Evaluación geriátrica integral para pacientes mayores ingresados en un servicio quirúrgico
Información
- DOI:
- https://doi.org/10.1002/14651858.CD012485.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 31 enero 2018see what's new
- Tipo:
-
- Intervention
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Práctica y organización sanitaria efectivas
- Copyright:
-
- Copyright © 2018 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
QD and GE coordinated the contributions from the co‐authors. QD, SC, TC, and GE worked on the methods sections. QD and GE drafted the clinical sections of the background, and TC was the contract person with the editorial base. QD and GE wrote the protocol with assistance from AT, SC, RK, and TC. TC devised and carried out the search strategy. QD, GE, and SC wrote the statistical analysis and data synthesis sections. RK, SC, QD, GE, and AT contributed significantly to the review. XS provided guidance for statistical analysis. Abstracts, results, discussion and conclusions were written by GE. Editing and revision of these sections was performed by the remainder of the team.
Sources of support
Internal sources
-
University of Alberta, Canada.
Salary support for: AT, TC, RK
External sources
-
Canadian Frailty Network, Canada.
Canadian Frailty Network Interdisciplinary Fellowship 2016 for: GE
-
Alberta Innovates Health Solutions, Canada.
AIHS Summer studentship for: QD
Declarations of interest
Gilgamesh Eamer: none known.
Amir Taheri: none known.
Sidian S Chen: none known.
Quinn Daviduck: none known.
Thane Chambers: none known.
Xinzhe Shi: none known.
Rachel G Khadaroo: none known.
Acknowledgements
As part of the pre‐publication editorial process, the protocol was commented on by Graham Ellis, Julia Worswick, Kristoffer Yungpeng Ding, Paul Miller, and Sasha Shepperd. We thank them for their valuable contribution to the protocol. We would like to thank Liz Dennett and Paul Miller for reviewing and providing excellent feedback on the search strategy.
The full review was commented on by Julia Worswick and Daniela Gonçalves Bradley before peer referee. Both provided critical appraisal and editorial assistance. External review was conducted by Lynn Shields, Andrea Schoenenberger, Sofia Massa, and Paul Miller. We are grateful for their thoughtful and thorough review and comments. Signe Flottorp and Sasha Shepperd provided editorial support.
Finally, we acknowledge the National Institute for Health Research, via Cochrane Infrastructure funding to the Effective Practice and Organisation of Care Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, National Institute for Health Research, National Health Service, or the Department of Health.
Version history
| Published | Title | Stage | Authors | Version |
| 2018 Jan 31 | Comprehensive geriatric assessment for older people admitted to a surgical service | Review | Gilgamesh Eamer, Amir Taheri, Sidian S Chen, Quinn Daviduck, Thane Chambers, Xinzhe Shi, Rachel G Khadaroo | |
| 2017 Jan 03 | Comprehensive geriatric assessment for improving outcomes in elderly patients admitted to a surgical service | Protocol | Gilgamesh Eamer, Amir Taheri, Sidian S Chen, Quinn Daviduck, Thane Chambers, Xinzhe Shi, Rachel G Khadaroo | |
Differences between protocol and review
We performed minimal subgroup analysis due to the small number of included trials. We were unable to assess comprehensive geriatric assessment (CGA) timing and emergency versus elective subgroup analyses. We performed surgical specialty subgroup analyses by excluding the non‐orthopedic study from analysis. We were unable to perform sensitivity analysis by bias due to the small number of low risk studies reporting each outcome. We were also unable to assess publication bias by constructing funnel plots, also due to the small number of included trials. We did not identify any cluster randomised trials for inclusion, so did not experience any unit of analysis issues. There were low attrition rates in all included studies, so we did not impute any missing data. We attempted to contact study authors who we felt may have had more data, but the time elapsed since may included studies were completed meant that few additional data were available.
Notes
This review is based on standard text and guidance provided by the Cochrane Effective Practice and Organisation of Care (EPOC) Group.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
- *Geriatric Assessment;
- *Length of Stay;
- Delirium [epidemiology];
- Elective Surgical Procedures [mortality];
- Hip Fractures [mortality, *surgery];
- Neoplasms [mortality, *surgery];
- Patient Readmission [statistics & numerical data];
- Postoperative Complications [epidemiology];
- Randomized Controlled Trials as Topic;
- Treatment Outcome;
Medical Subject Headings Check Words
Aged; Humans;
PICO

Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 Geriatric care versus control, Outcome 1 Mortality.

Comparison 1 Geriatric care versus control, Outcome 2 Discharge to an increased level of care.
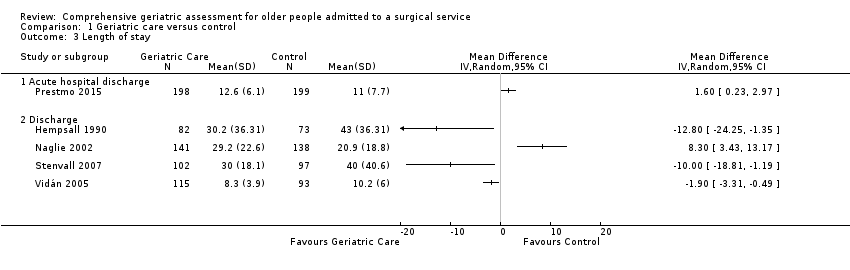
Comparison 1 Geriatric care versus control, Outcome 3 Length of stay.

Comparison 1 Geriatric care versus control, Outcome 4 Re‐admission.

Comparison 1 Geriatric care versus control, Outcome 5 Major complication.

Comparison 1 Geriatric care versus control, Outcome 6 Major complication ‐ delirium.
| Comprehensive geriatric assessment for older people admitted to a surgical service | ||||||
| Patient or population: Improving outcomes in older adult people admitted to a surgical service. | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
| Risk with control | Risk with geriatric care | |||||
| Mortality | 214 per 1000 | 182 per 1000 | RR 0.85 | 1316 | ⊕⊕⊕◯ 1 | Hip fracture studies. |
| Discharge to an increased level of care | 247 per 1000 | 176 per 1000 | RR 0.71 | 941 | ⊕⊕⊕⊕ | Hip fracture studies. |
| Length of stay | Meta‐analysis was not performed due to high heterogeneity (Analysis 1.3) | MD in studies ranged from ‐12.8 days to 8.3 days | ‐ | 841 | ⊕⊕⊕⊝ | Hip fracture studies ‐ length of stay until final discharge from hospital (including rehabilitation hospital). Meta‐analysis was not retained due to high heterogeneity (I² = 88%, P < 0.00001). |
| Re‐admission | 316 per 1000 | 316 per 1000 | RR 1.00 | 741 | ⊕⊕⊕⊝ | All studies included; removing elective surgical oncology study doesn't change effect. |
| Total cost | The mean total cost was EUR 59,486 | MD EUR 5154 lower | 397 | ⊕⊕⊕⊝ | 1 study reported cost. | |
| Major complication | Meta‐analysis was not performed due to high heterogeneity (Analysis 1.5) | Two studies reported this outcome with RRs of 0.74 and 1.16 | 579 | ⊕⊕⊝⊝ | Hempenius 2013 defined major as 2 or more complications. Vidán 2005 defined major as delirium, congestive heart failure, pneumonia, DVT, PE, pressure ulcer, arrhythmia and myocardial infarction. Meta‐analysis was not retained due to high heterogeneity (I² = 77%, P = 0.04). | |
| Major complication ‐ delirium | 327 per 1000 | 245 per 1000 | RR 0.75 | 705 | ⊕⊕⊝⊝ | Delirium assessed by Delirium Observation Scale (Hempenius 2013) or confusion assessment method (Marcantonio 2001; Vidán 2005) |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 We downgraded due to imprecision because there were wide confidence intervals that include both no effect and a high risk of benefit or harm. 2 We downgraded due to inconsistency because there was significant variability among studies. 3 We downgraded due to other considerations because costing was calculated in an imprecise manner (costs are presented as the total cost over one year, however the admission cost did not include rehabilitation hospital costs despite the authors identifying a higher proportion of control patients being transferred to rehabilitation centres before discharge). 4 We downgraded due to the high risk of bias. | ||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mortality Show forest plot | 5 | 1316 | Risk Ratio (IV, Random, 95% CI) | 0.85 [0.68, 1.05] |
| 1.1 4 to 6 months | 2 | 476 | Risk Ratio (IV, Random, 95% CI) | 0.74 [0.46, 1.20] |
| 1.2 1 year | 3 | 840 | Risk Ratio (IV, Random, 95% CI) | 0.87 [0.69, 1.11] |
| 2 Discharge to an increased level of care Show forest plot | 5 | 941 | Risk Ratio (IV, Random, 95% CI) | 0.71 [0.55, 0.92] |
| 2.1 Discharge | 1 | 108 | Risk Ratio (IV, Random, 95% CI) | 0.31 [0.12, 0.79] |
| 2.2 4 to 6 months | 2 | 344 | Risk Ratio (IV, Random, 95% CI) | 0.81 [0.54, 1.21] |
| 2.3 1 year | 2 | 489 | Risk Ratio (IV, Random, 95% CI) | 0.73 [0.52, 1.03] |
| 3 Length of stay Show forest plot | 5 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Acute hospital discharge | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Discharge | 4 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Re‐admission Show forest plot | 3 | 741 | Risk Ratio (IV, Random, 95% CI) | 1.00 [0.76, 1.32] |
| 4.1 1 to 3 months | 1 | 225 | Risk Ratio (IV, Random, 95% CI) | 1.25 [0.74, 2.09] |
| 4.2 1 year | 2 | 516 | Risk Ratio (IV, Random, 95% CI) | 0.95 [0.67, 1.33] |
| 5 Major complication Show forest plot | 2 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Discharge | 2 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Major complication ‐ delirium Show forest plot | 3 | Risk Ratio (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Discharge | 3 | 705 | Risk Ratio (IV, Random, 95% CI) | 0.75 [0.60, 0.94] |

