Intervensi farmakologi untuk mencegah mulut kering dan disfungsi kelenjar air liur selepas radioterapi
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Location: Turkey Number of centres: 1 Date of enrolment: July 1996 to January 1997 | |
| Participants | Inclusion criteria: aged between 18 to 70 years. Histopathologic diagnosis of SCC of head and neck (nasopharynx, larynx, oropharynx, hypopharynx, oral cavity). WHO performance status 0 to 2. Patients to receive primary or postoperative radiation treatment for a minimum of 46 Gy totally and treatment fields to include at least the tail of parotis (1/3), submandibular glands and part of sublingual and minor salivary glands Exclusion criteria: patients with a histopathologic diagnosis other than SCC. Patients with an autoimmune disorder (e.g. Sjögren Syndrome) or diseases effecting saliva secretion. Difficulty in co‐operation for saliva collection, understanding the questionnaire and attending the follow‐up visits Age (years): pilocarpine: median 55 years, range 38 to 68 years; control: median 50 years, range 30 to 61 years Gender (M:F): pilocarpine 12:0; control 11:1 Cancer type: tumour location: pilocarpine: larynx = 8, nasopharynx = 2 and oral cavity = 2; control: larynx = 7, nasopharynx = 4 and oral cavity = 1 Radiotherapy: pilocarpine: mean dose = 60.2 Gy (range 48 to 70 Gy), number of fractions = 30.1 (mean), treatment time = 44.9 days (mean); control: mean dose = 63.8 Gy (range 50 to 70 Gy), number of fractions = 31.9 (mean), treatment time = 48.2 days (mean) Chemotherapy: none Number randomised: 24 (12 per group) Number evaluated: 24 (no dropouts, although not all participants available at all time points) | |
| Interventions | Pilocarpine versus no intervention Pilocarpine: 5 mg 3 times daily (4% solution) for 3 months from the beginning of RT Control: no treatment | |
| Outcomes | Xerostomia: subjective evaluation scores for xerostomia (0 = no symptoms, 11 = severe xerostomia). Questionnaire included 5 questions Salivary flow rates: unstimulated and stimulated whole saliva secretion (unstimulated saliva pH measurements also recorded) Adverse effects: no serious toxicity Survival data: not reported Other oral symptoms: not reported Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: before RT, during RT, end of RT and 3 months after start of RT | |
| Funding | None | |
| Trial registration | Not registered nor published | |
| Sample size calculation presented | Not included | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Not explicit in trial report. Comment from author: "randomisation was performed with block randomisation with stratification of treatment fields" |
| Allocation concealment (selection bias) | Low risk | Comment from author: "sealed envelope were used for concealing" |
| Blinding (performance bias and detection bias) | High risk | Pilocarpine versus no intervention. Blinding not possible |
| Blinding (performance bias and detection bias) | High risk | Not possible due to 'no intervention' group and subjective assessment of xerostomia |
| Incomplete outcome data (attrition bias) | Low risk | Comment from author: "no dropouts" Number of participants available for assessment varies by time point, however, those missing for assessment unlikely to influence results |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Greece Number of centres: 1 Date of enrolment: January 1997 to January 1998 | |
| Participants | Inclusion criteria: histologically proven squamous cell carcinoma of the head and neck. A primary tumour greater than or = T2N0M0, expected survival time greater than or = 12 months, no evidence of metastasis, and no prior chemotherapy or RT. Normal liver and kidney function, adequate bone marrow reserve, no current or previous history of cardiovascular disease and no active systemic infection Exclusion criteria: not reported Age (years): amifostine: mean 53.3 (SD 6.9); control: mean 60.3 (SD 5.5) Gender: amifostine: 13 M, 9 F; control: 16 M, 7 F Cancer type: tumour location: (amifostine/control) nasopharynx = 2/3, oral cavity = 9/11, larynx = 6/6 and oropharynx = 5/3. TNM classification: (amifostine/control) T2 = 6/6, T3 = 13/16, T4 = 3/1, N0 = 12/14 and N1 to 3 = 10/9 Radiotherapy: mean total dose = amifostine: 66.8 Gy (SD 3.2); control: 66.4 Gy (SD 3.4). Treatment duration: mean = amifostine: 49.6 (SD 4.5) days; control: 55.9 (SD 8.9) Chemotherapy: carboplatin (90 mg/m²), once a week before RT in both groups Number randomised: 50 (amifostine 25, control 25) Number evaluated: 45 (amifostine 22, control 23) | |
| Interventions | Amifostine versus no intervention Amifostine (300 mg/m2), IV 30 minutes before RT on days 1 to 5 of each week. Antimetic treatment administered IV before the amifostine | |
| Outcomes | Xerostomia: incidence of late xerostomia (RTOG grade 2 or more ‐ measured on a 0 to 4 scale) Salivary flow rates: not reported Adverse effects: haematologic toxicity, nausea, vomiting and transient hypotension Survival data: progression‐free survival at 18 months Other oral symptoms: incidence of grade 3 or greater acute mucositis and dysphagia Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: xerostomia: 3, 6, 9, 12 and 18 months after RT; haematologic toxicity and acute non‐haematological toxicities (mucositis and dysphagia): weekly for 7 weeks during RT, then 1, 2 and 3 months after RT | |
| Funding | Not reported | |
| Trial registration | Not registered | |
| Sample size calculation presented | Yes | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomized (1:1)" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | High risk | Amifostine versus no intervention. Blinding not possible |
| Blinding (performance bias and detection bias) | High risk | Not possible due to 'no intervention' group and subjective assessment of xerostomia |
| Incomplete outcome data (attrition bias) | Low risk | 45/50 participants evaluated (equal dropouts between groups). 3 participants dropped out of the amifostine arm. 2 denied further treatment (1 = week 2 and 1 = week 4) and 1 was lost to follow‐up. In the control arm, 1 participant died and 1 received palliative treatment because of disease progression |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: France Number of centres: 27 Date of enrolment: March 2001 to January 2006 | |
| Participants | Inclusion criteria: newly diagnosed head and neck, eligible for radiotherapy. Over 75% of both parotid glands in field. Performance status ≤ 2, no distant metastases, neutrophils ≥ 2000/uL, platelets ≥ 1000,000/uL, creatine < 130 umol/L, aminotransferases ≤ 3 x the upper limit of normal, and ≥ 18 years Exclusion criteria: use of pilocarpine during RT and concomitant CT, second‐line treatment, incomplete assessment of salivary gland function Age: intravenous: mean 55.2 range 34 to 78; subcutaneous: mean 56.1 range 36 to 76 Gender: intravenous: 127 M, 16F; subcutaneous: 124 M, 24 F Cancer type: newly diagnosed squamous cell carcinoma of the head and neck, at all stages, and nodal status Radiotherapy: at least 40 Gy of radiation delivered postoperatively Chemotherapy: induction chemotherapy in 42 patients no concurrent chemotherapy Number randomised: 291 (intravenous 143, subcutaneous 148) Number evaluated: 127 (intravenous 67, subcutaneous 60) for xerostomia at 1 year | |
| Interventions | Intravenous versus subcutaneous amifostine Intravenous: 200 mg/m² daily, administered over 3 minutes, 15 to 30 minutes before RT Subcutaneous: 500 mg at 2 sites, 20 to 60 minutes before RT | |
| Outcomes | Xerostomia: grade 2 or above (0 to 4 scale). Physician graded via RTOG before treatment, every 3 months for the 1st year and then every 6 months Salivary flow rates: unstimulated and stimulated saliva (mg/min) Adverse effects: nausea, vomiting, hypotension, skin rash, local pain at injection site, fever, asthenia Survival data: locoregional control, overall survival Other oral symptoms: dysgeusia (taste disturbance), dysphagia (difficulty in swallowing), dysphonia (difficulty in speaking) ‐ these 3 items were combined with the patients' sensation of mouth dryness and assessed using a patient benefit questionnaire (see QoL); grade 3+ acute mucositis Other oral signs: not reported Quality of life: patient benefit questionnaire Patient satisfaction: not reported Cost data: not reported | |
| Funding | Externally funded by pharmaceutical company; Schering‐Plough, France | |
| Trial registration | ||
| Sample size calculation presented | Yes | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Authors claim "randomly assigned". No further details given |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding (performance bias and detection bias) | High risk | "Lack of double‐blind". Patients could not really be considered to be blinded as administration of amifostine differed |
| Blinding (performance bias and detection bias) | High risk | Patient‐reported outcome see above |
| Incomplete outcome data (attrition bias) | High risk | Large loss to follow‐up. Attrition likely to be related to outcome |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Europe, Canada, USA Number of centres: 35 to 40 (unclear) Date of enrolment: October 1995 to October 1997 33% dropout rate at 12 months | |
| Participants | Inclusion criteria: patients with newly diagnosed, previously untreated squamous cell head and neck cancer. Inclusion of ≥ 75% of both parotid glands within radiation field and ≥ 40 Gy. Karnofsky Performance Status ≥ 60, granulocyte ≥ 2000 microL and platelet count ≥ 100,000 microL Exclusion criteria: patients with T1N0 or T2N0 carcinomas of the true vocal cords and tumours of the major or minor salivary glands or history of malignancy other than in situ cervix carcinoma within 5 years preceding diagnosis. Pregnant women Age: amifostine: 36 to 76, median = 55 years; control: 28 to 78, median = 56 years Gender: amifostine 123 M, 27 F; control 120 M, 33 F Cancer type: head and neck, various tumour sites, stages and node stages Radiotherapy: amifostine: definitive = 50, postoperative high risk = 70 and postoperative low risk = 28; control: definitive = 52, postoperative high risk = 65 and postoperative low risk = 36. 1.8 to 2.0 Gy , 5 days a week over 5 to 7 weeks for a total dose of 50 to 70 Gy Chemotherapy: none Number randomised: 315 randomised, but 12 never received any treatment (amifostine 150, control 153) Number evaluated: xerostomia at 12 months: 203 (amifostine 97, control 106), all included in analysis for locoregional control, all who received at least 1 dose of amifostine were assessed for toxicity | |
| Interventions | Amifostine versus no intervention Amifostine: (200 mg/m²) 3 minute intravenous 15‐30 minutes before RT | |
| Outcomes | Xerostomia: incidence of grade 2+ acute (within 90 days of the start of RT) and chronic xerostomia (0 to 4 scale) Salivary flow rates: unstimulated and stimulated saliva production ‐ reported as median quantity (g) of saliva and also as number of participants producing > 0.1 g in 5 min ("a clinically relevant volume") Adverse effects: nausea, vomiting, hypotension, allergic response Survival data: locoregional control, progression‐free survival and overall survival at 24 months Other oral symptoms: oral discomfort, dysgeusia (taste disturbance), dysphagia (difficulty in swallowing), dysphonia (difficulty in speaking) ‐ all included in patient benefit questionnaire (see QoL); grade 3+ acute mucositis Other oral signs: not reported Quality of life: patient benefit questionnaire (8 items each on a 10‐point scale where higher = better QoL) Patient satisfaction: not reported Cost data: not reported Timing of assessment: xerostomia: within 3 months of start of RT, then at 12, 18 and 24 months; salivary flow rates: 12, 18 and 24 months after start of RT; quality of life: 12 months after start of RT | |
| Funding | Source of funding: Medimmune Oncology | |
| Trial registration | Not registered | |
| Sample size calculation presented | Yes | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "dynamic allocation process" (recognised methods referenced) |
| Allocation concealment (selection bias) | Low risk | Quote: "determined by a phone call from the enrolling institution to the protocol sponsor (US Bioscience)" Comment: it appears to be central/remote allocation |
| Blinding (performance bias and detection bias) | High risk | Amifostine versus no intervention |
| Blinding (performance bias and detection bias) | High risk | Open‐label, no blinded outcome assessment |
| Incomplete outcome data (attrition bias) | High risk | 315 enrolled and randomised; 12 never received any treatment or follow‐up. Overall attrition 36% |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Australia, Canada, USA Number of centres: 22 Date of conduct: September 1999 to May 2001 | |
| Participants | Inclusion criteria: adults with newly diagnosed head and neck cancer. Patients with unknown primary and extensive neck disease also eligible. Karnofsky Performance Status > 60, haemoglobin > 10 g/dL, plus other similar criteria Exclusion criteria: prior head and neck radiation therapy, prior surgery for primary tumour beyond biopsy, prior chemotherapy, known allergy to Escherichia coli‐derived products, participation in another study within the previous 30 days, refusal to use adequate contraception during study, pregnant or breastfeeding Age: palifermin: mean 54 (range 25‐80); placebo: mean 56 (range 42‐75) Gender: palifermin 55 M, 12 F; placebo 27 M 5 F Cancer type: primary locations: oral cavity, oropharynx/nasopharynx, hypopharynx/larynx Radiotherapy: isocentric 4 to 6 MV photons either standard fractionation (once daily 2 Gy fractions 5 days/week: total primary tumour dose 70 Gy) or hyperfractionation (single 2 Gy fraction followed by a planned 1‐week treatment break. Then twice‐daily radiation: total dose of 72 Gy/6.5 weeks). Varied by centre Number randomised: 101 (69 palifermin, 32 placebo) Number evaluated: varies by outcome but 97 (65 palifermin, 32 placebo) analysed for our primary outcome of xerostomia | |
| Interventions | Palifermin versus placebo Palifermin: 60 µg/kg by IV bolus injection on study day 1 (Friday) before 1st week of CRT. Subsequent doses administered for 7 consecutive weeks, on each Friday after completion of weekly radiation treatment. 2 additional doses given on weeks 8 and 9 Placebo: as above Follow‐up: 5 weeks after end of RT | |
| Outcomes | Xerostomia: incidence of grade 2 xerostomia using NCI CTC scale Salivary flow rates: not reported Adverse effects: nausea, vomiting, fever, constipation, dehydration, granulocytopenia, fatigue, diarrhoea, insomnia, anaemia, dysaphia, cough, headache, weight decrease, dizziness, anxiety, hypomagnesaemia Survival data: survival, progression‐free survival (up to 75 months) Other oral symptoms: mucositis (primary outcome of study), dysphagia Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported | |
| Funding | Pharmaceutical trial (Amgen) | |
| Trial registration | Not registered | |
| Sample size calculation presented | Yes | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "double‐blind, randomized, placebo‐controlled study" |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind randomised placebo‐controlled study" |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind randomised placebo‐controlled study". However there is a subjective element to the index |
| Incomplete outcome data (attrition bias) | Low risk | Xerostomia data on 97 out of 101 enrolled. Quote: "3 patients in palifermin group and 1 in the placebo group discontinued study treatment with adverse events not considered related to study treatment". Comment: unclear if 3 of these were missing for xerostomia |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Europe, USA Number of centres: 18 (15 Europe, 3 USA) Date of recruitment: October 1996 to October 1998 | |
| Participants | Inclusion criteria: at least 18 years of age scheduled for definitive or adjuvant chemoradiotherapy for histologically confirmed squamous cell carcinoma of the head and neck. Postsurgery the surgical wound must be healed but no later that 12 weeks after surgery. Inclusion of at least 75% of each parotid gland within radiation field. Life expectancy 12+ months, Karnofsky Performance Status 60+, adequate function of bone marrow, kidneys and the liver Exclusion criteria: evidence of distant metastatic disease, primary lesion of the parotid gland, or a history of prior malignancy within the past 5 years (other than non‐melanomatous skin cancers that are controlled or carcinoma in situ of the cervix). Scheduled to receive hyperfractionated or accelerated radiotherapy, previously treated with chemotherapy or other investigational therapies within 4 weeks of study entry. Pregnant women Age: amifostine: median 57 (range 29‐73); placebo: median 58 (range 23‐78) Gender: amifostine 54 M, 13 F; placebo 57 M, 8 F Cancer type: head and neck cancer, various primary sites and stages Radiotherapy: standard fractionation (1.8‐2.0 Gy per day, 5 days a week) over 6 to 7 weeks for a total dose of 60 to 70 Gy Chemotherapy: carboplatin 70 mg/m² IV over 30 minutes after amifostine and 30 minutes before RT Number enrolled: 132 Number randomised: 132 Number evaluated: 132 (ITT analysis) (67 amifostine; 65 placebo) | |
| Interventions | Amifostine versus placebo Amifostine: 300 mg/m² IV over 3 minutes (days 1‐5 and 21‐25 of treatment); 200 mg/m² IV over 3 minutes (days 6‐20 and 26‐30/35) | |
| Outcomes | Xerostomia: RTOG acute and late radiation morbidity scoring criteria; incidence of grade 2 or higher acute or late xerostomia (0 to 4 scale) Salivary flow rates: stimulated and unstimulated saliva measurements (not assessed as less than a 3rd of participants had salivary function at 1 year) Adverse effects: nausea, vomiting, allergic response, asthenia Survival data: locoregional failure rate, progression‐free survival and overall survival Other oral symptoms: RTOG acute and late radiation morbidity scoring criteria: grade 3 or higher acute mucositis Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: acute xerostomia and mucositis measured up to 90 days after start of RT; late xerostomia measured up to 12 months after start of RT | |
| Funding | Source of funding: MedImmune Oncology Inc grant | |
| Trial registration | Not registered | |
| Sample size calculation presented | Yes | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Assumed. Described as "dynamic allocation scheme", similar method to Brizel 2000 |
| Allocation concealment (selection bias) | Low risk | Fax of baseline data sent to central telephone number for randomisation number. Randomisation number identical to blinded drug container held at pharmacy |
| Blinding (performance bias and detection bias) | Low risk | Amifostine versus placebo |
| Blinding (performance bias and detection bias) | Low risk | Information provided by author: "blinded drug containers were kept at the pharmacy, treating physicians had no information about the randomization until the end of the follow‐up period" |
| Incomplete outcome data (attrition bias) | Low risk | Analyses carried out an ITT basis. Dropouts = 30 (23% dropout rate). Amifostine group = 21 (1 ‐ never treated, 16 ‐ toxicity, 1 ‐ patient request, 1 ‐ death, 2 ‐ other illness). Placebo group = 10 (1 ‐ never treated, 4 ‐ toxicity, 1 ‐ patient request, 1 ‐ death, 1 ‐ disease progression, 2 ‐ non‐compliance) |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: the Netherlands Number of centres: 2 Date of enrolment: April 1999 ‐ October 2003 | |
| Participants | Inclusion criteria: biopsy confirmed HNSCC, initial 5% (wt/vol) citric acid‐stimulated parotid salivary flow > 0.1 mL/min Exclusion criteria: previous irradiation and/or previous or concurrent chemotherapy, patients with salivary gland tumours, severe cardiovascular disease or chronic obstructive pulmonary disease, pregnant women Age: pilocarpine: 18‐60 years 50 participants, > 60 years 35 participants; placebo: 18‐60 years 42 participants, > 60 years 42 participants Gender (M:F): pilocarpine 22:63; placebo 13:71 Cancer type: oral cavity (17%), oropharynx (18%), larynx (51%), hypopharynx (7%), nasopharynx (4%), unknown primary (1%) (equally distributed across groups) Radiotherapy: clinical target volume of initial field encompassed the primary tumour site with 1.5 cm margin, neck node levels in which pathologic nodes were found and elective node areas on both sides. Conventional fractionation schedule. Received at least 40 Gy in daily 2 Gy fractions Chemotherapy: none Number randomised: 170 (85 per group) Number evaluated: 113 (pilocarpine 55, placebo 58) | |
| Interventions | Pilocarpine versus placebo Pilocarpine: 5 mg 4 times daily 2 days before start of RT until 14 days after RT Placebo: similar tablets, same schedule | |
| Outcomes | Xerostomia: from validated head‐and‐neck symptom questionnaire on 5‐point scale; LENT SOMA Salivary flow rates: parotid salivary flow using Carlson‐Crittenden cups, from left and right hand parotid glands simultaneously under standardised conditions for 10 min. Flow stimulated with 5% (wt/vol) citric acid. Parotid flow complication probability also reported Adverse effects: not reported Survival data: locoregional control Other oral symptoms: eating, swallowing Other oral signs: not reported Quality of life: some covered in validated head‐and‐neck symptom questionnaire on 5‐point scale Patient satisfaction: not reported Cost data: not reported Timing of assessment: before RT, 6 weeks, 6 months and 12 months postRT | |
| Funding | Not reported. Conflicts of interest: "none" reported | |
| Trial registration | Not registered | |
| Sample size calculation presented | Yes | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was executed by the hospital pharmacist by computer, using random permuted blocks within strata. The randomisation key was opened after the last saliva collection (1 year after the last patient was included and after completion of all planned assessments)" |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding (performance bias and detection bias) | Low risk | Quote: "Double‐blind randomised placebo‐controlled study". Intervention was tablets supplied by the pharmacy |
| Blinding (performance bias and detection bias) | Low risk | Quote: "Double‐blind randomised placebo‐controlled study". Intervention was tablets supplied by the pharmacy |
| Incomplete outcome data (attrition bias) | High risk | 32% missing at 12 months with no clear reasons given by study group |
| Selective reporting (reporting bias) | High risk | Adverse events and xerostomia data not fully reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Germany Number of centres: 1 Date of recruitment: not stated | |
| Participants | Inclusion criteria: stage III or IV carcinoma of the head and neck, aged 16 to 80 and no evidence of systemic infection or liver or renal impairment. Tumour resected or excised before adjuvant RT Exclusion criteria: not reported Age: amifostine: median 61 (range 40‐77); control: median 58 (range 38‐75) Gender: amifostine 13 M, 1 F; control 12 M, 2 F Cancer type: tumour location (amifostine/control): larynx = 3/1, hypopharynx = 4/3, mesopharynx = 3/7, nose = 2/1, mouth = 2/2 Radiotherapy: 2 Gy fractions, 5 days a week for 6 weeks; maximum dose of 60 Gy (encompassing 75% of the major salivary glands) Chemotherapy: 20 min IV infusion of carboplatin (70 mg/m² days 1 to 5 and 21 to 25 of treatment) Number randomised: 28 (14 amifostine, 14 control) Number evaluated: 28 | |
| Interventions | Amifostine versus no intervention Amifostine: (500 mg) 15 min IV before carboplatin (days 1 to 5 and days 21 to 25). Followed by antiemetic regimen to control nausea/vomiting Use of supportive drugs reported: (amifostine/control): G‐CSF: 2/7; GM‐CSF: 0/7; antibiotics: 4/10 | |
| Outcomes | Xerostomia: incidence and severity using WHO grading (0 to 4 scale ‐ we report grade 2 and above) Salivary flow rates: not reported Adverse effects: hypotension Survival data: not reported Other oral symptoms: dysgeusia (taste disturbance), dysphagia (difficulty in swallowing), mucositis (WHO) Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: economic evaluation (Bennett 2001) Timing of assessment: xerostomia at end of RT and 1 year; other oral symptoms at end of RT | |
| Funding | US Bioscience who produce Ethyol‐amifostine | |
| Trial registration | Not registered | |
| Sample size calculation presented | Not reported | |
| Notes | Additional data presented but included extra 11 patients in amifostine group who were not entered in the study (not included in analyses) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | High risk | Amifostine versus no intervention |
| Blinding (performance bias and detection bias) | High risk | Not blinded and xerostomia is a subjective outcome |
| Incomplete outcome data (attrition bias) | Low risk | All participants included in analysis |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Germany Number of centres: 6 Date of study: 2001 to 2007 | |
| Participants | Inclusion criteria: SCCHN with deficiency in selenium and if radiation field included 75% of the major salivary glands Exclusion criteria: none reported Age: median 63.2 range 38.7‐83.0 Gender (M:F): selenium 16:6; control 15:2 Cancer type: head and neck cancer Radiotherapy: 1.8 to 2.0 Gy to primary tumour and lymphatic neck during daily radiation treatment; to total dose 60‐72 Gy Chemotherapy: unclear Number randomised: 40: 22 selenium, 18 control Number evaluated: 39: 22 selenium, 17 control | |
| Interventions | Selenium versus no intervention Selenium: 500 µg sodium selenite, 2 days before RT, 500 µg selenite and radiation days (300 µg if official holiday). Administrated as oral fluid 1 hour before RT Control: no intervention | |
| Outcomes | Xerostomia: RTOG grade for xerostomia Salivary flow rates: not reported Adverse effects: serious adverse events reported Survival data: not reported Other oral symptoms: mucositis RTOG, dysgeusia (taste disturbance RTOG), dysphagia (difficulty in swallowing RTOG) Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: 1, 2, 3, 4, 5, 6, 7 weeks from start of RT and 6 weeks after RT | |
| Funding | Externally funded by Arzneimittel, Germany | |
| Trial registration | Unclear | |
| Sample size calculation presented | Not reported | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not given, stated "randomised" |
| Allocation concealment (selection bias) | Unclear risk | Allocation after consent obtained |
| Blinding (performance bias and detection bias) | High risk | Participants receive selenium oral fluid prior to radiotherapy or not. Blinding not possible |
| Blinding (performance bias and detection bias) | High risk | Participants receive selenium oral fluid prior to radiotherapy or not, and their subjective assessment of xerostomia is included |
| Incomplete outcome data (attrition bias) | Low risk | Initial study requiring 60 patients per arm stopped early due to slow accrual 113 screened. 93 selenium deficient. 40 consented. 1 withdrawal, 39 reported Selenium concentrations reported in other article elsewhere |
| Selective reporting (reporting bias) | High risk | Xerostomia but no standard deviations. Total adverse events reported but not per person |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Canada Number of centres: multicentre (unclear how many) Date of enrolment: September 1997 to September 1999 | |
| Participants | Inclusion criteria: SCCHN, non‐metastatic disease Exclusion criteria: none reported Age: lozenge median 59.7; placebo median 57.3 Gender (M:F) : lozenge (48:18), placebo (52:15) Cancer type: oral cavity, oropharynx, hypopharynx, nasopharynx, larynx Radiotherapy: conventional radical or postoperative radiotherapy to a dose of 50 Gy or greater delivered in once daily fractions (1.8 to 2.4 Gy) Chemotherapy: not mentioned, probably none Number randomised: 138 (69 per group) Number evaluated: 133 (lozenge 66; placebo 67) | |
| Interventions | Antimicrobial lozenge versus placebo Antimicrobial lozenge: BCoC, bacitracin, 6 mg; clotrimazole, 10 mg; gentamicin, 4 mg. Unclear how frequently taken or for how long Placebo: not described ‐ assumed similar | |
| Outcomes | Xerostomia: item on trial specific checklist ‐ 'Did you have mouth dryness (1‐4 scale)?' and NCIC CTG ECTC physician‐rated (using patient diary) Salivary flow rates: not reported Adverse effects: not reported Survival data: not reported Other oral symptoms: mucositis using OMAS (primary outcome), mouth pain, chewing, numbness, mouth opening, burning mouth Other oral signs: not reported Quality of life: 2 tools ‐ European Organisation for Research and Treatment of Cancer Quality of Life questionnaire (EORT QLQ‐C30), trial specific checklist Patient satisfaction: not reported Cost data: not reported Timing of assessment: 2, 4, 6 during RT; 8‐9, 12‐14, 24 weeks on study | |
| Funding | The National Cancer Institute of Canada, Clinical Trials Group | |
| Trial registration | Unclear | |
| Sample size calculation presented | No | |
| Notes | Primarily study to prevent mucositis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind controlled trial". Placebo tablets given |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind controlled trial". Placebo tablets given |
| Incomplete outcome data (attrition bias) | Low risk | Compliance with quality of life forms reported to be 93.3% but reasons for dropouts not reported. Similar low rates of attrition per group |
| Selective reporting (reporting bias) | High risk | Xerostomia reported, adverse events not reported for lozenge |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: USA Number of centres: unclear Date of randomisation: March 1998 to February 2000 | |
| Participants | Inclusion criteria: oral and oropharyngeal squamous cell carcinoma, Karnofsky Performance Score ≥ 60, no prior radiotherapy to the head and neck, planned irradiation of the oral cavity or oropharynx in which at least 50% of the major salivary glands are to receive > 50 Gy Exclusion criteria: salivary gland malignancy; use of cholinergic, anticholinergic, and tricyclic drugs; and patients with uncontrolled asthma, acute iritis, or narrow‐angle glaucoma Age: pilocarpine 60.8 years; placebo 59.3 years Gender (M:F): pilocarpine 93:28, placebo 92:32 Cancer type: oral cavity 52; nasopharynx 3; oropharynx 104; hypopharynx 11; other 13; unknown 18 (evenly distributed across groups) Radiotherapy: 60‐70 Gy with 50% of volume of major salivary glands receiving 50 Gy Chemotherapy: not stated Number randomised: 249; 3 ineligible, all from pilocarpine arm (121 pilocarpine, 125 placebo) Number evaluated: 166 end of RT (pilocarpine 89, placebo 77); 166 at 3 months (pilocarpine 85, placebo 81); 137 at 6 months (pilocarpine 68, placebo 69) | |
| Interventions | Pilocarpine versus placebo Pilocarpine: 5 mg tablets 4 times daily starting 3 days before RT and continuing for 3 months | |
| Outcomes | Xerostomia: not reported Salivary flow rates: salivary gland scintigraphy (stimulated and unstimulated) Adverse effects: drug toxicities reported Survival data: not reported Other oral symptoms: RTOG acute mucositis, mouth pain, dysgeusia (taste disturbance), dysmasesia (difficulty in chewing), dysphagia (difficulty in swallowing), dysphonia (difficulty in speaking) Other oral signs: not reported Quality of life: University of Washington QoL scale Patient satisfaction: not reported Cost data: not reported Timing of assessment: pretreatment, end of RT, 3 months after end of RT, 6 months after end of RT | |
| Funding | National Cancer Institute and MGI Pharma Inc. | |
| Trial registration | clinicaltrials.gov/show/NCT00003139ID ‐ 11 Protocol available | |
| Sample size calculation presented | Not reported | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | Low risk | Pilocarpine versus placebo |
| Blinding (performance bias and detection bias) | Low risk | Pilocarpine versus placebo |
| Incomplete outcome data (attrition bias) | Unclear risk | 213/249 available for analysis. Dropouts very high for salivary flow (33% end of RT and 3 months, 45% at 6 months) |
| Selective reporting (reporting bias) | High risk | Xerostomia not reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Canada Number of centres: 1 Date of randomisation: March 1998 to September 2001 | |
| Participants | Inclusion criteria: scheduled to receive external beam radiotherapy, using a bilateral radiation technique encompassing ≥ 2/3 of all major and minor salivary glands for a minimum of 5000 cGy (200 cGy per day) for 5‐7 weeks Exclusion criteria: clinically significant cardiovascular disease, chronic obstructive pulmonary disease, biliary tract disease, uncontrolled asthma, acute iritis, narrow angle glaucoma, participants who are pregnant or nursing. Hypersensitivity to pilocarpine, participants on tricyclic antidepressants, antihistamines with anticholinergic effects, beta blockers, or pilocarpine for ophthalmic indications were excluded Age (mean): pilocarpine 58 years; placebo 61 years Gender (M:F): pilocarpine 26:3, placebo 24:5 Cancer type: oral cavity 14; pharynx 13; tonsil 11; glottis 3; larynx 11; sinus 2; neck 1; unknown 1 (evenly distributed across groups) Radiotherapy: Mean dose = 64.7 Gy (pilocarpine group), 63.7 Gy (placebo group) Chemotherapy: pilocarpine 13 (45%); placebo 9 (32%) Number randomised: 58 Number evaluated: 58 (22 dropped out but ITT was used and missing data were calculated) | |
| Interventions | Pilocarpine versus placebo Phase 1 Placebo: identical tablets 5 times daily, half an hour before meals, before radiotherapy, and prior to sleep during the period of radiotherapy Phase 2 | |
| Outcomes | Xerostomia: subjective assessment of xerostomia: VAS (rated 0‐100) Salivary flow rates: whole saliva secretion (unstimulated and stimulated) using the SAXON test Adverse effects: not reported (data provided by author) Survival data: not reported Other oral symptoms: oral discomfort, difficulty with eating, dysphonia (difficulty in speaking), mucosal pain or burning (VAS, rated 0‐100) Other oral signs: not reported Quality of life: global quality of life, sleeping problems (VAS, rated 0‐100) Patient satisfaction: not reported Cost data: not reported Timing of assessment: prior to RT, end of RT, 5 weeks after end of RT | |
| Funding | Pharmacia Canada | |
| Trial registration | Not registered | |
| Sample size calculation presented | Not reported | |
| Notes | Phase 2 data not included in the review Additional data provided by author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment from author: "block of four using a random number table... allocation sequence prepared by pharmacy of Jewish General Hospital" |
| Allocation concealment (selection bias) | Low risk | Third party randomisation; coded bottles |
| Blinding (performance bias and detection bias) | Low risk | Bottles only distinguished by number allocated by pharmacy. Investigators, treating physicians and patients blinded |
| Blinding (performance bias and detection bias) | Low risk | Subjective outcomes self reported (patients unaware of treatment group) |
| Incomplete outcome data (attrition bias) | Low risk | Analysis carried out on ITT basis. 38% dropout rate. 58 randomised, 22 dropped out (9 pilocarpine, 13 placebo) |
| Selective reporting (reporting bias) | High risk | Adverse events not reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Germany Number of centres: 1 Date of randomisation: not stated | |
| Participants | Inclusion criteria: scheduled to receive adjuvant or sole radiotherapy for head and neck cancer to a scheduled dose of 60 Gy. Cranial border of the field above the chin‐mastoid line so salivary glands are located in the core irradiation field Exclusion criteria: salivary gland disorders Age: mean age = 55 years Gender: 22 M, 1 F Cancer type: head and neck Radiotherapy: total dose = 60 Gy Number randomised: 48 Number evaluated: 23 | |
| Interventions | Coumarin + troxerutin versus placebo Venalot Depot (coumarin 15 mg and troxerutin 90 mg) tablet: 2 tablets 3 times daily. Start 1 week before RT and 4 weeks after end of RT | |
| Outcomes | Xerostomia: not reported, only as part of total RTOG Salivary flow rates: stimulated and unstimulated using sialoscintigraphy (sialometry abandoned as primary marker as not successfully collected). Acute radiation side effects RTOG score but for all organs Adverse effects: reddened skin, nausea Survival data: locoregional control Other oral symptoms: not reported Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: 4 weeks after RT | |
| Funding | Not stated | |
| Trial registration | Unclear | |
| Sample size calculation presented | Not reported | |
| Notes | Unable to use data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | Low risk | Venalot Depot versus placebo |
| Blinding (performance bias and detection bias) | Low risk | Salivary flow rates objective outcome |
| Incomplete outcome data (attrition bias) | High risk | 48 randomised, 25 dropped out. Dropouts per group not specified |
| Selective reporting (reporting bias) | High risk | Xerostomia not reported. Data for total RTOG score presented but no break down by condition or organ |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Iran Number of centres: 1 Date of recruitment: 1998‐2000 | |
| Participants | Inclusion criteria: 18‐70 year old patients, irradiated to the head and neck, both parotid glands in the radiation fields (minimum 40 Gy). No previous history of irradiation in this region Age: mean across groups = 43 years (range 18 to 70 years) Gender (M:F): across groups 36:24 Cancer type: primary site of tumour. Pilocarpine group: nasopharynx (n = 17), neck adenopathy (n = 1). Placebo group: maxilla (n = 2), nasopharynx (n = 13), tongue (n = 1), tonsil (n = 5) Radiotherapy: standard fractionation (1.8 to 2 Gy per day, 5 days a week) and cobalt‐60 systems; mean parotid dose 58 Gy (pilocarpine 59 Gy; placebo 57 Gy) (range 45 to 70 Gy) Number randomised: 60 Number evaluated: 39 (18 pilocarpine, 21 placebo) | |
| Interventions | Pilocarpine versus placebo Pilocarpine hydrochloride: 5 mg 3 times daily for 3 months starting from the beginning of RT | |
| Outcomes | Xerostomia: subjective evaluation score for xerostomia using 6 questions evaluated using VAS (0‐100 mm). Objective grading of xerostomia according to the Late Effects of Normal Tissues Subjective, Objective, Management and Analytic (LENT SOMA) scale Salivary flow rates: not reported Adverse effects: lacrimation (excess tears, crying), nausea Survival data: overall survival Other oral symptoms: not reported Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: 6 months postRT | |
| Funding | Source of funding: Tehran University of Medical Sciences' research grant | |
| Trial registration | Not registered | |
| Sample size calculation presented | Not reported | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...randomisation was performed at the start of radiotherapy by the sealed envelope method" |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes, pharmacy involvement |
| Blinding (performance bias and detection bias) | Low risk | Capsules only distinguished by a number recorded by the drug manufacturer. Investigators, treating physicians and patients blinded |
| Blinding (performance bias and detection bias) | Low risk | Capsules only distinguished by a number recorded by the drug manufacturer. Investigators, treating physicians and patients blinded |
| Incomplete outcome data (attrition bias) | High risk | 60 enrolled. 13/31 (42%) dropouts in pilocarpine group; 8/29 (28%) dropouts in placebo group |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: USA Number of centres: 4 Date of enrolment: May 2003 to April 2006 | |
| Participants | Inclusion criteria: with stage III or IV, previously untreated, locally advanced, SCCHN. Primary tumour types allowed: oropharynx, hyperpharynx, oral cavity, larynx, unknown primary Exclusion criteria: grade > 2 peripheral neuropathy other serious comorbid illness, involuntary weight loss of > 20% of body weight in 3 months preceding study Age: amifostine mean 55; control 57 Gender: amifostine: 27 M, 2 F; control: 23 M, 6 F Cancer type: (amifostine/control) oropharynx = 18/17, oral cavity = 5/6, larynx = 3/5, unknown primary = 2/0, other = 1/1 Radiotherapy: concomitant boost radiation, 72 Gy in 42 fractions over 6 weeks. Use of IMRT not allowed Chemotherapy: 4 weekly doses of carboplatin/paclitaxel. Induction chemotherapy was used in 29 of 58 patients overall with docetaxel, cisplatin, and 5‐fluorouracil Number randomised: 58 (29 per group) Number evaluated: unclear for xerostomia | |
| Interventions | Amifostine versus no intervention Subcutaneous daily amifostine at dose of 500 mg 30‐60 min before daily RT (before morning dose only, when schedule moved to twice daily radiotherapy at day 19). Average number of amifostine doses was 25 (median 28 doses). Amifostine withheld for skin toxicity | |
| Outcomes | Xerostomia: Common Terminology Criteria for Adverse Events including xerostomia reported but not by group Salivary flow rates: saliva collection with and without citric acid simulation Adverse effects: not reported Survival data: overall survival, progression‐free survival, local control Other oral symptoms: Common Terminology Criteria for Adverse Events for mucositis, swallowing measured Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: xerostomia and mucositis assessed weekly throughout RT, then every 4 weeks after RT; salivary flow rate assessed at 12, 24 and 52 weeks after RT; dysphagia (swallowing) assessed at 8, 12, 24 and 52 weeks after RT; survival ‐ median follow‐up 34 months after RT, minimum 26 months | |
| Funding | Medimmune Oncology | |
| Trial registration | Not registered | |
| Sample size calculation presented | Yes | |
| Notes | Quote: "Study stopped before completion of planned accrual because IMRT was becoming de facto standard technique in treating head and neck cancer" Study focuses on survival Not able to use data ‐ contacted authors for data 19 February 2016 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation process was centralised and managed through the Dana‐Farber Cancer Institute protocol office" Comment: linked to Harvard University probably done well |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomisation process was centralised and managed through the Dana‐Farber Cancer Institute protocol office" |
| Blinding (performance bias and detection bias) | High risk | No intervention group as comparator ‐ not blinded |
| Blinding (performance bias and detection bias) | High risk | Subjective assessment of xerostomia |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear how many participants dropped out |
| Selective reporting (reporting bias) | High risk | Badly reported xerostomia and no adverse events |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: China Number of centres: 2 Date of conduct: 1 October 2007 to 31 July 2009 | |
| Participants | Inclusion criteria: quote: "First‐visit patients; diagnosed as mid/moderate to advanced/terminal nasopharyngeal squamous carcinoma through pathological and radiographic examinations; Karnosfsky score ≥ 60; expected survival period > 6 months; without severe complications (e.g. hypertension, coronary heart disease, diabetes, history of mental illness)" Exclusion criteria: see above Age: Jinlong: mean 46.3 (SD 7.4), median 53; control: mean 47.4 (SD 6.8), median 52 Gender: Jinlong: 33 M, 16 F; control: 34 M, 14 F Cancer type: nasopharyngeal squamous carcinoma Radiotherapy: dose 60 to 76 Gy, 2 Gy per day, 5 times a week Chemotherapy: "concurrent chemoradiotherapy" (no further details) Number randomised: 97 (Jinlong: 49, control: 48) Number evaluated: 95 (Jinlong: 48, control: 47) | |
| Interventions | Jinlong capsules versus no intervention 4 tablets once, 3 tablets every day Duration: 3 months Follow‐up: 12 weeks after treatment Quote: "Jinlong capsule is a modern 'fresh medicine preparation' made of fresh gecko and fresh long‐noded pit vipers, using cryogenic modern biochemical extracting and separation techniques. It maintained to the greatest degree the activity of effective ingredients of organisms, and reasonable compatibility among the ingredients. Basic research has shown that Jinlong can directly damage cancer cells by blocking the mitosis and proliferation of cancer cells, fix the p21 small protein molecule, restore the regulation of cancer cells, and turn cancer cells to normal cells..." | |
| Outcomes | Xerostomia: quote: "observe the patients for toxic and side effects during and after radiotherapy, assess the toxic and side effects according to RTOG's criteria" Salivary flow rates: not reported Adverse effects: leukopenia, nausea, vomiting, 1 participant had dizziness and blood pressure drop, 1 participant had skin rash Survival data: not reported Other oral symptoms: mucositis Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported | |
| Funding | Not reported; conflicts of interest: not reported | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly divided" |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | High risk | Jinlong versus no intervention |
| Blinding (performance bias and detection bias) | High risk | Jinlong versus no intervention |
| Incomplete outcome data (attrition bias) | Low risk | Quotes: "1 patient quit because of myocardial infarction (Tx Group)", "1 patient quit because of mucosa toxicity (control group)" |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: China Number of centres: 1 Date of conduct: not stated | |
| Participants | Inclusion criteria: aged 20‐70 years; Karnofsky Performance Score > 70; Hb 90 to 150/L; blood pressure 12‐20/8‐15 kPa; normal kidney and liver function; no severe infection such as septicaemia; no heart disease; no medical history of low blood pressure, no other cancer and no history of radiotherapy Exclusion criteria: see above Age: aged 20 to 70 (no further details) Gender: not reported Cancer type: amifostine: nasopharyngeal squamous cell carcinoma stage 1 = 1, stage 2 = 7, stage 3 = 8 and stage 4 = 1. Control: nasopharyngeal squamous cell carcinoma stage 1 = 1, stage 2 = 5, stage 3 = 1 and stage 4 = 1 Radiotherapy: conventional with nasopharyngeal tumour dose (65‐74 Gy) Number randomised: 32 (amifostine: 17; control: 15) Number evaluated: 32 (amifostine: 17; control: 15) ‐ 1 participant left amifostine group due to GI tract side effect but analysis states 17 in this group (possible ITT analysis) | |
| Interventions | Amifostine versus no intervention Amifostine (200 mg/m²), diluted with 'water for injection' at the concentration of 50 mg/mL, IV 15‐30 min before RT | |
| Outcomes | Xerostomia: "mucositis and xerostomia according to RTOG's criteria" (0‐4 scale; we report grade 2 and above) Salivary flow rates: "method used to measure the amount of saliva: put a 0.2 g cotton ball under patient's tongue, after 3 minutes, use electronic balance to measure its weight", reported as decrease in saliva/change score (unstimulated) Adverse effects: GI tract reaction/side effects (nausea and vomiting) Survival data: not reported Other oral symptoms: mucositis (RTOG criteria) Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: 3, 5 and 7 weeks after start of RT | |
| Funding | Not reported; conflicts of interest: not reported | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomized into" Comment: no further details given |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | High risk | Amifostine versus no intervention |
| Blinding (performance bias and detection bias) | High risk | Not possible due to no intervention group and subjective assessment of xerostomia |
| Incomplete outcome data (attrition bias) | Low risk | 1/32 participants dropped out, however, appears to be included in analysis |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Australia, Canada and Europe Number of centres: 38 hospitals Date of conduct: January 2005 to August 2007 | |
| Participants | Inclusion criteria: more than 18 years old; resected for pathohistologically documented high‐risk stage 2 to 4B SCC of the oral cavity, oropharynx, hypopharynx, or larynx; ECOG score of 0 to 2; at least 2 of 9 areas of the oral or oropharyngeal mucosa due to receive at least 50 Gy RT Exclusion criteria: tumours of the lips, paranasal sinuses, salivary glands, or unknown primary site; metastatic disease; history of chronic pancreatitis or acute pancreatitis within the last year; prior RT to the head and neck region or prior chemotherapy; previous treatment on this study or with other KGFs Age: palifermin: mean 56 (SD 8); placebo: mean 57 (SD 9) Gender: palifermin: 78 M, 14 F; placebo: 75 M, 19 F Cancer type: head and neck (oropharynx, oral cavity, larynx, hypopharynx, other) Radiotherapy: standard fractionation of once daily 2 Gy fractions, 5 days per week; total 60 Gy (for R0 resection) over 6 weeks, or 66 Gy (for R1 resection) over 7 weeks, both with allowable range of ± 15% Chemotherapy: cisplatin (100 mg/m²) IV after appropriate hydration on days 1 and 22 (for R0 resection), or days 1, 22 and 43 (for R1 resection) Number randomised: 186 (palifermin 92; placebo 94) Number evaluated: 186 (palifermin 92; placebo 94) | |
| Interventions | Palifermin versus placebo Palifermin: (120 µg/kg) 3 days prior to start of, and then once per week during radiochemotherapy, i.e. 7 doses for those with R0 resection, 8 doses for those with R1 resection (total dose = 840 or 960 µg/kg respectively) Placebo: same schedule with placebo | |
| Outcomes | Xerostomia: incidence of grade ≥ 2 xerostomia (Common Terminology Criteria for Adverse Events (CTCAE) v 3.0, assessed at months 4, 6, 8, 10, 12, reported only at month 4 Salivary flow rates: not reported Adverse effects: assessed weekly during study treatment Survival data: overall and progression‐free survival, incidence of disease recurrence and death Other oral symptoms: incidence of dysphagia (difficulty in swallowing), OMWQ‐HN 0 (no soreness) to 4 (extreme soreness) scale for mouth and throat soreness assessed weekly and reported as mean score Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported | |
| Funding | Quote: "This study was supported by Amgen" (Amgen also named as sponsor on trials registry ‐ pharmaceutical industry) | |
| Trial registration | NCT00131638 (clinicaltrials.gov/ct2/show/NCT00131638) | |
| Sample size calculation presented | Yes | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random assignment was made by a centralized interactive voice response system" |
| Allocation concealment (selection bias) | Low risk | Quote: "Random assignment was made by a centralized interactive voice response system" |
| Blinding (performance bias and detection bias) | Low risk | Quote: "placebo‐controlled, double‐blind study" |
| Blinding (performance bias and detection bias) | Low risk | Quote: "placebo‐controlled, double‐blind study" |
| Incomplete outcome data (attrition bias) | Low risk | All cases accounted for. ITT analysis (participants having no assessment assumed to have event) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. Low risk for xerostomia at the time point used in meta‐analysis (4 months) ‐ however, it should be noted that xerostomia was measured up to 12 months but data not reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: China Number of centres: 1 Date of conduct: January 2002 to June 2004 | |
| Participants | Inclusion criteria: head and neck patients confirmed by pathological examination Exclusion criteria: not reported Age (years): treatment: mean 51 (SD 19); control: mean 49 (SD 18) Gender: treatment: 36 M 34 F; control: 38 M, 32 F Cancer type: treatment: nasopharyngeal (52), tonsil (11) and tongue (7); cancer stage: I = 6, II = 20, III = 28 and IV = 16. Control: nasopharyngeal (51), tonsil (11) and tongue (8); cancer stage: I = 6, II = 19, III = 29 and IV = 16 Radiotherapy: overall dose: 70 Gy for nasopharyngeal carcinoma, 55‐70 Gy for carcinoma of tonsil and tongue Chemotherapy: none Number randomised: 140 (treatment 70, control 70) Number evaluated: 140 (treatment 70, control 70) | |
| Interventions | Shenqi Fanghou recipe versus no intervention Shenqi Fanghou recipe: dangshen (30 g), astragalus root (30 g), tuckahoe (30 g), Chinese yam (30 g), hedyotic diffusa (30 g), barbated skullcup herb (30 g), pueraria root (30 g), fragrant solomonseal rhizome (10 g), glossy privet fruit (10 g), stiff silkorm (10 g), grassleaf sweetflag rhizome (10 g), atractylodes macrocephala (10 g), semen coicis (50 g), dried tangerine peel (6 g), paris root (20 g), figwort root (15 g), common anemarrhena rhizome (15 g), gambir plant (15 g), scorpion (5 g), radix notoginseng (5 g), radix glycyrrhizae (5 g) Follow‐up: end of RT | |
| Outcomes | Xerostomia: subjective assessment of dry mouth: 1) mild: can eat dry cooked rice, 2) moderate: have difficulty in eating dry cooked rice, or 3) severe: cannot eat dry cooked rice Salivary flow rates: not reported Adverse effects: none Survival data: survival after a follow‐up of more than 1 year Other oral symptoms: oropharyngeal mucosa reaction, difficulty in mouth opening Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported | |
| Funding | Source of funding: government (The Bureau of Science and Technology of Shenzhen City); conflicts of interest: not reported | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly divided" Comment: no further details given |
| Allocation concealment (selection bias) | Unclear risk | Quote: "the envelop method was used to randomise" Comment: insufficient information |
| Blinding (performance bias and detection bias) | High risk | Shenqi Fanghon recipe versus no intervention |
| Blinding (performance bias and detection bias) | High risk | Not possible due to no intervention group and subjective assessment of xerostomia |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported (quote: "no adverse events") |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Brazil Number of centres: 1 Date of conduct: January 2010 to March 2012 | |
| Participants | Inclusion criteria: primary oral, oropharynx, or nasopharynx carcinomas (clinical stage ≥ II) scheduled to undergo 3‐D radiotherapy (RTC3D) or IMRT, ≤ 75 years of age Exclusion criteria: hypersensitivity to bethanechol, hypotension, hyperthyroidism, peptic ulcer disease, epilepsy, angina, parkinsonism, and patients using tricyclic antidepressants, and antihistamines Age: bethanechol: mean 55.9 (range 21 to 75); placebo: mean 55.8 (range 28 to 75) Gender: bethanechol: 37 M, 11 F; placebo: 39 M, 10 F Cancer type: oral cavity, oropharynx, nasopharynx Radiotherapy: once‐daily mega voltage (6 MV), given at 18 to 2.12 Gy per fraction, 5 days per week (duration unclear) for 7 weeks Chemotherapy: bethanechol 73%; placebo 71% (type of CT not reported) Number randomised: 97 (bethanechol 48, placebo 49) Number evaluated: 84 (bethanechol 42, placebo 42) | |
| Interventions | Bethanechol versus placebo Both groups: 1 tablet (25 mg) taken twice a day from beginning of RT and continued until 1 month after end of treatment (median 19 weeks) | |
| Outcomes | Xerostomia: observer‐based grade and scored according to the subjective measures of Eisbruch (grade 0 to 3) ‐ reported as grade 2 and above Salivary flow rates: whole unstimulated and stimulated saliva flows collected over 5 min each and reported in ml/min (reported by RT‐type subgroups ‐ we combined the subgroups but numbers were not reported so we used the number randomised from table 1), also scintigraphy undertaken Adverse effects: bethanechol toxicities using National Cancer Institute Common Terminology Criteria for Adverse Events – NCI CTCAE, v 3.0 Survival data: not reported Other oral symptoms: not reported Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: xerostomia assessed weekly to 3 months postRT; saliva flow assessed during RT (range 30 to 35 Gy) and 2 months postRT | |
| Funding | FAPESP (an independent public foundation) and CAPES (an organization of the Brazilian federal government under the Ministry of Education) | |
| Trial registration | Not registered | |
| Sample size calculation presented | Yes (reported in supplementary data online) | |
| Notes | Supplementary data online dx.doi.org/10.1016/j.radonc.2015.03.017 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using the Epi‐Info® software version 6.04b, eight lists with a randomized sequence for patient allocation were generated, because a separate list was needed for each of the 8 strata defined by the 3 dichotomous stratification factors (randomization codes with block‐size of eight)" |
| Allocation concealment (selection bias) | Unclear risk | Authors do not state who randomised the participants and whether it was in a concealed manner |
| Blinding (performance bias and detection bias) | Low risk | Quote: "a placebo was manipulated identical in color, shape and weight. Both bethanechol and placebo therapies were coded as A and B. The clinician, patients as well as the statistician were unaware of the trial groups" |
| Blinding (performance bias and detection bias) | Low risk | Placebo trial |
| Incomplete outcome data (attrition bias) | Low risk | 13 out of 97 dropped out with reasons for dropouts clearly stated by study group, but equal per group and similar reasons |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: the Netherlands Number of centres: 1 Date of recruitment: August 1999 to August 2003 | |
| Participants | Inclusion criteria: stage III/IVB squamous cell carcinoma of the oral cavity, oropharynx, hypopharynx and/or larynx or lymph node metastases in the head and neck area from an unknown primary. Treatment with bilateral primary or postoperative radiotherapy with curative intent. 75% of the parotid gland volume expected to receive a radiation dose of at least 40 Gy. Minimal life expectancy of 12 months and a WHO performance score from 0 to 2. Good understanding of the Dutch language Exclusion criteria: distant metastases (M1), previously irradiated patients, patients treated in combination with induction or concurrent chemotherapy, and patients with tumours that originated in the salivary glands. Pregnant patients, those participating in another investigational trial or in poor general health or psychological conditions. Patients who had severe cardiovascular disease, poor renal function or sustained hypotension not secondary to antihypertensive medication Age: mean age = 55 (24 to 73) Gender: AMI‐3: 20 M, 10 F; AMI‐5: 22 M, 8 F; control: 18 M, 13 F Cancer type: head and neck at various sites and stages and lymph node classifications Radiotherapy: megavolt equipment using isocentre techniques after 3‐dimensional planning. 2 opposing lateral fields with an anterior field to cover the lower jugular and supraclavicular lymph node areas. All received 46 Gy to treated areas, boost doses varied from 56 Gy (in patients who had negative surgical margins) to 63.5 Gy (in patients who had lymph node metastasis with extranodal spread or positive margins). Patients treated primarily with radiotherapy received 70 Gy to macroscopic tumour Chemotherapy: none Number randomised: 91 (AMI‐3: 30; AMI‐5: 30; control: 31) Number evaluated: 71 (xerostomia at 12 months) (AMI‐3: 22; AMI‐5: 27; control: 22) | |
| Interventions | 3 arms: Amifostine 1 versus amifostine 2 versus no intervention Group 1: amifostine 3 times weekly 200 mg/m² administered IV over 3 to 5 minutes 15 to 30 minutes before irradiation Group 2: amifostine 5 times weekly 200 mg/m² administered IV over 3 to 5 minutes 15 to 30 minutes before irradiation | |
| Outcomes | Xerostomia: late and acute radiation‐induced xerostomia at grade 2 and above (0 to 4 scale ‐ RTOG/EORTC Late Radiation Morbidity Scoring); patient‐rated xerostomia and sticky saliva using QLQ‐H&N35 (1 to 4 scale converted linearly to a 0 to 100 mm scale where higher scores = worse symptoms) ‐ not used Salivary flow rates: not reported Adverse effects: vomiting (emesis), nausea, hypotension, allergic reaction Survival data: locoregional tumour control and overall survival Other oral symptoms: not reported Other oral signs: not reported Quality of life: QoL‐C30 version 3.0, the EORCT Core Questionnaire with supplemental head and neck specific module (QLQ‐H&N35) Patient satisfaction: not reported Cost data: not reported Timing of assessment: xerostomia and QoL assessed at end of RT and 6, 12, 18 and 24 months after RT; survival assessed to 60 months but reported in text at 2 years | |
| Funding | Source of funding: not stated. Amifostine provided by Schering Plough | |
| Trial registration | Not registered | |
| Sample size calculation presented | Reported | |
| Notes | Have only reported locoregional tumour control and overall survival data narratively as it did not seem sensible to combine the 2 amifostine arms due to differing results. Numbers per group unclear for xerostomia at end of RT and therefore not able to use | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment performed at university medical centre using a permuted block design |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Blinding not possible |
| Blinding (performance bias and detection bias) | High risk | Blinding not mentioned. Xerosomia is subjective measure |
| Incomplete outcome data (attrition bias) | High risk | 22% dropouts at 12 months and difference in attrition between groups (i.e. no amifostine = 29%, amifostine3 = 27%, amifostine5 = 10%) |
| Selective reporting (reporting bias) | High risk | Quality of life was measured but not reported (only quote: "No significant differences") |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Brazil Number of centres: 1 Date of enrolment: October 2004 to July 2005 | |
| Participants | Inclusion criteria: adults with biopsy‐proven malignant neoplasm of the head and neck who received external beam RT Exclusion criteria: conditions which may introduce adverse reaction to bethanechol: tricyclic antidepressants, antihistamines, betablockers, hypersensitivity Age: bethanechol: mean 57 (SD 15); control: 55 (SD 13) Gender: bethanechol: 17 M 5 F; control: 16 M 5 F Cancer type: malignant neoplasm of head and neck Radiotherapy: external beam RT, encompassing 1 or more salivary glands, minimum 45 Gy Chemotherapy: bethanechol 23%; control 48% (type of CT not reported) Number randomised: 43 (bethanechol 22; control 21) Number evaluated: range over outcomes (and time points). Xerostomia VAS at 08 to 40 weeks after RT: 30 (bethanechol 13; control 17) | |
| Interventions | Bethanechol versus artificial saliva Bethanechol: 25 mg 3 times daily (6 am, 2 pm, 10 pm) administered with RT and used until end of RT Control: artificial saliva (OralBalance) ‐ schedule not reported | |
| Outcomes | Xerostomia: subjective VAS scale (length not mentioned ‐ not used), asking about dry mouth (yes/no) Salivary flow rates: whole resting saliva and whole stimulated saliva collected over 5 minutes and reported in ml/min Adverse effects: lacrimation, nervousness, frequent urination, sweating, warm face, cramps, diarrhoea, nausea Survival data: death Other oral: not reported Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: xerostomia and saliva flow assessed during RT (between 15th and 19th session), at end of RT and at least 2 months after RT (ranging from 8 to 40 weeks after) | |
| Funding | CAPES (an organization of the Brazilian federal government under the Ministry of Education) gave financial support, Apsel Laboratories provided bethanechol, and Laclede provided artificial saliva | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using the Epi‐info software version 6.04b, 6 lists with randomized sequence for patient allocation were generated (random codes with block‐size of 8). Prior to allocation patients were stratified by RT treatment and age" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | Quote: "...for obvious reasons it was not possible for the study to be double‐blinded" |
| Blinding (performance bias and detection bias) | High risk | Quote: "...for obvious reasons it was not possible for the study to be double‐blinded" |
| Incomplete outcome data (attrition bias) | High risk | Varies over outcomes. For xerostomia (VAS): 30% dropped out or died (bethanechol 41%; control 19%). Differential dropout and (apart from death) reasons for dropouts unclear |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Croatia Number of centres: unclear Date of conduct: unclear | |
| Participants | Inclusion criteria: patients scheduled to receive external beam radiation therapy to the major salivary glands completely or partially included in the field Exclusion criteria: significant cardiovascular, pulmonary, hepatic or pancreatic disorders or gastroduodenal ulcers Age: not reported Gender: not reported Cancer type: not reported Radiotherapy: weekly external beam radiation therapy for 4 to 8 weeks, no further details Chemotherapy: not stated Number randomised: unclear Number evaluated: 48 | |
| Interventions | Pilocarpine versus placebo Pilocarpine: 5 mg capsules 4 times daily starting the day before RT and continuing for 3 months | |
| Outcomes | Xerostomia: standardised questionnaire (subjective assessment, administered by clinician) Salivary flow rates: stimulated salivary flow rate (parotid saliva by Carlson‐Crittenden cup; submandibular/sublingual saliva by standardised suction device) Adverse effects: not reported Survival data: not reported Other oral symptoms: not reported Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: 3 months (end of drug treatment), 6 months and 12 months | |
| Funding | Unclear | |
| Trial registration | Unclear | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind; pilocarpine versus placebo |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind; pilocarpine versus placebo |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear of number randomised to each group, therefore number of dropouts unclear |
| Selective reporting (reporting bias) | High risk | Adverse effects not fully reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Spain Number of centres: 1 Date of enrolment: May 2004 to May 2007 | |
| Participants | Inclusion criteria: between 18 and 75 years of age. At least 10 teeth present in mouth. Willing to consent Exclusion criteria: presence of mucosal pathology, pregnant or undergoing orthodontic therapy Age: mouthwash: mean age 49.4 years (SD 15.4); control: mean age 54.3 years (SD 16.1) Gender (M:F): mouthwash 15:3, control 17:1 Cancer type: head and neck Radiotherapy: 50 to 80 Gy over 5 weeks Chemotherapy: probably none Number randomised: 36 (18 per group) Number evaluated: 16 at 4 weeks for stimulated saliva (mouthwash 9, control 7) | |
| Interventions | Antiseptic mouthrinse versus placebo Mouthwash: CHX 0.12% and 0.05% cetylpyridinium by oral rinse 15 ml twice daily (morning and night). From start of RT for 28 days Placebo: control without active ingredient | |
| Outcomes | Xerostomia: not assessed Salivary flow rates: stimulated saliva (ml/min), pH saliva (0/1/2) Adverse effects: none reported Survival data: not reported Other oral symptoms: hiposialosis (drooling), mucositis, plaque, gingivitis, caries Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: 14, 28 days after RT started (i.e. no time points of interest) | |
| Funding | Source of funding unclear; suspect pharmaceutical industry sponsored by intervention manufacture Perio‐Aid Tratamiento | |
| Trial registration | Unclear | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated list assigned by random number |
| Allocation concealment (selection bias) | Low risk | Allocated after inclusion corresponding to numerically coded mouthrinse. Code only broken at end of study |
| Blinding (performance bias and detection bias) | Low risk | List and numbered bottles provided by promoter. Participants and researchers blinded |
| Blinding (performance bias and detection bias) | Low risk | 1 single assessor blinded to allocation |
| Incomplete outcome data (attrition bias) | High risk | 56% attrition (antiseptic 50%, placebo 61%) for outcome of interest (salivary flow rates) at 4 weeks |
| Selective reporting (reporting bias) | High risk | Xerostomia not reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: North America and Europe Number of centres: 46 hospitals Date of conduct: August 2005 to September 2007 | |
| Participants | Inclusion criteria: newly diagnosed unresected stage III to IV SCC of oral cavity, oropharynx, nasopharynx, hypopharynx or larynx, planned RT dose of more than 50 Gy to 2 subsites or oral cavity and oropharynx Exclusion criteria: evidence of secondary malignancy Age: mean 55.5 (SD 8.5) Gender: 159 M, 29 F Cancer type: SCC of oral cavity, oropharynx, nasopharynx, hypopharynx or larynx Radiotherapy: mean 68 Gy in both arms for 43 days Chemotherapy: cisplatin 100 mg/m² IV infusion on days 1, 22, and 43 of RT Number randomised: 188 (94 per group) Number evaluated: 188, 185 adverse events | |
| Interventions | Palifermin versus placebo Palifermin administered IV at 180 µg/Kg over a period of 30 to 60 seconds, in 8 weekly doses 3 days. Bolus injection before radiotherapy, then at weekend Placebo: matching as above (1.2 ml of sterile water +) Follow‐up: median follow‐up 25.9 months palifermin, 25.0 placebo | |
| Outcomes | Xerostomia: incidence of grade ≥ 2 xerostomia (Common Terminology Criteria for Adverse Events (CTCAE) v 3.0 Dry Mouth/Xerostomia scale ‐ info from trials registry), assessed at months 4, 6, 8, 10, 12, reported only at month 4 Salivary flow rates: not reported Adverse effects: assessed by Common Terminology Criteria for Adverse Events: nausea, constipation, decreased weight, vomiting, anaemia, leukopenia, fatigue, dehydration Survival data: overall tumour response, time to locoregional tumour failure, incidence of secondary primary tumours, overall and progression‐free survival Other oral symptoms: dysphagia (difficulty in swallowing), OMWQ‐HN 0 (no soreness) to 4 (extreme soreness) scale for mouth and throat soreness (assessed twice weekly by trained evaluators during radiochemotherapy) Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported | |
| Funding | Externally funded by Amgen GSK | |
| Trial registration | NCT00101582 (clinicaltrials.gov/show/NCT00101582) | |
| Sample size calculation presented | Reported | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Centralised randomisation system. 1:1 allocation ratio |
| Allocation concealment (selection bias) | Low risk | Centralised randomisation for all sites, probably allocation concealment |
| Blinding (performance bias and detection bias) | Low risk | Quote: "placebo‐controlled, double‐blind study" |
| Blinding (performance bias and detection bias) | Low risk | Quote: "placebo‐controlled, double‐blind study" |
| Incomplete outcome data (attrition bias) | Low risk | All cases accounted for. ITT analysis (patients having no assessment assumed to have event) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. Low risk for xerostomia at the time point used in meta‐analysis (4 months) ‐ however, it should be noted that xerostomia was measured up to 12 months but data not reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Taiwan, Republic of China Number of centres: 1 Date of enrolment: January 2003 to November 2004 | |
| Participants | Inclusion criteria: histological evidence of carcinoma of head and neck, to receive RT, life expectancy ≥ 3 months, ECOG status ≤ 2. Criteria such as white blood cells, platelets, haemoglobin had to be within certain parameters Exclusion criteria: prior RT, presence of oral lesions, severe organ failure, brain metastasis Age: TWBXM: mean 51 (SD 15); placebo: 54 (SD 16) Gender: TWBXM: 29 M, 9 F; placebo: 32 M 3 F Cancer type: treatment group: head and neck cancer stage 0 = 4, I = 4, II = 10, III = 4, IVA = 12, IVB = 4. Control group: head and neck cancer stage 0 = 3, I = 5, II = 8, III = 4, IVA = 10, IVB = 5 Radiotherapy: TWBXM: mean dose 6944.9 cGy; placebo: mean dose 7098.4 cGy Chemotherapy: not mentioned probably not given Number randomised: 73 (TWBXM 38; placebo 35) Number evaluated: 71 (TWBXM 38; placebo 33) | |
| Interventions | Traditional Chinese medicine (TWBXM) versus placebo Tianwang Buxin Mini‐pills (TWBXM) ‐ 13 herbs listed in paper Placebo made of starch and designed to taste and look similar to intervention 3 g orally 3 times daily starting from initiation of RT until 1 month after RT completion Follow‐up: end of RT (end of RT for dichotomous data, 1 month postRT for continuous data) | |
| Outcomes | Xerostomia: RTOG grades by evaluating physician ‐ none, slight, moderate mouth dryness Salivary flow rates: not reported Adverse effects: EORTC QLQ‐C30 ‐ skin, nausea, vomiting, leukopenia, fatigue, pain, dyspnoea, insomnia, appetite loss, constipation, diarrhoea, body weight loss Survival data: not reported Other oral symptoms: EORTC QLQ‐C30 ‐ pain, swallowing, speech problems, mouth opening, teeth, mucositis, oral mucosa, loss of taste Other oral signs: not reported Quality of life: EORTC QLQ‐C30 and head and neck specific QLQ‐H & N35 Patient satisfaction: not reported Cost data: not reported | |
| Funding | Government. Committee on Chinese Medicine and Pharmacy, Department of Health, Executive Yuan, Taiwan (grants CCMP92‐RD‐011 and CCMP93‐RD‐008). Quote: "All authors declare that there are no conflicts of interest" | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | Problematic data ‐ emailed corresponding author 22 February 2016 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...randomized to study medicine according to a computer‐generated randomization schedule..." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Low risk | Quote: "All patients, the study nurses and doctors were blinded to the group of the treatment group" |
| Blinding (performance bias and detection bias) | Low risk | Quote: "All patients, the study nurses and doctors were blinded to the group of the treatment group" |
| Incomplete outcome data (attrition bias) | Low risk | The dropout rate was 3% to 7% (data reported inconsistently in the report) at the end of RT, which is the preferred time point for this review. However, there were 29 (40%) dropouts at the time point of 1 month postRT |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: USA Number of centres: 1 Date of conduct: not stated | |
| Participants | Inclusion criteria: not reported Exclusion criteria: not reported Age: pilocarpine: mean 51.5 years (range 29 to 76); placebo: 54.8 years (range 47 to 68) Gender (M:F): pilocarpine 9:2, placebo 9:2 Cancer type: nasopharyngeal cancer Radiotherapy: total dose 60 to 70 Gy Chemotherapy: some Number randomised: 22 (11 per group) Number evaluated: 11 per group for incidence of dry mouth. There are discrepancies over the numbers | |
| Interventions | Pilocarpine versus placebo Pilocarpine: 5 mg tablets 3 times daily ‐ 4 times daily, 2 weeks before RT and concurrently with RT Placebo | |
| Outcomes | Xerostomia: questionnaire Salivary flow rates: resting salivary flow Adverse effects: sweating, lacrimation (excess tears, crying), rhinorrhoea (watery discharge from the nose), diarrhoea, nausea, rhinitis, blurred vision, constipation, neuropathy Survival data: not reported Other oral symptoms: mucositis, dysphagia (difficulty in swallowing), dysgeusia (taste disturbance), pain Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: prior to radiation, weekly during treatment, end of RT, 3 months after RT | |
| Funding | Supported by a grant from MGI Pharma Inc. | |
| Trial registration | Not registered or published | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Contact with authors confirmed that the random allocation was conducted by pharmaceutical company, producing coded containers |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation sequence was provided in a logo‐type format and kept by our dental assistant (in a locked cabinet)" |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind" |
| Blinding (performance bias and detection bias) | Low risk | Quote: "double‐blind" |
| Incomplete outcome data (attrition bias) | Unclear risk | 2 dropped out because of adverse events (severe nausea and vomiting, and tumour growth). Unclear reasons for all dropouts for xerostomia outcome (6) |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: India Number of centres: 1 Date of conduct: not reported | |
| Participants | Inclusion criteria: locally advanced histologically proven squamous cell carcinoma of head and neck region. 75% or more of each parotid gland was included in the radiation portal. Age above 18 years. Expected survival > 12 months. Karnofsky Performance Status > 60. Normal haemogram, renal and liver functions, normal calcium levels Exclusion criteria: prior treatment for malignancy, associated hypotension or distant metastases Age: not reported Gender: 65% M Cancer type: head and neck Radiotherapy: external radiation therapy with gamma rays to a dose of 66 to 72 Gy with conventional fractionation Chemotherapy: 40 mg/m² cisplatin weekly Number randomised: 170 (85 per group) Number evaluated: 170 (85 per group) | |
| Interventions | Amifostine versus no intervention Amifostine: 250 mg IV over 3 minutes for 4 days a week from day 1 of radiotherapy until completion of treatment | |
| Outcomes | Xerostomia: acute and late xerostomia grade 2 and above (RTOG 0‐4 scale) Salivary flow rates: parotid scintigraphy (no data) Adverse effects: not reported Survival data: disease‐free survival at 24 months and tumour response Other oral symptoms: mucositis (RTOG) Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported | |
| Funding | Not reported | |
| Trial registration | Not registered or published | |
| Sample size calculation presented | No | |
| Notes | Abstract with additional information provided by study authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised but unclear method |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) | High risk | Not possible due to 'no treatment' group |
| Blinding (performance bias and detection bias) | High risk | Not possible due to 'no treatment' group. Xerostomia is subjective outcome |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | High risk | No information on adverse events |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: China Number of centres: 1 Date of conduct: October 2003 to October 2005 | |
| Participants | Inclusion criteria: quote: "1) H&N SC patients diagnosed with pathological examinations, who cannot endure surgery or cannot be treated with radical resection; 2) first‐visit patients who have not received cancer treatment, with no tumour metastasis; 3) WBC > 4.0*109/L, platelet count > 100.0*109/L, Hb > 10 g/L, normal function of heart, lungs, liver and kidneys; 4) Karnofsky score ≥ 60; 5) patients gave informed consent" Exclusion criteria: see above Age at baseline (years): amifostine: median 58; control: median 57 Gender: amifostine: 12 M, 6 F; control: 12 M, 6 F Cancer type: head and neck squamous carcinoma (amifostine/control): oral = 4/3, nasopharyngeal = 6/6, oropharyngeal = 5/5, hypopharyngeal = 1/1, laryngeal = 1/1, paranasalsinus = 1/1, glottis = 0/1 Radiotherapy: quote: "Primary site of tumour and cervical lymph nodes: 74.4 Gy overall, 1.2 Gy per time, 2 times per day (> 6 hours between these 2 times), for 4 to 5 weeks; separate routine fractionated RT for the neck area: 50 Gy overall, 25 times, 5 weeks" Chemotherapy: quote: "Continued IV infusion of 5 FU 750 mg/m² using pump, 24 hours per day for 3 days. On the 5th day after 5 FU use, intravenous infusion of cisplatin 50 mg/m² with 250 or 500 ml saline (2 to 4 hours). IV infusion of docetaxel 75 mg/m² with 250 ml saline (< 1.5 hours). Chemotherapy performed in rounds: 1st round – during RT, 2nd round – begin in the 5th week after RT, 3rd round – begin in the 9th week after RT" Number randomised: 37 (amifostine 18, control 19) Number evaluated: 36 (amifostine 18, control 18) | |
| Interventions | Amifostine versus no intervention Amifostine: quote: "400 mg amifostine each time, intravenous infusion 15 minutes before RT and chemotherapy (finish in 5 to 7 minutes)" Control: no intervention other than the same RT and chemotherapy | |
| Outcomes | Xerostomia: only results for 'acute' and 'chronic' dry mouth reported; time and standards for assessments not described Salivary flow rates: not reported Adverse effects: hypotension, nausea, vomiting, dizziness, fatigue, hiccup, sneezing, facial flush Survival data: not reported Other oral symptoms: mucositis Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: not reported (therefore unable to use data) | |
| Funding | Not reported; conflicts of interest: not reported | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients were randomized to" |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding (performance bias and detection bias) | High risk | Amifostine versus no intervention. Blinding not possible |
| Blinding (performance bias and detection bias) | High risk | Blinding not mentioned. Xerostomia is subjective measure |
| Incomplete outcome data (attrition bias) | Unclear risk | Quote: "1 patient in the amifostine group quitted due to financial reasons" |
| Selective reporting (reporting bias) | Unclear risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Brazil Number of centres: 1 Date of conduct: not reported | |
| Participants | Inclusion criteria: newly diagnosed head and neck cancer beginning treatment with RT Exclusion criteria: previous RT, concomitant chemotherapy, cardiopathy, hypertension, diabetes, allergy to pilocarpine, Sjögren syndrome, salivary gland tumours, chronic lung disease, glaucoma, peptic ulcer, taking betablockers or drugs that could alter salivary flow Age: mean 60 years (not given by group) Gender (M:F): 8:3 Cancer type: oral (n = 1); oropharynx (n = 3); mouth floor and tongue (n = 2); larynx (n = 4); pharynx (n = 1) Radiotherapy: 35 to 50 Gy, with daily doses about 2 Gy Chemotherapy: none Number randomised: unclear whether 29 or 11 (see attrition bias) Number evaluated: 11 (pilocarpine 5, placebo 6) | |
| Interventions | Pilocarpine versus placebo Pilocarpine: 5 mg 3 times daily for duration of RT Placebo: saline solution 3 times daily for duration of RT | |
| Outcomes | Xerostomia: patient‐reported feeling of dry mouth Salivary flow rates: unstimulated (USF) and stimulated saliva (SSF) (ml/min) Adverse effects: reported narratively Survival data: locoregional control: not reported Other oral symptoms: oral mucositis, ulcers Other oral signs: difficulty in eating Quality of life: only eating Patient satisfaction: not reported Cost data: not reported Timing of assessment: weekly during RT (4 weeks) | |
| Funding | The National Research Council (CNPq) | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...dispensing pharmacy held custody of the samples, separating those from the group who took pilocarpine solution from those which took the placebo. All patients were assigned a number corresponding to the medicine bottle. Researchers were not granted access to that information prior to the end of the survey" |
| Allocation concealment (selection bias) | Low risk | Quote: "...dispensing pharmacy held custody of the samples, separating those from the group who took pilocarpine solution from those which took the placebo. All patients were assigned a number corresponding to the medicine bottle. Researchers were not granted access to that information prior to the end of the survey" |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind ‐ see above |
| Blinding (performance bias and detection bias) | Low risk | Double‐blind ‐ see above |
| Incomplete outcome data (attrition bias) | High risk | Quote: "We pre‐selected 29 patients; however, the careful selection of the population was directly reflected in the number of enrolled patients and in the end, only 11 were included in the survey. We consider that this low number is a result not only of the exclusion stemming from previously established eligibility criteria but also from the breach of protocol" |
| Selective reporting (reporting bias) | High risk | Poorly reported data for xerostomia and no adverse events |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: India Number of centres: 1 Date of conduct: not stated | |
| Participants | Inclusion criteria: carcinoma of the head and neck stage III and IV, aged between 30 and 70, to receive RT, normal haematology, biochemistry and Karnofsky Performance Index > 70% Exclusion criteria: poor general condition, associated co‐morbidities, psychiatric conditions Age: 30‐70 Gender: unclear Cancer type: SCC of head and neck Radiotherapy: 60 Gy on cobolt 60 for 30 days over 6 weeks Chemotherapy: not reported but probably none Number randomised: 20 or 40 unclear Number evaluated: no apparent dropouts but unclear how many started | |
| Interventions | Tulasi (Ocimum Sanctum) versus placebo Tulasi (Ocimum Sanctum) Placebo: vitamin B complex 2 capsules of 250 mg orally half an hour prior to RT *Healthy control group also included but not used (not randomised) Follow‐up: 29 days of RT | |
| Outcomes | Xerostomia: unclear, quote: "patients were assessed at the end of every week for grade of mucositis, skin reaction and salivary status" Salivary flow rates: not reported Adverse effects: not reported Survival data: not reported Other oral symptoms: not reported Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported | |
| Funding | Not reported | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | No useable data ‐ emailed corresponding author 27 January 2016 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomized into 2 arms" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | Low risk | Placebo‐controlled |
| Blinding (performance bias and detection bias) | Low risk | Placebo‐controlled |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | High risk | No adverse event data reported. Poorly reported xerostomia |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Slovenia Number of centres: 1 Dates and duration of recruitment period: not stated | |
| Participants | Inclusion criteria: irradiated for head and neck cancer and salivary glands included in the irradiation field Exclusion criteria: not reported Age: aged 32 to 72, median 62 years Gender (M:F): 60:9 Cancer type: oral cavity (n = 14), oropharynx (n = 33), hypopharynx (n = 8), larynx (n = 11), other (n = 3) (evenly distributed across groups) Radiotherapy: 5 Gy per day, 5 days a week. Irradiated volume reduced twice during irradiation treatment: at 40 Gy for shielding the spinal cord and at 60 Gy for treating the area of original disease, up to 70 Gy. Postoperative patients received 50 Gy ‐ 56 Gy with parallel opposed portals only. 44 patients had postoperative RT and 25 were treated by RT alone Chemotherapy: not stated Number randomised: 69 (A: 9, B: 30, C: 30) Number evaluated: 69 (A: 9, B: 30, C: 30) | |
| Interventions | Pilocarpine (postRT) + Biperiden (during RT) versus no intervention Group Aª: pilocarpine during RT and 6 weeks after. Pilocarpine hydrochloride (5 mg) perorally 3 times daily administered 1 hour before irradiation | |
| Outcomes | Xerostomia: not reported Salivary flow rates: mean quantity of non‐stimulated saliva secretion (ml/min) Adverse effects: not reported Survival data: not reported Other oral symptoms: mucositis, swallowing WHO criteria Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: end of RT, 3 months, 6 months and 12 months after end of RT | |
| Funding | Source of funding: none | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ªGroup A data not used: randomisation to Group A was stopped after the first 9 patients for ethical reasons ‐ 3 months after RT total cessation of saliva secretion was observed in all except 1 patient Follow‐up: 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Information provided by author: "Sequence centrally generated" |
| Allocation concealment (selection bias) | Low risk | Author included the following in an email "randomization with permuted blocs, participants were allocated to the treatment groups randomly. Allocation sequence was generated centrally, treating physician (radiologist) enrolled patient and participants were assigned to the groups by specialist in dental medicine" Comment: centralised random allocation and was probably adequately concealed |
| Blinding (performance bias and detection bias) | High risk | No blinding undertaken |
| Blinding (performance bias and detection bias) | Low risk | Salivary flow objective measure |
| Incomplete outcome data (attrition bias) | Low risk | All randomised patients included in analysis |
| Selective reporting (reporting bias) | High risk | Xerostomia and adverse events not reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Thailand Number of centres: 1 Date of recruitment: January 1998 to January 1999 | |
| Participants | Inclusion criteria: histologically documented squamous cell carcinoma of head and neck who would receive definite or postoperative radiation Exclusion criteria: significant uncontrolled cardiac, pulmonary, renal or occular disease or required tricyclic antidepressants or antihistamine with anticholinergic effects, betablocker, pilocarpine for ophthalmic indications or chemotherapy Age: pilocarpine: 57 years; placebo: 58 years Gender (M:F): 49:11 Cancer type: oropharynx (n = 27); nasopharynx (n = 14); others (n = 19) Radiotherapy: Cobalt‐60 or 6 MV photon machine. Standard arrangement ‐ opposing lateral portals, loaded 1:1 and/or anterior low neck field. Both parotids treated to a dose of at least 50 Gy with an equal daily dose of 1.8‐2.0 Gy Chemotherapy: none Number randomised: 60 (30 per group) Number evaluated: 47 (25 pilocarpine; 22 placebo) | |
| Interventions | Pilocarpine versus placebo Pilocarpine jelly: self administered 5 mg 3 times daily at meal times for duration of RT (7 weeks) Follow‐up: 6 months after RT | |
| Outcomes | Xerostomia: subjective evaluation scores for xerostomia questionnaire (100 mm VAS for each of 5 questions) Salivary flow rates: not reported Adverse effects: reported ("non‐specific symptoms such as nausea, vomiting, dizziness, urinary frequency, palpitation, sweating and tearing") Survival data: not reported Other oral symptoms: not reported Other oral signs: disability to oral intake, amount of meals, use of analgesics Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: 6 months after RT | |
| Funding | Faculty of Medicine, Prince of Songkla University | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Information provided by author: "random number table" |
| Allocation concealment (selection bias) | Low risk | Information provided by author: "clinician not participating in study generated allocation sequence. Treatment codes concealed in sealed envelopes. Treatment coding not disclosed to investigator or patient" |
| Blinding (performance bias and detection bias) | Low risk | Quote: "identically appearing placebo... patients and investigators were unaware of which treatment was administered" |
| Blinding (performance bias and detection bias) | Low risk | Information provided by author: "treatment code was disclosed to the investigator only after completion of the analysis of the results of the study" |
| Incomplete outcome data (attrition bias) | Unclear risk | 22% dropout rate |
| Selective reporting (reporting bias) | High risk | Poor reporting of xerostomia without SD |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Germany Number of centres: 1 Date of conduct: October 1996 to February 1999 | |
| Participants | Inclusion criteria: advanced tumours of larynx, oro or hypopharynx, all received surgery and were to receive RT plus CT, pathologically confirmed cancer, between 18 and 70 years, performance status WHO 0‐II, adequate bone marrow and liver and renal function Exclusion criteria: severe internal medical disorders, hyper or hypotension, history of RT or CT, women with inadequate contraception, secondary malignancies, recurrent tumours Age: amifostine: mean 53.5; control: mean 55.1 Gender: amifostine: M 21, F 4; control: M 19, F 6 Cancer type: amifostine: SSC (24) and adenocarcinoma (1); control: SSC (24) and lymphoepithelial cancer (1) Radiotherapy: conventionally fractionated RT (5 x 2 Gy/week). Total dose 60 Gy for completely resected tumours, 70 Gy incomplete resected tumours Chemotherapy: individually planned. 70 mg/m² carboplatin on treatment days 1 to 5 and 29 to 33 just before RT session (all participants had this) Number randomised: 56 (not reported by group) Number evaluated: 50 (25 per group); 41 (amifostine 19, control 22) for xerostomia | |
| Interventions | Amifostine versus no intervention 250 mg amifostine given intravenously as short infusion over 10 to 15 minutes | |
| Outcomes | Xerostomia: RTOG (not useable) Salivary flow rates: not reported Adverse effects: skin toxicity, loss of hair Survival data: not reported Other oral symptoms: oral mucositis Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: weekly during RT until week 6 (during RT; no usable data) | |
| Funding | Not reported | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...were randomized to receive..." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) | High risk | No treatment control group |
| Blinding (performance bias and detection bias) | High risk | Xerostomia is a subjective assessment by the patient |
| Incomplete outcome data (attrition bias) | High risk | Reasons for dropouts by study group unclear. 6 dropouts altogether: allergic skin reaction (1) after 5th application of amifostine, patient refusal (3), second malignancy (1), surgical complications (1). 27% attrition overall for xerostomia ‐ participants with larynx cancer excluded from analysis |
| Selective reporting (reporting bias) | High risk | Xerostomia selectively and poorly reported (only significant data reported) |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: USA Number of centres: multisite unclear how many Date of conduct and duration of recruitment period: not stated | |
| Participants | Inclusion criteria: scheduled to receive external beam radiation therapy to the major salivary glands, completely or partially Exclusion criteria: significant cardiovascular, pulmonary, hepatic, or pancreatic disorders or gastroduodenal ulcers. Women with childbearing potential were required to have a pregnancy test with negative results before entry and to use contraception during the study Age: pilocarpine: 22 to 65 years, mean 42.6 years; placebo: 21 to 56 years, mean 40.2 years Gender (M:F): 6:4 Cancer type: mix of SCC, mucoepidermoid carcinoma, Hodgkin disease and malignant lymphoma Radiotherapy: mean dose 41.9 Gy Chemotherapy: not stated Number randomised: 10 (5 per group) Number evaluated: 9 (pilocarpine 5; placebo 4) | |
| Interventions | Pilocarpine versus placebo Pilocarpine: 5 mg capsules 4 times daily for 3 months starting the day before RT | |
| Outcomes | Xerostomia: subjective assessment using questionnaire Salivary flow rates: stimulated salivary flow rates (μl/min) Adverse effects: not reported Survival data: quote: "all tumour responded favourably and all were in complete remission for the remainder of the study" Other oral symptoms: not reported Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: 3, 4, 5, 6 and 12 months from start of RT | |
| Funding | National Institute of Dental and Craniofacial Research (NIDCR). Randomisation sequence generation and allocation were undertaken by US National Institutes of Health (NIH) pharmaceutical service | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation not explicit but conducted by NIH Pharmaceutical Development Service |
| Allocation concealment (selection bias) | Low risk | Conducted by NIH Pharmaceutical Development Service; intervention dispensed in coded bottles |
| Blinding (performance bias and detection bias) | Low risk | Pilocarpine versus placebo |
| Blinding (performance bias and detection bias) | Low risk | Participants are blinded and providing saliva and questionnaire data |
| Incomplete outcome data (attrition bias) | Low risk | 1/5 participants in placebo group dropped out. No dropouts in pilocarpine group |
| Selective reporting (reporting bias) | High risk | No adverse event data reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Thailand Number of centres: 5 Date of recruitment: February 1999 to September 2001 | |
| Participants | Inclusion criteria: histological proven squamous cell carcinoma of head and neck region; ECOG performance statue 0‐2; adequate bone marrow, liver and renal functions; age 18‐70 years; no prior definite/radical surgery, chemotherapy, radiotherapy or biological response modifier; no evidence of distant metastasis; life expectancy ≥ 12 months; able to comply with a follow‐up schedule; weight loss ≤ 10% in previous 3 months Exclusion criteria: concomitant malignant disease in other parts of the body; active uncontrolled infection; pregnant or lactating women; medical or psychiatric illness that compromise the patient's ability to complete the study; concomitant use of chemotherapy Age: amifostine: mean 55 (23‐70); control: mean 52 (23 to 69) Gender: amifostine: 24 M, 8 F; control: 27 M, 8 F Cancer type: oral cavity, oropharynx, nasopharynx, larynx, hypopharynx Radiotherapy: standard fractionation (2 Gy, 5 days a week). Duration: 5 to 8 weeks. Definite RT = 70 Gy. Postoperative RT = 50 Gy. Amifostine group: definite RT = 15; postoperative RT = 17. Control group: definite RT = 18; postoperative RT = 17 Number randomised: 67 (amifostine 32, control 35) Number evaluated: 62 (amifostine 32, control 30) | |
| Interventions | Amifostine versus no intervention Amifostine: (Ethyol) (200 mg/m²) IV (3 to 5 min), 30 min before RT. 5 consecutive days a week for 5 to 7 weeks (during RT) | |
| Outcomes | Xerostomia: 1) questionnaire (6 questions) (RTOG/EORTC acute and late radiation morbidity scoring criteria) for xerostomia: dryness of mouth, oral comfort, quality of sleep, ability to speak, ability to chew and swallow and ability to wear dentures (average score 0 to 10: 0 = normal); 2) RTOG 0 to 4 scale ‐ grade 2 and above Salivary flow rates: unstimulated and stimulated whole saliva collection (mg/5 min) and scintigraphy Adverse effects: nausea, vomiting, hypotension Survival data: disease‐free survival Other oral symptoms: mucositis (RTOG grade 2‐3) Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessments: weekly during RT (for 6 weeks), then at end of RT and at 1, 2, 3, 6, 12, 18 and 24 months after RT; survival at 24 months after RT | |
| Funding | Source of funding: unclear | |
| Trial registration | Not registered or published | |
| Sample size calculation presented | No | |
| Notes | Information on randomisation, and numbers and SDs from correspondence | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Central allocation |
| Blinding (performance bias and detection bias) | High risk | Amifostine versus no intervention |
| Blinding (performance bias and detection bias) | High risk | Xerostomia is subjective measure |
| Incomplete outcome data (attrition bias) | High risk | Quote: "We excluded 5 cases in the control as they did not have salivary gland function, or had severe salivary gland impairment" Comment: we are assuming that there were no other dropouts (assessment made on 32 in amifostine, 30 in control) |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: China Number of centres: 1 Date of recruitment: May 1996 to October 1997 | |
| Participants | Inclusion criteria: patients with head and neck cancer, pathology confirmed, aged 20 to 70 and radiation fields including the main salivary glands, total dose > 60 Gy Exclusion criteria: severe systemic disease or history of chronic diseases of the salivary glands Age (years): treatment: mean 46.8 (range 22 to 68); placebo: mean 45.5 (range 24 to 70) Gender: treatment: 20 M, 4 F; placebo: 21 M, 5 F Cancer type: treatment: nasopharyngeal = 17, throat = 4, tonsil = 3; placebo: nasopharyngeal = 18, throat = 4, tonsil = 3, hard palate = 1 Radiotherapy: 6 MV x‐ray with accelerator linear, SL‐75 produced by Philips. 2 Gy, 5 times per week for 6 to 7 weeks (total dose 60‐70 Gy) Chemotherapy: none Number randomised: 50 (treatment 24, placebo 26) Number evaluated: 50 (treatment 24, placebo 26) | |
| Interventions | Chinese medicine versus placebo (Dobell's solution) Chinese medicine and Dobell's solution (20 ml 3 times daily) rinsing and spray inhalation for the duration of the RT starting from the beginning of RT Placebo: Dobell's solution Follow‐up: end of RT | |
| Outcomes | Xerostomia: subjective evaluation score (VAS) for xerostomia, before and during the RT (at 10, 20, 30, 40, 50 and 60 Gy) Salivary flow rates: stimulated salivary flow rates, in morning around 9 am (at least 1 hour after breakfast) patients rinsed with water, then chewed gum and saliva collected after 5 minutes, before and during the RT (at 20, 40 and 60 Gy) Adverse effects: not reported Survival data: not reported Other oral symptoms: not reported Other oral signs: not reported Quality of life: not reported Patient satisfaction: not reported Cost data: not reported | |
| Funding | Not reported; conflicts of interest: not reported | |
| Trial registration | Not registered | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly divided" Comment: no further details given |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | Low risk | Placebo used |
| Blinding (performance bias and detection bias) | Low risk | Placebo used |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | High risk | Adverse effects not reported. Data for xerostomia not usable (reported as a graph with no SDs) |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Canada Number of centres: 1 Date and duration of recruitment period: not stated | |
| Participants | Inclusion criteria: squamous cell head and neck cancer, scheduled to receive RT with the inclusion of > 50% of both parotid glands in the radiation fields to doses > 50 Gy. Primary treatment and postoperative RT participants Exclusion criteria: previous RT or chemotherapy or pre‐existing xerostomia from other causes. Medical contraindication to pilocarpine Age: pilocarpine: mean 56.2 years; placebo: mean 57.8 years Gender (M:F): 94:36 Cancer type: SSC of head and neck Radiotherapy: 60‐70 Gy in 2 Gy daily fractions (68 participants), 60‐64 Gy in 40 fractions during 4 weeks using twice daily treatments (33 participants), 50 Gy in 25 daily fractions (7 participants), 60 Gy in 25 daily fractions (8 participants) and 51 Gy in 20 daily fractions (7 participants) Chemotherapy: not stated Number randomised: 130 (65 per group) Number evaluated: for xerostomia: 92 (pilocarpine 48, placebo 44) at 3 months postRT; 87 (pilocarpine 46, placebo 41) at 6 months postRT | |
| Interventions | Pilocarpine versus placebo Pilocarpine: 5 mg tablets 3 times daily starting day 1 of RT and continued until 1 month after completion of RT | |
| Outcomes | Xerostomia: VAS (patient‐completed) assessing patient's perception of dryness of their mouth (7 questions). Scores from 0 to 100, low scores = most difficulty Salivary flow rates: not reported Adverse effects: excessive sweating, acute toxicity of therapy (RTOG) Survival data: not reported Other oral symptoms: not reported Other oral signs: feeding tube inserted Quality of life: patients' quality of life (McMaster University Head and Neck Questionnaire (HNRQ)). Score 1‐7, lower score = poorer quality of life Patient satisfaction: not reported Cost data: not reported Timing of assessment: 1, 3 and 6 months after end of RT | |
| Funding | Unrestricted educational grant from Pharmacia Canada | |
| Trial registration | Not registered | |
| Sample size calculation presented | Yes | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information |
| Blinding (performance bias and detection bias) | Low risk | Pilocarpine versus placebo, "double‐blind" |
| Blinding (performance bias and detection bias) | Low risk | Self reported |
| Incomplete outcome data (attrition bias) | High risk | 130 participants randomised. 19/65 dropouts in pilocarpine group; 24/65 dropouts in placebo group. 8 in pilocarpine and 4 in placebo dropped out for toxicity, otherwise reasons unclear |
| Selective reporting (reporting bias) | Low risk | Xerostomia and adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Location: Japan Number of centres: 1 Date of conduct: January and October 2009 | |
| Participants | Inclusion criteria: head and neck cancer scheduled for RT or RT + CT Exclusion criteria: not reported Age: polaprezinc: 67.4 (range 53 to 78); control: 62.7 (range 35 to 86) Gender (M:F): polaprezinc 13:3, control 11:4 Cancer type: head and neck, mainly pharyngeal and laryngeal Radiotherapy (mean dose and duration): polaprezinc: 51 Gy (range 30‐70), 37 days (range 21‐55); control: 58 Gy (range 36‐70), 45 days (range 28‐79) Chemotherapy: some but unclear what, concomitantly carried out for 56% of polaprezinc and 80% of control Number randomised: 31 (polaprezinc 16, control 15) Number evaluated: 31 (polaprezinc 16, control 15) | |
| Interventions | Polaprezinc versus azulene oral rinse Polaprezinc granules (0.5 g) were dissolved in 20 ml of 5% sodium alginate Azulene oral rinse prepared by pouring 7 drops of 4% solution into 100 ml water Both groups administered via oral rinse. Rinse for 3 minutes, 4 times daily, from start to end RT. After rinsing, polaprezinc swallowed but azulene spat out. From start to end of RT | |
| Outcomes | Xerostomia: CTCAE 0‐3 grade Salivary flow rates: not reported Adverse effects: not reported Survival data: tumour response by RECIST criteria for specific group of patients Other oral symptoms: pain, dysgeusia (taste disturbance), mucositis Other oral signs: amount of meals Quality of life: not reported Patient satisfaction: not reported Cost data: not reported Timing of assessment: over RT period (maximum score) | |
| Funding | Source of funding unclear | |
| Trial registration | Unclear | |
| Sample size calculation presented | No | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...were randomly assigned". No details given |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding (performance bias and detection bias) | High risk | None. Polaprezinc swallowed after rinsing, while azulene is spat out. Quote: "open trial" |
| Blinding (performance bias and detection bias) | High risk | Xerostomia subjective measurement, and different interventions |
| Incomplete outcome data (attrition bias) | Low risk | None |
| Selective reporting (reporting bias) | High risk | No adverse events reported |
| Other bias | Low risk | No other sources of bias are apparent |
CHX = chlorhexidine; CRT = chemoradiotherapy; CT = chemotherapy; CTCAE = Common Terminology Criteria for Adverse Events; ECOG = Eastern Cooperative Oncology Group score; EORTC = European Organisation for Research and Treatment of Cancer; F = female; G‐CSF = granulocyte‐colony stimulating factor; GI = gastrointestinal; GM‐CSF = granulocyte‐macrophage colony‐stimulating factor; Gy = gray; HNSCC = head and neck squamous cell carcinoma; IMRT = intensity‐modulated radiation therapy; ITT = intention‐to‐treat; IV = intravenous; KGFs = keratinocyte growth factors; M = male; min = minute; MV = megavolt; NCI CTC = National Cancer Institute Common Toxicity Criteria; NCIC CTG ECTC = National Cancer Institute of Canada Clinical Trials Group Expanded Common Toxicity Criteria; OMAS = Oral Mucositis Assessment Scale; QoL = quality of life; RECIST = Response Evaluation Criteria In Solid Tumours; RT = radiotherapy; RTOG = Radiation Therapy Oncology Group; SC = subcutaneous; SCC = squamous cell carcinoma; SCCHN = squamous cell carcinoma of the head and neck; SD = standard deviation; TNM = tumour, node and metastasis; VAS = visual analogue scale; WHO = World Health Organization; wt/vol = weight/volume.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Not an RCT ‐ compares a subcutaneous amifostine group with the intravenous amifostine and no‐treatment arms from another study (Brizel 2000) | |
| Abstract; insufficient information | |
| CCT | |
| Not head and neck cancer patients | |
| Radioactive iodine not radiotherapy | |
| Abstract; insufficient information | |
| Salivary gland dysfunction was not a reported outcome | |
| Data unavailable for the outcomes of interest to this review | |
| Salivary gland dysfunction was not a reported outcome | |
| Abstract; insufficient information | |
| Not an RCT | |
| Radioactive iodine not radiotherapy | |
| Unclear whether this is an RCT or not. Study authors contacted February 2016 but no reply received | |
| Salivary gland dysfunction was not a reported outcome | |
| Quasi‐randomised trial (case history number) | |
| Abstract; insufficient information | |
| Abstract; insufficient information | |
| Not an RCT | |
| Quasi‐randomised trial | |
| No formal assessment of salivary gland dysfunction; data not presented for head and neck cancer patients | |
| Abstract; insufficient information | |
| Abstract; insufficient information | |
| Quasi‐randomised trial (alternate assignment) | |
| Abstract; insufficient information | |
| Abstract; insufficient information | |
| Not an RCT | |
| Abstract; insufficient information | |
| Abstract; insufficient information | |
| Quasi‐randomised trial (alternate assignment) | |
| Abstract; insufficient information | |
| Abstract; insufficient information | |
| Quasi‐randomised trial (day of birth) | |
| Dissertation; unable to obtain a copy | |
| Abstract; insufficient information | |
| Control group not relevant for this review | |
| Tirapazamine is cancer treatment drug not a radiation protector | |
| Abstract; insufficient information | |
| Not an RCT | |
| Intervention not defined as a pharmacological agent | |
| Abstract; insufficient information | |
| Salivary gland dysfunction measured as an adverse event following administration of G‐CSF | |
| Not an RCT | |
| Not an RCT | |
| Unclear whether this is an RCT or not | |
| Abstract; insufficient information | |
| Not an RCT |
CCT = controlled clinical trial; G‐CSF = granulocyte‐colony stimulating factor; RCT = randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT |
| Participants | Nasopharynx cancer patients with poorly differentiated squamous carcinoma, at clinical phase III to VI, aged 25 to 69 years, first session of treatment, radiation field included > 75% of the area of salivary glands |
| Interventions | Amifostine versus no intervention |
| Outcomes | Xerostomia; salivary flow rates; adverse effects |
| Notes | Method/scale used to assess xerostomia unclear and further information required from study authors; the results do not have the potential to change any conclusions of the review |
RCT = randomised controlled trial.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Topical and oral melatonin for preventing concurrent radiochemotherapy induced oral mucositis and xerostomia in head and neck cancer patients |
| Methods | Parallel, double‐blind RCT |
| Participants | Head and neck cancer adult patients |
| Interventions | Topical and oral melatonin versus placebo |
| Outcomes | Xerostomia; oral mucositis; quality of life |
| Starting date | July 2013 |
| Contact information | Nutjaree Pratheepawanit Johns, Khon Kaen University |
| Notes |
RCT = randomised controlled trial.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.1 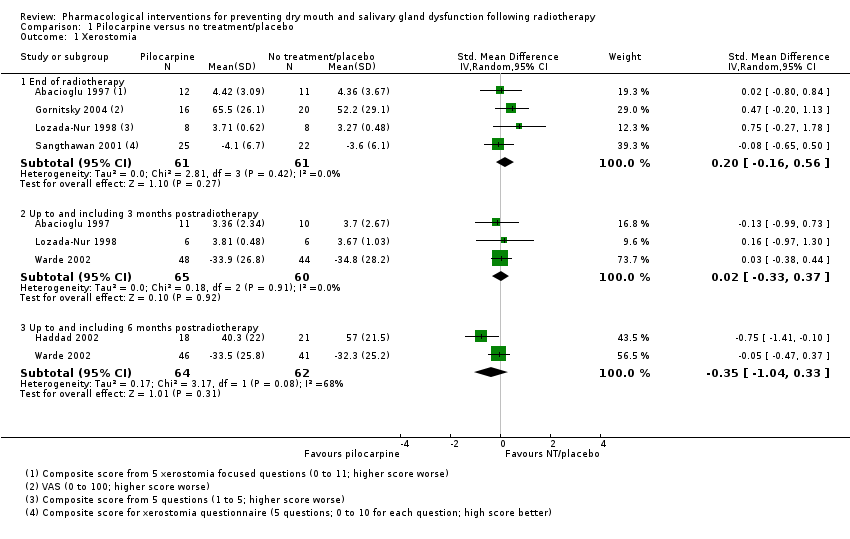 Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 1 Xerostomia. | ||||
| 1.1 End of radiotherapy | 4 | 122 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.16, 0.56] |
| 1.2 Up to and including 3 months postradiotherapy | 3 | 125 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.33, 0.37] |
| 1.3 Up to and including 6 months postradiotherapy | 2 | 126 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.04, 0.33] |
| 2 Xerostomia (LENT‐SOMA scale) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 2 Xerostomia (LENT‐SOMA scale). | ||||
| 2.1 Up to and including 6 months postradiotherapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Xerostomia Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 3 Xerostomia. | ||||
| 3.1 End of radiotherapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Up to and including 3 months postradiotherapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Salivary flow rate (unstimulated) Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 4 Salivary flow rate (unstimulated). | ||||
| 4.1 End of radiotherapy | 3 | 76 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.24, 0.72] |
| 4.2 Up to and including 3 months postradiotherapy | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐1.07, 0.54] |
| 5 Salivary flow rate (stimulated) Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 5 Salivary flow rate (stimulated). | ||||
| 5.1 End of radiotherapy | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.44, 0.59] |
| 5.2 Up to and including 3 months postradiotherapy | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.41, 1.21] |
| 5.3 Up to and including 6 months postradiotherapy | 1 | 9 | Std. Mean Difference (IV, Random, 95% CI) | 0.52 [‐0.84, 1.87] |
| 5.4 Up to and including 12 months postradiotherapy | 1 | 9 | Std. Mean Difference (IV, Random, 95% CI) | 0.53 [‐0.83, 1.88] |
| 6 Salivary flow rate (> 0 g) unstimulated Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.6 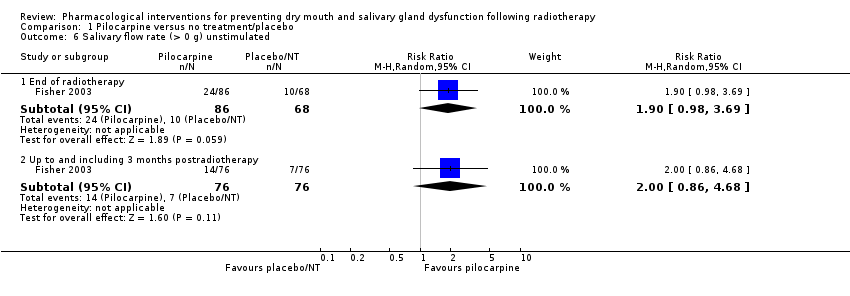 Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 6 Salivary flow rate (> 0 g) unstimulated. | ||||
| 6.1 End of radiotherapy | 1 | 154 | Risk Ratio (M‐H, Random, 95% CI) | 1.90 [0.98, 3.69] |
| 6.2 Up to and including 3 months postradiotherapy | 1 | 152 | Risk Ratio (M‐H, Random, 95% CI) | 2.0 [0.86, 4.68] |
| 7 Salivary flow rate (> 0 g) stimulated Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.7 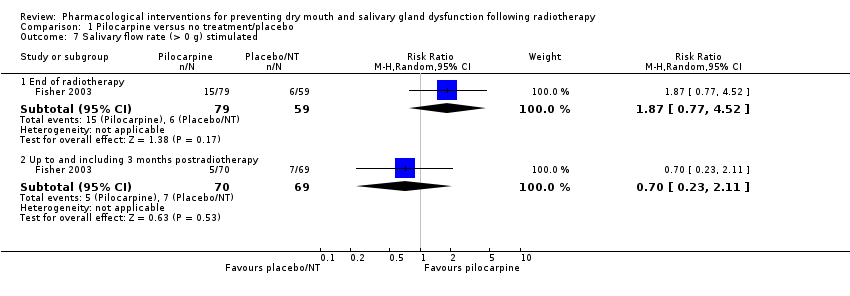 Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 7 Salivary flow rate (> 0 g) stimulated. | ||||
| 7.1 End of radiotherapy | 1 | 138 | Risk Ratio (M‐H, Random, 95% CI) | 1.87 [0.77, 4.52] |
| 7.2 Up to and including 3 months postradiotherapy | 1 | 139 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.23, 2.11] |
| 8 Overall survival Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 1.8  Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 8 Overall survival. | ||||
| 9 Quality of life Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.9  Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 9 Quality of life. | ||||
| 9.1 End of radiotherapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Up to and including 3 months postradiotherapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Up to and including 6 months postradiotherapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Salivary flow rate (unstimulated) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Biperiden plus pilocarpine versus no treatment, Outcome 1 Salivary flow rate (unstimulated). | ||||
| 1.1 End of radiotherapy | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.08, 0.12] |
| 1.2 Up to and including 3 months postradiotherapy | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Salivary flow rate (> 0 g) unstimulated Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.2 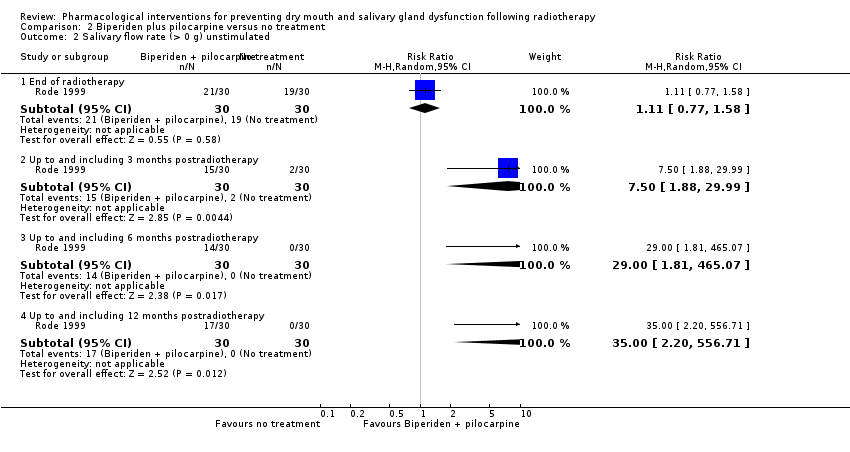 Comparison 2 Biperiden plus pilocarpine versus no treatment, Outcome 2 Salivary flow rate (> 0 g) unstimulated. | ||||
| 2.1 End of radiotherapy | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.77, 1.58] |
| 2.2 Up to and including 3 months postradiotherapy | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 7.50 [1.88, 29.99] |
| 2.3 Up to and including 6 months postradiotherapy | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 29.00 [1.81, 465.07] |
| 2.4 Up to and including 12 months postradiotherapy | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 35.00 [2.20, 556.71] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | |||||||||||||||||||||||||
| 1 Xerostomia (0 to 4 scale ‐ grade 2 or above) Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||
| Analysis 3.1 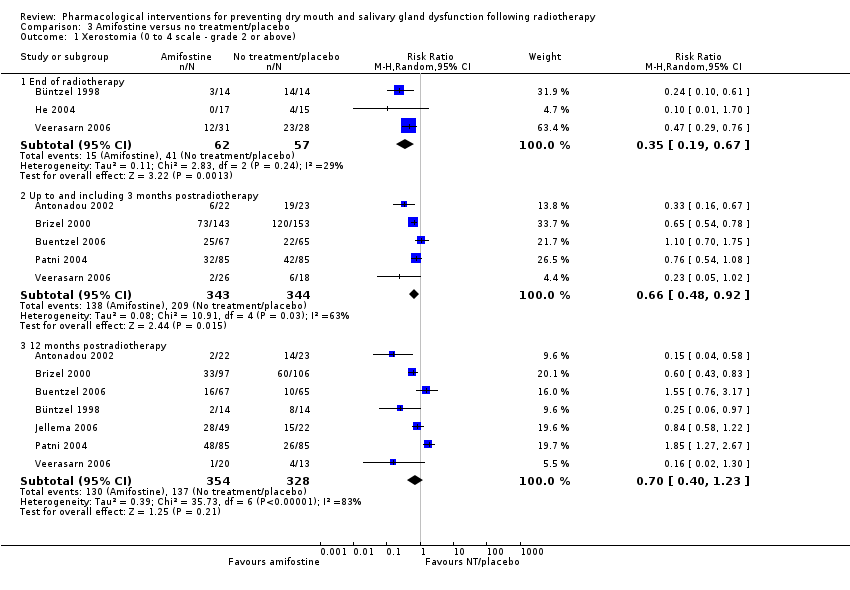 Comparison 3 Amifostine versus no treatment/placebo, Outcome 1 Xerostomia (0 to 4 scale ‐ grade 2 or above). | |||||||||||||||||||||||||||||
| 1.1 End of radiotherapy | 3 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.19, 0.67] | |||||||||||||||||||||||||
| 1.2 Up to and including 3 months postradiotherapy | 5 | 687 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.48, 0.92] | |||||||||||||||||||||||||
| 1.3 12 months postradiotherapy | 7 | 682 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.40, 1.23] | |||||||||||||||||||||||||
| 2 Salivary flow rate (unstimulated) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||
| Analysis 3.2  Comparison 3 Amifostine versus no treatment/placebo, Outcome 2 Salivary flow rate (unstimulated). | |||||||||||||||||||||||||||||
| 2.1 End of radiotherapy | 2 | 83 | Mean Difference (IV, Random, 95% CI) | 0.34 [0.07, 0.61] | |||||||||||||||||||||||||
| 2.2 Up to and including 3 months postradiotherapy | 1 | 41 | Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.90, 1.16] | |||||||||||||||||||||||||
| 2.3 12 months postradiotherapy | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 0.32 [0.09, 0.55] | |||||||||||||||||||||||||
| 3 Salivary flow rate (unstimulated) ‐ incidence of > 0.1 g in 5 min Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||
| Analysis 3.3  Comparison 3 Amifostine versus no treatment/placebo, Outcome 3 Salivary flow rate (unstimulated) ‐ incidence of > 0.1 g in 5 min. | |||||||||||||||||||||||||||||
| 3.1 12 months postradiotherapy | 1 | 175 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [1.13, 1.86] | |||||||||||||||||||||||||
| 4 Salivary flow rate (stimulated) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||
| Analysis 3.4 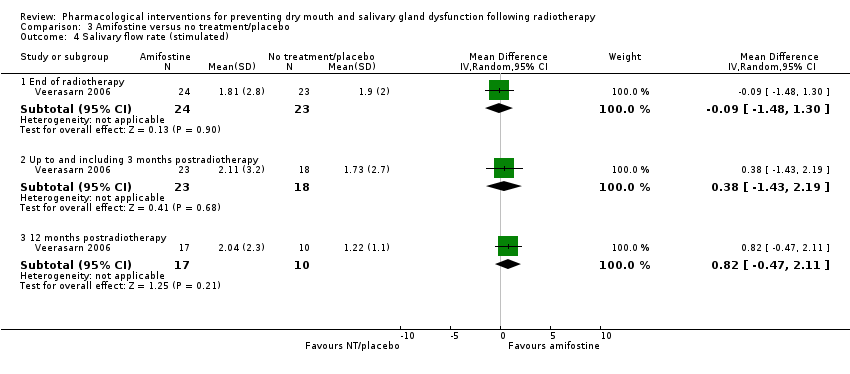 Comparison 3 Amifostine versus no treatment/placebo, Outcome 4 Salivary flow rate (stimulated). | |||||||||||||||||||||||||||||
| 4.1 End of radiotherapy | 1 | 47 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐1.48, 1.30] | |||||||||||||||||||||||||
| 4.2 Up to and including 3 months postradiotherapy | 1 | 41 | Mean Difference (IV, Random, 95% CI) | 0.38 [‐1.43, 2.19] | |||||||||||||||||||||||||
| 4.3 12 months postradiotherapy | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 0.82 [‐0.47, 2.11] | |||||||||||||||||||||||||
| 5 Salivary flow rate (stimulated) ‐ incidence of > 0.1 g in 5 min Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||
| Analysis 3.5  Comparison 3 Amifostine versus no treatment/placebo, Outcome 5 Salivary flow rate (stimulated) ‐ incidence of > 0.1 g in 5 min. | |||||||||||||||||||||||||||||
| 5.1 12 months postradiotherapy | 1 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.89, 1.41] | |||||||||||||||||||||||||
| 6 Overall survival at 12 to 24 months postradiotherapy Show forest plot | 2 | 271 | Hazard ratio (Random, 95% CI) | 1.18 [0.85, 1.66] | |||||||||||||||||||||||||
| Analysis 3.6  Comparison 3 Amifostine versus no treatment/placebo, Outcome 6 Overall survival at 12 to 24 months postradiotherapy. | |||||||||||||||||||||||||||||
| 7 Overall survival ‐ narrative data Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||
| Analysis 3.7
Comparison 3 Amifostine versus no treatment/placebo, Outcome 7 Overall survival ‐ narrative data. | |||||||||||||||||||||||||||||
| 8 Progression‐free survival at 12 to 24 months postradiotherapy Show forest plot | 2 | 247 | Hazard ratio (Random, 95% CI) | 0.94 [0.70, 1.27] | |||||||||||||||||||||||||
| Analysis 3.8 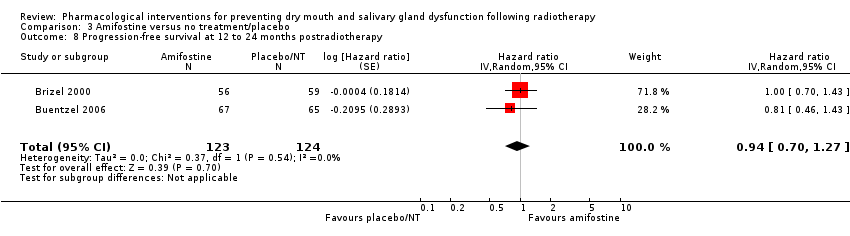 Comparison 3 Amifostine versus no treatment/placebo, Outcome 8 Progression‐free survival at 12 to 24 months postradiotherapy. | |||||||||||||||||||||||||||||
| 9 Progression‐free survival Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||
| Analysis 3.9  Comparison 3 Amifostine versus no treatment/placebo, Outcome 9 Progression‐free survival. | |||||||||||||||||||||||||||||
| 9.1 18 months postradiotherapy | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.81, 1.51] | |||||||||||||||||||||||||
| 10 Progression‐free survival ‐ narrative data Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||
| Analysis 3.10
Comparison 3 Amifostine versus no treatment/placebo, Outcome 10 Progression‐free survival ‐ narrative data. | |||||||||||||||||||||||||||||
| 11 Locoregional tumour control at 12 to 24 months postradiotherapy Show forest plot | 2 | 279 | Hazard ratio (Random, 95% CI) | 0.90 [0.74, 1.11] | |||||||||||||||||||||||||
| Analysis 3.11  Comparison 3 Amifostine versus no treatment/placebo, Outcome 11 Locoregional tumour control at 12 to 24 months postradiotherapy. | |||||||||||||||||||||||||||||
| 12 Locoregional tumour control ‐ narrative data Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||
| Analysis 3.12
Comparison 3 Amifostine versus no treatment/placebo, Outcome 12 Locoregional tumour control ‐ narrative data. | |||||||||||||||||||||||||||||
| 13 Disease‐free survival Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||
| Analysis 3.13 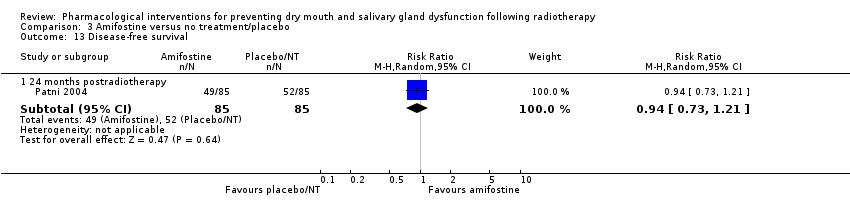 Comparison 3 Amifostine versus no treatment/placebo, Outcome 13 Disease‐free survival. | |||||||||||||||||||||||||||||
| 13.1 24 months postradiotherapy | 1 | 170 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.73, 1.21] | |||||||||||||||||||||||||
| 14 Disease‐free survival Show forest plot | Other data | No numeric data | |||||||||||||||||||||||||||
| Analysis 3.14
Comparison 3 Amifostine versus no treatment/placebo, Outcome 14 Disease‐free survival. | |||||||||||||||||||||||||||||
| 15 Quality of life (Patient Benefit Questionnaire) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | ||||||||||||||||||||||||||
| Analysis 3.15  Comparison 3 Amifostine versus no treatment/placebo, Outcome 15 Quality of life (Patient Benefit Questionnaire). | |||||||||||||||||||||||||||||
| 15.1 End of radiotherapy | 1 | 298 | Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.07, 0.83] | |||||||||||||||||||||||||
| 15.2 Up to and including 3 months postradiotherapy | 1 | 233 | Mean Difference (IV, Random, 95% CI) | 0.52 [‐0.02, 1.06] | |||||||||||||||||||||||||
| 15.3 12 months postradiotherapy | 1 | 180 | Mean Difference (IV, Random, 95% CI) | 0.70 [0.20, 1.20] | |||||||||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | |||||||||||||||
| 1 Xerostomia (0 to 4 scale ‐ grade 2 or above) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | ||||||||||||||||
| Analysis 4.1 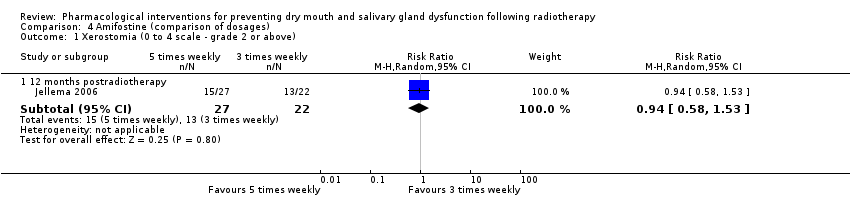 Comparison 4 Amifostine (comparison of dosages), Outcome 1 Xerostomia (0 to 4 scale ‐ grade 2 or above). | |||||||||||||||||||
| 1.1 12 months postradiotherapy | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.58, 1.53] | |||||||||||||||
| 2 Overall survival ‐ narrative data Show forest plot | Other data | No numeric data | |||||||||||||||||
| Analysis 4.2
Comparison 4 Amifostine (comparison of dosages), Outcome 2 Overall survival ‐ narrative data. | |||||||||||||||||||
| 3 Locoregional tumour control ‐ narrative data Show forest plot | Other data | No numeric data | |||||||||||||||||
| Analysis 4.3
Comparison 4 Amifostine (comparison of dosages), Outcome 3 Locoregional tumour control ‐ narrative data. | |||||||||||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (0 to 4 scale ‐ grade 2 or above) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 5.1  Comparison 5 Amifostine (intravenous versus subcutaneous), Outcome 1 Xerostomia (0 to 4 scale ‐ grade 2 or above). | ||||
| 1.1 Up to and including 3 months postradiotherapy | 1 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.76, 1.40] |
| 1.2 12 months postradiotherapy | 1 | 127 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.42, 0.88] |
| 2 Overall survival Show forest plot | 1 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| Analysis 5.2  Comparison 5 Amifostine (intravenous versus subcutaneous), Outcome 2 Overall survival. | ||||
| 2.1 48 months after radiotherapy | 1 | Hazard Ratio (Random, 95% CI) | 1.36 [0.89, 2.10] | |
| 3 Locoregional tumour control Show forest plot | 1 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| Analysis 5.3  Comparison 5 Amifostine (intravenous versus subcutaneous), Outcome 3 Locoregional tumour control. | ||||
| 3.1 48 months after radiotherapy | 1 | Hazard Ratio (Random, 95% CI) | 1.34 [0.76, 2.36] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 6.1  Comparison 6 Chinese medicine versus no treatment/placebo, Outcome 1 Xerostomia. | ||||
| 1.1 End of radiotherapy: Shenqi Fanghou recipe versus no intervention | 1 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.28, 0.55] |
| 1.2 End of radiotherapy: TWBXM versus placebo | 1 | 71 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.78, 1.03] |
| 1.3 Up to and including 3 months postradiotherapy: Jinlong capsules versus no intervention | 1 | 95 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.59, 1.36] |
| 2 Xerostomia Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 6.2  Comparison 6 Chinese medicine versus no treatment/placebo, Outcome 2 Xerostomia. | ||||
| 2.1 End of radiotherapy: TWBXM versus placebo | 1 | 68 | Mean Difference (IV, Random, 95% CI) | ‐2.41 [‐16.19, 11.37] |
| 2.2 Up to and including 3 months postradiotherapy: TWBXM versus placebo | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐17.21, 17.01] |
| 3 Salivary flow rate (stimulated) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 6.3 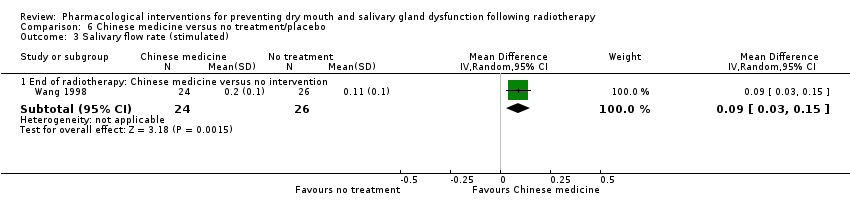 Comparison 6 Chinese medicine versus no treatment/placebo, Outcome 3 Salivary flow rate (stimulated). | ||||
| 3.1 End of radiotherapy: Chinese medicine versus no intervention | 1 | 50 | Mean Difference (IV, Random, 95% CI) | 0.09 [0.03, 0.15] |
| 4 Overall survival (12 months postRT) Show forest plot | 1 | 78 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.84, 1.30] |
| Analysis 6.4  Comparison 6 Chinese medicine versus no treatment/placebo, Outcome 4 Overall survival (12 months postRT). | ||||
| 5 Quality of life (EORTC‐C30) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 6.5  Comparison 6 Chinese medicine versus no treatment/placebo, Outcome 5 Quality of life (EORTC‐C30). | ||||
| 5.1 End of radiotherapy: TWBXM versus placebo | 1 | 68 | Mean Difference (IV, Random, 95% CI) | 2.39 [‐8.74, 13.52] |
| 5.2 Up to and including 3 months postradiotherapy: TWBXM versus placebo | 1 | 44 | Mean Difference (IV, Random, 95% CI) | 1.93 [‐13.04, 16.90] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (0 to 4 scale ‐ grade 2 or above) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 7.1  Comparison 7 Palifermin versus placebo, Outcome 1 Xerostomia (0 to 4 scale ‐ grade 2 or above). | ||||
| 1.1 Up to and including 3 months postRT | 3 | 471 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.77, 1.22] |
| 2 Overall survival at 42 to 72 months from baseline Show forest plot | 3 | Hazard Ratio (Random, 95% CI) | 1.00 [0.72, 1.39] | |
| Analysis 7.2  Comparison 7 Palifermin versus placebo, Outcome 2 Overall survival at 42 to 72 months from baseline. | ||||
| 3 Progression‐free survival at 42 to 72 months from baseline Show forest plot | 3 | Hazard Ratio (Random, 95% CI) | 1.06 [0.80, 1.42] | |
| Analysis 7.3  Comparison 7 Palifermin versus placebo, Outcome 3 Progression‐free survival at 42 to 72 months from baseline. | ||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (0 to 3 scale ‐ grade 2 or above) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 8.1  Comparison 8 Bethanechol versus placebo, Outcome 1 Xerostomia (0 to 3 scale ‐ grade 2 or above). | ||||
| 1.1 End of radiotherapy | 1 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.28, 0.66] |
| 1.2 Up to and including 3 months postradiotherapy | 1 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.65, 1.01] |
| 2 Salivary flow rate (unstimulated) ‐ ml/min Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 8.2  Comparison 8 Bethanechol versus placebo, Outcome 2 Salivary flow rate (unstimulated) ‐ ml/min. | ||||
| 2.1 2 months postradiotherapy | 1 | 97 | Mean Difference (IV, Random, 95% CI) | 0.19 [0.06, 0.32] |
| 3 Salivary flow rate (stimulated) ‐ ml/min Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 8.3  Comparison 8 Bethanechol versus placebo, Outcome 3 Salivary flow rate (stimulated) ‐ ml/min. | ||||
| 3.1 2 months postradiotherapy | 1 | 97 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.03, 0.33] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (dry mouth? yes/no) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 9.1 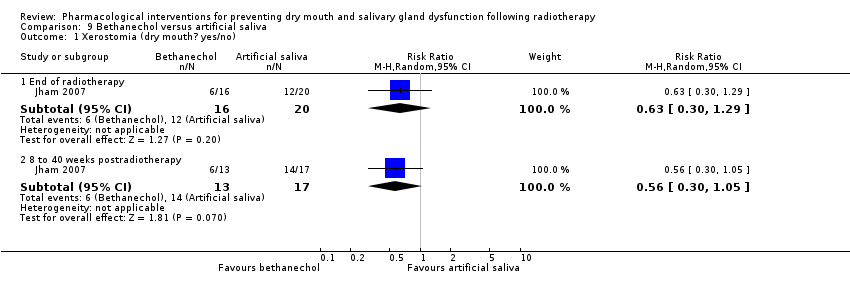 Comparison 9 Bethanechol versus artificial saliva, Outcome 1 Xerostomia (dry mouth? yes/no). | ||||
| 1.1 End of radiotherapy | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.30, 1.29] |
| 1.2 8 to 40 weeks postradiotherapy | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.30, 1.05] |
| 2 Salivary flow rate (unstimulated) ‐ ml/min Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 9.2 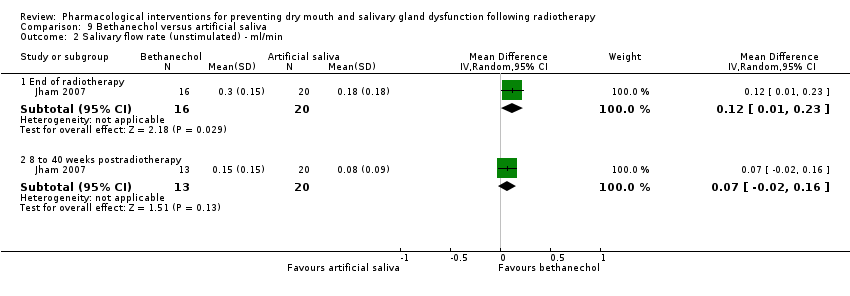 Comparison 9 Bethanechol versus artificial saliva, Outcome 2 Salivary flow rate (unstimulated) ‐ ml/min. | ||||
| 2.1 End of radiotherapy | 1 | 36 | Mean Difference (IV, Random, 95% CI) | 0.12 [0.01, 0.23] |
| 2.2 8 to 40 weeks postradiotherapy | 1 | 33 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.02, 0.16] |
| 3 Salivary flow rate (stimulated) ‐ ml/min Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 9.3  Comparison 9 Bethanechol versus artificial saliva, Outcome 3 Salivary flow rate (stimulated) ‐ ml/min. | ||||
| 3.1 End of radiotherapy | 1 | 32 | Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.03, 0.29] |
| 3.2 8 to 40 weeks postradiotherapy | 1 | 29 | Mean Difference (IV, Random, 95% CI) | 0.21 [0.01, 0.41] |
| 4 Overall survival Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 9.4  Comparison 9 Bethanechol versus artificial saliva, Outcome 4 Overall survival. | ||||
| 4.1 40 weeks postradiotherapy | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.43, 5.84] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||
| 1 Xerostomia Show forest plot | Other data | No numeric data | ||||||||
| Analysis 10.1
Comparison 10 Selenium versus no selenium, Outcome 1 Xerostomia. | ||||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (QoL response for dryness) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 11.1  Comparison 11 Antimicrobial lozenge versus placebo, Outcome 1 Xerostomia (QoL response for dryness). | ||||
| 1.1 Up to and including 3 months postradiotherapy | 1 | 133 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.97, 1.40] |
| 2 Quality of life Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 11.2  Comparison 11 Antimicrobial lozenge versus placebo, Outcome 2 Quality of life. | ||||
| 2.1 Up to and including 3 months postradiotherapy (change score over 6 months) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.65, 1.50] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (grade 2 or above) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 12.1  Comparison 12 Polaprezinc versus azulene oral rinse, Outcome 1 Xerostomia (grade 2 or above). | ||||
| 1.1 End of radiotherapy | 1 | 31 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.04, 0.65] |

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
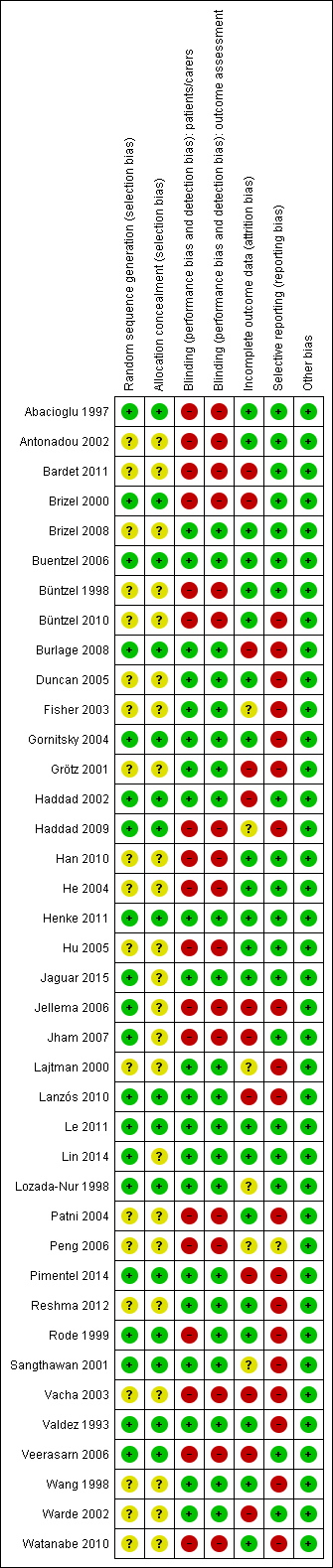
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 1 Xerostomia.

Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 2 Xerostomia (LENT‐SOMA scale).

Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 3 Xerostomia.

Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 4 Salivary flow rate (unstimulated).

Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 5 Salivary flow rate (stimulated).

Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 6 Salivary flow rate (> 0 g) unstimulated.
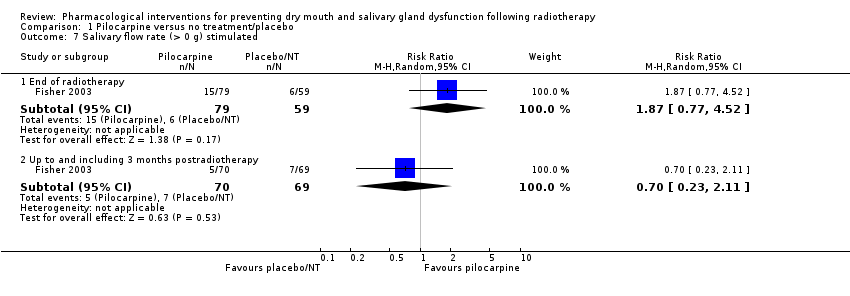
Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 7 Salivary flow rate (> 0 g) stimulated.

Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 8 Overall survival.

Comparison 1 Pilocarpine versus no treatment/placebo, Outcome 9 Quality of life.

Comparison 2 Biperiden plus pilocarpine versus no treatment, Outcome 1 Salivary flow rate (unstimulated).

Comparison 2 Biperiden plus pilocarpine versus no treatment, Outcome 2 Salivary flow rate (> 0 g) unstimulated.
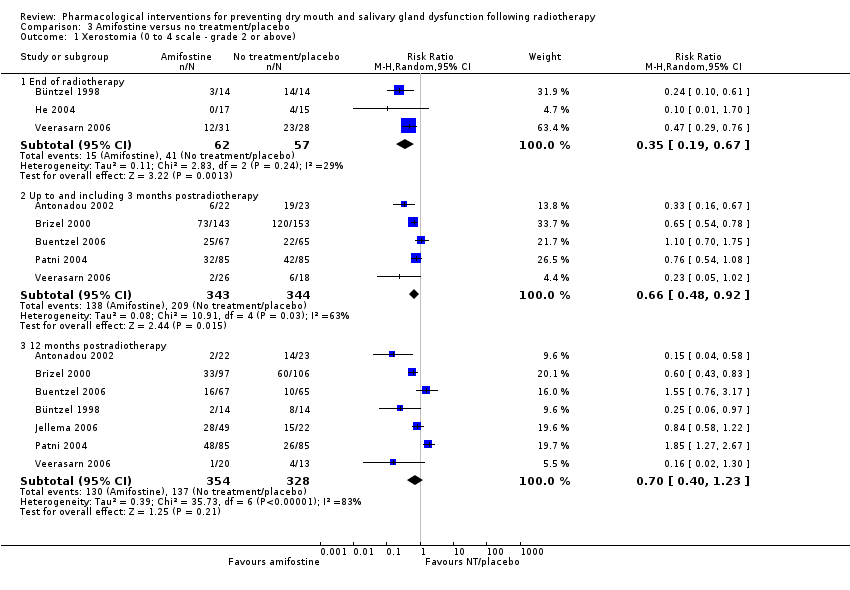
Comparison 3 Amifostine versus no treatment/placebo, Outcome 1 Xerostomia (0 to 4 scale ‐ grade 2 or above).

Comparison 3 Amifostine versus no treatment/placebo, Outcome 2 Salivary flow rate (unstimulated).
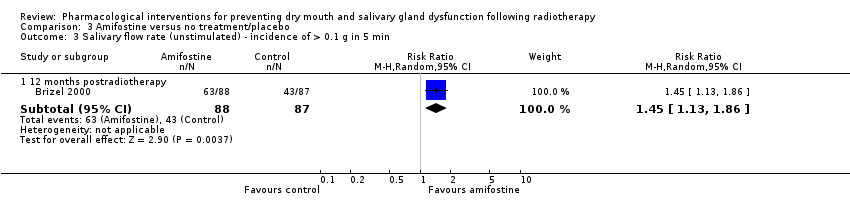
Comparison 3 Amifostine versus no treatment/placebo, Outcome 3 Salivary flow rate (unstimulated) ‐ incidence of > 0.1 g in 5 min.
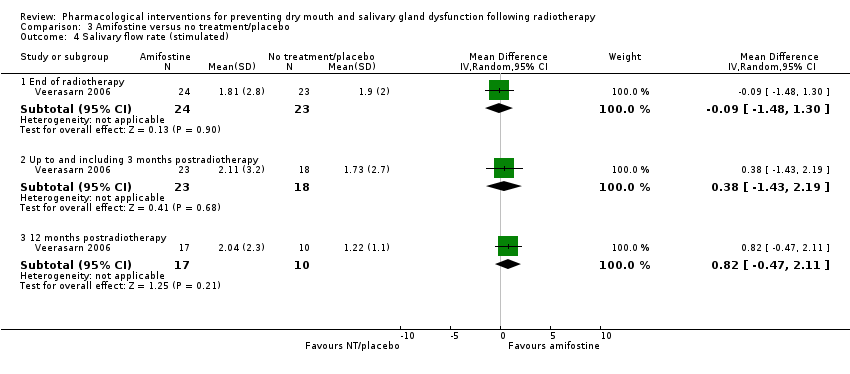
Comparison 3 Amifostine versus no treatment/placebo, Outcome 4 Salivary flow rate (stimulated).

Comparison 3 Amifostine versus no treatment/placebo, Outcome 5 Salivary flow rate (stimulated) ‐ incidence of > 0.1 g in 5 min.

Comparison 3 Amifostine versus no treatment/placebo, Outcome 6 Overall survival at 12 to 24 months postradiotherapy.
| Study | Time point | Amifostine | Control | Comments |
| Haddad 2009 | Median follow‐up 34 months after radiotherapy, minimum 26 months | "No differences noted" | ||
| Jellema 2006 | 24 months | 3 times weekly = 84% 5 times weekly = 58% | 70% | Reported narratively rather than as a risk ratio due to differing results in the amifostine arms |
Comparison 3 Amifostine versus no treatment/placebo, Outcome 7 Overall survival ‐ narrative data.

Comparison 3 Amifostine versus no treatment/placebo, Outcome 8 Progression‐free survival at 12 to 24 months postradiotherapy.

Comparison 3 Amifostine versus no treatment/placebo, Outcome 9 Progression‐free survival.
| Study | Time point | Amifostine | Control | Comments |
| Haddad 2009 | Median follow‐up 34 months after radiotherapy, minimum 26 months | "No differences noted" | ||
Comparison 3 Amifostine versus no treatment/placebo, Outcome 10 Progression‐free survival ‐ narrative data.

Comparison 3 Amifostine versus no treatment/placebo, Outcome 11 Locoregional tumour control at 12 to 24 months postradiotherapy.
| Study | Time point | Amifostine | Control | Comments |
| Haddad 2009 | Median follow‐up 34 months after radiotherapy, minimum 26 months | "No differences noted" | ||
| Jellema 2006 | 24 months | 3 times weekly = 67% 5 times weekly = 83% | 79% | Reported narratively rather than as a risk ratio due to differing results in the amifostine arms |
| Patni 2004 | 24 month | No data | No data | "Amifostine does not alter the response or the survival" |
Comparison 3 Amifostine versus no treatment/placebo, Outcome 12 Locoregional tumour control ‐ narrative data.

Comparison 3 Amifostine versus no treatment/placebo, Outcome 13 Disease‐free survival.
| Study | Time point | Amifostine | Control | Comments |
| Patni 2004 | 24 months | No data | No data | "Amifostine does not alter the response or the survival" |
| Veerasarn 2006 | 24 months | No data | No data | "There was no statistical difference in 2‐year disease‐free survival" |
Comparison 3 Amifostine versus no treatment/placebo, Outcome 14 Disease‐free survival.

Comparison 3 Amifostine versus no treatment/placebo, Outcome 15 Quality of life (Patient Benefit Questionnaire).

Comparison 4 Amifostine (comparison of dosages), Outcome 1 Xerostomia (0 to 4 scale ‐ grade 2 or above).
| Study | Time point | Amifostine 3 times weekly | Amifostine 5 times weekly | Comments |
| Jellema 2006 | 24 months | 84% | 58% | |
Comparison 4 Amifostine (comparison of dosages), Outcome 2 Overall survival ‐ narrative data.
| Study | Time point | Amifostine 3 times weekly | Amifostine 5 times weekly | Comments |
| Jellema 2006 | 24 months | 67% | 83% | |
Comparison 4 Amifostine (comparison of dosages), Outcome 3 Locoregional tumour control ‐ narrative data.
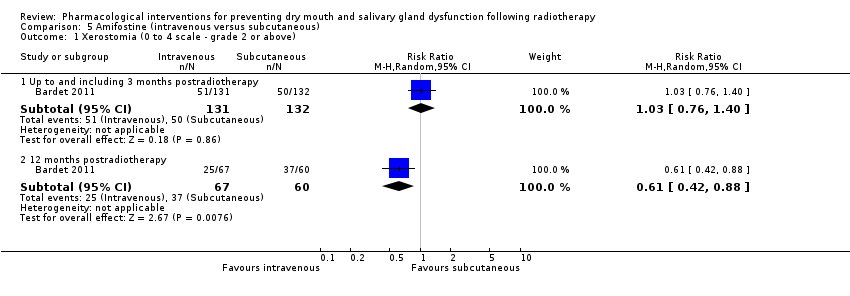
Comparison 5 Amifostine (intravenous versus subcutaneous), Outcome 1 Xerostomia (0 to 4 scale ‐ grade 2 or above).
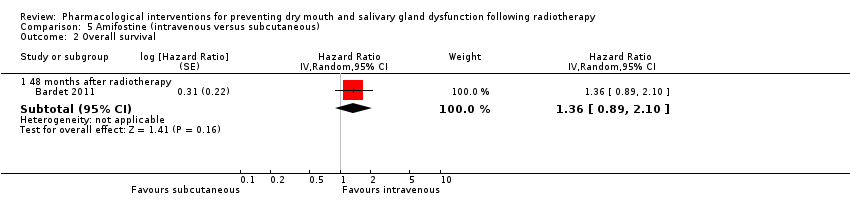
Comparison 5 Amifostine (intravenous versus subcutaneous), Outcome 2 Overall survival.

Comparison 5 Amifostine (intravenous versus subcutaneous), Outcome 3 Locoregional tumour control.
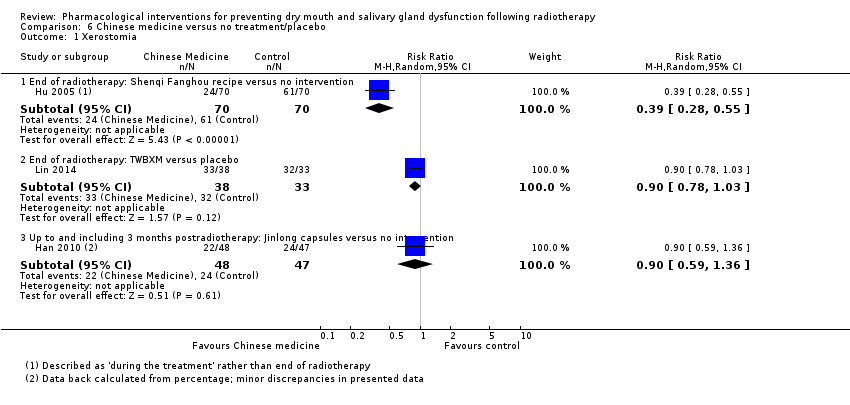
Comparison 6 Chinese medicine versus no treatment/placebo, Outcome 1 Xerostomia.
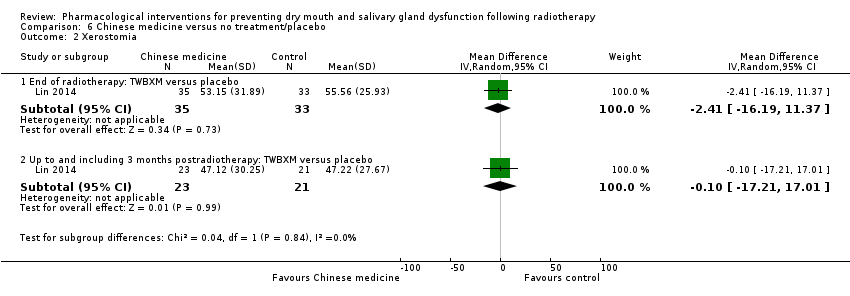
Comparison 6 Chinese medicine versus no treatment/placebo, Outcome 2 Xerostomia.
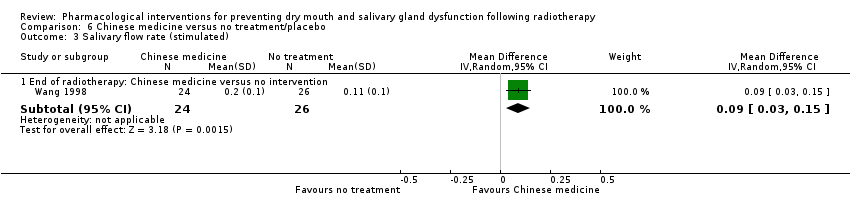
Comparison 6 Chinese medicine versus no treatment/placebo, Outcome 3 Salivary flow rate (stimulated).

Comparison 6 Chinese medicine versus no treatment/placebo, Outcome 4 Overall survival (12 months postRT).

Comparison 6 Chinese medicine versus no treatment/placebo, Outcome 5 Quality of life (EORTC‐C30).
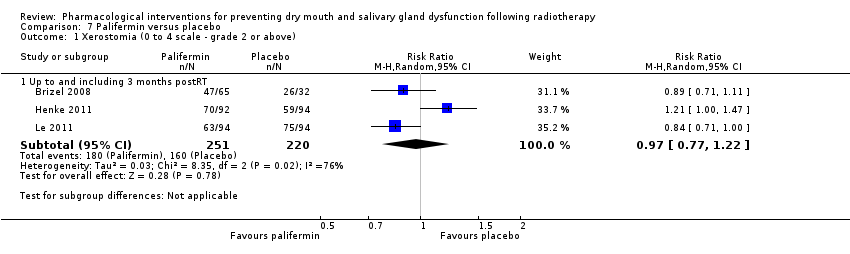
Comparison 7 Palifermin versus placebo, Outcome 1 Xerostomia (0 to 4 scale ‐ grade 2 or above).

Comparison 7 Palifermin versus placebo, Outcome 2 Overall survival at 42 to 72 months from baseline.

Comparison 7 Palifermin versus placebo, Outcome 3 Progression‐free survival at 42 to 72 months from baseline.
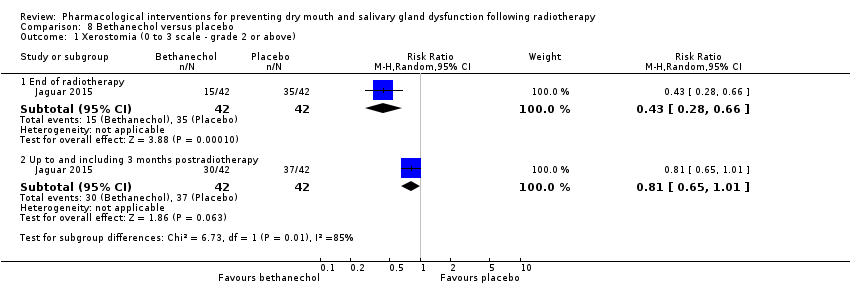
Comparison 8 Bethanechol versus placebo, Outcome 1 Xerostomia (0 to 3 scale ‐ grade 2 or above).

Comparison 8 Bethanechol versus placebo, Outcome 2 Salivary flow rate (unstimulated) ‐ ml/min.

Comparison 8 Bethanechol versus placebo, Outcome 3 Salivary flow rate (stimulated) ‐ ml/min.
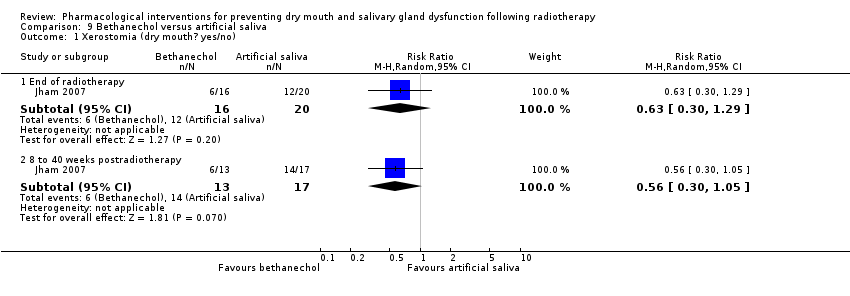
Comparison 9 Bethanechol versus artificial saliva, Outcome 1 Xerostomia (dry mouth? yes/no).
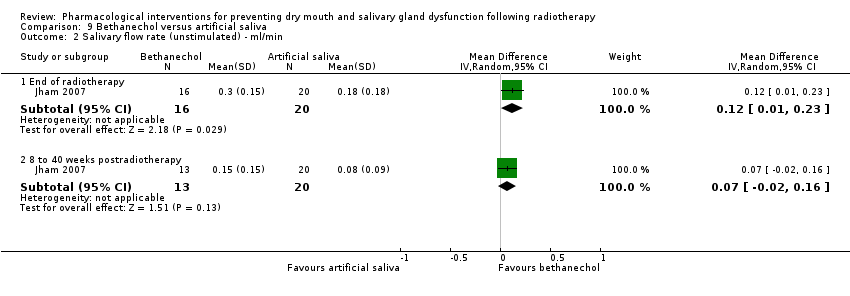
Comparison 9 Bethanechol versus artificial saliva, Outcome 2 Salivary flow rate (unstimulated) ‐ ml/min.

Comparison 9 Bethanechol versus artificial saliva, Outcome 3 Salivary flow rate (stimulated) ‐ ml/min.

Comparison 9 Bethanechol versus artificial saliva, Outcome 4 Overall survival.
| Study | |
| Büntzel 2010 | "comparing the mean value of xerostomia, no statistically significant difference can be seen between the groups" |
Comparison 10 Selenium versus no selenium, Outcome 1 Xerostomia.

Comparison 11 Antimicrobial lozenge versus placebo, Outcome 1 Xerostomia (QoL response for dryness).

Comparison 11 Antimicrobial lozenge versus placebo, Outcome 2 Quality of life.

Comparison 12 Polaprezinc versus azulene oral rinse, Outcome 1 Xerostomia (grade 2 or above).
| Pilocarpine compared to no treatment/placebo for preventing salivary gland dysfunction following radiotherapy | ||||||
| Patient or population: patients receiving radiotherapy on its own or in addition to chemotherapy to the head and neck region | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with no treatment/placebo | Risk with pilocarpine | |||||
| Xerostomia ‐ Up to and including 6 months postRT Studies used different ways of measuring the outcome and therefore we combined the studies using SMD | ‐ | SMD 0.35 lower | ‐ | 126 | ⊕⊝⊝⊝ | Insufficient evidence of a difference at this time point and also at the end of RT and 3 months postRT 1 of the 2 studies in this assessment showed inconsistent results when using an alternative way of measuring this outcome at the 6‐month time point. 2 further studies showed insufficient evidence of a difference, 1 at the end of RT and the other at 3 months postRT |
| Salivary flow rate (unstimulated) ‐ Up to and including 3 months postRT Studies used different ways of measuring the outcome and therefore we combined the studies using SMD | ‐ | MD 0.06 lower (0.23 lower to 0.11 higher) | ‐ | 24 | ⊕⊝⊝⊝ | Insufficient evidence of a difference at this time point and also at the end of RT Same results for stimulated salivary flow rates at end of RT, and 3, 6 and 12 months postRT Same results for a further study at the end of RT and 3 months postRT looking at whether or not stimulated and unstimulated salivary flow was > 0 g |
| Overall survival ‐ Up to and including 6 months postRT | 724 per 1000 | 775 per 1000 | RR 1.07 | 60 | ⊕⊝⊝⊝ | Insufficient evidence of a difference |
| Quality of life ‐ Up to and including 6 months postRT McMaster University Head and Neck Questionnaire (HNRQ). Score 1‐7, lower score = poorer quality of life | Control group mean was 5.3 | MD 0.20 higher | ‐ | 90 | ⊕⊝⊝⊝ | Insufficient evidence of a difference at this time point and also at the end of RT and 3 months postRT |
| Adverse effects | Insufficient evidence of a difference between groups for any reported adverse event, apart from for sweating where data from 5 studies showed an increased risk associated with pilocarpine (RR 2.98, 95% CI 1.43 to 6.22; P = 0.004; I2 = 0%; 389 participants; ⊕⊕⊝⊝ LOW4) | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded by 1 level for risk of bias, 1 level for imprecision (small sample size and 95% CIs include both possibility of benefit and harm), and 1 level for inconsistency (I2 = 68%). | ||||||
| Amifostine compared to no treatment/placebo for preventing salivary gland dysfunction following radiotherapy | ||||||
| Patient or population: patients receiving radiotherapy on its own or in addition to chemotherapy to the head and neck region | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with no treatment/placebo | Risk with amifostine | |||||
| Xerostomia (0‐4 scale ‐ grade 2 or above) ‐ 12 months postRT | 418 per 1000 | 292 per 1000 | RR 0.70 | 682 | ⊕⊕⊝⊝ | Insufficient evidence of a difference at this time point. However, both at the end of RT (RR 0.35, 95% CI 0.19 to 0.67; 3 studies, 119 participants) and up to 3 months postRT (RR 0.66, 95% CI 0.48 to 0.92; 5 studies, 687 participants), amifostine reduced the risk of developing grade ≥ 2 xerostomia |
| Salivary flow rate (mg/5 min) (unstimulated) ‐ 12 months postRT | Control group mean was 0.16 | MD 0.32 higher | ‐ | 27 | ⊕⊝⊝⊝ | Amifostine led to increased unstimulated saliva flow both at 12 months postRT and at the end of RT, but there was insufficient evidence of a difference at 3 months postRT. This evidence was supported by a further study showing a benefit for amifostine at 12 months postRT when looking at incidence of producing > 0.1 g of saliva over 5 minutes (RR 1.45, 95% CI 1.13 to 1.86; 175 participants). A further study narratively reported no difference Insufficient evidence of a difference in stimulated saliva flow at any time point |
| Overall survival at 12 to 24 months postRT | 450 per 1000** | 531 per 1000 | HR 1.18 | 271 | ⊕⊝⊝⊝ | Insufficient evidence to determine whether or not amifostine reduces overall survival, progression‐free survival, disease‐free survival or locoregional tumour control up to 24 months postRT |
| Quality of life (Patient Benefit Questionnaire) ‐ 12 months postRT 8 items each on a 10‐point scale where higher = better QoL | Control group mean was 6.66 | MD 0.7 higher | ‐ | 180 | ⊕⊝⊝⊝ | Amifostine led to a small improvement in quality of life at 12 months postRT, but there was insufficient evidence of a difference at the end of RT and 3 months postRT A further study narratively reported no difference at end of RT and 6, 12, 18, and 24 months postRT |
| Adverse effects |
There was insufficient evidence of a difference between groups for any other adverse events | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded by 1 level for risk of bias, and 1 level for inconsistency (I2 = 83%). | ||||||
| Palifermin compared to placebo for preventing salivary gland dysfunction following radiotherapy | ||||||
| Patient or population: patients receiving radiotherapy on its own or in addition to chemotherapy to the head and neck region | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with palifermin | |||||
| Xerostomia (0‐4 scale ‐ grade 2 or above) ‐ Up to and including 3 months postRT | 727 per 1000 | 705 per 1000 | RR 0.97 | 471 | ⊕⊕⊝⊝ | Insufficient evidence of a difference at this time point |
| Overall survival at 42 to 72 months from baseline | 450 per 1000** | 450 per 1000 | HR 1.00 | (3 studies) | ⊕⊕⊕⊝ | Insufficient evidence to determine whether or not amifostine reduces overall survival and progression‐free survival up to 72 months |
| Adverse effects | There was insufficient evidence of patients in either group experiencing more or less adverse events | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) **2014 5‐year overall survival rate of patients with head and neck squamous cell carcinoma (www.who.int/selection_medicines/committees/expert/20/applications/HeadNeck.pdf) | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded by 1 level for imprecision (95% CIs include both possibility of benefit and harm), and 1 level for inconsistency (I2 = 76%). | ||||||
| Outcome | Study ID | Time point | Pilocarpine | Control | Results | Comments |
| Oral related symptoms (other than salivary gland dysfunction/xerostomia) | ||||||
| Oral discomfort | End of radiotherapy | Mean 38.7 (SD 31.6) n = 16 | Mean 56.7 (SD 26.7) n = 20 | Mean difference ‐18.00 (95% CI ‐37.41 to 1.41), P = 0.07 | ||
| Speech difficulties | Mean 57.5 (SD 26.8) n = 16 | Mean 37.3 (SD 27.5) n = 18 | Mean difference 20.20 (95% CI 1.93 to 38.47), P = 0.03 | |||
| Eating difficulties | Mean 47.4 (SD 33.9) n = 15 | Mean 61.8 (SD 25.4) n = 17 | Mean difference ‐14.40 (95% CI ‐35.38 to 6.58), P = 0.18 | |||
| Mucosal pain | Mean 38.8 (SD 33.9) n = 17 | Mean 53.6 (SD 34.2) n = 19 | Mean difference ‐14.80 (95% CI ‐37.07 to 7.47), P = 0.19 | |||
| Oral complications | 1/5 | 4/6 | RR 0.30 (95% CI 0.05 to 1.89), P = 0.20 | |||
| Adverse events | ||||||
| Sweating | 2/12 | 0/12 | Random‐effects meta‐analysis of 5 studies: RR 2.98 (95% CI 1.43 to 6.22), P = 0.004 Heterogeneity: I2 = 0%, P = 0.52 | |||
| 18/118 | 5/114 | |||||
| 3/28 | 1/28 | |||||
| 5/12 | 1/12 | |||||
| 1/29 | 2/24 | |||||
| Chilling | 1/12 | 0/12 | RR 3.00 (95% CI 0.13 to 67.06), P = 0.49 | |||
| Nausea | 7/28 | 5/28 | Random‐effects meta‐analysis of 3 studies: RR 1.39 (95% CI 0.63 to 3.05), P = 0.41 Heterogeneity: I2 = 0%, P = 0.93 | |||
| 3/18 | 3/21 | |||||
| 2/12 | 1/12 | |||||
| Vomiting | 13/118 | 10/114 | Random‐effects meta‐analysis of 3 studies: RR 1.28 (95% CI 0.70 to 2.35), P = 0.43 Heterogeneity: I2 = 0%, P = 0.92 | |||
| 6/28 | 5/28 | |||||
| 2/12 | 1/12 | |||||
| Headache | 2/28 | 3/28 | RR 0.67 (95% CI 0.12 to 3.69), P = 0.64 | |||
| Excessive lacrimation (tears) | 3/118 | 0/114 | Random‐effects meta‐analysis of 3 studies: RR 2.54 (95% CI 0.70 to 9.17), P = 0.15 Heterogeneity: I2 = 0%, P = 0.71 | |||
| 1/18 | 0/21 | |||||
| 4/25 | 2/22 | |||||
| Dysphasia | 3/12 | 2/12 | RR 1.50 (95% CI 0.30 to 7.43), P = 0.62 | |||
| Weakness | 3/118 | 2/114 | RR 1.45 (95% CI 0.25 to 8.51), P = 0.68 | |||
| Nervous | 0/28 | 1/28 | Random‐effects meta‐analysis of 2 studies: RR 1.02 (95% CI 0.11 to 9.33), P = 0.99 Heterogeneity: I2 = 0%, P = 0.33 | |||
| 1/12 | 0/12 | |||||
| Rhinitis | 2/118 | 5/114 | Random‐effects meta‐analysis of 3 studies: RR 0.87 (95% CI 0.41 to 1.86), P = 0.72 Heterogeneity: I2 = 0%, P = 0.53 | |||
| 1/12 | 1/12 | |||||
| 8/29 | 6/24 | |||||
| Blurred vision | 1/12 | 0/12 | RR 3.00 (95% CI 0.13 to 67.06), P = 0.49 | |||
| Urinary frequency | 7/118 | 5/114 | Random‐effects meta‐analysis of 2 studies: RR 0.87 (95% CI 0.43 to 1.75), P = 0.70 Heterogeneity: I2 = 0%, P = 0.32 | |||
| 6/25 | 8/22 | |||||
| Dizziness | 0/28 | 2/28 | Random‐effects meta‐analysis of 2 studies: RR 0.80 (95% CI 0.18 to 3.45), P = 0.76 Heterogeneity: I2 = 13%, P = 0.28 | |||
| 4/25 | 3/22 | |||||
| Palpitation | 0/25 | 4/22 | RR 0.10 (95% CI 0.01 to 1.73), P = 0.11 | |||
| Skin flushing | 1/118 | 0/114 | RR 2.90 (95% CI 0.12 to 70.44), P = 0.51 | |||
| Motor tremors | 2/118 | 1/114 | RR 1.93 (95% CI 0.18 to 21.02), P = 0.59 | |||
| Sleep problems | End of radiotherapy | Mean 37.3 (SD 36.4) n = 17 | Mean 49.6 (SD 36.9) n = 19 | Mean difference ‐12.30 (95% CI ‐36.27 to 11.67), P = 0.31 | ||
| RTOG (grade 3; mucous membrane, pharynx and larynx) | No statistically significant difference between treatment groups | |||||
| CI = confidence interval; RR = risk ratio; RTOG = Radiation Therapy Oncology Group; SD = standard deviation. | ||||||
| Outcome | Study ID | Time point | Pilocarpine | Control | Results | Comments |
| Dysphagia (WHO grade 3+) | 12 months after RT | 1/30 | 4/30 | RR 0.25 (95% CI 0.03 to 2.11), P = 0.20 | ||
| CI = confidence interval; RR = risk ratio; RT = radiotherapy; WHO = World Health Organization. | ||||||
| Outcome | Study ID | Time point | Amifostine | Control | Results | Comments |
| Quality of life | Assessed at end of RT and 6, 12, 18 and 24 months after RT | No data | No data | "No significant differences between the 3 treatment arms" | ||
| Dysphagia (difficulty in swallowing) (0‐4 scale): grade 3 and above | End of RT | 14/22 | 23/23 | Random‐effects meta‐analysis of 2 studies: RR 0.50 (95% CI 0.17 to 1.48); P = 0.21 Heterogeneity: I2 = 40%, P = 0.20 | ||
| 1/14 | 5/14 | |||||
| 4 weeks after RT | 2/22 | 3/23 | RR 0.70 (95% CI 0.13 to 3.78); P = 0.68 | By 8 weeks after RT, no participants had grade 3 or above dysphagia | ||
| Dysgeusia (taste disturbance) (0‐4 scale): grade 2 and above | End of RT | 3/14 | 14/14 | RR 0.24 (95% CI 0.10 to 0.61); P = 0.003 | ||
| Cost data (mean per patient supportive care costs) | End of RT | USD 4401 | USD 5873 | P = 0.02 | ||
| Vomiting | 1/22 | 0/23 | Random‐effects meta‐analysis of 5 studies: RR 4.90 (95% CI 2.87 to 8.38); P < 0.00001 Heterogeneity: I2 = 0%, P = 0.96 | |||
| 55/150 | 11/153 | |||||
| 8/66 | 2/64 | |||||
| 1/17 | 0/15 | "1 patient left due to gastrointestinal tract reaction/side effect, all other patients completed the treatment" "At the beginning of treatment, nausea and vomiting was obvious for amifostine group, but after treating with metoclopramide, there was no significant difference between 2 groups in gastrointestinal tract reaction/side effect" | ||||
| 10/60 | 0/31 | |||||
| 10/18 | Data not reported in control group. Unknown if this was due to 0 events | |||||
| 18/32 | Data not reported in control group. Unknown if this was due to 0 events | |||||
| Hypotension | 3/22 | 0/23 | Random‐effects meta‐analysis of 3 studies: RR 9.20 (95% CI 2.84 to 29.83); P = 0.0002 Heterogeneity: I2 = 0%, P = 0.88 | |||
| 22/150 | 2/153 | |||||
| 2/14 | 0/14 | |||||
| 5/32 | Data not reported in control group. Unknown if this was due to 0 events | |||||
| Nausea | 66/150 | 25/153 | Random‐effects meta‐analysis of 4 studies: RR 2.60 (95% CI 1.81 to 3.74); P < 0.00001 Heterogeneity: I2 = 0%, P = 0.45 | |||
| 4/66 | 4/64 | |||||
| 1/17 | 0/15 | "1 patient left due to gastrointestinal tract reaction/side effect, all other patients completed the treatment" "At the beginning of treatment, nausea and vomiting was obvious for amifostine group, but after treating with metoclopramide, there was no significant difference between 2 groups in gastrointestinal tract reaction/side effect" | ||||
| 23/60 | 3/31 | |||||
| 10/18 | Data not reported in control group. Unknown if this was due to 0 events | |||||
| 20/32 | Data not reported in control group. Unknown if this was due to 0 events | |||||
| Allergic response | 8/150 | 0/153 | Random‐effects meta‐analysis of 3 studies: RR 7.51 (95% CI 1.40 to 40.39); P = 0.02 Heterogeneity: I2 = 0%, P = 0.77 | |||
| 2/66 | 0/64 | |||||
| 4/60 | 0/31 | |||||
| Asthenia (weakness or lack of energy) | 3/66 | 1/64 | RR 2.91 (95% CI 0.31 to 27.24); P = 0.35 | |||
| Alopecia | Similar in both groups and increased continuously during the treatment | |||||
| Skin toxicity | Similar in both groups and increased continuously during the treatment | |||||
| Hot flush | "..dizziness, fatigue, hiccup, sneezing, facial flush all in less than 5% of the patients" | |||||
| 17/32 | Data not reported in control group. Unknown if this was due to 0 events | |||||
| Somnolence (drowsiness) | 18/32 | Data not reported in control group. Unknown if this was due to 0 events | ||||
| Sneezing | "..dizziness, fatigue, hiccup, sneezing, facial flush all in less than 5% of the patients" | |||||
| 13/32 | Data not reported in control group. Unknown if this was due to 0 events | |||||
| Hiccup | "..dizziness, fatigue, hiccup, sneezing, facial flush all in less than 5% of the patients" | |||||
| 10/32 | Data not reported in control group. Unknown if this was due to 0 events | |||||
| Dizziness | "...dizziness, fatigue, hiccup, sneezing, facial flush all in less than 5% of the patients" | |||||
| Fatigue | "..dizziness, fatigue, hiccup, sneezing, facial flush all in less than 5% of the patients" | |||||
| CI = confidence interval; RR = risk ratio; RT = radiotherapy; USD = US dollars. | ||||||
| Outcome | Study ID | Time point | Amifostine 3 times weekly | Amifostine 5 times weekly | Results | Comments |
| Quality of life | Assessed at end of RT and 6, 12, 18 and 24 months after RT | No data | No data | "No significant differences between the 3 treatment arms" | ||
| Nausea | 9/30 | 14/30 | RR 0.64 (95% CI 0.33 to 1.25); P = 0.19 | |||
| Vomiting | 2/30 | 8/30 | RR 0.25 (95% CI 0.06 to 1.08); P = 0.06 | |||
| Allergic response | 2/30 | 2/30 | RR 1.00 (95% CI 0.15 to 6.64); P = 1 | |||
| CI = confidence interval; RR = risk ratio; RT = radiotherapy. | ||||||
| Outcome | Study ID | Time point | Intravenous | Subcutaneous | Results | Comments |
| Nausea/vomiting | 29% | 36% | P = 0.267 | |||
| Hypotension | 20% | 8% | P = 0.007 | |||
| Skin rash | 10% | 22% | P = 0.012 | |||
| Local pain at injection site | 0% | 8% | P = 0.001 | |||
| Fever | 2% | 0% | P = 0.256 | |||
| Asthenia (weakness or lack of energy) | 1% | 6% | P = 0.054 |
| Outcome | Study ID | Intervention | Time point | Study | Control | Results | Comments |
| Dysphasia (difficulty in swallowing) (score for EORTC‐H&N35 questionnaire: mean (SD)) | Chinese medicine (TWBXM) | End of RT | 50.2 (26.3); n = 35 | 38.9 (25.9); n = 33 | P = 0.07 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 30.2 (29.8); n = 23 | 26.7 (24.8); n = 21 | P = 0.65 | |||
| Dysgeusia (taste disturbance) (0 to 3 scale): grade 1 and above | Chinese medicine (TWBXM) | End of RT | 32/38 | 29/33 | RR 0.96 (95% CI 0.79 to 1.16); P = 0.13 | ||
| Speech difficulty (mean (SD) score for EORTC‐H&N35 questionnaire) | Chinese medicine (TWBXM) | End of RT | 36.3 (26.7); n = 35 | 28.6 (26.2); n = 33 | P = 0.23 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 27.4 (28.6); n = 23 | 22.7 (19.5); n = 21 | P = 0.50 | |||
| Difficulty in mouth opening (mean (SD) score for EORTC‐H&N35 questionnaire) | Chinese medicine (TWBXM) | End of RT | 39.6 (28.2); n = 35 | 41.4 (27.7); n = 33 | P = 0.79 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 32.2 (31.5); n = 23 | 33.3 (24.1); n = 21 | P = 0.88 | |||
| Difficulty in mouth opening (0 to 2 scale): grade 1 and above | Chinese medicine (Shenqi Fanghou recipe) | "During the treatment" | 22/70 | 52/70 | RR 0.42 (95% CI 0.29 to 0.61); P < 0.001 | ||
| Skin toxicity (0 to 3 scale): grade 1 and above | Chinese medicine (TWBXM) | End of RT | 35/38 | 30/33 | RR 1.01 (95% CI 0.88 to 1.17); P = 0.82 | ||
| Skin toxicity (0 to 4 scale): grade 1 and above | Chinese medicine (Shenqi Fanghou recipe) | "During the treatment" | 57/70 | 68/70 | RR 0.84 (95% CI 0.74 to 0.94); P = 0.002 | ||
| Skin toxicity (prevalence according to RTOG standards) | Chinese medicine (Jinlong capsule) | 46.82% | 58.32% | Quote: "toxicities during and after treatment were assessed" Comment: time point for assessment unclear; minor discrepancies in presented data | |||
| Nausea/vomiting (0 to 3 scale): grade 1 and above | Chinese medicine (TWBXM) | End of RT | 12/38 | 4/33 | RR 2.61 (95% CI 0.93 to 7.30); P = 0.183 | ||
| Hoarseness | Chinese medicine (TWBXM) | End of RT | 1/38 | 3/33 | RR 0.29 (95% CI 0.03 to 2.65); P = 0.26 | ||
| Fatigue (mean (SD) score for EORTC‐C30 questionnaire) | Chinese medicine (TWBXM) | End of RT | 43.2 (26.2); n = 35 | 42.4 (23.0); n = 33 | P = 0.88 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 31.2 (28.3); n = 23 | 36.4 (25.0); n = 21 | P = 0.51 | |||
| Pain (mean (SD) score for EORTC‐C30 questionnaire) | Chinese medicine (TWBXM) | End of RT | 46.8 (23.2); n = 35 | 41.7 (27.4); n = 33 | P = 0.40 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 35.9 (27.0); n = 23 | 40.9 (29.9); n = 21 | P = 0.54 | |||
| Pain (mean (SD) score for EORTC‐H&N35 questionnaire) | Chinese medicine (TWBXM) | End of RT | 55.4 (25.1); n = 35 | 42.4 (20.5); n = 33 | P = 0.02 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 31.6 (24.2); n = 23 | 37.8 (23.3); n = 21 | P = 0.35 | |||
| Dyspnea (mean (SD) score for EORTC‐C30 questionnaire) | Chinese medicine (TWBXM) | End of RT | 17.1 (23.1); n = 35 | 16.7 (20.7); n = 33 | P = 0.93 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 20.5 (21.2); n = 23 | 13.6 (22.2); n = 21 | P = 0.28 | |||
| Insomnia (mean (SD) score for EORTC‐C30 questionnaire) | Chinese medicine (TWBXM) | End of RT | 40.5 (25.0); n = 35 | 31.2 (25.3); n = 33 | P = 0.13 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 30.8 (24.8); n = 23 | 31.8 (28.1); n = 21 | P = 0.28 | |||
| Appetite loss (mean (SD) score for EORTC‐C30 questionnaire) | Chinese medicine (TWBXM) | End of RT | 45.0 (30.7); n = 35 | 45.8 (29.0); n = 33 | P = 0.91 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 28.2 (26.1); n = 23 | 34.9 (30.0); n = 21 | P = 0.42 | |||
| Constipation (mean (SD) score for EORTC‐C30 questionnaire) | Chinese medicine (TWBXM) | End of RT | 37.8 (27.4); n = 35 | 29.2 (20.3); n = 33 | P = 0.15 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 29.5 (30.3); n = 23 | 25.7 (20.4); n = 21 | P = 0.63 | |||
| Diarrhoea (mean (SD) score for EORTC‐C30 questionnaire) | Chinese medicine (TWBXM) | End of RT | 9.0 (15.0); n = 35 | 6.2 (13.2); n = 33 | P = 0.42 | ||
| Chinese medicine (TWBXM) | 1 month after RT | 9.0 (15.1); n = 23 | 6.1 (16.7); n = 21 | P = 0.53 | |||
| Adverse effects | Chinese medicine (Jinlong capsule) | Leukopenia, nausea, vomiting, 1 participant had dizziness and blood pressure drop, 1 participant had skin rash | Not reported | ||||
| Adverse effects | Chinese medicine (Shenqi Fanghou recipe) | "During the treatment" | No adverse event | Not reported | |||
| CI = confidence interval; EORTC = European Organisation for Research and Treatment of Cancer; H&N = head and neck; RR = risk ratio; RT = radiotherapy; RTOG = Radiation Therapy Oncology Group; SD = standard deviation; TWBXM = Tianwang Buxin Mini‐pills. | |||||||
| Outcome | Study ID | Time point | Palifermin | Placebo | Results |
| Oral related symptoms (other than salivary gland dysfunction/xerostomia) | |||||
| Dysphagia | 3 months postRT | 29/94 | 19/91 | Random‐effects meta‐analysis of 3 studies: RR 1.32 (95% CI 0.55 to 3.13); P = 0.54 Heterogeneity: I2 = 94%, P < 0.00001 | |
| 61/64 | 31/32 | ||||
| 32/92 | 20/93 | ||||
| Mouth and throat soreness ‐ 0 (no soreness) to 4 (extreme soreness) OMWQ‐HN scale | 3 months postRT | n = 94, mean = 1.66, SD = 0.73 | n = 94, mean = 1.86, SD = 0.65 | Random‐effects meta‐analysis of 2 studies: mean difference ‐0.12 (95% CI ‐0.27 to 0.02); P = 0.10 Heterogeneity: I2 = 13%, P = 0.28 | |
| n = 92, mean = 1.52, SD = 0.69 | n = 94, mean = 1.57, SD = 0.63 | ||||
| Adverse events | |||||
| Nausea | 47/94 | 42/91 | Random‐effects meta‐analysis of 2 studies: RR 0.96 (95% CI 0.77 to 1.19); P = 0.69 Heterogeneity: I2 = 28%, P = 0.24 | ||
| 48/67 | 26/32 | ||||
| Fever | 30/67 | 13/32 | RR 1.10 (95% CI 0.67 to 1.81); P = 0.70 | ||
| Constipation | 31/94 | 24/91 | Random‐effects meta‐analysis of 2 studies: RR 1.15 (95% CI 0.82 to 1.60); P = 0.42 Heterogeneity: I2 = 0%, P = 0.57 | ||
| 28/67 | 13/32 | ||||
| Diarrhoea | 14/67 | 8/32 | Random‐effects meta‐analysis of 2 studies: RR 1.28 (95% CI 0.49 to 3.36); P = 0.61 Heterogeneity: I2 = 57%, P = 0.13 | ||
| 11/92 | 5/93 | ||||
| Insomnia | 12/67 | 4/32 | Random‐effects meta‐analysis of 2 studies: RR 0.77 (95% CI 0.23 to 2.55); P = 0.67 Heterogeneity: I2 = 63%, P = 0.10 | ||
| 5/92 | 12/93 | ||||
| Dyspnea | 9/67 | 1/32 | RR 1.10 (95% CI 0.67 to 1.81); P = 0.70 | ||
| Cough | 8/67 | 5/32 | RR 0.76 (95% CI 0.27 to 2.15); P = 0.61 | ||
| Headache | 8/67 | 2/32 | Random‐effects meta‐analysis of 2 studies: RR 2.13 (95% CI 0.86 to 5.28); P = 0.10 Heterogeneity: I2 = 0%, P = 0.86 | ||
| 9/92 | 4/93 | ||||
| Decreased weight | 29/94 | 27/91 | Random‐effects meta‐analysis of 2 studies: RR 1.01 (95% CI 0.67 to 1.52); P = 0.96 Heterogeneity: I2 = 0%, P = 0.73 | ||
| 7/67 | 4/32 | ||||
| Dizziness | 5/67 | 4/32 | RR 0.60 (95% CI 0.17 to 2.07); P = 0.42 | ||
| Anxiety | 4/67 | 5/32 | RR 0.38 (95% CI 0.11 to 1.33); P = 0.13 | ||
| Hypomagnesemia | 4/67 | 4/32 | RR 0.48 (95% CI 0.13 to 1.79); P = 0.27 | ||
| Vomiting | 26/94 | 26/91 | Random‐effects meta‐analysis of 2 studies: RR 0.98 (95% CI 0.72 to 1.33); P = 0.89 Heterogeneity: I2 = 0%, P = 0.96 | ||
| 33/67 | 16/32 | ||||
| Radiation skin injury | 25/94 | 13/91 | RR 1.10 (95%CI 0.67 to 1.81); P = 0.70 | ||
| Anaemia | 21/94 | 34/91 | Random‐effects meta‐analysis of 2 studies: RR 0.83 (95% CI 0.33 to 2.05); P = 0.68 Heterogeneity: I2 = 54%, P = 0.14 | ||
| 10/67 | 3/32 | ||||
| Fatigue | 21/94 | 20/91 | Random‐effects meta‐analysis of 3 studies: RR 0.88 (95% CI 0.60 to 1.30); P = 0.52 Heterogeneity: I2 = 2%, P = 0.36 | ||
| 7/92 | 14/93 | ||||
| 17/67 | 8/32 | ||||
| Leukopenia | 21/94 | 12/91 | Random‐effects meta‐analysis of 2 studies: RR 1.01 (95% CI 0.37 to 2.78); P = 0.98 Heterogeneity: I2 = 79%, P = 0.03 | ||
| 12/92 | 20/93 | ||||
| Granulocytopenia | 20/67 | 6/32 | RR 1.59 (95% CI 0.47 to 5.39); P = 0.45 | ||
| Pharyngolaryngeal pain | 20/94 | 23/91 | RR 0.84 (95% CI 0.50 to 1.42); P = 0.52 | ||
| Hypokalemia | 19/94 | 8/91 | RR 2.04 (95% CI 0.98 to 4.28); P = 0.06 | ||
| Pyrexia | 16/94 | 19/91 | RR 0.82 (95% CI 0.45 to 1.48); P = 0.50 | ||
| Mucosal inflammation | 4/92 | 10/93 | RR 0.40 (95% CI 0.13 to 1.24); P = 0.11 | ||
| Asthenia | 13/92 | 7/93 | RR 1.88 (95% CI 0.78 to 4.49); P = 0.16 | ||
| Abdominal pain | 7/92 | 2/93 | RR 3.54 (95% CI 0.75 to 16.58); P = 0.11 | ||
| Back pain | 6/92 | 1/93 | RR 6.07 (95% CI 0.74 to 49.40); P = 0.09 | ||
| Febrile neutropenia | 1/92 Considered "serious adverse event" | 0/93 | RR 3.03 (95% CI 0.13 to 73.48); P = 0.50 | ||
| Dehydration | 13/94 | 19/91 | Random‐effects meta‐analysis of 3 studies: RR 0.75 (95% CI 0.45 to 1.25); P = 0.27 Heterogeneity: I2 = 30%, P = 0.24 | ||
| 6/92 | 13/93 | ||||
| 20/67 | 8/32 | ||||
| CI = confidence interval; OMWQ‐HN = Oral Mucositis Weekly Questionnaire ‐ Head and Neck Cancer; RR = risk ratio; RT = radiotherapy; SD = standard deviation. | |||||
| Outcome | Study ID | Results |
| Adverse effects | No statistical difference between the groups in bethanechol‐related toxicity. Quote: "No patient experienced severe (grade 3) toxicity and no one dropped out of the study due to adverse effects" |
| Outcome | Study ID | Time point | Bethanechol | Artificial saliva | Results | Comments |
| Lacrimation (watering eyes) | End of RT | 3/22 | 0/21 | RR 6.70 (95% CI 0.37 to 122.29); P = 0.2 | ||
| Nervousness | 3/22 | 0/21 | RR 6.70 (95% CI 0.37 to 122.29); P = 0.2 | |||
| Frequent urination | 3/22 | 0/21 | RR 6.70 (95% CI 0.37 to 122.29); P = 0.2 | |||
| Sweating | 2/22 | 0/21 | RR 4.78 (95% CI 0.24 to 94.12); P = 0.3 | "1 patient using bethanechol dropped out of the study due to excessive sweating (Grade 2 severity; National Cancer Institute Common Terminology Criteria for Adverse Events – NCI CTCAE, v 3" | ||
| Warm face | 2/22 | 0/21 | RR 4.78 (95% CI 0.24 to 94.12); P = 0.3 | |||
| Cramps | 1/22 | 0/21 | RR 2.87 (95% CI 0.12 to 66.75); P = 0.51 | |||
| Diarrhoea | 1/22 | 0/21 | RR 2.87 (95% CI 0.12 to 66.75); P = 0.51 | |||
| Nausea | 1/22 | 2/21 | RR 0.48 (95% CI 0.05 to 4.88); P = 0.53 | |||
| CI = confidence interval; RR = risk ratio; RT = radiotherapy. | ||||||
| Outcome | Study ID | Time point | Reported in text |
| Loss of taste | 6 weeks after end RT | "Ageusia was milder in the selenium group. But the difference was not significant" | |
| Dysphagia | 6 weeks after end RT | "The only significant difference was observed at week 7, when the selenium group had developed a mean value of 1.533 versus 2.167 in the control group (P = 0.05)" | |
| Adverse events | 6 weeks after end RT | "23 serious adverse events (SAEs) were seen in the selenium group, compared to 22 in the control group (P = 0.476). No statistically significant differences in toxicities were found using the 2‐tailed Fisher's exact test" | |
| RT = radiotherapy. | |||
| Outcome | Study ID | Time point | Antiseptic rinse | Placebo | Results |
| Drooling | 4 weeks from baseline | Increased 6 No change or decreased 8 6/14 | Increased 3 No change or decreased 7 3/10 | RR 1.43 (95% CI 0.46 to 4.39); P = 0.53 | |
| Adverse events | "No relevant adverse events were reported in any group" | ||||
| CI = confidence interval; RR = risk ratio. | |||||
| Outcome | Study ID | Time point | Antimicrobial lozenge | Placebo | Results |
| Mouth pain | Worse over 6 months | 32/66 | 32/62 | RR 0.94 (95% CI 0.66 to 1.33); P=0.72 | |
| Sore/burning mouth | Worse over 6 months | 32/65 | 32/62 | RR 0.95 (95% CI 0.68 to 1.35); P=0.79 | |
| Throat pain | Worse over 6 months | 29/66 | 36/65 | RR 0.79 (95% CI 0.56 to 1.12); P=0.19 | |
| Dryness in mouth | Worse over 6 months | 55/66 | 46/65 | RR 1.18 (95% CI 0.97 to 1.42); P=0.09 | |
| Nausea | Worse over 6 months | 27/66 | 14/65 | RR 1.90 (95% CI 1.10 to 3.28); P=0.02 | |
| Diarrhoea | Worse over 6 months | 6/66 | 3/65 | RR 1.97 (95% CI 0.51 to 7.54); P=0.32 | |
| Constipation | Worse over 6 months | 24/66 | 26/65 | RR 0.91 (95% CI 0.59 to 1.42); P=0.67 | |
| CI = confidence interval; RR = risk ratio. | |||||
| Outcome | Study ID | Time point | Polaprezinc | Azulene rinse | Results |
| Pain > 2 (0‐3 scale) | Over RT period | 5/16 | 13/15 | RR 0.36 (95% CI 0.17 to 0.77); P = 0.008 | |
| Taste disturbance > 2 (0‐3 scale) | Over RT period | 1/16 | 8/15 | RR 0.12 (95% CI 0.02 to 0.83); P = 0.03 | |
| Disability of oral intake | Over RT period | 2/16 | 6/15 | RR 0.31 (95% CI 0.07 to 1.31); P = 0.11 | |
| CI = confidence interval; RR = risk ratio; RT = radiotherapy. | |||||
| Outcome | Study ID | Results |
| Adverse events | "No adverse events could be attributed to the experimental medication" |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia Show forest plot | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 End of radiotherapy | 4 | 122 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.16, 0.56] |
| 1.2 Up to and including 3 months postradiotherapy | 3 | 125 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.33, 0.37] |
| 1.3 Up to and including 6 months postradiotherapy | 2 | 126 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐1.04, 0.33] |
| 2 Xerostomia (LENT‐SOMA scale) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Up to and including 6 months postradiotherapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Xerostomia Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 End of radiotherapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Up to and including 3 months postradiotherapy | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Salivary flow rate (unstimulated) Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 End of radiotherapy | 3 | 76 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.24, 0.72] |
| 4.2 Up to and including 3 months postradiotherapy | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐1.07, 0.54] |
| 5 Salivary flow rate (stimulated) Show forest plot | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 End of radiotherapy | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.44, 0.59] |
| 5.2 Up to and including 3 months postradiotherapy | 1 | 24 | Std. Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.41, 1.21] |
| 5.3 Up to and including 6 months postradiotherapy | 1 | 9 | Std. Mean Difference (IV, Random, 95% CI) | 0.52 [‐0.84, 1.87] |
| 5.4 Up to and including 12 months postradiotherapy | 1 | 9 | Std. Mean Difference (IV, Random, 95% CI) | 0.53 [‐0.83, 1.88] |
| 6 Salivary flow rate (> 0 g) unstimulated Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 End of radiotherapy | 1 | 154 | Risk Ratio (M‐H, Random, 95% CI) | 1.90 [0.98, 3.69] |
| 6.2 Up to and including 3 months postradiotherapy | 1 | 152 | Risk Ratio (M‐H, Random, 95% CI) | 2.0 [0.86, 4.68] |
| 7 Salivary flow rate (> 0 g) stimulated Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 End of radiotherapy | 1 | 138 | Risk Ratio (M‐H, Random, 95% CI) | 1.87 [0.77, 4.52] |
| 7.2 Up to and including 3 months postradiotherapy | 1 | 139 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.23, 2.11] |
| 8 Overall survival Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 9 Quality of life Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9.1 End of radiotherapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Up to and including 3 months postradiotherapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 Up to and including 6 months postradiotherapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Salivary flow rate (unstimulated) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 End of radiotherapy | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.08, 0.12] |
| 1.2 Up to and including 3 months postradiotherapy | 1 | 17 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Salivary flow rate (> 0 g) unstimulated Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 End of radiotherapy | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.77, 1.58] |
| 2.2 Up to and including 3 months postradiotherapy | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 7.50 [1.88, 29.99] |
| 2.3 Up to and including 6 months postradiotherapy | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 29.00 [1.81, 465.07] |
| 2.4 Up to and including 12 months postradiotherapy | 1 | 60 | Risk Ratio (M‐H, Random, 95% CI) | 35.00 [2.20, 556.71] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (0 to 4 scale ‐ grade 2 or above) Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 End of radiotherapy | 3 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.19, 0.67] |
| 1.2 Up to and including 3 months postradiotherapy | 5 | 687 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.48, 0.92] |
| 1.3 12 months postradiotherapy | 7 | 682 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.40, 1.23] |
| 2 Salivary flow rate (unstimulated) Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 End of radiotherapy | 2 | 83 | Mean Difference (IV, Random, 95% CI) | 0.34 [0.07, 0.61] |
| 2.2 Up to and including 3 months postradiotherapy | 1 | 41 | Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.90, 1.16] |
| 2.3 12 months postradiotherapy | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 0.32 [0.09, 0.55] |
| 3 Salivary flow rate (unstimulated) ‐ incidence of > 0.1 g in 5 min Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 12 months postradiotherapy | 1 | 175 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [1.13, 1.86] |
| 4 Salivary flow rate (stimulated) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 End of radiotherapy | 1 | 47 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐1.48, 1.30] |
| 4.2 Up to and including 3 months postradiotherapy | 1 | 41 | Mean Difference (IV, Random, 95% CI) | 0.38 [‐1.43, 2.19] |
| 4.3 12 months postradiotherapy | 1 | 27 | Mean Difference (IV, Random, 95% CI) | 0.82 [‐0.47, 2.11] |
| 5 Salivary flow rate (stimulated) ‐ incidence of > 0.1 g in 5 min Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 12 months postradiotherapy | 1 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.89, 1.41] |
| 6 Overall survival at 12 to 24 months postradiotherapy Show forest plot | 2 | 271 | Hazard ratio (Random, 95% CI) | 1.18 [0.85, 1.66] |
| 7 Overall survival ‐ narrative data Show forest plot | Other data | No numeric data | ||
| 8 Progression‐free survival at 12 to 24 months postradiotherapy Show forest plot | 2 | 247 | Hazard ratio (Random, 95% CI) | 0.94 [0.70, 1.27] |
| 9 Progression‐free survival Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1 18 months postradiotherapy | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.81, 1.51] |
| 10 Progression‐free survival ‐ narrative data Show forest plot | Other data | No numeric data | ||
| 11 Locoregional tumour control at 12 to 24 months postradiotherapy Show forest plot | 2 | 279 | Hazard ratio (Random, 95% CI) | 0.90 [0.74, 1.11] |
| 12 Locoregional tumour control ‐ narrative data Show forest plot | Other data | No numeric data | ||
| 13 Disease‐free survival Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.1 24 months postradiotherapy | 1 | 170 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.73, 1.21] |
| 14 Disease‐free survival Show forest plot | Other data | No numeric data | ||
| 15 Quality of life (Patient Benefit Questionnaire) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 End of radiotherapy | 1 | 298 | Mean Difference (IV, Random, 95% CI) | 0.38 [‐0.07, 0.83] |
| 15.2 Up to and including 3 months postradiotherapy | 1 | 233 | Mean Difference (IV, Random, 95% CI) | 0.52 [‐0.02, 1.06] |
| 15.3 12 months postradiotherapy | 1 | 180 | Mean Difference (IV, Random, 95% CI) | 0.70 [0.20, 1.20] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (0 to 4 scale ‐ grade 2 or above) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 12 months postradiotherapy | 1 | 49 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.58, 1.53] |
| 2 Overall survival ‐ narrative data Show forest plot | Other data | No numeric data | ||
| 3 Locoregional tumour control ‐ narrative data Show forest plot | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (0 to 4 scale ‐ grade 2 or above) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Up to and including 3 months postradiotherapy | 1 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.76, 1.40] |
| 1.2 12 months postradiotherapy | 1 | 127 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.42, 0.88] |
| 2 Overall survival Show forest plot | 1 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 48 months after radiotherapy | 1 | Hazard Ratio (Random, 95% CI) | 1.36 [0.89, 2.10] | |
| 3 Locoregional tumour control Show forest plot | 1 | Hazard Ratio (Random, 95% CI) | Subtotals only | |
| 3.1 48 months after radiotherapy | 1 | Hazard Ratio (Random, 95% CI) | 1.34 [0.76, 2.36] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 End of radiotherapy: Shenqi Fanghou recipe versus no intervention | 1 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.28, 0.55] |
| 1.2 End of radiotherapy: TWBXM versus placebo | 1 | 71 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.78, 1.03] |
| 1.3 Up to and including 3 months postradiotherapy: Jinlong capsules versus no intervention | 1 | 95 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.59, 1.36] |
| 2 Xerostomia Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 End of radiotherapy: TWBXM versus placebo | 1 | 68 | Mean Difference (IV, Random, 95% CI) | ‐2.41 [‐16.19, 11.37] |
| 2.2 Up to and including 3 months postradiotherapy: TWBXM versus placebo | 1 | 44 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐17.21, 17.01] |
| 3 Salivary flow rate (stimulated) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 End of radiotherapy: Chinese medicine versus no intervention | 1 | 50 | Mean Difference (IV, Random, 95% CI) | 0.09 [0.03, 0.15] |
| 4 Overall survival (12 months postRT) Show forest plot | 1 | 78 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.84, 1.30] |
| 5 Quality of life (EORTC‐C30) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 End of radiotherapy: TWBXM versus placebo | 1 | 68 | Mean Difference (IV, Random, 95% CI) | 2.39 [‐8.74, 13.52] |
| 5.2 Up to and including 3 months postradiotherapy: TWBXM versus placebo | 1 | 44 | Mean Difference (IV, Random, 95% CI) | 1.93 [‐13.04, 16.90] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (0 to 4 scale ‐ grade 2 or above) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Up to and including 3 months postRT | 3 | 471 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.77, 1.22] |
| 2 Overall survival at 42 to 72 months from baseline Show forest plot | 3 | Hazard Ratio (Random, 95% CI) | 1.00 [0.72, 1.39] | |
| 3 Progression‐free survival at 42 to 72 months from baseline Show forest plot | 3 | Hazard Ratio (Random, 95% CI) | 1.06 [0.80, 1.42] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (0 to 3 scale ‐ grade 2 or above) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 End of radiotherapy | 1 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.28, 0.66] |
| 1.2 Up to and including 3 months postradiotherapy | 1 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.65, 1.01] |
| 2 Salivary flow rate (unstimulated) ‐ ml/min Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 2 months postradiotherapy | 1 | 97 | Mean Difference (IV, Random, 95% CI) | 0.19 [0.06, 0.32] |
| 3 Salivary flow rate (stimulated) ‐ ml/min Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 2 months postradiotherapy | 1 | 97 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.03, 0.33] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (dry mouth? yes/no) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 End of radiotherapy | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.30, 1.29] |
| 1.2 8 to 40 weeks postradiotherapy | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.30, 1.05] |
| 2 Salivary flow rate (unstimulated) ‐ ml/min Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 End of radiotherapy | 1 | 36 | Mean Difference (IV, Random, 95% CI) | 0.12 [0.01, 0.23] |
| 2.2 8 to 40 weeks postradiotherapy | 1 | 33 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.02, 0.16] |
| 3 Salivary flow rate (stimulated) ‐ ml/min Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 End of radiotherapy | 1 | 32 | Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.03, 0.29] |
| 3.2 8 to 40 weeks postradiotherapy | 1 | 29 | Mean Difference (IV, Random, 95% CI) | 0.21 [0.01, 0.41] |
| 4 Overall survival Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 40 weeks postradiotherapy | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.43, 5.84] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia Show forest plot | Other data | No numeric data | ||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (QoL response for dryness) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Up to and including 3 months postradiotherapy | 1 | 133 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.97, 1.40] |
| 2 Quality of life Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Up to and including 3 months postradiotherapy (change score over 6 months) | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.65, 1.50] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Xerostomia (grade 2 or above) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 End of radiotherapy | 1 | 31 | Risk Ratio (M‐H, Random, 95% CI) | 0.17 [0.04, 0.65] |

