Interwencje neonatologiczne w celu zapobiegania wystąpienia mózgowego porażenia dziecięcego: przegląd przeglądów systematycznych Cochrane
Appendices
Appendix 1. Ongoing reviews
| Protocol citation | Overview outcomes pre‐specified in protocol |
| Abiramalatha T, Thomas N, Gupta V, Viswanathan A, McGuire W. High versus standard volumes of enteral feeds for preterm or low birth weight infants (Protocol). Cochrane Database of Systematic Reviews 2016, Issue 10. | Secondary outcomes pre‐specified include:
|
| Amari S, Shahrook S, Ota E, Mori R. Branched‐chain amino acid supplementation for improving nutrition in term and preterm neonates (Protocol). Cochrane Database of Systematic Reviews 2016, Issue 7. | Primary outcomes pre‐specified include:
|
| Askie LM, Darlow BA, Davis PG, Finer N, Stenson B, Vento M, Whyte R. Effects of targeting higher versus lower arterial oxygen saturations on death or disability in preterm infants (Protocol). Cochrane Database of Systematic Reviews 2014, Issue 7. | Primary outcomes pre‐specified include:
Secondary outcomes pre‐specified include:
|
| Choo YM, Ahmad Kamar A, Tengku Kamalden TAF, Looi ML, Tan K, Lai NM. Lutein and zeaxanthin for reducing morbidity and mortality in preterm infants (Protocol). Cochrane Database of Systematic Reviews 2016, Issue 5. | Secondary outcomes pre‐specified include:
|
| Dawson JA, Davis PG, Foster JP. Routine oro/nasopharyngeal suction versus no suction in the delivery room (Protocol). Cochrane Database of Systematic Reviews 2013, Issue 1. | Secondary outcomes pre‐specified include:
|
| Foster JP, Buckmaster A, Sinclair L, Lees S, Guaran R. Nasal continuous positive airway pressure (nCPAP) for term neonates with respiratory distress (Protocol). Cochrane Database of Systematic Reviews 2015, Issue 11. | Secondary outcomes pre‐specified include:
|
| Foster JP, Taylor C, Bredemeyer SL. Topical anaesthesia for needle‐related pain in newborn infants (Protocol). Cochrane Database of Systematic Reviews 2013, Issue 1. | Secondary outcomes pre‐specified include:
|
| Good M, Jones LJ, Osborn DA, Abdel‐Latif ME. Transfusion of fresh versus non‐fresh (older) red blood cell in neonates (Protocol). Cochrane Database of Systematic Reviews 2015, Issue 11. | Secondary outcomes pre‐specified include:
|
| Gordon A, Greenhalgh M, McGuire W. Early planned removal versus expectant management of peripherally inserted central catheters to prevent infection in newborn infants (Protocol). Cochrane Database of Systematic Reviews 2016, Issue 4. | Secondary outcomes pre‐specified include:
|
| Gordon A, Greenhalgh M, McGuire W. Early planned removal of umbilical venous catheters to prevent infection in newborn infants (Protocol). Cochrane Database of Systematic Reviews 2016, Issue 4. | Secondary outcomes pre‐specified include:
|
| Green DS, Abdel‐Latif ME, Jones LJ, Osborn DA. Pharmacological interventions for prevention and treatment of upper gastrointestinal bleeding in newborn infants (Protocol). Cochrane Database of Systematic Reviews 2015, Issue 7. | Secondary outcomes pre‐specified include:
|
| Han S, Yu Z, Guo X, Dong X, Chen X, Soll R. Intratracheal instillation of corticosteroids using surfactant as a vehicle for the prevention of chronic lung disease in preterm infants with respiratory distress syndrome (Protocol). Cochrane Database of Systematic Reviews 2011, Issue 4 | Secondary outcomes pre‐specified include:
|
| Hegarty JE, Harding JE, Crowther CA, Brown J, Alsweiler J. Oral dextrose gel for the prevention of hypoglycaemia in newborn infants (Protocol). Cochrane Database of Systematic Reviews 2016, Issue 4. | Primary outcomes pre‐specified include:
Secondary outcomes pre‐specified include:
|
| Hyttel‐Sorensen S, Støy Saem L, Greisen G, Als‐Nielsen B, Gluud C. Cerebral near‐infrared spectroscopy monitoring for prevention of brain injury in very preterm infants (Protocol). Cochrane Database of Systematic Reviews 2015, Issue 2. | Primary outcomes pre‐specified include:
|
| Jauncey‐Cooke J, Bogossian F, Hough JL, Schibler A, Davies MW, Grant CA, Gibbons K, East CE. Lung recruitment manoeuvres for reducing respiratory morbidity in mechanically ventilated neonates (Protocol). Cochrane Database of Systematic Reviews 2012, Issue 7. | Secondary outcomes pre‐specified include:
|
| Kaempfen S, Neumann RP, Jost K, Schulzke SM. Beta‐blockers for prevention and treatment of retinopathy of prematurity in preterm infants (Protocol). Cochrane Database of Systematic Reviews 2015, Issue 9. | Secondary outcomes pre‐specified include:
|
| Kent A, Kecskes Z. Magnesium sulfate for term infants following perinatal asphyxia (Protocol). Cochrane Database of Systematic Reviews 2003, Issue 2. | Primary outcomes pre‐specified include:
|
| Kulasekaran K, Sargent PH, Flenady V. Milrinone for the treatment of cardiac dysfunction in neonates (Protocol). Cochrane Database of Systematic Reviews 2004, Issue 4. | Secondary outcomes pre‐specified include:
|
| Lai NM, Ahmad Kamar A, Choo YM, Kong JY, Ngim CF. Fluid supplementation for neonatal unconjugated hyperbilirubinaemia (Protocol). Cochrane Database of Systematic Reviews 2015, Issue 9. | Primary outcomes pre‐specified include:
Secondary outcomes pre‐specified include:
|
| Lui K, Foster JP, Davis PG, Ching SK, Oei JL, Osborn DA. Higher versus lower oxygen concentrations titrated to target oxygen saturations during resuscitation of preterm infants at birth (Protocol). Cochrane Database of Systematic Reviews 2012, Issue 11. | Primary outcomes pre‐specified include:
|
| Malhotra A, Veldman A. Recombinant activated Factor VII for prevention and treatment of intraventricular haemorrhage in neonates (Protocol). Cochrane Database of Systematic Reviews 2011, Issue 3. | Primary outcomes pre‐specified include:
|
| McCarthy LK, Davis PG, O'Donnell CPF. Nasal airways (single or double prong, long or short) for neonatal resuscitation (Protocol). Cochrane Database of Systematic Reviews 2011, Issue 5. | Secondary outcomes pre‐specified include:
|
| Molloy EJ, McCallion N, O'Donnell CPF, Davis PG. Heliox for prevention of morbidity and mortality in ventilated newborn infants (Protocol). Cochrane Database of Systematic Reviews 2008, Issue 3. | Secondary outcomes pre‐specified include:
|
| Neary E, Ni Ainle F, El‐Khuffash A, Cotter M, Kirkham C, McCallion N. Plasma transfusion to prevent intraventricular haemorrhage in very preterm infants (Protocol). Cochrane Database of Systematic Reviews 2016, Issue 9. | Primary outcomes pre‐specified include:
|
| O'Donnell CPF, Davis PG, Morley CJ. Endotracheal intubation versus face mask for newborns resuscitated with positive pressure ventilation at birth (Protocol). Cochrane Database of Systematic Reviews 2004, Issue 4. | Secondary outcomes pre‐specified include:
|
| O'Donnell CPF, Davis PG, Morley CJ. Manual ventilation devices for neonatal resuscitation (Protocol). Cochrane Database of Systematic Reviews 2004, Issue 3. | Secondary outcomes pre‐specified include:
|
| Onland W, De Jaegere APMC, Offringa M, van Kaam A. Systemic corticosteroid regimens for prevention of bronchopulmonary dysplasia in preterm infants (Protocol). Cochrane Database of Systematic Reviews 2014, Issue 1. | Secondary outcomes pre‐specified include:
|
| Onyango AB, Suresh G, Were F. Intermittent phototherapy versus continuous phototherapy for neonatal jaundice (Protocol). Cochrane Database of Systematic Reviews 2009, Issue 4. | Primary outcomes pre‐specified include:
|
| Pierro M, Thébaud B, Soll R. Mesenchymal stem cells for the prevention and treatment of bronchopulmonary dysplasia in preterm infants (Protocol). Cochrane Database of Systematic Reviews 2015, Issue 11. | Secondary outcomes pre‐specified include:
|
| Rivas‐Fernandez M, Roqué i Figuls M, Tobias A, Balaguer A. Different strains of probiotics for preventing morbidity and mortality in preterm infants: a network meta‐analysis (Protocol). Cochrane Database of Systematic Reviews 2016, Issue 8. | Secondary outcomes pre‐specified include:
|
| Romantsik O, Calevo MG, Bruschettini M. Head midline position for preventing the occurrence or extension of germinal matrix‐intraventricular hemorrhage in preterm infants (Protocol). Cochrane Database of Systematic Reviews 2016, Issue 9. | Secondary outcomes pre‐specified include:
|
| Seliem W, Bhutta ZA, Soll R, McGuire W. Topical emollient therapy for preventing infection in preterm infants in low‐ or middle‐income countries (Protocol). Cochrane Database of Systematic Reviews 2007, Issue 3. | Secondary outcomes pre‐specified include:
|
| Shah D, Tracy M. Cutaneous antisepsis for prevention of intravascular catheter–associated infection in newborn infants (Protocol). Cochrane Database of Systematic Reviews 2014, Issue 3. | Secondary outcomes pre‐specified include:
|
| Sinn JKH, Kumar K, Osborn DA, Bolisetty S. Higher versus lower amino acid intake in parenteral nutrition for newborn infants (Protocol). Cochrane Database of Systematic Reviews 2006, Issue 2. | Primary outcomes pre‐specified include:
Secondary outcomes pre‐specified include:
|
| Van Rostenberghe H, Ho JJ, Quah BS, Noraida R. The effects of thyroxine on end organ damage in asphyxiated neonates (Protocol). Cochrane Database of Systematic Reviews 2009, Issue 4. | Primary outcomes pre‐specified include:
|
| Xiong T, Chen H, Mu D. Effect of pre‐exchange albumin infusion on neonatal hyperbilirubinaemia and long‐term developmental outcomes (Protocol). Cochrane Database of Systematic Reviews 2014, Issue 2. | Primary outcomes pre‐specified include:
|
| Xiong T, Li H, Zhao J, Dong W, Qu Y, Wu T, Mu D. Hyperbaric oxygen for term newborns with hypoxic ischemic encephalopathy (Protocol). Cochrane Database of Systematic Reviews 2011, Issue 8. | Primary outcomes pre‐specified include:
|
| Yu B, Li S, Zhou D, Davis PG. Subcutaneous reservoir drainage versus ventriculoperitoneal shunt for the treatment of posthemorrhagic hydrocephalus in preterm infants (Protocol). Cochrane Database of Systematic Reviews 2009, Issue 3. | Primary outcomes pre‐specified include:
|
| Yu Z, Guo X, Han S, Lu J, Sun Q. Erythropoietin for term and late preterm infants with hypoxic ischemic encephalopathy (Protocol). Cochrane Database of Systematic Reviews 2010, Issue 1. | Primary outcomes pre‐specified include:
Secondary outcomes pre‐specified include:
|
| Yu Z, Sun Q, Han S, Lu J, Ohlsson A, Guo X. Erythropoietin for preterm infants with hypoxic ischaemic encephalopathy (Protocol). Cochrane Database of Systematic Reviews 2012, Issue 12. | Primary outcomes pre‐specified include:
Secondary outcomes pre‐specified include:
|
Abbreviations: ABR: auditory brainstem response; BSID: Bayley Scales of Infant Development; DQ: developmental quotient; GMDS: Griffith Mental Development Scales; GMFCS: Gross Motor Function Classification System; IQ; intelligence quotient; MACS: Manual Ability Classification System; MDI: Mental Development Index; PDI: Psychomotor Development Index; SD: standard deviation; VA: visual acuity
Appendix 2. Reviews awaiting further classification
| Review citation | Overview outcomes pre‐specified in review with no outcome data | Main conclusion(s) of review |
| Abdel‐Latif ME, Osborn DA. Intratracheal Clara cell secretory protein (CCSP) administration in preterm infants with or at risk of respiratory distress syndrome. Cochrane Database of Systematic Reviews 2011, Issue 5. | Primary outcomes pre‐specified include:
| "There are insufficient data to determine the role of rhCC10 in clinical practice. Further studies are required to determine if rhCC10 reduces lung inflammation in infants at risk of CLD, and to determine dose and dosing strategy" |
| Abdel‐Latif ME, Osborn DA. Laryngeal mask airway surfactant administration for prevention of morbidity and mortality in preterm infants with or at risk of respiratory distress syndrome. Cochrane Database of Systematic Reviews 2011, Issue 7. | Primary outcomes pre‐specified include:
| "There is evidence from a single small trial that LMA surfactant administration in preterm infants ≥ 1200 g with established RDS may have a short term effect in reducing oxygen requirements although the study is underpowered to detect important clinical effects. Adequately powered trials are required to determine the effect of LMA surfactant administration for prevention or treatment of RDS in preterm infants. LMA surfactant administration should be limited to clinical trials" |
| Abdel‐Latif ME, Osborn DA. Pharyngeal instillation of surfactant before the first breath for prevention of morbidity and mortality in preterm infants at risk of respiratory distress syndrome. Cochrane Database of Systematic Reviews 2011, Issue 3. | Primary outcomes pre‐specified include:
| No included trials. "There were no data from randomised controlled or quasi‐randomised trials that evaluated the effect of intrapartum instillation of pharyngeal surfactant before the first breath. Evidence from animal and observational human studies suggest that pharyngeal instillation of surfactant before the first breath is potentially safe, feasible and may be effective. Well designed trials are needed" |
| Abdel‐Latif ME, Osborn DA. Nebulised surfactant in preterm infants with or at risk of respiratory distress syndrome. Cochrane Database of Systematic Reviews 2012, Issue 10. | Primary outcomes pre‐specified include:
| "There are insufficient data to support or refute the use of nebulised surfactant in clinical practice. Adequately powered trials are required to determine the effect of nebulised surfactant administration for prevention or early treatment of RDS in preterm infants. Nebulised surfactant administration should be limited to clinical trials" |
| Ainsworth S, McGuire W. Percutaneous central venous catheters versus peripheral cannulae for delivery of parenteral nutrition in neonates. Cochrane Database of Systematic Reviews 2015, Issue 10. | Primary outcomes pre‐specified include:
| "Data from one small trial suggest that use of percutaneous central venous catheters to deliver parenteral nutrition increases nutrient input. The significance of this in relation to long‐term growth and developmental outcomes is unclear. Three trials suggest that use of percutaneous central venous catheters decreases the number of catheters/cannulae needed to deliver nutrition. No evidence suggests that percutaneous central venous catheter use increases risks of adverse events, particularly invasive infection, although none of the included trials was large enough to rule out an effect on uncommon severe adverse events such as pericardial effusion" |
| Alcock GS, Liley H. Immunoglobulin infusion for isoimmune haemolytic jaundice in neonates. Cochrane Database of Systematic Reviews 2002, Issue 3. | Outcomes pre‐specified include:
| "Although the results show a significant reduction in the need for exchange transfusion in those treated with intravenous immunoglobulin, the applicability of the results is limited. The number of studies and infants included is small and none of the three included studies was of high quality. The protocols of two of the studies mandated the use of early exchange transfusion, limiting the generalizability of the results. Further well designed studies are needed before routine use of intravenous immunoglobulin can be recommended for the treatment of isoimmune haemolytic jaundice" |
| Anabrees J, AlFaleh K. Fluid restriction and prophylactic indomethacin versus prophylactic indomethacin alone for prevention of morbidity and mortality in extremely low birth weight infants. Cochrane Database of Systematic Reviews 2011, Issue 7. | Secondary outcomes pre‐specified include:
| No included trials "We found no randomized controlled trials to investigate the possible interaction between fluid restriction and indomethacin prophylaxis versus indomethacin prophylaxis alone in ELBW infants. A well‐designed randomized trial is needed to address this question" |
| Austin N, Cleminson J, Darlow BA, McGuire W. Prophylactic oral/topical non‐absorbed antifungal agents to prevent invasive fungal infection in very low birth weight infants. Cochrane Database of Systematic Reviews 2015, Issue 10. | Primary outcomes pre‐specified include:
| "The finding of a reduction in risk of invasive fungal infection in very low birth weight infants treated with oral/topical non‐absorbed antifungal prophylaxis should be interpreted cautiously because of methodological weaknesses in the included trials. Further large randomised controlled trials in current neonatal practice settings are needed to resolve this uncertainty. These trials might compare oral/topical non‐absorbed antifungal agents with placebo, with each other, or with systemic antifungal agents and should include an assessment of effect on long‐term neurodevelopmental outcomes" |
| Bahadue FL, Soll R. Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome. Cochrane Database of Systematic Reviews 2012, Issue 11. | Secondary outcomes pre‐specified include:
| "Early selective surfactant administration given to infants with RDS requiring assisted ventilation leads to a decreased risk of acute pulmonary injury (decreased risk of pneumothorax and pulmonary interstitial emphysema) and a decreased risk of neonatal mortality and chronic lung disease compared to delaying treatment of such infants until they develop worsening RDS" |
| Rivas‐Fernandez M, Roqué i Figuls M, Diez‐Izquierdo A, Escribano J, Balaguer A. Infant position in neonates receiving mechanical ventilation. Cochrane Database of Systematic Reviews 2016, Issue 11. | Secondary outcomes pre‐specified include:
| "This update of our last review in 2013 supports previous conclusions. Evidence of low to moderate quality favours the prone position for slightly improved oxygenation in neonates undergoing mechanical ventilation. However, we found no evidence to suggest that particular body positions during mechanical ventilation of the neonate are effective in producing sustained and clinically relevant improvement" |
| Balain M, Oddie SJ, McGuire W. Antimicrobial‐impregnated central venous catheters for prevention of catheter‐related bloodstream infection in newborn infants. Cochrane Database of Systematic Reviews 2015, Issue 9. | Secondary outcomes pre‐specified include:
| "Although the data from one small trial indicates that antimicrobial‐impregnated central venous catheters might prevent catheter‐related bloodstream infection in newborn infants, the available evidence is insufficient to guide clinical practice. A large, simple and pragmatic randomised controlled trial is needed to resolve on‐going uncertainty" |
| Bassler D, Kreutzer K, McNamara P, Kirpalani H. Milrinone for persistent pulmonary hypertension of the newborn. Cochrane Database of Systematic Reviews 2010, Issue 11. | Primary outcomes pre‐specified include:
| "The efficacy and safety of milrinone in the treatment of PPHN are not known and its use should be restricted within the context of RCTs. Such studies should address a comparison of milrinone with placebo (in clinical situations where iNO is not available) or, in well resourced countries, should compare milrinone with iNO or as an adjunct to iNO compared with iNO alone" |
| Basuki F, Hadiati DR, Turner T, McDonald S, Hakimi M. Dilute versus full strength formula in exclusively formula‐fed preterm or low birth weight infants. Cochrane Database of Systematic Reviews 2013, Issue 11. | Secondary outcomes pre‐specified include:
| "There is evidence from three small, old trials at unclear risk of bias that use of dilute formula in preterm or low birth weight formula‐fed infants leads to an important reduction in the time taken for these infants to attain an adequate energy intake. There was no evidence of important differences in feeding intolerance. The impact on serious gastrointestinal problems, including necrotising enterocolitis, was not reported. Further randomised trials are needed to confirm these results" |
| Beveridge CJE, Wilkinson AR. Sodium bicarbonate infusion during resuscitation of infants at birth. Cochrane Database of Systematic Reviews 2006, Issue 1. | Secondary outcomes pre‐specified include:
| "There is insufficient evidence from randomised controlled trials to determine whether the infusion of sodium bicarbonate reduces mortality and morbidity in infants receiving resuscitation in the delivery room at birth" |
| Bhola K, Foster JP, Osborn DA. Chest shielding for prevention of a haemodynamically significant patent ductus arteriosus in preterm infants receiving phototherapy. Cochrane Database of Systematic Reviews 2015, Issue 11. | Secondary outcomes pre‐specified include:
| "The available evidence is very low quality and insufficient to assess the safety or efficacy of chest shield during phototherapy for prevention of PDA in preterm infants. Further trials of chest shielding are warranted, particularly in settings where infants are not receiving prophylactic or early echocardiographic targeted cyclo‐oxygenase inhibitors for PDA" |
| Booth D, Evans DJ. Anticonvulsants for neonates with seizures. Cochrane Database of Systematic Reviews 2004, Issue 3. | Primary outcomes pre‐specified include:
| "At present there is little evidence from randomised controlled trials to support the use of any of the anticonvulsants currently used in the neonatal period. In the literature, there remains a body of opinion that seizures should be treated because of the concern that seizures in themselves may be harmful, although this is only supported by relatively low grade evidence (Levene 2002; Massingale 1993). Development of safe and effective treatment strategies relies on future studies of high quality (randomised controlled trials with methodology that assures validity) and of sufficient size to have the power to detect clinically important reductions in mortality and severe neurodevelopmental disability in addition to any short term reduction in seizure burden" |
| Bottino M, Cowett RM, Sinclair JC. Interventions for treatment of neonatal hyperglycemia in very low birth weight infants. Cochrane Database of Systematic Reviews 2011, Issue 10. | Primary outcomes pre‐specified include:
| "Evidence from randomized trials in hyperglycemic VLBW neonates is insufficient to determine the effects of treatment on death or major morbidities. It remains uncertain whether the hyperglycemia per se is a cause of adverse clinical outcomes or how the hyperglycemia should be treated. Much larger randomized trials in hyperglycemic VLBW neonates that are powered on clinical outcomes are needed in order to determine whether, and how, the hyperglycemia should be treated" |
| Brion LP, Bell EF, Raghuveer TS. Vitamin E supplementation for prevention of morbidity and mortality in preterm infants. Cochrane Database of Systematic Reviews 2003, Issue 4. | Primary outcomes pre‐specified include:
| "Vitamin E supplementation in preterm infants reduced the risk of intracranial hemorrhage but increased the risk of sepsis. In very low birth weight infants, vitamin E increased the risk of sepsis, and reduced the risk of severe retinopathy and blindness among those examined. Evidence does not support the routine use of vitamin E supplementation by intravenous route at high doses or aiming at serum tocopherol levels greater than 3.5 mg/dl" |
| Brown JVE, Embleton ND, Harding JE, McGuire W. Multi‐nutrient fortification of human milk for preterm infants. Cochrane Database of Systematic Reviews 2016, Issue 5. | Primary outcomes pre‐specified include:
| "Limited available data do not provide strong evidence that feeding preterm infants with multi‐nutrient fortified breast milk compared with unfortified breast milk affects important outcomes, except that it leads to slightly increased in‐hospital growth rates" |
| Brown JVE, Moe‐Byrne T, McGuire W. Glutamine supplementation for young infants with severe gastrointestinal disease. Cochrane Database of Systematic Reviews 2014, Issue 12. | Primary outcomes pre‐specified include:
| "The available data from randomised controlled trials do not suggest that glutamine supplementation has any important benefits for young infants with severe gastrointestinal disease" |
| Bruschettini M, Romantsik O, Zappettini S, Banzi R, Ramenghi LA, Calevo MG. Antithrombin for the prevention of intraventricular hemorrhage in very preterm infants. Cochrane Database of Systematic Reviews 2016, Issue 3. | Secondary outcomes pre‐specified include:
| "The administration of antithrombin seems not to reduce the incidence and severity of intraventricular hemorrhage in very preterm infants. Limited evidence is available on other clinically relevant outcomes. Given the imprecision of the estimate, the results of this systematic review are consistent with either a benefit or a detrimental effect of antithrombin and do not provide a definitive answer to the review question" |
| Bruschettini M, Zappettini S, Moja L, Calevo MG. Frequency of endotracheal suctioning for the prevention of respiratory morbidity in ventilated newborns. Cochrane Database of Systematic Reviews 2016, Issue 3. | Secondary outcomes pre‐specified include:
| "There was insufficient evidence to identify the ideal frequency of ETT suctioning in ventilated neonates. Future research should focus on the effects in the very preterm newborns, that is, the most vulnerable population as concerns the risk of both lung and brain damage. Assessment should include the cases of prolonged ventilation, when more abundant, dense secretions are common. Clinical trials might include comparisons between 'as‐scheduled' versus 'as‐needed' endotracheal suctioning, that is, based on specific indications, as well frequent versus less frequent suctioning schedules" |
| Bruschettini M, Romantsik O, Zappettini S, Banzi R, Ramenghi LA, Calevo MG. Heparin for the prevention of intraventricular haemorrhage in preterm infants. Cochrane Database of Systematic Reviews 2016, Issue 5. | Secondary outcomes pre‐specified include:
| "There is very limited data on the effect of prophylactic administration of heparin on the incidence and severity of IVH in very preterm neonates. Both the identified trials used heparin in the context of maintaining umbilical line patency and not specifically as an agent to prevent germinal matrix‐intraventricular haemorrhage. Given the imprecision of our estimates, the results of this systematic review are consistent with either a benefit or a detrimental effect of heparin and do not provide a definitive answer to the review question. Limited evidence is available on other clinically relevant outcomes" |
| Bruschettini M, Romantsik O, Zappettini S, Ramenghi LA, Calevo MG. Transcutaneous carbon dioxide monitoring for the prevention of neonatal morbidity and mortality. Cochrane Database of Systematic Reviews 2016, Issue 2. | Primary outcomes pre‐specified include:
Secondary outcomes pre‐specified include:
| No included trials "There was no evidence to recommend or refute the use of transcutaneous CO2 monitoring in neonates. Well‐designed, adequately powered randomized controlled studies are necessary to address efficacy and safety of transcutaneous CO2 monitoring in neonates" |
| Cleminson J, McGuire W. Topical emollient for preventing infection in preterm infants. Cochrane Database of Systematic Reviews 2016, Issue 1. | Secondary outcomes pre‐specified include:
| "The available data do not provide evidence that the use of emollient therapy prevents invasive infection or death in preterm infants in high‐, middle‐ or low‐income settings. Some evidence of an effect of topical vegetable oils on neonatal growth exists but this should be interpreted with caution because lack of blinding may have introduced caregiver or assessment biases. Since these interventions are low cost, readily accessible, and generally acceptable, further randomised controlled trials, particularly in both community‐ and health care facility‐based settings in low‐income countries, may be justified" |
| Clerihew L, McGuire W. Antifungal therapy for newborn infants with invasive fungal infection. Cochrane Database of Systematic Reviews 2012, Issue 6. | Primary outcomes pre‐specified include:
| "There are insufficient data to inform practice. Large randomised controlled trials are required to compare antifungal drugs, drug preparations or drug combinations for treating newborn infants with invasive fungal infection" |
| Cooke L, Steer PA, Woodgate PG. Indomethacin for asymptomatic patent ductus arteriosus in preterm infants. Cochrane Database of Systematic Reviews 2003, Issue 1. | Outcomes pre‐specified include:
| "This review demonstrates a significant decrease in the incidence of symptomatic PDA following treatment of an asymptomatic PDA with indomethacin. There is also a small but statistically significant decrease in the duration of requirement for supplemental oxygen. There are no reported long term outcomes in the included trials, and so it is not possible to comment on possible long term effects. Further studies are required to determine the long term benefits or harms of closing a PDA prior to the onset of symptoms" |
| Davies MW, Kimble RM, Woodgate PG. Ward reduction without general anaesthesia versus reduction and repair under general anaesthesia for gastroschisis in newborn infants. Cochrane Database of Systematic Reviews 2002, Issue 3. | Outcomes pre‐specified include:
| No included trials "There is no evidence from RCTs to support or refute the practice of ward reduction for the immediate management of gastroschisis. There is an urgent need for RCTs to compare ward reduction versus reduction under general anaesthesia in infants with gastroschisis. Initial trials would best be limited to those infants with uncomplicated gastroschisis (using pre‐defined selection criteria excluding infants that are unstable, have gut perforation, necrosis or atresia, have other organs requiring reduction besides bowel, or are considered to need a silo prior to any reduction). Trials should use adequate pain relief and specify a pre‐defined time period after which manual reduction is abandoned" |
| Davies MW, Woodgate PG. Tracheal gas insufflation for the prevention of morbidity and mortality in mechanically ventilated newborn infants. Cochrane Database of Systematic Reviews 2002, Issue 2. | Outcomes pre‐specified include:
| "There is evidence from a single RCT that TGI may reduce the duration of mechanical ventilation in preterm infants ‐ although the data from this small study do not give sufficient evidence to support the introduction of TGI into clinical practice. The technical requirements for performing TGI (as performed in the single included study) are great. There is no statistically significant reduction in the total duration of respiratory support or hospital stay. TGI cannot be recommended for general use at this time" |
| De Paoli AG, Davis PG, Faber B, Morley CJ. Devices and pressure sources for administration of nasal continuous positive airway pressure (NCPAP) in preterm neonates. Cochrane Database of Systematic Reviews 2008, Issue 1. | Secondary outcomes pre‐specified include:
| "Short binasal prong devices are more effective than single prongs in reducing the rate of re‐intubation. Although the Infant Flow Driver appears more effective than Medicorp prongs the most effective short binasal prong device remains to be determined. The improvement in respiratory parameters with short binasal prongs suggests they are more effective than nasopharyngeal CPAP in the treatment of early RDS. Further studies incorporating longer‐term outcomes are required. Studies are also needed to determine the optimal pressure source for the delivery of NCPAP" |
| Dimmick SJ, Badawi N, Randell T. Thyroid hormone supplementation for the prevention of morbidity and mortality in infants undergoing cardiac surgery. Cochrane Database of Systematic Reviews 2004, Issue 3. | Outcomes pre‐specified include:
| "At present, there is a lack of evidence concerning the effects of triiodothyronine supplementation in infants undergoing cardiac surgery. Further randomised controlled trials which include sufficiently large subject numbers in a variety of different age strata (neonates, infants and older children) need to be undertaken" |
| Foster JP, Psaila K, Patterson T. Non‐nutritive sucking for increasing physiologic stability and nutrition in preterm infants. Cochrane Database of Systematic Reviews 2016, Issue 10. | Secondary outcomes pre‐specified include:
| "Meta‐analysis demonstrated a significant effect of NNS on the transition from gavage to full oral feeding, transition from start of oral feeding to full oral feeding, and length of hospital stay. None of the trials reported any adverse effects. Well‐designed, adequately powered studies using reliable methods of randomisation, concealment of treatment allocation and blinding of the intervention and outcome assessors are needed. In order to facilitate meta‐analysis of these data, future research should involve outcome measures consistent with those used in previous studies" |
| Görk AS, Ehrenkranz RA, Bracken MB. Continuous infusion versus intermittent bolus doses of indomethacin for patent ductus arteriosus closure in symptomatic preterm infants. Cochrane Database of Systematic Reviews 2008, Issue 1. | Secondary outcomes pre‐specified include:
| "The available data is insufficient to draw conclusions regarding the efficacy of continuous indomethacin infusion vs. bolus injections for the treatment of PDA. Although continuous indomethacin seems to cause less alterations in cerebral, renal and mesenteric circulations, the clinical meaning of this effect is unclear. Definitive recommendations about the preferred method of indomethacin administration in premature infants cannot be made based on the current findings of this review" |
| Henderson G, Anthony MY, McGuire W. Formula milk versus maternal breast milk for feeding preterm or low birth weight infants. Cochrane Database of Systematic Reviews 2007, Issue 4. | Primary outcomes pre‐specified include:
| No included trials "There are no data from randomised trials of formula milk versus maternal breast milk for feeding preterm or low birth weight infants. This may relate to a perceived difficulty of allocating an alternative feed to an infant whose mother wishes to feed with her own breast milk. Maternal breast milk remains the default choice of enteral nutrition because observational studies, and meta‐analyses of trials comparing feeding with formula milk versus donor breast milk, suggest that feeding with breast milk has major non‐nutrient advantages for preterm or low birth weight infants" |
| Henderson G, Fahey T, McGuire W. Nutrient‐enriched formula milk versus human breast milk for preterm infants following hospital discharge. Cochrane Database of Systematic Reviews 2007, Issue 4. | Primary outcomes pre‐specified include:
| No included trials "There are no data from randomised controlled trials to determine whether feeding preterm infants following hospital discharge with nutrient‐enriched formula milk versus human breast milk affects growth and development. Mothers who wish to breast feed, and their health care advisors, would require very clear evidence that feeding with a nutrient‐enriched formula milk had major advantages for their infants before electing not to feed (or to reduce feeding) with maternal breast milk. If evidence from trials that compared feeding preterm infants following hospital discharge with nutrient‐enriched versus standard formula milk demonstrated an effect on growth or development, then this might strengthen the case for undertaking trials of nutrient‐enriched formula milk versus human breast milk" |
| Henderson‐Smart DJ, Wilkinson AR, Raynes‐Greenow CH. Mechanical ventilation for newborn infants with respiratory failure due to pulmonary disease. Cochrane Database of Systematic Reviews 2002, Issue 4. | Secondary outcomes pre‐specified include:
| "When MV was introduced in the 1960s to treat infants with severe respiratory failure due to pulmonary disease, trials showed an overall reduction in mortality which was most marked in infants born with a birthweight of more than 2 kg. This review does not provide information to evaluate the relative benefits or harms of MV in the setting of modern perinatal care" |
| Ho JJ, Henderson‐Smart DJ, Davis PG. Early versus delayed initiation of continuous distending pressure for respiratory distress syndrome in preterm infants. Cochrane Database of Systematic Reviews 2002, Issue 2. | Secondary outcomes pre‐specified include:
| "Early application of CDP has a clinical benefit in the treatment of RDS in that it reduces subsequent use of IPPV and thus may be useful in preventing the adverse effects of this treatment. However, many of the trials were done in the 1970s and 1980s and re‐evaluation of the strategy of early CDP in the era of antenatal steroid use and early surfactant administration is indicated focusing on administration methods" |
| Ho JJ, Rasa G. Magnesium sulfate for persistent pulmonary hypertension of the newborn. Cochrane Database of Systematic Reviews 2007, Issue 3. | Secondary outcomes pre‐specified include:
| No included trials "On the basis of the current lack of evidence, the use of magnesium sulphate cannot be recommended in the treatment of PPHN. Randomised controlled trials are recommended" |
| Hunt R, Osborn DA. Dopamine for prevention of morbidity and mortality in term newborn infants with suspected perinatal asphyxia. Cochrane Database of Systematic Reviews 2002, Issue 3. | Primary outcomes pre‐specified include:
(Review reports on 'neurodevelopmental disability' for 1 RCT (14 infants), which did not include cerebral palsy) | "There is currently insufficient evidence from randomised controlled trials that the use of dopamine in term infants with suspected perinatal asphyxia improves mortality or long‐term neurodevelopmental outcome. The question of whether dopamine improves outcome for term infants with suspected perinatal asphyxia has not been answered. Further research is required to determine whether or not the use of dopamine improves mortality and long‐term morbidity for these infants and if so, issues such as which infants, at what dose and with what co‐interventions should be addressed" |
| Hunt R, Davis PG, Inder TE. Replacement of estrogens and progestins to prevent morbidity and mortality in preterm infants. Cochrane Database of Systematic Reviews 2004, Issue 4. | Primary outcomes pre‐specified include:
| "The one small randomised controlled trial demonstrated neither evidence of benefit or harm related to the replacement of estradiol and progesterone in preterm infants less than 30 weeks' gestation. A properly powered randomised controlled trial is required to determine whether or not administration of estradiol or progesterone, either alone or in combination, and at varying doses, confers any clinically significant benefits, or poses any risk, to the preterm infant" |
| Ibrahim H, Sinha IP, Subhedar NV. Corticosteroids for treating hypotension in preterm infants. Cochrane Database of Systematic Reviews 2011, Issue 12. | Primary outcomes pre‐specified include:
| "Hydrocortisone may be as effective as dopamine when used as a primary treatment for hypotension. But the long term safety data on the use of hydrocortisone in this manner is unknown. Steroids are effective in treatment of refractory hypotension in preterm infants without an increase in short term adverse consequences. However, long term safety or benefit data is lacking. With long term benefit or safety data lacking steroids cannot be recommended routinely for the treatment of hypotension in preterm infants" |
| Ibrahim MDH, Sinn JKH, McGuire W. Iodine supplementation for the prevention of mortality and adverse neurodevelopmental outcomes in preterm infants. Cochrane Database of Systematic Reviews 2006, Issue 2. | Primary outcomes pre‐specified include:
| "There are insufficient data at present to determine whether providing preterm infants with supplemental iodine (to match fetal accretion rates) prevents morbidity and mortality in preterm infants. Future randomised controlled trials of iodine supplementation should focus on extremely preterm and extremely low birth weight infants, the group at greatest risk of transient hypothyroxinaemia. These trials should aim to assess the effect of iodine supplementation on clinically important outcomes including respiratory morbidity and longer term neurodevelopment" |
| Inglis GDT, Davies MW. Prophylactic antibiotics to reduce morbidity and mortality in neonates with umbilical venous catheters. Cochrane Database of Systematic Reviews 2005, Issue 4. | Secondary outcomes pre‐specified include:
| "There is insufficient evidence from randomised trials to support or refute the use of prophylactic antibiotics when UVCs are inserted in newborn infants. There is no evidence to support or refute continuing antibiotics once initial cultures rule out infection in newborn infants with UVCs" |
| Inglis GDT, Jardine LA, Davies MW. Prophylactic antibiotics to reduce morbidity and mortality in ventilated newborn infants. Cochrane Database of Systematic Reviews 2007, Issue 3. | Secondary outcomes pre‐specified include:
| "There is insufficient evidence from randomised trials to support or refute the use of prophylactic antibiotics when starting mechanical ventilation in newborn infants, or to support or refute continuing antibiotics once initial cultures have ruled out infection in mechanically ventilated newborn infants" |
| Inglis GDT, Jardine LA, Davies MW. Prophylactic antibiotics to reduce morbidity and mortality in neonates with umbilical artery catheters. Cochrane Database of Systematic Reviews 2007, Issue 4. | Secondary outcomes pre‐specified include:
| "There is insufficient evidence from randomised trials to support or refute the use of prophylactic antibiotics when umbilical artery catheters are inserted in newborn infants, and no evidence to support or refute continuing antibiotics once initial cultures rule out infection in newborn infants with umbilical artery catheters" |
| Jardine LA, Inglis GDT, Davies MW. Prophylactic systemic antibiotics to reduce morbidity and mortality in neonates with central venous catheters. Cochrane Database of Systematic Reviews 2008, Issue 1. | Secondary outcomes pre‐specified include:
| "Prophylactic systemic antibiotics in neonates with a central venous catheter reduces the rate of proven or suspected septicaemia. However, this may not be clinically important in the face of no significant difference in overall mortality and the lack of data on long‐term neurodevelopmental outcome. Furthermore, there is a lack of data pertaining to the potentially significant disadvantages of this approach such as the selection of resistant organisms. The routine use of prophylactic antibiotics in infants with central venous catheters in neonatal units cannot currently be recommended" |
| Jardine LA, Inglis GDT, Davies MW. Strategies for the withdrawal of nasal continuous positive airway pressure (NCPAP) in preterm infants. Cochrane Database of Systematic Reviews 2011, Issue 2. Art. No.: CD006979. DOI: 10.1002/14651858.CD006979.pub2. | Secondary outcomes pre‐specified include:
| "Infants who have their NCPAP pressure weaned to a predefined level and then stop NCPAP completely have less total time on NCPAP and shorter durations of oxygen therapy and hospital stay compared with those that have NCPAP removed for a predetermined number of hours each day. Future trials of withdrawing NCPAP should compare proposed strategies with weaning NCPAP pressure to a predefined level and then stopping NCPAP completely. Clear criteria need to be established for the definition of stability prior to attempting to withdraw NCPAP" |
| Kaushal A, McDonnell CG, Davies MW. Partial liquid ventilation for the prevention of mortality and morbidity in paediatric acute lung injury and acute respiratory distress syndrome. Cochrane Database of Systematic Reviews 2013, Issue 2. | Secondary outcomes pre‐specified include:
| "There is no evidence from RCTs to support or refute the use of partial liquid ventilation in children with acute lung injury or acute respiratory distress syndrome. Adequately powered, high quality RCTs are still needed to assess its efficacy. Clinically relevant outcome measures should be assessed (mortality at discharge and later, duration of both respiratory support and hospital stay, and long‐term neurodevelopmental outcomes). The studies should be published in full" |
| Kecskes Z, Healy G, Jensen A. Fluid restriction for term infants with hypoxic‐ischaemic encephalopathy following perinatal asphyxia. Cochrane Database of Systematic Reviews 2005, Issue 3. | Primary outcomes pre‐specified include:
| No included trials "Given that fluid restriction for the treatment of hypoxic ischaemic encephalopathy following perinatal asphyxia is recommended in standard textbooks, there is a need for randomised, controlled trials to establish if this practice affects mortality and morbidity. As it may not be ethical to include neonates with acute renal failure in a randomised trial, these babies will have to be excluded from the trial. These studies should investigate the effects of fluid management on outcomes such as mortality, seizure activity, evidence of cerebral damage on histology, and effects on renal function and electrolytes" |
| Keir AK, Wilkinson D, Andersen C, Stark MJ. Washed versus unwashed red blood cells for transfusion for the prevention of morbidity and mortality in preterm infants. Cochrane Database of Systematic Reviews 2016, Issue 1. | Primary outcomes pre‐specified include:
Secondary outcomes pre‐specified include:
| "We identified a single small study. The results from this study show a high level of uncertainty, as the confidence intervals are consistent with both a large improvement or a serious harm caused by the intervention. Consequently, there is insufficient evidence to support or refute the use of washed RBCs to prevent the development of significant neonatal morbidities or mortality. Further clinical trials are required to assess the potential effects of pre‐transfusion washing of RBCs for preterm or very low birth weight infants, or both, on short‐ and long‐term outcomes" |
| Kylat RI, Ohlsson A. Recombinant human activated protein C for severe sepsis in neonates. Cochrane Database of Systematic Reviews 2012, Issue 4. | Secondary outcomes pre‐specified include:
| "Despite the scientific rationale for its use, there is insufficient data to use rhAPC for the management of severe sepsis in newborn infants. Due to the results among adults with lack of efficacy, an increase in bleeding and resulting withdrawal of rhAPC from the market, neonates should not be treated with rhAPC and further trials should not be conducted" |
| Lai NM, Foong SC, Foong WC, Tan K. Co‐bedding in neonatal nursery for promoting growth and neurodevelopment in stable preterm twins. Cochrane Database of Systematic Reviews 2016, Issue 4. | Secondary outcomes pre‐specified include:
| "Evidence on the benefits and harms of co‐bedding for stable preterm twins was insufficient to permit recommendations for practice. Future studies must be adequately powered to detect clinically important differences in growth and neurodevelopment. Researchers should assess harms such as infection, along with medication errors and caregiver satisfaction" |
| Lai NM, Rajadurai SV, Tan K. Increased energy intake for preterm infants with (or developing) bronchopulmonary dysplasia/chronic lung disease. Cochrane Database of Systematic Reviews 2006, Issue 3. | Secondary outcomes pre‐specified include:
| No included trials "To date, no randomised controlled trials are available that examine the effects of increased versus standard energy intake for preterm infants with (or developing) CLD/BPD. Research should be directed at evaluating the effects of various levels of energy intake on this group of infants on clinically important outcomes like mortality, respiratory status, growth and neurodevelopment. The benefits and harms of various ways of increasing energy intake, including higher energy density of milk feed and/or fluid volume (clinically realistic target volume should be set), parenteral nutrition, and the use of various constituents of energy like carbohydrate, protein and fat for this purpose also need to be assessed" |
| Lai NM, Taylor JE, Tan K, Choo YM, Ahmad Kamar A, Muhamad NA. Antimicrobial dressings for the prevention of catheter‐related infections in newborn infants with central venous catheters. Cochrane Database of Systematic Reviews 2016, Issue 3. | Secondary outcomes pre‐specified include:
| "Based on moderate‐quality evidence, chlorhexidine dressing/alcohol skin cleansing reduced catheter colonisation, but made no significant difference in major outcomes like sepsis and CRBSI compared to polyurethane dressing/povidone‐iodine cleansing. Chlorhexidine dressing/alcohol cleansing posed a substantial risk of contact dermatitis in preterm infants, although it was unclear whether this was contributed mainly by the dressing material or the cleansing agent. While silver‐alginate patch appeared safe, evidence is still insufficient for a recommendation in practice. Future research that evaluates antimicrobial dressing should ensure blinding of caregivers and outcome assessors and ensure that all participants receive the same co‐interventions, such as the skin cleansing agent. Major outcomes like sepsis, CRBSI and mortality should be assessed in infants of different gestation and birth weight" |
| Lai M, Inglis GDT, Hose K, Jardine LA, Davies MW. Methods for securing endotracheal tubes in newborn infants. Cochrane Database of Systematic Reviews 2014, Issue 7. | Secondary outcomes pre‐specified include:
| "This review highlighted the need for further well designed and completed studies to be conducted for this common neonatal procedure. Evidence is lacking to determine the most effective and safe method to stabilise the endotracheal tube in the ventilated neonate" |
| Lawn CJ, Weir FJ, McGuire W. Base administration or fluid bolus for preventing morbidity and mortality in preterm infants with metabolic acidosis. Cochrane Database of Systematic Reviews 2005, Issue 2. | Secondary outcomes pre‐specified include:
| "There is insufficient evidence from randomised controlled trials to determine whether infusion of base or fluid bolus reduces morbidity and mortality in preterm infants with metabolic acidosis. Further large randomised trials are needed" |
| Malwade US, Jardine LA. Home‐ versus hospital‐based phototherapy for the treatment of non‐haemolytic jaundice in infants at more than 37 weeks' gestation. Cochrane Database of Systematic Reviews 2014, Issue 6. | Primary outcomes pre‐specified include:
| No included trials "No high‐quality evidence is currently available to support or refute the practice of home‐based phototherapy for non‐haemolytic jaundice in infants at more than 37 weeks' gestation" |
| McGuire W, Fowlie PW, Evans DJ. Naloxone for preventing morbidity and mortality in newborn infants of greater than 34 weeks' gestation with suspected perinatal asphyxia. Cochrane Database of Systematic Reviews 2004, Issue 1. | Primary outcomes pre‐specified include:
| "There are insufficient data available to evaluate the safety and effectiveness of the routine use of naloxone for newborn infants of greater than 34 weeks' gestation with suspected perinatal asphyxia. A further randomised controlled trial is needed to determine if naloxone benefits newborn infants with suspected perinatal asphyxia. Such a trial should assess clinically important outcomes such as mortality, and adverse short and long term neurological outcomes" |
| Morgan J, Bombell S, McGuire W. Early trophic feeding versus enteral fasting for very preterm or very low birth weight infants. Cochrane Database of Systematic Reviews 2013, Issue 3. | Secondary outcomes pre‐specified include:
| "The available trial data do not provide evidence of important beneficial or harmful effects of early trophic feeding for very preterm or very low birth weight infants. The applicability of these findings to extremely preterm, extremely low birth weight or growth restricted infants is limited. Further randomised controlled trials would be needed to determine how trophic feeding compared with enteral fasting affects important outcomes in this population" |
| Morgan J, Young L, McGuire W. Slow advancement of enteral feed volumes to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database of Systematic Reviews 2015, Issue 10. | Secondary outcomes pre‐specified include:
| "The available trial data suggest that advancing enteral feed volumes at daily increments of 30 to 40 mL/kg (compared to 15 to 24 mL/kg) does not increase the risk of NEC or death in VLBW infants. Advancing the volume of enteral feeds at slow rates results in several days of delay in establishing full enteral feeds and increases the risk of invasive infection. The applicability of these findings to extremely preterm, extremely low birth weight, or growth‐restricted infants is limited. Further randomised controlled trials in these populations may be warranted to resolve this uncertainty" |
| Morgan J, Young L, McGuire W. Delayed introduction of progressive enteral feeds to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database of Systematic Reviews 2014, Issue 12. | Secondary outcomes pre‐specified include:
| "The evidence available from randomised controlled trials suggested that delaying the introduction of progressive enteral feeds beyond four days after birth did not reduce the risk of developing NEC in very preterm or VLBW infants, including growth‐restricted infants. Delaying the introduction of progressive enteral feeds resulted in a few days' delay in establishing full enteral feeds but the clinical importance of this effect was unclear. The applicability of these findings to extremely preterm or extremely low birth weight was uncertain. Further randomised controlled trials in this population may be warranted" |
| Mosalli R, AlFaleh K. Prophylactic surgical ligation of patent ductus arteriosus for prevention of mortality and morbidity in extremely low birth weight infants. Cochrane Database of Systematic Reviews 2008, Issue 1. | Secondary outcomes pre‐specified include:
| "Prophylactic surgical ligation of the PDA did not decrease mortality or BPD in ELBW infants. A significant reduction of stage II or III NEC was noted. Based on the current evidence, the high rate of spontaneous closure, availability of effective safe medical therapies, and the potential short and long‐term complications of surgical ligation, the use such prophylactic surgical therapy is not indicated in the management of the preterm infants" |
| O'Donnell CPF, Bruschettini M, Davis PG, Morley CJ, Moja L, Calevo MG, Zappettini S. Sustained versus standard inflations during neonatal resuscitation to prevent mortality and improve respiratory outcomes. Cochrane Database of Systematic Reviews 2015, Issue 7. | Secondary outcomes pre‐specified include:
| "At present there is insufficient evidence from clinical trials to determine the efficacy and safety of initial sustained lung inflation for newborn infants resuscitated with PPV. RCTs comparing PPV with and without sustained inflations at neonatal resuscitation are warranted" |
| Ogunlesi TA, Odigwe CC, Oladapo OT. Adjuvant corticosteroids for reducing death in neonatal bacterial meningitis. Cochrane Database of Systematic Reviews 2015, Issue 11. | Secondary outcomes pre‐specified include:
| "Very low‐quality data from two randomised controlled trials suggest that some reduction in death and hearing loss may result from use of adjunctive steroids alongside standard antibiotic therapy for treatment of patients with neonatal meningitis. Benefit is not yet seen with regards to reduction in neurological sequelae. Researchers who wish to clarify these findings must conduct more robustly designed trials with greater numbers of participants, evaluating more relevant outcomes and providing adequate follow‐up" |
| Onland W, Offringa M, van Kaam A. Late (≥ 7 days) inhalation corticosteroids to reduce bronchopulmonary dysplasia in preterm infants. Cochrane Database of Systematic Reviews 2012, Issue 4. | Secondary outcomes pre‐specified include:
| "Based on the results of the currently available evidence, inhalation corticosteroids initiated at ≥ 7 days of life for preterm infants at high risk of developing BPD cannot be recommended at this point in time. More and larger randomised, placebo‐controlled trials are needed to establish the efficacy and safety of inhalation corticosteroids" |
| Osborn DA, Evans NJ. Early volume expansion versus inotrope for prevention of morbidity and mortality in very preterm infants. Cochrane Database of Systematic Reviews 2001, Issue 2. | Primary outcomes pre‐specified include:
| "Dopamine was more successful than albumin at correcting low BP in hypotensive preterm infants, many of whom had already received volume. Neither intervention has been shown to be superior at improving blood flow or in improving mortality and morbidity in preterm infants. The trials do not allow any firm conclusions to be made as to whether or when volume or dopamine should be used in preterm infants" |
| Osborn DA, Hunt R. Postnatal thyroid hormones for preterm infants with transient hypothyroxinaemia. Cochrane Database of Systematic Reviews 2007, Issue 1. | Primary outcomes pre‐specified include:
| "There is insufficient evidence to determine whether use of thyroid hormones for treatment of preterm infants with transient hypothyroxinaemia results in changes in neonatal morbidity and mortality, or reductions in neurodevelopmental impairments. Further research is required" |
| Osborn DA, Hunt R. Postnatal thyroid hormones for respiratory distress syndrome in preterm infants. Cochrane Database of Systematic Reviews 2007, Issue 1. | Primary outcomes pre‐specified include:
| "There is no evidence from controlled clinical trials that postnatal thyroid hormone treatment reduces the severity of respiratory distress syndrome, neonatal morbidity or mortality in preterm infants with respiratory distress syndrome" |
| Özek E, Soll R, Schimmel MS. Partial exchange transfusion to prevent neurodevelopmental disability in infants with polycythemia. Cochrane Database of Systematic Reviews 2010, Issue 1. | Primary outcomes pre‐specified include:
| "There are no proven clinically significant short or long‐term benefits of PET in polycythemic newborn infants who are clinically well or who have minor symptoms related to hyperviscosity. PET may lead to an increase in the risk of NEC. The data regarding developmental follow‐up are extremely imprecise due to the large number of surviving infants who were not assessed and, therefore, the true risks and benefits of PET are unclear" |
| Paradisis M, Osborn DA. Adrenaline for prevention of morbidity and mortality in preterm infants with cardiovascular compromise. Cochrane Database of Systematic Reviews 2004, Issue 1. | Primary outcomes pre‐specified include:
| "There are insufficient data on the use of adrenaline infusions in preterm infants with cardiovascular compromise to make recommendations for practice. There is a need for larger trials to determine whether adrenaline is effective in reducing morbidity and mortality in preterm infants with cardiovascular compromise" |
| Pfister RH, Soll R, Wiswell TE. Protein‐containing synthetic surfactant versus protein‐free synthetic surfactant for the prevention and treatment of respiratory distress syndrome. Cochrane Database of Systematic Reviews 2009, Issue 4. | Secondary outcomes pre‐specified include:
| "In the one trial comparing protein containing synthetic surfactants compared to protein free synthetic surfactant for the prevention of RDS, no statistically different clinical differences in death and chronic lung disease were noted. Clinical outcomes between the two groups were generally similar although the group receiving protein containing synthetic surfactants did have decreased incidence of respiratory distress syndrome. Further well designed studies comparing protein containing synthetic surfactant to the more widely used animal derived surfactant extracts are indicated" |
| Pfister RH, Soll R, Wiswell TE. Protein containing synthetic surfactant versus animal derived surfactant extract for the prevention and treatment of respiratory distress syndrome. Cochrane Database of Systematic Reviews 2007, Issue 4. | Secondary outcomes pre‐specified include:
| "In two trials of protein containing synthetic surfactants compared to animal derived surfactant extract, no statistically different clinical differences in death and chronic lung disease were noted. In general, clinical outcomes between the two groups were similar. Further well designed studies of adequate size and power will help confirm and refine these findings" |
| Pilley E, McGuire W. Pre‐discharge "car seat challenge" for preventing morbidity and mortality in preterm infants. Cochrane Database of Systematic Reviews 2006, Issue 1. | Secondary outcomes pre‐specified include:
| No included trials "It is unclear whether undertaking a pre‐discharge car seat challenge is beneficial or harmful to preterm infants. Further studies are needed to determine whether the car seat challenge accurately predicts the risk of clinically significant adverse events in preterm infants travelling in car seats. If this is shown to be the case then a large randomised controlled trial is needed to provide an unbiased assessment of its utility in pre‐discharge assessment" |
| Quigley M, McGuire W. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane Database of Systematic Reviews 2014, Issue 4. | Primary outcomes pre‐specified include:
| "In preterm and low birth weight infants, feeding with formula compared with donor breast milk results in a higher rate of short‐term growth but also a higher risk of developing necrotising enterocolitis. Limited data on the comparison of feeding with formula versus nutrient‐fortified donor breast milk are available. This limits the applicability of the findings of this review as nutrient fortification of breast milk is now a common practice in neonatal care. Future trials may compare growth, development and adverse outcomes in infants who receive formula milk versus nutrient‐fortified donor breast milk given as a supplement to maternal expressed breast milk or as a sole diet" |
| Qureshi MJ, Kumar M. D‐Penicillamine for preventing retinopathy of prematurity in preterm infants. Cochrane Database of Systematic Reviews 2013, Issue 9. | Secondary outcomes pre‐specified include:
| "Administration of prophylactic D‐penicillamine in preterm infants does not prevent acute or severe ROP, death or neurodevelopmental delay. D‐penicillamine cannot be recommended for the prevention of ROP based on the available evidence" |
| Rojas‐Reyes MX, Morley CJ, Soll R. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database of Systematic Reviews 2012, Issue 3. | Secondary outcomes pre‐specified include:
(Review notes that 2 RCTs have reported on cerebral palsy, but not in the 'acceptable range' pre‐specified; therefore no results were reported: "Neurodevelopmental outcome: For this outcome, we considered any trial reporting at approximately 2 years' corrected age (acceptable range 18 months to 28 months) any of the following entities cerebral palsy, intellectual disability or developmental delay (Bayley Scales of Infant Development Mental Developmental Index < 70), legal blindness (< 20/200 visual acuity), and hearing deficit (aided or < 60 dB on audiometric testing). The composite outcome "neurodevelopmental impairment" would be defined as having any one of the aforementioned deficits. Two trials Sinkin 1998; Vaucher 1993 performed a follow‐up study including infants recruited in the Kendig 1991 and Merritt 1991 trials respectively. Sinkin 1998 reported cerebral palsy but in 148 children at school age, no data were available from ages between 18 and 28 months. Vaucher 1993 reported on cerebral palsy and developmental delay in 145 survivors at 12 months' corrected age. No one study reporting neurodevelopmental outcomes at 24 months' corrected age was found") | "Although the early trials of prophylactic surfactant administration to infants judged to be at risk of developing RDS compared with selective use of surfactant in infants with established RDS demonstrated a decreased risk of air leak and mortality, recent large trials that reflect current practice (including greater utilization of maternal steroids and routine post delivery stabilization on CPAP) do not support these differences and demonstrate less risk of chronic lung disease or death when using early stabilization on CPAP with selective surfactant administration to infants requiring intubation" |
| Rojas‐Reyes MX, Orrego‐Rojas PA. Rescue high‐frequency jet ventilation versus conventional ventilation for severe pulmonary dysfunction in preterm infants. Cochrane Database of Systematic Reviews 2015, Issue 10. | Secondary outcomes pre‐specified include:
| "Study authors reported no significant differences in overall mortality between rescue high‐frequency jet ventilation and conventional ventilation and presented highly imprecise results for important adverse effects such as intraventricular haemorrhage, new air leaks, airway obstruction and necrotising tracheobronchitis. The overall quality of evidence is affected by limitations in trial design and by imprecision due to the small number of infants in the included study. Existing evidence does not support the use of high‐frequency jet ventilation as rescue therapy in preterm infants. Studies that target populations at greatest risk and that have sufficient power to assess important outcomes are needed. These trials should incorporate long‐term pulmonary and neurodevelopmental outcomes" |
| Romantsik O, Bruschettini M, Zappettini S, Ramenghi LA, Calevo MG. Heparin for the treatment of thrombosis in neonates. Cochrane Database of Systematic Reviews 2016, Issue 11. | Secondary outcomes pre‐specified include:
| "We found no studies that met our inclusion criteria and no evidence from randomized controlled trials to recommend or refute the use of heparin for treatment of neonates with thrombosis" |
| Sankar MJ, Sankar J, Mehta M, Bhat V, Srinivasan R. Anti‐vascular endothelial growth factor (VEGF) drugs for treatment of retinopathy of prematurity. Cochrane Database of Systematic Reviews 2016, Issue 2. | Secondary outcomes pre‐specified include:
| "Implications for practice: Intravitreal bevacizumab reduces the risk of refractive errors during childhood when used as monotherapy while intravitreal pegaptanib reduces the risk of retinal detachment when used in conjunction with laser therapy in infants with type 1 ROP. Quality of evidence was, however, low for both the outcomes because of the risk of detection and other biases. Effect on other critical outcomes and, more importantly, the long‐term systemic adverse effects of the drugs are not known. The insufficient data precludes strong conclusions favouring routine use of intravitreal anti‐VEGF agents in preterm infants with type 1 ROP. Implications for research: Further studies are needed to evaluate the effect of anti‐VEGF agents on structural and functional outcomes in childhood and delayed systemic adverse effects such as myocardial dysfunction and adverse neurodevelopmental outcomes" |
| Schulzke SM, Kaempfen S, Trachsel D, Patole SK. Physical activity programs for promoting bone mineralization and growth in preterm infants. Cochrane Database of Systematic Reviews 2014, Issue 4. | Secondary outcomes pre‐specified include:
| "Some evidence suggests that physical activity programs might promote short‐term weight gain and bone mineralization in preterm infants. Data are inadequate to allow assessment of harm or long‐term effects. Current evidence does not support the routine use of physical activity programs in preterm infants. Further trials incorporating infants with a high baseline risk of osteopenia are required. These trials should address adverse events, long‐term outcomes, and the effects of nutritional intake (calories, protein, calcium, phosphorus)" |
| Shah PS, Ohlsson A. Alpha‐1 proteinase inhibitor (a1PI) for preventing chronic lung disease in preterm infants. Cochrane Database of Systematic Reviews 2001, Issue 3. | Secondary outcomes pre‐specified include:
(Review reports on 'Developmental delay amongst infants assessed' for 1 RCT (83 infants); however it was not clear whether this included cerebral palsy (in review or RCT (published as abstract only)) | "Prophylactic administration of a1PI did not reduce the risk of CLD at 36 weeks or long term adverse developmental outcomes in preterm neonates" |
| Shah PS, Kaufman DA. Antistaphylococcal immunoglobulins to prevent staphylococcal infection in very low birth weight infants. Cochrane Database of Systematic Reviews 2009, Issue 2. | Secondary outcomes pre‐specified include:
| "Antistaphylococcal immunoglobulins (INH A‐21 and Altastaph) are not recommended for prevention of staphylococcal infections in preterm or VLBW neonates. Further research to investigate the efficacy of other products such as Pagibaximab is needed" |
| Shah SS, Ohlsson A, Halliday HL, Shah VS. Inhaled versus systemic corticosteroids for preventing chronic lung disease in ventilated very low birth weight preterm neonates. Cochrane Database of Systematic Reviews 2012, Issue 5. | Secondary outcomes pre‐specified include:
| "This review found no evidence that early inhaled steroids confer important advantages over systemic steroids in the management of ventilator dependent preterm infants. Neither inhaled steroids nor systemic steroids can be recommended as a part of standard practice for ventilated preterm infants. Because they might have fewer adverse effects than systemic steroids, further randomised controlled trials of inhaled steroids are needed that address risk/benefit ratio of different delivery techniques, dosing schedules and long‐term effects, with particular attention to neurodevelopmental outcome" |
| Shah SS, Ohlsson A, Halliday HL, Shah VS. Inhaled versus systemic corticosteroids for the treatment of chronic lung disease in ventilated very low birth weight preterm infants. Cochrane Database of Systematic Reviews 2012, Issue 5. | Secondary outcomes pre‐specified include:
| "This review found no evidence that inhaled corticosteroids confer net advantages over systemic corticosteroids in the management of ventilator dependent preterm infants. Neither inhaled steroids nor systemic steroids can be recommended as standard treatment for ventilated preterm infants. There was no evidence of difference in effectiveness or side‐effect profiles for inhaled versus systemic steroids. A better delivery system guaranteeing selective delivery of inhaled steroids to the alveoli might result in beneficial clinical effects without increasing side‐effects. To resolve this issue, studies are needed to identify the risk/benefit ratio of different delivery techniques and dosing schedules for the administration of these medications. The long‐term effects of inhaled steroids, with particular attention to neurodevelopmental outcome, should be addressed in future studies" |
| Shah PS, Ohlsson A. Sildenafil for pulmonary hypertension in neonates. Cochrane Database of Systematic Reviews 2011, Issue 8. | Secondary outcomes pre‐specified include:
| "Sildenafil in the treatment of PPHN has significant potential especially in resource limited settings. However, a large scale randomised trial comparing sildenafil with the currently used vasodilator, inhaled nitric oxide, is needed to assess efficacy and safety" |
| Sinclair JC, Bottino M, Cowett RM. Interventions for prevention of neonatal hyperglycemia in very low birth weight infants. Cochrane Database of Systematic Reviews 2011, Issue 10. | Primary outcomes pre‐specified include:
| "Glucose infusion rate: There is insufficient evidence from trials comparing lower with higher glucose infusion rates to inform clinical practice. Large randomized trials are needed, powered on clinical outcomes including death, major morbidities and adverse neurodevelopment. Insulin infusion: The evidence reviewed does not support the routine use of insulin infusions to prevent hyperglycemia in VLBW neonates. Further randomized trials of insulin infusion may be justified. They should enrol extremely low birth weight neonates at very high risk for hyperglycemia and neonatal death. They might use real time glucose monitors if these are validated for clinical use. Refinement of algorithms to guide insulin infusion is needed to enable tight control of glucose concentrations within the target range" |
| Singh N, Halliday HL, Stevens TP, Suresh G, Soll R, Rojas‐Reyes MX. Comparison of animal‐derived surfactants for the prevention and treatment of respiratory distress syndrome in preterm infants. Cochrane Database of Systematic Reviews 2015, Issue 12. | Secondary outcomes pre‐specified include:
| "Significant differences in clinical outcome were noted in the comparison trials of modified minced lung surfactant extract (beractant) compared with porcine minced lung surfactant extract (poractant alfa) including a significant increase in the risk of mortality prior to discharge, death or oxygen requirement at 36 weeks' postmenstrual age, PDA requiring treatment and "receiving > 1 dose of surfactant" in infants treated with modified bovine minced lung surfactant extract compared with porcine minced lung surfactant extract. The difference in these outcomes was limited to studies using a higher initial dose of porcine minced lung surfactant extract. It is uncertain whether the observed differences are from differences in dose or from source of extraction (porcine vs. bovine) because of the lack of dose‐equivalent comparison groups with appropriate sample size. No differences in clinical outcomes were observed in comparative trials between bovine lung lavage surfactant and modified bovine minced lung surfactants" |
| Soll R, Özek E. Prophylactic animal derived surfactant extract for preventing morbidity and mortality in preterm infants. Cochrane Database of Systematic Reviews 1997, Issue 4. | Secondary outcomes pre‐specified include:
| "Prophylactic intratracheal administration of animal derived surfactant extract to infants judged to be at risk of developing respiratory distress syndrome has been demonstrated to improve clinical outcome. Infants who receive prophylactic animal derived surfactant extract have a decreased risk of pneumothorax, a decreased risk of PIE, a decreased risk of mortality, and a decreased risk of BPD or death" |
| Stevens TP, Blennow M, Myers EH, Soll R. Early surfactant administration with brief ventilation vs. selective surfactant and continued mechanical ventilation for preterm infants with or at risk for respiratory distress syndrome. Cochrane Database of Systematic Reviews 2007, Issue 4. | Secondary outcomes pre‐specified include:
| "Early surfactant replacement therapy with extubation to NCPAP compared with later selective surfactant replacement and continued mechanical ventilation with extubation from low ventilator support is associated with less need mechanical ventilation, lower incidence of BPD and fewer air leak syndromes. A lower treatment threshold (FIO2 < 0.45) confers greater advantage in reducing the incidences of airleak syndromes and BPD; moreover a higher treatment threshold (FIO2 at study > 0.45) was associated with increased risk of PDA. These data suggest that treatment with surfactant by transient intubation using a low treatment threshold (FIO2 < 0.45) is preferable to later, selective surfactant therapy by transient intubation using a higher threshold for study entry (FIO2 > 0.45) or at the time of respiratory failure and initiation of mechanical ventilation" |
| Stewart A, Inglis GDT, Jardine LA, Koorts P, Davies MW. Prophylactic antibiotics to reduce morbidity and mortality in newborn infants with intercostal catheters. Cochrane Database of Systematic Reviews 2012, Issue 4. | Secondary outcomes pre‐specified include:
| No included trials "There are no data from randomised trials to either support or refute the use of antibiotic prophylaxis for intercostal catheter insertion in neonates. Any randomised controlled trials of antibiotic prophylaxis would need to account for the fact that neonates who require insertion of an intercostal catheter may already be receiving antibiotics for other indications" |
| Subramaniam P, Ho JJ, Davis PG. Prophylactic nasal continuous positive airway pressure for preventing morbidity and mortality in very preterm infants. Cochrane Database of Systematic Reviews 2016, Issue 6. | Secondary outcomes pre‐specified include:
| "There is insufficient evidence to evaluate prophylactic CPAP compared to oxygen therapy and other supportive care. However when compared to mechanical ventilation prophylactic nasal CPAP in very preterm infants reduces the need for mechanical ventilation and surfactant and also reduces the incidence of BPD and death or BPD" |
| Tan K, Lai NM, Sharma A. Surfactant for bacterial pneumonia in late preterm and term infants. Cochrane Database of Systematic Reviews 2012, Issue 2. | Secondary outcomes pre‐specified include:
| No included trials "There is no evidence from randomised controlled trials (RCTs) to support or refute the efficacy of surfactant in near‐term and term infants with proven or suspected bacterial pneumonia. RCTs are still required to answer this question" |
| Thayyil S, Milligan D. Single versus double volume exchange transfusion in jaundiced newborn infants. Cochrane Database of Systematic Reviews 2006, Issue 4. | Primary outcomes pre‐specified include:
Secondary outcomes pre‐specified include:
| "There was insufficient evidence to support or refute the use of single volume exchange transfusion as opposed to double volume exchange transfusion in jaundiced newborns. A change from the current practice of double volume exchange transfusions for severe jaundice in newborns infant, cannot be recommended on current evidence" |
| Vasudevan C, Oddie SJ, McGuire W. Early removal versus expectant management of central venous catheters in neonates with bloodstream infection. Cochrane Database of Systematic Reviews 2016, Issue 4. | Primary outcomes pre‐specified include:
| No included trials "There are no trial data to guide practice regarding early removal versus expectant management of central venous catheters in newborn infants with bloodstream infections. A simple and pragmatic randomised controlled trial is needed to resolve the uncertainty about optimal management in this common and important clinical scenario" |
| Verner AM, McGuire W, Craig JS. Effect of taurine supplementation on growth and development in preterm or low birth weight infants. Cochrane Database of Systematic Reviews 2007, Issue 4. | Secondary outcomes pre‐specified include:
| "Despite that lack of evidence of benefit from randomised controlled trials, it is likely that taurine will continue to be added to formula milks and parenteral nutrition solutions used for feeding preterm and low birth weight infants given the putative association of taurine deficiency with various adverse outcomes. Further randomised controlled trials of taurine supplementation versus no supplementation in preterm or low birth weight infants are unlikely to be viewed as a research priority, but there may be issues related to dose or duration of supplementation in specific subgroups of infants that merit further research" |
| Watson J, McGuire W. Responsive versus scheduled feeding for preterm infants. Cochrane Database of Systematic Reviews 2016, Issue 8. | Secondary outcomes pre‐specified include:
| "Overall, the data do not provide strong or consistent evidence that responsive feeding affects important outcomes for preterm infants or their families. Some (low quality) evidence exists that preterm infants fed in response to feeding and satiation cues achieve full oral feeding earlier than infants fed prescribed volumes at scheduled intervals. This finding should be interpreted cautiously because of methodological weaknesses in the included trials. A large RCT would be needed to confirm this finding and to determine if responsive feeding of preterm infants affects other important outcomes" |
| Wilkinson D, Andersen C, O'Donnell CPF, De Paoli AG, Manley BJ. High flow nasal cannula for respiratory support in preterm infants. Cochrane Database of Systematic Reviews 2016, Issue 2. | Secondary outcomes pre‐specified include:
| "HFNC has similar rates of efficacy to other forms of non‐invasive respiratory support in preterm infants for preventing treatment failure, death and CLD. Most evidence is available for the use of HFNC as post‐extubation support. Following extubation, HFNC is associated with less nasal trauma, and may be associated with reduced pneumothorax compared with nasal CPAP. Further adequately powered randomised controlled trials should be undertaken in preterm infants comparing HFNC with other forms of primary non‐invasive support after birth and for weaning from non‐invasive support. Further evidence is also required for evaluating the safety and efficacy of HFNC in extremely preterm and mildly preterm subgroups, and for comparing different HFNC devices" |
| Wong V, Cheuk DKL, Chu V. Acupuncture for hypoxic ischemic encephalopathy in neonates. Cochrane Database of Systematic Reviews 2013, Issue 1. | Primary outcomes pre‐specified include:
| No included trials "The rationale for acupuncture in neonates with HIE is unclear and the evidence from randomized controlled trial is lacking. Therefore, we do not recommend acupuncture for the treatment of HIE in neonates. High quality randomized controlled trials on acupuncture for HIE in neonates are needed" |
| Woodgate PG, Flenady V, Steer PA. Intramuscular penicillin for the prevention of early onset group B streptococcal infection in newborn infants. Cochrane Database of Systematic Reviews 2004, Issue 2. | Secondary outcomes pre‐specified include:
| "This review does not support the routine use of intramuscular penicillin to prevent EOGBSD in newborn infants. There is a discrepancy between this finding and the results of a number of larger non‐randomised trials. Explanations for this are proposed. There is a need for this intervention to be tested as a component of the existing prevention strategies in widespread use" |
| Young L, Embleton ND, McCormick FM, McGuire W. Multinutrient fortification of human breast milk for preterm infants following hospital discharge. Cochrane Database of Systematic Reviews 2013, Issue 2. | Primary outcomes pre‐specified include:
| "The limited available data do not provide convincing evidence that feeding preterm infants with multinutrient fortified breast milk compared with unfortified breast milk following hospital discharge affects important outcomes including growth rates during infancy. There are no data on long‐term growth. Since fortifying breast milk for infants fed directly from the breast is logistically difficult and has the potential to interfere with breast feeding, it is important to determine if mothers would support further trials of this intervention" |
| Young L, Morgan J, McCormick FM, McGuire W. Nutrient‐enriched formula versus standard term formula for preterm infants following hospital discharge. Cochrane Database of Systematic Reviews 2012, Issue 3. | Primary outcomes pre‐specified include:
| "Current recommendations to prescribe "post‐discharge formula" for preterm infants following hospital discharge are not supported by the available evidence. Some limited evidence exists that feeding preterm infants following hospital discharge with "preterm formula" (which is generally only available for in‐hospital use) may increase growth rates up to 18 months corrected age" |
| Ziino AJA, Davies MW, Davis PG. Epinephrine for the resuscitation of apparently stillborn or extremely bradycardic newborn infants. Cochrane Database of Systematic Reviews 2002, Issue 3. | Primary outcomes pre‐specified include:
Secondary outcomes pre‐specified include:
| No included trials "No randomised, controlled trials evaluating the administration of epinephrine to the apparently stillborn or extremely bradycardic newborn infant were found. Similarly, no randomised, controlled trials that addressed the issues of optimum dosage and route of administration of epinephrine were found. Current recommendations for the use of epinephrine in newborn infants are based only on evidence derived from animal models and the human adult literature. Randomised trials in neonates are urgently required to determine the role of epinephrine in this population" |
Abbreviations: AN/AD: Auditory Neuropathy/Auditory Dyssynchrony; anti‐VEGF: anti‐vascular endothelial growth factor; BIND: bilirubin‐induced neurological dysfunction; BP: blood pressure; BPD: bronchopulmonary dysplasia; BSID: Bayley Scales of Infant Development; CDP: continuous distending pressure; CGA: corrected gestational age; CLD: chronic lung disease; CO2: carbon dioxide; CPAP: continuous positive airway pressure; CRBSI: catheter‐related bloodstream infection; DQ: developmental quotient; ELBW: extremely low birthweight; EOGBSD: early‐onset group B streptococcus disease; ETT: endotracheal tube; FIO2: fraction of inspired oxygen; GMDS: Griffith Mental Development Scales; GMFCS: Gross Motor Function Classification System; HFNC: high‐flow nasal cannula; HIE: hypoxic‐ischaemic encephalopathy; iNO: inhaled nitric oxide; IPPV: intermittent positive‐pressure ventilation; IQ; intelligence quotient; IVH: intraventricular haemorrhage; LMA: laryngeal mask airway; MDI: Mental Development Index; Movement ABC: Movement Assessment Battery for Children; MV mechanical ventilation; NCPAP: nasal continuous positive airway pressure; NEC: necrotising enterocolitis; PDA: patent ductus arteriosus; PDI: Psychomotor Development Index; PET: partial exchange transfusion; PIE: pulmonary interstitial emphysema; PPHN: persistent pulmonary hypertension of the newborn; PPV: positive‐pressure ventilation; RBCs: red blood cells; RCT: randomised controlled trial; RDS: respiratory distress syndrome; rhAPC: recombinant human activated protein C; ROP: retinopathy of prematurity; S‐B: Stanford–Binet; SD: standard deviation; TGI: tracheal gas insufflation; UVCs: umbilical venous catheters; VA: visual acuity; VLBW: very low birthweight.
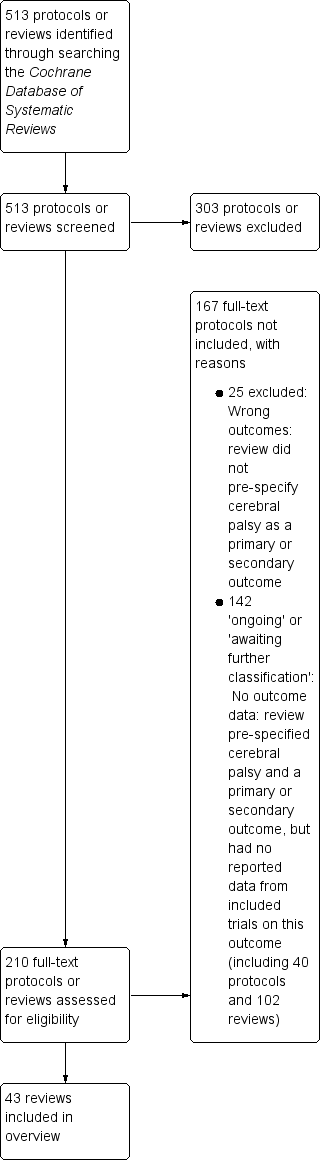
Study flow diagram.
| Review ID and title | Reason for exclusion |
| Email for clinical communication between patients/caregivers and healthcare professionals | Wrong participants (not neonates):
|
| Parent‐infant psychotherapy for improving parental and infant mental health | Wrong participants (not neonates):
|
| Body positioning for spontaneously breathing preterm infants with apnoea | Secondary outcomes pre‐specified include the following:
No outcome data for these outcomes |
| C‐reactive protein for diagnosing late‐onset infection in newborn infants | Protocol for diagnostic test accuracy review |
| G‐CSF and GM‐CSF for treating or preventing neonatal infections | Secondary outcomes pre‐specified include:
No outcome data for cerebral palsy (single study results reported "cognition, language and social developmental performance scores were within the normal range for age and motor deficits were 'typical of high‐risk, low birth weight neonates'. However there was no comparison made between G‐CSF and control infants" |
| Intravenous dexamethasone for extubation of newborn infants | No pre‐specified outcome focused on development/disability at follow‐up |
| High‐frequency jet ventilation vs high‐frequency oscillatory ventilation for pulmonary dysfunction in preterm infants | Secondary neonatal outcomes pre‐specified include:
No outcome data for this outcome (no included trials) |
| Treatment of infantile spasms | Outcomes pre‐specified include:
No outcome data for cerebral palsy (single‐study results reported related to BSID; VABS; 'cognitive development'; Japanese Tumor Scale; DDST) |
| Antiviral therapy for symptomatic congenital cytomegalovirus infection in neonates and infants up to 3 months of age | Protocol Primary outcomes pre‐specified include:
|
| Lay health workers in primary and community health care for maternal and child health and management of infectious diseases | No pre‐specified outcome focused on development/disability at follow‐up |
| Surgical vs medical treatment with cyclo‐oxygenase inhibitors for symptomatic patent ductus arteriosus in preterm infants | Secondary outcomes pre‐specified include:
No outcome data for this outcome |
| Cycled light in the intensive care unit for preterm and low birthweight infants | Secondary outcomes pre‐specified include:
No outcome data for these outcomes |
| Transcutaneous screening for hyperbilirubinaemia in neonates | Protocol No pre‐specified outcome focused on development/disability at follow‐up |
| Granulocyte transfusions for neonates with confirmed or suspected sepsis and neutropaenia | Primary outcomes pre‐specified include:
No outcome data for this outcome |
| Molecular assays for diagnosis of sepsis in neonates | Protocol for diagnostic test accuracy review |
| Pentoxifylline for treatment of sepsis and necrotising enterocolitis in neonates | Secondary outcomes pre‐specified include:
No outcome data for this outcome |
| Hypothermia for neuroprotection in children after cardiopulmonary arrest | Primary outcomes pre‐specified include:
No outcome data for these outcomes (no included trials) |
| Intraventricular antibiotics for bacterial meningitis in neonates | Secondary outcomes pre‐specified include:
No outcome data for this outcome |
| Metalloporphyrins for treatment of unconjugated hyperbilirubinaemia in neonates | Outcomes pre‐specified include:
No outcome data for these outcomes |
| Periodic change of body position under phototherapy in term and late preterm neonates with hyperbilirubinaemia | Protocol Secondary outcomes pre‐specified include:
|
| Short‐duration vs standard‐duration antibiotic regimens for treatment of neonatal bacterial infection | Protocol Secondary outcomes pre‐specified include:
|
| Steroid therapy for meconium aspiration syndrome in newborn infants | Primary outcomes pre‐specified include:
No outcome data for this outcome |
| Diuretic therapy for newborn infants with post‐haemorrhagic ventricular dilatation | Outcomes pre‐specified include:
Data reported for these outcomes; no outcome data for cerebral palsy. "The larger trial showed that acetazolamide and furosemide treatment resulted in a borderline increase in the risk for motor impairment at one year (RR 1.27, 95% CI 1.02 ‐ 1.58; RD 0.16, 95% CI 0.02 ‐ 0.31), but did not significantly affect the risk for the combined outcome of delay, disability or motor impairment among survivors, or the risk of the combined outcome of death, delay, disability or impairment at one year" |
| Repeated lumbar or ventricular punctures in newborns with intraventricular haemorrhage | Outcomes pre‐specified include:
Data reported for these outcomes; no outcome data for cerebral palsy. "The tables and figures show that none of the trials found a significant effect of CSF tapping on a) need for shunt b) death c) major disability in survivors d) multiple disability in survivors e) death or disability. Similarly, meta‐analysis of the results of all included trials shows no significant effect of CSF tapping on any of these outcomes" |
| Permissive hypercapnia for prevention of morbidity and mortality in mechanically ventilated newborn infants | Outcomes pre‐specified include:
No outcome data for this outcome |
| Abbreviations: BIND: bilirubin‐induced neurological dysfunction; BSID: Bayley Scales of Infant Development; CI: confidence interval; CSF: cerebrospinal fluid; DDST: Denver Developmental Screening Test; G‐CSF: granulocyte‐colony stimulating factor; GM‐CSF: granulocyte‐macrophage colony‐stimulating factor; RD: risk difference; RR: risk ratio; VABS: Vineland Adaptive Behavior Scales. | |
| Review ID and title | Date of search and date assessed as up‐to‐date | No. included trials (countries and publication years) | No. participants in included trials | Inclusion criteria for 'Types of participants' | Relevant comparison interventions (no. trials and participants) | Overview outcomes for which data were reported (no. trials and participants) |
| Neonatal care: asphyxia | ||||||
| Allopurinol for preventing mortality and morbidity in newborn infants with hypoxic‐ischaemic encephalopathy | Searches: March 2012 Up‐to‐date: | 3 RCTs (Countries: Netherlands, Turkey; Published: 1990s: 1 RCT; 2000s: 2 RCTs) | 114 infants | Newborn infants (> 34 weeks' gestation) with hypoxic‐ischaemic encephalopathy defined as clinical evidence of cardiorespiratory or neurological depression (Apgar score < 7 at 5 minutes and beyond after birth) and/or evidence of severe metabolic acidosis in intrapartum foetal, umbilical arterial cord, or very early neonatal blood samples (pH < 7 or base deficit > 12 mmol/L), and/or clinical or electro‐encephalographic (multi‐channel or amplitude integrated) evidence of neonatal encephalopathy (MacLennan 1999) | Allopurinol vs control (3 RCTs, 114 neonates) | Severity of cerebral palsy ("Severe quadriplegia in surviving infants" (3 RCTs, 73 children); reported as a primary outcome) Other composite outcome that includes cerebral palsy as a component ("Death or severe neurodevelopmental disability in survivors" (3 RCTs, 110 children); reported as a primary outcome) |
| Cooling for newborns with hypoxic‐ischaemic encephalopathy | 1 May 2012 | 11 RCTs (Countries: China: 2 RCTs; New Zealand: 1 RCT; Turkey: 1 RCT; USA; 3 RCTs; international: 4 RCTs Published: 1990s: 1 RCT; 2000s: 7 RCTs; 2010s: 3 RCTs) | 1505 infants | 1. Newborn infants of 35 weeks' gestation or greater 2. Evidence of peripartum asphyxia, with each enrolled infant satisfying at least 1 of the following criteria: a. Apgar score of 5 or less at 10 minutes b. Mechanical ventilation or resuscitation at 10 minutes c. Cord pH < 7.1, or arterial pH < 7.1, or base deficit of 12 or more within 60 minutes of birth 3. Evidence of encephalopathy according to Sarnat staging (Finer 1981; Sarnat 1976): a. Stage 1 (mild): hyperalertness, hyper‐reflexia, dilated pupils, tachycardia, absence of seizures b. Stage 2 (moderate): lethargy, hyper‐reflexia, miosis, bradycardia, seizures, hypotonia with weak suck and Moro c. Stage 3 (severe): stupor, flaccidity, small to mid position pupils that react poorly to light, decreased stretch reflexes, hypothermia, and absent Moro No major congenital abnormalities recognisable at birth | Therapeutic hypothermia vs standard care (11 RCTs, 1505 neonates) | Cerebral palsy ("Cerebral palsy in survivors assessed" (7 RCTs, 881 children) and "Outcome at 6 to 7 years of age: Cerebral palsy" (1 RCT, 121 children); reported as secondary outcomes) Other composite outcomes that include cerebral palsy as a component ("Death or major disability in survivors assessed" (8 RCTs, 1344 children); reported as a primary outcome) ("Major neurodevelopmental disability" (8 RCTs, 1344 children); "Major neurodevelopmental disability in survivors assessed" (8 RCTs, 917 children); "Outcome at 6 to 7 years of age: death or moderate‐to‐severe disability" (1 RCT, 190 children); "Outcome at 6 to 7 years of age: moderate‐to‐severe disability" (1 RCT, 119 children); reported as secondary outcomes) Motor dysfunction ("Neuromotor delay (BSID PDI more than 2 SD below mean) in survivors assessed" (6 RCTs, 657 children); reported as a secondary outcome) |
| Prophylactic barbiturate use for the prevention of morbidity and mortality following perinatal asphyxia | 30 November 2015 | 9 RCTs (Countries: Finland: 1 RCT; India: 2 RCTs; Mexico: 1 RCT; Romania: 1 RCT; South Africa: 1 RCT; Spain: 1 RCT; USA: 2 RCTs; Published: 1980s: 2 RCTs; 1990s: 2 RCTs; 2000s: 2 RCTs; 2010s: 3 RCTs) | 456 infants |
| Barbiturates vs control (8 RCTs, 439 neonates) | Cerebral palsy ("Cerebral palsy" (2 RCTs, 69 children); reported as a secondary outcome) Other composite outcomes that include cerebral palsy as a component ("Death or major neurodevelopmental disability" (1 RCT, 31 children); reported as a primary outcome) ("Major neurodevelopmental disability" (1 RCT, 31 children); reported as a secondary outcome) |
| Neonatal care: haemorrhage: periventricular/intraventricular | ||||||
| Ethamsylate for the prevention of morbidity and mortality in preterm or very low birth weight infants | Search: 24 August 2009 Up‐to‐date: 22 September 2009 | 7 RCTs (Countries: France, Greece, UK: 1 RCT; India: 1 RCT; Switzerland: 1 RCT; Taiwan: 1 RCT; Turkey: 1 RCT; UK: 2 RCTs; Published: 1980s: 3 RCTs; 1990s: 4 RCTs) | 1410 infants | Preterm infants born before and including 34 weeks plus 6 days' completed gestation or with birthweight < 2000 g | Ethamsylate vs placebo (7 RCTs, 1410 neonates) | Cerebral palsy ("Cerebral palsy in surviving children available for follow‐up" (3 RCTs, 532 children); reported as a primary outcome) Other composite outcomes that include cerebral palsy as a component ("Neurodevelopmental disability at 2 years of age in surviving children available for follow‐up" (3 RCTs, 532 children); "Death or any disability by 2 years of age in children with known outcome at any point in time" (7 RCTs, 1334 children); reported as primary outcomes) |
| Postnatal phenobarbital for the prevention of intraventricular haemorrhage in preterm infants | Search: 31 October 2012 Up‐to‐date: 17 December 2012 | 12 RCTs (Countries: not reported; Published: 1980s: 8 RCTs; 1990s: 1 RCT: 2000s: 3 RCTs) | 982 infants | Newborn infants (less than 24 hours old) with gestational age < 34 weeks or birthweight < 1500 g. We included preterm infants with gestational age 33 to 36 weeks or birthweight up to 1750 g, if they were mechanically ventilated. We excluded infants with serious congenital malformations | Phenobarbital vs control (12 RCTs, 982 neonates) | Other composite outcomes that include cerebral palsy as a component ("Mild neurodevelopmental impairment" (1 RCT, 101 children); "Severe neurodevelopmental impairment" (1 RCT, 101 children); reported as secondary outcomes) |
| Neonatal care: hypotension | ||||||
| The effect of inotropes on morbidity and mortality in preterm infants with low systemic or organ blood flow | 19 May 2010 | 1 RCT (Country: not reported; Published: 2000s) | 42 infants | Preterm infants (< 37 weeks' gestational age) with low SBF or organ blood flow in the neonatal period. Low SBF may be determined on the basis of echocardiographically measured ventricular outputs or surrogates for SBF such as SVC flow. Low organ blood flow may be determined on the basis of techniques including ultrasound Doppler, near infrared spectroscopy, or xenon clearance techniques when evidence in the literature suggests that measurement is associated with substantial clinical outcomes and/or actual organ blood flow. The review does not include studies that include surrogates of flow such as BP, ultrasound Doppler‐measured velocities, pulsatility, or resistive indices | Dobutamine vs dopamine in preterm infants with low superior vena cava flow (1 RCT, 42 neonates) | Cerebral palsy ("Cerebral palsy at 3 years in survivors assessed" (1 RCT, 13 children); reported as a primary outcome) Other composite outcomes that include cerebral palsy as a component ("Disability at 3 years in survivors assessed" (1 RCT, 13 children); "Death or disability at 3 years" (1 RCT, 37 children); "Death or disability at latest follow‐up" (1 RCT, 41 children); reported as primary outcomes) |
| Neonatal care: fluid therapy | ||||||
| Early volume expansion for prevention of morbidity and mortality in very preterm infants | 30 July 2008 | 8 RCTs (Countries: not reported; Published: 1970s: 1 RCT; 1980s: 1 RCT; 1990s: 4 RCTs; 2000s: 2 RCTs) | 1185 infants | Very preterm infants born ≦ 32 weeks' gestation or ≦ 1500 g and enrolled and treated the first 72 hours after birth. Trials were eligible if they enrolled unselected preterm infants, preterm infants with clinically suspected poor perfusion (e.g. low BP, poor cutaneous perfusion, metabolic acidosis), or preterm infants with low blood flow (e.g. determined by Doppler ultrasound). Low BP may be defined as BP less than a specified percentile of a standard chart, mean BP ≦ 30 mmHg in any preterm infant, or mean BP ≦ 1 mmHg per week of gestation | Volume vs no treatment in very preterm infants (5 RCTs, 978 neonates) Gelatin vs fresh frozen plasma in hypotensive infants (1 RCT, 519 neonates) | Cerebral palsy ("Cerebral palsy in survivors" (1 RCT, 604 children; and 1 RCT, 399 children); reported as a primary outcome) Other composite outcomes that include cerebral palsy as a component ("Severe neurodevelopmental disability in survivors" (1 RCT, 604 children; and 1 RCT, 399 children); "Death or severe neurodevelopmental disability" (1 RCT, 776 children; and 1 RCT, 518 children); reported as primary outcomes) |
| Neonatal care: patent ductus arteriosus | ||||||
| Prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants | Searches: April 2010 Up‐to‐date: | 19 RCTs (Countries: North America: 13 RCTs; Latin America, Europe, Asia: 6 RCTs; Published: 1980s: 11 RCTs; 1990s: 7 RCTs; 2000s; 1 RCT) | 2872 infants | Preterm neonates (less than 37 weeks' completed gestation) | Prophylactic IV indomethacin vs placebo or no drug (19 RCTs, 2872 neonates) | Cerebral palsy ("Neurological assessments (18‐54 months: Cerebral palsy" (4 RCTs, 1372 children); "School age neurological assessments: Cerebral palsy aged 8 years" (1 RCT, 304 children); reported as primary outcomes) Other composite outcome that includes cerebral palsy as a component ("Death or severe neurosensory impairment" (3 RCTs, 1491 children); reported as a primary outcome) |
| Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants | 7 May 2014 | 33 RCTs (Countries: Albania: 1 RCT; Belgium: 2 RCTs; Czech Republic: 1 RCT; China: 1 RCT; Egypt: 1 RCT; India: 1 RCT; Iran: 3 RCTs; Israel: 1 RCT; Italy: 6 RCTs; Poland: 1 RCT; Qatar: 1 RCT; Spain: 2 RCTs; Taiwan: 2 RCTs; Thailand: 2 RCTs; Tunisia: 1 RCT; Turkey: 3 RCTs; UK: 2 RCTs; USA: 2 RCTs; Published: 1990s: 4 RCTs; 2000s: 18 RCTs; 2010s: 11 RCTs) | 2190 infants | Preterm infants less than 37 weeks' gestational age or LBW infants (less than 2500 g) with PDA diagnosed either clinically or by echocardiographically (ECHO) guided criteria in the neonatal period (less than 28 days) | Oral ibuprofen vs IV ibuprofen (data for maximum of 4 RCTs, 304 neonates) | Cerebral palsy ("Moderate/severe cerebral palsy at 18‐24 months" (1 RCT, 57 children); reported as a secondary outcome) |
| Neonatal care: blood disorders | ||||||
| Early erythropoietin for preventing red blood cell transfusion in preterm and/or low birth weight infants | 1 July 2013 | 27 RCTs (Countries: Austria: 2 RCTs; Bangladesh: 1 RCT; Chile: 1 RCT; China: 2 RCTs; Greece: 3 RCTs; Iran: 1 RCT; Italy: 2 RCTs; Mexico: 1 RCT; New Zealand: 1 RCT; Poland: 1 RCT; Singapore: 1 RCT; South Africa: 1 RCT; Switzerland: 1 RCT; Turkey: 1 RCT; USA: 5 RCTs; Europe: 3 RCTs; Published 1990s: 12 RCTs; 2000s: 13 RCTs; 2010s: 2 RCTs) | 2209 infants | Preterm (< 37 weeks) and/or LBW (< 2500 g) neonates less than 8 days of age | Erythropoietin vs placebo or no treatment (27 RCTs, 2209 neonates) Darbepoetin alfa vs placebo or no treatment (1 RCT, 66 neonates) | Cerebral palsy ("Cerebral palsy at 18 ‐ 22 months' corrected age (in children examined)" (2 RCTs, 153 children; and 1 RCT, 51 children); reported as secondary outcomes) Other composite outcome that includes cerebral palsy as a component ("Any neurodevelopmental impairment at 18‐22 months' corrected age (in children examined)" (1 RCT< 99 children); reported as a secondary outcome) Motor dysfunction ("PDI < 70 at 18 ‐ 22 months' corrected age (in children examined)" (1 RCT, 90 children); reported as a secondary outcome) |
| Low versus high haemoglobin concentration threshold for blood transfusion for preventing morbidity and mortality in very low birth weight infants | Search: August 2011 Up‐to‐date: 1 September 2011 | 5 RCTs (Countries: Canada: 1 RCT; International (Canada, USA, Australia): 1 RCT; Taiwan: 1 RCT; USA: 2 RCTs; Published: 1980s: 1 RCT; 1990s: 1 RCT; 2000s: 3 RCTs) | 670 infants | VLBW infants (i.e. of birthweight less than or equal to 1500 g, or less than 32 weeks' gestational age) admitted to NICU at less than 1 week of age. We aimed specifically to include studies of infants receiving all levels of intensive care | Transfusion at a low haemoglobin or haematocrit level (restrictive) vs transfusion at a high haemoglobin or haematocrit level (liberal) (4 RCTs, 614 neonates) | Cerebral palsy ("Neurosensory impairment at 18‐21 months' follow‐up among survivors: Cerebral palsy" (1 RCT, 335 children); reported as a secondary outcome) Other composite outcomes that include cerebral palsy as a component ("Death or severe morbidity: at 18‐21 months' follow‐up with MDI < 70" (1 RCT, 421 children); "Death or severe morbidity: at 18‐21 months' follow‐up with MDI < 85" (1 RCT, 421 children); reported as primary outcomes) ("Neurosensory impairment at 18‐21 months' follow‐up among survivors: any neurosensory impairment" (1 RCT, 328 children); reported as a secondary outcome) |
| Neonatal care: pulmonary hypertension | ||||||
| Endothelin receptor antagonists for persistent pulmonary hypertension in term and late preterm infants | 28 December 2015 | 2 RCTs (Countries: Saudi Arabia: 1 RCT; unclear (multi‐centre): 1 RCT; Published: 2010s: 2 RCTs) | 68 infants | Late preterm infants (born at 34+0 to 36+6 weeks), term infants (born at 37+0 to 41+6 weeks), and post‐term infants (i.e. born after 41+6 weeks' gestation) until post‐menstrual age (PMA) up to 44 weeks with PPHN were eligible for inclusion. The diagnosis of PPHN was clinical or was based on echocardiography. Clinical diagnosis of PPHN was considered when there was hypoxaemia refractory to oxygen therapy and mechanical ventilation (Roberts 1997). The echocardiographic diagnosis of PPHN was made by demonstrating the presence of extrapulmonary right‐to‐left shunting at the ductal or atrial level, near or suprasystemic pulmonary arterial pressures, and doppler evidence of tricuspid regurgitation (Dhillon 2012; Stayer 2010) | Endothelin receptor antagonists vs placebo (1 RCT, 47 neonates) | Cerebral palsy ("Cerebral palsy" (1 RCT, 37 children); reported as a secondary outcome) Motor dysfunction ("Adverse neurodevelopmental outcome at 6 months" (1 RCT, 37 children); reported as a secondary outcome) |
| Neonatal care: resuscitation | ||||||
| Air versus oxygen for resuscitation of infants at birth | Search: December 2003/January 2004 Up‐to‐date: 15 February 2005 | 5 RCTs (Countries: India: 1 RCT; 6 countries: 1 RCT; not reported: 3 RCTs Published: 1990s: 2 RCTs; 2000s: 3 RCTs) | 1302 infants | Term or preterm neonates requiring IPPV at birth | Room air vs 100% oxygen (5 RCTs, 1302 neonates) | Cerebral palsy ("Long‐term neurodevelopmental outcome: cerebral palsy in those followed up at 18‐24 months" (1 RCT, 213 children); reported as a post hoc outcome) Motor dysfunction ("Long‐term neurodevelopmental outcome: not walking in those followed up at 18‐24 months" (1 RCT, 213 children); reported as a post hoc outcome) |
| Neonatal care: nitric oxide | ||||||
| Inhaled nitric oxide for respiratory failure in preterm infants | Search: June 2010 Up‐to‐date: 12 October 2010 | 14 RCTs (Countries: Europe: 3 RCTs; Taiwan: 1 RCT; USA: 1 RCT; not reported/unclear: 9 RCTs Published: 1990s: 3 RCTs; 2000s: 11 RCTs) | 3430 infants | Premature infants (less than 35 weeks' gestation) with respiratory failure after adequate treatment with surfactant | Inhaled NO compared with control; analyses conducted based on:
| Cerebral palsy ("Cerebral palsy"; reported as an outcome (2 RCTs, 209 children; 2 RCTs, 498 children; and 2 RCTs, 593 children) (not separated into primary/secondary)) Other composite outcome that includes cerebral palsy as a component ("Neurodevelopmental disability" (2 RCTs, 208 children; 2 RCTs, 498 children; and 2 RCTs, 593 children); reported as an outcome (not separated into primary/secondary)) Motor dysfunction ("Bayley MDI or PDI <‐2SD" (1 RCT, 138 children); reported as an outcome (not separated into primary/secondary)) |
| Nitric oxide for respiratory failure in infants born at or near term | Search: November 2005 Up‐to‐date: | 14 RCTs (Countries: 33 French and Belgian Units: 1 RCT; not reported: 13 RCTs Published: 1990s: 11 RCTs; 2000s: 3 RCTs) | 1715 infants | Newborn infants (< 1 month of age) with hypoxaemia suspected to be due to lung disease, pulmonary hypertension with right‐to‐left shunting, or both Only studies in term and near‐term infants (> 34 weeks' gestation) were included Efforts were made in all studies to exclude infants with intracardiac shunting due to structural congenital heart disease Infants with diaphragmatic hernia may respond differently from other near term infants (from preliminary data), and as far as possible results from infants with diaphragmatic hernias have been evaluated separately | Inhaled NO vs control (10 RCTs, 1068 infants) Inhaled NO vs control in infants with diaphragmatic hernia (2 RCTs, 84 neonates) | Cerebral palsy ("Cerebral palsy among survivors" (2 RCTs, 299 children; and 1 RCT, 22 children); reported as an outcome (not separated into primary/secondary)) Other composite outcome that includes cerebral palsy as a component ("Neurodevelopmental disability at 18 to 24 months among survivors" (2 RCTs, 301 children); reported as an outcome (not separated into primary/secondary)) Motor dysfunction ("Bayley PDI more than 2 SD below the mean" (2 RCTs, 283 children); reported as an outcome (not separated into primary/secondary)) |
| Neonatal care: apnoea | ||||||
| Methylxanthine treatment for apnoea in preterm infants | Search: Up‐to‐date: | 6 RCTs (Countries: not reported Published: 1980s: 3 RCTs; 1990s: 1 RCT; 2000s: 2 RCTs) | 959 infants | Preterm infants with recurrent apnoea. There must have been an effort to exclude specific secondary causes of apnoea | Any methylxanthine vs control (placebo or no drug therapy) (6 RCTs, 959 neonates) | Cerebral palsy ("Cerebral palsy" (1 RCT, 729 children); reported as a secondary outcome) Other composite outcome that includes cerebral palsy as a component ("Death or major disability by late infancy" (1 RCT, 767 children); reported as a secondary outcome) |
| Prophylactic methylxanthine for prevention of apnoea in preterm infants | Search: August 2010 Up‐to‐date: 29 September 2010 | 3 RCTs (Countries: not reported Published: 1980s: 2 RCTs; 2000s: 1 RCT) | 557 infants | Preterm infants, particularly those born at less than 34 weeks' gestation, who are at risk of developing recurrent apnoea, bradycardia, and hypoxic episodes | Prophylactic methylxanthine vs control (3 RCTs, 557 neonates) | Cerebral palsy ("Cerebral palsy" (1 RCT, 415 children); reported as a secondary outcome) Other composite outcome that includes cerebral palsy as a component ("Death or major disability" (1 RCT, 423 children); reported as a secondary outcome) |
| Neonatal care: respiratory distress syndrome | ||||||
| Inositol in preterm infants at risk for or having respiratory distress syndrome | 14 September 2014 | 4 RCTs (Countries: Finland: 2 RCTs; USA: 2 RCTs Published: 1980s: 1 RCT; 1990s: 2 RCTs; 2010s: 1 RCT) | 429 infants | Preterm infants (< 37 weeks' post‐menstrual age) or LBW (< 2500 g) infants | Inositol supplementation (repeat doses) vs control (3 RCTs, 355 neonates) | Other composite outcomes that include cerebral palsy as a component ("Major neural developmental impairment at one year corrected age" (1 RCT, 169 children); reported as a secondary outcome) Motor dysfunction ("Minor neural developmental impairment at one year corrected age" (1 RCT, 169 children); reported as a secondary outcome) |
| Animal derived surfactant extract for treatment of respiratory distress syndrome | Search: December 2008 Up‐to‐date: 13 February 2009 | 13 RCTs (Countries: not reported Published: 1980s: 7 RCTs; 1990s: 6 RCTs) | 1611 infants | Preterm infants (< 37 weeks' gestation) with clinical and/or radiological evidence of respiratory distress syndrome requiring assisted ventilation | Animal‐derived surfactant extract treatment of respiratory distress (all infants) (13 RCTs, 1611 neonates) | Cerebral palsy ("Cerebral palsy" (1 RCT, 73 children); reported as a secondary outcome) Other composite outcome that includes cerebral palsy as a component ("Major neurodevelopmental disability in survivors" (1 RCT, 73 children); reported as a secondary outcome) |
| Synthetic surfactant for respiratory distress syndrome in preterm infants | Search: Up‐to‐date: | 6 RCTs (Countries: not clearly reported; Canada/USA/both: 3 RCTs Published; 1980s: 1 RCT; 1990s: 5 RCTs) | 2358 infants | Neonates with clinical and radiological evidence of respiratory distress syndrome requiring assisted ventilation | Synthetic surfactant vs control (6 RCTs, 2358 neonates) | Cerebral palsy ("Cerebral palsy in survivors examined" (5 RCTs, 1557 children); reported as an outcome (not separated into primary/secondary)) Severity of cerebral palsy ("Moderate ‐ severe cerebral palsy in survivors examined" (5 RCTs, 1557 children); reported as an outcome (not separated into primary/secondary)) |
| Prophylactic protein free synthetic surfactant for preventing morbidity and mortality in preterm infants | Search: September 2009 Up‐to‐date: 27 October 2009 | 7 RCTs (Countries: 1: UK; 6 RCTs: not reported Published: 1980s: 3 RCTs; 1990s: 4 RCTs) | 1583 infants | Premature infants with or without evidence of surfactant deficiency | Prophylactic synthetic surfactant vs control (7 RCTs, 1583 neonates) | Cerebral palsy ("Cerebral palsy, 1‐2 years" (4 RCTs, 670 children); reported as a secondary outcome) Severity of cerebral palsy ("Cerebral palsy, moderate/severe" (4 RCTs, 670 children); reported as a secondary outcome) |
| Neonatal care: mechanical ventilation | ||||||
| Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants | 30 November 2014 | 19 RCTs (Countries: not reported Published: 1980s: 1 RCT; 1990s: 6 RCTs; 2000s: 10 RCTs; 2010s: 2 RCTs) | 4096 infants | Preterm or LBW infants with pulmonary dysfunction, mainly due to respiratory distress syndrome, who were considered to require IPPV | High‐frequency oscillatory ventilation vs conventional ventilation (19 RCTs, 4096 neonates) | Cerebral palsy (reported in text as a secondary outcome (3 RCTs)) |
| Continuous distending pressure for respiratory distress in preterm infants | 30 April 2015 | 6 RCTs (Countries: not reported Published: 1970s: 4 RCTs; 1990s: 1 RCT; 2000s: 1 RCT) | 355 infants | Preterm infants with respiratory failure | Continuous distending pressure vs standard care (6 RCTs, 355 neonates) | Cerebral palsy ("Cerebral palsy" (1 RCT, 36 children); reported as a secondary outcome) Other composite outcomes that include cerebral palsy as a component ("Death or severe disability" (1 RCT, 38 children); "Severe disability" (1 RCT, 37 children); "Any disability" (1 RCT, 37 children); reported as secondary outcomes) |
| Prophylactic methylxanthines for endotracheal extubation in preterm infants | Search: Up‐to‐date: 16 August 2010 | 7 RCTs (Countries: not reported Published: 1980s: 3 RCTs; 1990s: 3 RCTs; 2000s: 1 RCT) | 916 infants | Preterm or LBW infants being weaned from IPPV | Methylxanthine vs control (7 RCTs, 914 neonates) | Cerebral palsy ("Cerebral palsy" (1 RCT, 644 children); reported as a secondary outcome) Other composite outcome that includes cerebral palsy as a component ("Death or major disability by 18‐21 months" (1 RCT, 676 children); reported as a secondary outcome) |
| Long versus short inspiratory times in neonates receiving mechanical ventilation | Search: Up‐to‐date: | 5 RCTs (Countries: not reported Published: 1980s: 3 RCTs; 19980s; 2 RCTs) | 694 infants | Term and preterm infants at less than 28 days of age and requiring conventional mechanical ventilation. No restrictions on underlying pathophysiology were applied | Long vs short inspiratory times (5 RCTs, 694 neonates) | Cerebral palsy ("Cerebral palsy in survivors less than 33 weeks' gestation at birth" (1 RCT, 177 children); reported as a secondary outcome) |
| Volume‐targeted versus pressure‐limited ventilation in the neonate | Search: January 2010 Up‐to‐date: | 12 RCTs (Countries: not reported Published: 1990s: 2 RCTs; 2000s: 10 RCTs) | 693 infants | All intubated infants of less than 28 days' corrected age who were being mechanically ventilated with IPPV at the time of study entry. Infants of all gestational ages and both paralysed and non‐paralysed infants were eligible | Volume‐targeted vs pressure‐limited ventilation (12 RCTs, 693 neonates) | Other composite outcomes that include cerebral palsy as a component ("Severe disability (any definition)" (2 RCTs, 209 children); "Severe disability (any definition) or death" (1 RCT, 109 children; reported as outcomes from post hoc meta‐analyses) Motor dysfunction ("Gross motor developmental issue (any definition)" (1 RCT, 128 children); reported as an outcome from a post hoc meta‐analysis) |
| Neonatal care: bronchopulmonary dysplasia | ||||||
| Early (< 8 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants | Search: August 2013 Up‐to‐date: 18 February 2014 | 29 RCTs (Countries: not reported Published: 1970s: 1 RCT; 1990s: 17 RCTs; 2000s: 10 RCTs; 2010s: 1 RCT) | 3750 infants | Preterm infants at risk of developing chronic lung disease, including those who were ventilator dependent | Early (< 8 days) postnatal corticosteroids vs control (29 RCTs, 3750 neonates) | Cerebral palsy ("Cerebral palsy" (12 RCTs, 1452 children); "Cerebral palsy in survivors assessed" (12 RCTs, 959 children); reported as primary outcomes) Cerebral palsy or death ("Death or cerebral palsy" (12 RCTs, 1452 children); reported as a primary outcome) Other composite outcomes that include cerebral palsy as a component ("Major neurosensory disability (variable criteria ‐ see individual studies)" (7 RCTs, 1233 children); "Major neurosensory disability (variable criteria) in survivors examined" (7 RCTs, 799 children); "Death or major neurosensory disability (variable criteria)" (7 RCTs, 1233 children); reported as primary outcomes) Motor dysfunction ("Bayley Psychomotor Developmental Index (PDI) <‐2SD" (3 RCTs, 842 children); "Bayley PDI <‐2SD in tested survivors" (3 RCTs, 528 children); reported as primary outcomes) |
| Moderately early (7‐14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants | Search: October 2002 Up‐to‐date: 11 November 2008 | 7 RCTs (Countries: not reported Published: 1980s: 1 RCT; 1990s: 6 RCTs) | 669 infants | Preterm babies developing chronic lung disease including those who were ventilator dependent | Moderately early (7‐14 days) postnatal corticosteroids vs control (7 RCTs, 659 neonates) | Cerebral palsy ("Cerebral palsy" (4 RCTs, 204 children); "Cerebral palsy in survivors assessed" (4 RCTs, 130 children); reported as review outcomes (not separated into primary and secondary)) Cerebral palsy or death ("Death or cerebral palsy" (4 RCTs, 204 children); reported as a review outcome) Other composite outcomes that include cerebral palsy as a component ("Major neurosensory disability (variable criteria ‐ see individual studies)" (2 RCTs, 96 children); "Major neurosensory disability (variable criteria) in survivors assessed" (2 RCTs, 56 children); "Death or major neurosensory disability (variable criteria)" (2 RCTs, 96 children); reported as review outcomes) |
| Late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants | Search: August 2013 Up‐to‐date: 18 February 2014 | 21 RCTs (Countries: Australia, Canada, New Zealand: 1 RCT; 6 countries: 1 RCT; not reported: 19 RCTs Published: 1980s: 5 RCTs; 1990s: 12 RCTs; 2000s: 3 RCTs; 2010s: 1 RCT) | 1424 infants | Preterm infants with evolving or established chronic lung disease, defined as oxygen‐dependent, ventilator‐dependent, or both, with or without radiographic changes of BPD | Late (> 7 days) postnatal corticosteroids vs control (21 RCTs, 1424 neonates) | Cerebral palsy ("Cerebral palsy: at 1 to 3 years" (14 RCTs, 876 children); "Cerebral palsy: at latest reported age" (15 RCTs, 855 children); "Cerebral palsy in survivors assessed: at 1 to 3 years" (14 RCTs, 631 children); "Cerebral palsy in survivors assessed: at latest reported age" (15 RCTs, 591 children); reported as primary outcomes) Cerebral palsy or death ("Death or cerebral palsy: at 1 to 3 years" (14 RCTs, 876 children); "Death or cerebral palsy: at latest reported age" (15 RCTs, 855 children); reported as primary outcomes) Other composite outcomes that include cerebral palsy as a component ("Major neurosensory disability (variable criteria ‐ see individual studies)" (8 RCTs, 655 children); "Major neurosensory disability (variable criteria) in survivors assessed" (8 RCTs, 480 children); "Death or major neurosensory disability (variable criteria)" (8 RCTs, 655 children); reported as primary outcomes) Motor dysfunction ("Bayley Psychomotor Developmental Index (PDI) < ‐2 SD" (1 RCT, 118 children); "Bayley PDI < ‐2 SD in survivors tested" (1 RCT, 90 children); reported as primary outcomes) |
| Early administration of inhaled corticosteroids for preventing chronic lung disease in ventilated very low birth weight preterm neonates | 29 July 2011 | 7 RCTs (Countries: Canada: 1 RCT; China: 1 RCT; Germany: 1 RCT; UK: 1 RCT; USA: 1 RCT; not reported: 2 RCTs Published: 1990s: 5 RCTs; 2000s: 2 RCTs) | 495 infants | Ventilator‐dependent preterm neonates with birthweight ≤ 1500 g and postnatal age < 2 weeks | Early inhaled steroids (< 2 weeks) vs placebo (7 RCTs, 495 neonates) | Cerebral palsy ("Cerebral palsy" (1 RCT, 56 children); reported as a secondary outcome) Motor dysfunction ("Mean developmental index on BSID‐II < 2 SD of the mean" (1 RCT, 56 children); reported as a secondary outcome) |
| Vitamin A supplementation to prevent mortality and short‐ and long‐term morbidity in very low birth weight infants | 1 May 2016 | 11 RCTs (Countries: Greece: 1 RCT; South Africa: 1 RCT; Thailand: 1 RCT; UK: 2 RCTs; USA: 6 RCTs Published: 1980s: 2 RCTs; 1990s: 4 RCTs; 2000s: 3 RCTs: 2010s: 2 RCTs) | 1580 infants | VLBW infants (defined as birthweight ≤ 1500 g or at less than 32 weeks' gestation) | Supplemental vitamin A vs no supplementation (10 RCTs, 1460 neonates) | Other composite outcomes that include cerebral palsy as a component ("Neurodevelopmental impairment at 18 to 22 months" (1 RCT, 538 children); "Death or neurodevelopmental impairment at 18 to 22 months" (1 RCT, 687 children); reported as secondary outcomes) |
| Neonatal care: infections: necrotising enterocolitis | ||||||
| Probiotics for prevention of necrotising enterocolitis in preterm infants | 1 October 2013 | 24 RCTs (Countries: Australia and New Zealand: 1 RCT; Brazil: 1 RCT; Colombia: 1 RCT; France: 1 RCT; Germany: 2 RCTs; Greece: 2 RCTs; India: 1 RCT; Israel: 1 RCT; Italy: 4 RCTs; Japan: 2 RCTs; Taiwan: 2 RCTs; Turkey: 1 RCT; UK: 1 RCT; USA: 1 RCT; not reported; 3 RCTs Published: 1980s: 1 RCT; 1990s: 2 RCTs; 2000s: 12 RCTs; 2010s: 9 RCTs) | 5529 infants (20 RCTs with reported outcomes) | Preterm infants at < 37 weeks and birthweight < 2500 g, or both | Probiotics vs control (20 RCTs, 5529 neonates) | Other composite outcome that includes cerebral palsy as a component ("Mental retardation and cerebral palsy" (1 RCT, 85 children); reported as a secondary outcome) |
| Arginine supplementation for prevention of necrotising enterocolitis in preterm infants | Search: August 2010 Up‐to‐date: 28 November 2010 | 1 RCT (Country: not reported Published; 2000s) | 152 infants | Preterm infants less than 37 weeks' gestation at birth | Arginine supplementation vs placebo (1 RCT, 152 neonates) | Cerebral palsy ("Cerebral palsy" (1 RCT, 135 children); reported as a post hoc secondary outcome) Other composite outcome that includes cerebral palsy as a component ("Major neurodevelopmental disability" (1 RCT, 132 children); reported as a post hoc secondary outcome) |
| Neonatal care: infections: fungal infections | ||||||
| Prophylactic systemic antifungal agents to prevent mortality and morbidity in very low birth weight infants | Search: August 2015 Up‐to‐date: 1 September 2015 | 15 RCTs (Countries: India: 2 RCTs; Italy: 2 RCTs; Korea: 1 RCT; Saudi Arabia: 1 RCT; Turkey: 2 RCTs; USA: 7 RCTs Published: 2000s: 7 RCTs; 2010s: 8 RCTs) | 1690 infants | Very preterm or VLBW infants with or without evidence of fungal colonisation but without evidence of invasive fungal infection at study entry | Systemic antifungal agent vs placebo or no drug (10 RCTs, 1371 neonates) | Cerebral palsy ("Cerebral palsy" (1 RCT, 219 children); reported as a primary outcome) Other composite outcome that includes cerebral palsy as a component ("Neurodevelopmental impairment (composite)" (1 RCT, 171 children); reported as a primary outcome) |
| Neonatal care: infections: herpes simplex | ||||||
| Antiviral agents for treatment of herpes simplex virus infection in neonates | Search: November 2008 Up‐to‐date: 14 March 2009 | 2 RCTs (Countries: USA: 2 RCTs Published: 1980s: 1 RCT; 1990s: 1 RCT) | 273 infants | Hospitalised newborn infants less than 1 month of age with virologically confirmed HSV infection | Vidarabine vs placebo (1 RCT, 56 neonates) Aciclovir vs vidarabine (1 RCT, 202 neonates) | Cerebral palsy ("Cerebral palsy in CNS HSV neonatal infection up to three years by HSV serotype: HSV‐1" (1 RCT, 9 children); "Cerebral palsy in CNS HSV neonatal infection up to three years by HSV serotype: HSV‐2" (1 RCT, 14 children); reported as primary outcomes) Other composite outcomes that include cerebral palsy as a component ("Abnormal neurodevelopment at one year" (1 RCT, 56 children; and 1 RCT, 202 children); "Abnormal neurodevelopment or death at approximately one year of age" (1 RCT, 56 children; and 1 RCT, 202 children); reported as primary outcomes) |
| Neonatal care: jaundice | ||||||
| Prophylactic phototherapy for preventing jaundice in preterm or low birth weight infants | 31 March 2011 | 9 RCTs (Countries: USA: 6 RCTs; Brazil: 1 RCT; Canada: 1 RCT; India: 1 RCT Published: 1960s: 2 RCTs; 1970s: 1 RCT; 1980s: 2 RCTs; 2000s: 4 RCTs) | 3449 infants |
Originally (in the protocol), the focus of the review was narrower (to include VLBW infants; < 1500 g birthweight); however, so as not to lose valuable information, we made a post hoc decision to include any study that involved LBW (< 2500 g birthweight) or preterm infants We excluded studies of infants with a known cause that can lead to significant hyperbilirubinaemia, such as ABO incompatibility, Rh incompatibility, minor blood group incompatibility, or G‐6PD deficiency | Prophylactic phototherapy vs control (9 RCTs, 3449 neonates) | Cerebral palsy ("Cerebral palsy" (2 RCTs, 756 children); reported as a primary outcome) Other composite outcomes that include cerebral palsy as a component ("Neurodevelopmental impairment" (1 RCT, 1804 children); reported as a primary outcome) |
| Neonatal care: hypoglycaemia | ||||||
| Oral dextrose gel for the treatment of hypoglycaemia in newborn infants | 29 February 2016 | 2 RCTs (Countries: Ireland: 1 RCT; New Zealand: 1 RCT; Published: 2000s: 1 RCT; 2010s: 1 RCT) | 317 infants | We included newborn infants from birth to discharge home who were hypoglycaemic (blood glucose concentrations below the normal range, investigator defined) for any reason. We excluded infants who had received prior IV treatment for maintenance of glucose control at the time of hypoglycaemia | Dextrose gel vs control (2 RCTs, 317 neonates) | Cerebral palsy ("Cerebral palsy and severity at age 2 years or older" (1 RCT, 183 children); reported as a secondary outcome) Other composite outcomes that include cerebral palsy as a component ("Major neurosensory disability (2‐year follow‐up)" (1 RCT, 184 children); reported as a primary outcome) ("Developmental disability at age 2 years or older" (1 RCT, 184 children); reported as a secondary outcome) |
| Neonatal care: parenteral feeding | ||||||
| Glutamine supplementation to prevent morbidity and mortality in preterm infants | 18 December 2015 | 12 RCTs (Countries: China; 1 RCT; Greece: 1 RCT; Malaysia: Published: 1990s: 2 RCTs; 2000s: 6 RCTs; 2010s: 4 RCTs) | 2877 infants | We included preterm infants (gestational age < 37 weeks) admitted to neonatal intensive or special care units or comparable settings after birth. When participants in a trial included both term and preterm infants, we sought subgroup data from the report or from trial authors | Glutamine supplementation vs no supplementation (12 RCTs, 2877 neonates) | Other composite outcome that includes cerebral palsy as a component ("Neurodevelopmental impairment" (1 RCT, 72 children); reported as a primary outcome) |
| Neonatal care: other | ||||||
| Thyroid hormones for preventing neurodevelopmental impairment in preterm infants | Search: Up‐to‐date: 1 February 2009 | 5 RCTs (Countries: not reported; Published: 1980s: 2 RCTs; 1990s: 2 RCTs; 2000s; 1 RCT) | 362 infants | Studies that enrolled and treated preterm infants in the neonatal period | Thyroid hormones vs control (5 RCTs, 362 neonates) | Cerebral palsy ("Cerebral palsy in survivors" (1 RCT, 156 children); reported as a primary outcome) Cerebral palsy or death ("Death or cerebral palsy" (1 RCT, 200 children); reported as a primary outcome) |
| Prophylactic postnatal thyroid hormones for prevention of morbidity and mortality in preterm infants | Search: Up‐to‐date: 12 October 2006 | 4 RCTs (Countries: not reported; Published: 1990s: 2 RCTs; 2000s: 2 RCTs) | 318 infants | Studies that enrolled preterm infants (born < 37 completed weeks' gestation) in the neonatal period. Trials that enrolled infants on the basis of results of abnormal thyroid function tests (known congenital hypothyroidism or transient hypothyroxinaemia), or with only respiratory distress syndrome, were excluded | Prophylactic thyroid hormones vs no thyroid hormones (4 RCTs, 318 neonates) | Cerebral palsy ("Cerebral palsy in survivors" (1 RCT, 156 children); reported as a primary outcome) Cerebral palsy or death ("Death or cerebral palsy" (1 RCT, 200 children); reported as a primary outcome) |
| Sound reduction management in the neonatal intensive care unit for preterm or very low birth weight infants | 18 December 2014 | 1 RCT (Country: USA; Published: 2009) | 34 infants | Preterm infants (< 32 weeks' post‐menstrual age or < 1500 g birthweight) cared for in the resuscitation area, during transport, or once admitted to an NICU or a stepdown unit | Silicone earplugs vs no earplugs (1 RCT, 34 infants) | Cerebral palsy ("Cerebral palsy at 18 to 22 months' corrected age" (1 RCT, 14 children); reported as a primary outcome) |
| Kangaroo mother care to reduce morbidity and mortality in low birthweight infants | 30 June 2016 | 21 RCTs (Countries: 13 RCTs in low‐ or middle‐income countries: Colombia: 1 RCT; Ecuador: | 3042 infants | LBW infants (defined as birthweight < 2500 g) regardless of gestational age | Kangaroo mother care vs conventional neonatal care (20 RCTs, 2969 neonates) | Cerebral palsy ("Cerebral palsy at 12 months' corrected age" (1 RCT, 588 children); reported as a primary outcome) |
| Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants | 15 August 2015 | 25 RCTs (Countries: not reported; Published: 1970s: 1 RCT; 1980s: 5 RCTs; 1990s: | 3615 infants | Preterm infants born at < 37 weeks' gestational age (according to best obstetrical estimate at the time of delivery). We excluded studies that did not report outcomes for preterm infants separately from those for infants born at term | Early developmental intervention vs standard follow‐up (25 RCTs, 3615 neonates) | Cerebral palsy ("Rate of cerebral palsy" (7 RCTs, 985 children); reported as a secondary outcome) Motor dysfunction ("Motor outcome at school age (low score on Movement ABC)" (2 RCTs, 333 children); reported as a secondary outcome) |
| Abbreviations: BP: blood pressure; BPD: bronchopulmonary dysplasia; BSID: Bayley Scales of Infant Development; CNS: central nervous system; ECHO: echocardiogram; g: grams; G‐6PD: glucose‐6‐phosphate dehydrogenase; HSV: herpes simplex virus; IPPV: intermittent positive‐pressure ventilation; IV: intravenous; LBW: low birthweight; MDI: Mental Development Index; Movement‐ABC: Movement Assessment Battery for Children; NICU: neonatal intensive care unit; NO: nitric oxide; PDA: patent ductus arteriosus; PDI: Psychomotor Development Index; PMA: post‐menstrual age; PPHN: persistent pulmonary hypertension of the newborn; RCT: randomised controlled trial; Rh: Rhesus; SBF: systemic blood flow; SD: standard deviation; SVC: superior vena cava; VLBW: very low birthweight. | ||||||
| Review ID and title | Summary of trial limitations (risk of bias)* |
| Neonatal care: asphyxia | |
| Allopurinol for preventing mortality and morbidity in newborn infants with hypoxic‐ischaemic encephalopathy | Random sequence generation: 2 RCTs low risk; 1 RCT unclear risk Allocation concealment: 3 RCTs low risk Blinding: 2 RCTs low risk; 1 RCT high risk Incomplete outcome data: 3 RCTs low risk Overall: "Although small, the trials were generally of good methodological quality" |
| Cooling for newborns with hypoxic‐ischaemic encephalopathy | Random sequence generation: 9 RCTs low risk; 1 RCT unclear risk; 1 RCT high risk Allocation concealment: 8 RCTs low risk; 2 RCTs unclear risk; 1 RCT high risk Blinding (participants and personnel): 11 RCTs high risk Blinding (outcome assessors): 10 RCTs low risk; 1 RCT unclear risk Incomplete outcome data: 6 RCTs low risk; 1 RCT unclear risk; 4 RCTs high risk Selective reporting: 11 RCTs low risk Overall: "Several limitations of the available evidence should be noted" |
| Prophylactic barbiturate use for the prevention of morbidity and mortality following perinatal asphyxia | Random sequence generation: 7 RCTs low risk; 2 RCTs unclear risk Allocation concealment: 4 RCTs low risk; 4 RCTs unclear risk; 1 RCT high risk Blinding: 4 RCTs unclear risk; 5 RCTs high risk Incomplete outcome data: 6 RCTs low risk; 2 RCTs unclear risk; 1 RCT high risk Selective reporting: 9 RCTs low risk |
| Neonatal care: haemorrhage: periventricular/intraventricular | |
| Ethamsylate for the prevention of morbidity and mortality in preterm or very low birth weight infants | Adequate sequence generation: 4 RCTs yes; 2 RCTs unclear; 1 RCT no Allocation concealment: 3 RCTs yes; 2 RCT unclear; 2 RCTs no Blinding: 4 RCTs yes; 3 RCTs unclear Incomplete outcome data addressed: 5 RCTs yes; 1 RCT unclear; 1 RCT no Free of selective reporting: 7 RCTs yes Free of other bias: 7 RCTs yes |
| Postnatal phenobarbital for the prevention of intraventricular haemorrhage in preterm infants | Random sequence generation: 5 RCTs low risk; 6 RCTs unclear risk; 1 RCT high risk Allocation concealment: 4 RCTs low risk; 7 RCTs unclear risk; 1 RCT high risk Blinding (participants and personnel): 2 RCTs low risk; 10 RCTs high risk Blinding (outcome assessors): 6 RCTs low risk; 6 RCTs unclear risk Incomplete outcome data: 8 RCTs low risk; 4 RCTs unclear risk Selective reporting: 2 RCTs low risk; 10 RCTs unclear risk |
| Neonatal care: hypotension | |
| The effect of inotropes on morbidity and mortality in preterm infants with low systemic or organ blood flow | Adequate sequence generation: 1 RCT yes Allocation concealment: 1 RCT yes Blinding (outcomes): 1 RCT yes Blinding (intervention): 1 RCT yes Incomplete outcome data addressed: 1 RCT yes Free of selective reporting: 1 RCT yes Free of other bias: 1 RCT yes Overall: "The study was of adequate methodology" |
| Neonatal care: fluid therapy | |
| Early volume expansion for prevention of morbidity and mortality in very preterm infants | Adequate randomisation: 7 RCTs yes; 1 RCT unclear Allocation concealment: 7 RCTs yes; 1 RCT unclear Blinding of intervention: 1 RCT yes; 7 RCTs no Blinding of measurement: 3 RCTs yes; 1 RCT unclear; 4 RCTs no Losses to follow‐up: 5 RCTs none; 1 RCT unclear; 2 RCTs yes |
| Neonatal care: patent ductus arteriosus | |
| Prophylactic intravenous indomethacin for preventing mortality and morbidity in preterm infants | Blinding of randomisation: 12 RCTs yes; 7 RCTs can't tell Blinding of intervention: 16 RCTs yes; 2 RCTs can't tell; 1 RCT no Blinding of outcome assessment: 16 RCTs yes; 2 RCTs can't tell; 1 RCT no Complete follow‐up (short‐term outcomes): 18 RCTs yes; 1 RCT no Overall: "Overall, the quality of the trials was good" |
| Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants | Random sequence generation: 9 RCTs low risk; 24 RCTs unclear risk Allocation concealment: 18 RCTs low risk; 14 RCTs unclear risk; 1 RCT high risk Blinding: 6 RCTs low risk; 7 RCTs unclear risk; 20 RCTs high risk Incomplete outcome data: 28 RCTs low risk; 3 RCTs unclear risk; 2 RCTs high risk Selective reporting: 5 RCTs low risk; 28 RCTs unclear risk Other: 29 RCTs low risk; 4 RCTs unclear risk Overall: "Study quality was variable…we identified concerns about bias in most individual studies and therefore for the group of studies included as well" |
| Neonatal care: blood disorders | |
| Early erythropoietin for preventing red blood cell transfusion in preterm and/or low birth weight infants | Random sequence generation: 8 RCTs low: risk; 19 RCTs unclear risk Allocation concealment: 13 RCTs low risk; 14 RCTs unclear risk Blinding: 12 RCTs low risk; 3 RCTs unclear risk; 12 RCTs high risk Incomplete outcome data: 23 RCTs low risk; 2 RCTs unclear risk; 2 RCTs high risk Selective reporting: 1 RCT low risk; 26 RCTs unclear risk Other: 26 RCTs low risk; 1 RCT unclear risk |
| Low versus high haemoglobin concentration threshold for blood transfusion for preventing morbidity and mortality in very low birth weight infants | Allocation concealment: 4 RCTs low risk; 1 RCT unclear risk Blinding: 1 RCT unclear risk; 4 RCTs high risk Incomplete outcome data: 3 RCTs low risk; 1 RCT unclear risk; 1 RCT high risk Selective reporting: 1 RCT low risk; 3 RCTs unclear risk; 1 RCT high risk Overall: "This review consists of five randomised controlled trials in which there appears to be no allocation bias; the overall level of evidence is high" |
| Neonatal care: pulmonary hypertension | |
| Endothelin receptor antagonists for persistent pulmonary hypertension in term and late preterm infants | Random sequence generation: 1 RCT low risk; 1 RCT unclear risk Allocation concealment: 2 RCT unclear risk Blinding (participants and personnel): 2 RCTs low risk Blinding (outcome assessors): 2 RCTs low risk Incomplete outcome data: 1 RCT low risk; 1 RCT high risk Selective reporting: 1 RCT low risk; 1 RCT unclear risk Other: 2 RCTs low risk Overall: "the quality of evidence was considered low because of the very small sample size and methodological issues in the included studies" |
| Neonatal care: resuscitation | |
| Air versus oxygen for resuscitation of infants at birth | Concealment of allocation: 2 RCTs yes; 3 RCTs no Blinding of intervention: 2 RCTs yes; 3 RCTs no Blinding of outcome assessment: 2 RCTs yes; 3 RCTs no Completeness of follow‐up (short‐term): 4 RCTs yes; 1 RCT no Completeness of follow‐up (long‐term): 3 RCTs no; 2 RCTs unclear |
| Neonatal care: nitric oxide | |
| Inhaled nitric oxide for respiratory failure in preterm infants | Allocation concealment: 12 RCTs low risk; 2 RCTs unclear risk Blinding: 7 RCTs low risk; 7 RCTs high risk Incomplete outcome data: 14 RCTs low risk Selective reporting: 8 RCTs low risk; 6 RCTs not reported Other: 3 RCTs low risk; 4 RCTs high risk; 7 RCTs not reported |
| Nitric oxide for respiratory failure in infants born at or near term | Masking of allocation: 10 RCTs yes; 4 RCTs cannot tell Masking of intervention: 6 RCTs yes; 8 RCTs no Masking of outcome assessment: 6 RCTs yes; 1 RCT can’t tell; 7 RCTs no Completeness of follow‐up: 13 RCTs yes; 1 RCT can't tell Overall: "The overall quality of these studies is quite variable" |
| Neonatal care: apnoea | |
| Methylxanthine treatment for apnoea in preterm infants | Random sequence generation: 1 RCT high risk; 5 RCTs not reported Allocation concealment: 2 RCTs low risk; 2 RCTs unclear risk; 2 RCTs high risk Blinding: 4 RCTs low risk; 2 RCTs high risk Incomplete outcome data: 3 RCTs low risk; 1 RCT unclear risk; 2 RCTs high risk Selective reporting: 2 RCTs low risk; 1 RCT unclear risk; 2 RCTs high risk; 1 RCT not reported Overall: "There was variation in trial design" |
| Prophylactic methylxanthine for prevention of apnoea in preterm infants | Allocation concealment: 3 RCTs low risk Blinding: 3 RCTs low risk Incomplete outcome data: 3 RCTs low risk Selective reporting: 2 RCTs low risk; 1 RCT not reported Overall: "Three studies are generally of high quality" |
| Neonatal care: respiratory distress syndrome | |
| Inositol in preterm infants at risk for or having respiratory distress syndrome | Random sequence generation: 1 RCT low risk; 3 RCTs unclear risk Allocation concealment: 2 RCTs low risk; 2 RCTs unclear risk Blinding: 2 RCTs low risk; 2 RCTs unclear risk Incomplete outcome data: 4 RCTs low risk Selective reporting: 3 RCTs low risk; 1 RCT unclear risk Other: 3 RCTs high risk; 1 RCT low risk Overall: "Study quality varied and interim analyses had occurred in all trials" |
| Animal derived surfactant extract for treatment of respiratory distress syndrome | Blinding of randomisation: 10 RCTs yes; 3 RCTs not described Blinding of intervention: 8 RCTs yes; 1 RCT not described; 4 RCTs no Blinding of outcome measurement: 6 RCTs yes; 4 RCTs not described; 2 RCTs no; 1 RCT not reported Complete follow‐up (short‐term): 13 RCTs yes Complete follow‐up (long‐term): 4 RCTs yes; 9 RCTs no Overall: "studies are of high methodological quality" |
| Synthetic surfactant for respiratory distress syndrome in preterm infants | Blinding of randomisation: 6 RCTs yes Blinding of intervention: 5 RCTs yes; 1 RCT no Blinding of outcome measurement: 5 RCTs yes; 1 RCT no Complete follow‐up (short term): 6 RCTs yes Complete follow‐up (long term): 80 to 100% |
| Prophylactic protein free synthetic surfactant for preventing morbidity and mortality in preterm infants | Adequate sequence generation: 6 RCTs unclear: 1 RCT not reported Allocation concealment: 7 RCTs yes Blinding of intervention: 5 RCTs yes; 1 RCT unclear; 1 RCT no Blinding of outcome measurement: 6 RCTs yes; 1 RCT no Incomplete outcome data addressed: 5 RCTs yes; 2 RCTs unclear Free of selective reporting: 7 RCTs yes Free of other bias: 7 RCTs yes |
| Neonatal care: mechanical ventilation | |
| Elective high frequency oscillatory ventilation versus conventional ventilation for acute pulmonary dysfunction in preterm infants | Random sequence generation: 11 RCTs low risk; 8 RCTs unclear risk Allocation concealment: 7 RCTs low risk; 12 RCTs unclear risk Blinding of participants and personnel: 19 RCTs high risk Blinding of outcome assessment: 7 RCTs low risk; 12 RCTs unclear risk Incomplete outcome data: 19 RCTs low risk Overall: "The quality of the studies was generally high" |
| Continuous distending pressure for respiratory distress in preterm infants | Random sequence generation: 2 RCTs low risk; 3 RCTs unclear risk; 1 RCT high risk Allocation concealment: 4 RCTs low risk; 1 RCT unclear risk; 1 RCT high risk Blinding (intervention): 6 RCTs high risk Blinding (short term outcomes): 6 RCTs high risk (1 RCT low risk for long term outcomes) Incomplete outcome data (short term outcomes): 3 RCTs low risk; 3 RCTs unclear risk (1 RCT low risk for long‐term outcomes) Selective reporting: 2 RCTs low risk; 4 RCTs unclear risk Other: 6 RCTs unclear risk Overall: "These data should be interpreted with caution as in the studies reviewed, the numbers of infants were small, blinding of treatment was not possible and blinding of the outcome assessment was reported in only one study for the outcomes in childhood, thus possibly introducing bias" |
| Prophylactic methylxanthines for endotracheal extubation in preterm infants | Sequence generation: 1 RCT low risk; 6 RCTs not reported Allocation concealment: 6 RCTs low risk; 1 RCT unclear risk Blinding: 6 RCTs low risk; 1 RCT high risk Incomplete outcome data: 3 RCTs low risk; 3 RCTs high risk; 1 RCT not reported Selective reporting: 4 RCTs low risk; 2 RCTs high risk; 1 RCT not reported Other: 1 RCT low risk; 6 RCTs not reported |
| Long versus short inspiratory times in neonates receiving mechanical ventilation | Concealment of allocation: 1 RCT yes; 1 RCT cannot tell; 3 RCTs no Blinding of intervention: 5 RCTs no Blinding of outcome measurement: 3 RCTs no; 2 RCTs some Completeness of follow‐up (short term outcomes): 5 RCTs yes |
| Volume‐targeted versus pressure‐limited ventilation in the neonate | Sequence generation: 6 RCTs low risk; 6 RCTs unclear risk Allocation concealment: 11 RCTs low risk; 1 RCT unclear risk Blinding: 12 RCTs high risk Incomplete outcome data: 12 RCTs low risk Selective reporting: 10 RCTs low risk; 1 RCT unclear risk; 1 RCT high risk Other: 5 RCTs low risk; 5 RCTs unclear risk; 2 RCTs high risk Overall: "There are no major concerns about the methodology used in the twelve trials included in this review" |
| Neonatal care: bronchopulmonary dysplasia | |
| Early (< 8 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants | Random sequence generation: 15 RCTs low risk; 14 RCTs unclear risk Allocation concealment: 27 RCTs low risk; 2 RCTs unclear risk Blinding of participants and personnel: 23 RCTs low risk; 2 RCTs unclear risk; 4 RCTs high risk Blinding of outcome assessment: 23 RCTs low risk; 2 RCTs unclear risk; 4 RCTs high risk Incomplete outcome data: 28 RCTs low risk; 1 RCT unclear risk Overall: "Overall the risk of bias was low for most studies" |
| Moderately early (7‐14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants | Blinding of randomisation/allocation concealment: 7 RCTs yes/low risk Blinding of intervention: 5 RCTs yes; 2 RCTs no Blinding of outcome measurement: 5 RCTs yes; 1 RCT some; 1 RCT cannot tell Complete follow‐up: 6 RCTs yes/almost; 1 RCT no Overall: "the methodological quality of the studies to determine long‐term outcome is limited in some cases" |
| Late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants | Random sequence generation: 12 RCTs low risk; 9 RCTs unclear risk Allocation concealment: 17 RCTs low risk; 4 RCTs unclear risk Blinding of participants and personnel: 15 RCTs low risk; 4 RCTs unclear risk; 2 RCTs high risk Blinding of outcome assessment: 16 RCTs low risk; 4 RCTs unclear risk; 1 RCT high risk Incomplete outcome data: 20 RCTs low risk; 1 RCT unclear risk Overall: "Overall the risk of bias was low for most studies" |
| Early administration of inhaled corticosteroids for preventing chronic lung disease in ventilated very low birth weight preterm neonates | Random sequence generation: 7 RCTs unclear risk Allocation concealment: 7 RCTs low risk Blinding of participants and personnel: 7 RCTs low risk Blinding of outcome assessment: 1 RCT low risk; 6 RCTs unclear risk Incomplete outcome data: 6 RCTs low risk; 1 RCT unclear risk Overall: "Overall, the studies included for this review were of high methodological quality" |
| Vitamin A supplementation to prevent mortality and short‐ and long‐term morbidity in very low birth weight infants | Random sequence generation: 9 RCTs low risk; 2 RCTs unclear risk Allocation concealment: 8 RCTs low risk; 3 RCTs unclear risk Blinding: 6 RCTs low risk; 2 RCTs unclear risk; 3 RCTs high risk Incomplete outcome data: 9 RCTs low risk; 1 RCT unclear risk; 1 RCT high risk Selective reporting: 8 RCTs low risk; 2 RCTs unclear risk; 1 RCT high risk Other: 2 RCTs low risk; 6 RCTs unclear risk; 2 RCTs high risk; 1 RCT not reported |
| Neonatal care: infections: necrotising enterocolitis | |
| Probiotics for prevention of necrotising enterocolitis in preterm infants | Random sequence generation: 15 RCTs low risk; 8 RCTs unclear risk; 1 RCT high risk Allocation concealment: 11 RCTs low risk; 12 RCTs unclear risk; 1 RCT high risk Blinding: 15 RCTs low risk; 9 RCTs unclear risk Incomplete outcome data: 21 RCTs low risk; 2 RCTs unclear risk; 1 RCT high risk Selective reporting: 17 RCTs low risk; 6 RCTs high risk; 1 RCT not reported Other: 14 RCTs low risk; 10 RCTs not reported Overall: "Eleven of our included trials were classified as high quality trials" |
| Arginine supplementation for prevention of necrotising enterocolitis in preterm infants | Masking of randomisation: 1 RCT yes Masking of intervention: 1 RCT yes Masking of outcome assessment: 1 RCT yes Completeness of follow‐up: 1 RCT yes Overall: "The methodological quality of the included study was good" |
| Neonatal care: infections: fungal infections | |
| Prophylactic systemic antifungal agents to prevent mortality and morbidity in very low birth weight infants | Allocation concealment: 12 RCTs low risk; 3 RCTs unclear risk Blinding of participants and personnel: 10 RCTs low risk; 3 RCTs unclear risk; 2 RCTs high risk Blinding of outcome assessment: 10 RCTs low risk; 3 RCTs unclear risk; 2 RCTs high risk Incomplete outcome data: 15 RCTs low risk Overall: "The included trials were generally of good methodological quality" |
| Neonatal care: infections: herpes simplex | |
| Antiviral agents for treatment of herpes simplex virus infection in neonates | Allocation concealment: 1 RCT unclear; 1 RCT inadequate Overall: "The two trials... have a number of methodological flaws" |
| Neonatal care: jaundice | |
| Prophylactic phototherapy for preventing jaundice in preterm or low birth weight infants | Random sequence generation: 4 RCTs low risk; 3 RCTs unclear risk; 2 RCTs high risk Allocation concealment: 3 RCTs low risk; 4 RCTs unclear risk; 2 RCTs high risk Blinding: 1 RCT low risk; 2 RCTs unclear risk; 6 RCTs high risk Incomplete outcome data: 8 RCTs low risk; 1 RCT high risk Selective reporting: 2 RCTs low risk; 7 RCTs unclear risk Other: 7 RCTs low risk Overall: "In general, the overall methodological quality of the included studies was acceptable" |
| Neonatal care: hypoglycaemia | |
| Oral dextrose gel for the treatment of hypoglycaemia in newborn infants | Random sequence generation: 1 RCT low risk; 1 RCT unclear risk Allocation concealment: 1 RCT low risk; 1 RCT unclear risk Blinding of participants and personnel: 1 RCT low risk; 1 RCT unclear risk Blinding of outcome assessors: 1 RCT low risk; 1 RCT unclear risk Incomplete outcome data: 1 RCT low risk; 1 RCT high risk Selective reporting: 1 RCT low risk; 1 RCT unclear risk Other: 1 RCT low risk; 1 RCT unclear risk |
| Neonatal care: parenteral feeding | |
| Glutamine supplementation to prevent morbidity and mortality in preterm infants | Random sequence generation: 8 RCTs low risk; 3 RCTs unclear risk; 1 RCT high risk Allocation concealment: 8 RCTs low risk; 2 RCTs unclear risk; 2 RCTs high risk Blinding: 10 RCTs low risk; 2 RCTs unclear risk Incomplete outcome data: 8 RCTs low risk; 2 RCTs unclear risk; 2 RCTs high risk Overall: "in general the trials were of good quality" |
| Neonatal care: other | |
| Thyroid hormones for preventing neurodevelopmental impairment in preterm infants | Blinding of randomisation/allocation concealment: 4 RCTs yes; 1 RCT no Blinding of intervention: 4 RCTs yes; 1 RCT no Blinding of outcome assessment: 4 RCTs yes; 1 RCT not stated Complete follow‐up: 2 RCTs yes; 3 RCTs no Overall: "four studies... were of good methodology" |
| Prophylactic postnatal thyroid hormones for prevention of morbidity and mortality in preterm infants | Allocation concealment: 4 RCTs low risk Blinding of intervention: 4 RCTs yes Blinding of outcome assessment: 3 RCTs yes; 1 RCT probably Complete follow‐up: 3 RCTs yes; 1 RCT no Overall: "All studies... were of adequate methodology" |
| Sound reduction management in the neonatal intensive care unit for preterm or very low birth weight infants | Random sequence generation: 1 RCT low risk Allocation concealment: 1 RCT low risk Blinding of participants and personnel: 1 RCT high risk Blinding of outcome assessment: 1 RCT low risk Incomplete outcome data: 1 RCT low risk Selective reporting: 1 RCT low risk Other: 1 RCT low risk Overall: "We considered the overall risk of bias to be low" |
| Kangaroo mother care to reduce morbidity and mortality in low birthweight infants | Random sequence generation: 21 RCTs low risk Allocation concealment: 10 RCTs low risk; 11 RCTs unclear risk Blinding of participants and personnel: 21 RCTs high risk Blinding of outcome assessment: 2 RCTs low risk; 15 RCTs unclear risk; 4 RCTs high risk Incomplete outcome data: 14 RCTs low risk; 3 RCTs unclear risk; 4 RCTs high risk Selective reporting: 16 RCTs low risk; 3 RCTs unclear risk; 2 RCTs high risk Other: 15 RCTs low risk; 3 RCTs unclear risk; 3 RCTs high risk Overall: "The methodological quality of the included trials was mixed" |
| Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants | Random sequence generation: 11 RCTs low risk; 8 RCTs unclear risk; 5 RCTs high risk; 1 RCT not reported Allocation concealment: 11 RCTs low risk; 9 RCTs unclear risk; 5 RCTs high risk Blinding of participants and personnel: 2 RCTs low risk; 4 RCTs unclear risk; 19 RCTs high risk Blinding of outcome assessment: 21 RCTs low risk; 3 RCTs unclear risk; 1 RCT high risk Incomplete outcome data: 12 RCTs low risk; 4 RCTs unclear risk; 9 RCT high risk Selective reporting: 3 RCTs unclear risk; 6 RCT high risk; 16 RCTs not reported Overall: "The methodological quality of included studies was variable" |
| Abbreviations: RCT: randomised controlled trial. | |
| Review ID | AMSTAR criteria | TOTAL SCORE | ||||||||||
| 'A priori' design | Duplicate selection and extraction | Comprehensive search | Grey literature considered | Included and excluded studies lists | Characteristics of included studies | Quality assessed and documented | Quality considered for conclusions | Methods for combining studies appropriate | Publication bias considered or assessed | Conflicts stated | ||
| Neonatal care: asphyxia | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | 10/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| Neonatal care: haemorrhage: periventricular/intraventricular | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| Neonatal care: hypotension | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | ✗ | 9/10 HIGH QUALITY | |
| Neonatal care: fluid therapy | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| Neonatal care: patent ductus arteriosus | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| Neonatal care: blood disorders | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| Neonatal care: pulmonary hypertension | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | ✗ | 9/10 HIGH QUALITY | |
| Neonatal care: resuscitation | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| Neonatal care: nitric oxide | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | ✗ | ✗ | 8/11 HIGH QUALITY | |
| ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 8/11 HIGH QUALITY | |
| Neonatal care: apnoea | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| Neonatal care: respiratory distress syndrome | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| ? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 8/11 HIGH QUALITY | |
| ? | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✗ | ✗ | 6/11 MODERATE QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| Neonatal care: mechanical ventilation | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 8/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| Neonatal care: bronchopulmonary dysplasia | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✗ | ✗ | 7/11 MODERATE QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| Neonatal care: infections: necrotising enterocolitis | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ? | ✓ | ✓ | ✓ | N/A | ✗ | ✗ | 7/10 HIGH QUALITY | |
| Neonatal infections: fungal infections | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| Neonatal infections: herpes simplex | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✗ | ✗ | 8/10 HIGH QUALITY | |
| Neonatal care: jaundice | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✗ | ✗ | 8/11 HIGH QUALITY | |
| Neonatal care: hypoglycaemia | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 11/11 HIGH QUALITY | |
| Neonatal care: parenteral feeding | ||||||||||||
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| Neonatal care: other | ||||||||||||
| ✓ | ? | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 8/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | ✗ | 9/10 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | 10/11 HIGH QUALITY | |
| ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✗ | ✗ | 9/11 HIGH QUALITY | |
| Review ID | ROBIS domains | OVERALL RISK OF BIAS | |||
| Study eligibility criteria | Identification and selection of studies | Data collection and study appraisal | Synthesis and findings | ||
| Neonatal care: asphyxia | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: haemorrhage: periventricular/intraventricular | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: hypotension | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: fluid therapy | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: patent ductus arteriosus | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: blood disorders | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: pulmonary hypertension | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: resuscitation | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: nitric oxide | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Unclear risk | Low risk | Low risk | UNCLEAR RISK | |
| Neonatal care: apnoea | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: respiratory distress syndrome | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Unclear risk | Low risk | Low risk | Low risk | LOW RISK | |
| Unclear risk | Unclear risk | Unclear risk | Unclear risk | UNCLEAR RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: mechanical ventilation | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: bronchopulmonary dysplasia | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Unclear risk | Unclear risk | Unclear risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal infections: necrotising enterocolitis | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal infections: fungal infections | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal infections: herpes simplex | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: jaundice | |||||
| Low risk | Low risk | Low risk | Unclear risk | LOW RISK | |
| Neonatal care: hypoglycaemia | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: parenteral feeding | |||||
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Neonatal care: other | |||||
| Low risk | Unclear risk | Unclear risk | Low risk | UNCLEAR RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Unclear risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Low risk | Low risk | Low risk | Low risk | LOW RISK | |
| Intervention and comparison | Outcome | Assumed risk with comparator | Corresponding risk with intervention | Relative effect (95% CI) | Number of participants (trials) | Quality of the evidence (GRADE) | Comments |
| Neonatal care: asphyxia | |||||||
| Therapeutic hypothermia vs standard care for newborns with hypoxic‐ischaemic encephalopathy (Jacobs 2013) | Cerebral palsy in survivors assessed at 18 to 24 months | 352 per 1000 (143/406) | 232 per 1000 (190 to 289) | RR 0.66 (0.54 to 0.82) | 881 (7 RCTs) | HIGH | Not downgraded |
| Cerebral palsy at 6 to 7 years | 288 per 1000 (15/52) | 173 per 1000 (89 to 340) | RR 0.60 (0.31 to 1.18) | 121 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with small sample size | |
| Barbiturates (phenobarbital) vs conventional therapy for prevention of morbidity and mortality following perinatal asphyxia (Young 2016) | Cerebral palsy at 3 to 6 years | 242 per 1000 (8/33) | 141 per 1000 (46 to 412) | RR 0.58 (0.19 to 1.70) | 69 (2 RCTs) | VERY LOW | Study limitations (‐1): unblinded studies; concern regarding performance bias and detection bias Imprecision (‐1): 95% CIs were wide and imprecise (GRADED by review authors themselves) |
| Neonatal care: haemorrhage: periventricular/intraventricular | |||||||
| Ethamsylate vs placebo for prevention of morbidity and mortality in preterm or very low birthweight infants (Hunt 2010) | Cerebral palsy in surviving children available for follow‐up at 2 years up to 3.5 to 4.2 years (only cerebral palsy significant enough to cause moderate or severe impairment was included) | 78 per 1000 (21/270) | 88 per 1000 (50 to 156) | RR 1.13 (0.64 to 2.00) | 532 (3 RCTs) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect |
| Neonatal care: hypotension | |||||||
| Dobutamine vs dopamine in preterm infants with low superior vena cava flow (Osborn 2007b) | Cerebral palsy at 3 years in survivors assessed | 429 per 1000 (3/7) | 69 per 1000 (4 to 1131) | RR 0.16 (0.01 to 2.64) | 13 (1 RCT) | VERY LOW | Study limitations (‐1): 5/18 surviving infants were not assessed at 3 years of age Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with very small sample size |
| Neonatal care: fluid therapy | |||||||
| Volume vs no treatment for prevention of morbidity and mortality in very preterm infants (Osborn 2004) | Cerebral palsy in survivors at 2 years | 132 per 1000 (27/205) | 100 per 1000 (63 to 158) | RR 0.76 (0.48 to 1.20) | 604 (1 RCT) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect |
| Gelatin vs fresh frozen plasma for prevention of morbidity and mortality in very preterm infants (Osborn 2004) | 103 per 1000 (21/203) | 97 per 1000 (54 to 175) | RR 0.94 (0.52 to 1.69) | 399 (1 RCT) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect | |
| Neonatal care: patent ductus arteriosus | |||||||
| Prophylactic indomethacin vs placebo for preventing mortality and morbidity in preterm infants (Fowlie 2010) | Cerebral palsy at 18 to 54 months | 111 per 1000 (77/694) | 115 per 1000 (85 to 155) | RR 1.04 (0.77 to 1.40) | 1372 (4 RCTs) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect |
| Cerebral palsy at 8 years | 76 per 1000 (11/145) | 94 per 1000 (45 to 199) | RR 1.24 (0.59 to 2.62) | 304 (1 RCT) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect | |
| Oral ibuprofen vs intravenous ibuprofen for treatment of patent ductus arteriosus in preterm or low birthweight (or both) infants (Ohlsson 2015) | Moderate or severe cerebral palsy at 18 to 24 months | 74 per 1000 (2/27) | 100 per 1000 (18 to 554) | RR 1.35 (0.24 to 7.48) | 57 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at unclear risk of selection and reporting bias; high risk of performance, detection, and attrition bias Imprecision (‐2): wide CI crossing line of no effect; small sample size and few events |
| Neonatal care: blood disorders | |||||||
| Erythropoietin vs placebo for preventing red blood cell transfusion in preterm and/or low birthweight infants (Ohlsson 2014) | Cerebral palsy at 18 to 22 months' corrected age (in children examined) | 187 per 1000 (14/75) | 123 per 1000 (58 to 256) | RR 0.66 (0.31 to 1.37) | 153 (2 RCTs) | VERY LOW | Study limitations (‐1): 1 RCT at unclear risk of selection bias and high risk of attrition bias (˜73% follow‐up) Inconsistency (‐1): I² = 72% Imprecision (‐2): wide CI crossing line of no effect; small sample sizes |
| Darbepoetin alfa vs placebo for preventing red blood cell transfusion in preterm and/or low birthweight infants (Ohlsson 2014) | 208 per 1000 (5/24) | 17 per 1000 (0 to 292) | RR 0.08 (0.00 to 1.40) | 51 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with small sample size and few events | |
| Transfusion at a restrictive vs a liberal haemoglobin threshold for preventing morbidity and mortality in very low birthweight infants (Whyte 2011) | Cerebral palsy at 18 to 21 months' follow‐up among survivors | 52 per 1000 (9/172) | 68 per 1000 (29 to 159) | RR 1.29 (0.55 to 3.03) | 335 (1 RCT) | LOW | Study limitations (‐1): 1 RCT at high risk of performance bias and unclear risk of reporting bias Imprecision (‐1): wide CI crossing line of no effect |
| Neonatal care: pulmonary hypertension | |||||||
| Endothelin receptor antagonists vs placebo for persistent pulmonary hypertension in term and late preterm infants (More 2016) | Cerebral palsy at 6 months (delayed motor development and spasticity) | 214 per 1000 (3/14) | 19 per 1000 (0 to 345) | RR 0.09 (0.00 to 1.61) | 37 (1 RCT) | LOW | Study limitation (‐1): 8/23 infants in the placebo group were excluded from analysis Imprecision (‐1): 1 RCT; small sample size (GRADED by review authors themselves) |
| Neonatal care: resuscitation | |||||||
| Room air vs 100% oxygen for resuscitation of infants at birth (Tan 2005) | Cerebral palsy in those followed up at 18 to 24 months | 74 per 1000 (9/122) | 99 per 1000 (41 to 239) | RR 1.34 (0.55 to 3.24) | 213 (1 RCT) | VERY LOW | Study limitations (‐2): 1 qRCT with no blinding and < 70% follow‐up Imprecision (‐1): wide CI crossing line of no effect |
| Neonatal care: nitric oxide | |||||||
| Inhaled NO vs placebo for respiratory failure in preterm infants (entry before 3 days based on oxygenation) (Barrington 2010) | Cerebral palsy at 18 to 22 months (moderate/severe or disabling) | 100 per 1000 (11/110) | 185 per 1000 (93 to 371) | RR 1.85 (0.93 to 3.71) | 209 (2 RCTs) | LOW | Imprecision (‐2): wide CI crossing line of no effect; small sample sizes |
| Inhaled NO vs placebo or no treatment for respiratory failure in preterm infants (entry after 3 days based on BPD risk) (Barrington 2010) | Cerebral palsy at 2 years' corrected age or 30 months (1 RCT all severities; 1 RCT moderate/severe or disabling) | 56 per 1000 (14/248) | 62 per 1000 (30 to 126) | RR 1.10 (0.54 to 2.23) | 498 (2 RCTs) | LOW | Study limitations (‐1): 1 RCT with no blinding of intervention or outcome measurement Imprecision (‐1): wide CI crossing line of no effect; small sample sizes |
| Inhaled NO vs placebo for respiratory failure in preterm infants (studies of routine use in intubated preterm infants) (Barrington 2010) | Cerebral palsy at 1 or 2 years' corrected age (1 RCT all severities; 1 RCT moderate/severe or disabling) | 70 per 1000 (20/286) | 66 per 1000 (36 to 119) | RR 0.94 (0.51 to 1.70) | 593 (2 RCTs) | LOW | Study limitations (‐1): 2 RCTs with 74%‐82% follow‐up Imprecision (‐1): wide CI crossing line of no effect |
| Inhaled nitric oxide vs placebo for respiratory failure in infants born at or near term (Finer 2006) | Cerebral palsy among survivors at 13 or 18 to 24 months | 89 per 1000 (16/179) | 91 per 1000 (44 to 191) | RR 1.02 (0.49 to 2.14) | 299 (2 RCTs) | LOW | Study limitations (‐1): 1 RCT masking of allocation, masking of outcomes. and completeness of follow‐up Imprecision (‐1): wide CI crossing line of no effect |
| "This group has now published follow up data, including neurodevelopmental outcomes, which were obtained by telephone interview of 60 of the 83 survivors of the original trial. The interview was conducted between one and four years of age... Although cerebral palsy [was] reported it is unclear how [it] was defined... It is not, therefore, possible to add any of these data to the meta‐analysis, but they do appear to show no evidence of neurodevelopmental impairment due to inhaled nitric oxide therapy" | NOT GRADED | ||||||
| Inhaled nitric oxide vs placebo for respiratory failure in infants with diaphragmatic hernias born at or near term (Finer 2006) | Cerebral palsy among survivors at 18 to 24 months | (0/14) | (2/8) | RR 8.33 (0.45 to 154.78) | 22 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with 76% follow‐up of survivors Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Neonatal care: apnoea | |||||||
| Caffeine vs placebo for treatment of apnoea in preterm infants (Henderson‐Smart 2010b) | Cerebral palsy at 18 to 21 months' corrected age | 50 per 1000 (18/361) | 30 per 1000 (14 to 62) | RR 0.60 (0.29 to 1.25) | 729 (1 RCT) | LOW | Study limitations (‐1): results based on 1 RCT subgroup from post hoc subgroup analyses (randomisation not stratified according to indication for inclusion) Imprecision (‐1): wide CI crossing line of no effect |
| Caffeine vs placebo for prevention of apnoea in preterm infants (Henderson‐Smart 2010c) | Cerebral palsy at 18 to 21 months' corrected age | 45 per 1000 (9/200) | 46 per 1000 (19 to 112) | RR 1.03 (0.43 to 2.49) | 415 (1 RCT) | LOW | Study limitations (‐1): results based on 1 RCT subgroup from post hoc subgroup analyses (randomisation not stratified according to indication for inclusion) Imprecision (‐1): wide CI crossing line of no effect |
| Neonatal care: respiratory distress syndrome | |||||||
| Animal‐derived surfactant extract vs no treatment for treatment of respiratory distress syndrome (Seger 2009) | Cerebral palsy at 1 and 2 years' corrected age | 207 per 1000 (6/29) | 182 per 1000 (70 to 470) | RR 0.88 (0.34 to 2.27) | 73 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with no blinding of intervention; and blinding of outcome measurement not reported Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Synthetic surfactant vs placebo for respiratory distress syndrome in preterm infants (Soll 2000) | Cerebral palsy in survivors examined at 1 year (in 4 of the 5 RCTs) | 96 per 1000 (74/767) | 73 per 1000 (53 to 101) | RR 0.76 (0.55 to 1.05) | 1557 (5 RCTs) | MODERATE | Imprecision (‐1): wide CI crossing the line of no effect |
| Prophylactic protein‐free synthetic surfactant vs placebo for preventing morbidity and mortality in preterm infants (Soll 2010) | Cerebral palsy at 1 or 2 years | 153 per 1000 (49/320) | 142 per 1000 (52 to 204) | RR 0.93 (0.64 to 1.33) | 670 (4 RCTs) | LOW | Study limitations (‐1): "Somewhat fewer infants who received surfactant failed to return for follow‐up evaluation (typical relative risk 0.63, 95% CI 0.48, 0.82; typical risk difference ‐0.10, 95% CI ‐0.15, ‐0.04)" Imprecision (‐1): wide CI crossing the line of no effect |
| Neonatal care: mechanical ventilation | |||||||
| Elective high‐frequency oscillatory ventilation vs conventional ventilation for acute pulmonary dysfunction in preterm infants (Cools 2015) | Cerebral palsy |
| NOT GRADED | "The age and methods of assessment varied between studies so the results were presented in the text and not included in a meta‐analysis" | |||
| Continuous distending pressure vs standard care for respiratory distress in preterm infants (Ho 2015) | Cerebral palsy at 9 to 15 years | (0/18) | (2/18) | RR 5.0 (0.26 to 97.37) | 36 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at unclear risk of selection and attrition bias and high risk of performance bias Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Prophylactic methylxanthines (caffeine) vs placebo for endotracheal extubation in preterm infants (Henderson‐Smart 2010) | Cerebral palsy at 18 to 21 months' corrected age | 115 per 1000 (39/339) | 62 per 1000 (37 to 106) | RR 0.54 (0.32 to 0.92) | 644 (1 RCT) | MODERATE | Study limitations (‐1): results based on 1 RCT subgroup from post hoc subgroup analyses (randomisation not stratified according to indication for inclusion) |
| Long vs short inspiratory times in neonates receiving mechanical ventilation (Kamlin 2003) | Cerebral palsy in survivors less than 33 weeks' gestation at birth at 18 months | 133 per 1000 (12/90) | 387 per 1000 (129 to 1153) | RR 2.9 (0.97 to 8.65) | 177 ( 1 RCT) | VERY LOW | Study limitations: 1 RCT at high risk of performance bias; follow‐up of subset (< 33 weeks only) Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Neonatal care: bronchopulmonary dysplasia | |||||||
| Early (< 8 days) postnatal corticosteroids vs placebo or no treatment for preventing chronic lung disease in preterm infants (Doyle 2014b) | Cerebral palsy at 11 months to 7 to 9 years | 88 per 1000 (63/715) | 128 per 1000 (93 to 174) | RR 1.45 (1.06 to 1.98) | 1452 (12 RCTs) | MODERATE | Study limitations (‐1): 4 RCTs at unclear risk of selection bias; 2 RCTs at high risk of performance and detection bias; 2 RCTs had 13%‐53% follow‐up overall |
| Cerebral palsy in survivors assessed at 11 months to 7 to 9 years | 134 per 1000 (63/470) | 201 per 1000 (151 to 268) | RR 1.50 (1.13 to 2.00) | 959 (12 RCTs) | MODERATE | Study limitations (‐1): 4 RCTs at unclear risk of selection bias; 2 RCTs at high risk of performance and detection bias; 2 RCTs had 13%‐53% follow‐up overall | |
| Moderately early (7‐14 days) postnatal corticosteroids vs placebo or no treatment for preventing chronic lung disease in preterm infants (Halliday 2003) | Cerebral palsy at 12 months' corrected age up to 90 months | 105 per 1000 (10/95) | 108 per 1000 (49 to 236) | RR 1.03 (0.47 to 2.24) | 204 (4 RCTs) | VERY LOW | Study limitations (‐1): 2 RCTs with 68%‐70% follow‐up; 1 RCT with unclear blinding of outcome assessment Imprecision (‐2): wide CI crossing line of no effect; small sample sizes |
| Cerebral palsy in survivors assessed at 12 months' corrected age up to 90 months | 175 per 1000 (10/57) | 146 per 1000 (68 to 305) | RR 0.83 (0.39 to 1.74) | 130 (4 RCTs) | VERY LOW | Study limitations (‐1): 2 RCTs with 68%‐70% follow‐up; 1 RCT with unclear blinding of outcome assessment Imprecision (‐2): wide CI crossing line of no effect; small sample sizes | |
| Late (> 7 days) postnatal corticosteroids vs placebo or no treatment for chronic lung disease in preterm infants (Doyle 2014) | Cerebral palsy at 1 to 3 years | 127 per 1000 (55/433) | 135 per 1000 (97 to 191) | RR 1.06 (0.76 to 1.50) | 876 (14 RCTs) | LOW | Study limitations (‐1): 5 RCTs unclear risk of selection bias; 5 RCTs with follow‐up from 32% to 78% Imprecision (‐1): wide CI crossing line of no effect |
| Cerebral palsy at 1 to 3 years in survivors assessed | 172 per 1000 (53/309) | 180 per 1000 (129 to 252) | RR 1.05 (0.75 to 1.47) | 631 (14 RCTs) | LOW | Study limitations (‐1): 5 RCTs unclear risk of selection bias; 5 RCTs with follow‐up between 32% and 78% Imprecision (‐1): wide CI crossing line of no effect | |
| Cerebral palsy at latest reported age (from 1 year up to 17 years) | 121 per 1000 (51/423) | 135 per 1000 (95 to 193) | RR 1.12 (0.79 to 1.60) | 855 (15 RCTs) | LOW | Study limitations (‐1): 5 RCTs unclear risk of selection bias; 7 RCTs with follow‐up between 32% and 78% Imprecision (‐1): wide CI crossing line of no effect | |
| Cerebral palsy at latest reported age in survivors assessed (from 1 year up to 17 years) | 170 per 1000 (49/289) | 190 per 1000 (134 to 268) | RR 1.12 (0.79 to 1.58) | 591 (15 RCTs) | LOW | Study limitations (‐1): 5 RCTs unclear risk of selection bias; 7 RCTs with follow‐up between 32% and 78% Imprecision (‐1): wide CI crossing line of no effect | |
| Early inhaled corticosteroids vs placebo for preventing chronic lung disease in ventilated very low birthweight preterm neonates (Shah 2012) | Cerebral palsy (age not reported in review; from trial manuscript: 3 years) | 107 per 1000 (3/28) | 143 per 1000 (35 to 581) | RR 1.33 (0.33 to 5.42) | 56 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at unclear risk of selection bias and detection bias Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Neonatal care: necrotising enterocolitis | |||||||
| Arginine supplementation vs placebo for prevention of necrotising enterocolitis in preterm infants (Shah 2007) | Cerebral palsy at 36 months' post‐menstrual age | 55 per 1000 (4/73) | 48 per 1000 (12 to 208) | RR 0.88 (0.21 to 3.80) | 135 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Neonatal care: fungal infections | |||||||
| Systemic antifungal agent vs placebo to prevent mortality and morbidity in very low birthweight infants (Cleminson 2015) | Cerebral palsy at 18 to 22 months post term | 112 per 1000 (12/107) | 108 per 1000 (50 to 228) | RR 0.96 (0.45 to 2.03) | 219 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Neonatal care: herpes simplex | |||||||
| Aciclovir vs vidarabine for treatment of herpes simplex virus infection in neonates (Jones 2009) | Cerebral palsy in CNS HSV neonatal infection up to 3 years by HSV serotype: HSV‐1 | (0/4) | (0/5) | Not estimable | 9 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with design limitations (inadequate allocation concealment) Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Cerebral palsy in CNS HSV neonatal infection up to 3 years by HSV serotype: HSV‐2 | 625 per 1000 (5/8) | 669 per 1000 (306 to 1456) (4/6) | RR 1.07 (0.49 to 2.33) | 14 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with design limitations (inadequate allocation concealment) Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT | |
| Neonatal care: jaundice | |||||||
| Prophylactic phototherapy vs standard care for preventing jaundice in preterm or low birthweight infants (Okwundu 2012) | Cerebral palsy in all infants (birthweight < 2500 g) at 1 year or 18 months | Medium risk population: 84 per 1000 (18/394) | Medium risk population: 81 per 1000 (42 to 155) | RR 0.96 (0.50 to 1.85) | 756 (2 RCTs) | MODERATE | Study limitations (‐1): "There was no mention of blinding of the outcome assessors in two of the studies" (GRADED by review authors themselves) |
| Cerebral palsy in all infants (birthweight < 1000 g) at 18 months | 250 per 1000 (4/16) | 72 per 1000 (10 to 568) | RR 0.29 (0.04 to 2.27) | 30 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with no blinding Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT | |
| Cerebral palsy at 6 years | "Secondary reports emanating from Brown 1985 at six‐year follow‐up also showed that there was no significant difference in the rate of cerebral palsy between the phototherapy and control group" | NOT GRADED | |||||
| Neonatal care: hypoglycaemia | |||||||
| Dextrose gel vs placebo for treatment of hypoglycaemia in newborn infants (Weston 2016) | Cerebral palsy at age 2 years | (0/93) | (2/90) | RR 5.16 (0.25 to 106.12) | 183 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with 78% follow‐up Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Neonatal care: parenteral feeding | |||||||
| Glutamine supplementation vs placebo to prevent morbidity and mortality in preterm infants (Moe‐Byrne 2016) | Cerebral palsy at 2 years | "van den Berg 2005 reported neurodevelopmental outcomes for infants aged two years post term. Outcomes assessed included... incidence of cerebral palsy... No significant differences between the glutamine and the control groups were reported for any of these individual outcomes" | NOT GRADED | ||||
| Neonatal care: other | |||||||
| Thyroid hormones vs placebo for preventing neurodevelopmental impairment in preterm infants (Osborn 2001) | Cerebral palsy at 5.7 years | 120 per 1000 (9/75) | 86 per 1000 (34 to 221) | RR 0.72 (0.28 to 1.84) | 156 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Prophylactic thyroid hormones vs placebo for prevention of morbidity and mortality in preterm infants (Osborn 2007) | |||||||
| Silicone earplugs vs no earplugs in the neonatal intensive care unit for preterm or very low birthweight infants (Almadhoob 2015) | Cerebral palsy at 18 to 22 months' corrected age | (0/7) | (1/7) | RR 3.0 (0.14 to 63.15) | 14 (1 RCT) | VERY LOW | Study limitations (‐1): "Because of funding restraints only the ELBW infants could be followed at 18 to 22 months corrected age" (14/24 survivors) Imprecision (‐1): wide CI crossing line of no effect; 1 small RCT |
| Kangaroo mother care vs conventional neonatal care to reduce morbidity and mortality in low birthweight infants (Conde‐Agudelo 2016) | Cerebral palsy at 12 months' corrected age | 25 per 1000 (7/280) | 16 per 1000 (5 to 51) | RR 0.65 (0.21 to 2.02) | 588 (1 RCT) | LOW | Study limitation (‐1): 1 RCT with unclear risk of selection bias; high risk of performance and detection bias Imprecision (‐1): wide CI crossing line of no effect |
| Early developmental intervention vs standard follow‐up post hospital discharge to prevent motor and cognitive impairment in preterm infants (Spittle 2015) | Cerebral palsy at 18 months to 6 years | 79 per 1000 (32/405) | 65 per 1000 (41 to 100) | RR 0.82 (0.52 to 1.27) | 985 (7 RCTs) | LOW | Study limitations (‐1): 7 RCTs at unclear/high risk of performance bias; 2 RCTs at unclear/high risk of selection bias and unclear/high risk of attrition bias; 1 RCT at unclear risk of detection bias Imprecision (‐1): wide CI crossing line of no effect |
| Abbreviations: BPD: bronchopulmonary dysplasia; CI: confidence interval; CNS: central nervous system; CV: conventional ventilation; ELBW: extremely low birthweight; g: grams; GRADE: Grades of Recommendation, Assessment, Development and Evaluation; HFOV: high‐frequency oscillatory ventilation; HSV: herpes simplex virus; NO: nitric oxide; OR: odds ratio; P: P value; qRCT: quasi‐randomised controlled trial; RCT: randomised controlled trial; RR: risk ratio. | |||||||
| Intervention and comparison | Outcome | Subgroup or sensitivity analysis | Assumed risk with comparator | Corresponding risk with intervention | Relative effect (95% CI) | Number of participants (trials) | Test for subgroup differences | |
| Neonatal care: asphyxia | ||||||||
| Therapeutic hypothermia vs standard care for newborns with hypoxic‐ischaemic encephalopathy (Jacobs 2013) | Cerebral palsy in survivors assessed at 18 to 24 months | Method of cooling | Selective head cooling with mild hypothermia | 338 per 1000 (49/145) | 220 per 1000 (155 to 318) | RR 0.65 (0.46 to 0.94) | 312 (3 RCTs) | Chi² = 0.01, df = 1 (P = 0.93), I² = 0.0% |
| Whole body cooling | 360 per 1000 (94/261) | 241 per 1000 (187 to 310) | RR 0.67 (0.52 to 0.86) | 569 (4 RCTs) | ||||
| Neonatal care: haemorrhage: periventricular/intraventricular | ||||||||
| Ethamsylate vs placebo for prevention of morbidity and mortality in preterm or very low birthweight infants (Hunt 2010) | Cerebral palsy in surviving children available for follow‐up at 3 years up to 3.5 to 4.2 years | Infants < 31 completed weeks or < 1500 g | 84 per 1000 (14/167) | 69 per 1000 (32 to 147) | RR 0.82 (0.38 to 1.75) | 328 (2 RCTs) | Not applicable | |
| Neonatal care: fluid therapy | ||||||||
| Volume vs no treatment for prevention of morbidity and mortality in very preterm infants (Osborn 2004) | Cerebral palsy in survivors at 2 years | Type of volume used | Fresh frozen plasma | 132 per 1000 (27/205) | 104 per 1000 (61 to 177) | RR 0.79 (0.46 to 1.34) | 408 (1 RCT) | Not performed (as conducted as separate comparison) |
| Gelatin | 132 per 1000 (27/205) | 97 per 1000 (53 to 169) | RR 0.74 (0.42 to 1.28) | 401 (1 RCT) | ||||
| Timing of treatment | Early treatment (< 24 hours age) | 132 per 1000 (27/205) | 100 per 1000 (63 to 158) | RR 0.76 (0.48 to 1.20) | 604 (1 RCT) | Not applicable | ||
| Types of infant enrolled | Unselected preterm infants (not selected on the basis of cardiovascular compromise) | |||||||
| Methodological quality | Complete follow‐up for neurodevelopmental outcomes | |||||||
| Neonatal care: respiratory distress syndrome | ||||||||
| Animal‐derived surfactant extract vs no treatment for treatment of respiratory distress syndrome (Seger 2009) | Cerebral palsy at 1 and 2 years' corrected age | Surfactant product | Porcine surfactant extract | 207 per 1000 (6/29) | 182 per 1000 (70 to 470) | RR 0.88 (0.34 to 2.27) | 73 (1 RCT) | Not applicable |
| Prophylactic protein‐free synthetic surfactant vs placebo for preventing morbidity and mortality in preterm infants (Soll 2010) | Cerebral palsy at 1 or 2 years | Surfactant product | Exosurf Neonatal | 158 per 1000 (44/279) | 144 per 1000 (98 to 211) | RR 0.91 (0.62 to 1.34) | 591 (3 RCTs) | Not applied in review |
| DPPC/HDL | 122 per 1000 (5/41) | 132 per 1000 (41 to 420) | RR 1.08 (0.34 to 3.44) | 79 (1 RCT) | ||||
| Neonatal care: mechanical ventilation | ||||||||
| Continuous distending pressure vs standard care for respiratory distress in preterm infants (Ho 2015) | Cerebral palsy at 9 to 15 years | Type of continuous distending pressure | Continuous negative pressure | (0/18) | (2/18) | RR 5.0 (0.26 to 97.37) | 36 (1 RCT) | Not applicable |
| Neonatal care: bronchopulmonary dysplasia | ||||||||
| Early (< 8 days) postnatal corticosteroids vs placebo or no treatment for preventing chronic lung disease in preterm infants (Doyle 2014b) | Cerebral palsy at 11 months to 7 to 9 years | Type of corticosteroid used | Dexamethasone | 89 per 1000 (40/449) | 156 per 1000 (107 to 227) | RR 1.75 (1.20 to 2.55) | 921 (7 RCTs) | Chi² = 2.96, df = 1 (P = 0.09), I² = 66% |
| Hydrocortisone | 86 per 1000 (23/266) | 84 per 1000 (48 to 146) | RR 0.97 (0.55 to 1.69) | 531 (5 RCTs) | ||||
| Cerebral palsy in survivors assessed at 11 months to 7 to 9 years | Type of corticosteroid used | Dexamethasone | 139 per 1000 (40/288) | 253 per 100 (179 to 357) | RR 1.82 (1.29 to 2.57) | 586 (7 RCTs) | Chi² = 3.99, df = 1 (P = 0.05), I² = 75% | |
| Hydrocortisone | 126 per 1000 (23/182) | 120 per 1000 (71 to 206) | RR 0.95 (0.56 to 1.63) | 373 (5 RCTs) | ||||
| Neonatal care: other | ||||||||
| Prophylactic thyroid hormones vs placebo for prevention of morbidity and mortality in preterm infants (Osborn 2007) | Cerebral palsy at 5.7 years | Dosing strategy | T4 8 mcg/kg/d, day 1 to 42 | 120 per 1000 (9/75) | 86 per 1000 (34 to 221) | RR 0.72 (0.28 to 1.84) | 156 (1 RCT) | Not applicable |
| Timing | Commenced < 48 hours | |||||||
| Methodological quality | Studies with adequate methods | |||||||
| Early developmental intervention vs standard follow‐up post hospital discharge to prevent motor and cognitive impairment in preterm infants (Spittle 2015) | Cerebral palsy at 18 months to 6 years | Commencement of intervention | Inpatient | 79 per 1000 (12/152) | 74 per 1000 (36 to 152) | RR 0.94 (0.46 to 1.93) | 354 (3 RCTs) | Not applied in review |
| Post hospital discharge | 79 per 1000 (20/253) | 59 per 1000 (34 to 105) | RR 0.75 (0.43 to 1.33) | 631 (4 RCTs) | ||||
| Focus of intervention | Parent‐infant relationship and Infant development | 77 per 1000 (21/272) | 52 per 1000 (29 to 90) | RR 0.67 (0.38 to 1.17) | 716 (4 RCTs) | Not applied in review | ||
| Infant development | 83 per 1000 (11/133) | 97 per 1000 (46 to 203) | RR 1.17 (0.56 to 2.46) | 269 (3 RCTs) | ||||
| Quality of studies | Higher‐quality studies | 82 per 1000 (25/304) | 72 per 1000 (44 to 116) | RR 0.87 (0.53 to 1.41) | 776 (5 RCTs) | Not applied in review | ||
| Lower‐quality studies | 69 per 1000 (7/101) | 43 per 1000 (14 to 130) | RR 0.62 (0.20 to 1.87) | 209 (2 RCTs) | ||||
| Abbreviations: CI: confidence interval; DPPC/HDL: dipalmitoylphosphatidylcholine/high‐density lipoprotein; g: grams; P: P value; RCT: randomised controlled trial; RR: risk ratio; T4: thyroxine. | ||||||||
| Intervention and comparison | Outcome | Assumed risk with comparator | Corresponding risk with intervention | Relative effect (95% CI) | Number of participants (trials) | Quality of the evidence (GRADE) | Comments |
| Neonatal care: bronchopulmonary dysplasia | |||||||
| Early (< 8 days) postnatal corticosteroids vs placebo or no treatment for preventing chronic lung disease in preterm infants (Doyle 2014b) | Cerebral palsy or death at 11 months to 7 to 9 years | 352 per 1000 (252/715) | 384 per 1000 (334 to 441) | RR 1.09 (0.95 to 1.25) | 1452 (12 RCTs) | MODERATE | Study limitations (‐1): 4 RCTs at unclear risk of selection bias; 2 RCTs at high risk of performance and detection bias; 2 RCTs had 13% to 53% follow‐up overall |
| Moderately early (7‐14 days) postnatal corticosteroids vs placebo or no treatment for preventing chronic lung disease in preterm infants (Halliday 2003) | Cerebral palsy or death at 12 months' corrected age up to 90 months | 316 per 1000 (30/95) | 262 per 1000 (174 to 388) | RR 0.83 (0.55 to 1.23) | 204 (4 RCTs) | VERY LOW | Study limitations (‐1): 2 RCTs with 68% to 70% follow‐up; 1 RCT with unclear blinding of outcome assessment Imprecision (‐2): wide CI crossing line of no effect; small sample sizes |
| Late (> 7 days) postnatal corticosteroids vs placebo or no treatment for chronic lung disease in preterm infants (Doyle 2014) | Cerebral palsy or death at 1 to 3 years | 328 per 1000 (142/433) | 302 per 1000 (249 to 367) | RR 0.92 (0.76 to 1.12) | 876 (14 RCTs) | LOW | Study limitations (‐1): 5 RCTs unclear risk of selection bias; 5 RCTs with follow‐up between 32% and 78% Imprecision (‐1): wide CI crossing line of no effect |
| Cerebral palsy or death at latest reported age (from 1 year up to 17 years) | 312 per 1000 (132/423) | 296 per 1000 (240 to 362) | RR 0.95 (0.77 to 1.16) | 855 (15 RCTs) | LOW | Study limitations (‐1): 5 RCTs unclear risk of selection bias; 7 RCTs with follow‐up between 32% and 78% Imprecision (‐1): wide CI crossing line of no effect | |
| Neonatal care: other | |||||||
| Thyroid hormones vs placebo for preventing neurodevelopmental impairment in preterm infants (Osborn 2001) | Cerebral palsy or death at 5.7 years | 300 per 1000 (30/100) | 210 per 1000 (129 to 342) | RR 0.70 (0.43 to 1.14) | 200 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Prophylactic thyroid hormones vs placebo for prevention of morbidity and mortality in preterm infants (Osborn 2007) | |||||||
| Abbreviations: CI: confidence interval; GRADE: Grades of Recommendation, Assessment, Development and Evaluation; RCT: randomised controlled trial; RR: risk ratio. | |||||||
| Intervention and comparison | Outcome | Assumed risk with comparator | Corresponding risk with intervention | Relative effect (95% CI) | Number of participants (trials) | Quality of the evidence (GRADE) | Comments |
| Neonatal care: asphyxia | |||||||
| Allopurinol vs placebo or no drug for preventing mortality and morbidity in newborn infants with hypoxic‐ischaemic encephalopathy (Chaudhari 2012) | Severe quadriplegia in surviving infants (18 months and 4 to 8 years) | 343 per 1000 (12/35) | 202 per 1000 (96 to 435) | RR 0.59 (0.28 to 1.27) | 73 (3 RCTs) | VERY LOW | Study limitations (‐1): 1 RCT with unclear risk of selection bias and high risk of performance/detection bias Imprecision (‐2): wide CI crossing line of no effect; small sample sizes with few events |
| Neonatal care: respiratory distress syndrome | |||||||
| Synthetic surfactant vs placebo for respiratory distress syndrome in preterm infants (Soll 2000) | Moderate to severe cerebral palsy in survivors examined at 1 year (in 4 of the 5 RCTs) | 55 per 1000 (42/767) | 41 per 1000 (26 to 64) | RR 0.75 (0.48 to 1.16) | 1557 (5 RCTs) | MODERATE | Imprecision (‐1): wide CI crossing the line of no effect |
| Prophylactic protein‐free synthetic surfactant vs placebo for preventing morbidity and mortality in preterm infants (Soll 2010) | Moderate/severe cerebral palsy at 1 or 2 years | 75 per 1000 (24/320) | 69 per 1000 (40 to 119) | RR 0.92 (0.53 to 1.59) | 670 (4 RCTs) | LOW | Study limitations (‐1): "Somewhat fewer infants who received surfactant failed to return for follow‐up evaluation (typical relative risk 0.63, 95% CI 0.48, 0.82; typical risk difference ‐0.10, 95% CI ‐0.15, ‐0.04)" Imprecision (‐1): wide CI crossing the line of no effect |
| Abbreviations: CI: confidence interval; GRADE: Grades of Recommendation, Assessment, Development and Evaluation; RCT: randomised controlled trial; RR: risk ratio. | |||||||
| Intervention and comparison | Outcome | Assumed risk with comparator | Corresponding risk with intervention | Relative effect (95% CI) | Number of participants (trials) | Quality of the evidence (GRADE) | Comments |
| Neonatal care: asphyxia | |||||||
| Allopurinol vs placebo or no drug for preventing mortality and morbidity in newborn infants with hypoxic‐ischaemic encephalopathy (Chaudhari 2012) | Death or severe neurodevelopmental disability in survivors (18 months and 4 to 8 years) (defined as any 1 or combination of the following: non‐ambulant cerebral palsy, severe developmental delay assessed via validated tools, auditory and visual impairment) | 611 per 1000 (33/54) | 477 per 1000 (342 to 660) | RR 0.78 (0.56 to 1.08) | 110 (3 RCTs) | VERY LOW | Study limitations (‐1): 1 RCT with unclear risk of selection bias and high risk of performance/detection bias Imprecision (‐2): wide CI crossing line of no effect; small sample sizes |
| Therapeutic hypothermia vs standard care for newborns with hypoxic‐ischaemic encephalopathy (Jacobs 2013) | Death or major disability in survivors assessed at 18 to 24 months (defined as cerebral palsy, developmental delay (BSID or GMDS assessment > 2 SD below the mean) or intellectual impairment (IQ > 2 SD below mean), blindness (vision < 6/60 in both eyes), sensorineural deafness requiring amplification) | 614 per 1000 (409/666) | 461 per 1000 (418 to 510) | RR 0.75 (0.68 to 0.83) | 1344 (8 RCTs) | HIGH | Not downgraded |
| Major neurodevelopmental disability at 18 to 24 months (defined as cerebral palsy, developmental delay (BSID or GMDS assessment > 2 SD below the mean) or intellectual impairment (IQ > 2 SD below mean), blindness (vision < 6/60 in both eyes), sensorineural deafness requiring amplification) | 249 per 1000 (166/666) | 192 per 1000 (157 to 234) | RR 0.77 (0.63 to 0.94) | 1344 (8 RCTs) | HIGH | Not downgraded | |
| Major neurodevelopmental disability in survivors assessed at 18 to 24 months (defined as cerebral palsy, developmental delay (BSID or GMDS assessment > 2 SD below the mean) or intellectual impairment (IQ > 2 SD below mean), blindness (vision < 6/60 in both eyes), sensorineural deafness requiring amplification) | 393 per 1000 (166/422) | 264 per 1000 (216 to 315) | RR 0.67 (0.55 to 0.80) | 917 (8 RCTs) | HIGH | Not downgraded | |
| Death or moderate to severe disability at 6 to 7 years (defined as IQ ≥ 2 SD below the mean, a GMF level of 3 or greater, bilateral deafness (with or without amplification), bilateral blindness, or refractory epilepsy) | 645 per 1000 (60/93) | 523 per 1000 (413 to 671) | RR 0.81 (0.64 to 1.04) | 190 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with small sample size | |
| Moderate‐to‐severe disability at 6 to 7 years (defined as IQ ≥ 2 SD below the mean, a GMF level of 3 or greater, bilateral deafness (with or without amplification), bilateral blindness or refractory epilepsy) | 380 per 1000 (19/50) | 350 per 1000 (217 to 562) | RR 0.92 (0.57 to 1.48) | 119 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with small sample size | |
| Barbiturates (phenobarbital) vs conventional therapy for prevention of morbidity and mortality following perinatal asphyxia (Young 2016) | Death or major neurodevelopmental disability follow‐up: > 12 months (3 years) (defined as cerebral palsy, developmental delay (BSID or GMDS assessment > 2 SD below the mean) or intellectual impairment (IQ > 2 SD below mean), blindness (vision < 6/60 in both eyes), or sensorineural deafness requiring amplification) | 813 per 1000 (13/16) | 268 per 1000 (114 to 634) | RR 0.33 | 31 (1 RCT) | VERY LOW | Study limitations (‐1): unblinded study; concern regarding performance bias, detection bias, and incomplete follow‐up (graded by review authors themselves) |
| Major neurodevelopmental disability follow‐up: > 12 months (3 years) (defined as cerebral palsy, developmental delay (BSID or GMDS assessment > 2 SD below the mean) or intellectual impairment (IQ > 2 SD below mean), blindness (vision < 6/60 in both eyes), or sensorineural deafness requiring amplification) | 563 per 1000 (9/16) | 135 per 1000 (34 to 518) | RR 0.24 | 31 (1 RCT) | VERY LOW | Study limitations (‐1): unblinded study; concern regarding performance bias, detection bias, and incomplete follow‐up (graded by review authors themselves) | |
| Neonatal care: haemorrhage: periventricular/intraventricular | |||||||
| Ethamsylate vs placebo for prevention of morbidity and mortality in preterm or very low birthweight infants (Hunt 2010) | Neurodevelopmental disability at 2 years of age in surviving children available for follow‐up (defined as cerebral palsy on clinical examination, developmental delay > 2 SD below population mean on any standard test of development, or blindness (VA < 6/60), or deafness (any hearing impairment requiring amplification) at any time after 2 years' corrected age) | 170 per 1000 (46/270) | 135 per 1000 (90 to 199) | RR 0.79 (0.53 to 1.17) | 532 (3 RCTs) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect |
| Death or any disability by 2 years of age in children with known outcome at any point in time (not defined in review) | 338 per 1000 (233/690) | 324 per 1000 (277 to 375) | RR 0.96 (0.82 to 1.11) | 1334 (7 RCTs) | LOW | Study limitations (‐1): 4 RCTs at unclear risk of selection bias; 3 RCTs at unclear risk of bias due to lack of blinding Imprecision (‐1): wide CIs crossing line of no effect | |
| Phenobarbital vs no treatment for prevention of intraventricular haemorrhage in preterm infants (Smit 2013) | Severe neurodevelopmental impairment at 27 months (defined as clinical cerebral palsy or DQ below the range that can be measured) | 74 per 1000 (4/54) | 107 per 1000 (30 to 373) | RR 1.44 (0.41 to 5.04) | 101 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at high risk of performance bias) and unclear risk of other bias Imprecision (‐2): wide CI crossing line of no effect; small sample size, low event rate |
| Mild neurodevelopmental impairment at 27 months (defined as DQ < 80 or motor abnormality on examination) | 111 per 1000 (6/54) | 63 per 1000 (17 to 241) | RR 0.57 (0.15 to, 2.17) | 101 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at high risk of performance bias) and unclear risk of other bias Imprecision (‐2): wide CI crossing line of no effect; small sample size, low event rate | |
| Neonatal care: hypotension | |||||||
| Dobutamine vs dopamine in preterm infants with low superior vena cava flow (Osborn 2007b) | Disability at 3 years in survivors (defined as GMDS quotient ≤ 70, cerebral palsy, blind (VA < 6/60) or deaf (hearing aids)) | 714 per 1000 (5/7) | 71 per 1000 (7 to 1114) | RR 0.10 (0.01 to 1.56) | 13 (1 RCT) | VERY LOW | Study limitations (‐1): 5/18 surviving infants were not assessed at 3 years Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with very small sample size |
| Death or disability at 3 years (defined as GMDS quotient ≤ 70, cerebral palsy, blind (VA < 6/60) or deaf (hearing aids)) | 882 per 1000 (15/17) | 697 per 1000 (503 to 979) | RR 0.79 (0.57 to 1.11) | 37 (1 RCT) | VERY LOW | Study limitations (‐1): 5/18 surviving infants were not assessed at 3 years Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with very small sample size | |
| Death or disability at latest follow‐up (1 to 3 years) (defined as GMDS quotient ≤ 70, cerebral palsy, blind (VA < 6/60) or deaf (hearing aids)) | 750 per 1000 (15/20) | 713 per 1000 (495 to 1035) | RR 0.95 (0.66 to 1.38) | 41 (1 RCT) | VERY LOW | Study limitations (‐1): 5/18 surviving infants were not assessed at 3 years Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with very small sample size | |
| Neonatal care: fluid therapy | |||||||
| Volume vs no treatment for prevention of morbidity and mortality in very preterm infants (Osborn 2004) | Severe neurodevelopmental disability in survivors at 2 years (defined as blind, dead, unable to walk, DQ > 3 SD below the mean, or another severe disability) | 141 per 1000 (29/205) | 113 per 1000 (74 to 174) | RR 0.80 (0.52 to 1.23) | 604 (1 RCT) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect |
| Gelatin vs fresh frozen plasma for prevention of morbidity and mortality in very preterm infants (Osborn 2004) | 113 per 1000 (23/203) | 112 per 1000 (65 to 195) | RR 0.99 (0.57 to 1.72) | 399 (1 RCT) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect | |
| Volume vs no treatment for prevention of morbidity and mortality in very preterm infants (Osborn 2004) | Death or severe neurodevelopmental disability in survivors at 2 years (defined as blind, dead, unable to walk, DQ > 3 SD below the mean, or another severe disability) | 318 per 1000 (82/258) | 318 per 1000 (254 to 394) | RR 1.00 (0.80 to 1.24) | 776 (1 RCT) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect |
| Gelatin vs fresh frozen plasma for prevention of morbidity and mortality in very preterm infants (Osborn 2004) | 300 per 1000 (77/257) | 333 per 1000 (258 to 428) | RR 1.11 (0.86 to 1.43) | 518 (1 RCT) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect | |
| Neonatal care: patent ductus arteriosus | |||||||
| Prophylactic indomethacin vs placebo for preventing mortality and morbidity in preterm infants (Fowlie 2010) | Death or severe neurodevelopmental disability at 18 to 36 months (defined as any 1 or a combination of the following: non‐ambulant cerebral palsy, developmental delay (DQ < 70), auditory and visual impairment) | 400 per 1000 (299/748) | 407 per 1000 (360 to 460) | RR 1.02 (0.90 to 1.15) | 1491 (3 RCTs) | MODERATE | Study limitations (‐1): 2 RCTs at unclear risk of attrition bias (> 25% loss to follow‐up) |
| Neonatal care: blood disorders | |||||||
| Erythropoietin vs placebo for preventing red blood cell transfusion in preterm and/or low birthweight infants (Ohlsson 2014) | Any neurodevelopmental impairment at 18 to 22 months' corrected age (in children examined) (not defined in review; definition from trial manuscript: 1 of the following: MDI < 70, PDI < 70, moderate or severe cerebral palsy, blindness, or deafness) | 451 per 1000 (23/51) | 437 per 1000 (280 to 681) | RR 0.97 (0.62 to 1.51) | 99 (1 RCT) | VERY LOW | Study limitations: 1 RCT at unclear risk of selection bias and high risk of attrition bias (˜73% follow‐up) Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with small sample size |
| Transfusion at a restrictive vs a liberal haemoglobin threshold for preventing morbidity and mortality in very low birthweight infants (Whyte 2011) | Any neurosensory impairment at 18 to 21 months' follow‐up among survivors (defined as cognitive delay (MDI < 70), cerebral palsy, severe visual impairment, severe hearing impairment) | 220 per 1000 (37/168) | 289 per 1000 (198 to 418) | RR 1.31 (0.90 to 1.90) | 328 (1 RCT) | LOW | Study limitations (‐1): 1 RCT at high risk of performance bias and unclear risk of reporting bias Imprecision (‐1): wide CI crossing line of no effect |
| Death or severe morbidity at 18 to 21 months' follow‐up (defined as cognitive delay (MDI < 70), cerebral palsy, severe visual impairment, severe hearing impairment) | 385 per 1000 (82/213) | 450 per 1000 (362 to 566) | RR 1.17 (0.94 to 1.47) | 421 (1 RCT) | LOW | Study limitations (‐1): 1 RCT at high risk of performance bias and unclear risk of reporting bias Imprecision (‐1): wide CI crossing line of no effect | |
| Death or severe morbidity at 18 to 21 months' follow‐up (defined as cognitive delay (MDI < 85), cerebral palsy, severe visual impairment, severe hearing impairment) | 498 per 1000 (106/213) | 602 per 1000 (503 to 717) | RR 1.21 (1.01 to 1.44) | 421 (1 RCT) | MODERATE | Study limitations (‐1): 1 RCT at high risk of performance bias and unclear risk of reporting bias | |
| Neonatal care: nitric oxide | |||||||
| Inhaled NO vs placebo for respiratory failure in preterm infants (entry before 3 days based on oxygenation) (Barrington 2010) | Neurodevelopmental disability at 18 to 22 months (defined as moderate or severe cerebral palsy, blind, deaf, BSID MDI < 70, or PDI < 70) | 455 per 1000 (50/110) | 477 per 1000 (355 to 636) | RR 1.05 (0.78 to 1.40) | 208 (2 RCTs) | LOW | Imprecision (‐2): wide CI crossing line of no effect; small sample sizes |
| Inhaled NO vs placebo or no treatment for respiratory failure in preterm infants (entry after 3 days based on BPD risk) (Barrington 2010) | Neurodevelopmental disability at 2 years' corrected age or 30 months (defined as 1 RCT: moderate or severe cerebral palsy, blind, deaf, BSID MDI < 70, or PDI < 70; 1 RCT: cerebral palsy, BSID MDI or PDI < 71, or sensorineural impairment) | 480 per 1000 (119/248) | 432 per 1000 (355 to 523) | RR 0.90 (0.74 to 1.09) | 498 (2 RCTs) | LOW | Study limitations (‐1): 1 RCT with no blinding of intervention or outcome measurement Imprecision (‐1): wide CI crossing line of no effect; small sample sizes |
| Inhaled NO vs placebo for respiratory failure in preterm infants (studies of routine use in intubated preterm infants) (Barrington 2010) | Neurodevelopmental disability at 1 or 2 years' corrected age (defined as 1 RCT: cerebral palsy, blind, severe hearing loss, BSID MDI < 70, or PDI < 70; 1 RCT: cerebral palsy, bilateral blindness, bilateral hearing loss, or BSID score > 2 SD below the mean) | 364 per 100 (104/286) | 327 per 1000 (262 to 411) | RR 0.90 (0.72 to 1.13) | 593 (2 RCT) | VERY LOW | Study limitations (‐1): 2 RCTs with 74% to 82% follow‐up Imprecision (‐1): wide CI crossing line of no effect Inconsistency (‐1): substantial heterogeneity I² = 83% |
| Inhaled nitric oxide vs control for respiratory failure in infants born at or near term (Finer 2006) | Neurodevelopmental disability among survivors at 13 or 18 to 24 months (defined as 1 RCT: cerebral palsy, BSID MDI or PDI < 2 SD below the mean, blind or hearing impaired; or 1 RCT: cerebral palsy, > 2 mild (mild neurological abnormalities; mild reductions in BSID scores 1 to 2 SD below the mean), or at least 1 severe impairment) | 265 per 1000 (48/181) | 257 per 1000 (175 to 382) | RR 0.97 (0.66 to 1.44) | 301 (2 RCTs) | LOW | Study limitations (‐1): 1 RCT masking of allocation, masking of outcomes, and completeness of follow‐up 'can't tell' Imprecision (‐1): wide CI crossing line of no effect |
| Neonatal care: apnoea | |||||||
| Caffeine vs placebo for apnoea in preterm infants (Henderson‐Smart 2010b) | Death or major disability at 18 to 21 months' corrected age (defined as cognitive delay, cerebral palsy, deafness, or blindness) | 417 per 1000 (153/367) | 354 per 1000 (296 to 421) | RR 0.85 (0.71 to 1.01) | 767 (1 RCT) | LOW | Study limitations (‐1): results based on 1 RCT subgroup from post hoc subgroup analyses (randomisation not stratified according to indication for inclusion) Imprecision (‐1): wide CI crossing line of no effect |
| Caffeine vs placebo for prevention of apnoea in preterm infants (Henderson‐Smart 2010c) | Death or major disability at 18 to 21 months' corrected age (not defined in review; definition from trial manuscript: cerebral palsy, cognitive delay, severe hearing loss, or bilateral blindness) | 431 per 1000 (88/204) | 431 per 1000 (345 to 535) | RR 1.00 (0.80 to 1.24) | 423 (1 RCT) | LOW | Study limitations (‐1): results based on 1 RCT subgroup from post hoc subgroup analyses (randomisation not stratified according to indication for inclusion) Imprecision (‐1): wide CI crossing line of no effect |
| Neonatal care: respiratory distress syndrome | |||||||
| Inositol supplementation (repeat doses) vs placebo in preterm infants at risk for or having respiratory distress syndrome (Howlett 2015) | Major neural developmental impairment at 1 year corrected age (defined as sensory deficit, cerebral palsy, developmental delay, severe hypotonia) | 178 per 1000 (13/73) | 94 per 1000 (43 to 207) | RR 0.53 (0.24 to 1.16) | 169 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at unclear risk of selection, performance, detection, and reporting bias, and at high risk of other bias Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with small sample size |
| Animal‐derived surfactant extract vs no treatment for treatment of respiratory distress syndrome (Seger 2009) | Major developmental disability in survivors at 1 and 2 years' corrected age (defined as severe forms of cerebral palsy, blindness, deafness requiring hearing aids, or GMDS DQ < 70) | 34 per 1000 (1/29) | 114 per 1000 (5 to 923) | RR 3.30 (0.14 to 26.78) | 73 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with no blinding of intervention; and blinding of outcome measurement not reported Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Neonatal care: mechanical ventilation | |||||||
| Continuous distending pressure vs standard care for respiratory distress in preterm infants (Ho 2015) | Death or severe disability at 9 to 15 years (not defined in review; severe disability as defined below) | 158 per 1000 (3/19) | 210 per 1000 (54 to 816) | RR 1.33 (0.34 to 5.17) | 38 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at unclear risk of selection and attrition bias and high risk of performance bias Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Severe disability at 9 to 15 years (not defined in review; definition from trial manuscript: unable to undertake activity without aids or assistance most of the time, or completely dependent on carer: WASI ≤ 69; GMF level 4 to 5, arms: needs assistance to feed and dress; VA < 6/60, gross movement/light and dark only or worse; hearing loss not corrected with age; parent and teacher overall difficulties (Q26), "Yes" and impact score 6 to 10 parent and 3 to 6 teacher; or other condition needs supervision/aid constantly ‐ includes continuous home oxygen; communication severely limited) | 158 per 1000 (3/19) | 167 per 1000 (38 to 722) | RR 1.06 (0.24 to 4.57) | 37 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at unclear risk of selection and attrition bias and high risk of performance bias Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT | |
| Any disability at 9 to 15 years (not defined in review; definition from trial manuscript: mild: some loss of function but able to function independently; moderate: aids or assistance needed for some tasks. Moderate difficulty in doing some activities; severe: unable to undertake activity without aids or assistance most of the time, or completely dependent on carer; includes neuromotor components includes GMF levels 1 to 5) | 632 per 1000 (12/19) | 392 per 1000 (196 to 764) | RR 0.62 (0.31 to 1.21) | 37 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at unclear risk of selection and attrition bias and high risk of performance bias Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT | |
| Prophylactic methylxanthines (caffeine) vs placebo for endotracheal extubation in preterm infants (Henderson‐Smart 2010) | Death or major disability at 18 to 21 months' corrected age (defined as cognitive delay, cerebral palsy, deafness, or blindness) | 525 per 1000 (189/360) | 446 per 1000 (383 to 520) | RR 0.85 (0.73 to 0.99) | 676 (1 RCT) | MODERATE | Study limitations (‐1): results based on 1 RCT subgroup from post hoc subgroup analyses (randomisation not stratified according to indication for inclusion) |
| Volume‐targeted vs pressure‐limited ventilation in the neonate (Wheeler 2010) | Severe disability (any definition) at 6 to 18 months and 22 months (definitions not reported in review; definitions from trial manuscripts: 1 RCT: abnormal neurological evaluation (gross or fine motor delay) or BSID MDI < 70; 1 RCT: cerebral palsy severe enough to hamper gross motor activity, deafness needing hearing aids, registered blind or partially sighted) | 176 per 1000 (18/102) | 152 per 1000 (83 to 281) | RR 0.86 (0.47 to 1.59) | 209 (2 RCTs) | LOW | Indirectness (‐1): post hoc analysis including 2 RCTs with varied definitions Imprecision (‐1): wide CI crossing line of no effect (post hoc analysis in review) |
| Severe disability (any definition) at 22 months or death (definition not reported in review; definition from trial manuscript: cerebral palsy severe enough to hamper gross motor activity, deafness needing hearing aids, registered blind or partially sighted) | 327 per 1000 (17/52) | 177 per 1000 (88 to 347) | RR 0.54 (0.27 to 1.06) | 109 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT (post hoc analysis in review) | |
| Neonatal care: bronchopulmonary dysplasia | |||||||
| Early (< 8 days) postnatal corticosteroids vs placebo or no treatment for preventing chronic lung disease in preterm infants (Doyle 2014b) | Major neurosensory disability at 18 to 22 months to 53 months (variable criteria reported in review: 1 RCT: non‐ambulant cerebral palsy, global retardation (not specified), blindness, or deafness; 1 RCT: moderate or severe cerebral palsy, blindness, deafness, or BSID MDI or PDI < ‐2 SD; 1 RCT: cerebral palsy, BSID MDI or PDI < 71, blindness or deafness; 1 RCT: severe motor dysfunction (child non‐ambulant), or BSID MDI or PDI <‐2 SD; 2 RCTs: cerebral palsy, blindness, deafness, or developmental delay (BSID MDI < 70 (< ‐2 SD) or GMDS DQ < 70); 1 RCT: cerebral palsy, functional blindness, functional deafness, developmental delay (BSID MDI < 70 (<‐2 SD)), or motor delay (BSID PDI < 70 (<‐2 SD)) | 199 per 1000 (121/607) | 231 per 1000 (187 to 285) | RR 1.16 (0.94 to 1.43) | 1233 (7 RCTs) | LOW | Study limitations (‐1): 2 RCTs at unclear risk of selection bias; 1 RCT at high risk of performance and detection bias Imprecision (‐1): wide CI crossing line of no effect |
| Major neurosensory disability in survivors examined at 18 to 22 months to 53 months (variable criteria as above) | 307 per 1000 (121/394) | 350 per 1000 (289 to 424) | RR 1.14 (0.94 to 1.38) | 799 (7 RCTs) | LOW | Study limitations (‐1): 2 RCTs at unclear risk of selection bias; 1 RCT at high risk of performance and detection bias Imprecision (‐1): wide CI crossing line of no effect | |
| Death or major neurosensory disability at 18 to 22 months to 53 months (variable criteria as above) | 466 per 1000 (283/607) | 490 per 1000 (434 to 545) | RR 1.05 (0.93 to 1.17) | 1233 (7 RCTs) | MODERATE | Study limitations (‐1): 2 RCTs at unclear risk of selection bias; 1 RCT at high risk of performance and detection bias | |
| Moderately early (7‐14 days) postnatal corticosteroids vs placebo for preventing chronic lung disease in preterm infants (Halliday 2003) | Major neurosensory disability at 15 months' corrected age up to 90 months (variable criteria reported in review: 1 RCT: any of cerebral palsy or a BSID MDI or PDI < ‐ 1 SD; 1 RCT: not specified) | 98 per 1000 (4/41) | 123 per 1000 (44 to 340) | RR 1.26 (0.45 to 3.49) | 96 (2 RCTs) | VERY LOW | Study limitations (‐1): 1 RCT with 70% follow‐up and unclear blinding of outcome assessment Imprecision (‐2): wide CI crossing line of no effect; small sample sizes |
| Major neurosensory disability in survivors assessed at 15 months' corrected age up to 90 months (variable criteria reported in review as above) | 174 per 1000 (4/23) | 155 per 1000 (66 to 365) | RR 0.89 (0.38 to 2.10) | 56 (2 RCTs) | VERY LOW | Study limitations (‐1): 1 RCT with 70% follow‐up and unclear blinding of outcome assessment Imprecision (‐2): wide CI crossing line of no effect; small sample sizes | |
| Death or major neurosensory disability at 15 months' corrected age up to 90 months (variable criteria reported in review as above) | 366 per 1000 (15/41) | 373 per 1000 (241 to 571) | RR 1.02 (0.66 to 1.56) | 96 (2 RCTs) | VERY LOW | Study limitations (‐1): 1 RCT with 70% follow‐up and unclear blinding of outcome assessment Imprecision (‐2): wide CI crossing line of no effect; small sample sizes | |
| Late (> 7 days) postnatal corticosteroids vs placebo or no treatment for chronic lung disease in preterm infants (Doyle 2014) | Major neurosensory disability at 1 year corrected age up to 11 years (variable criteria reported in review: 1 RCT: non‐ambulant cerebral palsy, < 50% of age level on the Minnesota CDI, or predicted special schooling for sensory or other impairment; 1 RCT: abnormal neurological examination (i.e. cerebral palsy), cognitive delay (IQ < 71) or not in a regular classroom; 1 RCT: severe disability ‐ bilateral blindness, cerebral palsy with the child unlikely ever to walk or BSID MDI < 55 (< ‐3 SD)) or moderate disability ‐ deafness, cerebral palsy in children not walking at 2 years but expected to walk, or MDI from 55 to < 70 (‐3 SD to < ‐2 SD); 1 RCT: cerebral palsy, blindness, deafness requiring hearing aids or worse, or developmental delay (defined as BSID MDI < 70); 1 RCT: more than mild cerebral palsy, blindness, deafness, or needing extra help with schooling; 1 RCT: blindness, cerebral palsy or a BSID MDI < 70 OR cerebral palsy or mental retardation (IQ < 70 on either the DAS or the WISC‐III and a VABS composite score < 70); 1 RCT: not specified; 1 RCT moderate or severe cerebral palsy, bilateral blindness, deafness or an MDI < 2 SD | 169 per 1000 (54/320) | 197 per 1000 (143 to 270) | RR 1.17 (0.85 to 1.60) | 655 (8 RCTs) | LOW | Study limitations (‐1): 3 RCTs with unclear risk of selection bias; 3 RCTs with follow‐up rates 60% to 78% Imprecision (‐1): wide CI crossing line of no effect |
| Major neurosensory disability in survivors assessed at 1 year corrected age up to 11 years (variable criteria reported in review as above) | 231 per 1000 (54/234) | 254 per 1000 (187 to 346) | RR 1.10 (0.81 to 1.50) | 480 (8 RCTs) | LOW | Study limitations (‐1): 3 RCTs with unclear risk of selection bias; 3 RCTs with follow‐up rates 60% to 78% Imprecision (‐1): wide CI crossing line of no effect | |
| Death or major neurosensory disability at 1 year corrected age up to 11 years (variable criteria reported in review as above) | 375 per 1000 (120/320) | 390 per 1000 (323 to 473) | RR 1.04 (0.86 to 1.26) | 655 (8 RCTs) | LOW | Study limitations (‐1): 3 RCTs with unclear risk of selection bias; 3 RCTs with follow‐up rates 60% to 78% Imprecision (‐1): wide CI crossing line of no effect | |
| Supplemental vitamin A vs a sham injection to prevent mortality and short‐ and long‐term morbidity in very low birthweight infants (Darlow 2016) | Neurodevelopmental impairment at 18 to 24 months (defined as BSID‐II MDI < 70, PDI < 70, any cerebral palsy, blind in both eyes, or bilateral hearing aids ) | 481 per 1000 (128/266) | 428 per 1000 (356 to 520) | RR 0.89 (0.74 to 1.08) | 538 (1 RCT) | LOW | Imprecision (‐2): "Concerning imprecision: does not met the optimal information size criteria" (graded by review authors themselves) |
| Death or neurodevelopmental impairment at 18 to 24 months (defined as BSID‐II MDI < 70, PDI < 70, any cerebral palsy, blind in both eyes, or bilateral hearing aids) | 596 per 1000 (204/342) | 549 per 1000 (483 to 626) | RR 0.92 (0.81 to 1.05) | 687 (1 RCT) | MODERATE | Imprecision (‐1): wide CIs crossing line of no effect | |
| Neonatal care: necrotising enterocolitis | |||||||
| Probiotics vs control (distilled water) for prevention of necrotising enterocolitis in preterm infants (AlFaleh 2014) | Mental retardation and cerebral palsy at 6 years | 47 per 1000 (2/43) | 47 per 1000 (7 to 323) | RR 1.02 (0.15 to 6.94) | 85 (1 RCT) | VERY LOW | Study limitation (‐1): 1 RCT at unclear risk for selection, performance, and detection bias; and high risk of attrition and reporting bias Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Arginine supplementation vs placebo for prevention of necrotising enterocolitis in preterm infants (Shah 2007) | Major neurodevelopmental disability at 36 months' post‐menstrual age (definition not reported in review; definition from trial manuscript: presence of 1 or more of cerebral palsy, cognitive delay (index < 70), bilateral blindness, bilateral hearing loss requiring aids) | 127 per 1000 (9/71) | 82 per 1000 (29 to 232) | RR 0.65 (0.23 to 1.83) | 132 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Neonatal care: fungal infections | |||||||
| Systemic antifungal agent vs placebo to prevent mortality and morbidity in very low birthweight infants (Cleminson 2015) | Neurodevelopmental impairment (composite) at 18 to 22 months (defined as at least 1 of (i) BSID‐III cognition composite score < 70, (ii) cerebral palsy, (iii) deafness or, (iv) blindness) | 274 per 1000 (23/84) | 309 per 1000 (194 to 496) | RR 1.13 (0.71 to 1.81) | 171 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Neonatal care: herpes simplex | |||||||
| Vidarabine vs placebo for treatment of herpes simplex virus infection in neonates (Jones 2009) | Abnormal neurodevelopment at approximately 1 year of age (not defined in review; definition from trial manuscript: spasticity or hemiparesis only; or combinations of microcephaly, paresis, spasticity, seizures, blindness, or deafness) | 214 per 1000 (6/28) | 321 per 1000 (133 to 782) | RR 1.50 (0.62 to 3.65) | 56 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with design limitations (method of randomisation not stated) Imprecision (‐2): wide CIs crossing line of no effect; 1 small RCT |
| Abnormal neurodevelopment or death at approximately 1 year of age (not defined in review; definition from trial manuscript as above) | 750 per 1000 (21/28) | 645 per 1000 (450 to 915) | RR 0.86 (0.60 to 1.22) | 56 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with design limitations (method of randomisation not stated) Imprecision (‐2): wide CIs crossing line of no effect; 1 small RCT | |
| Aciclovir vs vidarabine for treatment of herpes simplex virus infection in neonates (Jones 2009) | Abnormal neurodevelopment at approximately 1 year of age (not defined in review; definition from trial manuscript: mild impairment: only occular sequelae; moderate neurological impairment: hemiparesis or a persistent seizure disorder and no more than a 3‐month developmental delay; severe neurological sequelae: microcephaly, spastic quadriplegia, chorioretinitis or blindness, and a serious developmental delay of > 3 months according to the DDST) | 263 per 1000 (25/95) | 216 per 1000 (132 to 353) | RR 0.82 (0.50 to 1.34) | 202 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with design limitations (inadequate allocation concealment) Imprecision (‐2): wide CIs crossing line of no effect; 1 small RCT |
| Abnormal neurodevelopment or death at approximately 1 year of age (not defined in review definition from trial manuscript as above) | 463 per 1000 (44/95) | 366 per 1000 (264 to 509) | RR 0.79 (0.57 to 1.10) | 202 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with design limitations (inadequate allocation concealment) Imprecision (‐2): wide CIs crossing line of no effect; 1 small RCT | |
| Neonatal care: jaundice | |||||||
| Prophylactic phototherapy vs standard care for preventing jaundice in preterm or low birthweight infants (Okwundu 2012) | Neurodevelopmental impairment at 18 to 22 months (defined as blindness, severe hearing loss, and moderate or severe cerebral palsy) | 305 per 1000 (275/902) | 259 per 1000 (226 to 302) | RR 0.85 (0.74 to 0.99) | 1804 (1 RCT) | MODERATE | Study limitations (‐1): 1 RCT with high risk of attrition bias |
| Neonatal care: hypoglycaemia | |||||||
| Dextrose gel vs placebo for treatment of hypoglycaemia in newborn infants (Weston 2016) | Major neurosensory disability at 2 years (defined as any of the following: legal blindness, sensorineural deafness requiring hearing aids, moderate or severe cerebral palsy, developmental delay/intellectual impairment (defined as DQ < 2 SD below the mean)) | 11 per 1000 (1/94) | 67 per 1000 (8 to 543) | RR 6.27 (0.77 to 51.03) | 184 (1 RCT) | VERY LOW | Study limitations (‐1): "Evidence is based on a single trial" Imprecision (‐2):"Wide confidence intervals, low event rates and small sample sizes are suggestive of imprecision: (graded by review authors themselves) |
| Developmental disability at 2 years (defined as cognitive, language, or motor score below ‐1 SD, or cerebral palsy, blindness, or deafness) | 32/94 | 34/90 | RR 1.11 (0.75 to 1.63) | 184 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT with 78% follow‐up Imprecision: wide CI crossing line of no effect; 1 small RCT | |
| Neonatal care: parenteral feeding | |||||||
| Glutamine supplementation vs placebo to prevent morbidity and mortality in preterm infants (Moe‐Byrne 2016) | Neurodevelopmental impairment at 2 years post term (defined as BSID‐II MDI ≤ 85, PDI ≤ 85, cerebral palsy, blindness in 1 or both eyes, or hearing loss requiring amplification) | 375 per 1000 (12/32) | 401 per 1000 | RR 1.07 (0.59 to 1.92) | 72 (1 RCT) | LOW | Imprecision (‐2): "Total sample size = 72" (graded by review authors themselves) |
| Abbreviations: BSID: Bayley Scales of Infant Development; CDI: Child Development Inventory; CI: confidence interval; DAS: Differential Ability Scales; DDST: Denver Developmental Screening Test; DQ: development quotient; GMDS: Griffiths Mental Development Scales; GMF: gross motor function; GRADE: Grades of Recommendation, Assessment, Development and Evaluation; IQ: intelligence quotient; MDI: Mental Development Index; PDI: Psychomotor Development Index; RCT: randomised controlled trial; RR: risk ratio; SD: standard deviation; VA: visual acuity; VABS: Vineland Adaptive Behaviour Scales; WASI: Wechsler Abbreviated Scale of Intelligence; WISC: Wechsler Intelligence Scale for Children. | |||||||
| Intervention and comparison | Outcome | Assumed risk with comparator | Corresponding risk with intervention | Relative effect (95% CI) | Number of participants (trials) | Quality of the evidence (GRADE) | Comments |
| Neonatal care: asphyxia | |||||||
| Therapeutic hypothermia vs standard care for newborns with hypoxic‐ischaemic encephalopathy (Jacobs 2013) | Neuromotor delay (BSID PDI > 2 SD below mean) in survivors assessed at 18 to 24 months | 349 per 1000 (104/298) | 262 per 1000 (206 to 328) | RR 0.75 (0.59 to 0.94) | 657 (6 RCTs) | HIGH | Not downgraded |
| Neonatal care: blood disorders | |||||||
| Erythropoietin vs placebo for preventing red blood cell transfusion in preterm and/or low birthweight infants (Ohlsson 2014) | PDI < 70 at 18 to 22 months' corrected age (in children examined) | 133 per 1000 (6/45) | 311 per 1000 (131 to 737) | RR 2.33 (0.98 to 5.53) | 90 (1 RCT) | VERY LOW | Study limitations: 1 RCT at unclear risk of selection bias and high risk of attrition bias (˜73% follow‐up) Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with small sample size |
| Neonatal care: pulmonary hypertension | |||||||
| Endothelin receptor antagonists vs placebo for persistent pulmonary hypertension in term and late preterm infants (More 2016) | Adverse neurological outcomes at 6 months (defined as clinical or electrographically proven seizures, abnormal muscle tone, abnormal deep tendon reflexes, delayed motor milestones, or abnormal auditory brainstem response) | 286 per 1000 (4/14) | 20 per 1000 (0 to 343) | RR 0.07 (0.00 to 1.20) | 37 (1 RCT) | LOW | Study limitation (‐1): 8/23 infants in the placebo group were excluded from analysis Imprecision (‐1): single RCT, small sample size (graded by review authors themselves) |
| Neonatal care: resuscitation | |||||||
| Room air vs 100% oxygen for resuscitation of infants at birth (Tan 2005) | Not walking in those followed up at 18 to 24 months | 107 per 1000 (13/122) | 110 per 1000 (4 to 240) | RR 1.03 (0.04 to 2.25) | 213 (1 RCT) | VERY LOW | Study limitations (‐2): 1 qRCT with no blinding, and < 70% follow‐up Imprecision (‐1): wide CI crossing line of no effect |
| Neonatal care: nitric oxide | |||||||
| Inhaled NO vs placebo for respiratory failure in preterm infants (studies of routine use in intubated preterm infants) (Barrington 2010) | BSID MDI or PDI < ‐ 2 SD at 2 years' corrected age | 412 per 1000 (28/68) | 231 per 1000 (136 to 383) | RR 0.56 (0.33 to 0.93) | 138 (1 RCT) | MODERATE | Study limitations (‐1): 1 small RCT with 82% follow‐up |
| Inhaled nitric oxide vs control for respiratory failure in infants born at or near term (Finer 2006) | BSID PDI > 2 SD below the mean at 13 or 18 to 24 months | 148 per 1000 (25/169) | 161 per 1000 (86 to 300) | RR 1.09 (0.58 to 2.03) | 283 (2 RCTs) | LOW | Study limitations (‐1): 1 RCT masking of allocation, masking of outcomes, and completeness of follow‐up 'can't tell' Inconsistency (‐1): substantial heterogeneity (I² = 77%) Note: error in review for Ninos 1996 data; intervention and control group data switched; this has been rectified in this analysis |
| Neonatal care: respiratory distress syndrome | |||||||
| Inositol supplementation (repeat doses) vs placebo in preterm infants at risk for or having respiratory distress syndrome (Howlett 2015) | Minor neural developmental impairment at 1 year corrected age (defined as sensorimotor abnormality and/or developmental delay) | 137 per 1000 (10/73) | 115 per 1000 (52 to 255) | RR 0.84 (0.38 to 1.86) | 169 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at unclear risk of selection, performance, detection, and reporting bias, and at high risk of other bias Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with small sample size |
| Neonatal care: mechanical ventilation | |||||||
| Volume‐targeted vs pressure‐limited ventilation in the neonate (Wheeler 2010) | Gross Motor Developmental Issue (any definition) at 6 to 18 months (defined as gross motor delay) | 172 per 1000 (11/64) | 172 per 1000 (81 to 368) | RR 1.00 (0.47 to 2.14) | 128 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT (post hoc analysis in review) |
| Neonatal care: bronchopulmonary dysplasia | |||||||
| Early (< 8 days) postnatal corticosteroids vs placebo for preventing chronic lung disease in preterm infants (Doyle 2014b) | BSID PDI < ‐ 2 SD at 18 to 22 months or 25 months | 146 per 1000 (61/419) | 170 per 1000 (124 to 233) | RR 1.17 (0.85 to 1.60) | 842 (3 RCTs) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect |
| BSID PDI < ‐ 2 SD in tested survivors at 18 to 22 months or 25 months | 232 per 1000 (61/263) | 271 per 1000 (202 to 364) | RR 1.17 (0.87 to 1.57) | 528 (3 RCTs) | MODERATE | Imprecision (‐1): wide CI crossing line of no effect | |
| Late (> 7 days) postnatal corticosteroids vs placebo or no treatment for chronic lung disease in preterm infants (Doyle 2014) | BSID PDI < ‐ 2 SD at 1 year corrected age | 180 per 1000 (11/61) | 141 per 1000 (61 to 325) | RR 0.78 (0.34 to 1.80) | 118 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with small sample size |
| BSID PDI < ‐ 2 SD in survivors assessed at 1 year corrected age | 256 per 1000 (11/43) | 171 per 1000 (77 to 384) | RR 0.67 (0.30 to 1.50) | 90 (1 RCT) | LOW | Imprecision (‐2): wide CI crossing line of no effect; 1 RCT with small sample size | |
| Early inhaled corticosteroids vs placebo for preventing chronic lung disease in ventilated very low birthweight preterm neonates (Shah 2012) | Mean developmental index on BSID‐II < 2 SD of the mean (age not reported in review;from trial manuscript: 3 years) | 143 per 1000 (4/28) | 179 per 1000 (53 to 596) | RR 1.25 (0.37 to 4.17) | 56 (1 RCT) | VERY LOW | Study limitations (‐1): 1 RCT at unclear risk of selection bias and detection bias Imprecision (‐2): wide CI crossing line of no effect; 1 small RCT |
| Neonatal care: other | |||||||
| Early developmental intervention vs standard follow‐up post hospital discharge to prevent motor and cognitive impairment in preterm infants (Spittle 2015) | Motor outcome at school age (5 years) (defined as low score on Movement ABC) | 378 per 1000 (51/135) | 423 per 1000 (329 to 544) | RR 1.12 (0.87 to 1.44) | 333 (2 RCTs) | LOW | Study limitations (‐1): 2 RCTs at high risk of attrition bias and unclear risk of performance bias Imprecision (‐1): wide CI crossing line of no effect |
| Abbreviations: BSID: Bayley Scales of Infant Development; CI: confidence interval; GRADE: Grades of Recommendation, Assessment, Development and Evaluation; MDI: Mental Development Index; Movement ABC: Movement Assessment Battery for Children; PDI: Psychomotor Development Index; qRCT: quasi‐randomised controlled trial; RCT: randomised controlled trial; RR: risk ratio; SD: standard deviation | |||||||

