غربالگری هیستروسکوپی در زنان نابارور و زنان تحت کمک‐باروری
چکیده
پیشینه
غربالگری هیستروسکوپی (hysteroscopy) در زنان با ناباروری غیرقابل توجیه یا پیش از تلقیح داخل رحمی (intrauterine insemination; IUI) یا لقاح آزمایشگاهی (in vitro fertilization; IVF) ممکن است پاتولوژیهای داخل رحمی را نشان دهد که به وسیله اولتراسوند ترانسواژینال روتین شناسایی نشده باشد. هیستروسکوپی، چه فقط تشخیصی و چه جراحی (operative)، ممکن است پیامدهای تولید مثل را بهبود بخشد.
اهداف
ارزیابی اثربخشی و ایمنی غربالگری هیستروسکوپی در زنان ناباروری که تحت ارزیابی برای ناباروری قرار دارند و در زنان ناباروری که تحت IUI یا IVF هستند.
روشهای جستوجو
پایگاه ثبت تخصصی گروه زنان و باروری در کاکرین؛ CENTRAL CRSO؛ MEDLINE؛ Embase؛ ClinicalTrials.gov؛ پلتفرم بینالمللی پایگاه ثبت کارآزماییهای بالینی سازمان جهانی بهداشت (سپتامبر 2018) جستوجو کردیم. فهرست منابع مقالات مرتبط را جستوجو کردیم و مجموعه مقالات کنفرانسهای مرتبط را به صورت دستی جستوجو کردیم.
معیارهای انتخاب
کارآزماییهای تصادفیسازی و کنترل شدهای که غربالگری هیستروسکوپی را با عدم مداخله در زنان ناباروری که مایل به بارداری خودبهخودی بودند، یا پیش از انجام IUI یا IVF، مقایسه کرده بودند.
گردآوری و تجزیهوتحلیل دادهها
ما بهطور مستقل از هم مطالعات را غربال کردیم، دادهها را استخراج و خطر سوگیری (bias) را ارزیابی کردیم. پیامدهای اولیه ما نرخ تولد زنده و عوارض پس از هیستروسکوپی بود. دادهها را با استفاده از خطر نسبی (RR) و مدل اثر‐ثابت (fixed‐effect) تجزیهوتحلیل کردیم. کیفیت شواهد را با استفاده از سیستم درجهبندی توصیه، ارزیابی، توسعه و ارزشیابی (GRADE) بررسی کردیم.
نتایج اصلی
ما 11 مطالعه را بازیابی کردیم. فقط یک کارآزمایی را در این مرور گنجاندیم که غربالگری هیستروسکوپی را در برابر عدم انجام آن در زنان مبتلا به قدرت پائین باروری غیرقابل توجیه که در صدد بودند بارداری خودبهخودی داشته باشند، مقایسه کرده بود. ما مطمئن نیستیم که نرخ بارداری در حال وقوع به دنبال غربالگری هیستروسکوپی در زنان با قدرت پائین باروری غیرقابل توجیه به مدت حداقل دو سال بهبود مییابد یا خیر (RR: 4.30؛ 95% CI؛ 29.2 تا 07.8؛ 1 RCT؛ شرکتکنندگان = 200؛ شواهد با کیفیت بسیار پائین). انتظار میرود انجام غربالگری هیستروسکوپی برای کلینیک عادی با نرخ بارداری در حال وقوع 10% بدون هیستروسکوپی، منجر به نرخ بارداری در حال وقوع بین 23% و 81% شود. مطالعه وارد شده هیچ حادثه جانبی را در بازوهای درمانی گزارش نکرد. ما مطمئن نیستیم که پس از غربالگری هیستروسکوپی در زنان با حداقل دو سال قدرت پائین باروری غیرقابل توجیه، نرخ بارداری بالینی بهبود مییابد (RR: 3.80؛ 95% CI؛ 2.31 تا 6.24؛ 1 RCT؛ شرکتکنندگان = 200؛ شواهد با کیفیت بسیار پائین) یا نرخ سقط جنین (RR: 2.80؛ 95% CI؛ 1.05 تا 7.48؛ 1 RCT؛ شرکتکنندگان = 200؛ شواهد با کیفیت بسیار پائین) افزایش مییابد یا خیر.
ده کارآزمایی را شامل 1836 زن تحت غربالگری هیستروسکوپی و 1914 زن را که پیش از IVF تحت هیستروسکوپی قرار نگرفته بودند، وارد کردیم. محدودیتهای اصلی در کیفیت شواهد، گزارشدهی ناکافی شیوههای مطالعه و ناهمگونی آماری بالا بودند. خطر سوگیری (bias) برای پنهانسازی تخصیص در هشت مورد از ده کارآزمایی، نامشخص بود.
ممکن است انجام غربالگری هیستروسکوپی پیش از IVF، نرخ تولد زنده را افزایش دهد (RR: 1.26؛ 95% CI؛ 1.11 تا 1.43؛ 6 RCT؛ شرکتکنندگان = 2745؛ I² = 69%؛ شواهد با کیفیت پائین). انتظار میرود انجام غربالگری هیستروسکوپی برای کلینیک عادی با نرخ تولد زنده معادل 22%، منجر به نرخ تولد زنده 25% و 32% شود. با این حال، تجزیهوتحلیل حساسیت از طریق تجمیع نتایج حاصل از کارآزماییهایی با خطر پائین سوگیری، بیانگر عدم افزایش نرخ تولد زنده به دنبال غربالگری هیستروسکوپی بود (RR: 0.99؛ 95% CI؛ 0.82 تا 1.18؛ 2 RCT؛ شرکتکنندگان = 1452؛ I² = 0%).
فقط چهار کارآزمایی عوارض پس از هیستروسکوپی را گزارش کرده بودند؛ از این تعداد، سه کارآزمایی هیچ رخدادی را در هیچ یک از گروهها رکورد نکرده بودند. ما مطمئن نیستیم که غربالگری هیستروسکوپی با حوادث جانبی بیشتری مرتبط است یا خیر (نسبت شانس (OR) پتو: 7.47؛ 95% CI؛ 0.15 تا 376.42؛ 4 RCT؛ شرکتکنندگان = 1872؛ I² = قابل اجرا نیست؛ شواهد با کیفیت بسیار پائین).
امکان دارد انجام غربالگری هیستروسکوپی پیش از IVF، نرخ بارداری بالینی را افزایش دهد (RR: 1.32؛ 95% CI؛ 1.20 تا 1.45؛ 10 RCT؛ شرکتکنندگان = 3750؛ I² = 49%؛ شواهد با کیفیت پائین). انتظار میرود انجام غربالگری هیستروسکوپی برای بالین معمول با نرخ بارداری بالینی 28%، سبب نرخ بارداری بالینی بین 33% و 40% شود.
ممکن است تفاوتی اندک یا عدم تفاوت در نرخ سقط جنین پس از غربالگری هیستروسکوپی وجود داشته باشد (RR: 1.01؛ 95% CI؛ 0.67 تا 1.50؛ 3 RCT؛ شرکتکنندگان = 1669؛ I² = 0%؛ شواهد با کیفیت پائین).
ما هیچ کارآزمایی را نیافتیم که غربالگری هیستروسکوپی را در برابر عدم هیستروسکوپی پیش از IUI مقایسه کرده باشد.
نتیجهگیریهای نویسندگان
در حال حاضر شواهدی با کیفیت بالا برای تایید استفاده معمول از هیستروسکوپی به عنوان ابزار غربالگری در جمعیت عمومی زنان نابارور با اولتراسوند یا عکس رنگی رحم (هیستروسالپینگوگرام (hysterosalpingogram)) طبیعی در بررسی پایه باروری برای بهبود نرخ موفقیت باروری وجود ندارد.
شواهدی با کیفیت پائین در زنان تحت IVF، شامل تمام مطالعات گزارش دهنده این پیامدها، نشان میدهد که اجرای غربالگری هیستروسکوپی پیش از IVF میتواند نرخ تولد زنده و بارداری بالینی را افزایش دهد. با این حال، نتایج تجمعی از فقط دو کارآزمایی با خطر پائین سوگیری، نشان دهنده مزیت غربالگری هیستروسکوپی پیش از IVF نبود.
از آنجایی که مطالعات نشان دهنده تاثیر، مواردی هستند که پنهانسازی تخصیص نامشخصی دارند، ما مطمئن نیستیم که غربالگری روتین هیستروسکوپی، تولد زنده و بارداری بالینی را برای همه زنان, یا افراد دارای دو یا تعداد بیشتری تلاش IVF ناموفق، افزایش میدهد یا خیر. دادههای کافی برای نتیجهگیری در مورد ایمنی غربالگری هیستروسکوپی وجود ندارد.
PICOs
خلاصه به زبان ساده
غربالگری هیستروسکوپی (hysteroscopy) در زنان نابارور که در تلاش برای باروری خودبهخودی هستند، و پیش از لقاح آزمایشگاهی.
سوال مطالعه مروری
ارزیابی ایمنی و سودمندی انجام غربالگری هیستروسکوپی بر پیامدهای تولید مثلی در زنانی که برای باروری خودبهخودی تلاش میکنند و کسانی که تحت لقاح آزمایشگاهی (in vitro fertilisation; IVF) قرار میگیرند.
پیشینه
پیشنهاد شده که در زنان دچار مشکل ناشناخته در باردار شدن یا افرادی که به دنبال درمان پیشرفته باروری مانند تلقیح داخل رحمی یا IVF هستند، انجام هیستروسکوپی (دیدن درون رحم با استفاده از یک تلسکوپ) ممکن است به بهبود موفقیت کمک کند. شاید اولتراسوند روتین انجام شده طی بررسی کامل، ناهنجاریهای کوچک درون رحمی را که امکان دارد با انجام هیستروسکوپی به طور همزمان تشخیص داده و درمان شوند، از قلم بیندازد. همچنین ممکن است موفقیت را به وسیله تسهیل تلقیح بعدی یا انتقال جنین از طریق عریض کردن مسیر به رحم (اتساع دهانه رحم) یا به دلیل تاثیر خراشاننده بر آندومتر (لایه پوششی رحم) که میتواند به پیشرفت لانهگزینی جنین (چسبندگی به لایه پوششی رحم) کمک کند، افزایش دهد.
ویژگیهای مطالعه
برای زنانی که تمایل به بارداری خودبهخودی داشتند، یک کارآزمایی (200 زن) را یافتیم. برای زنان تحت IVF، ده کارآزمایی (3750 زن) را وارد کردیم. همه کارآزماییها تاثیرات غربالگری هیستروسکوپی را در مقایسه با عدم هیستروسکوپی ارزیابی کرده بودند. شواهد تا سپتامبر 2018 بهروز است.
نتایج کلیدی
هیستروسکوپی در زنانی که تمایل به بارداری خودبهخودی داشتند، مرتبط با شانس بیشتر بارداری در حال وقوع و بارداری بالینی در یک مطالعه با خطر سوگیری (bias) بالا بود. این کارآزمایی هیچ حادثه جانبی را پس از هیستروسکوپی گزارش نکرده بود. نرخ سقط جنین پس از هیستروسکوپی بیشتر بود.
در زنان تحت IVF، مطالعات وارد شده پیشنهاد کردند که انجام غربالگری هیستروسکوپی در ابتدا، شانس تولد زنده یا بارداری بالینی را افزایش میدهد. با این حال، حوادث جانبی پس از هیستروسکوپی بهطورضعیفی گزارش شده بود و در نتیجه، ما قادر به ارزیابی ایمنی این مداخله نبودیم. انتظار میرود برای زنان در بالین معمول با نرخ تولد زنده 22%، انجام غربالگری هیستروسکوپی سبب نرخ تولد زنده بین 25% و 32% شود. خطر سقط جنین پس از هیستروسکوپی افزایش نیافته بود.
هیچ کارآزمایی را با زنانی که به دنبال تلقیح داخل رحمی بودند، نیافتیم.
کیفیت شواهد
شواهدی با کیفیت بسیار پائین از یک مطالعه در زنانی که تمایل به باردار شدن خودبهخودی داشتند، وجود داشت.
شواهدی با کیفیت پائین موجود بود که نشان میداد غربالگری هیستروسکوپی که پیش از IVF انجام گیرد، ممکن است احتمال تولد زنده یا بارداری بالینی را افزایش دهد و شواهدی با کیفیت بسیار پائین درباره حوادث جانبی پس از هیستروسکوپی وجود داشت. کیفیت شواهد، به علت خطر سوگیری و ناهمگونی آماری، کاهش پیدا کرده بود.
Authors' conclusions
Summary of findings
| Hysteroscopy compared with no hysteroscopy in women wishing to conceive spontaneously | ||||||
| Patient or population: women with unexplained subfertility wishing to conceive spontaneously Settings: Arafa Hospital, Fayoum, Egypt Intervention: screening hysteroscopy Comparison: no hysteroscopy | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Risk with no hysteroscopy | Risk with hysteroscopy | |||||
| Live birth | 100 per 1000 | 430 per 1000 (229 to 807) | RR 4.30 (2.29 to 8.07) | 200 (1 RCT) | ⊕⊕⊝⊝ | |
| Adverse events | 0 per 1000 | 0 per 1000 (0 to 0) | not estimable | (1 RCT) | ⊕⊝⊝⊝ | |
| Clinical pregnancy | 150 per 1000 | 570 per 1000 (347 to 936) | RR 3.80 (2.31 to 6.24) | 200 (1 RCT) | ⊕⊕⊝⊝ | |
| Miscarriage | 50 per 1000 | 140 per 1000 (52 to 374) | RR 2.80 (1.05 to 7.48) | 200 (1 RCT) | ⊕⊝⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aVery serious risk of bias, downgraded by two levels: unclear random sequence generation and allocation concealment ‐ high risk of selective outcome reporting | ||||||
| Screening hysteroscopy versus no hysteroscopy in women before IVF | ||||||
| Patient or population: women before IVF treatment | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with no hysteroscopy | Risk with hysteroscopy | |||||
| Live birth | 221 per 1000 | 279 per 1000 | RR 1.26 | 2745 | ⊕⊕⊝⊝ | |
| Adverse events | 0 per 1000 | 0 per 1000 | Peto OR 7.47 | 1872 | ⊕⊕⊝⊝ | |
| Clinical pregnancy | 278 per 1000 | 368 per 1000 | RR 1.32 | 3750 | ⊕⊕⊝⊝ | |
| Miscarriage | 53 per 1000 | 53 per 1000 | RR 1.01 | 1669 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aSerious risk of bias, downgraded by one level: only two studies had low risk of bias for all the domains. The rest of the studies had unclear risk for allocation concealment. One study was categorised at high risk for 'other' domain. There is a likely chance of overestimating the treatment. | ||||||
Background
Description of the condition
According to the International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization's (WHO) revised glossary of assisted reproductive technology, subfertility is “a disease of the reproductive system, defined by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse, or due to an impairment of a person's capacity, either as an individual, or with his or her partner” (Zegers‐Hochschild 2017). It is estimated that 72.4 million women are subfertile, and that 40.5 million of these are currently seeking fertility treatment (Boivin 2007). A basic subfertility evaluation comprises tests for ovulation, tubal patency, and a transvaginal ultrasound to rule out uterine or ovarian pathology for the female partner, and semen analysis for the male partner (ASRM 2016). The evaluation of the uterine cavity could be considered an important step in the investigation of all subfertile women, as the uterine cavity and its inner layer, the endometrium, are assumed to be important for implantation of the human embryo.
In women undergoing in vitro fertilisation (IVF), despite numerous technological advances, live‐birth rates are between 21% and 25% (Mansour 2014; EIM/ESHRE 2016). Even after transferring euploid embryos following pre‐implantation genetic screening, pregnancy rate is only around 64% (Fiorentino 2014). Embryo implantation remains one of the crucial steps that determines the success of an IVF cycle. The successful implantation is dependent on embryo‐uterine 'cross talk', which is mediated through various factors, such as cytokines, growth factors, and adhesion molecules (Singh 2011; Zhang 2013). Uterine factors, such as polyps and adhesions, may negatively impact the outcomes of IVF (Taylor 2008).
Description of the intervention
Hysteroscopy can both evaluate the uterine cavity for pathology, and either during the same procedure or in a further procedure, treat polyps, adhesions, septa, and fibroids. Screening hysteroscopy is carried out in asymptomatic women, with no detectable uterine cavity abnormalities on pelvic imaging. Hysteroscopy is a commonly performed gynaecological procedure with low complication rates (0.1% to 0.95% (Jansen 2000)). It can be carried out in an outpatient setting without general or regional anaesthesia. Various methods of pain relief are used, such as local, oral, or intravenous analgesia, either alone or in combination (Ahmad 2017). It is considered the gold standard for the diagnosis of uterine cavity pathology (Taylor 2008;Bosteels 2015).
Hysteroscopy allows the direct visualisation of the uterine cavity through a rigid, semi‐rigid, or flexible endoscope. During hysteroscopy, the instrument is passed through the cervix into the uterine cavity. For optimal visualisation, a distension medium, commonly saline, is used to expand the uterine cavity. The hysteroscope consists of a rigid telescope with a proximal eyepiece, and a distal objective lens that can be angled at 0° to allow direct viewing, or offset at various angles to provide a forward‐oblique view. The total working diameters of modern diagnostic hysteroscopes are typically 2.5 to 4.0 mm. Operative hysteroscopy requires adequate visualisation through a continuous fluid circulation using an in‐ and outflow channel. The outer diameters of modern operative hysteroscopes have been reduced to a diameter of between 4.0 and 5.5 mm. The sheath system contains one or two 1.6 to 2.0 mm working channels for the insertion of small biopsy forceps, scissors, retraction loops and morcellators, or unipolar or bipolar electro diathermy instruments.
In clinical practice, evaluation of the uterine cavity is usually done with a transvaginal ultrasound scan (TVS) prior to IVF. Due to the perceived advantages of hysteroscopy over TVS, such as the potential for simultaneous detection and treatment of intrauterine pathologies, use of a pre‐IVF screening hysteroscopy has gained widespread acceptance (Campo 2014).
How the intervention might work
It is assumed that uterine cavity abnormalities may interfere with factors that regulate the embryo‐endometrium interplay, for example, hormones and cytokines, reducing the possibility of pregnancy. Many hypotheses have been formulated in the literature as to how endometrial polyps, submucous fibroids, intrauterine adhesions, and uterine septa may impair implantation of the human embryo; nevertheless, the precise mechanisms of the action through which each one of these cavity abnormalities affects this essential reproductive process are poorly understood.
Screening hysteroscopy in woman prior to IVF may reveal intrauterine pathology that may not be detected by routine TVS. The reported rate of intrauterine pathology is 12% in women undergoing first IVF (Smit 2016), and 27% in women with recurrent implantation failure (RIF) (El‐Toukhy 2016). Hysteroscopy allows detection and treatment of many of these intrauterine pathologies, which may improve IVF outcomes (Oliveira 2003). Cervical dilation during pre‐IVF hysteroscopy may facilitate subsequent embryo transfers, which could possibly improve outcomes. Another proposed mechanism to help improve IVF outcomes following hysteroscopy is local endometrial injury caused during the invasive procedure. The inflammatory reaction following endometrial injury leads to a release of cytokines and growth factors, which may help implantation and improve clinical pregnancy rates following IVF (Barash 2003; Nastri 2015).
Why it is important to do this review
Although detection of intrauterine pathologies in women with normal TVS prior to IVF is perceived as one of the benefits of performing hysteroscopy, we wish to evaluate whether treating these pathologies improves outcomes following IVF (Oliveira 2003; Pundir 2014; Smit 2016). Current guidelines do not advocate the routine use of screening hysteroscopy during the initial infertility work‐up (Crosignani 2000; NICE 2013). Due to uncertainty about the role of screening hysteroscopy in women with normal TVS during infertility work‐up, and prior to IVF, it is important to conduct a systematic appraisal of the current evidence.
Objectives
To assess the effectiveness and safety of screening hysteroscopy in subfertile women undergoing evaluation for infertility and subfertile women undergoing intrauterine insemination (IUI) or in vitro fertilisation (IVF).
Methods
Criteria for considering studies for this review
Types of studies
Published and unpublished randomised controlled trials (RCT) were eligible for inclusion. We excluded non‐randomised studies and quasi‐randomised trials.
Types of participants
-
Subfertile women, with otherwise unexplained infertility, in whom routine imaging did not show uterine cavity abnormalities, who wished to conceive spontaneously
-
Subfertile women, in whom routine imaging did not show uterine cavity abnormalities, and before treatment with IUI.
-
Women in whom routine imaging did not show uterine cavity abnormalities, and before treatment with IVF.
We excluded subfertile women with suspected uterine cavity abnormalities (present on any imaging techniques), as this topic is covered by another Cochrane review (Bosteels 2015).
Types of interventions
We included the following three randomised comparisons:
-
A routine screening hysteroscopy, with or without treatment of any detected uterine cavity abnormalities, versus no hysteroscopy, in subfertile women wishing to conceive spontaneously.
-
A routine screening hysteroscopy, with or without treatment of any detected uterine cavity abnormalities, versus no hysteroscopy, before intrauterine insemination (IUI).
-
A routine screening hysteroscopy, with or without treatment of any detected uterine cavity abnormalities, versus no hysteroscopy, before in vitro fertilisation (IVF).
Types of outcome measures
Primary outcomes
-
Live birth or (in studies that do not report live birth) ongoing pregnancy. The live‐birth delivery rate (whether or not after assisted reproduction) was defined as delivery of a live foetus after 20 completed weeks of gestational age. We counted the delivery of singleton, twin, or multiple pregnancies as one live birth. The ongoing pregnancy rate (whether or not after assisted reproduction) was defined as evidence of a gestational sac with foetal heart motion at 12 weeks, confirmed by ultrasound. We counted multiple gestational sacs as one ongoing pregnancy. We used ongoing pregnancy as a surrogate outcome for live birth.
-
Adverse events: the incidence of complications due to the hysteroscopy procedure, analysed as a composite measure of any adverse events (including perforation, infection, vasovagal attacks).
Secondary outcomes
-
Clinical pregnancy rate (whether or not after assisted reproduction), defined as ultrasound evidence of a gestational sac.
-
Miscarriage rate (whether or not after assisted reproduction), defined as the spontaneous loss of a clinical pregnancy that occurred before 20 completed weeks of gestation (18 weeks post‐fertilisation) or, if gestational age was unknown, the loss of an embryo or foetus of less than 400 grams.
We did not exclude studies on the basis of their reported outcome measures. We reported any lack of data for key outcomes in the final results and discussion.
Search methods for identification of studies
We searched for all published and unpublished RCTs of routine hysteroscopy in infertile women, without language restriction, and in consultation with the Cochrane Gynaecology and Fertility Group (CGF) Information Specialist.
Electronic searches
We searched the following electronic databases, trial registers, and web sites from inception to 05 September 2018:
-
Cochrane CGF Specialised Register, ProCite platform, searched 05 September 2018 (Appendix 1);
-
Cochrane Central Register of Studies (CENTRAL CRSO), Web platform, searched 05 September 2018 (Appendix 2);
-
MEDLINE, Ovid platform, searched from 1946 to 05 September 2018 (Appendix 3);
-
Embase, Ovid platform, searched from 1980 to 05 September 2018(Appendix 4);
-
PsycINFO, Ovid platform, searched from 1806 to 05 September 2018 (Appendix 5);
-
CINAHL (Cumulative Index to Nursing and Allied Health Literature), EBSCO platform, searched from 1961 to 05 September 2018 (Appendix 6);
-
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov);
-
World Health Organization International Trials Registry Platform (www.who.int/trialsearch/Default.aspx);
-
DARE (Database of Abstracts of Reviews of Effects) on the Cochrane Library for reference lists from relevant non‐Cochrane reviews (onlinelibrary.wiley.com/o/cochrane/cochrane_cldare_articles_fs.html);
-
Web of Knowledge (another source of trials and conference abstracts (wokinfo.com/));
-
OpenGrey for unpublished literature from Europe (www.opengrey.eu/);
-
LILACS (Latin American and Caribbean Health Science Information database) (regional.bvsalud.org/php/index.php?lang=en);
-
PubMed and Google for recent trials not yet indexed in MEDLINE.
We combined the MEDLINE search with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials, which appears in Section 6.4.11 of the Cochrane Handbook for Systematic Reviews of Interventions (Lefebre 2011).
We combined the Embase, PsycINFO, and CINAHL searches with trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN (www.sign.ac.uk/search‐filters.html)).
Searching other resources
Four review authors (JB, SS for non‐IVF comparisons; MSK, SKS for IVF comparison) handsearched reference lists of articles retrieved by the search, and contacted experts in the field to obtain additional data. We also handsearched relevant journals and conference abstracts that were not covered in the GFG register, in liaison with the Information Specialist.
Data collection and analysis
Selection of studies
Two review authors (MSK, SKS) conducted an initial screen of titles and abstracts identified by the search, after which we retrieved the full texts of all potentially eligible studies. Four review authors (SS, JB, SKS, MSK) independently examined these full‐text articles for compliance with the inclusion criteria, and selected studies eligible for inclusion in the review. We corresponded with study investigators as required to clarify study eligibility. Disagreements as to study eligibility were resolved by discussion or by a fifth review author (BWJM). We documented the selection process with a PRISMA flow chart.
Data extraction and management
Four review authors (JB, MSK, SKS, SS) independently extracted data from eligible studies using a data extraction form designed and pilot‐tested by the review authors. Any disagreement was resolved by discussion or by a fifth review author (BWJM). We extracted data that included study characteristics and outcome data (Appendix 7). We corresponded with study investigators for further data on methods or results, or both, as required. We included studies irrespective of whether outcomes were reported in a 'usable' way.
Assessment of risk of bias in included studies
Four review authors (JB, SS for non‐IVF comparisons; MSK, SKS for IVF comparison) independently assessed the included studies for risk of bias using the Cochrane 'Risk of bias' assessment tool (Higgins 2011). We assessed the following items: selection (random sequence generation and allocation concealment); performance (blinding of participants and personnel); detection (blinding of outcome assessors); attrition (incomplete outcome data); reporting (selective reporting); and other bias. Disagreements were resolved by discussion or by a fifth review author. We described all judgements fully, and presented the conclusions in the 'Risk of bias' table, which were incorporated into the interpretation of review findings by means of sensitivity analyses (see Sensitivity analysis). Selective reporting is a type of reporting bias that affects the internal validity of an individual study. It refers to the selective reporting of some outcomes (e.g. positive outcomes) and the failure to report others (e.g. adverse events). We took care to search for within‐trial selective reporting, such as trials failing to report obvious outcomes, or reporting them in insufficient detail to allow inclusion. We compared the outcomes between the published protocol and the final published study. Where identified studies failed to report the primary outcome of live birth, but did report interim outcomes, such as clinical pregnancy, we undertook informal assessment as to whether the interim values (e.g. pregnancy rates) were similar to those reported in studies that also reported live birth.
Measures of treatment effect
For dichotomous data (e.g. live‐birth rates), we used the number of events in the control and intervention groups of each study to calculate risk ratios (RR). We used Peto odds ratio (OR) for outcomes with low event rates. We reversed the direction of effect of individual studies, if required, to ensure consistency across trials. We presented 95% confidence intervals (CI) for all outcomes. We compared the magnitude and direction of effect reported by studies with how they were presented in the current review, taking account of legitimate differences.
Unit of analysis issues
The primary analysis was per woman randomised; we included per pregnancy data for some outcomes (for the outcome miscarriage). We counted multiple live births (e.g. twins or triplets) as one live‐birth event.
Dealing with missing data
We analysed the data on an intention‐to‐treat basis to the greatest degree possible, and attempted to obtain missing data from the original authors. We assumed live births or clinical pregnancies would not be present in women without a reported outcome. For other outcomes, we analysed only the available data.
For Imputated data, we had planned to conduct sensitivity analysis (see Sensitivity analysis).
Assessment of heterogeneity
We considered whether the clinical and methodological characteristics of the included studies were sufficiently similar for meta‐analysis to provide a clinically meaningful summary. We assessed statistical heterogeneity using the I² statistic. An I² measurement greater than 50% indicated substantial heterogeneity (Higgins 2011).
Assessment of reporting biases
In view of the difficulty of detecting and correcting for publication bias and other reporting biases, the review authors aimed to minimise the potential impact of these biases by ensuring a comprehensive search for eligible studies, and by being alert for duplication of data. Since there were fewer than 10 studies in each population, we did not use a funnel plot.
Data synthesis
Four review authors (JB, SS for non‐IVF comparisons; MSK, SKS for IVF comparison) entered the data and performed the statistical analysis using Review Manager 5 (RevMan 2014). We combined the data using a fixed‐effect model for the following comparisons.
-
Hysteroscopy versus no hysteroscopy for subfertile women wishing to conceive spontaneously
-
Hysteroscopy versus no hysteroscopy for subfertile women undergoing IUI
-
Hysteroscopy versus no hysteroscopy for women undergoing IVF
We displayed an increase in the odds of a particular outcome, which may be beneficial (e.g. live birth) or detrimental (e.g. adverse effects of the hysteroscopy) graphically in the meta‐analyses to the right of the centre‐line, and a decrease in the odds of an outcome to the left of the centre‐line.
Subgroup analysis and investigation of heterogeneity
We conducted the following subgroup analysis:
For women undergoing IVF:
-
First IVF versus two or more IVF failures.
Sensitivity analysis
We conducted sensitivity analyses for the primary outcome live birth and an important secondary outcome (clinical pregnancy rate) to determine whether the conclusions were robust to arbitrary decisions made regarding eligibility and analysis. These analyses included consideration of whether the review conclusions would have differed if:
-
eligibility had been restricted to studies without high or unclear risk of bias in any domain;
-
a random‐effects model had been adopted;
-
alternative imputation strategies had been implemented;
-
the summary effect measure had been odds ratio rather than risk ratio;
-
the primary outcome had been limited to live birth.
Overall quality of the body of evidence: 'Summary of findings' table
We prepared a 'Summary of findings' table using GRADEpro GDT and Cochrane methods (GRADEpro GDT; Higgins 2011). This table evaluated the overall quality of the body of evidence for all review outcomes (live birth, adverse events, clinical pregnancy, and miscarriage), for the following comparisons: a screening hysteroscopy versus no hysteroscopy in subfertile women wishing to conceive spontaneously; and a screening hysteroscopy versus no hysteroscopy in women before IVF. We assessed the quality of the evidence using GRADE criteria (risk of bias, consistency of effect, imprecision, indirectness, and publication bias). Two review authors independently made judgements about evidence quality (high, moderate, low, or very low), with any disagreements resolved by discussion. They justified, documented, and incorporated the judgments into report of results for each outcome.
We extracted study data, formatted our comparisons in data tables, and prepared a 'Summary of findings' table before writing the results and conclusions of our review.
Results
Description of studies
Results of the search
We ran our electronic search on 05 September 2018. The targeted search resulted in 761 records, out of which 227 were duplicate records. Two teams of review authors (JB and SS; MSK and SKS) screened the records simultaneously and independently, and examined the titles and abstracts to identify potentially eligible studies among the remaining 534 records.
After independent assessment, two authors (JB, SS) found five potentially eligible studies for the randomised comparisons in subfertile women wishing to conceive spontaneously, or before intrauterine insemination (IUI); we only included one trial (Seyam 2015). One study is awaiting classification (Moramezi 2012). We excluded three trials for not addressing the research question of interest (Brown 2000; El‐Khayat 2015; Shokeir 2016). See the 'Characteristics of excluded studies' tables.
Two authors (MSK, SKS) independently assessed studies that evaluated screening hysteroscopy before in vitro fertilisation (IVF), and found 24 records of potentially eligible studies. We excluded seven trials (Fatemi 2010; Wang 2011; Kasius 2013; Kamel 2015; Zhang 2015; Hebeisha 2018; Siristatidis 2017), and included ten trials in the review (Demirol 2004; Rama Raju 2006; El‐Nashar 2011; Aghahosseini 2012; Shawki 2012; Elsetohy 2015; El‐Toukhy 2016; Smit 2016; Alleyassin 2017; Juul Hare 2018). For two included trials, there were two published protocols and one conference abstract (Smit 2016; El‐Toukhy 2016). We identified four ongoing trials (NCT02245750; NCT03173404; PACTR201402000691997; UMIN000025679). See the 'Characteristics of ongoing studies' tables.
When combining all the populations evaluated under this review, we found 26 potentially eligible studies, out of which we included 11 trials for quantitative synthesis. The search results are summarized in the PRISMA flow chart (Figure 1).

Study flow diagram
Included studies
See 'Characteristics of included studies' tables.
Design
We included a total of 11 randomised controlled trials (RCT) in the review. Out of these 11 included trials, eight were completed and published as full articles (Demirol 2004; Rama Raju 2006; Shawki 2012; Elsetohy 2015; Seyam 2015; El‐Toukhy 2016; Smit 2016; Alleyassin 2017), and three were conference abstracts (El‐Nashar 2011; Aghahosseini 2012; Juul Hare 2018). Three were multicentre trials, conducted in the Netherlands (Smit 2016), European centres (El‐Toukhy 2016), and Denmark (Juul Hare 2018). The remaining eight trials were single centre trials. Two were conducted in Iran (Aghahosseini 2012; Alleyassin 2017), four in Egypt (El‐Nashar 2011; Shawki 2012; Elsetohy 2015; Seyam 2015), one in India (Rama Raju 2006), and one in Turkey (Demirol 2004).
One of the studies was partly funded by the European Society of Human Reproduction and Embryology, the European Society for Gynaecological Endoscopy (ESGE), and the Karl Storz Company provided the hysteroscopy equipment for all centres (El‐Toukhy 2016). The Dutch Organisation for Health Research and Development (ZonMW) funded the other multicentre trial (Smit 2016). The rest of the trials did not acknowledge any funding support.
Participants
Seyam 2015 enrolled 200 women with unexplained subfertility who attended a single centre in Egypt. The basic work‐up included a hysterosalpingogram (HSG) and a transvaginal ultrasound to screen for uterine pathology and tubal patency. The authors of this RCT did not report whether or not a prior hysteroscopy or a concomitant endometrial biopsy were done. We could not obtain further clarification.
The characteristics of the participants among the IVF population are shown in Table 1. Three trials included subfertile women undergoing their first IVF (Elsetohy 2015; Smit 2016; Alleyassin 2017). Four trials included women with two or more IVF failures (Demirol 2004; Rama Raju 2006; Aghahosseini 2012; El‐Toukhy 2016). Two trials included an unselected IVF population (El‐Nashar 2011; Shawki 2012). One trial included women with one IVF failure who were undergoing their second IVF treatment (Juul Hare 2018). In six trials, participants had an additional radiological procedure, in the form of a HSG, as an inclusion criteria (Demirol 2004; Rama Raju 2006; Aghahosseini 2012; Shawki 2012; Elsetohy 2015; Alleyassin 2017). Two trials excluded participants with a history of previous hysteroscopy (Smit 2016; Alleyassin 2017); and one trial included women with a previous history of hysteroscopy in both the intervention and control arms (El‐Toukhy 2016).
| Study ID | Population | Previous HSG or hysteroscopy | Intervention | Additional endometrial biopsy | Detected abnormalities treated | Timing of hysteroscopy |
| Unexplained infertility of 2 years duration | Normal HSG | Hysteroscopy | No | Yes | Follicular phase | |
| Two or more IVF failures | Normal HSG; no hysteroscopy in previous 2 months | Hysteroscopy | No | No details | No details available | |
| First IVF | Normal HSG; women with history of hysteroscopy excluded. | Hysteroscopy | No | Yes | Preceding cycle; luteal phase | |
| Two or more IVF failures | Normal HSG; no details of history of hysteroscopy | Hysteroscopy | No | Yes | Preceding cycle; follicular phase | |
| Unselected IVF population | No details of HSG; no details of history of hysteroscopy | Hysteroscopy | Yes | Yes | No details | |
| First IVF | Normal HSG; no details of history of hysteroscopy | Hysteroscopy | No | Yes | Within 3 months of IVF; follicular phase | |
| Two or more IVF failures | Hysteroscopy done within two months were excluded; Included women with previous history of hysteroscopy (45% in hysteroscopy group vs 44% in control) | Hysteroscopy | No | Yes; (only one partial septum not treated). | Preceding cycle; follicular phase | |
| One IVF failure | No details available | Hysteroscopy | Yes | No details available | No details available | |
| Two or more IVF failures | Normal HSG; no details of history of hysteroscopy | Hysteroscopy | Yes | Yes | Preceding cycle; follicular phase | |
| Unselected IVF population | Normal HSG; no details of history of hysteroscopy | Hysteroscopy | Those with suspicious lesion after injecting methylene blue were biopsied. | Yes | No details available | |
| First IVF | Excluded those with previous hysteroscopy | Hysteroscopy | No | Yes; (31/43 abnormalities treated; 5 septum and 2 submucous fibroids not treated) | 1 to 3 months before IVF; follicular phase |
IVF: in vitro fertilisation
HSG: hysterosalpingography
Interventions
Seyam 2015 randomly compared office microhysteroscopy versus no hysteroscopy in women with unexplained subfertility, for a mean duration of two years. Hysteroscopy was done in the follicular phase. When pathology was detected, treatment was done, including hysteroscopic resection of endometrial polyps and submucous fibroids, and excision of a uterine septum.
Cycle characteristics of included studies of an IVF population are shown in (Table 1). Among the IVF population, the hysteroscopy was performed in the luteal phase in one trial (Alleyassin 2017), and in the follicular phase in five trials (Demirol 2004; Rama Raju 2006; Elsetohy 2015; El‐Toukhy 2016; Smit 2016). In four trials, the IVF was performed in the immediate cycle following hysteroscopy (Demirol 2004; Rama Raju 2006; El‐Toukhy 2016; Alleyassin 2017); while in two trials, IVF was performed within one to three months after hysteroscopy (Elsetohy 2015; Smit 2016). No information on timing of hysteroscopy was available for four trials (El‐Nashar 2011; Aghahosseini 2012; Shawki 2012; Juul Hare 2018).
In three trials, hysteroscopy was combined with endometrial biopsy in the intervention arm, but no procedure was done in the control arm (Rama Raju 2006; El‐Nashar 2011; Juul Hare 2018). In six trials, hysteroscopy was done in the intervention arm, while no intervention was done in control arm (Demirol 2004; Aghahosseini 2012; Elsetohy 2015; El‐Toukhy 2016; Smit 2016; Alleyassin 2017). In one trial, investigators performed an endometrial biopsy of suspicious lesions after injecting methylene blue in the hysteroscopy arm, while no intervention was done in the control arm (Shawki 2012).
In six trials, investigators performed a hysteroscopy and treated all of the detected intracavitary abnormalities prior to IVF in the intervention arm (Demirol 2004; Rama Raju 2006; El‐Nashar 2011; Shawki 2012; Elsetohy 2015; Alleyassin 2017). In two trials, some of the intracavitary abnormalities detected during hysteroscopy were treated in the intervention arm, while some were not treated (El‐Toukhy 2016; Smit 2016). In two trials, it was not clear if detected abnormalities were treated (Aghahosseini 2012; Juul Hare 2018).
Outcomes
Seyam 2015 did not report the primary outcome of live birth; the study report indicated the assessment of the cumulative ongoing pregnancy rate, although ongoing pregnancy was not defined. We used the data for this outcome as a surrogate for live birth. This study assessed an outcome measure ‐ patient compliance ‐ which was not of interest to this Cochrane Review.
Among the IVF population, six trials reported the primary outcome of live birth (Rama Raju 2006; Aghahosseini 2012; Elsetohy 2015; El‐Toukhy 2016; Smit 2016; Juul Hare 2018). Four trials reported the primary outcome of adverse events (Elsetohy 2015; El‐Toukhy 2016; Smit 2016; Juul Hare 2018). All ten trials reported clinical pregnancy rate as an outcome.
Excluded studies
We excluded three trials for not addressing the research questions of interest for the randomised comparisons in subfertile women wishing to conceive spontaneously or before IUI (Brown 2000; El‐Khayat 2015; Shokeir 2016). See 'Characteristics of excluded studies' tables.
Among the IVF population, we excluded seven trials in ten records (Fatemi 2010; Wang 2011; Kasius 2013; Kamel 2015; Zhang 2015; Hebeisha 2018; Siristatidis 2017). Two trials were non‐randomised, and hence, excluded (Kamel 2015; Siristatidis 2017). One was a prevalence study (Fatemi 2010), and another was a cost analysis study (Kasius 2013). One study was excluded due to a different study population (women with endometritis (Wang 2011)), and another study was excluded because hysteroscopy was performed in both the intervention and control arms, and those with intracavitary abnormalities were excluded (Zhang 2015). In another trial, the investigators mainly evaluated the role of endometrial scratch before Intracytoplasmic sperm injection (ICSI), and excluded women who were found to have intracavitary abnormalities during hysteroscopy (Hebeisha 2018).
Risk of bias in included studies
We assessed the included studies for methodological quality using the Cochrane ’Risk of bias’ tool (Higgins 2011). See the ’Risk of bias’ graph (Figure 2), and ’Risk of bias’ summary (Figure 3).

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
Generation of random sequence
Eight studies used adequate methods for random sequence generation and were at low risk of selection bias (Demirol 2004; Rama Raju 2006; Shawki 2012; Elsetohy 2015; El‐Toukhy 2016; Smit 2016; Alleyassin 2017; Juul Hare 2018). Two multicentre trials among these seven studies used an intended third party trial management system (El‐Toukhy 2016), and web‐based randomisation (Smit 2016). The remaining three studies did not report the method used for randomisation clearly, and we categorised them as unclear risk of bias (El‐Nashar 2011; Aghahosseini 2012; Seyam 2015).
Allocation concealment
Only two studies clearly stated the method of allocation concealment and we rated them at low risk of bias (El‐Toukhy 2016; Smit 2016). The remaining nine trials did not state the method of allocation concealment clearly, and we assessed them as unclear risk of bias (Demirol 2004; Rama Raju 2006; El‐Nashar 2011; Aghahosseini 2012; Shawki 2012; Elsetohy 2015; Seyam 2015; Alleyassin 2017; Juul Hare 2018).
Blinding
Most of the studies did not report blinding of either clinician or participant. One study mentioned blinding of clinician and embryologist (Alleyassin 2017), and one study mentioned blinding of embryologist and researcher for allocated group (El‐Toukhy 2016). Since the outcomes (live birth, complications following hysteroscopy, ongoing and clinical pregnancy) were objective, we did not downgrade the quality of the studies for lack of blinding. Further, It was unlikely that the hysteroscopies were not performed according to the required standards, due to a lack of blinding. For these stated reasons, we deemed all the included studies to be at low risk of this bias.
Incomplete outcome data
Seven studies were deemed to be at low risk of attrition bias (Demirol 2004; Shawki 2012; Elsetohy 2015; Seyam 2015; El‐Toukhy 2016; Smit 2016; Juul Hare 2018). Four studies did not mention about dropouts, and not enough information was available to make a judgement, hence, we deemed them as unclear risk of bias (Rama Raju 2006; El‐Nashar 2011; Aghahosseini 2012; Alleyassin 2017).
Selective reporting
We judged Seyam 2015 to be at high risk of selective outcome reporting (live birth, primary outcome of interest not reported, even though study duration was long enough (seven years), giving sufficient time for authors to capture live birth data). We judged six trials evaluating women undergoing IVF at low risk of bias for selective reporting (Rama Raju 2006; Aghahosseini 2012; Elsetohy 2015; El‐Toukhy 2016; Smit 2016; Juul Hare 2018), and four trials as unclear risk of bias, since live birth was not reported (Demirol 2004; El‐Nashar 2011; Shawki 2012; Alleyassin 2017).
Other potential sources of bias
Two trials, published as conference abstracts, did not have enough information available for us to judge, hence, we deemed both of these studies as unclear risk of bias (El‐Nashar 2011; Aghahosseini 2012). One of these trials had an uneven distribution of randomised participants (142 versus 211), with substantially higher control numbers, with no clear available explanation (Aghahosseini 2012). We deemed another trial, which was also only available as a conference abstract, as high risk for this domain, due to premature termination of the trial. The authors made the decision due to slow recruitment (Juul Hare 2018). We did not observe any potential source of bias in the remaining eight trials, and deemed them to be at low risk (Demirol 2004; Rama Raju 2006; Shawki 2012; Elsetohy 2015; Seyam 2015; El‐Toukhy 2016; Smit 2016; Alleyassin 2017).
Effects of interventions
See: Summary of findings for the main comparison Screening hysteroscopy versus no hysteroscopy in women wishing to conceive spontaneously; Summary of findings 2 Screening hysteroscopy versus no hysteroscopy in women before IVF
1. A routine screening hysteroscopy, including hysteroscopic treatment of any detected uterine cavity abnormalities, versus no hysteroscopy, in subfertile women wishing to conceive spontaneously
Primary outcomes
1.1 Live birth rate
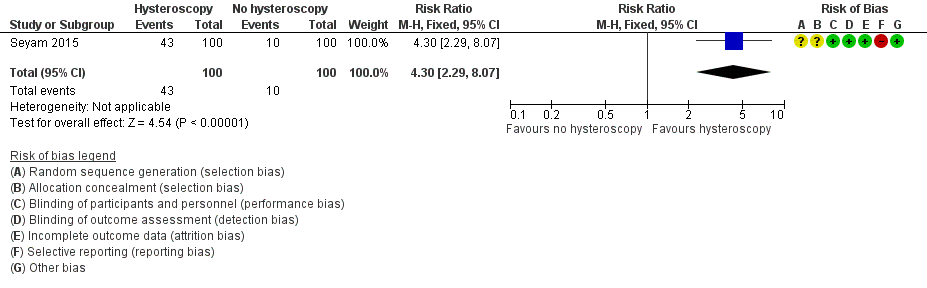
Seyam 2015 reported data on ongoing pregnancies: we used these data as a surrogate outcome for the primary outcome of effectiveness, the live birth rate. There is very low‐quality evidence, and we are uncertain whether ongoing pregnancy rate improves following screening hysteroscopy in women with at least two years of unexplained subfertility compared to no hysteroscopy (risk ratio (RR) 4.30, 95% confidence interval (CI) 2.29 to 8.07; 1 RCT; participants = 200; Analysis 1.1; Figure 4). If 10% of women achieve an ongoing pregnancy without hysteroscopy, the evidence suggests that 43% of women (95% CI 23% to 81%) will achieve an ongoing pregnancy after hysteroscopy.
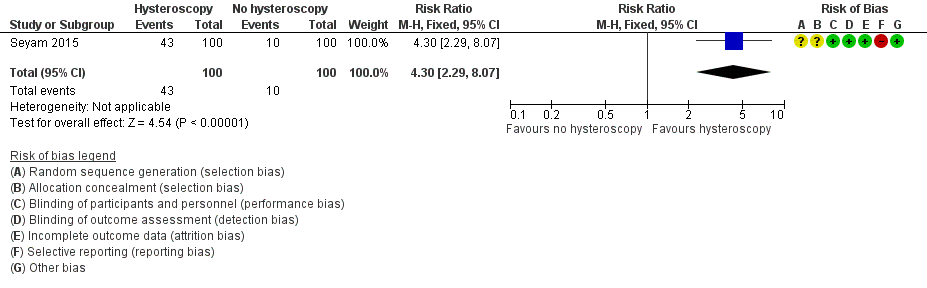
Forest plot of comparison 1. Screening hysteroscopy versus no hysteroscopy in subfertile women. Outcome 1.1. Ongoing pregnancy was used as a surrogate outcome for live birth
1.2 Adverse events
Seyam 2015 reported no adverse events in either treatment arm. The effect estimate is not estimable (Analysis 1.2).
Secondary outcomes
1.3 Clinical pregnancy rate
There is very low‐quality evidence, and we are uncertain whether clinical pregnancy rate improves following screening hysteroscopy in women with at least two years of unexplained subfertility compared to no hysteroscopy (RR 3.80, 95% CI 2.31 to 6.24; 1 RCT; participants = 200; Analysis 1.3). If 15% of women achieve a clinical pregnancy without hysteroscopy, the evidence suggests that 57% of women (95% CI 35% to 94%) will achieve an clinical pregnancy after hysteroscopy.
1.4 Miscarriage rate
There is very low‐quality evidence, and we are uncertain whether miscarriage rate increases following screening hysteroscopy compared to no hysteroscopy in women with at least two years of unexplained subfertility compared to no hysteroscopy (RR 2.80, 95% CI 1.05 to 7.48; 1 RCT; participants = 200; Analysis 1.4).
Sensitivity analyses
Sensitivity analyses on the choice of the summary effect measure (OR versus RR versus RD) or the analysis model (random‐effects versus fixed‐effect model) did not demonstrate differences of the direction of the treatment effect or the statistical significance tests for the outcomes live birth and clinical pregnancy.
2. Hysteroscopy versus no hysteroscopy for subfertile women undergoing intrauterine insemination (IUI)
We found no trials that investigated this comparison.
3. A routine screening hysteroscopy, including hysteroscopic treatment of any detected uterine cavity abnormalities, versus no hysteroscopy before in vitro fertilisation (IVF)
We pooled results from ten trials (3750 women) for this comparison (Demirol 2004; Rama Raju 2006; El‐Nashar 2011; Aghahosseini 2012; Shawki 2012; Elsetohy 2015; El‐Toukhy 2016; Smit 2016; Alleyassin 2017). Investigators of three trials reported performing endometrial biopsy along with hysteroscopy in the intervention arm (Rama Raju 2006; El‐Nashar 2011; Juul Hare 2018).
Primary outcomes
3.1 Live birth rate
Six trials reported live birth rate. Low quality‐evidence indicates that performing screening hysteroscopy before IVF may increase live birth rate compared to no hysteroscopy (RR 1.26, 95% CI 1.11 to 1.43; 6 RCTs; participants = 2745, I² = 69%; Analysis 2.1; Figure 5). For a typical clinic with 22% live birth rate, performing a screening hysteroscopy would be expected to result in live birth rates between 25% and 32%.

Forest plot of comparison 2. Screening hysteroscopy versus no hysteroscopy in women under IVF. Outcome 2.1. Live birth.
Sensitivity analysis
We performed sensitivity analysis, and after removing two trials in which an additional procedure (endometrial biopsy) was performed along with hysteroscopy, the result did not change (Rama Raju 2006; Juul Hare 2018): there was an increase in live birth rate in the intervention group (RR 1.19, 95% CI 1.03 to 1.37; 4 RCTs; participants = 2008; I² = 77%). When we removed four trials with unclear or high risk for bias for any domain (Rama Raju 2006; Aghahosseini 2012; Elsetohy 2015; Juul Hare 2018), the pooled result showed no increase in live birth rate following screening hysteroscopy (RR 0.99, 95% CI 0.82 to 1.18; 2 RCTs; participants = 1452; I² = 0%). Sensitivity analyses on the choice of the summary effect measure (OR versus RR ), or the analysis model (fixed‐effect versus random‐effects model) did not demonstrate differences in the direction of the treatment effect, or the statistical significance tests.
Subgroup analysis
We conducted a priori subgroup analyses based on the number of IVF attempts for: an unselected IVF population, before first IVF attempt, and after two or more IVF failures. It showed no evidence of a difference between the subgroups; test for subgroup differences: Chi² = 0.35, df = 2 (P = 0.84), I² = 0%.
3.1.1 Live birth rate in unselected population
There was no evidence of a difference in live birth rate following screening hysteroscopy versus no hysteroscopy in an unselected IVF population (RR 1.23, 95% CI 0.63 to 2.40; 1 RCT; participants = 217; I² = not applicable; Analysis 2.1; Figure 5).
3.1.2 Live birth rate before first IVF
There was no evidence of a difference in live birth rate following screening hysteroscopy versus no hysteroscopy in women undergoing their first IVF (RR 1.20, 95% CI 0.96 to 1.49; 2 RCTs; participants = 953; I² = 86%; Analysis 2.1; Figure 5).
2.1.3 Live birth rate after two or more IVF failures
There was an increase in live birth rate following screening hysteroscopy versus no hysteroscopy in women with two or more IVF failures (RR 1.30, 95% CI 1.10 to 1.53; 3 RCTs; participants = 652; I² = 78%; Analysis 2.1; Figure 5).
3.2 Adverse events
Four trials reported adverse events. Three trials did not report any adverse events following hysteroscopy (Elsetohy 2015; El‐Toukhy 2016; Juul Hare 2018). One trial reported a case of endometritis in the hysteroscopy arm (Smit 2016). There is very low‐quality evidence, and we are uncertain whether screening hysteroscopy is associated with higher adverse events versus no hysteroscopy (Peto odds ratio (OR) 7.47, 95% CI 0.15 to 376.42; 4 RCTs; participants = 1872; I² = not applicable; Analysis 2.2).
Secondary outcomes
3.3 Clinical pregnancy rate
Ten trials reported clinical pregnancy rate. Low‐quality evidence indicates that performing screening hysteroscopy before IVF may increase clinical pregnancy rate compared to no hysteroscopy (RR 1.32, 95% CI 1.20 to 1.45; 10 RCTs; participants = 3750; I² = 49%; Analysis 2.3; Figure 6). For a typical clinic with 28% clinical pregnancy rate, performing a screening hysteroscopy would be expected to result in clinical pregnancy rates between 33% and 40%.

Forest plot of comparison 2. Screening hysteroscopy versus no hysteroscopy in women under IVF. Outcome 2.3. Clinical pregnancy
Sensitivity analysis
We conducted a sensitivity analysis by removing eight trials with unclear or high risk for bias for any domain (Demirol 2004; Rama Raju 2006; El‐Nashar 2011; Aghahosseini 2012; Shawki 2012; Elsetohy 2015; Alleyassin 2017; Juul Hare 2018), which showed no increase in clinical pregnancy rate following screening hysteroscopy (RR 1.03, 95% CI 0.87 to 1.21; 2 RCTs; participants = 1452; I² = 0%). Sensitivity analyses on the choice of the summary effect measure (OR versus RR ), or the analysis model (fixed‐effect versus random‐effects model), did not demonstrate differences in the direction of the treatment effect, or the statistical significance tests.
Subgroup analysis
We conducted subgroup analysis according to the number of IVF attempts. It showed no evidence of a difference between the subgroups: test for subgroup differences: Chi² = 1.96, df = 2 (P = 0.38), I² = 0%.
2.3.1 Clinical pregnancy rate in unselected IVF population
There was an increase in clinical pregnancy rate following screening hysteroscopy in an unselected IVF population (RR 1.40, 95% CI 1.07 to 1.84; 3 RCTs; participants = 581; I² = 0%; Analysis 2.3; Figure 6).
2.3.2 Clinical pregnancy rate before first IVF
There was an increase in clinical pregnancy rate following screening hysteroscopy before first IVF (RR 1.20, 95% CI 1.02 to 1.41; 3 RCTs; participants = 1173; I² = 63%; Analysis 2.3; Figure 6).
2.3.3 Clinical pregnancy rate after two or more IVF failures
There was an increase in clinical pregnancy rate following screening hysteroscopy in women with two or more IVF failures (RR 1.37, 95% CI 1.21 to 1.56; 4 RCTs; participants = 1996; I² = 72%; Analysis 2.3; Figure 6).
3.4 Miscarriage rate per woman randomised
Three trials reported miscarriage rate. Low‐quality evidence indicates that there may be little or no difference in miscarriage rate following screening hysteroscopy versus no hysteroscopy (RR 1.01, 95% CI 0.67 to 1.50; 3 RCTs; participants = 1669; I² = 0%; Analysis 2.4). There may be little or no difference in miscarriage rate per pregnancy between the two groups (RR 0.97, 95% CI 0.67 to 1.40).
Subgroup analysis, according to the number of IVF attempts, showed no evidence of a difference between the subgroups; test for subgroup differences: Chi² = 1.07, df = 2 (P = 0.59), I² = 0%.
In the subgroup analysis, there was one trial each under unselected population, first IVF, and two or more IVF failures, and we noted little or difference between the miscarriage rate between the two groups.
Discussion
Summary of main results
Screening hysteroscopy versus no hysteroscopy in subfertile women wishing to conceive spontaneously
We retrieved only one single‐centre study, which reported ongoing pregnancy as a surrogate outcome for live birth. There was very low‐quality evidence, and we are uncertain whether a screening hysteroscopy improves the ongoing or clinical pregnancy rates in women with at least two years of unexplained subfertility compared to no hysteroscopy (summary of findings Table for the main comparison). The included trial reported no adverse events (complications following hysteroscopy) in either comparison arm. Evidence was very low‐quality, and we are uncertain whether screening hysteroscopy increases miscarriage rate compared to no hysteroscopy.
Screening hysteroscopy versus no hysteroscopy before intrauterine insemination (IUI)
We found no studies that investigated this comparison.
Sreening hysteroscopy versus no hysteroscopy before in vitro fertilisation (IVF)
There was low‐quality evidence that indicates that performing a screening hysteroscopy before IVF may increase the live birth and clinical pregnancy rates compared to no hysteroscopy (summary of findings Table 2). Sensitivity analysis performed by excluding those studies in which hysteroscopy was combined with endometrial biopsy, showed similar estimates for live birth and clinical pregnancy rates between the two groups. Importantly, sensitivity analysis done by pooling only trials with low risk of bias showed no improvement in live birth and clinical pregnancy rates following screening hysteroscopy. With very low‐quality evidence, we are uncertain whether screening hysteroscopy is associated with higher adverse events (complications related to hysteroscopy) versus no hysteroscopy. Low‐quality evidence indicates little or no difference in miscarriage rate following screening hysteroscopy versus no hysteroscopy.
Overall completeness and applicability of evidence
At present, there is no high‐quality evidence to support the routine use of hysteroscopy as a screening tool in the general subfertile population, for improving reproductive outcomes. We retrieved only one trial, that provided very low‐quality evidence, and assessed the effects of screening hysteroscopy in women with unexplained subfertility trying to conceive spontaneously.
The current review suggests that screening hysteroscopy may increase live birth and clinical pregnancy rates compared to no intervention, in women undergoing IVF. However, the applicability of the evidence may have some limitations and may vary according to different subpopulations. The subgroup analysis suggests that screening hysteroscopy may benefit women with two or more IVF failures.
We observed the presence of variations in eligibility criteria among individual trials in terms of additional radiological procedures done (e.g. hysterosalpingogram (HSG)) before 2D ultrasound versus only 2D ultrasound, hysteroscopy naive versus previous history of hysteroscopy, hysteroscopy alone versus hysteroscopy and endometrial biopsy, and treatment of all detected intracavitary abnormalities versus selective treatment (Table 1).The literature suggests that the diagnostic accuracy of 2D transvaginal ultrasound is suboptimal in terms of detecting intrauterine pathologies, such as polyps and adhesions, compared to other diagnostic procedures, such as sonohysterography or hysterosalpingography (Salle 1999; Ragni 2005). Trials including additional radiological procedures (e.g. HSG) would screen out more women with abnormalities, compared to trials relying solely on 2D transvaginal ultrasound before IVF, thereby, introducing some degree of heterogeneity. Further, there is supportive evidence of benefit of endometrial scratching (a procedure similar to endometrial biopsy) before IVF, and the addition of the same, along with screening hysteroscopy, may influence the true estimate (Nastri 2015). There is evidence of improved reproductive outcomes following treatment of intracavitary uterine abnormalities, such as a uterine septum and polyp (Bosteels 2015; ASRM 2016). The current review included a trial in which few women who were detected to have intracavitary abnormalities did not undergo correction in the intervention arm, and this could be a possible source of heterogeneity (Table 1). There could be some clinical heterogeneity among studies due to these stated variations in trials' protocols, as well as inclusion and exclusion criteria for recruited participants. In the IVF population, due to the high statistical heterogeneity for outcomes, such as live birth (69%) and clinical pregnancy (49%), these results should be interpreted with caution.
The optimum timing to perform hysteroscopy is still not clear, since the time interval between screening hysteroscopy and IVF varied between one and three months, although most included studies performed the hysteroscopy in the preceding menstrual cycle. Further, since the review included only studies involving fresh IVF cycles, the evidence cannot be extrapolated to other types of ART treatments, such as frozen cycles. Importantly, the complications associated with hysteroscopy were reported by very few studies.
Quality of the evidence
The current review had three comparisons
-
Hysteroscopy versus no hysteroscopy for subfertile women wishing to conceive spontaneously
-
Hysteroscopy versus non hysteroscopy for subfertile women undergoing IUI.
-
Hysteroscopy versus no hysteroscopy for women undergoing IVF.
In the comparison for subfertile women with unexplained subfertility wishing to conceive spontaneously, we reported ongoing pregnancy (as a surrogate for live birth) rate, adverse events (complications following hysteroscopy), clinical pregnancy rate, and miscarriage rate. The quality of the evidence was very low for the outcomes ongoing pregnancy and clinical pregnancy rates. Only one trial was included, and we downgraded by two levels for risk of bias and one level for indirectness. We assessed the evidence to be very low‐quality for miscarriage rate, downgrading by one level each for risk of bias, indirectness, and imprecision.
We did not find any trials that compared screening hysteroscopy versus no hysteroscopy before IUI.
For the comparison with the greatest number of studies, i.e. studying an IVF population, we reported on live birth, adverse events (complications following hysteroscopy), clinical pregnancy rate, and miscarriage rate. Overall, the evidence for live birth and clinical pregnancy was of low quality. We found the majority of the studies with unclear descriptions of allocation concealment, hence, we downgraded by one level for risk of bias. We found substantial statistical heterogeneity (49% to 69%), which could not be explained on the basis of differences in population or intervention, hence, we downgraded the evidence by a further one level for the live birth and clinical pregnancy outcomes. The adverse events outcome, which comprised of complications following hysteroscopy, was poorly reported, and we graded it as very low‐quality evidence (downgraded risk of bias by one, plus two levels for imprecision). We graded the miscarriage rate outcome as low‐quality evidence due to risk of bias (downgraded by one level), and imprecision (downgraded by one level).
Potential biases in the review process
We aimed to search for and identify all the studies eligible for this review. The search was comprehensive, and included identifying ongoing studies through trial registries. We also tried contacting authors for additional information and clarification regarding their published data. However, for conference abstracts, it was difficult to contact authors because of the absence of contact addresses or information. We requested clarification regarding data from nine authors of the included studies, and got a satisfactory reply from three authors. Additionally, two authors of this review (BWM and FB) were investigators and authors of one of the included trials (Smit 2016). However, both these authors did not participate in selection of the studies or in extracting data from that study.
Agreements and disagreements with other studies or reviews
One systematic review evaluated the role of diagnostic hysteroscopy in infertile couples and women undergoing IVF (Di Spiezio Sardo 2016). For subfertile women wishing to conceive spontaneously, the findings are in accordance with the present Cochrane Review: there is only a limited body of evidence on the role of hysteroscopy as a screening tool in the early assessment of infertile women. More research is needed.
An earlier systematic review evaluated the role of office hysteroscopy in women undergoing IVF, and included both randomised (N = 2) and non‐randomised trials (N = 3 (El‐Toukhy 2008)).The included studies had women who were both undergoing their first IVF, and those with two or more IVF failures. The authors found a significant increase in clinical pregnancy following hysteroscopy after pooling the results from both the randomised and non‐randomised trials (RR = 1.75, 95% CI 1.51 to 2.03). The authors suggested benefit could be due to the treatment of intracavitary abnormalities; negotiation of the cervical canal, thus, facilitating the subsequent embryo transfer; or inadvertent endometrial injury during hysteroscopy. These results are in agreement with current review findings, where we found a possible benefit of screening hysteroscopy, especially in women with two or more IVF failures.
Another systematic review evaluated the role of routine hysteroscopy before the first IVF, and included one RCT and five non‐randomised trials (Pundir 2014). The authors reported significantly higher clinical pregnancy rate after pooling the results (RR, 1.44, 95% CI 1.08 to 1.92). The pooled RR for live birth was 1.30 (95% CI 1.00 to 1.67). The authors suggested improved IVF outcomes following routine hysteroscopy in women undergoing their first IVF. In the subgroup population of women undergoing their first IVF, the current review did not find an increase in live birth or clinical pregnancy following screening hysteroscopy. The reason for the difference from the earlier review could be due to the inclusion of non‐randomised trials, which often overestimate the treatment effect.
In a fourth systematic review, the authors pooled three trials under the diagnostic hysteroscopy group, and found increased live birth following hysteroscopy compared to control (RR1.48, 95% CI 1.20 to 1.81); the quality of the evidence was very low. The pooled results from seven trials, found an increase in clinical pregnancy following hysteroscopy (RR 1.45, 95% CI 1.26 to 1.67); the quality of the evidence was moderate (Di Spiezio Sardo 2016). The current review pooled results from an additional three trials (Smit 2016; Alleyassin 2017; Juul Hare 2018). However, the results from both these reviews are in broad agreement.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Forest plot of comparison 1. Screening hysteroscopy versus no hysteroscopy in subfertile women. Outcome 1.1. Ongoing pregnancy was used as a surrogate outcome for live birth

Forest plot of comparison 2. Screening hysteroscopy versus no hysteroscopy in women under IVF. Outcome 2.1. Live birth.

Forest plot of comparison 2. Screening hysteroscopy versus no hysteroscopy in women under IVF. Outcome 2.3. Clinical pregnancy

Comparison 1 Screening hysteroscopy versus no hysteroscopy in subfertile women wishing to conceive spontaneously, Outcome 1 Live birth.

Comparison 1 Screening hysteroscopy versus no hysteroscopy in subfertile women wishing to conceive spontaneously, Outcome 2 Adverse outcomes.

Comparison 1 Screening hysteroscopy versus no hysteroscopy in subfertile women wishing to conceive spontaneously, Outcome 3 Clinical pregnancy.

Comparison 1 Screening hysteroscopy versus no hysteroscopy in subfertile women wishing to conceive spontaneously, Outcome 4 Miscarriage.

Comparison 2 Screening hysteroscopy versus no hysteroscopy in women before IVF, Outcome 1 Live birth.

Comparison 2 Screening hysteroscopy versus no hysteroscopy in women before IVF, Outcome 2 Adverse outcomes.

Comparison 2 Screening hysteroscopy versus no hysteroscopy in women before IVF, Outcome 3 Clinical pregnancy.

Comparison 2 Screening hysteroscopy versus no hysteroscopy in women before IVF, Outcome 4 Miscarriage.
| Hysteroscopy compared with no hysteroscopy in women wishing to conceive spontaneously | ||||||
| Patient or population: women with unexplained subfertility wishing to conceive spontaneously Settings: Arafa Hospital, Fayoum, Egypt Intervention: screening hysteroscopy Comparison: no hysteroscopy | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Risk with no hysteroscopy | Risk with hysteroscopy | |||||
| Live birth | 100 per 1000 | 430 per 1000 (229 to 807) | RR 4.30 (2.29 to 8.07) | 200 (1 RCT) | ⊕⊕⊝⊝ | |
| Adverse events | 0 per 1000 | 0 per 1000 (0 to 0) | not estimable | (1 RCT) | ⊕⊝⊝⊝ | |
| Clinical pregnancy | 150 per 1000 | 570 per 1000 (347 to 936) | RR 3.80 (2.31 to 6.24) | 200 (1 RCT) | ⊕⊕⊝⊝ | |
| Miscarriage | 50 per 1000 | 140 per 1000 (52 to 374) | RR 2.80 (1.05 to 7.48) | 200 (1 RCT) | ⊕⊝⊝⊝ | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aVery serious risk of bias, downgraded by two levels: unclear random sequence generation and allocation concealment ‐ high risk of selective outcome reporting | ||||||
| Screening hysteroscopy versus no hysteroscopy in women before IVF | ||||||
| Patient or population: women before IVF treatment | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with no hysteroscopy | Risk with hysteroscopy | |||||
| Live birth | 221 per 1000 | 279 per 1000 | RR 1.26 | 2745 | ⊕⊕⊝⊝ | |
| Adverse events | 0 per 1000 | 0 per 1000 | Peto OR 7.47 | 1872 | ⊕⊕⊝⊝ | |
| Clinical pregnancy | 278 per 1000 | 368 per 1000 | RR 1.32 | 3750 | ⊕⊕⊝⊝ | |
| Miscarriage | 53 per 1000 | 53 per 1000 | RR 1.01 | 1669 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| aSerious risk of bias, downgraded by one level: only two studies had low risk of bias for all the domains. The rest of the studies had unclear risk for allocation concealment. One study was categorised at high risk for 'other' domain. There is a likely chance of overestimating the treatment. | ||||||
| Study ID | Population | Previous HSG or hysteroscopy | Intervention | Additional endometrial biopsy | Detected abnormalities treated | Timing of hysteroscopy |
| Unexplained infertility of 2 years duration | Normal HSG | Hysteroscopy | No | Yes | Follicular phase | |
| Two or more IVF failures | Normal HSG; no hysteroscopy in previous 2 months | Hysteroscopy | No | No details | No details available | |
| First IVF | Normal HSG; women with history of hysteroscopy excluded. | Hysteroscopy | No | Yes | Preceding cycle; luteal phase | |
| Two or more IVF failures | Normal HSG; no details of history of hysteroscopy | Hysteroscopy | No | Yes | Preceding cycle; follicular phase | |
| Unselected IVF population | No details of HSG; no details of history of hysteroscopy | Hysteroscopy | Yes | Yes | No details | |
| First IVF | Normal HSG; no details of history of hysteroscopy | Hysteroscopy | No | Yes | Within 3 months of IVF; follicular phase | |
| Two or more IVF failures | Hysteroscopy done within two months were excluded; Included women with previous history of hysteroscopy (45% in hysteroscopy group vs 44% in control) | Hysteroscopy | No | Yes; (only one partial septum not treated). | Preceding cycle; follicular phase | |
| One IVF failure | No details available | Hysteroscopy | Yes | No details available | No details available | |
| Two or more IVF failures | Normal HSG; no details of history of hysteroscopy | Hysteroscopy | Yes | Yes | Preceding cycle; follicular phase | |
| Unselected IVF population | Normal HSG; no details of history of hysteroscopy | Hysteroscopy | Those with suspicious lesion after injecting methylene blue were biopsied. | Yes | No details available | |
| First IVF | Excluded those with previous hysteroscopy | Hysteroscopy | No | Yes; (31/43 abnormalities treated; 5 septum and 2 submucous fibroids not treated) | 1 to 3 months before IVF; follicular phase | |
| IVF: in vitro fertilisation HSG: hysterosalpingography | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Live birth Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.3 [2.29, 8.07] |
| 2 Adverse outcomes Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Clinical pregnancy Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.8 [2.31, 6.24] |
| 4 Miscarriage Show forest plot | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.8 [1.05, 7.48] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Live birth Show forest plot | 6 | 2745 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [1.11, 1.43] |
| 1.1 Unselected | 1 | 217 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.63, 2.40] |
| 1.2 First IVF | 2 | 953 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.96, 1.49] |
| 1.3 Two or more IVF failures | 3 | 1575 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [1.10, 1.53] |
| 2 Adverse outcomes Show forest plot | 4 | 1872 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.47 [0.15, 376.42] |
| 2.1 Unselected | 1 | 217 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 First IVF | 2 | 953 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 7.47 [0.15, 376.42] |
| 2.3 Two or more IVF failures | 1 | 702 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Clinical pregnancy Show forest plot | 10 | 3750 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.32 [1.20, 1.45] |
| 3.1 Unselected | 3 | 581 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [1.07, 1.84] |
| 3.2 First IVF | 3 | 1173 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [1.02, 1.41] |
| 3.3 Two or more IVF failures | 4 | 1996 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [1.21, 1.56] |
| 4 Miscarriage Show forest plot | 3 | 1669 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.67, 1.50] |
| 4.1 Unselected | 1 | 217 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.81 [0.12, 68.33] |
| 4.2 First IVF | 1 | 750 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.59, 2.80] |
| 4.3 Two or more IVF failures | 1 | 702 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.55, 1.42] |

