Rehabilitación cardíaca con ejercicios para pacientes adultos con angina estable
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Study design: RCT No. of centres: 1 Country: United Kingdom Dates participants recruited: September 2008‐February 2010 When randomised: after written consent and all baseline measures were collected (approximately 48 hours) Maximum follow up: 6 months | |
| Participants | Inclusion criteria: confirmed diagnosis of stable angina, able to read and speak fluent English, had regular access to the Internet, were computer literate and had not had conventional cardiac rehabilitation within the previous year. Exclusion criteria: unstable angina, significant cardiac arrhythmia, any co‐morbidities preventing physical activity, or were severely anxious/depressed. Severely anxious/depressed participants were excluded by eliminating anyone with a history of being prescribed medication for either anxiety or depression. N randomised: total: 94; intervention: 48; comparator: 46 (47 randomised to comparator but 1 dropped out at baseline) Diagnosis (% of participants):
Age (mean ±SD): total: 66.24; intervention: 66.27±8.35; comparator: 66.20±10.06 Percentage male: total: 74%; intervention: 71%; comparator: 78% | |
| Interventions | Description: online web‐based intervention with physical activity measured over a 2‐day period using a monitor. The intervention was delivered at home via the Internet and called 'ActivateYourHeart'. Individuals were given tailored goals for exercise. The programme aimed to improve participants' cardiac risk profile within 4 stages and was designed to be completed within 6 weeks. Baseline data were used to set individualised, tailored goals focused on exercise, diet, emotions and smoking behaviour. The intervention used the following behaviour change techniques: setting/reviewing behavioural goals, self‐monitoring, feedback on behaviour, graded tasks, social reward, providing information about health consequences, and reducing negative emotions. Modality: being “physically active”. This was determined by online assessment by meeting goals (online exercise diary). Dose: individualised daily exercise (most commonly walking) Length of session: not reported Intermittent nurse or exercise specialist support? Programme users could initiate contact with cardiac rehabilitation nurses for advice and support via an online email link or by joining a scheduled synchronized chat room held on a weekly basis. The cardiac nurses were based at University Hospitals of Leicester. | |
| Outcomes | HRQL and anxiety and depression (assessed using validated instruments (Seattle Angina Questionnaire (SAQ) and The MacNew questionnaire)) | |
| Notes | The exercise was self‐directed and documented by participants and not led by clinicians. Trial was registered with the ISRCTN registry. Registration number: ISRCTN90110503 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computerized block randomization list was produced by our departmental statistician" |
| Allocation concealment (selection bias) | Low risk | "Allocation concealment was achieved by sequentially numbered sealed envelopes, opened after baseline data collection for each participant by the researcher carrying out the fieldwork" |
| Blinding of outcome assessment (detection bias) | High risk | "Participants and the outcome assessor were not blinded to group allocation" |
| Incomplete outcome data (attrition bias) | Low risk | All withdrawals and dropouts described, with similar reasons for missing outcome data comparable across groups. 10/95 (11% attrition) dropped out at 6 weeks and 21/95 (23% attrition) dropped out at 6 months |
| Selective reporting (reporting bias) | High risk | Two intended outcomes (cost and level of positivity) originally reported in the trial protocol were not reported or mentioned in the full report |
| Groups balanced at baseline | Low risk | Demographic characteristics of both groups were well balanced |
| Groups received comparable care except the intervention | High risk | Intervention group participants were offered a 6‐week web‐based rehabilitation programme while control group received usual care by GP that set individualized tailored goals focused on exercise (e.g. being physically active for 30 minutes, 5 times a week), diet (e.g. eating more fruit/vegetables and reducing salt intake), emotions (e.g. managing stress and other negative emotions), and smoking (e.g. reduce cigarette smoking if relevant). "The program also contained information to help users understand heart disease. Program users could initiate contact with cardiac rehabilitation nurses for advice and support via an online email link or by joining a scheduled synchronized chat room held on a weekly basis." Not offered to control group. |
| Methods | Study design: RCT No. of centres: 1 Country: Germany Dates participants recruited: March 1997‐March 2001 When randomised: March 1997‐March 2001 Maximum follow up: 12 months | |
| Participants | Inclusion criteria: eligible participants had class I to III angina pectoris (classified according to the Canadian Cardiovascular Society) with documented myocardial ischaemia during stress ECG and/or 99mTc scintigraphy. Only participants living within a 25 km radius of the host institution were recruited. N randomised: total: 101; intervention: 51; comparator: 50 Diagnosis (% of participants):
Age (mean ±SD): total: not reported; intervention: 62±1; comparator: 60±1 Percentage male: 100% | |
| Interventions | Description: during the first 2 weeks, participants exercised in the hospital 6 times per day for 10 minutes on a bicycle ergometer at 70% of the symptom‐limited maximal heart rate. Before discharge from the hospital, a maximal symptom‐limited ergospirometry was performed to calculate the target heart rate for home training, which was defined as 70% of the maximal heart rate during symptom‐limited exercise. participants were asked to exercise on their bicycle ergometer close to the target heart rate for 20 minutes per day and to participate in one 60‐minute group training session of aerobic exercise per week. Dose: 48 x 7 x 20 mins Length of session: 20 minutes Intermittent nurse or exercise specialist support? Not reported Co‐interventions: participants recommended to receive acetylsalicyl acid, beta‐blockers, angiotensin‐converting enzyme inhibitors and statins (according to common guidelines) Comparator: Description: The control group all received standard PCI (to target lesion performed 14.8 +/‐ 3.3 days post randomisation) but no exercise. Co‐interventions: All participants were given acetylsalicyclic acid (100 mg/d) and clopidogrel (300 mg/d) on the day before the procedure. | |
| Outcomes | Angina symptoms (CCS), exercise capacity, revascularisations, myocardial infarction, cost effectiveness, combined clinical endpoint (death cardiac, stroke, CABG, PCI, AMI, worsening angina with objective evidence resulting in hospitalisation) | |
| Notes | Source of Funding: unconditional scientific grant from Aventis Germany Conflicts of Interest: does not declare conflict of interest Two‐year results of this study are reported by Walther 2008. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear if clinician or participant‐led treatment allocation: "Patients were randomly assigned to either stent angioplasty or exercise training by drawing an envelope with the treatment assignment enclosed" |
| Allocation concealment (selection bias) | Unclear risk | It is unclear if envelopes were sequentially numbered or opaque. |
| Blinding of outcome assessment (detection bias) | Low risk | "Initially and after 12 months, the angina pectoris status of all participants was classified according to CCS class by a physician blinded for patient assignment, and a symptom‐limited ergospirometry was performed" |
| Incomplete outcome data (attrition bias) | Low risk | All dropouts and withdrawals were described. Intervention: 4/51 lost to follow‐up Control: 3/50 lost to follow‐up No loss to follow‐up for primary endpoint analysis |
| Selective reporting (reporting bias) | Unclear risk | Study protocol was not available |
| Groups balanced at baseline | Low risk | "Both groups were comparable with regard to baseline characteristics and medical therapy (Table 1), which remained unchanged during follow‐up" |
| Groups received comparable care except the intervention | Low risk | "The control group all received PCI as part of the study however repeat coronary angiography was performed to assess the long‐term result of the coronary intervention in the PCI group and to monitor the progression of atherosclerosis in both groups." |
| Methods | Study design: RCT No. of centres: 1 Country: China Dates participants recruited: September 2002‐December 2003 When randomised: unclear Maximum follow up: 6 months | |
| Participants | Inclusion criteria: first hospitalisation with either angina pectoris or myocardial infarction, willing to participate in this study, able to speak, read and write Chinese, living at home with family after hospital discharge, living in Chengdu and available for telephone follow‐up, and with fasting blood sample taken for lipid test within 24 hours of hospitalisation Exclusion criteria: planning for surgical treatment; with pre‐existing mobility problems; with hypothyroidism or nephrotic syndrome; with diagnosed psychosis or currently undergoing anti‐psychosis treatment; and with terminal illness N Randomised: total: 167; intervention: 83; comparator: 84 Diagnosis (% of participants):
Age (mean ±SD): total: not reported; intervention: 62.11±97.44; comparator: 61.37±7.61 Percentage male: total: 71.2%; intervention: 68.7%; comparator: 73.8% | |
| Interventions | Description: 12‐week home‐based cardiac rehabilitation intervention in two phases: hospital‐based patient/family education (topics included physical exercise) and home‐based rehabilitation care which included setting daily behavioural goals for walking performance. Components: exercise and behaviour change Dose: NR Length of session: NR Intermittent nurse or exercise specialist support? Patients were supervised, coached and supported by an experienced cardiac nurse throughout a 12‐week period. Follow‐up care was via home visits and telephone calls. Co‐interventions: education given regarding CHD, medication management, angina prevention and management, smoking cessation and family support. Family members were encouraged and instructed to participate in lifestyle change and provide support to patient. Comparator: Description: routine care Co‐interventions: none | |
| Outcomes | Exercise capacity (Jenkins Activity Checklist for Walking) | |
| Notes | Source of funding: The Hong Kong Polytechnic University, Hong Kong, China. No usable data for our review was measured in this study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Computer‐generalized random table" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Low risk | Intervention: 9/83 (11%) lost to follow‐up Control: 17/84 (20%) lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Groups balanced at baseline | Low risk | No differences between groups |
| Groups received comparable care except the intervention | Unclear risk | Intervention received education about a variety of topics (CHD and self‐management principles, medication management, angina prevention and management, dietary management, smoking cessation and family support) in addition to exercise |
| Methods | Study design: RCT No. of centres: 1 Country: India Dates participants recruited: NR When randomised: NR Maximum follow up: 12 months | |
| Participants | Inclusion criteria: have chronic stable angina and angiographically proven CAD Exclusion criteria: participants with recent (within last six months) myocardial infarction or unstable angina N Randomised: total: 42; intervention: 21; comparator: 21 Diagnosis (% of participants):
Age (mean ±SD): total: NR; intervention:51±9; comparator:52±10 Percentage male: 100% | |
| Interventions | Description: yoga lifestyle intervention programme, including yoga exercises, dietary management, moderate aerobic exercise and stress management. Participants and their spouses spent 4 days at a yoga residential centre undergoing training in yoga and various yogic lifestyle techniques. They did yoga exercises at home for 90 mins/day. Intervention consisted of yogic lifestyle techniques and stress management (health rejuvenation exercises, breathing exercises, relaxation exercises, stretch relaxation, and meditation), dietary control and moderate aerobic exercises. Components: exercises, psychosocial support and diet advice Dose: 48 x 7 x 90 mins Intermittent nurse or exercise specialist support? Yoga specialist support on a fortnightly basis; going to the hospital for assessment on a monthly basis. Co‐interventions: relaxation, reflection, stress management, diet advice Comparator: Description: Usual care (including medical therapy, risk factor control, diet advice and moderate aerobic exertion) Co‐interventions: None described | |
| Outcomes | All‐cause mortality, severity of angina, revascularisation, exercise capacity | |
| Notes | Source of Funding: Central Research Institute of Yoga, Ministry of Health, Government of India Conflicts of Interest: NR | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) | Unclear risk | Withdrawals and drop outs not described |
| Selective reporting (reporting bias) | High risk | The study protocol was not available. In the methods section, participants are described as being assessed monthly but only results at 12 months are reported. |
| Groups balanced at baseline | High risk | Participants in yoga group baseline experienced more angina episodes/week |
| Groups received comparable care except the intervention | High risk | "The active group was treated with a user‐friendly program consisting of yoga, control of risk factors, diet control and moderate aerobic exercise. The control group was managed by conventional methods, i.e. risk factor control and American Heart Association step I diet." |
| Methods | Study design: RCT No. of centres: 1 Country: not reported Dates participants recruited: not reported When randomised: on entry to study Maximum follow up: 6 months | |
| Participants | Inclusion criteria: diagnosis of stable angina pectoris Exclusion criteria: participants with hypertension, valve disease, cardiac arrhythmia, and participants on digoxin, beta‐blocker, or nifedipine therapy N Randomised: total: 24; intervention: 12; comparator: 12 Diagnosis (% of participants):
Age (mean ±SD): total: 50; intervention: 51 (not reported); comparator: 49 (not reported) Percentage male: total: 88%; intervention: 83%; comparator: 92% | |
| Interventions | Description: the participants randomised into the training group undertook the Canadian Air Force programme (5BX/XBX) under supervision in the hospital which required only 11 to 12 minutes of daily physical training. The programme lasted six months, and during hospital sessions the participants exercised with electrodes attached in CM5 position. The participants started training at the lowest physical capacity level, and progressed by increasing this level according to their age and sex. If the level of exercise was well tolerated the patient was asked to perform the same level at home during the week and return so that the level could be adjusted under supervision. If, during the performance of an increased level of exercise, anginal pain and/or ischaemic ST depression occurred, the participants were maintained at the previous level of exercise. Resistance training included? Not reported Total duration: 6 months Intermittent nurse or exercise specialist support? Not reported Co‐interventions: advice and usual care from consultant cardiologist Comparator: Description: normal daily activities Co‐interventions: advice and usual care from consultant cardiologist | |
| Outcomes | Exercise capacity | |
| Notes | Sources of Funding: British Heart Foundation and the Wellcome Trust Conflicts of interest: NR | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "On entry to the study, the patients were randomised into two groups." Randomisation process not described |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Low risk | Assessment of repeatability of test was blinded: "…HR/ST thresholds obtained were used for analysis of repeatability of the test, in a blinded fashion as was previously described; all tracings were copied and the five used in the repeatability tests were randomly interspersed by a person other than the observer." |
| Incomplete outcome data (attrition bias) | High risk | Intervention: 0/12 (0%) lost to follow‐up Control: 7/12 (58%) lost to follow‐up “In the control group an independent decision to start medical treatment with drugs was made during routine cardiological follow‐up on the basis of deterioration of symptoms.” |
| Selective reporting (reporting bias) | Unclear risk | Study protocol was not available |
| Groups balanced at baseline | Unclear risk | No significant differences in baseline characteristics however these were only data on age, gender and duration of exercise, no other clinical data gathered. |
| Groups received comparable care except the intervention | Low risk | “Clinically, the two groups were managed identically by the consultant cardiologist (WW). Each patient was advised to stop smoking and avoid increases in body weight.” |
| Methods | Study design: RCT (same trial as Niebauer 1995) No. of centres: 1 Country: Germany Dates participants recruited: NR When randomised: after introductory study familiarising participants with aims of study, randomisation process and alternative therapeutic approaches, and after written consent obtained Maximum follow up: 12 months | |
| Participants | Inclusion criteria: male gender, stable symptoms, willingness to participate in the study for at least 12 months, coronary artery stenoses well documented by angiography, and permanent residence within 25 km of the training facilities at Heidelberg. Exclusion criteria: unstable angina pectoris, left main coronary artery stenosis > 25% luminal diameter reduction, severely depressed left ventricular function (ejection fraction < 35%), significant valvular heart disease, insulin‐dependent diabetes mellitus, primary hypercholesterolemia (type II hyperlipoproteinemia, low density lipoprotein > 210 mg/dl), and occupational, orthopaedic, and other conditions precluding regular participation in exercise sessions N Randomised: total: 113; intervention: 56; comparator: 57 Diagnosis (% of participants): AMI 66%
Age (mean ±SD): Total: not reported; intervention: 52.8±5.8; comparator: 54.2±7.7 Percentage male: 100% | |
| Interventions | Description: regular physical exercise and low fat diet (diet advice given during initial 3‐week stay on metabolic ward). Daily exercise at home on a cycle ergometer for a minimum of 20 minutes close to their target heart rates, which were determined as 75% of the maximal heart rate during symptom‐limited exercise. In addition, participants were expected to participate in at least two group training sessions consisting of intensive physical exercise of 60 minutes each week. Components: exercise, educational and behavioural Modality: cycle ergometer Resistance training included? No Total duration: 12 months Intermittent nurse or exercise specialist support? Instructions, given during initial 3 weeks on a metabolic ward, on how to lower the fat content of their regular diet. Information sessions conducted at regular intervals five times a year for participants and their spouses to discuss dietary, psychosocial, and exercise‐related problems. In addition, participants were offered opportunities to discuss personal questions and problems after each training session. Does not state who delivers this. Not performed for control group. Co‐interventions: regular anti‐anginal medication (including beta blocking agents), low cholesterol diet and advice (as above) Comparator: Description: usual care rendered by private physicians. participants assigned to the control group spent 1 week on the metabolic ward, where they received identical instructions about the necessity of regular physical exercise and how to lower fat consumption. They were served a low‐fat diet corresponding to the American Heart Association recommendations, phase 1, and they were encouraged to participate in local coronary exercise groups. Adherence to these guidelines was left to their own initiative | |
| Outcomes | All‐cause mortality, myocardial infarction, revascularisations, exercise capacity, adverse events | |
| Notes | Source of funding: grant from Bundesministerium fir Forschung und Technologie, Bonn, FRG. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Process of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | "Sealed envelopes were used to randomize participants between intervention and control groups." |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details of blinding for outcomes were reported. |
| Incomplete outcome data (attrition bias) | High risk | Intervention: 16/56 (29 %) lost to follow‐up Control: 5/57 (9%) lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Study protocol was not available |
| Groups balanced at baseline | Low risk | No significant differences in baseline characteristics |
| Groups received comparable care except the intervention | High risk | "Patients assigned to the control group spent 1 week on the metabolic ward, where they received identical instructions about the necessity of regular physical exercise and how to lower fat consumption. They were served a low‐fat diet corresponding to the American Heart Association recommendations, phase 1,30 and they were encouraged to participate in local coronary exercise groups. Adherence to these guidelines, however, was left to their own initiative, and "usual care" was rendered by their private physicians. They were asked not to take lipid‐lowering medications." In addition to receiving exercise and dietary advice, the intervention group also received regular information sessions "conducted at regular intervals five times a year for participants and their spouses to discuss dietary, psychosocial, and exercise‐related problems". |
| Methods | Study design: RCT No. of centres: 1 Country: United Kingdom Dates participants recruited: not reported When randomised: after study by planar thallium scintigraphy, they were then randomised. Maximum follow up: 12 months | |
| Participants | Inclusion criteria: < 60 years old, male, chronic stable angina ≥ 6 months’ duration and a positive exercise tolerance test Exclusion criteria: previous myocardial infarction, coronary bypass surgery or angioplasty, recent unstable angina, diabetes mellitus, uncontrolled hypertension, valvular heart disease and physical handicap N Randomised: total: 40; intervention: 20; comparator: 20 Diagnosis (% of participants):
Age (mean ±SD): total: 52; intervention: 53; comparator: 51 Percentage male: 100% | |
| Interventions | Description: the training group undertook the Canadian Airforce Program for Physical Fitness. This is a brief 11 ‐minute daily exercise program of 5 callisthenic exercises requiring no equipment. It was prescribed for daily home use, with exercise levels increasing in intensity at weekly intervals to achieve a progressive increase in physical fitness. Participants moved to the next level if the previous level could be completed within 11 minutes without excessive chest pain or dyspnoea. No limit was placed on the maximum exercise level. A weekly hospital supervised session was used to initiate new participants and monitor early progress Resistance training included? No Total duration: 12 months Intermittent nurse or exercise specialist support? Yes Co‐interventions: initial weekly hospital visit for monitoring. Subsequent attendance optional. Comparator: Description: The control subjects were informed that mild exercise may be beneficial and were advised with respect to diet and smoking habits. They were formally followed up at 3‐month intervals throughout the study, as was the exercise group, but were granted open access to the controlling physician at any time in order to counteract possible bias resulting from weekly contact with the exercise group. | |
| Outcomes | All‐cause mortality, myocardial infarction, exercise capacity | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After thallium scintigraphy, patients were randomly allocated to training and control groups" No description of randomisation process |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) | Unclear risk | Blinding not reported |
| Incomplete outcome data (attrition bias) | Low risk | All withdrawals and drop outs described Intervention: 3/20 (15%) lost to follow‐up Control: 4/20 (20%) lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Study protocol was not available |
| Groups balanced at baseline | Low risk | "There were no significant differences between the groups” |
| Groups received comparable care except the intervention | Low risk | Control group received advice on exercise, smoking and diet |
AMI: acute myocardial infarction
CABG: coronary artery bypass graft
CAD: coronary artery disease
CCS: Canadian Cardiovascular Society
CHD: coronary heart disease
ECG: electrocardiogram
GP: general practitioner
HRQL: health‐related quality of life
N: number
NR: not reported
PCI: percutaneous coronary intervention
RCT: randomised controlled trial
SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Participants receive exercise + PCI or no exercise + PCI and so we had concern that co‐intervention (PCI) would confound the comparison. | |
| Mixed population—angina population < 50% | |
| Comparator received exercise | |
| Mixed population—angina population < 50% | |
| Comparator received exercise | |
| Mixed population—angina population < 50% | |
| Follow‐up only 4 months | |
| Conference abstract ‐ paper not published in full. Unable to contact authors to check for inclusion due to age of publication. | |
| No structured exercise component | |
| Population included mixed CHD | |
| Mixed population—angina population < 50% | |
| Population did not have angina | |
| No structured exercise component | |
| Mixed population—angina population < 50% |
CHD: coronary heart disease
PCI: percutaneous coronary intervention
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A Clinical Trial of a Self‐Management Education Program for People With Chronic Stable Angina |
| Methods | RCT |
| Participants | Adults with chronic stable angina |
| Interventions | Chronic Angina Self‐Management Program |
| Outcomes | SF‐36; Seattle Angina Questionnaire |
| Starting date | September 2003 |
| Contact information | https://clinicaltrials.gov/ct2/show/NCT00350922 (last accessed 01 Sept 2017) |
| Notes |
| Trial name or title | The Effect of Exercise on Peripheral Blood Gene Expression in Angina |
| Methods | RCT |
| Participants | Adults with stable angina |
| Interventions | Exercise training |
| Outcomes | Seattle Angina questionnaire (SAQ) |
| Starting date | Not reported |
| Contact information | BMC Public Health 2010;10:620. |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 All‐cause mortality Show forest plot | 3 | 195 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.18, 5.67] |
| Analysis 1.1 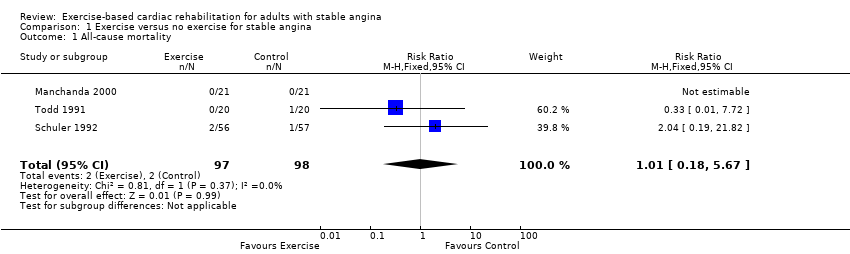 Comparison 1 Exercise versus no exercise for stable angina, Outcome 1 All‐cause mortality. | ||||
| 2 Acute myocardial infarction (AMI) Show forest plot | 3 | 254 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.07, 1.63] |
| Analysis 1.2 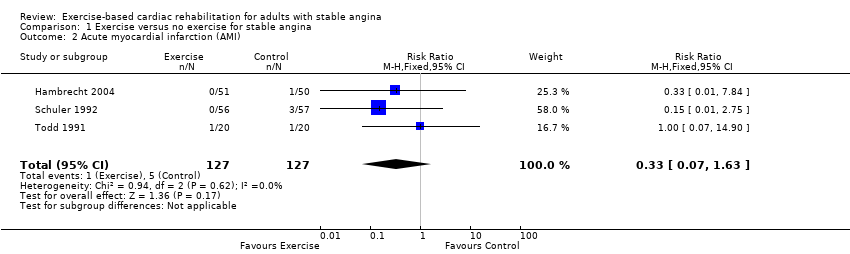 Comparison 1 Exercise versus no exercise for stable angina, Outcome 2 Acute myocardial infarction (AMI). | ||||
| 3 Revascularisation procedure (CABG or PCI) Show forest plot | 3 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.11, 0.64] |
| Analysis 1.3  Comparison 1 Exercise versus no exercise for stable angina, Outcome 3 Revascularisation procedure (CABG or PCI). | ||||
| 4 Exercise capacity Show forest plot | 5 | 267 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.45 [0.20, 0.70] |
| Analysis 1.4  Comparison 1 Exercise versus no exercise for stable angina, Outcome 4 Exercise capacity. | ||||
| 5 Cardiovascular‐related hospital admissions Show forest plot | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.10] |
| Analysis 1.5 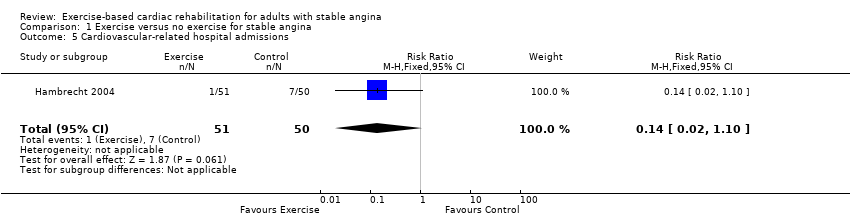 Comparison 1 Exercise versus no exercise for stable angina, Outcome 5 Cardiovascular‐related hospital admissions. | ||||

PRISMA flow diagram of trial selection
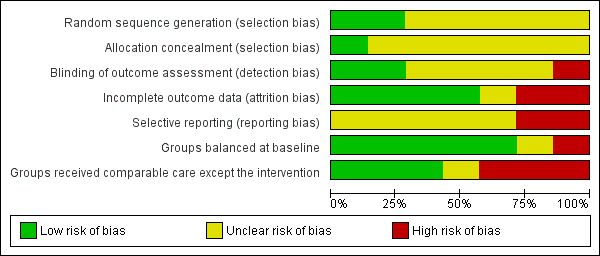
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Exercise versus no exercise for stable angina, Outcome 1 All‐cause mortality.

Comparison 1 Exercise versus no exercise for stable angina, Outcome 2 Acute myocardial infarction (AMI).

Comparison 1 Exercise versus no exercise for stable angina, Outcome 3 Revascularisation procedure (CABG or PCI).
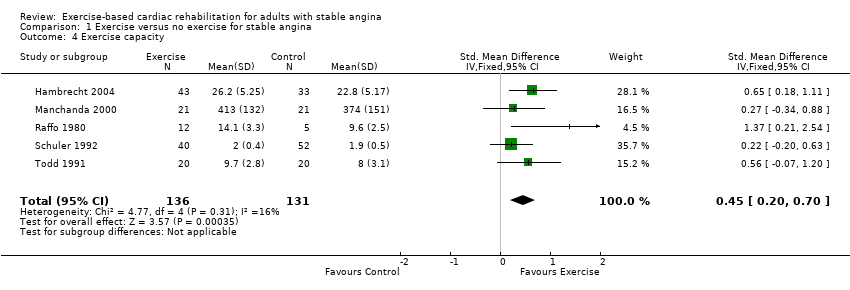
Comparison 1 Exercise versus no exercise for stable angina, Outcome 4 Exercise capacity.
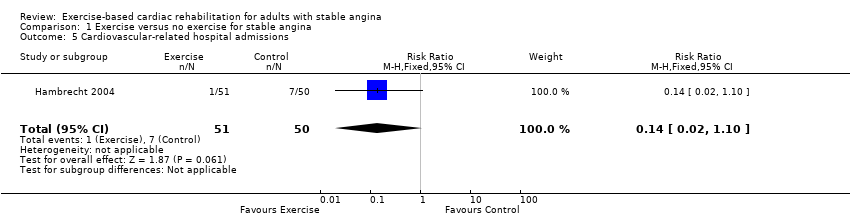
Comparison 1 Exercise versus no exercise for stable angina, Outcome 5 Cardiovascular‐related hospital admissions.
| Exercise‐based cardiac rehabilitation (CR) compared to usual care for patients with stable angina | ||||||
| Patient or population: adults with stable angina | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with usual care | Risk with exercise‐based cardiac rehabilitation | |||||
| All‐cause mortality Follow‐up: 12 months | Study population | RR 1.01 | 195 | ⊕⊝⊝⊝ | We are uncertain about the effect of exercise‐based CR on all‐cause mortality compared to usual care. | |
| 20 per 1,000 | 21 per 1,000 | |||||
| Acute myocardial infarction (AMI) Follow‐up: 12 months | Study population | RR 0.33 | 254 | ⊕⊝⊝⊝ | We are uncertain about the effect of exercise‐based CR on AMI compared to usual care. | |
| 39 per 1,000 | 13 per 1,000 | |||||
| Exercise capacity (assessed using a variety of outcomes including VO2 max and duration of exercise) Follow‐up: range 6 to 12 months | The mean exercise capacity in the intervention groups was 0.45 standard deviations higher | 267 | ⊕⊕⊝⊝ | Using Cohen's rule of thumb a SMD of 0.2 represents a small effect, 0.5 a moderate effect and 0.8 a large effect between groups (Cohen 1988). Exercise‐based CR may slightly improve exercise capacity compared to usual care. | ||
| Cardiovascular‐related hospital admissions Follow‐up: 12 months | Study population | RR 0.14 (0.02 to 1.1) | 101 | ⊕⊝⊝⊝ | We are uncertain about the effect of exercise‐based CR on cardiovascular‐related hospital admissions compared to usual care. | |
| 140 per 1000 | 20 per 1000 (2 to 154) | |||||
| Health‐related quality of life (assessed with: Seattle Angina Questionnaire and The MacNew Questionnaire) | One study showed improvement in emotional score at 6‐week follow up, and benefits in angina frequency and social HRQL score at 6 months follow‐up. | Not estimable | 94 (1 RCT) | ⊕⊝⊝⊝ | We are uncertain about the effect of exercise‐based CR on quality of life compared to usual care. | |
| Return to work | No studies were found that looked at return to work. | |||||
| Adverse events (e.g. skeletomuscular injury) Follow‐up: 12 months | Only one study looked at adverse events and reported that there were no adverse events during the exercise‐based CR. | Not estimable | 101 (1 RCT) | ⊕⊝⊝⊝ | We are uncertain about the effect of exercise‐based CR on adverse events compared to usual care. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Some concerns with random sequence generation, allocation concealment, blinding of outcome assessment and selective reporting; bias likely, therefore quality of evidence downgraded by one level 2 Some concern with applicability to review question as participants in all studies were limited to middle‐aged men, therefore quality of evidence downgraded by one level 3 Imprecise due to small number of participants (less than 300) and confidence intervals including potential for important harm or benefit as 95% CI crosses RR of 0.75 and 1.25, therefore quality of evidence downgraded by two levels 4 Some concerns with random sequence generation, allocation concealment, blinding of outcome assessment, selective reporting and unbalanced groups at baseline; bias likely, therefore quality of evidence downgraded by one level 5 Some concern with random sequence generation, allocation concealment, blinding of outcome assessment, high loss to follow‐up, selective reporting and unbalanced groups at baseline; serious bias likely, therefore quality of evidence downgraded by two levels 6 Imprecise due to small number of participants (less than 300) therefore quality of evidence downgraded by one level 7 Some concerns with random sequence generation, allocation concealment and selective reporting; bias likely, therefore quality of evidence downgraded by one level 8 Some concerns with blinding of outcome assessment, selective reporting and groups not receiving comparable care; bias likely, therefore quality of evidence downgraded by one level 9 Imprecise due to very small number of participants therefore quality of evidence downgraded by two levels | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 All‐cause mortality Show forest plot | 3 | 195 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.18, 5.67] |
| 2 Acute myocardial infarction (AMI) Show forest plot | 3 | 254 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.07, 1.63] |
| 3 Revascularisation procedure (CABG or PCI) Show forest plot | 3 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.11, 0.64] |
| 4 Exercise capacity Show forest plot | 5 | 267 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.45 [0.20, 0.70] |
| 5 Cardiovascular‐related hospital admissions Show forest plot | 1 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.10] |

