Estrategias para mejorar la implementación de políticas o prácticas en el lugar de trabajo orientadas al tabaco, el alcohol, la dieta, la actividad física y la obesidad
Appendices
Appendix 1. Search strategy
Database: MEDLINE 1946 to present with daily update (OVID)
Search strategy:
# Searches
1 Workplace/
2 Work/
3 Occupational Health/
4 Occupational Medicine/
5 1 or/1‐4
6 Health Behavior/
7 Health Education/
8 Health Promotion/
9 Healthy People Programs/
10 exp Primary Prevention/
11 Randomized Controlled Trial/
12 Controlled Clinical Trial/
13 Clinical Trials as Topic/
14 Random Allocation/
15 Evaluation Studies/
16 Comparative Study/
17 random*.tw.
18 trial.tw.
19 groups.tw.
20 placebo.tw.
21 experiment*.tw.
22 (time adj series).tw.
23 (pretest or pre test or posttest or post test).tw.
24 impact.tw.
25 change*.tw.
26 evaluat*.tw.
27 effect*.tw.
28 "before and after".tw.
29 intervention*.tw.
30 program*.tw.
31 compare*.tw.
32 (control or controls* or controla* or controle* or controli or controll*).tw.
33 or/6‐32
34 implement*.mp.
35 dissemin*.mp.
36 adopt*.mp.
37 practice*.mp.
38 organi?ational change*.mp.
39 diffus*.mp.
40 (system* adj2 change*).mp.
41 quality improvement*.mp.
42 transform*.mp.
43 translat*.mp.
44 transfer*.mp.
45 uptake*.mp.
46 sustainab*.mp.
47 institutionali*.mp.
48 routin*.mp.
49 maintenance.mp.
50 capacity.mp.
51 incorporat*.mp.
52 adher*.mp.
53 integrat*.mp.
54 scal*.mp.
55 ((polic* or practice* or program* or innovation*) adj5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)).mp.
56 or/34‐55
57 exp Obesity/
58 Weight Gain/
59 exp Weight Loss/
60 obes*.af.
61 (weight gain or weight loss).af.
62 (overweight or over weight or overeat* or over eat*).af.
63 weight change*.af.
64 ((bmi or body mass index) adj2 (gain or loss or change)).af.
65 exp Primary Prevention/
66 (primary prevention or secondary prevention).af.
67 (preventive measure* or preventative measure*).af.
68 (preventive care or preventative care).af.
69 (obesity adj2 (prevent* or treat*)).af.
70 or/57‐69
71 exp Exercise/
72 physical inactivity.mp.
73 physical activity.mp.
74 exp Motor Activity/
75 (physical education and training).mp.
76 exp "Physical Education and Training"/
77 Physical Fitness/
78 sedentary.tw.
79 exp Life Style/
80 exp Leisure Activities/
81 exp Sports/
82 Dancing/
83 dancing.mp.
84 (exercise* adj aerobic*).tw.
85 sport*.tw.
86 ((life style or life style) adj5 activ*).tw.
87 or/71‐86
88 exp Diet/
89 nutrition*.mp.
90 healthy eating.mp.
91 fruit*.tw.
92 vegetable*.tw.
93 canteen.mp.
94 menu.tw.
95 (calorie or calories).tw.
96 energy intake.tw.
97 energy density.tw.
98 eating.tw.
99 (feeding behavior or feeding behaviour).tw.
100 dietary intake.tw.
101 food.tw.
102 soft drink*.tw.
103 soda.tw.
104 sweetened drink*.tw.
105 fat.tw.
106 confectionary.tw.
107 menu planning.tw.
108 feeding program*.tw.
109 nutrition program*.tw.
110 nutritional program*.tw.
111 cafeteria*.tw.
112 nutritional status.tw.
113 or/88‐112
114 exp Smoking/
115 exp "tobacco Use Cessation"/
116 smok*.mp.
117 nicotine.mp.
118 tobacco use*.tw.
119 tobacco.mp.
120 exp tobacco/
121 or/114‐120
122 cessation.tw.
123 prevent*.tw.
124 stop*.tw.
125 quit*.tw.
126 abstin*.tw.
127 abstain*.tw.
128 reduc*.tw.
129 "tobacco use disorder".mp.
130 ex‐smoker*.mp.
131 anti‐smok*.mp.
132 or/122‐131
133 121 and 132
134 exp Alcohols/
135 exp Alcohol Drinking/
136 exp Alcohol Abuse/
137 exp Alcohol, Ethyl/ae
138 alcohol*.mp.
139 Drink*.mp.
140 liquor*.mp.
141 beer*.mp.
142 wine*.mp.
143 spirit*.mp.
144 drunk*.mp.
145 intoxicat*.mp.
146 binge.mp.
147 or/134‐146
148 70 or 87 or 113 or or 133 or 147
149 5 and 33 and 56 and 148
Database: MEDLINE In‐Process & Other Non‐Indexed Citations (OVID)
Search strategy:
# Searches
1 workplace*.mp.
2 work.mp.
3 Occupational Health.mp.
4 Occupational Medicine.mp.
5 1 or 2 or 3 or 4
6 Health Behavio?r*.mp.
7 Health Education.mp.
8 health promotion.mp.
9 Healthy People Program*.mp.
10 Primary Prevention.mp.
11 Randomized Controlled Trial/
12 Controlled Clinical Trial/
13 Evaluation Studies/
14 Comparative Study/
15 random*.tw.
16 trial.tw.
17 groups.tw.
18 placebo.tw.
19 experiment*.tw.
20 (time adj series).tw.
21 (pretest or pre test or posttest or post test).tw.
22 impact.tw.
23 change*.tw.
24 evaluat*.tw.
25 effect*.tw.
26 "before and after".tw.
27 intervention*.tw.
28 program*.tw.
29 compare*.tw.
30 (control or controls* or controla* or controle* or controli or controll*).tw.
31 or/6‐30
32 implement*.mp.
33 dissemin*.mp.
34 adopt*.mp.
35 practice*.mp.
36 organi?ational change*.mp.
37 diffus*.mp.
38 (system* adj2 change*).mp.
39 quality improvement*.mp.
40 transform*.mp.
41 translat*.mp.
42 transfer*.mp.
43 uptake*.mp.
44 sustainab*.mp.
45 institutionali*.mp.
46 routin*.mp.
47 maintenance.mp.
48 capacity.mp.
49 incorporat*.mp.
50 adher*.mp.
51 integrat*.mp.
52 scal*.mp.
53 ((polic* or practice* or program* or innovation*) adj5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)).mp.
54 or/32‐53
55 exp Obesity/
56 Weight Gain/
57 exp Weight Loss/
58 obes*.af.
59 (weight gain or weight loss).af.
60 (overweight or over weight or overeat* or over eat*).af.
61 weight change*.af.
62 ((bmi or body mass index) adj2 (gain or loss or change)).af.
63 exp Primary Prevention/
64 (primary prevention or secondary prevention).af.
65 (preventive measure* or preventative measure*).af.
66 (preventive care or preventative care).af.
67 (obesity adj2 (prevent* or treat*)).af.
68 or/55‐67
69 exp Exercise/
70 physical inactivity.mp.
71 physical activity.mp.
72 exp Motor Activity/
73 (physical education and training).mp.
74 exp "Physical Education and Training"/
75 Physical Fitness/
76 sedentary.tw.
77 exp Life Style/
78 exp Leisure Activities/
79 exp Sports/
80 Dancing/
81 dancing.mp.
82 (exercise* adj aerobic*).tw.
83 sport*.tw.
84 ((life style or life style) adj5 activ*).tw.
85 or/69‐84
86 exp Diet/
87 nutrition*.mp.
88 healthy eating.mp.
89 fruit*.tw.
90 vegetable*.tw.
91 canteen.mp.
92 menu.tw.
93 (calorie or calories).tw.
94 energy intake.tw.
95 energy density.tw.
96 eating.tw.
97 (feeding behavior or feeding behaviour).tw.
98 dietary intake.tw.
99 food.tw.
100 soft drink*.tw.
101 soda.tw.
102 sweetened drink*.tw.
103 fat.tw.
104 confectionary.tw.
105 menu planning.tw.
106 feeding program*.tw.
107 nutrition program*.tw.
108 nutritional program*.tw.
109 cafeteria*.tw.
110 nutritional status.tw.
111 or/86‐110
112 exp Smoking/
113 exp "tobacco Use Cessation"/
114 smok*.mp.
115 nicotine.mp.
116 tobacco use*.tw.
117 tobacco.mp.
118 exp tobacco/
119 or/112‐118
120 cessation.tw.
121 prevent*.tw.
122 stop*.tw.
123 quit*.tw.
124 abstin*.tw.
125 abstain*.tw.
126 reduc*.tw.
127 "tobacco use disorder".mp.
128 ex‐smoker*.mp.
129 anti‐smok*.mp.
130 or/120‐129
131 119 and 130
132 exp Alcohols/
133 exp Alcohol Drinking/
134 exp Alcohol Abuse/
135 exp Alcohol, Ethyl/ae
136 alcohol*.mp.
137 Drink*.mp.
138 liquor*.mp.
139 beer*.mp.
140 wine*.mp.
141 spirit*.mp.
142 drunk*.mp.
143 intoxicat*.mp.
144 binge.mp.
145 or/132‐144
146 68 or 85 or 111 or 131 or 145
147 5 and 31 and 54 and 146
Database: PsycINFO 1806 to May 2016 (OVID)
Search strategy:
# Searches
1 WORKPLACE INTERVENTION/ or Workplace.mp.
2 work.mp.
3 exp Occupational Health/
4 Occupational Medicine.mp.
5 1 or 2 or 3 or 4
6 Health Behavior/
7 Health Education/
8 Health Promotion/
9 Healthy People Program*.mp.
10 Primary prevention.mp.
11 exp Clinical Trials/
12 Evaluation Stud*.mp.
13 Comparative Stud*.mp.
14 random*.tw.
15 trial.tw.
16 groups.tw.
17 placebo.tw.
18 experiment*.tw.
19 (time adj series).tw.
20 (pretest or pre test or posttest or post test).tw.
21 impact.tw.
22 change*.tw.
23 evaluat*.tw.
24 effect*.tw.
25 "before and after".tw.
26 intervention*.tw.
27 program*.tw.
28 compare*.tw.
29 (control or controls* or controla* or controle* or controli or controll*).tw.
30 or/6‐29
31 implement*.mp.
32 dissemin*.mp.
33 adopt*.mp.
34 practice*.mp.
35 organi?ational change*.mp.
36 diffus*.mp.
37 (system* adj2 change*).mp.
38 quality improvement*.mp.
39 transform*.mp.
40 translat*.mp.
41 transfer*.mp.
42 uptake*.mp.
43 sustainab*.mp.
44 institutionali*.mp.
45 routin*.mp.
46 maintenance.mp.
47 capacity.mp.
48 incorporat*.mp.
49 adher*.mp.
50 integrat*.mp.
51 scal*.mp.
52 ((polic* or practice* or program* or innovation*) adj5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*)).mp.
53 or/31‐52
54 Obesity/
55 Weight Gain/
56 Weight Loss/
57 obes*.af.
58 (weight gain or weight loss).af.
59 (overweight or over weight or overeat* or over eat*).af.
60 weight change*.af.
61 ((bmi or body mass index) adj2 (gain or loss or change)).af.
62 (primary prevention or secondary prevention).af.
63 (preventive measure* or preventative measure*).af.
64 (preventive care or preventative care).af.
65 (obesity adj2 (prevent* or treat*)).af.
66 or/54‐65
67 exp EXERCISE/
68 physical inactivity.mp.
69 exp Physical Activity/
70 Motor Activity.mp.
71 (physical education and training).mp.
72 exp Physical Education/
73 Physical Fitness/
74 exp SEDENTARY BEHAVIOR/ or sedentary.mp.
75 exp Lifestyle/
76 exp Leisure Time/ or Leisure Activities.mp.
77 exp SPORTS/
78 exp Dance/ or Dancing.mp.
79 (exercise* adj aerobic*).tw.
80 sport*.tw.
81 ((life style or life style) adj5 activ*).tw.
82 or/67‐81
83 Diet.mp.
84 nutrition*.mp.
85 healthy eating.mp.
86 fruit*.tw.
87 vegetable*.tw.
88 canteen.mp.
89 menu.tw.
90 (calorie or calories).tw.
91 energy intake.tw.
92 energy density.tw.
93 eating.tw.
94 (feeding behavior or feeding behaviour).tw.
95 dietary intake.tw.
96 food.tw.
97 soft drink*.tw.
98 soda.tw.
99 sweetened drink*.tw.
100 fat.tw.
101 confectionary.tw.
102 menu planning.tw.
103 feeding program*.tw.
104 nutrition* program*.tw.
105 cafeteria*.tw.
106 nutritional status.tw.
107 or/83‐106
108 exp TOBACCO SMOKING/
109 Smoking Cessation/
110 smok*.mp.
111 nicotine.mp.
112 tobacco.mp.
113 or/108‐112
114 cessation.tw.
115 prevent*.tw.
116 stop*.tw.
117 quit*.tw.
118 abstin*.tw.
119 abstain*.tw.
120 reduc*.tw.
121 "tobacco use disorder".mp.
122 ex‐smoker*.mp.
123 anti‐smok*.mp.
124 or/114‐123
125 113 and 124
126 exp ALCOHOLS/
127 exp Binge Drinking/ or exp Alcoholism/
128 exp Alcohol Abuse/
129 alcohol*.mp.
130 Drink*.mp.
131 liquor*.mp.
132 beer*.mp.
133 wine*.mp.
134 spirit*.mp.
135 drunk*.mp.
136 intoxicat*.mp.
137 binge.mp.
138 or/126‐137
139 66 or 82 or 107 or 125 or 138
140 5 and 30 and 53 and 139
141 1 or 3 or 4
142 30 and 53 and 139 and 141
Database: CINAHL (EBSCO)
# Query
S1 (MH "Work Environment") OR "Workplace"
S2 (MH "Work")
S3 (MH "Occupational Health")
S4 (MH "Occupational Medicine")
S5 S1 OR S2 OR S3 OR S4
S6 (MH "Health Behavior")
S7 (MH "Health Education")
S8 (MH "Health Promotion")
S9 Healthy People Program*
S10 (MH "Preventive Health Care") OR "Primary Prevention"
S11 (MH "Randomized Controlled Trials")
S12 (MH "Clinical Trials+")
S13 (MH "Random Assignment")
S14 (MH "Evaluation Research")
S15 (MH "Comparative Studies")
S16 TI random* OR AB random*
S17 TI trial OR AB trial
S18 TI groups OR AB groups
S19 TI placebo OR AB placebo
S20 TI experiment* OR AB experiment*
S21 TI (time n1 series) OR AB (time n1 series)
S22 TI ( (pretest or pre test or posttest or post test) ) OR AB ( (pretest or pre test or posttest or post test) )
S23 TI impact OR AB impact
S24 TI change* OR AB change*
S25 TI evaluat* OR AB evaluat*
S26 TI effect* OR AB effect*
S27 TI ( "before and after" ) OR AB ( "before and after" )
S28 TI intervention* OR AB intervention*
S29 TI program* OR AB program*
S30 TI compare* OR AB compare*
S31 TI ( (control or controls* or controla* or controle* or controli or controll*) ) OR AB ( (control or controls* or controla* or controle* or controli or controll*) )
S32 S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31
S33 implement*
S34 dissemin*
S35 adopt*
S36 practice*
S37 "organi?ational change*"
S38 diffus*
S39 (system* n2 change*)
S40 "quality improvement*"
S41 transform*
S42 translat*
S43 transfer*
S44 uptake*
S45 sustainab*
S46 institutionali*
S47 routin*
S48 maintenance
S49 capacity
S50 incorporat*
S51 adher*
S52 integrat*
S53 scal*
S54 ((polic* or practice* or program* or innovation*) n5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*))
S55 S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54
S56 (MH "Obesity+")
S57 (MH "Weight Gain")
S58 (MH "Weight Loss+")
S59 obes*
S60 (weight gain or weight loss)
S61 (overweight or over weight or overeat* or over eat*)
S62 "weight change*"
S63 ((bmi or body mass index) n2 (gain or loss or change))
S64 (primary prevention or secondary prevention)
S65 (preventive measure* or preventative measure*)
S66 (preventive care or preventative care)
S67 S56 OR S57 OR S58 OR S59 OR S60 OR S61 OR S62 OR S63 OR S64 OR S65 OR S66
S68 (MH "Exercise+")
S69 "physical inactivity"
S70 (MH "Physical Activity")
S71 (MH "Motor Activity+")
S72 (MH "Physical Education and Training")
S73 "physical education and training"
S74 (MH "Physical Fitness")
S75 TI sedentary OR AB sedentary
S76 (MH "Life Style+")
S77 (MH "Leisure Activities+")
S78 (MH "Sports+")
S79 (MH "Dancing") OR "Dancing"
S80 TI (exercise* n1 aerobic*) OR AB (exercise* n1 aerobic*)
S81 TI sport* OR AB sport*
S82 TI ( ((life style or life style) n5 activ*) ) OR AB ( ((life style or life style) n5 activ*) )
S83 S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82
S84 (MH "Diet+")
S85 "nutrition*"
S86 "healthy eating"
S87 TI fruit* OR AB fruit*
S88 TI vegetable* OR AB vegetable*
S89 canteen
S90 TI menu OR AB menu
S91 TI ( (calorie or calories) ) OR AB ( (calorie or calories) )
S92 TI "energy intake" OR AB "energy intake"
S93 TI "energy density" OR AB "energy density"
S94 TI eating OR AB eating
S95 TI ( (feeding behavior or feeding behaviour) ) OR AB ( (feeding behavior or feeding behaviour) )
S96 TI "dietary intake" OR AB "dietary intake"
S97 TI food OR AB food
S98 TI "soft drink*" OR AB "soft drink*"
S99 TI soda OR AB soda
S100 TI "sweetened drink*" OR AB "sweetened drink*"
S101 TI fat OR AB fat
S102 TI confectionary OR AB confectionary
S103 TI "menu planning" AND AB "menu planning"
S104 TI "feeding program*" OR AB "feeding program*"
S105 TI "nutrition program*" OR AB "nutrition program*"
S106 TI "nutritional program*" OR AB "nutritional program*"
S107 TI cafeteria* OR AB cafeteria*
S108 TI "nutritional status" OR AB "nutritional status"
S109 S84 OR S85 OR S86 OR S87 OR S88 OR S89 OR S90 OR S91 OR S92 OR S93 OR S94 OR S95 OR S96 OR S97 OR S98 OR S99 OR S100 OR S101 OR S102 OR S103 OR S104 OR S105 OR S106 OR S107 OR S108
S110 (MH "Smoking+")
S111 (MH "Smoking Cessation Programs")
S112 smok*
S113 nicotine
S114 (MH "Tobacco+") OR "tobacco"
S115 S110 OR S111 OR S112 OR S113 OR S114
S116 TI cessation OR AB cessation
S117 TI prevent* OR AB prevent*
S118 TI stop* OR AB stop*
S119 TI quit* OR AB quit*
S120 TI abstin* OR AB abstin*
S121 TI abstain* OR AB abstain*
S122 TI reduc* OR AB reduc*
S123 TI "tobacco use disorder" OR AB "tobacco use disorder"
S124 TI ex‐smoker* OR AB ex‐smoker*
S125 TI anti‐smok* OR AB anti‐smok*
S126 S116 OR S117 OR S118 OR S119 OR S120 OR S121 OR S122 OR S123 OR S124 OR S125
S127 S115 AND S126
S128 (MH "Alcohols+")
S129 (MH "Alcohol Drinking+")
S130 (MH "Alcohol Abuse")
S131 alcohol*
S132 Drink*
S133 liquor*
S134 beer*
S135 wine*
S136 spirit*
S137 drunk*
S138 intoxicat*
S139 binge
S140 S128 OR S129 OR S130 OR S131 OR S132 OR S133 OR S134 OR S135 OR S136 OR S137 OR S138 OR S139
S141 S67 OR S83 OR S109 OR S127 OR S140
S142 S5 AND S32 AND S55 AND S141
Database: the Cochrane Library (Wiley)
ID Search
#1 MeSH descriptor: [Workplace] this term only
#2 MeSH descriptor: [Work] this term only
#3 MeSH descriptor: [Occupational Health] this term only
#4 MeSH descriptor: [Occupational Medicine] this term only
#5 {or #1‐#4}
#6 MeSH descriptor: [Health Behavior] this term only
#7 MeSH descriptor: [Health Education] this term only
#8 MeSH descriptor: [Health Promotion] this term only
#9 MeSH descriptor: [Healthy People Programs] this term only
#10 MeSH descriptor: [Primary Prevention] explode all trees
#11 MeSH descriptor: [Randomized Controlled Trial] this term only
#12 MeSH descriptor: [Controlled Clinical Trial] this term only
#13 MeSH descriptor: [Clinical Trials as Topic] this term only
#14 MeSH descriptor: [Random Allocation] this term only
#15 MeSH descriptor: [Evaluation Studies] this term only
#16 MeSH descriptor: [Comparative Study] this term only
#17 random*:ti,ab
#18 trial:ti,ab
#19 groups:ti,ab
#20 placebo:ti,ab
#21 experiment*:ti,ab
#22 (time near/1 series):ti,ab
#23 (pretest or pre test or posttest or post test):ti,ab
#24 impact:ti,ab
#25 change*:ti,ab
#26 evaluat*:ti,ab
#27 effect*:ti,ab
#28 "before and after":ti,ab
#29 intervention*:ti,ab
#30 program*:ti,ab
#31 compare*:ti,ab
#32 (control or controls* or controla* or controle* or controli or controll*):ti,ab
#33 {or #6‐#32}
#34 implement*
#35 dissemin*
#36 adopt*
#37 practice*
#38 organi?ational change*
#39 diffus*
#40 (system* near/2 change*)
#41 quality improvement*
#42 transform*
#43 translat*
#44 transfer*
#45 uptake*
#46 sustainab*
#47 institutionali*
#48 routin*
#49 maintenance
#50 capacity
#51 incorporat*
#52 adher*
#53 integrat*
#54 scal*
#55 ((polic* or practice* or program* or innovation*) near/5 (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*))
#56 {or #34‐#55}
#57 MeSH descriptor: [Obesity] explode all trees
#58 MeSH descriptor: [Weight Gain] this term only
#59 MeSH descriptor: [Weight Loss] this term only
#60 obes*
#61 (weight gain or weight loss)
#62 (overweight or over weight or overeat* or over eat*)
#63 weight change*
#64 ((bmi or body mass index) near/2 (gain or loss or change))
#65 MeSH descriptor: [Primary Prevention] explode all trees
#66 (primary prevention or secondary prevention)
#67 (preventive measure* or preventative measure*)
#68 (preventive care or preventative care)
#69 (obesity near/2 (prevent* or treat*))
#70 {or #57‐#69}
#71 MeSH descriptor: [Exercise] explode all trees
#72 physical inactivity
#73 physical activity
#74 MeSH descriptor: [Motor Activity] explode all trees
#75 "physical education and training"
#76 MeSH descriptor: [Physical Education and Training] explode all trees
#77 MeSH descriptor: [Physical Fitness] this term only
#78 sedentary:ti,ab
#79 MeSH descriptor: [Life Style] explode all trees
#80 MeSH descriptor: [Leisure Activities] explode all trees
#81 MeSH descriptor: [Sports] explode all trees
#82 MeSH descriptor: [Dancing] this term only
#83 dancing
#84 (exercise* near/1 aerobic*)
#85 sport*:ti,ab
#86 ((life style or life style) near/5 activ*):ti,ab
#87 {or #71‐#86}
#88 MeSH descriptor: [Diet] explode all trees
#89 nutrition*
#90 healthy eating
#91 fruit*:ti,ab
#92 vegetable*:ti,ab
#93 canteen
#94 menu:ti,ab
#95 (calorie or calories):ti,ab
#96 energy intake:ti,ab
#97 energy density:ti,ab
#98 eating:ti,ab
#99 (feeding behavior or feeding behaviour):ti,ab
#100 dietary intake:ti,ab
#101 food:ti,ab
#102 soft drink*:ti,ab
#103 soda:ti,ab
#104 sweetened drink*:ti,ab
#105 fat:ti,ab
#106 confectionary:ti,ab
#107 menu planning:ti,ab
#108 feeding program*:ti,ab
#109 nutrition program*:ti,ab
#110 nutritional program*:ti,ab
#111 cafeteria*:ti,ab
#112 nutritional status:ti,ab
#113 {or #88‐#112}
#114 MeSH descriptor: [Smoking] explode all trees
#115 MeSH descriptor: [Tobacco Use Cessation] explode all trees
#116 smok*
#117 nicotine
#118 tobacco use*
#119 tobacco
#120 MeSH descriptor: [Tobacco] explode all trees
#121 {or #114‐#120}
#122 cessation:ti,ab
#123 prevent*:ti,ab
#124 stop*:ti,ab
#125 quit*:ti,ab
#126 abstin*:ti,ab
#127 abstain*:ti,ab
#128 reduc*:ti,ab
#129 "tobacco use disorder":ti,ab
#130 ex‐smoker*:ti,ab
#131 anti‐smok*:ti,ab
#132 {or #122‐#131}
#133 {and #121, #132}
#134 MeSH descriptor: [Alcohols] explode all trees
#135 MeSH descriptor: [Alcohol Drinking] explode all trees
#136 MeSH descriptor: [Alcoholism] explode all trees
#137 MeSH descriptor: [Ethanol] explode all trees
#138 alcohol*
#139 Drink*
#140 liquor*
#141 beer*
#142 wine*
#143 spirit*
#144 drunk*
#145 intoxicat*
#146 binge
#147 {or #134‐#146}
#148 {or #70, #87, #113, #133, #147}
#149 {and #5, #33, #56, #148}
Database: ERIC (Proquest)
Work or workplace or “occupational medicine” or “occupational health”
And
“health behavior*” or “health behaviour*” or “health education” or “health promotion” or “primary prevention” or random* or “evaluation stud*” or “comparative stud*” or trial or groups or placebo or experiment* or (time and series) or pretest or “pre test” or posttest or “post test” or impact or change* or evaluat* or effect* or “before and after” or intervention* or program* or compare* or control or controls* or controla* or controle* or controli or controll*
and
implement* or disseminat* or adopt* or practice* or organi?ational change* or diffus* or (system* and change*) or quality improvement* or transform* or translat* or transfer* or uptake* or sustainab* or institutionali* or routin* or maintenance or capacity or incorporat* or adher* or integrat* or scal* or ((polic* or practice* or program* or innovation*) and (performance or feedback or prompt* or reminder* or incentive* or penalt* or communicat* or social market* or professional development or network* or leadership or opinion leader* or consensus process* or change manage* or train* or audit*))
and
obes* or weight gain or weight loss or overweight or over weight or overeat* or over eat* or weight change* or ((bmi or body mass index) and (gain or loss or change)) or primary prevention or secondary prevention or preventive measure* or preventative measure* or preventive care or preventative care or (obesity and (prevent* or treat*)) or exercise or physical inactivity or physical activity or Motor Activity or (physical education and training) or Physical Fitness or sedentary or Life Style or Leisure Activiti* or sport* or dancing or diet or nutrition* or healthy eating or fruit* or vegetable* or canteen or food or menu or calorie or calories or energy intake or energy density or eating or feeding behavior or feeding behaviour or dietary intake or soft drink* or soda or sweetened drink* or fat or confectionary or feeding program* or cafeteria* or ((smok* or tobacco or nictotine) and (cessation or stop* or quit* or abstin* or abstain* or reduc* or ex‐smoker* or anti‐smok*)) or alcohol* or drink* or liquor* or beer* or wine* or spirit* or drunk* or intoxicat* or binge
Database: Dissertations and Theses
Title: workplace or work or occupational health or occupational medicine
AND
Title: alcohol or smoking or tobacco or lifestyle or diet or nutrition or healthy eating or physical activity or exercise or obesity or weight
Database: SCOPUS (SCOPUS website)
TITLE‐ABS‐KEY ( workplace OR "occupational medicine" OR "occupational health" )
AND TITLE‐ABS‐KEY ( "health behavior*" OR "health behaviour*" OR "health education" OR "health promotion" OR "primary prevention" OR random* OR "evaluation stud*" OR "comparative stud*" OR trial OR groups OR placebo OR experiment* OR ( time AND series ) OR pretest OR "pre test" OR posttest OR "post test" OR impact OR change* OR evaluat* OR effect* OR "before and after" OR intervention* OR program* OR compare* OR control OR controls* OR controla* OR controle* OR controli OR controll* )
AND TITLE‐ABS‐KEY ( implement* OR disseminat* OR adopt* OR practice* OR organi?ational change* OR diffus* OR ( system* AND change* ) OR quality improvement* OR transform* OR translat* OR transfer* OR uptake* OR sustainab* OR institutionali* OR routin* OR maintenance OR capacity OR incorporat* OR adher* OR integrat* OR scal* OR ( ( polic* OR practice* OR program* OR innovation* ) AND ( performance OR feedback OR prompt* OR reminder* OR incentive* OR penalt* OR communicat* OR social market* OR professional development OR network* OR leadership OR opinion leader* OR consensus process* OR change manage* OR train* OR audit* ) ) )
AND TITLE‐ABS‐KEY (obes* or weight gain or weight loss or overweight or over weight or overeat* or over eat* or weight change* or ((bmi or body mass index) and (gain or loss or change)) or primary prevention or secondary prevention or preventive measure* or preventative measure* or preventive care or preventative care or (obesity and (prevent* or treat*)) or exercise or physical inactivity or physical activity or Motor Activity or (physical education and training) or Physical Fitness or sedentary or Life Style or Leisure Activiti* or sport* or dancing or diet or nutrition* or healthy eating or fruit* or vegetable* or canteen or food or menu or calorie or calories or energy intake or energy density or eating or feeding behavior or feeding behaviour or dietary intake or soft drink* or soda or sweetened drink* or fat or confectionary or feeding program* or cafeteria* or ((smok* or tobacco or nictotine) and (cessation or stop* or quit* or abstin* or abstain* or reduc* or ex‐smoker* or anti‐smok*)) or alcohol* or drink* or liquor* or beer* or wine* or spirit* or drunk* or intoxicat* or binge)
AND ( LIMIT‐TO ( SUBJAREA , "MEDI" ) OR LIMIT‐TO ( SUBJAREA , "SOCI" ) OR LIMIT‐TO ( SUBJAREA , "NURS" ) OR LIMIT‐TO ( SUBJAREA , "HEAL" ) ) AND ( LIMIT‐TO ( EXACTKEYWORD , "Human" ) OR LIMIT‐TO ( EXACTKEYWORD , "Humans" ) ) AND ( EXCLUDE ( SUBJAREA , "BUSI" ) OR EXCLUDE ( SUBJAREA , "CENG" ) OR EXCLUDE ( SUBJAREA , "CHEM" ) OR EXCLUDE ( SUBJAREA , "COMP" ) OR EXCLUDE ( SUBJAREA , "DECI" ) OR EXCLUDE ( SUBJAREA , "ARTS" ) OR EXCLUDE ( SUBJAREA , "ECON" ) OR EXCLUDE ( SUBJAREA , "PHYS" ) OR EXCLUDE ( SUBJAREA , "MATH" ) OR EXCLUDE ( SUBJAREA , "ENER" ) OR EXCLUDE ( SUBJAREA , "VETE" ) )
Database: the Campbell Library (the Campbell Library Website)
Work OR workplace or occupational health OR occupational medicine (separate searches)
Appendix 2. 'Risk of bias' assessment tool
| RANDOM SEQUENCE GENERATION Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence | |
| Criteria for the judgement of a 'High risk' of bias | The investigators describe a non‐random component in the sequence generation process. Usually, the description would involve some systematic, non‐random approach, for example:
Other non‐random approaches happen much less frequently than the systematic approaches mentioned above and tend to be obvious. They usually involve judgement or some method of non‐ random categorisation of participants, for example:
|
| Criteria for the judgement of a low risk of bias | The investigators describe a random component in the sequence generation process such as:
*Minimisation may be implemented without a random element, and this is considered to be equivalent to being random |
| Criteria for the judgement of an unclear risk of bias | Insufficient information about the sequence generation process to permit judgement of low or high risk |
| ALLOCATION CONCEALMENT Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to consignment | |
| Criteria for the judgement of a high risk of bias | Participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on:
|
| Criteria for the judgement of a low risk of bias | Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation:
|
| Criteria for the judgement of an unclear risk of bias | Insufficient information to permit judgement of low or high risk. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgement ‐ for example if the use of assignment envelopes is described, but it remains unclear whether envelopes were sequentially numbered, opaque and sealed |
| BLINDING OF PARTICIPANTS AND PERSONNEL Performance bias due to knowledge of the allocated interventions by participants and personnel during the study | |
| Criteria for the judgement of a high risk of bias | Any one of the following:
|
| Criteria for the judgement of a low risk of bias | Any one of the following:
|
| Criteria for the judgement of a low risk of bias | Any one of the following:
|
| BLINDING OF OUTCOME ASSESSMENT Detection bias due to knowledge of the allocated interventions by outcome assessors | |
| Criteria for the judgement of a high risk of bias | Any one of the following:
|
| Criteria for the judgement of a low risk of bias | Any one of the following:
|
| Criteria for the judgement of an unclear risk of bias | Any one of the following:
|
| INCOMPLETE OUTCOME DATA Attrition bias due to amount, nature or handling of incomplete outcome data | |
| Criteria for the judgement of a high risk of bias | Any one of the following:
|
| Criteria for the judgement of a low risk of bias | Any one of the following:
|
| Criteria for the judgement of an unclear risk of bias | Any one of the following:
|
| SELECTIVE REPORTING Reporting bias due to selective outcome reporting | |
| Criteria for the judgement of a high risk of bias | Any one of the following:
|
| Criteria for the judgement of a low risk of bias | Any of the following:
|
| Criteria for the judgement of an unclear risk of bias | Insufficient information to permit judgement of low or high risk. It is likely that most studies will fall into this category. |
| OTHER BIAS Bias due to problems not covered elsewhere in the table | |
| Criteria for the judgement of a high risk of bias | There is at least one important risk of bias. For example, the study:
|
| Criteria for the judgement of a low risk of bias | The study appears to be free of other sources of bias |
| Criteria for the judgement of an unclear risk of bias | There may be a risk of bias, but there is either:
|
Appendix 3. Risk of bias assessment ‐ review secondary outcomes
Bandoni 2010
| Risk of bias | ||
| Bias | Author's judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear | No information on method of generating random sequence |
| Allocation concealment (selection bias) | Unclear | No information on whether allocation was concealed prior to assignment |
| Blinding of participants and personnel (performance bias) Employee health behaviours (diet) | High | Component of intervention was distribution of educational materials to workers and product labelling (Bandoni 2010, p 976) |
| Blinding of outcome assessment (detection bias) Employee health behaviours (diet) | High | Worker self‐report of amount of fruit and vegetables consumed in interview with researchers during visit – neither blind (Bandoni 2010, p 977). |
| Incomplete outcome data (attrition bias) Employee health behaviours (diet) | Unclear | At baseline, 1296 individuals (intervention: 651; control: 645) were studied. Postintervention 1214 individuals (intervention: 630; control: 584). Independent samples (Bandoni 2010, p 977). Greater proportion drop in participation in control group compared to intervention group. Unclear if this biased results |
| Selective reporting (reporting bias) | Unclear | No mention of a priori registration of measures or publication of protocol |
| Recruitment to cluster | Low | All workers in participating workplaces invited to participate (Bandoni 2010, p 976) |
| Baseline imbalances | Low | After adjustment for socio‐demographic characteristics (sex, education and age), the effect of the intervention on the consumption of fruits and vegetables by workers remained significant (Bandoni 2010, p 979) |
| Loss of clusters | Unclear | One company dropped out – final sample intervention: 15; control: 14. Analysis did not include imputation of missing data so unclear whether this biased results (Bandoni 2010, p 976) |
| Incorrect analysis | Unclear | No mention of adjustment for clustering within workplace clusters. Unclear what impact this may have on study findings |
| Compatibility with individually randomised controlled trials (herd effect) | Not applicable given secondary measure | — |
| Other bias | Low | — |
Biener 1999
| Risk of bias | ||
| Bias | Author's judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear | No information on method of generating random sequence |
| Allocation concealment (selection bias) | Unclear | No information on whether allocation was concealed prior to assignment |
| Blinding of participants and personnel (performance bias) Employee health behaviours (diet and tobacco use) | High | Intervention implementation actively involved workplace staff participation at all organisational levels |
| Blinding of outcome assessment (detection bias) Employee health behaviours (diet and tobacco use) | High | Tobacco use self‐reported by employees using survey; diet self‐reported using food frequency questionnaire (Abrams 1994) Methods of distribution of employee survey varied by study center, which could contribute to elevated risk of bias if differences between intervention and control groups. Florida and Brown mailed surveys to each employee in the work site, Dana‐Farber mailed surveys to a random sample of employees in each work site, and MD Anderson administered questionnaires to employees at mandatory work site meetings (Sorensen 1996, p 940) |
| Incomplete outcome data (attrition bias) Employee health behaviours (diet and tobacco use) | Low | At baseline, the overall response rate to the employee survey was 69% (average work‐site response rate, 72%; study center mean range, 61% to 89%). The overall response rate at the follow‐up survey was 71% (average work‐site response rate, 75%; study center mean range 68% to 86%). The interaction of the response rate subgroup (cutpoint, 65%) and the intervention group indicated no relationship between the intervention effects and the work site's response rate to the individual survey (smallest P = 0.24) (Sorensen 1996, p 943). |
| Selective reporting (reporting bias) | Low | All pre‐specified outcomes (Abrams 1994, Fig 1) reported in Sorensen 1996 and Biener 1999 |
| Recruitment to cluster | Unclear | The methods of recruitment varied by study center, which could contribute to elevated risk of bias if differences between intervention and control groups. Florida and Brown mailed surveys to each employee in the work site, Dana‐Farber mailed surveys to a random sample of employees in each work site, and MD Anderson administered questionnaires to employees at mandatory work site meetings (Sorensen 1996 p 940) |
| Baseline imbalances | Low | Clusters matched and no significant baseline imbalances in outcomes measure for individual level data (Sorensen 1996) and demographic characteristics (Biener 1999) |
| Loss of clusters | Unclear | 114 worksites initially recruited, 3 (2 intervention, 1 control) dropped out due to economic dislocations, leaving 111 in final sample. For pairwise analyses, three pairs were excluded, leaving a total of 108 work sites (Sorensen 1996) |
| Incorrect analysis | Low | Analysis adjusted for clustering effect (intraclass correlation) (Abrams 1994) |
| Compatibility with individually randomised controlled trials (herd effect) | Not applicable given secondary measure | — |
| Other bias | Low | — |
Parker 2010
| Risk of bias | ||
| Bias | Author's judgement | Support for judgement |
| Random sequence generation (selection bias) | High | Non‐randomised trial |
| Allocation concealment (selection bias) | High | Non‐randomised trial |
| Blinding of participants and personnel (performance bias) Employee health behaviours (diet, physical activity and weight status) | High: (diet and physical activity) Low: (weight status) | Self‐reported health behaviours Objective biometric measures |
| Blinding of outcome assessment (detection bias) Employee health behaviours (diet, physical activity and weight status) | High (diet and physical activity) Low (weight status) | Self‐reported health behaviours Objective biometric measures |
| Incomplete outcome data (attrition bias) Employee health behaviours (diet, physical activity and weight status) | Low | Attrition was 54.3% and 45.1% for the intervention and control group respectively. To address the issue of missing data, several statistical approaches were used to adjust for the potential bias due to attrition (Goetzel 2010, p 300). |
| Selective reporting (reporting bias) | Unclear | Wilson 2007 indicates primary outcome BMI and development work of environmental assessment tool demonstrates intention to include in outcome assessment. No indications that any predetermined outcomes were otherwise omitted |
| Recruitment to cluster | Low | No difference in recruitment methods across treatment groups, with all employees at all study sites encouraged to participate in the health risk assessment (HRA) and biometric screening programmes (Goetzel 2010, p 292) |
| Baseline imbalances | Low | When comparing overweight and obesity prevalence between subjects at intervention and control sites, there were no significant differences between groups at baseline. Adjustment undertaken to correct for baseline imbalances in demographic characteristics using propensity score weights (Goetzel 2010, pp 292‐3). |
| Loss of clusters | Low | No loss of clusters (Parker 2010) |
| Incorrect analysis | Low | Worksite's influence on outcomes was evaluated by including a site‐level variable in the predictive models (adjustment for clustering) (Goetzel 2010, p 294) |
| Compatibility with individually randomised controlled trials (herd effect) | Not applicable given secondary measure. | — |
| Risk of bias due to confounding factors (adequate adjustment) | Low | Adjusted for baseline imbalances in demographic characteristics using propensity score weights (Goetzel 2010, pp 292‐3) |
Hannon 2012
| Risk of bias | ||
| Random sequence generation (selection bias) | Low | Block randomisation undertaken by statistician (assume computerised) (Hannon 2012, p 127) |
| Allocation concealment (selection bias) | Low | Block randomisation undertaken by statistician (assume computerised) (Hannon 2012, p 127) |
| Blinding of participants and personnel (performance bias) cost estimates | High | Intervention implementation actively involved workplace staff participation. |
| Blinding of outcome assessment (detection bias) cost estimates | High | Outcomes self‐reported by workplace staff (Hannon 2012, p 127) |
| Incomplete outcome data (attrition bias) cost estimates | Unclear | Response rate to cost outcome questions 77% at baseline and 71% at follow‐up. Unclear whether similar across groups (Hannon 2012, p 129) |
| Selective reporting (reporting bias) | Unclear | No mention of a priori registration of measures or publication of protocol |
| Other bias | Low | — |
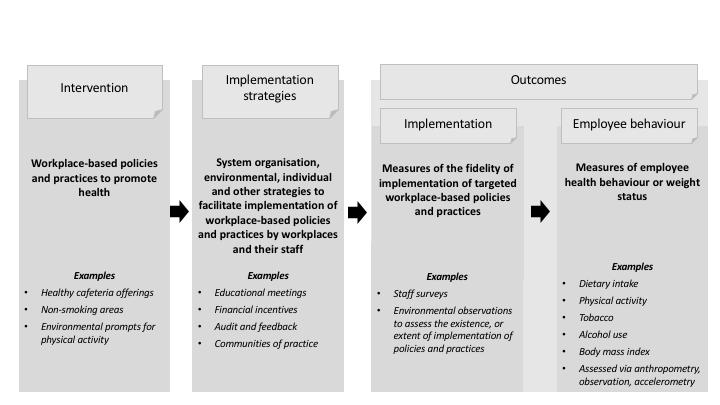
Review logic model

Study selection flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Implementation strategy versus control, outcome: 1.1 Implementation score.

Comparison 1 Implementation strategy versus control, Outcome 1 Implementation score.
| Strategies to improve the implementation of workplace‐based health promotion versus no implementation strategy: findings from randomised controlled trials | ||||||
| Patient or population: workplace employees Settings: any work setting, of any employment sector and geographical location, staffed by employees Intervention: any strategy (e.g. educational materials; educational meetings; audit and feedback; local opinion leaders; tailored intervention) with the intention of improving the implementation of health‐promoting policies or practices targeting diet, physical activity, obesity, tobacco use and alcohol use in the workplace setting Comparison: no intervention e.g. wait‐list, usual practice or minimal support control (4 trials) Summary of findings for the main comparison were based on included randomised trials only. | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Risk with no intervention | Risk with implementation interventions | |||||
| Implementation of workplace‐based policies or practices targeting diet, physical activity, obesity, tobacco use or alcohol use | The mean implementation score was 42.1a | The implementation score in the intervention group was 0.1 lower (3.8 lower to 3.5 higher) | Scores estimated using a standardised mean difference of −0.01 (−0.32 to 0.30) and a standard deviation of 11.8a | 191 workplaces | ⊕⊕⊝⊝ | One RCT that compared a workplace cafeteria nutrition intervention to a wait‐list control could not be synthesised in the meta‐analysis (Bandoni 2010). The trial reported a significant improvement on the single primary measure of implementation included in the review. One RCT reported additional dichotomous implementation outcomes that could not be synthesised in the meta‐analysis (Biener 1999). The trial reported a significant improvement on 1 out of 3 implementation outcomes included in the review. |
| Employee dietary intake | — | — | — | 19,419 participants (2 RCTs) | ⊕⊝⊝⊝ | Mixed results were reported for this outcome. One RCT found a workplace cafeteria nutrition intervention effective in increasing fruit and vegetable consumption (Bandoni 2010). The other RCT found a worksite cancer control intervention effective in decreasing dietary intake of fat and increasing fruit and vegetable intake; however, it was not effective in increasing fibre consumption (Biener 1999). |
| Employee tobacco use | — | — | — | 18,205 participants (1 RCT) | ⊕⊕⊝⊝ | One RCT which compared a worksite cancer control intervention to a minimal support control group reported no effect on smoking prevalence or the proportion of smokers who quit (Biener 1999). |
| Employee physical activity, weight status, and alcohol use | No RCTs reported these outcomes. | |||||
| Cost or cost‐effectiveness | — | — | — | 46 workplaces (1 RCT) | ⊕⊕⊝⊝ | One RCT reported an increase in employer costs in the implementation intervention group compared to the control group (Hannon 2012). |
| Unintended adverse effects | No RCTs reported this outcome. | |||||
| GRADE Working Group grades of evidence | ||||||
| aWe used the postintervention mean and standard deviation of the control group from Hannon 2012 for the risk with no intervention to re‐express the SMD in terms of a mean implementation score. | ||||||
| Trial (study design) | Workplace setting | Intervention and comparison (sample sizes) | Implementation outcomes and effects | Secondary outcomes and effects |
| (RCT) | Workplaces predominantly from industrial sector Region: Brazil | Educational meetings and educational materials (15 workplaces; 630 employees) vs Wait‐list control (14 workplaces; 584 employees) | Quantity fruits and vegetables in lunch meals (g/meal), measured via food service manager self‐reported survey (validity NR). Greater increase in intervention (adjusted MD 49.05 g, 95% CI 8.38 to 89.71) | Employee fruit and vegetable consumption (g/day), measured via self‐reported survey (validity NR). Slightly greater increase in intervention (adjusted effect estimate 11.75 g, 95% CI 2.73 to 20.77) |
| (RCT) | Small‐ to medium‐sized workplaces in manufacturing, transportation and utilities, and personal and household services industries Region: USA | Tailored intervention; local opinion leaders; local consensus process and educational materials (17 workplaces; n employees NR) vs Wait‐list control (17 workplaces; n employees NR) | Implementation of 11 practices supportive of healthy eating, physical activity and weight control, measured via scores derived from environmental assessment checklist (validity NR). NS difference 9/11 practices. Higher scores in intervention for notices encouraging physical activity (adjusted effect estimate 0.33, 95% CI 0.00 to 0.85) and healthy eating (0.40, 95% CI 0.00 to 1.46) | NR |
| (RCT) | Workplaces from manufacturing, communications, public service and utilities sectors Region: USA | Local opinion leaders; local consensus process; educational meetings; and educational outreach visits (55 workplaces; 8914 employees) vs Minimal support control comprising printed health promotion materials (56 workplaces; 9291 employees) | Workplace tobacco control policy restrictiveness and compliance, measured via scores derived from employee self‐reported survey (validity NR). NS difference restrictiveness: adjusted difference 0.01 (SE 0.09) or compliance: 0.03 (SE 0.07) % workplaces reporting improvement in cafeteria and vending machine nutrition labelling and healthy catering policy, measured via organisational informant interview (validity NR). NS difference cafeteria labelling (MD 13.4%, P = 0.72) or catering policy (MD 10.9%, P = 0.30). Greater improvement in intervention vending machine labelling (MD 39.6%, P < 0.01) | Employee smoking prevalence and % of quitters, measured via self‐reported survey (validity NR). NS difference in prevalence (difference −0.66%, 95% CI −3.0 to 1.2) or quit rate (1.53%, 95% CI −1.0 to 3.7) % dietary energy from fat, % increase in fibre (g/1000 kcal, and % increase in fruit and vegetables (servings/day), measured via Block FFQ (validated). Greater increase in intervention fruit and vegetables (adjusted increase 5.6%, SE 1.3, P < 0.001) and % dietary fat lower (adjusted difference −0.35%, SE 0.16, P < 0.05). NS difference fibre (adjusted increase 1.7%, SE 0.87, P > 0.05) |
| (RCT) | Low‐wage, mid‐sized workplaces predominantly from education, health, manufacturing and retail sectors Region: USA | Audit and feedback; clinical practice guidelines; local consensus process; educational materials; educational outreach; and tailored intervention (23 workplaces; n employees NR) vs Wait‐list control (23 workplaces; n employees NR) | Implementation of 16 best practices for health promotion recommended by CPSTF Community Guide; measured via score derived from workplace self‐reported survey (validity NR). NS difference in total score mean (SD): intervention baseline 31.5 (8.3), follow‐up 39.2 (11.2) vs control baseline 36.8 (11.7), follow‐up 42.1 (11.8), P = 0.33 | Workplace costs (per worker) for health promotion, measured via workplace self‐reported survey (validity NR). Costs increased slightly more in intervention, mean total costs (range): intervention baseline USD 8.30 (0.00 to 35.00), follow‐up USD 10.10 (0.00 to 53.00) vs control baseline USD 11.00 (0.00 to 53.00), follow‐up USD 11.80 (1.00 to 43.00) |
| (non‐randomised, controlled trial) | Manufacturing, research and development and administrative facilities from a large science and technology company Region: USA | Moderate‐intensity intervention: tailored intervention; local opinion leaders; educational meetings (4 workplaces; 382 employees) or High‐intensity intervention: moderate strategies + local consensus process; audit and feedback; monitoring of performance; and other (5 workplaces; 1520 employees) vs Wait‐list control (3 workplaces; 529 employees) | Implementation of policies and practices promoting healthy eating, physical activity and weight control, measured via scores derived from EAT (validated tool). Relative to control, greater increase in total EAT score for moderate intensity intervention (contrast estimate 9.68, SE 3.48, P = 0.009) and high intensity intervention (16.99, SE 3.37, P < 0.001) | % employees classified high risk poor nutrition and poor physical activity, measured via self‐reported HRA survey. Relative to control, NS difference for poor nutrition: moderate (estimate −7.7%, P = 0.068), high (−4.6%, P = 0.16), or poor physical activity: moderate (−1.6%, P = 0.77) or high (−0.7%, P = 0.89) Weight (kg), BMI (kg/m2) and % employees overweight or obese. Relative to control, greater reduction in weight for moderate (estimate −2.1, P = 0.033), high (−1.5, P = 0.015) and in BMI moderate (−0.3, P = 0.034), high (−0.2, P = 0.008). NS difference % obese: moderate (0.1%, P = 0.88), high (0.3%, P =0.95), or % overweight: moderate (4.4%, P = 0.47); high (5.5%, P = 0.22) |
| BMI: body mass index; CI: confidence interval; CPSTF: Community Preventive Services Task Force, US Department of Health and Human Services; EAT: environmental assessment tool;FFQ: food frequency questionnaire; HRA: health risk assessment; MD: mean difference; NR: not reported; NS: not significant; RCT: randomised controlled trial; SD: standard deviation; SE: standard error. | ||||
| Trial (study design) | Workplace setting | Intervention and comparison (sample sizes) | Implementation outcomes and effects | Secondary outcomes and effects |
| (non‐randomised trial) | NHS trusts including ambulance, mental health and acute care Region: UK | Cohort C1: clinical practice guidelines and audit and feedback (26 workplaces; n employees NR) vs Cohort B: clinical practice guidelines; audit and feedback; educational meetings; and tailored intervention (36 workplaces; n employees NR) | Implementation of 6 sets NICE guidance for workplace health promotion addressing: obesity, physical activity, smoking, long‐term sickness absence and mental health, measured via score on organisational audit self‐reported by staff (validity NR). Greater increase in score for cohort B (adjusted median total score difference: 22.17 vs 4.94, P < 0.001) | NR |
| (non‐randomised controlled trial) | Manufacturing, research and development and administrative facilities from a large science and technology company Region: USA | Moderate‐intensity intervention: tailored intervention; local opinion leaders; educational meetings (4 workplaces; 382 employees) or High‐intensity intervention: moderate strategies + local consensus process; audit and feedback; monitoring of performance; and other (5 workplaces; 1520 employees) | Implementation of workplace policies and practices promoting healthy eating, physical activity and weight control, measured via scores derived from EAT (validated tool). Greater increase in total EAT score for high‐intensity intervention (contrast estimate 7.31, SE 3.10, P = 0.024) | NR |
| EAT: environmental assessment tool; NHS: National Health Service; NICE: National Institute of Clinical Excellence; NR: not reported; SE: standard error. | ||||
| EPOC subcategory | Definition |
| Audit and feedback | A summary of health workers' performance over a specified period of time, given to them in a written, electronic or verbal format. The summary may include recommendations for clinical action. |
| Clinical practice guidelines | Clinical guidelines are systematically developed statements to assist healthcare providers and patients to decide on appropriate health care for specific clinical circumstances (US Institute of Medicine). |
| Educational materials | Distribution to individuals, or groups, of educational materials to support clinical care, i.e. any intervention in which knowledge is distributed. For example this may be facilitated by the Internet, learning critical appraisal skills; skills for electronic retrieval of information, diagnostic formulation; question formulation |
| Educational meetings | Courses, workshops, conferences or other educational meetings |
| Educational outreach visits | Personal visits by a trained person to health workers in their own settings, to provide information with the aim of changing practice |
| Local consensus process | Formal or informal local consensus processes, for example agreeing a clinical protocol to manage a patient group, adapting a guideline for a local health system or promoting the implementation of guidelines |
| Local opinion leaders | The identification and use of identifiable local opinion leaders to promote good clinical practice |
| Monitoring the performance of the delivery of healthcare | Monitoring of health services by individuals or healthcare organisations, for example by comparing with an external standard |
| Tailored interventions | Interventions to change practice that are selected based on an assessment of barriers to change, for example through interviews or surveys. |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Implementation score Show forest plot | 3 | 164 | Std. Mean Difference (Random, 95% CI) | ‐0.01 [‐0.32, 0.30] |

