استفاده از ایریدوتومی برای آهسته شدن سرعت پیشروی از دست رفتن میدان دید در گلوکوم زاویه بسته
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor: [Glaucoma, Angle‐Closure] explode all trees
#2 (angle* near/3 closure*)
#3 (angle* near/3 close*)
#4 (Uncompensat* near/2 glaucoma*)
#5 (Narrow* near/2 angle*)
#6 (occlude* near/3 angle*)
#7 Acute glaucoma*
#8 (APAC or AACG or PACG or PACS)
#9 pupillary block glaucoma*
#10 {or #1‐#9}
#11 MeSH descriptor: [Laser Therapy] explode all trees
#12 MeSH descriptor: [Lasers] explode all trees
#13 Laser*
#14 (iridotom* or LPI)
#15 {or #11‐#14}
#16 #10 AND #15
Appendix 2. MEDLINE (Ovid) search strategy
1. exp Glaucoma, Angle‐Closure/
2. (angle* adj3 closure*).tw.
3. (angle* adj3 close*).tw.
4. (Uncompensat* adj2 glaucoma*).tw.
5. (Narrow* adj2 angle*).tw.
6. (occlude* adj3 angle*).tw.
7. Acute glaucoma*.tw.
8. (APAC or AACG or PACG or PACS).tw.
9. pupillary block glaucoma.tw.
10. or/1‐9
11. exp Laser Therapy/
12. exp Lasers/
13. Laser*.tw.
14. (iridotom* or LPI).tw.
15. or/11‐14
16. 10 and 15
Appendix 3. Embase.com search strategy
#1 'closed angle glaucoma'/exp
#2 (angle* NEAR/3 closure*):ab,ti
#3 (angle* NEAR/3 close*):ab,ti
#4 (uncompensat* NEAR/2 glaucoma*):ab,ti
#5 (narrow* NEAR/2 angle*):ab,ti
#6 (occlude* NEAR/3 angle*):ab,ti
#7 (acute NEAR/1 glaucoma*):ab,ti
#8 apac:ab,ti OR aacg:ab,ti OR pacg:ab,ti OR pacs:ab,ti
#9 ('pupillary block' NEAR/2 glaucoma):ab,ti
#10 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9
#11 'low level laser therapy'/exp
#12 'laser'/exp
#13 laser*:ab,ti
#14 'iridotomy'/exp
#15 iridotom*:ab,ti OR lpi:ab,ti
#16 #11 OR #12 OR #13 OR #14 OR #15
#17 #10 AND #16
Appendix 4. PubMed search strategy
1. (angle*[tw] AND closure*[tw]) NOT Medline[sb]
2. (angle*[tw] AND close*[tw]) NOT Medline[sb]
3. (Uncompensat*[tw] AND glaucoma*[tw]) NOT Medline[sb]
4. (Narrow*[tw] AND angle*[tw]) NOT Medline[sb]
5. (occlude*[tw] AND angle*[tw]) NOT Medline[sb]
6. Acute glaucoma*[tw] NOT Medline[sb]
7. (APAC[tw] or AACG[tw] or PACG[tw] or PACS[tw]) NOT Medline[sb]
8. pupillary block glaucoma[tw] NOT Medline[sb]
9. #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8
10. Laser*[tw] NOT Medline[sb]
11. (iridotom*[tw] OR LPI[tw]) NOT Medline[sb]
12. #10 OR #11
13. #9 AND #12
Appendix 5. LILACS search strategy
("Glaucoma de Ángulo Cerrado" OR "Glaucoma de Ângulo Fechado" OR MH:C11.525.381.056$ OR (angle$ AND (closure$ OR close$ OR narrow$ OR occlude$)) OR (Uncompensat$ glaucoma$) OR (Acute glaucoma$) OR (pupillary block glaucoma$) OR APAC OR AACG OR PACG OR PACS) AND (Laser$ OR iridotom$ or LPI OR MH:E02.594$ OR MH:E04.014.520$ OR MH:E07.632.490$ OR MH:E07.710.520$ OR MH:SP4.011.087.698.384.075.166.027$ OR MH:VS2.006.002.009$)
Appendix 6. ClinicalTrials.gov search strategy
Angle closure glaucoma OR Acute glaucoma OR pupillary block glaucoma
Appendix 7. WHO ICTRP search strategy
Angle closure glaucoma OR Acute glaucoma OR pupillary block glaucoma OR narrow‐angle glaucoma OR uncompensated glaucoma OR uncompensative glaucoma
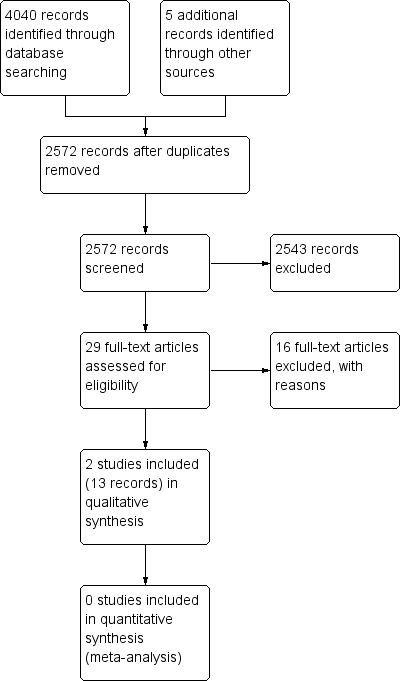
Study flow diagram.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
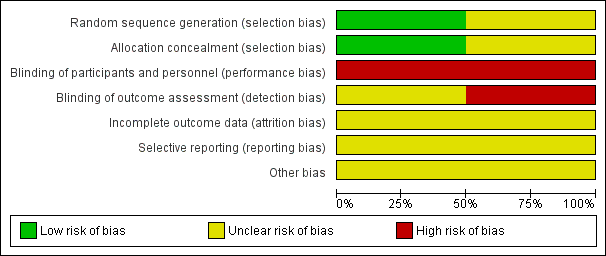
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Comparison 1 Iridotomy vs No treatment, Outcome 1 Angle Width.

Comparison 1 Iridotomy vs No treatment, Outcome 2 Adverse events.
| Iridotomy compared to no iridotomy for patients with primary angle‐closure suspect, primary angle closure, or primary angle‐closure glaucoma | ||||||
| Patient or population: patients with primary angle‐closure suspect, primary angle closure, or primary angle‐closure glaucoma | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of eyes | Certainty of the evidence | Comments | |
| Risk with no iridotomy | Risk with Iridotomy | |||||
| Proportion of progressive visual field loss at 1 year | Not reported | Not reported | ‐ | ‐ | ‐ | |
| Intraocular pressure: mean IOP at 1 year | Not reported | Not reported | ‐ | ‐ | ‐ | |
| Gonioscopic findings: mean angle width at 1 year | The mean angle width was 11.3° in the no iridotomy group | The mean angle width in the iridotomy group was 12.7° higher | MD 12.7 | 1550 | ⊕⊕⊕⊝ | Participants in the study were primary angle‐closure suspects. Data were only available at 18 months. |
| Need for additional surgery: proportion of participants who received additional surgery to control IOP at 1 year | Not reported | Not reported | ‐ | ‐ | ‐ | |
| Medications: mean number of medications used to control IOP at 1 year | Not reported | Not reported | ‐ | ‐ | ‐ | |
| Quality of life measures | Not reported | Not reported | ‐ | ‐ | ‐ | |
| Adverse events ‒ IOP spike (rise greater than or equal to 8 mmHg) at 1 hour | 4 per 1000 | 98 per 1000 | RR 24.00 | 1468 | ⊕⊕⊝⊝ | Participants in the study were primary angle‐closure suspects. |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded by one level for risk of bias, as the study is at unclear risk of bias for incomplete outcome data, selective outcome reporting, and other sources of bias due to the lack of availability of a full trial report. 2 Downgraded by one level for imprecision, as the confidence interval of the risk ratio between the groups is wide. | ||||||
| Primary angle‐closure suspect (PACS) | Primary angle closure (PAC) | Primary angle‐closure glaucoma (PACG) | |
| Iridotrabecular contact greater than or equal to 180° | X | X | X |
| Elevated intraocular pressure OR peripheral anterior synechiae | X | X | |
| Optic nerve damage | X |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Angle Width Show forest plot | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Adverse events Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 IOP spike (rise greater than or equal to 8 mmHg) at 1 hour | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |

