Cirugía reconstructiva para el tratamiento de las úlceras por presión
Appendices
Appendix 1. Search strategies
Cochrane Wounds Specialised Register
1 MESH DESCRIPTOR surgical flaps EXPLODE ALL AND INREGISTER
2 MESH DESCRIPTOR Reconstructive Surgical Procedures EXPLODE ALL AND INREGISTER
3 MESH DESCRIPTOR Wound Closure Techniques EXPLODE ALL AND INREGISTER
4 MESH DESCRIPTOR skin transplantation EXPLODE ALL AND INREGISTER
5 (surger* or surgical*) AND INREGISTER
6 (primary near3 closure*) AND INREGISTER
7 (skin near3 (graft* or transplant*)) AND INREGISTER
8 ((surg* or reconstruct* or random or region* or muscle or musculocutaneous or fascial* or fasciocutaneous* or perforat* or free) near2 flap*) AND INREGISTER
9 "tissue expansion" AND INREGISTER
10 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9
11 MESH DESCRIPTOR Pressure Ulcer EXPLODE ALL AND INREGISTER
12 (pressure NEXT (ulcer* or sore* or injur*)) AND INREGISTER
13 (decubitus NEXT (ulcer* or sore*)) AND INREGISTER
14 ((bedsore* or bed sore*)) AND INREGISTER
15 #11 OR #12 OR #13 OR #14
16 #10 AND #15
The Cochrane Central Register of Controlled Clinical Trials (CENTRAL)
#1 MeSH descriptor: [Surgical Flaps] explode all trees
#2 MeSH descriptor: [Reconstructive Surgical Procedures] explode all trees
#3 MeSH descriptor: [Wound Closure Techniques] explode all trees
#4 MeSH descriptor: [Skin Transplantation] explode all trees
#5 (surger* or surgical*):ti
#6 (primary near/3 closure*):ti,ab,kw
#7 (skin near/3 (graft* or transplant*)):ti,ab,kw
#8 ((surg* or reconstruct* or random or region* or muscle or musculocutaneous or fascial* or fasciocutaneous* or perforat* or free) near/3 flap*):ti,ab,kw
#9 "tissue expansion":ti,ab,kw
#10 {or #1‐#9}
#11 MeSH descriptor: [Pressure Ulcer] explode all trees
#12 (pressure next (ulcer* or sore* or injur*)):ti,ab,kw
#13 (decubitus next (ulcer* or sore*)):ti,ab,kw
#14 ((bed next sore*) or bedsore*):ti,ab,kw
#15 {or #11‐#14}
#16 (#10 and #15)
Cochrane Central Register of Controlled Trials (CENTRAL) searched via the Cochrane Wounds Specialised Register (Trial Registry specific search)
1 MESH DESCRIPTOR surgical flaps EXPLODE ALL AND CENTRAL:TARGET
2 MESH DESCRIPTOR Reconstructive Surgical Procedures EXPLODE ALL AND CENTRAL:TARGET
3 MESH DESCRIPTOR Wound Closure Techniques EXPLODE ALL AND CENTRAL:TARGET
4 MESH DESCRIPTOR skin transplantation EXPLODE ALL AND CENTRAL:TARGET
5 (surger* or surgical*) AND CENTRAL:TARGET
6 (primary near3 closure*) AND CENTRAL:TARGET
7 (skin near3 (graft* or transplant*)) AND CENTRAL:TARGET 1
8 ((surg* or reconstruct* or random or region* or muscle or musculocutaneous or fascial* or fasciocutaneous* or perforat* or free) near2 flap*) AND CENTRAL:TARGET
9 "tissue expansion" AND CENTRAL:TARGET
10 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 AND CENTRAL:TARGET
11 MESH DESCRIPTOR Pressure Ulcer EXPLODE ALL AND CENTRAL:TARGET
12 (pressure NEXT (ulcer* or sore* or injur*)) AND CENTRAL:TARGET
13 (decubitus NEXT (ulcer* or sore*)) AND CENTRAL:TARGET
14 ((bedsore* or bed sore*)) AND CENTRAL:TARGET
15 #11 OR #12 OR #13 OR #14 AND CENTRAL:TARGET
16 #10 AND #15 AND CENTRAL:TARGET
17 (NCT0* or ACTRN* or ChiCTR* or DRKS* or EUCTR* or eudract* or IRCT* or ISRCTN* or JapicCTI* or JPRN* or NTR0* or NTR1* or NTR2* or NTR3* or NTR4* or NTR5* or NTR6* or NTR7* or NTR8* or NTR9* or SRCTN* or UMIN0*):AU AND CENTRAL:TARGET
18 http*:SO AND CENTRAL:TARGET
19 #17 OR #18
20 #16 AND #19
Ovid MEDLINE
1 exp Surgical Flaps/
2 exp Reconstructive Surgical Procedures/
3 exp Wound Closure Techniques/
4 exp Skin Transplantation/
5 (surger* or surgical*).ti.
6 (primary adj3 closure*).ti,ab.
7 (skin adj3 (graft* or transplant*)).ti,ab.
8 ((surg* or reconstruct* or random or region* or muscle or musculocutaneous or fascial* or fasciocutaneous* or perforat* or free) adj2 flap*).ti,ab.
9 tissue expansion.ti,ab.
10 or/1‐9
11 exp Pressure Ulcer/
12 (pressure adj (ulcer* or sore* or injur*)).ti,ab.
13 (decubitus adj (ulcer* or sore*)).ti,ab.
14 (bedsore* or bed sore*).ti,ab.
15 or/11‐14
16 10 and 15
17 randomized controlled trial.pt.
18 controlled clinical trial.pt.
19 randomized.ab.
20 placebo.ab.
21 drug therapy.fs.
22 randomly.ab.
23 trial.ab.
24 groups.ab.
25 or/17‐24
26 exp animals/ not humans.sh.
27 25 not 26
28 16 and 27
Ovid Embase
1 exp skin graft/
2 exp tissue flap/
3 exp tissue expansion/
4 exp reconstructive surgery/
5 exp wound closure/
6 (surger* or surgical*).ti.
7 (primary adj3 closure*).ti,ab.
8 (skin adj3 (graft* or transplant*)).ti,ab.
9 ((surg* or reconstruct* or random or region* or muscle or musculocutaneous or fascial* or fasciocutaneous* or perforat* or free) adj2 flap*).ti,ab.
10 tissue expansion.ti,ab.
11 or/1‐10
12 exp decubitus/
13 (pressure adj (ulcer* or sore* or injur*)).ti,ab.
14 (decubitus adj (ulcer* or sore*)).ti,ab.
15 (bedsore* or bed sore*).ti,ab.
16 or/12‐15
17 11 and 16
18 Randomized controlled trial/
19 Controlled clinical study/
20 Random$.ti,ab.
21 randomization/
22 intermethod comparison/
23 placebo.ti,ab.
24 (compare or compared or comparison).ti.
25 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab.
26 (open adj label).ti,ab.
27 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab.
28 double blind procedure/
29 parallel group$1.ti,ab.
30 (crossover or cross over).ti,ab.
31 ((assign$ or match or matched or allocation) adj5 (alternate or group$1 orintervention$1 or patient$1 or subject$1 or participant$1)).ti,ab.
32 (assigned or allocated).ti,ab.
33 (controlled adj7 (study or design or trial)).ti,ab.
34 (volunteer or volunteers).ti,ab.
35 human experiment/
36 trial.ti.
37 or/18‐36
38 (random$ adj sampl$ adj7 (cross section$ or questionnaire$1 or survey$ or database$1)).ti,ab. not (comparative study/ or controlled study/ or randomi?ed controlled.ti,ab. or randomly assigned.ti,ab.)
39 Cross‐sectional study/ not (randomized controlled trial/ or controlled clinical study/ or controlled study/ or randomi?ed controlled.ti,ab. or control group$1.ti,ab.)
40 (((case adj control$) and random$) not randomi?ed controlled).ti,ab.
41 (Systematic review not (trial or study)).ti.
42 (nonrandom$ not random$).ti,ab.
43 Random field$.ti,ab.
44 (random cluster adj3 sampl$).ti,ab.
45 (review.ab. and review.pt.) not trial.ti.
46 we searched.ab. and (review.ti. or review.pt.)
47 update review.ab.
48 (databases adj4 searched).ab.
49 (rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys or trout or marmoset$1).ti. and animal experiment/
50 Animal experiment/ not (human experiment/ or human/)
51 or/38‐50
52 37 not 51
53 17 and 52
EBSCO CINAHL Plus
S40 S16 AND S39
S39 S38 NOT S37
S38 S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31
S37 S35 NOT S36
S36 MH (human)
S35 S32 OR S33 OR S34
S34 TI (animal model*)
S33 MH (animal studies)
S32 MH animals+
S31 AB (cluster W3 RCT)
S30 MH (crossover design) OR MH (comparative studies)
S29 AB (control W5 group)
S28 PT (randomized controlled trial)
S27 MH (placebos)
S26 MH (sample size) AND AB (assigned OR allocated OR control)
S25 TI (trial)
S24 AB (random*)
S23 TI (randomised OR randomized)
S22 MH cluster sample
S21 MH pretest‐posttest design
S20 MH random assignment
S19 MH single‐blind studies
S18 MH double‐blind studies
S17 MH randomized controlled trials
S16 S10 AND S15
S15 S11 OR S12 OR S13 OR S14
S14 TI decubitus ulcer OR AB decubitus ulcer
S13 TI ( bed sore* or bedsore* ) or AB ( bed sore* or bedsore* )
S12 TI ( pressure ulcer* or pressure sore* or pressure injur* ) or AB ( pressure ulcer* or pressure sore* or pressure injur*)
S11 (MH "Pressure Ulcer+")
S10 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9
S9 TI tissue expansion OR AB tissue expansion
S8 TI ((surg* or reconstruct* or random or region* or muscle or musculocutaneous or fascial* or fasciocutaneous* or perforat* or free) N2 flap*) OR AB ((surg* or random or region* or muscle or musculocutaneous or fascial* or fasciocutaneous* or perforat* or free) N2 flap*)
S7 TI (skin N3 (graft* or transplant*)) or AB (skin N3 (graft* or transplant*))
S6 TI ((primary or wound*) N3 closure*)) OR AB ((primary or wound*)N3 closure*))
S5 TI surger* or surgical*
S4 (MH "Skin Transplantation")
S3 (MH "Surgery, Reconstructive+")
S2 (MH "Tissue Expansion")
S1 (MH "Surgical Flaps+")
US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov)
Surgery OR reconstruction OR flap OR graft OR transplant | Pressure Ulcer
Surgery OR reconstruction OR flap OR graft OR transplant | Pressure Injury
Surgery OR reconstruction OR flap OR graft OR transplant | Pressure Ulcers Stage III
Surgery OR reconstruction OR flap OR graft OR transplant | Pressure Ulcer, Stage IV
World Health Organization International Clinical Trials Registry Platform (ICTRP)
(surgery OR reconstruction OR flap OR graft OR transplant) [Intervention]
AND pressure ulcer [Title]
(surgery OR reconstruction OR flap OR graft OR transplant) [Intervention]
AND pressure ulcer [Condition]
(surgery OR reconstruction OR flap OR graft OR transplant)[Intervention]
AND Pressure sore [Title]
(surgery OR reconstruction OR flap OR graft OR transplant)[Intervention]
AND Pressure sore [Condition]
(surgery OR reconstruction OR flap OR graft OR transplant)[Intervention]
AND decubitus [Title]
(surgery OR reconstruction OR flap OR graft OR transplant) [Intervention]
AND decubitus [Condition]
Appendix 2. Risk of bias assessment (individually randomised controlled trials)
1. Was the allocation sequence randomly generated?
Low risk of bias: the investigators describe a random component in the sequence generation process such as: referring to a random number table; using a computer random number generator; coin tossing; shuffling cards or envelopes; throwing dice; drawing of lots.
High risk of bias: the investigators describe a non‐random component in the sequence generation process. Usually, the description would involve some systematic, non‐random approach, for example: sequence generated by odd or even date of birth; sequence generated by some rule based on date (or day) of admission; sequence generated by some rule based on hospital or clinic record number.
Unclear: insufficient information about the sequence generation process to permit judgement of low or high risk of bias.
2. Was the treatment allocation adequately concealed?
Low risk of bias: participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, web‐based and pharmacy‐controlled randomisation); sequentially numbered drug containers of identical appearance; sequentially numbered, opaque, sealed envelopes.
High risk of bias: participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on: use of an open random allocation schedule (e.g. a list of random numbers); assignment envelopes without appropriate safeguards (e.g. envelopes were unsealed, non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure.
Unclear: insufficient information to permit judgement of low or high risk of bias. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgement, for example if the use of assignment envelopes is described, but it remains unclear whether envelopes were sequentially numbered, opaque and sealed.
3. Blinding – was knowledge of the allocated interventions adequately prevented during the study?
Low risk of bias: any one of the following.
-
No blinding, but the review authors judge that the outcome and the outcome measurement are unlikely to be influenced by lack of blinding.
-
Blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken.
-
Either participants or some key study personnel were not blinded, but outcome assessment was blinded and the non‐blinding of others unlikely to introduce bias.
High risk of bias: any one of the following:
-
No blinding or incomplete blinding, and the outcome or outcome measurement is likely to be influenced by lack of blinding.
-
Blinding of key study participants and personnel attempted, but likely that the blinding could have been broken.
-
Either participants or some key study personnel were not blinded, and the non‐blinding of others likely to introduce bias.
Unclear: any one of the following:
-
Insufficient information to permit judgement of low or high risk of bias.
-
The study did not address this outcome.
4. Were incomplete outcome data adequately addressed?
Low risk of bias: any one of the following.
-
No missing outcome data.
-
Reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to introduce bias).
-
Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups.
-
For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk not enough to have a clinically relevant impact on the intervention effect estimate.
-
For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size.
-
Missing data have been imputed using appropriate methods.
High risk of bias: any one of the following.
-
Reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups.
-
For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk enough to induce clinically relevant bias in intervention effect estimate.
-
For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes enough to induce clinically relevant bias in observed effect size.
-
'As‐treated' analysis done with substantial departure of the intervention received from that assigned at randomisation.
-
Potentially inappropriate application of simple imputation.
Unclear: any one of the following.
-
Insufficient reporting of attrition/exclusions to permit judgement of low or high risk of bias (e.g. number randomised not stated, no reasons for missing data provided).
-
The study did not address this outcome.
5. Are reports of the study free of suggestion of selective outcome reporting?
Low risk of bias: any of the following.
-
The study protocol is available and all of the study's prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way.
-
The study protocol is unavailable but it is clear that the published reports include all expected outcomes, including those that were prespecified (convincing text of this nature may be uncommon).
High risk of bias: any one of the following:
-
Not all of the study's prespecified primary outcomes have been reported.
-
One or more primary outcomes are reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not prespecified.
-
One or more reported primary outcomes were not prespecified (unless clear justification for their reporting is provided, such as an unexpected adverse effect).
-
One or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis.
-
The study report fails to include results for a key outcome that would be expected to have been reported for such a study.
Unclear: insufficient information to permit judgement of low or high risk of bias. It is likely that the majority of studies will fall into this category.
6. Other sources of potential bias
Low risk of bias: the study appears to be free of other sources of bias.
High risk of bias: there is at least one important risk of bias. For example, the study:
-
had a potential source of bias related to the specific study design used;
-
has been claimed to have been fraudulent; or
-
had some other problem.
Unclear: there may be a risk of bias, but there is either:
-
insufficient information to assess whether an important risk of bias exists; or
-
insufficient rationale or evidence that an identified problem will introduce bias.
Appendix 3. Risk of bias assessment (cluster‐randomised controlled trials)
In cluster‐randomised trials, particular biases to consider include the following.
-
Recruitment bias. This can occur when individuals are recruited to the trial after the clusters have been randomised, as the knowledge of whether each cluster is an 'intervention' or 'control' cluster could affect the types of participants recruited.
-
Baseline imbalance. Cluster‐randomised trials often randomise all clusters at once, so lack of concealment of an allocation sequence should not usually be an issue. However, because small numbers of clusters are randomised, there is a possibility of chance baseline imbalance between the randomised groups, in terms of either the clusters or the individuals. Although not a form of bias as such, the risk of baseline differences can be reduced by using stratified or pair‐matched randomisation of clusters. Reporting of the baseline comparability of clusters, or statistical adjustment for baseline characteristics, can help reduce concern about the effects of baseline imbalance.
-
Loss of clusters. Occasionally complete clusters are lost from a trial, and have to be omitted from the analysis. Just as for missing outcome data in individually randomised trials, this may lead to bias. In addition, missing outcomes for individuals within clusters may also lead to a risk of bias in cluster‐randomised trials.
-
Incorrect analysis. Many cluster‐randomised trials are analysed by incorrect statistical methods, not taking the clustering into account. Such analyses create a 'unit of analysis error' and produce over‐precise results (the standard error of the estimated intervention effect is too small) and P values that are too small. They do not lead to biased estimates of effect. However, if they remain uncorrected, they will receive too much weight in a meta‐analysis.
-
Comparability with individually randomised trials. In a meta‐analysis including both cluster and individually randomised trials, or including cluster‐randomised trials with different types of clusters, possible differences between the intervention effects being estimated need to be considered. For example, in a vaccine trial of infectious diseases, a vaccine applied to all individuals in a community would be expected to be more effective than if the vaccine was applied to only half of the people. Another example is provided by a Cochrane Review of hip protectors. The cluster trials showed large positive effect whereas individually randomised trials did not show any clear benefit. One possibility is that there was a 'herd effect' in the cluster‐randomised trials (which were often performed in nursing homes, where compliance with using the protectors may have been enhanced). In general, such 'contamination' would lead to underestimates of effect. Thus, if an intervention effect is still demonstrated despite contamination in those trials that were not cluster‐randomised, a confident conclusion about the presence of an effect can be drawn. However, the size of the effect is likely to be underestimated. Contamination and 'herd effects' may be different for different types of cluster.
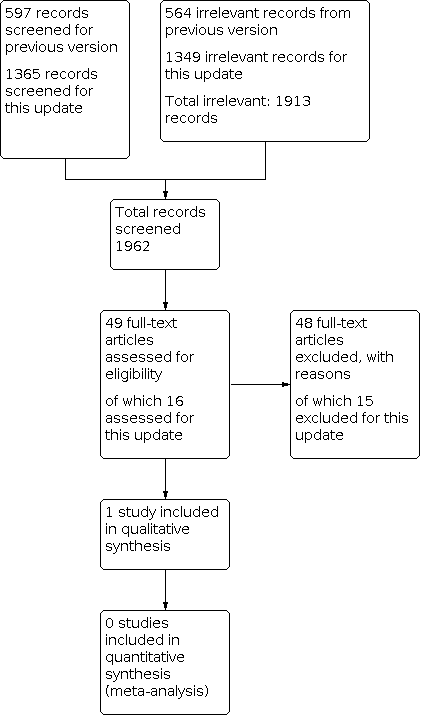
Study flow diagram.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
| Cone of pressure flap compared with standard flap technique | ||||||
| Patient or population: people with stage IV pressure ulcers | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Certainty of the evidence | Comments | |
|---|---|---|---|---|---|---|
| Risk with standard flap | Risk with COP flap | |||||
| Complete healing of surgical wound Follow‐up: 16 months | Study population | Not calculable | 20 (1 RCT) | ⊕⊝⊝⊝ | The included study reported that minor complications, including delayed wound healing and wound dehiscence that did not require surgical intervention, were comparable between the groups. We could not calculate an effect estimate and are uncertain of the effect of the interventions on wound healing. | |
| Not calculable | Not calculable | |||||
| Wound dehiscence Follow‐up: 16 months | Study population | Not calculable | 20 (1 RCT) | ⊕⊝⊝⊝ | The included study reported that minor complications, including delayed wound healing and wound dehiscence that did not require surgical intervention, were comparable between the groups. We could not calculate an effect estimate and are uncertain of the effect of the interventions on wound dehiscence. | |
| Not calculable | Not calculable | |||||
| Pressure ulcer recurrence | Study population | Not calculable | 20 (1 RCT) | ⊕⊝⊝⊝ | The included study did not clearly report the proportion of participants in each group with pressure ulcer recurrence. We could not calculate an effect estimate and are uncertain of the effect of the interventions on ulcer recurrence. | |
| Not calculable | Not calculable | |||||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; COP: cone of pressure; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence | ||||||
| aDowngraded two levels for high risk of bias in multiple domains, and two levels for imprecision due to low participant number and incomplete reporting. | ||||||

