Home use of interdental cleaning devices, in addition to toothbrushing, for preventing and controlling periodontal diseases and dental caries
Abstract
Background
Dental caries (tooth decay) and periodontal diseases (gingivitis and periodontitis) affect the majority of people worldwide, and treatment costs place a significant burden on health services. Decay and gum disease can cause pain, eating and speaking difficulties, low self‐esteem, and even tooth loss and the need for surgery. As dental plaque is the primary cause, self‐administered daily mechanical disruption and removal of plaque is important for oral health. Toothbrushing can remove supragingival plaque on the facial and lingual/palatal surfaces, but special devices (such as floss, brushes, sticks, and irrigators) are often recommended to reach into the interdental area.
Objectives
To evaluate the effectiveness of interdental cleaning devices used at home, in addition to toothbrushing, compared with toothbrushing alone, for preventing and controlling periodontal diseases, caries, and plaque. A secondary objective was to compare different interdental cleaning devices with each other.
Search methods
Cochrane Oral Health’s Information Specialist searched: Cochrane Oral Health’s Trials Register (to 16 January 2019), the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library, 2018, Issue 12), MEDLINE Ovid (1946 to 16 January 2019), Embase Ovid (1980 to 16 January 2019) and CINAHL EBSCO (1937 to 16 January 2019). The US National Institutes of Health Trials Registry (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform were searched for ongoing trials. No restrictions were placed on the language or date of publication.
Selection criteria
Randomised controlled trials (RCTs) that compared toothbrushing and a home‐use interdental cleaning device versus toothbrushing alone or with another device (minimum duration four weeks).
Data collection and analysis
At least two review authors independently screened searches, selected studies, extracted data, assessed studies' risk of bias, and assessed evidence certainty as high, moderate, low or very low, according to GRADE. We extracted indices measured on interproximal surfaces, where possible. We conducted random‐effects meta‐analyses, using mean differences (MDs) or standardised mean differences (SMDs).
Main results
We included 35 RCTs (3929 randomised adult participants). Studies were at high risk of performance bias as blinding of participants was not possible. Only two studies were otherwise at low risk of bias. Many participants had a low level of baseline gingival inflammation.
Studies evaluated the following devices plus toothbrushing versus toothbrushing: floss (15 trials), interdental brushes (2 trials), wooden cleaning sticks (2 trials), rubber/elastomeric cleaning sticks (2 trials), oral irrigators (5 trials). Four devices were compared with floss: interdental brushes (9 trials), wooden cleaning sticks (3 trials), rubber/elastomeric cleaning sticks (9 trials) and oral irrigators (2 trials). Another comparison was rubber/elastomeric cleaning sticks versus interdental brushes (3 trials).
No trials assessed interproximal caries, and most did not assess periodontitis. Gingivitis was measured by indices (most commonly, Löe‐Silness, 0 to 3 scale) and by proportion of bleeding sites. Plaque was measured by indices, most often Quigley‐Hein (0 to 5).
Primary objective: comparisons against toothbrushing alone
Low‐certainty evidence suggested that flossing, in addition to toothbrushing, may reduce gingivitis (measured by gingival index (GI)) at one month (SMD ‐0.58, 95% confidence interval (CI) ‐1.12 to ‐0.04; 8 trials, 585 participants), three months or six months. The results for proportion of bleeding sites and plaque were inconsistent (very low‐certainty evidence).
Very low‐certainty evidence suggested that using an interdental brush, plus toothbrushing, may reduce gingivitis (measured by GI) at one month (MD ‐0.53, 95% CI ‐0.83 to ‐0.23; 1 trial, 62 participants), though there was no clear difference in bleeding sites (MD ‐0.05, 95% CI ‐0.13 to 0.03; 1 trial, 31 participants). Low‐certainty evidence suggested interdental brushes may reduce plaque more than toothbrushing alone (SMD ‐1.07, 95% CI ‐1.51 to ‐0.63; 2 trials, 93 participants).
Very low‐certainty evidence suggested that using wooden cleaning sticks, plus toothbrushing, may reduce bleeding sites at three months (MD ‐0.25, 95% CI ‐0.37 to ‐0.13; 1 trial, 24 participants), but not plaque (MD ‐0.03, 95% CI ‐0.13 to 0.07).
Very low‐certainty evidence suggested that using rubber/elastomeric interdental cleaning sticks, plus toothbrushing, may reduce plaque at one month (MD ‐0.22, 95% CI ‐0.41 to ‐0.03), but this was not found for gingivitis (GI MD ‐0.01, 95% CI ‐0.19 to 0.21; 1 trial, 12 participants; bleeding MD 0.07, 95% CI ‐0.15 to 0.01; 1 trial, 30 participants).
Very‐low certainty evidence suggested oral irrigators may reduce gingivitis measured by GI at one month (SMD ‐0.48, 95% CI ‐0.89 to ‐0.06; 4 trials, 380 participants), but not at three or six months. Low‐certainty evidence suggested that oral irrigators did not reduce bleeding sites at one month (MD ‐0.00, 95% CI ‐0.07 to 0.06; 2 trials, 126 participants) or three months, or plaque at one month (SMD ‐0.16, 95% CI ‐0.41 to 0.10; 3 trials, 235 participants), three months or six months, more than toothbrushing alone.
Secondary objective: comparisons between devices
Low‐certainty evidence suggested interdental brushes may reduce gingivitis more than floss at one and three months, but did not show a difference for periodontitis measured by probing pocket depth. Evidence for plaque was inconsistent.
Low‐ to very low‐certainty evidence suggested oral irrigation may reduce gingivitis at one month compared to flossing, but very low‐certainty evidence did not suggest a difference between devices for plaque.
Very low‐certainty evidence for interdental brushes or flossing versus interdental cleaning sticks did not demonstrate superiority of either intervention.
Adverse events
Studies that measured adverse events found no severe events caused by devices, and no evidence of differences between study groups in minor effects such as gingival irritation.
Authors' conclusions
Using floss or interdental brushes in addition to toothbrushing may reduce gingivitis or plaque, or both, more than toothbrushing alone. Interdental brushes may be more effective than floss. Available evidence for tooth cleaning sticks and oral irrigators is limited and inconsistent. Outcomes were mostly measured in the short term and participants in most studies had a low level of baseline gingival inflammation. Overall, the evidence was low to very low‐certainty, and the effect sizes observed may not be clinically important. Future trials should report participant periodontal status according to the new periodontal diseases classification, and last long enough to measure interproximal caries and periodontitis.
PICO
Plain language summary
Home use of devices for cleaning between the teeth (in addition to toothbrushing) to prevent and control gum diseases and tooth decay
Review question
How effective are home‐use interdental cleaning devices, plus toothbrushing, compared with toothbrushing only or use of another device, for preventing and controlling periodontal (gum) diseases (gingivitis and periodontitis), tooth decay (dental caries) and plaque?
Background
Tooth decay and gum diseases affect most people. They can cause pain, difficulties with eating and speaking, low self‐esteem, and, in extreme cases, may lead to tooth loss and the need for surgery. The cost to health services of treating these diseases is very high.
As dental plaque (a layer of bacteria in an organic matrix that forms on the teeth) is the root cause, it is important to remove plaque from teeth on a regular basis. While many people routinely brush their teeth to remove plaque up to the gum line, it is difficult for toothbrushes to reach into areas between teeth ('interdental'), so interdental cleaning is often recommended as an extra step in personal oral hygiene routines. Different tools can be used to clean interdentally, such as dental floss, interdental brushes, tooth cleaning sticks, and water pressure devices known as oral irrigators.
Study characteristics
Review authors working with Cochrane Oral Health searched for studies up to 16 January 2019. We identified 35 studies (3929 adult participants). Participants knew that they were in an experiment, which might have affected their teeth cleaning or eating behaviour. Some studies had other problems that might make their findings less reliable, such as people dropping out of the study or not using the assigned device.
Studies evaluated the following devices plus toothbrushing compared to toothbrushing only: floss (15 studies), interdental brushes (2 studies), wooden cleaning sticks (2 studies), rubber/elastomeric cleaning sticks (2 studies) and oral irrigators (5 studies). Four devices were compared with floss: interdental brushes (9 studies), wooden cleaning sticks (3 studies), rubber/elastomeric cleaning sticks (9 studies), oral irrigators (2 studies). Three studies compared rubber/elastomeric cleaning sticks with interdental brushes.
No studies evaluated decay, and few evaluated severe gum disease. Outcomes were measured at short (one month to six weeks) and medium term (three and six months).
Key results
We found that using floss, in addition to toothbrushing, may reduce gingivitis in the short and medium term. It is unclear if it reduces plaque.
Using an interdental brush, in addition to a toothbrush, may reduce gingivitis and plaque in the short term.
Using wooden tooth cleaning sticks may be better than toothbrushing only for reducing gingivitis (measured by bleeding sites) but not plaque in the medium term (only 24 participants).
Using a tooth cleaning stick made of rubber or an elastomer may be better than toothbrushing only for reducing plaque but not gingivitis in the short term (only 30 participants).
Toothbrushing plus oral irrigation (water pressure) may reduce gingivitis in the short term, but there was no evidence for this in the medium term. There was no evidence of a difference in plaque.
Interdental brushes may be better than flossing for gingivitis at one and three months. The evidence for plaque is inconsistent. There was no evidence of a difference between the devices for periodontitis measured by probing pocket depth.
There is some evidence that oral irrigation may be better than flossing for reducing gingivitis (but not plaque) in the short term.
The available evidence for interdental cleaning sticks did not show them to be better or worse than floss or interdental brushes for controlling gingivitis or plaque.
The studies that measured 'adverse events' found no serious effects and no evidence of differences between study groups in minor effects such as gum irritation.
Certainty of the evidence
The evidence is low to very low‐certainty. The effects observed may not be clinically important. Studies measured outcomes mostly in the short term and many participants had a low level of gum disease at the beginning of the studies.
Future research
Future studies should use the new periodontal diseases classification to describe the gum health of participants, and they should last long enough to measure periodontitis and tooth decay.
Authors' conclusions
Summary of findings
| Flossing plus toothbrushing for periodontal disease and dental caries in adults | ||||||
| Population: adults, 16 years and older Comparison: toothbrushing only | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Toothbrushing only | Flossing plus toothbrushing | |||||
| Gingivitis measured by gingival index SD units: investigators measured gingivitis using different scales Lower score means less severe gingivitis Follow‐up: 1 month | The gingivitis score in the flossing group was on average 0.58 SDs lower (95% CI 0.04 lower to 1.12 lower) than the control group | ‐ | 585 | ⊕⊕⊝⊝ | Flossing also reduced gingivitis at 3 months (‐0.33, ‐0.50 to ‐0.17, 4 studies, 570 participants) and 6 months (‐0.68, ‐0.95 to ‐0.42, 4 studies, 564 participants). | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 1 month | The median score in the control group was 0.16 | The mean score in the intervention group was 0.03 less (0.14 less to 0.08 more) | ‐ | 158 (2 studies) | ⊕⊝⊝⊝ | 3‐month follow‐up: ‐0.14 (‐0.37 to 0.09, 2 studies, 240 participants) 6‐month follow‐up: ‐0.06 (‐0.09 to ‐0.03; 1 study, 210 participants) |
| Periodontitis | One study measured probing pocket depth but no data were reported. | |||||
| Interproximal caries | No included study assessed caries as an outcome. | |||||
| Plaque SD units: investigators measured plaque using different scales Lower score means less plaque Follow‐up: 1 month | The plaque score in flossing group was on average 0.42 SDs lower (0.85 lower to 0.02 higher) than the control group | ‐ | 542 | ⊕⊝⊝⊝ | Significant difference found for plaque at 3 months (SMD 0.20, ‐0.36 to ‐0.04, 5 studies, 594 participants), but not at 6 months (‐0.13, ‐0.30 to 0.05, 3 studies, 487 participants). | |
| Harms and adverse effects | Adverse effects were assessed and reported in seven studies. Three reported no adverse events on the oral hard or soft tissues. Four reported sporadic adverse events with mild severity, with no evidence of a difference between the flossing plus toothbrushing group and toothbrushing only group. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to high and unclear risk of bias in the studies and substantial heterogeneity 2 Downgraded three levels due to high and unclear risk of bias in the studies, substantial heterogeneity and lack of precision in the estimate | ||||||
| Interdental brushing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Toothbrushing only | Interdental brush plus toothbrushing | |||||
| Gingivitis measured by gingival index SD units: investigators measure gingivitis using different scales Lower score means less severe gingivitis Follow‐up: 1 month | The gingivitis score in interdental brush group was on average 0.53 SDs lower (0.23 to 0.83 lower) than the control group | ‐ | 62 | ⊕⊝⊝⊝ | ||
| Gingivitis measured by proportion of bleeding sites Follow‐up: 1 month | The mean score in the control group was 0.19 | The mean score in the interdental brush group was 0.05 less (0.13 less to 0.03 more) | ‐ | 31 (1 study) | ⊕⊕⊝⊝ | |
| Periodontitis | One study measured probing pocket depth but no data were reported. | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: investigators measure plaque using different scales Lower score means less plaque Follow‐up: 1 month | The plaque score in the interdental brush group was on average 1.07 SDs lower (0.63 to 1.51 lower) than the control group | ‐ | 93 | ⊕⊕⊝⊝ | ||
| Harms and adverse outcomes | Neither study reported any information about adverse events. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to being based on only one small trial at unclear risk of bias 2 Downgraded three levels due to being based on only one small trial at unclear risk of bias 3 Downgraded two levels due to being based on only two small trials at unclear risk of bias | ||||||
| Wooden interdental cleaning stick compared to flossing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Toothbrushing alone | Wooden cleaning stick plus toothbrushing | |||||
| Gingivitis measured by gingival index | Not measured | ‐ | ‐ | ‐ | ‐ | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 3 months | The mean gingivitis score in the control group was 0.90 | The mean gingivitis score in the intervention group was | ‐ | 24 (1 study) | ⊕⊝⊝⊝ | 3‐month data only |
| Periodontitis | No included study assessed periodontitis as an outcome | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque Follow‐up: 3 months | The mean plaque in the control group was 0.22 | The mean plaque score in the intervention group was | ‐ | 24 | ⊕⊝⊝⊝ | 3‐month data only |
| Harms and adverse outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to there being only one small trial at unclear risk of bias 2 Downgraded three levels due to there being only one small trial, at unclear risk of bias, and lack of precision in the estimate | ||||||
| Interdental cleaning stick compared to flossing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Toothbrush alone | Cleaning stick plus toothbrushing | |||||
| Gingivitis measured by gingival index Lower score means less severe gingivitis Follow‐up: 1 month | The mean score in the control group was 0.22 | The mean score in the intervention group was on average 0.01 lower (0.19 lower to 0.21 higher) than the control group.1 | ‐ | 12 | ⊕⊝⊝⊝ | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 1 month | The mean score in the control group was 0.19 | The mean score in the intervention group was 0.07 lower (0.15 lower to 0.01 higher) | ‐ | 30 (1 study) | ⊕⊝⊝⊝ | |
| Periodontitis | One study measured probing pocket depth but no data were reported. | |||||
| Interproximal caries | No included study assessed caries as an outcome. | |||||
| Plaque (proportion of sites with plaque) Follow‐up: 1 month | The mean plaque in the control group was 0.42 | The mean plaque score in the intervention group was | ‐ | 30 | ⊕⊝⊝⊝ | |
| Harms and adverse outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to being based on single small study at high risk of bias, and lack of precision in the estimate | ||||||
| Oral irrigation plus toothbrushing compared to toothbrushing alone for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Toothbrushing alone | Oral irrigation plus toothbrushing | |||||
| Gingivitis measured by gingival index SD units: investigators measure gingivitis using different scales Lower score means less severe gingivitis Follow‐up: 1 month | The gingivitis score in oral irrigation group was on average 0.48 SDs lower (0.06 lower to 0.89 lower) than the control group. | ‐ | 380 | ⊕⊝⊝⊝ | No significant evidence of a difference at 3 months (SMD ‐0.13, ‐0.44 to 0.17; 2 trials, 163 participants) or 6 months (MD ‐0.33, ‐0.74 to 0.08; 1 trial, 109 participants) | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 1 month | The mean score in the control group was 0.30 | The mean score in the intervention group was the same (0.07 lower to 0.06 higher) | ‐ | 126 (2 studies) | ⊕⊕⊝⊝ | Nor any evidence of a difference at 3 months (MD ‐0.04, ‐0.13 to 0.05, 1 study, 54 participants) |
| Periodontitis | Measured in one study but useable data not provided | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: Lower score means less plaque. Follow‐up: 1 month | The plaque score in the oral irrigation group was on average 0.16 SDs lower (0.41 lower to 0.10 higher)1 than the control group | ‐ | 235 | ⊕⊕⊝⊝ | Nor did the evidence suggest benefit from the oral irrigator at 3 months (SMD 0.06, ‐0.25 to 0.37; 2 studies, 163 participants) or 6 months (MD 0.22, ‐0.59 to 0.15; 1 study, 109 participants) | |
| Harms and adverse outcomes | Three studies reported that there were no adverse events, one reported one incidence of aphthous ulcer in irrigator group, one reported oral lacerations but found no difference between the interventions, and one did not measure adverse events. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels as studies at unclear risk of bias, with substantial heterogeneity and imprecise estimate | ||||||
| Interdental brushing compared to flossing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Flossing | Interdental brush (IDB) | |||||
| Gingivitis measured by gingival index SD units: investigators measure gingivitis using different scales Lower score means less severe gingivitis | The gingivitis score in the IDB group was on average 0.40 SDs lower (0.11 to 0.70 lower)1than the flossing group | ‐ | 183 | ⊕⊕⊝⊝ | Not measured at 3 months | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 4 to 6 weeks | The mean score in the flossing group was 0.20 | The mean score in the IDB group was 0.06 lower (0.08 to 0.03 lower) | ‐ | 234 (6 studies) | ⊕⊕⊝⊝ | Results at 3 months also indicated a small benefit for interdental brushes: MD ‐0.10 (‐0.15 to ‐0.04), 2 studies, 106 participants. |
| Periodontitis Probing pocket depth in mm Follow‐up: 4 to 6 weeks | The mean PPD score for the flossing group was 5.01 mm | The mean PPD score in the IDB group was0.06 lower (0.27 lower to 0.16 higher) | ‐ | 107 (3 studies) | ⊕⊕⊝⊝ | Results were consistent at 3 months: MD 0.01 mm (‐0.29 to 0.31), 1 parallel‐group study, 77 participants. |
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: Lower score means less plaque | The plaque in the IDB group was on average 0.47 SDs lower (0.84 to 0.11 lower) than the flossing group | ‐ | 290 | ⊕⊝⊝⊝ | This benefit for IDB compared to flossing for parallel‐group studies is not supported by the meta‐analysis of the split‐mouth studies at one month (SMD ‐0.07 (‐0.32 to 0.18), 3 studies, 66 participants). Nor by the 3‐month data (MD ‐0.12, 95% ‐0.33 to 0.10; two trials (one parallel and one split‐mouth), 106 participants). | |
| Harms and adverse outcomes | Five studies reported there were no adverse events. Two studies reported on problems with the use of interdental brushes or floss, which sometimes caused soreness. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to studies at unclear risk of bias, imprecise estimate (although consistent) 2 Downgraded two levels due to studies at unclear risk of bias, moderate heterogeneity 3 Downgraded two levels due to studies at unclear risk of bias, imprecise estimate 4 Downgraded three levels due to unclear risk of bias, imprecise estimates and moderate heterogeneity | ||||||
| Wooden cleaning stick compared to flossing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Flossing plus toothbrushing | Wooden cleaning stick plus toothbrushing | |||||
| Gingivitis measured by gingival index | Not measured | |||||
| Gingivitis measured by proportion of bleeding sites Follow‐up: 3 months | The mean gingivitis score in the control group was 0.64 | The mean gingivitis score in the intervention group was | ‐ | 24 (1 study) | ⊕⊝⊝⊝ | Only 3‐month data useable |
| Periodontitis | No included study assessed periodontitis | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque Follow‐up: 3 months | The mean plaque in the control group was 0.88 | The mean plaque score in the intervention group was | ‐ | 24 | ⊕⊝⊝⊝ | Only 3‐month data useable |
| Harms and adverse outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to there being only one small trial, at unclear risk of bias, and lack of precision of estimate | ||||||
| Interdental cleaning stick compared to interdental brushing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Floss | Cleaning stick | |||||
| Gingivitis measured by gingival index SD units: investigators measure gingivitis using different scales Lower score means less severe gingivitis. Follow‐up: 4 to 6 weeks | The gingivitis score in the cleaning stick group was on average | ‐ | 256 | ⊕⊝⊝⊝ | Nor was there was evidence that one intervention performed better than the other with regards to gingivitis control at 3 months (MD 0.01, 95% CI ‐0.08 to 0.10, 1 study, 145 participants). | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 4 to 6 weeks | The mean score in the floss group was 0.22 | The mean score in the cleaning stick group was 0.03 lower (0.08 lower to 0.03 higher) | ‐ | 212 (5 studies) | ⊕⊕⊝⊝ | Nor was there was evidence that one intervention performed better than the other with regards to bleeding sites at 3 months (MD 0.01, 95% CI ‐0.03 to 0.05, 1 study, 145 participants) |
| Periodontitis | One study measured periodontitis but the data were not usable | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: investigators measure plaque using different scales Lower score means less plaque Follow‐up: 4 to 6 weeks | The plaque score in the cleaning stick group was on average | ‐ | 273 | ⊕⊝⊝⊝ | ||
| Harms and adverse outcomes | Five studies assessed adverse events. One did not report findings, but the others reported either no adverse events or minor adverse events that did not significantly differ between interventions. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to one study being at high risk of bias (others unclear), moderate heterogeneity and serious imprecision 2 Downgraded two levels due to studies at unclear risk of bias and moderate heterogeneity 3 Downgraded three levels due to studies at unclear risk of bias, moderate heterogeneity and serious imprecision | ||||||
| Oral irrigation compared to flossing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Flossing | Oral irrigation | |||||
| Gingivitis measured by gingival index SD units: investigators measure gingivitis using different scales Lower score means less severe gingivitis | The mean score in the floss group was 1.14 | The mean score in the irrigator group was 0.06 lower (0.12 lower to 0.00) | ‐ | 63 | ⊕⊝⊝⊝ | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 1 month | The mean score in the floss group was 0.56 | The mean score in the irrigator group was 0.12 lower (0.19 lower to 0.05 lower) | ‐ | 133 (2 studies) | ⊕⊕⊝⊝ | |
| Periodontitis | No included study assessed periodontitis | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: investigators measure plaque using different scales Lower score means less plaque | The plaque in the oral irrigation group was on average | ‐ | 133 | ⊕⊝⊝⊝ | ||
| Harms and adverse outcomes | Both studies reported there were no adverse events in either study group. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to single small study at unclear risk of bias 2 Downgraded three levels due to single small study at unclear risk of bias with serious imprecision | ||||||
| Interdental cleaning stick compared to interdental brushing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| IDB | Stick | |||||
| Gingivitis measured by gingival index Lower score means less severe gingivitis Follow‐up: 4 to 6 weeks | The mean score in the interdental brush group was 0.78 | The mean score in the cleaning stick group was 0.10 (0.32 lower to 0.52 higher) | ‐ | 61 | ⊕⊝⊝⊝ | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 4 to 6 weeks | The mean score in the interdental brush group was 0.14 | The mean score in the cleaning stick group was 0.02 lower (0.10 lower to 0.06 higher) | ‐ | 31 (1 study) | ⊕⊝⊝⊝ | |
| Periodontitis | Two studies measured periodontitis but data not presented or usable | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: investigators measure plaque using different scales Lower score means less plaque Follow‐up: 4 to 6 weeks | The plaque score in the cleaning stick group was on average | ‐ | 92 | ⊕⊝⊝⊝ | ||
| Harms and adverse outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to single study at unclear risk of bias and serious imprecision 2 Downgraded three levels due to single study at unclear risk of bias and imprecision 3 Downgraded three levels due to 2 small studies at unclear risk of bias and serious imprecision | ||||||
Background
Description of the condition
Periodontal diseases
Periodontal diseases are multifactorial oral health conditions (Llorente 2006; Timmerman 2006), consisting of a diverse family of pathological conditions affecting the periodontium (a collective term that comprises gingival tissue, periodontal ligament, cementum and alveolar bone). Periodontal diseases include two main conditions: gingivitis and periodontitis. Gingivitis is the presence of gingival inflammation without loss of connective tissue attachment and appears as red, puffy, shiny gums that bleed easily (Mariotti 1999). Periodontitis is inflammation and destruction of the supportive tissues of teeth and is, by its behaviour, characterised as aggressive or chronic (Armitage 1999). Periodontitis can influence quality of life through psychosocial impacts as a result of negative effects on comfort, function, appearance, and socialisation (Durham 2013; Needleman 2004), and can lead to tooth loss (Broadbent 2011).
Some form of periodontal disease affects the majority of the population, and is found in high‐, middle‐ and low‐income countries (Adult Dental Health Survey 2009; Eke 2012). A 2009 survey in the UK found only 17% of adults had healthy gums; 66% had visible plaque; and of those with plaque, 65% had bleeding gums compared with 33% with no plaque (Adult Dental Health Survey 2009). Whilst more severe forms of periodontal disease, with alveolar bone loss, are much less common, gingivitis is prevalent at all ages and is the most common form of periodontal disease (Mariotti 1999). The exact prevalence of periodontitis is difficult to establish across studies because of non‐standardised criteria, different study population characteristics, different clinical measurements, and the use of partial versus full mouth examinations (Cobb 2009; Savage 2009). Of particular concern are the differing definitions and clinical measurements used (Cobb 2009; Savage 2009). A global workshop organised by the American Academy of Periodontology and the European Federation of Periodonotology took place in 2017 to produce an updated classification scheme for periodontal and peri‐implant diseases (Caton 2018; Chapelle 2018; Papapanou 2018). This has provided "a staging and grading system for periodontitis that is based primarily upon attachment and bone loss and classifies the disease into four stages based on severity (I, II, III or IV) and three grades based on disease susceptibility (A, B or C)" (Dietrich 2019).
The primary aetiological factor in the development of periodontal diseases (and dental caries) is dental plaque (Dalwai 2006; Kuramitsu 2007; Marsh 2006; Periasamy 2009; Selwitz 2007). Dental plaque is a highly organised and specialised biofilm comprising of an intercellular matrix consisting of various micro‐organisms and their by‐products. The bacteria found within dental plaque mutually support each other, using chemical messengers, in a complex and highly evolved community, that protects them from an individual's immune system and chemical agents such as antimicrobial mouth rinses. Bacteria in biofilm are 1000 to 1500 times more resistant to antibiotics than in their free‐floating state, reducing the effectiveness of chemical agents as a solo treatment option. Therefore, disruption of the oral biofilm via mechanical methods remains one of the best treatment options (Chandki 2011). Calcified plaque (calculus) is not involved in the pathogenesis of periodontal diseases but it provides an ideal surface to collect further dental plaque and acts as a 'retention web' for bacteria, protecting plaque from appropriate preventive and therapeutic periodontal measures (Ismail 1994; Lindhe 2003).
Since periodontal diseases are inflammatory, bacterially‐mediated diseases that trigger the host's immune system, it is postulated that the individual's oral health status may influence their systemic health. Susceptibility to periodontal diseases is variable and depends upon the interaction of various risk factors, for example genetic makeup, smoking, stress, immunocompromising diseases, immunosuppressive drugs, and certain systemic diseases (Van Dyke 2005). Studies have shown some possible associations between periodontal diseases and coronary heart disease (Machuca 2012), hyperlipidaemia (Fentoğlu 2012), preterm births (Huck 2011), and lack of glycaemic control in people with diabetes mellitus (Columbo 2012; Simpson 2015). Socioeconomic factors, for instance educational and income levels, have been found to be strongly associated with the prevalence and severity of periodontal diseases (Borrell 2012).
Dental caries
Dental caries is a multifactorial, bacterially‐mediated, chronic disease (Addy 1986; Richardson 1977; Rickard 2004). It is the most common disease in the world (Frencken 2017; WHO 1990), affecting most school‐aged children and the vast majority of adults (Petersen 2003). Although the prevalence and severity of dental caries in most industrialised countries has substantially decreased in the past two decades (Marthaler 1996), this preventable disease continues to be a common public health problem in some parts of these countries (RCSEng 2018), and in other parts of the world (Burt 1998). In 2017, dental caries affected the permanent teeth of 2.3 billion people globally (GHDx 2017).
Deep pits and fissures, as well as interdental spaces, represent areas of increased risk for the collection and accumulation of dental plaque and are therefore regarded as susceptible tooth surfaces for the occurrence of carious lesions. The presence and growth of dental plaque is further encouraged by compromised host response factors, for example reduced salivary flow (hyposalivation) (Murray 1989). Fermentation of sugars by cariogenic bacteria within the plaque results in localised demineralisation of the tooth surface, which may ultimately result in cavity formation (Marsh 2006; Selwitz 2007).
People with carious teeth may experience pain and discomfort (Milsom 2002; Shepherd 1999); and, if left untreated, may lose their teeth. In the United Kingdom, tooth decay accounts for almost half of all dental extractions performed (Chadwick 1999).
Description of the intervention
Although the incidence of periodontal diseases and dental caries differs, based on regional, social, and genetic factors, the prevention of both diseases has a significant healthcare and economic benefit for society as a whole and for individuals. Prevention of dental caries and periodontal diseases is generally regarded as a priority for oral healthcare professionals because it is more cost‐effective than treating it (Brown 2002; Burt 1998). Daily mechanical disruption and removal of dental plaque is considered important for oral health maintenance (Rosing 2006; Zaborskis 2010). Additional professional plaque removal can sometimes be required, though the routine provision of this for people who regularly attend the dentist has recently been questioned (Lamont 2018). People routinely use toothbrushes at home to remove supragingival dental plaque, but toothbrushes are unable to penetrate the interdental area where periodontal diseases first develop and are prevalent (Asadoorian 2006; Berchier 2008; Berglund 1990; Casey 1988). Besides toothbrushing, which is the most common method for removing dental plaque (Addy 1986; Mak 2011; Richardson 1977), different interdental aids to plaque removal, for example, dental floss or interdental brushes, are widely available and often recommended for use in addition to toothbrushing (Bosma 2011; Särner 2010). Whilst floss can be used in all interdental spaces, the interdental brush and other interdental cleaning aids require sufficient interdental space to be used by patients. The choice of interdental cleaning aid will depend on the size of the space and the ability of the patient to use it.
Toothbrushes
Regular daily toothbrushing is a key strategy for preventing and controlling periodontal diseases and dental caries, because it disrupts supragingival dental plaque and reduces the number of periodontal pathogens in supragingival plaque (Caton 2018; Chandki 2011; Ismail 1994; Needleman 2004; Rosing 2006; Zaborskis 2010). In order to achieve highest level of dental plaque removal, various types of toothbrushes have been designed, and different toothbrushing techniques have been developed over time (Lindhe 2003). In an update of a Cochrane systematic review published in 2014 that included 56 randomised controlled trials (RCTs), moderate‐certainty evidence suggested that powered toothbrushes are more effective in reducing plaque and gingivitis than manual toothbrushes in the short and long term, with very few adverse events reported overall and no apparent differences between the two toothbrushing regimens (Yacob 2014). However, the observed likely benefit of powered toothbrushing is of unclear clinical significance, as it reduced dental plaque by 11% after one to three months of use, and by 21% after three months of use. As for clinical signs of gingivitis, there was a reduction of 6% at one month and 11% after three months of use.
Although toothbrushing is effective in removing dental plaque from buccal and lingual tooth surfaces, because of their shape, toothbrushes are not able to penetrate interdental areas and adequately clean interproximal teeth surfaces (Christou 1998). Likewise, toothbrushes are able to reach only 0.9 mm under the gingival margin, and therefore cannot reduce the rate of subgingival areas affected by periodontal pathogens (Waerhaug 1981; Xiemenez‐Fyvie 2000). Interdental plaque accumulates more quickly, is more prevalent, and more acidogenic than plaque on other tooth surfaces (Cumming 1973; Igarashi 1989; Lindhe 2003; Lovdal 1961; Warren 1996). It is important that plaque is controlled in the interdental areas because these are the sites where periodontal diseases occur more frequently, with greater severity (Asadoorian 2006; Berchier 2008; Berglund 1990; Christou 1998; Lindhe 2003; Loe 1965). Caries also occurs more often on the interproximal tooth surfaces (Berglund 1990; Casey 1988; Lindhe 2003).
Dental floss
The concept of interdental cleaning with a filamentous material was first introduced by Levi Spear Parmly, as a measure for preventing dental disease together with a dentifrice and toothbrush (Parmly 1819). Unwaxed silk floss was first produced in 1882, by Codman & Shurtleff, but it was Johnson & Johnson who made silk floss widely available from 1887, as a by‐product of sterile silk leftover from the manufacture of sterile sutures (Johnson & Johnson).
Since dental floss is able to remove some interproximal plaque (Asadoorian 2006; Waerhaug 1981), it is thought that frequent regular dental flossing will reduce the risk of periodontal diseases and interproximal caries (Hujoel 2006). Daily dental flossing in combination with toothbrushing for the prevention of periodontal diseases and caries is frequently recommended for both children and adults (Bagramian 2009; Brothwell 1998). However, patient compliance with daily dental flossing is low (Schuz 2009). People attribute their lack of dental flossing compliance to lack of motivation and difficulties using floss (Asadoorian 2006). A study of a cohort of young people at ages 15, 18, and 26 found that at age 26, only 51% of both females and males believed that using dental floss was important, with females rating flossing more important than males (Broadbent 2006).
Certain organisations, for example the American Dental Association, recommend that children’s teeth are flossed as soon as they have two teeth that touch. However, studies that measure compliance show that few children have their teeth flossed or use floss: a study in West Virginia found that only 21% of children had their teeth flossed (Wiener 2009). When measures are taken to increase compliance, for example using behavioural change techniques, then the proportion of adolescent flossing increases (Gholami 2015).
Interdental brushes
Interdental brushes are small cylindrical or cone‐shaped bristles on a thin wire that may be inserted between the teeth. They have soft nylon filaments aligned at right angles to a central stiffened rod, often twisted stainless steel wire, very similar to a bottle brush. Interdental brushes used for cleaning around implants have coated wire to avoid scratching the implants or causing galvanic shock. They are available in a range of different widths to match the interdental space and their shape can be conical or cylindrical. Most are round in section, although interdental brushes with a more triangular cross‐section can also be found on the market. Originally, interdental brushes were recommended by dental professionals to patients with large embrasure spaces between the teeth (Slot 2008; Waerhaug 1976), caused by the loss of interdental papilla mainly due to periodontal destruction. Patients who had interdental papillae that filled the embrasure space were usually recommended to use dental floss as an interdental cleansing tool. However, with the greater range of interdental brush sizes and cross‐sectional diameters now available, they are considered a potentially suitable alternative to dental floss for patients who have interdental papillae that fill the interdental space (Imai 2011). Daily dental flossing adherence is low because it requires a certain degree of dexterity and motivation (Asadoorian 2006), whereas interdental brushes have been shown as being easier to use and are therefore preferred by patients (Christou 1998; Imai 2010). Furthermore, when compared to dental floss, they are thought to be more effective in plaque removal because the bristles fill the embrasure and are able to deplaque the invaginated areas on the tooth and root surfaces (Bergenholtz 1984; Christou 1998; Imai 2011; Jackson 2006; Kiger 1991; Waerhaug 1976). However, there are conflicting study results regarding the efficacy of interdental brushes in the reduction of clinical parameters of gingival inflammation (Jackson 2006; Noorlin 2007); and whether they are only suitable for patients with moderate to severe attachment loss and open embrasures, or whether they are a suitable aid for healthy patients to prevent gingivitis who have sufficient interdental space to accommodate them (Gjermo 1970; Imai 2011).
Tooth cleaning sticks
Sticks and twigs, composed of bone, ivory, metal, plastic, quills, wood, and other substances, have been used for cleaning tooth surfaces and interdentally since prehistoric times (Christen 2003). The continuing use of hard materials for cleaning interdentally has been questioned (Mandel 1990); however, they continue to be used in different parts of the world. The meswak (or miswak) is one of the most widely used tooth cleaning sticks (Saha 2012); however, it is important to differentiate its use between cleaning tooth surfaces and interdentally (Furuta 2011). Toothpicks continue to be used, particularly in the United States and Scandinavia, predominantly in older age groups (Sarner 2010), whereas dental floss and interdental brushes are more likely to be used by younger people. Toothpicks are commonly used in East Asia such as in China, Korea, and Japan, though the main purpose is to remove food debris in the interdental areas. Interdental rubber tip stimulators, usually consisting of a carrying handle and disposable rubber tip stimulator, are readily available and are designed to stimulate gingival blood flow and remove interdental plaque.
Oral irrigators
Oral irrigation with water under pressure has been available for just over fifty years (Lyle 2012), and the benefits are described as the removal of biofilm from tooth surfaces and bacteria from periodontal pockets. Oral irrigators were first designed to be used supragingivally, using water pressure to displace and remove plaque, relying on pressure to irrigate subgingival regions (Goyal 2012). Since then, various tips have been designed that may be used subgingivally and several manufacturers provide products to do this.
How the intervention might work
Dental plaque‐induced gingivitis and incipient, non‐cavitated carious lesions are reversible (Mariotti 1999; Silverstone 1983). The progression in either disease may be attributed to a change in the environmental equilibrium that favours disease conditions. For example, gingivitis has been shown to be a risk factor in the clinical course of chronic periodontitis (Schatzle 2009); and it is important to treat gingivitis when inflammation is only in the gingival tissues and has not affected other parts of the periodontal system (Mariotti 1999). Early carious lesions can be arrested in the enamel and may or may not progress to the dentine depending on the dynamic equilibrium between demineralisation and remineralisation (Marinho 2003; Marinho 2013; Marinho 2015).
Periodontal diseases
Gingival diseases are classified as one of the periodontal diseases (Armitage 1999; Caton 2018), and are categorised as either dental plaque‐induced diseases or non‐plaque‐induced gingival lesions. Gingival inflammation, gingivitis, induced by dental plaque is an inflammatory response of the gingival tissues caused by bacteria in dental plaque (Page 1986), and characterised by swelling, redness and bleeding on probing. If dental plaque is left in place for more than two weeks, then gingivitis will occur (Loe 1965). The severity of gingivitis can be modified by factors other than plaque (Trombelli 2013).
Periodontal diseases are complex interactions of bacteria and the immune system (Page 2007; Sanz 2011); and dental plaque is the primary aetiological factor (Marsh 2006). Dental plaque may be either supragingival or subgingival and the plaque biofilm comprises different bacterial colonies at the supragingival or subgingival levels. By disrupting the plaque, the main cause of periodontal diseases can be removed. Although there is a lack of RCT evidence for the best approaches to ensuring periodontal health is maintained after treatment for periodontitis (Manresa 2015), a key aspect of supportive periodontal therapy is training in self‐administered mechanical plaque removal techiques, and this is also widely regarded as a crucial part of preventive strategies (Greenwell 2001; Lindhe 2003).
Dental caries
Dental plaque contains many bacterial species that are acidogenic. In 1890, Miller published 'The microorganisms of the human mouth' which postulated that oral bacteria found in plaque were acidogenic, but, as no specific bacteria were implicated, it became known as the "non‐specific plaque hypothesis" (Ring 2002). Later, Loesche 1976 postulated a "specific plaque theory", implicating Streptococcus mutans and Lactobacillus acidophilus as the primary bacteria involved in caries generation. Since then, the importance of the plaque biofilm has been recognised and an “ecological plaque hypothesis” proposed (Marsh 1994).
Acidogenic plaque bacteria utilise dietary sugars to demineralise dental tissues, which may progress into carious tooth lesions. The most susceptible regions of teeth to caries are the occlusal and interdental surfaces (Demirci 2010). Interdental plaque is more prevalent (Lindhe 2003), forms more readily (Igarashi 1989) and is more acidogenic than plaque on other tooth surfaces in the mouth. Therefore, interdental cleaning is often recommended as an adjunctive self care therapy, particularly when caries risk is increased (Sarner 2010; Wright 1977). Removal of dental plaque by mechanical interdental cleaning should reduce the frequency and degree of demineralisation interproximally and lead to decreased caries incidence.
Why it is important to do this review
Effective oral hygiene is a crucial factor in maintaining good oral health, which is, in turn, associated with overall health and health‐related quality of life (McGrath 2002; Sheiham 2005). Poor oral health may affect appearance in terms of stained or missing teeth; can contribute to bad breath (Morita 2001); and negatively influence self confidence, self esteem, and the ability to communicate (Exley 2009). Poor oral health is often accompanied by pain arising from carious lesions, which may lead to discomfort when eating, drinking, and speaking (Dahl 2011). Individuals with high levels of dental plaque, after accounting for sex, socioeconomic status, and dental care attendance frequency, are more likely to experience dental caries and periodontal diseases (Broadbent 2011).
The regular and effective removal of dental plaque by toothbrushing is important for the prevention and successful management of common oral diseases, in conjunction with use of fluoride toothpaste (Walsh 2019). Mechanical interdental cleaning, using either dental floss, interdental brushes, or tooth cleaning sticks, is widely recommended and advertised, but it is unclear whether there is a benefit in using interdental cleaning devices as an adjunct to toothbrushing and if a particular type of interdental cleaning device is superior to others. What the benefits may be for children and adolescents is unknown.
This review, which incorporates and expands previous reviews on flossing (Sambunjak 2011) and interdental brushing (Poklepovic Pericic 2013), was identified as a topic of clinical priority when Cochrane Oral Health undertook a comprehensive prioritisation exercise (Worthington 2015). A systematic review and meta‐analysis, combining the results of randomised controlled trials, will provide health care commissioners, practitioners, and consumers with evidence about the effectiveness of mechanical interdental cleaning at home for oral health.
Objectives
To evaluate the effectiveness of interdental cleaning devices used at home, in addition to toothbrushing, compared with toothbrushing alone, for preventing and controlling periodontal diseases, caries, and plaque. A secondary objective was to compare different interdental cleaning devices with each other.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), including split‐mouth design, cross‐over trials and cluster‐randomised trials, that lasted four weeks or more. We included data from both periods of a cross‐over trial only if there was a washout period of at least two weeks before the cross‐over. Studies were included irrespective of publication status and language.
Types of participants
The review included studies of dentate participants irrespective of age, race, sex, socioeconomic status, geographical location, background exposure to fluoride, initial dental health status, setting, or time of intervention. We excluded studies if the majority of participants had any orthodontic appliances. Likewise, we excluded studies if participants were selected on the basis of special (general or oral) health conditions (for example, severely immunocompromised people), or if the majority of participants had severe periodontal disease.
Types of interventions
We included all trials that compared a combination of toothbrushing and any home‐use mechanical interdental cleaning device with toothbrushing alone, or with another mechanical interdental cleaning device.
We excluded intervention or control groups receiving any additional active agent(s) (i.e. caries‐preventive agents) as part of the study (e.g. chlorhexidine mouthwash, additional fluoride‐based procedures, oral hygiene procedures, xylitol chewing gum), in addition to interdental cleaning procedures or toothbrushing. However, we included studies using floss impregnated with active agents such as chlorhexidine or fluoride. We included studies that involved participants in both groups receiving additional measures as part of their routine oral care, such as oral hygiene advice, supervised brushing, fissure sealants, etc. We excluded studies that compared two variations of the same type of interdental cleaning device.
Types of outcome measures
Primary outcomes
Outcomes did not form part of the inclusion criteria. We included all RCTs of home‐use devices in this review, even if they did not report these outcomes.
-
Gingivitis ‐ assessed by gingival indices and bleeding indices in separate analyses;
-
Periodontitis ‐ assessed by clinical attachment loss and pocket probing depth;
-
Interproximal caries ‐ assessed by (a) progression of caries into enamel or dentine, (b) change in decayed, missing and filled tooth surfaces (D(M)FS) index, (c) radiographic evidence. Studies had to contain explicit criteria for diagnosing dental caries. As caries increment could be reported differently in different trials, we planned to use a set of a priori rules to choose the primary outcome data for analysis from each study (Marinho 2013; see Table 1);
-
Plaque – assessed by plaque scores or indices;
-
Harms and adverse effects.
| As we were aware that caries increment could be reported differently in different trials, we developed a set of a priori rules to choose the primary outcome data (decayed, missing or filled surfaces (D(M)FS)) for analysis from each study, drawing on Marinho 2013: DFS data would be chosen over DMFS data, and these would be chosen over DS or FS; data for 'all surface types combined' would be chosen over data for 'specific types' only; data for 'all erupted and erupting teeth combined' would be chosen over data for 'erupted' only, and these over data for 'erupting' only; data from 'clinical and radiological examinations combined' would be chosen over data from 'clinical' only, and these over 'radiological' only; data for dentinal/cavitated caries lesions would be chosen over data for enamel/non‐cavitated lesions; net caries increment data would be chosen over crude (observed) increment data; and follow‐up nearest to three years (often the one at the end of the treatment period) would be chosen over all other lengths of follow‐up, unless otherwise stated. When no specification was provided with regard to the methods of examination adopted, diagnostic thresholds used, groups of teeth and types of tooth eruption recorded, and approaches for reversals adopted, the primary choices described above were assumed. |
For gingivitis, plaque and adverse effects, we considered outcomes at all time points measured by the included studies except those with a duration of less than one month. We planned to use only data with at least six months' follow‐up for the outcomes of clinical attachment loss, pocket probing depth, and interproximal caries.
Secondary outcomes
-
Halitosis;
-
Patient satisfaction;
-
Cost of intervention.
Search methods for identification of studies
Electronic searches
Cochrane Oral Health’s Information Specialist conducted systematic searches in the following databases for randomised controlled trials and controlled clinical trials. There were no language, publication year, or publication status restrictions:
-
Cochrane Oral Health’s Trials Register (searched 16 January 2019) (see Appendix 1);
-
Cochrane Central Register of Controlled Trials (CENTRAL; 2018, Issue 12) in the Cochrane Library (searched 16 January 2019) (see Appendix 2);
-
MEDLINE Ovid (1946 to 16 January 2019) (see Appendix 3);
-
Embase Ovid (1980 to 16 January 2019) (see Appendix 4);
-
CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature; 1937 to 16 January 2019) (see Appendix 5).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials as described in the Cochrane Handbook for Systematic Reviews of Interventions, Chapter 6 (Lefebvre 2011).
We also initially searched Web of Science Conference Proceedings, but discontinued this search due to a poor yield of studies for inclusion (see Appendix 6 for details of the search strategy).
Searching other resources
The following trial registries were searched for ongoing studies:
-
US National Institutes of Health Trials Register (http://clinicaltrials.gov) (to 16 January 2019) (see Appendix 7);
-
The WHO Clinical Trials Registry Platform (http://apps.who.int/trialsearch/default.aspx) (to 16 January 2019) (see Appendix 8).
We searched the reference lists of included studies and relevant systematic reviews for further studies.
We did not perform a separate search for adverse effects of interventions used; we considered adverse effects described in included studies only.
Data collection and analysis
Selection of studies
Two review authors independently carried out the selection of studies and made decisions about eligibility; one of them a methodologist and the other a topic area specialist. The search was designed to be sensitive and include controlled clinical trials; these were filtered out early in the selection process if they were not randomised. If the relevance of a study report was unclear, we read the full text and resolved disagreements by discussion with other authors.
Data extraction and management
At least two review authors independently extracted data; at least one of them a methodologist and one a topic area specialist. We compared the extracted data and identified disagreements, which we then resolved by consensus.
We extracted and entered the following data into a customised collection form. We had previously designed a data extraction form for a similar review (Sambunjak 2011).
-
Study characteristics: design, including details if a study differed from standard parallel‐group design, e.g. split‐mouth or cross‐over; recruitment period, setting.
-
Participants: number randomised and evaluated (by group); inclusion and exclusion criteria; demographic characteristics of participants: age, sex, country of origin, ethnicity, socioeconomic status, comorbidity, condition‐related health status. We recorded demographic characteristics for the study as a whole and for each intervention group, when available.
-
Intervention and control groups: type of interdental cleaning procedure, including type of toothbrush (powered or manual) and type of toothpaste (with or without fluoride); frequency of interdental cleaning procedure; duration of the intervention period; whether the participants were trained/instructed how to brush interdentally, floss or toothbrush, or a combination of all three, and by whom; length of follow‐up; loss to follow‐up; assessment of adherence; level of fluoride in the water supply.
-
Outcomes: detailed description of the outcomes of interest (both beneficial and adverse), including the definition and timing of measurement; methods of assessment; other outcomes reported in the included studies that were not outcomes of this review (we did not extract results for these outcomes).
-
Data on funding sources if reported.
We intended to enter the data from cross‐over studies, split‐mouth studies, and for the prevented fraction, into RevMan (Review Manager (RevMan)) using the generic inverse variance outcome type.
We extracted both gingival indices and bleeding indices (assessed as bleeding either present or absent on a site) where both were reported. We extracted data from indices assessed on the interproximal sites if available; otherwise we used the indices on the sites reported.
In studies that used both bleeding on probing (BOP) and Eastman Interdental Bleeding Index (EIBI), we included EIBI in the meta‐analyses. The suitability of the EIBI is justified by its reproducibility and high inter‐examiner and intra‐examiner reliability (Blieden 1992).
Assessment of risk of bias in included studies
We assessed the risk of bias in each study using Cochrane's 'Risk of bias' tool as described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The tool addresses seven domains: random sequence generation, allocation sequence concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other issues. For split‐mouth and cross‐over designs, our assessment of risk of bias included additional considerations such as suitability of the design, and risk of carry‐over or spill‐over effects.
At least two review authors, a methodologist and a topic area specialist, independently carried out the assessment of risk of bias. They were not blinded to the names of the authors, institutions, journal or results of a study. We assigned a judgement of low, high or unclear risk of bias for each domain within each included study, recording in the relevant 'Risk of bias' domain the rationale for our judgement. We tested the data collection forms and assessments of the risk of bias on a pilot sample of articles. As protocols were not available for many studies, we compared the outcomes listed in the methods sections in a publication against those results reported to assess selective reporting bias. If some indications of reporting bias were found, we contacted the study authors for clarification. If information was missing from the included reports, we attempted to contact the study investigators to obtain it. If standard deviations were missing and we were unable to estimate these, we assessed selective reporting as having high risk of bias. If a study reported measured adverse effects but did not report findings, we judged it to have unclear risk of selective reporting bias.
If compliance was not assessed in a study, we judged the risk of 'other bias' to be unclear. If compliance was poor, we judged the study to be at high risk of bias. Where a study noted baseline difference, we assumed this to be an imbalance greater than what would be expected by chance and we assessed the risk of 'other bias' as high.
In our assessment of the overall risk of bias in a study, we did not include the domain of performance bias. All studies were at high risk of this because it is not possible to blind study participants to the interventions of interest in an ethical experimental situation. Removing performance bias from consideration, we assessed a study as at high risk of bias if we had judged at least one domain as having high risk of bias, unclear if at least one domain was unclear and none were high, and low if all domains were assessed as being at low risk of bias.
Measures of treatment effect
For gingivitis and plaque outcomes, we expected most measures of treatment effect to be continuous; although these measures are sometimes dichotomous at a site level, they are treated as continuous when averaged over sites within the mouth. We used the mean difference (MD) (or difference in means), or standardised mean difference (SMD) when combining different clinical indices. We calculated the corresponding 95% confidence intervals (CIs) for each result.
We intended to analyse clinical attachment loss and probing pocket depth as continuous measures; however, there were no clinical attachment data.
For caries outcomes, we intended to calculate the prevented fraction (PF), where appropriate. The PF is expressed as the mean increment in the control group minus the mean increment in the intervention group divided by the mean increment in the control group, i.e. the caries increment in the treatment group expressed as a percentage of the control group. There were no caries data reported.
Unit of analysis issues
The units of analysis were individual participants or groups of measuring sites within individual participants (e.g. interproximal sites: proportion of sites that have bleeding averaged over the number of participants). We intended to contact study authors to obtain data in the right form; however, this was not necessary. We intended to analyse split‐mouth, cross‐over and cluster trials taking the clustering into account as described in Chapter 16 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Depending on the interventions being included in multi‐arm studies, we either combined groups (if straightforward), or presented the arms separately (e.g. automated versus manual floss), ensuring that there was no double counting of participants in the control arms.
Dealing with missing data
As described in Table 16.1.a in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), there are several types of missing data in a systematic review or meta‐analysis. The problems of missing studies and outcomes are addressed in the Assessment of reporting biases part of this review. A common problem was missing summary data, such as standard deviations for continuous outcomes. Missing summary data were not a reason to exclude a study from the review and we used the methods outlined in section 16.1.3 of the Cochrane Handbook for Systematic Reviews of Interventions to impute missing standard deviations (Higgins 2011).
For the data judged to be 'missing at random', i.e. their being missing was unrelated to their actual values, we conducted analyses using the available data only. This was the default option for all studies, so it was unnecessary to perform a sensitivity analysis to assess how the changes in assumptions might have affected the results.
Assessment of heterogeneity
Prior to meta‐analysis, we assessed studies for clinical homogeneity with respect to the type of intervention, control group, and outcomes. We did not combine results of clinically heterogeneous studies. For studies judged as clinically homogeneous, we tested for statistical heterogeneity using the Chi² test and I² statistic. We interpreted a Chi² test resulting in a P value less than 0.10 as indicating significant statistical heterogeneity. In order to assess and quantify the possible magnitude of inconsistency (i.e. heterogeneity) across studies, we used the I² statistic, roughly interpreting values under 40% as low or no heterogeneity, values between 40 and 70% as moderate heterogeneity, and values over 70% as substantial.
Assessment of reporting biases
If there had been at least 10 studies included in a meta‐analysis, we would have created a funnel plot of effect estimates against their standard errors to assess a possible between‐study reporting bias. If an asymmetry of the funnel plot had been found either by inspection or statistical tests, we would have considered possible explanations and taken this into account in the interpretation of the overall estimate of treatment effects.
Data synthesis
We undertook meta‐analysis including only studies reporting the same outcomes. When there were a number of different indices measuring the same outcome (either plaque or gingivitis), we used the standardised mean difference (SMD), along with the appropriate 95% CI, to combine the results in meta‐analysis. Meta‐analysis of split‐mouth and cross‐over studies were combined where possible but it is inappropriate to combine these when using SMD. Some studies measured plaque and gingivitis on selected sites and we used indices based on these data if the interproximal site data were not available. We planned to combine risk ratios for binary data. As considerable heterogeneity was expected in the included studies, we undertook a random‐effects model as the primary method of meta‐analysis.
Subgroup analysis and investigation of heterogeneity
We planned the following subgroup analyses. We decided to conduct them if there was heterogeneity (P value < 0.1) and there were at least 10 studies in the meta‐analysis.
-
Age (child, adult) and dentition (primary, permanent).
-
Periodontal status at baseline.
-
Trained (instructed) versus untrained (uninstructed) interdental cleaning.
-
Funded versus unfunded studies.
Sensitivity analysis
The primary meta‐analyses included all eligible studies irrespective of their risk of bias. We intended to conduct sensitivity analyses by excluding studies:
-
at high risk of bias (excluding participant blinding from this overall study‐level assessment of risk of bias);
-
with estimated standard deviations;
-
using split‐mouth and cross‐over designs.
Summarising findings and assessing the certainty of the evidence
We adopted the GRADE system for evaluating the certainty of the evidence of systematic reviews (Guyatt 2008; Guyatt 2008a; Higgins 2011), and used it to construct 'Summary of findings' tables for the main comparisons and key outcomes: gingivitis, periodontitis, interproximal caries, plaque, adverse events (harms). We assessed the certainty of the body of evidence with reference to the overall risk of bias of the included studies (excluding performance bias), directness of the evidence, consistency of the results, precision of the estimates and the risk of publication bias. We classified the certainty of the body of evidence into four categories: high, moderate, low, and very low.
Summary of findings and assessment of the certainty of the evidence
Results
Description of studies
Results of the search
We retrieved a total of 10,203 references from electronic searches. After finding and deleting duplicates, we had 4733 references, which consisted of titles with or without abstracts. Four authors independently screened the titles and abstracts against the inclusion criteria for the review and discarded 4597 references. We identified two additional studies from screening reference lists. We obtained full‐text copies of the 138 references and four authors considered them independently. Following this, we rejected 42 records, listed 59 records as excluded studies and one as awaiting classification. We included 36 articles (see Included studies and Excluded studies). Thus, our total was 35 included studies (36 articles). Figure 1 shows the flow of studies.
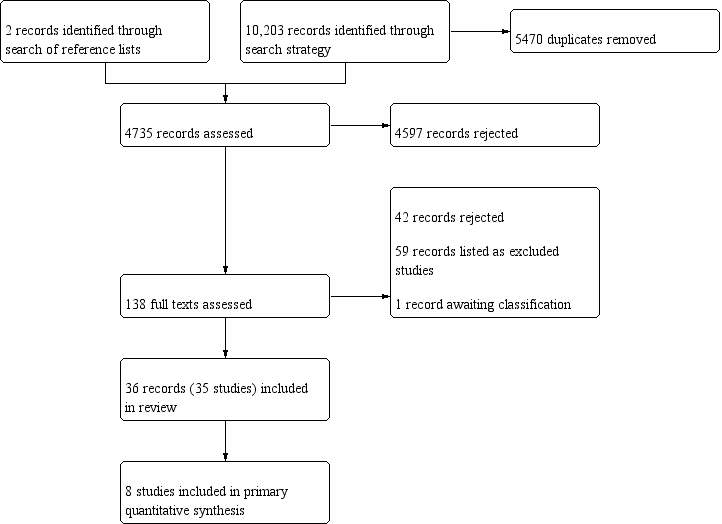
Study flow diagram
Included studies
Thirty‐five studies met the inclusion criteria for this review (see Characteristics of included studies).
Design
Three studies used a split‐mouth design (Christou 1998; Imai 2011; Ishak 2007). Gordon 1996 was a cross‐over study; however, the second period was used to measure preference, with no clinical data measured. We therefore used the data from the first period only, treating it as a parallel‐group study. We also used first‐period data only from Hague 2007 as, although it was described as a cross‐over study, the same control group was used throughout. The remaining studies were of parallel design.
Sample sizes
The studies randomised a total of 3929 participants, with individual study sample sizes ranging between 18 (Ishak 2007) and 362 (Bauroth 2003) participants. The studies evaluated approximately 3734 participants (some studies did not state the number of analysed participants), but we did not include all study arms in the review. The largest number of participants included in a single meta‐analysis was 585 (eight studies).
Setting
Twenty‐three studies were conducted in the USA; three in the Netherlands (Christou 1998; Rosema 2008; Rosema 2011); two in Canada (Goyal 2012; Imai 2011); one in Germany (Zimmer 2006); two in the UK (Ishak 2007; Jackson 2006); one in Italy (Graziani 2017); and one in Guatemala (NCT00855933). Cronin 1997 and Cronin 2005 did not report location. All the the studies that reported location were conducted in high‐income countries so we have no known data from low‐ and middle‐income countries.
Eighteen studies were conducted in an academic setting and one was conducted in a private practice dental centre (Lobene 1982). The other studies did not mention the type of setting.
Thirty‐one studies were single‐centre; four studies did not state how many centres were involved (Bauroth 2003; Biesbrock 2007; Cronin 1997; Cronin 2005).
Participants
Age and sex
No included studies were conducted with children or adolescents. In the studies reporting the age of participants, ages ranged between 18 and 78 years; 21 studies reported the mean age, which ranged from 20 to 53 years. Most studies included both males and females (two did not say, but inclusion criteria implied both were included). Twelve studies did not report the ratio of males to females. In the other studies, the proportion of males to females, in percentage, ranged from 7/53 to 60/40 (11% to 60% males). Zimmer 2006 included equal numbers of males and females. Twenty studies reported including more females than males, and more males than females were reported in three studies (Christou 1998; Goyal 2012; Schiff 2006).
Periodontal status at baseline
The studies predate the new periodontal classification system agreed at the 2017 World Workshop on the Classification of Periodontal and Peri‐implant Diseases and Conditions (Caton 2018; Chapelle 2018; Papapanou 2018). In general, it was difficult to classify and categorise participant periodontal status at baseline because insufficient information was provided by the studies.
In Christou 1998, all participants had moderate to severe periodontitis. Jackson 2006 included people with moderate periodontitis (at least one shallow pocket or at least one deep pocket > 6 mm in 4 of 6 sextants).
Smith 1988 reported that all participants were patients with periodontitis on maintenance programmes, and Walsh 1985 included participants with generalisable interproximal gingival bleeding in 25% of sites exhibiting PDs at least 4 mm or more, suggesting periodontitis; however, neither of these two studies provided a clear definition of the stage of the disease.
Two studies explicitly described that they included mixed diagnoses: Ishak 2007 stated that participants had been diagnosed with gingivitis or moderate periodontitis, and Lewis 2004 stated that included participants had either gingivitis or slight chronic periodontitis (chronic gingival inflammation with pocket depth (PD) ≥ 4 mm and clinical attachment loss ≥ 2 mm).
Participants in Graziani 2017 did not have periodontitis; they were described "periodontally healthy", defined as "absence of proximal attachment loss of > 3 mm in > 2 adjacent teeth". Graziani 2017 provided measurements of clinical attachment loss (CAL), pocket depth (PD), and inflammation to confirm this designation.
Meklas 1972 and Vogel 1975 included dental students with no information regarding their baseline oral status.
All other studies reported bleeding measurements of different values, suggesting various levels of inflammation of marginal periodontal tissues. The mean values, when presented, tended to be low, but because ranges were not usually provided, nor any further data (clinical scores, e.g. CAL, PD), periodontitis among these participants could not be ruled out.
Details per study are presented in Characteristics of included studies and Additional tables. In summary, most studies included participants with slight to moderate periodontal diseases, with the majority of studies excluding advanced periodontal diseases, such as severe periodontitis.
Smoking status
Twenty‐four studies did not report the smoking status of participants, including one that recorded smoking but did not report it (Zimmer 2006). Eight studies reported the percentage of participants who smoked: Bauroth 2003 (75%), Graziani 2017 (57%), Hague 2007 (8%), Jackson 2006 (38%), Lewis 2004 (10%), Rosema 2008 (11%), Sharma 2002 (25%) and Yost 2006 (10%). Three studies consisted only of non‐smokers (Goyal 2012; Ishak 2007; Mwatha 2017).
Socioeconomic status
None of the included studies reported the participants' socioeconomic status.
Interventions
Toothbrushing was undertaken by all participants in all studies. The participants in 33 of the 35 studies used a manual toothbrush; in Goyal 2012, participants used a sonic toothbrush and in Biesbrock 2007, participants used a powered toothbrush. The studies evaluated the use of floss (automated or manual), interdental brush, tooth cleaning stick ‐ wooden or rubber (manual or electric), and oral irrigation to remove plaque from the teeth.
The number of study arms varied from two to six; the number of arms used in our analyses varied from two to four. See Table 2. For Lobene 1982, we combined waxed, unwaxed, and minted floss arms. Comparisons evaluated in the studies are presented in the table below.
| Parallel studies | Number of study arms | Number used in review analyses |
| Graziani 2017 | 4 | 4 |
| Lobene 1982 | 4 | 4 |
| Smith 1988 | 4 | 4 |
| Finkelstein 1990* | 5 | 3 |
| Jared 2005 | 5 | 3 |
| Vogel 1975 | 4 | 3 |
| Yost 2006 | 4 | 3 |
| Barnes 2005 | 3 | 3 |
| Hague 2007 | 3 | 3 |
| Walsh 1985 | 3 | 3 |
| Biesbrock 2007 | 6 | 2 |
| Goyal 2012 | 4 | 2 |
| Mwatha 2017 | 4 | 2 |
| NCT01250769 | 4 | 2 |
| Walsh 1989 | 4 | 2 |
| Zimmer 2006 | 4 | 2 |
| Bauroth 2003 | 3 | 2 |
| Cronin 2005 | 3 | 2 |
| Rosema 2008 | 3 | 2 |
| Rosema 2011 | 3 | 2 |
| Schiff 2006 | 3 | 2 |
| Sharma 2002 | 3 | 2 |
| Cronin 1997 | 2 | 2 |
| Frascella 2000 | 2 | 2 |
| Gordon 1996 | 2 | 2 |
| Isaacs 1999 | 2 | 2 |
| Jackson 2006 | 2 | 2 |
| Kazmierczak 1994 | 2 | 2 |
| Lewis 2004* | 2 | 2 |
| Meklas 1972 | 2 | 2 |
| NCT00855933 | 2 | 2 |
| Yankell 2002 | 2 | 2 |
| Split‐mouth studies | Number of study arms | Number used in review analyses |
| Imai 2011 | 3 | 3 |
| Christou 1998 | 2 | 2 |
| Ishak 2007 | 2 | 2 |
*No data used
| Interdental cleaning device | Toothbrushing only | Floss | Interdental brush |
| Floss | 15 studies: Bauroth 2003; Biesbrock 2007; Finkelstein 1990; Graziani 2017; Hague 2007; Jared 2005; Lobene 1982; Mwatha 2017; NCT00855933; Rosema 2008; Schiff 2006; Sharma 2002; Vogel 1975; Walsh 1985; Zimmer 2006 | ‐ | ‐ |
| Interdental brush | 2 studies: Graziani 2017; Jared 2005 | 9 studies: Christou 1998; Graziani 2017; Imai 2011; Ishak 2007; Jackson 2006; Jared 2005; Smith 1988; Yankell 2002; Yost 2006 | ‐ |
| Wooden tooth cleaning sticks | 2 studies: Finkelstein 1990; Walsh 1985 | 3 studies: Finkelstein 1990; Lewis 2004; Walsh 1985 | ‐ |
| Rubber/elastomeric tooth cleaning sticks | 2 studies: Graziani 2017; Vogel 1975 | 9 studies: Cronin 1997; Cronin 2005; Gordon 1996; Graziani 2017; Isaacs 1999; Kazmierczak 1994; Smith 1988; Vogel 1975; Yost 2006 | 3 studies: Graziani 2017; Smith 1988; Yost 2006 |
| Oral irrigation | 5 studies: Frascella 2000; Goyal 2012; Meklas 1972; NCT01250769; Walsh 1989 | 2 studies: Barnes 2005; Rosema 2011 | ‐ |
Training
No specific instructions were given for the use of any of the distributed oral hygiene materials in one study (Yankell 2002), where only one brush size was used. There was no information about training in NCT00855933 and NCT01250769. In all remaining studies, participants were provided with detailed instructions on the use of the assigned product. There was often detailed information on the size of the brushes to be used, and how this was determined for each individual participant (see Characteristics of included studies).
Outcomes
Tooth sites
Twenty‐three studies provided data for the interproximal sites only (Bauroth 2003; Christou 1998; Cronin 1997; Cronin 2005; Gordon 1996; Graziani 2017; Hague 2007; Imai 2011; Isaacs 1999; Ishak 2007; Jackson 2006; Jared 2005; Kazmierczak 1994; Lewis 2004 ; Schiff 2006; Sharma 2002; Smith 1988; Vogel 1975; Yankell 2002; Yost 2006; Zimmer 2006). Goyal 2012 provided data from interproximal sites only for plaque, and from mixed sites for gingivitis. Finkelstein 1990 used interproximal sites for gingivitis and other for plaque. We were unable to use the data for Finkelstein 1990, Lewis 2004 or Smith 1988. The remaining studies only presented the indices measured on mixed sites, including the interproximal sites.
Gingivitis
Seventeen studies used more than one gingivitis index.
The most commonly used index was the Löe & Silness Gingival Index (LSGI) or a modification of it (14 studies: Barnes 2005; Biesbrock 2007; Cronin 1997; Cronin 2005; Finkelstein 1990; Hague 2007; Isaacs 1999; Lobene 1982; Schiff 2006; Smith 1988; Vogel 1975; Walsh 1989; Yost 2006). Seven studies used the Lobene Modified Interproximal Gingival Index (Bauroth 2003; Gordon 1996; Goyal 2012; Jared 2005; Mwatha 2017; Sharma 2002; Yankell 2002). Six studies used the Eastman Interdental Bleeding Index (Finkelstein 1990; Imai 2011; Jackson 2006; Lewis 2004; Yankell 2002; Yost 2006). Two studies used each of the Bleeding Index (Bauroth 2003; Kazmierczak 1994); the Lobene Modified Gingival Index (Kazmierczak 1994; NCT00855933); the Papillary Bleeding Index (Gordon 1996; Zimmer 2006); the Gingival Bleeding Index (Mwatha 2017; NCT01250769); and the Bleeding on Marginal Probing Index (Rosema 2008; Rosema 2011);
One study used each of the following: Carter & Barnes Bleeding Index (Barnes 2005); Löe & Silness Bleeding scores (when scoring 2 or 3 on the LSGI) (Cronin 2005); modified gingival index (Frascella 2000); angular bleeding index (Frascella 2000); Full Mouth Bleeding Score (Graziani 2017); Angulated Bleeding Index (Graziani 2017); Bleeding on Probing Index (Ishak 2007); Relative Interdental Papillae Level (mm) (Jackson 2006); Pocket Depth (mm) (Jackson 2006), bleeding on probing (Jackson 2006; Walsh 1989), Bleeding on probing (Van der Weijden modification) (+/‐) (Jared 2005), and one study used bleeding on probing assessed by using Angulated Bleeding Index (0/1) and Periodontal Pocket Bleeding Index and probing depth (mm) assessed using a force controlled probe (Christou 1998); Russell modified Periodontal Index (Meklas 1972); Ainamo & Bay Gingival Bleeding Index (Sharma 2002); Interproximal Bleeding on Probing Index (0/1) evaluated as percentage of bleeding interproximal surfaces (Walsh 1985); and Intracrevicular exudate sampling (Vogel 1975).
Plaque
Most studies used one plaque index. Lewis 2004 and Zimmer 2006 used more than one plaque index, while NCT00855933 and NCT01250769 did not measure plaque.
The index used most often was the Quigley‐Hein Plaque Index or a modification of it. This was used in 15 studies: original (Zimmer 2006); Turesky modification (Bauroth 2003; Cronin 1997; Hague 2007; Isaacs 1999; Jared 2005; Kazmierczak 1994; Lobene 1982; Rosema 2011; Schiff 2006; Sharma 2002; Yankell 2002); Turesky‐Gilmore‐Glickman modification (Frascella 2000); Volpe modification (Christou 1998); Benson modification (Yost 2006); and Paraskevas modification (Rosema 2008).
The Silness & Löe Plaque Index was used in five studies (Imai 2011; Jackson 2006; Smith 1988; Walsh 1985; Walsh 1989), and the Proximal/Marginal Plaque Index or a modification of it was used in four studies (Barnes 2005; Cronin 2005; Gordon 1996; Zimmer 2006). The Navy Plaque Index (Rustogi modification) was used in three studies (Biesbrock 2007; Goyal 2012; Mwatha 2017).
One study used each of the Global Plaque Index (Finkelstein 1990); Full Mouth Plaque Score (Graziani 2017); supra‐ and subgingival plaque examined using dental floss, with visible plaque deposits scored positive (Ishak 2007); O'Leary Plaque Index and Interproximal Plaque Index (Lewis 2004); a 3‐point plaque index (Meklas 1972); Podchladley's Total Plaque Index (Vogel 1975); and Modified Proximal Plaque Index (Zimmer 2006).
The indices used for gingivitis and plaque in each study are listed in Table 3, and in more detail in the Characteristics of included studies tables.
| Study | Gingivitis index (scale) | Plaque index (scale) |
| Löe & Silness Gingival Index (0 to 3) Carter & Barnes Bleeding Index (0/1) | Proximal/Marginal Plaque Index (0‐5) | |
| Lobene Modified Interproximal Gingival Index (0 to 4) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index (0 to 3) | Navy Plaque Index (Rustogi modification) (0 /1) | |
| Bleeding on probing assessed by using Angulated Bleeding Index (0/1) and Periodontal Pocket Bleeding Index (0/1) | Volpe modification of Quigley and Hein Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index (0 to 3) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index (0 to 3) Löe & Silness Bleeding scores (when scoring 2 or 3 on the Löe & Silness Gingival Index) | Proximal/Marginal Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index modified to include visual assessment only (0 to 3) Eastman Interdental Bleeding Index (0/1) | Global Plaque Index (0 to 100%) | |
| Modified gingival index Angular bleeding index | Turesky‐Gilmore‐Glickman modification of the Quigley‐Hein Plaque Index | |
| Lobene Modified Gingival Index (0 to 4) Papillary Bleeding Index (0/1) | Proximal/Marginal Plaque Index (0 to 5) | |
| Lobene Modified Gingival Index (0 to 4) | Navy Plaque Index (Rustogi modification) (0/1 for each of the 9 tooth surfaces) | |
| Full Mouth Bleeding Score (0/1) Angulated Bleeding Index (0/1) | Full Mouth Plaque Score (percentage of areas containing plaque) | |
| Löe & Silness Gingival Index (0 to 3) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Eastman Interdental Bleeding Index (0/1) | Silness & Löe Plaque Index (0 to 3) (modified) | |
| Löe & Silness Gingival Index (0 to 3) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Bleeding on Probing Index (0/1) | Visible plaque deposits were scored as positive | |
| Eastman Interdental Bleeding Index (0/1) Bleeding on probing (0/1) Relative Interdental Papillae Level (mm) | Silness & Löe Plaque Index (0 to 3) | |
| Lobene Modified Gingival Index (0 to 4) Bleeding on probing (Van der Weijden modification) (+/‐) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Lobene Modified Gingival Index (0 to 4) Bleeding Index (0/1) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Eastman Interdental Bleeding Index (0/1) | O'Leary Plaque Index (0/1) Interproximal Plaque Index (0/1) | |
| Löe & Silness Gingival Index (0 to 3) | Quigley‐Hein Plaque Index (0 to 5) | |
| Russell modified Periodontal Index (0 to 2) | 3‐point plaque index (0 to 2) | |
| Lobene Modified Gingival Index (0 to 4) Gingival Bleeding Index (0/1) | Navy Plaque Index (Rustogi modification) (0/1 for each of the nine tooth surfaces) | |
| Lobene Modified Gingival Index (0 to 4) | ‐ | |
| Modified Gingival Index (0 to 4) Gingival Bleeding Index (0 to 3) | ‐ | |
| Bleeding on Marginal Probing Index (0 to 2) | Paraskevas modification of Quigley & Hein Plaque Index (0 to 5) | |
| Bleeding on Marginal Probing Index (0 to 2) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index (0 to 3) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Lobene Modified Gingival Index (0 to 4) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index (0 to 3) | Silness & Löe Plaque Index (0 to 3) | |
| Löe & Silness Gingival Index (0 to 3) Intracrevicular exudate sampling | Podchladley's Total Plaque Index (0/1) | |
| Interproximal Bleeding on Probing Index (0/1) evaluated as percentage of bleeding interproximal surfaces | Silness & Löe Plaque Index (evaluated as percentage of interproximal surfaces scored positive for plaque) (0/1) | |
| Löe & Silness Gingival Index (0 to 3) Bleeding on probing | Silness & Löe Plaque Index (0 to 3) | |
| Eastman Interdental Bleeding Index (0/1) Lobene Modified Gingival Index (0 to 4) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Eastman Interdental Bleeding Index (0/1) Löe & Silness Gingival Index (0 to 3) | Benson modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Papillary Bleeding Index (1 to 4) | Quigley & Hein Plaque Index (0 to 5) Modified Proximal Plaque Index |
Periodontitis
Six studies measured probing pocket depth (PPD) in mm (Christou 1998; Graziani 2017; Ishak 2007; Jackson 2006; Smith 1988; Walsh 1989), most of which assessed interdental brushes versus floss. Five studies measured PPD at four to six weeks, with Smith 1988 also measuring at eight weeks, and Jackson 2006 at 12 weeks. Walsh 1989 measured at three months and six months, though were unable to use data at six months as participants received professional scale and polish after three months. We were unable to use the data from Smith 1988 and no data were reported from Graziani 2017.
Walsh 1989 also measured attachment loss but did not report results numerically.
Interproximal caries
None of the studies assessed this outcome.
Adverse effects
Adverse effects were measured by self report in five studies: questionnaire in Christou 1998, Ishak 2007 and Jared 2005, and adherence diary in Mwatha 2017 and Yost 2006. They were assessed by an examiner in 17 studies (Bauroth 2003; Biesbrock 2007; Cronin 1997; Cronin 2005; Frascella 2000; Gordon 1996; Goyal 2012; Hague 2007; Imai 2011; Isaacs 1999; Kazmierczak 1994; Meklas 1972; Mwatha 2017; Rosema 2008; Sharma 2002; Walsh 1989; Yost 2006; Zimmer 2006). NCT01250769 measured adverse events systematically but did not specify the method. Four of these studies failed to report their findings in the Results (Bauroth 2003; Jared 2005; Kazmierczak 1994; Yost 2006).
An additional seven studies that had not described how they would measure adverse effects, simply reported that there were no adverse effects (or no adverse effects related to treatment) (Barnes 2005; Frascella 2000; Jackson 2006; NCT00855933; Rosema 2011; Schiff 2006; Yankell 2002).
Seven studies did not mention anything about adverse events (Finkelstein 1990; Graziani 2017; Lewis 2004; Lobene 1982; Smith 1988; Vogel 1975; Walsh 1985).
Halitosis
None of the studies assessed this outcome.
Patient satisfaction
None of the studies assessed this outcome.
Cost of intervention
None of the studies assessed this outcome.
Timing of outcome measurement
Outcomes were most commonly measured in the short term. We did not consider measurements at less than four weeks (Barnes 2005; Goyal 2012; Graziani 2017; Hague 2007; Jared 2005; Kazmierczak 1994; Lewis 2004; Lobene 1982; Meklas 1972; Mwatha 2017; NCT01250769; Rosema 2011; Vogel 1975; Yankell 2002). Most studies measured at one month (Barnes 2005; Biesbrock 2007; Cronin 1997; Cronin 2005; Frascella 2000; Gordon 1996; Goyal 2012; Graziani 2017; Hague 2007; Ishak 2007; Jared 2005; Lobene 1982; Mwatha 2017; NCT00855933; NCT01250769; Rosema 2011; Smith 1988; Vogel 1975; Yankell 2002; Zimmer 2006) or six weeks (Christou 1998; Finkelstein 1990; Imai 2011; Jackson 2006; Kazmierczak 1994; Lewis 2004; Yost 2006). Five studies also measured at two months (Biesbrock 2007; Frascella 2000; Lobene 1982; Smith 1988; Zimmer 2006).
Twelve studies measured medium‐term outcomes: at 10 weeks (Rosema 2008) or three months (Bauroth 2003; Finkelstein 1990; Imai 2011; Isaacs 1999; Jackson 2006; Lewis 2004; Schiff 2006; Sharma 2002; Walsh 1985; Walsh 1989). Meklas 1972 measured at six time points within six months. Six studies also measured outcomes at six months (Bauroth 2003; Isaacs 1999; Rosema 2008; Schiff 2006; Sharma 2002; Walsh 1989) and nine months (Rosema 2008).
No studies measured outcomes in the long term.
We used outcomes from four to six weeks, three months and six months in our analyses.
Data considerations for exploration of heterogeneity
We did not explore heterogeneity through formal subgroup analyses due to there being fewer than 10 studies in all meta‐analyses. Informal analyses did not explain heterogeneity in the analyses.
Age and dentition
For age and dentition, none of the studies were conducted with children or on the deciduous dentition.
Baseline periodontal status
As explained above, it was difficult to categorise the periodontal disease status of participants in the included studies as they did not describe the baseline periodontal status of participants in terms of either the 1999 or 2017 classifications of periodontal diseases (Armitage 1999; Caton 2018), and many of the studies did not provide sufficient detail for the review authors to make that judgement.
Training
Most studies provided some type of training. Eighteen studies used supervised instruction (51%), but there were insufficient studies in any one meta‐analysis to make subgroup analyses meaningful.
Funding
Most studies were funded through manufacturers or grant awards. Details are given in Table 4. Eight studies did not report on funding (Gordon 1996; Imai 2011; Kazmierczak 1994; Lobene 1982; Sharma 2002; Smith 1988; Vogel 1975; Walsh 1985).
| Cronin 1997 and Isaacs 1999 were supported by Braun AG, Germany (Braun Oral‐B Interclean ID2); Yankell 2002 by Dental Concepts, Paramus, USA (oral hygiene devices); Jackson 2006 and Schiff 2006 by the Colgate Palmolive Company (toothbrushes, floss and toothpaste); Meklas 1972 by the General Electric Company (Aqua Pulse Oral Irrigator); Zimmer 2006 and Ishak 2007 by GlaxoSmithKline (manual toothbrush and floss); Finkelstein 1990 by Johnson & Johnson (waxed floss); Cronin 2005 by Oral‐B (manual toothbrush and flosser); Biesbrock 2007; NCT00855933 and Rosema 2008 by Procter and Gamble (sponsorship) (DE International supplied the toothpaste for Rosema 2008); Yost 2006 and Jared 2005 by Sunstar Inc. (GUM, manual toothbrush); Barnes 2005, Goyal 2012 and Rosema 2011 by Waterpik Inc., Fort Collins, USA (oral irrigator); Hague 2007 by William Getgey Company (ultra‐flosser); and NCT01250769 was sponsored by Philips Oral Healthcare. Walsh 1989 was partially funded by Xouth, Inc, Lancaster, PA, USA. In Bauroth 2003, the authors were affiliated to industry, Pfizer; in Frascella 2000, the authors were affiliated to Braun and Procter and Gamble; and in Mwatha 2017, the authors AM, MO, SS, MW and WJ were employees of Philips (Sonicare Toothbrush). The Italian Ministry of Health and Tuscan region provided a grant to Graziani 2017; the State Scholarship Foundation of Greece grant‐aided Christou 1998 (Entra‐Lactona BV provided brushes and interdental brushes); a University of Tennessee College of Dentistry Alumni Grant was given to Lewis 2004. |
We categorised 24 studies as industry funded (69%), but there were not enough studies in any one meta‐analysis to justify subgroup analysis.
Sensitivity analysis
To assess the robustness of the findings, we conducted sensitivity analyses, as planned, by removing the studies at overall high risk of bias (which did not take into account performance bias, which cannot be avoided in these type of studies), by removing studies with estimated standard deviations, and by removing split‐mouth studies when these had been combined with parallel‐group studies in meta‐analysis (see Table 5). We judged these not to undermine the findings of our main analyses, which are presented in the Effects of interventions section below. It was not necessary to conduct sensitivity analysis removing cross‐over studies as we used only first‐period data from cross‐over studies included in this review.
| Analysis | Studies removed (and reason) | Result | Consistency with main analysis |
| Comparison 1: floss plus toothbrushing versus toothbrushing only | |||
| 1.1 GI at 1 month | Vogel (high risk of bias relating to poor compliance; estimated standard deviations) | SMD ‐0.61, 95% CI ‐1.19 to ‐0.03; high heterogeneity (I2 = 90%; P value < 0.001); 7 studies, 573 participants | Essentially the same |
| 1.2 GI at 3 months | Barouth (high risk of attrition bias; use of negative control rinse) | SMD ‐0.30, 95% CI ‐0.62 to 0.02; no heterogeneity (I2 = 0%; P value = 0.81); 2 studies, 151 participants | Confidence interval is larger and includes possibility of floss providing no additional benefit over toothbrushing |
| 1.3 GI at 6 months | Barouth (high risk of attrition bias and use of negative control rinse) | SMD ‐0.55, 95% CI ‐0.91 to ‐0.18; no/low heterogeneity (I2 = 21%; P value = 0.26); 2 studies, 151 participants | Slightly lower estimate, with larger confidence interval |
| 1.5 Bleeding at 3 months | Barouth (high risk of attrition bias; use of negative control rinse) | MD ‐0.26, 95% CI ‐0.36 to ‐0.16; 1 study, 24 participants | Shows clear benefit for floss (main analysis is equivocal) |
| 1.8 Plaque at 3 months | Barouth (high risk of attrition bias; use of negative control rinse) and | SMD ‐0.13, 95% CI ‐0.43 to 0.17; no heterogeneity (I2 = 0%; P value = 0.49); 3 studies, 175 participants | Slightly lower estimate, with wider confidence interval that includes the possibility of no difference or slight benefit for toothbrushing only |
| 1.9 Plaque at 6 months | Barouth (high risk of attrition bias; use of negative control rinse) | MD ‐0.02, ‐0.11 to 0.07; 1 study, 74 participants | Essentially the same |
| Comparison 6: interdental brush plus toothbrushing versus floss plus toothbrushing | |||
| 6.1 GI at 1 month | Yost (estimated standard deviations) | SMD ‐0.51, 95% CI ‐0.87 to ‐0.15; no/low heterogeneity (I2 = 0%, P value = 0.56); 2 studies, 121 participants | Slightly larger effect, marginally wider confidence interval |
| 6.2 Bleeding at 4 to 6 weeks | Christou, Imai, Ishak (split‐mouth studies) | MD ‐0.10, 95% CI ‐0.15 to ‐0.05; no heterogeneity (I2 = 0%, P value = 0.78); 3 studies, 169 participants | Essentially the same |
| 6.3 Bleeding at 3 months | Imai (split‐mouth study) | MD ‐0.06, 95% CI ‐0.12 to 0.00; 1 study, 77 participants | Essentially the same, though confidence interval includes zero |
| 6.4 Plaque at 1 month | Yost (estimated standard deviations) | SMD ‐0.55, 95% CI ‐1.00 to ‐0.11; moderate heterogeneity (I2 = 62%, P value = 0.05); 4 studies, 228 participants | Essentially the same |
| 6.8 Plaque at 3 months | Imai (split‐mouth study) | MD ‐0.24, 95% CI ‐0.41 to ‐0.07; 1 study, 77 participants | Shows clear benefit for interdental brush (main analysis is equivocal) |
| Comparison 9: rubber/elastomeric cleaning stick plus toothbrushing versus floss plus toothbrushing | |||
| 9.1 GI at 1 month | Vogel (high risk of bias relating to poor compliance; estimated standard deviations) Yost (estimated standard deviations) | SMD ‐0.37, 95% CI ‐1.07 to 0.34; high heterogeneity (I2 = 80%, P value < 0.002); 4 studies, 183 participants | Slightly bigger point estimate but wider confidence interval; both analyses include all possibilities, i.e. that flossing is better or that it gives no benefit or that it is worse than toothbrushing only |
| 9.5 Plaque at 1 month | Yost (estimated standard deviations) | SMD ‐0.09, 95% CI ‐0.57 to 0.39; high heterogeneity (I2 = 65%, P value = 0.02); 5 studies, 212 participants | Essentially the same |
| Comparison 11: interdental cleaning stick plus toothbrushing versus interdental brush plus toothbrushing | |||
| 11.3 Plaque at 1 month | Yost (estimated standard deviations) | MD 0.01, 95% CI ‐0.08 to 0.09; 1 study, 31 participants | Essentially the same |
CI: confidence interval
GI: gingivitis index
MD: mean difference
SMD: standardised mean difference
Excluded studies
After having screened 138 full texts of the studies, we rejected 42 outright, and explained the reasons for our decision in the case of 59 records. These reasons are presented in the Characteristics of excluded studies tables.
Risk of bias in included studies
Allocation
Only four studies were at low risk of selection bias (Frascella 2000; Graziani 2017; Imai 2011; Zimmer 2006).
Random sequence generation
Ten studies adequately generated the allocation sequence (Frascella 2000; Gordon 1996; Graziani 2017; Hague 2007; Imai 2011; Ishak 2007; Jackson 2006; Lewis 2004; Rosema 2008; Rosema 2011; Zimmer 2006). The rest were unclear as the reports did not provide any details of how the randomisation was performed.
Allocation concealment
Five studies adequately concealed allocation (Christou 1998; Frascella 2000; Graziani 2017; Imai 2011; Zimmer 2006). The rest were unclear as reports did not mention any attempt to conceal allocation.
Blinding
Performance bias
We assessed all included studies as being at high risk of bias as participants were not described as blinded, and would not have been blinded if they had consented to participate in the study.
Detection bias
We assessed 22 studies as being at low risk of bias as examiners did not know which group participants had been allocated to.
We did not assess any of the studies as being at high risk of detection bias; however, we considered 13 studies to be unclear as there was either no specific report on how the blinding of outcome assessors was carried out or blinding of outcome assessors was not mentioned (Barnes 2005; Finkelstein 1990; Gordon 1996; Isaacs 1999; Kazmierczak 1994; Meklas 1972; Mwatha 2017; NCT00855933; NCT01250769; Smith 1988; Vogel 1975; Yankell 2002; Yost 2006).
Incomplete outcome data
We assessed 24 studies as being at low risk of bias. We judged 10 studies to be unclear (Christou 1998; Frascella 2000; Isaacs 1999; Kazmierczak 1994; Lewis 2004; Lobene 1982; Meklas 1972; Smith 1988; Vogel 1975; Walsh 1989). We considered Bauroth 2003 to be at high risk of attrition bias as participants were excluded from analysis based on poor compliance, and the numbers per group were not reported.
Selective reporting
We judged 24 studies to be at low risk of outcome reporting bias as they reported their planned or expected outcomes (Barnes 2005; Christou 1998; Cronin 1997; Cronin 2005; Frascella 2000; Gordon 1996; Goyal 2012; Graziani 2017; Hague 2007; Imai 2011; Isaacs 1999; Ishak 2007; Jackson 2006; Lobene 1982; Meklas 1972; Mwatha 2017; NCT00855933; NCT01250769; Rosema 2008; Rosema 2011; Schiff 2006; Walsh 1989; Yankell 2002; Zimmer 2006).
Where studies mentioned adverse effects in their Methods section but did not report any findings, we judged the risk of reporting bias as unclear (Bauroth 2003, Biesbrock 2007; Jared 2005, Kazmierczak 1994; Walsh 1985; Yost 2006): Jared 2005 used diaries to collect data on possible adverse effects, and there were oral tissue assessments in Bauroth 2003, Kazmierczak 1994 and Yost 2006. Biesbrock 2007 performed assessments of oral tissue and reported that no participants were lost due to adverse events, but provided no information on whether there were any adverse events. We assessed Walsh 1985 as unclear because they used a continuous measure but interpreted it as binary.
We assessed five studies as being at high risk of outcome reporting bias: three did not report standard deviations (Finkelstein 1990; Lewis 2004; Vogel 1975); Sharma 2002 did not report means and standard deviations for bleeding outcomes; the graphs in Smith 1988 were drawn with insufficient accuracy (and no standard deviations) to use the data.
Other potential sources of bias
We assessed six studies to be at low risk of any other potential risks of bias (Frascella 2000; Hague 2007; Imai 2011; Ishak 2007; Walsh 1989; Zimmer 2006).
We considered 28 studies to be unclear in terms of their risk of other potential sources of bias as compliance was not mentioned, not assessed, or not adequately reported (Barnes 2005; Bauroth 2003; Biesbrock 2007; Christou 1998; Cronin 1997; Cronin 2005; Finkelstein 1990; Gordon 1996; Goyal 2012; Graziani 2017; Isaacs 1999; Jackson 2006; Jared 2005; Kazmierczak 1994; Lewis 2004; Lobene 1982; Meklas 1972; Mwatha 2017; NCT00855933; NCT01250769; Rosema 2008; Rosema 2011; Schiff 2006; Sharma 2002; Smith 1988; Walsh 1985; Yankell 2002; Yost 2006). In addition, Cronin 1997 and Rosema 2008 had imbalances in baseline values between the intervention groups.
We judged Vogel 1975 to be at high risk of other bias due to poor compliance in one of the study groups.
Overall bias
Aside from performance bias, which was high risk in all of these studies, we judged two studies be at low risk of bias overall (Imai 2011; Zimmer 2006). We considered 27 studies to be unclear (Barnes 2005; Biesbrock 2007; Christou 1998; Cronin 1997; Cronin 2005; Frascella 2000; Gordon 1996; Goyal 2012; Graziani 2017; Hague 2007; Isaacs 1999; Ishak 2007; Jackson 2006; Jared 2005; Kazmierczak 1994; Lobene 1982; Meklas 1972; Mwatha 2017; NCT00855933; NCT01250769; Rosema 2008; Rosema 2011; Schiff 2006; Walsh 1985; Walsh 1989; Yankell 2002; Yost 2006), and six to be at high risk of bias (Bauroth 2003; Finkelstein 1990; Lewis 2004; Sharma 2002; Smith 1988; Vogel 1975).
See Figure 2 below for a summary of the risk of bias for each included study.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Effects of interventions
See: Summary of findings for the main comparison Flossing plus toothbrushing compared with toothbrushing alone for periodontal diseases and dental caries in adults; Summary of findings 2 Interdental brushing with toothbrushing compared to toothbrushing alone for periodontal diseases and dental caries in adults; Summary of findings 3 Wooden cleaning stick plus toothbrushing compared to toothbrushing alone for periodontal diseases and dental caries in adults; Summary of findings 4 Rubber/elastomeric cleaning stick plus toothbrushing compared to toothbrushing alone for periodontal diseases and dental caries in adults; Summary of findings 5 Oral irrigation plus toothbrushing compared to toothbrushing alone for periodontal diseases and dental caries in adults; Summary of findings 6 Interdental brushing compared to flossing for periodontal diseases and dental caries in adults; Summary of findings 7 Wooden cleaning stick compared to flossing for periodontal diseases and dental caries in adults; Summary of findings 8 Rubber/elastomeric cleaning stick compared to flossing for periodontal diseases and dental caries in adults; Summary of findings 9 Oral irrigation compared to flossing for periodontal diseases and dental caries in adults; Summary of findings 10 Rubber/elastomeric interdental cleaning stick compared to interdental brush for periodontal diseases and dental caries in adults
Comparison 1: Toothbrushing plus flossing versus toothbrushing alone (control)
Fifteen studies compared toothbrushing plus flossing with toothbrushing alone (Bauroth 2003; Biesbrock 2007; Finkelstein 1990; Graziani 2017; Hague 2007; Jared 2005; Lobene 1982; Mwatha 2017; Rosema 2008; Schiff 2006; Sharma 2002; Vogel 1975; Walsh 1985; Zimmer 2006). We assessed four studies as being at high risk of bias and one at low risk of bias. In 10 studies, the risk of bias was unclear. One study used an automated flosser (Biesbrock 2007). Two studies used a 'negative control placebo rinse' (Bauroth 2003; Sharma 2002). Further details of the studies included in this comparison are shown in Table 6. See also summary of findings Table for the main comparison.
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| High | Interproximal | Lobene Modified Interproximal Gingival Index (0 to 4) | Final score at 3 and 6 months | Final score at 3 and 6 months | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 3 and 6 months | N/R | Adverse events were assessed, but not reported. Performed soft‐tissue assessments at baseline, 3, and 6 months. | |
| Unclear | With other sites | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | ‐ | Navy Plaque Index (Rustogi modification) (0 /1) | Final score at 1 month | N/R | Reported mild gingival inflammation in the flossing plus toothbrushing group, which was resolved after few days and was not a reason to drop out | |
| High | Interproximal data presented for gingivitis and other sites for plaque | Löe & Silness Gingival Index modified to include visual assessment only (0 to 3) | No SDs and unable to estimate | ‐ | Global Plaque Index (0 to 100%) | No SDs and unable to estimate | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 1 month | Mentioned as outcome but no data reported | Did not consider adverse effects | |
| (crossover design but we used only first‐period data ‐ see Characteristics of included studies for details) | Unclear | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | ‐ | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Safety assessments were performed at each visit. Overall, two out of 76 participants enrolled in the study, both in the automated flosser group, presented with trauma of the attached gingiva in the oral or buccal areas of the posterior teeth at the second visit resulting from improper use of the flosser. |
| Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | Final score at 1 month | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Adverse events were assessed, but not reported. Participants were issued a diary to keep a log of any symptoms experienced. However, no data regarding adverse events were reported in Results. | |
| Unclear | With other sites | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | ‐ | Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Did not consider adverse effects | |
| Unclear | With other sites | Russel Modified Gingival Index (0 to 2) | Final score at 1 month | Final score at 1 month | Navy Plaque Index (Rustogi modification) (0/1 for each of the nine tooth surfaces) | Final score at 1 month | N/R | Safety assessments were carried out by clinical examinations and by evaluating participants' diary cards. Three gingival irritations and one case of gum soreness were reported in the flossing group. | |
| Unclear | With other sites | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | ‐ | N/R | ‐ | N/R | None identified | |
| Unclear | With other sites | Bleeding on Marginal Probing Index (0 to 2) | Final score at 3 and 6 months | ‐ | Paraskevas modification of Quigley & Hein Plaque Index (0 to 5) | Final score at 3 months | N/R | No adverse effects on the oral hard or soft tissues observed by the examiner or reported by the participants. Used two indices to assess possible adverse effects and found no statistically significant difference in either staining or abrasion between the flossing and toothbrushing only groups at 10 weeks, 6 months and 9 months (P < 0.05). | |
| Unclear | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 3 and 6 months | ‐ | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 3 and 6 months | N/R | No adverse effects on the oral hard or soft tissues observed by the examiner or reported by the participants | |
| High | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 3 and 6 months | ‐ | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 3 and 6 months | N/R | No adverse effects on the oral hard or soft tissues observed by the examiner or reported by the participants | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month Imputed SD from control group of studies using this index | ‐ | Podchladley's Total Plaque Index (0/1) | Unable to impute SD for this index | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | ‐ | ‐ | Final score at 3 months | Silness & Löe Plaque Index (evaluated as percentage of interproximal surfaces scored positive for plaque) (0/1) | Final score at 3 months | N/R | Did not consider adverse effects | |
| Low | Interproximal | Papillary Bleeding Index (1 to 4) | Final score at 1 month | ‐ | Quigley & Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Participants reported mild gingival abrasions in three out of 39 participants at 1‐month time point, and in one of 39 participants at 2 months. In the toothbrush‐only arm, 1 in 39 participants at 1‐month time point reported discomfort in taste and bleeding of gingiva, respectively. No side effects were reported at 2‐month time point |
N/R: not reported
SD: standard deviation
Gingivitis (Gingival Index)
Low‐certainty evidence suggested that flossing in addition to toothbrushing reduced gingivitis at one, three, and six months in comparison with toothbrushing alone (summary of findings Table for the main comparison). The standardised mean difference (SMD) at one month was ‐0.58 (95% confidence interval (CI) ‐1.12 to ‐0.04; 8 trials, 585 participants; Analysis 1.1). There was substantial heterogeneity between the studies (I2 = 89%, P < 0.001). At three months, the SMD was ‐0.33 (95% CI ‐0.50 to ‐0.17; 4 trials, 570 participants; no heterogeneity; Analysis 1.2). At six months, the SMD was ‐0.68 (95% CI ‐0.95 to ‐0.42; 4 trials, 564 participants; moderate heterogeneity (I2 = 55%, P = 0.09); Analysis 1.3).
Gingivitis (proportion of bleeding sites)
Bauroth 2003, Graziani 2017, Mwatha 2017 and Walsh 1985 measured the proportion of bleeding sites. There was very low‐certainty evidence of no significant difference between flossing and toothbrushing only groups at one month (MD ‐0.03, 95% CI ‐0.14 to 0.08; 2 trials, 158 participants; substantial heterogeneity (I2 = 83%, P = 0.01); Analysis 1.4), or three months (MD ‐0.14, 95% CI ‐0.37 to 0.09; 2 trials, 240 participants; substantial heterogeneity (I2 = 95%, P < 0.001); Analysis 1.5). At six months, one trial at high risk of bias found a small difference in favour of flossing (MD ‐0.06, 95% CI ‐0.09 to ‐0.03; 210 participants; very low‐certainty evidence; Analysis 1.6).
Periodontitis
Graziani 2017 measured periodontitis but no data were reported.
Interproximal caries
No studies reported interproximal caries.
Plaque
Fourteen studies reported plaque data. We were unable to use the data from two studies that did not report standard deviations (Finkelstein 1990; Vogel 1975).
The pooled estimate at one month showed very low‐certainty evidence of a possible small benefit for flossing plus toothbrushing (SMD ‐0.42, 95% CI ‐0.85 to 0.02; seven trials, 542 participants; P = 0.06), with substantial heterogeneity (I2 = 83%, P < 0.0001; Analysis 1.7). Very low‐certainty evidence of a possible benefit for flossing was found at the three‐month time point (SMD ‐0.20, 95% CI ‐0.36 to ‐0.04; 5 trials, 594 participants), with no evidence of heterogeneity (I2 = 0%, P = 0.74; Analysis 1.8); however, we were unable to claim a benefit for flossing plus toothbrushing at six months (SMD ‐0.13, 95% CI ‐0.30 to 0.05; P = 0.53; 3 trials, 487 participants; no heterogeneity; Analysis 1.9).
Adverse effects
Overall, there were no serious adverse events reported for this comparison. Details about adverse events are described in Table 6.
Secondary outcomes
Halitosis, patient satisfaction, and cost of intervention were not measured in these studies.
Comparison 2: Toothbrushing plus interdental brushing versus toothbrushing alone
Two studies compared toothbrushing plus using an interdental brush with toothbrushing alone (Graziani 2017; Jared 2005), and reported data at one month. Both were at unclear risk of bias. The details of the studies included in this comparison are shown in Table 7. See also summary of findings Table 2.
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 1 month | Mentioned as outcome but no data reported | Did not consider adverse effects | |
| Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | ‐ | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Adverse events were assessed, but not reported. Participants were issued a diary to keep a log of any symptoms experienced. However, no data regarding adverse events were reported in Results. |
N/R: not reported
See summary of findings Table 2.
Gingivitis (Gingival Index)
There was very low‐certainty evidence that interdental brushes reduced gingivitis compared to toothbrushing alone at one month (MD ‐0.53, 95% CI ‐0.83 to ‐0.23; 1 trial, 62 participants; Analysis 2.1).
Gingivitis (proportion of bleeding sites)
There was very low‐certainty evidence that interdental brushes did not reduce proportion of bleeding sites more than toothbrushing alone (one‐month MD ‐0.05, 95% CI ‐0.13 to 0.03; 1 trial, 31 participants; very low‐certainty evidence; Analysis 2.2).
Periodontitis
Graziani 2017 measured periodontitis but no data were reported.
Interproximal caries
Neither study reported interproximal caries.
Plaque
There was low‐certainty evidence that interdental brushes reduced plaque compared to toothbrushing alone at one month (SMD ‐1.07, 95% CI ‐1.58 to ‐0.69; 2 trials, 93 participants; Analysis 2.3). There was no evidence of heterogeneity (I2 = 0%, P = 0.48).
Adverse effects
Graziani 2017 did not report on adverse effects. In Jared 2005, each participant was given a diary to keep a log of any symptoms experienced; however, data concerning adverse events were not reported in Results.
Secondary outcomes
Halitosis, patient satisfaction, and cost of intervention were not measured in these studies.
Comparison 3: Toothbrushing plus use of wooden cleaning sticks versus toothbrushing alone
Two studies made this comparison (Finkelstein 1990; Walsh 1985); however, we were only able to use the data from Walsh 1985 as Finkelstein 1990 did not provide standard deviations. Walsh 1985, which was at unclear risk of bias, measured outcomes at three months. The details of the studies included in this comparison are shown in Table 8. See also summary of findings Table 3.
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| High | Interproximal data presented for gingivitis and other sites for plaque | Löe & Silness Gingival Index modified to include visual assessment only (0 to 3) | None ‐ no SDs and unable to estimate | ‐ | Global Plaque Index (0 to 100%) | None ‐ no SDs and unable to estimate | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | ‐ | ‐ | Final score at 3 months | Silness & Löe Plaque Index (evaluated as percentage of interproximal surfaces scored positive for plaque) (0/1) | Final score at 3 months | N/R | Did not consider adverse effects |
N/R: not reported
Gingivitis (Gingival Index)
We were unable to use Finkelstein 1990 data, and Walsh 1985 did not measure this.
Gingivitis (proportion of bleeding sites)
There was very low‐certainty evidence to claim a benefit for wooden cleaning sticks in reducing proportion of bleeding sites compared to toothbrushing alone at three months (MD (mean proportion of bleeding sites) ‐0.25, 95% CI ‐0.37 to ‐0.13; 1 trial, 24 participants; Analysis 3.1). This was the only time point providing useable data.
Periodontitis
No studies reported periodontitis.
Interproximal caries
No studies reported interproximal caries.
Plaque
There was very low‐certainty evidence that wooden cleaning sticks did not reduce plaque more than toothbrushing alone (MD (mean proportion of sites with plaque) ‐0.03, 95% CI ‐0.13 to 0.07; 1 trial, 24 participants; Analysis 3.2). This was the only time point providing useable data.
Adverse events
Neither of the studies assessing this comparison reported on adverse effects .
Other outcomes
Halitosis, patient satisfaction, and cost of intervention were not measured in these studies.
Comparison 4: Toothbrushing plus use of rubber/elastomeric cleaning sticks versus toothbrushing alone
Two studies made this comparison (Graziani 2017; Vogel 1975), one at unclear and one at high risk of bias. The details of the studies included in this comparison are shown in Table 9. See also summary of findings Table 4.
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | Interproximal | ‐ | ‐ | Final score at one month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 1 month | Mentioned as outcome but no data reported | Did not consider adverse effects | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at one month | ‐ | Podchladley's Total Plaque Index (0/1) | Unable to impute for index | N/R | Did not consider adverse effects |
N/R: not reported
Gingivitis (Gingival Index)
There was no evidence that rubber/elastomeric cleaning sticks reduced plaque at one month (MD ‐0.01, 95% CI ‐0.19 to 0.21; 1 trial, 12 participants; Analysis 4.1) (very low‐certainty evidence). This was the only time point reporting data.
Gingivitis (proportion of bleeding sites)
There was no evidence that rubber/elastomeric cleaning sticks reduced proportion of bleeding sites at one month (MD ‐0.07, 95% CI ‐0.15 to 0.01; 1 trial, 30 participants; Analysis 4.2) (very low‐certainty evidence). This was the only time point reporting data.
Periodontitis
No studies reported periodontitis.
Interproximal caries
No studies reported interproximal caries.
Plaque
There was very low‐certainty evidence that wooden cleaning sticks reduced plaque at one month: MD (full mouth plaque score) ‐0.22, 95% CI ‐0.41 to ‐0.03; 1 trial, 30 participants; Analysis 4.3). This was the only time point providing useable data.
Adverse events
Neither study reported on adverse effects (Graziani 2017; Vogel 1975).
Other outcomes
Halitosis, patient satisfaction, and cost of intervention were not measured in these studies.
Comparison 5: Toothbrushing plus oral irrigation versus toothbrushing alone
Five studies, all at unclear risk of bias, compared toothbrushing plus oral irrigation versus toothbrushing alone (Frascella 2000; Goyal 2012; Meklas 1972; NCT01250769; Walsh 1989). The details of the studies included in this comparison are shown in Table 10. See also summary of findings Table 5.
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | With other sites | Modified gingival index (0 to 3) | Final score at 1 month | Final score at 1 month | Turesky‐Gilmore‐Glickman modification of the Quigley‐Hein Plaque Index | Final score at 1 month | N/R | Safety mentioned and "no problems" reported; not clear how this was assessed | |
| Unclear | Interproximal for plaque; other sites for gingivitis | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | Final score at 1 month | Navy Plaque Index (Rustogi modification) (0/1 for each of the nine tooth surfaces) | Final score at 1 month | N/R | Reported that there were no adverse effects | |
| Unclear | With other sites | Russell modified Periodontal Index (0 to 2) | Final score at 1, 3, and 6 months | ‐ | 3‐point plaque index (0 to 2) | Final score at 1, 3 and 6 months | N/R | Reported adverse events in terms of oral lacerations, with no significant difference between the study arms (toothbrushing and oral irrigation 8/55; toothbrushing only 7/54) | |
| Unclear | With other sites | Modified Gingival Index (0 to 4) | Final score at 1 month | ‐ | N/R | ‐ | N/R | 1 serious (arm deep vein thrombosis) in Gp C ‐ unrelated to treatment, and 1 minor in Gp D ‐ aphthous ulcer above tooth #7 on attached gingiva | |
| Unclear | With other sites | Löe & Silness Gingival Index (0 to 3) | Final score at 3 months (6‐month data not used) | Final score at 3 months (6‐month data not used) | Silness & Löe Plaque Index (visible plaque or not ‐ 0, 1) | Final score at 3 months (6‐month data not used) | ‐ | No injury to hard or soft tissues. No soft tissue changes. |
N/R: not reported
Gingivitis (Gingival Index)
Goyal 2012 and NCT01250769 provided gingivitis data for one month, Frascella 2000 for one and two months, Meklas 1972 for one, two, three, four, five, six months, and Walsh 1989 for three months. The meta‐analysis for one month indicated that the water irrigator may reduce gingivitis (SMD ‐0.48, 95% CI ‐0.89 to ‐0.06; 4 trials, 380 participants; Analysis 5.1). There was substantial heterogeneity (I2 = 73%, P value = 0.01). At three and six months, there was no significant difference between groups (3‐month SMD ‐0.13, 95% CI ‐0.44 to 0.17, 2 trials, 163 participants; no heterogeneity; Analysis 5.2; 6‐month MD ‐0.33, 95% CI ‐0.74 to 0.08, 1 trial, 109 participants; Analysis 5.3). The evidence was very low‐certainty.
Gingivitis (proportion of bleeding sites)
The mean score in the oral irrigation group was the same as the toothbrushing‐only group at one month (MD ‐0.00, 95% CI ‐0.07 to 0.06; 2 trials, 126 participants; moderate heterogeneity (I2 = 48%, P = 0.16); Analysis 5.4) (low‐certainty evidence). At three months, the MD was ‐0.04 (95% CI ‐0.13 to 0.05, 1 trial, 54 participants) (Analysis 5.5).
Periodontitis
Walsh 1989 reported the proportion of sites with > 4 mm pocket depth at three months, but not mean PD measurements. Walsh 1989 also measured attachment loss, but did not provide data. The authors stated that, "there was essentially no change in attachment loss in any of the groups during the experimental period".
Interproximal caries
No studies reported interproximal caries.
Plaque
Goyal 2012 provided plaque data for one month, Frascella 2000 provided data for one and two months, Meklas 1972 provided data for one, two, three, four, five, six months and Walsh 1989 provided data at three and six months. The meta‐analysis for one month indicated no evidence that the use of the oral irrigator reduced plaque more than toothbrushing alone (SMD ‐0.16, 95% CI ‐0.41 to 0.10; 3 trials, 235 participants; no heterogeneity; Analysis 5.6). There was also no evidence of a change in plaque at three months (SMD 0.06, ‐0.25 to 0.37; 2 trials, 163 participants; no heterogeneity; Analysis 5.7) or six months (MD 0.22, ‐0.59 to 0.15; 1 trial, 109 participants; Analysis 5.8). The certainty of the evidence was low.
Adverse events
Some participants in both groups in Meklas 1972 had oral lacerations (with no difference between intervention arms). Frascella 2000, Goyal 2012 and Walsh 1989 reported that there were no adverse events. NCT01250769 found one serious event (arm deep vein thrombosis) that was unrelated to treatment, and one minor event in one of the oral irrigator groups, an aphthous ulcer. See Table 10.
Other outcomes
Halitosis, patient satisfaction, and cost of intervention were not measured in these studies.
Comparison 6: Interdental brush versus floss
Nine studies compared toothbrushing plus use of an interdental brush with toothbrushing plus flossing (Christou 1998; Graziani 2017; Imai 2011; Ishak 2007; Jackson 2006; Jared 2005; Smith 1988; Yankell 2002; Yost 2006). Yankell 2002 used an automated flosser. We included the six‐week data from Yost 2006 in the one‐month analysis. Imai 2011 was at low risk of bias; Smith 1988 was at high risk; and the rest were unclear. We were unable to use the data from Smith 1988. We analysed the parallel‐group and split‐mouth studies (Christou 1998; Imai 2011; Ishak 2007) separately when using SMD. The details of the studies included in this comparison are shown in Table 11. See also summary of findings Table 6.
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 1 month | Mentioned PPD in mm as outcome but no data reported | Did not consider adverse effects | |
| Unclear | Interproximal | ‐ | ‐ | Final score at 1 and 3 months | Silness & Löe Plaque Index (0 to 3) | Final score at 1 and 3 months | PPD in mm | No adverse effects observed or reported during the study in either group | |
| Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | ‐ | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Adverse events were assessed, but not reported. Participants were issued a diary to keep a log of any symptoms experienced. However, no data regarding adverse events were reported in Results. | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Unable to use data | ‐ | Silness & Löe Plaque Index (0 to 3) | Unable to use data | PPD in mm but unable to use data | Did not consider adverse effects | |
| Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | Final score at 1 month | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | ‐ | Study reported "There were no untoward side effects, reported or observed, at any time during the study, attributed to any of the dental products distributed in this study." | |
| Unclear | Interproximal | Eastman Interdental Bleeding Index (0/1) | Final score at 1 month | ‐ | Benson modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Examinations of the oral soft tissue were performed at the final visit, but were not reported. | |
| Christou 1998 (split‐mouth design) | Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Volpe modification of Quigley and Hein Plaque Index (0 to 5) | Final score at 1 month | PPD in mm | Participants reported significantly more problems when using the floss than IDB. The most common problem was difficulty in flossing posterior areas of mouth. |
| Imai 2011 (split‐mouth design) | Low | Interproximal | ‐ | ‐ | Final score at 1 and 3 months | Silness & Löe Plaque Index (0 to 3) | Final score at 1 and 3 months | N/R | No adverse effects observed or reported during the study in either group |
| Ishak 2007 (split‐mouth design) | Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Visible plaque deposits were scored as positive | Final score at 1 month | PPD in mm | Participants encountered problems with both interventions. The IDBs tended to bend, buckle and |
N/R: not reported
PPD: pocket probing depth
Gingivitis (Gingival Index)
There was low‐certainty evidence of a reduction in gingivitis at one month in the parallel‐group studies when interdental brushes were used rather than floss (SMD ‐0.40, 95% CI ‐0.70 to ‐0.11; 3 trials, 183 participants; no heterogeneity; Analysis 6.1).
Gingivitis (proportion of bleeding sites)
There was low‐certainty evidence of a reduction in bleeding sites at four to six weeks when interdental brushes were used rather than floss (MD ‐0.06, 95% CI ‐0.08 to ‐0.03; 6 trials (3 parallel and 3 split‐mouth), 234 participants; Analysis 6.2). There was moderate heterogeneity (I2 = 41%, P = 0.13).
At three months, low‐certainty evidence from the combined results of one parallel‐group study (Jackson 2006) and one split‐mouth study (Imai 2011) also indicated a possible benefit for interdental brushes (MD ‐0.10, 95% CI ‐0.15 to ‐0.04); 2 trials, 106 participants; moderate heterogeneity (I2 = 69%, P = 0.07); Analysis 6.3).
Periodontitis
Five studies measured mean probing pocket depth scores (PPD) in mm (Christou 1998; Graziani 2017; Ishak 2007; Jackson 2006; Smith 1988). We were unable to use the data presented from Smith 1988, and data were not presented for Graziani 2017. Graziani 2017 stated there was no evidence of a difference in PPD measurements between the interdental brush and floss groups. There was no evidence of a difference between interdental brushes and floss with respect to mean PPD at four to six weeks (MD ‐0.06, 95% CI ‐0.27 to 0.16; 3 trials, 107 participants; no heterogeneity; Analysis 6.4) (low‐certainty evidence). One parallel‐group study also presented 12‐week data for PPD (MD 0.01 mm, 95% CI ‐0.29 to 0.31, 77 participants; Analysis 6.5), which provided no evidence of a difference (very low‐certainty evidence).
Interproximal caries
No studies reported interproximal caries.
Plaque
There was very low‐certainty evidence of a reduction in plaque at one month in the parallel‐group studies when interdental brushes were used (SMD ‐0.47, 95% CI ‐0.84 to ‐0.11; 5 trials, 290 participants; moderate heterogeneity (I2 = 57%, P = 0.05); Analysis 6.6). This finding, however, was not supported by the data from the three split‐mouth studies (SMD ‐0.07, 95% CI ‐0.32 to 0.18; substantial heterogeneity (I2 = 90%, P < 0.001; Analysis 6.7), nor from the data available for three months (MD ‐0.12, 95% ‐0.33 to 0.10; 2 trials, 106 participants; substantial heterogeneity (I2 = 80%, P = 0.02); Analysis 6.8).
Adverse events
Six studies reported on adverse events, none of which identified clinical problems. Two reported difficulties using the devices. Further details are described in Table 11.
Other outcomes
Halitosis, patient satisfaction, and cost of intervention were not measured in these studies.
Comparison 7: Wooden cleaning stick versus floss
Three studies made this comparison (Finkelstein 1990; Lewis 2004; Walsh 1985); however, we were only able to use the data from Walsh 1985 as Finkelstein 1990 and Lewis 2004 did not provide standard deviations. The details of the studies included in this comparison are shown in Table 12. See also summary of findings Table 7.
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| High | Interproximal data presented for gingivitis and other sites for plaque | Löe & Silness Gingival Index modified to include visual assessment only (0 to 3) | No SDs and unable to estimate | ‐ | Global Plaque Index (0 to 100%) | No SDs and unable to estimate | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | Eastman Interdental Bleeding Index (0/1) | No SDs and unable to estimate | ‐ | O'Leary Plaque Index (0/1) | No SDs and unable to estimate | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | ‐ | ‐ | Final score at 3 months | Silness & Löe Plaque Index (evaluated as percentage of interproximal surfaces scored positive for plaque) (0/1) | Final score at 3 months | N/R | Did not consider adverse effects |
N/R: not reported
Gingivitis (Gingival Index)
Not measured.
Gingivitis (proportion of bleeding sites)
There was no evidence to claim a benefit for either wooden cleaning sticks or floss in reducing gingivitis at three months (MD (mean proportion of bleeding sites) 0.01, 95% CI ‐0.12 to 0.14; 1 trial, 24 participants; Analysis 7.1) (very low‐certainty evidence). This was the only time point providing useable data.
Periodontitis
No studies reported periodontitis.
Interproximal caries
No studies reported interproximal caries.
Plaque
There was no evidence that wooden cleaning sticks reduced plaque (MD (mean proportion of sites with plaque) 0.02, 95% CI ‐0.06 to 0.10; 1 trial, 24 participants; Analysis 7.2) (very low‐certainty evidence). This was the only time point providing useable data.
Adverse events
Neither of the studies assessing this comparison reported on adverse effects.
Other outcomes
Halitosis, patient satisfaction, and cost of intervention were not measured in these studies.
Comparison 8: Rubber/elastomeric interdental cleaning stick versus floss
Nine trials compared toothbrushing plus rubber interdental cleaning sticks with toothbrushing plus flossing. Five used a manual cleaning stick (Graziani 2017; Kazmierczak 1994; Smith 1988; Vogel 1975; Yost 2006), and four were powered (Cronin 1997; Cronin 2005; Gordon 1996; Isaacs 1999). We are unable to use the data from Smith 1988. We used six‐week data from Yost 2006. The details of the studies included in this comparison are shown in Table 13. See summary of findings Table 8.
| Study (parallel group design unless noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | Final score at 1 month | Turesky modification of Quigley Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | There was no significant difference in soft tissue pathology between the groups. | |
| Unclear | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | Final score at 1 month | Proximal/Marginal Plaque index (0 to 5) | Final score at 1 month | N/R | No significant differences in the proportion of hard and soft tissue abnormalities between groups were found | |
| Gordon 1996 (crossover but first‐period data only used ‐ see Characteristics of included studies for details) | Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | Final score at 1 month | Proximal/Marginal Plaque index (0 to 5) | Final score at 1 month | N/R | No significant soft tissue pathology was noted in any of the participants in either group |
| Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 1 month | Mentioned as outcome but no data reported | Did not consider adverse effects | |
| Unclear | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 3 months | Final score at 3 months | Turesky modification of Quigley Hein Plaque Index (0 to 5) | Unable to use data | N/R | There was no difference in the soft tissue status of the participants in the study groups. At 6 months, healthy soft tissue was found in 66/73 and 65/72 participants in cleaning sticks versus floss groups, respectively | |
| Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4 | Final score at 1 month | Final score at 1 month | Turesky modification of Quigley Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Did not consider adverse effects | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Unable to use data | ‐ | Silness & Löe Plaque Index (0 to 3) | Unable to use data | PPD in mm but unable to use data | Did not consider adverse effects | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | ‐ | Podchladley's Total Plaque Index (0/1) | Unable to impute for index | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | Eastman Interdental Bleeding Index (0/1) | Final score at 6 weeks | ‐ | Benson modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 6 weeks | N/R | Examinations of the oral soft tissue were performed at the final visit, but were not reported. |
N/R: not reported
PPD: pocket probing depth
Gingivitis (Gingival Index)
There was no evidence that one intervention performed better than the other with regards to gingivitis control at one month to six weeks (SMD ‐0.22, 95% CI ‐0.69 to 0.24; 6 trials, 256 participants) or three months (SMD 0.01, 95% CI ‐0.08 to 0.10; 1 trial, 145 participants; very low‐certainty evidence) (Analysis 8.1; Analysis 8.2). There was substantial heterogeneity in the one‐month result (I2 = 67%, P = 0.009).
Gingivitis (proportion of bleeding sites)
Neither rubber/elastomeric cleaning sticks or floss were superior for reducing proportion of bleeding sites at one month (MD (mean proportion of bleeding sites) 0.03, 95% CI ‐0.08 to 0.03; 5 trials, 212 participants; Analysis 8.3) (low‐certainty evidence). There was moderate heterogeneity (I2 = 59%, P = 0.04). The result was similar at three months (MD 0.01, ‐0.03 to 0.05, 1 trial, 145 participants; very low‐certainty evidence; Analysis 8.4).
Periodontitis
Smith 1988 measured PPD but we were unable to use the data presented.
Interproximal caries
No studies reported interproximal caries.
Plaque
There was no evidence that one intervention performed better than the other with regards to plaque control at one month (SMD ‐0.08, 95% CI ‐0.46 to 0.29; 6 trials, 273 participants; moderate heterogeneity (I2 = 57%, P value = 0.04); very low‐certainty evidence; Analysis 8.5).
Adverse events
Two studies did not report adverse events and the other two reported adverse events as described in Table 13.
Other outcomes
Halitosis, patient satisfaction, and cost of intervention were not measured in these studies.
Comparison 9: Oral irrigation versus floss
Two trials (Barnes 2005; Rosema 2011), both at unclear risk of bias, provided gingivitis and plaque data at one month comparing oral irrigation with flossing. The details of the studies included in this comparison are shown in Table 14. See summary of findings Table 9.
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | With other sites | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | Final score at 1 month | Proximal/Marginal Plaque Index (0 to 5) | Final score at 1 month | N/R | Reported that there were no adverse events in any study group. | |
| Unclear | With other sites | Bleeding on Marginal Probing Index (0 to 2) | Final score at 1 month | Final score at 1 month | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Reported that there were no adverse events in any study group. |
N/R: not reported
Gingivitis (Gingival Index)
There was very low‐certainty evidence of a possible reduction in gingivitis at one month when oral irrigation was compared to flossing, though the result was also compatible with no difference between the interventions (MD ‐0.06, 95% CI ‐0.12 to ‐0.00; 1 trial, 63 participants; Analysis 9.1).
Gingivitis (proportion of bleeding sites)
There was low‐certainty evidence of a reduction in proportion of bleeding sites at one month when oral irrigation was compared to flossing (MD ‐0.12, 95% CI ‐0.19 to ‐0.05; 2 trials, 133 participants; no heterogeneity (I2 = 1%, P = 0.34); Analysis 9.2).
Periodontitis
No studies reported periodontitis.
Interproximal caries
No studies reported interproximal caries.
Plaque
There was no evidence of a difference in plaque at one month for either oral irrigation or flossing (SMD 0.31, 95% CI ‐0.08 to 0.70; 2 trials, 133 participants; low heterogeneity (I2 = 22%, P = 0.26); very low‐certainty evidence; Analysis 9.3).
Adverse events
Both Barnes 2005 and Rosema 2011 reported that there were no adverse events in any study group. See Table 14.
Other outcomes
Halitosis, patient satisfaction, and cost of intervention were not measured in these studies.
Comparison 10: Interdental cleaning stick versus interdental brush
Three trials compared rubber/elastomeric interdental cleaning sticks with interdental brushes (Graziani 2017; Smith 1988; Yost 2006). We were unable to use data from one trial (Smith 1988). We used six‐week data from Yost 2006. The studies were at unclear risk of bias. The details of the studies included in this comparison are shown in Table 15. See summary of findings Table 10.
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | Interproximal | Full Mouth Bleeding Score (0/1) | Final score at 6 weeks | Final score at 1 month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 6 weeks | Mentioned as outcome but no data reported | Did not consider adverse effects | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Unable to use data | ‐ | Silness & Löe Plaque Index (0 to 3) | Unable to use data | PPD in mm but unable to use data | Did not consider adverse effects | |
| Unclear | Interproximal | Eastman Interdental Bleeding Index (0/1) | Final score at 6 weeks | ‐ | Benson modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 6 weeks | N/R | Examinations of the oral soft tissue were performed at the final visit, but were not reported. |
IDB: interdental brush
N/R: not reported
PPD: pocket probing depth
Gingivitis (Gingival Index)
There was no evidence that one intervention performed better than the other with regards to gingivitis control at six weeks (MD 0.10, 95% CI ‐0.32 to 0.52; 1 trial, 61 participants; very low‐certainty evidence; Analysis 10.1).
Gingivitis (proportion of bleeding sites)
There was no evidence that one intervention performed better than the other with regards to reducing proportion of bleeding sites at one month (MD ‐0.02, 95% CI ‐0.10 to 0.06; 1 trial, 31 participants; very low‐certainty evidence; Analysis 10.2).
Periodontitis
Smith 1988 measured PPD but we were unable to use the data presented. Graziani 2017 also measured PPD but did not provide data.
Interproximal caries
No studies reported interproximal caries.
Plaque
There was no evidence that one intervention performed better than the other with regards to plaque control at one month to six weeks (SMD 0.08, 95% CI ‐0.33 to 0.49; 2 trials, 92 participants; no heterogeneity; very low‐certainty evidence; Analysis 10.3).
Adverse events
Graziani 2017 and Smith 1988 did not measure adverse effects. In Yost 2006, examinations of the oral soft tissue were performed at the final visit, but were not reported. See Table 15.
Other outcomes
Halitosis, patient satisfaction, and cost of intervention were not measured in these studies.
Discussion
Summary of main results
This review found five devices that were used in addition to toothbrushing and compared with toothbrushing alone: floss (15 trials), interdental brushes (2 trials), wooden cleaning sticks (2 trials), rubber/elastomeric cleaning sticks (2 trials), oral irrigators (5 trials). Four devices were compared with flossing: interdental brushes (9 trials), wooden cleaning sticks (3 trials), rubber/elastomeric cleaning sticks (9 trials), oral irrigators (2 trials). The other comparison was between rubber/elastomeric cleaning sticks and interdental brushes (3 trials).
Most of the trials presented results for gingivitis and plaque, which we analysed at one, three, and six months. Six studies evaluated periodontitis, but data were only useable for one comparison: interdental brushes versus flossing. Some studies considered possible harm from the interventions. None of the studies measured interproximal caries. Nor did they measure our secondary outcomes of halitosis, patient satisfaction and costs.
Participants in most studies had a low level of gingival inflammation at baseline, and outcomes were measured most commonly in the short term. Overall, the evidence was low to very low‐certainty, and the effect sizes observed may not be clinically important.
Comparisons with toothbrushing alone
For flossing plus toothbrushing compared to toothbrushing alone, there was low‐certainty evidence of flossing reducing gingivitis at one month. This was confirmed at three and six months. There was very low‐certainty evidence that did not show that flossing reduced plaque more than toothbrushing alone at one month or six months; there was some evidence for an effect at three months.
Using an interdental brush in addition to cleaning the teeth with a toothbrush may reduce gingivitis (measured by gingival index) and plaque, but not proportion of bleeding sites. The evidence was low to very low‐certainty, being based on only one or two small studies, and only measured at the one‐month time point.
Using wooden interdental toothcleaning sticks in addition to toothbrushing may reduce gingivitis measured by proportion of bleeding sites, but not plaque, when measured at three months. The evidence was very low‐certainty, being based on only 24 participants.
Using rubber/elastomeric interdental toothcleaning sticks in addition to toothbrushing did not appear to reduce gingivitis at one month any more than toothbrushing alone, but there may be a reduction in plaque. The evidence was very low‐certainty, being based on 12 or 30 participants.
Toothbrushing plus oral irrigation (pulsing water) may reduce gingivitis measured by a gingival index more than toothbrushing alone at one month, but the evidence was very low‐certainty, and this effect was not seen at three or six months. Low‐certainty evidence did not show a clear difference between groups for reduction in proportion of bleeding sites at one or three months, or plaque at one, three, or six months.
Comparisons between different interdental cleaning aids
Interdental brushes may be better than flossing for reducing gingivitis at one and three months (low‐certainty evidence). The evidence for a reduction in plaque was inconsistent (very‐low certainty evidence). There was no evidence that either device was superior for reducing periodontitis (low‐certainty evidence).
Wooden cleaning sticks or rubber/elastomeric cleaning sticks did not seem to be better or worse than flossing at controlling gingivitis or plaque at three months (low‐ to very low‐certainty evidence).
There was some evidence that oral irrigation may be better than flossing for reducing gingivitis at one month (low‐ to very low‐certainty evidence). The evidence did not show either intervention to be superior for reducing plaque (very low‐certainty evidence).
There was no evidence that rubber/elastomeric interdental cleaning sticks were better or worse than interdental brushes for controlling gingivitis and plaque (very low‐certainty evidence).
Adverse events
Adverse events were presented for some of the trials; however, there were no severe adverse events reported and no evidence of differences between study groups. One study reported on problems using the interventions (interdental brush versus floss), in particular, soreness caused when interdental brushes become stuck between the teeth.
Overall completeness and applicability of evidence
The evidence was limited in applicability and was incomplete. The included studies only presented data on gingivitis, plaque, and adverse events; most did not measure or report other important outcomes such as periodontitis or interproximal caries. One reason for this is that larger, longer term studies are needed to measure these outcomes. Costs were another outcome not reported although this may be an important consideration for patients.
Another weakness in the included trials in terms of the completeness and applicability of evidence is the low level of gingivitis and plaque in many of the participants. For example, if studies reporting gingivitis at one month using the Löe and Silness Gingival Index are examined, the mean values for the toothbrushing‐only group for the four studies varied between 0.14 and 0.84 (median 0.47), which is very low considering that this index is on a 0‐ to 3‐point scale. This means that even large effect sizes on a SMD scale are probably clinically unimportant, and that trialists may not be selecting the right participants to answer questions about the efficacy of these interventions. We also considered bleeding data measured as the proportion of bleeding sites per participant, as we thought this would make the clinical interpretation of data presented easier, along with a judgement of clinical importance. Surprisingly, however, there was little correlation between the two, which made the interpretation more complex and challenging. In addition, we are not aware that a minimally important clinical difference has been established for the commonly used gingival and plaque scales.
We included only studies on adults. There have been no studies of mechanical interdental cleaning for children at home, though there has been some research on supervised interventions delivered in schools and professional interventions delivered in the primary dental care setting. This was summarised in the systematic review by Hujoel (Hujoel 2006).
Quality of the evidence
We included 35 trials that randomised 3929 participants and evaluated approximately 3734 participants; however, many of the meta‐analyses only included a small number of trials and participants. All trials were at high risk of performance bias as participants knew which interdental aids they were using. While recognising this performance bias risk, we omitted this domain from the overall 'risk of bias' assessment that informed our assessment of the certainty of the evidence because lack of blinding is unavoidable and any behaviour change related to knowledge of these interventions can be regarded as an integral part of the intervention, and incorporated into estimates of 'real world' effectiveness. When performance bias was omitted from the overall 'risk of bias' assessment, we judged two trials (6%) to be at low risk of bias, six trials (17%) to be at high risk and 27 trials (77%) to be unclear.
The largest body of evidence we identified was for flossing and toothbrushing compared with toothbrushing only (15 studies). The body of evidence for this comparison for both gingivitis and plaque was low‐ and very low‐certainty, respectively, due to the risk of bias in the studies, substantial unexplained heterogeneity, and lack of precision in the effect estimates. We assessed the body of evidence for all comparisons and outcomes as low‐ or very low‐certainty.
The studies included in this review used many different gingivitis and plaque indices. This meant that we had to estimate a standardised mean difference (SMD) effect estimate in some cases. We did not back‐translate this to a common index as there were only two trials at low risk of bias (excluding performance bias). It would be sensible for clinicians to agree on a common index to use for both these measures; this would enable results of future studies to be pooled, which would aid precision and interpretability of effect estimates, and also help establish minimal clinically important differences. Support to select the most appropriate outcome measurement is available through the COSMIN initiative (COSMIN 2018).
Potential biases in the review process
We estimated the standard deviations for some trials that did not report these. We undertook this only for the most commonly reported gingivitis (Löe and Silness Gingival Index) and plaque indices (Turesky modification of the Quigley Hein Index). When we undertook sensitivity analyses, by removing studies with estimated standard deviations, the effect estimates were similar.
Two review authors (P Imai and HV Worthington) were each authors on an included trial; however, the assessment of these two trials was independently undertaken by other members of the review team.
The toothbrushing‐only group in two trials that compared this group to a toothbrushing plus flossing group, also included use of a 'placebo' negative control rinse. We included these studies as the rinse may help to counteract any performance bias, and our sensitivity analyses omitting these studies led to similar effect estimates.
There were some studies of manual cleaning sticks, while others were automated. There were some studies that used electric toothbrushes in both arms. We conducted meta‐analyses even if it meant combining automated and manual devices; we would have conducted subgroup analyses had there been sufficient studies.
Many of the included studies were funded by pharmaceutical companies who made the intervention being evaluated. We are unsure whether or not this has introduced publication bias into the effect estimates. It is, however, noted that there are similar numbers of head‐to‐head studies and studies comparing the intervention with toothbrushing alone.
We excluded studies that evaluated use of multiple devices, supervised use of interdental cleaning devices, or dental health professional delivery of mechanical interdental cleaning. In the update of this review, we may consider including these studies to gain a greater understanding of the best use of interdental cleaning devices for preventing or controlling periodontal diseases and dental caries.
Agreements and disagreements with other studies or reviews
This review includes updates of two previously published Cochrane reviews on flossing and interdental brushing (Sambunjak 2011; Poklepovic Pericic 2013), conducted by some of the same authors. The flossing review included a section that compared the findings to Berchier 2008, and the findings of the interdental brushing review were compared to those of the reviews by Slot 2008 and Imai 2012.
Berchier 2008 had reported that "both plaque and gingivitis values show no significant effects", and noted "a trend in favour of brushing and floss", questioning whether lack of statistically significant findings might be due to a lack of power. The current review found that toothbrushing plus flossing reduced gingivitis scores at one, three, and six months, compared to toothbrushing alone, with effects on plaque being less clear.
Slot 2008 looked at the effect of interdental brushing with toothbrushing compared to toothbrushing alone or another interdental device, on plaque and "parameters of gingival inflammation". The findings were broadly similar to this review; however, the meta‐analyses were conducted on specific indices for plaque and gingivitis rather than combining them using standardised mean differences. The authors concluded that use of interdental brushes compared to toothbrushing alone showed "a positive significant difference with respect to plaque, bleeding and probing pocket depth", which is in agreement with this review for plaque and gingivitis; however, we did not find any PPD data for this comparison. The authors also reported that interdental brushes appeared to reduce plaque when compared with flossing, which is also in agreement with this review; however, we found interdental brushes also appeared to reduce gingivitis, but not PPD. The overall findings of Imai 2012 were similar to our review, i.e. that interdental brushing is more effective than floss in reducing gingivitis and plaque scores; however, Imai 2012 included only four studies looking at this comparison, compared to nine in our review.
Hoenderdos 2008 is a systematic review that assessed the efficacy of wood sticks, used for interdental cleaning, on plaque levels and gingival inflammation. They found that wood sticks had "no visible effect on interdental plaque and did not reduce the gingival index. However, woodsticks were effective in reducing interdental gingival inflammation when tendency to bleeding was investigated". We also found some evidence for an effect on bleeding at three months, albeit based on just 24 participants. There was no RCT evidence to assess gingivitis measured by a gingival index. Hoenderdos 2008 included CCTs as well as RCTs, and studies with shorter outcome assessment time points than this review did, with more restricted types of handheld wooden toothpicks, so the two reviews are not directly comparable.
A systematic review published in 2008 looked at the effect of oral irrigation as an adjunct to brushing (Husseini 2008). This review included seven studies, both RCTs and CCTs, and reached the conclusion that as an adjunct to brushing "the oral irrigator does not have a beneficial effect in reducing visible plaque, however there is a positive trend in favour of oral irrigation improving gingival health". This aligned with our review, which found that there may be an effect of oral irrigators on gingivitis measured by gingival index at one month, but did not find this at any other time point, or for the outcomes of bleeding or plaque.
A recent network meta‐analysis included different interproximal cleaning aids of oral hygiene methods (Kotsakis 2017), with the aim of ranking them in order of importance for reducing gingival inflammation. The results included 22 trials looking at 10 interdental oral hygiene aids as adjuncts to toothbrushing. Interdental brushes yielded the largest reduction in the Gingival Index (GI) followed by water‐jet. The authors reported that all the aids except toothpicks reduced the Gingival Index when compared to toothbrushing alone. This did not align entirely with our findings. We did note that the Kotsakis 2017 review did not assess heterogeneity or transitivity, discuss the impact of sparse networks, or consider results with respect to the certainty of the evidence.

Study flow diagram

Risk of bias summary: review authors' judgements about each risk of bias item for each included study
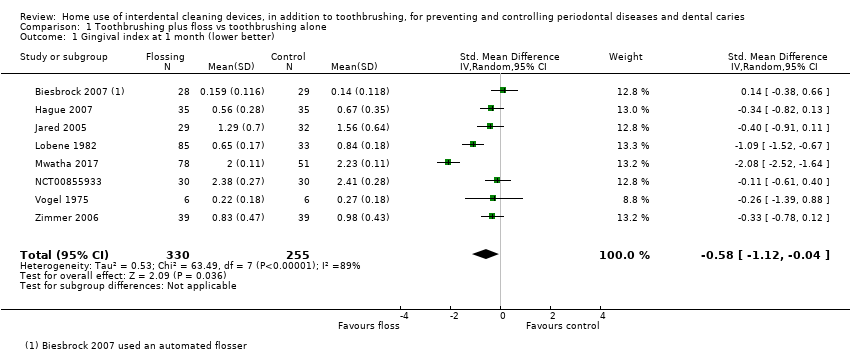
Comparison 1 Toothbrushing plus floss vs toothbrushing alone, Outcome 1 Gingival index at 1 month (lower better).

Comparison 1 Toothbrushing plus floss vs toothbrushing alone, Outcome 2 Gingival index 3 months (lower better).

Comparison 1 Toothbrushing plus floss vs toothbrushing alone, Outcome 3 Gingival index at 6 months (lower better).

Comparison 1 Toothbrushing plus floss vs toothbrushing alone, Outcome 4 Bleeding at 1 month (lower better).
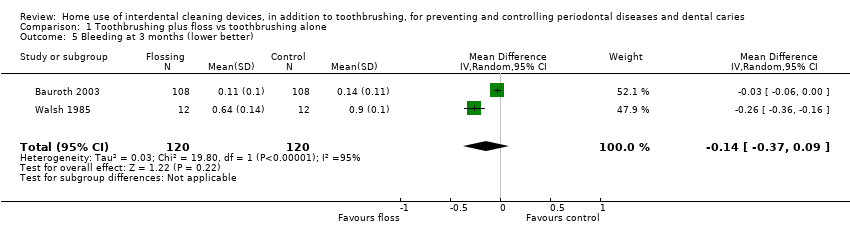
Comparison 1 Toothbrushing plus floss vs toothbrushing alone, Outcome 5 Bleeding at 3 months (lower better).

Comparison 1 Toothbrushing plus floss vs toothbrushing alone, Outcome 6 Bleeding at 6 months (lower better).
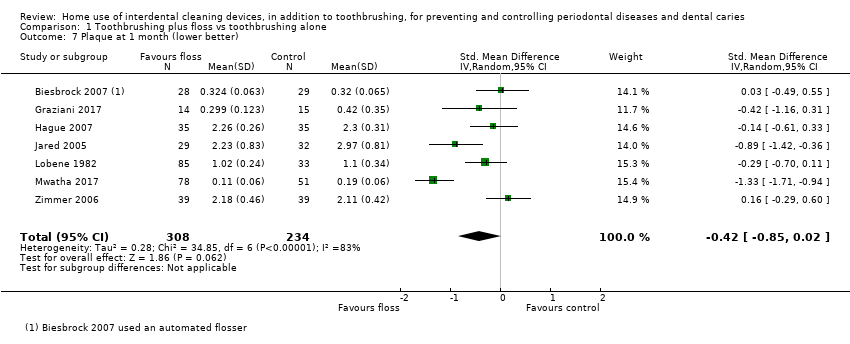
Comparison 1 Toothbrushing plus floss vs toothbrushing alone, Outcome 7 Plaque at 1 month (lower better).

Comparison 1 Toothbrushing plus floss vs toothbrushing alone, Outcome 8 Plaque at 3 months (lower better).

Comparison 1 Toothbrushing plus floss vs toothbrushing alone, Outcome 9 Plaque at 6 months (lower better).
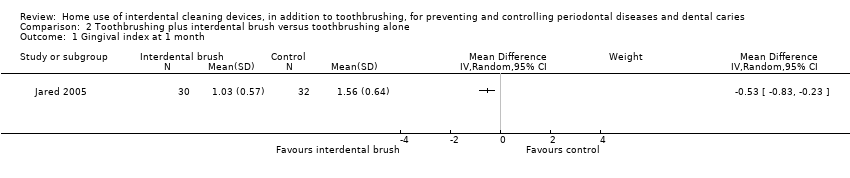
Comparison 2 Toothbrushing plus interdental brush versus toothbrushing alone, Outcome 1 Gingival index at 1 month.

Comparison 2 Toothbrushing plus interdental brush versus toothbrushing alone, Outcome 2 Bleeding at 1 month.
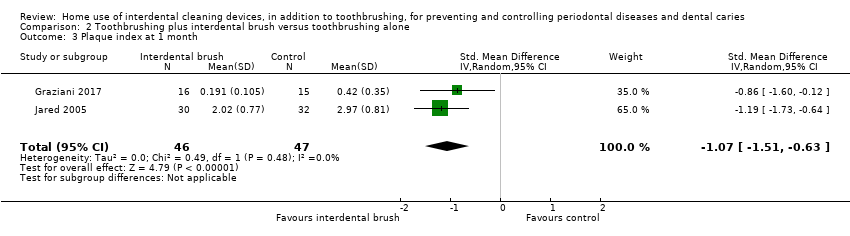
Comparison 2 Toothbrushing plus interdental brush versus toothbrushing alone, Outcome 3 Plaque index at 1 month.
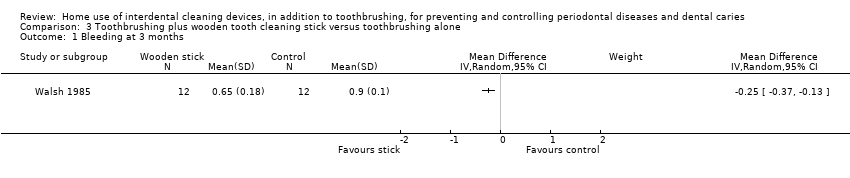
Comparison 3 Toothbrushing plus wooden tooth cleaning stick versus toothbrushing alone, Outcome 1 Bleeding at 3 months.
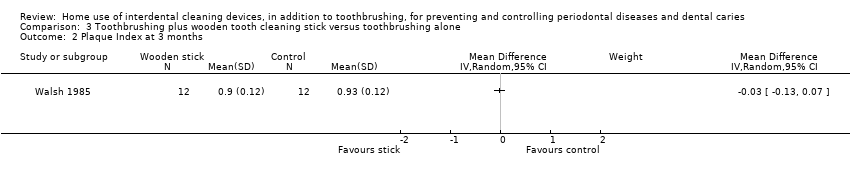
Comparison 3 Toothbrushing plus wooden tooth cleaning stick versus toothbrushing alone, Outcome 2 Plaque Index at 3 months.

Comparison 4 Toothbrushing plus rubber/elastomeric tooth cleaning stick versus toothbrushing alone, Outcome 1 Gingival Index at 1 month.
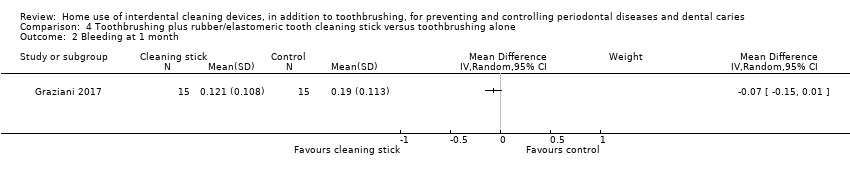
Comparison 4 Toothbrushing plus rubber/elastomeric tooth cleaning stick versus toothbrushing alone, Outcome 2 Bleeding at 1 month.

Comparison 4 Toothbrushing plus rubber/elastomeric tooth cleaning stick versus toothbrushing alone, Outcome 3 Plaque Index at 1 month.

Comparison 5 Toothbrushing plus oral irrigation versus toothbrushing alone, Outcome 1 Gingivitis at 1 month (lower better).
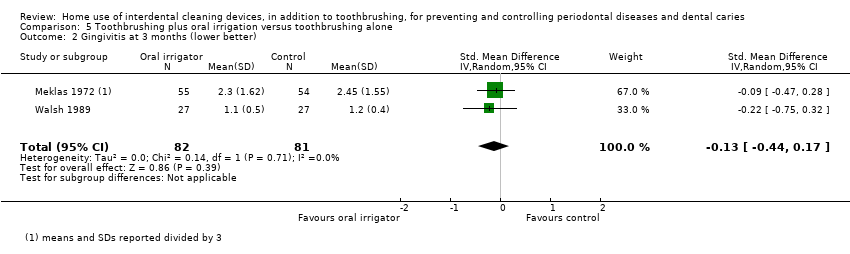
Comparison 5 Toothbrushing plus oral irrigation versus toothbrushing alone, Outcome 2 Gingivitis at 3 months (lower better).
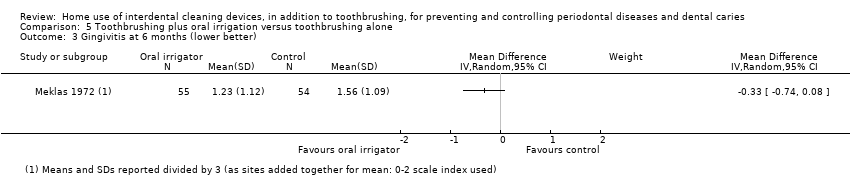
Comparison 5 Toothbrushing plus oral irrigation versus toothbrushing alone, Outcome 3 Gingivitis at 6 months (lower better).
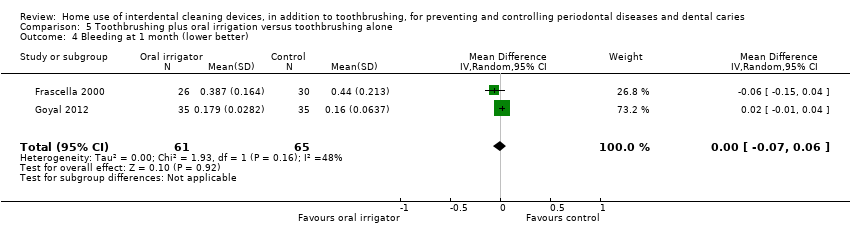
Comparison 5 Toothbrushing plus oral irrigation versus toothbrushing alone, Outcome 4 Bleeding at 1 month (lower better).
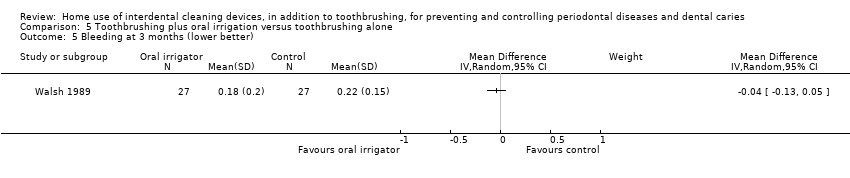
Comparison 5 Toothbrushing plus oral irrigation versus toothbrushing alone, Outcome 5 Bleeding at 3 months (lower better).
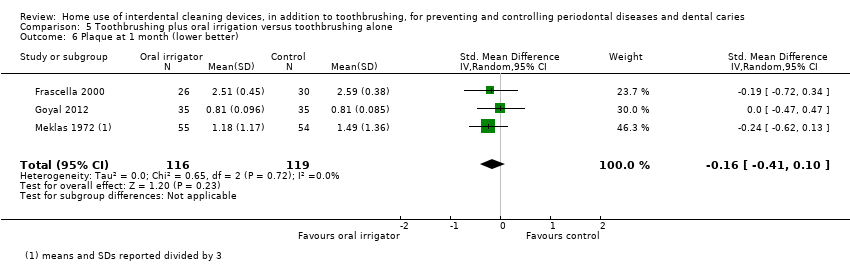
Comparison 5 Toothbrushing plus oral irrigation versus toothbrushing alone, Outcome 6 Plaque at 1 month (lower better).

Comparison 5 Toothbrushing plus oral irrigation versus toothbrushing alone, Outcome 7 Plaque at 3 months (lower better).
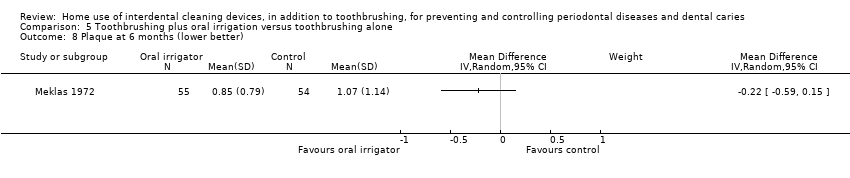
Comparison 5 Toothbrushing plus oral irrigation versus toothbrushing alone, Outcome 8 Plaque at 6 months (lower better).
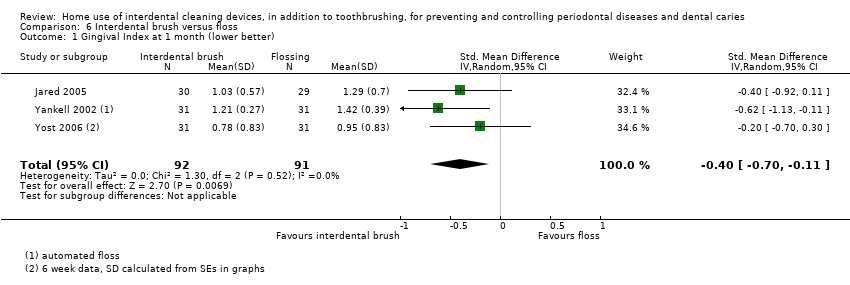
Comparison 6 Interdental brush versus floss, Outcome 1 Gingival Index at 1 month (lower better).

Comparison 6 Interdental brush versus floss, Outcome 2 Bleeding at 4/6 weeks.

Comparison 6 Interdental brush versus floss, Outcome 3 Bleeding at 3 months.

Comparison 6 Interdental brush versus floss, Outcome 4 Probing pocket depth at 4 to 6 weeks.
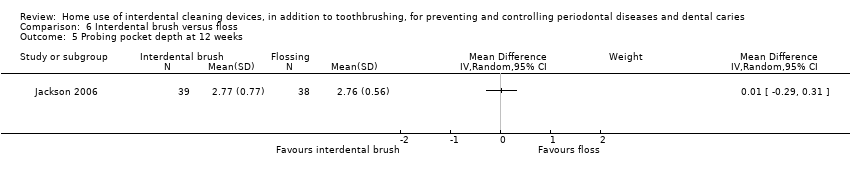
Comparison 6 Interdental brush versus floss, Outcome 5 Probing pocket depth at 12 weeks.

Comparison 6 Interdental brush versus floss, Outcome 6 Plaque at 1 month (lower better) (parallel group studies).

Comparison 6 Interdental brush versus floss, Outcome 7 Plaque at 1 month (split‐mouth studies).
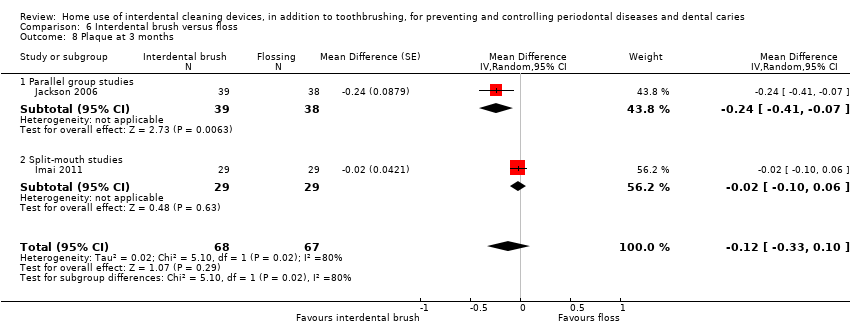
Comparison 6 Interdental brush versus floss, Outcome 8 Plaque at 3 months.
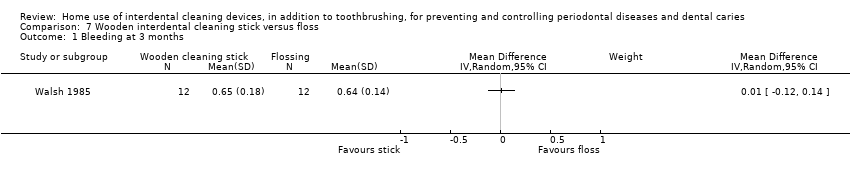
Comparison 7 Wooden interdental cleaning stick versus floss, Outcome 1 Bleeding at 3 months.

Comparison 7 Wooden interdental cleaning stick versus floss, Outcome 2 Plaque index at 3 months.

Comparison 8 Rubber/elastomeric interdental cleaning stick versus floss, Outcome 1 Gingival index at 1 month/6 weeks.

Comparison 8 Rubber/elastomeric interdental cleaning stick versus floss, Outcome 2 Gingival index at 3 months.

Comparison 8 Rubber/elastomeric interdental cleaning stick versus floss, Outcome 3 Bleeding at 1 month/6 weeks (lower better).
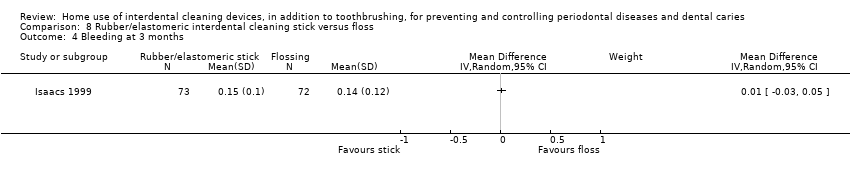
Comparison 8 Rubber/elastomeric interdental cleaning stick versus floss, Outcome 4 Bleeding at 3 months.

Comparison 8 Rubber/elastomeric interdental cleaning stick versus floss, Outcome 5 Plaque index at 1 month/6 weeks.
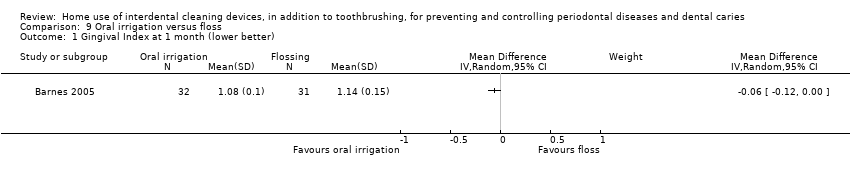
Comparison 9 Oral irrigation versus floss, Outcome 1 Gingival Index at 1 month (lower better).

Comparison 9 Oral irrigation versus floss, Outcome 2 Bleeding at 1 month (lower better).

Comparison 9 Oral irrigation versus floss, Outcome 3 Plaque Index at 1 month (lower better).
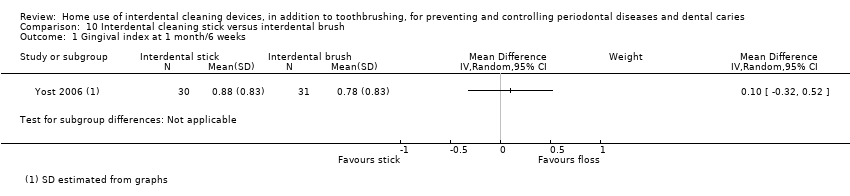
Comparison 10 Interdental cleaning stick versus interdental brush, Outcome 1 Gingival index at 1 month/6 weeks.

Comparison 10 Interdental cleaning stick versus interdental brush, Outcome 2 Bleeding at 1 month/6 weeks.

Comparison 10 Interdental cleaning stick versus interdental brush, Outcome 3 Plaque index at 1 month/6 weeks.
| Flossing plus toothbrushing for periodontal disease and dental caries in adults | ||||||
| Population: adults, 16 years and older Comparison: toothbrushing only | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Toothbrushing only | Flossing plus toothbrushing | |||||
| Gingivitis measured by gingival index SD units: investigators measured gingivitis using different scales Lower score means less severe gingivitis Follow‐up: 1 month | The gingivitis score in the flossing group was on average 0.58 SDs lower (95% CI 0.04 lower to 1.12 lower) than the control group | ‐ | 585 | ⊕⊕⊝⊝ | Flossing also reduced gingivitis at 3 months (‐0.33, ‐0.50 to ‐0.17, 4 studies, 570 participants) and 6 months (‐0.68, ‐0.95 to ‐0.42, 4 studies, 564 participants). | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 1 month | The median score in the control group was 0.16 | The mean score in the intervention group was 0.03 less (0.14 less to 0.08 more) | ‐ | 158 (2 studies) | ⊕⊝⊝⊝ | 3‐month follow‐up: ‐0.14 (‐0.37 to 0.09, 2 studies, 240 participants) 6‐month follow‐up: ‐0.06 (‐0.09 to ‐0.03; 1 study, 210 participants) |
| Periodontitis | One study measured probing pocket depth but no data were reported. | |||||
| Interproximal caries | No included study assessed caries as an outcome. | |||||
| Plaque SD units: investigators measured plaque using different scales Lower score means less plaque Follow‐up: 1 month | The plaque score in flossing group was on average 0.42 SDs lower (0.85 lower to 0.02 higher) than the control group | ‐ | 542 | ⊕⊝⊝⊝ | Significant difference found for plaque at 3 months (SMD 0.20, ‐0.36 to ‐0.04, 5 studies, 594 participants), but not at 6 months (‐0.13, ‐0.30 to 0.05, 3 studies, 487 participants). | |
| Harms and adverse effects | Adverse effects were assessed and reported in seven studies. Three reported no adverse events on the oral hard or soft tissues. Four reported sporadic adverse events with mild severity, with no evidence of a difference between the flossing plus toothbrushing group and toothbrushing only group. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to high and unclear risk of bias in the studies and substantial heterogeneity 2 Downgraded three levels due to high and unclear risk of bias in the studies, substantial heterogeneity and lack of precision in the estimate | ||||||
| Interdental brushing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Toothbrushing only | Interdental brush plus toothbrushing | |||||
| Gingivitis measured by gingival index SD units: investigators measure gingivitis using different scales Lower score means less severe gingivitis Follow‐up: 1 month | The gingivitis score in interdental brush group was on average 0.53 SDs lower (0.23 to 0.83 lower) than the control group | ‐ | 62 | ⊕⊝⊝⊝ | ||
| Gingivitis measured by proportion of bleeding sites Follow‐up: 1 month | The mean score in the control group was 0.19 | The mean score in the interdental brush group was 0.05 less (0.13 less to 0.03 more) | ‐ | 31 (1 study) | ⊕⊕⊝⊝ | |
| Periodontitis | One study measured probing pocket depth but no data were reported. | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: investigators measure plaque using different scales Lower score means less plaque Follow‐up: 1 month | The plaque score in the interdental brush group was on average 1.07 SDs lower (0.63 to 1.51 lower) than the control group | ‐ | 93 | ⊕⊕⊝⊝ | ||
| Harms and adverse outcomes | Neither study reported any information about adverse events. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to being based on only one small trial at unclear risk of bias 2 Downgraded three levels due to being based on only one small trial at unclear risk of bias 3 Downgraded two levels due to being based on only two small trials at unclear risk of bias | ||||||
| Wooden interdental cleaning stick compared to flossing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Toothbrushing alone | Wooden cleaning stick plus toothbrushing | |||||
| Gingivitis measured by gingival index | Not measured | ‐ | ‐ | ‐ | ‐ | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 3 months | The mean gingivitis score in the control group was 0.90 | The mean gingivitis score in the intervention group was | ‐ | 24 (1 study) | ⊕⊝⊝⊝ | 3‐month data only |
| Periodontitis | No included study assessed periodontitis as an outcome | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque Follow‐up: 3 months | The mean plaque in the control group was 0.22 | The mean plaque score in the intervention group was | ‐ | 24 | ⊕⊝⊝⊝ | 3‐month data only |
| Harms and adverse outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to there being only one small trial at unclear risk of bias 2 Downgraded three levels due to there being only one small trial, at unclear risk of bias, and lack of precision in the estimate | ||||||
| Interdental cleaning stick compared to flossing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Toothbrush alone | Cleaning stick plus toothbrushing | |||||
| Gingivitis measured by gingival index Lower score means less severe gingivitis Follow‐up: 1 month | The mean score in the control group was 0.22 | The mean score in the intervention group was on average 0.01 lower (0.19 lower to 0.21 higher) than the control group.1 | ‐ | 12 | ⊕⊝⊝⊝ | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 1 month | The mean score in the control group was 0.19 | The mean score in the intervention group was 0.07 lower (0.15 lower to 0.01 higher) | ‐ | 30 (1 study) | ⊕⊝⊝⊝ | |
| Periodontitis | One study measured probing pocket depth but no data were reported. | |||||
| Interproximal caries | No included study assessed caries as an outcome. | |||||
| Plaque (proportion of sites with plaque) Follow‐up: 1 month | The mean plaque in the control group was 0.42 | The mean plaque score in the intervention group was | ‐ | 30 | ⊕⊝⊝⊝ | |
| Harms and adverse outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to being based on single small study at high risk of bias, and lack of precision in the estimate | ||||||
| Oral irrigation plus toothbrushing compared to toothbrushing alone for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Toothbrushing alone | Oral irrigation plus toothbrushing | |||||
| Gingivitis measured by gingival index SD units: investigators measure gingivitis using different scales Lower score means less severe gingivitis Follow‐up: 1 month | The gingivitis score in oral irrigation group was on average 0.48 SDs lower (0.06 lower to 0.89 lower) than the control group. | ‐ | 380 | ⊕⊝⊝⊝ | No significant evidence of a difference at 3 months (SMD ‐0.13, ‐0.44 to 0.17; 2 trials, 163 participants) or 6 months (MD ‐0.33, ‐0.74 to 0.08; 1 trial, 109 participants) | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 1 month | The mean score in the control group was 0.30 | The mean score in the intervention group was the same (0.07 lower to 0.06 higher) | ‐ | 126 (2 studies) | ⊕⊕⊝⊝ | Nor any evidence of a difference at 3 months (MD ‐0.04, ‐0.13 to 0.05, 1 study, 54 participants) |
| Periodontitis | Measured in one study but useable data not provided | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: Lower score means less plaque. Follow‐up: 1 month | The plaque score in the oral irrigation group was on average 0.16 SDs lower (0.41 lower to 0.10 higher)1 than the control group | ‐ | 235 | ⊕⊕⊝⊝ | Nor did the evidence suggest benefit from the oral irrigator at 3 months (SMD 0.06, ‐0.25 to 0.37; 2 studies, 163 participants) or 6 months (MD 0.22, ‐0.59 to 0.15; 1 study, 109 participants) | |
| Harms and adverse outcomes | Three studies reported that there were no adverse events, one reported one incidence of aphthous ulcer in irrigator group, one reported oral lacerations but found no difference between the interventions, and one did not measure adverse events. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels as studies at unclear risk of bias, with substantial heterogeneity and imprecise estimate | ||||||
| Interdental brushing compared to flossing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Flossing | Interdental brush (IDB) | |||||
| Gingivitis measured by gingival index SD units: investigators measure gingivitis using different scales Lower score means less severe gingivitis | The gingivitis score in the IDB group was on average 0.40 SDs lower (0.11 to 0.70 lower)1than the flossing group | ‐ | 183 | ⊕⊕⊝⊝ | Not measured at 3 months | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 4 to 6 weeks | The mean score in the flossing group was 0.20 | The mean score in the IDB group was 0.06 lower (0.08 to 0.03 lower) | ‐ | 234 (6 studies) | ⊕⊕⊝⊝ | Results at 3 months also indicated a small benefit for interdental brushes: MD ‐0.10 (‐0.15 to ‐0.04), 2 studies, 106 participants. |
| Periodontitis Probing pocket depth in mm Follow‐up: 4 to 6 weeks | The mean PPD score for the flossing group was 5.01 mm | The mean PPD score in the IDB group was0.06 lower (0.27 lower to 0.16 higher) | ‐ | 107 (3 studies) | ⊕⊕⊝⊝ | Results were consistent at 3 months: MD 0.01 mm (‐0.29 to 0.31), 1 parallel‐group study, 77 participants. |
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: Lower score means less plaque | The plaque in the IDB group was on average 0.47 SDs lower (0.84 to 0.11 lower) than the flossing group | ‐ | 290 | ⊕⊝⊝⊝ | This benefit for IDB compared to flossing for parallel‐group studies is not supported by the meta‐analysis of the split‐mouth studies at one month (SMD ‐0.07 (‐0.32 to 0.18), 3 studies, 66 participants). Nor by the 3‐month data (MD ‐0.12, 95% ‐0.33 to 0.10; two trials (one parallel and one split‐mouth), 106 participants). | |
| Harms and adverse outcomes | Five studies reported there were no adverse events. Two studies reported on problems with the use of interdental brushes or floss, which sometimes caused soreness. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded two levels due to studies at unclear risk of bias, imprecise estimate (although consistent) 2 Downgraded two levels due to studies at unclear risk of bias, moderate heterogeneity 3 Downgraded two levels due to studies at unclear risk of bias, imprecise estimate 4 Downgraded three levels due to unclear risk of bias, imprecise estimates and moderate heterogeneity | ||||||
| Wooden cleaning stick compared to flossing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Flossing plus toothbrushing | Wooden cleaning stick plus toothbrushing | |||||
| Gingivitis measured by gingival index | Not measured | |||||
| Gingivitis measured by proportion of bleeding sites Follow‐up: 3 months | The mean gingivitis score in the control group was 0.64 | The mean gingivitis score in the intervention group was | ‐ | 24 (1 study) | ⊕⊝⊝⊝ | Only 3‐month data useable |
| Periodontitis | No included study assessed periodontitis | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque Follow‐up: 3 months | The mean plaque in the control group was 0.88 | The mean plaque score in the intervention group was | ‐ | 24 | ⊕⊝⊝⊝ | Only 3‐month data useable |
| Harms and adverse outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to there being only one small trial, at unclear risk of bias, and lack of precision of estimate | ||||||
| Interdental cleaning stick compared to interdental brushing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Floss | Cleaning stick | |||||
| Gingivitis measured by gingival index SD units: investigators measure gingivitis using different scales Lower score means less severe gingivitis. Follow‐up: 4 to 6 weeks | The gingivitis score in the cleaning stick group was on average | ‐ | 256 | ⊕⊝⊝⊝ | Nor was there was evidence that one intervention performed better than the other with regards to gingivitis control at 3 months (MD 0.01, 95% CI ‐0.08 to 0.10, 1 study, 145 participants). | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 4 to 6 weeks | The mean score in the floss group was 0.22 | The mean score in the cleaning stick group was 0.03 lower (0.08 lower to 0.03 higher) | ‐ | 212 (5 studies) | ⊕⊕⊝⊝ | Nor was there was evidence that one intervention performed better than the other with regards to bleeding sites at 3 months (MD 0.01, 95% CI ‐0.03 to 0.05, 1 study, 145 participants) |
| Periodontitis | One study measured periodontitis but the data were not usable | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: investigators measure plaque using different scales Lower score means less plaque Follow‐up: 4 to 6 weeks | The plaque score in the cleaning stick group was on average | ‐ | 273 | ⊕⊝⊝⊝ | ||
| Harms and adverse outcomes | Five studies assessed adverse events. One did not report findings, but the others reported either no adverse events or minor adverse events that did not significantly differ between interventions. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to one study being at high risk of bias (others unclear), moderate heterogeneity and serious imprecision 2 Downgraded two levels due to studies at unclear risk of bias and moderate heterogeneity 3 Downgraded three levels due to studies at unclear risk of bias, moderate heterogeneity and serious imprecision | ||||||
| Oral irrigation compared to flossing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Flossing | Oral irrigation | |||||
| Gingivitis measured by gingival index SD units: investigators measure gingivitis using different scales Lower score means less severe gingivitis | The mean score in the floss group was 1.14 | The mean score in the irrigator group was 0.06 lower (0.12 lower to 0.00) | ‐ | 63 | ⊕⊝⊝⊝ | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 1 month | The mean score in the floss group was 0.56 | The mean score in the irrigator group was 0.12 lower (0.19 lower to 0.05 lower) | ‐ | 133 (2 studies) | ⊕⊕⊝⊝ | |
| Periodontitis | No included study assessed periodontitis | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: investigators measure plaque using different scales Lower score means less plaque | The plaque in the oral irrigation group was on average | ‐ | 133 | ⊕⊝⊝⊝ | ||
| Harms and adverse outcomes | Both studies reported there were no adverse events in either study group. | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to single small study at unclear risk of bias 2 Downgraded three levels due to single small study at unclear risk of bias with serious imprecision | ||||||
| Interdental cleaning stick compared to interdental brushing for periodontal diseases and dental caries in adults | ||||||
| Population: adults, 16 years and older | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Certainty of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| IDB | Stick | |||||
| Gingivitis measured by gingival index Lower score means less severe gingivitis Follow‐up: 4 to 6 weeks | The mean score in the interdental brush group was 0.78 | The mean score in the cleaning stick group was 0.10 (0.32 lower to 0.52 higher) | ‐ | 61 | ⊕⊝⊝⊝ | |
| Gingivitis measured by proportion of bleeding sites Follow‐up: 4 to 6 weeks | The mean score in the interdental brush group was 0.14 | The mean score in the cleaning stick group was 0.02 lower (0.10 lower to 0.06 higher) | ‐ | 31 (1 study) | ⊕⊝⊝⊝ | |
| Periodontitis | Two studies measured periodontitis but data not presented or usable | |||||
| Interproximal caries | No included study assessed caries as an outcome | |||||
| Plaque SD units: investigators measure plaque using different scales Lower score means less plaque Follow‐up: 4 to 6 weeks | The plaque score in the cleaning stick group was on average | ‐ | 92 | ⊕⊝⊝⊝ | ||
| Harms and adverse outcomes | Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1 Downgraded three levels due to single study at unclear risk of bias and serious imprecision 2 Downgraded three levels due to single study at unclear risk of bias and imprecision 3 Downgraded three levels due to 2 small studies at unclear risk of bias and serious imprecision | ||||||
| As we were aware that caries increment could be reported differently in different trials, we developed a set of a priori rules to choose the primary outcome data (decayed, missing or filled surfaces (D(M)FS)) for analysis from each study, drawing on Marinho 2013: DFS data would be chosen over DMFS data, and these would be chosen over DS or FS; data for 'all surface types combined' would be chosen over data for 'specific types' only; data for 'all erupted and erupting teeth combined' would be chosen over data for 'erupted' only, and these over data for 'erupting' only; data from 'clinical and radiological examinations combined' would be chosen over data from 'clinical' only, and these over 'radiological' only; data for dentinal/cavitated caries lesions would be chosen over data for enamel/non‐cavitated lesions; net caries increment data would be chosen over crude (observed) increment data; and follow‐up nearest to three years (often the one at the end of the treatment period) would be chosen over all other lengths of follow‐up, unless otherwise stated. When no specification was provided with regard to the methods of examination adopted, diagnostic thresholds used, groups of teeth and types of tooth eruption recorded, and approaches for reversals adopted, the primary choices described above were assumed. |
| Parallel studies | Number of study arms | Number used in review analyses |
| Graziani 2017 | 4 | 4 |
| Lobene 1982 | 4 | 4 |
| Smith 1988 | 4 | 4 |
| Finkelstein 1990* | 5 | 3 |
| Jared 2005 | 5 | 3 |
| Vogel 1975 | 4 | 3 |
| Yost 2006 | 4 | 3 |
| Barnes 2005 | 3 | 3 |
| Hague 2007 | 3 | 3 |
| Walsh 1985 | 3 | 3 |
| Biesbrock 2007 | 6 | 2 |
| Goyal 2012 | 4 | 2 |
| Mwatha 2017 | 4 | 2 |
| NCT01250769 | 4 | 2 |
| Walsh 1989 | 4 | 2 |
| Zimmer 2006 | 4 | 2 |
| Bauroth 2003 | 3 | 2 |
| Cronin 2005 | 3 | 2 |
| Rosema 2008 | 3 | 2 |
| Rosema 2011 | 3 | 2 |
| Schiff 2006 | 3 | 2 |
| Sharma 2002 | 3 | 2 |
| Cronin 1997 | 2 | 2 |
| Frascella 2000 | 2 | 2 |
| Gordon 1996 | 2 | 2 |
| Isaacs 1999 | 2 | 2 |
| Jackson 2006 | 2 | 2 |
| Kazmierczak 1994 | 2 | 2 |
| Lewis 2004* | 2 | 2 |
| Meklas 1972 | 2 | 2 |
| NCT00855933 | 2 | 2 |
| Yankell 2002 | 2 | 2 |
| Split‐mouth studies | Number of study arms | Number used in review analyses |
| Imai 2011 | 3 | 3 |
| Christou 1998 | 2 | 2 |
| Ishak 2007 | 2 | 2 |
| *No data used | ||
| Study | Gingivitis index (scale) | Plaque index (scale) |
| Löe & Silness Gingival Index (0 to 3) Carter & Barnes Bleeding Index (0/1) | Proximal/Marginal Plaque Index (0‐5) | |
| Lobene Modified Interproximal Gingival Index (0 to 4) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index (0 to 3) | Navy Plaque Index (Rustogi modification) (0 /1) | |
| Bleeding on probing assessed by using Angulated Bleeding Index (0/1) and Periodontal Pocket Bleeding Index (0/1) | Volpe modification of Quigley and Hein Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index (0 to 3) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index (0 to 3) Löe & Silness Bleeding scores (when scoring 2 or 3 on the Löe & Silness Gingival Index) | Proximal/Marginal Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index modified to include visual assessment only (0 to 3) Eastman Interdental Bleeding Index (0/1) | Global Plaque Index (0 to 100%) | |
| Modified gingival index Angular bleeding index | Turesky‐Gilmore‐Glickman modification of the Quigley‐Hein Plaque Index | |
| Lobene Modified Gingival Index (0 to 4) Papillary Bleeding Index (0/1) | Proximal/Marginal Plaque Index (0 to 5) | |
| Lobene Modified Gingival Index (0 to 4) | Navy Plaque Index (Rustogi modification) (0/1 for each of the 9 tooth surfaces) | |
| Full Mouth Bleeding Score (0/1) Angulated Bleeding Index (0/1) | Full Mouth Plaque Score (percentage of areas containing plaque) | |
| Löe & Silness Gingival Index (0 to 3) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Eastman Interdental Bleeding Index (0/1) | Silness & Löe Plaque Index (0 to 3) (modified) | |
| Löe & Silness Gingival Index (0 to 3) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Bleeding on Probing Index (0/1) | Visible plaque deposits were scored as positive | |
| Eastman Interdental Bleeding Index (0/1) Bleeding on probing (0/1) Relative Interdental Papillae Level (mm) | Silness & Löe Plaque Index (0 to 3) | |
| Lobene Modified Gingival Index (0 to 4) Bleeding on probing (Van der Weijden modification) (+/‐) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Lobene Modified Gingival Index (0 to 4) Bleeding Index (0/1) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Eastman Interdental Bleeding Index (0/1) | O'Leary Plaque Index (0/1) Interproximal Plaque Index (0/1) | |
| Löe & Silness Gingival Index (0 to 3) | Quigley‐Hein Plaque Index (0 to 5) | |
| Russell modified Periodontal Index (0 to 2) | 3‐point plaque index (0 to 2) | |
| Lobene Modified Gingival Index (0 to 4) Gingival Bleeding Index (0/1) | Navy Plaque Index (Rustogi modification) (0/1 for each of the nine tooth surfaces) | |
| Lobene Modified Gingival Index (0 to 4) | ‐ | |
| Modified Gingival Index (0 to 4) Gingival Bleeding Index (0 to 3) | ‐ | |
| Bleeding on Marginal Probing Index (0 to 2) | Paraskevas modification of Quigley & Hein Plaque Index (0 to 5) | |
| Bleeding on Marginal Probing Index (0 to 2) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index (0 to 3) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Lobene Modified Gingival Index (0 to 4) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Löe & Silness Gingival Index (0 to 3) | Silness & Löe Plaque Index (0 to 3) | |
| Löe & Silness Gingival Index (0 to 3) Intracrevicular exudate sampling | Podchladley's Total Plaque Index (0/1) | |
| Interproximal Bleeding on Probing Index (0/1) evaluated as percentage of bleeding interproximal surfaces | Silness & Löe Plaque Index (evaluated as percentage of interproximal surfaces scored positive for plaque) (0/1) | |
| Löe & Silness Gingival Index (0 to 3) Bleeding on probing | Silness & Löe Plaque Index (0 to 3) | |
| Eastman Interdental Bleeding Index (0/1) Lobene Modified Gingival Index (0 to 4) | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Eastman Interdental Bleeding Index (0/1) Löe & Silness Gingival Index (0 to 3) | Benson modification of Quigley‐Hein Plaque Index (0 to 5) | |
| Papillary Bleeding Index (1 to 4) | Quigley & Hein Plaque Index (0 to 5) Modified Proximal Plaque Index |
| Cronin 1997 and Isaacs 1999 were supported by Braun AG, Germany (Braun Oral‐B Interclean ID2); Yankell 2002 by Dental Concepts, Paramus, USA (oral hygiene devices); Jackson 2006 and Schiff 2006 by the Colgate Palmolive Company (toothbrushes, floss and toothpaste); Meklas 1972 by the General Electric Company (Aqua Pulse Oral Irrigator); Zimmer 2006 and Ishak 2007 by GlaxoSmithKline (manual toothbrush and floss); Finkelstein 1990 by Johnson & Johnson (waxed floss); Cronin 2005 by Oral‐B (manual toothbrush and flosser); Biesbrock 2007; NCT00855933 and Rosema 2008 by Procter and Gamble (sponsorship) (DE International supplied the toothpaste for Rosema 2008); Yost 2006 and Jared 2005 by Sunstar Inc. (GUM, manual toothbrush); Barnes 2005, Goyal 2012 and Rosema 2011 by Waterpik Inc., Fort Collins, USA (oral irrigator); Hague 2007 by William Getgey Company (ultra‐flosser); and NCT01250769 was sponsored by Philips Oral Healthcare. Walsh 1989 was partially funded by Xouth, Inc, Lancaster, PA, USA. In Bauroth 2003, the authors were affiliated to industry, Pfizer; in Frascella 2000, the authors were affiliated to Braun and Procter and Gamble; and in Mwatha 2017, the authors AM, MO, SS, MW and WJ were employees of Philips (Sonicare Toothbrush). The Italian Ministry of Health and Tuscan region provided a grant to Graziani 2017; the State Scholarship Foundation of Greece grant‐aided Christou 1998 (Entra‐Lactona BV provided brushes and interdental brushes); a University of Tennessee College of Dentistry Alumni Grant was given to Lewis 2004. |
| Analysis | Studies removed (and reason) | Result | Consistency with main analysis |
| Comparison 1: floss plus toothbrushing versus toothbrushing only | |||
| 1.1 GI at 1 month | Vogel (high risk of bias relating to poor compliance; estimated standard deviations) | SMD ‐0.61, 95% CI ‐1.19 to ‐0.03; high heterogeneity (I2 = 90%; P value < 0.001); 7 studies, 573 participants | Essentially the same |
| 1.2 GI at 3 months | Barouth (high risk of attrition bias; use of negative control rinse) | SMD ‐0.30, 95% CI ‐0.62 to 0.02; no heterogeneity (I2 = 0%; P value = 0.81); 2 studies, 151 participants | Confidence interval is larger and includes possibility of floss providing no additional benefit over toothbrushing |
| 1.3 GI at 6 months | Barouth (high risk of attrition bias and use of negative control rinse) | SMD ‐0.55, 95% CI ‐0.91 to ‐0.18; no/low heterogeneity (I2 = 21%; P value = 0.26); 2 studies, 151 participants | Slightly lower estimate, with larger confidence interval |
| 1.5 Bleeding at 3 months | Barouth (high risk of attrition bias; use of negative control rinse) | MD ‐0.26, 95% CI ‐0.36 to ‐0.16; 1 study, 24 participants | Shows clear benefit for floss (main analysis is equivocal) |
| 1.8 Plaque at 3 months | Barouth (high risk of attrition bias; use of negative control rinse) and | SMD ‐0.13, 95% CI ‐0.43 to 0.17; no heterogeneity (I2 = 0%; P value = 0.49); 3 studies, 175 participants | Slightly lower estimate, with wider confidence interval that includes the possibility of no difference or slight benefit for toothbrushing only |
| 1.9 Plaque at 6 months | Barouth (high risk of attrition bias; use of negative control rinse) | MD ‐0.02, ‐0.11 to 0.07; 1 study, 74 participants | Essentially the same |
| Comparison 6: interdental brush plus toothbrushing versus floss plus toothbrushing | |||
| 6.1 GI at 1 month | Yost (estimated standard deviations) | SMD ‐0.51, 95% CI ‐0.87 to ‐0.15; no/low heterogeneity (I2 = 0%, P value = 0.56); 2 studies, 121 participants | Slightly larger effect, marginally wider confidence interval |
| 6.2 Bleeding at 4 to 6 weeks | Christou, Imai, Ishak (split‐mouth studies) | MD ‐0.10, 95% CI ‐0.15 to ‐0.05; no heterogeneity (I2 = 0%, P value = 0.78); 3 studies, 169 participants | Essentially the same |
| 6.3 Bleeding at 3 months | Imai (split‐mouth study) | MD ‐0.06, 95% CI ‐0.12 to 0.00; 1 study, 77 participants | Essentially the same, though confidence interval includes zero |
| 6.4 Plaque at 1 month | Yost (estimated standard deviations) | SMD ‐0.55, 95% CI ‐1.00 to ‐0.11; moderate heterogeneity (I2 = 62%, P value = 0.05); 4 studies, 228 participants | Essentially the same |
| 6.8 Plaque at 3 months | Imai (split‐mouth study) | MD ‐0.24, 95% CI ‐0.41 to ‐0.07; 1 study, 77 participants | Shows clear benefit for interdental brush (main analysis is equivocal) |
| Comparison 9: rubber/elastomeric cleaning stick plus toothbrushing versus floss plus toothbrushing | |||
| 9.1 GI at 1 month | Vogel (high risk of bias relating to poor compliance; estimated standard deviations) Yost (estimated standard deviations) | SMD ‐0.37, 95% CI ‐1.07 to 0.34; high heterogeneity (I2 = 80%, P value < 0.002); 4 studies, 183 participants | Slightly bigger point estimate but wider confidence interval; both analyses include all possibilities, i.e. that flossing is better or that it gives no benefit or that it is worse than toothbrushing only |
| 9.5 Plaque at 1 month | Yost (estimated standard deviations) | SMD ‐0.09, 95% CI ‐0.57 to 0.39; high heterogeneity (I2 = 65%, P value = 0.02); 5 studies, 212 participants | Essentially the same |
| Comparison 11: interdental cleaning stick plus toothbrushing versus interdental brush plus toothbrushing | |||
| 11.3 Plaque at 1 month | Yost (estimated standard deviations) | MD 0.01, 95% CI ‐0.08 to 0.09; 1 study, 31 participants | Essentially the same |
| CI: confidence interval | |||
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| High | Interproximal | Lobene Modified Interproximal Gingival Index (0 to 4) | Final score at 3 and 6 months | Final score at 3 and 6 months | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 3 and 6 months | N/R | Adverse events were assessed, but not reported. Performed soft‐tissue assessments at baseline, 3, and 6 months. | |
| Unclear | With other sites | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | ‐ | Navy Plaque Index (Rustogi modification) (0 /1) | Final score at 1 month | N/R | Reported mild gingival inflammation in the flossing plus toothbrushing group, which was resolved after few days and was not a reason to drop out | |
| High | Interproximal data presented for gingivitis and other sites for plaque | Löe & Silness Gingival Index modified to include visual assessment only (0 to 3) | No SDs and unable to estimate | ‐ | Global Plaque Index (0 to 100%) | No SDs and unable to estimate | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 1 month | Mentioned as outcome but no data reported | Did not consider adverse effects | |
| (crossover design but we used only first‐period data ‐ see Characteristics of included studies for details) | Unclear | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | ‐ | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Safety assessments were performed at each visit. Overall, two out of 76 participants enrolled in the study, both in the automated flosser group, presented with trauma of the attached gingiva in the oral or buccal areas of the posterior teeth at the second visit resulting from improper use of the flosser. |
| Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | Final score at 1 month | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Adverse events were assessed, but not reported. Participants were issued a diary to keep a log of any symptoms experienced. However, no data regarding adverse events were reported in Results. | |
| Unclear | With other sites | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | ‐ | Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Did not consider adverse effects | |
| Unclear | With other sites | Russel Modified Gingival Index (0 to 2) | Final score at 1 month | Final score at 1 month | Navy Plaque Index (Rustogi modification) (0/1 for each of the nine tooth surfaces) | Final score at 1 month | N/R | Safety assessments were carried out by clinical examinations and by evaluating participants' diary cards. Three gingival irritations and one case of gum soreness were reported in the flossing group. | |
| Unclear | With other sites | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | ‐ | N/R | ‐ | N/R | None identified | |
| Unclear | With other sites | Bleeding on Marginal Probing Index (0 to 2) | Final score at 3 and 6 months | ‐ | Paraskevas modification of Quigley & Hein Plaque Index (0 to 5) | Final score at 3 months | N/R | No adverse effects on the oral hard or soft tissues observed by the examiner or reported by the participants. Used two indices to assess possible adverse effects and found no statistically significant difference in either staining or abrasion between the flossing and toothbrushing only groups at 10 weeks, 6 months and 9 months (P < 0.05). | |
| Unclear | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 3 and 6 months | ‐ | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 3 and 6 months | N/R | No adverse effects on the oral hard or soft tissues observed by the examiner or reported by the participants | |
| High | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 3 and 6 months | ‐ | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 3 and 6 months | N/R | No adverse effects on the oral hard or soft tissues observed by the examiner or reported by the participants | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month Imputed SD from control group of studies using this index | ‐ | Podchladley's Total Plaque Index (0/1) | Unable to impute SD for this index | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | ‐ | ‐ | Final score at 3 months | Silness & Löe Plaque Index (evaluated as percentage of interproximal surfaces scored positive for plaque) (0/1) | Final score at 3 months | N/R | Did not consider adverse effects | |
| Low | Interproximal | Papillary Bleeding Index (1 to 4) | Final score at 1 month | ‐ | Quigley & Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Participants reported mild gingival abrasions in three out of 39 participants at 1‐month time point, and in one of 39 participants at 2 months. In the toothbrush‐only arm, 1 in 39 participants at 1‐month time point reported discomfort in taste and bleeding of gingiva, respectively. No side effects were reported at 2‐month time point | |
| N/R: not reported | |||||||||
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 1 month | Mentioned as outcome but no data reported | Did not consider adverse effects | |
| Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | ‐ | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Adverse events were assessed, but not reported. Participants were issued a diary to keep a log of any symptoms experienced. However, no data regarding adverse events were reported in Results. | |
| N/R: not reported | |||||||||
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| High | Interproximal data presented for gingivitis and other sites for plaque | Löe & Silness Gingival Index modified to include visual assessment only (0 to 3) | None ‐ no SDs and unable to estimate | ‐ | Global Plaque Index (0 to 100%) | None ‐ no SDs and unable to estimate | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | ‐ | ‐ | Final score at 3 months | Silness & Löe Plaque Index (evaluated as percentage of interproximal surfaces scored positive for plaque) (0/1) | Final score at 3 months | N/R | Did not consider adverse effects | |
| N/R: not reported | |||||||||
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | Interproximal | ‐ | ‐ | Final score at one month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 1 month | Mentioned as outcome but no data reported | Did not consider adverse effects | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at one month | ‐ | Podchladley's Total Plaque Index (0/1) | Unable to impute for index | N/R | Did not consider adverse effects | |
| N/R: not reported | |||||||||
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | With other sites | Modified gingival index (0 to 3) | Final score at 1 month | Final score at 1 month | Turesky‐Gilmore‐Glickman modification of the Quigley‐Hein Plaque Index | Final score at 1 month | N/R | Safety mentioned and "no problems" reported; not clear how this was assessed | |
| Unclear | Interproximal for plaque; other sites for gingivitis | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | Final score at 1 month | Navy Plaque Index (Rustogi modification) (0/1 for each of the nine tooth surfaces) | Final score at 1 month | N/R | Reported that there were no adverse effects | |
| Unclear | With other sites | Russell modified Periodontal Index (0 to 2) | Final score at 1, 3, and 6 months | ‐ | 3‐point plaque index (0 to 2) | Final score at 1, 3 and 6 months | N/R | Reported adverse events in terms of oral lacerations, with no significant difference between the study arms (toothbrushing and oral irrigation 8/55; toothbrushing only 7/54) | |
| Unclear | With other sites | Modified Gingival Index (0 to 4) | Final score at 1 month | ‐ | N/R | ‐ | N/R | 1 serious (arm deep vein thrombosis) in Gp C ‐ unrelated to treatment, and 1 minor in Gp D ‐ aphthous ulcer above tooth #7 on attached gingiva | |
| Unclear | With other sites | Löe & Silness Gingival Index (0 to 3) | Final score at 3 months (6‐month data not used) | Final score at 3 months (6‐month data not used) | Silness & Löe Plaque Index (visible plaque or not ‐ 0, 1) | Final score at 3 months (6‐month data not used) | ‐ | No injury to hard or soft tissues. No soft tissue changes. | |
| N/R: not reported | |||||||||
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 1 month | Mentioned PPD in mm as outcome but no data reported | Did not consider adverse effects | |
| Unclear | Interproximal | ‐ | ‐ | Final score at 1 and 3 months | Silness & Löe Plaque Index (0 to 3) | Final score at 1 and 3 months | PPD in mm | No adverse effects observed or reported during the study in either group | |
| Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | ‐ | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Adverse events were assessed, but not reported. Participants were issued a diary to keep a log of any symptoms experienced. However, no data regarding adverse events were reported in Results. | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Unable to use data | ‐ | Silness & Löe Plaque Index (0 to 3) | Unable to use data | PPD in mm but unable to use data | Did not consider adverse effects | |
| Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | Final score at 1 month | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | ‐ | Study reported "There were no untoward side effects, reported or observed, at any time during the study, attributed to any of the dental products distributed in this study." | |
| Unclear | Interproximal | Eastman Interdental Bleeding Index (0/1) | Final score at 1 month | ‐ | Benson modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Examinations of the oral soft tissue were performed at the final visit, but were not reported. | |
| Christou 1998 (split‐mouth design) | Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Volpe modification of Quigley and Hein Plaque Index (0 to 5) | Final score at 1 month | PPD in mm | Participants reported significantly more problems when using the floss than IDB. The most common problem was difficulty in flossing posterior areas of mouth. |
| Imai 2011 (split‐mouth design) | Low | Interproximal | ‐ | ‐ | Final score at 1 and 3 months | Silness & Löe Plaque Index (0 to 3) | Final score at 1 and 3 months | N/R | No adverse effects observed or reported during the study in either group |
| Ishak 2007 (split‐mouth design) | Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Visible plaque deposits were scored as positive | Final score at 1 month | PPD in mm | Participants encountered problems with both interventions. The IDBs tended to bend, buckle and |
| N/R: not reported | |||||||||
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| High | Interproximal data presented for gingivitis and other sites for plaque | Löe & Silness Gingival Index modified to include visual assessment only (0 to 3) | No SDs and unable to estimate | ‐ | Global Plaque Index (0 to 100%) | No SDs and unable to estimate | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | Eastman Interdental Bleeding Index (0/1) | No SDs and unable to estimate | ‐ | O'Leary Plaque Index (0/1) | No SDs and unable to estimate | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | ‐ | ‐ | Final score at 3 months | Silness & Löe Plaque Index (evaluated as percentage of interproximal surfaces scored positive for plaque) (0/1) | Final score at 3 months | N/R | Did not consider adverse effects | |
| N/R: not reported | |||||||||
| Study (parallel group design unless noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | Final score at 1 month | Turesky modification of Quigley Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | There was no significant difference in soft tissue pathology between the groups. | |
| Unclear | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | Final score at 1 month | Proximal/Marginal Plaque index (0 to 5) | Final score at 1 month | N/R | No significant differences in the proportion of hard and soft tissue abnormalities between groups were found | |
| Gordon 1996 (crossover but first‐period data only used ‐ see Characteristics of included studies for details) | Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4) | Final score at 1 month | Final score at 1 month | Proximal/Marginal Plaque index (0 to 5) | Final score at 1 month | N/R | No significant soft tissue pathology was noted in any of the participants in either group |
| Unclear | Interproximal | ‐ | ‐ | Final score at 1 month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 1 month | Mentioned as outcome but no data reported | Did not consider adverse effects | |
| Unclear | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 3 months | Final score at 3 months | Turesky modification of Quigley Hein Plaque Index (0 to 5) | Unable to use data | N/R | There was no difference in the soft tissue status of the participants in the study groups. At 6 months, healthy soft tissue was found in 66/73 and 65/72 participants in cleaning sticks versus floss groups, respectively | |
| Unclear | Interproximal | Lobene Modified Gingival Index (0 to 4 | Final score at 1 month | Final score at 1 month | Turesky modification of Quigley Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Did not consider adverse effects | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Unable to use data | ‐ | Silness & Löe Plaque Index (0 to 3) | Unable to use data | PPD in mm but unable to use data | Did not consider adverse effects | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | ‐ | Podchladley's Total Plaque Index (0/1) | Unable to impute for index | N/R | Did not consider adverse effects | |
| Unclear | Interproximal | Eastman Interdental Bleeding Index (0/1) | Final score at 6 weeks | ‐ | Benson modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 6 weeks | N/R | Examinations of the oral soft tissue were performed at the final visit, but were not reported. | |
| N/R: not reported | |||||||||
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | With other sites | Löe & Silness Gingival Index (0 to 3) | Final score at 1 month | Final score at 1 month | Proximal/Marginal Plaque Index (0 to 5) | Final score at 1 month | N/R | Reported that there were no adverse events in any study group. | |
| Unclear | With other sites | Bleeding on Marginal Probing Index (0 to 2) | Final score at 1 month | Final score at 1 month | Turesky modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 1 month | N/R | Reported that there were no adverse events in any study group. | |
| N/R: not reported | |||||||||
| Study (parallel group design unless otherwise noted) | Risk of bias assessment | Interproximal sites only or with other sites | Gingivitis index (scale) | Gingivitis final score or change in score, time points | Bleeding Index (0 or 1) time points | Plaque index (scale) | Plaque final score or change in score, time points | Probing depth change | Adverse events |
| Unclear | Interproximal | Full Mouth Bleeding Score (0/1) | Final score at 6 weeks | Final score at 1 month | Full Mouth Plaque Score (percentage of areas containing plaque) | Final score at 6 weeks | Mentioned as outcome but no data reported | Did not consider adverse effects | |
| High | Interproximal | Löe & Silness Gingival Index (0 to 3) | Unable to use data | ‐ | Silness & Löe Plaque Index (0 to 3) | Unable to use data | PPD in mm but unable to use data | Did not consider adverse effects | |
| Unclear | Interproximal | Eastman Interdental Bleeding Index (0/1) | Final score at 6 weeks | ‐ | Benson modification of Quigley‐Hein Plaque Index (0 to 5) | Final score at 6 weeks | N/R | Examinations of the oral soft tissue were performed at the final visit, but were not reported. | |
| IDB: interdental brush | |||||||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingival index at 1 month (lower better) Show forest plot | 8 | 585 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.12, ‐0.04] |
| 2 Gingival index 3 months (lower better) Show forest plot | 4 | 570 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.50, ‐0.17] |
| 3 Gingival index at 6 months (lower better) Show forest plot | 4 | 564 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐0.95, ‐0.42] |
| 4 Bleeding at 1 month (lower better) Show forest plot | 2 | 158 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.14, 0.08] |
| 5 Bleeding at 3 months (lower better) Show forest plot | 2 | 240 | Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.37, 0.09] |
| 6 Bleeding at 6 months (lower better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7 Plaque at 1 month (lower better) Show forest plot | 7 | 542 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐0.85, 0.02] |
| 8 Plaque at 3 months (lower better) Show forest plot | 5 | 594 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.36, ‐0.04] |
| 9 Plaque at 6 months (lower better) Show forest plot | 3 | 487 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.09, 0.03] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingival index at 1 month Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2 Bleeding at 1 month Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3 Plaque index at 1 month Show forest plot | 2 | 93 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐1.51, ‐0.63] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Bleeding at 3 months Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2 Plaque Index at 3 months Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingival Index at 1 month Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2 Bleeding at 1 month Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3 Plaque Index at 1 month Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingivitis at 1 month (lower better) Show forest plot | 4 | 380 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.89, ‐0.06] |
| 2 Gingivitis at 3 months (lower better) Show forest plot | 2 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.44, 0.17] |
| 3 Gingivitis at 6 months (lower better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4 Bleeding at 1 month (lower better) Show forest plot | 2 | 126 | Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐0.07, 0.06] |
| 5 Bleeding at 3 months (lower better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6 Plaque at 1 month (lower better) Show forest plot | 3 | 235 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.41, 0.10] |
| 7 Plaque at 3 months (lower better) Show forest plot | 2 | 163 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.25, 0.37] |
| 8 Plaque at 6 months (lower better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingival Index at 1 month (lower better) Show forest plot | 3 | 183 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.70, ‐0.11] |
| 2 Bleeding at 4/6 weeks Show forest plot | 6 | 299 | Mean Difference (Random, 95% CI) | ‐0.06 [‐0.08, ‐0.03] |
| 2.1 Parallel‐group studies | 3 | 169 | Mean Difference (Random, 95% CI) | ‐0.10 [‐0.15, ‐0.05] |
| 2.2 Split‐mouth studies | 3 | 130 | Mean Difference (Random, 95% CI) | ‐0.04 [‐0.07, ‐0.02] |
| 3 Bleeding at 3 months Show forest plot | 2 | 135 | Mean Difference (Random, 95% CI) | ‐0.10 [‐0.15, ‐0.04] |
| 3.1 Parallel‐group studies | 1 | 77 | Mean Difference (Random, 95% CI) | ‐0.06 [‐0.12, 0.00] |
| 3.2 Split‐mouth studies | 1 | 58 | Mean Difference (Random, 95% CI) | ‐0.12 [‐0.13, ‐0.11] |
| 4 Probing pocket depth at 4 to 6 weeks Show forest plot | 3 | 137 | Mean Difference (Random, 95% CI) | ‐0.06 [‐0.27, 0.16] |
| 4.1 Parallel‐group studies | 1 | 77 | Mean Difference (Random, 95% CI) | 0.01 [‐0.28, 0.30] |
| 4.2 Split‐mouth studies | 2 | 60 | Mean Difference (Random, 95% CI) | ‐0.13 [‐0.44, 0.18] |
| 5 Probing pocket depth at 12 weeks Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6 Plaque at 1 month (lower better) (parallel group studies) Show forest plot | 5 | 290 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.84, ‐0.11] |
| 7 Plaque at 1 month (split‐mouth studies) Show forest plot | 3 | Std. Mean Difference (Random, 95% CI) | ‐0.07 [‐0.32, 0.18] | |
| 8 Plaque at 3 months Show forest plot | 2 | 135 | Mean Difference (Random, 95% CI) | ‐0.12 [‐0.33, 0.10] |
| 8.1 Parallel group studies | 1 | 77 | Mean Difference (Random, 95% CI) | ‐0.24 [‐0.41, ‐0.07] |
| 8.2 Split‐mouth studies | 1 | 58 | Mean Difference (Random, 95% CI) | ‐0.02 [‐0.10, 0.06] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Bleeding at 3 months Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2 Plaque index at 3 months Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingival index at 1 month/6 weeks Show forest plot | 6 | 256 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.69, 0.24] |
| 1.1 Manual sticks | 3 | 93 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.89, 0.56] |
| 1.2 Powered sticks | 3 | 163 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.36, 0.37] |
| 2 Gingival index at 3 months Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3 Bleeding at 1 month/6 weeks (lower better) Show forest plot | 5 | 212 | Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.08, 0.03] |
| 3.1 Manual sticks | 2 | 49 | Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.16, 0.06] |
| 3.2 Powered sticks | 3 | 163 | Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.07, 0.05] |
| 4 Bleeding at 3 months Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5 Plaque index at 1 month/6 weeks Show forest plot | 6 | 273 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.46, 0.29] |
| 5.1 Manual sticks | 3 | 110 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.72, 0.07] |
| 5.2 Powered sticks | 3 | 163 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.41, 0.70] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingival Index at 1 month (lower better) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2 Bleeding at 1 month (lower better) Show forest plot | 2 | 133 | Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.19, ‐0.05] |
| 3 Plaque Index at 1 month (lower better) Show forest plot | 2 | 133 | Std. Mean Difference (IV, Random, 95% CI) | 0.31 [‐0.08, 0.70] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Gingival index at 1 month/6 weeks Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2 Bleeding at 1 month/6 weeks Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3 Plaque index at 1 month/6 weeks Show forest plot | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.33, 0.49] |

