انجام تمرینات ورزشی پیش از جراحی برای بیماران مبتلا به سرطان سلول غیر‐کوچک ریه
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع اضافی
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ir a:
| Methods | Two randomised controlled trials Setting: USA (University of Pittsburgh and Mayo Clinic) Study duration: Study 1 – 18 months. Exercise training ‐ 4 weeks. Study 2 – 1 year. Exercise training ‐ 1 week. | |
| Participants | Participants were included in the studies if they were undergoing lung cancer resection by open thoracotomy (segmentectomy, lobectomy, or pneumonectomy) or by video‐assisted thoracoscopy (at least lobectomy), and had moderate to severe chronic obstructive pulmonary disease. Study 1 – 9 participants were randomised in 18 months from a large surgical practice (5 hospitals: academic (three) and community (two)) Study 2 – 19 participants (mean age 72 ± 7 years – control group; 70 ± 9 years – exercise group) were randomised in one year from one site (Mayo Clinic). 2 were considered inoperable and therefore, post‐operative data are missing. | |
| Interventions | Study 1 Control (N = 4): usual care, which was not defined in the paper. Exercise (N = 5): four weeks of preoperative pulmonary rehabilitation that followed American Thoracic Society/ European Respiratory Society guidelines on exercise prescription (details on the exercise training program were not given). Study 2 Control (N = 9): usual care, which was not defined in the paper. Exercise (N = 10): twice‐daily, ten‐session preoperative pulmonary rehabilitation that included 20 minutes of lower extremity endurance training on a treadmill, upper extremity endurance training on an arm ergometer, strengthening exercises for upper and lower limbs with Thera‐band (every second day), 15 to 10 minutes of inspiratory muscle training, 10 minutes of pursed‐lip breathing and prescription of weekend exercises based on their performance during the pulmonary rehabilitation program. | |
| Outcomes | The outcomes of the two studies were hospital length of stay and postoperative pulmonary complications, defined as pneumonia (new infiltrate + either fever (> 38.5° C) and white cell count > 11,000, or fever and purulent secretions), severe atelectasis (requiring bronchoscopy), prolonged chest tubes (> 7 days), and prolonged mechanical ventilation (> 24 h). | |
| Notes | Study 1 had poor recruitment (providers were not willing to delay the curative surgery for 4 weeks) and was stopped, due to the low likelihood of meaningful accrual during the funding period. Therefore, only data from study 2 have been extracted for this systematic review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: Insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Comment: Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | High risk | Comment: No blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: “Outcomes were obtained using chart review by a nurse trained in the abstraction of the desired outcomes from the medical records and blinded to the treatment” |
| Incomplete outcome data (attrition bias) | Low risk | Quote: “Two patients (one on each arm) were missing length of stay data; because they were considered inoperable once they were in the operating room and were excluded from the outcome analysis” Comment: Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. |
| Selective reporting (reporting bias) | High risk | Quote: “Patients did not improve the shuttle walk test after the short term PR (P = NS)”. Comment: One of the outcomes of interest in the review (exercise capacity) is reported incompletely, so it could not be entered in a meta‐analysis. |
| Other bias | High risk | Comment: Study 1 ceased early due to poor recruitment |
| Methods | Randomised controlled trial Setting: Department of Thoracic Surgery, West China Hospital, China. Study duration: One week before lung resection until hospital discharge. | |
| Participants | 60 patients who were ≥ 70 yr (mean age 71.6 ± 1.9 years – control group; 72.5 ± 3.4 years – exercise group), with NSCLC, referred for lung resection. | |
| Interventions | Control (N = 30): conventional preoperative respiratory management, and no formal preoperative exercise training. Exercise (N = 30): abdominal breathing training, expiration exercises and aerobic training using the NuStep (NuStep, Inc. Ann Arbor, MI). | |
| Outcomes | Post‐intervention: 6‐minute walk distance, health‐related quality of life, and pulmonary function. Postoperatively: length of hospital stay, postoperative complications. | |
| Notes | N/A | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “…randomly allocated into the PR or control (non‐pulmonary rehabilitation, NPR) group.” Comment: insufficient information to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | High risk | Comment: No blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: “All participants were assessed, and data were recorded by a physiotherapist who was blinded to the grouping and the study purpose.” |
| Incomplete outcome data (attrition bias) | Low risk | Quote: “During the study, four patients in the PR group suspended the training because they could not endure the highly intensive regimen, one perceived a lack of benefit, and one suffered from knee pain. According to the intention‐to‐treat principle, we included those who did not complete the regimen in the final analysis” |
| Selective reporting (reporting bias) | High risk | Comment: protocol was registered retrospectively (ChiCTR‐IOR‐16008109). Age inclusion criterion on the registration was different (> 60 yr) and two outcome measures (cardiopulmonary function and blood gas analysis) listed on the registration were not reported in the published study. |
| Other bias | Low risk | Comment: the study appears to be free of other sources of bias |
| Methods | Randomised controlled trial Setting: teaching hospital in Ceara, Brazil Study duration: March 2008 to March 2011. Exercise training ‐ 4 weeks preoperatively. Assessments were performed before and after the preoperative intervention. Postoperative outcomes were obtained from medical records. | |
| Participants | 24 participants (mean age 69 ± 7 years – control group; 65 ± 8 years – exercise group) with non‐small cell lung cancer, who were undergoing lung resection via open thoracotomy or video‐assisted thoracoscopy, and had impaired lung function. 31 patients recruited, 7 patients were excluded, 5 of whom refused participation, and 2 who did not meet inclusion criteria because of normal pulmonary function. | |
| Interventions | Control (N = 12): usual care that consisted of instructions about lung expansion techniques. Exercise (N = 12): 5 sessions/week for 4 weeks of upper and lower limb endurance training (prescribed at 80% of maximum work rate achieved during a treadmill incremental test), inspiratory muscle training as well as flexibility, stretching, and balance exercises. Both groups had education: classes about the importance of preoperative and postoperative care and knowledge of the surgical process, energy conservation techniques, relaxation and stress management techniques, focus on nutrition, and the need to seek health services when necessary. | |
| Outcomes | Post‐intervention: physical capacity measured using the following tests: unsupported upper limb exercise test (UULEX), endurance testing, and the 6‐min walk test (6MWT). Quality of life was assessed using the Medical Outcomes Study 36 – Item Short Form Health Survey (SF‐36). Feelings of anxiety and depression were determined using the Hospital Anxiety and Depression Scale (HADS). Serum levels of fibrinogen and albumin were measured using a blood sample collected in disposable Vacutainer tubes. Lung function was assessed using spirometry. Postoperatively: length of hospital stay and postoperative pulmonary complications: pneumonia (new infiltrate plus either fever (temperature > 38° C), and white blood cell count > 11,000, or fever and purulent secretions), bronchopleural fistula, bronchospasm, severe atelectasis (confirmed by chest radiographs, requiring chest physiotherapy or bronchoscopy), prolonged need for chest tubes (> 7 d), and prolonged mechanical ventilation (> 48 h)). | |
| Notes | This study was published in two different papers. The paper published in 2013 focused on postoperative outcomes, whereas the paper published in 2014 focused on post‐intervention (preoperative) outcomes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “patients were randomly assigned to undergo a preoperative PR or CPT program. The randomisation was done in blocks of 4”. Comment: Insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Quote: “The randomisation was done in blocks of 4, and individual allocations were placed in sealed envelopes. An external investigator blinded to the allocation sequence picked the envelopes” Comment: Insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | High risk | Quote: “Single‐blinded”. Comment: No blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) | Unclear risk | Quote: “Postoperative outcomes were obtained from the medical records by a physical therapist blinded to the treatment assignment” Comment: although postoperative outcomes were obtained by a physical therapist blinded to the treatment assignment, it is not clear whether post‐intervention outcome measures were taken by a blind assessor. Therefore, there is insufficient information to permit judgement. |
| Incomplete outcome data (attrition bias) | High risk | Quote: 2013 study ‐ “Three patients in the CPT arm were not submitted to lung resection because of inoperable cancer.” Quote: 2014 study ‐ “All 24 participants successfully completed the training assignments.” Comment: 2013 study ‐ All patients accounted for. Greater drop‐outs in control group but reasons given. |
| Selective reporting (reporting bias) | High risk | Comment: Some reported outcomes were not pre‐specified in the study protocol (UTN Number: U1111‐1122‐2906) and not all of the study’s pre‐specified outcomes were reported. |
| Other bias | Low risk | Comment: The study appears to be free of other sources of bias |
| Methods | Randomised controlled trial Setting: not described. The study was undertaken in Turkey. Study duration: between January 2007 and August 2008. Exercise training ‐ One week before lung resection until hospital discharge. | |
| Participants | 60 patients (mean age 55 ± 8 years – control group; 54 ± 9 years – exercise group), with NSCLC (stage I to IIIB), referred for lung resection. | |
| Interventions | Control (N = 30): usual care with no formal preoperative exercise training. Exercise (N = 30): intensive physical therapy (IPT; chest physiotherapy and walking exercise). Chest physiotherapy consisted of diaphragmatic, pursed lip, segmental breathing exercise, usage of incentive spirometry, coughing exercise. The walking exercise was done by the patient on a treadmill three times a day, according to the patient's tolerance to exercise speed and time. *Postoperatively ‐ Routine physical therapy was performed until discharge in both groups. | |
| Outcomes | Post‐intervention: lung function, arterial blood gases Postoperatively: length of hospital stay, postoperative complications, mortality | |
| Notes | Nil | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Comment: different quotes in two parts of the paper. Both methods described are at high risk of failure. Quotes: 1 “… randomly allocated (according to hospital record number) to control or study group.”; 2 "Allocation was based on hospital record number." |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | High risk | Comment: no blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | Low risk | Comment: The study appears to be free of other sources of bias |
| Methods | Randomised controlled trial Setting: outpatient clinic. The study was undertaken in Naples, Italy. Study duration: February 2010 until December 2011 | |
| Participants | 40 patients (23 males; age 65 ± 7 years) with chronic obstructive pulmonary disease, undergoing lobectomy (via open thoracotomy) for stage I/II NSCLC were enrolled in the study. | |
| Interventions | Control (N = not reported): usual care with no formal exercise training. Exercise (N = not reported): 3‐week (15 3‐h sessions, from Monday to Friday) preoperative outpatient intensive pulmonary rehabilitation program based on high‐intensity training of both upper‐ and lower‐limb muscles (the upper limbs with the rowing ergometer, and the lower limbs by means of the treadmill and the ergometric bicycle). The exercise work load for each patient was set according to the results of the cardiopulmonary exercise test, starting with 70% of the maximum work rate and increased by 10 W when the patient was able to tolerate the set load for 30 min. The program also included respiratory exercises on the bench, mattress pad and wall bars. | |
| Outcomes | Post‐intervention and 60 days postoperatively: lung function (forced expired volume in 1 second, forced vital capacity, and diffusing capacity for carbon monoxide); dyspnoea (Borg scale), and exercise capacity (peak oxygen uptake during the cardiopulmonary exercise test). | |
| Notes | The study did not report on length of hospital stay or postoperative pulmonary complications. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Patients were randomly assigned to two groups” Comment: insufficient information about the sequence generation process to permit judgement |
| Allocation concealment (selection bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Blinding of participants and personnel (performance bias) | High risk | Comment: no blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Incomplete outcome data (attrition bias) | Unclear risk | Comment: Insufficient reporting of attrition/exclusions to permit judgement |
| Selective reporting (reporting bias) | Unclear risk | Comment: insufficient information to permit judgement |
| Other bias | High risk | Comment: number of participants in each group not reported. |
NSCLC ‐ non‐small cell lung cancer
Characteristics of excluded studies [ordered by study ID]
Ir a:
| Study | Reason for exclusion |
| Not an RCT | |
| Conference abstract. Unpublished study | |
| Not an RCT | |
| Did not reply to contact attempts | |
| No exercise training | |
| Did not reply to contact attempts | |
| Not an RCT | |
| Not an RCT | |
| Included early postoperative exercise training | |
| Not an RCT | |
| Conference abstract. Unpublished study |
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Risk of developing a postoperative pulmonary complication Show forest plot | 4 | 158 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.17, 0.61] |
| Analysis 1.1  Comparison 1 Intervention group versus control group, Outcome 1 Risk of developing a postoperative pulmonary complication. | ||||
| 2 Number of days patients needed an intercostal catheter Show forest plot | 2 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐3.33 [‐5.35, ‐1.30] |
| Analysis 1.2  Comparison 1 Intervention group versus control group, Outcome 2 Number of days patients needed an intercostal catheter. | ||||
| 3 Postoperative length of hospital stay Show forest plot | 4 | 158 | Mean Difference (IV, Fixed, 95% CI) | ‐4.24 [‐5.43, ‐3.06] |
| Analysis 1.3  Comparison 1 Intervention group versus control group, Outcome 3 Postoperative length of hospital stay. | ||||
| 4 Preoperative exercise capacity (6‐minute walk distance) Show forest plot | 2 | 81 | Mean Difference (IV, Fixed, 95% CI) | 18.23 [8.50, 27.96] |
| Analysis 1.4  Comparison 1 Intervention group versus control group, Outcome 4 Preoperative exercise capacity (6‐minute walk distance). | ||||
| 5 Forced vital capacity (% pred) Show forest plot | 2 | 84 | Mean Difference (IV, Fixed, 95% CI) | 2.97 [1.78, 4.16] |
| Analysis 1.5  Comparison 1 Intervention group versus control group, Outcome 5 Forced vital capacity (% pred). | ||||
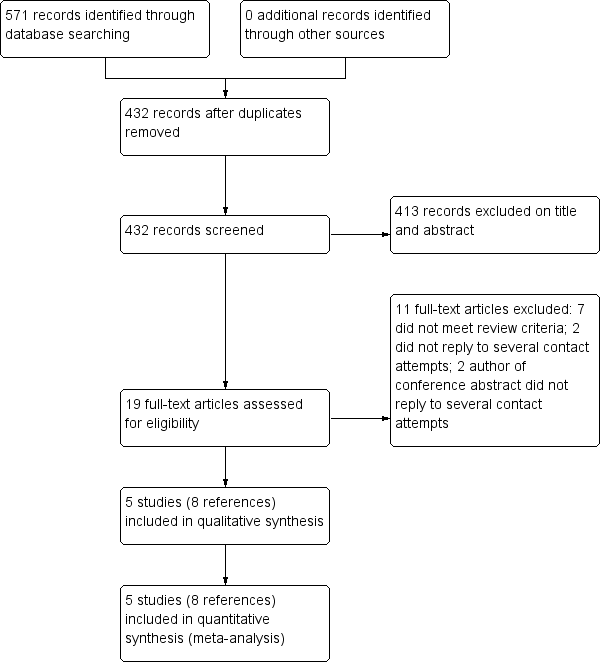
Flow diagram of references identified, excluded, and included in review
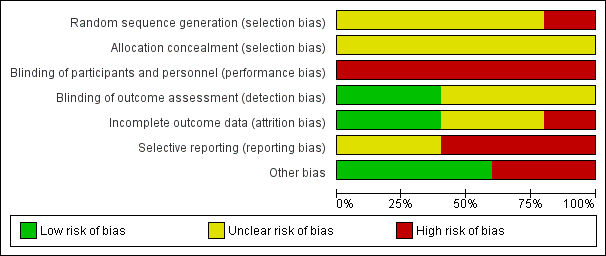
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Forest plot of comparison: 1 Intervention group versus control group, outcome: 1.1 Risk of developing a postoperative pulmonary complication.
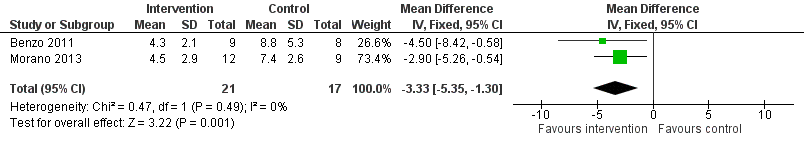
Forest plot of comparison: 1 Intervention group versus control group, outcome: 1.2 Number of days patients needed an intercostal catheter.
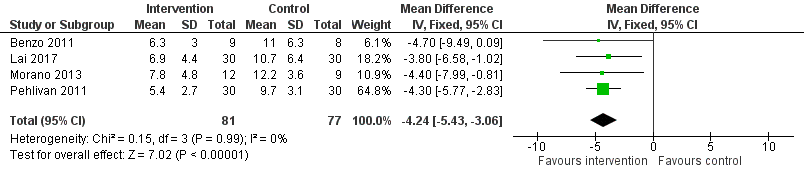
Forest plot of comparison: 1 Intervention group versus control group, outcome: 1.3 Postoperative length of hospital stay.

Comparison 1 Intervention group versus control group, Outcome 1 Risk of developing a postoperative pulmonary complication.

Comparison 1 Intervention group versus control group, Outcome 2 Number of days patients needed an intercostal catheter.

Comparison 1 Intervention group versus control group, Outcome 3 Postoperative length of hospital stay.
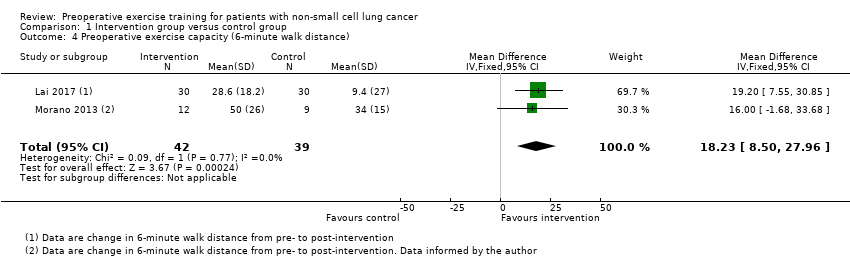
Comparison 1 Intervention group versus control group, Outcome 4 Preoperative exercise capacity (6‐minute walk distance).

Comparison 1 Intervention group versus control group, Outcome 5 Forced vital capacity (% pred).
| Preoperative exercise training compared to no exercise training for patients scheduled to undergo lung resection for non‐small cell lung cancer | ||||||
| Patient or population: patients scheduled to undergo lung resection for non‐small cell lung cancer | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | № of participants | Quality of the evidence | Comments | |
| Risk with no exercise training | Risk with preoperative exercise training | |||||
| Number of patients who developed postoperative pulmonary complications | Study population | RR 0.33 | 158 | ⊕⊕⊝⊝ | ||
| 22 per 100 | 7 per 100 | |||||
| Number of days patients needed an intercostal catheter | The mean number of days patients needed an intercostal catheter in the control groups ranged from 7.4 to 8.8 days | The number of days patients needed an intercostal catheter in the intervention groups was, on average, 3.33 fewer days | ‐ | 38 | ⊕⊕⊝⊝ | |
| Postoperative length of hospital stay | The mean postoperative length of hospital stay in the control groups ranged from 9.7 to 12.2 days | The postoperative length of hospital stay in the intervention groups was, on average, 4.34 fewer days (95% CI 5.65 to 3.03 fewer days) | ‐ | 158 | ⊕⊕⊝⊝ | |
| Post‐intervention exercise capacity assessed with: 6‐minute walk distance (6MWD) | The mean post‐intervention exercise capacity in the control groups ranged from 340 to 434 metres in 6 minutes. | The post‐intervention exercise capacity in the intervention groups was, on average, 18.23 metres more | ‐ | 81 | ⊕⊕⊝⊝ | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Significant risk of bias across the studies 2 Small sample sizes across the studies, some with wide confidence intervals | ||||||
| Study | Results |
| Number of patients who developed a postoperative pulmonary complication: Intervention group (IG): 3 of 9 (33%) Control Group (CG): 5 of 8 (63%) P = 0.23 (between‐group) Number of days patients needed a chest tube: IG: 4.3 ± 2.1 days CG: 8.8 ± 5.3 days P = 0.03 (between‐group) Postoperative length of hospital stay: IG: 6.3 ± 3.0 days CG: 11.0 ± 6.3 days P = 0.058 (between‐group) | |
| Number of patients who developed a postoperative pulmonary complication: IG: 4 of 30 (13%) CG: 11 of 30 (37%) P = 0.037 (between‐group) Postoperative length of hospital stay: IG: 6.9 ± 4.4 days CG: 10.7 ± 6.4 days P = 0.01 (between‐group) Exercise capacity: Six‐Minute Walk Distance (6MWD), in metres: IG: 30 participants completed; CG: 30 participants completed; Preoperative measurements: baseline and post‐intervention: Mean ± standard deviation (SD): IG: 431.7 ± 102.8 m to 460.3 ± 93.6 m; CG: 434.5 ± 86.2 m to 443.9 ± 88.4 m P = 0.029 (between‐group) | |
| Number of patients who developed a postoperative pulmonary complication: IG: 2 of 12 (17%) CG: 7 of 9 (78%) P = 0.01 (between‐group) Number of days patients needed a chest tube: IG: 4.5 ± 2.9 days CG: 7.4 ± 2.6 days P = 0.03 (between‐group) Postoperative length of hospital stay: IG: 7.8 ± 4.8 days CG: 12.2 ± 3.6 days P = 0.04 (between‐group) Exercise capacity: Six‐Minute Walk Distance (6MWD), in metres: IG: 12 participants completed; CG: 12 participants completed; Preoperative measurements: baseline and post‐intervention: Mean ± standard deviation (SD): IG: 425.5 ± 85.3 m to 475 ± 86.5 m (P < 0.01); CG: 339.6 ± 107 m to 335 ± 107 m (P > 0.05) P < 0.001 (between‐group) Lung function: (i) Forced expired volume in one second (FEV1; % predicted): IG: 12 participants completed; CG: 12 participants completed; Preoperative measurements: baseline and post‐intervention: IG: 48.1 ± 13.9% to 54.8 ± 22.4% (P = 0.08); CG: 51.7 ± 9.8% to 58.8 ± 13.0% (P = 0.23) Between‐group difference was not calculated (ii) Forced vital capacity (FVC; % predicted): IG: 12 participants completed; CG: 12 participants completed; Preoperative measurements: baseline and post‐intervention: Median (interquartile range): IG: 62.5% (49 to 71) to 76% (65 to 79.7); P = 0.02; CG: 62.5% (56 to 92) to 71% (63.2 to 89); P = 0.37 Between‐group difference was not calculated | |
| Number of patients who developed a postoperative pulmonary complication: IG: 1 of 30 (3%) CG: 5 of 30 (17%) P = 0.04 (between‐group) Postoperative length of hospital stay: IG: 5.4 ± 2.7 days CG: 9.7 ± 3.1 days P < 0.001 (between‐group) Lung function: (i) FEV1; % predicted: IG: 30 participants completed; CG: 30 participants completed; Preoperative measurements: change from baseline to post‐intervention: IG: 15.84 ± 2.10%; CG: 9.92 ± 3.5% P = 0.3 (between‐group) (ii) FVC; % predicted: IG: 30 participants completed; CG: 30 participants completed; Preoperative measurements: baseline and post‐intervention: IG: 19.26 ± 2.33%; CG: 16.3 ± 2.4% P = 0.6 (between‐group) | |
| Exercise capacity: Peak rate of oxygen uptake (VO2peak), in ml/kg/min: IG: 20 participants completed; CG: 20 participants completed; Preoperative measurements: baseline and post‐intervention: IG: 14.9 ± 2.3 ml/kg/min to 17.8 ± 2.1 ml/kg/min; CG: 14.8 ± 1.4 ml/kg/min to 14.5 ± 1.2 ml/kg/min P < 0.001 (between‐group) Lung function: FEV1; % predicted: IG: 20 participants completed; CG: 20 participants completed; Preoperative measurements: baseline and post‐intervention: IG: 57.4 ± 19.1% to 59.8 ± 19.2%; CG: 57.6 ± 16.9% to 57.5 ± 17.0% P > 0.05 (between‐group) | |
| Intervention group (IG), Control Group (CG) | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Risk of developing a postoperative pulmonary complication Show forest plot | 4 | 158 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.17, 0.61] |
| 2 Number of days patients needed an intercostal catheter Show forest plot | 2 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐3.33 [‐5.35, ‐1.30] |
| 3 Postoperative length of hospital stay Show forest plot | 4 | 158 | Mean Difference (IV, Fixed, 95% CI) | ‐4.24 [‐5.43, ‐3.06] |
| 4 Preoperative exercise capacity (6‐minute walk distance) Show forest plot | 2 | 81 | Mean Difference (IV, Fixed, 95% CI) | 18.23 [8.50, 27.96] |
| 5 Forced vital capacity (% pred) Show forest plot | 2 | 84 | Mean Difference (IV, Fixed, 95% CI) | 2.97 [1.78, 4.16] |

