknown difference);
-
type of intervention in RCTs (e.g. nutrition counselling only versus nutrition counselling plus food provided);
-
adherence to fat intake goals in the intervention group in RCTs (e.g. achieved 30%TE from fat or less versus did not achieve this);
-
weight status at baseline (e.g. by BMI‐for‐age z‐score);
-
reported estimated energy reduction in the intervention compared with the control group during the intervention period in RCTs (e.g. estimated energy intake the same or greater in the lower fat group, energy intake 1 kcal/day to 100 kcal/day lower in the lower fat group, 101 kcal/day to 200 kcal/day lower in the lower fat group, greater than 200 kcal/day lower in the lower fat group); and
-
cohort studies that statistically adjusted for energy intake when relating total fat intake to body fatness versus cohort studies that did not adjust for energy intake.
Sensitivity analysis
Where possible, we carried out sensitivity analyses for primary outcomes, assessing the effect of:
-
our selected time point ranges by including only the longest follow‐up data per study; and
-
our selected time point ranges by including only the shortest follow‐up data per study.
We had planned to perform other sensitivity analyses; however, since we only identified three RCTs and did not meta‐analyse cohort studies, we deemed other sensitivity analyses inappropriate. In future updates, it may be feasible to assess the influence of excluding studies with unclear or inadequate allocation concealment in RCTs, performing fixed‐effect meta‐analyses (rather than random‐effects) (Higgins 2011b), excluding studies with only a subset of eligible participants, excluding studies that were not free of systematic differences in care (performance bias) (or where it was unclear) and excluding studies that were not free of dietary differences other than total fat (or where it was unclear).
Results
Description of studies
The flow diagram of search results and study selection for this systematic review update is presented in Figure 1.
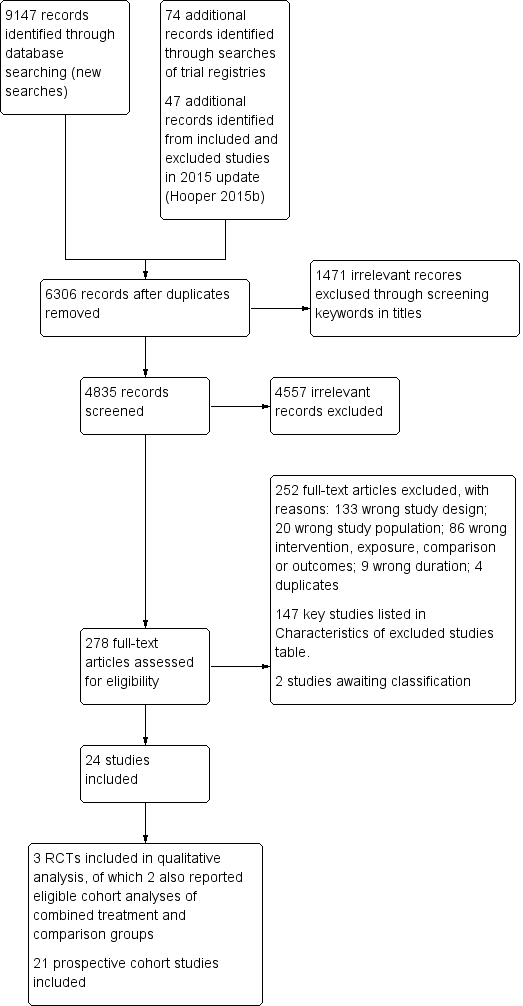
Study flow diagram. RCT: randomised controlled trial.
Results of the search
The search for RCTs and cohort studies in adults and children in a previous version of this review (Hooper 2012) identified 32,220 titles and abstracts from the electronic searches plus 28 further potential studies from other sources. For the previous update (Hooper 2015a), the electronic searches identified 7729 possible titles and abstracts, plus review authors assessed a further 24 potential studies after checking for potentially relevant trials and cohort studies included in other systematic reviews. Of these 7753 potential titles and abstracts, the review authors assessed 218 full‐text articles for eligibility (additional to the 465 assessed for the original review). This review in adults and children in 2015 included one RCT and 11 cohort studies in children (Hooper 2015b). Our flow diagram in Figure 1 does not include the search results from previous versions of this review, as they also included studies in adults and are thus not combinable with the search results for this review update.
Our new search strategy tailored for children (Appendix 1), yielded 9301 records, with 6306 records remaining following duplicate removal. After removing obviously ineligible records using a keyword search, we screened 4835 titles and abstracts, with 278 full‐texts identified as potentially eligible. After excluding 252 studies with reasons and two studies awaiting classification, we included 24 studies comprising three parallel‐group RCTs (reported in 12 records) and 21 prospective cohort studies (92 eligible analyses, reported in 47 records) (Figure 1). Two of the included RCTs (Obarzanek 2001 (RCT); Tershakovec 1998 (RCT)) also reported eligible cohort analyses that we included with the cohort data, and these are presented throughout the review as two 'additional' study references (Obarzanek 1997 (cohort); Tershakovec 1998 (cohort)).
Included studies
See Characteristics of included studies table for detailed characteristics of all included studies.
Randomised controlled trials
Study location, participants and duration
-
Mihas 2010: conducted in Greece; boys and girls aged 12 to 13 years with no known cardiovascular disease risk factors; follow‐up over 17 months.
-
Obarzanek 2001 (RCT): conducted in the USA; boys and girls aged seven to 11 years with primary elevated serum LDL‐cholesterol levels; follow‐up over approximately seven years.
-
Tershakovec 1998 (RCT): conducted in the USA; boys and girls aged four to 11 years who were hypercholesterolaemic; follow‐up over one year.
Interventions
Detailed descriptions of the interventions in the three RCTs are shown in Table 1.
| Recipients | Why | What (materials) | What (procedures) | Who provided | How and where | When and how much | Strategies to improve or maintain intervention fidelity; tailoring and modification | Extent of intervention fidelity |
| 4‐ to 9‐year‐old children with hypercholesterolaemia (plasma total cholesterol > 4.55 mmol/L, fasting plasma LDL‐C 2.77‐4.24 mmol/L for boys and 2.90‐4.24 mmol/L for girls), at ≥ 85% of ideal body weight. | Limited dietary fat was recommended for children aged > 2 years, but there were concerns that lower fat intake of children may affect their growth. Trial evaluated growth of children with hypercholesterolaemia completing an innovative, physician‐initiated, home‐based nutrition education programme or standard nutrition counselling that aimed to lower dietary fat intake. | Nutrition education programme complied with recommendations of the National Cholesterol Education Program Expert Panel on Blood Cholesterol Levels in Children and Adolescents. | Children and ≥ 1 parent (usually mother) attended 45‐ to 60‐minute counselling session with paediatric dietician. Children and parents in at‐risk control and not‐at‐risk control groups were not provided educational information or materials. | 1) Not described; 2) paediatric registered dieticians. | 1) Audiotape stories and picture books and follow‐up paper/pencil activities for children as well as manual for parents. Story and activities to be completed each week; 2) face‐to‐face individual counselling by a dietician. 1) At home; 2) paediatric practice. | 10 weeks with 1) talking‐book lesson; 2) 45‐60 minutes counselling session each week. | Not described Tailoring and modification of intervention during trial were not described. | 1) 71/88; 2) 77/86 completed intervention programmes and returned for evaluation at 3 months after baseline. |
| Prepubertal boys and girls aged 8‐11 years with LDL‐C levels ≥ 80th and < 98th percentiles for age and sex percentiles of the Lipid Research Clinics population. | Aimed to assess feasibility, safety, efficacy and acceptability of lowering dietary intake of total fat, saturated fat and cholesterol to decrease LDL‐C levels. | Intervention group received dietary counselling sessions based on National Cholesterol Education Programme guidelines: 28% of energy from total fat, < 8% from saturated fat, > 9% from polyunsaturated fat, and < 75 mg/1000 kcal of cholesterol per day, not to exceed 150 mg/day. Guidebooks including activities and recipes on diets and food recommendations given to participants and their families. | In first 6 months, 6 weekly and then 5 biweekly group sessions were led by nutritionists and behaviourists, and 2 individual visits were held with nutritionist. Over second 6 months, 4 group and 2 individual sessions were held. During 2nd and 3rd years, group and individual maintenance sessions were held 4‐6 times/year, with monthly telephone contacts between group sessions. During 4th year of follow‐up, 2 group events + 2 individual visits conducted with additional telephone contacts as appropriate. | Nutritionists and behaviourists | 1) Group sessions and 2) individual visits were held, accompanied by telephone contacts in between sessions. 1) At clinics, 2) at home | 6 weekly, 5 biweekly group sessions and 2 individual visits during first 6 months; 4 group and 2 individual sessions during second 6 months; 4‐6 maintenance sessions with telephone contacts between sessions during 2nd and 3rd years; 2 group and 2 individual sessions with telephone contacts as appropriate by 4th year. | By 4th year of follow‐up, individual visits used an individualised approach based on motivational interviewing and stage of change for increasingly busy teenagers. Tailoring and modification of intervention during trial not described. | 295/334 attended the last visit (> 5 years' follow‐up). |
| Students aged 12‐13 years from an urban area in Greece. | Aimed to evaluate the short‐term (15‐day) and long‐term (12‐month) effects of a 12‐week school‐based health and nutrition interventional programme regarding energy and nutrient intake, dietary changes and BMI. | Teaching material for teachers and workbooks for students on nutrition‐dietary habits and physical activity and health based on Social Learning Theory Model were developed and distributed to teacher and each student. | Multicomponent workbooks covering mainly dietary issues, but also dental health hygiene and consumption attitudes, were produced with each student being supplied a workbook. The class home economics teacher implemented 12‐hour‐classroom curriculum incorporating health and nutrition promotion during 12 weeks. 2 meetings were conducted with parents (given screening results of children; presentations given on dietary habits of children to improve health profile of children and prevent development of chronic diseases in the future). Cues and reinforcing messages in the form of posters and displays were provided in the classroom. | Educational intervention (classroom curriculum) delivered by class home economics teachers who were trained and supervised by health visitor or family doctor. | Classroom curriculum; cues and reinforcing messages in the form of posters and displays provided in classroom; nutrition education meetings for parents in group. At school. | 12 hours of classroom material, 2 meetings for parents during a 12‐week period. | Health visitor or family doctor supervised the programme implementation of class home economics teachers who were given 2 × 3‐hour seminars with aims to familiarise teachers about objectives of intervention and their role therein, and to increase their awareness of significance of incorporating health and nutrition in their curriculum before delivering the intervention. Tailoring and modification of intervention during trial not described. | 107/109 participation rates at 15‐days' follow‐up and 98/109 at 12 months' follow‐up. |
aTIDieR: Template for Intervention Description and Replication, template for this table from Hoffman 2017.
BMI: body mass index; LDL‐C: low‐density lipoprotein cholesterol; RCT: randomised controlled trial.
Funding and authors' declarations of interest
The older of the US trials was funded by the National Heart, Lung, and Blood Institute (HL43880‐03), the Howard Heinz Endowment, and the University of Pennsylvania Research Foundation (Tershakovec 1998 (RCT)), and the other US trial by the National Heart, Lung, and Blood Institute (Obarzanek 2001 (RCT)). There were no authors' declarations of interest reported for these trials in the articles we assessed. The trial in Greece was funded by the Ministry of Education and the National Foundation for the Youth and the authors declared no competing interests (Mihas 2010).
Prospective cohort studies
Study location, participants and duration
In most studies, children or families were recruited conveniently from schools, communities, daycare centres, clinics or hospitals, or were sampled from existing large cohort study samples. Participants in all included cohort analyses were healthy children, except for the two cohort analyses of the RCTs that included children with hypercholesteraemia (Tershakovec 1998 (cohort)) or primary elevated serum LDL‐cholesterol levels (Obarzanek 1997 (cohort)).
Mean age at baseline ranged across studies from two years to 14 years. Five studies followed children from baseline to one year (Bogaert 2003; Butte 2007; Niinikoski 1997a; Schwandt 2011; Tershakovec 1998 (cohort)), five studies for more than one to two years (Davison 2001; Klesges 1995; Lee 2001; Lee 2012; Setayeshgar 2017), seven studies for more than two to five years (Appannah 2015; Berkey 2005; Boreham 1999; Cohen 2014; Jago 2005; Obarzanek 1997 (cohort); Shea 1993), four studies for more than five to 10 years (Ambrosini 2016; Brixval 2009; Morrison 2008; Skinner 2004), and two studies followed children for more than 10 years (Alexy 2004; Magarey 2001).
Of the 21 included prospective cohort studies, one study was conducted in a middle‐income country (Korea; Lee 2012). All the others were conducted in high‐income countries, as follows: 10 in the USA (Berkey 2005; Butte 2007; Cohen 2014; Davison 2001; Jago 2005; Klesges 1995; Lee 2001; Morrison 2008; Shea 1993; Skinner 2004), one in Canada (Setayeshgar 2017), one in the UK (Ambrosini 2016), one in Northern Ireland (Boreham 1999), two in Germany (Alexy 2004; Schwandt 2011), one in Denmark (Brixval 2009), one in Finland (Niinikoski 1997a), and three in Australia (Appannah 2015; Bogaert 2003; Magarey 2001). Most studies included both sexes and all ethnicities, except one study that only included white children (Skinner 2004), one study that only included Hispanic children (Butte 2007), two studies that only included girls (Cohen 2014; Lee 2001), one study that only included white girls (Davison 2001), and one study that only included black and white girls (Morrison 2008).
Exposures
Exposures to total daily fat intake were estimated using different methods including 24‐hour dietary recall, FFQ and DRs. To examine associations with body fatness outcomes over time, total fat intake exposure estimates were expressed in different units, and applied in different ways across studies, as follows:
-
binary fat intake exposures: lower versus higher percentiles of fat intake, or lower versus higher fat intake groups (based on dietary intake assessments), and using cut‐offs of %TE from fat (e.g. 30%TE or less and greater than 30%TE or less than 30%TE and greater than 35%TE) (Alexy 2004; Ambrosini 2016; Lee 2001; Niinikoski 1997a; Shea 1993; Tershakovec 1998 (cohort);
-
continuous fat intake exposures: in %TE, absolute number of grams, per 10 grams of intake, by number of servings (Berkey 2005; Bogaert 2003; Boreham 1999; Brixval 2009; Butte 2007; Cohen 2014; Davison 2001; Jago 2005; Klesges 1995; Lee 2012; Morrison 2008; Obarzanek 1997 (cohort); Schwandt 2011; Setayeshgar 2017; Skinner 2004), or as a high‐fat dietary pattern in two studies (Ambrosini 2016; Appannah 2015), with two studies using both binary and continuous fat intake exposures to apply the exposure variables in analyses (Appannah 2015; Magarey 2001).
Figure 2 presents the spread of the different ways in which total fat intake estimates were expressed and applied to examine associations with body fatness in the 81 analyses that reported primary outcomes (weight, BMI, waist circumference, body fat and skinfold thickness) in the five time point ranges. The heterogeneous application of fat intake exposure at different time points for different outcomes across the included studies is evident in Figure 2.

The bubble‐plot presents the spread of the different ways in which total fat intake estimates were expressed and applied to examine associations with body fatness in the 81 analyses, reporting primary outcomes in the five time point ranges. Combining the many various total fat intake exposure estimates reporting on the same outcome in the same time point range was deemed inappropriate. BMI: body mass index; WC: waist circumference; yr: year.
The studies reporting dietary patterns as the exposure used reduced rank regression to identify dietary patterns or combinations of food intake, that attempted to explain the maximum variation in a set of response variables hypothesised to be on the pathway between food intake and obesity (Ambrosini 2016; Appannah 2015). Participants were scored for each dietary pattern at each age using a z‐score that quantified how their reported dietary intake reflected each dietary pattern relative to other respondents in the study sample. The model used calculates dietary z‐scores for each respondent as a linear, weighted combination of all their standardised food group intakes by using weights unique to each dietary pattern. Increasing intakes of foods with positive factor loadings increases the dietary pattern z‐score, and increasing intakes of foods with negative factor loadings decreases the dietary pattern z‐score. The energy‐dense, high‐fat, low‐fibre dietary pattern reflected high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, and fried and roasted potatoes (high intake of these foods increased the participant's dietary pattern z‐score).
Funding and authors' declarations of interest
Five of the 21 cohort studies had combined public and private funding including from the food industry and financial services industry (Berkey 2005; Bogaert 2003; Lee 2001; Niinikoski 1997a; Skinner 2004). In these studies, no author declarations of interest were reported. Two studies did not report their funding sources (Brixval 2009; Lee 2012), and in these studies, authors declared no conflicts of interests. The remaining 14 cohort studies were publicly funded, with six of these reporting no conflicts of interest by authors (Ambrosini 2016; Appannah 2015; Butte 2007; Cohen 2014; Morrison 2008; Setayeshgar 2017), and the rest containing no author declarations of interest.
Excluded studies
After full‐text screening, we excluded 252 studies. Key studies (n = 147) with their reasons for exclusion are in the Characteristics of excluded studies table. Briefly, 133 studies were excluded for inappropriate study design (98 did not analyse children's baseline to fat intake to body fatness at least 12 months later; 16 cross‐sectional; five reviews; two editorials; three analysed twin‐pairs; six non‐RCTs; one randomised fewer than six clusters; one case‐control; one prediction model used), 20 for unsuitable study population (e.g. adults or overweight children with intention to reduce weight), 58 for inappropriate intervention (e.g. school lunch programme), 14 for inappropriate exposure (e.g. dairy food intake or cereal intake), eight for no eligible outcomes reported and our outcomes deemed to be outside of the scope of the study (e.g. psychological outcomes), six for inappropriate comparison, nine for inappropriate duration (e.g. less than one year for cohort studies) and four duplicates. We excluded the Special Turku Coronary Risk Factor Intervention Project (STRIP) trial (Niinikoski 2014), as the primary intention of the intervention was to reduce saturated fat intake through replacement with unsaturated fat, thus changing the 'quality' of fat intake or composition of fat intake. Our question primarily concerns the quantity of total fat intake.
Studies awaiting classification
We found two published abstracts from the one study awaiting assessment (Khalil 2015) and contacted the authors for additional information, but did not receive a response in time for assessment for inclusion in this review. We also contacted the authors of Twisk 1998, but did not receive the requested information in time.
Ongoing studies
We found no eligible ongoing studies.
Risk of bias in included studies
Figure 3 represents each risk of bias item presented as percentages across all included RCTs and across all included cohort studies. A visual representation of the risk of bias for each domain per included RCT and cohort study is presented in Figure 4. For the two trials that also report eligible cohort analyses (Obarzanek 1997 (cohort); Tershakovec 1998 (cohort)), we reported risk of bias judgements for each study design.
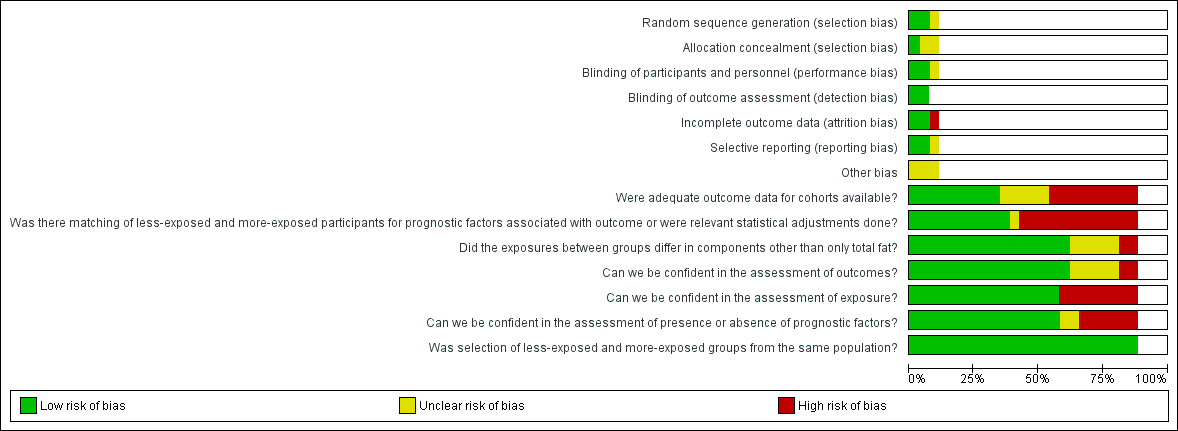
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
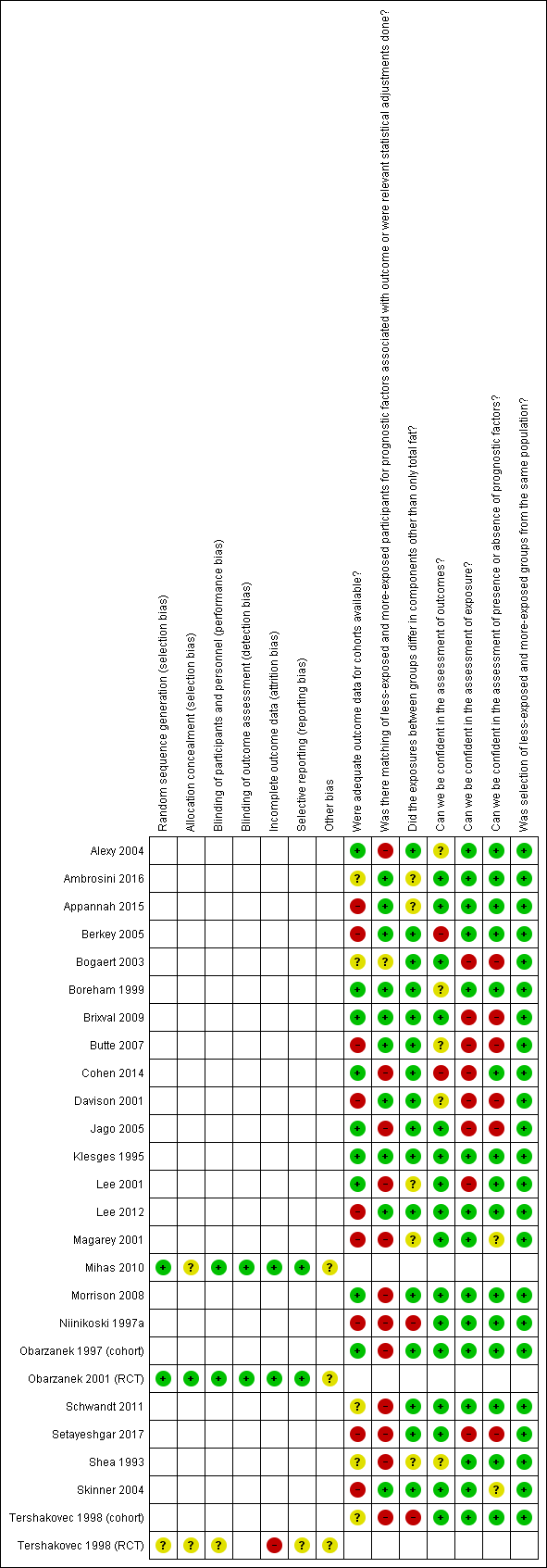
Risk of bias summary: review authors' judgements about each risk of bias item for each included study. RCT: randomised controlled trial.
See the Characteristics of included studies table for details of risk of bias judgements per trial and per cohort study.
Validity of randomised controlled trials
Allocation (selection bias)
We judged two RCTs to have an unclear risk of selection bias because allocation concealment was not reported (Mihas 2010; Tershakovec 1998 (RCT)), and Tershakovec 1998 (cohort) also lacked clarity in the reporting of random sequence generation. Obarzanek 2001 (RCT) was at low risk of selection bias.
Blinding (performance bias and detection bias)
Tershakovec 1998 (RCT) did not report on blinding and we judged this study at unclear risk of performance and detection bias. Obarzanek 2001 (RCT) reported blinding of outcome assessors and not of participants. However, since this was unlikely to have influenced the primary study outcomes, we judged this trial at low risk for performance and detection bias. Similarly, we judged Mihas 2010 at low risk of bias for this domain because although the authors reported blinding was not feasible, it was unlikely that the primary outcome was influenced by a lack of blinding.
Incomplete outcome data (attrition bias)
We assessed those studies that lost more than 10% of participants in total at high risk of attrition bias, unless they adequately report dropout analyses showing no differences in reasons and key characteristics between completers and non‐completers. Attrition rates were greater than 10% over the one‐year follow‐up for Tershakovec 1998 (RCT) and reasons for missing outcome data per group were not provided; thus, it was at high risk of bias. We assessed the other two RCTs at low risk of attrition bias due to reported attrition rates of less than 10% (Mihas 2010; Obarzanek 2001 (RCT)).
Selective reporting (reporting bias)
Tershakovec 1998 (cohort) was at unclear risk of reporting bias because outcomes reported by the authors were not prespecified. We judged the other two RCTs at low risk of reporting bias because they prespecified their outcomes in the methods section and addressed them in the results section (Mihas 2010; Obarzanek 2001 (RCT)). Generating funnel plots was not possible due to the small number of included trials.
Other potential sources of bias
All three RCTs were at unclear risk of 'other bias' because limited information on the control diet prescription made it difficult to judge if the intervention and control diets differed in components other than only total fat.
Validity of cohort studies
Was adequate outcome data available? (attrition bias)
Nine studies were at high risk of attrition bias due to high attrition (greater than 5% attrition per year) and reasons for attrition were not reported or incompletely described (Appannah 2015; Berkey 2005; Butte 2007; Davison 2001; Lee 2012; Magarey 2001; Niinikoski 1997a; Setayeshgar 2017; Skinner 2004). Four studies with high attrition conducted dropout analyses of baseline anthropometric and dietary intake variables: two were at low risk of bias because they adequately reported no difference between completers and non‐completers (Brixval 2009; Klesges 1995); and the other two were at unclear risk of bias because insufficient information was provided to permit judgement (Bogaert 2003; Tershakovec 1998 (cohort)). Attrition bias could not be determined for two studies (judged at unclear risk of bias), as Shea 1993 did not report how many children completed the last follow‐up visit, and Schwandt 2011 reported the dropout analysis inadequately. The remaining seven studies had low risk of attrition bias.
Was there matching of less‐exposed and more‐exposed participants for prognostic factors associated with outcome, or were relevant statistical adjustments done? (selection bias)
Eight studies compared outcome data in less‐exposed versus more‐exposed groups and none of these matched their participants for prognostic factors (Alexy 2004; Ambrosini 2016; Appannah 2015; Lee 2001; Magarey 2001; Niinikoski 1997a; Shea 1993; Tershakovec 1998 (cohort)). Twelve studies were at high risk of selection bias due to no or incomplete adjustment for important prognostic variables, namely, age, sex, energy intake, ethnicity, parental BMI, physical activity (and/or screen time), pubertal stage and socioeconomic (income and educational) status (Alexy 2004; Cohen 2014; Jago 2005; Lee 2001; Magarey 2001; Morrison 2008; Niinikoski 1997a; Obarzanek 1997 (cohort); Schwandt 2011; Setayeshgar 2017; Shea 1993; Tershakovec 1998 (cohort)). We judged Bogaert 2003 to have an unclear risk of selection bias because prognostic variables included in the analyses were not described. The remaining 10 studies were at low risk of bias for this domain.
Did the exposures between groups differ in components other than only total fat? (performance bias)
Two trials that reported eligible cohort analyses comparing less‐exposed and more‐exposed groups were at high risk of bias because the exposures in the original trial groupings differed in components other than only total fat (Niinikoski 1997a; Tershakovec 1998 (cohort)). The risk was unclear in the other five studies that reported data on less‐exposed versus more‐exposed groups (Ambrosini 2016; Appannah 2015; Lee 2001; Magarey 2001; Shea 1993), and low risk in one (Alexy 2004). We judged the other 15 studies that only reported single group associations between fat intake and weight over time as low risk of bias for this domain.
Can we be confident in the assessment of outcomes? (detection bias)
Cohen 2014 and Berkey 2005 were at high risk of detection bias because methods for measuring body fat were inconsistent across different time points during the study , and self‐reporting of weight and height was used, respectively. The risk was unclear in five studies that did not provide sufficient detail to make a judgement (Alexy 2004; Boreham 1999; Butte 2007; Davison 2001; Shea 1993), and the remaining studies had a low risk of detection bias.
Can we be confident in the assessment of exposure? (detection bias)
Fifteen of 23 studies were at low risk as they assessed dietary intake repeatedly throughout the duration of the study using recognised or validated methods such as three‐day, four‐day or seven‐day food records, FFQs, and multiple 24‐hour recall questionnaires. Three studies used multiple 24‐hour recall questionnaires (Lee 2012; Obarzanek 1997 (cohort); Tershakovec 1998 (cohort)). Seven studies were at high risk of bias for this domain, since they only assessed dietary intake at baseline (regardless of the methods they used) (Bogaert 2003; Brixval 2009; Butte 2007; Cohen 2014; Davison 2001; Lee 2001; Setayeshgar 2017), and one study used direct observation for dietary assessments, which is likely to introduce the Hawthorne effect (Jago 2005).
Can we be confident in the assessment of presence or absence of prognostic factors? (selection bias)
In this domain, we specifically looked at our most important prognostic factors, such as physical activity, parental BMI, pubertal stage and whether these factors were adequately assessed in the included cohort studies. We judged 15/23 studies at low risk of bias for this domain. Twelve of these studies repeatedly ascertained or measured the prognostic factors using validated methods, which were well described in the reports (Ambrosini 2016; Appannah 2015; Berkey 2005; Boreham 1999; Cohen 2014; Klesges 1995; Lee 2012; Morrison 2008; Niinikoski 1997a; Obarzanek 1997 (cohort); Schwandt 2011; Tershakovec 1998 (cohort)). We allocated low risk of bias to three studies that did not apply, and thus did not measure, prognostic factors in their studies (Alexy 2004; Lee 2001; Shea 1993). We allocated high risk to studies that performed a single assessment (Bogaert 2003; Brixval 2009; Butte 2007; Setayeshgar 2017), multiple assessments but with inconsistent methods (Davison 2001), direct observation of physical activity (Jago 2005), and self‐reported parental weight and height and pubertal stage (Brixval 2009; Butte 2007). The risk of bias was unclear for studies that did not adequately describe measurement methods for physical activity (Skinner 2004) and parental weight and height (Magarey 2001).
Was selection of less‐exposed and more‐exposed groups from the same population? (selection bias)
We considered all included cohort studies at low risk of bias for this domain because they all recruited children from the same cohort sample or study population.
Effects of interventions
See: Summary of findings for the main comparison Total fat intake 30% or less of total energy compared to usual fat intake for body weight in children (RCTs)a ; Summary of findings 2 Total fat intake and body weight in children (cohort studies)a,b
Effects of reducing dietary fat to 30% or less of total energy on body fatness in children (as seen in RCTs)
summary of findings Table for the main comparison presents the effects of a total fat intake of 30% or less in relation to total energy (≤ 30%TE) compared to usual or modified fat intake for bodyweight in children for data from RCTs. The data for all time points are presented in Appendix 2.
Primary outcomes
Weight
We have presented a summary of MDs and 95% CI between intervention and control groups for weight outcomes over time in Table 2 and Analysis 1.1. No pooling of data was possible due to the use of different outcomes by the two trials. We extracted weight‐for‐age z‐scores from Tershakovec 1998 (RCT) at baseline, and end values at six months (MD ‐0.14, 95% CI ‐0.45 to 0.17; n = 149; very low‐quality evidence), and 12 months (MD ‐0.18, 95% CI ‐0.51 to 0.15; n = 151; very‐low quality evidence); we are uncertain whether lower fat intake had an effect on weight‐for‐age z‐scores. Obarzanek 2001 (RCT) reported bodyweight (kg), and we extracted data at baseline and end values at 12 months (MD ‐0.50 kg, 95% CI ‐1.78 to 0.78; n = 620; low‐quality evidence), and three years (MD ‐0.60 kg, 95% CI ‐2.39 to 1.19; n = 612; low‐quality evidence). Fat intake of ≤ 30%TE versus usual or modified total fat intake in children may have made little or no difference to weight (kg) over these follow‐up periods.
| Outcome Study ID | Follow‐up from baseline | |||||
| Baseline Mean (SD)a | 6 months MD (95% CI) | > 6 to 12 months MD (95% CI) | > 1 to 2 years MD (95% CI) | > 2 to 5 years MD (95% CI) | > 5 years MD (95% CI) | |
| Weight‐for‐age z‐scoreb | ||||||
| 0.04 (1.02); 0.26 (0.93) | ‐0.14 (‐0.45 to 0.17) | ‐0.18b (‐0.51 to 0.15) | ND | ND | ND | |
| Body weight (kg)b | ||||||
| 32.7 (6.8); 33.1 (6.9) | ND | ‐0.50b (‐1.78 to 0.78) | ND | ‐0.60 (‐2.39 to 1.19) | ND | |
| BMI (kg/m2) | ||||||
| 17.5 (2.3); 17.6 (2.4) | ND | ‐0.30 (‐0.75 to 0.15) | ND | 0.00 (‐0.63 to 0.63) | ‐0.10 (‐0.75 to 0.55) | |
| 24 (3.1); 24.3 (3.3) | ND | ND | ‐1.50 (‐2.45 to ‐0.55) | ND | ND | |
aReduced fat intake group (≤ 30%TE); usual fat intake group.
bWeight‐for‐age z‐score and weight (kg) could not be pooled.
%TE: percentage of total energy; BMI: body mass index; CI: confidence interval; MD: mean difference; ND: no data in this time point range; SD: standard deviation.
Body mass index
We have presented a summary of MDs and 95% CI between intervention and control groups for BMI over time in Table 2 and Analysis 1.2. The trials did not report BMI data over similar time ranges and so could not be pooled. For Obarzanek 2001 (RCT) we extracted baseline and end values at 12 months, five years and last visit (approximately six to 10 years). Obarzanek 2001 (RCT) found that fat intake of ≤ 30%TE may make little or no difference to children's BMI (kg/m2) at 12 months (MD ‐0.30 kg/m2, 95% CI ‐0.75 to 0.15; n = 620; low‐quality evidence), five years (MD 0.0 kg/m2, 95% CI ‐0.63 to 0.63; n = 541; low‐quality evidence), or at last visit (MD ‐0.10 kg/m2, 95% CI ‐0.75 to 0.55; n = 576; low‐quality evidence), when compared to usual or modified fat intake. For Mihas 2010, we were able to extract BMI data for baseline and end values 17 months later. This trial reported that after 17 months, a fat intake of ≤ 30%TE compared to usual fat intake probably reduced children's BMI (MD ‐1.5 kg/m2, 95% CI ‐2.45 to ‐0.55; n = 191; moderate‐quality evidence). We conducted sensitivity analyses to exclude possible effects of our selected time ranges, by including BMI data from only the longest follow‐up periods per study (Mihas 2010 at 12 months, and Obarzanek 2001 (RCT) at more than five years; Analysis 1.3). This analysis showed significant heterogeneity, to the extent that we could not pool the data (Chi2 P = 0.02; I2 = 82.5%). Similarly, pooling data from the shortest follow‐up periods per study showed significant heterogeneity (Mihas 2010 at 12 months and Obarzanek 1997 (cohort) at 12 months; Analysis 1.4) (Chi2 P = 0.03; I2 = 80%), and precluded the pooling of these data.
Secondary outcomes
Serum lipids
We have presented a summary of MDs and 95% CI between intervention and control groups for serum lipids over time Table 3 and in Analysis 1.5; Analysis 1.6; Analysis 1.7; Analysis 1.8.
| Outcome | Follow‐up from baseline | |||||
| Baseline Mean (SD)a | 6 months MD (95% CI) | > 6 to 12 months MD (95% CI) | > 1 to 2 years MD (95% CI) | > 2 to 5 years MD (95% CI) | > 5 years MD (95% CI) | |
| Total cholesterol (mmol/L) | 5.17 (0.38); 5.17 (0.38) | ND | ‐0.15 (‐0.24 to ‐0.06) | ND | ‐0.06 (‐0.17 to 0.05) | ‐0.02 (‐0.13 to 0.09) |
| LDL‐C (mmol/L) | 3.38 (0.31); 3.38 (0.3) | ND | ‐0.12 (‐0.20 to ‐0.04) | ND | ‐0.09 (‐0.17 to ‐0.01) | 0.01 (‐0.01 to 0.03) |
| HDL‐C (mmol/L) | 1.48 (0.28); 1.47 (0.29) | ND | ‐0.03 (‐0.08 to 0.02) | ND | ‐0.01 (‐0.06 to 0.04) | 0.02 (‐0.03 to 0.07) |
| Triglycerides (mmol/L) | 0.9 (0.33); 0.92 (0.32) | ND | ‐0.01 (‐0.08 to 0.06) | ND | 0.06 (‐0.04 to 0.16) | 0.03 (‐0.06 to 0.12) |
| SBP (mmHg) | 97.31 (9.1); 97.55 (9.4) | ND | ‐0.40 (‐1.70 to 0.90) | ND | ‐0.40 (‐1.84 to 1.04) | ND |
| DBP (mmHg) | 61.97 (9.54); 61.67 (10.23) | ND | ‐0.50 (‐2.00 to 1.00) | ND | ‐0.90 (‐2.30 to 0.50) | ND |
aReduced fat intake group (≤ 30%TE); usual fat intake group.
%TE: percentage of total energy; CI: confidence interval; DBP: diastolic blood pressure; HDL‐C: high‐density lipoprotein cholesterol; LDL‐C: low‐density lipoprotein cholesterol; MD: mean difference; ND: no data in this time point range; SBP: systolic blood pressure; SD: standard deviation.
Only Obarzanek 2001 (RCT) reported serum lipids, and we extracted baseline data and end values at 12‐month follow‐up for total cholesterol, LDL‐cholesterol, HDL‐cholesterol and triglycerides (mmol/L). Additionally, we extracted end values for total cholesterol, HDL‐cholesterol and triglycerides at five years after baseline and at last visit (approximately six to 10 years after baseline). For LDL‐cholesterol, we could not extract variances from the five‐year figures, therefore we used end values and their SDs reported per group at three years. For the last visit, we extracted change scores for LDL‐cholesterol and calculated SDs from a reported P value. This trial found that fat intake of ≤ 30%TE probably reduced total cholesterol slightly over 12 months compared to controls (MD ‐0.15 mmol/L, 95% CI ‐0.24 to ‐0.06; n = 618; moderate‐quality evidence), but may have made little or no difference over longer time periods (at five years MD ‐0.06 mmol/L, 95% CI ‐0.17 to 0.05; n = 522; low‐quality evidence; at last visit MD ‐0.02 mmol/L, 95% CI ‐0.13 to 0.09; n = 548; low‐quality evidence).
Obarzanek 2001 (RCT) also found that fat intake of ≤ 30%TE probably decreased LDL‐cholesterol slightly at 12 months (MD ‐0.12 mmol/L, 95% CI ‐0.20 to ‐0.04; n = 618, moderate‐quality evidence) and for the time period of two to five years (MD ‐0.09, 95% CI ‐0.17 to ‐0.01; n = 623; moderate‐quality evidence) compared to controls, but probably made little or no difference over longer periods. For HDL‐cholesterol fat intake of ≤ 30%TE versus fat intake > 30%TE probably made little or no difference to levels at 12 months (MD ‐0.03 mmol/L, 95% CI ‐0.08 to 0.02; n = 618; moderate‐quality evidence), five years (MD ‐0.01 mmol/L, 95% CI ‐0.06 to 0.04; n = 522; moderate‐quality evidence), or last visit (MD 0.02 mmol/L, 95% CI ‐0.03 to 0.07; n = 548; moderate‐quality evidence) (Obarzanek 2001 (RCT)).
Results for triglycerides in children also showed that fat intake of ≤ 30%TE probably made little or no difference to triglyceride levels at 12 months (MD ‐0.01 mmol/L, 95% CI ‐0.08 to 0.06; n = 618; moderate‐quality evidence), and may have made little or no difference at five years (MD 0.06 mmol/L, 95% CI ‐0.04 to 0.16; n = 522; low‐quality evidence), or last visit (MD 0.03 mmol/L, 95% CI ‐0.06 to 0.12; n = 548; low‐quality evidence) (Obarzanek 2001 (RCT)).
Systolic and diastolic blood pressure
We have presented a summary of MDs and 95% CI between intervention and control groups for SBP and DBP over time in Table 3 and Analysis 1.9 and Analysis 1.10. Only Obarzanek 2001 (RCT) reported blood pressure (mmHg) and we extracted baseline data and end values at 12 months (SBP MD ‐0.40 mmHg, 95% CI ‐1.70 to 0.90; n = 621; DBP MD ‐0.50 mmHg, 95% CI ‐2.00 to 1.00; n = 621), and three years (SBP MD ‐0.40 mmHg, 95%CI ‐1.84 to 1.04; n = 583; DBP MD ‐0.90 mmHg, 95% CI ‐2.30 to 0.50; n = 583).
Height (adverse outcome)
We have presented a summary of MDs and 95% CI between intervention and control groups for height outcomes over time in Table 4 and Analysis 1.11. Pooling of data was not possible due to use of different outcomes by the two trials. We extracted height‐for‐age z‐scores from Tershakovec 1998 (RCT) at baseline, and end values at six months (MD ‐0.02, 95% CI ‐0.06 to 0.02; n = 149; very low‐quality evidence), and 12 months (MD ‐0.05, 95% CI ‐0.08 to 0.02; n = 151; very low‐quality evidence), and, due to the very low quality of the evidence, we are uncertain whether lower fat intake had an effect on height‐for‐age z‐scores.
| Outcome Study ID | Follow‐up from baseline | |||||
| Baseline Mean (SD)a | 6 months MD (95% CI) | > 6 to 12 months MD (95% CI) | > 1 to 2 years MD (95% CI) | > 2 to 5 years MD (95% CI) | > 5 years MD (95% CI) | |
| Height‐for‐age z‐scoreb | ||||||
| ‐0.12 (1.02); 0.06 (0.93) | ‐0.02 (‐0.06 to 0.02) | ‐0.05b (‐0.08 to‐0.02) | ND | ND | ND | |
| Height (cm)b | ||||||
| 136.2 (6.8); 136.5 (7) | ND | 0.00b (‐1.11 to 1.11) | ND | ‐0.10 (‐1.54 to 1.34) | ‐0.06 (‐2.06 to 0.86) | |
aReduced fat intake group (≤ 30%TE); usual fat intake group.
bHeight‐for‐age z‐score and height (cm) cannot be pooled.
%TE: percentage of total energy; CI: confidence interval; MD: mean difference; ND: no data in this time point range; RCT: randomised controlled trial; SD: standard deviation.
Obarzanek 2001 (RCT) reported height (cm); we extracted data at baseline and end values at 12 months, five years, and approximately six to 10 years from baseline (last visit). Lower versus usual or modified fat intake may have made little or no difference to height over 12 months (MD 0 cm, 95% CI ‐1.11 to 1.11; n = 642; low‐quality evidence), five years (MD ‐0.10 cm, 95% CI ‐ 1.54 to 1.34; n = 540; low‐quality evidence), or more than five years (MD ‐0.60 cm, 95% CI ‐2.06 to 0.86; n = 577; low‐quality evidence) (Obarzanek 2001 (RCT)).
Tertiary outcomes
Dietary intake
We have presented a summary of MDs and 95% CI between intervention and control groups for dietary intake variables over time in Table 5 and in Analysis 1.12; Analysis 1.13; Analysis 1.14; Analysis 1.15; Analysis 1.16. The two trials did not report eligible dietary outcomes for similar time ranges and thus we could not pool the data. End values for energy (kJ), fat, saturated fat, protein and carbohydrate intake (%TE) were reported by Obarzanek 2001 (RCT) at 12 months and three years, and by Mihas 2010 at 17 months. In both trials, the differences in the proportion of TE provided by the macronutrients (fat, protein and carbohydrates) in the diets of children in intervention groups showed lower intake of total fat (range of 95% CI ‐6.91 to ‐3.55% of TE) and greater intake of total protein (range of 95% CI 0.38 to 1.48% of TE) and total carbohydrates (range of 95% CI 1.16 to 4.84% of TE), compared to control groups, at all reported time points, which is in line with the diets being tested.
| Outcome Study ID | Follow‐up from baseline | |||||
| Baseline Mean (SD)a | 6 months MD (95% CI) | > 6 to 12 months MD (95% CI) | > 1 to 2 years MD (95% CI) | > 2 to 5 years MD (95% CI) | > 5 years MD (95% CI) | |
| Energy (kJ) | ||||||
| 7364 (1832); 7229 (1841) | ND | ‐356.00 (‐655.22 to ‐56.78) | ND | ‐602.00 (‐943.94 to ‐260.06) | ND | |
| 8503.3 (1419.3); 8583.7 (1522.4) | ND | ND | ‐645.50 (‐1075.66 to ‐215.34) | ND | ND | |
| Fat (%TE) | ||||||
| 33.4 (5.5); 34 (4.9) | ND | ‐4.60 (‐5.50 to ‐3.70) | ND | ‐4.40 (‐5.25 to ‐3.55) | ND | |
| 35.4 (4.7); 36.2 (5.2) | ND | ND | ‐5.60 (‐6.91 to ‐4.29) | ND | ND | |
| Saturated fat (%TE) | ||||||
| 12.5 (2.7); 12.7 (2.5) | ND | ‐2.60 (‐3.02 to ‐2.18) | ND | ‐2.10 (‐2.49 to ‐1.71) | ND | |
| 12.4 (2.0); 12.8 (2.3) | ND | ND | ‐3.10 (‐3.78 to ‐2.42) | ND | ND | |
| Protein (%TE) | ||||||
| 14.8 (2.8); 14.6 (2.7) | ND | 1.00 (0.52 to 1.48) | ND | 0.90 (0.38 to 1.42) | ND | |
| 15.3 (1.4); 14.9 (1.8) | ND | ND | 1.30 (0.80 to 1.80) | ND | ND | |
| Carbohydrates (%TE) | ||||||
| 53.0 (6.7); 52.8 (6.2) | ND | 3.70 (2.63 to 4.77) | ND | 3.30 (2.25 to 4.35) | ND | |
| 49.7 (6.2); 48.4 (6.8) | ND | ND | 3.00 (1.16 to 4.84) | ND | ND | |
aReduced fat intake group (≤ 30%TE); usual fat intake group.
%TE: percentage of total energy; MD: mean difference; ND: no data in this time point range; RCT: randomised controlled trial; SD: standard deviation.
Associations between total dietary fat exposure and measures of body fatness in children (as seen in cohort studies)
summary of findings Table 2 and Appendix 3 present a summary of the association between total dietary fat exposure, weight and body fatness in children for data from prospective cohort studies. Importantly, some cohort studies reported more than one eligible analysis for the same outcome, as a continuous or binary outcome (e.g. BMI in kg/m2 and overweight/obese according to IOTF cut‐offs). Where a single study reported different analyses for the same important outcome in the same participants (e.g. BMI z‐scores versus BMI cut‐offs for overweight and obesity), we selected the most relative continuous analysis for inclusion in the table. Similarly, when a single study reported different measures of the exposure in relation to the same outcome in the same participants (e.g. total fat intake in absolute grams versus as %TE), we selected the most relative continuous exposure for the table. In this way, we were careful not to use the same study sample of participants more than once per outcome and time range in summary of findings Table 2 nor Appendix 3.
We considered meta‐analyses of cohort studies, but considered that the methodologies, analysis methods, dietary assessments, ages at baseline, applications of total fat intake exposure and eligible outcome measures were so varied across studies in the five time ranges, that combining studies was not appropriate. In addition, important information, such as measures of variation and numerical results, were not reported in many of the studies.
Primary outcomes
Weight
We have summarised the various standardised and unstandardised weight outcomes, total fat exposure variables and results of reported associations, including adjustments made within each time range in Table 6.
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) | |
| Weight at 1 year: 4 cohort studies; 4 analyses (n ˜ 1949) in boys and girls aged 2‐11 years | |||||||||
| 2 years old; mean end values per group | Relative weightb | % | 1 | Total fat intake (single 4‐day dietary record at baseline, 1.5 and 2 years) | LF (27.7‐28.7 %TE; HF (> 28.7 %TE) | n overall = 740 (LF = 35, HF = 705); mean end values (SD). Baseline: LF = 1 (8); HF = 1 (8). At 1 year: LF = 1 (7); HF = 1 (8); P = 0.81. After 1 year, no difference in relative weight change of children with LF intake compared to children with HF intakes. | 0 No | No matching reported. No adjustment for prognostic variables. | |
| 6.8 years old; regression | Weight | kg | 1 | Total fat intake (single 7‐day weighed dietary record at baseline and 1 year) | g | n overall = 411; regression result. B = 0.09, SE 0.019; P < 0.05. After 1 year, for every 1 g increase in total fat intake of children, weight will increase by 0.09 kg. | + No | Adjusted for age, gender and physical activity. | |
| 11 years old; regression | Weight | kg/year | 1 | Total fat intake (multiple 24‐hour dietary recalls at baseline) | %TE | n overall = 798; regression result. B = 0.044, SE 0.018; P = 0.014. For every 1% increase in energy intake from total fat in children, weight will increase by 0.04 kg/year. | + No | Adjusted for gender, age, age squared, Tanner stage and BMI. | |
| 6.2 years old; mean end values per group | Weight | z‐score | 1 | Total fat intake (multiple 24‐hour dietary recalls at baseline and 1 year) | LF quintile (24 %TE) HF quintile (34%TE) | n overall = NR (LF = NR, HF = NR); mean end values (SD NR). Baseline: LF = ‐0.21; HF = 0.44. At 1 year: LF = ‐0.14; HF = 0.45. After 1 year, weight‐for‐age of children with LF intake will increase by 0.07 z‐scores on average, and by 0.01 z‐scores in children with HF intake. | ‐ No | No matching reported. No adjustment for prognostic variables. | |
| Weight at > 1to 2 years: 1 cohort study; 1 analysis (n = 126) in boys and girls aged 2 years | |||||||||
| 2 years old; mean end values per group | Weight | kg | 2 | Total fat intake (single 3‐day weighed dietary records at baseline and 2 years) | LF < 30%TE; HF > 35%TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 12.6 (1); HF = 12.8 (1.7). At 2 years: LF (n = 20) 18.4 (2.6); HF (n = 76) 17.9 (2.1); P > 0.05. After 2 years, weight of children with LF intake will increase by 5.8 kg on average, and by 5.1 kg on average in children with HF intake. | ‐ No | No matching reported. No adjustment for prognostic variables. | |
| Weight at > 2to 5 years: 4 cohort studies; 4 analyses (n = 13,802) in boys and girls aged 2‐14 years | |||||||||
| 4.4 years old; mean change per group | Weight | kg/year | 2.1 | Total fat intake (multiple FFQs at baseline) | LF ≤ 30%TE; HF > 30%TE | n overall = 215 (LF = 37, HF = 178); mean change (SD). Baseline: NR. LF = 3 (1.3); HF = 2.8 (1.3); P > 0.05 MD 0.2 (95% CI ‐0.26 to 0.66). After 2 years, children with LF intake will gain on average 0.2 kg/year more than children with HF intakes. | ‐ No | No matching reported. No adjustment for prognostic variables. | |
| 9‐14 years‐old; regression | Weight | kg, 1‐year change | 3 | Total fat intake (single FFQ at baseline, 1, 2 and 3 years) | g | n overall = 12,829; only reported as text. After 3 years, "Dairy fat was not a stronger predictor of weight gain than other types of fat, and no fat (dairy, vegetable, or other) intake was significantly associated with weight gain after energy adjustment, nor was total fat intake." | 0 Yes | Adjusted for age, ethnicity, pubertal stage, annual height growth, baseline BMI and same‐year physical activity. | |
| 9.6 years old; regression | Weight | kg | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | %TE | n overall = 632; regression results. B = ‐0.0011, P = 0.8. After 3 years, for every 1% increase in total energy intake from total fat of children, weight will decrease by 0.0011 kg. | ‐ Yes | Adjusted for gender, physical activity, treatment, visit number, other sources of energy than fat and interactions: fat intake‐by‐treatment, fat intake‐by‐gender, fat intake‐by‐visit number and visit number‐by‐treatment. | |
| 2 years‐old; mean end values per group | Weight | kg | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | LF < 30%TE; HF > 35%TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 12.6 (1); HF = 12.8 (1.7). At 4 years: LF (n = 14) 20.7 (3.4); HF (n = 88) 21.7 (3); P > 0.05. After 4 years, weight of children with LF intake will increase by 8.1 kg on average, and by 8.9 kg on average in children with HF intake. | + No | No matching reported. No adjustment for prognostic variables. | |
| Weight at > 5to 10 years: 1 cohort study; 1 analysis (n = 126) in boys and girls aged 2 years | |||||||||
| 2 yrs‐old; mean end values per group | Weight | kg | 6 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years; single 4‐day weighed dietary record at 6 years) | LF < 30 %TE; HF > 35 %TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 12.6 (1); HF = 12.8 (1.7). At 6 years: LF (n = 13) 29.4 (5.9); HF (n = 72) 26.7 (4.3); P > 0.05. After 6 years, weight of children with LF intake will increase by 16.8 kg on average, and by 13.9 kg on average in children with HF intake. | ‐ No | No matching reported. No adjustment for prognostic variables. | |
aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction, inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome.
bRelative weight, deviation in percentages from the mean weight of healthy Finnish children of the same height and gender.
%TE: percentage of total energy; B: unstandardized beta‐coefficient; BMI: body mass index; CI: confidence interval; FFQ: Food Frequency Questionnaire; LF: low fat; HF: high fat; n: number of participants; NA: not applicable; MD: mean difference; NR: not reported; SD: standard deviation; SE: standard error.
Four cohort studies reported weight outcomes at one‐year follow‐up in four analyses (n = approximately 1949) in boys and girls (mean age at baseline: two to 11 years), and none of these studies adjusted for TE intake in their analyses (Butte 2007; Niinikoski 1997a; Schwandt 2011; Tershakovec 1998 (cohort)). The two studies that examined total fat intake exposure as a continuous variable at one year, reported positive associations: for every 1 g increase in total fat intake of children, weight increased by 0.09 kg (Schwandt 2011), and for every 1% increase in energy intake from total fat in children, weight increased by 0.04 kg/year (Butte 2007). After one year, Niinikoski 1997a analysed total fat intake as a binary variable and reported the same relative mean weight change in low‐fat compared to high‐fat intake children (low‐fat group 1% (SD 7), high‐fat group 1% (SD 8), P = 0.81). Tershakovec 1998 (cohort) used quintiles of fat intake and reported that weight‐for‐age of children with low‐fat intake increased by 0.07 z‐scores on average, and by 0.01 z‐scores in children with high‐fat intake.
Magarey 2001 reported weight at two‐year follow‐up (boys and girls, aged two years at baseline, n = 126) in a single analysis as mean end values in a low‐fat group (< 30%TE) and a high‐fat group (> 30%TE) based on baseline fat intake, and found that weight increased by 5.8 kg on average with low‐fat intake, and by 5.1 kg on average with high‐fat intake.
At 2 to 5 years, Berkey 2005 (n = 12 829) and Obarzanek 1997 (cohort) (n = 632) examined associations (regressions) between weight and continuous exposure to fat (absolute grams and %TE) in nine‐ to 14‐year olds, with adjustments for TE intake, and reported no or negligible associations. Magarey 2001 reported mean end values per group in two‐year olds (cut‐offs of fat intake < 30%TE and > 35%TE), and Shea 1993 reported mean change per group in four‐year olds, with exposure to lower fat versus higher fat intake groups (cut‐offs of fat intake ≤ 30%TE and > 30%TE). With no adjustment for TE intake, Magarey 2001 found that after four years, weight of children with low‐fat intake increased by 8.1 kg on average, and by 8.9 kg on average in children with high‐fat intake (n = 126), and Shea 1993 found that children with low‐fat intake gained on average 0.2 kg/year more than children with high‐fat intake (n = 215).
Magarey 2001 also reported the same analysis at six years (5 to 10 years), and, with no adjustment for TE, found that the weight of children with low‐fat intake increased by 16.8 kg on average, and that of children with high‐fat intake increased by 13.9 kg on average (n = 126).
Body mass index
We have summarised BMI outcomes (standardised and unstandardised), total fat exposure descriptions, and results of reported associations within each time range, including the adjustments made in Table 7.
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted? (yes/no) | Matched groups or adjusted for (or both) |
| BMI at 1 year: 3 cohort studies; 4 analyses (n ˜ 11,180) in boys and girls aged 7‐14 years | ||||||||
| 9‐14 years; regression | BMI | kg/m2, 1‐year change | 1 | Total fat intake (single FFQ at baseline and 1 year) | g | n girls = 6149; regression result. B = 0.0008, SE 0.0016, P = 632. After 1 year, for every 1 g increase in total fat intake, BMI will increase by 0.0008 kg/m2 in girls. | + Yes | Adjusted for total energy intake, age, ethnicity, pubertal stage, annual height growth, baseline BMI and physical activity. |
| 9‐14 years; regression | BMI | kg/m2, 1‐year change | 1 | Total fat intake (single FFQ at baseline and 1 year) | g | n boys = 4620; regression result. B = ‐0.0015, SE 0.0017, P = 0.375. After 1 year, for every 1 g increase in the total fat intake, BMI will decrease by 0.0015 kg/m2 in boys. | ‐ Yes | Adjusted for total energy intake, age, ethnicity, pubertal stage, annual height growth, baseline BMI and physical activity. |
| 8.6 years; regression | BMI | z‐score | 1 | Total fat intake (single 3‐day record at baseline) | %TE | n overall = NR; regression result = NR. "We are unable to demonstrate a positive relation between dietary fat and BMI z‐score change from baseline to 12 months." | 0 NR | Prognostic variables were adjusted for, but not specified which one. |
| 6.8 years; regression | BMI | kg/m2 | 1 | Total fat intake (single 7‐day weighed record at baseline and 1 year) | g | n overall = 411; regression result. B = 0.08, SE 0.007, P = 0.085. After 1 year, for every 1 g increase in the total intake, BMI will increase by 0.08 kg/m2. | + No | Adjusted for age, sex and physical activity. |
| BMI at > 1to 2 years: 7 cohort studies; 10 analyses (n = 3347) in boys and girls aged 2‐13 years | ||||||||
| 3.6 years; mean end values per group | BMI | kg/m2 | 1.5 | Total fat intake (single 3‐day unweighed food record at baseline) | LF quintile (30.4%TE); HF quintile (41.8 %TE) | n boys, at baseline = 438; At 1.5 years = 383 (LF = NR, HF = NR); mean end values (SD). Baseline: LF = 16.6 (95% CI 16.4 to 16.8); HF = 16.3 (95% CI 16.1 to 16.5). At 1.5 years: LF = 16.1 (95% CI 15.8 to 16.3); HF = 15.7 (95% CI 15.5 to 16.0). After 18 months, average BMI decreased by 0.5 kg/m2 among boys in LF intake (30.4%TE) group and by 0.6 kg/m2 in boys in HF intake (41.8%TE) group. | ‐ No | No matching reported. No adjustment for prognostic variables. |
| 3.6 years; mean end values per group | BMI | kg/m2 | 1.5 | Total fat intake (single 3‐day unweighed food record at baseline) | LF quintile (30.4 %TE); HF quintile (41.8 %TE) | n girls, at baseline = 351; at 1.5 years = 323) (LF = NR, HF = NR); mean end values (SD). Baseline: LF = 16.6 (95% CI 16.3 to 16.9); HF = 16.4 (95% CI 16.1 to 16.7). At 1.5 years: LF = 16.1 (95% CI 15.7 to 16.4); HF = 16.1 (95% CI 15.8 to 116.4). After 18 months,average BMI decreased by 0.5 kg/m2 among girls in LF intake group (30.4%TE) and by 0.3 kg/m2 in girls in HF intake group (41.8%TE). | + No | No matching reported. No adjustment for prognostic variables. |
| 5.4 years; regression | BMI | kg/m2, 2‐years change | 2 | Total fat intake (multiple 24‐hour recalls at baseline) | %TE | n overall = 168; regression result. R2 = 0.26, P entry = 0.01, F‐test = 9.27, df = 6, P change = 0.0001. "Percentage of fat intake, baseline BMI, family risk of overweight, mothers’ BMI, fathers’ enjoyment of activity explained 26% of the variance in the change of BMI." | + Yes | Adjusted for age, baseline BMI, family risk of overweight, mothers' change in BMI and fathers' enjoyment of activity. |
| 4.4 years; regression | BMI | kg/m2, 2‐years change | 2 | Change (year 2 to 3 of follow‐up) in total fat intake (single FFQ at baseline, 1 and 2 years) | %TE | n overall = 146; regression result. B = ‐0.04, P = 0.011, t value = 2.58. After 2 years, for every 1% increase in energy intake from total fat from year 2 to 3 of follow‐up, BMI will decrease by 0.04 kg/m2. | ‐ No | Adjusted for age, sex, parental BMI and physical activity. |
| 4.4 years; regression | BMI | kg/m2, 2‐years change | 2 | Baseline dietary fat (single FFQ) | %TE | n overall = 146; regression result. B = 0.034, P = 0.0521, t value = 1.96. After 2 years, for every 1% increase in energy intake from baseline total fat, BMI will increase by 0.034 kg/m2. | + No | Adjusted for age, sex, parental BMI and physical activity. |
| 5 years; mean end values; mean change per groups | BMI | kg/m2 | 2 | Total fat intake (multiple 24‐hour recalls at baseline) | LF ≤ 30%TE; HF > 30%TE | n girls = 192 (LF = 84; HF = 108); mean end values (SD); mean change (SD). Baseline: LF = 15.8 (1.83); HF = 16 (2.08). At 2 years: LF = 16.4 (1.83); HF = 16.9 (3.12); change LF = 0.6 (0.92); change HF = 1.0 (2.08); P < 0.05. MD ‐0.4 (95% CI ‐0.84 to 0.04) After 2 years, LF intake (≤ 30%TE) will result in 0.4 kg/m2 smaller increase in BMI on average compared to HF intake (> 0%TE) in girls. | + No | No matching reported. No adjustment for prognostic variables. |
| 7.3 years; regression | BMI 1st graders | kg/m2, 2‐years change | 2 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 2 years) | %TE | n overall = 474; regression result. B = 0.021 (95% CI ‐0.004 to 0.046), P = 0.104. After 2 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.021 kg/m2. | + Yes | Adjusted for age, gender, sexual maturation at 6 years' follow‐up, baseline BMI, exercise frequency, screen time, sleep duration, meal skipping and snacking, parental BMI and SES. |
| 10 years; regression | BMI 4th graders | kg/m2, 2‐years change | 2 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 2 years) | %TE | n overall = 1030; regression result. B = ‐0.007 (95% CI ‐0.024 to 0.012), P = 0.449. After 2 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.007 kg/m2. | ‐ Yes | Adjusted for age, gender, sexual maturation at 6 years' follow‐up, baseline BMI, exercise frequency, screen time, sleep duration, meal skipping and snacking, parental BMI and SES. |
| 2 years; regression | BMI | z‐score | 2 | Total fat intake (single 3‐day weighed dietary record at baseline and 2 years) | NR | n overall = 155; regression result. β = 0.079, P > 0.1; R2 = 0.493, P < 0.0001. After 2 years, increase in the total fat intake will increase BMI by 0.079 z‐score. | + Yes | Adjusted for baseline BMI‐z score, gender, mother's BMI and father's BMI. |
| 12.5 years; regression | BMI | z‐score | 2 | Total fat intake (single 24‐hour recall at baseline) | per 10 g | n overall = 330; regression result. β = 0.009 (95% CI ‐0.006 to ‐0.02), P = NS. After 2 years, for every 10 g increase in total fat intake, BMI will increase by 0.009 z‐score. | + Yes | Adjusted for baseline BMI z‐score, moderate to vigorous physical activity, vegetables and fruit, fibre, milk, sodium and added sugar intakes. |
| BMI at > 2to 5 years: 7 cohort studies; 11 analyses (n = 4491) in boys and girls aged 2‐14 years | ||||||||
| 4.4 years; mean change per group | BMI | kg/m2 per year | 2.1 | Total fat intake (multiple FFQs at baseline) | LF ≤ 30%TE; HF > 30%TE | n overall = 215 (LF = 37, HF = 178); mean change (SD). LF = 0.2 (0.81), HF = 0.18 (0.68); P > 0.05. MD 0.02 (95% CI ‐0.26 to 0.30). After 25 months, LF intake (≤ 30%TE) will result in a 0.02 kg/m2 per year greater increase in BMI on average, compared to HF intake (> 30%TE). | ‐ No | No matching reported. No adjustment for prognostic variables. |
| 14 years; regression | BMI | z‐score | 3 | Energy‐dense, HF and low‐fibre dietary patternc (single FFQ at baseline and 3 years) | z‐score | n girls = 649; regression result. β = 0.99 (95% CI ‐0.05 to 0.05), P = NR. After 3 years, for every 1 z‐score increase in the energy‐dense, HF and low‐fibre dietary pattern z‐score, BMI will increase by 0.99 z‐score in girls. | + NA; exposure included energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 14 years; regression | BMI | z‐score | 3 | Energy‐dense, HF and low‐fibre dietary patternc (single FFQ at baseline and 3 years) | z‐score | n boys = 699; regression result. β = 0.03 (95% CI ‐0.01 to 0.08), P = NR. After 3 years, for every 1 z‐score increase in the energy‐dense, HF and low‐fibre dietary pattern, BMI will increase by 0.03 z‐score in boys. | + NA; exposure included energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 14 years; regression and OR higher vs lower dietary pattern z‐score | BMI | Overweight/obese by IOTF;d odds | 3 | Energy‐dense, HF and low‐fibre dietary patternc (single FFQ at baseline and 3 years) | z‐score | n girls = 649; regression result. OR = 1.02 (95% CI 0.87 to 1.19), P = NR. After 3 years, the ratio of odds for being overweight/obese was 1.02 greater in girls with higher dietary pattern z‐scores compared to the odds in girls with lower dietary pattern z‐scores. | + NA; exposure included energy intake | Adjusted for age, dietary misreporting, physical activity and smoking. |
| 14 years; regression and OR higher vs lower dietary pattern z‐score | BMI | Overweight/obese by IOTF;d odds | 3 | Energy‐dense, HF and low‐fibre dietary patternc(single FFQ) at baseline and 3 years) | z‐score | n boys = 699; regression result. OR = 1.04 (95% CI 0.9 to 1.2), P = NR. After 3 years, the ratio of odds for being overweight/obese is 1.04 greater in boys with higher dietary pattern z‐scores compared to the odds in boys with lower dietary pattern z‐scores. | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical activity and smoking. |
| 9.7 years; regression | BMI | z‐score, 3‐years change | 3 | Dietary fat (single 24‐hour recall at baseline) | %TE | n boys = 181; regression result. β = ‐0.63 (95% CI ‐2.07 to 0.82), P = 0.39. After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.63 z‐score in boys. | ‐ Yes | Adjusted for age, physical activity level, dietary volume and puberty at baseline. |
| 9.7 years; regression | BMI | z‐score, 3‐years change | 3 | Dietary fat (single 24‐hour recall at baseline) | %TE | n girls = 217; regression result. β = 0.07 (95% CI ‐1.08 to 1.25), P = 0.72. After 3 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.07 z‐score in girls. | + Yes | Adjusted for age, physical activity level, dietary volume and puberty at baseline. |
| 13.9 years; regression | BMI | Percentile, % | 3 | Total fat intake (single FFQ at baseline, 1, 2 and 3 years) | %TE | n girls = 265; regression result. B = ‐0.01, SE = 0.01, P = 0.16. After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.01 percentile in girls. | ‐ No | Adjusted for age, ethnicity, protein calories, CHO calories, physical activity, physical inactivity and SES. |
| 4.4 years; regression | BMI | kg/m2 | 3 | Total fat intake (observed 4‐day dietary intake at baseline, 1 and 2 years and 3‐day dietary intake at 3 years) | %TE | n overall = 133; regression result. R2 = 0.65, P = NR. "Dietary factors were not associated with BMI across the three study years." | NR Yes | Adjusted for ethnicity, gender, baseline BMI, TV viewing, sedentary behaviour, physical activity, dietary behaviours and interaction terms for variables differing by year. |
| 9.6 years; regression | BMI | kg/m2 | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | %TE | n overall = 632; regression result. B = ‐0.00008, P = 0.9. After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.00008 kg/m2. | ‐ Yes | Adjusted for gender, physical activity, treatment, visit number, other sources of energy than fat, and for interactions: fat intake‐by‐treatment, fat intake‐by‐gender, fat intake‐by‐visit number and visit number‐by‐treatment. |
| 2 years; regression | BMI | z‐score | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | NR | n overall = 152; regression result. β = 0.087, P > 0.1; R2 = 0.48, P < 0.0001. After 4 years, increase in the total fat intake, will increase BMI by 0.087 z‐score. The model explained 48% of variance in the change of BMI z‐score. | + Yes | Adjusted for baseline BMI‐z score, gender, mother's BMI and father's BMI. |
| BMI at > 5to 10 years: 4 cohort studies; 6 analyses (n = 1158) in boys and girls aged 2‐10 years | ||||||||
| 9.6 years; regression | BMI | z‐score, 6‐years change | 6 | Dietary fat (single 24‐hour recall at baseline) | %TE | n girls = 177; regression result. β = 0.005, SE 0.008, P = 0.54. After 6 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.005 z‐score in girls. | + Yes | Adjusted for age, puberty status, parent's income level, self‐reported activity, inactivity and number of overweight parents. |
| 9.6 years; regression | BMI | z‐score, 6‐years change | 6 | Dietary fat (single 24‐hour recall at baseline) | %TE | n boys = 147; regression result. β = ‐0.011, SE 0.009, P = 0.2. After 6 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.011 z‐score in boys. | ‐ Yes | Adjusted for age, puberty status, parent's income level, self‐reported activity, inactivity and number of overweight parents. |
| 2 years; regression | BMI | kg/m2 | 6 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, every year during 4, 5 and 6 years) | g | n overall = 70; regression result. B = 0.01, SE 0.01, P = 0.0039, F‐test = 9; R2 = 0.43, P = 0.0001, F‐test = 17.6. After 6 years, for every 1 g increases in the fat intake, BMI will increase by 0.01 kg/m2. | ‐ No | Adjusted for baseline BMI, birthweight, cereal introduction age, breastfeeding duration, dietary variety score 42‐84 months, adiposity rebound, picky eater at age 6 years, sedentary activity at ages 6 and 7 years, foods liked at age 8 years, mother's BMI and father's BMI. |
| 2 years; regression | BMI | z‐score | 9 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6 and 9 years) | NR | n overall = 243; regression result. β = 0.122, P > 0.1; R2 = 0.38, P < 0.0001. After 9 years, increase in the total fat intake will increase BMI by 0.122 z‐score. | + Yes | Adjusted for baseline BMI‐z score, gender and parental BMI. |
| 10.1 years; regression | BMI | kg/m2, 10‐years change | 10 | Total fat intake (single 3‐day dietary records at 1, 2, 3, 4, 5, 7, 8 and 10 years) × baseline IR | %TE | n white girls = 241; regression result. B = 0.029, SE 0.0028, P < 0.0001, partial R2 = 27. After 10 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.029 kg/m2 in white girls. | + Yes | Adjusted for age, BMI, IR and maturation stage at baseline; change in IR over 10 years' follow‐up; percentage of calories from protein, fat and CHO (mean of interviews) during 10 years' follow‐up; and interaction terms (nutrients × baseline IR). |
| 10.1 years; regression | BMI | kg/m2, 10‐years change | 10 | Total fat intake (single 3‐day dietary records at 1, 2, 3, 4, 5, 7, 8 and 10 years) × baseline IR | %TE | n black girls = 280; regression result. B = 0.012, SE 0.0032, P = 0.0002, partial R2 = 3.6. After 10 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.012 kg/m2 in black girls. | ‐ Yes | Adjusted for age, BMI, IR and maturation stage at baseline; change in IR over 10 years' follow‐up; percentage of calories from protein, fat and CHO (mean of interviews) during 10 years' follow‐up; and interaction terms (nutrients × baseline IR). |
| BMI at > 10 years: 2 cohort studies; 2 analyses (n = 330) in boys and girls aged 2‐3 years | ||||||||
| 2 years; regression | BMI | z‐score | 13 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6, 9, 11 and 13 years) | NR | n overall = 218; regression result. β = 0.16, 0.05 < P ≤ 0.1; R2 = 0.23, P < 0.0001. After 13 years, increase in the total fat intake will increase BMI by 0.16 z‐score. | + Yes | Adjusted for baseline BMI‐z score, gender, mother's BMI and father's BMI. |
| 3.2 years; mean end values per group | BMI | z‐score | 17 | Total fat intake (single 3‐day weighed dietary record at baseline and each year follow‐up) | LF (32%TE); HF (40%TE) | n overall = 112 (LF = 55; HF = 57); mean end values (SD). Baseline: LF = 0.36 (0.75); HF = 0.07 (0.81). At 17 years: LF = 0.23 (0.9); HF = 0.11 (1.09). After 17 years, on average BMI decrease 0.13 z‐score in the LF (32%TE) group while increase 0.04 z‐score in the HF (40%TE) group. | + No | No matching reported. No adjustments for prognostic variables. |
aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome.
bUnpublished data provided by study authors.
c"Energy dense, high fat, low fibre" dietary pattern reflected high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes, the high intake of these foods increase the individual’s dietary pattern z‐score.
dOverweight/obese was defined by IOTF for children aged 14 years (boys, BMI > 22.62 kg/m2; girls, BMI > 23.34 kg/m2), and aged 17 years (boys, BMI > 24.46 kg/m2; girls, BMI > 24.70 kg/m2).
%TE: percentage of total energy; B: unstandardised beta‐coefficient; β: standardised beta‐coefficient; BMI: body mass index; CHO: carbohydrate; CI: confidence interval; df: degrees of freedom; FFQ: Food Frequency Questionnaire; HF: high fat; IR: insulin resistance; IOTF: International Obesity Task Force; LF: low fat; MD: mean difference; n: number of participants; NA: not applicable; NR: not reported; NS: not significant; OR: odds ratio; SD: standard deviation; SE: standard error; SES: socioeconomic status; TV: television.
At one year follow‐up, two studies reported associations of fat intake (continuous) with BMI (kg/m2); Schwandt 2011 in children who were seven years old at baseline (n = 411), while Berkey 2005 reported one‐year change in BMI in children who were nine to 14 years old at baseline (girls n = 6149, boys n = 4620). Bogaert 2003 reported this association using standardised BMI (z‐score) as an outcome in children who were nine years old at baseline (n = not reported). The large Berkey 2005 study, which adjusted for TE and most important prognostic variables, reported no association between total fat intake (in grams) and BMI in boys and girls.
At 1 to 2 years follow‐up, seven studies (10 analyses; n = 3347) reported on BMI in children between two and 13 years of age. Ambrosini 2016 (boys n = 383, girls n = 323) and Lee 2001 (n = 192 girls) reported the relationship between BMI, two‐year BMI change or BMI z‐scores, and lower and higher fat intake groups (lowest and highest quintiles of fat intake and ≤ 30%TE and > 30%TE) in children who were four to five years old at baseline, while Davison 2001; Klesges 1995; Lee 2012; and Setayeshgar 2017 used continuous fat intake (%TE and per 10 g) in their analyses of children who were four to 13 years old at baseline. The four studies that adjusted for TE intake reported the following: "Percentage of fat intake, baseline BMI, family risk of overweight, mothers’ BMI, fathers’ enjoyment of activity explained 26% of the variance in the change of BMI." (Davison 2001; n = 168); for every 1% increase in energy intake from total fat, BMI increased by 0.021 kg/m2 in first graders (mean age: 7.3 years) (n = 474), and for every 1% increase in energy intake from total fat, BMI decreased by 0.007 kg/m2 in fourth graders (mean age: 10 years) (n = 1030) (Lee 2012). Greater total fat intake increased BMI by 0.079 z‐scores (Magarey 2001; n = 155); and for every 10 g increase in total fat intake, BMI increased by 0.009 z‐scores (Setayeshgar 2017; n = 330).
Three studies did not adjust for energy intake, and found the following:
-
average BMI in boys (n = 383) decreased by 0.5 kg/m2 in the low‐fat group (30.4%TE) and by 0.6 kg/m2 in the high‐fat group (41.8%TE) (Ambrosini 2016);
-
average BMI in girls (n = 323) decreased by 0.5 kg/m2 in the low‐fat group (30.4%TE) and by 0.3 kg/m2 in the high‐fat group (41.8%TE) (Ambrosini 2016);
-
for every 1% increase in energy intake from total fat in year two to three of follow‐up, BMI decreased by 0.04 kg/m2;
-
for every 1% increase in energy intake from baseline total fat, BMI increased by 0.034 kg/m2 (Klesges 1995; n = 146);
-
low‐fat intake (≤ 30%TE) resulted in 0.4 kg/m2 smaller increase in BMI on average compared to high‐fat intake (> 0%TE) in girls (Lee 2001; n = 192).
Various continuous and binary measures of BMI were related to a high‐fat dietary pattern z‐score (Appannah 2015), and other continuous measures of total fat intake (Brixval 2009; Cohen 2014; Jago 2005; Obarzanek 1997 (cohort)), or lower and higher fat intake groups (Shea 1993), at 2 to 5 years follow‐up in children aged two to 14 years. The four studies that adjusted their analyses for TE intake found the following:
-
for every 1% increase in energy intake from total fat, BMI decreased by 0.63 z‐scores in boys (n = 181), but increased by 0.07 z‐scores in girls (n = 217) (Brixval 2009);
-
Jago 2005 (n = 133) reported that "Dietary factors were not associated with BMI across the three study years";
-
for every 1% increase in energy intake from total fat, BMI decreased by 0.00008 kg/m2 (Obarzanek 1997 (cohort); n = 632);
-
an increase in total fat intake increased BMI by 0.087 z‐scores (Magarey 2001; n = 152).
The two studies that did not adjust for energy intake reported the following:
-
low‐fat intake (≤ 30%TE) resulted in a 0.02 kg/m2 per year greater increase in BMI on average compared to high‐fat intake (> 30%TE) (Shea 1993; n = 215);
-
for every 1% increase in energy intake from total fat, BMI decreased by 0.01 percentile in girls (Cohen 2014; n = 265).
In the Appannah 2015 study, where energy adjustment was not applicable as it was part of the dietary pattern exposure, the authors found that for every 1 z‐score increase in the energy‐dense, high‐fat and low‐fibre dietary pattern, BMI increased by 0.03 z‐scores in boys and by 0.99 z‐scores in girls. In different analyses the odds ratio (OR) for being overweight/obese was 1.04 greater in boys and 1.02 greater in girls with higher dietary pattern z‐scores, compared to boys and girls with lower dietary pattern z‐scores (girls n = 649, boys n = 699).
In studies following children for 5 to 10 years, fat intake (%TE or grams) was related to BMI z‐scores (Magarey 2001), change in BMI (Brixval 2009; Morrison 2008), or absolute BMI (Skinner 2004). The three studies that adjusted for TE intake reported the following:
-
for every 1% increase in energy intake from total fat, BMI decreased by 0.011 z‐scores in boys (n = 147) (Brixval 2009), but.
-
for every 1% increase in energy intake from total fat, BMI increased by 0.005 z‐scores in girls (n = 177) (Brixval 2009);
-
an increase in total fat intake increased BMI by 0.122 z‐scores (Magarey 2001; n = 243);
-
for every 1% increase in energy intake from total fat, BMI increased by 0.029 kg/m2 in white girls (n = 241) and by 0.012 kg/m2 in black girls (n = 280) (Morrison 2008).
Without adjusting for energy intake, Skinner 2004 (n = 70) reported that for every 1 g increase in the fat intake, BMI increased by 0.01 kg/m2.
After 13 years of follow‐up and with adjustment for energy intake, Alexy 2004 (n = 112) reported that an increase in the total fat intake increased BMI by 0.16 z‐scores. Without adjustment for energy, Magarey 2001 (n = 218) found that after 17 years, on average BMI decreased 0.13 z‐scores in the low‐fat group (32%TE), but increased 0.04 z‐scores in the high‐fat group (40%TE).
Waist circumference
We have summarised standardised and unstandardised waist circumference outcomes, fat intake exposure variables used, and results of reported associations within each time range, including adjustments made, in Table 8.
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted? (yes/no) | Matched groups or adjusted for (or both) | |
| Waist circumference at > 1to 2 years: 1 cohort study; 1 analysis (n = 310) in boys and girls aged 13 years | |||||||||
| 12.5 years; regression | WC | cm | 2 | Total fat intake (single 24‐hour recall at baseline) | per 10 g | n overall = 310, regression result. B = 0.31 (95% CI 0.08 to 0.58), P ≤ 0.05. After 2 years, for every 10‐g increase in the total fat intake of children, WC will increase by 0.31 cm. | + No | Age, gender, baseline BMI z‐score, baseline WC, moderate to vigorous physical activity, vegetables and fruit, fibre, milk, sodium and added sugar. | |
| Waist circumference at > 2to 5 years: 1 cohort study; 4 analyses (n = 2680) in boys and girls aged 14 years | |||||||||
| 14 years; regression and OR higher vs lower dietary pattern z‐score | WC | WC ≥ 80 cm, odds | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n boys = 697, regression result. OR = 1 (95% CI 0.82 to 1.22). After 3 years, the ratio of odds that WC is ≥ 80 cm is the same in boys with higher dietary pattern z‐scores compared to the odds in boys with lower dietary pattern z‐scores, during the period from 14 to 17 years of age. | 0 NA; exposure includes energy intake | Age, dietary misreporting, physical fitness, smoking and BMI z‐score. | |
| 14 years; regression and OR higher vs lower dietary pattern z‐score | WC | WC ≥ 80 cm, odds | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n girls = 643, regression result. OR = 1.28 (95% CI 1.00 to 1.63). After 3 years, the ratio of odds that WC is ≥ 80 cm is 1.28 greater in girls with higher dietary pattern z‐scores compared to the odds in girls with lower dietary pattern z‐scores, during the period from 14 to 17 years of age. | + NA; exposure includes energy intake | Age, dietary misreporting, physical fitness, smoking and BMI z‐score. | |
| 14 years; regression | WC | z‐score | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n boys = 697, regression result. β = 0.003 (95% CI ‐0.02 to 0.03). After 3 years, for every 1 unit increase in z‐score of the energy‐dense, high‐fat and low‐fibre dietary pattern of boys, WC will increase by 0.003 z‐scores. | + NA; exposure includes energy intake | Age, dietary misreporting, physical fitness, smoking and BMI z‐score. | |
| 14 years; regression | WC | z‐score | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n girls = 643, regression result. β = 0.04 (95% CI 0.01 to 0.07). After 3 years, for every 1 unit increase in z‐score of the energy‐dense, high‐fat and low‐fibre dietary pattern of girls, WC will increase by 0.04 z‐scores. | + NA; exposure includes energy intake | Age, dietary misreporting, physical fitness, smoking and BMI z‐score. | |
| Waist circumference at > 5to 10 years: 1 cohort study; 2 analyses (n = 512) in girls aged 10 years | |||||||||
| 10.1 years; regression | WC | cm, 10‐years change | 10 | Total fat intake (single 3‐day dietary records at 1, 2, 3, 4, 5, 7, 8 and 10 years) × baseline IR | %TE | n white girls = 236. B = 0.053, SE 0.0065, P < 0.0001. After 10 years, for every 1% increase in energy intake from total fat in white girls, WC will increase by 0.053 cm. | + Yes | Age, WC, IR, and maturation stage at baseline; change in IR over 10‐years follow‐up; percentage of calories from protein, fat, and CHO (mean of interviews) during 10‐years follow‐up; and interaction terms (nutrients × baseline IR). | |
| 10.1 years; regression | WC | cm, 10‐years change | 10 | Total fat intake (single 3‐day dietary records at 1, 2, 3, 4, 5, 7, 8 and 10 years) × baseline IR | %TE | n black girls = 276. B = 0.028, SE 0.0056, P < 0.0001. After 10 years, for every 1% increase in energy intake from total fat in black girls, WC will increase by 0.028 cm. | + Yes | "Age, waist circumference, IR, and maturation stage at baseline; change in IR over 10‐y follow‐up; percentage of calories from protein, fat, and CHO (mean of interviews) during 10‐y follow‐up; and interaction terms (nutrients baseline IR)." | |
aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome.
b"Energy dense, high fat, low fibre" dietary pattern reflected high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes, the high intake of these foods increase the individual’s dietary pattern z‐score.
%TE: percentage of total energy; B: unstandardised beta‐coefficient; β: standardised beta‐coefficient; BMI: body mass index; CHO: carbohydrate; CI: confidence interval; FFQ: Food Frequency Questionnaire; IR: insulin resistance; n: number of participants; NA: not applicable; OR: odds ratio; WC: waist circumference.
Only Setayeshgar 2017 (n = 310) reported waist circumference in relation to total fat intake per 10 g at two years. With no adjustment for total energy intake, they found that for every 10 g increase in total fat intake of children, waist circumference increased by 0.31 cm. Appannah 2015 reported the association between a high‐fat dietary pattern z‐scores and various measures of waist circumference at 2 to 5 years, and found that after three years, for every one unit increase in z‐score of the energy‐dense, high‐fat and low‐fibre dietary pattern, waist circumference in boys (n = 697) increased by 0.003 z‐scores, and waist circumference in girls (n = 643) increased by 0.04 z‐scores. Morrison 2008 related total fat intake (%TE) to 10‐year change in waist circumference (cm), and, with TE intake adjustment, reported that for every 1% increase in energy intake from total fat, waist circumference increased by 0.053 cm in white girls (n = 236), and by 0.028cm in black girls (n = 276).
Body fat and fat mass index
We have summarised the various outcomes, exposures and results of reported associations within each time range, for body fat, in Table 9, and for fat mass index in Table 10, including adjustments made.
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (years) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) | |||
| Body fat at 1 year: 1 cohort study; 1 analysis (n = 411) in boys and girls aged 7 years | |||||||||||
| 6.8 years; regression | Body fat (skinfold thickness) | % | 1 | Total fat intake (single 7‐day weighed dietary record at baseline and 1 year) | g | n overall = 411, regression result. B = 0.011, SE 0.017, P < 0.05. After 1 year, for every 1 g increase in the total fat intake of children, body fat will increase by 0.01%. | + No | Adjusted for age, gender and physical activity. | |||
| Body fat at > 1to 2 years: 1 cohort study; 1 analysis (n = 625) in boys and girls aged 5 years | |||||||||||
| 5.2 years; regression | Body fat (DEXA) | kg | 2 | Energy‐dense, high‐fat, low‐fibre dietary patternc (single 3‐day dietary record at baseline and 2 years) | z‐score | n overall = 625, regression result. B = 0.28 (95% CI 0.05 to 0.53), P = 0.02. After 2 years, for every 1 unit increase in the dietary pattern z‐score of children, body fat will increase by 0.28 kg. | + NA; exposure includes energy intake | Adjusted for height at age 9 years, gender, misreporting status, maternal BMI, maternal education (5 categories), overweight status (by BMI) at baseline and television watching at 54 months. | |||
| Body fat at > 2to 5 years: 3 cohort studies; 6 analyses (n = 968) in boys and girls aged 2‐14 years | |||||||||||
| 13.9 years; regression | Body fat (skinfold thickness, BIA) | % | 3‐5 | Total fat intake (single FFQ at baseline and once during follow‐up period) | %TE | n girls = 265, regression result. B = ‐0.005, SE 0, P = 0.03. After 3‐5 years, for every 1 % increase in energy intake from total fat of girls, body fat will decrease by 0.005%. | ‐ No | Adjusted for age, ethnicity, protein calories, CHO calories, physical activity, physical inactivity and SES. | |||
| 5.2 years; regression | Body fat (DEXA) | kg | 4 | Energy‐dense, high‐fat, low‐fibre dietary patternc (single 3‐day dietary record at baseline and 2 years) | z‐score | n overall = 483, regression result. B = 0.15 (95 % CI ‐0.15 to 0.45), P = 0.34. After 4 years, for every 1 unit increase in the dietary pattern z‐score of children, body fat will increase by 0.15 kg. | + NA; exposure includes energy intake | Adjusted for height at age 9 years, gender, misreporting status, maternal BMI, maternal education (5 categories), overweight status (by BMI) at baseline and television watching at 54 months. | |||
| 2 years; regression | Body fat (DEXA) | % | 4 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, and yearly at 4 years) | NR | n overall = 53, regression result. B = 0.619, SE 0.261, P = 0.02, F‐test = 5.63, R2 = 0.51, p = 0.0001, F‐test = 7.88. After 4 years, for every 1 unit increase in total fat intake of children, body fat will increase by 0.61%. | + No | Adjusted for baseline BMI, parental BMI, gender, protein, calcium and monounsaturated fat. | |||
| 2 years; regression | Body fat (DEXA) | g | 4 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, and yearly at 4 years) | NR | n overall = 53, regression result. B = 178.65, SE 70.06, P = 0.01, F‐test = 6.5, R2 = 0.51, P = 0.0001, F‐test = 9.84. After 4 years, for every 1 unit increase in total fat intake of children, body fat will increase by 178 g. | + No | Adjusted for baseline BMI, parental BMI, gender, protein, calcium and monounsaturated fat. | |||
| 2 years; regression | Body fat (DEXA) | % | 4 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, and yearly at 4 years). | Number of servings | n overall = 53, regression result. B = 0.465, SE 0.255, P = 0.07, F‐test = 3.34. R2 = 0.47, P = 0.0001, F‐test = 6.93. After 4 years, for every 1 unit increase in the number of fat servings, body fat will increase by 0.47%. | + No | Adjusted for baseline BMI, parental BMI, gender, protein, calcium and monounsaturated fat. | |||
| 2 years; regression | Body fat (DEXA) | g | 4 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, and yearly at 4 years). | Number of servings | n overall = 53, regression result. B = 136.48, SE 69.74, P = 0.06, F‐test = 3.83, R2 = 0.47, p = 0.0001, F‐test = 8.31. After 4 years, for every 1 unit increase in the number of fat servings, body fat will increase by 136 g. | + No | Adjusted for baseline BMI, parental BMI, gender, protein, calcium and monounsaturated fat. | |||
| Body fat at > 5to 10 years: 1 cohort study; 3 analyses (n = 156) in boys and girls aged 2 years | |||||||||||
| 2 years; regression | Body fat (DEXA) | % | 6 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, every year during 4, 5 and 6 years). | g | n overall = 52, regression result. B = 0.08, partial R2 = 0.06, P = 0.001, F‐test = 4.66, R2 = 0.336, P = 0.002. After 6 years, for every 1 g increase in total fat intake of children, body fat will increase by 0.08%. | + No | Adjusted for gender, sedentary activity, intakes of calcium and polyunsaturated fat. | |||
| 2 years; regression | Body fat (DEXA) | % | 6 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day dietary record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, every year during 4, 5 and 6 years). | g | n overall = 52, regression result. B = 0.09, partial R2 = 0.02, P = 0.001, F‐test = 4.37, R2 = 0.322, P = 0.002. After 6 years, for every 1 g increase in total fat intake, body fat will increase by 0.09%. | + No | Adjusted for gender, sedentary activity, calcium intake, and polyunsaturated fat intake and father's BMI. | |||
| 2 years; regression | Body fat (DEXA) | kg | 6 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, every year during 4, 5 and 6 years) | g | N overall = 52, regression result. B = 0.034, partial R2 = 0.06, P = 0.01, F‐test = 4.19, R2 = 0.26, P = 0.006. After 6 years, for every 1 g increase in total fat intake of children, body fat will increase by 0.03 kg. | + No | Adjusted for sedentary activity, calcium intake and polyunsaturated fat intake. | |||
aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction, inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association between total fat intake and the outcome.
bUnpublished data provided by study authors.
c"Energy dense, high fat, low fibre" dietary pattern reflected high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes, the high intake of these foods increase the individual's dietary pattern z‐score.
%TE: percentage of total energy; B: unstandardised beta‐coefficient; BIA: bioelectrical impedance, BMI: body mass index; CHO, carbohydrate; CI: confidence interval; DEXA: dual energy X‐ray absorptiometry; FFQ: food frequency questionnaire; n: number of participants; NA: not applicable; NR: not reported; SD: standard deviation; SE: standard error; SES: socioeconomic status.
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| Fat mass index at > 2to 5 years: 1 cohort study; 1 analysis (n = 4002) in boys and girls aged 8 years | ||||||||
| 7.5 years; regression | Fat mass indexb | z‐score | 4 | Energy‐dense, high‐fat, low‐fibre dietary patternc (single 3‐day dietary records at baseline and 2 years) | z‐score | n overall = 4002, regression result. β = 0.07 (95% CI 0.05 to 0.10), P ≤ 0.0001. After 4 years, for every 1 z‐score increase in the dietary pattern, the fat mass index will increase by 0.07 z‐scores. | + NA; exposure includes energy intake | Adjusted for gender, age at dietary assessment, dietary misreporting, total physical activity at 11 years, maternal prepregnancy BMI and maternal education. |
| Fat mass index at > 5to 10 years: 1 cohort study; 5 analyses (n = 21,542) in boys and girls aged 8 years | ||||||||
| 7.5 years; regression | Fat mass indexb | z‐score | 8 | Energy‐dense, high‐fat, high‐sugar, low‐fibre dietary patternc (single 3‐day dietary record at baseline, 3 and 6 years) | z‐score | n overall = 4729, regression result. β = 0.04 (95% CI 0.01 to 0.08), P = 0.028. After 8 years, for every 1 z‐score increase in the dietary pattern, the fat mass index will increase by 0.04 z‐scores. | + NA; exposure includes energy intake | Adjusted for age, gender, dietary misreporting, physical activity and maternal social class. |
| 7.5 years; regression | Fat mass indexb | z‐score | 8 | Non‐energy‐dense, high‐sugar, LF dietary patternd (single 3‐day dietary record at baseline, 3 and 6 years) | z‐score | n overall = 4729, regression result. β = ‐0.03 (95% CI ‐0.07 to 0.02), P = 0.22. After 8 years, for every 1 z‐score increase in the dietary pattern, the fat mass index will decrease by 0.03 z‐scores. | ‐ NA; exposure includes energy intake | Adjusted for age, gender, dietary misreporting, physical activity and maternal social class. |
| 7.5 years; regression | Fat mass indexb | z‐score | 8 | Energy‐dense, high‐fat, low‐fibre dietary patternc (single 3‐day dietary record at baseline, 3 and 6 years) | z‐score | n overall = 2626, regression result. β = 0.06 (95% CI 0.03 to 0.10), P = 0.0004. After 8 years, for every 1 z‐score increase in the dietary pattern, the fat mass index will increase by 0.06 z‐scores. | + NA; exposure includes energy intake | Adjusted for gender, age at dietary assessment, dietary misreporting, total physical activity at 11 years, maternal pre‐pregnancy BMI and maternal education. |
| 7.5 years; regression | Fat mass indexb | FMI z‐score > 80th percentile; odds | 8 | Energy‐dense, high‐fat, high‐sugar, low‐fibre dietary patternc (single 3‐day dietary record at baseline, 3 and 6 years) | z‐score | n overall = 4729, regression result. OR 1.11 (95% CI 0.97 to 1.28), P = 0.14. After 8 years, the ratio of odds for having FMI z‐score > 80th percentile is 1.11 greater in children with higher dietary pattern z‐scores compared to the odds in children with lower dietary pattern z‐scores. | + NA; exposure includes energy intake | Adjusted for age, gender, dietary misreporting, physical activity and maternal social class. |
| 7.5 years; regression | Fat mass indexb | FMI z‐score > 80th percentile; odds | 8 | Non‐energy‐dense, high‐sugar, LF dietary patternd (single 3‐day dietary record at baseline, 3 and 6 years) | z‐score | n overall = 4729, regression result. OR 0.92 (95% CI 0.78 to 1.09), P = 0.34. After 8 years, the ratio of odds for having FMI z‐score > 80th percentile is 0.92 smaller in children with higher dietary pattern z‐scores compared to the odds in children with lower dietary pattern z‐scores. | ‐ NA; exposure includes energy intake | Adjusted for age, gender, dietary misreporting, physical activity and maternal social class. |
aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome;
bFMI was calculated by dividing fat mass (measured by dual‐energy X‐ray Absorptiometry) (kg) by height (m) raised to the optimum power (calculated by using log‐log regression analysis) to remove any residual correlation between fat mass and height;
c"Energy‐dense, high‐fat, low‐fibre" dietary pattern reflected high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes, the high intake of these foods increase the individual’s dietary pattern z‐score.
dNon‐energy‐dense, high‐sugar, low‐fat dietary pattern reflected higher intakes of sugary foods including sugar‐sweetened beverages, fruit juices, ready‐to‐eat breakfast cereals (low‐fibre breakfast cereals) and low intakes of whole milk, margarines and oils, cheese and crisps.
β: standardised beta‐coefficient; BMI: body mass index; FMI: Fat Mass Index ; n: number of participants; NA: not applicable; OR: odds ratio.
Schwandt 2011 (n = 411) reported the association between body fat (%; calculated from skinfold thickness) and total fat intake (g) at one‐year follow‐up, and found that for every 1 g increase in children's total fat intake, body fat increased by 0.01% (with no energy intake adjustment). Ambrosini 2016 reported the link between body fat (kg; measured by dual energy X‐ray absorptiometry (DEXA)) and high‐fat dietary pattern z‐scores at two years, where for every one unit increase in the dietary pattern z‐score, children's body fat increased by 0.28 kg (n = 625), and at four years where for every one unit increase in the dietary pattern z‐score, body fat increased by 0.15 kg (n = 483). For this later time range, Cohen 2014 and Skinner 2004 related various measures of total fat intake to body fat (% and g). With no energy adjustment, Skinner 2004 found that after four years (n = 53), for every one unit increase in children's total fat intake, body fat increased by 0.61% or 178 g (both measured by DEXA), and after six years (n = 52), for every 1 g increase in total fat intake, body fat increased by 0.09% or 30 g (both measured by DEXA).
Ambrosini 2016 was the only study to report analyses on various measures of fat mass index in relation to a high‐fat dietary pattern at 2 to 5 years (one analysis, n = 4002) and to a high‐fat and a low‐fat dietary pattern at 5 to 10 years (four analyses, n = 2626 to 4729). Fat mass index was calculated by dividing fat mass (kg; measured by DEXA) by height (m) raised to the optimum power (calculated by using log‐log regression analysis) to remove any residual correlation between fat mass and height.
This trial used two dietary patterns, high‐fat and low‐fat. The energy‐dense, low‐fibre high‐fat dietary pattern reflected high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes. High intake of these foods increases the individuals' dietary pattern z‐score. The non‐energy‐dense, high‐sugar, low‐fat dietary pattern reflected higher intakes of sugary foods including sugar‐sweetened beverages, fruit juices, ready‐to‐eat breakfast cereals (low‐fibre breakfast cereals) and low intakes of whole milk, margarines and oils, cheese and crisps. After four years, for every one z‐score increase in the high‐fat dietary pattern, the fat mass index increased by 0.07 z‐scores. After eight years, analyses showed that for every one z‐score increase in the high‐fat dietary pattern, the fat mass index increased by 0.06 z‐scores, and in a different analysis that the ratio of odds for having fat mass index z‐score greater than the 80th percentile was 1.11 greater in children with greater high‐fat dietary pattern z‐scores compared to the odds in children with smaller z‐scores. After eight years, for every one z‐score increase in the low‐fat dietary pattern, the fat mass index decreased by 0.03 z‐scores, and in a different analysis, the OR for having a fat mass index z‐score greater than the 80th percentile was 0.92 smaller in children with greater low‐fat dietary pattern z‐scores compared to the odds in children with smaller z‐scores (Ambrosini 2016).
Skinfold thickness
We have summarised sums of multiple skinfold thickness measurements (standardised and unstandardised), fat intake exposure variables and results of reported associations within each time range in Table 11. We have summarised single skinfold thickness measurements (subscapular and triceps) in Table 12, including adjustments made.
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| Sum of 4 skinfolds (BC, TC, SC, SI) at 1 year: 1 cohort study; 1 analysis (n = NR) in boys and girls aged 6 years | ||||||||
| 6.2 years; mean end values per group | Sum of skinfolds (BC, TC, SS, SI) | mm | 1 | Total fat intake (multiple 24‐hour recalls at baseline, 3 and 6 months and 1 year) | LF quintile (24%TE); HF quintile (34%TE) | n overall = NR (LF = NR, HF = NR), mean end values (95% CI). Baseline: LF = 24.7 (95% CI 23 to 26.5); HF = 28.8 (95% CI 26.1 to 31.8). At 1 year: (reported in the figure without exact values), LF = lower than baseline; HF = greater than baseline. After 1 year, the sum of skinfolds will decrease in children with a low‐fat intake, and increase in children with high‐fat intake | + No | No matching reported. No adjustment for prognostic variables. |
| Sum of 4 skinfolds (BC, TC, SC, SI) at > 1to 2 years: 1 cohort study; 1 analysis (n = 126) in boys and girls aged 2 years | ||||||||
| 2 years; mean end values per group | Sum of skinfolds (TC, BC, SS, SI) | mm | 2 | Total fat intake (single 3‐day weighed dietary record at baseline and 2 years) | LF < 30%TE; HF > 35%TE | n overall = 126 (LF = 14, HF = 112), mean end values (SD). Baseline: LF = 33.4 (6.8); HF = 32.8 (6.3). At 2 years: LF (n = 20) = 31 (9.2); HF (n = 76) = 31.4 (6.3); P > 0.05. After 2 years, the sum of skinfolds of children with LF intakes will decrease by 2.4 mm on average, and by 1.4 mm in children with HF intake. | + No | No matching reported. No adjustment for prognostic variables. |
| Sum of 4 skinfolds at > 2to 5 years: 1 cohort study; 1 analysis (n ˜ 126) in boys and girls aged 2 years | ||||||||
| 2 years; mean end values per group | Sum of skinfolds (TC, BC, SS, SI) | mm | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | LF < 30%TE; HF > 35%TE | n overall = 126 (LF = 14, HF = 112), mean end values (SD). Baseline: LF = 33.4 (6.8); HF = 32.8 (6.3); P > 0.05. At 4 years: LF (n = 14) = 27.2 (8); HF (n = 88) = 29.2 (8.9); P > 0.05. After 4 years, the sum of skinfolds of children with LF intakes will decrease by 6.2 mm on average, and by 3.6 mm in children with HF intake | + Yes | No matching reported. No adjustment for prognostic variables. |
| Sum of 4 skinfolds at > 5to 10 years: 1 cohort study; 1 analysis (n = 126) in boys and girls aged 2 years | ||||||||
| 2 years; mean end values per group | Sum of skinfolds (TC, BC, SS, SI) | mm | 6 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6 years) | LF < 30%TE; HF > 35%TE | n overall = 126 (LF=14, HF=112), mean end values (SD). Baseline LF = 33.4 (6.8); HF = 32.8 (6.3), P > 0.05. At 6 years: LF (n = 13) = 32.8 (13.3); HF (n = 72) = 31.8 (12.8), P > 0.05. After 6 years, the sum of skinfolds of children with LF intakes will decrease by 0.6 mm on average, and by 1 mm in children with HF intake. | ‐ No | No matching reported. No adjustment for prognostic variables. |
| Sum of 3 skinfolds at > 2to 5 years: 1 cohort study; 1 analysis (n = NR) in boys and girls aged 10 years | ||||||||
| 9.6 years; regression | Sum of skinfolds (TC, SS, SI) | mm | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | %TE | n overall = NR; regression result. B = ‐0.005, P = 0.2. After 3 years, for every 1% increase in energy intake from total fat of children, the sum of skinfolds will decrease by 0.005 mm | ‐ Yes | Adjusted for gender, physical activity, treatment, visit number, other sources of energy than fat, and for interactions: fat intake‐by‐treatment, fat intake‐by‐sex, fat intake‐by‐visit number and visit number‐by‐treatment. |
| Sum of 2 skinfolds at > 1to 2 years: 1 cohort study; 1 analysis (n = 192) in girls aged 5 years | ||||||||
| 5 years; mean change per group | Sum of skinfolds (TC, SS) | mm | 2 | Total fat intake (multiple 24‐hour recall at baseline) | LF ≤ 30%TE, HF > 30%TE | n girls = 192 (LF = 84; HF = 108); mean change (SD). Baseline: NR. LF = 0.9 (3.67), HF = 2.1 (5.2); P < 0.05. MD ‐1.2 (95% CI ‐2.46 to 0.06). After 2 years, the sum of skinfolds of girls with LF intake will increase on average by 1.2 mm less than girls with HF intake. | + No | No matching reported. No adjustment for prognostic variables. |
aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction, inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome.
%TE: percentage of total energy; BC: biceps; CI: confidence interval; HF: high fat; LF: low fat; MD: mean difference; n: number of participants; NA: not applicable; NR: not reported; SD: standard deviation; SI: supra‐ileac; SS: subscapular; TC: triceps.
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| Subscapular skinfold at > 1to 2 years: 1 cohort study; 1 analysis (n = 155) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Subscapular skinfold | z‐score | 2 | Total fat intake (single 3‐day weighed dietary record at baseline and 2 years) | NR | n overall = 155; regression result. β = 0.081, P > 0.1, R2 = 0.47, P < 0.001. After 2 years, increase in the total fat intake will increase subscapular skinfold by 0.081 z‐score | + Yes | Adjusted for subscapular z‐score at baseline, energy intake, gender, mother' subscapular and father' subscapular. |
| Subscapular skinfold at > 2to 5 years: 1 cohort study; 1 analysis (n = 152) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Subscapular skinfold | z‐score | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | NR | n overall = 152; regression result. β = 0.072, P > 0.1, R2 = 0.38, P < 0.001. After 4 years, increase in the total fat intake will increase subscapular skinfold by 0.072 z‐score. | + Yes | Adjusted for subscapular z‐score at baseline, energy intake, gender, mother' subscapular and father' subscapular. |
| Subscapular skinfold at > 5to 10 years: 1 cohort study; 1 analysis (n = 243) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Subscapular skinfold | z‐score | 9 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6 and 9 years) | NR | n overall = 243; regression result. β = 0.069, P > 0.1, R2 = 0.26, P < 0.001. After 9 years, increase in the total fat intake will increase subscapular skinfold by 0.069 z‐score. | + Yes | Adjusted for subscapular z‐score at baseline, energy intake, gender, mother' subscapular and father' subscapular. |
| Subscapular skinfold at > 10 years: 1 cohort study; 1 analysis (n = 218) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Subscapular skinfold | z‐score | 13 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6, 9, 11 and 13 years) | NR | n overall = 218; regression result. β = 0.233, P ≤ 0.01. After 13 years, increase in the total fat intake will increase subscapular skinfold by 0.233 z‐score. | + Yes | Adjusted for subscapular z‐score at baseline, energy intake, gender, mother' subscapular and father' subscapular. |
| Triceps skinfold at > 1to 2 years: 1 cohort study; 1 analysis (n = 155) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Triceps skinfold | z‐score | 2 | Total fat intake (single 3‐day weighed dietary record at baseline and 2 years) | NR | n overall = 155; regression result. β = 0.038, P > 0.1, R2 = 0.27, P ≤ 0.001. After 2 years, increase in the total fat intake will increase triceps skinfold by 0.038 z‐score. | + Yes | Adjusted for triceps z‐score at baseline, gender, mother's triceps and father's triceps. |
| Triceps skinfold at > 2to 5 years: 1 cohort study; 1 analysis (n = 152) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Triceps skinfold | z‐score | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | NR | n overall = 152; regression result. Β = 0.11, P > 0.1, R2 = 0.043, P > 0.01. After 4 years, increase in the total fat intake will increase triceps skinfold by 0.11 z‐score | + Yes | Adjusted for triceps z‐score at baseline, gender, mother's triceps and father's triceps. |
| Triceps skinfold at > 5to 10 years: 1 cohort study; 1 analysis (n = 243) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Triceps skinfold | z‐score | 9 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6 and 9 years) | NR | n overall = 243; regression result. β = 0.059, P > 0.1; R2 = 0.12, P ≤ 0.01. After 9 years, increase in the total fat intake will increase triceps skinfold by 0.059 z‐score | + Yes | Adjusted for triceps z‐score at baseline, gender, mother's triceps and father's triceps. |
| Triceps skinfold at > 10 years: 1 cohort study; 1 analysis (n = 218) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Triceps skinfold | z‐score | 13 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6, 9, 11 and 13 years) | NR | n overall = 218; regression result. β = 0.164; 0.05 < P ≤ 0.1. After 13 years, increase in the total fat intake will increase triceps skinfold by 0.164 z‐score | + Yes | Adjusted for triceps z‐score at baseline, gender, mother's triceps and father's triceps. |
aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome;
B: unstandardised beta‐coefficient; β: standardised beta‐coefficient; n: number of participants; NR: not reported.
Lee 2001 reported the mean change in the sum of triceps and subscapular skinfolds in lower fat (< 30%TE) versus a higher fat (> 30%TE) intake groups at two years, where the sum of two skinfolds of girls with low‐fat intake increased on average by 1.2 mm less than in girls with high‐fat intake (n = 192). Obarzanek 1997 (cohort) related the sum of triceps, subscapular and supra‐ileac skinfolds to total fat intake (%TE) after three years and showed that for every 1% increase in energy intake from total fat in children, the sum of three skinfolds decreased by 0.005 mm (n = not reported). Magarey 2001 reported the mean change in the sum of biceps, triceps, subscapular and supra‐ileac skinfolds in a lower fat (< 30%TE) versus higher fat (> 35%TE) intake group after two years and saw that the sum of four skinfolds decreased by 2.4 mm on average in children with low‐fat intakes, and by 1.4 mm in children with high‐fat intake (n =126). At four years the sum of four skinfolds of children with low‐fat intakes had decreased by 6.2 mm on average, and by 3.6 mm in children with high‐fat intake (n = 126). At six years the sum of skinfolds of children with low‐fat intakes had decreased by 0.6 mm on average, and by 1 mm in children with high‐fat intake; n = 126). Tershakovec 1998 (cohort) agreed with this finding, showing that after one year the sum of skinfolds decreased in children in the lowest quintile of fat intake and increased in children in the highest quintile of fat intake.
Magarey 2001 also related total fat intake to standardised triceps and standardised subscapular skinfold thicknesses:
-
at two years when increase in the total fat intake increased triceps skinfold thickness by 0.038 z‐scores (n = 155), and subscapular skinfold thickness by 0.081 z‐scores (n = 155);
-
at four years when increase in total fat intake increased triceps skinfold thickness by 0.11 z‐scores (n = 152), and subscapular skinfold thickness by 0.072 z‐scores (n = 152);
-
at nine years when increase in total fat intake increased triceps skinfold thickness by 0.059 z‐scores (n = 243), and subscapular skinfold thickness by 0.069 z‐scores (n = 243); and
-
at 13 years when increase in total fat intake increased triceps skinfold thickness by 0.164 z‐scores (n = 218); and subscapular skinfold by 0.069 z‐scores (n = 243).
Secondary outcomes
Blood lipids and blood pressure
We have summarised results of reported associations between total fat intake and LDL‐cholesterol, HDL‐cholesterol and triglycerides within each time range, including adjustments made, in Table 13.
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| LDL‐C at > 2to 5 years: 1 cohort study; 2 analyses (n = 1163) in boys and girls aged 14 years | ||||||||
| 14 years; regression | LDL‐C | mmol/L | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n girls = 558, regression result. B = 0.04 (95% CI ‐0.01 to 0.08). After 3 years, for every 1 z‐score increase in the dietary pattern, LDL‐C will increase by 0.04 mmol/L in girls. | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 14 years; regression | LDL‐C | mmol/L | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n boys = 605, regression result. B = 0.001 (95% CI ‐0.04 to 0.03). After 3 years, for every 1 z‐score increase in the dietary pattern, LDL‐C will increase by 0.001 mmol/L in boys. | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| HDL‐C at > 2to 5 years: 2 cohort studies; 3 analyses (n = 1393) in boys and girls aged 13 and 14 years | ||||||||
| 14 years; regression; | HDL‐C | mmol/L | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n girls = 558, regression result. B = 0.02 (95% CI 0.002 to 0.04). After 3 years, for every 1 z‐score increase in the dietary pattern HDL‐C will increase by 0.02 mmol/L in girls. | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 14 years; regression; | HDL‐C | mmol/L | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n boys = 605, regression result. B = ‐0.002 (95% CI ‐0.02 to 0.01). After 3 years, for every 1 z‐score increase in the dietary pattern HDL‐C will decrease by 0.002 mmol/L in boys. | ‐ NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 12.5 years; regression; | HDL‐C | mmol/L | 3 | Total fat intake (dietary history at baseline and 3 years) | %TE | n girls = 230, regression result. β = ‐0.21, SE 0.1, P = 0.031. After 3 years, for every 1% increase in energy intake from total fat, HDL‐C will decrease by 0.21 mmol/L in girls. | ‐ Yes | Adjusted for sexual maturation, SES, cholesterol intake, CHO intake, cigarette smoking |
| Triglycerides at > 2to 5 years: 1 cohort study; 2 analyses (n = 1163) in boys and girls aged 14 years | ||||||||
| 14 years; regression | Triglycerides | % | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (multiple FFQs at baseline and 3 years) | z‐score | n girls = 558, regression result. B = 1 (95% CI 0 to 3). After 3 years, for every 1 z‐score increase in the dietary pattern, triglycerides will increase by 1% in girls. | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 14 years; regression | Triglycerides | % | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (multiple FFQs at baseline and 3 years) | z‐score | n boys = 605, regression result. B = 1 (95% CI 0 to 3). After 3 years, for every 1 z‐score increase in the dietary pattern, triglycerides will increase by 1% in boys | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome.
b"Energy dense, high fat, low fibre" dietary pattern was defined as high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes, the high intake of these foods increase the individual’s dietary pattern z‐score.
%TE: percentage of total energy; B: unstandardised beta‐coefficient; BMI: body mass index; CHO: carbohydrate; FFQ: food frequency questionnaire; LDL‐C: low‐density lipoprotein cholesterol; HDL‐C: high‐density lipoprotein cholesterol; NA: not applicable; SE: standard error; SES: socioeconomic status.
After three years, Appannah 2015 reported that:
-
for every 1 z‐score increase in the high‐fat dietary pattern, LDL‐cholesterol increased by 0.04 mmol/L in girls (n = 558); and by 0.001 mmol/L in boys (n = 605);
-
for every 1 z‐score increase in the high‐fat dietary pattern, HDL‐cholesterol increased by 0.02 mmol/L in girls (n = 558), and by 0.002 in boys (n = 605);
-
for every 1 z‐score increase in the high‐fat dietary pattern, triglycerides increased by 1% in girls (n = 558), and boys (n = 605).
Boreham 1999 examined the association between total fat intake (%TE) and HDL‐cholesterol in girls (n = 230) after three years, and reported that for every 1% increase in energy intake from total fat, HDL‐cholesterol decreased by 0.21 mmol/L (with adjustment for energy intake).
We have summarised standardised and unstandardised SBP and DBP outcomes, fat intake exposure variables and results of reported associations within each time range, in Table 14, including adjustments made. Two studies related SBP and DBP to total fat intake per 10 g at two years (Setayeshgar 2017; n = 310), and in absolute grams at three years (Obarzanek 1997 (cohort); n = not reported). According to Setayeshgar 2017, with no adjustment for TE intake, for every 10 g increase in total fat intake, SBP increased by 0.03 z‐scores and DBP increased by 0.03 z‐scores. With adjustment for TE intake, for every 1 g increase in total fat intake, SBP increased by 0.4 mmHg and DBP increased by 0.43 mmHg (Obarzanek 1997 (cohort)).
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| SBP at > 1to 2 years: 1 cohort study; 1 analysis (n = 310) in boys and girls aged 13 years | ||||||||
| 12.5 years; regression | SBP | z‐score | 2 | Total fat intake (single 24‐hour recall at baseline) | per 10 g | n overall = 310; regression result. β = 0.03 (95% CI 0.00004 to 0.06), P < 0.05. After 2 years, for every 10 g increase in total fat intake, SBP will increase by 0.03 z‐score | + No | Adjusted for baseline BMI z‐score, baseline SBP and DBP, moderate to vigorous physical activity, vegetables and fruit, fibre, milk, sodium and added sugar. |
| SBP at > 2to 5 years: 1 cohort study; 1 analysis (n = NR) in boys and girls aged 10 years | ||||||||
| 9.6 years; regression | SBP | mmHg | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | g | n overall = NR; regression result. B = 0.4, P < 0.1. After 3 years, for every 1 g increase in total fat intake, SBP will increase by 0.4 mmHg | + Yes | Adjusted for height, weight and gender, with all sources of calories in the model. |
| DBP at > 1to 2 years: 1 cohort study; 1 analysis (n = 310) in boys and girls aged 13 years | ||||||||
| 12.5 years; regression | DBP | z‐score | 2 | Total fat intake (single 24‐hour recall at baseline) | per 10 g | n overall = 310. β = 0.03 (95% CI 0.003 to 0.05), P < 0.05. After 2 years, for every 10 g increase in total fat intake, DBP will increase by 0.03 z‐scores | + No | Adjusted for baseline BMI z‐score, baseline SBP and DBP, moderate to vigorous physical activity, vegetables and fruit, fibre, milk, sodium and added sugar. |
| DBP at > 2to 5 years: 1 cohort study; 1 analysis (n = NR) in boys and girls aged 10 years | ||||||||
| 9.6 years; regression | DBP | mmHg | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | g | n overall = NR. B = 0.43, 0.01 < P < 0.06. After 3 years, for every 1 g increase in total fat intake, DBP will increase by 0.43 mmHg | + Yes | Adjusted for height, weight and gender, with all sources of calories in the model. |
aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome.
B: unstandardised beta coefficient; β: standardised beta‐coefficient; BMI: body mass index; CI: confidence interval; DBP: diastolic blood pressure; NR: not reported; SBP: systolic blood pressure.
Height
We have summarised the various standardised and unstandardised height outcomes, total fat exposure variables and results of reported associations within each time range, including adjustments made, in Table 15.
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| Height at 1 year: 2 cohort studies; 2 analyses (n ˜ 740) in children aged 2‐6 years | ||||||||
| 2 years; mean end values per group | Relative heightb | % | 1 | Total fat intake (single 4‐day dietary record at baseline, 1.5 and 2 years) | LF (27.7‐28.7 %TE); HF (> 28.7 %TE) | n overall = 740 (LF = 35, HF = 705); mean end values (SD). Baseline: LF = 0.30 (0.9); HF = 0.32 (0.9). At 1 year: LF = 0.18 (1.0); HF = 0.16 (0.9); P = 0.93. After 1 year, on average children with LF intake (27.7‐28.7 %TE) have a relative height change of 0.12% compared to 0.16% for children with HF intake (> 28.7 %TE). | ‐ No | No matching reported. No adjustment for prognostic variables. |
| 6.2 years; mean end values per group | Height | z‐score | 1 | Total fat intake (multiple 24‐hour dietary recalls at baseline and 1 year) | LF quintile (24%TE) HF quintile (34%TE) | n overall = NR (LF = NR, HF = NR); mean end values (SD NR). Baseline: LF = ‐0.23; HF = 0.17. At 1 year: LF = ‐0.11; HF = 0.22. After 1 year, on average children in LF intake (24%TE) quintile gain 0.12 z‐score in height while children in HF intake (34%TE) quintile gain 0.05 z‐score in height. | + No | No matching reported. No adjustment for prognostic variables. |
| Height at > 1to 2 years: 2 cohort study; 3 analysis (n = 836) in boys and girls aged 2‐4 years | ||||||||
| 3.6 years; mean end values per group | Height | cm | 1.5 | Total fat intake (single 3‐day unweighed food record at baseline) | LF quintile (30.4%TE) HF quintile (41.8%TE) | n boys, at baseline = 439; at 1.5 years = 387 (LF = NR, HF = NR); mean end values (SD). Baseline: LF = 99.9 (95% CI 99.2 to 100.5); HF = 99.3 (95% CI 98.7 to 99.9). At 1.5 years: LF = 110.7 (95% CI 109.9 to 111.5); HF = 109.9 (95% CI 109.1 to 110.7). After 1.5 years, on average boys with LF intake (30.4%TE) quintile gain 10.8 cm in height while boys with HF intake (41.8%TE) quintile gain 10.6 cm in height. | ‐ No | No matching reported. No adjustment for prognostic variables. |
| 3.6 years; mean end values per group | Height | cm | 1.5 | Total fat intake (single 3‐day unweighed food record at baseline) | LF quintile (30.4%TE) HF quintile (41.8%TE) | n girls, at baseline = 351; at 1.5 years = 323) (LF = NR, HF = NR); mean end values (SD). Baseline: LF = 99.9 (95% CI 98.0 to 99.8). HF = 98.3 (95% CI 97.6 to 99.1). At 1.5 years: LF = 110.0 (95% CI 108.9 to 111.1); HF = 109.3 (95% CI 108.3 to 110.3). After 1.5 years, on average girls in LF intake (30.4%TE) quintile will gain10.1 cm in height while girls in HF intake (41.8%TE) quintile will gain 11 cm in height. | + No | No matching reported. No adjustment for prognostic variables. |
| 2 years; mean end values per group | Height | cm | 2 | Total fat intake (single 3‐day weighed dietary records at baseline and 2 years) | LF < 30%TE HF > 35%TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 86.1 (2.6); HF = 87.7 (3.3). At 2 years: LF (n = 20) = 107 (5.5); HF (n = 76) = 106 (3.9); P = NS. After 2 years, on average children with LF intake (< 30%TE) gain 20.9 cm in height, while children with HF intake > 35%TE) gain 18.3 cm in height. | ‐ No | No matching reported. No adjustment for prognostic variables. |
| Height at > 2to 5 years: 3 cohort studies; 3 analyses (n = 973) in boys and girls aged 2‐10 years | ||||||||
| 4.4 years; mean change per group | Height | cm/year | 2.1 | Total fat intake (multiple FFQs at baseline) | LF ≤ 30%TE HF > 30%TE | n overall = 215 (LF = 37, HF = 178), mean change (SD). Baseline: LF = 6.8 (1.4); HF = 6.4 (0.8); P > 0.05. MD 0.2 (95% CI ‐0.24 to 0.64). After 2 years, LF intake (≤ 30%TE) will result in a 0.2 cm/year greater increase in height on average compared to HF intake (> 30%TE). | ‐ No | No matching reported. No adjustment for prognostic variables. |
| 9.6 years regression | Height | cm | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | %TE | n overall = 632; regression results. B = ‐0.0009, P = 0.6. After 3 years, for every 1% increase in energy intake from fat, height in children will decrease by 0.0009 cm on average. | ‐ Yes | Adjusted for gender, physical activity, treatment, visit number, other sources of energy than fat, and for interactions: fat intake‐by‐treatment, fat intake‐by‐gender, fat intake‐by‐visit number and visit number‐by‐treatment. |
| 2 years; mean end values per group | Height | cm | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | LF < 30%TE HF > 35%TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 86.1 (2.6); HF = 87.7 (3.3). At 4 years: LF (n = 14) = 114 (5.5); HF (n = 88) = 116 (4.3); P > 0.05. After 4 years, on average children with LF intake (< 30%TE) gain 27.9 cm in height, while children with HF intake (> 35%TE) gain 28.3 cm in height. | + No | No matching reported. No adjustment for prognostic variables. |
| Height at > 5to 10 years: 1 cohort study; 1 analysis (n = 126) in boys and girls aged 2 years | ||||||||
| 2 years; mean end values per group | Height | cm | 6 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years; single 4‐day weighed dietary record at 6 years) | LF < 30%TE HF > 35%TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 86.1 (2.6); HF = 87.7 (3.3). At 6 years: LF (n = 13) = 131 (7.7); HF (n = 72) = 128 (5.2); P > 0.05. At 6 years, on average children in LF intake (< 30%TE) gain 44.9 cm in height while children in HF intake (> 35%TE) gain 40.3 cm in height. | ‐ No | No matching reported. No adjustment for prognostic variables. |
aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome.
bRelative height, deviation in percentages from the mean height of healthy Finnish children of the same height and gender.
%TE: percentage of total energy; FFQ: Food Frequency Questionnaire; LF: low fat; HF: high fat; MD: mean difference; NA: not applicable; NR: not reported; SD: standard deviation.
After one year, Niinikoski 1997a (n = 740) reported that on average children with low‐fat intake (27.7% to 28.7%TE) had a relative height change of 0.12% compared to 0.16% for children with high‐fat intake (> 28.7%TE), with no adjustment for energy intake. After one year, Tershakovec 1998 (cohort) (n = not reported) found that on average children in the low‐fat intake (24%TE) quintile gained 0.12 z‐scores in height while children in the high‐fat intake (34%TE) quintile gained 0.05 z‐scores in height.
After 1.5 years, Ambrosini 2016 reported that boys (n = 387) in the low‐fat intake (30.4%TE) quintile gained 10.8 cm in height on average, while boys in the high‐fat intake (41.8%TE) quintile gained 10.6 cm; girls (n = 323) in the low‐fat intake quintile gained 10.1 cm in height on average, while high‐fat intake quintile girls gained 11 cm on average. Magarey 2001 reported mean end values for height in the lower and higher fat intake groups after two years; children with low‐fat intake (< 30%TE) gained 20.9 cm in height on average, while children with high‐fat intake (> 35%TE) gained 18.3 cm in height (n = 126).
Shea 1993 (n = 215) reported that low‐fat intake (≤ 30%TE) resulted in a 0.2 cm/year greater increase in height on average compared to high‐fat intake (> 30%TE) at 25‐month follow‐up. At three years, Obarzanek 1997 (cohort) reported that for every 1% increase in energy intake from fat, the increase in children's height decreased by 0.0009 cm on average; and at four years, Magarey 2001 found that average children with low‐fat intake (< 30%TE) had gained 27.9 cm in height, on average, while children with high‐fat intake (> 35%TE) gained 28.3 cm in height.
Magarey 2001 (n = 126) reported that at six years children with low‐fat intake (< 30%TE) had gained 44.9 cm in height, while children with high‐fat intake (> 35%TE) had gained 40.3 cm in height.
Discussion
Summary of main results
Our review aimed to assess the effects of total fat intake on measures of weight and body fatness in children and young people not aiming to lose weight. We included 24 studies comprising three parallel‐group RCTs (reported in 12 records) and 21 prospective cohort studies (92 eligible analyses, reported in 47 records), with 23 being conducted in high‐income countries.
Randomised controlled trials
Although RCT evidence was limited to one study reporting the same outcome per time point range, and by lack of results for all important outcomes at all time points, the evidence was of low to moderate quality for most outcomes (summary of findings Table for the main comparison; all time points presented in Appendix 2).
Body mass index and weight
Compared to fat intake greater than 30% of total energy (TE), lower total fat intake (30%TE or less) probably decreased BMI in children over a period of one to two years (MD ‐1.5 kg/m2, 95% CI ‐2.45 to ‐0.55; 1 RCT; n = 191; moderate‐quality evidence). This finding was not consistent for comparisons in children at six to 12 months' follow‐up (1 RCT; n = 620; low‐quality evidence) nor over the longer follow‐up periods. Lower total fat intake (30%TE or less) compared to usual/modified fat intake may make little or no difference to weight (kg) in children over a five‐year period (MD ‐0.60 kg, 95% CI ‐2.39 to 1.19; 1 RCT; n = 612; low‐quality evidence), and we are uncertain if it has an effect on weight‐for‐age in children over a 12‐month period (1 RCT; n = 149; very low‐quality evidence). It should be noted that none of the included trials set out to answer the review question whether lower fat compared to higher fat diets are safe and effective for preventing abnormal weight gain over the longer term, in generally healthy children with healthy bodyweights.
Blood lipids
Lower total fat intake (30%TE or less) probably slightly reduced total cholesterol in children over a 12‐month period when compared to fat intake greater than 30%TE (MD ‐0.15, 95% CI ‐0.24 to ‐0.06; 1 RCT; n = 618; moderate‐quality evidence), but may make little or no difference over longer time periods (1 RCT per outcome per time point range, low‐quality evidence). Compared to fat intake greater than 30%TE, lower total fat intake (30%TE or less) probably decreased LDL‐cholesterol in children over a 12‐month period (MD ‐0.12 mmol/L, 95% CI ‐0.20 to ‐0.04; 1 RCT; n = 618, moderate‐quality evidence) and over a two‐ to five‐year period (MD ‐0.09, 95% CI ‐0.17 to ‐0.01; 1 RCT; n = 623; moderate‐quality evidence). Lower total fat intake (30%TE or less) versus fat intake greater than 30%TE probably made little or no difference to HDL‐cholesterol (1 study, moderate‐quality evidence) and triglycerides in children over the various reported time point ranges (1 study, low‐ to moderate‐quality evidence).
Height
When compared to fat intake greater than 30%TE, we were uncertain whether lower total fat intake (30%TE or less) reduced height‐for‐age in children over a 12‐month period (1 study; very low‐quality evidence) and may have made little or no difference to height in children over a longer time point ranges (1 RCT per outcome per time point range, low‐quality evidence).
Dietary intakes
Both RCTs that reported dietary intake data at various time point ranges show that, compared to the group with fat intake greater than 30%TE, children with lower fat intake had lower TE intake from total and saturated fat intake (%TE) and consequently greater proportions of total energy from carbohydrates and protein at all reported time point ranges. This indicates a certain level of adherence to the lower and higher fat diets being compared in these two trials.
Summary of evidence from randomised controlled trials
In summary, limited evidence from three trials in high‐income countries that randomised 1054 children to a lower total fat intake (30%TE or less) versus usual or modified fat intake, but with no intention to reduce weight, showed small reductions in BMI, total‐cholesterol and LDL‐cholesterol at some time points with lower fat intake compared to controls, and no consistent differences in effects on weight and HDL‐cholesterol. There were no adverse effects on height. Inclusion of hypercholesteraemic children in two trials may limit generalisability of these findings.
Cohort studies
We identified more eligible evidence in prospective cohort studies, but heterogeneous reporting and methods across studies, and the judgements of predominantly very low‐quality evidence, made it difficult to draw any firm conclusions. Thus, the true relationships may be substantially different from those reported (summary of findings Table 2; all time points presented in Appendix 3). Bearing the quality of evidence in mind, and although measures of total fat intake, magnitudes of associations and adjustments for prognostic variables in the included cohort studies varied considerably, over half of the included analyses that reported on primary outcomes suggested that total fat intake and body fatness measures moved in the same direction.
In trying to form a general picture for BMI, as one of the key outcomes, 11/18 analyses that explicitly adjusted for TE intake showed small positive associations, and 6/18 showed small inverse associations, between various measures of total fat intake and BMI across the various time point ranges. In analyses that did not adjust for energy intake (or where this was not applicable as it was included as part of the exposure variable), 9/14 analyses reported positive relationships between various total fat intake measures and BMI across time points.
Most of the included cohort studies were not designed to primarily answer the question whether total fat intake during childhood is a risk factor for abnormal weight gain, but sought to examine the relationship between total fat intake over time in normal weight children and its influence on or relationship with measures of body fatness.
Summary of evidence from cohort studies
In summary, associations in 21 prospective cohort studies (n = approximately 25,059 completed), of which 20 were done in high‐income countries, that related total fat intake to later measures of body fatness in children were inconsistent and the quality of this evidence was mostly very low, meaning that the true effect is likely to be substantially different form the estimate of effect.
Overall completeness and applicability of evidence
We searched and screened carefully to identify all relevant RCTs and cohort studies in children that assessed the relationship between total fat intake and measures of body fatness. We searched for trials that lowered total fat intake to 30%TE or less in one group and not in the other group, regardless of the primary aims or outcomes mentioned in the title or abstracts. The three trials reported the same outcomes but at different time points, which meant that only one study reported the same outcome in the same predefined time point range for all eligible outcomes. Findings from two of the three RCTs were directly applicable only to children with raised blood lipids in high‐income countries, with limited applicability in generally healthy children in all settings.
We may have been limited in how well we were able to assess completeness for cohort studies, where the risk of missing studies was perhaps greater, since relevant analyses may be described and reported in the text and did not appear in the title or abstract. Findings of all except three of the cohorts were directly applicable to generally healthy children in high‐income countries, with limited applicability in LMICs.
Quality of the evidence
The reporting of trials included in this review was generally poor, with very heterogeneous methods and approaches used for outcomes and exposures. We contacted study authors but did not receive timely responses from most authors. Our risk of bias assessment identified the following to be of high concern in the cohort studies: selection bias (related mainly to the lack of matching or adjusting for all key prognostic variables), and attrition bias and detection bias (related to mostly to assessment of exposure).
Our GRADE assessments for RCTs (summary of findings Table for the main comparison; Appendix 2) varied from very low to moderate, and in cohort studies (summary of findings Table 2; Appendix 3) from very low to low in one outcome, which means that future research is likely to impact on the findings. Therefore, our confidence in the validity of the findings was limited.
We considered the GRADE domain indirectness to be problematic in this body of evidence as two trials only included children with raised blood lipids (Obarzanek 2001 (RCT); Tershakovec 1998 (RCT)). For the GRADE domain imprecision, it was very difficult to come up with specific thresholds for benefit or harm for our outcomes due to the many other factors that influence these outcomes, as is often the case with nutrition outcomes (especially in children). Therefore, we used the following approach to grading imprecision: we downgraded all outcomes with a 95% CI that crossed the null for serious imprecision, the implication being that any outcome where the intervention or exposure may result in a greater risk of a negative outcome, no matter how small, was downgraded. Conversely, when the 95% CI did not cross the null, we did not downgrade for imprecision if the optimal information size criterion was met (calculation of the number of patients required for an adequately powered individual trial), and downgraded if the optimal information size was not met. The exception to downgrading for serious imprecision when a 95% CI crossed the null, was when an outcome had a very narrow 95% CI around the null, such that we were quite confident that the results are reflecting a true null effect.
Potential biases in the review process
The decision to exclude trials that aimed to reduce weight may have led to a lower number of included RCTs. However, this exclusion served to avoid the potential confounding effects of dieting and unconscious energy restriction or other diet changes. Restricting inclusion to studies with a minimum of six months' duration for RCTs or one year' duration for cohorts could have led to missing some potentially eligible studies. However, our question, and the time‐dependant nature of the relationship between fat intake and our primary outcomes made it important for us to examine this relationship over a longer period. Trials with a longer follow‐up period ensure that data are relevant to long‐term changes in fatness, which affects longer‐term health. It could also be argued that our choice of predefined time point ranges may have introduced bias. This could not be explored in full due to the inability to perform all sensitivity analyses. However, the two possible sensitivity analyses showed high heterogeneity, as expected, when we ignored predefined time point ranges, and the same outcomes in two trials were pooled at longest and shortest time point ranges.
We were not able to search the reference lists of all included studies and any systematic reviews identified, due to time constraints. Therefore, there is a possibility that we missed some relevant evidence. However, the authors of the previous update did search the bibliographies of all identified systematic reviews up to 2015 for further trials and cohort studies, reducing the risk that we omitted relevant trials.
Behavioural adherence is one of the key determinants of the effects of dietary interventions and, similarly, components of the diet other than total fat are also likely to influence effects on eligible outcomes. We sought to investigate these effects using subgroup analyses, but the data did not allow this. We sought to assess the causal pathway between restriction of energy from fat and weight using subgroup analyses, but this was not possible. Many of the cohort analyses show that energy intake was important in mediating the effect of lowering fat intake on bodyweight. Fourteen of the included studies were published before 2005. With the rising obesity trend, most recent studies focused on weight reduction and were thus ineligible for this review.
Agreements and disagreements with other studies or reviews
Evidence on the link between dietary fat intake and body fatness in non‐obese children across systematic reviews was sparse. Also, findings were limited by the variety of outcome measurements used, and reliable dietary intake and adherence data was at best challenging to obtain. In the previous version of this review, Hooper 2015a (search date November 2014) concluded that the "effect of reducing total fat was not consistently reflected in cohort studies assessing the relationship between total fat intake and later measures of body fatness or change in body fatness in studies of children, young people or adults." Similarly, Rouhani 2016 examined evidence from observational studies (search date January 2015) and 14/37 included studies were in children aged between two and 18 years. They found that in cohort studies (some of which overlapped with our included cohort studies), a higher dietary energy density (including higher fat intakes) was directly associated with weight gain, adjusted means for BMI, and adiposity risk. However, similar to our review, they reported considerable heterogeneity. Additionally, they did not perform analyses separately in children only.
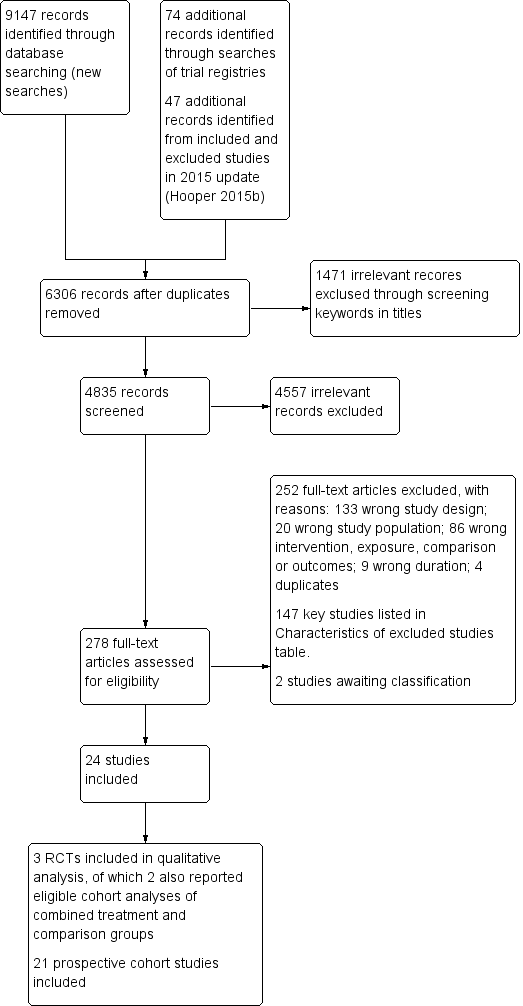
Study flow diagram. RCT: randomised controlled trial.

The bubble‐plot presents the spread of the different ways in which total fat intake estimates were expressed and applied to examine associations with body fatness in the 81 analyses, reporting primary outcomes in the five time point ranges. Combining the many various total fat intake exposure estimates reporting on the same outcome in the same time point range was deemed inappropriate. BMI: body mass index; WC: waist circumference; yr: year.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study. RCT: randomised controlled trial.

Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 1 Weight outcomes (standardised and unstandardised end values).
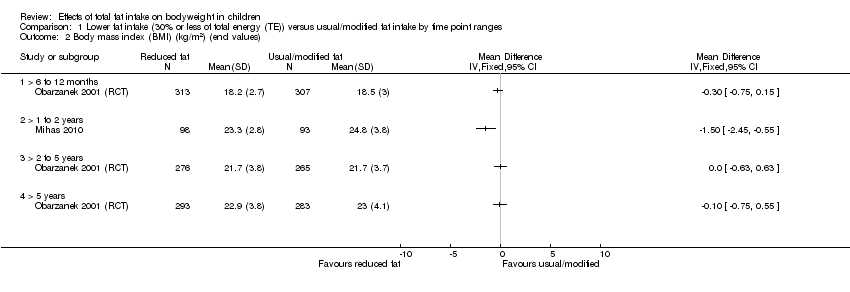
Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 2 Body mass index (BMI) (kg/m2) (end values).

Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 3 BMI (kg/m2) (end values): sensitivity analysis (longest follow‐up data only).

Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 4 BMI (kg/m2) (end values): sensitivity analysis (shortest follow‐up data only).

Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 5 Total cholesterol (mmol/L) (end values).
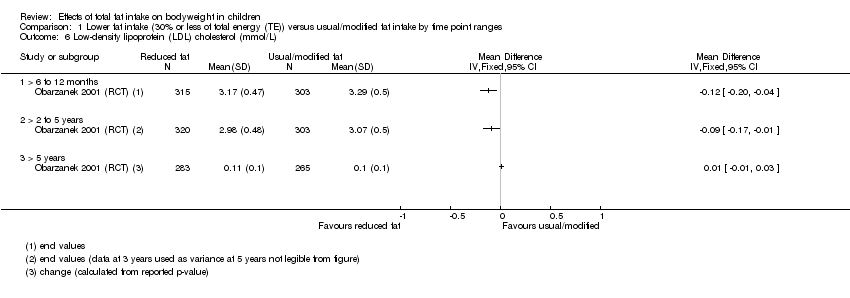
Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 6 Low‐density lipoprotein (LDL) cholesterol (mmol/L).

Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 7 High‐density lipoprotein (HDL)‐cholesterol (mmol) (end values).
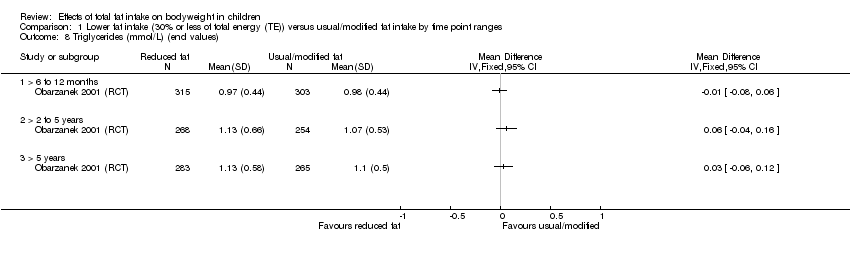
Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 8 Triglycerides (mmol/L) (end values).

Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 9 Systolic blood pressure (mmHg) (end values).
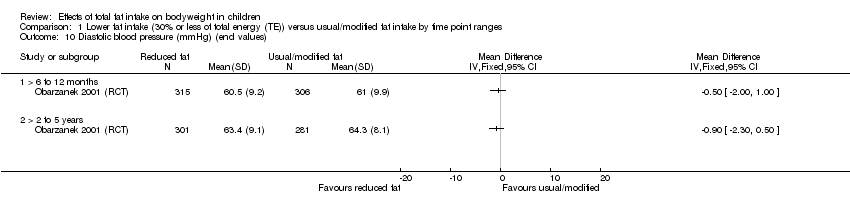
Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 10 Diastolic blood pressure (mmHg) (end values).

Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 11 Height outcomes (standardised and unstandardised end values).

Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 12 Energy intake (kJ) (end values).

Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 13 Fat intake (%TE) (end values).
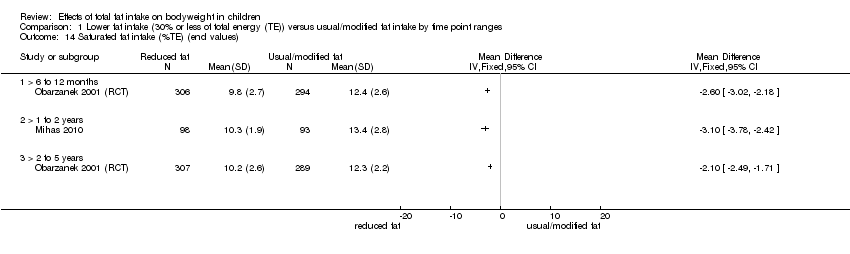
Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 14 Saturated fat intake (%TE) (end values).

Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 15 Protein intake (%TE) (end values).
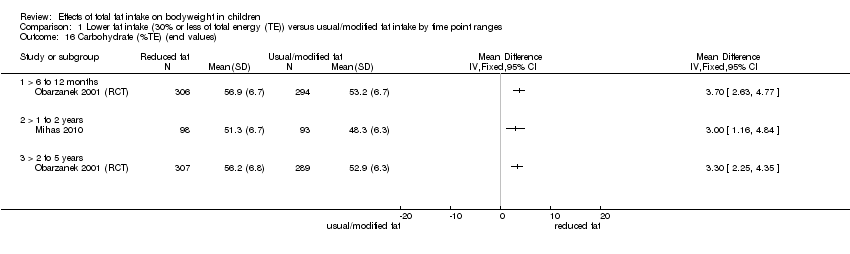
Comparison 1 Lower fat intake (30% or less of total energy (TE)) versus usual/modified fat intake by time point ranges, Outcome 16 Carbohydrate (%TE) (end values).
| Total fat intake ≤ 30% of total energy compared to usual fat intake for bodyweight in children (RCTs) A comprehensive table including data for all time points for each outcome can be found in Appendix 2 | |||||
| Patient or population: boys and girls aged 24 months to 18 years Setting: paediatric practices, schools and health maintenance organisations in high‐income countries Intervention: lower total fat intake ≤ 30%TE Comparison: usual or modified fat intake | |||||
| Outcomes (at time point ranges where data were reported) | No of participants (No of studies) | Illustrated comparative effect (95% CI) | Quality | What happens | |
| Usual fat intake1 | Effect difference with total fat ≤ 30% of total energy2 | ||||
| Weight‐for‐age z‐score Follow‐up: range 6 to 12 months | 151 (1 RCT) | The mean weight‐for‐age z‐score in control group was 0.29 | MD 0.18 lower | ⊕⊝⊝⊝ | We were uncertain whether lower total fat intake (≤ 30%TE) had an effect on weight‐for‐age in children over a 12‐month period (1 study). |
| Weight (kg) | 620 (1 RCT) | The mean weight (kg) in control group was 38.2 | MD 0.5 lower | ⊕⊕⊝⊝ | Lower total fat intake (≤ 30%TE) may have made little or no difference to weight in children over a 5‐year period (1 study). |
| Follow‐up: range 2 to 5 years | 612 (1 RCT) | The mean weight (kg) in control group was 49.5 | MD 0.6 lower | ⊕⊕⊝⊝ | |
| BMI (kg/m2) | 620 (1 RCT) | The mean BMI (kg/m2) in control group was 18.5 | MD 0.3 lower | ⊕⊕⊝⊝ | Lower total fat intake (≤ 30%TE) may have made little or no difference to BMI in children over a 1‐year period (1 study). |
| Follow‐up: range 1 to 2 years | 191 (1 RCT) | The mean BMI (kg/m2) in control group was 24.8 | MD 1.5 lower | ⊕⊕⊕⊝ | Lower total fat intake (≤ 30%TE) probably reduced BMI in children over a period of 1 to 2 years (1 study). |
| Follow‐up: range 2 to 5 years | 541 (1 RCT) | The mean BMI (kg/m2) in control group was 21.7 | MD 0 | ⊕⊕⊝⊝ | Lower total fat intake (≤ 30%TE) may have made little or no difference to BMI in children over a 2 to 5‐year period and > 5‐years (1 study). Please see Appendix 2 for Data for > 5 years. |
| Total cholesterol (mmol/L) | 618 (1 RCT) | The mean total cholesterol (mmol/L) in control group was 5.1 | MD 0.15 lower | ⊕⊕⊕⊝ | Total fat intake ≤ 30%TE probably slightly reduced total cholesterol in children over a 12‐month period (1 study). |
| Follow‐up: range 2 to 5 years | 522 (1 RCT) | The mean total cholesterol (mmol/L) in control group was 4.6 | MD 0.06 lower | ⊕⊕⊝⊝ | Lower total fat intake (≤ 30%TE) may have made little or no difference to total cholesterol in children over a 2 to 5‐year period and > 5‐years (1 study). Please see Appendix 2 for Data for > 5 years. |
| LDL‐C (mmol/L) | 618 (1 RCT) | The mean LDL‐C (mmol/L) in control group was 3.29 | MD 0.12 lower | ⊕⊕⊕⊝ | Lower total fat intake (≤ 30%TE) probably reduced LDL‐C in children over a 12‐month period (1 study) and over a 2 to 5‐year period (1 study). Please see Appendix 2 for Data for > 5 years. |
| Follow‐up: range 2 to 5 years | 623 (1 RCT) | The mean LDL‐C (mmol/L) in control group was 3.07 | MD 0.09 lower | ⊕⊕⊕⊝ | |
| HDL‐C (mmol/L) | 618 (1 RCT) | The mean HDL‐C (mmol/L) in control group was 1.47 | MD 0.03 lower | ⊕⊕⊕⊝ | Lower total fat intake (≤ 30%TE) probably made little or no difference to HDL‐C in children over a 6 to 12‐month period (1 study) and over a 2 to 5‐year period (1 study). Please see Appendix 2 for Data for > 5 years. |
| Follow‐up: range 2 to 5 years | 522 (1 RCT) | The mean HDL‐C (mmol/L) in control group was 1.32 | MD 0.01 lower | ⊕⊕⊕⊝ | |
| Triglycerides (mmol/L) | 618 (1 RCT) | The mean triglycerides (mmol/L) in control group was 0.98 | MD 0.01 lower | ⊕⊕⊕⊝ | Lower total fat intake (≤ 30%TE) probably made little or no difference to triglycerides in children over a 6 to 12‐month period (1 study). Please see Appendix 2 for Data for > 2 years. |
| Height‐for‐age z‐score Follow‐up: range 6 to 12 months | 151 (1 RCT) | The mean height‐for‐age z‐score in control group was 0.05 | MD 0.05 lower | ⊕⊝⊝⊝ | We were uncertain whether lower total fat intake (≤ 30%TE) reduced height‐for‐age in children over a 12‐month period (1 study). |
| Height (cm) | 642 (1 RCT) | The mean height (cm) in control group was 143.1 | MD 0 | ⊕⊕⊝⊝ | Lower total fat intake (≤ 30%TE) may have made little or no difference to height in children over a period > 5 years (1 study). |
| Follow‐up: range 2 to 5 years | 540 (1 RCT) | The mean height (cm) in control group was 167.4 | MD 0.10 lower | ⊕⊕⊝⊝ | |
| %TE: percentage of total energy; BMI: body mass index; CI: confidence interval; HDL‐C: high‐density lipoprotein cholesterol; LDL‐C: low‐density lipoprotein cholesterol; MD: mean difference; RCT: randomised controlled trial. aNotes: For all outcomes, there were too few studies to assess publication bias. | |||||
| GRADE Working Group grades of evidence | |||||
| 1Mean change observed between baseline and follow‐up in the control group. 2Difference in intervention group (and its 95% confidence interval) was based on the assumed change in the comparison group (and its 95% confidence interval). 3Downgraded by 1 for risk of bias: unclear risk of bias across all domains. 4Only 1 study for this outcome, therefore we could not rate for inconsistency. 5Downgraded by 1 for indirectness: participants were children with raised blood lipids, thus results may not be directly generalisable to all children. 6Downgraded by 1 for imprecision: small sample size and confidence interval included no effect and important benefit or harm. 7Not downgraded for serious risk of bias; a well‐conducted trial (methods in place to minimise risk of selection, performance, detection, attrition and reporting bias). 8Downgraded by 1 for imprecision: confidence interval included no effect and important benefit or harm. 9Downgraded by 1 for risk of bias: allocation concealment not reported. 10Not downgraded for serious imprecision: both bounds of the confidence interval indicate benefit, and calculated optimal information size met (158 patients are required to have a 80% chance of detecting, as significant at the 5% level, an important decrease in BMI of 1.7 kg/m2 (the average of the change across the 50th to 97th percentiles in 12.5 year‐olds, as per BMI‐for‐age tables, Centers of Disease Control & Prevention, 2000). 11Not downgraded for serious imprecision: both bounds of the confidence interval indicate benefit. 12Not downgraded for serious imprecision: precise estimate of no effect. 13Downgraded by 1 for imprecision: small sample size (optimal information size not met). | |||||
| Total fat intake and bodyweightin children (cohort studies) A comprehensive table including data for all time points for each outcome can be found in Appendix 3 | ||||
| Patient or population: boys and girls aged 24 months to 18 years Setting: communities, schools, households, healthcare centres in high‐income countries Exposure: total fat intake | ||||
| Outcomes | No of studies (No of participants) | Impact | Quality | What happens |
| Weight (kg) Follow‐up: 2 to 5 years | 4 cohort studies (13,802) | 2 studies that adjusted for TE intake: After 3 years, "Dairy fat was not a stronger predictor of weight gain than other types of fat, and no fat (dairy, vegetable, or other) intake was significantly associated with weight gain after energy adjustment, nor was total fat intake;" no numerical results reported. After 3 years, for every 1% increase in TE intake from total fat of children, weight will decrease by 0.0011 kg. 2 studies that did not adjust for TE intake: After 4 years, weight of children with low‐fat intake (< 30%TE) will increase by 8.1 kg on average, and by 8.9 kg on average in children with high‐fat intake (> 35%TE). After 2 years, children with low‐fat intake (≤ 30%TE) will gain on average 0.2 kg per year more than children with high‐fat intakes (> 30%TE) | ⊕⊝⊝⊝ | When adjusted for TE, we were uncertain whether fat intake was associated with weight in children over 2 to 5 years. When not adjusted for TE, we were uncertain whether lower fat was associated with weight in children over 2 to 5 years. |
| Follow‐up: 5 to 10 years | 1 cohort study (126) | 1 study that did not adjust for TE intake: After 6 years, weight of children with low‐fat intake (< 30%TE) will increase by 16.8 kg on average, and by 13.9 kg on average in children with high‐fat intake (> 35%TE) | ⊕⊝⊝⊝ | We were uncertain whether fat intake was associated with weight over 5 to 10 years (1 study). |
| BMI (kg/m2, kg/m2 per year, z‐score, percentile) Follow‐up: 2 to 5 years | 7 cohort studies (3143) | 4 studies that adjusted for TE intake: After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.63 z‐score in boys but increase by 0.07 z‐score in girls. "Dietary factors were not associated with BMI across the three study years." After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.00008 kg/m2. After 4 years, increase in the total fat intake, will increase BMI by 0.087 z‐score. The model explained 48% of variance in the change of BMI z‐score. 2 studies that did not adjust for TE intake: After 2.08 years, low‐fat intake (≤ 30%TE) will result in a 0.02 kg/m2 per year greater increase in BMI on average, compared to high‐fat intake (> 30%TE). After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.01 percentile in girls. 1 study where TE adjustment was not applicable, as TE was part of exposure: After 3 years, for every 1 z‐score increase in the energy‐dense, high‐fat and low‐fibre dietary pattern, BMI will increase by 0.03 z‐score in boys and by 0.99 z‐score in girls. After 3 years, the ratio of odds for being overweight/obese was 1.04 greater in boys and 1.02 greater in girls with higher dietary pattern z‐scores, compared to the odds in boys and girls with lower dietary pattern z‐scores. | ⊕⊝⊝⊝ Very low6,7,8 | We were uncertain whether fat intake was associated with BMI in children over 2 to 10 years. |
| Follow‐up: 5 to 10 years | 4 cohort studies (1158) | 3 studies that adjusted for TE intake: After 6 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.011 z‐score in boys but increase by 0.005 z‐score in girls. After 9 years, increase in the total fat intake will increase BMI by 0.122 z‐score. After 10 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.029 kg/m2 in white girls and by 0.012 kg/m2 in black girls. 1 study that did not adjust for TE intake: After 6 years, for every 1 g increases in the fat intake, BMI will increase by 0.01 kg/m2 | ⊕⊝⊝⊝ | |
| LDL‐C (mmol/L) Follow‐up: 2 to 5 years | 1 cohort study (1163) | 1 study where TE adjustment not applicable, as TE was part of exposure: After 3 years, for every 1 z‐score increase in the energy‐dense, high‐fat and low‐fibre dietary pattern, LDL‐C will increase by 0.001 mmol/L in boys and 0.04 mmol/L in girls | ⊕⊝⊝⊝ | We were uncertain whether fat intake was associated with LDL‐C in children over 2 to 5 years (1 study). |
| HDL‐C (mmol/L) Follow‐up: 2 to 5 years | 2 cohort studies (1393) | 1 study that adjusted for TE intake: After 3 years, for every 1% increase in energy intake from total fat, HDL‐C will decrease by 0.21 mmol/L in girls. 1 study where TE adjustment not applicable, as TE was part of exposure: After 3 years, for every 1 z‐score increase in the energy‐dense, high‐fat and low‐fibre dietary pattern, HDL‐C will decrease by 0.002 mmol/L in boys but increase by 0.02 mmol/L in girls. | ⊕⊕⊝⊝ | When adjusted for TE, fat intake may be inversely associated with HDL‐C in girls over 2 to 5 years (1 study). When not adjusted for TE, fat intake may make little or no difference to HDL‐C in girls over 2 to 5 years (1 study). |
| Triglycerides (mmol/L) Follow‐up: 2 to 5 years | 1 cohort study (1163) | 1 study where TE adjustment not applicable, as TE was part of exposure: After 3 years, for every 1 z‐score increase in the energy‐dense, high‐fat and low‐fibre dietary pattern, triglycerides will increase by 1% in either boys or girls. | ⊕⊝⊝⊝ | We were uncertain whether fat intake was associated with triglycerides in children over 2 to 5 years (1 study). |
| Height (cm) Follow‐up: 2 to 5 years | 3 cohort studies (973) | 1 study that adjusted for TE intake: After 3 years, for every 1% increase in energy intake from fat, height in children will decrease by 0.0009 cm on average. 2 studies that did not adjust for TE intake: After 2 years, low‐fat intake (≤ 30%TE) will result in a 0.2 cm per year greater increase in height on average compared to high‐fat intake (> 30%TE). After 4 years, on average children in low‐fat intake (< 30%TE) gain 27.9 cm in height, while children in high‐fat intake (> 35%TE) gain 28.3 cm in height. | ⊕⊝⊝⊝ | We were uncertain whether fat intake was associated with height in children over 2 to 10 years. |
| Follow‐up: 5 to 10 years Age at baseline: 2 years | 1 cohort study (126) | 1 study that did not adjust for TE intake: At 6 years, on average children in low‐fat intake (< 30%TE) gain 44.9 cm in height while children in high‐fat intake (> 35%TE) gain 40.3 cm in height. | ⊕⊝⊝⊝ | |
| BMI: body mass index; HDL‐C: high‐density lipoprotein cholesterol; LDL‐C: low‐density lipoprotein cholesterol; MD: mean difference; TE: total energy. aNotes: Some cohort studies reported more than one eligible analysis for the same outcome (e.g. BMI as continuous or binary outcome) or different measures of exposure (e.g. fat intake as continuous %TE or as binary classification of less‐exposed vs more‐exposed). In these cases, we selected outcomes and exposure measures so as not to use the same study sample of participants more than once per outcome and time point range in the table. For all outcomes, there were too few studies to assess publication bias. | ||||
| GRADE Working Group grades of evidence | ||||
| 1Although, risk of bias was concerning (studies with strong contributions did not adjust for all important prognostic variables), plausible residual confounding would likely reduce the demonstrated effect in the studies that did not adjust for total energy intake; thus we chose not to downgrade for risk of bias. 2Downgraded by 1 for imprecision: in studies reporting variance, the variance included no effect and important benefit or harm. 3Although risk of selection bias (no matching of exposed and non‐exposed groups, or statistical adjustments) and attrition bias (> 50% attrition) was concerning, plausible residual confounding would likely reduce the demonstrated effect as this study did not adjust for total energy; thus we chose not to downgrade for selection bias. 4Only 1 study for this outcome, therefore we could not rate for inconsistency. 5Downgraded by 1 for indirectness: a single study in a high‐income country likely has limited generalisability. 6Imprecision was considered, but we considered a decision would not impact on the rating and thus no judgement was made for imprecision. 7Downgraded by 1 for risk of bias: risk of selection bias: 5 studies did not match exposed and non‐exposed groups or make important statistical adjustments; high risk of detection bias: dietary assessment for 3 studies were not adequately rigorous. 8Downgraded by 1 for inconsistency: some studies reported small to large positive associations between exposure and outcome, while others reported no association or a small to medium inverse association between exposure and outcome. 9Downgraded by 1 for risk of bias: risk of selection bias: 2 studies with strongest contributions, did not adjust for all important prognostic variables; high risk of detection bias: dietary assessment in 1 study was not adequately rigorous. 10Downgraded by 1 for risk of bias: risk of selection bias; no matching of exposed and unexposed groups or adjustment for all important prognostic variables. 11Study was judged to have a lower overall risk of bias; attrition < 50% and satisfactory assessment of exposure. 12Not downgraded for serious imprecision as judged to be precise estimates of no effect in both studies. | ||||
| Recipients | Why | What (materials) | What (procedures) | Who provided | How and where | When and how much | Strategies to improve or maintain intervention fidelity; tailoring and modification | Extent of intervention fidelity |
| 4‐ to 9‐year‐old children with hypercholesterolaemia (plasma total cholesterol > 4.55 mmol/L, fasting plasma LDL‐C 2.77‐4.24 mmol/L for boys and 2.90‐4.24 mmol/L for girls), at ≥ 85% of ideal body weight. | Limited dietary fat was recommended for children aged > 2 years, but there were concerns that lower fat intake of children may affect their growth. Trial evaluated growth of children with hypercholesterolaemia completing an innovative, physician‐initiated, home‐based nutrition education programme or standard nutrition counselling that aimed to lower dietary fat intake. | Nutrition education programme complied with recommendations of the National Cholesterol Education Program Expert Panel on Blood Cholesterol Levels in Children and Adolescents. | Children and ≥ 1 parent (usually mother) attended 45‐ to 60‐minute counselling session with paediatric dietician. Children and parents in at‐risk control and not‐at‐risk control groups were not provided educational information or materials. | 1) Not described; 2) paediatric registered dieticians. | 1) Audiotape stories and picture books and follow‐up paper/pencil activities for children as well as manual for parents. Story and activities to be completed each week; 2) face‐to‐face individual counselling by a dietician. 1) At home; 2) paediatric practice. | 10 weeks with 1) talking‐book lesson; 2) 45‐60 minutes counselling session each week. | Not described Tailoring and modification of intervention during trial were not described. | 1) 71/88; 2) 77/86 completed intervention programmes and returned for evaluation at 3 months after baseline. |
| Prepubertal boys and girls aged 8‐11 years with LDL‐C levels ≥ 80th and < 98th percentiles for age and sex percentiles of the Lipid Research Clinics population. | Aimed to assess feasibility, safety, efficacy and acceptability of lowering dietary intake of total fat, saturated fat and cholesterol to decrease LDL‐C levels. | Intervention group received dietary counselling sessions based on National Cholesterol Education Programme guidelines: 28% of energy from total fat, < 8% from saturated fat, > 9% from polyunsaturated fat, and < 75 mg/1000 kcal of cholesterol per day, not to exceed 150 mg/day. Guidebooks including activities and recipes on diets and food recommendations given to participants and their families. | In first 6 months, 6 weekly and then 5 biweekly group sessions were led by nutritionists and behaviourists, and 2 individual visits were held with nutritionist. Over second 6 months, 4 group and 2 individual sessions were held. During 2nd and 3rd years, group and individual maintenance sessions were held 4‐6 times/year, with monthly telephone contacts between group sessions. During 4th year of follow‐up, 2 group events + 2 individual visits conducted with additional telephone contacts as appropriate. | Nutritionists and behaviourists | 1) Group sessions and 2) individual visits were held, accompanied by telephone contacts in between sessions. 1) At clinics, 2) at home | 6 weekly, 5 biweekly group sessions and 2 individual visits during first 6 months; 4 group and 2 individual sessions during second 6 months; 4‐6 maintenance sessions with telephone contacts between sessions during 2nd and 3rd years; 2 group and 2 individual sessions with telephone contacts as appropriate by 4th year. | By 4th year of follow‐up, individual visits used an individualised approach based on motivational interviewing and stage of change for increasingly busy teenagers. Tailoring and modification of intervention during trial not described. | 295/334 attended the last visit (> 5 years' follow‐up). |
| Students aged 12‐13 years from an urban area in Greece. | Aimed to evaluate the short‐term (15‐day) and long‐term (12‐month) effects of a 12‐week school‐based health and nutrition interventional programme regarding energy and nutrient intake, dietary changes and BMI. | Teaching material for teachers and workbooks for students on nutrition‐dietary habits and physical activity and health based on Social Learning Theory Model were developed and distributed to teacher and each student. | Multicomponent workbooks covering mainly dietary issues, but also dental health hygiene and consumption attitudes, were produced with each student being supplied a workbook. The class home economics teacher implemented 12‐hour‐classroom curriculum incorporating health and nutrition promotion during 12 weeks. 2 meetings were conducted with parents (given screening results of children; presentations given on dietary habits of children to improve health profile of children and prevent development of chronic diseases in the future). Cues and reinforcing messages in the form of posters and displays were provided in the classroom. | Educational intervention (classroom curriculum) delivered by class home economics teachers who were trained and supervised by health visitor or family doctor. | Classroom curriculum; cues and reinforcing messages in the form of posters and displays provided in classroom; nutrition education meetings for parents in group. At school. | 12 hours of classroom material, 2 meetings for parents during a 12‐week period. | Health visitor or family doctor supervised the programme implementation of class home economics teachers who were given 2 × 3‐hour seminars with aims to familiarise teachers about objectives of intervention and their role therein, and to increase their awareness of significance of incorporating health and nutrition in their curriculum before delivering the intervention. Tailoring and modification of intervention during trial not described. | 107/109 participation rates at 15‐days' follow‐up and 98/109 at 12 months' follow‐up. |
| aTIDieR: Template for Intervention Description and Replication, template for this table from Hoffman 2017. BMI: body mass index; LDL‐C: low‐density lipoprotein cholesterol; RCT: randomised controlled trial. | ||||||||
| Outcome Study ID | Follow‐up from baseline | |||||
| Baseline Mean (SD)a | 6 months MD (95% CI) | > 6 to 12 months MD (95% CI) | > 1 to 2 years MD (95% CI) | > 2 to 5 years MD (95% CI) | > 5 years MD (95% CI) | |
| Weight‐for‐age z‐scoreb | ||||||
| 0.04 (1.02); 0.26 (0.93) | ‐0.14 (‐0.45 to 0.17) | ‐0.18b (‐0.51 to 0.15) | ND | ND | ND | |
| Body weight (kg)b | ||||||
| 32.7 (6.8); 33.1 (6.9) | ND | ‐0.50b (‐1.78 to 0.78) | ND | ‐0.60 (‐2.39 to 1.19) | ND | |
| BMI (kg/m2) | ||||||
| 17.5 (2.3); 17.6 (2.4) | ND | ‐0.30 (‐0.75 to 0.15) | ND | 0.00 (‐0.63 to 0.63) | ‐0.10 (‐0.75 to 0.55) | |
| 24 (3.1); 24.3 (3.3) | ND | ND | ‐1.50 (‐2.45 to ‐0.55) | ND | ND | |
| aReduced fat intake group (≤ 30%TE); usual fat intake group. bWeight‐for‐age z‐score and weight (kg) could not be pooled. %TE: percentage of total energy; BMI: body mass index; CI: confidence interval; MD: mean difference; ND: no data in this time point range; SD: standard deviation. | ||||||
| Outcome | Follow‐up from baseline | |||||
| Baseline Mean (SD)a | 6 months MD (95% CI) | > 6 to 12 months MD (95% CI) | > 1 to 2 years MD (95% CI) | > 2 to 5 years MD (95% CI) | > 5 years MD (95% CI) | |
| Total cholesterol (mmol/L) | 5.17 (0.38); 5.17 (0.38) | ND | ‐0.15 (‐0.24 to ‐0.06) | ND | ‐0.06 (‐0.17 to 0.05) | ‐0.02 (‐0.13 to 0.09) |
| LDL‐C (mmol/L) | 3.38 (0.31); 3.38 (0.3) | ND | ‐0.12 (‐0.20 to ‐0.04) | ND | ‐0.09 (‐0.17 to ‐0.01) | 0.01 (‐0.01 to 0.03) |
| HDL‐C (mmol/L) | 1.48 (0.28); 1.47 (0.29) | ND | ‐0.03 (‐0.08 to 0.02) | ND | ‐0.01 (‐0.06 to 0.04) | 0.02 (‐0.03 to 0.07) |
| Triglycerides (mmol/L) | 0.9 (0.33); 0.92 (0.32) | ND | ‐0.01 (‐0.08 to 0.06) | ND | 0.06 (‐0.04 to 0.16) | 0.03 (‐0.06 to 0.12) |
| SBP (mmHg) | 97.31 (9.1); 97.55 (9.4) | ND | ‐0.40 (‐1.70 to 0.90) | ND | ‐0.40 (‐1.84 to 1.04) | ND |
| DBP (mmHg) | 61.97 (9.54); 61.67 (10.23) | ND | ‐0.50 (‐2.00 to 1.00) | ND | ‐0.90 (‐2.30 to 0.50) | ND |
| aReduced fat intake group (≤ 30%TE); usual fat intake group. %TE: percentage of total energy; CI: confidence interval; DBP: diastolic blood pressure; HDL‐C: high‐density lipoprotein cholesterol; LDL‐C: low‐density lipoprotein cholesterol; MD: mean difference; ND: no data in this time point range; SBP: systolic blood pressure; SD: standard deviation. | ||||||
| Outcome Study ID | Follow‐up from baseline | |||||
| Baseline Mean (SD)a | 6 months MD (95% CI) | > 6 to 12 months MD (95% CI) | > 1 to 2 years MD (95% CI) | > 2 to 5 years MD (95% CI) | > 5 years MD (95% CI) | |
| Height‐for‐age z‐scoreb | ||||||
| ‐0.12 (1.02); 0.06 (0.93) | ‐0.02 (‐0.06 to 0.02) | ‐0.05b (‐0.08 to‐0.02) | ND | ND | ND | |
| Height (cm)b | ||||||
| 136.2 (6.8); 136.5 (7) | ND | 0.00b (‐1.11 to 1.11) | ND | ‐0.10 (‐1.54 to 1.34) | ‐0.06 (‐2.06 to 0.86) | |
| aReduced fat intake group (≤ 30%TE); usual fat intake group. bHeight‐for‐age z‐score and height (cm) cannot be pooled. %TE: percentage of total energy; CI: confidence interval; MD: mean difference; ND: no data in this time point range; RCT: randomised controlled trial; SD: standard deviation. | ||||||
| Outcome Study ID | Follow‐up from baseline | |||||
| Baseline Mean (SD)a | 6 months MD (95% CI) | > 6 to 12 months MD (95% CI) | > 1 to 2 years MD (95% CI) | > 2 to 5 years MD (95% CI) | > 5 years MD (95% CI) | |
| Energy (kJ) | ||||||
| 7364 (1832); 7229 (1841) | ND | ‐356.00 (‐655.22 to ‐56.78) | ND | ‐602.00 (‐943.94 to ‐260.06) | ND | |
| 8503.3 (1419.3); 8583.7 (1522.4) | ND | ND | ‐645.50 (‐1075.66 to ‐215.34) | ND | ND | |
| Fat (%TE) | ||||||
| 33.4 (5.5); 34 (4.9) | ND | ‐4.60 (‐5.50 to ‐3.70) | ND | ‐4.40 (‐5.25 to ‐3.55) | ND | |
| 35.4 (4.7); 36.2 (5.2) | ND | ND | ‐5.60 (‐6.91 to ‐4.29) | ND | ND | |
| Saturated fat (%TE) | ||||||
| 12.5 (2.7); 12.7 (2.5) | ND | ‐2.60 (‐3.02 to ‐2.18) | ND | ‐2.10 (‐2.49 to ‐1.71) | ND | |
| 12.4 (2.0); 12.8 (2.3) | ND | ND | ‐3.10 (‐3.78 to ‐2.42) | ND | ND | |
| Protein (%TE) | ||||||
| 14.8 (2.8); 14.6 (2.7) | ND | 1.00 (0.52 to 1.48) | ND | 0.90 (0.38 to 1.42) | ND | |
| 15.3 (1.4); 14.9 (1.8) | ND | ND | 1.30 (0.80 to 1.80) | ND | ND | |
| Carbohydrates (%TE) | ||||||
| 53.0 (6.7); 52.8 (6.2) | ND | 3.70 (2.63 to 4.77) | ND | 3.30 (2.25 to 4.35) | ND | |
| 49.7 (6.2); 48.4 (6.8) | ND | ND | 3.00 (1.16 to 4.84) | ND | ND | |
| aReduced fat intake group (≤ 30%TE); usual fat intake group. %TE: percentage of total energy; MD: mean difference; ND: no data in this time point range; RCT: randomised controlled trial; SD: standard deviation. | ||||||
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) | |
| Weight at 1 year: 4 cohort studies; 4 analyses (n ˜ 1949) in boys and girls aged 2‐11 years | |||||||||
| 2 years old; mean end values per group | Relative weightb | % | 1 | Total fat intake (single 4‐day dietary record at baseline, 1.5 and 2 years) | LF (27.7‐28.7 %TE; HF (> 28.7 %TE) | n overall = 740 (LF = 35, HF = 705); mean end values (SD). Baseline: LF = 1 (8); HF = 1 (8). At 1 year: LF = 1 (7); HF = 1 (8); P = 0.81. After 1 year, no difference in relative weight change of children with LF intake compared to children with HF intakes. | 0 No | No matching reported. No adjustment for prognostic variables. | |
| 6.8 years old; regression | Weight | kg | 1 | Total fat intake (single 7‐day weighed dietary record at baseline and 1 year) | g | n overall = 411; regression result. B = 0.09, SE 0.019; P < 0.05. After 1 year, for every 1 g increase in total fat intake of children, weight will increase by 0.09 kg. | + No | Adjusted for age, gender and physical activity. | |
| 11 years old; regression | Weight | kg/year | 1 | Total fat intake (multiple 24‐hour dietary recalls at baseline) | %TE | n overall = 798; regression result. B = 0.044, SE 0.018; P = 0.014. For every 1% increase in energy intake from total fat in children, weight will increase by 0.04 kg/year. | + No | Adjusted for gender, age, age squared, Tanner stage and BMI. | |
| 6.2 years old; mean end values per group | Weight | z‐score | 1 | Total fat intake (multiple 24‐hour dietary recalls at baseline and 1 year) | LF quintile (24 %TE) HF quintile (34%TE) | n overall = NR (LF = NR, HF = NR); mean end values (SD NR). Baseline: LF = ‐0.21; HF = 0.44. At 1 year: LF = ‐0.14; HF = 0.45. After 1 year, weight‐for‐age of children with LF intake will increase by 0.07 z‐scores on average, and by 0.01 z‐scores in children with HF intake. | ‐ No | No matching reported. No adjustment for prognostic variables. | |
| Weight at > 1to 2 years: 1 cohort study; 1 analysis (n = 126) in boys and girls aged 2 years | |||||||||
| 2 years old; mean end values per group | Weight | kg | 2 | Total fat intake (single 3‐day weighed dietary records at baseline and 2 years) | LF < 30%TE; HF > 35%TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 12.6 (1); HF = 12.8 (1.7). At 2 years: LF (n = 20) 18.4 (2.6); HF (n = 76) 17.9 (2.1); P > 0.05. After 2 years, weight of children with LF intake will increase by 5.8 kg on average, and by 5.1 kg on average in children with HF intake. | ‐ No | No matching reported. No adjustment for prognostic variables. | |
| Weight at > 2to 5 years: 4 cohort studies; 4 analyses (n = 13,802) in boys and girls aged 2‐14 years | |||||||||
| 4.4 years old; mean change per group | Weight | kg/year | 2.1 | Total fat intake (multiple FFQs at baseline) | LF ≤ 30%TE; HF > 30%TE | n overall = 215 (LF = 37, HF = 178); mean change (SD). Baseline: NR. LF = 3 (1.3); HF = 2.8 (1.3); P > 0.05 MD 0.2 (95% CI ‐0.26 to 0.66). After 2 years, children with LF intake will gain on average 0.2 kg/year more than children with HF intakes. | ‐ No | No matching reported. No adjustment for prognostic variables. | |
| 9‐14 years‐old; regression | Weight | kg, 1‐year change | 3 | Total fat intake (single FFQ at baseline, 1, 2 and 3 years) | g | n overall = 12,829; only reported as text. After 3 years, "Dairy fat was not a stronger predictor of weight gain than other types of fat, and no fat (dairy, vegetable, or other) intake was significantly associated with weight gain after energy adjustment, nor was total fat intake." | 0 Yes | Adjusted for age, ethnicity, pubertal stage, annual height growth, baseline BMI and same‐year physical activity. | |
| 9.6 years old; regression | Weight | kg | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | %TE | n overall = 632; regression results. B = ‐0.0011, P = 0.8. After 3 years, for every 1% increase in total energy intake from total fat of children, weight will decrease by 0.0011 kg. | ‐ Yes | Adjusted for gender, physical activity, treatment, visit number, other sources of energy than fat and interactions: fat intake‐by‐treatment, fat intake‐by‐gender, fat intake‐by‐visit number and visit number‐by‐treatment. | |
| 2 years‐old; mean end values per group | Weight | kg | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | LF < 30%TE; HF > 35%TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 12.6 (1); HF = 12.8 (1.7). At 4 years: LF (n = 14) 20.7 (3.4); HF (n = 88) 21.7 (3); P > 0.05. After 4 years, weight of children with LF intake will increase by 8.1 kg on average, and by 8.9 kg on average in children with HF intake. | + No | No matching reported. No adjustment for prognostic variables. | |
| Weight at > 5to 10 years: 1 cohort study; 1 analysis (n = 126) in boys and girls aged 2 years | |||||||||
| 2 yrs‐old; mean end values per group | Weight | kg | 6 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years; single 4‐day weighed dietary record at 6 years) | LF < 30 %TE; HF > 35 %TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 12.6 (1); HF = 12.8 (1.7). At 6 years: LF (n = 13) 29.4 (5.9); HF (n = 72) 26.7 (4.3); P > 0.05. After 6 years, weight of children with LF intake will increase by 16.8 kg on average, and by 13.9 kg on average in children with HF intake. | ‐ No | No matching reported. No adjustment for prognostic variables. | |
| aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction, inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome. bRelative weight, deviation in percentages from the mean weight of healthy Finnish children of the same height and gender. %TE: percentage of total energy; B: unstandardized beta‐coefficient; BMI: body mass index; CI: confidence interval; FFQ: Food Frequency Questionnaire; LF: low fat; HF: high fat; n: number of participants; NA: not applicable; MD: mean difference; NR: not reported; SD: standard deviation; SE: standard error. | |||||||||
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted? (yes/no) | Matched groups or adjusted for (or both) |
| BMI at 1 year: 3 cohort studies; 4 analyses (n ˜ 11,180) in boys and girls aged 7‐14 years | ||||||||
| 9‐14 years; regression | BMI | kg/m2, 1‐year change | 1 | Total fat intake (single FFQ at baseline and 1 year) | g | n girls = 6149; regression result. B = 0.0008, SE 0.0016, P = 632. After 1 year, for every 1 g increase in total fat intake, BMI will increase by 0.0008 kg/m2 in girls. | + Yes | Adjusted for total energy intake, age, ethnicity, pubertal stage, annual height growth, baseline BMI and physical activity. |
| 9‐14 years; regression | BMI | kg/m2, 1‐year change | 1 | Total fat intake (single FFQ at baseline and 1 year) | g | n boys = 4620; regression result. B = ‐0.0015, SE 0.0017, P = 0.375. After 1 year, for every 1 g increase in the total fat intake, BMI will decrease by 0.0015 kg/m2 in boys. | ‐ Yes | Adjusted for total energy intake, age, ethnicity, pubertal stage, annual height growth, baseline BMI and physical activity. |
| 8.6 years; regression | BMI | z‐score | 1 | Total fat intake (single 3‐day record at baseline) | %TE | n overall = NR; regression result = NR. "We are unable to demonstrate a positive relation between dietary fat and BMI z‐score change from baseline to 12 months." | 0 NR | Prognostic variables were adjusted for, but not specified which one. |
| 6.8 years; regression | BMI | kg/m2 | 1 | Total fat intake (single 7‐day weighed record at baseline and 1 year) | g | n overall = 411; regression result. B = 0.08, SE 0.007, P = 0.085. After 1 year, for every 1 g increase in the total intake, BMI will increase by 0.08 kg/m2. | + No | Adjusted for age, sex and physical activity. |
| BMI at > 1to 2 years: 7 cohort studies; 10 analyses (n = 3347) in boys and girls aged 2‐13 years | ||||||||
| 3.6 years; mean end values per group | BMI | kg/m2 | 1.5 | Total fat intake (single 3‐day unweighed food record at baseline) | LF quintile (30.4%TE); HF quintile (41.8 %TE) | n boys, at baseline = 438; At 1.5 years = 383 (LF = NR, HF = NR); mean end values (SD). Baseline: LF = 16.6 (95% CI 16.4 to 16.8); HF = 16.3 (95% CI 16.1 to 16.5). At 1.5 years: LF = 16.1 (95% CI 15.8 to 16.3); HF = 15.7 (95% CI 15.5 to 16.0). After 18 months, average BMI decreased by 0.5 kg/m2 among boys in LF intake (30.4%TE) group and by 0.6 kg/m2 in boys in HF intake (41.8%TE) group. | ‐ No | No matching reported. No adjustment for prognostic variables. |
| 3.6 years; mean end values per group | BMI | kg/m2 | 1.5 | Total fat intake (single 3‐day unweighed food record at baseline) | LF quintile (30.4 %TE); HF quintile (41.8 %TE) | n girls, at baseline = 351; at 1.5 years = 323) (LF = NR, HF = NR); mean end values (SD). Baseline: LF = 16.6 (95% CI 16.3 to 16.9); HF = 16.4 (95% CI 16.1 to 16.7). At 1.5 years: LF = 16.1 (95% CI 15.7 to 16.4); HF = 16.1 (95% CI 15.8 to 116.4). After 18 months,average BMI decreased by 0.5 kg/m2 among girls in LF intake group (30.4%TE) and by 0.3 kg/m2 in girls in HF intake group (41.8%TE). | + No | No matching reported. No adjustment for prognostic variables. |
| 5.4 years; regression | BMI | kg/m2, 2‐years change | 2 | Total fat intake (multiple 24‐hour recalls at baseline) | %TE | n overall = 168; regression result. R2 = 0.26, P entry = 0.01, F‐test = 9.27, df = 6, P change = 0.0001. "Percentage of fat intake, baseline BMI, family risk of overweight, mothers’ BMI, fathers’ enjoyment of activity explained 26% of the variance in the change of BMI." | + Yes | Adjusted for age, baseline BMI, family risk of overweight, mothers' change in BMI and fathers' enjoyment of activity. |
| 4.4 years; regression | BMI | kg/m2, 2‐years change | 2 | Change (year 2 to 3 of follow‐up) in total fat intake (single FFQ at baseline, 1 and 2 years) | %TE | n overall = 146; regression result. B = ‐0.04, P = 0.011, t value = 2.58. After 2 years, for every 1% increase in energy intake from total fat from year 2 to 3 of follow‐up, BMI will decrease by 0.04 kg/m2. | ‐ No | Adjusted for age, sex, parental BMI and physical activity. |
| 4.4 years; regression | BMI | kg/m2, 2‐years change | 2 | Baseline dietary fat (single FFQ) | %TE | n overall = 146; regression result. B = 0.034, P = 0.0521, t value = 1.96. After 2 years, for every 1% increase in energy intake from baseline total fat, BMI will increase by 0.034 kg/m2. | + No | Adjusted for age, sex, parental BMI and physical activity. |
| 5 years; mean end values; mean change per groups | BMI | kg/m2 | 2 | Total fat intake (multiple 24‐hour recalls at baseline) | LF ≤ 30%TE; HF > 30%TE | n girls = 192 (LF = 84; HF = 108); mean end values (SD); mean change (SD). Baseline: LF = 15.8 (1.83); HF = 16 (2.08). At 2 years: LF = 16.4 (1.83); HF = 16.9 (3.12); change LF = 0.6 (0.92); change HF = 1.0 (2.08); P < 0.05. MD ‐0.4 (95% CI ‐0.84 to 0.04) After 2 years, LF intake (≤ 30%TE) will result in 0.4 kg/m2 smaller increase in BMI on average compared to HF intake (> 0%TE) in girls. | + No | No matching reported. No adjustment for prognostic variables. |
| 7.3 years; regression | BMI 1st graders | kg/m2, 2‐years change | 2 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 2 years) | %TE | n overall = 474; regression result. B = 0.021 (95% CI ‐0.004 to 0.046), P = 0.104. After 2 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.021 kg/m2. | + Yes | Adjusted for age, gender, sexual maturation at 6 years' follow‐up, baseline BMI, exercise frequency, screen time, sleep duration, meal skipping and snacking, parental BMI and SES. |
| 10 years; regression | BMI 4th graders | kg/m2, 2‐years change | 2 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 2 years) | %TE | n overall = 1030; regression result. B = ‐0.007 (95% CI ‐0.024 to 0.012), P = 0.449. After 2 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.007 kg/m2. | ‐ Yes | Adjusted for age, gender, sexual maturation at 6 years' follow‐up, baseline BMI, exercise frequency, screen time, sleep duration, meal skipping and snacking, parental BMI and SES. |
| 2 years; regression | BMI | z‐score | 2 | Total fat intake (single 3‐day weighed dietary record at baseline and 2 years) | NR | n overall = 155; regression result. β = 0.079, P > 0.1; R2 = 0.493, P < 0.0001. After 2 years, increase in the total fat intake will increase BMI by 0.079 z‐score. | + Yes | Adjusted for baseline BMI‐z score, gender, mother's BMI and father's BMI. |
| 12.5 years; regression | BMI | z‐score | 2 | Total fat intake (single 24‐hour recall at baseline) | per 10 g | n overall = 330; regression result. β = 0.009 (95% CI ‐0.006 to ‐0.02), P = NS. After 2 years, for every 10 g increase in total fat intake, BMI will increase by 0.009 z‐score. | + Yes | Adjusted for baseline BMI z‐score, moderate to vigorous physical activity, vegetables and fruit, fibre, milk, sodium and added sugar intakes. |
| BMI at > 2to 5 years: 7 cohort studies; 11 analyses (n = 4491) in boys and girls aged 2‐14 years | ||||||||
| 4.4 years; mean change per group | BMI | kg/m2 per year | 2.1 | Total fat intake (multiple FFQs at baseline) | LF ≤ 30%TE; HF > 30%TE | n overall = 215 (LF = 37, HF = 178); mean change (SD). LF = 0.2 (0.81), HF = 0.18 (0.68); P > 0.05. MD 0.02 (95% CI ‐0.26 to 0.30). After 25 months, LF intake (≤ 30%TE) will result in a 0.02 kg/m2 per year greater increase in BMI on average, compared to HF intake (> 30%TE). | ‐ No | No matching reported. No adjustment for prognostic variables. |
| 14 years; regression | BMI | z‐score | 3 | Energy‐dense, HF and low‐fibre dietary patternc (single FFQ at baseline and 3 years) | z‐score | n girls = 649; regression result. β = 0.99 (95% CI ‐0.05 to 0.05), P = NR. After 3 years, for every 1 z‐score increase in the energy‐dense, HF and low‐fibre dietary pattern z‐score, BMI will increase by 0.99 z‐score in girls. | + NA; exposure included energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 14 years; regression | BMI | z‐score | 3 | Energy‐dense, HF and low‐fibre dietary patternc (single FFQ at baseline and 3 years) | z‐score | n boys = 699; regression result. β = 0.03 (95% CI ‐0.01 to 0.08), P = NR. After 3 years, for every 1 z‐score increase in the energy‐dense, HF and low‐fibre dietary pattern, BMI will increase by 0.03 z‐score in boys. | + NA; exposure included energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 14 years; regression and OR higher vs lower dietary pattern z‐score | BMI | Overweight/obese by IOTF;d odds | 3 | Energy‐dense, HF and low‐fibre dietary patternc (single FFQ at baseline and 3 years) | z‐score | n girls = 649; regression result. OR = 1.02 (95% CI 0.87 to 1.19), P = NR. After 3 years, the ratio of odds for being overweight/obese was 1.02 greater in girls with higher dietary pattern z‐scores compared to the odds in girls with lower dietary pattern z‐scores. | + NA; exposure included energy intake | Adjusted for age, dietary misreporting, physical activity and smoking. |
| 14 years; regression and OR higher vs lower dietary pattern z‐score | BMI | Overweight/obese by IOTF;d odds | 3 | Energy‐dense, HF and low‐fibre dietary patternc(single FFQ) at baseline and 3 years) | z‐score | n boys = 699; regression result. OR = 1.04 (95% CI 0.9 to 1.2), P = NR. After 3 years, the ratio of odds for being overweight/obese is 1.04 greater in boys with higher dietary pattern z‐scores compared to the odds in boys with lower dietary pattern z‐scores. | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical activity and smoking. |
| 9.7 years; regression | BMI | z‐score, 3‐years change | 3 | Dietary fat (single 24‐hour recall at baseline) | %TE | n boys = 181; regression result. β = ‐0.63 (95% CI ‐2.07 to 0.82), P = 0.39. After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.63 z‐score in boys. | ‐ Yes | Adjusted for age, physical activity level, dietary volume and puberty at baseline. |
| 9.7 years; regression | BMI | z‐score, 3‐years change | 3 | Dietary fat (single 24‐hour recall at baseline) | %TE | n girls = 217; regression result. β = 0.07 (95% CI ‐1.08 to 1.25), P = 0.72. After 3 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.07 z‐score in girls. | + Yes | Adjusted for age, physical activity level, dietary volume and puberty at baseline. |
| 13.9 years; regression | BMI | Percentile, % | 3 | Total fat intake (single FFQ at baseline, 1, 2 and 3 years) | %TE | n girls = 265; regression result. B = ‐0.01, SE = 0.01, P = 0.16. After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.01 percentile in girls. | ‐ No | Adjusted for age, ethnicity, protein calories, CHO calories, physical activity, physical inactivity and SES. |
| 4.4 years; regression | BMI | kg/m2 | 3 | Total fat intake (observed 4‐day dietary intake at baseline, 1 and 2 years and 3‐day dietary intake at 3 years) | %TE | n overall = 133; regression result. R2 = 0.65, P = NR. "Dietary factors were not associated with BMI across the three study years." | NR Yes | Adjusted for ethnicity, gender, baseline BMI, TV viewing, sedentary behaviour, physical activity, dietary behaviours and interaction terms for variables differing by year. |
| 9.6 years; regression | BMI | kg/m2 | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | %TE | n overall = 632; regression result. B = ‐0.00008, P = 0.9. After 3 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.00008 kg/m2. | ‐ Yes | Adjusted for gender, physical activity, treatment, visit number, other sources of energy than fat, and for interactions: fat intake‐by‐treatment, fat intake‐by‐gender, fat intake‐by‐visit number and visit number‐by‐treatment. |
| 2 years; regression | BMI | z‐score | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | NR | n overall = 152; regression result. β = 0.087, P > 0.1; R2 = 0.48, P < 0.0001. After 4 years, increase in the total fat intake, will increase BMI by 0.087 z‐score. The model explained 48% of variance in the change of BMI z‐score. | + Yes | Adjusted for baseline BMI‐z score, gender, mother's BMI and father's BMI. |
| BMI at > 5to 10 years: 4 cohort studies; 6 analyses (n = 1158) in boys and girls aged 2‐10 years | ||||||||
| 9.6 years; regression | BMI | z‐score, 6‐years change | 6 | Dietary fat (single 24‐hour recall at baseline) | %TE | n girls = 177; regression result. β = 0.005, SE 0.008, P = 0.54. After 6 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.005 z‐score in girls. | + Yes | Adjusted for age, puberty status, parent's income level, self‐reported activity, inactivity and number of overweight parents. |
| 9.6 years; regression | BMI | z‐score, 6‐years change | 6 | Dietary fat (single 24‐hour recall at baseline) | %TE | n boys = 147; regression result. β = ‐0.011, SE 0.009, P = 0.2. After 6 years, for every 1% increase in energy intake from total fat, BMI will decrease by 0.011 z‐score in boys. | ‐ Yes | Adjusted for age, puberty status, parent's income level, self‐reported activity, inactivity and number of overweight parents. |
| 2 years; regression | BMI | kg/m2 | 6 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, every year during 4, 5 and 6 years) | g | n overall = 70; regression result. B = 0.01, SE 0.01, P = 0.0039, F‐test = 9; R2 = 0.43, P = 0.0001, F‐test = 17.6. After 6 years, for every 1 g increases in the fat intake, BMI will increase by 0.01 kg/m2. | ‐ No | Adjusted for baseline BMI, birthweight, cereal introduction age, breastfeeding duration, dietary variety score 42‐84 months, adiposity rebound, picky eater at age 6 years, sedentary activity at ages 6 and 7 years, foods liked at age 8 years, mother's BMI and father's BMI. |
| 2 years; regression | BMI | z‐score | 9 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6 and 9 years) | NR | n overall = 243; regression result. β = 0.122, P > 0.1; R2 = 0.38, P < 0.0001. After 9 years, increase in the total fat intake will increase BMI by 0.122 z‐score. | + Yes | Adjusted for baseline BMI‐z score, gender and parental BMI. |
| 10.1 years; regression | BMI | kg/m2, 10‐years change | 10 | Total fat intake (single 3‐day dietary records at 1, 2, 3, 4, 5, 7, 8 and 10 years) × baseline IR | %TE | n white girls = 241; regression result. B = 0.029, SE 0.0028, P < 0.0001, partial R2 = 27. After 10 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.029 kg/m2 in white girls. | + Yes | Adjusted for age, BMI, IR and maturation stage at baseline; change in IR over 10 years' follow‐up; percentage of calories from protein, fat and CHO (mean of interviews) during 10 years' follow‐up; and interaction terms (nutrients × baseline IR). |
| 10.1 years; regression | BMI | kg/m2, 10‐years change | 10 | Total fat intake (single 3‐day dietary records at 1, 2, 3, 4, 5, 7, 8 and 10 years) × baseline IR | %TE | n black girls = 280; regression result. B = 0.012, SE 0.0032, P = 0.0002, partial R2 = 3.6. After 10 years, for every 1% increase in energy intake from total fat, BMI will increase by 0.012 kg/m2 in black girls. | ‐ Yes | Adjusted for age, BMI, IR and maturation stage at baseline; change in IR over 10 years' follow‐up; percentage of calories from protein, fat and CHO (mean of interviews) during 10 years' follow‐up; and interaction terms (nutrients × baseline IR). |
| BMI at > 10 years: 2 cohort studies; 2 analyses (n = 330) in boys and girls aged 2‐3 years | ||||||||
| 2 years; regression | BMI | z‐score | 13 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6, 9, 11 and 13 years) | NR | n overall = 218; regression result. β = 0.16, 0.05 < P ≤ 0.1; R2 = 0.23, P < 0.0001. After 13 years, increase in the total fat intake will increase BMI by 0.16 z‐score. | + Yes | Adjusted for baseline BMI‐z score, gender, mother's BMI and father's BMI. |
| 3.2 years; mean end values per group | BMI | z‐score | 17 | Total fat intake (single 3‐day weighed dietary record at baseline and each year follow‐up) | LF (32%TE); HF (40%TE) | n overall = 112 (LF = 55; HF = 57); mean end values (SD). Baseline: LF = 0.36 (0.75); HF = 0.07 (0.81). At 17 years: LF = 0.23 (0.9); HF = 0.11 (1.09). After 17 years, on average BMI decrease 0.13 z‐score in the LF (32%TE) group while increase 0.04 z‐score in the HF (40%TE) group. | + No | No matching reported. No adjustments for prognostic variables. |
| aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome. bUnpublished data provided by study authors. c"Energy dense, high fat, low fibre" dietary pattern reflected high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes, the high intake of these foods increase the individual’s dietary pattern z‐score. dOverweight/obese was defined by IOTF for children aged 14 years (boys, BMI > 22.62 kg/m2; girls, BMI > 23.34 kg/m2), and aged 17 years (boys, BMI > 24.46 kg/m2; girls, BMI > 24.70 kg/m2). %TE: percentage of total energy; B: unstandardised beta‐coefficient; β: standardised beta‐coefficient; BMI: body mass index; CHO: carbohydrate; CI: confidence interval; df: degrees of freedom; FFQ: Food Frequency Questionnaire; HF: high fat; IR: insulin resistance; IOTF: International Obesity Task Force; LF: low fat; MD: mean difference; n: number of participants; NA: not applicable; NR: not reported; NS: not significant; OR: odds ratio; SD: standard deviation; SE: standard error; SES: socioeconomic status; TV: television. | ||||||||
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted? (yes/no) | Matched groups or adjusted for (or both) | |
| Waist circumference at > 1to 2 years: 1 cohort study; 1 analysis (n = 310) in boys and girls aged 13 years | |||||||||
| 12.5 years; regression | WC | cm | 2 | Total fat intake (single 24‐hour recall at baseline) | per 10 g | n overall = 310, regression result. B = 0.31 (95% CI 0.08 to 0.58), P ≤ 0.05. After 2 years, for every 10‐g increase in the total fat intake of children, WC will increase by 0.31 cm. | + No | Age, gender, baseline BMI z‐score, baseline WC, moderate to vigorous physical activity, vegetables and fruit, fibre, milk, sodium and added sugar. | |
| Waist circumference at > 2to 5 years: 1 cohort study; 4 analyses (n = 2680) in boys and girls aged 14 years | |||||||||
| 14 years; regression and OR higher vs lower dietary pattern z‐score | WC | WC ≥ 80 cm, odds | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n boys = 697, regression result. OR = 1 (95% CI 0.82 to 1.22). After 3 years, the ratio of odds that WC is ≥ 80 cm is the same in boys with higher dietary pattern z‐scores compared to the odds in boys with lower dietary pattern z‐scores, during the period from 14 to 17 years of age. | 0 NA; exposure includes energy intake | Age, dietary misreporting, physical fitness, smoking and BMI z‐score. | |
| 14 years; regression and OR higher vs lower dietary pattern z‐score | WC | WC ≥ 80 cm, odds | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n girls = 643, regression result. OR = 1.28 (95% CI 1.00 to 1.63). After 3 years, the ratio of odds that WC is ≥ 80 cm is 1.28 greater in girls with higher dietary pattern z‐scores compared to the odds in girls with lower dietary pattern z‐scores, during the period from 14 to 17 years of age. | + NA; exposure includes energy intake | Age, dietary misreporting, physical fitness, smoking and BMI z‐score. | |
| 14 years; regression | WC | z‐score | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n boys = 697, regression result. β = 0.003 (95% CI ‐0.02 to 0.03). After 3 years, for every 1 unit increase in z‐score of the energy‐dense, high‐fat and low‐fibre dietary pattern of boys, WC will increase by 0.003 z‐scores. | + NA; exposure includes energy intake | Age, dietary misreporting, physical fitness, smoking and BMI z‐score. | |
| 14 years; regression | WC | z‐score | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n girls = 643, regression result. β = 0.04 (95% CI 0.01 to 0.07). After 3 years, for every 1 unit increase in z‐score of the energy‐dense, high‐fat and low‐fibre dietary pattern of girls, WC will increase by 0.04 z‐scores. | + NA; exposure includes energy intake | Age, dietary misreporting, physical fitness, smoking and BMI z‐score. | |
| Waist circumference at > 5to 10 years: 1 cohort study; 2 analyses (n = 512) in girls aged 10 years | |||||||||
| 10.1 years; regression | WC | cm, 10‐years change | 10 | Total fat intake (single 3‐day dietary records at 1, 2, 3, 4, 5, 7, 8 and 10 years) × baseline IR | %TE | n white girls = 236. B = 0.053, SE 0.0065, P < 0.0001. After 10 years, for every 1% increase in energy intake from total fat in white girls, WC will increase by 0.053 cm. | + Yes | Age, WC, IR, and maturation stage at baseline; change in IR over 10‐years follow‐up; percentage of calories from protein, fat, and CHO (mean of interviews) during 10‐years follow‐up; and interaction terms (nutrients × baseline IR). | |
| 10.1 years; regression | WC | cm, 10‐years change | 10 | Total fat intake (single 3‐day dietary records at 1, 2, 3, 4, 5, 7, 8 and 10 years) × baseline IR | %TE | n black girls = 276. B = 0.028, SE 0.0056, P < 0.0001. After 10 years, for every 1% increase in energy intake from total fat in black girls, WC will increase by 0.028 cm. | + Yes | "Age, waist circumference, IR, and maturation stage at baseline; change in IR over 10‐y follow‐up; percentage of calories from protein, fat, and CHO (mean of interviews) during 10‐y follow‐up; and interaction terms (nutrients baseline IR)." | |
| aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome. b"Energy dense, high fat, low fibre" dietary pattern reflected high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes, the high intake of these foods increase the individual’s dietary pattern z‐score. %TE: percentage of total energy; B: unstandardised beta‐coefficient; β: standardised beta‐coefficient; BMI: body mass index; CHO: carbohydrate; CI: confidence interval; FFQ: Food Frequency Questionnaire; IR: insulin resistance; n: number of participants; NA: not applicable; OR: odds ratio; WC: waist circumference. | |||||||||
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (years) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) | |||
| Body fat at 1 year: 1 cohort study; 1 analysis (n = 411) in boys and girls aged 7 years | |||||||||||
| 6.8 years; regression | Body fat (skinfold thickness) | % | 1 | Total fat intake (single 7‐day weighed dietary record at baseline and 1 year) | g | n overall = 411, regression result. B = 0.011, SE 0.017, P < 0.05. After 1 year, for every 1 g increase in the total fat intake of children, body fat will increase by 0.01%. | + No | Adjusted for age, gender and physical activity. | |||
| Body fat at > 1to 2 years: 1 cohort study; 1 analysis (n = 625) in boys and girls aged 5 years | |||||||||||
| 5.2 years; regression | Body fat (DEXA) | kg | 2 | Energy‐dense, high‐fat, low‐fibre dietary patternc (single 3‐day dietary record at baseline and 2 years) | z‐score | n overall = 625, regression result. B = 0.28 (95% CI 0.05 to 0.53), P = 0.02. After 2 years, for every 1 unit increase in the dietary pattern z‐score of children, body fat will increase by 0.28 kg. | + NA; exposure includes energy intake | Adjusted for height at age 9 years, gender, misreporting status, maternal BMI, maternal education (5 categories), overweight status (by BMI) at baseline and television watching at 54 months. | |||
| Body fat at > 2to 5 years: 3 cohort studies; 6 analyses (n = 968) in boys and girls aged 2‐14 years | |||||||||||
| 13.9 years; regression | Body fat (skinfold thickness, BIA) | % | 3‐5 | Total fat intake (single FFQ at baseline and once during follow‐up period) | %TE | n girls = 265, regression result. B = ‐0.005, SE 0, P = 0.03. After 3‐5 years, for every 1 % increase in energy intake from total fat of girls, body fat will decrease by 0.005%. | ‐ No | Adjusted for age, ethnicity, protein calories, CHO calories, physical activity, physical inactivity and SES. | |||
| 5.2 years; regression | Body fat (DEXA) | kg | 4 | Energy‐dense, high‐fat, low‐fibre dietary patternc (single 3‐day dietary record at baseline and 2 years) | z‐score | n overall = 483, regression result. B = 0.15 (95 % CI ‐0.15 to 0.45), P = 0.34. After 4 years, for every 1 unit increase in the dietary pattern z‐score of children, body fat will increase by 0.15 kg. | + NA; exposure includes energy intake | Adjusted for height at age 9 years, gender, misreporting status, maternal BMI, maternal education (5 categories), overweight status (by BMI) at baseline and television watching at 54 months. | |||
| 2 years; regression | Body fat (DEXA) | % | 4 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, and yearly at 4 years) | NR | n overall = 53, regression result. B = 0.619, SE 0.261, P = 0.02, F‐test = 5.63, R2 = 0.51, p = 0.0001, F‐test = 7.88. After 4 years, for every 1 unit increase in total fat intake of children, body fat will increase by 0.61%. | + No | Adjusted for baseline BMI, parental BMI, gender, protein, calcium and monounsaturated fat. | |||
| 2 years; regression | Body fat (DEXA) | g | 4 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, and yearly at 4 years) | NR | n overall = 53, regression result. B = 178.65, SE 70.06, P = 0.01, F‐test = 6.5, R2 = 0.51, P = 0.0001, F‐test = 9.84. After 4 years, for every 1 unit increase in total fat intake of children, body fat will increase by 178 g. | + No | Adjusted for baseline BMI, parental BMI, gender, protein, calcium and monounsaturated fat. | |||
| 2 years; regression | Body fat (DEXA) | % | 4 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, and yearly at 4 years). | Number of servings | n overall = 53, regression result. B = 0.465, SE 0.255, P = 0.07, F‐test = 3.34. R2 = 0.47, P = 0.0001, F‐test = 6.93. After 4 years, for every 1 unit increase in the number of fat servings, body fat will increase by 0.47%. | + No | Adjusted for baseline BMI, parental BMI, gender, protein, calcium and monounsaturated fat. | |||
| 2 years; regression | Body fat (DEXA) | g | 4 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, and yearly at 4 years). | Number of servings | n overall = 53, regression result. B = 136.48, SE 69.74, P = 0.06, F‐test = 3.83, R2 = 0.47, p = 0.0001, F‐test = 8.31. After 4 years, for every 1 unit increase in the number of fat servings, body fat will increase by 136 g. | + No | Adjusted for baseline BMI, parental BMI, gender, protein, calcium and monounsaturated fat. | |||
| Body fat at > 5to 10 years: 1 cohort study; 3 analyses (n = 156) in boys and girls aged 2 years | |||||||||||
| 2 years; regression | Body fat (DEXA) | % | 6 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, every year during 4, 5 and 6 years). | g | n overall = 52, regression result. B = 0.08, partial R2 = 0.06, P = 0.001, F‐test = 4.66, R2 = 0.336, P = 0.002. After 6 years, for every 1 g increase in total fat intake of children, body fat will increase by 0.08%. | + No | Adjusted for gender, sedentary activity, intakes of calcium and polyunsaturated fat. | |||
| 2 years; regression | Body fat (DEXA) | % | 6 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day dietary record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, every year during 4, 5 and 6 years). | g | n overall = 52, regression result. B = 0.09, partial R2 = 0.02, P = 0.001, F‐test = 4.37, R2 = 0.322, P = 0.002. After 6 years, for every 1 g increase in total fat intake, body fat will increase by 0.09%. | + No | Adjusted for gender, sedentary activity, calcium intake, and polyunsaturated fat intake and father's BMI. | |||
| 2 years; regression | Body fat (DEXA) | kg | 6 | Longitudinal dietary fat (single 24‐hour dietary recall and 2‐day food record at baseline, every 3 months during 1 year, every 6 months during 2 and 3 years, every year during 4, 5 and 6 years) | g | N overall = 52, regression result. B = 0.034, partial R2 = 0.06, P = 0.01, F‐test = 4.19, R2 = 0.26, P = 0.006. After 6 years, for every 1 g increase in total fat intake of children, body fat will increase by 0.03 kg. | + No | Adjusted for sedentary activity, calcium intake and polyunsaturated fat intake. | |||
| aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction, inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association between total fat intake and the outcome. bUnpublished data provided by study authors. c"Energy dense, high fat, low fibre" dietary pattern reflected high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes, the high intake of these foods increase the individual's dietary pattern z‐score. %TE: percentage of total energy; B: unstandardised beta‐coefficient; BIA: bioelectrical impedance, BMI: body mass index; CHO, carbohydrate; CI: confidence interval; DEXA: dual energy X‐ray absorptiometry; FFQ: food frequency questionnaire; n: number of participants; NA: not applicable; NR: not reported; SD: standard deviation; SE: standard error; SES: socioeconomic status. | |||||||||||
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| Fat mass index at > 2to 5 years: 1 cohort study; 1 analysis (n = 4002) in boys and girls aged 8 years | ||||||||
| 7.5 years; regression | Fat mass indexb | z‐score | 4 | Energy‐dense, high‐fat, low‐fibre dietary patternc (single 3‐day dietary records at baseline and 2 years) | z‐score | n overall = 4002, regression result. β = 0.07 (95% CI 0.05 to 0.10), P ≤ 0.0001. After 4 years, for every 1 z‐score increase in the dietary pattern, the fat mass index will increase by 0.07 z‐scores. | + NA; exposure includes energy intake | Adjusted for gender, age at dietary assessment, dietary misreporting, total physical activity at 11 years, maternal prepregnancy BMI and maternal education. |
| Fat mass index at > 5to 10 years: 1 cohort study; 5 analyses (n = 21,542) in boys and girls aged 8 years | ||||||||
| 7.5 years; regression | Fat mass indexb | z‐score | 8 | Energy‐dense, high‐fat, high‐sugar, low‐fibre dietary patternc (single 3‐day dietary record at baseline, 3 and 6 years) | z‐score | n overall = 4729, regression result. β = 0.04 (95% CI 0.01 to 0.08), P = 0.028. After 8 years, for every 1 z‐score increase in the dietary pattern, the fat mass index will increase by 0.04 z‐scores. | + NA; exposure includes energy intake | Adjusted for age, gender, dietary misreporting, physical activity and maternal social class. |
| 7.5 years; regression | Fat mass indexb | z‐score | 8 | Non‐energy‐dense, high‐sugar, LF dietary patternd (single 3‐day dietary record at baseline, 3 and 6 years) | z‐score | n overall = 4729, regression result. β = ‐0.03 (95% CI ‐0.07 to 0.02), P = 0.22. After 8 years, for every 1 z‐score increase in the dietary pattern, the fat mass index will decrease by 0.03 z‐scores. | ‐ NA; exposure includes energy intake | Adjusted for age, gender, dietary misreporting, physical activity and maternal social class. |
| 7.5 years; regression | Fat mass indexb | z‐score | 8 | Energy‐dense, high‐fat, low‐fibre dietary patternc (single 3‐day dietary record at baseline, 3 and 6 years) | z‐score | n overall = 2626, regression result. β = 0.06 (95% CI 0.03 to 0.10), P = 0.0004. After 8 years, for every 1 z‐score increase in the dietary pattern, the fat mass index will increase by 0.06 z‐scores. | + NA; exposure includes energy intake | Adjusted for gender, age at dietary assessment, dietary misreporting, total physical activity at 11 years, maternal pre‐pregnancy BMI and maternal education. |
| 7.5 years; regression | Fat mass indexb | FMI z‐score > 80th percentile; odds | 8 | Energy‐dense, high‐fat, high‐sugar, low‐fibre dietary patternc (single 3‐day dietary record at baseline, 3 and 6 years) | z‐score | n overall = 4729, regression result. OR 1.11 (95% CI 0.97 to 1.28), P = 0.14. After 8 years, the ratio of odds for having FMI z‐score > 80th percentile is 1.11 greater in children with higher dietary pattern z‐scores compared to the odds in children with lower dietary pattern z‐scores. | + NA; exposure includes energy intake | Adjusted for age, gender, dietary misreporting, physical activity and maternal social class. |
| 7.5 years; regression | Fat mass indexb | FMI z‐score > 80th percentile; odds | 8 | Non‐energy‐dense, high‐sugar, LF dietary patternd (single 3‐day dietary record at baseline, 3 and 6 years) | z‐score | n overall = 4729, regression result. OR 0.92 (95% CI 0.78 to 1.09), P = 0.34. After 8 years, the ratio of odds for having FMI z‐score > 80th percentile is 0.92 smaller in children with higher dietary pattern z‐scores compared to the odds in children with lower dietary pattern z‐scores. | ‐ NA; exposure includes energy intake | Adjusted for age, gender, dietary misreporting, physical activity and maternal social class. |
| aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome; bFMI was calculated by dividing fat mass (measured by dual‐energy X‐ray Absorptiometry) (kg) by height (m) raised to the optimum power (calculated by using log‐log regression analysis) to remove any residual correlation between fat mass and height; c"Energy‐dense, high‐fat, low‐fibre" dietary pattern reflected high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes, the high intake of these foods increase the individual’s dietary pattern z‐score. dNon‐energy‐dense, high‐sugar, low‐fat dietary pattern reflected higher intakes of sugary foods including sugar‐sweetened beverages, fruit juices, ready‐to‐eat breakfast cereals (low‐fibre breakfast cereals) and low intakes of whole milk, margarines and oils, cheese and crisps. β: standardised beta‐coefficient; BMI: body mass index; FMI: Fat Mass Index ; n: number of participants; NA: not applicable; OR: odds ratio. | ||||||||
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| Sum of 4 skinfolds (BC, TC, SC, SI) at 1 year: 1 cohort study; 1 analysis (n = NR) in boys and girls aged 6 years | ||||||||
| 6.2 years; mean end values per group | Sum of skinfolds (BC, TC, SS, SI) | mm | 1 | Total fat intake (multiple 24‐hour recalls at baseline, 3 and 6 months and 1 year) | LF quintile (24%TE); HF quintile (34%TE) | n overall = NR (LF = NR, HF = NR), mean end values (95% CI). Baseline: LF = 24.7 (95% CI 23 to 26.5); HF = 28.8 (95% CI 26.1 to 31.8). At 1 year: (reported in the figure without exact values), LF = lower than baseline; HF = greater than baseline. After 1 year, the sum of skinfolds will decrease in children with a low‐fat intake, and increase in children with high‐fat intake | + No | No matching reported. No adjustment for prognostic variables. |
| Sum of 4 skinfolds (BC, TC, SC, SI) at > 1to 2 years: 1 cohort study; 1 analysis (n = 126) in boys and girls aged 2 years | ||||||||
| 2 years; mean end values per group | Sum of skinfolds (TC, BC, SS, SI) | mm | 2 | Total fat intake (single 3‐day weighed dietary record at baseline and 2 years) | LF < 30%TE; HF > 35%TE | n overall = 126 (LF = 14, HF = 112), mean end values (SD). Baseline: LF = 33.4 (6.8); HF = 32.8 (6.3). At 2 years: LF (n = 20) = 31 (9.2); HF (n = 76) = 31.4 (6.3); P > 0.05. After 2 years, the sum of skinfolds of children with LF intakes will decrease by 2.4 mm on average, and by 1.4 mm in children with HF intake. | + No | No matching reported. No adjustment for prognostic variables. |
| Sum of 4 skinfolds at > 2to 5 years: 1 cohort study; 1 analysis (n ˜ 126) in boys and girls aged 2 years | ||||||||
| 2 years; mean end values per group | Sum of skinfolds (TC, BC, SS, SI) | mm | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | LF < 30%TE; HF > 35%TE | n overall = 126 (LF = 14, HF = 112), mean end values (SD). Baseline: LF = 33.4 (6.8); HF = 32.8 (6.3); P > 0.05. At 4 years: LF (n = 14) = 27.2 (8); HF (n = 88) = 29.2 (8.9); P > 0.05. After 4 years, the sum of skinfolds of children with LF intakes will decrease by 6.2 mm on average, and by 3.6 mm in children with HF intake | + Yes | No matching reported. No adjustment for prognostic variables. |
| Sum of 4 skinfolds at > 5to 10 years: 1 cohort study; 1 analysis (n = 126) in boys and girls aged 2 years | ||||||||
| 2 years; mean end values per group | Sum of skinfolds (TC, BC, SS, SI) | mm | 6 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6 years) | LF < 30%TE; HF > 35%TE | n overall = 126 (LF=14, HF=112), mean end values (SD). Baseline LF = 33.4 (6.8); HF = 32.8 (6.3), P > 0.05. At 6 years: LF (n = 13) = 32.8 (13.3); HF (n = 72) = 31.8 (12.8), P > 0.05. After 6 years, the sum of skinfolds of children with LF intakes will decrease by 0.6 mm on average, and by 1 mm in children with HF intake. | ‐ No | No matching reported. No adjustment for prognostic variables. |
| Sum of 3 skinfolds at > 2to 5 years: 1 cohort study; 1 analysis (n = NR) in boys and girls aged 10 years | ||||||||
| 9.6 years; regression | Sum of skinfolds (TC, SS, SI) | mm | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | %TE | n overall = NR; regression result. B = ‐0.005, P = 0.2. After 3 years, for every 1% increase in energy intake from total fat of children, the sum of skinfolds will decrease by 0.005 mm | ‐ Yes | Adjusted for gender, physical activity, treatment, visit number, other sources of energy than fat, and for interactions: fat intake‐by‐treatment, fat intake‐by‐sex, fat intake‐by‐visit number and visit number‐by‐treatment. |
| Sum of 2 skinfolds at > 1to 2 years: 1 cohort study; 1 analysis (n = 192) in girls aged 5 years | ||||||||
| 5 years; mean change per group | Sum of skinfolds (TC, SS) | mm | 2 | Total fat intake (multiple 24‐hour recall at baseline) | LF ≤ 30%TE, HF > 30%TE | n girls = 192 (LF = 84; HF = 108); mean change (SD). Baseline: NR. LF = 0.9 (3.67), HF = 2.1 (5.2); P < 0.05. MD ‐1.2 (95% CI ‐2.46 to 0.06). After 2 years, the sum of skinfolds of girls with LF intake will increase on average by 1.2 mm less than girls with HF intake. | + No | No matching reported. No adjustment for prognostic variables. |
| aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction, inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome. %TE: percentage of total energy; BC: biceps; CI: confidence interval; HF: high fat; LF: low fat; MD: mean difference; n: number of participants; NA: not applicable; NR: not reported; SD: standard deviation; SI: supra‐ileac; SS: subscapular; TC: triceps. | ||||||||
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| Subscapular skinfold at > 1to 2 years: 1 cohort study; 1 analysis (n = 155) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Subscapular skinfold | z‐score | 2 | Total fat intake (single 3‐day weighed dietary record at baseline and 2 years) | NR | n overall = 155; regression result. β = 0.081, P > 0.1, R2 = 0.47, P < 0.001. After 2 years, increase in the total fat intake will increase subscapular skinfold by 0.081 z‐score | + Yes | Adjusted for subscapular z‐score at baseline, energy intake, gender, mother' subscapular and father' subscapular. |
| Subscapular skinfold at > 2to 5 years: 1 cohort study; 1 analysis (n = 152) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Subscapular skinfold | z‐score | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | NR | n overall = 152; regression result. β = 0.072, P > 0.1, R2 = 0.38, P < 0.001. After 4 years, increase in the total fat intake will increase subscapular skinfold by 0.072 z‐score. | + Yes | Adjusted for subscapular z‐score at baseline, energy intake, gender, mother' subscapular and father' subscapular. |
| Subscapular skinfold at > 5to 10 years: 1 cohort study; 1 analysis (n = 243) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Subscapular skinfold | z‐score | 9 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6 and 9 years) | NR | n overall = 243; regression result. β = 0.069, P > 0.1, R2 = 0.26, P < 0.001. After 9 years, increase in the total fat intake will increase subscapular skinfold by 0.069 z‐score. | + Yes | Adjusted for subscapular z‐score at baseline, energy intake, gender, mother' subscapular and father' subscapular. |
| Subscapular skinfold at > 10 years: 1 cohort study; 1 analysis (n = 218) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Subscapular skinfold | z‐score | 13 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6, 9, 11 and 13 years) | NR | n overall = 218; regression result. β = 0.233, P ≤ 0.01. After 13 years, increase in the total fat intake will increase subscapular skinfold by 0.233 z‐score. | + Yes | Adjusted for subscapular z‐score at baseline, energy intake, gender, mother' subscapular and father' subscapular. |
| Triceps skinfold at > 1to 2 years: 1 cohort study; 1 analysis (n = 155) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Triceps skinfold | z‐score | 2 | Total fat intake (single 3‐day weighed dietary record at baseline and 2 years) | NR | n overall = 155; regression result. β = 0.038, P > 0.1, R2 = 0.27, P ≤ 0.001. After 2 years, increase in the total fat intake will increase triceps skinfold by 0.038 z‐score. | + Yes | Adjusted for triceps z‐score at baseline, gender, mother's triceps and father's triceps. |
| Triceps skinfold at > 2to 5 years: 1 cohort study; 1 analysis (n = 152) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Triceps skinfold | z‐score | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | NR | n overall = 152; regression result. Β = 0.11, P > 0.1, R2 = 0.043, P > 0.01. After 4 years, increase in the total fat intake will increase triceps skinfold by 0.11 z‐score | + Yes | Adjusted for triceps z‐score at baseline, gender, mother's triceps and father's triceps. |
| Triceps skinfold at > 5to 10 years: 1 cohort study; 1 analysis (n = 243) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Triceps skinfold | z‐score | 9 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6 and 9 years) | NR | n overall = 243; regression result. β = 0.059, P > 0.1; R2 = 0.12, P ≤ 0.01. After 9 years, increase in the total fat intake will increase triceps skinfold by 0.059 z‐score | + Yes | Adjusted for triceps z‐score at baseline, gender, mother's triceps and father's triceps. |
| Triceps skinfold at > 10 years: 1 cohort study; 1 analysis (n = 218) in boys and girls aged 2 years | ||||||||
| 2 years; regression | Triceps skinfold | z‐score | 13 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years, single 4‐day weighed dietary record at 6, 9, 11 and 13 years) | NR | n overall = 218; regression result. β = 0.164; 0.05 < P ≤ 0.1. After 13 years, increase in the total fat intake will increase triceps skinfold by 0.164 z‐score | + Yes | Adjusted for triceps z‐score at baseline, gender, mother's triceps and father's triceps. |
| aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome; B: unstandardised beta‐coefficient; β: standardised beta‐coefficient; n: number of participants; NR: not reported. | ||||||||
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| LDL‐C at > 2to 5 years: 1 cohort study; 2 analyses (n = 1163) in boys and girls aged 14 years | ||||||||
| 14 years; regression | LDL‐C | mmol/L | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n girls = 558, regression result. B = 0.04 (95% CI ‐0.01 to 0.08). After 3 years, for every 1 z‐score increase in the dietary pattern, LDL‐C will increase by 0.04 mmol/L in girls. | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 14 years; regression | LDL‐C | mmol/L | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n boys = 605, regression result. B = 0.001 (95% CI ‐0.04 to 0.03). After 3 years, for every 1 z‐score increase in the dietary pattern, LDL‐C will increase by 0.001 mmol/L in boys. | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| HDL‐C at > 2to 5 years: 2 cohort studies; 3 analyses (n = 1393) in boys and girls aged 13 and 14 years | ||||||||
| 14 years; regression; | HDL‐C | mmol/L | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n girls = 558, regression result. B = 0.02 (95% CI 0.002 to 0.04). After 3 years, for every 1 z‐score increase in the dietary pattern HDL‐C will increase by 0.02 mmol/L in girls. | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 14 years; regression; | HDL‐C | mmol/L | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (single FFQ at baseline and 3 years) | z‐score | n boys = 605, regression result. B = ‐0.002 (95% CI ‐0.02 to 0.01). After 3 years, for every 1 z‐score increase in the dietary pattern HDL‐C will decrease by 0.002 mmol/L in boys. | ‐ NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 12.5 years; regression; | HDL‐C | mmol/L | 3 | Total fat intake (dietary history at baseline and 3 years) | %TE | n girls = 230, regression result. β = ‐0.21, SE 0.1, P = 0.031. After 3 years, for every 1% increase in energy intake from total fat, HDL‐C will decrease by 0.21 mmol/L in girls. | ‐ Yes | Adjusted for sexual maturation, SES, cholesterol intake, CHO intake, cigarette smoking |
| Triglycerides at > 2to 5 years: 1 cohort study; 2 analyses (n = 1163) in boys and girls aged 14 years | ||||||||
| 14 years; regression | Triglycerides | % | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (multiple FFQs at baseline and 3 years) | z‐score | n girls = 558, regression result. B = 1 (95% CI 0 to 3). After 3 years, for every 1 z‐score increase in the dietary pattern, triglycerides will increase by 1% in girls. | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| 14 years; regression | Triglycerides | % | 3 | Energy‐dense, high‐fat and low‐fibre dietary patternb (multiple FFQs at baseline and 3 years) | z‐score | n boys = 605, regression result. B = 1 (95% CI 0 to 3). After 3 years, for every 1 z‐score increase in the dietary pattern, triglycerides will increase by 1% in boys | + NA; exposure includes energy intake | Adjusted for age, dietary misreporting, physical fitness, smoking and BMI z‐score. |
| aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome. b"Energy dense, high fat, low fibre" dietary pattern was defined as high intakes of processed meat, chocolate and confectionery, low‐fibre bread, crisps and savoury snacks, fried and roasted potatoes, the high intake of these foods increase the individual’s dietary pattern z‐score. %TE: percentage of total energy; B: unstandardised beta‐coefficient; BMI: body mass index; CHO: carbohydrate; FFQ: food frequency questionnaire; LDL‐C: low‐density lipoprotein cholesterol; HDL‐C: high‐density lipoprotein cholesterol; NA: not applicable; SE: standard error; SES: socioeconomic status. | ||||||||
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| SBP at > 1to 2 years: 1 cohort study; 1 analysis (n = 310) in boys and girls aged 13 years | ||||||||
| 12.5 years; regression | SBP | z‐score | 2 | Total fat intake (single 24‐hour recall at baseline) | per 10 g | n overall = 310; regression result. β = 0.03 (95% CI 0.00004 to 0.06), P < 0.05. After 2 years, for every 10 g increase in total fat intake, SBP will increase by 0.03 z‐score | + No | Adjusted for baseline BMI z‐score, baseline SBP and DBP, moderate to vigorous physical activity, vegetables and fruit, fibre, milk, sodium and added sugar. |
| SBP at > 2to 5 years: 1 cohort study; 1 analysis (n = NR) in boys and girls aged 10 years | ||||||||
| 9.6 years; regression | SBP | mmHg | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | g | n overall = NR; regression result. B = 0.4, P < 0.1. After 3 years, for every 1 g increase in total fat intake, SBP will increase by 0.4 mmHg | + Yes | Adjusted for height, weight and gender, with all sources of calories in the model. |
| DBP at > 1to 2 years: 1 cohort study; 1 analysis (n = 310) in boys and girls aged 13 years | ||||||||
| 12.5 years; regression | DBP | z‐score | 2 | Total fat intake (single 24‐hour recall at baseline) | per 10 g | n overall = 310. β = 0.03 (95% CI 0.003 to 0.05), P < 0.05. After 2 years, for every 10 g increase in total fat intake, DBP will increase by 0.03 z‐scores | + No | Adjusted for baseline BMI z‐score, baseline SBP and DBP, moderate to vigorous physical activity, vegetables and fruit, fibre, milk, sodium and added sugar. |
| DBP at > 2to 5 years: 1 cohort study; 1 analysis (n = NR) in boys and girls aged 10 years | ||||||||
| 9.6 years; regression | DBP | mmHg | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | g | n overall = NR. B = 0.43, 0.01 < P < 0.06. After 3 years, for every 1 g increase in total fat intake, DBP will increase by 0.43 mmHg | + Yes | Adjusted for height, weight and gender, with all sources of calories in the model. |
| aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome. B: unstandardised beta coefficient; β: standardised beta‐coefficient; BMI: body mass index; CI: confidence interval; DBP: diastolic blood pressure; NR: not reported; SBP: systolic blood pressure. | ||||||||
| Study ID; mean age at baseline; analysis | Outcome | Outcome units | Time point (year) | Exposure | Exposure unit | Results of association (all reported values) | Direction;a energy intake adjusted (yes/no) | Matched groups or adjusted for (or both) |
| Height at 1 year: 2 cohort studies; 2 analyses (n ˜ 740) in children aged 2‐6 years | ||||||||
| 2 years; mean end values per group | Relative heightb | % | 1 | Total fat intake (single 4‐day dietary record at baseline, 1.5 and 2 years) | LF (27.7‐28.7 %TE); HF (> 28.7 %TE) | n overall = 740 (LF = 35, HF = 705); mean end values (SD). Baseline: LF = 0.30 (0.9); HF = 0.32 (0.9). At 1 year: LF = 0.18 (1.0); HF = 0.16 (0.9); P = 0.93. After 1 year, on average children with LF intake (27.7‐28.7 %TE) have a relative height change of 0.12% compared to 0.16% for children with HF intake (> 28.7 %TE). | ‐ No | No matching reported. No adjustment for prognostic variables. |
| 6.2 years; mean end values per group | Height | z‐score | 1 | Total fat intake (multiple 24‐hour dietary recalls at baseline and 1 year) | LF quintile (24%TE) HF quintile (34%TE) | n overall = NR (LF = NR, HF = NR); mean end values (SD NR). Baseline: LF = ‐0.23; HF = 0.17. At 1 year: LF = ‐0.11; HF = 0.22. After 1 year, on average children in LF intake (24%TE) quintile gain 0.12 z‐score in height while children in HF intake (34%TE) quintile gain 0.05 z‐score in height. | + No | No matching reported. No adjustment for prognostic variables. |
| Height at > 1to 2 years: 2 cohort study; 3 analysis (n = 836) in boys and girls aged 2‐4 years | ||||||||
| 3.6 years; mean end values per group | Height | cm | 1.5 | Total fat intake (single 3‐day unweighed food record at baseline) | LF quintile (30.4%TE) HF quintile (41.8%TE) | n boys, at baseline = 439; at 1.5 years = 387 (LF = NR, HF = NR); mean end values (SD). Baseline: LF = 99.9 (95% CI 99.2 to 100.5); HF = 99.3 (95% CI 98.7 to 99.9). At 1.5 years: LF = 110.7 (95% CI 109.9 to 111.5); HF = 109.9 (95% CI 109.1 to 110.7). After 1.5 years, on average boys with LF intake (30.4%TE) quintile gain 10.8 cm in height while boys with HF intake (41.8%TE) quintile gain 10.6 cm in height. | ‐ No | No matching reported. No adjustment for prognostic variables. |
| 3.6 years; mean end values per group | Height | cm | 1.5 | Total fat intake (single 3‐day unweighed food record at baseline) | LF quintile (30.4%TE) HF quintile (41.8%TE) | n girls, at baseline = 351; at 1.5 years = 323) (LF = NR, HF = NR); mean end values (SD). Baseline: LF = 99.9 (95% CI 98.0 to 99.8). HF = 98.3 (95% CI 97.6 to 99.1). At 1.5 years: LF = 110.0 (95% CI 108.9 to 111.1); HF = 109.3 (95% CI 108.3 to 110.3). After 1.5 years, on average girls in LF intake (30.4%TE) quintile will gain10.1 cm in height while girls in HF intake (41.8%TE) quintile will gain 11 cm in height. | + No | No matching reported. No adjustment for prognostic variables. |
| 2 years; mean end values per group | Height | cm | 2 | Total fat intake (single 3‐day weighed dietary records at baseline and 2 years) | LF < 30%TE HF > 35%TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 86.1 (2.6); HF = 87.7 (3.3). At 2 years: LF (n = 20) = 107 (5.5); HF (n = 76) = 106 (3.9); P = NS. After 2 years, on average children with LF intake (< 30%TE) gain 20.9 cm in height, while children with HF intake > 35%TE) gain 18.3 cm in height. | ‐ No | No matching reported. No adjustment for prognostic variables. |
| Height at > 2to 5 years: 3 cohort studies; 3 analyses (n = 973) in boys and girls aged 2‐10 years | ||||||||
| 4.4 years; mean change per group | Height | cm/year | 2.1 | Total fat intake (multiple FFQs at baseline) | LF ≤ 30%TE HF > 30%TE | n overall = 215 (LF = 37, HF = 178), mean change (SD). Baseline: LF = 6.8 (1.4); HF = 6.4 (0.8); P > 0.05. MD 0.2 (95% CI ‐0.24 to 0.64). After 2 years, LF intake (≤ 30%TE) will result in a 0.2 cm/year greater increase in height on average compared to HF intake (> 30%TE). | ‐ No | No matching reported. No adjustment for prognostic variables. |
| 9.6 years regression | Height | cm | 3 | Total fat intake (multiple 24‐hour recalls at baseline, 1 and 3 years) | %TE | n overall = 632; regression results. B = ‐0.0009, P = 0.6. After 3 years, for every 1% increase in energy intake from fat, height in children will decrease by 0.0009 cm on average. | ‐ Yes | Adjusted for gender, physical activity, treatment, visit number, other sources of energy than fat, and for interactions: fat intake‐by‐treatment, fat intake‐by‐gender, fat intake‐by‐visit number and visit number‐by‐treatment. |
| 2 years; mean end values per group | Height | cm | 4 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years) | LF < 30%TE HF > 35%TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 86.1 (2.6); HF = 87.7 (3.3). At 4 years: LF (n = 14) = 114 (5.5); HF (n = 88) = 116 (4.3); P > 0.05. After 4 years, on average children with LF intake (< 30%TE) gain 27.9 cm in height, while children with HF intake (> 35%TE) gain 28.3 cm in height. | + No | No matching reported. No adjustment for prognostic variables. |
| Height at > 5to 10 years: 1 cohort study; 1 analysis (n = 126) in boys and girls aged 2 years | ||||||||
| 2 years; mean end values per group | Height | cm | 6 | Total fat intake (single 3‐day weighed dietary record at baseline, 2 and 4 years; single 4‐day weighed dietary record at 6 years) | LF < 30%TE HF > 35%TE | n overall = 126 (LF = 14, HF = 112); mean end values (SD). Baseline: LF = 86.1 (2.6); HF = 87.7 (3.3). At 6 years: LF (n = 13) = 131 (7.7); HF (n = 72) = 128 (5.2); P > 0.05. At 6 years, on average children in LF intake (< 30%TE) gain 44.9 cm in height while children in HF intake (> 35%TE) gain 40.3 cm in height. | ‐ No | No matching reported. No adjustment for prognostic variables. |
| aDirection refers to whether there was a positive (+: exposure and outcome moved in the same direction), inverse/negative (‐: exposure and outcome moved in opposite directions) or zero (0: no association) between total fat intake and the outcome. bRelative height, deviation in percentages from the mean height of healthy Finnish children of the same height and gender. %TE: percentage of total energy; FFQ: Food Frequency Questionnaire; LF: low fat; HF: high fat; MD: mean difference; NA: not applicable; NR: not reported; SD: standard deviation. | ||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Weight outcomes (standardised and unstandardised end values) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 > 6 to 12 months | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Body mass index (BMI) (kg/m2) (end values) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 > 1 to 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.4 > 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 BMI (kg/m2) (end values): sensitivity analysis (longest follow‐up data only) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 > 1 to 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 > 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 BMI (kg/m2) (end values): sensitivity analysis (shortest follow‐up data only) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 > 1 to 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Total cholesterol (mmol/L) (end values) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 > 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Low‐density lipoprotein (LDL) cholesterol (mmol/L) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 > 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 High‐density lipoprotein (HDL)‐cholesterol (mmol) (end values) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 > 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Triglycerides (mmol/L) (end values) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 > 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Systolic blood pressure (mmHg) (end values) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Diastolic blood pressure (mmHg) (end values) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Height outcomes (standardised and unstandardised end values) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 > 6 to 12 months | 2 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.3 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.4 > 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Energy intake (kJ) (end values) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 > 1 to 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Fat intake (%TE) (end values) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 13.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 > 1 to 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Saturated fat intake (%TE) (end values) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 14.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 > 1 to 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Protein intake (%TE) (end values) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 > 1 to 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.3 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Carbohydrate (%TE) (end values) Show forest plot | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 16.1 > 6 to 12 months | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 > 1 to 2 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 > 2 to 5 years | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

