L’iridotomie pour ralentir la progression de la perte du champ visuel dans le glaucome à angle fermé
Referencias
References to studies included in this review
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Study design: randomized controlled trial Study grouping: parallel group Sample size calculation: not reported | |
| Participants | Enrollment: 476 participants with bilateral narrow angles from Singapore Baseline Characteristics: Overall
Inclusion criteria: participants with bilateral narrow angle, age 50 years and older who provide informed consent obtained prior to or at the baseline visit Exclusion criteria: presence of PAS, IOP > 21 mm Hg; glaucomatous optic neuropathy and/or cup‐to‐disc ratio > 0.7; secondary angle closure such as uveitis; neovascularization etc.; prior intraocular surgery or penetrating eye injury; corneal disorders such as corneal endothelial dystrophy except mild corneal guttae; evidence of prior acute angle closure event; high risk of acute angle closure; significant cataract and visual acuity less than 20/40; constant use of contact lens for refractive correction; chronic use of topical or systemic steroids; established retinopathies on ocular treatments (e.g. Diabetic); any other disease which is likely to cause field loss in next 3 years; severe health problems decreasing life expectancy to less than 1 year. | |
| Interventions | Intervention 1: iridotomy using sequential argon–neodymium–yttrium–aluminum–garnet laser with argon settings of 500 mW to 1000 mW power with a spot size of 50 mA for a duration of 0.05 seconds and a yttrium–aluminum–garnet setting of 2 mJ to 5 mJ and pretreatment with 2% pilocarpine instilled into the eye.
Intervention 2: no treatment | |
| Outcomes | Primary outcomes, per trial registration
Secondary outcomes, per trial registration
Intervals at which outcomes assessed: 1 year, 2 years, 3 years, 4 years, and 5 years. | |
| Notes | Start date: January 2005 Funding source(s): National Medical Research Council (NMRC), Singapore Conflicts of interest: none Publication language: English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported in available records. |
| Allocation concealment (selection bias) | Unclear risk | Not reported in available records. |
| Blinding of participants and personnel (performance bias) | High risk | Trial described as "Open‐label" on ClinicalTrials.gov (NCT00347178). |
| Blinding of outcome assessment (detection bias) | High risk | Trial described as "Open‐label" on ClinicalTrials.gov (NCT00347178). |
| Incomplete outcome data (attrition bias) | Unclear risk | Full trial report not yet published. |
| Selective reporting (reporting bias) | Unclear risk | Full trial report not yet published. |
| Other bias | Unclear risk | Full trial report not yet published. |
| Methods | Study design: randomized controlled trial Study grouping: parallel group Sample size calculation: trial was designed to detect a 30% difference in the rate of progression from PACS to PAC; estimated 870 participants needed assuming an attrition rate up to 20%; power not reported | |
| Participants | Enrollment: 775 participants from China (ZAP; Jiang 2014 report) Baseline Characteristics: Overall
Inclusion criteria: 'static' gonioscopy identifying 6 or more clock hours of angle circumference in which the posterior (usually pigmented) trabecular meshwork cannot be seen in both eyes Exclusion criteria: evidence of primary angle closure (a narrow angle as defined above, but with PAS and/or IOP > 21 mmHg) or glaucomatous optic neuropathy; age less than 50 years or greater than 70 years of age; plan to move from the area within the next 5 years; severe health problems precluding follow‐up such as end‐stage heart disease, kidney disease, or lung disease, or terminal cancer; prior intraocular surgery or penetrating eye injury as observed by the clinician examining the subject (i.e. not per patient report); media opacity preventing laser iridotomy (e.g. corneal opacity); evidence of a prior acute angle closure attack (the presence of iris whorling, focal iris atrophy, or glaucomflecken with a history of an acute red eye and decreased vision); people who are unable to give their own informed consent; people with an excessively high risk of acute angle closure crisis (i.e. subjects who have a rise in IOP of > 15 mmHg on dilation with phenylephrine 5% and tropicamide 0.5% (in either eye) or a rise in IOP of > 15 mmHg after a 15‐minute dark‐prone provocative test); best corrected visual acuity worse than 20/40 presumed due to cataract. | |
| Interventions | Intervention 1: iridotomy using neodymium‐yttrium–aluminum–garnet (Nd:YAG) laser (Visulas YAG III; Zeiss Meditec, Dublin, CA) starting at 1.5 mJ with 1 drop of pilocarpine 2% (Pharmacy of Zhongshan Ophthalmic Center, Guangzhou, China) instilled in the intervention eye 15 minutes before treatment.
Intervention 2: no treatment | |
| Outcomes | Primary outcomes, per trial registration
Secondary outcomes, per trial registration
Intervals at which outcomes assessed: 6, 18, 30, 42, 54, and 72 months | |
| Notes | Start date: March 2008 Funding source(s): Fight for Sight; Sun Yat‐sen Univeristy Clinical Research 5010 Project; Fundamental Research Funds of State Key Lab Conflicts of interest: none Publication language: English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A computer‐generated list of random numbers was used to select the eye to be treated by LPI." |
| Allocation concealment (selection bias) | Low risk | "The random number was kept in a sealed envelope with the corresponding sequential number written on the cover and was opened by a masked research nurse prior to LI treatment." |
| Blinding of participants and personnel (performance bias) | High risk | "Single centre randomised controlled trial (not masked)" |
| Blinding of outcome assessment (detection bias) | Unclear risk | Intraocular pressure was measured by a research nurse who was unaware of treatment status of each eye; however, there is insufficient information for all outcomes. |
| Incomplete outcome data (attrition bias) | Unclear risk | Full trial report not yet published. Only immediate IOP change, risk factors for IOP spikes, and angle width after laser treatment in PACGs treated by prophylactic LPI is reported for this trial. The data on other outcomes from the RCT are not reported though secondary analysis using nested observational designs have been published. |
| Selective reporting (reporting bias) | Unclear risk | Full trial report not yet published. |
| Other bias | Unclear risk | Full trial report not yet published‐‐limited amount of data has been reported. |
IOP: intraocular pressure
PI: laser peripheral iridotomy
PACG: primary angle‐closure glaucoma
PAS: peripheral anterior synechiae
RCT: randomized controlled trial
SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Intervention did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Study design did not meet the eligibility criteria | |
| Intervention did not meet the eligibility criteria |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Angle Width Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.1  Comparison 1 Iridotomy vs No treatment, Outcome 1 Angle Width. | ||||
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.2  Comparison 1 Iridotomy vs No treatment, Outcome 2 Adverse events. | ||||
| 2.1 IOP spike (rise greater than or equal to 8 mmHg) at 1 hour | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
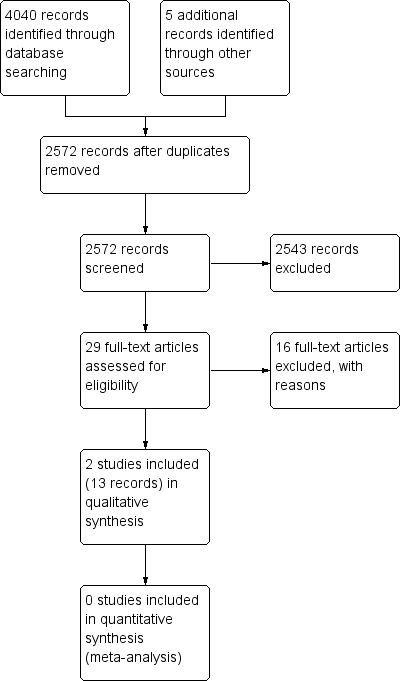
Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
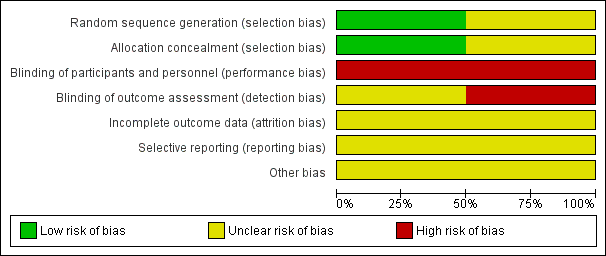
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Iridotomy vs No treatment, Outcome 1 Angle Width.

Comparison 1 Iridotomy vs No treatment, Outcome 2 Adverse events.
| Iridotomy compared to no iridotomy for patients with primary angle‐closure suspect, primary angle closure, or primary angle‐closure glaucoma | ||||||
| Patient or population: patients with primary angle‐closure suspect, primary angle closure, or primary angle‐closure glaucoma | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of eyes | Certainty of the evidence | Comments | |
| Risk with no iridotomy | Risk with Iridotomy | |||||
| Proportion of progressive visual field loss at 1 year | Not reported | Not reported | ‐ | ‐ | ‐ | |
| Intraocular pressure: mean IOP at 1 year | Not reported | Not reported | ‐ | ‐ | ‐ | |
| Gonioscopic findings: mean angle width at 1 year | The mean angle width was 11.3° in the no iridotomy group | The mean angle width in the iridotomy group was 12.7° higher | MD 12.7 | 1550 | ⊕⊕⊕⊝ | Participants in the study were primary angle‐closure suspects. Data were only available at 18 months. |
| Need for additional surgery: proportion of participants who received additional surgery to control IOP at 1 year | Not reported | Not reported | ‐ | ‐ | ‐ | |
| Medications: mean number of medications used to control IOP at 1 year | Not reported | Not reported | ‐ | ‐ | ‐ | |
| Quality of life measures | Not reported | Not reported | ‐ | ‐ | ‐ | |
| Adverse events ‒ IOP spike (rise greater than or equal to 8 mmHg) at 1 hour | 4 per 1000 | 98 per 1000 | RR 24.00 | 1468 | ⊕⊕⊝⊝ | Participants in the study were primary angle‐closure suspects. |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded by one level for risk of bias, as the study is at unclear risk of bias for incomplete outcome data, selective outcome reporting, and other sources of bias due to the lack of availability of a full trial report. 2 Downgraded by one level for imprecision, as the confidence interval of the risk ratio between the groups is wide. | ||||||
| Primary angle‐closure suspect (PACS) | Primary angle closure (PAC) | Primary angle‐closure glaucoma (PACG) | |
| Iridotrabecular contact greater than or equal to 180° | X | X | X |
| Elevated intraocular pressure OR peripheral anterior synechiae | X | X | |
| Optic nerve damage | X |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Angle Width Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 IOP spike (rise greater than or equal to 8 mmHg) at 1 hour | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

