Amilasa en el líquido de drenaje para el diagnóstico de la fuga pancreática en la resección post‐pancreática
Información
- DOI:
- https://doi.org/10.1002/14651858.CD012009.pub2Copiar DOI
- Base de datos:
-
- Cochrane Database of Systematic Reviews
- Versión publicada:
-
- 07 abril 2017see what's new
- Tipo:
-
- Diagnostic
- Etapa:
-
- Review
- Grupo Editorial Cochrane:
-
Grupo Cochrane de Salud digestiva
- Copyright:
-
- Copyright © 2017 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Cifras del artículo
Altmetric:
Citado por:
Autores
Contributions of authors
TD independently screened the literature, extracted and analysed data. TD also wrote the first draft of the review based on a previously published protocol as per part of a MSc project in Evidence‐based Healthcare.
KS Gurusamy wrote the protocol, independently screened the literature, extracted data, and guided and supervised TD. He also revised the review draft significantly after submission of the MSc project.
M Yaghoobi and BR Davidson critically commented on the review.
Sources of support
Internal sources
-
University College London, UK.
Support salary, consumables (including printing, photocopying), and equipment (including laptop, scanner, printer, and any other equipment) necessary to complete the review in addition to payment for editorial support.
External sources
-
National Institute for Health Research, UK.
Support salary, consumables (including printing, photocopying), and equipment (including laptop, scanner, printer, and any other equipment) necessary to complete the review in addition to payment for editorial support.
Declarations of interest
This report is independent research funded by the National Institute for Health Research (NIHR Cochrane Programme Grants, 13/89/03 ‐ Evidence‐based diagnosis and management of upper digestive, hepato‐biliary, and pancreatic disorders). The views expressed in this publication are those of the author(s) and not necessarily those of the National Health Service, the NIHR or the Department of Health.
TBUD: none known.
MY: none known.
BD: none known.
KSG: none known.
Acknowledgements
We thank the Cochrane Upper Gastrointestinal and Pancreatic Diseases (UGPD) Group, the United Kingdom Support Unit for Diagnostic Test Accuracy (DTA) Reviews, and the DTA editorial team for their advice in the preparation of this review. We also thank the librarians at Knowledge Centre, Bodleian Health Care Libraries, University of Oxford for supporting the author/student TD with a laptop and obtaining full texts of articles.
Version history
| Published | Title | Stage | Authors | Version |
| 2017 Apr 07 | Amylase in drain fluid for the diagnosis of pancreatic leak in post‐pancreatic resection | Review | Tsetsegdemberel Bat‐Ulzii Davidson, Mohammad Yaghoobi, Brian R Davidson, Kurinchi Selvan Gurusamy | |
| 2015 Dec 18 | Pancreatic amylase in drain fluid for the diagnosis of pancreatic leak in post pancreatic resection | Protocol | Kurinchi Selvan Gurusamy, Mohammad Yaghoobi, Brian R Davidson | |
Differences between protocol and review
-
Because of the lack of any studies using the reference standards described in the protocol, we accepted ISGPF grades B and C POPF as reference standards. People with grade C POPF require surgery while those with grade B POPF usually do not undergo surgery and may require minimally invasive drainage (Bassi 2005). These people with grade B POPF do not have sepsis but have localised intra‐abdominal infection. Although the intra‐abdominal infections are usually because of pancreatic leaks in people undergoing pancreatic resection (these leaks are usually at least partially 'contained' (i.e. the effects limited) by the body's defence mechanism), one cannot be sure that the intra‐abdominal infection was because of pancreatic leak. So, the reference standards used in this review might misclassify the target condition of pancreatic leak.
-
We searched MEDLINE through OvidSP platform rather than the PubMed platform. This was to avoid limitations of the search strategy in truncating the words searched to 600 variations when truncation terms were used.
Keywords
MeSH
Medical Subject Headings (MeSH) Keywords
Medical Subject Headings Check Words
Aged; Female; Humans; Male; Middle Aged;
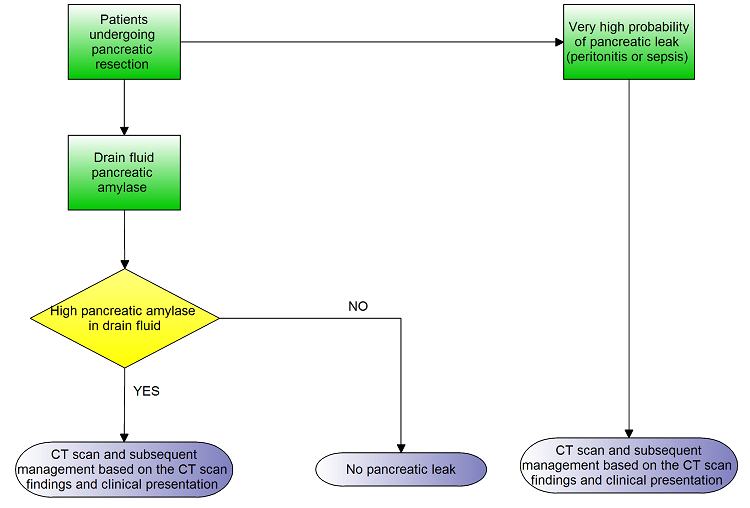
Clinical pathway

Study flow diagram.

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study

Forest plot of tests: The numbers following POD (postoperative day) indicate the number of the postoperative day. The numbers or text following DFA (drain fluid amylase) indicate the threshold. The drain fluid amylase measured on 5th postoperative day using a threshold of more than three times serum amylase provides the best sensitivity with high specificity. However, this is based on a single study with small sample size. Another study which used the same threshold between 3 days and 5 days has much less diagnostic test accuracy introducing significant uncertainty in the findings.

Plot of sensitivity and specificity in the ROC (receiver operating characteristics) space: The numbers following POD (postoperative day) indicate the number of the postoperative day. The numbers or text following DFA (drain fluid amylase) indicate the threshold. The drain fluid amylase measured on 5th postoperative day using a threshold of more than three times serum amylase provides the best sensitivity with high specificity. However, this is based on a single study with small sample size. Another study which used the same threshold between 3 days and 5 days has much less diagnostic test accuracy introducing significant uncertainty in the findings.

POD:3 DFA > 600 IU/L.

POD:3 to 5 DFA > 3 times serum amylase.

POD:4 DFA > 647 U/L.

POD:5 DFA > 3 times serum amylase.
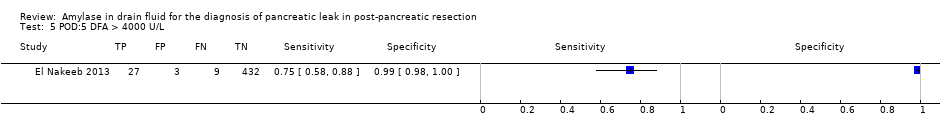
POD:5 DFA > 4000 U/L.
| Population | People undergoing pancreatic resection | ||||||||
| Setting | Secondary care in various countries | ||||||||
| Target condition | Clinically significant pancreatic leak | ||||||||
| Reference standard | International Study Group on Pancreatic Fistula (ISGPF) grade B or C | ||||||||
| Median prevalence of pancreatic leak | 15.9% | ||||||||
| Index test1 | Sensitivity | Specificity | Post‐test probability of a positive test2 | Post‐test probability of a negative test2 | Number of studies | Number of participants | Risk of bias | Applicability concerns | Plain language interpretation |
| POD:3 DFA > 600 IU/L | 0.86 (95% CI 0.68 to 0.96) | 0.73 (95% CI 0.65 to 0.80) | 37.9% (95% CI 31.1% to 45.1%) | 3.4% (95% CI 1.4% to 8.2%) | 1 | 182 | Unclear | High | At the median pre‐test probability of 16%, out of 100 people with positive test, 38 people (95% CI 31 to 45) have clinically significant pancreatic leak. At the same pre‐test probability, out of 100 people with negative test, 3 people (95% CI 1 to 8) have clinically significant pancreatic leak. |
| POD:3 to 5 DFA > 3 times serum amylase | 0.79 (95% CI 0.49 to 0.95) | 0.78 (95% CI 0.65 to 0.89) | 40.8% (95% CI 27.7% to 55.5%) | 4.9% (1.8% to 12.5%) | 1 | 65 | High | High | At the median pre‐test probability of 16%, out of 100 people with positive test, 41 people (95% CI 28 to 56) have clinically significant pancreatic leak. At the same pre‐test probability, out of 100 people with negative test, 5 people (95% CI 2 to 13) have clinically significant pancreatic leak. |
| POD:4 DFA > 647 U/L | 0.72 (95% CI 0.53 to 0.86) | 0.91 (95% CI 0.82 to 0.97) | 60.7% (95% CI 41.1% to 77.4%) | 5.5% (95% CI 3.2% to 9.3%) | 1 | 100 | High | High | At the median pre‐test probability of 16%, out of 100 people with positive test, 61 people (95% CI 41 to 77) have clinically significant pancreatic leak. At the same pre‐test probability, out of 100 people with negative test, 6 people (95% CI 3 to 9) have clinically significant pancreatic leak. |
| POD:5 DFA > 3 times serum amylase | 1.00 (95% CI 0.29 to 1.00) | 0.94 (95% CI 0.82 to 0.99) | 74.8% (95% CI 49.8% to 89.9%) | 0% (95% CI not estimable) | 1 | 50 | Unclear | High | At the median pre‐test probability of 16%, out of 100 people with positive test, 75 people (95% CI 50 to 90) have clinically significant pancreatic leak. It was not possible to estimate the number of people with clinically significant pancreatic leak when the test was negative. |
| POD:5 DFA > 4000 U/L | 0.75 (95% CI 0.58 to 0.88) | 0.99 (95% CI 0.98 to 1.00) | 95.4% (95% CI 86.8% to 98.5%) | 4.6% (95% CI 2.6% to 7.8%) | 1 | 471 | High | High | At the median pre‐test probability of 16%, out of 100 people with positive test, 95 people (95% CI 87 to 99) have clinically significant pancreatic leak. At the same pre‐test probability, out of 100 people with negative test, 5 people (95% CI 3 to 8) have clinically significant pancreatic leak. |
| Interpretation | The drain fluid amylase measured on 5th postoperative day using a threshold of more than three times serum amylase provides the best sensitivity with high specificity. A negative test more or less rules out pancreatic leak. However, this is based on a single study with small sample size. Another study which used the same threshold between 3 days and 5 days has much less diagnostic test accuracy introducing significant uncertainty in the findings. | ||||||||
| 1The numbers following POD (postoperative day) indicate the number of the postoperative day. The numbers or text following DFA (drain fluid amylase) indicate the threshold. 2All post‐test probabilities were calculated at the median prevalence (pre‐test probability) of pancreatic leak in the studies. At the lower quartile of the prevalence of 7.6%, the post‐test probabilities of pancreatic leak of positive POD:3 DFA > 600 IU/L, POD:3 to 5 DFA > 3 times serum amylase, POD:4 DFA > 647 U/L, POD:5 DFA > 3 times serum amylase, and POD:5 DFA > 4000 U/L were 21.0% (95% CI 16.5% to 26.4%), 23.2% (95% CI 14.3% to 35.2%), 40.3% (95% CI 23.4% to 59.9%), 56.5% (95% CI 30.3% to 79.5%), and 90.0% (95% CI 74.2% to 96.6%) respectively. At the same pre‐test probability, the post‐test probabilities of pancreatic leak of negative POD:3 DFA > 600 IU/L, POD:3 to 5 DFA > 3 times serum amylase, POD:4 DFA > 647 U/L, POD:5 DFA > 3 times serum amylase, and POD:5 DFA > 4000 U/L were 1.5% (95% CI 0.6% to 3.7%), 2.2% (95% CI 0.8% to 5.9%), 2.5% (95% CI 1.4% to 4.3%), 0% (95% CI not estimable), and 2.0% (95% CI 1.2% to 3.5%) respectively. At the upper quartile of the prevalence of 21.5%, the post‐test probabilities of pancreatic leak of positive POD:3 DFA > 600 IU/L, POD:3 to 5 DFA > 3 times serum amylase, POD:4 DFA > 647 U/L, POD:5 DFA > 3 times serum amylase, and POD:5 DFA > 4000 U/L were 46.9% (95% CI 39.6% to 54.4%), 50.0% (95% CI 35.7% to 64.3%), 69.1% (95% CI 50.3% to 83.2%), 81.1% (95% CI 59.0% to 92.8%), and 96.8% (95% CI 90.5% to 98.9%) respectively. At the same pre‐test probability, the post‐test probabilities of pancreatic leak of negative POD:3 DFA > 600 IU/L, POD:3 to 5 DFA > 3 times serum amylase, POD:4 DFA > 647 U/L, POD:5 DFA > 3 times serum amylase, and POD:5 DFA > 4000 U/L were 4.9% (95% CI 2.0% to 11.4%), 7.0% (95% CI 2.7% to 17.1%), 7.8% (95% CI 4.6% to 12.9%), 0% (95% CI not estimable), and 6.5% (95% CI 3.8% to 10.8%) respectively. CI = confidence intervals | |||||||||
| Grade | A | B | C |
| Clinical conditions | Well | Often well | Usually ill |
| Ultrasound/CT (computed tomogram) (if obtained) | Negative | Negative/positive | Positive |
| Persistent drainage (after 3 weeks) | No | Usually yes | Yes |
| Reoperation | No | No | Yes |
| Death related to postoperative pancreatic fistula | No | No | Possibly yes |
| Signs of infections | No | Yes | Yes |
| Sepsis | No | No | Yes |
| Readmission | No | Yes/no | Yes/no |
| Modified from Bassi 2005. | |||
| Domain 1: Patient selection | Patient sampling | Patients who have undergone pancreatic resection with drain fluid at least 48 hours after pancreatic resection irrespective of the volume of the drain fluid. |
| Was a consecutive or random sample of patients enrolled? | Yes: if a consecutive sample or a random sample of patients with pancreatic resection with drain fluid at least 48 hours after pancreatic resection was included in the study. | |
| Was a case‐control design avoided? | Yes: if a cohort of patients with pancreatic resection with drain fluid at least 48 hours after pancreatic resection was studied. | |
| Did the study avoid inappropriate exclusions? | Yes: if all patients with pancreatic resection with drain fluid at least 48 hours after pancreatic resection were included. | |
| Could the selection of patients have introduced bias? | Low risk of bias: if 'yes' classification for all of the above 3 questions. High risk of bias: if 'no' classification for any of the above 3 questions. Unclear risk of bias: if 'unclear' classification for any of the above 3 questions but without a 'no' classification for any of the above 3 questions. | |
| Patient characteristics and setting | Yes: if all patients with pancreatic resection with drain fluid at least 48 hours after pancreatic resection were included. | |
| Are there concerns that the included patients and setting do not match the review question? | Low concern: if the patient characteristics and setting were classified as 'yes'. Unclear concern: if the patient characteristics and setting were classified as 'unclear'. High concern: if the patient characteristics and setting were classified as 'no'. | |
| Domain 2: Index test | Index test(s) | Amylase in drain fluid. |
| Were the index test results interpreted without knowledge of the results of the reference standard? | The index test would always be conducted though not interpreted before the reference standard. Yes: if the index test was conducted and interpreted without the knowledge of the results of the reference standard. | |
| If a threshold was used, was it pre‐specified? | Yes: if a pre‐specified threshold was used. No: if a pre‐specified threshold was not used. Unclear: if it was not clear whether the threshold used was pre‐specified. | |
| Could the conduct or interpretation of the index test have introduced bias? | Low risk of bias: if 'yes' classification for both of the above questions. High risk of bias: if 'no' classification for any of the above 2 questions. Unclear risk of bias: if 'unclear' classification for any of the above 2 questions but without a 'no' classification for any of the above 2 questions. | |
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern: if the criteria for positive index test was clearly stated. High concern: if the criteria for positive index test was not stated. | |
| Domain 3: Target condition and reference standard | Target condition and reference standard(s) | Target condition: clinically significant pancreatic leak (requiring clinical intervention). Planned reference standards (see below).
|
| Is the reference standard(s) likely to correctly classify the target condition? | Yes: if pancreatic leak was confirmed at reoperation. Unclear: although we planned to exclude studies if the reference standard was not described adequately or was not one of the above planned reference standards, this would have meant that there would have been no studies included in the review. So, we accepted the ISGPF grades B and C as an appropriate references standard and classified the answer to this signalling question as unclear. | |
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes: if the reference standard was interpreted without the knowledge of the results of the index test. | |
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk of bias: if 'yes' classification for both of the above 2 questions. High risk of bias: if 'no' classification for any of the above 2 questions. Unclear risk of bias: if 'unclear' classification for any of the above 2 questions but without a 'no' classification for any of the above 2 questions. | |
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Although we anticipated that all of the included studies would be classified as 'low concern' because of the reference standards we planned to use, we have classified all the studies as 'high concern' because of the reference standards that we accepted. | |
| Domain 4: Flow and timing | Flow and timing | Patients may have progression or resolution of pancreatic leak if there is a long delay between index test and reference standard. An arbitrary 2 weeks was chosen as an acceptable delay between index test and reference standard. |
| Was there an appropriate interval between index test and reference standard? | Yes: if the time interval between index test and reference standard was less than 2 weeks. | |
| Did all patients receive a reference standard? | Yes: if all patients received a reference standard. | |
| Did all patients receive the same reference standard? | Yes: if all the patients received the same reference standard. Unclear: if this information was not clear. Because of the inclusion criteria, all the studies in this review were classified as 'yes' for this signalling question. | |
| Were all patients included in the analysis? | Yes: if all the patients are included in the analysis irrespective of whether the results were interpretable. | |
| Could the patient flow have introduced bias? | Low risk of bias: if 'yes' classification for all the above 4 questions. High risk of bias: if 'no' classification for any of the above 4 questions. Unclear risk of bias: if 'unclear' classification for any of the above 4 questions but without a 'no' classification for any of the above 4 questions. | |
| ISGPF = International Study Group on Pancreatic Fistula | ||
| Test | No. of studies | No. of participants |
| 1 POD:3 DFA > 600 IU/L Show forest plot | 1 | 182 |
| 2 POD:3 to 5 DFA > 3 times serum amylase Show forest plot | 1 | 65 |
| 3 POD:4 DFA > 647 U/L Show forest plot | 1 | 100 |
| 4 POD:5 DFA > 3 times serum amylase Show forest plot | 1 | 50 |
| 5 POD:5 DFA > 4000 U/L Show forest plot | 1 | 471 |

