18F‐PET mit Florbetaben zur frühzeitigen Diagnose von Alzheimer‐Demenz und anderen Formen der Demenz bei Personen mit leichter kognitiver Beeinträchtigung
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Study characteristics | |||
| Patient sampling | Forty‐five older adults who were referred from local memory clinics in Australia. No further details of patient sampling and recruitment were reported. Participants had to be at least 60 years old and to have had at least 7 years of formal schooling. They were also required to communicate fluently in English. Exclusion criteria included the presence of dementia, a score lower than 23 on the MMSE, the presence of other conditions that may impair their cognition and independence, including other neurological (stroke, multiple sclerosis, epilepsy, moderate‐severe traumatic brain injury), psychiatric (psychotic symptoms, bipolar disorder), or substance use conditions (e.g. drug and alcohol dependence, use of acetylcholinesterase inhibitors and memantine. | ||
| Patient characteristics and setting | 45 MCI participants diagnosed by the Petersen 2004 and Winblad 2004 criteria. Demographic data were reported for 45 MCI participants (with SUVR); demographic data were not available for those classified by visual assessment. 18F‐florbetaben positive: 24, 18F‐florbetaben negative: 21 Gender: not described Age Mean (SD): 18F‐florbetaben positive: 73.5 (6.9), 18F‐florbetaben negative:71.8 (6.1) years APOE ϵ4 carrier: not reported MMSE Mean (SD) 18F‐florbetaben positive: 26.7 (1.9), 18F‐florbetaben negative: 27.9 (1.4) Years of education Mean (SD): 18F‐florbetaben positive: 13.8 (4.2), 18F‐florbetaben negative: 13.5 (3.0) Sources of referral: not reported Setting: secondary care (memory clinic) | ||
| Index tests | Administration instructions and tracer dosis 18F‐florbetaben was injected intravenously over 38 ± 17 s, with a mean specific activity at the time of injection of 60 ± 29 GBq/μmol. Each participant received on average 286 ± 19 MBq of 18F‐florbetaben. PET imaging was conducted using a 3D GSO Phillips Allegro PET camera. A 2‐min transmission scan using a rotating 137Cs source was done for attenuation correction immediately prior to scanning. Images obtained between 90 to 110 min post injection were analysed. Images were reconstructed using a 3D RAMLA. Image interpretation PET images were processed with a semiautomatic volume of interest (VOI) method. This method used a preset template of narrow cortical VOI that was applied to either the spatially normalized 18F‐florbetaben scan or via placement on the subject’s spatially normalized coregistered MRI by a single operator who was blinded to the subject’s clinical status. Minor manual adjustments on the MRI were made to ensure that overlap with white matter and cerebrospinal fluid was minimized. Spatial normalization and coregistration of the PET and MRI images was performed using SPM8. Mean radioactivity values were obtained from VOI for cortical, subcortical, and cerebellar regions. The cerebellar cortical VOI was placed taking care to avoid cerebellar white matter. No correction for partial volume effect was applied to the PET data.
Baseline 18F‐florbetaben PET images underwent visual assessment by five independent nuclear medicine physicians blinded to clinical data. Readers had limited or no prior experience with amyloid PET visual interpretation and were trained on an electronic training tool. The image assessment was performed on axial slices, in a grey scale. The regional cortical tracer uptake (RCTU) scoring system was used to assess the beta‐amyloid deposition in the following four regions: frontal cortex, posterior cingulate/precuneus, lateral temporal cortex, and parietal cortex. A RCTU value of 1, 2, or 3 was assigned if either no, moderate, or pronounced tracer uptake was observed respectively as described below: 1 No tracer uptake: Tracer uptake (i.e. signal intensity) in grey matter in the region is lower than in white matter 2 Moderate tracer uptake: Smaller area(s) of tracer uptake equal to or higher than that present in white matter; ‐ extending beyond the white matter rim to the outer cortical margin. ‐ involving the majority of the slices within the respective region. 3 Pronounced tracer uptake: A large confluent area of tracer uptake equal to or higher than that present in white matter; ‐ extending beyond the white matter rim to the outer cortical margin. ‐ and involving the entire region including the majority of the slices within the respective region. The RCTU scores for the four brain regions were condensed into a binary brain amyloid plaque load (BAPL) score with positive or negative interpretation as described below: 18F‐florbetaben PET scan negative: scan without β‐amyloid deposition (RCTU score 1 in each of the 4 brain regions 1, 2, 3, and 4). 18F‐florbetaben PET scan positive: scan with moderate β‐amyloid deposition (RCTU score 2 in any or all of the 4 brain regions 1, 2, 3, and 4 and no score 3 in these 4 regions) or scan with pronounced β‐amyloid deposition (RCTU score 3 at least in one of the brain regions 1, 2, 3, and 4). The majority read approach established the final result.
PET images were processed with a semiautomatic volume of interest (VOI) method. This method used a preset template of narrow cortical VOI that was applied to either the spatially normalized 18F‐florbetaben scan or via placement on the subject’s spatially normalised coregistered MRI by a single operator who was blinded to the subject’s clinical status. Minor manual adjustments on the MRI were made to ensure that overlap with white matter and cerebrospinal fluid was minimized. Spatial normalization and coregistration of the PET and MRI images was performed using SPM8. Mean radioactivity values were obtained from VOI for cortical, subcortical, and cerebellar regions. The cerebellar cortical VOI were placed taking care to avoid cerebellar white matter. No correction for partial volume effect was applied to the PET data. The standardised uptake value (SUV), defined as the decay‐corrected brain radioactivity concentration normalised for injected dose and body weight, was calculated for all regions. These were then used to derive the SUV ratio (SUVR), which was referenced to cerebellar cortex. Neocortical Aβ burden was expressed as the average SUVR of the area‐weighted mean for the following cortical ROIs: frontal (consisting of dorsolateral prefrontal, ventrolateral prefrontal, and orbitofrontal regions), superior parietal, lateral temporal, lateral occipital, and anterior and posterior cingulate. The prespecified SUVR used was ≥ 1.45. | ||
| Target condition and reference standard(s) | Target condition as ADD with NINCDS‐ADRDA criteria were established with access to all study results and personal medical records | ||
| Flow and timing | Duration of follow‐up: 4 years Number included in analysis: 45 participants Visual Assessment: 25 18F‐florbetaben (+) and 20 18F‐florbetaben (‐) Progression from MCI to ADD by visual assessment: 18F‐florbetaben (+): 21 MCI to ADD and 4 MCI‐MCI; 18F‐florbetaben (‐): 0 MCI to ADD and 20 MCI‐MCI TP = 21; FP = 4; FN = 0; TN = 20 Progression from MCI to any other form of dementia (non‐ADD) by visual assessment: 18F‐florbetaben (+): 0 MCI to non‐ADD and 25 MCI‐MCI; 18F‐florbetaben (‐): 5 MCI to non‐ADD and 15 MCI‐MCI TP = 0; FP = 25; FN = 5; TN = 15 Progression from MCI to any form of dementia by visual assessment: 18F‐florbetaben (+): 21 MCI to any dementia and 4 MCI‐MCI; 18F‐florbetaben (‐): 5 MCI to any dementia and 15 MCI‐MCI TP = 21; FP = 4; FN = 5; TN = 15 SUVR: 24 18F‐florbetaben (+) and 21 18F‐florbetaben (‐) Progression from MCI to ADD by SUVR: 18F‐florbetaben (+): 21 MCI to ADD and 3 MCI‐MCI; 18F‐florbetaben (‐): 0 MCI to ADD and 21 MCI‐MCI TP = 21; FP = 3; FN= 0; TN = 21 Progression from MCI to any other form of dementia (non‐ADD) by SUVR: 18F‐florbetaben (+): 0 MCI to non‐ADD and 24 MCI‐MCI or ADD; 18F‐florbetaben (‐): 5 MCI to non‐ADD and 16 MCI‐MCI or ADD TP = 0; FP = 24; FN = 5; TN = 16 Progression from MCI to any form of dementia by SUVR: 18F‐florbetaben (+): 21 MCI to any dementia and 3 MCI‐MCI; 18F‐florbetaben (‐): 5 MCI to any dementia and 16 MCI‐MCI TP = 21; FP = 3; FN = 5; TN = 16 | ||
| Comparative | |||
| Notes | |||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Unclear | Low | ||
| DOMAIN 2: Index Test All tests | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Was the PET scan interpretation done by a trained reader physician? | Yes | ||
| Was there a clear definition of a positive result? | Yes | ||
| Low | Low | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| High | High | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Did all patients receive the same reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Was the study free of commercial funding? | No | ||
| High | |||
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| No data for constructing a 2 x 2 table was provided. The study focused on different cortical thickness subgroups and the progression to dementia in aMCI participants whom were evaluated at baseline with PiB PET or 18F‐florbetaben. We emailed the authors to resolve this issue, however, no response from the lead author was received. |
ADD: Alzheimer's disease dementia
APOE: Apolipoprotein E
BAPL: Brain amyloid plaque load
FN: False negative
FP: False positive
MCI: Mild cognitive impairment
MMSE: Mini Mental State Examination
MRI: Magnetic resonance imaging
NINCDS‐ADRDA: National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association
PET: Positron emission tomography
RCTU: Regional cortical tracer uptake
RAMLA: Row action maximum likelihood algorithm
ROI: Region of interest
SD: Standard deviation
SPM8: Statistical parametric mapping 8
SUV: Standardised uptake value
SUVR: Standardised uptake value ratio
TN: True negative
TP: True positive
VOI: Volume of interest
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Predictive value of biomarkers in patients with amnestic mild cognitive impairment |
| Target condition and reference standard(s) | Cognitive decline after two years of follow‐up, reference standard not specified |
| Index and comparator tests | 18F‐florbetaben |
| Starting date | June 2014 |
| Contact information | [email protected] |
| Notes | Dr. Vandenberghe was contacted; he provided requested information regarding the tracer used; email from Dr. Vandenberghe on 23/01/17 |
| Trial name or title | Amyloid‐PET as a diagnostic marker in daily practice |
| Target condition and reference standard(s) | Progression to dementia, reference standard not specified |
| Index and comparator tests | 18F‐florbetaben |
| Starting date | January 2015 |
| Contact information | Alzheimer Center, VU University Medical Center Alzheimer Center |
| Notes |
| Trial name or title | Amyloid load in prodromal ADD with limbic‐predominant phenotype |
| Target condition and reference standard(s) | Clinical 'indices', reference standard not specified |
| Index and comparator tests | 18F‐florbetaben |
| Starting date | March 2015 |
| Contact information | Medicina Nucleare, IRCCS Ospedale San Raffaele |
| Notes |
| Trial name or title | BAY 94‐9172 PET/CT in cognitively normal older adults, older adults with mild cognitive impairment, and older adults with Alzheimer's disease |
| Target condition and reference standard(s) | Alzheimer's disease, reference standard not specified |
| Index and comparator tests | 18F‐florbetaben |
| Starting date | 2010 |
| Contact information | Oksana Taterina, [email protected] Yaakov Stern, [email protected] |
| Notes |
| Trial name or title | Alzheimer's disease neuroimaging initiative 3 (ADNI3) protocol |
| Target condition and reference standard(s) | Rate of progression to dementia due to ADD, reference standard not specified |
| Index and comparator tests | 18F‐florberaben, 18F‐florbetapir |
| Starting date | October 2016 |
| Contact information | Dr. Paul Aisen, Director, Alzheimer's Therapeutic Research Institute, University of Southern California |
| Notes |
ADD: Alzheimer's disease dementia
ADNI3: Alzheimer's disease neuroimaging initiative 3
CT: Computed tomography
PET: Positron emission tomography
Data
Presented below are all the data for all of the tests entered into the review.
| Test | No. of studies | No. of participants |
| 1 18F‐florbetaben visual assessment and progression to ADD Show forest plot | 1 | 45 |
| Test 1  18F‐florbetaben visual assessment and progression to ADD. | ||
| 2 18F‐florbetaben SUVR and progression to ADD Show forest plot | 1 | 45 |
| Test 2  18F‐florbetaben SUVR and progression to ADD. | ||
| 3 18F‐florbetaben visual assessment and progression to any other form of non‐ADD Show forest plot | 1 | 45 |
| Test 3  18F‐florbetaben visual assessment and progression to any other form of non‐ADD. | ||
| 4 18F‐florbetaben SUVR and progression to any other form of non‐ADD Show forest plot | 1 | 45 |
| Test 4  18F‐florbetaben SUVR and progression to any other form of non‐ADD. | ||
| 5 18F‐florbetaben visual assessment and progression to any form of dementia Show forest plot | 1 | 45 |
| Test 5  18F‐florbetaben visual assessment and progression to any form of dementia. | ||
| 6 18F‐florbetaben SUVR and progression to any form of dementia Show forest plot | 1 | 45 |
| Test 6  18F‐florbetaben SUVR and progression to any form of dementia. | ||

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study

Forest plot of tests: 1 18F‐florbetaben visual assessment and progression to ADD, 2 18F‐florbetaben SUVR and progression to ADD, 3 18F‐florbetaben visual assessment and progression to any other form of non‐ADD, 4 18F‐florbetaben SUVR and progression to any other form of non‐ADD, 5 18F‐florbetaben visual assessment and progression to any form of dementia, 6 18F‐florbetaben SUVR and progression to any form of dementia.
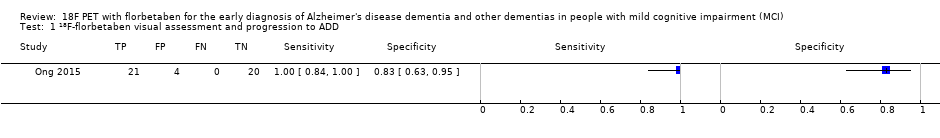
18F‐florbetaben visual assessment and progression to ADD.

18F‐florbetaben SUVR and progression to ADD.

18F‐florbetaben visual assessment and progression to any other form of non‐ADD.

18F‐florbetaben SUVR and progression to any other form of non‐ADD.

18F‐florbetaben visual assessment and progression to any form of dementia.

18F‐florbetaben SUVR and progression to any form of dementia.
| What is the diagnostic accuracy of 18F‐florbetaben PET amyloid biomarker for predict progression to ADD or any other form of dementia (non‐ADD) or any form of dementia in people with MCI? | |||||||
| Descriptive | |||||||
| Patient population | Participants diagnosed with MCI at baseline using any of the Petersen criteria or Winblad criteria or CDR = 0.5 or any 16 definitions included by Matthews (Matthews 2008) | ||||||
| Sources of referral | Memory clinic | ||||||
| MCI criteria | Petersen criteria 2004 and Winblad 2004 (Petersen 2004; Winblad 2004) | ||||||
| Sampling procedure | unclear | ||||||
| Prior testing | The only testing prior performing the 18F‐florbetaben PET amyloid biomarker was the application of diagnostic criteria for identifying participants with MCI | ||||||
| Settings | Secondary care | ||||||
| Index test | 18F‐florbetaben PET | ||||||
| Threshold prespecified at baseline | Yes | ||||||
| Threshold interpretation | Visual and quantitative | ||||||
| Threshold | Visual: if any tracer uptake was visible in any of the frontal, parietal, temporal, and posterior cingulate/precuneus cortices SUVR (Standardised Uptake Volume ratio) of ROI: > 1.45 | ||||||
| 18F‐florbetaben retention region | Visual: frontal, parietal, temporal, and posterior cingulate/precuneus cortices Global cortex (SUVR) SUVR: Global cortex | ||||||
| Reference Standard | For Alzheimer’s disease dementia: NINCDS‐ADRDA (McKhann 1984) For Lewy body dementia: McKeith criteria (McKeith 2005) For frontotemporal dementia: Lund criteria (Brun 1994) For progressive supranuclear palsy: Preliminary NINDS criteria (Hauw 1994) | ||||||
| Target condition | Progression from MCI to Alzheimer’s disease dementia or any other forms of dementia or any form of dementia. | ||||||
| Included studies | Prospectively well‐defined cohorts with any accepted definition of MCI (as above). One study (N = 45 participants) was included. Number of participants included in analysis: 45. | ||||||
| Quality concerns | Patient characteristics were poorly reported. Reference standard diagnosis was made with knowledge of the index test. Applicability concerns were high in reference standard. | ||||||
| Limitations | We were not able to calculate a summary of sensitivity and specificity due to insufficient number of studies. Investigation of heterogeneity and sensitivity analysis were not done due to insufficient number of studies. | ||||||
| Test | Studies | Cases/Participants | Sensitivity | Specificity | Consequences in a cohort of 100 | ||
| Proportion converting1 | Missed cases2 | Overdiagnosed | |||||
| Alzheimer's disease dementia | |||||||
| 18F‐florbetaben (visual assessment) | 1 | 21/45 | 100% (95% CI 84% to 100%) | 83% (95% CI 63% to 95%) | 47 | 0 | 9 |
| 18F‐florbetaben (SUVR) | 1 | 21/45 | 100% (95% CI 84% to 100%) | 88% (95% CI 68% to 97%) | 47 | 0 | 6 |
| Any other form of dementia (non‐ADD) | |||||||
| 18F‐florbetaben (visual assessment) | 1 | 5/45 | 0% (95% CI 0% to 52%) | 38% (95% CI 23% to 54%) | 11 | 11 | 55 |
| 18F‐florbetaben (SUVR) | 1 | 5/45 | 0% (95% CI 0% to 52%) | 40% (95% CI 25% to 57%) | 11 | 11 | 53 |
| Any form of dementia | |||||||
| 18F‐florbetaben (visual assessment) | 1 | 26/45 | 81% (95% CI 61% to 93%) | 79% (95% CI 54% to 94%) | 58 | 11 | 9 |
| 18F‐florbetaben (SUVR) | 1 | 26/45 | 81% (95% CI 61% to 93%) | 84% (95% CI 60% to 97%) | 58 | 11 | 7 |
| Investigation of heterogeneity and sensitivity analysis: The planned investigations of heterogeneity or sensitivity analyses were not possible due to a limited number of studies available for each analysis. | |||||||
| Conclusions:18F‐florbetaben PET scan has a good sensitivity achieved especially in predicting the progression from MCI to ADD. The quality of evidence was weak because it was based on only one study (45 participants) and there was high risk of bias due to the knowledge of the reference standard to do the diagnosis at four‐year follow‐up and due to possible conflict of interest detected. There is a need for conducting studies using standardised 18F‐florbetaben PET scan methodology in larger populations. Regarding the aforementioned we do not recommend the use in clinical practice until the DTA performance will be clearly demonstrated. | |||||||
| 1. Proportion converting to ADD or any other form of dementia (non‐ADD) or any form of dementia in the included study 2. Missed and overdiagnosed numbers were computed using the proportion converting to the target condition. ADD: Alzheimer's disease dementia NINDS: National Institute of Neurological Disorders and Stroke | |||||||
| Test | No. of studies | No. of participants |
| 1 18F‐florbetaben visual assessment and progression to ADD Show forest plot | 1 | 45 |
| 2 18F‐florbetaben SUVR and progression to ADD Show forest plot | 1 | 45 |
| 3 18F‐florbetaben visual assessment and progression to any other form of non‐ADD Show forest plot | 1 | 45 |
| 4 18F‐florbetaben SUVR and progression to any other form of non‐ADD Show forest plot | 1 | 45 |
| 5 18F‐florbetaben visual assessment and progression to any form of dementia Show forest plot | 1 | 45 |
| 6 18F‐florbetaben SUVR and progression to any form of dementia Show forest plot | 1 | 45 |


