نقش آنتیبیوتیکهای ماکرولیدی در درمان برونشکتازی
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع مطالعات در انتظار ارزیابی
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Aims: to investigate whether 1 year of long‐term low‐dose macrolide treatment added to standard therapy is effective in reducing exacerbation frequency in patients with non‐CF bronchiectasis Design: randomised, double‐blind, placebo‐controlled trial Total study duration: 30 months Number of study centres and locations: 14, Netherlands Study setting: outpatient clinics Methods of recruitment: outpatient clinics at each study centre by the pulmonary physician or the study investigator Withdrawals: 1 in each group owing to adverse events Study start/end dates: April 2008/September 2010 Analysis by intent‐to‐treat: yes | |
| Participants | 83 adults randomised Inclusion criteria: individuals 18 years of age or older with non‐CF bronchiectasis diagnosed by plain bronchography or high‐resolution computed tomography, ≥ 3 lower respiratory tract infections (LRTIs) treated with oral or intravenous antibiotics in the preceding year, and ≥ 1 sputum culture yielding ≥ 1 bacterial respiratory pathogen in the preceding year Exclusion criteria: prolonged (> 4 weeks) macrolide therapy during the previous 3 months, oral or intravenous corticosteroids within 30 days of screening, or any antimicrobial treatment for an LRTI in the previous 2 weeks Mean age: intervention group: 59.9 years; control group: 64.6 years Gender: intervention group: 25 females, 18 males; control group: 28 females, 12 males Bronchiectasis diagnosis: plain bronchography or HRCT Severity of condition: not reported Baseline lung function: FEV1 (% predicted): intervention group: 77.7, control group: 82.7; FVC (% predicted): intervention group: 91.9, control group: 98.5 Smoking history: 2% current, 44% former, 54% never Baseline imbalances: no statistically significant differences between groups | |
| Interventions | Intervention group: azithromycin (n = 43) Dose: 250 mg; delivery mode: oral; frequency: 1/d; duration: 52 weeks Control group: placebo (n = 40) Placebo tablets indistinguishable from azithromycin were manufactured by a licensed trial pharmacy. Adherence: empty blister‐pack count: intervention group: 96.5%; control group: 98% Run‐in phase: following randomisation, participants observed for clinical stability for 2 weeks Run‐out phase: variable run‐out period of ≥ 90 days after 1 year of intervention | |
| Outcomes | Primary: number of infectious exacerbations, defined as an increase in respiratory symptoms requiring antibiotic treatment. Two types of exacerbations ‐ a protocol‐defined exacerbation (PDE) and a non‐PDE Secondary: lung function, CRP level, WBC count, microbiological evaluation, LRTI, HRQoL, and adverse events Post hoc analysis: time to a first exacerbation | |
| Notes | Power calculation: assuming that azithromycin would reduce the number of exacerbations by at least one‐third, a 1‐sided significance level of P = 0.05, with 80% power and estimated 20% dropout = total of 90 patients, for 36 per group Trial registration: clinicaltrials.gov Identifier: NCT00415350 Conflicts of interest: Dr. Boersma reported serving on an advisory board, and receiving payment from Pfizer, for an educational presentation. No other review authors reported COIs. Funders: Dr. Altenberg and Dr. Boersma were supported by a research grant from the Forest Medical School, an independent scientific institution based in the Alkmaar Medical Centre. The study was also supported by an unrestricted research grant from GlaxoSmithKline, and Teva Netherlands supplied the azithromycin tablets. Role of the sponsors: Funders had no role in the design and conduct of the study; collection, analysis, and interpretation of data; or preparation, review, or approval of the manuscript. Ethical approval: yes Conclusions: Macrolide maintenance therapy was effective in reducing exacerbations in patients with non‐CF bronchiectasis. In this trial, azithromycin treatment resulted in improved lung function and better quality of life but involved an increase in gastrointestinal adverse effects and high rates of macrolide resistance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Permuted block randomisation was performed centrally with equally sized blocks of 10. |
| Allocation concealment (selection bias) | Low risk | Placebo and azithromycin tablets were provided in identical, individually numbered boxes, with each box containing a year's supply of study medication for 1 participant. Numbers on the boxes matched treatment allocation, in accordance with a computer‐generated allocation sequence that was kept in a safe place in the pharmacy providing the study medication. |
| Blinding of participants and personnel (performance bias) | Low risk | All participants were seen by the investigator and were sequentially assigned a subject identification code through double‐blinded allocation to azithromycin or placebo treatment. Placebo tablets were indistinguishable from azithromycin tablets with respect to appearance, feel, and taste. |
| Blinding of outcome assessment (detection bias) | Low risk | Attending physicians reporting study outcomes were blinded to group allocation. It is unlikely that blinding was ineffective. |
| Incomplete outcome data (attrition bias) | Low risk | Balanced between groups with similar reasons for withdrawal |
| Selective reporting (reporting bias) | Low risk | Study protocol prepublished and all prespecified outcomes reported |
| Other bias | Low risk | None identified |
| Methods | Aims: to determine whether roxithromycin would alter clinical outcomes Design: randomised, double‐blind, placebo‐controlled trial Total study duration: 6 months Number of study centres and locations: 1, Thailand Study setting: outpatient department, Songklanagarind Hospital Methods of recruitment: unclear Withdrawals: intervention group: 4, control group: 5 Study start/end dates: March 2011/September 2011 Analysis by intent‐to‐treat: unclear | |
| Participants | 30 adults were randomised. Inclusion criteria: adults aged 15 to 75 years; symptomatic patients, with total symptoms score* ≥ 2 per day; stable clinical state; absence of deterioration in cough, dyspnoea, wheezing, fever, chest pain at least 2 weeks before randomisation Exclusion criteria: adverse drug reaction to macrolides; recent exacerbation within 2 weeks before randomisation; history of macrolide therapy within 2 weeks before randomisation; active malignancy and end‐stage disease, such as chronic heart failure, chronic renal failure, and cirrhosis; inability of patients to perform lung function tests due to haemoptysis, AFB positivity, aortic aneurysm, and unstable angina; women who were lactating Mean age: intervention group: 67 years; control group: 64 years Gender: intervention group: 9 women, 6 men; control group: 14 women, 1 man Bronchiectasis diagnosis: HRCT Severity of condition: intervention group: 13 (range 9‐19); control group: 12 (range 5‐19) (Bhalla) Baseline lung function: FEV1 (% predicted): intervention group: 53.5 ± 13.9; control group: 61.7 ± 19.2; FVC (% predicted): intervention group: 65.4 ± 20; control group: 66.9 ± 14.3 Smoking history: 20% former, 80% never; smoking history in pack‐years: intervention group: 6.7 years; control group: 0.7 years Baseline imbalances: no statistically significant differences between groups | |
| Interventions | Intervention group: roxithromycin (n = 15) Dose: 300 mg; delivery mode: oral; frequency: once daily; duration: 12 weeks Control group: placebo (n = 15) Co‐interventions: mucolytic drugs (93%), SABA (73%), theophylline (63%), and a combination of LABA/ICS (47%) Adherence: not reported Run‐in phase: not reported Run‐out phase: 12‐week wash | |
| Outcomes | Primary: quality of life (SGRQ) Secondary: exacerbations, sputum volume, pulmonary function tests Post hoc analysis: not reported | |
| Notes | Power calculation: estimated 61 patients needed to detect an increment in SGRQ scores of 12% with roxithromycin as compared with placebo with statistical power (1 minus the β value) of 80%, allowing for a type I (α) error of 0.05 Trial registration: not reported Conflicts of interest: not reported Funders: not reported Role of the sponsors: not reported Ethical approval: yes Conclusions: 12‐week roxithromycin 300 mg once daily in symptomatic stable bronchiectatic patients; did not show significant improvement in QoL by SGRQ scores, reduced sputum volume, or improved lung function | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Eligible subjects were randomized (1:1) into the treatment and control groups by block of four randomization method"; insufficient detail |
| Allocation concealment (selection bias) | Unclear risk | "30 patients were randomly allocated"; insufficient detail |
| Blinding of participants and personnel (performance bias) | Unclear risk | Insufficient detail |
| Blinding of outcome assessment (detection bias) | Unclear risk | Insufficient detail |
| Incomplete outcome data (attrition bias) | Unclear risk | 9 patients withdrew (30%), but no further details were reported. |
| Selective reporting (reporting bias) | Unclear risk | The protocol was not prespecified. |
| Other bias | Unclear risk | Details of funding sources were not reported. |
| Methods | Aims: to determine whether long‐term, low‐dose azithromycin would improve pulmonary function and decrease incidences of infection and exacerbation Design: open‐label, cross‐over, randomised controlled (no intervention) trial Total study duration: 12 months Number of study centres and location: 1, USA Study setting: outpatient clinic Methods of recruitment: unclear Withdrawals: 1, who provided insufficient data for analysis Study start/end dates: January 2001/December 2001 Analysis by intent‐to‐treat: no | |
| Participants | 12 adults were randomised. Inclusion criteria: patients aged > 18 years with a clinical diagnosis of bronchiectasis confirmed by HRCT, demonstrating airways larger than accompanying vessels Exclusion criteria: patients with a history of serious intolerance, allergy, or sensitivity to azithromycin or macrolides. In addition, if the investigator believed that the patient may not be able to follow instructions, the patient was excluded. Mean age: 70.8; SD 9.7 years Gender: 6 women, 5 men Bronchiectasis diagnosis: HRCT Severity of condition: not reported Baseline lung function (intervention group, control group): FEV1 (% predicted): 65.3, SD 15.1; FVC (% predicted): 48.5, SD 19.9 Smoking history: present or ex‐smoker: 8; never: 3 Baseline imbalances: not reported | |
| Interventions | Intervention group: azithromycin plus usual medications (n = 8) Dose: 500 mg; delivery mode: oral; frequency: 2/week (Monday and Thursday); duration: 6 months If participants complained of intolerable adverse events from the azithromycin regimen but wanted to continue in the study, their azithromycin regimen was reduced to 250 mg orally every Monday, Wednesday, and Friday. Control group: usual medications alone (n = 3) Adherence: 85% to 108% on azithromycin (1 person took an additional dose) Run‐in phase: 1‐month washout in participants who received azithromycin first Run‐out phase: unclear | |
| Outcomes | Primary: did not state which of the outcomes below was primary Secondary: pulmonary function tests (diary card), PF measurements, 24‐hour sputum volume Post‐hoc analysis: unclear | |
| Notes | Power calculation: By a paired t‐lest power calculation, the original proposed sample size of 30 participants would have provided 92.5% power at an alpha of 0.1 to identify a 50% change in 24‐hour sputum volume. However, only 11 of the 12 enrolled participants completed the study; therefore, the power to identify the same extent of change in 24‐hour sputum volume fell to 56%. Trial registration: not reported Conflicts of interest: no conflicts of interest for 6 study authors. One had received payments from several pharmaceutical companies including Pfizer, Bayer, Abbott, and Bristol Myers Squibb. Funders: The first year of the study was unfunded, although investigators received donations of study medication from local sales representatives. In the second year, a small unrestricted stipend was received from the manufacturer of azithromycin that covered participant incidentals (i.e. travel expenses, extra pulmonary function tests only). Role of the sponsors: unclear Ethical approval: yes Conclusions: The results of this pilot study support past data regarding probable disease‐modifying benefits of long‐term macrolide use in the treatment of individuals with chronic inflammatory pulmonary disorders. Long‐ term therapy with twice‐weekly azithromycin was well tolerated and may provide added benefit for patients with bronchiectasis without the adverse effect of immunosuppression, which is demonstrated with corticosteroids. Given that significant findings were identified in a study with such a limited sample size, additional large‐scale trials are warranted. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Allocation concealment (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Blinding of participants and personnel (performance bias) | High risk | Open‐label study |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Incomplete outcome data (attrition bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Other bias | High risk | "Because of the randomization schedule and less than expected numbers at enrolment, the distribution of patients between the two study phases they received first was heavily biased, with 8 of II (73%) patients receiving the azithromycin phase first". The randomisation schedule was ineffective, with most receiving the active intervention in the first phase. |
| Methods | Aims: to explore the effect of long‐term therapy with azithromycin on airway oxidative stress markers in exhaled breath condensate (EBC) Design: open‐label, randomised controlled (no intervention) trial Total study duration: 12 months Number of study centres and location: 1, Spain Study setting: outpatient clinic Methods of recruitment: invited patients with confirmed diagnosis of bronchiectasis attending clinic at University Hospital La Fe Withdrawals: 6. Numbers per study group not reported Study start/end date: 2005 Analysis by intent‐to‐treat: no | |
| Participants | 36 adults were randomised. Inclusion criteria: stable, without change in medication or symptoms, emergency department visits or hospitalisations in the previous 4 weeks Exclusion criteria: positive sweat test for CF, bronchiectasis secondary to CF, pulmonary surgical processes, immunodeficiency secondary to HIV, malignancy, common variable immunodeficiency, emphysema, allergic bronchopulmonary aspergillosis or diffuse interstitial pulmonary disease, intolerance to macrolides, severe liver disease Mean age: 58 years; intervention group: 57 years; control group: 61 years Gender: intervention group: 9 women, 7 men; control group: 7 women, 7 men Bronchiectasis diagnosis: clinical data and HRCT Severity of condition: intervention group: 22; control group: 31 (Bhalla) Baseline lung function: FEV1 (% predicted): intervention group: 56, SD 6; control group: 58, SD 7 Smoking history: not reported Baseline imbalances: no statistically significant differences between groups | |
| Interventions | Intervention group: azithromycin plus usual care (n = 16) Dose: 250 mg; delivery mode: oral; frequency: 3/week; duration: 3 months Control group: usual care alone (n = 14) Participants in both groups continued taking their habitual treatment to the same doses, including inhaled steroids, bronchodilators, mucolytic therapy, and physiotherapy. In cases of severe exacerbations, steroids or antibiotics were recommended. Adherence: not reported Run‐in phase: unclear Run‐out phase: unclear | |
| Outcomes | Primary: changes in airway oxidative stress markers (FeNO, 8‐isoprostane, nitrites (NO2), and nitrates (NO3)) Secondary: changes in lung function (FVC, FEV1 (pre‐ and post‐BD), FEV1/FVC, total lung capacity, colour and volume of sputum, number of exacerbations, hospital admissions, functional capacity, health‐related quality of life Post hoc analysis: colonised vs not colonised with Pseudomonas aeruginosa | |
| Notes | Power calculation: based on expected 10% difference in FeNO between groups with 90% power and 5% statistical significance Trial registration: clinicaltrials.gov: NTC01463371 Conflicts of interest: not reported Funders: Fundacion Valenciana de Neumologia Role of the sponsors: not reported Ethical approval: yes Conclusions: 3‐month treatment with azithromycin; clinical benefit in patients with non‐CF bronchiectasis but no effect on airway oxidative stress markers | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Allocation concealment (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Blinding of participants and personnel (performance bias) | High risk | Study investigators were blinded to group allocation, but this was an open‐label study. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Incomplete outcome data (attrition bias) | Unclear risk | Six participants were lost to follow‐up. No reasons for missing data were provided. |
| Selective reporting (reporting bias) | Low risk | Study protocol was published and all prespecified (primary and secondary) outcomes were reported. |
| Other bias | Low risk | None identified |
| Methods | Aims: to investigate the efficacy of once‐daily roxithromycin for improving clinical outcomes Design: double‐blind, randomised, placebo‐controlled trial Total study duration: 6 months Number of study centres and location: 1, Thailand Study setting: outpatient department, Songklanagarind Hospital Methods of recruitment: not reported Withdrawals: none Study start/end dates: June 2010/November 2010 Analysis by intent‐to‐treat: yes | |
| Participants | 26 adults were randomised. Inclusion criteria: aged 18 years and above, diagnosis of bronchiectasis, symptomatic bronchiectasis Exclusion criteria: macrolides in previous year, exacerbation of bronchiectasis in previous 3 months, allergy to macrolides, active malignancy, active or recent pulmonary infection within 3 months, pregnancy Mean age: intervention group: 55 years; control group: 60 years Gender: intervention group: 4 women, 8 men; control group: 8 women, 6 men Bronchiectasis diagnosis: chest radiograph and HRCT; diagnosis confirmed by pulmonologist Severity of condition: described as "severe" Baseline lung function: FEV1 (L): intervention group: 1.53 ± 0.62; control group: 1.31 ± 0.44; FVC (L): intervention group: 2.27 ± 0.79; control group: 1.98 ± 0.55 Smoking history: present 2 (8%),former: 6 (23%), never 18 (69%) Baseline imbalances: no statistically significant differences between groups | |
| Interventions | Intervention group: roxithromycin (n = 12) Dose: 300 mg; delivery mode: oral; frequency: once daily; duration: 8 weeks Control group: placebo (n = 14) Adherence: not reported Run‐in phase: not reported Run‐out phase: not reported | |
| Outcomes | Primary: symptoms scores, pulmonary function tests (FEV1 L, FVC L) Secondary: safety, tolerability, drug resistance Post hoc analysis: not reported | |
| Notes | Power calculation: not reported Trial registration: unclear Conflicts of interest: not stated Funders: Faculty and Hospital Fund for Research, Songklanagarind Hospital Role of the sponsors: not reported Ethical approval: not reported Conclusions: Once‐daily roxithromycin showed benefit for clinical outcomes as well as quality of life. Larger studies on the effects of macrolide in bronchiectasis treatment with longer follow‐up times should be done. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Allocation concealment (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Blinding of participants and personnel (performance bias) | Low risk | Double‐blind effectiveness was confirmed by contact with trial authors. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Incomplete outcome data (attrition bias) | Low risk | No withdrawals were reported. |
| Selective reporting (reporting bias) | Unclear risk | Informaiton was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Other bias | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Methods | Aims: to determine whether roxithromycin can reduce the degree of airway responsiveness in bronchiectasis Design: double‐blind, randomised, placebo‐controlled trial Total study duration: 12 weeks Number of study centres and location: 1, South Korea Study setting: outpatient clinic, Seoul National University Hospital Methods of recruitment: selected from the outpatient clinic list Withdrawals: 2 (1 in each group) removed by investigators owing to non‐compliance Study start/end dates: October 1995/February 1996 Analysis by intent‐to‐treat: no | |
| Participants | 25 children were randomised. Inclusion criteria: increased airway responsiveness (defined as a provocative concentration of methacholine causing a 20% fall in FEV1 (PC20) < 25 mg/mL evaluated by the dosimeter method Exclusion criteria: not explicitly stated but patients with cystic fibrosis, humoral immune deficiency, bronchopulmonary aspergillosis, excluded; also, those who had taken antibiotics or corticosteroids or who had an upper respiratory tract infection in the past month Mean age: intervention group: 13.3 years; control group: 12.9 years Gender: intervention group: 6 girls, 7 boys; control group: 5 girls, 7 boys Bronchiectasis diagnosis: clinical features; confirmed by computed tomography, with bronchography when necessary Baseline lung function: FEV1 (% predicted): intervention group: 83 ± 6; control group: 84 ± 7 Smoking history: not applicable Severity of condition: not reported Baseline imbalances: 3 asthmatic patients in the intervention group and 4 in the control group. In the initial methacholine challenge test, 3 participants in the intervention group and 2 in the control group did not attain a maximal response plateau. No other significant differences were noted at baseline. | |
| Interventions | Intervention group: roxithromycin (n = 13) Dose: 4 mg/kg; delivery mode: oral; frequency: 2/d; duration: 12 weeks Control group: placebo (n = 12) Adherence: used packets or drug sachets monitored for compliance; 2 participants withdrew owing to non‐compliance Run‐in phase: not reported Run‐out phase: not reported | |
| Outcomes | Primary: unclear which of the outcomes below were primary Secondary: FEV1, sputum colour (sputum purulence score), sputum ‐ polymorphonuclear leucocyte (PMN) (sputum leucocyte score) Post hoc analysis: unclear | |
| Notes | Power calculation: not reported Trial registration: not reported Conflicts of interest: not reported Funders: Seoul National University Hospital Research Fund Role of the sponsors: not reported Ethical approval: yes Conclusions: Roxithromycin may decrease the degree of airway responsiveness in patients with bronchiectasis and increased airway responsiveness. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The study was conducted in a double‐blind, randomized, placebo‐controlled fashion after the preliminary methacholine challenge test". Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Allocation concealment (selection bias) | Unclear risk | "A doctor (not responsible for follow‐up or data analysis) was assigned the task of dividing the patients into two groups". Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Blinding of participants and personnel (performance bias) | Unclear risk | "The study was conducted in a double‐blind, randomized, placebo‐controlled fashion after the preliminary methacholine challenge test". Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Incomplete outcome data (attrition bias) | Low risk | Two participants (1 in each group) were withdrawn from the study because of non‐compliance with medication or regular check‐up. Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups. |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Other bias | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Methods | Aims: to assess the effect of roxithromycin on inflammation media in induced sputum, dilated bronchial wall thickness, SGRQ scores, and exacerbation rates Design: open‐label, randomised controlled trial Total study duration: 6 months Number of study centres and location: 1, Qinzhou City, Guangxi Province, China Study setting: hospital Methods of recruitment: not reported Withdrawals: 4, number per group not reported; reasons for withdrawal not reported Study start/end dates: June 2007/June 2010 Analysis by intent‐to‐treat: no | |
| Participants | 50 adults were randomised. Inclusion criteria: aged 18 to 65 years with bronchiectasis diagnosed by HRCT Exclusion criteria: allergy to macrolide, cirrhosis, liver dysfunction and exacerbation. Bronchiectasis exacerbation was defined as abnormalities in 4 of the following 9 symptoms, signs, or laboratory findings: change in sputum production (consistency, colour, volume, or hemoptysis); increased dyspnoea (chest congestion or shortness of breath); increased cough; fever (38° C); increased wheezing; decreased exercise tolerance, malaise, fatigue, or lethargy; FEV1 or FVC decreased 10% from a previously recorded value; radiographic changes indicative of a new pulmonary process; or changes in chest sounds. Concomitant medications unclear Mean age: intervention group: 47, SD 8; control group: 49, SD 9 (range 29‐67) Gender: intervention group: 12 male, 13 female; control group: 14 male, 11 female Bronchiectasis criteria: HRCT Severity of condition: not reported Baseline lung function (intervention group, control group): not reported Smoking history: intervention group, control group, pack‐years: not reported Baseline imbalances: not reported | |
| Interventions | Intervention group: roxithromycin + ambroxol hydrochloride (n = 25) Dose (Rox): 15 g (150 mg); delivery mode: oral; frequency: 1/d; duration: 6 months+ Dose (AH): 30 mg; delivery mode: oral; frequency: 3/d; duration: 6 months Control group: oral ambroxol hydrochloride (n = 25) Dose: 30 mg; delivery mode: oral; frequency: 3/d; duration: 6 months Adherence: not reported Run‐in phase: not reported Run‐out phase: not reported | |
| Outcomes | Primary: unclear Secondary: SGRQ and MRC Breathlessness Scale Time points: baseline, 6 months Post hoc analysis: unclear | |
| Notes | Power calculation: not reported Trial registration: not reported Conflicts of interest: unclear Funders: Chinese Medical Association Chronic Pulmonary Disease Fund (07010150023), Guangxi Province Department of Science Youth Fund (0991019), Guangxi Province Health Department Self‐funded Research Project (Z2007047) Role of the sponsors: unclear Ethical approval: unclear Conclusions: Scores for bronchial wall thickening of bronchiectasis were increased in participants with stable bronchiectasis. Low‐dose roxithromycin combined with ambroxol hydrochloride significantly improved degree of dyspnoea and reduced scores for extent of bronchiectasis, scores for bronchial wall thickening of bronchiectasis, and global CT scores as compared with treatment with ambroxol hydrochloride alone in participants with bronchiectasis who were in stable condition. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "random number table" |
| Allocation concealment (selection bias) | Unclear risk | Information in study report was insufficient. |
| Blinding of participants and personnel (performance bias) | High risk | Reporting was unclear, but this was an open‐label study. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessors were blinded to group allocation. |
| Incomplete outcome data (attrition bias) | Unclear risk | 4 withdrawals were reported, but numbers for each group were not given. |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Other bias | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Methods | Aims: to assess effects of roxithromycin on inflammation media in induced sputum, dilated bronchial wall thickness, SGRQ scores, and exacerbation of bronchiectasis in patients in stable condition Design: open‐label, randomised controlled trial Total study duration: 26 months Number of study centres and location: 1, China Study setting: Tenth Affiliated Hospital of Guangxi Medical University Methods of recruitment: unclear Withdrawals: intervention group: 4; control group: 5 Study start/end dates: May 2009/July 2011 Analysis by intent‐to‐treat: no | |
| Participants | 52 adults randomised; 43 completed Inclusion criteria: between 18 and 65 years of age and hospitalised at the Tenth Affiliated Hospital of Guangxi Medical University directed by First Affiliated Hospital of Guangxi Medical University, Qinzhou, China, from May 2009 to July 2011 Exclusion criteria: protocol‐defined exacerbation (PDE) of bronchiectasis. PDE was prospectively defined as abnormalities in 4 of the following 9 symptoms, signs, or laboratory findings: change in sputum production (consistency, colour, volume, or haemoptysis); increased dyspnoea (chest congestion or shortness of breath); increased cough; fever (> 38° C); increased wheezing; decreased exercise tolerance, malaise, fatigue, or lethargy; FEV1 or FVC decreasing 10% from a previously recorded value; radiographic changes indicative of a new pulmonary process; or changes in chest sounds. Patients with CF who had documented clinical, radiological, and genotypic features and abnormal sweat test results (sweat sodium and chloride > 60 mmol/L) were excluded. Patients who were allergic to macrolides and patients with impaired hepatic disease or diabetes mellitus were also excluded. Mean age: intervention group: 47.1 years; control group: 49.2 years Gender: intervention group: 11 women, 11 men; control group: 9 women, 12 men Bronchiectasis diagnosis: standard chest radiograph compatible with bronchiectasis, for instance, fusiform infiltrates of mucoid impaction, "signet ring", or "tram tracks"; chest CT showing ectasia of peripheral bronchi, fluid‐filled airways, or thickening of the mucosa; daily chronic sputum production or haemoptysis ‐ all confirmed at baseline by HRCT Severity of condition: global CT score: intervention group: 9.47; control group: 9.54 Baseline lung function (intervention group, control group): FEV1 (L) 1.59, 1.63; FEV1 (% predicted): 66.8, 67.4; FVC (L) 2.27, 2.34; FVC (% predicted): not reported; FEV1/FVC: 70, 69.6 Smoking history: intervention group: 4.7 pack‐years; control group: 4.3 pack‐years Baseline imbalances: no significant differences between study groups at baseline | |
| Interventions | Intervention group: roxithromycin (n = 22) Dose: 150 mg; delivery mode: oral; frequency: 1/d; duration: 6 months Control group: no treatment (n = 21) Adherence: Treatment adherence was encouraged by telephone calls from the study co‐ordinator and by measurement of pill counts. Run‐in phase: 1‐month run‐in period free of exacerbation symptoms before baseline sampling Run‐out phase: not reported | |
| Outcomes | Primary: not specified Secondary: sputum production, lung function, inflammatory markers (including IL‐8, neutrophil elastase (NE), MMP‐9, tissue inhibitor of metalloproteinases‐1 (TIMP‐1), hyaluronidase (HA), and type IV collagen concentration in induced sputum), total and differential sputum cell counts, quality of life (SGRQ), dyspnoea, CT evaluation of the thorax Time points: baseline, 6 months Post hoc analysis: NA | |
| Notes | Power calculation: not reported Trial registration: not reported Conflicts of interest: none Funders: Trial authors acknowledge support from the Medical Experiment Center of Guangxi Medical University. The study was supported by grants from the Special Foundation for Chronic Respiratory Disease of Chinese Medical Association (no. 07010150023) and Youth Science Fund of Guangxi Zhuang Autonomous Region in China (no. 0991019). Role of the sponsors: not reported Ethical approval: yes Conclusions: Treatment with roxithromycin can decrease airway inflammation and reduce airway thickness of dilated bronchus, both of which are positively associated with chronic airway inflammation in steady‐state bronchiectasis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Eligible participants were randomly assigned to control and roxithromycin groups; information is insufficient to permit judgement of 'low risk' or 'high risk'. |
| Allocation concealment (selection bias) | Low risk | Study report information was insufficient. |
| Blinding of participants and personnel (performance bias) | High risk | Reporting was unclear but this was an open‐label study. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Incomplete outcome data (attrition bias) | Low risk | Withdrawal was balanced between groups. |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Other bias | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Methods | Aims: to demonstrate effects of azithromycin on sputum volume, quality of life, and independence, and to estimate duration of effects of azithromycin after cessation of therapy Design: double‐blind, randomised, placebo‐controlled trial Total study duration: 26 weeks Number of study centres and location: single, Malaysia Study setting: Respiratory Clinic, Hospital Taiping, Taiping; unclear whether in‐patient or out‐patient setting Methods of recruitment: not reported Withdrawals: 10 adults lost to follow‐up (intervention group: 6; control group: 4) Study start/end dates: November 2011/December 2013 Analysis by intent‐to‐treat: no | |
| Participants | 78 adults were randomised. Inclusion criteria: over 18 years of age with diagnosis of bronchiectasis, reproducible spirometry and chronic sputum production documented in second week of the run‐in period; stable for 6 weeks before study entry Exclusion criteria: pregnant and lactating, active tuberculosis, malignancy Mean age: intervention group: 65.94 years; control group: 59.74 years Gender: intervention group: 24 women, 15 men; control group: 26 women, 13 men Bronchiectasis diagnosis: HRCT Severity of condition: not reported Baseline lung function (intervention group, control group): FEV1 (L): 1.09, 1.17; FVC (L): 1.56, 1.69; FEV1/FVC: 72.6, 70.90 Smoking history: intervention group: 11 current smokers, 28 non‐smokers; control group: 11 current smokers, 28 non‐smokers Baseline imbalances: no significant differences between treatment groups at baseline with respect to age, gender, weight, height, smoking status, serum albumin and creatinine levels, SGRQ scores, and lung function. Baseline sputum volume was significantly higher in the azithromycin group. | |
| Interventions | Intervention group: azithromycin (n = 39) Dose: 1000 mg; delivery mode: oral; frequency: weekly; duration: 12 weeks Control group: placebo (n = 39) Identical to Zithromax tablets Adherence: not reported Run‐in phase: 2 weeks Run‐out phase: 12 weeks; both groups received placebo | |
| Outcomes | Primary: 24‐hour sputum volume (percentage change from baseline) Secondary: SGRQ score, SGRQ (change in score from baseline) and spirometric assessment of FVC and FEV1, adverse events, serious adverse events Post hoc analysis: unclear | |
| Notes | Power calculation: "The study was powered to detect differences in sputum volume, quality of life and spirometry values with azithromycin treatment". Trial registration: clinicaltrials.gov: NCT02107274 Conflicts of interest: See role of sponsors below; conflicts of interest for individual trial authors not stated Funders: grant approved by the Ministry of Health of Malaysia. Study medications were manufactured and provided by Pfizer Inc. (Ann Arbor, Ml, USA). Role of the sponsors: Pfizer Ltd. (Sandwich, Kent, UK) was not involved in study design, data collection, or data interpretation. Ethical approval: yes (local institutional ethics committee) Conclusions: 12‐Week administration of 1000 mg azithromycin weekly in pulmonary bronchiectasis significantly reduced mean sputum volume, improved health status, and stabilised lung function. Azithromycin had a 'carryover effect' on sputum volume and health status for 12 weeks after cessation of therapy. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number sequence in a 1:1 ratio |
| Allocation concealment (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Blinding of participants and personnel (performance bias) | Low risk | Patients were randomised to receive 12 weeks of placebo or azithromycin in a 1:1 ratio in a double‐blinded fashion. |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding was maintained from randomisation until database lock unless any patient emergencies arose. |
| Incomplete outcome data (attrition bias) | Low risk | Ten participants did not complete the study and were excluded from analyses. Four participants were lost to follow‐up for logistic reasons. Another 4 had gastrointestinal (GI) disturbances, which consisted predominantly of diarrhoea. Two deaths were recorded in the treatment arm. Both participants passed away owing to severe pneumonia. Missing outcome data were balanced in numbers across intervention groups, and reasons for missing data were similar across groups. |
| Selective reporting (reporting bias) | Low risk | The study protocol is available, and all of the study's prespecified (primary and secondary) outcomes of interest in the review have been reported in the prespecified way. |
| Other bias | High risk | Groups were not balanced at baseline with regard to the primary outcome – sputum volume. |
| Methods | Aims: to evaluate the efficacy of erythromycin compared with placebo in reducing the number of pulmonary exacerbations among children with HIV‐related bronchiectasis over a period of 52 weeks Design: randomised, double‐blind, placebo‐controlled trial Total study duration: not reported Number of study centres and location: single, South Africa Study setting: Paediatric Chest Clinic, Steve Biko Academic Hospital, Pretoria Methods of recruitment: not reported Withdrawals: 1 child died after randomisation, but group allocation was not stated, and 10 were lost to follow‐up (intervention group: 6; control group: 4) Study start/end dates: January 2009/June 2012 Analysis by intent‐to‐treat: no | |
| Participants | 42 children were randomised. Inclusion criteria: children aged 6 to 18 years with confirmed HIV infection. The presence of bronchiectasis was confirmed on HRCT scanning, with exclusion of other causes of bronchiectasis, including a sweat test to rule out CF. All children had to be able to perform reliable pulmonary function tests. Exclusion criteria: abnormal liver function tests (ALT/AST > 2.5 times normal); abnormal urea/creatinine; use of carbamazepine, warfarin, cyclosporine, or long‐term midazolam Mean age: intervention group: 8.4 years; control group: 9.1 years Gender: intervention group: 4 girls, 13 boys; control group: 9 girls, 5 boys Bronchiectasis diagnosis: HRCT scanning Severity of condition: Bhalla score: intervention group: 15; control group: 11.5 Baseline lung function (intervention group, control group): FEV1 (% predicted): 56, 53.6; FVC (% predicted): 49, 45 Baseline imbalances: Characteristics of the 2 study arms were generally balanced, with the exception of gender distribution, with more males (76%) in the erythromycin arm and more females in the placebo arm (64%). CD4 count (%) and CD4 (total × 106) were significantly lower and Bhalla score significantly higher in the intervention group than in the control group (worse). | |
| Interventions | Intervention group: erythromycin (n = 17) Dose: 125 mg per oral suspension if < 15 kg body weight, or 250 mg per oral suspension if ≥ 15 kg body weight; delivery mode: oral; frequency: daily; duration: 52 weeks Control group: placebo (n = 14) Adherence: Compliance was assessed with use of a medication diary and verbal interviews. 90% of participants in each arm took their medication. Run‐in phase: unclear Run‐out phase: unclear | |
| Outcomes | Primary: exacerbations (protocol defined as the presence of ≥ 2 of the following: increased tachypnoea or dyspnoea, change in frequency of cough, increase in sputum productivity, fever, chest pain, new infiltrates on chest x‐ray) Secondary: pulmonary function parameters (FEV1, FVC, FEF), BMI z‐score, CD4 count (%), CD4 (total* 108), proinflammatory and anti‐inflammatory chemokines and cytokines, Bhalla score Post hoc analysis: unclear | |
| Notes | Power calculation: Sample size calculation was based on the number of pulmonary exacerbations requiring antibiotic therapy, estimated at 3 per year. A sample size of 20 participants per study arm was determined to have 90% power to detect a clinically relevant reduction in exacerbations of 30%, when a mean of 2 and a standard deviation of 1 exacerbation were assumed; and with a presumed dropout rate of 10% when testing was 1sided at the 0.05 level of significance. Trial registration: not reported Conflicts of interest: not declared Funders: unrestricted grant from the Research Development Program of the University of Pretoria. Adcock Ingram South Africa donated erythromycin. Role of the funders/sponsors: not reported Ethical approval: yes Conclusions: Administration of HAART and adjunctive care, which includes airway clearance and treatment of exacerbations, in children with HIV‐related bronchiectasis is associated with significant improvement in pulmonary function tests and IL‐8, with no additional benefit derived from the use of erythromycin. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned (1:1) to the erythromycin group (55%) or to the placebo group (45%). |
| Allocation concealment (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Blinding of participants and personnel (performance bias) | Unclear risk | All study personnel performing clinical evaluations were blinded to treatment assignment. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Two blinded radiologists carried out the CT scan. Additional details on outcome blinding were not reported. |
| Incomplete outcome data (attrition bias) | Unclear risk | 10 participants were lost to follow‐up ‐ 4 in the placebo group and 6 in the intervention group; no reasons were provided. |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Other bias | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Methods | Aims: to test the hypothesis that azithromycin would decrease the frequency of exacerbations, increase lung function, and decrease the severity of symptoms Design: randomised placebo‐controlled trial Total study duration: 12 months Number of study centres and location: single, Azerbaijan Study setting: hospital clinic Methods of recruitment: not reported Withdrawals: unclear Study start/end dates: February 2011/February 2012 Analysis by intent‐to‐treat: unclear | |
| Participants | 65 adults were randomised. Inclusion criteria: not reported Exclusion criteria: not reported Mean age: not reported Gender: not reported Bronchiectasis diagnosis: not reported Severity of condition: not reported Baseline lung function: not reported Smoking history: not reported Baseline imbalances: not reported | |
| Interventions | Intervention group: azithromycin (n = 35) Dose: 500 mg; delivery mode: oral; frequency: 3 days per week; duration: 6 months Control group: placebo (n = 30) Adherence: unclear Run‐in phase: unclear Run‐out phase: unclear | |
| Outcomes | Primary: event‐based exacerbations, times of first exacerbation, adverse events, serious adverse events Secondary: sputum volume and purulence, FEV1, systemic and local markers of infection (leucocyte count, CRP, neutrophil count of induced sputum, interleukin‐6 (IL‐6) in induced sputum), adverse events (e.g. cardiac arrhythmias, gastrointestinal symptoms, hearing impairment) | |
| Notes | Conference abstract only. Additional information provided by personal communication | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Allocation concealment (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Blinding of participants and personnel (performance bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Incomplete outcome data (attrition bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Other bias | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk' as only data from the conference abstract were available. |
| Methods | Aims: to test the hypothesis that low‐dose erythromycin would reduce pulmonary exacerbations in patients with non‐CF bronchiectasis with a history of frequent exacerbations Design: randomised, double‐blind, placebo‐controlled study Total study duration: 26 months Number of study centres and location: single, Australia Study setting: regional adult CF centre, respiratory medicine department, Australian University Teaching Hospital; out‐patient setting Methods of recruitment: patients attending the centre, referral from respiratory physicians at other centres, and public radio advertisements Withdrawals: 10; intervention group: 5 (2 lost to follow‐up, 1 lost for possible QTc prolongation, 1 moved, 1 unable to continue); control group: 5 (2 lost to follow‐up, 1 with nausea, 1 withdrawn by physician, 1 unable to continue) Study start/end dates: October 2008/December 2011 Analysis by intent‐to‐treat: yes, using LOCF for missing data | |
| Participants | 117 adults were randomised. Inclusion criteria: confirmed diagnosis of bronchiectasis and clinically stable for at least 4 weeks before enrolment (defined as no symptoms of exacerbation, no requirement for supplemental antibiotic therapy, and FEV1 within 10% of best recently recorded value when available) Exclusion criteria: CF, current mycobacterial disease or bronchopulmonary aspergillosis, any reversible cause for exacerbations, maintenance oral antibiotic prophylaxis, prior macrolide use except short‐term use, changes to medications in the preceding 4 weeks, cigarette smoking within 6 months, medications or comorbidities with the potential for important interactions with erythromycin Mean age: intervention group: 61.1 years; control group: 63.5 years Gender: intervention group: 38 women, 21 men; control group: 33 women, 25 men Bronchiectasis diagnosis: HRCT scan and clinical diagnosis (≥ 2 separate pulmonary exacerbations requiring supplemental systemic antibiotic therapy in the preceding 12 months, and daily sputum production) Severity of condition: 35% of adults had more than 5 exacerbations in the previous year. Bhalla score was not reported. Baseline lung function (intervention group, control group): FEV1 (postbronch % predicted): 70.2, 73.6 Smoking history: intervention group: ex‐smokers: 10, 2.3 pack‐years: non‐smokers: 49; control group: ex‐smokers: 15, 2.9 pack‐years: non‐smokers: 44 Baseline imbalances: no significant between‐group differences | |
| Interventions | Intervention group: erythromycin ethylsuccinate (n = 59) Dose: 400 mg (equivalent to 250 mg erythromycin base); delivery mode: oral; frequency: 2/d; duration: 48 weeks Control group: placebo (n = 58) spray‐dried lactose/magnesium stearate tablets Adherence: assessed at each visit by pill counts (intervention group: 95.6%; control group: 96.5%) Run‐in phase: unclear Run‐out phase: 4‐week washout period Erythromycin and placebo tablets were manufactured and supplied by Alpha Pharm and were identical in shape, appearance, and taste. | |
| Outcomes | Primary: mean rate of protocol‐defined pulmonary exacerbation (PDPE) per patient per year (required antibiotic administration for a sustained (> 24‐hour) increase in sputum volume or purulence accompanied by new deteriorations in ≥ 2 additional symptoms: sputum volume, sputum purulence, cough, dyspnoea, chest pain, or hemoptysis Secondary: rate of all pulmonary events (i.e. PDPEs plus non‐PDPEs) for which participants commenced antibiotics, total days of antibiotics, change in the proportion of commensal oropharyngeal streptococci resistant to macrolides, symptoms (LCQ), quality of life (SGRQ), 24‐hour sputum weight, FEV1 percent predicted, CRP level, exercise capacity (6MWT), sputum bacteriology, and sputum inflammatory cell counts. Safety endpoints included adverse events, liver function test results, and electrocardiogram findings. Post hoc analysis: unclear | |
| Notes | Power calculation: Assuming a baseline (SD) annual rate of exacerbations in the control group of 2.9 (1.2), 98 participants gave 90% power at the 5% significance level to show a 28% reduction in exacerbation rate with erythromycin ‐ a much more conservative estimate of efficacy than the 50% reduction seen in our uncontrolled pilot data. Assuming 20% attrition, the required sample size was increased to 118. Trial registration: anzctr.org.au Identifier: ACTRN12609000578202 Conflicts of interest: Dr. Serisier received honoraria, speakers' fees, and travel support from a range of pharmaceutical companies including GSK, Boehringer‐Ingelheim, AstraZeneca, Phebra, and Pharmaxis. Dr. Bowler received honoraria, speakers' fees, and travel support from a range of pharmaceutical companies including GSK, Boehringer‐Ingelheim, AstraZeneca, and Novartis. Other trial authors reported no conflicts of interest. Funders: Mater Adult Respiratory Research Trust Fund. No pharmaceutical company or other agency (including medical writers) had any role in this study. Role of the sponsors: The funding source had no role in design and conduct of the study; collection, analysis, and interpretation of data; or preparation, review, or approval of the manuscript. Ethical approval: yes Conclusions: Among patients with non‐CF bronchiectasis, 12‐ month use of erythromycin compared with placebo resulted in a modest decrease in the rate of pulmonary exacerbations and an increased rate of macrolide resistance. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation sequences, blocked in random groups of 2, 4, and 8 and stratified for the presence of sputum Pseudomonas aeruginosa at screening, were held by the Department of Pharmacy. |
| Allocation concealment (selection bias) | Low risk | The independent trial pharmacist dispensed blinded study drug according to the randomisation sequence. |
| Blinding of participants and personnel (performance bias) | Low risk | Trial participants, trial supervisors, and all trial staff directly involved in participant care were unaware of treatment assignment at all times. |
| Blinding of outcome assessment (detection bias) | Low risk | All participants and study personnel were masked to treatment assignment, including all investigators involved in sample processing and data entry. |
| Incomplete outcome data (attrition bias) | Low risk | Loss of follow‐up was similar in both groups. |
| Selective reporting (reporting bias) | Low risk | All measurements stated in the methods were reported in the results section. Extended methods were available online (http://www.jama.com). |
| Other bias | Low risk | Trial authors used LOCF methods to impute missing data for ITT analyses, but robustness was confirmed via multiple imputation techniques to assess sensitivity. |
| Methods | Aims: to establish whether long‐term (12 to 24 months) antibiotic treatment with azithromycin would reduce the rate of pulmonary exacerbations in indigenous children with non‐cystic fibrosis bronchiectasis; also to monitor for serious adverse events associated with azithromycin and examine its effect on nasopharyngeal carriage of bacterial pathogens. Design: double‐blind, randomised, placebo‐controlled trial Total study duration: 25 months Number of study centres and location: multi‐centre, Australia and New Zealand Study setting: community clinics in central and northern Australia and urban Maori and Pacific Island children from a tertiary paediatric hospital in Auckland Methods of recruitment: Children entered the study when they were clinically stable (≥ 8 weeks after their last exacerbation) as decided by clinic staff. Withdrawals: intervention group: 4 (1 was withdrawn by physician, 1 was withdrawn by parent, 1 refused meds, 1 fulfilled exit criteria); control group: 4 (2 withdrawn by physician, 1 moved out of study, 1 fulfilled exit criteria) Study start/end dates: November 2008/December 2010 Analysis by intent‐to‐treat: Analysis of the primary endpoint was by intention‐to‐treat. Analysis of secondary endpoints was by modified intention‐to‐treat, excluding participants with missing data, except for analysis of nasal swabs, which was done only for participants with swabs available from baseline and last clinic visits. | |
| Participants | 89 children were randomised. Inclusion criteria: aged 1 to 8 years, living within the study area, had bronchiectasis confirmed radiographically by HRCT scans or chronic suppurative lung disease (bronchiectasis suspected clinically when HRCT scans were unavailable), and had ≥ 1 pulmonary exacerbation in the past 12 months Exclusion criteria: receiving chemotherapy, immunosuppressive treatment, or long‐term antibiotics; had an underlying cause for their bronchiectasis (e.g. cystic fibrosis, primary immunodeficiency), other chronic disorders (e.g. cardiac, neurological, renal, or hepatic abnormality), or macrolide hypersensitivity Mean age: intervention group: 3.99 years; control group: 4.22 years Gender: intervention group: 19 girls, 26 boys; control group: 23 girls, 21 boys Bronchiectasis diagnosis: HRCT scans or chronic suppurative lung disease (bronchiectasis suspected clinically when HRCT scans were unavailable) Severity of condition: Bhalla score not reported Baseline lung function: not reported Baseline imbalances: The most substantial difference was mechanical ventilation, with more children in the placebo group needing ventilation as neonates compared with those in the azithromycin group (22% vs 5%). However, participants in the azithromycin group were less likely to be premature (29% vs 39%), fewer had proven bronchiectasis (76% vs 89%), and their first admission to hospital for respiratory disease occurred later in life (mean of 6.5 vs 4.2 months). | |
| Interventions | Intervention group: azithromycin (n = 45) Dose: 30 mg/kg, maximum 600 mg; delivery mode: oral; frequency: once a week; duration: 24 months Study drug was administered under direct supervision at the community clinic (Australia) or at the child's home, preschool, or school (New Zealand). Control group: placebo (n = 44) Placebo medication was similar in appearance, taste, smell, and packaging to the active medication and had no active ingredients. Adherence: Research nurses contacted the community clinic and the child's caregiver, preschool, or school weekly to record drug adherence (children receiving medication and, if any, children who were absent from the community) and any issues with administration, such as the child spitting out the medication. These data were recorded in a participant medication logbook. Study personnel completed a medical review every 3 to 4 months. Intervention group: 88%; control group: 84% Run‐in phase: Children who were already receiving azithromycin (4 in each treatment group) had the antibiotic discontinued and underwent a 3‐month washout period before commencing the study. Run‐out phase: unclear Both azithromycin and placebo were provided in powder format and were reconstituted with 9 mL of sterile water to syrup for oral use (40 mg/mL). | |
| Outcomes | Primary: pulmonary exacerbation rate (treatment by clinic or hospital staff with antibiotics for any of the following (as recorded in the medical chart): increased cough, dyspnoea, increased sputum volume or colour intensity, new chest examination or radiographic findings, deterioration in predicted FEV1 percentage > 10%, or haemoptysis) Secondary: time to first pulmonary exacerbation, duration of exacerbation episode (discharge date minus admission date plus 1 day), severity (admission to hospital, oxygen supplementation), weight‐for‐age z‐scores (z‐score at last study clinic minus its value at baseline), respiratory signs and symptoms (assessed by study personnel on history and physical examination), sputum characteristics, school absenteeism, FEV1 % predicted in those aged 6 years and older, serious adverse events, and antibiotic resistance in bacterial pathogens cultured from deep nasal swabs Post hoc analysis: post hoc subgroup analyses for participants taking ≥ 70% of their expected doses, those who received the intervention for 23 to 24 months, children with HRCT‐proven bronchiectasis, children with ≥ 2 hospital‐managed pulmonary exacerbations before enrolment, children with ≥ 10 pulmonary exacerbations before enrolment, those without a history of mechanical ventilation, and those carrying any respiratory bacterial pathogens at baseline | |
| Notes | Power calculation: Sample size and power calculations were based on previous data; we anticipated that participants in the placebo group would have 4 episodes during the 24‐month trial period. Guided by results from an earlier randomised trial of azithromycin in patients with CF, we assumed pulmonary exacerbations would be reduced by 50% in the intervention group and by 15% in the placebo group. 51 participants per group would give 90% power to detect an average difference of 1.4 respiratory exacerbations per participant over a 2‐year period at the 5% level of significance. Trial registration: Australian New Zealand Clinical Trials Registry, number ACTRN12610000383066 Conflicts of interest: Trial authors declared they had no conflicts of interest. Funders: National Health and Medical Research Council (NHMRC) of Australia (project grant numbers 389837 (clinical component), 545223 (microbiology component), and CRE for lung health 1040830 (feedback)); Telstra Foundation (seeding grant ‐ Telstra Community Development Grant, 2004); Health Research Council of New Zealand (grant number 08/158); and Auckland Medical Research Foundation (grant number 81542) Role of the sponsors: Sponsors of the study had no role in study design, data collection, data analysis, or data interpretation, nor in writing of the report. Ethical approval: yes Conclusions: Once‐weekly azithromycin for up to 24 months decreased pulmonary exacerbations among indigenous children with non‐cystic fibrosis bronchiectasis or chronic suppurative lung disease. However, this strategy was accompanied by increased carriage of azithromycin‐resistant bacteria, the clinical consequences of which are uncertain, and will need careful monitoring and further study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent statistician used a computer‐generated permuted‐block design to provide the randomisation sequences. Children were allocated in a 1:1 ratio (stratified by study site and exacerbation frequency in the preceding 12 months (1‐2 vs > 3 episodes)) to azithromycin or placebo. |
| Allocation concealment (selection bias) | Low risk | Allocation concealment was achieved by use of sequentially numbered, double‐sealed, opaque envelopes. An independent person at the Queensland Institute of Medical Research (Brisbane, QLD, Australia) prepared the individual envelopes labelled with a randomisation number that contained the treatment code inside. |
| Blinding of participants and personnel (performance bias) | Low risk | Study drugs (powder for reconstitution to suspension) were provided in identical packaging, and the placebo (Institute of Drug Technology, Melbourne, VIC, Australia) was much the same in appearance, taste, and smell to azithromycin (Pfizer Australia, West Ryde, NSW, Australia). Participants, families, health professionals, and study personnel were unaware of treatment assignment until data analysis was completed. |
| Blinding of outcome assessment (detection bias) | Low risk | Investigators collecting data were unaware of the treatment assigned to each child. |
| Incomplete outcome data (attrition bias) | Low risk | Eight children (4 per group) ceased the intervention early, mainly after they were withdrawn by their treating physician or because they experienced treatment failure (2 in the azithromycin group, 3 in the placebo group). |
| Selective reporting (reporting bias) | Low risk | The study protocol is available, and all of the study's prespecified (primary and secondary) outcomes of interest to the review were reported in the prespecified way. |
| Other bias | Low risk | Baseline imbalances were tested in post hoc subgroup analyses and showed increased efficacy for the intervention group, although as the trial authors note, analyses were not hypothesis driven and results should therefore be interpreted with caution. |
| Methods | Aims: to test whether azithromycin decreases the frequency of exacerbations, increases lung function, and improves HRQoL in patients with non‐CF bronchiectasis Design: randomised, double‐blind, placebo‐controlled trial Total study duration: 18 months Number of study centres and location: 3, New Zealand Study setting: health centres Methods of recruitment: not reported Withdrawals: 4 withdrew from the azithromycin group (1 had adverse events, 2 were lost to follow‐up, 1 withdrew consent); 10 withdrew from the placebo group (2 had adverse events, 3 were lost to follow‐up, 4 withdrew consent, 1 had cultured Mycobacterium avium intracellulare in sputum). Study start/end dates: February 2008/October 2009 Analysis by intent‐to‐treat: yes | |
| Participants | 141 adults were randomised. Inclusion criteria: ≥ 18 years of age, ≥ 1 pulmonary exacerbation requiring antibiotic treatment in the past year, and diagnosis of bronchiectasis defined by HRCT scan Exclusion criteria: history of CF; hypo‐gammaglobulinaemia; allergic bronchopulmonary aspergillosis; positive culture of non‐tuberculous mycobacteria in the past 2 years or at screening; macrolide treatment for more than 3 months in the past 6 months; or unstable arrhythmia Mean age: intervention group: 60.9 years; control group: 59 years Gender: intervention group: 48 women, 23 men; control group: 50 women, 20 men Bronchiectasis diagnosis: HRCT scan Severity of condition: Bhalla score not reported Baseline lung function (intervention group, control group): FEV1 (% predicted): 67.1, 67.3; FVC (% predicted): 77.7, 78.5; FEV1/FVC: 65.4%, 64.7% Smoking history: not reported Baseline imbalances: unclear | |
| Interventions | Intervention group: azithromycin (n = 71) Dose: 500 mg; delivery mode: oral; frequency: 3/week (Monday, Wednesday, and Friday); duration: 6 months Control group: placebo (n = 70) Adherence: intervention group: 97.9%; control group: 98.3%, assessed by pill counts Run‐in phase: not reported Run‐out phase: followed up for another 6 months without treatment | |
| Outcomes | Primary: rate of event‐based exacerbations in the first 6 months (increase in or new onset of ≥ 1 pulmonary symptom (sputum volume, sputum purulence, or dyspnoea) requiring treatment with antibiotics), FEV1 before bronchodilation, and SGRQ total score at the end of the treatment period Secondary: time to first exacerbation, rate of symptom‐based exacerbations (increase in or new onset of ≥ 1 pulmonary symptom reported on the daily diary card and mean of 3 symptom scores from the daily diary card on 2 consecutive days had to increase by ≥ 1 point (on a 5‐point scale) compared with the same calculation 1 week earlier), prebronchodilator and postbronchodilator FVC, postbronchodilator FEV1, exercise capacity (as measured by the 6MWT), SGRQ total score at 12 months, concentration of CRP (assessed only at 6 months), sputum cell counts and microbiology, and adverse events Post hoc analysis: unclear | |
| Notes | Power calculation: We estimated that about 134 patients would need to be enrolled for the study to have 80% power to detect a 33% difference between the 2 groups in the Poisson frequency of exacerbations during the 6‐month treatment period, assuming a 2‐sided level of 0 to 5 and a 10% dropout rate. With the assumption of normality, the study had power of 89% to detect a difference of 0 to 16 L in the prebronchodilator FEV1 and power of 87% to detect a difference of 8 units in SGRQ total score. Trial registration: Australian New Zealand Clinical Trials Registry, number ACTRN12607000641493 Conflicts of interest: Trial authors declared they had no conflicts of interest. Funders: Health Research Council of New Zealand and Auckland District Health Board Charitable Trust Role of the sponsors: The sponsor had no role in study design, data collection, data analysis, or data interpretation. The data monitoring committee of the sponsor provided feedback on the completed report. The corresponding author had full access to all data in the study and had final responsibility for the decision to submit for publication. Ethical approval: yes Conclusions: Azithromycin, taken 3 times a week for 6 months, decreased the frequency of event‐based exacerbations and increased the time to first exacerbation in patients with non‐cystic fibrosis bronchiectasis. A treatment effect on exacerbations was evident 6 months after completion of treatment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐ generated random number list. Patients were randomly assigned in a 1:1 ratio with a permuted block size of 6 and sequential assignment, stratified by centre. |
| Allocation concealment (selection bias) | Low risk | Randomly assigned to receive azithromycin or placebo by a statistician independent of the reporting statistician |
| Blinding of participants and personnel (performance bias) | Low risk | Participants, research assistants, and investigators were masked to treatment allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Participants, research assistants, and investigators were masked to treatment allocation. |
| Incomplete outcome data (attrition bias) | Low risk | 4 withdrew from the intervention group and 10 from the placebo group for similar reasons. |
| Selective reporting (reporting bias) | Low risk | All outcomes specified in the protocol were reported. |
| Other bias | Low risk | None identified |
| Methods | Aims: to evaluate effects of macrolide antibiotics on the process of inflammation (by measuring IL‐8, TNF‐a, IL‐10 levels and cell profiles in BAL fluid), pulmonary function, and sputum production in children with steady‐state bronchiectasis, secondary to causes other than CF or primary immunodeficiencies Design: randomised controlled trial (open‐label, as no placebo) Total study duration: 12 months Number of study centres and location: single, Turkey Study setting: Department of Paediatric Chest Diseases at Hecettepe University Faculty of Medicine Methods of recruitment: unclear Withdrawals: none Study start/end dates: April 1999/March 2000 Analysis by intent‐to‐treat: yes | |
| Participants | 34 children were randomised. Inclusion criteria: diagnosis of bronchiectasis not due to CF or primary immunodeficiencies, clinically stable with no evidence of acute pulmonary exacerbations; no history of upper or lower respiratory tract infection for at least 4 weeks before start of the study. No patients had received antibiotics within 4 months of study entry. None had taken oral or inhaled corticosteroids before or during the study. Exclusion criteria: not reported Mean age: intervention group: 13.1 years; control group: 11.9 years Gender: intervention group: 9 girls, 8 boys; control group: 6 girls, 11 boys Bronchiectasis diagnosis: clinical and high‐resolution computed tomography Severity of condition: not reported Baseline lung function (intervention group, control group): FEV1 (% predicted): 74, 79 Baseline imbalances: Data show no statistically significant differences between study and control groups in age, sex, FEV1, or oxygen saturation. But among inflammatory parameters, IL‐8 and TNF‐a levels in BAL fluid were significantly higher at the beginning of the study in the treatment group than in the control group (P = 0.02 and P = 0.02, respectively). | |
| Interventions | Intervention group: clarithromycin (CAM) + supportive therapies (n = 17) Dose: 15 mg/kg; delivery mode: oral; frequency: daily; duration: 3 months plus supportive therapies (mucolytic and expectorant medications and postural drainage) Control group: supportive therapies alone (mucolytic and expectorant medications and postural drainage) (NB: no placebo) (n = 17) Adherence: not reported Run‐in phase: unclear Run‐out phase: unclear | |
| Outcomes | Primary: unclear Secondary: unclear BAL cytokine levels (IL‐8, IL‐10, TNF‐alpha); BAL cell profiles (cell number, neutrophils, macrophages); culture test (aerobic and anaerobic bacteria, fungi, and mycobacteria); pulmonary function test (FEV1, FEF); oxygen saturation; sputum volume Post hoc analysis: unclear | |
| Notes | Power calculation: not reported Trial registration: not reported Conflicts of interest: not reported Funders: SANOVEL Pharmaceuticals Inc., supplied cytokine kits. Role of the sponsors: not reported Ethical approval: not reported Conclusions: Use of CAM in children with steady‐state bronchiectasis results in laboratory improvement by reducing inflammatory processes in the lungs. No corresponding clinical improvement could be shown, and although this is possible with long‐term use, trial validation is necessary. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Information about the sequence generation process was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Allocation concealment (selection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel were not blinded as trial was not placebo‐controlled. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Incomplete outcome data (attrition bias) | Low risk | Treatment protocols for all participants were completed without interruption, as none experienced acute infection during follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Information was insufficient to permit judgement of 'low risk' or 'high risk'. |
| Other bias | High risk | Inflammatory markers were significantly higher in the intervention group at baseline; it is unclear whether this was controlled for in the change analysis. |
6MWT: six‐minute walking test; AFB: acid‐fast bacilli; ALT: alanine aminotransferase; AST: aspartate aminotransferase; BAL: bronchoalveolar lavage; BMI: body mass index; CD4: cluster of differentiation 4; CF: cystic fibrosis; COI: conflict of interest; CRP: serum C‐reactive protein; CT: computed tomography; EBC: exhaled breath condensate; FEF: forced expiratory flow; FeNO: fractional exhaled nitric oxide; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; HAART: highly active antiretroviral therapy; HIV: human immunodeficiency virus; HRCT: high resolution computed tomography; HRQoL: health related quality of life; ICS: inhaled corticosteroids; IL‐6: interleukin‐6; IL‐8: Interleukin‐8; IL‐10: Interleukin‐10; ITT: intention to treat; LABA: long‐acting beta‐agonist; LCQ: Leicester Cough Questionnaire; LOCF: last observation carried forward; LRTI: lower respiratory tract Infection; MMP‐9: matrix metallopeptidase‐9; MRC: Medical Research Council; NE: neutrophil elastase; NO2: nitrite; NO3: nitrate; PC20: the Provocative Concentration of methacholine causing a 20% drop in FEV1; PDE: protocol‐defined exacerbation; PDPE: protocol‐defined pulmonary exacerbation; PF: pulmonary function; PMN: polymorphonuclear leucocyte; QoL: quality of life; QTc: the QT interval; SABA: short‐acting beta‐agonist; SD: standard deviation; SGRQ: St. George's Respiratory Questionnaire; TIMP‐1: tissue inhibitor of metalloproteinases‐1; TNF‐alpha: tumour necrosis factor‐alpha; WBC: white blood cell count.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Protocol | |
| Not an RCT | |
| Not an RCT; not exclusively bronchiectasis; duration of treatment < 4 weeks | |
| Not an RCT | |
| Not an RCT | |
| Not an RCT | |
| Macrolide used for treatment as opposed to prevention; duration of treatment < 4 weeks | |
| Not an RCT |
RCT: randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Aims: to evaluate effects of low‐dose erythromycin on sputum volume and lung function indices in steady‐state bronchiectasis Design: double‐blind placebo‐controlled trial (trial authors contacted to determine whether randomised) Total study duration: 6 months Number of study centres and location: single, Hong Kong Study setting: outpatient clinics at the University of Hong Kong Methods of recruitment: not reported Withdrawals: intervention group: 3 withdrawals ‐ 2 were unreliable attenders, 1 developed a maculopapular rash 5 days after erythromycin therapy; control group: 0 withdrawals Study start/end dates: October 1996/April 1997 Analysis by intent‐to‐treat: no |
| Participants | 24 adults were randomised. Inclusion criteria: 24‐hour sputum volume > 10 mL; absence of unstable systemic disease; and "steady‐state" bronchiectasis (< 10% alteration of 24‐hour sputum volume, forced expiratory volume in 1 second (FEV1), and forced vital capacity (FVC); in the absence of deterioration in cough, dyspnoea, wheezing, fever, or chest pain at baseline visits) Exclusion criteria: unreliable clinic attendance, adverse reaction to macrolides, women who were lactating Mean age: intervention group: 50 years; control group: 59 years Gender: intervention group: 8 women, 3 men; control group; 8 women, 2 men Bronchiectasis diagnosis: high‐resolution computed tomography (HRCT) Severity of condition: not reported Baseline lung function: not reported Smoking history: intervention group: never: 10, ex‐smoker: 1; control group: never: 8, ex‐smoker: 2 Baseline imbalances: no significant differences between groups |
| Interventions | Intervention group: erythromycin (n = 11) Dose: 500 mg; delivery mode: oral; frequency: 2/d; duration: 8 weeks Control group: placebo (n = 10) Adherence: not reported Run‐in phase: unclear Run‐out phase: unclear |
| Outcomes | Primary: unclear which is the primary outcome Secondary: unclear 24‐Hour sputum volume; sputum leucocyte density (per mL); sputum pathogenic density (colony‐forming unit (cfu) ‐ mL˜); sputum (sol phase) IL‐la, TNF‐a, and LTB4; pulmonary function test (FEV1, FVC) Post hoc analysis: unclear |
| Notes | Power calculation: Based on trial authors' experience, daily sputum volume might vary by as much as 10% between days in patients with stable bronchiectasis. With acceptance of a type I error of 0.05 and a type II error of 0.20 (power 0.80), study size for a randomised placebo‐controlled study of 20 participants (10 in each treatment group) would allow detection of 12% change in sputum volume. Trial registration: not reported Conflicts of interest: not declared Funders: CRCG grant from the University of Hong Kong Role of the sponsors: not reported Ethical approval: yes Conclusions: Results of this preliminary study, which is the first controlled study on the effects of erythromycin in chronic bronchial sepsis, show the efficacy of low‐dose and moderately long‐term erythromycin in steady‐state bronchiectasis. Low‐dose and long‐term erythromycin therapy might be a disease‐modifying treatment for idiopathic bronchiectasis. Additional studies should be performed to establish dose response, appropriate duration of therapy, and criteria for patient selection. |
cfu: colony‐forming unit; FEV1: forced expiratory volume in one second; FVC: forced vital capacity; HRCT: high‐resolution computed tomography; IL: interleukin; LTB: leukotriene B; TNF: tumour necrosis factor.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ≥ 1 exacerbation Show forest plot | 3 | 341 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.22, 0.54] |
| Analysis 1.1 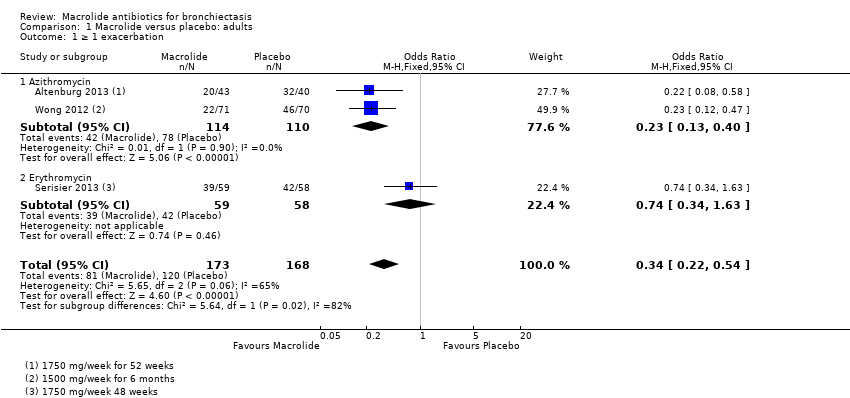 Comparison 1 Macrolide versus placebo: adults, Outcome 1 ≥ 1 exacerbation. | ||||
| 1.1 Azithromycin | 2 | 224 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.13, 0.40] |
| 1.2 Erythromycin | 1 | 117 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.34, 1.63] |
| 2 Hospitalisation: all‐cause Show forest plot | 2 | 151 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.19, 1.62] |
| Analysis 1.2 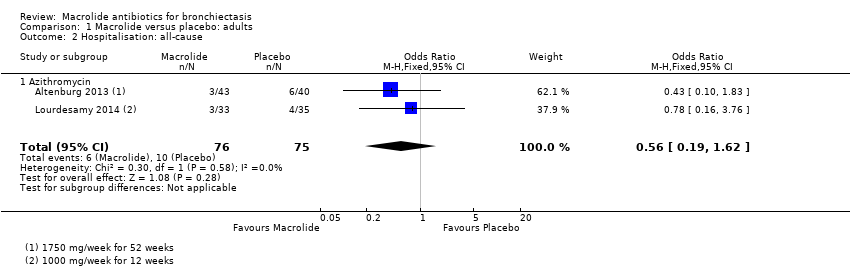 Comparison 1 Macrolide versus placebo: adults, Outcome 2 Hospitalisation: all‐cause. | ||||
| 2.1 Azithromycin | 2 | 151 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.19, 1.62] |
| 3 Serious adverse events Show forest plot | 3 | 326 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.20, 1.23] |
| Analysis 1.3  Comparison 1 Macrolide versus placebo: adults, Outcome 3 Serious adverse events. | ||||
| 3.1 Azithromycin | 2 | 209 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.20, 1.34] |
| 3.2 Erythromycin | 1 | 117 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.07] |
| 4 Sputum weight (g): endpoint Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1 Macrolide versus placebo: adults, Outcome 4 Sputum weight (g): endpoint. | ||||
| 4.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 FEV1 (% predicted): endpoint Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.5  Comparison 1 Macrolide versus placebo: adults, Outcome 5 FEV1 (% predicted): endpoint. | ||||
| 5.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 FEV1 (% predicted): change (post bronchodilator) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.6  Comparison 1 Macrolide versus placebo: adults, Outcome 6 FEV1 (% predicted): change (post bronchodilator). | ||||
| 6.1 Erythromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 FEV1 (L): endpoint Show forest plot | 2 | 94 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.17, 0.22] |
| Analysis 1.7 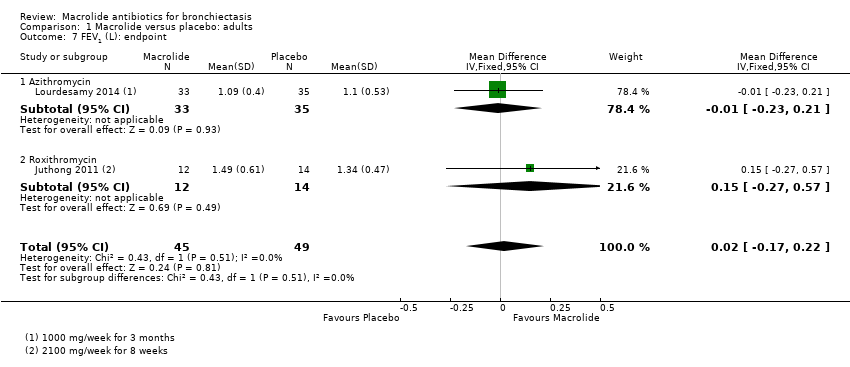 Comparison 1 Macrolide versus placebo: adults, Outcome 7 FEV1 (L): endpoint. | ||||
| 7.1 Azithromycin | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.23, 0.21] |
| 7.2 Roxithromycin | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.27, 0.57] |
| 8 FEV1 (L): change Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.8 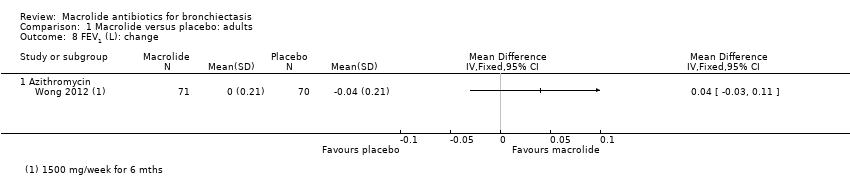 Comparison 1 Macrolide versus placebo: adults, Outcome 8 FEV1 (L): change. | ||||
| 8.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 FVC (% predicted): endpoint Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.9 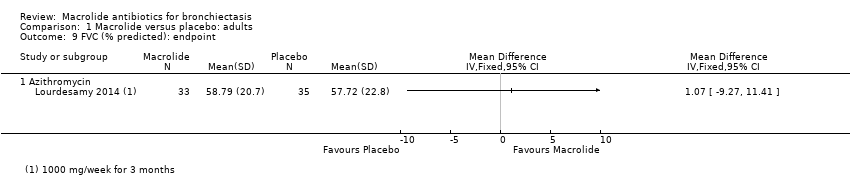 Comparison 1 Macrolide versus placebo: adults, Outcome 9 FVC (% predicted): endpoint. | ||||
| 9.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 FVC (L): endpoint Show forest plot | 2 | 94 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.19, 0.36] |
| Analysis 1.10 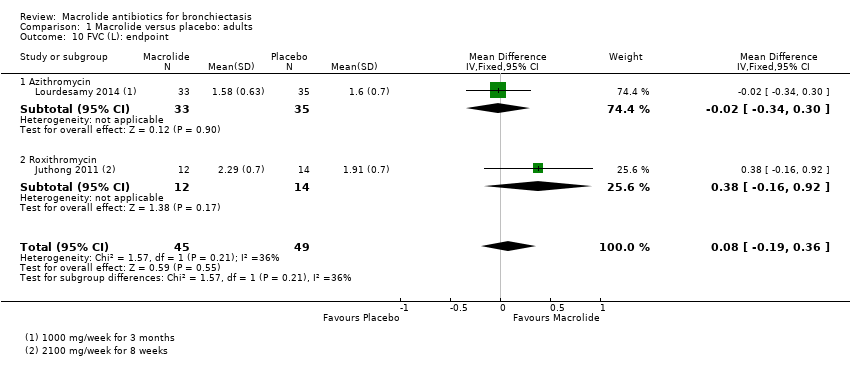 Comparison 1 Macrolide versus placebo: adults, Outcome 10 FVC (L): endpoint. | ||||
| 10.1 Azithromycin | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.34, 0.30] |
| 10.2 Roxithromycin | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 0.38 [‐0.16, 0.92] |
| 11 FVC (L): change Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.11  Comparison 1 Macrolide versus placebo: adults, Outcome 11 FVC (L): change. | ||||
| 11.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 FEV1/FVC: endpoint Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.12  Comparison 1 Macrolide versus placebo: adults, Outcome 12 FEV1/FVC: endpoint. | ||||
| 12.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Adverse events Show forest plot | 5 | 435 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.51, 1.35] |
| Analysis 1.13  Comparison 1 Macrolide versus placebo: adults, Outcome 13 Adverse events. | ||||
| 13.1 Azithromycin | 3 | 292 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.41, 1.45] |
| 13.2 Erythromycin | 1 | 117 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.51, 2.62] |
| 13.3 Roxithromycin | 1 | 26 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.83] |
| 14 Azithromycin‐resistant bacteria (any) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.14  Comparison 1 Macrolide versus placebo: adults, Outcome 14 Azithromycin‐resistant bacteria (any). | ||||
| 14.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 6‐Minute walk test: change Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.15 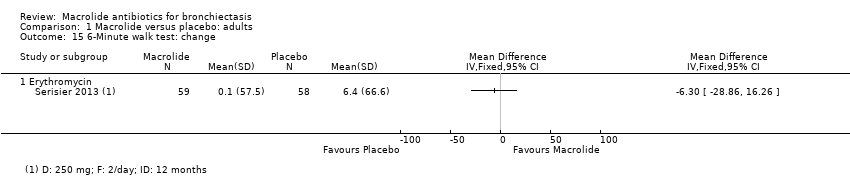 Comparison 1 Macrolide versus placebo: adults, Outcome 15 6‐Minute walk test: change. | ||||
| 15.1 Erythromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Quality of life: endpoint Show forest plot | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐8.90 [‐13.13, ‐4.67] |
| Analysis 1.16  Comparison 1 Macrolide versus placebo: adults, Outcome 16 Quality of life: endpoint. | ||||
| 16.1 Azithromycin | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐8.90 [‐13.13, ‐4.67] |
| 17 Quality of life: change Show forest plot | 4 | 305 | Mean Difference (IV, Fixed, 95% CI) | ‐2.86 [‐5.67, ‐0.04] |
| Analysis 1.17 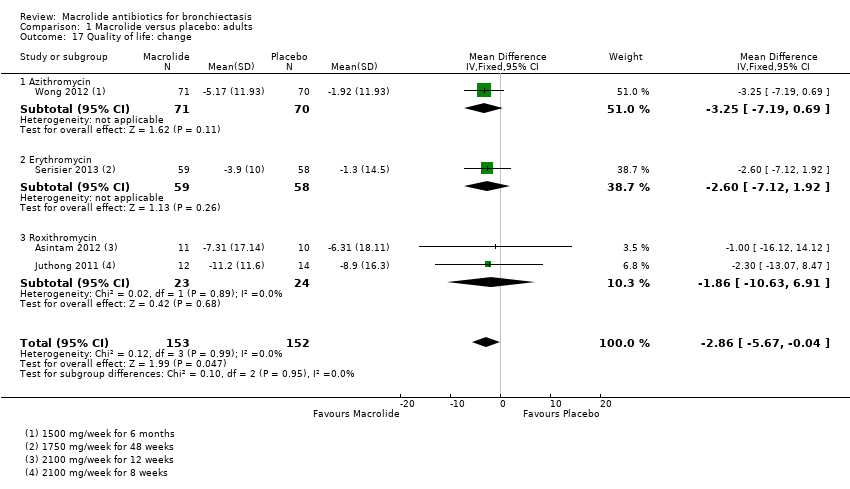 Comparison 1 Macrolide versus placebo: adults, Outcome 17 Quality of life: change. | ||||
| 17.1 Azithromycin | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | ‐3.25 [‐7.19, 0.69] |
| 17.2 Erythromycin | 1 | 117 | Mean Difference (IV, Fixed, 95% CI) | ‐2.60 [‐7.12, 1.92] |
| 17.3 Roxithromycin | 2 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐1.86 [‐10.63, 6.91] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ≥ 1 exacerbation Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 2.1 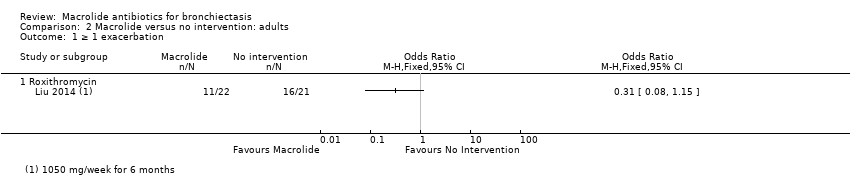 Comparison 2 Macrolide versus no intervention: adults, Outcome 1 ≥ 1 exacerbation. | ||||
| 1.1 Roxithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 QoL SGRQ: endpoint total score Show forest plot | 2 | 89 | Mean Difference (IV, Fixed, 95% CI) | ‐8.81 [‐14.33, ‐3.28] |
| Analysis 2.2 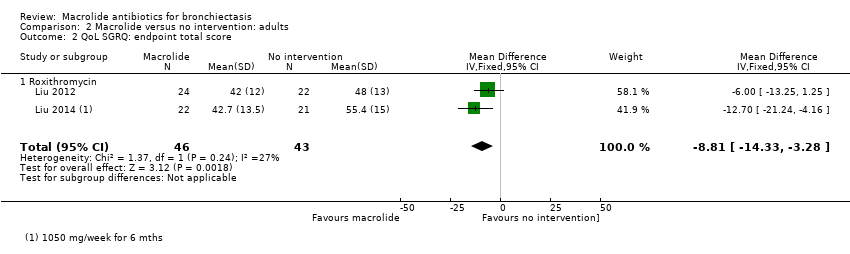 Comparison 2 Macrolide versus no intervention: adults, Outcome 2 QoL SGRQ: endpoint total score. | ||||
| 2.1 Roxithromycin | 2 | 89 | Mean Difference (IV, Fixed, 95% CI) | ‐8.81 [‐14.33, ‐3.28] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Hospitalisation: all‐cause Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.1 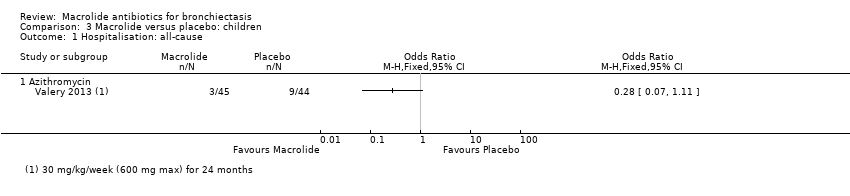 Comparison 3 Macrolide versus placebo: children, Outcome 1 Hospitalisation: all‐cause. | ||||
| 1.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Serious adverse events Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.2 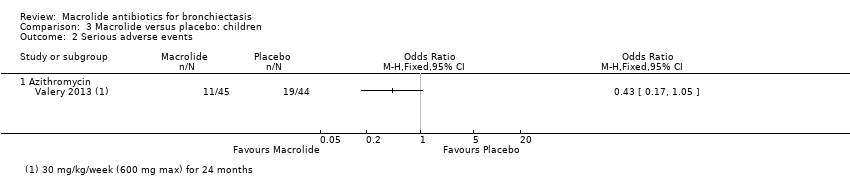 Comparison 3 Macrolide versus placebo: children, Outcome 2 Serious adverse events. | ||||
| 2.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Sputum purulence score: endpoint Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.3  Comparison 3 Macrolide versus placebo: children, Outcome 3 Sputum purulence score: endpoint. | ||||
| 3.1 Roxithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 FEV1 (% predicted): endpoint Show forest plot | 2 | 65 | Mean Difference (IV, Fixed, 95% CI) | 1.73 [‐3.32, 6.78] |
| Analysis 3.4  Comparison 3 Macrolide versus placebo: children, Outcome 4 FEV1 (% predicted): endpoint. | ||||
| 4.1 Azithromycin | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 3.70 [‐5.99, 13.39] |
| 4.2 Roxithromycin | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐4.91, 6.91] |
| 5 Adverse events Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.5 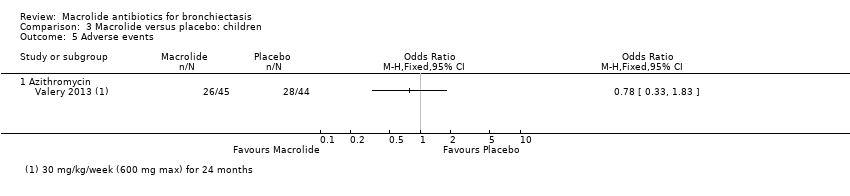 Comparison 3 Macrolide versus placebo: children, Outcome 5 Adverse events. | ||||
| 5.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Azithromycin‐resistant bacteria (any) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.6 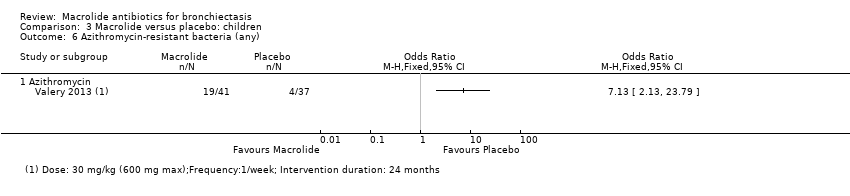 Comparison 3 Macrolide versus placebo: children, Outcome 6 Azithromycin‐resistant bacteria (any). | ||||
| 6.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Azithromycin‐resistant Streptococcus pneumoniae Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.7  Comparison 3 Macrolide versus placebo: children, Outcome 7 Azithromycin‐resistant Streptococcus pneumoniae. | ||||
| 7.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Azithromycin‐resistant Staphylococcus aureus Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 3.8  Comparison 3 Macrolide versus placebo: children, Outcome 8 Azithromycin‐resistant Staphylococcus aureus. | ||||
| 8.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

Study flow diagram.
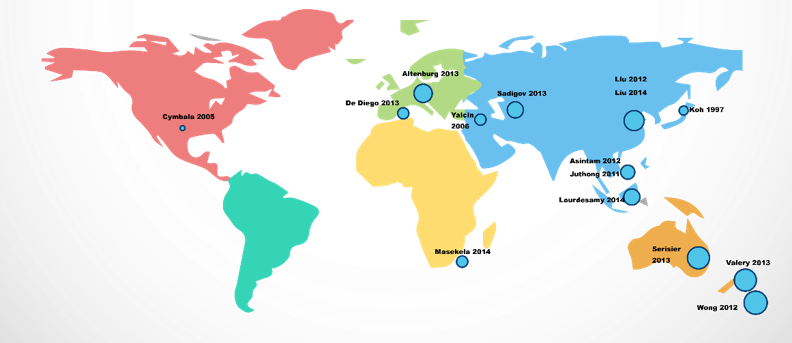
Global distribution of studies.
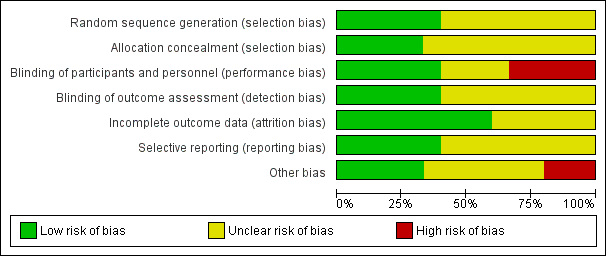
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
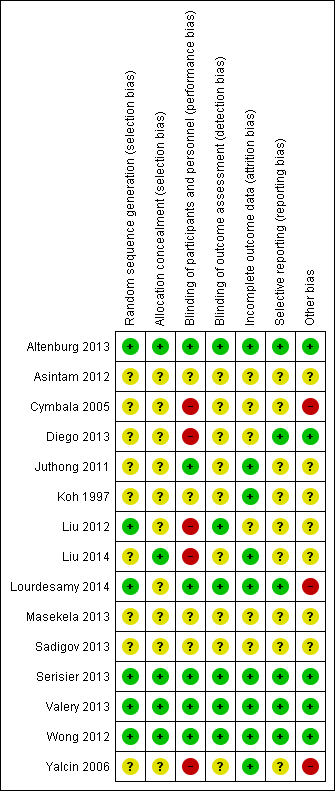
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Analysis 1.1. Cates plot showing the absolute reduction in numbers of participants experiencing one or more exacerbations in adults treated with macrolides compared with placebo (OR 0.34, 95% CI 0.22 to 0.54). 714 people per 1000 in the placebo group experienced one or more exacerbations compared with 459 (95% CI 355 to 574) per 1000 in the macrolide group.
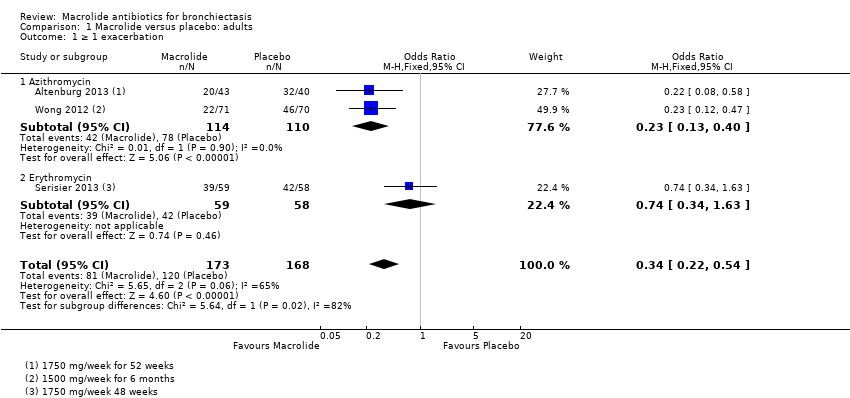
Comparison 1 Macrolide versus placebo: adults, Outcome 1 ≥ 1 exacerbation.
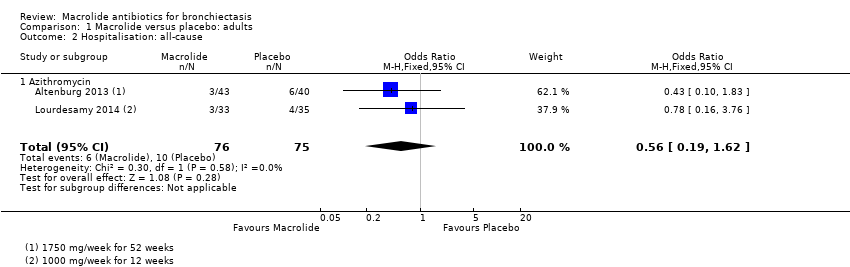
Comparison 1 Macrolide versus placebo: adults, Outcome 2 Hospitalisation: all‐cause.
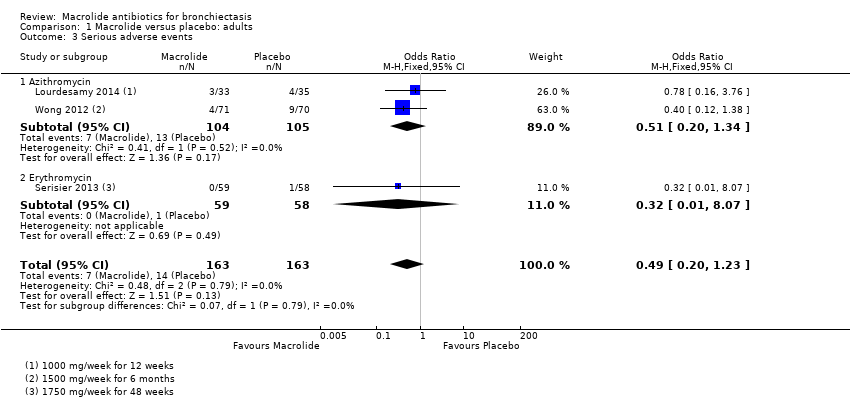
Comparison 1 Macrolide versus placebo: adults, Outcome 3 Serious adverse events.

Comparison 1 Macrolide versus placebo: adults, Outcome 4 Sputum weight (g): endpoint.

Comparison 1 Macrolide versus placebo: adults, Outcome 5 FEV1 (% predicted): endpoint.
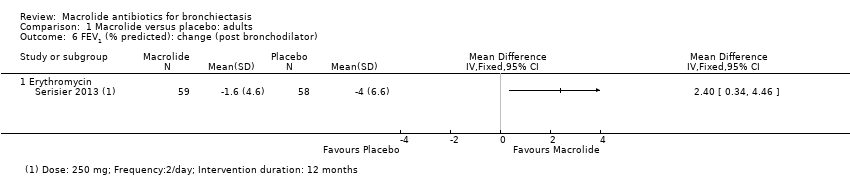
Comparison 1 Macrolide versus placebo: adults, Outcome 6 FEV1 (% predicted): change (post bronchodilator).

Comparison 1 Macrolide versus placebo: adults, Outcome 7 FEV1 (L): endpoint.
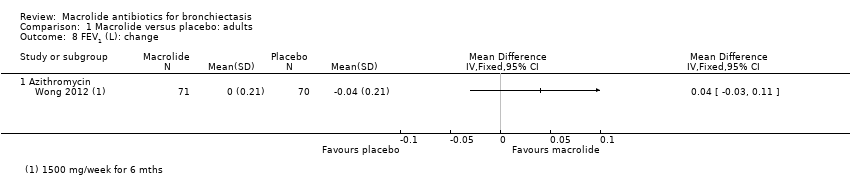
Comparison 1 Macrolide versus placebo: adults, Outcome 8 FEV1 (L): change.

Comparison 1 Macrolide versus placebo: adults, Outcome 9 FVC (% predicted): endpoint.

Comparison 1 Macrolide versus placebo: adults, Outcome 10 FVC (L): endpoint.
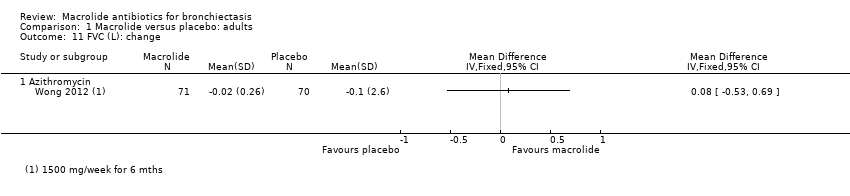
Comparison 1 Macrolide versus placebo: adults, Outcome 11 FVC (L): change.

Comparison 1 Macrolide versus placebo: adults, Outcome 12 FEV1/FVC: endpoint.

Comparison 1 Macrolide versus placebo: adults, Outcome 13 Adverse events.

Comparison 1 Macrolide versus placebo: adults, Outcome 14 Azithromycin‐resistant bacteria (any).
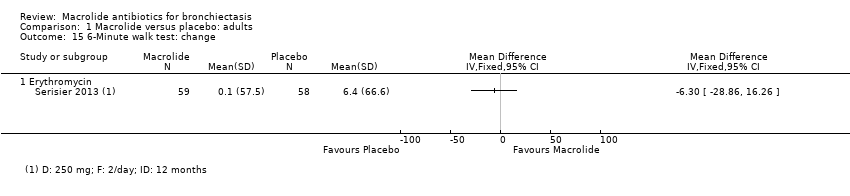
Comparison 1 Macrolide versus placebo: adults, Outcome 15 6‐Minute walk test: change.

Comparison 1 Macrolide versus placebo: adults, Outcome 16 Quality of life: endpoint.
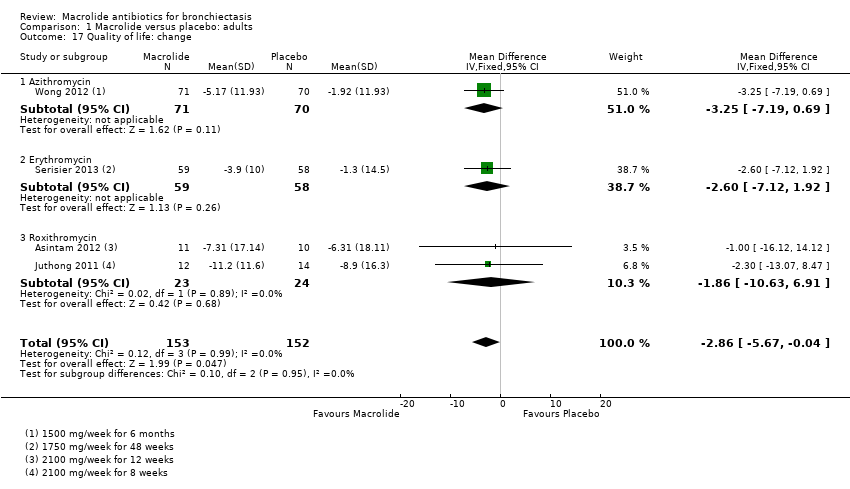
Comparison 1 Macrolide versus placebo: adults, Outcome 17 Quality of life: change.

Comparison 2 Macrolide versus no intervention: adults, Outcome 1 ≥ 1 exacerbation.

Comparison 2 Macrolide versus no intervention: adults, Outcome 2 QoL SGRQ: endpoint total score.

Comparison 3 Macrolide versus placebo: children, Outcome 1 Hospitalisation: all‐cause.
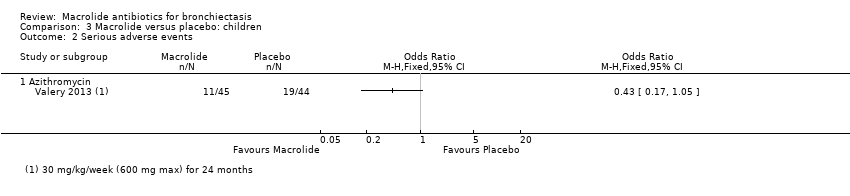
Comparison 3 Macrolide versus placebo: children, Outcome 2 Serious adverse events.
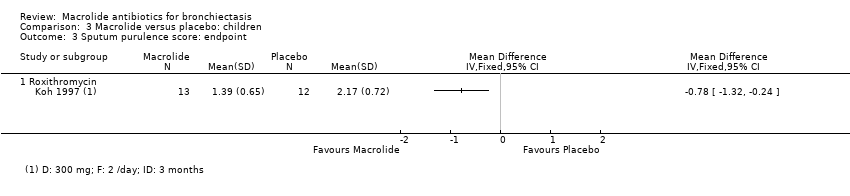
Comparison 3 Macrolide versus placebo: children, Outcome 3 Sputum purulence score: endpoint.
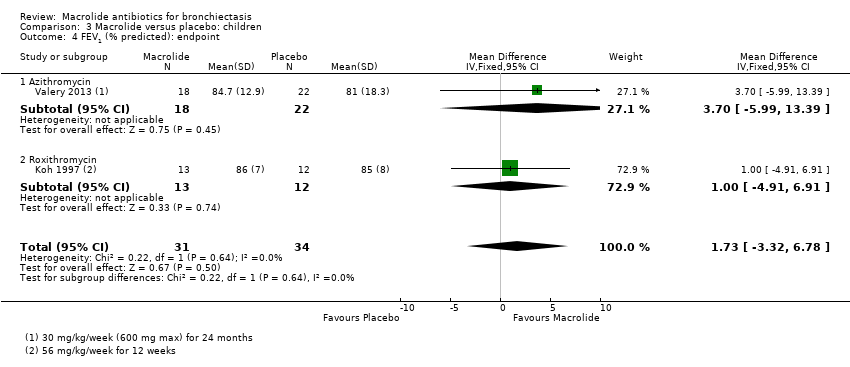
Comparison 3 Macrolide versus placebo: children, Outcome 4 FEV1 (% predicted): endpoint.

Comparison 3 Macrolide versus placebo: children, Outcome 5 Adverse events.

Comparison 3 Macrolide versus placebo: children, Outcome 6 Azithromycin‐resistant bacteria (any).
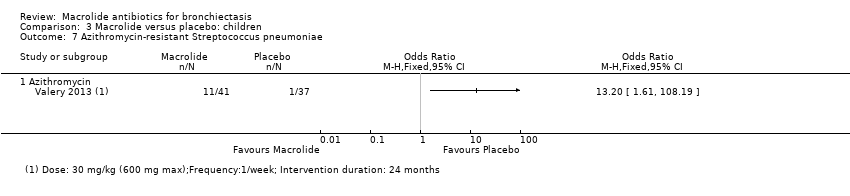
Comparison 3 Macrolide versus placebo: children, Outcome 7 Azithromycin‐resistant Streptococcus pneumoniae.
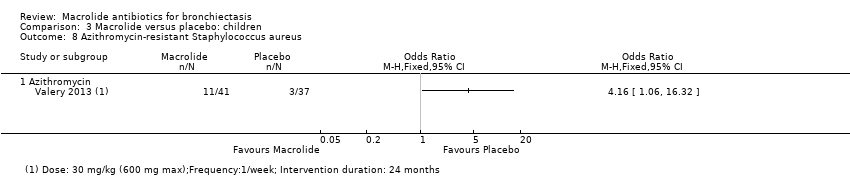
Comparison 3 Macrolide versus placebo: children, Outcome 8 Azithromycin‐resistant Staphylococcus aureus.
| Macrolides compared with placebo for adults with bronchiectasis | ||||||
| Patient or population: adults with bronchiectasis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with macrolides | |||||
| ≥ 1 exacerbation | 714 per 1000 | 459 per 1000 | OR 0.34 | 341 | ⊕⊕⊕⊝ | 2 studies azithromycin (1750 mg/week for 52 weeks; 1500 mg/week for 6 months) 1 study erythromycin (3500 mg/week for 48 weeks) |
| Hospitalisation: all cause | 133 per 1000 | 79 per 1000 | OR 0.56 | 151 | ⊕⊕⊝⊝ | 2 studies azithromycin (1000 mg/week for 12 weeks; 1750 mg/week for 52 weeks) |
| Serious adverse events | 86 per 1000 | 44 per 1000 | OR 0.49 | 326 | ⊕⊕⊝⊝ | 2 studies azithromycin (1500 mg/week for 6 months; 1000 mg/week for 12 weeks) 1 study erythromycin (3500 mg/week for 48 weeks) |
| All‐cause mortality | 0 per 1000 | 0 per 1000 | not estimable | 540 | ⊕⊕⊝⊝ | 4 studies azithromycin (1000 to 1750 mg/week for 12 to 52 weeks) |
| Quality of life: endpoint | Mean SGRQ score at endpoint in placebo groups was 39.1 points. | MD 8.90 lower (13.13 lower to 4.67 lower) | ‐ | 68 | ⊕⊕⊕⊝ | 1 study azithromycin (1000 mg/week for 12 weeks) |
| Quality of life: change | Mean change in SGRQ score ranged from ‐1.3 to ‐8.9 points. | MD 2.86 lower | ‐ | 305 | ⊕⊕⊝⊝ | 1 study azithromycin (1500 mg/week for 6 months) |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aEffect observed only with azithromycin (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). bUnclear allocation concealment and baseline imbalances on Lourdesamy (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). cTwo small studies and wide confidence interval (one point deducted for imprecision). dWide confidence interval (one point deducted for imprecision). eIn three of the seven studies, study methods were not clearly reported (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). fA total of 28 participants across four studies were lost to follow‐up with no further details available and unclear details of withdrawals in one study (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). gRandomisation, blinding, and other study methods unclear in two studies (Asintam; Juthong) (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). hWide confidence interval and mean difference does not exceed the threshold for clinical significance (one point deducted for imprecision). | ||||||
| Macrolides compared with no intervention for adults with bronchiectasis | ||||||
| Patient or population: adults with bronchiectasis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with no intervention | Risk with macrolides | |||||
| ≥ 1 exacerbation | Study population | OR 0.31 | 43 | ⊕⊕⊕⊝ | Roxithromycin (1050 mg/week for 6 months) | |
| 762 per 1000 | 498 per 1000 | |||||
| Hospitalisations ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Serious adverse events ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Mortality | No deaths in two trials, although in 1 study (azithromycin), 6 participants were lost to follow‐up | not estimable | 88 | ⊕⊝⊝⊝ | 1 study azithromycin (750 mg/week for 3 months) | |
| QoL SGRQ: endpoint total score | Mean SGRQ: endpoint total score of 51.7 points | MD 8.81 lower (14.33 lower to 3.28 lower) | ‐ | 89 | ⊕⊕⊕⊝ | 1 study roxithromycin (1050 mg/week for 6 months) |
| QoL SGRQ: change in total score | Mean SGRQ: change in total score of 4.1 | MD 12 lower | ‐ | 30 | ⊕⊕⊕⊝ | Azithromycin (750 mg/week for 3 months) |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aOpen‐label study (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). bUnclear randomisation and study methods (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). c6 participants in one study lost to follow‐up and no further details reported (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). | ||||||
| Macrolides compared with placebo for children with bronchiectasis | ||||||
| Patient or population: children with bronchiectasis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with macrolides | |||||
| Exacerbation frequency | Number of exacerbations 195 (median: 4 range 0‐14) | Number of exacerbations 104 (median: 2 range 0‐9) | IRR 0.50 95% CI 0.35 to 0.71 | 89 | ⊕⊕⊝⊝ | Azithromycin (30 mg/kg/week for up to 24 months) |
| Hospitalisation: all‐cause | 205 per 1000 | 67 per 1000 | OR 0.28 | 89 | ⊕⊕⊝⊝ | Azithromycin (30 mg/kg/week for 24 months) |
| Serious adverse events | 432 per 1000 | 246 per 1000 | OR 0.43 | 89 | ⊕⊕⊝⊝ | Azithromycin (30 mg/kg/week for 24 months) |
| Mortality | 1 child died but study group was not stated. | ‐ | 42 | ⊕⊕⊝⊝ | Erythromycin (875 to 1750 mg/kg/week for 52 weeks) | |
| Quality of life not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aWide confidence interval that includes 1 (no difference) (one point deducted for imprecision). bLow event rates and low numbers (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). cUnclear information on randomisation, blinding, and other study methods (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). dNo information on participants lost to follow‐up (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). | ||||||
| Macrolides compared with no intervention for children with bronchiectasis | ||||||
| Patient or population: children with bronchiectasis | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | No. of participants | Quality of the evidence | Comments | |
| Risk with no intervention | Risk with macrolides | |||||
| Exacerbations ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Hospitalisation ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Serious adverse events ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Mortality | 0 per 1000 | 0 per 1000 | not estimable | 34 | ⊕⊕⊝⊝ | Clarithromycin (105 mg/kg/week for 3 months) |
| Quality of life ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence. | ||||||
| aInsufficient information on study methods and procedures (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). bNot blinded (one point deducted in relation to design and implementation of available studies suggesting likelihood of bias). | ||||||
| Study | Adults/ Children | No. of participants | Type of macrolide | Macrolide dose | Frequency | Delivery mode | Combined weekly dose | Comparison | Duration (months unless stated) |
| Altenburg 2013 | Adults | 83 | Azithromycin | 250 mg | Once daily | Oral | 1750 mg | Placebo | 12 |
| Asintam 2012 | Adults | 30 | Roxithromycin | 300 mg | Once daily | Oral | 2100 mg | Placebo | 12 weeks |
| Cymbala 2005 | Adults | 12 | Azithromycin | 500 mg | 3 days per week | Oral | 1000 mg | No intervention | 6 |
| Diego 2013 | Adults | 36 | Azithromycin | 250 mg | 3 days per week | Oral | 750 mg | No intervention | 3 |
| Juthong 2011 | Adults | 26 | Roxithromycin | 300 mg | Once daily | Oral | 2100 mg | Placebo | 8 weeks |
| Koh 1997 | Children | 25 | Roxithromycin | 4 mg/kg | Twice daily | Oral | 56 mg/kg | Placebo | 12 weeks |
| Liu 2012 | Adults | 50 | Roxithromycin, ambroxol hydrochloride | 150 mg | Once daily | Oral | 1050 mg | Ambroxol hydrochloride (no intervention) | 6 |
| Liu 2014 | Adults | 52 | Roxithromycin | 150 mg | Once daily | Oral | 1050 mg | No intervention | 6 |
| Lourdesamy 2014 | Adults | 78 | Azithromycin | 1000 mg | Weekly | 1000 mg | Placebo | 3 | |
| Masekela 2013 | Children | 42 | Erythromycin | 125 mg for children weighing < 15 kg and 250 mg ≥ 15 kg | Daily | Oral | 875 mg for children weighing < 15 kg and 1750 mg ≥ 15 kg | Placebo | 12 |
| Sadigov 2013 | Adults | 65 | Azithromycin | 500 mg | 3 days per week | Oral | 1500 mg | Placebo | 6 |
| Serisier 2013 | Adults | 117 | Erythromycin | 250 mg | Twice daily | Oral | 3500 mg | Placebo | 11 |
| Valery 2013 | Children | 89 | Azithromycin | 30 mg/kg up to a maximum of 600 mg | Once a week | Oral | 30 mg/kg up to a maximum of 600 mg | Placebo | 24 |
| Wong 2012 | Adults | 141 | Azithromycin | 500 mg | 3 days per week | Oral | 1500 mg | Placebo | 6 |
| Yalcin 2006 | Children | 34 | Clarithromycin, supportive therapies | 15 mg/kg | Daily | Oral | 105 mg/kg | Supportive therapies (no intervention) | 3 |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ≥ 1 exacerbation Show forest plot | 3 | 341 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.22, 0.54] |
| 1.1 Azithromycin | 2 | 224 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.13, 0.40] |
| 1.2 Erythromycin | 1 | 117 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.34, 1.63] |
| 2 Hospitalisation: all‐cause Show forest plot | 2 | 151 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.19, 1.62] |
| 2.1 Azithromycin | 2 | 151 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.19, 1.62] |
| 3 Serious adverse events Show forest plot | 3 | 326 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.20, 1.23] |
| 3.1 Azithromycin | 2 | 209 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.20, 1.34] |
| 3.2 Erythromycin | 1 | 117 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 8.07] |
| 4 Sputum weight (g): endpoint Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 FEV1 (% predicted): endpoint Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 FEV1 (% predicted): change (post bronchodilator) Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Erythromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 FEV1 (L): endpoint Show forest plot | 2 | 94 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.17, 0.22] |
| 7.1 Azithromycin | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.23, 0.21] |
| 7.2 Roxithromycin | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.27, 0.57] |
| 8 FEV1 (L): change Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 FVC (% predicted): endpoint Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 FVC (L): endpoint Show forest plot | 2 | 94 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.19, 0.36] |
| 10.1 Azithromycin | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.34, 0.30] |
| 10.2 Roxithromycin | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 0.38 [‐0.16, 0.92] |
| 11 FVC (L): change Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 FEV1/FVC: endpoint Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Azithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Adverse events Show forest plot | 5 | 435 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.51, 1.35] |
| 13.1 Azithromycin | 3 | 292 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.41, 1.45] |
| 13.2 Erythromycin | 1 | 117 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.51, 2.62] |
| 13.3 Roxithromycin | 1 | 26 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.83] |
| 14 Azithromycin‐resistant bacteria (any) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 14.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 6‐Minute walk test: change Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Erythromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Quality of life: endpoint Show forest plot | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐8.90 [‐13.13, ‐4.67] |
| 16.1 Azithromycin | 1 | 68 | Mean Difference (IV, Fixed, 95% CI) | ‐8.90 [‐13.13, ‐4.67] |
| 17 Quality of life: change Show forest plot | 4 | 305 | Mean Difference (IV, Fixed, 95% CI) | ‐2.86 [‐5.67, ‐0.04] |
| 17.1 Azithromycin | 1 | 141 | Mean Difference (IV, Fixed, 95% CI) | ‐3.25 [‐7.19, 0.69] |
| 17.2 Erythromycin | 1 | 117 | Mean Difference (IV, Fixed, 95% CI) | ‐2.60 [‐7.12, 1.92] |
| 17.3 Roxithromycin | 2 | 47 | Mean Difference (IV, Fixed, 95% CI) | ‐1.86 [‐10.63, 6.91] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 ≥ 1 exacerbation Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Roxithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 QoL SGRQ: endpoint total score Show forest plot | 2 | 89 | Mean Difference (IV, Fixed, 95% CI) | ‐8.81 [‐14.33, ‐3.28] |
| 2.1 Roxithromycin | 2 | 89 | Mean Difference (IV, Fixed, 95% CI) | ‐8.81 [‐14.33, ‐3.28] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Hospitalisation: all‐cause Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Serious adverse events Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Sputum purulence score: endpoint Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Roxithromycin | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 FEV1 (% predicted): endpoint Show forest plot | 2 | 65 | Mean Difference (IV, Fixed, 95% CI) | 1.73 [‐3.32, 6.78] |
| 4.1 Azithromycin | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | 3.70 [‐5.99, 13.39] |
| 4.2 Roxithromycin | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐4.91, 6.91] |
| 5 Adverse events Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Azithromycin‐resistant bacteria (any) Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Azithromycin‐resistant Streptococcus pneumoniae Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Azithromycin‐resistant Staphylococcus aureus Show forest plot | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 Azithromycin | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

