Interventions for improving adults' use of primary oral health care services
Abstract
This is a protocol for a Cochrane Review (Intervention). The objectives are as follows:
To assess the effectiveness of interventions aimed at improving adults’ use of primary dental care services in order to improve their oral health and quality of life.
Background
Primary health care includes all services provided on a first contact basis by individuals or teams to maintain good health or to restore health where a breakdown has occurred (Loupe 1978). In high‐income countries most dental services are delivered as primary care in community settings, and involve relatively simple procedures provided by 'generalists'; who in the main have, or aspire to have, a long‐term relationship with their patients (Morris 2001). Patients' care is usually the responsibility of a general dental practitioner, although a wider dental team are often involved in delivering aspects of their care (Dyer 2014).
In low‐income countries services are often limited by workforce capacity. For example, in Africa the dentist to population ratio is approximately 1:150,000 compared to about 1:2,000 in most industrialised countries (WHO 2015). Consequently care provided by dentists is mostly confined to regional or central hospitals in urban areas (WHO 2015). Often wider primary dental care programmes exist which seek to provide scientifically sound but technologically appropriate and affordable, community‐based care according to the principles of a Primary Health Care Approach (WHO 1978). An example of this is the Basic Package of Oral Care (BPOC) programme which has three components: urgent care, affordable fluoride toothpaste and atraumatic restorative treatment (ART) (Frencken 2002). These programmes aim to widen the accessibility of both preventive and curative care whilst taking into account challenging environmental conditions and limited resources. Delivery of community‐based dental health programmes in low‐income countries, particularly in rural areas, may involve community health workers trained to provide dental examinations, preventive advice and urgent care for the relief of pain (Davis 1991).
This primary healthcare model is not restricted to low‐income countries ‐ outreach programmes for underserved groups in high‐income countries may follow the same model: such as the use of nursing and dental students in the USA to provide onsite dental examinations, education, urgent and comprehensive dental health care for inner‐city homeless adults (Lashley 2008). Thus, primary dental care services are defined as first contact, community‐based healthcare services, largely, but not exclusively delivered in general dental practice. These services can be concerned not just with dental (tooth‐related) problems, but with disorders/diseases related to the mouth in general, for example detection of oral cancer affecting the cheek etc.
Problems with the availability, affordability and acceptability of primary dental care services may limit access (Harris 2013; Penchansky 1981). Another reason for under‐utilisation is a lack of perceived need (Blaikie 1979). Access can be compromised at many levels (see Figure 1). Firstly, at the micro‐level (the individual or psychological level) ‐ dental anxiety, self‐identity (e.g. a low self‐esteem), self‐regulation (e.g. self‐efficacy), social competence, sense of coherence and coping, thought suppression, self‐evaluation of oral health and perceived susceptibility to poor oral health, seriousness and care efficacy ‐ can all influence care‐seeking barriers (Harris 2017). Secondly, at the meso‐level (social processes and community structures) ‐ social support and engagement, transport availability, and the volume, format and range of information about dental health and availability of services ‐ are potentially limiting factors, contributing to societal definitions of dental health, potential distrust of services, and an individual's willingness and ability to seek dental health care (Harris 2017).
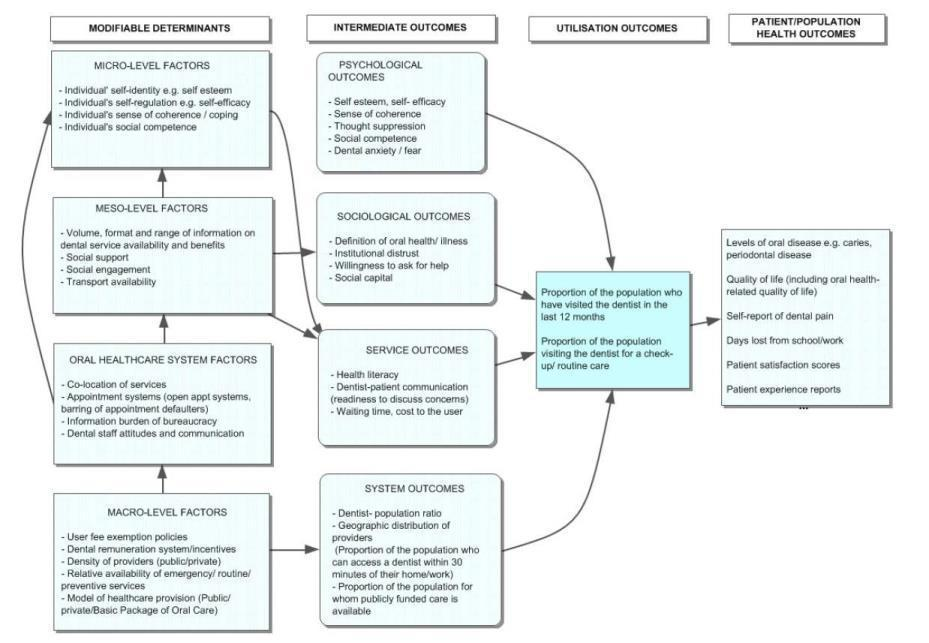
Logic model outlining multi‐level factors that influence the utilisation of primary oral health care services, and health outcomes that may result
Thirdly, at the macro‐level (over‐arching population‐wide structures and policies), a range of factors limit access. Dentistry is distinct from other health services in many countries because patient co‐payment (user‐fees) are a feature of services, with the balance between public and private sector provision an important consideration; generally because of low prioritisation. Macro‐level policies on user‐fees are important not just in high‐income countries (Ikenwilo 2013), but in low and middle‐income countries too (Lagarde 2011; Nyamuryekung'e 2015). Policies on provider incentives which stimulate location in underserved areas, and provision of services for high‐need low‐income groups, influence service availability (Whittaker 2012). Lastly, factors at the service level influence access. Information and appointment systems place bureaucratic and health literacy demands on patients which may be overwhelming, particularly for people from low socioeconomic status (SES) backgrounds (Rudd 2012). Insensitive and culturally inappropriate communication by providers, as well personal and professional attitudes that stereotype the oral health values and treatment preferences of low SES patients, influence not only patients' immediate experience of dental care, but their future pattern of dental visiting too (Freeman 2002).
Although there is evidence children's use of dental services is correlated with that of their parents, their are additional factors, especially in adolescents, which influence children's visiting behaviour (Attwood 1993). So while mothers' attitudes and beliefs about dental care are major determinants of whether she takes her child to the dentist (Milgrom 1998), the relationship is relatively unclear and authors conclude that the area needs to be explored further (Wigen 2009). Consequently, the review is limited to adults' use of dental services. In any case, other Cochrane Reviews on school‐based programmes to improve oral health have been undertaken or are under production (Arora 2017; Cooper 2013). A separate Cochrane Review limited to interventions with pregnant women and new mothers for preventing caries in children, is also underway (Riggs 2016).
Access to primary dental care contributes to the improvement of oral health through early diagnosis, advice, clinical prevention and treatment of conditions such as dental caries, periodontal disease and oral cancer (WHO 2015). Dental check‐ups allow oral diseases to be identified at an early stage, giving an opportunity for early intervention. In the case of dental caries, if care is delayed until symptoms occur, demineralisation can be so advanced that extraction rather than tooth restoration may be the only treatment option available. Evidence from a number of studies shows that people who visit a dentist regularly have better oral health outcomes, even after controlling for SES (McGrath 2001; Petersen 2004; Saunders 2004). A cohort study from New Zealand even shows that after controlling for SES and oral hygiene, adults who are regular dental visitors have better oral health at any given age, with the association strongest, the longer routine dental visiting is maintained (Thomson 2010). Since uptake of dental examinations (check‐ups) is a key indicator of future oral health problems (Newhouse 1993), promoting dental visits for check‐ups is a common modern strategy in preventive dental care (Davenport 2003; Locker 2001).
Description of the condition
Major oral diseases (untreated dental caries, severe periodontitis and severe tooth loss) affect 3.9 billion people worldwide (Marcenes 2013). In the 2010 Global Burden of Disease study, untreated dental caries in permanent teeth was the most prevalent disease identified in the entire study (a global prevalence of 35% for all ages combined). The experience of pain, problems with eating, chewing, smiling and communication due to missing, discoloured or damaged teeth have a major impact on people’s daily lives and well‐being (Matthias 1995). Moreover, oral diseases restrict activities at school, at work and at home causing millions of school and work hours to be lost each year throughout the world (Petersen 2005). In addition, oral diseases combine to account for 15 million disability‐adjusted life‐years (DALYs) globally (1.9% of all years lived with disability (YLDs); 0.6% of all DALYs), implying an average health loss of 224 years per 100,000 population (Marcenes 2013).
The measure most often used to indicate dental care service use is utilisation rate i.e. the proportion of the population who have visited the dentist in the last 12 months (Harris 2013). A study that compared the use of dental services in 21 OECD countries indicated that the annual probability of visiting a dentist varies markedly between countries, from between one‐third of the population in Southern Europe, to 60% to70% in Sweden and the UK, and around 80% in Denmark and the Netherlands (van Doorslaer 2004). In USA, this rate is around 42% of the adult civilian population who live in the community as opposed to institutions such as nursing homes (Christian 2013), whereas in some low and medium‐income countries, the annual probability of visiting the dentist is as low as 9% in Nigeria (Adegbembo 1994), and 23% in China (Lo 2001).
This basic measure of utilisation, however, only really captures initial utilisation, i.e. whether the individual or group makes contact with dental services for any type of care (urgent, therapeutic and or preventive). A further utilisation measure which captures ongoing engagement and care is also necessary, for example, whether the individual or group receive non‐urgent care, i.e. the reason for the last visit to the dentist (proportion of the population, by age group, visiting the dentist for a check‐up/routine/urgent care) (Harris 2013). Whilst 50% of Europeans report that the reason for their last dental visit was a check‐up, for 17%, the reason for their last visit was for urgent care (Eurobarometer 2010). However, this also varies significantly between countries. For example, 79% of people from the Netherlands, and 72% of people from the UK report that their last visit to a dentist was for a check‐up, compared to 20% of Bulgarians (Eurobarometer 2010). Moreover, as many as 40% of people in Bulgaria and Romania went to a dentist for urgent care last time they made a visit (Eurobarometer 2010).
In low‐income countries, the proportion of adults reporting their last dental visit was for a check‐up, is even lower: a study in Sri Lankan city shows only 10% of employed adults attended for a check‐up on their last visit (Ekanayake 2002). In low‐income countries, sometimes even when in pain, people do not use dental services, and instead may self‐medicate (Tapsoba 2006). For example, a survey of adults in the capital city of Burkina Faso, which is fairly typical of many major towns in sub‐Saharan Africa, found that of those who reported experiencing an oral health problem during the past 12 months (62% of these involved pain or acute discomfort affecting daily life), just 28% used dental services (Varenne 2006). The remainder of those who had experienced an oral health problem, used self‐medication with either modern or traditional medicine (48%) or sought no treatment at all (24%).
Description of the intervention
This Cochrane Review will include any intervention that aims to increase the proportion of the population using dental services. These might be delivered in clinical settings, for example to people using urgent dental care services, or in a wider public health context for example by contacting people in the street, or via social media. Of particular interest will be interventions that lead to higher proportions using services for ‘routine check‐ups’ (either with or without diagnostic radiographs) and preventive care, with a particular focus on SES inequalities associated with these interventions. Preventive care here includes non‐invasive primary or secondary prevention such as the giving of health education advice, the application of fluoride varnish or fissure sealants, and routine prophylactic care for periodontal disease such as scaling and polishing. The ‘routine check‐up’ is defined as a "clinical examination, advice, charting and report" (NHS Executive 2002). Although another Cochrane Review concludes there is a lack of evidence relating to the risks and benefits of altering the length of the recall period between check‐ups, it nevertheless recognised that a dental check‐up is valuable in detecting early signs and symptoms of early disease, including oral cancer (Brocklehurst 2013; Riley 2013).
With a shift towards a preventive philosophy of dental care, a minimal intervention approach is taken in the hope that early cavities will re‐mineralise before a filling is needed (Christian 2015). Conservation of teeth with fillings, crowns and root canal treatment is also preferred over extraction. However a possible harmful effect of increasing the utilisation of dental services is that dentists may intervene with restorations or extractions earlier than the patient would have experienced otherwise, and so we will include in the review, consideration of reductions in oral health associated with supplier‐induced demand (SID). In dentistry evidence suggests that patients’ recall by dentists for check‐ups involves inducement (Grytten 1991; Sintonen 1995).
Following the logic model based on a synthesis of theory (Figure 1) (see the 'How the intervention might work' section), we identified a range of possible interventions and intermediate outcomes (Figure 2). In Figure 2, types of interventions to improve adults use of primary dental care services are depicted in boxes; with linkages given to main intermediate outcomes (circles), and through these to the primary outcome of access to primary dental care. Figure 2 also sets out the interventions in four quadrants (micro‐level, meso‐level, service‐level, macro‐level), allowing for linkages between interventions.
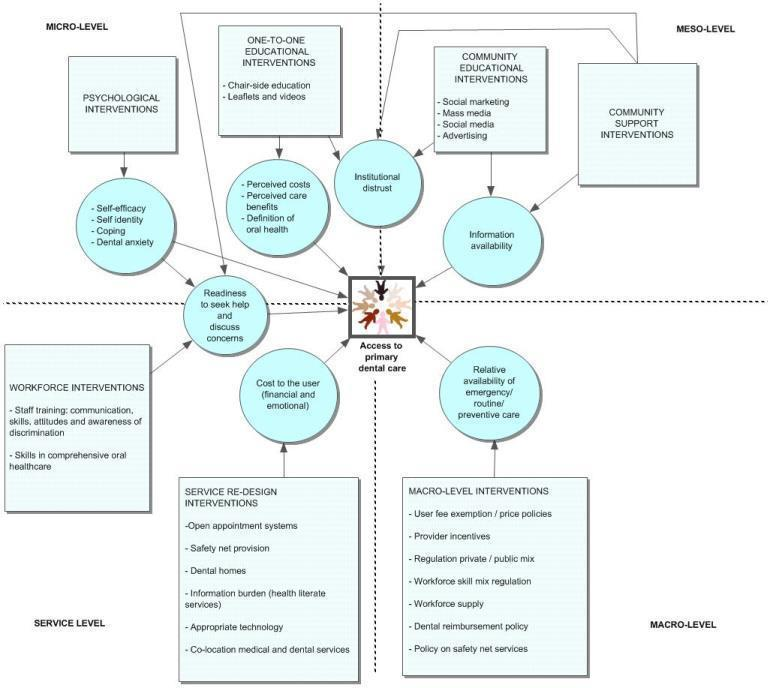
Intervention types (squares) positioned at the system, micro, meso and macro level, with intermediate outcomes (circles)
Within each of the four levels, there may be several types of interventions and mixed interventions. The following outlines the main types of interventions with respect to each level, although the list of intervention type will not be limited to these subgroups or examples.
Micro‐level (interventions targeted to individual users or non‐users of services)
-
Psychological interventions: for example, targeting self‐efficacy, sense of coherence, coping, self‐identity, dental anxiety. These include any interventions designed on the basis of psychological models to change behaviour, such as a Dutch study based on Ajzen & Fisbein's Theory of Reasoned Action (ter Horst 1985).
-
Educational interventions: for example, chairside education, leaflets or videos, targeting perceived care efficacy, costs and benefits of care, perceived availability, definition of oral health, susceptibility to oral disease, institutional distrust. An example is the mailing of postcards to targeted individuals with a message about care availability (Dela Cruz 2012).
Meso‐level
-
Community education: for example, advertising, social marketing, health promotion displays in public places, mass media, social media.
-
Community support: for example, community advocates to support care users.
Service‐level
-
Service design: for example, appointment systems, reducing information burden and bureaucracy associated with accessing care, signage, co‐location of dental with medical services, virtual dental homes, use of appropriate technology and materials in outreach programmes, local organisation of safety net services.
-
Workforce training: for example, dental team communication skills and awareness raising in providing for diverse patients' needs, skills in providing comprehensive primary dental care, training of community health workers to deliver Basic Package of Oral Care or similar, use of dental students to provide community programmes.
Macro‐level
-
User fee and price policies.
-
Provider incentives to locate in underserved areas and to provide care for low SES groups; remuneration for providers of safety net services.
-
Regulation of public/private sector dental care provision.
-
Workforce regulation including the use of dental auxiliaries and community health workers.
-
Policies on workforce supply and their geographic distribution.
-
Dental reimbursement policies.
-
Policy on safety net services.
Multi‐level interventions
-
Interventions which have multiple components and involve multiple levels will be grouped separately; for example, studies involving both patient education (micro‐level) and appointment scheduling (service level) (Cibulka 2011).
How the intervention might work
Logic models offer a framework to help systematic reviewers think conceptually when faced with a diverse range of outcomes and potential effect mediators and moderators (Baxter 2010). They can also direct the review process itself by giving a tool with which to narrow the scope of the review, identify the most relevant inclusion criteria and draw out policy‐relevant conclusions when interpreting results (Anderson 2011). Drawing from a systematic review of theory explaining socioeconomic inequalities in the preventive use of dental services (Harris 2017), and adapting this to the objectives of this review, we constructed a logic model (Figure 1).
Logic models portray the logical reasoning that connects intervention programme inputs to intended outcomes (Whitehead 2007). Our logic model identifies different levels where interventions might be positioned: the micro‐level, the meso‐level and the macro‐level. There are linkages between the various levels as well as feedback loops (for example, improving dentist‐patient communication can reduce the coping burden at the individual level). This recognises that the processes involved in using dental services are not linear, but dynamic and recursive (Harris 2017), and so our approach is therefore preferable than using a more linear model, based on the conceptualisation of a series of barriers/enablers of service utilisation (Penchansky 1981). The approach also allows for the design of multiple level, linked strategies to improve access to primary dental care services (Comino 2012).
The logic model suggests that several sets of interventions may be effective, since they aim to influence multiple factors influencing primary dental care service usage.
Why it is important to do this review
Against a background of growing privatisation in Europe (Maarse 2006), rising numbers of people find private care unaffordable. In many countries some degree of patient co‐payment for dental care is involved, even in public service facilities. A study of the public dental service in Tanzania quantified costs of using dental services in terms of out‐of‐pocket payment by patients as a proportion of the average daily resources required for basic living (DRC) (Nyamuryekung'e 2015). They found that tooth extractions cost patients an average of four times their DRC and restorations nearly ten times their DRC (Nyamuryekung'e 2015). In some Eastern European countries third‐party payment systems have been introduced, with no priority placed on preventive care (WHO 2012).
Although numerous studies document sociodemographic differences and predictors of the use of dental services in various populations (Christian 2013; Pavi 1995), and several narrative reviews summarising barriers and facilitators to the regular use of dental services exist (Freeman 1999), there are no systematic reviews of interventions aiming to increase the uptake of dental care in the literature. A recent systematic review and synthesis of theory explaining how inequalities in dental service utilisation identifies that a multi‐level perspective is necessary to capture the various active ingredients and synergies between multi‐component interventions in this complex area (Harris 2017). A systematic review of interventions to enhance access more widely in primary health care generally, confirms that many levels (individual users and providers of services, communities, and health services and systems) all influence outcomes, and that multiple, linked strategies targeting different levels of the healthcare system are needed (Comino 2012).
Inequalities in oral health are observed to be widening in some industrialised countries (Bernabé 2014). A SES gradient is observed in preventive dental visiting, and evidence points to this contributing at least in part to inequalities in oral health (lower SES groups have poorer oral health in parallel with their social position (Saunders 2004). Although the extent of the service contribution has yet to be quantified, international modelling data from the health sector in general suggests that health care provision may contribute to up to 25% of education‐related inequalities in health outcomes (Booske 2010). Interventions that promote the regular utilisation of dental services are therefore an important means through which inequalities may be addressed, and complementary to population‐wide efforts to promote oral health.
With some well‐meaning interventions aimed at improving access to health care actually shown to increase inequalities (Chapman 2004), an assessment of the impact of any interventions on inequalities in service use is important. For example: walk‐in centres have been found to attract largely white, middle‐class patients with minor or self‐limiting complaints (Schiff 1992). Users of telephone call lines, such as NHS Direct, also appear to be the same people who readily make use of pre‐existing health services, that is the white, healthy, middle‐class (Chapman 2004). This type of unintended consequence can be considered to be an opportunity cost harms (Lorenc 2013), and as such, this Cochrane Review has the potential to influence public health policy decisions on funding public health interventions in this area, if such adverse effects are identified.
Objectives
To assess the effectiveness of interventions aimed at improving adults’ use of primary dental care services in order to improve their oral health and quality of life.
Methods
Criteria for considering studies for this review
Types of studies
We will include a variety of study designs based on the criteria outlined by the Cochrane Effective Practice and Organisation of Care (EPOC) Group (EPOC 2013).
-
Randomised controlled trials (RCTs), including cluster‐RCTs: any experimental design where adults are allocated to an interventions to improve their use of dental services; or where groups of people (e.g. dental care providers), communities or areas are randomised to receive such interventions, with outcomes measured at the population level, and where both baseline and follow up primary outcome data is available. For cluster‐RCTs we will only include studies with at least two intervention sites and two comparator sites.
-
Quasi‐RCTs with either individual or cluster randomisation: we will include studies with at least two intervention sites and two comparator sites where both baseline and follow‐up primary outcome data is available.
-
Non‐randomised controlled trials (NRTs): these are experimental studies in which people are allocated to intervention/control groups using methods that are not random. We will only include studies with at least two intervention sites and two comparator sites and where both baseline and follow up primary outcome data is available.
-
Controlled before‐and‐after studies (CBAs) – i.e. studies where observations are made before and after implementation of an intervention, both in a group which receives the intervention and in a control group which does not. These are distinguishable from NRTs since CBAs are controlled observation studies where allocation to groups occurs naturally, whereas in NRTs participants are deliberately allocated experimentally by authors/collaborators. We will include these studies provided the timing of the period of the study in both the intervention and comparator are comparable and pre‐ and post‐intervention periods of measurement of both groups are the same; and where there is at least two control and two intervention sites. We will compare both groups for key characteristics.
-
Interrupted time series (ITS): according to Cochrane EPOC guidelines these studies must use multiple time points before and after the intervention so that the intervention effect can be compared with the pre‐intervention trend. To be included, ITS studies must have a clearly defined point in time when the intervention occurred; and there should be three data points before and three data points after the intervention.
If the same outcome data are presented in more than one paper, we will include the paper with the most data in the review. Where study authors report on different outcomes or use different analytical methods across different publications on the same population, we will report these additional data.
Types of participants
Adults (aged ≥ 18 years) who have the potential to use primary dental care services for non‐urgent care. We will include adults from high‐, middle‐ and low‐income countries.
We will exclude studies that include participants with medical conditions that influence their oral health needs or the way care is provided. Examples are adults with learning disabilities, people living with HIV/AIDS, and the physically disabled. We will also exclude studies that involve the provision of services specifically for people identified as dentally anxious and needing specialist dental care as a result.
Types of interventions
Intervention
We will include interventions that aim to increase the proportion of the population using dental services for check‐ups and preventive visits, as well as interventions which aim to widen the availability, uptake and accessibility of all forms of non‐urgent primary dental care services by adults. For both types of interventions we will assess health equity impacts. We will include services provided by both the public and the private sector. We will include interventions targeted at carers who facilitate the uptake of services for other adults, but will limit this to interventions where the outcomes are measures of adult utilisation and oral health. We will exclude interventions which aim to change the use of services by children. In the case of studies that report data on both children and adults, we will exclude studies if we cannot separate data on adults' service use.
We will include interventions targeted at the micro‐level, meso‐level, service‐level or macro‐level, as outlined in Figure 1 and Figure 2, as well as multi‐level, multi‐strategy interventions. Micro‐level interventions will be individual or group interventions. Whilst meso‐, service‐ or macro‐level interventions may target dental practitioners, communities or populations, the outcome measure will be utilisation rate of service users at a group, community or population level.
We will exclude service use of specialist dental services, such as orthodontics, oral surgery (secondary or tertiary care).
No minimum time period of intervention will be applied.
Comparison
Interventions may be compared with no intervention or usual care; or an alternative intervention also aimed at improving dental service use.
Types of outcome measures
Potential outcomes are outlined in the logic model Figure 1, but will not be confined to these measures in the review. We will not exclude studies based on the absence of reported primary outcomes or secondary outcomes alone. The minimum follow‐up period for interventions will be four weeks.
Primary outcomes
Dental service use as measured by proportion of the population who:
-
attend primary dental care services for non‐urgent care (Non‐urgent care will include: check‐ups, preventive or routine care);
-
attend primary dental services for urgent dental care;
-
do not attend primary dental care services for any type of care.
Secondary outcomes
We have grouped secondary outcomes according to: clinical dental outcome measures; patient self‐report measures; other measures; and any adverse effects.
Clinical outcome measures
-
Proportion of decayed teeth that are untreated.
-
Number of sound (not decayed or treated) teeth.
-
Number of decayed, missing and filled teeth.
-
Number of teeth/proportion of people with oral sepsis.
-
Proportion of people with a Basic Periodontal Examination greater than a score of two.
-
Proportion of people with periodontal sites that bleed on probing.
-
Community Periodontal Index of Treatment Need(CPITN), plaque scores.
-
Oral cancer and pre‐malignant disease diagnosis.
Patient self‐report measures
-
Pain.
-
Oral health‐related quality of life (OHQoL) impacts and OHQoL components, such as function (e.g. eating, aesthetics).
-
General health‐related quality of life measured by EQ‐5D‐5L (EuroQol) or similar.
-
Dental anxiety.
-
Knowledge and attitudes of patients/the public relating to oral health and disease.
-
Psychological measures such as patients’ self‐efficacy, coping.
-
Measures of patient social capital including social engagement.
Other measures
-
Resource use from the consumer viewpoint: patient or carer’s time spent attending the dentist, transportation costs to services.
-
Cost of intervention.
-
Waiting time for appointments.
-
Health literacy of the consumer.
-
Healthcare provider job satisfaction and job stress.
-
Community social capital.
-
Preventive use of non‐dental health care services.
Any adverse effects
We will report any adverse effects, such as a reduction in the number of sound (untreated) teeth (indication of supplier induced demand); any widening of SES differences in oral health and dental service utilisation; and any increase in healthcare provider workload, job stress or reduction in job satisfaction.
Search methods for identification of studies
The review will use a sensitive search strategy for electronic bibliographic databases, bibliographies of included articles and grey literature sources. We will conduct forward and backward citation searching and will also contact authors of included papers to identify additional published and unpublished references.
We will conduct the search without language restrictions and limit this to publications from 1990 up to the present. Findings from publications before 1990 may be out of date in the changing environment of primary dental care systems.
Electronic searches
We will use Boolean operators and Medical Subject Headings (MeSH) through the following databases.
-
Cochrane Central Register of Studies (CENTRAL).
-
Cochrane Oral Health Specialised Trials Register.
-
Ovid MEDLINE.
-
Embase.
-
CINAHL (EBSCO).
-
PsycINFO.
-
ASSIA.
-
LILACs.
-
Scopus.
-
3ie Impact evaluation database.
The search strategy draft is in Appendix 1. The search strategy is based on one MeSH context (e.g. dental/oral) search term AND one intervention search term (e.g. removal/introduction of patients’ charges) AND one primary outcome search term (e.g. utilisation, attendance). We will specifically design the search depending on the database requirements. No age group or study design filters will be applied. An example of the search strategy and terms for MEDLINE is presented in Appendix 2. We will adapt the MEDLINE search strategy for other databases and translate the MeSH terms to the controlled vocabularies as appropriate. We will apply shorter, less complex strategies to open access databases since these do not usually support complex Boolean or other operators.
Searching other resources
We will search the World Health Organization (WHO) International Clinical Trials Registry Platform Search Portal (ICTRP) (http://apps.who.int/trialsearch/)
Also we will check the following grey literature or combined sources (grey literature and academic literature) databases.
-
Grey literature report (www.greylit.org/library/search).
-
ProQuest Dissertations & Theses Global.
-
Conference proceedings of the International Association for Dental Research (IADR).
In addition, we will perform a targeted keyword search (term ‐ “dental visiting”) of the WHO website (www.who.int/en/).
We will check the reference lists of included papers for further relevant studies.
Handsearching
We will only include handsearching that is done as part of the Cochrane worldwide handsearching programme and uploaded to CENTRAL.
Data collection and analysis
Selection of studies
We will download all the titles and abstracts identified through electronic searching to a reference manager database. We will then remove duplicate references, and number the remaining references.
Two review authors (HR and BC) will independently screen the titles and abstracts to identify potentially eligible studies. HR and BC will assess and subsequently compare an initial sample of 30 titles and abstracts for inclusion consensus (i.e. inter‐reviewer reliability). We will resolve discrepancies through discussion or, if required, with a third review author (CO). In addition, 10% of titles and abstracts screened by each review author will be re‐scored (with blinding) to review extent of intra‐reviewer reliability. We will not report reviewer reliability statistics (e.g. Kappa values) because an arbitrary Kappa cut‐off point is unlikely to convey the impact on any real disagreements on the review. Rather, we will use the reliability data to indicate where a revisiting of eligibility criteria or data collection coding is needed, and will report any changes that result. We will obtain full‐text articles of all potentially eligible studies to assess using the pre‐specified eligibility criteria. If there is ambiguity we will seek clarification from the publication authors and re‐assess the articles. We will list all studies excluded after full‐text assessment and the reasons for exclusion in a ‘Characteristics of excluded studies’ table. We will illustrate the study selection process in a PRISMA diagram.
Data extraction and management
If a single publication reports two or more studies, we will extract data from the each study separately. If the findings from a single study is spread across more than one publication, we will count the study as one and extract the data as one publication. For studies with more than one intervention comparator, we will extract the results for each intervention arm.
Two review authors (HR and LB) will independently extract data from the studies using a detailed data extraction form. We will resolve any discrepancies through discussion, or if necessary by consulting a third review author (BC). We will extract the following study information.
-
Study details: citation, start and end dates, location, study design, unit of randomisation, unit of analysis, country and important contextual details about the health system.
-
Participant details: study population eligibility (inclusion and exclusion) criteria, ages, population size, and attrition rate.
-
Details about the interventions: by level (micro‐, meso‐, service‐ and macro‐level), and type of intervention as outlined in the bulleted lists of Figure 2. For each intervention we will extract information (where available) on the following:
-
format of the intervention (e.g. if an educational intervention at the micro‐level, leaflets, video, on‐to‐one discussion etc);
-
any theoretical model underpinning the intervention;
-
personnel delivering the intervention;
-
time taken to deliver the intervention, length of intervention period, length of follow‐up;
-
primary outcome and all secondary outcomes available.
-
For each dichotomous outcome, we will extract information on the number of participants using dental services and the number of participants in each case group. For each continuous outcome we will extract the means or geometric means and standard deviations (SDs) (or information to estimate the SDs) for each case group together with the numbers of participants in each group.
We will also extract medians and ranges if these are reported in place of means and SDs. We will contact the authors of the primary studies for any unclear or missing data.
Assessment of risk of bias in included studies
Two review authors (HR and BC) will independently assess risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We will resolve any differences in opinion through discussion or, if necessary, by consulting a third review author (RH). We will present our 'Risk of bias' assessments will be presented in study information tables and also in a 'Risk of bias' summary and 'Risk of bias' graph.
For RCTs and NRS conducted prospectively we will assess the risk of bias according to the following domains.
-
Random sequence generation.
-
Allocation concealment.
-
Blinding of participants and personnel.
-
Blinding of outcome assessment.
-
Incomplete outcome data.
-
Selective outcome reporting.
-
Baseline outcomes measurement.
-
Baseline characteristics.
-
Other bias e.g. use of validated outcome measures; intention‐to‐treat analysis; final outcome controlled for baseline behaviour; statistical analyses used to account for clustering in cluster‐RCTs.
For interrupted time‐series studies, we will assess the risk of bias for the following.
-
Intervention independence from other changes.
-
Prespecification of intervention effect.
-
Influence of intervention on data collection.
-
Blinding of outcome assessors.
-
Incomplete outcome data.
-
Selective outcome reporting.
-
Appropriateness of analysis including adjusting of estimates of intervention effects.
-
Other risks of bias e.g. seasonality; consideration of changes in secular trends; use of standardised protocols; comparability of groups
Measures of treatment effect
For dichotomous data, we will use risk ratios (RR) to measure treatment effect. We will present continuous data as mean differences (MDs) with 95% confidence intervals (CIs), calculated from the mean change (and the SD) between intervention and control groups. We will present risk ratios and mean differences with 95% CIs. We will report medians and ranges in table format only.
Unit of analysis issues
Cluster‐RCTs
If findings are reported at the individual level, we will report the method used to take account of clustering. In case the clustering effect was not taken into account, we will adjust the sample size to allow for comparison with a sample of individuals. When possible we will calculate the intracluster correlation coefficient (ICC) as described by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Multiple time points
We will group outcomes measured at similar points or at similar age points, when outcomes are measured on participants at multiple time points, and we will use the average effect size to avoid dependence problems. We will use a single measure that is closest to a one year follow‐up when a primary outcome study reports multiple measures at different points in time.
Studies with multiple treatment arms
We will include multi‐armed trials in the analyses along with individually randomised trials. We will include the relevant intervention groups in a pair‐wise comparison of intervention groups. We will combine groups to created single pair‐wise comparison using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Dealing with missing data
We will not apply any imputation measures for missing data. We will attempt to contact the study authors if there is missing or unclear data. If we cannot obtain this data, we will note this in the study’s data extraction form and in the ‘Risk of bias’ table.
Assessment of heterogeneity
We will limit pooling data to studies with similar study designs and types of interventions (see the 'Data synthesis' section). We will also assess clinical heterogeneity by exploring this between studies that include participants with a specific age range (e.g. elderly participants only); studies undertaken in different settings (e.g. considering differences between high‐, middle‐ and low‐income countries); and health systems with different remuneration arrangements. For studies that appear similar we will assess statistical heterogeneity by visually inspecting forest plots to detect overlapping CIs, applying the Chi² test (P value < 0.05 considered statistically significant), and also by using the I² statistic.
Assessment of reporting biases
If more than 10 studies within the same intervention category and assessing comparable outcomes in the same population meet the inclusion criteria, we will use funnel plots to assess the risk of reporting bias, and we will perform statistical tests of asymmetry, such as Begg and Egger’s tests (Sterne 2008).
Data synthesis
We will analyse data using Review Manager 5 (RevMan 5) software (RevMan 2014). We will undertake data synthesis on the two primary outcome measures where the type of intervention is similar, e.g. meso‐level, community education, advertising (at the level of the bullets within Figure 2). Where there is sufficient secondary outcome data, we will also synthesise these using the same approaches and principles as used for primary outcomes. We will first group comparisons according to the level of the intervention (e.g. meso‐level), and then according to the interventions within the level (i.e. community education).
Although we will not undertake an economic evaluation, we will summarise data on the implementation cost of the interventions since this might inform resource allocation.
For continuous data when outcomes are measured on different scales, we will use standardised mean differences (SMDs) when we combine data in the meta‐analysis. Due to the expected diversity of the interventions and outcomes it may not be possible to pool the results.
Where substantial methodological or statistical heterogeneity exists, we will not pool study results in a meta‐analysis. We will not pool results with different study designs, for example RCTs and NRTs. We will also be cautious about pooling any results from NRTs, recognising that in these types of study design there is a greater chance of confounding effect since study arms are not virtually similar at baseline due to randomisation. For meta‐analysis of dichotomous data we will use the Mantel‐Haenszel method. We will use a random‐effects model in the presence of moderate heterogeneity of treatment effects and a fixed‐effect model in the absence of heterogeneity.
We will perform a narrative synthesis of the results and will group our findings by the level of intervention type (micro‐, meso‐, macro‐, service‐ or multi‐level) and context (low‐, middle‐ and high‐income countries).
We will present the following outcomes in a 'Summary of findings' table for each of the following intervention groupings.
-
Proportion of the population attending primary dental care services for non‐urgent care.
-
Proportion of population visiting a dentist in the last 12 or 24 months for any reason.
-
Proportion of decayed teeth that are untreated.
-
SES differences in oral health and dental service utilisation.
-
Number of sound untreated teeth.
-
Self‐reported pain.
-
Oral health‐related quality of life.
-
General health‐related quality of life.
We will assess the quality of the evidence across each outcome measure using the GRADE approach. If feasible, we will use the computer software GRADEpro Guideline Development Tool (GDT) to prepare the ‘Summary of findings’ tables (GRADEpro GDT 2015). The quality rating across studies has four levels: high, moderate, low or very low. Randomised trials are categorised as high quality but can be downgraded; similarly, observational studies are categorised as low quality and may be downgraded or upgraded. We will assess the following five factors:
-
Limitations in the design and implementation of available studies suggesting high likelihood of bias.
-
Indirectness of evidence (indirect population, intervention, control, outcomes).
-
Unexplained heterogeneity or inconsistency of results (including problems with subgroup analysis).
-
Imprecision of result (wide CIs).
-
Probability of publication bias.
Subgroup analysis and investigation of heterogeneity
If statistical heterogeneity is present, we will attempt to further investigate potentially influential study characteristics by conducting subgroup analysis. We will undertake subgroup analyses with respect to the primary outcome.
-
Type of study design.
-
SES of participants.
-
Studies that take place in high‐income countries versus low‐ and middle‐income countries as defined by the World Bank (World Bank 2016).
-
Health system setting where participants are eligible/ineligible for free dental care.
Sensitivity analysis
We will perform a sensitivity analysis provided there are sufficient trials (i.e. two or more). We will conduct a sensitivity analysis for service utilisation by excluding studies that are either at unclear or high risk of bias for the five bias domains considered most important to this topic (e.g. selection, performance, detection, attrition and reporting bias).

Logic model outlining multi‐level factors that influence the utilisation of primary oral health care services, and health outcomes that may result

Intervention types (squares) positioned at the system, micro, meso and macro level, with intermediate outcomes (circles)

