Joga stosowana łącznie z innymi metodami leczenia w porównaniu z leczeniem standardowym u chorych na schizofrenię
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (according to the ICD‐10 criteria). Exclusion criteria: learning disability, physical disabilities, critical medical conditions, late onset schizophrenia and whose primary diagnosis was directly linked to substance abuse. | |
| Interventions | 1.Yoga package: drama, music, dance and yoga therapies were incorporated into a 'comprehensive program', for 6 hours per day, conducted over a period of 3 weeks, and conducted on 8 days over this period, conducted by instructors from the 'Abhina Academy of Performing Arts, Sri Lanka'. Specific interventions employed were 'breathing control training, identification and correct interpretation of basic emotions, observation of others behaviour and mimicking, attention enhancing procedures, maintaining correct body posture' (N=33). 2. Standard care: received standard care including medication and occupational therapy activities (N=40). Participants in both groups continued on pharmacotherapy. | |
| Outcomes | Leaving the study early. Unable to use Mental state: PANSS ‐ only median (IQR) reported for this data as non‐normally distributed Self‐esteem: RSES ‐ no data reported Satisfaction: 'pre‐tested' questionnaire ‐ no data reported | |
| Notes | *20 of the participants were admitted for treatment under court orders to the forensic psychiatry unit of the hospital, **age range not stated, ***exact number not specified For declaration of interest: 'none' indicated by authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: Patients were "randomly allocation" Response: Sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | Concealment strategy was not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | No details specified. |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Investigators assessing the outcome measures were blind to the treatment modality employed" Response: Low risk |
| Incomplete outcome data (attrition bias) | Low risk | No withdrawals reported in this study, appears to be low risk. |
| Selective reporting (reporting bias) | High risk | No data provided for RSES or satisfaction measures. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (according to the ICD‐10 criteria). Exclusion criteria: Major physical problems, organic mental disorder, co‐morbid psychiatric disorder, history suggestive of MR, epilepsy, head injury, concurrent active medical disorder and active psychopathology that interfere with following and understanding instructions, history of substance abuse. | |
| Interventions | 1.Yoga: 1‐month yoga training with ''motivational and feedback session'' for about 1.5 hours delivered by a trained yoga instructor from the Ranchi Institute. The techniques consisted of the following yoga postures (asanas): (i) standing postures, (ii) lying postures (supine and prone), (iii) sitting postures, (iv) pranayama‐breathing exercises. (N=15). 2. Standard‐care: participants did not receive any add‐on intervention. (N=15). Participants in both groups continued on pharmacotherapy (participants were on risperidone, and olanzapine with doses regulated according to requirements). | |
| Outcomes | Leaving the study early. Unable to use Mental state: PANSS ‐ mean (SD) for individual variable scores only included General well‐being: PGI general well‐being measure (Hindi version) ‐ mean (SD) for individual variable scores only included Activities of daily living: checklist for basic living skills ‐ mean (SD) for individual variable scores only included Disability: Indian disability evaluation and assessment scale: IDEAS ‐ mean (SD) for individual variable scores only included | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomly assigned" Response: Unclear risk as method of sequence generation was not specified. |
| Allocation concealment (selection bias) | Unclear risk | Concealment strategy was not described. |
| Blinding of participants and personnel (performance bias) | Unclear risk | No details provided. |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details provided. |
| Incomplete outcome data (attrition bias) | Unclear risk | Although number of participants who dropped out were low (n=1 per group) and balanced between groups, participants who dropped out were not included in the final analysis. |
| Selective reporting (reporting bias) | High risk | PGI general well‐being measure is a 20‐item scale, but results for only 7 items were reported. |
| Methods | Allocation: randomised. | |
| Participants | Diagnosis: schizophrenia (according to the CCMD‐3 criteria). Exclusion criteria: ''serious body disease'', incorporative patients. ''Normal treatment'' will be given to both groups | |
| Interventions | 1.Yoga: 8 weeks yoga training with ''related relaxation exercises'', ''and patients will communicate each other to share their experiences'' with counselling and question and answers session for about 1 hour delivered by two senior nurses with training in ''basic yoga theory''. The yoga consisted of the following elements: (i) ''attention concentrating'', (ii) ''breathe adjusting'', (iii) simple meditation. Yoga progressed in terms of dosage and complexity once ''basic rules'' were mastered (N=46). 2. Standard‐care control: participants did not receive any add‐on intervention (N=42). Participants in both groups continued on pharmacotherapy. | |
| Outcomes | Quality of life: GQOLI‐74. | |
| Notes | *age range not supplied, **gender of 10 people who left early not detailed, Study took place July‐Nov 2005. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: ''following the tossing coin method we randomly divided..'' Response: likely to be adequate |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding of participants and personnel (performance bias) | Unclear risk | No details provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details provided |
| Incomplete outcome data (attrition bias) | High risk | Quote: ''there are 10 cases being dropped (8 cases from yoga group and 2 cases from normal control'' Response: High risk of bias as unbalanced drop‐outs which were not included in analysis. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes appeared to be reported. |
| Other bias | Unclear risk | Original paper in Chinese, relied on a translation. |
CCMD‐3: Chinese Classification of Mental Disorders
GQOLI‐74: General Quality of Life Inventory‐74
ICD‐10: International Classification of Mental and Behavioural Disorders
IDEAS: Indian Disability Evaluation and Assessment Scale
IQR: interquartile range
MR: mental retardation
PANSS: Positive and Negative Syndrome Scale
PGI: Post Graduate Institute
RSES: Rosenberg Self Esteem Score
SD: Standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Allocation: randomised. Participants: people with schizophrenia. Intervention: yoga as a stand alone entity, not as part of a package of care versus exercise and treatment as usual. | |
| Allocation: not randomised. | |
| Allocation: randomised. Participants: people with schizophrenia. Intervention: yoga as a stand alone entity, not as part of a package of care versus exercise and treatment as usual. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga as a stand alone entity, not as part of a package of care versus exercise. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga as a stand alone entity, not as part of a package of care versus exercise. | |
| Allocation: randomised. Participants: people with schizophrenia. Intervention: yoga plus regular day care programme versus standard care consisting of regular day care programme not yoga as part of a package of care versus standard care. | |
| Allocation: randomised. Participants: people with schizophrenia. Intervention: yoga plus regular day care programme versus standard care consisting of regular day care programme not yoga as part of a package of care versus standard care. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga as a stand alone entity, not as part of a package of care versus ''A simple exercise''. | |
| Allocation: 'quasi' randomised not randomised as stated in protocol. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga as a stand alone entity, not as part of a package of care versus standard care. | |
| Allocation: randomised. Participants: people with schizophrenia. Interventions: yoga as a stand alone entity, not as part of a package of care versus standard care. | |
| Allocation: ''double blind''. Participants: people with schizophrenia. Interventions: "Tagara" (local drug with antipsychotic properties) and "Brahmyadiyoga" (an herbal compound) versus chlorpromazine versus placebo, not yoga as part of a package of care. | |
| Allocation: randomised. Participants: people with schizophrenia or related disorders. Interventions: yoga as a stand alone entity, not as part of a package of care versus exercise therapy. | |
| Allocation: ''double blind''. Participants: people with schizophrenia. Interventions: "Tagara" (local drug with antipsychotic properties) and "Brahmyadiyoga" (an herbal compound) versus chlorpromazine versus placebo, not yoga as part of a package of care. | |
| Allocation: treatments randomised. Participants: people with schizophrenia. Intervention: yoga and aerobic exercise performed, but results present effect of a single session of yoga or aerobic exercise separately, rather than effect of cumulative package. | |
| Allocation: randomised. Participants: people with schizophrenia. Intervention: yoga as a stand alone entity, not as part of a package of care versus standard care control. | |
| Allocation: randomised. Participants: caregivers of people with schizophrenia, not people with schizophrenia. | |
| Allocation: randomised. Participants: people with schizophrenia. Intervention: yoga as a stand alone entity, not as part of a package of care versus standard care control. | |
| Allocation: participants randomly selected but not randomly allocated to intervention/control group. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Effects study of yoga therapy on the association of mental illness with metabolic disorders |
| Methods | Allocation: randomised. Blinding: no details given. Duration: no details given. Design: parallel. Setting: Toyko Metropolitan Matsuzawa Hospital. |
| Participants | Diagnosis: schizophrenia (DSM IV). Exclusion criteria: patients with diabetes, renal failure, pervasive development disorders, mental retardation. |
| Interventions | 1. Yoga therapy: (no further details given). 2. 'A simple exercise': (no further details given). |
| Outcomes | Oxidative‐stress markers (no further outcomes listed). |
| Starting date | 05 December 2014. |
| Contact information | Masanari Itokawa (itokawa‐[email protected]), Hiromi Idozawa (Chiken‐[email protected]) |
| Notes | Contacted for study information 16.02.16, no reply. |
DSM IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size | ||||||||||||||||||||||||||||||||||||
| 1 Mental state: 1. Average score (PANSS, low = good) Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| Analysis 1.1
Comparison 1 Yoga package versus standard care, Outcome 1 Mental state: 1. Average score (PANSS, low = good). | ||||||||||||||||||||||||||||||||||||||||
| 2 Global state: General well‐being: not improved (PGI general well‐being measure, low = good) Show forest plot | Other data | No numeric data | ||||||||||||||||||||||||||||||||||||||
| Analysis 1.2
Comparison 1 Yoga package versus standard care, Outcome 2 Global state: General well‐being: not improved (PGI general well‐being measure, low = good). | ||||||||||||||||||||||||||||||||||||||||
| 3 Quality of life: Average end‐point score (GQOLI‐74, high = good) short term Show forest plot | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 22.93 [19.74, 26.12] | ||||||||||||||||||||||||||||||||||||
| Analysis 1.3  Comparison 1 Yoga package versus standard care, Outcome 3 Quality of life: Average end‐point score (GQOLI‐74, high = good) short term. | ||||||||||||||||||||||||||||||||||||||||
| 4 Leaving the study early: any reason (low = good) short term Show forest plot | 3 | 193 | Risk Difference (M‐H, Fixed, 95% CI) | 0.06 [‐0.01, 0.13] | ||||||||||||||||||||||||||||||||||||
| Analysis 1.4 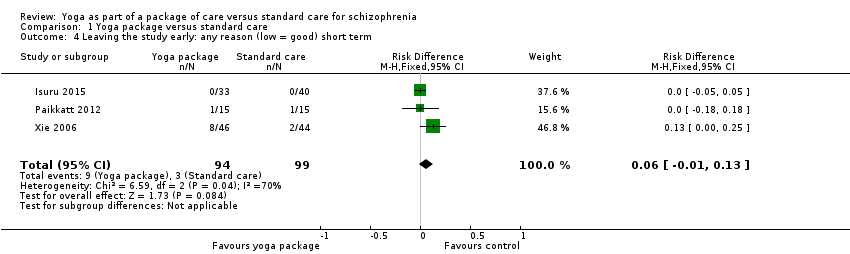 Comparison 1 Yoga package versus standard care, Outcome 4 Leaving the study early: any reason (low = good) short term. | ||||||||||||||||||||||||||||||||||||||||
| 5 Activities of daily living (Checklist for basic living skills, low=good) Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only | |||||||||||||||||||||||||||||||||||||
| Analysis 1.5 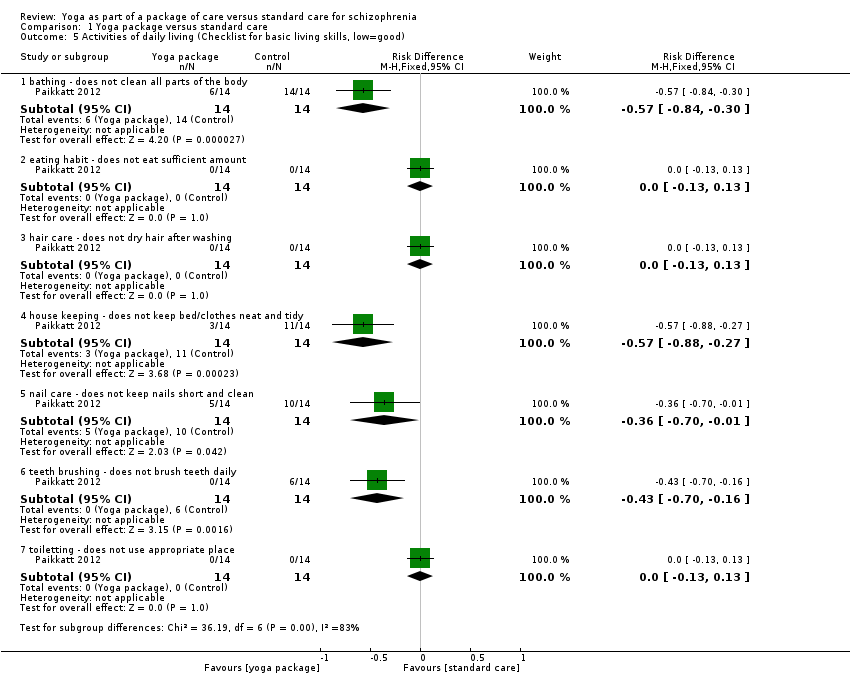 Comparison 1 Yoga package versus standard care, Outcome 5 Activities of daily living (Checklist for basic living skills, low=good). | ||||||||||||||||||||||||||||||||||||||||
| 5.1 bathing ‐ does not clean all parts of the body | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.57 [‐0.84, ‐0.30] | ||||||||||||||||||||||||||||||||||||
| 5.2 eating habit ‐ does not eat sufficient amount | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] | ||||||||||||||||||||||||||||||||||||
| 5.3 hair care ‐ does not dry hair after washing | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] | ||||||||||||||||||||||||||||||||||||
| 5.4 house keeping ‐ does not keep bed/clothes neat and tidy | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.57 [‐0.88, ‐0.27] | ||||||||||||||||||||||||||||||||||||
| 5.5 nail care ‐ does not keep nails short and clean | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.36 [‐0.70, ‐0.01] | ||||||||||||||||||||||||||||||||||||
| 5.6 teeth brushing ‐ does not brush teeth daily | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.43 [‐0.70, ‐0.16] | ||||||||||||||||||||||||||||||||||||
| 5.7 toiletting ‐ does not use appropriate place | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] | ||||||||||||||||||||||||||||||||||||

Study flow diagram.
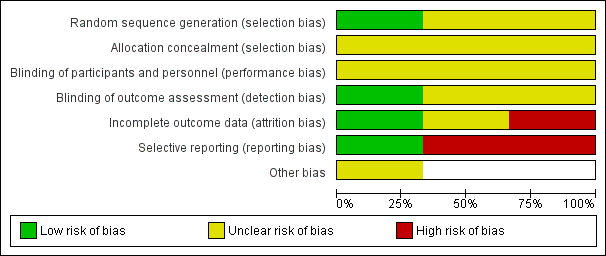
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
| Study | Variable | Yoga package, median (interquartile range) (n = 33) | Control (median, interquartile range) (n = 40) |
| Isuru 2015 | PANSS positive | 15.0 (10.0 to 17.5) | 16.0 (14.0 to 18.0) |
| Isuru 2015 | PANSS negative | 17.0 (11.0 to 22.5) | 18.0 (15.0 to 22.0) |
| Isuru 2015 | PANSS total | 61.0 (49.5 to 72.0) | 63.5 (54.5 to 72.8) |
Comparison 1 Yoga package versus standard care, Outcome 1 Mental state: 1. Average score (PANSS, low = good).
| Study | Sub‐sections | Yoga Package (n = 14) | Control (n = 14) |
| Paikkatt 2012 | Not feeling happiness | 0 | 9 |
| Paikkatt 2012 | Not feeling satisfied | 4 | 4 |
| Paikkatt 2012 | Inadequate sleep | 2 | 2 |
| Paikkatt 2012 | Feeling good | 1 | 7 |
| Paikkatt 2012 | Not in control of anger | 1 | 3 |
| Paikkatt 2012 | Not feeling worthy | 1 | 7 |
| Paikkatt 2012 | Not feeling healthy | 0 | 4 |
Comparison 1 Yoga package versus standard care, Outcome 2 Global state: General well‐being: not improved (PGI general well‐being measure, low = good).

Comparison 1 Yoga package versus standard care, Outcome 3 Quality of life: Average end‐point score (GQOLI‐74, high = good) short term.
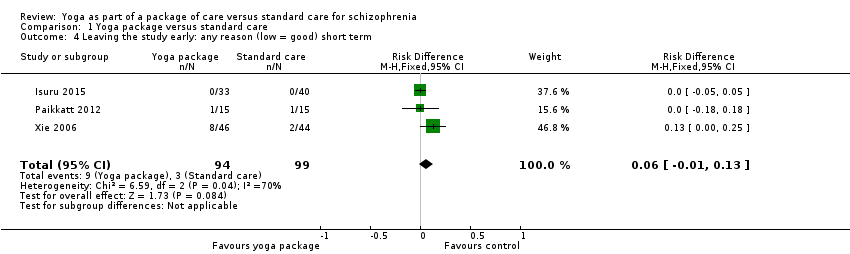
Comparison 1 Yoga package versus standard care, Outcome 4 Leaving the study early: any reason (low = good) short term.
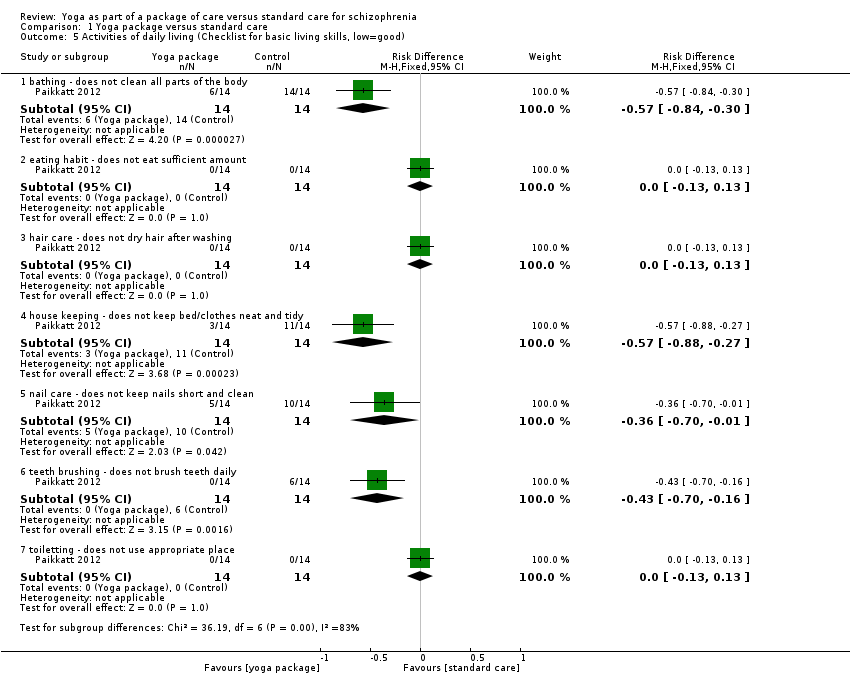
Comparison 1 Yoga package versus standard care, Outcome 5 Activities of daily living (Checklist for basic living skills, low=good).
| Methods | Allocation: randomised (clearly described). |
| Participants | Diagnosis: people with a clinical diagnosis of schizophrenia using DSM‐IV criteria. |
| Interventions | 1. Yoga: the yoga intervention should be clearly described and consist of the following components: (i) shithileekarana vyayama (loosening exercises) for approximately 10 minutes, (ii) yoga postures (asanas) for approximately 20 minutes, (iii) breathing exercises and relaxation techniques for approximately 20 minutes using a manualised protocol, yoga programme for 12 weeks, 3 times weekly, follow‐up at 6 months and 1 year, yoga delivered by a trained yoga instructor, meditation not included. 2. Standard‐care control. All groups stable pharmacotherapy. |
| Outcomes | Mental state (binary outcomes). Relapses (binary outcomes). Quality of life (binary outcomes). Disability (binary outcomes). Activities of daily living (binary outcomes). Costs: cost of services, cost of care. Adverse events related to yoga (number and type of injuries). Service outcomes: days in hospital, time attending outpatient psychiatric clinic. |
| Notes | Adherence should be logged with participants expected to adhere to 70% to 75% of scheduled sessions. |
| DSM‐IV:Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition | |
| Yoga package versus standard care for schizophrenia | ||||||
| Patient or population: patients with schizophrenia | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Yoga package versus standard care | |||||
| Mental State: clinically important change | No useable mental state data reported. | |||||
| Social functioning: clinically important change | No study reported on social functioning. | |||||
| Adverse events: clinically important adverse effect | No study reported on adverse effects. | |||||
| Quality of life: clinically important change* Follow‐up: mean 4 weeks | The mean quality of life (GQOLI‐74) in the intervention groups was | 80 | ⊕⊕⊝⊝ | * Clinically important data not available: nearest outcome reported were Average endpoint scores on the GQOLI‐74 | ||
| Leaving the study early: any reason Leaving the study early: participants lost to follow‐up ‐ short term (low=good) | Low1 | 0.06 [‐ 0.01 to 0.13] | 193 (3 studies) | ⊕⊕⊕⊝ | ||
| 800 per 1000 | 1000 per 1000 (640 to 1000) | |||||
| Moderate1 | ||||||
| 900 per 1000 | 1000 per 1000 (720 to 1000) | |||||
| High1 | ||||||
| 1000 per 1000 | 1000 per 1000 (800 to 1000) | |||||
| Costs of care: direct and indirect | No study reported direct or indirect costs of care. | |||||
| Physical health: clinically important change | No study reported on physical health. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Imprecision: Downgraded one level as a number of participants withdrew from two trials, not accounted for in final analysis. 3Imprecision: Downgraded one level due to relatively small number of participants included. | ||||||
| Review number | Review Title | Status |
| 1 | Yoga versus standard care for schizophrenia | |
| 2 | Yoga versus non‐standard care for schizophrenia | |
| 3 | Yoga as part of a package of care versus standard care | Current review |
| 4 | Yoga as part of a package of care versus non‐standard care |
| Intervention | Plus | Control | Participants | Reference tag | Proposed relevant Cochrane review |
| Yoga | Nil | Exercise | People with schizophrenia | Bhatia 2017; Duraiswamy 2007; Lin 2015; Manjunath 2013; Varambally 2012; JPRN‐UMIN000013746 | Yoga versus non‐standard care for schizophrenia |
| Counselling | Standard care | ||||
| Motivational and feedback session | |||||
| Nil | Caregivers of people with schizophrenia | ‐ | |||
| Yoga | Non‐standard care | People with schizophrenia | Yoga as part of a package of care versus non‐standard care | ||
| Chlorpromazine | Nil | Placebo | Chlorpromazine versus placebo for schizophrenia | ||
| 'Tagara' (local drug with antipsychotic properties) and 'Brahmyadiyoga' (an herbal compound) | Nil | Chlorpromazine | Chlorpromazine versus herbal compounds for schizophrenia |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mental state: 1. Average score (PANSS, low = good) Show forest plot | Other data | No numeric data | ||
| 2 Global state: General well‐being: not improved (PGI general well‐being measure, low = good) Show forest plot | Other data | No numeric data | ||
| 3 Quality of life: Average end‐point score (GQOLI‐74, high = good) short term Show forest plot | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 22.93 [19.74, 26.12] |
| 4 Leaving the study early: any reason (low = good) short term Show forest plot | 3 | 193 | Risk Difference (M‐H, Fixed, 95% CI) | 0.06 [‐0.01, 0.13] |
| 5 Activities of daily living (Checklist for basic living skills, low=good) Show forest plot | 1 | Risk Difference (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 bathing ‐ does not clean all parts of the body | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.57 [‐0.84, ‐0.30] |
| 5.2 eating habit ‐ does not eat sufficient amount | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] |
| 5.3 hair care ‐ does not dry hair after washing | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] |
| 5.4 house keeping ‐ does not keep bed/clothes neat and tidy | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.57 [‐0.88, ‐0.27] |
| 5.5 nail care ‐ does not keep nails short and clean | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.36 [‐0.70, ‐0.01] |
| 5.6 teeth brushing ‐ does not brush teeth daily | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.43 [‐0.70, ‐0.16] |
| 5.7 toiletting ‐ does not use appropriate place | 1 | 28 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.13, 0.13] |

