ارزیابی جامع سالمندان برای افراد مسن پذیرفته شده در یک مرکز خدمات جراحی
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع مطالعات در حال انجام
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Study design: Randomized trial. Study grouping: Parallel group. Study duration: June 2007 to September 2010 | |
| Participants | Setting: Inpatient hospital Country: The Neatherlands Baseline characteristics Geriatric care (n=148)
Control (n=149)
Inclusion criteria: Aged over 65 years, elective surgery for a solid tumour and Groningen Frailty Indicator > 3. Exclusion criteria: Groningen Frailty Indicator ≤ 3, unable to complete the study protocol and follow‐up schedule, unable to fill in the questionnaires used in this study. Pretreatment: No significant difference between groups. | |
| Interventions | Intervention characteristics Geriatric care
Control
| |
| Outcomes | Outcomes reported in the study matching our primary and secondary outcomes Mortality
Major complication ‐ delirium
Discharge to an increased level of care
Major complication ‐ cardiovascular
Major complication ‐ pulmonary
| |
| Identification | Sponsorship source: Netherlands Organisation for Health Research and Development. Country: Netherlands. Setting: University, teaching and community hospitals. Author's name: Liesbeth Hempenius. Institution: University of Groningen Email: [email protected] Address: University Center for Geriatric Medicine, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Interactive voice randomization service provided by the University Medical Centre Groningen with stratification tumour type and location. |
| Allocation concealment (selection bias) | Low risk | Judgement comment: Allocation by voice response service. |
| Blinding of participants and personnel (performance bias) | High risk | Participants from both arms were cared for by the same surgical team raising. Geriatric consultation was provided to the intervention arm but the primary outcome (delirium) is prone to bias. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "The doctor diagnosing a possible delirium was, however, masked to the study group". However, all other staff involved in the study were not blinded. |
| Baseline demographics between groups | Low risk | Demographics were similar between study arms. |
| Incomplete outcome data (attrition bias) | Low risk | Low attrition. |
| Protection from cross‐contamination | High risk | Quote: "As mentioned before, the ward and research nurses were not blinded to the group to which a patient was randomised. This could lead to contamination, that is, additional interventions in the standard care group. In the case of contamination, one would expect a decrease in the difference in the incidence rate of delirium between the groups as the study progressed. As the lines in Figure 2 are not convergent, this argues against contamination." |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Low risk | Judgement comment: Lower external validity due to strict inclusion criteria. |
| Methods | Study design: Randomized trial based on home address before admission Study grouping: Parallel group. Study duration: 16 months, unclear start date | |
| Participants | Setting: Inpatient hospital Country: United Kingdom Baseline characteristics Geriatric care (n=82)
Control (n=73)
Inclusion criteria: Fractured neck of femur aged over 65 years. Exclusion criteria: No exclusion criteria were reported Pretreatment: No difference between the groups. | |
| Interventions | Intervention characteristics Geriatric care
Control
| |
| Outcomes | Outcomes reported in the study matching our primary and secondary outcomes Mortality
Length of stay
Discharge to an increased level of care
| |
| Identification | Sponsorship source Country: UK. Setting: General hospital. Author's name: VJ Hempsall. Institution: Departments of Community Medicine' and Geriatric Medicine. Address: Department of Community Medicine, Royal Victoria Hospital, Shelley Road, Bournemouth BH1 4HX. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Random sequence was generated based on the participants geographic origin. |
| Allocation concealment (selection bias) | High risk | Allocation was by geography or origin. |
| Blinding of participants and personnel (performance bias) | Low risk | Unable to blind participants from the nature of their study arm, however the primary outcomes measured (mortality and LOS) are not prone to bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Unable to blind participants from the nature of their study arm, however the primary outcomes measured (mortality and LOS) are not prone to bias. |
| Baseline demographics between groups | Low risk | Populations were similar for reported demographic and medical variables. |
| Incomplete outcome data (attrition bias) | Low risk | Low dropout rate. |
| Protection from cross‐contamination | Unclear risk | Quote: "A prospective comparison was made of the outcome of patients from two geographical sectors, both receiving identical initial treatment at Poole General Hospital." |
| Selective reporting (reporting bias) | High risk | Did not report all outcomes that were expected. |
| Other bias | Low risk | No other bias noted. |
| Methods | Study design: Randomized trial. Study grouping: Parallel group. Study duration: 18 months, unclear start date | |
| Participants | Setting: Inpatient hospital Country: United Kingdom Baseline characteristics Geriatric care (n=54)
Control (n=54)
Inclusion criteria: Women aged 65 years and over with proximal femur fracture. Exclusion criteria: Died before becoming fit enough to enter the trial, pathological fractures, likely to be discharged within seven days of entering the trial, patient would return to nursing home after operation for further rehab, unfit for transfer. Pretreatment: Mental status. | |
| Interventions | Intervention characteristics Geriatric care
Control
| |
| Outcomes | Outcomes reported in the study matching our primary and secondary outcomes Discharge to an increased level of care
| |
| Identification | Sponsorship source: Forth Valley Health Board. Country: UK. Setting: District hospital acute admission ward and rehabilitation ward. Authors name: David C Kennie. Institution: Department of Geriatric Medicine, Royal infirmary, Stirling. Address: Department of Geriatric Medicine, Royal Infirmary, Stirling FK82AU. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sealed envelope randomization. |
| Allocation concealment (selection bias) | Unclear risk | Random sequence allocation but unclear if it was concealed before allocation. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were not blinded, but the outcome (discharge location) is not very prone to bias. |
| Blinding of outcome assessment (detection bias) | Unclear risk | The authors do not describe how or who assessed outcomes. The authors make no mention of blinding the outcome assessors. |
| Baseline demographics between groups | Unclear risk | The authors did not report comprehensive demographic data for the control and experimental arms. |
| Incomplete outcome data (attrition bias) | Low risk | Low attrition noted. |
| Protection from cross‐contamination | Low risk | Judgement comment: Participants were treated in different hospitals after initial postoperative recovery. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Unclear risk | This study examined women and cannot necessarily be applied to men. |
| Methods | Study design: Randomized trial. Study grouping: Parallel group. Study duration: Not reported | |
| Participants | Setting: Inpatient hospital Country: United States of America Baseline characteristics Geriatric care (n=62)
Control (n=64)
Inclusion criteria: 65 years and older with primary hip fracture. Exclusion criteria: Presence of metastatic cancer, life expectancy to less than 6 months, inability to obtain informed consent within 24 hours of surgery or 48 hours of admission. Pretreatment: Pre‐fracture dementia and ADL impairment, both higher in the usual‐care group. | |
| Interventions | Intervention characteristics Geriatric care
Control
| |
| Outcomes | Outcomes reported in the study matching our primary and secondary outcomes Major complication ‐ delirium
Major complication ‐ severe delirium
Days of delirium per episode
Discharge to an increased level of care
| |
| Identification | Sponsorship source: Older Americans Independence Center P60‐AG08812‐06, Charles Farnsworth Trust, Charles A King Trust. Country: USA. Setting: Tertiary academic center. Authors name: Edward R Marcantonio. Institution: Hebrew Rehabilitation Center for Aged. Address: 1200 Centre Street, Boston, MA 02131. | |
| Notes | We contacted the author for mortality and length of stay mean and standard deviation but the study is 16 years old and this information has been lost Marcantonio 2016 [pers comm]. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sealed envelope randomisation. |
| Allocation concealment (selection bias) | Low risk | No evidence that there was any deviation from standard randomisation techniques. |
| Blinding of participants and personnel (performance bias) | Low risk | Participants were not blinded to the intervention but the personnel assessing delirium were blind to the arm and there was reportedly no inadvertent unblinding. |
| Blinding of outcome assessment (detection bias) | Low risk | The assessor of delirium was blinded to the intervention arm of each participant. |
| Baseline demographics between groups | Low risk | There were no significant differences between trial arms in measured variables. |
| Incomplete outcome data (attrition bias) | Low risk | There was very low attrition in the trial. |
| Protection from cross‐contamination | High risk | Quote: "Sixty‐two of the 126 study patients were randomly assigned to proactive geriatrics consultation." Judgement comment: Orthopedics remained the primary physician in both arms of the study, raising significant risk of cross‐contamination. |
| Selective reporting (reporting bias) | Unclear risk | There is no evidence of selective reporting; however, we requested additional information from the authors including mortality. To date, the authors have been unable to provide further information. |
| Other bias | Unclear risk | Quote: "intervention involved 10 modules and multiple possible recommendations. Although we have re‐ ported what was recommended and the percent adherence, our design does not allow us to answer “What really made the difference?” |
| Methods | Study design: Randomized trial. Study grouping: Parallel group. Study duration: June 1993 to September 1997 | |
| Participants | Setting: Inpatient hospital Country: Canada Baseline characteristics Geriatric care (n=141)
Control (n=138)
Inclusion criteria: Aged at least 70 years, surgical repair of hip fracture. Exclusion criteria: Fracture occurring in an acute care hospital, pathologic fracture, multiple trauma, previous surgery on the fractured hip, expected survival fewer than 6 months, residence in a nursing home and dependence on at least one person for ambulation before the fracture, or residence outside metropolitan Toronto. Pretreatment: No statistically significant differences. | |
| Interventions | Intervention characteristics Geriatric care
Control
| |
| Outcomes | Outcomes reported in the study matching our primary and secondary outcomes Mortality
Length of stay
Discharge to an increased level of care
| |
| Identification | Sponsorship source: Ontario Ministry of Health Physicians Services Incorporated Foundation. Country: Canada. Setting: Teaching hospital. Authors name: Gary Naglie. Institution: UniversityHealth Network and Mount Sinai Hospital, Toronto. Email: [email protected] Address: Toronto general hospital, Rm. EN G‐233, 200 Elizabeth St, Toronto ON M5G 2C4. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified computer generated randomisation with block size of 4. |
| Allocation concealment (selection bias) | Low risk | Quote: "Orthopedic residents, who were blinded to block size, assigned the patients to treatment group according to sequentially numbered, sealed, opaque envelopes that were colour‐coded by stratum." |
| Blinding of participants and personnel (performance bias) | Low risk | Participants and outcome assessors were not blind, however the primary outcomes are not prone to bias (mortality and discharge location). |
| Blinding of outcome assessment (detection bias) | Low risk | Primary outcomes are at low risk of detection bias, follow‐up was conducted by blinded research assistants. |
| Baseline demographics between groups | Low risk | Quote: "There were no statistically significant differences between the intervention and control groups for any baseline characteristics". |
| Incomplete outcome data (attrition bias) | Low risk | There is no evidence of incomplete outcome reporting. |
| Protection from cross‐contamination | Low risk | Quote: "Staff in the interdisciplinary care ward held twice‐weekly rounds to develop and monitor treatment plans, whereas the usual care ward had no such rounds. The staff on the inter‐ disciplinary care ward worked together for a 10‐month pilot period before the start of the study." |
| Selective reporting (reporting bias) | Low risk | There is no evidence of selective reporting, all expected outcomes are present. |
| Other bias | Low risk | There is no evidence of additional bias. |
| Methods | Study design: Randomized trial. Study grouping: Parallel group. Study duration: April 18, 2008 to December 30, 2011 | |
| Participants | Setting: Inpatient hospital Country: Norway Baseline characteristics Geriatric care (n=198)
Control (n=199)
Inclusion criteria: Hip fractures, home‐dwelling people, aged 70 years or older who had been able to walk 10 m before the fracture. Exclusion criteria: Pathological fractures, multiple traumas, short life expectancy, who were living permanently in nursing homes or already participating in the investigation. Pretreatment: Baseline characteristics did not differ between the groups (table 2). | |
| Interventions | Intervention characteristics Geriatric care
Control
| |
| Outcomes | Outcomes reported in the study matching our primary and secondary outcomes Mortality
Length of stay
Total cost
Discharge to an increased level of care
Re‐admission
| |
| Identification | Sponsorship source: Norwegian Research Council, Central Norway Regional Health Authority, St Olav Hospital Trust and Fund for Research and Innovation, Liaison Committee between Central Norway Regional Health Authority and the Norwegian University of Science and Technology, the Department of Neuroscience at the Norwegian University of Science and Technology, Foundation for Scientific and Industrial Research at the Norwegian Institute of Technology (SINTEF), and the Municipality of Trondheim. Country: Norway. Setting: Regional referral hospital. Authors' names: Anders Prestmo, Gunhild Hagen. Institution: Department of Neuroscience, Norwegian University of Science and Technology. Email: [email protected] Address: Post Box 8905, N‐7491 Trondheim, Norway. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomisation. |
| Allocation concealment (selection bias) | Low risk | Computer randomised with unknown block size in emergency department. |
| Blinding of participants and personnel (performance bias) | Unclear risk | The outcomes studied are somewhat prone to performance bias and the manuscript does not clarify if the assessors were blinded to the intervention arm. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "Assessments were done by assessors who were not associated with patient care." Judgement comment: Does not say if assessors were blinded. |
| Baseline demographics between groups | Low risk | Quote: "Baseline characteristics did not differ between the groups". |
| Incomplete outcome data (attrition bias) | Low risk | All expected outcomes were reported. |
| Protection from cross‐contamination | Low risk | Each study arm was cared for on a different ward by separate staff including separate physicians. |
| Selective reporting (reporting bias) | Low risk | All expected results were reported. |
| Other bias | Low risk | No other risk of bias was noted. |
| Methods | Study design: Randomized trial. Study grouping: Parallel group. Study duration: May 2000 to December 2003 | |
| Participants | Setting: Inpatient hospital Country: Sweeden Baseline characteristics Geriatric care (n=102)
Control (n=97)
Inclusion criteria: Femoral neck fracture, aged ≥ 70 years. Exclusion criteria: Severe rheumatoid arthritis, severe hip osteoarthritis, pathological fracture, severe kidney failure, bedridden before the fracture. Pretreatment: Significant depression in control group. | |
| Interventions | Intervention characteristics Geriatric care
Control
| |
| Outcomes | Outcomes reported in the study matching our primary and secondary outcomes Length of stay
Mortality
Discharge to an increased level of care
Re‐admission
| |
| Identification | Sponsorship source: Vårdal Foundation”, the Joint Com‐mittee of the Northern Health Region of Sweden (Visare Norr), the JC Kempe Memorial Foundation, the Dementia Fund, the Foundation of the Medical Faculty, the Borgerskapet of Umeå Research Foundation, the Erik and Anne‐Marie Detlof’s Foundation, University of Umeå and the County Council of Västerbotten (“Dagmar”, “FoU”, and “Äldre Centrum Västerbotten”) and the Swedish Research Council, grants K2002‐27VP‐14165‐02B, K2002‐27VX‐14172‐02B, K2005‐27VX‐15357‐01A. Country: Sweden. Setting: University Hospital. Authors name: Michael Stenvall. Institution: Umeå University. Email: [email protected] Address: Department of Community Medicine and Rehabilitation, Geriatric Medicine, Umeå University, SE‐901 87 Umeå, Sweden. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Opaque sealed envelope randomisation. |
| Allocation concealment (selection bias) | Low risk | Judgement comment: opaque sealed envelopes to allocate participants. Envelopes were opened immediately before surgery to ensure similar pre‐operative treatment. |
| Blinding of participants and personnel (performance bias) | Low risk | Outcomes assessed are unlikely to be influenced by bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The assessors were aware of the study‐group allocation during the study period." However the outcomes measured are not prone to bias (mortality, re‐admission and discharge location). |
| Baseline demographics between groups | Low risk | There were small differences at baseline between groups, however all outcome were analyzed after controlling for these differences. |
| Incomplete outcome data (attrition bias) | Low risk | All expected outcomes were reported. |
| Protection from cross‐contamination | Unclear risk | Judgement comment: Staff were aware of the study but participants were not cared for on the same ward. It is unclear if the orthopedic surgeons were actively involved in the postoperative care of the intervention cohort. |
| Selective reporting (reporting bias) | Low risk | There is no evidence of selective reporting. |
| Other bias | Low risk | No other evidence of bias was noted. |
| Methods | Study design: Randomized trial. Study grouping: Parallel group Study duration: February 1, 1997 to December 15, 1998 | |
| Participants | Setting: Inpatient hospital Country: Spain Baseline characteristics Geriatric care (n=155)
Control (n=164)
Inclusion criteria: Aged 65 years and over, who were admitted to Hospital General Universitario between 1 February and 15 December 1997 for acute hip fracture surgery. Exclusion criteria: Inability to walk before the fracture, dependency in all basic ADLs (ADL50), pathological hip fracture and known terminal illnesses, defined as those associated with a life expectancy of fewer than 12 months. Pretreatment: No significant differences. | |
| Interventions | Intervention characteristics Geriatric care
Control
| |
| Outcomes | Outcomes reported in the study matching our primary and secondary outcomes Mortality
Major complication
Major complication ‐ delirium
Length of stay
| |
| Identification | Sponsorship source: The study was supported by a grant from the Fondo de Investigaciones Sanitarias (FIS 97/0542), Ministerio de Sanidad, Spain. Country: Spain. Setting: University hospital. Author's name: Maite Vidan. Institution: Hospital General Universitario Gregorio Maran. Email: [email protected] Address: Department of Geriatric Medicine, Hospital General Universitario Gregorio, Dr. Esquerdo 46, 28007, Spain. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After baseline assessment, patients were randomised to the intervention or usual care group," Quote: "Homogeneity of groups according to stratified randomisation was proved." Quote: "After baseline assessment, patients were randomised to the intervention or usual care group, stratified by pre‐fracture ADL level: inde‐ pendent in four or more or less than four ADLs." Judgement comment: Does not explain randomization procedure. |
| Allocation concealment (selection bias) | Unclear risk | It is unclear how randomization was performed. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Composit outcome includes delirium and it is not clear if the assessor was blinded. Outher outcomes, including LOS and mortality are not prone to this bias. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: "The baseline assessment was made using personal patient interviews on admission, before randomisation." but it is unclear if the chart review was conducted by a blinded individual. |
| Baseline demographics between groups | Low risk | No difference between arms at baseline. |
| Incomplete outcome data (attrition bias) | Unclear risk | Attrition is not reported. |
| Protection from cross‐contamination | High risk | The intervention and control arms shared the same wards and used the same allied health services. |
| Selective reporting (reporting bias) | Low risk | No evidence of selective reporting. |
| Other bias | Low risk | No other sources of bias identified |
ADL: activities of daily living; CCI: Charlson Comorbidity Index; DVT: deep vein thrombosis; LOS ‐ length of stay; MI: myocardial infarction; PE: pulmonary embolism; SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Wrong setting. | |
| Wrong intervention. | |
| Wrong outcomes. | |
| Wrong outcomes. | |
| No full geriatric assessment. | |
| Wrong patient population. | |
| Wrong patient population. | |
| Wrong patient population. | |
| Wrong patient population. | |
| Wrong comparator. | |
| Wrong intervention. | |
| Wrong patient population. | |
| Wrong patient population. | |
| Adult population. | |
| Wrong outcomes. | |
| Wrong patient population. | |
| Study was terminated earlier due to insufficient enrollment of participants. | |
| Wrong outcomes. | |
| Adult population. | |
| Wrong outcomes. | |
| Wrong outcomes. | |
| Adult population. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Unknown |
| Methods | Randomized controlled comparison of orthopedic versus orthogeriatric care of older people with hip fracture. |
| Participants | People aged 65 years and older, who could walk outdoors before fracture, presenting with low‐impact hip fracture. |
| Interventions | Orthogeriatric care compared to usual orthopedic care. |
| Outcomes | Estimate the effect of orthogeriatric co management on the prescription of appropriate anti fracture therapy at hospital discharge. The secondary aim of the study is to evaluate adherence to treatments, mobility and functional independence at 6 and 12 months from surgery. |
| Starting date | Unknown. |
| Contact information | Unknown. |
| Notes | University of Perugia, Perugia, Italy. |
| Trial name or title | EGeSOR |
| Methods | Open‐label, multicenter, randomised, controlled, parallel‐group trial. |
| Participants | People aged 70 years or older and receiving standard care for head and neck squamous cell carcinoma. |
| Interventions | Comprehensive geriatric assessment and standardized geriatric care. |
| Outcomes | The primary endpoint, assessed after 6 months, is a composite criterion including death, functional impairment [Activities of Daily Living score decrease ≥ 2], and weight loss ≥10%. Secondary endpoints include progression‐free survival, unscheduled admissions, quality of life, treatment toxicities, costs, and completion of the planned cancer treatment. |
| Starting date | Unknown |
| Contact information | |
| Notes |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 5 | 1316 | Risk Ratio (IV, Random, 95% CI) | 0.85 [0.68, 1.05] |
| Analysis 1.1  Comparison 1 Geriatric care versus control, Outcome 1 Mortality. | ||||
| 1.1 4 to 6 months | 2 | 476 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.46, 1.20] |
| 1.2 1 year | 3 | 840 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.69, 1.11] |
| 2 Discharge to an increased level of care Show forest plot | 5 | 941 | Risk Ratio (IV, Random, 95% CI) | 0.71 [0.55, 0.92] |
| Analysis 1.2  Comparison 1 Geriatric care versus control, Outcome 2 Discharge to an increased level of care. | ||||
| 2.1 Discharge | 1 | 108 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.12, 0.79] |
| 2.2 4 to 6 months | 2 | 344 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.54, 1.21] |
| 2.3 1 year | 2 | 489 | Risk Ratio (IV, Random, 95% CI) | 0.73 [0.52, 1.03] |
| 3 Length of stay Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 Geriatric care versus control, Outcome 3 Length of stay. | ||||
| 3.1 Acute hospital discharge | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Discharge | 4 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Re‐admission Show forest plot | 3 | 741 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.76, 1.32] |
| Analysis 1.4  Comparison 1 Geriatric care versus control, Outcome 4 Re‐admission. | ||||
| 4.1 1 to 3 months | 1 | 225 | Risk Ratio (IV, Random, 95% CI) | 1.25 [0.74, 2.09] |
| 4.2 1 year | 2 | 516 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.67, 1.33] |
| 5 Major complication Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 Geriatric care versus control, Outcome 5 Major complication. | ||||
| 5.1 Discharge | 2 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Major complication ‐ delirium Show forest plot | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.6  Comparison 1 Geriatric care versus control, Outcome 6 Major complication ‐ delirium. | ||||
| 6.1 Discharge | 3 | 705 | Risk Ratio (IV, Random, 95% CI) | 0.75 [0.60, 0.94] |

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Geriatric care versus control, Outcome 1 Mortality.

Comparison 1 Geriatric care versus control, Outcome 2 Discharge to an increased level of care.
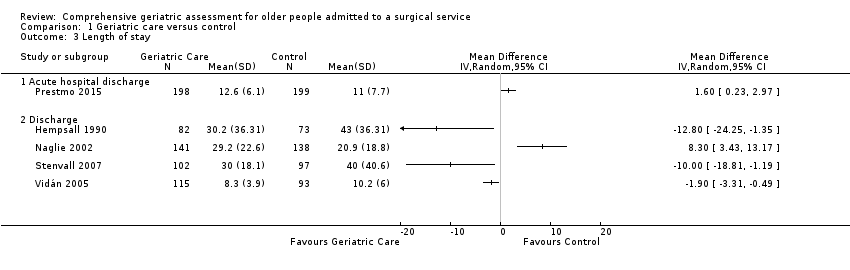
Comparison 1 Geriatric care versus control, Outcome 3 Length of stay.

Comparison 1 Geriatric care versus control, Outcome 4 Re‐admission.

Comparison 1 Geriatric care versus control, Outcome 5 Major complication.

Comparison 1 Geriatric care versus control, Outcome 6 Major complication ‐ delirium.
| Comprehensive geriatric assessment for older people admitted to a surgical service | ||||||
| Patient or population: Improving outcomes in older adult people admitted to a surgical service. | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with control | Risk with geriatric care | |||||
| Mortality | 214 per 1000 | 182 per 1000 | RR 0.85 | 1316 | ⊕⊕⊕◯ 1 | Hip fracture studies. |
| Discharge to an increased level of care | 247 per 1000 | 176 per 1000 | RR 0.71 | 941 | ⊕⊕⊕⊕ | Hip fracture studies. |
| Length of stay | Meta‐analysis was not performed due to high heterogeneity (Analysis 1.3) | MD in studies ranged from ‐12.8 days to 8.3 days | ‐ | 841 | ⊕⊕⊕⊝ | Hip fracture studies ‐ length of stay until final discharge from hospital (including rehabilitation hospital). Meta‐analysis was not retained due to high heterogeneity (I² = 88%, P < 0.00001). |
| Re‐admission | 316 per 1000 | 316 per 1000 | RR 1.00 | 741 | ⊕⊕⊕⊝ | All studies included; removing elective surgical oncology study doesn't change effect. |
| Total cost | The mean total cost was EUR 59,486 | MD EUR 5154 lower | 397 | ⊕⊕⊕⊝ | 1 study reported cost. | |
| Major complication | Meta‐analysis was not performed due to high heterogeneity (Analysis 1.5) | Two studies reported this outcome with RRs of 0.74 and 1.16 | 579 | ⊕⊕⊝⊝ | Hempenius 2013 defined major as 2 or more complications. Vidán 2005 defined major as delirium, congestive heart failure, pneumonia, DVT, PE, pressure ulcer, arrhythmia and myocardial infarction. Meta‐analysis was not retained due to high heterogeneity (I² = 77%, P = 0.04). | |
| Major complication ‐ delirium | 327 per 1000 | 245 per 1000 | RR 0.75 | 705 | ⊕⊕⊝⊝ | Delirium assessed by Delirium Observation Scale (Hempenius 2013) or confusion assessment method (Marcantonio 2001; Vidán 2005) |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 We downgraded due to imprecision because there were wide confidence intervals that include both no effect and a high risk of benefit or harm. 2 We downgraded due to inconsistency because there was significant variability among studies. 3 We downgraded due to other considerations because costing was calculated in an imprecise manner (costs are presented as the total cost over one year, however the admission cost did not include rehabilitation hospital costs despite the authors identifying a higher proportion of control patients being transferred to rehabilitation centres before discharge). 4 We downgraded due to the high risk of bias. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 5 | 1316 | Risk Ratio (IV, Random, 95% CI) | 0.85 [0.68, 1.05] |
| 1.1 4 to 6 months | 2 | 476 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.46, 1.20] |
| 1.2 1 year | 3 | 840 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.69, 1.11] |
| 2 Discharge to an increased level of care Show forest plot | 5 | 941 | Risk Ratio (IV, Random, 95% CI) | 0.71 [0.55, 0.92] |
| 2.1 Discharge | 1 | 108 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.12, 0.79] |
| 2.2 4 to 6 months | 2 | 344 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.54, 1.21] |
| 2.3 1 year | 2 | 489 | Risk Ratio (IV, Random, 95% CI) | 0.73 [0.52, 1.03] |
| 3 Length of stay Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Acute hospital discharge | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Discharge | 4 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Re‐admission Show forest plot | 3 | 741 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.76, 1.32] |
| 4.1 1 to 3 months | 1 | 225 | Risk Ratio (IV, Random, 95% CI) | 1.25 [0.74, 2.09] |
| 4.2 1 year | 2 | 516 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.67, 1.33] |
| 5 Major complication Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Discharge | 2 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Major complication ‐ delirium Show forest plot | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Discharge | 3 | 705 | Risk Ratio (IV, Random, 95% CI) | 0.75 [0.60, 0.94] |

