Interventions for preventing oral mucositis in patients with cancer receiving treatment: cytokines and growth factors
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Trial design: parallel (2 arms) Location: Institut Gustave Roussy, Villejuif, France Number of centres: 1 Study duration: February 2005 to September 2006 | |
| Participants | Inclusion criteria: adults with metastatic colorectal adenocarcinoma (grade 3 to 4); life expectancy greater than 3 months; receiving 5FU‐based chemotherapy Exclusion criteria: HIV; pregnant or lactating; unlikely to comply with interventions; participation in another trial in the previous 12 months (unless regarding chemotherapeutic protocols); undergone a total colectomy; state of subocclusion; chronic inflammatory diseases of the digestive tract; radiation enteropathy Cancer type: metastatic colorectal adenocarcinoma (grade 3 to 4) Cancer treatment: 5FU‐based chemotherapy Age at baseline (years): median 60 (not reported by group) Gender: not reported Number randomised: 22 (not reported by group) Number evaluated: 13 (Group A: 9; Group B: 4) | |
| Interventions | Comparison: TGF‐beta(2) versus placebo Group A: nutritional supplement of proteins, carbohydrates, fats, vitamins and minerals, with TGF‐beta(2) (2 ng/mg protein); formulas were in powder form, mixed with cool previously boiled water at 0.23 g/mL (100 kcl/100 mL); during each cycle participants received 750 mL to 1000 mL per day plus any other food desired; formula administered for 2 days before, 2 days during, and 3 days after chemotherapy (7 days/cycle) Group B: same as above without the TGF‐beta(2) Compliance: "Nine randomised patients who never ate the formula were excluded from the study" (not reported by group) Duration of treatment: "3 months (test or control formula), for a minimum of one and a maximum of eight cycles of treatment" | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: "This study was funded by Nestec Ltd" ‐ Nestlé (manufacturer of the intervention) Declarations/conflicts of interest: 6 of the 9 authors were either consultants (1) or employees (5) of Nestlé Data handling by review authors: reported in additional table Other information of note: "Due to low accrual of patients (22 patients were enrolled and randomised in 18 months), the study was prematurely stopped" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned" Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "randomly assigned" Comment: insufficient information to determine whether or not the random sequence was adequately concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind" and "The test formula differed only by containing an additional..." Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind" Comment: it is not clear who was blinded. There are subjective elements to the assessment of oral mucositis using this scale, requiring the patient's assessment of pain/soreness and their ability to swallow but, as the participants were unaware of their group allocation, the assessment of oral mucositis can be considered to be blinded |
| Incomplete outcome data (attrition bias) | High risk | Overall attrition was 41% although it was not reported by group |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (7 arms) dose‐ranging study Location: Universities of Minnesota and Michigan, USA Number of centres: 2 Study duration: not reported | |
| Participants | Inclusion criteria: aged 3 to 65 years; diagnosed with haematological malignancy (including myelodysplastic syndromes); ECOG score of 0 to 2; eligible for allogeneic HSCT after conditioning treatment with chemotherapy with or without TBI Exclusion criteria: received previous allogeneic HSCT; due to receive a T‐cell‐depleted donor graft; active chronic skin disease; pre‐existent inflammatory bowel disease; uncontrolled (antibiotic‐resistant) bacterial infection; hepatitis; HIV Cancer type: haematologic: ALL (Group A: 12%; Group B: 3%); AML (Group A: 35%; Group B: 39%); CML (Group A: 10%; Group B: 26%); MDS (Group A: 9%; Group B: 19%); NHL (Group A: 19%; Group B: 3%); Hodgkin's (Group A: 1%; Group B: 0%); Other (Group A: 14%; Group B: 10%) Cancer treatment: both centres had allogeneic HSCT on day 0 but differed in conditioning regimen and GVHD prophylaxis as follows:
Both centres received G‐CSF (filgrastim) 5 µg/kg per day from 24 hours after HSCT until neutrophil recovery Age at baseline (years): Group A: median 46 (range 7 to 65); Group B: median 46 (range 7 to 63) Gender: both groups 58% male Number randomised: 100 (Group A: 69; Group B: 31) Number evaluated: 96 (Group A: 65; Group B: 31) | |
| Interventions | Comparison: KGF (palifermin) versus placebo (4 KGF arms and 3 placebo arms were each combined into a single arm) Group A: KGF
Group B: placebo with matching schedule to either the 6, 9 or 12 dose regimen Compliance: Group A: 20 did not receive all study doses (17 of these were replaced to allow a full assessment of safety); Group B: 2 did not receive all study doses (1 replaced) Duration of treatment: varied from 13 days (6 doses) to 27 days (12 doses) ‐ see above | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: government grants from NIH and FDA, and also supported by Amgen (pharmaceutical industry) Declarations/conflicts of interest: not reported Data handling by review authors: the data for incidence of mucositis were not reported separately for each dose and therefore it was not possible to include head‐to‐head comparisons of different dosages in this review; the data for incidence of mucositis were presented in subgroups of those that did or did not receive the final methotrexate infusion on day 11 but we used the overall data in our meta‐analyses (the study authors report that there was no difference between these subgroups) Other information of note: the study authors report a greater decrease in incidence of grade 3 to 4 (severe) oral mucositis due to palifermin in the Minnesota participants (who received a more mucotoxic conditioning regimen) than in the Michigan participants | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients...were randomly assigned..." Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "patients...were randomly assigned..." Comment: insufficient information to determine whether or not the random sequence was adequately concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, placebo‐controlled" Comment: it is not clear who was blinded. There are subjective elements to the assessment of oral mucositis using this scale, requiring the patient's assessment of pain/soreness and their ability to swallow but, as the participants were unaware of their group allocation, the assessment of oral mucositis can be considered to be blinded |
| Incomplete outcome data (attrition bias) | Low risk | Quote: "Data for all patients randomly assigned and who received a transplant were used in all other analyses (intent‐to‐treat)" Comment: although 18 participants (Group A: 17; Group B: 1) were replaced to allow a full assessment of safety, it seems that the originally randomised participants were included in the analyses Overall attrition was 4% (Group A: 6%; Group B: 0%) for the oral mucositis incidence outcome. The reasons were unclear but this proportion of attrition is unlikely to have biased the results |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (3 arms) Location: Europe (Italy, France, the Netherlands, Ireland, Germany, UK, Denmark, Austria, Switzerland, Czech Republic, Sweden, Hungary, Belgium, Finland) Number of centres: 39 Study duration: December 2006 to February 2009 | |
| Participants | Inclusion criteria: aged between 18 and 70 years; due to receive high‐dose melphalan; ECOG score of 0 to 2 (or 3, if reason was due to multiple myeloma); at least 2 x 10⁶ CD34+ cells per kg; corrected carbon monoxide diffusing capacity 50% or higher of predicted; absolute neutrophil count at least 1.5 x 10⁹/L and platelets at least 100 x 10⁹/L; total bilirubin 2 mg/dL or lower; aspartate aminotransferase and/or alanine aminotransferase 4 x institutional upper limit of normal or lower Exclusion criteria: not reported Cancer type: multiple myeloma Cancer treatment: 1‐day administration of high‐dose melphalan (200 mg/m²) on day ‐2, followed by auto‐SCT on day 0 Age at baseline (years): Group A: median 55 (range 32 to 69); Group B: median 58 (range 40 to 68); Group C: median 58 (range 41 to 68) Gender: Group A: 54% male; Group B: 55% male; Group C: 58% male Number randomised: 281 (Group A: 109; Group B: 115; Group C: 57) Number evaluated: 281 (Group A: 109; Group B: 115; Group C: 57) | |
| Interventions | Comparison: KGF versus placebo Group A: KGF (60 µg/kg) daily IV on days ‐6, ‐5, and ‐4, then placebo on days 0 (the day of auto‐SCT), 1, and 2 (total dose = 180 µg/kg) Group B: KGF (60 µg/kg) daily IV on days ‐6, ‐5, ‐4, 0, 1, and 2 (total dose = 360 µg/kg) Group C: placebo daily IV on days ‐6, ‐5, ‐4, 0, 1, and 2 Compliance: Group A: 8% discontinued; Group B: 12% discontinued; Group C: 4% discontinued; (point of discontinuation or number of treatments not stated for any group) Duration of treatment: 6 treatment days (over 9 days) | |
| Outcomes |
| |
| Notes | Sample size calculation: 275 participants required at 95% power and 5% significance to detect an odds ratio of at least 3.5 between placebo and KGF in grade 2 to 4 oral mucositis Funding: sponsored by Swedish Orphan Biovitrum (pharmaceutical industry); KGF and placebo manufactured and packaged by Amgen (pharmaceutical industry) Declarations/conflicts of interest: 2 authors were employees of the sponsors; the remaining authors declared no competing financial interests Data handling by review authors: we combined the 2 KGF groups to make a single pairwise comparison against placebo; we also made a separate comparison of the 2 KGF regimens Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed by using an interactive‐voice‐response‐system before planned admission" Comment: large multicentre trial using high‐tech randomisation method ‐ likely to be done properly |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomization was performed by using an interactive‐voice‐response‐system before planned admission" Comment: large multicentre trial using high‐tech randomisation method ‐ likely to be done properly |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "Study drug...packaged...in identical vials" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, placebo‐controlled" Comment: it is not clear who was blinded. There are subjective elements to the assessment of lower grades of oral mucositis using the WHO scale, requiring the patient's assessment of pain/soreness and their ability to swallow. Higher grades have more objective elements so may not be affected by potential lack of blinding of the assessor. This would be the same for other subjective and objective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately (although quality of life reported with no SD or P values, this does not affect the risk of bias judgement for other outcomes) |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Australia Number of centres: 23 Study duration: recruitment from September 2006 to April 2010 | |
| Participants | Inclusion criteria: aged 15 to 60 years with newly diagnosed and previously untreated (except for hydroxycarbamide for high presenting white blood cell count) acute myeloid leukaemia ‐ all subtypes except t(15;17) or variants, or core‐binding factor AML (t(8;21) or inv(16) or variants); ECOG score of 0 to 3; no history of cancer (other than basal cell skin cancer or carcinoma of the cervix in situ, or other localised cancer treated by surgical excision only more than 5 years earlier without evidence of recurrence in the intervening period) Exclusion criteria: not reported Cancer type: acute myeloid leukaemia Cancer treatment: induction chemotherapy consisting of: idarubicin 9 mg/m² daily IV infusion on days 1 to 3; etoposide 75 mg/m² daily IV infusion on days 1 to 7; cytarabine 3 g/m² 12‐hourly IV infusion on days 1, 3, 5, and 7 All participants received G‐CSF (pegfilgrastim) 6 mg subcutaneously on day 8 Age at baseline (years): Group A: mean 46 (SD 12; range 17 to 60); Group B: mean 44 (SD 12; range 16 to 60) Gender: Group A: 61% male; Group B: 67% male Number randomised: 160 (Group A: 79; Group B: 81) Number evaluated: 151 (Group A: 73; Group B: 78) | |
| Interventions | Comparison: KGF (palifermin) versus placebo Group A: KGF (60 µg/kg) daily IV on days ‐3, ‐2, ‐1 prior to chemotherapy and for 3 days after completion of chemotherapy (total dose = 360 µg/kg) Group B: same schedule with placebo Compliance: received all 3 pre‐chemotherapy doses: Group A: 97%; Group B: 100%; received all 3 post‐chemotherapy doses: Group A: 95%; Group B: 96% Duration of treatment: 6 treatment days (over 14 days) | |
| Outcomes |
| |
| Notes | Sample size calculation: 128 per group required to detect a reduction in grade 3 to 4 mucositis from 22% to 10% at 70% power and 5% significance Funding: "This study was funded in part from Project Grant 302133 from the National Health and Medical Research Council of Australia" (government); KGF and placebo provided by Amgen (pharmaceutical industry) Declarations/conflicts of interest: "The authors have no conflicts of interest to declare" Data handling by review authors: N/A Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible patients were randomized 1:1 using a block randomization technique and stratification by participating centre to receive placebo or palifermin" Comment: large multicentre trial using block randomisation and stratification ‐ likely to be done properly |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Eligible patients were randomized 1:1 using a block randomization technique and stratification by participating centre to receive placebo or palifermin" Comment: insufficient information to determine whether or not the random sequence was adequately concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "placebo‐controlled" and "Both investigators and patients were blinded to the randomization outcome" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "placebo‐controlled" and "Both investigators and patients were blinded to the randomization outcome" Comment: investigators assessed oral mucositis, which would have partly relied on patient's assessment of pain/soreness and their ability to swallow; both investigators and patients were blinded |
| Incomplete outcome data (attrition bias) | Low risk | Overall attrition was 6% (Group A: 8%; Group B: 4%) for the oral mucositis incidence outcome. The reasons were similar between groups and this proportion of attrition is unlikely to have biased the results |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Australia, Canada and USA Number of centres: 22 Study duration: September 1999 to May 2001 | |
| Participants | Inclusion criteria: adults with newly diagnosed stage III/IVa or IVb squamous carcinoma of the oral cavity, oropharynx, nasopharynx, hypopharynx, and larynx (or with unknown primary and extensive neck disease) undergoing CRT intended to be curative; Karnofsky performance score of 60 or higher; haemoglobin 10 g/dL or higher; white blood cell count 3.5 x 10⁹/L or higher or absolute neutrophil count 1.5 x 10⁹/L or higher; platelet count 100 x 10⁹/L or higher; serum bilirubin 1.5 mg/dL or lower; serum creatinine lower than 2.0 mg/dL (plus a 24‐hour urinary creatinine clearance 50 mL/min in those aged 60 years or older) Exclusion criteria: previous RT to the head and neck; previous surgery for the primary tumour (not including biopsy); previous CT; allergy to Escherichia coli‐derived products; participation in any other investigational study within the 30 days prior to this study; refusal to use adequate contraception during the study; pregnant or breastfeeding Cancer type: head and neck: oral (Group A: 12%; Group B: 6%); oropharynx/nasopharynx (Group A: 61%; Group B: 66%); hypopharynx/larynx (Group A: 27%; Group B: 28%) Cancer treatment:
Age at baseline (years): Group A: mean 54 (SD 10; range 25 to 80); Group B: mean 56 (SD 10; range 42 to 75) Gender: Group A: 82% male; Group B: 84% male Number randomised: 101 (Group A: 69; Group B: 32) Number evaluated: 97 (Group A: 65; Group B: 32) | |
| Interventions | Comparison: KGF (palifermin) versus placebo Group A: KGF 60 µg/kg once weekly by IV bolus injection starting on the Friday before CRT began (on the following Monday), then each Friday after completion of RT for 7 weeks, and 2 more doses after completion of CRT i.e. 10 doses in total (total dose = 600 µg/kg) Group B: same schedule with matching placebo Compliance: 99 participants (Group A: 67; Group B: 32) received at least 1 dose of their allocated intervention; 69 participants completed the full course (Group A: 47; Group B: 22); mean number of doses (Group A: 8.4; Group B: 9.1) Duration of treatment: 9 weeks (10 doses) | |
| Outcomes |
| |
| Notes | Sample size calculation: based on a previous study, 99 participants required to detect a 30% difference in the duration of grade 2 or higher oral mucositis with 80% power provided that the mean duration in the placebo arm was 56 days Funding: "Supported by Amgen Inc" (pharmaceutical industry) Declarations/conflicts of interest: multiple and involving: employment or leadership positions with the funders (Amgen); consultant or advisory roles with the funders and other pharmaceutical companies; stock ownership with the funders; honoraria from the funders and other pharmaceutical companies; research funding from the funders and other pharmaceutical companies Data handling by review authors: the data for incidence of mucositis were presented in subgroups of those that received standard or hyperfractionated RT but we used the overall data in our meta‐analyses; for the interruptions to radiotherapy outcome, we used the data for breaks longer than 4 days as these could be pooled with other studies in this comparison Other information of note: the study authors report a greater decrease in incidence due to palifermin in the hyperfractionated subgroup than in the standard subgroup (see figure 3A in the study report) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly assigned..." Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were randomly assigned..." Comment: insufficient information to determine whether or not the random sequence was adequately concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double blinded" and "Palifermin...or matching placebo was administered by intravenous bolus" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double blinded" and "Palifermin...or matching placebo was administered by intravenous bolus" Comment: it is not clear who was blinded. There are subjective elements to the assessment of oral mucositis using this scale, requiring the patient's assessment of pain/soreness and their ability to swallow but, as the participants were unaware of their group allocation, the assessment of oral mucositis can be considered to be blinded. The other outcomes are objective and therefore unlikely to be affected by any potential lack of blinding of the outcome assessor(s) |
| Incomplete outcome data (attrition bias) | Low risk | Overall attrition was 4% (Group A: 6%; Group B: 0%) for the oral mucositis incidence outcome. The reasons were unclear but this proportion of attrition is unlikely to have biased the results |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (5 arms) dose‐ranging study Location: Duke University Medical Centre, Durham, North Carolina, USA Number of centres: 1 Study duration: not reported | |
| Participants | Inclusion criteria: premenopausal or perimenopausal patients with histologically confirmed metastatic breast cancer who had chemotherapy for inoperable or metastatic disease; performance status of 0 or 1 (CALGB criteria) Exclusion criteria: metastatic disease involving the central nervous system; pregnant Cancer type: stage IV breast Cancer treatment: AFM regimen (21‐day cycle): 5FU (500 mg/m²/day) continuous infusion on days 1 to 5; adriamycin (25 mg/m²) IV bolus on days 3 to 5; methotrexate (250 mg/m²) IV on day 15 (if oral mucositis less than grade 3) Age at baseline (years): mean 44 (not reported by group) Gender: 49 female; 1 male (not reported by group) Number randomised: 50 (not reported by group) Number evaluated: 45 (Group A: 36; Group B: 9) | |
| Interventions | Comparison: GM‐CSF (molgramostim) versus placebo Group A: GM‐CSF
Group B: (n = 9 analysed) same schedule with matching placebo mouthwash Compliance: (not reported by group) mouthwash therapy was discontinued if the participant experienced oral mucositis of grade 3 or above; 30 participants took at least 80% of their prescribed doses; 11 participants discontinued mouthwash therapy within 3 days prior to day 15; 4 participants discontinued mouthwash therapy between day 15 and day 21 Duration of treatment: 21 days (first treatment cycle of AFM) | |
| Outcomes |
| |
| Notes | Sample size calculation: this was done but the numbers required are not reported Funding: "...supported in part by National Cancer Institute (Bethesda, MD) grant number PO1‐47741‐A4" Declarations/conflicts of interest: not reported Data handling by review authors: we combined the 4 GM‐CSF groups to make a single pairwise comparison against placebo and, in order to make a head‐to‐head comparison of doses, we grouped the 2 lower doses (0.01 µg/mL and 0.1 µg/mL) together and grouped the 2 higher doses (1 µg/mL and 10 µg/mL) together to make pairwise groups for comparison Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomized by the Duke Cancer Center Protocol Office according to a block randomization scheme and assigned a unique identifier number which designated the GM‐CSF dose level to be received" Comment: method of sequence generation not fully described but was done by a dedicated specialist centre so was probably done adequately |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomized by the Duke Cancer Center Protocol Office" and "The patient supply of mouthwash was labelled to correspond with the assigned identifier number and dispensed by the Pharmacy. The patient assignment information was maintained by the Pharmacy" Comment: the entire randomisation process was performed by third party so the random sequence is unlikely to have been manipulated |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "The patient assignment information was maintained by the Pharmacy" Comment: it is not clear who was blinded. There are subjective elements to the assessment of oral mucositis using this scale, requiring the patient's assessment of pain/soreness and their ability to swallow but, as the participants were unaware of their group allocation, the assessment of oral mucositis can be considered to be blinded |
| Incomplete outcome data (attrition bias) | Unclear risk | Overall attrition was 10%. Reasons for attrition fully reported. If all participants would have developed severe oral mucositis or dropped out due to severe oral mucositis and were all from 1 particular group, this would have biased the results. However, attrition was not reported by group, so it is unclear |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Italy Number of centres: 4 Study duration: May 2007 to June 2011 | |
| Participants | Inclusion criteria: aged 0 to 17 years with leukaemia, lymphoma or solid tumour; due to receive a first autologous PBSCT Exclusion criteria: not reported Cancer type: leukaemia/lymphoma (Group A: 22%; Group B: 17%); solid (Group A: 78%; Group B: 83%) (neuroblastoma, Ewing sarcoma/peripheral neuroectodermal tumour, medulloblastoma, Wilms tumour, central nervous system tumour) Cancer treatment: all participants had autologous PBSCT on day 0 but differed in conditioning regimen as follows:
Age at baseline (years): Group A: median 11.1 (range 1.7 to 17.4); Group B: median 11.9 (range 1.6 to 17.2) Gender: Group A: 66% male; Group B: 59% male Number randomised: 61 (Group A: 32; Group B: 29) Number evaluated: 61 (Group A: 32; Group B: 29) | |
| Interventions | Comparison: G‐CSF (pegfilgrastim) versus G‐CSF (filgrastim) Group A: pegfilgrastim single dose (100 µg/kg; maximum 6 mg) injected on day 3 Group B: filgrastim (5 µg/kg per day; maximum 300 µg per day) injected by 9 or more doses starting on day 3 (total dose = at least 45 µg/kg) Compliance: all participants received their allocated intervention with no discontinuations Duration of treatment: Group A: 1 day; Group B: 9 or more days | |
| Outcomes |
| |
| Notes | Sample size calculation: based on the noninferiority of pegfilgrastim versus filgrastim in speeding the recovery of polymorphonuclear cells Funding: "The authors have no support or funding to report" Declarations/conflicts of interest: "The authors have declared that no competing interests exist" Data handling by review authors: N/A Other information of note: G‐CSF administration only began after the chemotherapy and PBSCT were completed, by which point oral mucositis may have already begun to develop | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computer‐generated randomisation list was drawn up at Data Office Centre of AIEOP in Bologna, Italy, by a statistician not involved in patient management" Comment: adequate method used |
| Allocation concealment (selection bias) | Low risk | Quote: "The list was stored by sequentially numbered sealed envelopes that was concealed to investigators until the completion of recruitment. The local investigator ...assigned each eligible patient to randomization list by phoning to AIEOP Data Office Centre" Comment: ideal method of concealment used |
| Blinding of participants and personnel (performance bias) | High risk | Treatment regimens were different so blinding not possible |
| Blinding of outcome assessment (detection bias) | Unclear risk | It would be possible to blind the outcome assessor for oral mucositis, but it was not mentioned |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: cross‐over (2 arms) Location: Cancer Centre and Department of Otolaryngology, Veterans General Hospital, Taiwan, Republic of China Number of centres: 1 Study duration: not reported | |
| Participants | Inclusion criteria: diagnosed stage IV SCC of head and neck, previously untreated or locally recurrent after previous surgery or radiotherapy or both; ECOG score of 2 or above; adequate bone marrow, liver and renal function Exclusion criteria: concurrent medical illness; local radiotherapy to oropharynx region in the previous 3 months Cancer type: head and neck: nasopharyngeal (Group A: 44%; Group B: 27%); tongue (Group A: 22%; Group B: 36%); hypopharynx (Group A: 11%; Group B: 18%); buccal (Group A: 11%; Group B: 9%); tonsillar (Group A: 11%; Group B: 9%) Cancer treatment: PFL regimen (21‐day cycle): cisplatin (20 mg/m²/day), 5FU (800 mg/m²/day) and leucovorin (90 mg/m²/day) IV for days 1 to 4; cycle repeated every 3 weeks (study consisted of 2 cycles) Age at baseline (years): Group A: median 44 (range 36 to 62); Group B: median 49 (range 40 to 66) Gender: Group A: 89% male; Group B: 91% male Number randomised: 20 (Group A: 9; Group B: 11) ‐ figures for first cycle Number evaluated: 20 (Group A: 9; Group B: 11) | |
| Interventions | Comparison: GM‐CSF versus no treatment Group A: GM‐CSF (4 µg/kg) subcutaneously from day 5 to 14 (total dose = 40 µg) Group B: no treatment Compliance: not reported Duration of treatment: 10 days (days 5 to 14 of 21‐day cycle) | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: "..supported in part by Department of Health, Taiwan, Republic of China, research grant no. DOH 83‐HR‐202" and "GM‐CSF (supplied by Schering Plough Corp, Kenilworth, NJ)" (pharmaceutical industry) Declarations/conflicts of interest: not reported Data handling by review authors: as stated in the methods section, we would only include first‐period data from cross‐over studies due to potential for period effects (which were reported in this study). The only usable data in this study were reported in the text as incidence of severe gross mucositis for the first cycle Other information of note: the authors report a significant period effect of GM‐CSF (P < 0.01), whereby the benefits continued into the second cycle | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomized to receive GM‐CSF or no therapy" Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were randomized to receive GM‐CSF or no therapy" Comment: insufficient information to determine whether or not the random sequence was adequately concealed |
| Blinding of participants and personnel (performance bias) | High risk | Comparison with no treatment so blinding not possible |
| Blinding of outcome assessment (detection bias) | Unclear risk | It would be possible to blind the outcome assessor, as the data we used were assessed by a physician using an objective scale. However, it was not mentioned |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants appear to be included in the analyses |
| Selective reporting (reporting bias) | Low risk | Although most of the data were not usable in this review, this does not seem to be due to selective reporting |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: USA Number of centres: 14 Study duration: recruitment from May 1988 to November 1989 | |
| Participants | Inclusion criteria: newly diagnosed small‐cell lung cancer meeting standard criteria for end‐organ function; ECOG score of 0 to 2 Exclusion criteria: previous radiotherapy; other serious medical illnesses precluding participation Cancer type: small‐cell lung cancer Cancer treatment: CAE regimen (21‐day cycle): cyclophosphamide (1000 mg/m²) and doxorubicin (50 mg/m²) on day 1; etoposide (120 mg/m²) on days 1 to 3; all by IV; repeated for up to 6 cycles Age at baseline (years): Group A: mean 61 (SD 10; range 31 to 78); Group B: mean 62 (SD 8; range 31 to 80) Gender: Group A: 65% male; Group B: 63% male Number randomised: 211 (Group A: 101; Group B: 110) Number evaluated: 195 (Group A: 93; Group B: 102) ‐ figures for first cycle | |
| Interventions | Comparison: G‐CSF (r‐metHuG‐CSF) (filgrastim) versus placebo Group A: G‐CSF (230 µg/m²) self‐administered subcutaneously on days 4 to 17 (total dose = 3220 µg/m²) Group B: as above but with placebo Compliance: not reported Duration of treatment: 14 days during a 21‐day cycle | |
| Outcomes |
| |
| Notes | Sample size calculation: based on a difference of 20% in the incidence of fever with neutropenia over the 6 cycles Funding: "The study was designed, coordinated, and analyzed in conjunction with Amgen, the supplier of the G‐CSF" Declarations/conflicts of interest: not reported but some authors were employed by Amgen (pharmaceutical industry) Data handling by review authors: for oral mucositis, we only used the data from the first cycle due to the reasons listed above (under 'Interventions') Other information of note: G‐CSF administration only began after the 3‐day chemotherapy was completed, by which point oral mucositis may have already begun to develop. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly assigned to chemotherapy followed by study drug (either placebo or G‐CSF)" Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The patients were randomly assigned to chemotherapy followed by study drug (either placebo or G‐CSF)" Comment: insufficient information to determine whether or not the random sequence was adequately concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "Placebo was supplied in matching vials for double blinding" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Placebo was supplied in matching vials for double blinding" Comment: it is not clear who was blinded. There are subjective elements to the assessment of oral mucositis using this scale, requiring the patient's assessment of pain/soreness and their ability to swallow but, as the participants were unaware of their group allocation, the assessment of oral mucositis can be considered to be blinded |
| Incomplete outcome data (attrition bias) | Low risk | Overall attrition was 8% (Group A: 8%; Group B: 7%) for the oral mucositis incidence outcome. The reasons were reported and similar between groups, and this proportion of attrition is unlikely to have biased the results |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Ravenna, Italy Number of centres: 1 Study duration: recruitment from July 1997 to February 2002 | |
| Participants | Inclusion criteria: 14 years of age or older; hospitalised for high‐dose chemotherapy with autologous PBSCT Exclusion criteria: not reported Cancer type: breast (Group A: 17.5%; Group B: 27.5%); Ewing's sarcoma (Group A: 41.5%; Group B: 28.5%); osteosarcoma (Group A: 13%; Group B: 14%); NHL (Group A: 15%; Group B: 11.5%); germ cell tumours (Group A: 11%; Group B: 16%); small‐cell lung (Group A: 2%; Group B: 0%); soft tissue sarcoma (Group A: 0%; Group B: 2.5%) Cancer treatment: high‐dose chemotherapy with autologous PBSCT; chemotherapy regimens were categorised into high risk and low risk and this was used as a stratification factor for randomisation, therefore high‐ and low‐risk participants were equally distributed across groups Age at baseline (years): Group A: median 29 (range 15 to 57); Group B: median 29 (range 17 to 61) Gender: Group A: 59% male; Group B: 55% male Number randomised: 90 (Group A: 46; Group B: 44) Number evaluated: 90 (Group A: 46; Group B: 44) | |
| Interventions | Comparison: GM‐CSF versus placebo Group A: GM‐CSF mouthwash 150 µg/day in 100 cm³ of sterile water taken in 4 doses per day; mouthrinsing performed for 1 minute each time; treatment started on the day after the completion of chemotherapy and continued until bone marrow recovery (absolute neutrophil count > 500/mm³) or resolution of mucositis if still persistent after bone marrow recovery (total dose = variable) Group B: as above but with placebo (sterile water) Compliance: all but 7 participants regularly completed mouthwashes: 1 participant in the placebo group had none due to persistent vomiting; 6 (4 in placebo group and 2 in GM‐CSF group) started treatment but interrupted it early due to nausea and vomiting Duration of treatment: variable and dependent on bone marrow recovery/resolution of mucositis | |
| Outcomes |
| |
| Notes | Sample size calculation: 90 participants required to detect 25% minimal difference in the rate of severe mucositis at 90% power and 5% significance Funding: no external funding (from correspondence with authors) Declarations/conflicts of interest: not reported Data handling by review authors: the data for incidence of mucositis were presented in subgroups of those at low or high risk of mucositis but we used the overall data in our meta‐analyses Other information of note: there does not appear to be any difference in risk of any or severe mucositis between the low‐ and high‐risk subgroups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote from correspondence with authors: "The randomization list was centralized" |
| Allocation concealment (selection bias) | Low risk | Quote from correspondence with authors: "The randomization list was centralized" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, randomized, placebo‐controlled study" and "The color, odor, texture and taste of both solutions were virtually identical" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, randomized, placebo‐controlled study" Comment: it is not clear who was blinded. There are subjective elements to the assessment of oral mucositis using this scale, requiring the patient's assessment of pain/soreness and their ability to swallow but, as the participants were unaware of their group allocation, the assessment of oral mucositis can be considered to be blinded |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Department of Hematology and Oncology, University Hospital Freiburg, Germany Number of centres: 1 Study duration: March 2006 to December 2010 | |
| Participants | Inclusion criteria: adults aged 18 to 75 years with either: high‐grade non‐Hodgkin's lymphoma with high‐risk syndrome (> 2 risk factors according to age‐adapted IPI = international prognostic index) in the first complete remission; Hodgkin's lymphoma in the first recurrence; recurrence of follicular lymphoma; primary therapy of a coat‐cell lymphoma (MCL) in stage II‐IV; due to receive BEAM chemotherapy followed by autologous PBSCT; Karnofsky performance score more than 60%; life expectancy more than 3 months Exclusion criteria: previous therapy using palifermin; severe concomitant diseases with organ failure; pregnancy, lactation, positive pregnancy test; hypersensitivity to 1 of the trial drugs; severe psychiatric illness; HIV disease or immunologic deficiency; known central nervous system involvement Cancer type: haematologic: diffuse large‐cell lymphoma (Group A: 33%; Group B: 42%); B‐cell type acute lymphocytic leukaemia (Group A: 10%; Group B: 6%); T‐cell non‐Hodgkin's lymphoma (Group A: 13%; Group B: 11%); follicular/mantle cell lymphoma (Group A: 27%; Group B: 28%); Hodgkin's lymphoma (Group A: 17%; Group B: 14%) Cancer treatment: prior to receiving autologous PBSCT on day 0, participants received BEAM conditioning regimen from day ‐8 to ‐2: carmustine (BCNU) 300 mg/m²; etoposide 800 mg/m²; cytosine arabinoside 1600 mg/m²; melphalan 140 mg/m² Age at baseline (years): (ITT population) Group A: median 50 (range 22 to 71); Group B: median 55 (range 22 to 73) Gender: (ITT population) Group A: 57% male; Group B: 61% male Number randomised: 73 (Group A: 37; Group B: 36) Number evaluated: ITT: 66 (Group A: 30; Group B: 36); PP: 54 (Group A: 22; Group B: 32) | |
| Interventions | Comparison: KGF (palifermin) plus best supportive care versus best supportive care alone Group A: KGF (60 µg/kg) by IV daily for 3 days (days ‐10, ‐9, ‐8) prior to conditioning regimen and autologous PBSCT and then for 3 days after (days 0, 1, 2) (total dose = 360 µg/kg) Group B: best supportive care ("effective oral hygiene like teeth brushing, oral rinsing") beginning on day ‐8 (the day of hospital admission for BEAM conditioning) Compliance: Group A: 7/37 withdrew before therapy started, 3/37 had a different conditioning regimen to that specified in the study protocol (unclear if they still received KGF), 5/37 either had no KGF or did not receive all doses; Group B: 4/36 had a different conditioning regimen to that specified in the study protocol (unclear if they still received control intervention) Duration of treatment: 6 treatment days (over 13 days) | |
| Outcomes |
| |
| Notes | Sample size calculation: 76 participants required to detect 30% difference in the rate of severe mucositis at 80% power and 5% significance Funding: Amgen (pharmaceutical industry) Declarations/conflicts of interest: not reported Data handling by review authors: data for ITT population used Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned" Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "randomly assigned" Comment: insufficient information to determine whether or not the random sequence was adequately concealed |
| Blinding of participants and personnel (performance bias) | High risk | Quote: "The randomization result was known to the patient as well as to the practitioners before the start of therapy" |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "The randomization result was known to the patient as well as to the practitioners before the start of therapy" |
| Incomplete outcome data (attrition bias) | High risk | Overall attrition was 10% (Group A: 19%; Group B: 0%) for the ITT population. All 7 participants died before therapy started. Although this reason is not related to the outcomes, the balance created by randomisation may have been lost |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (3 arms) Location: USA Number of centres: 8 Study duration: not reported | |
| Participants | Inclusion criteria: aged 18 years or older; due to receive autologous HSCT with a conditioning regimen with a high propensity for producing mucositis (typically 50% incidence of NCI‐CTC grade 3 or 4 when receiving standard mucositis management); Karnofsky performance score of 70%; free of acute or significant chronic dental or periodontal disease at baseline examination Exclusion criteria: previous HSCT; visible oral ulcerations at screening; pregnant or breastfeeding; childbearing potential or not using adequate contraception; history of allergy to Escherichia coli‐derived products; posterior subcapsular cataract identified at screening; history of thyroid disease prior to receiving chemotherapy (except for hypothyroidism adequately controlled with replacement therapy); history or clinical evidence of active significant acute or chronic diseases that may affect evaluation or interpretation of the effects of the study medication on mucositis; following medications: interleukin 11, topical steroids, sucralfate, hydrogen peroxide, pilocarpine, misoprostol, oral chlorhexidine rinses, or any agent that would affect the assessment of changes in the appearance of mucositis during the study Cancer type: lymphoma (Group A: 64%; Group B: 71%; Group C: 57%); other haematologic malignancy (Group A: 36%; Group B: 29%; Group C: 43%) Cancer treatment: prior to receiving autologous HSCT, participants received the following conditioning regimens:
Age at baseline (years): Group A: mean 54 (SD 10); Group B: mean 47 (SD 10); Group C: mean 51 (SD 15) Gender: Group A: 79% male; Group B: 64% male; Group C: 79% male Number randomised: 42 (Group A: 14; Group B: 14; Group C: 14) Number evaluated: 42 (Group A: 14; Group B: 14; Group C: 14) | |
| Interventions | Comparison: KGF‐2 (repifermin) versus placebo Group A: KGF‐2 (25 µg/kg) by IV daily for 3 days prior to conditioning regimen and autologous HSCT and then for 10 days after (total dose = 325 µg/kg) Group B: KGF‐2 (50 µg/kg) as above (total dose = 650 µg/kg) Group C: placebo as above Compliance: not reported Duration of treatment: 13 treatment days (over a longer period dependent on conditioning regimen) | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: not reported Declarations/conflicts of interest: not reported Data handling by review authors: we combined the 2 KGF‐2 groups to make a single pairwise comparison against placebo and we also made a comparison of the 2 different KGF‐2 dosages against each other Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote from correspondence with authors: "The method to implement the random allocation was by central telephone" |
| Allocation concealment (selection bias) | Low risk | Quote from correspondence with authors: "The method to implement the random allocation was by central telephone" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blinded, placebo‐controlled" |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blinded, placebo‐controlled" |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Iran Number of centres: not reported Study duration: not reported | |
| Participants | Inclusion criteria: previously untreated acute lymphoblastic leukaemia patients; aged between 5 and 18 years Exclusion criteria: any other systemic disease; presence of oral mucositis or other oral lesions prior to chemotherapy; history of dermatology or respiratory hypersensitivity; acute lymphoblastic leukaemia recurrence Cancer type: acute lymphoblastic leukaemia (ALL) Cancer treatment: induction chemotherapy protocol consisted of standard risk B‐precursor ALL (COG)/dexamethasone, vincristine, L‐asparaginase, intrathecal (methotrexate + ara‐C + hydrocortisone). The intensification protocol was dexamethasone, vincristine, L‐asparaginase/ dexamethasone, cyclophosphamide/6‐thioguanine + cytarabine + intrathecal methotrexate Age at baseline (years): Group A: mean 8.8 (SD 2.5); Group B: mean 8.4 (SD 2.2); overall range: 5 to 18 Gender: Group A: 49% male; Group B: 49% male Number randomised: 90 (Group A: 45; Group B: 45) Number evaluated: 90 (Group A: 45; Group B: 45) | |
| Interventions | Comparison: KGF (palifermin) versus chlorhexidine Group A: KGF (60 µg/kg) by IV bolus daily for 3 days prior to chemotherapy regimen and then for 3 days after (total dose = 360 µg/kg) Group B: chlorhexidine (concentration not reported) mouthwash used for 1 minute once daily for 3 days prior to chemotherapy regimen and then for 3 days after Compliance: not reported Duration of treatment: 6 treatment days (over an unspecified longer period) | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: not reported Declarations/conflicts of interest: "There is no conflict of interest in relation to this study" Data handling by review authors: we report the data at 2 weeks as they represent the maximum oral mucositis score experienced better than those at 1 week Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were randomly assigned to the palifermin or control group by using the table of random numbers" Comment: adequate method used |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The patients were randomly assigned to the palifermin or control group by using the table of random numbers" |
| Blinding of participants and personnel (performance bias) | High risk | Comparison with chlorhexidine so blinding not possible |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "Each patient was evaluated for oral lesions one and two weeks after the chemotherapy completion by the same specialist who was blind to the type of treatment" and "This limited use of chlorhexidine was to prevent the adverse effects like tooth discoloration and temporally taste changes" |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Australia, Canada, and Europe (Austria, France, Germany, Italy, Spain, UK) Number of centres: 38 Study duration: recruitment from January 2005 to August 2007 | |
| Participants | Inclusion criteria: more than 18 years old; resected for pathohistologically documented high‐risk stage 2 to 4B SCC of the oral cavity, oropharynx, hypopharynx, or larynx; ECOG score of 0 to 2; at least 2 of 9 areas of the oral or oropharyngeal mucosa due to receive at least 50 Gy RT Exclusion criteria: tumours of the lips, paranasal sinuses, salivary glands, or unknown primary site; metastatic disease; history of chronic pancreatitis or acute pancreatitis within the last year; prior RT to the head and neck region or prior chemotherapy; previous treatment on this study or with other KGFs Cancer type: head and neck: oropharynx (Group A: 47%; Group B: 48%); oral cavity (Group A: 32%; Group B: 27%); larynx (Group A: 11%; Group B: 15%); hypopharynx (Group A: 10%; Group B: 10%); other (Group A: 1%; Group B: 1%) Cancer treatment: after R0 or R1 resection:
Age at baseline (years): Group A: mean 56 (SD 8); Group B: mean 57 (SD 9) Gender: Group A: 85% male; Group B: 80% male Number randomised: 186 (Group A: 92; Group B: 94) Number evaluated: 186 (Group A: 92; Group B: 94) | |
| Interventions | Comparison: KGF (palifermin) versus placebo Group A: KGF (120 µg/kg) 3 days prior to start of, and then once per week during radiochemotherapy, i.e. 7 doses for those with R0 resection, 8 doses for those with R1 resection (total dose = 840 µg/kg or 960 µg/kg respectively) Group B: same schedule with placebo Compliance: 78% of participants in KGF group completed all planned doses compared to 86% in placebo group Duration of treatment: 7 or 8 treatment days (over 7 or 8 weeks), depending on R0 or R1 resection respectively | |
| Outcomes |
| |
| Notes | Sample size calculation: assuming 60% of placebo group would develop grade 3 to 4 mucositis, 90 per group required to detect a reduction of at least 25% at 90% power and 5% significance Funding: "This study was supported by Amgen" (Amgen also named as sponsor on trials registry ‐ pharmaceutical industry) Declarations/conflicts of interest: some authors had both employment or leadership positions and stock ownership within Amgen Data handling by review authors: N/A Other information of note: study originally randomised participants to 3 arms (180 µg/kg once per week for 7 weeks, 180 µg/kg once per week for 4 weeks followed by placebo for the next 3 doses, or placebo throughout) but, after 1 serious adverse event of respiratory insufficiency reported in 1 of the first 10 participants, the data monitoring committee decided to restart the study using 120 µg/kg doses, excluding the 17 randomised participants from the efficacy assessments. The arm with KGF for 4 weeks followed by placebo was stopped due to slow recruitment, after enrolment of 38 participants, and the results analysed in a separate appendix | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random assignment was made by a centralized interactive voice response system" Comment: large multicentre trial using high‐tech randomisation method ‐ likely to be done properly |
| Allocation concealment (selection bias) | Low risk | Quote: "Random assignment was made by a centralized interactive voice response system" Comment: large multicentre trial using high‐tech randomisation method ‐ likely to be done properly |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, randomized, placebo‐controlled" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, randomized, placebo‐controlled" Comment: it is not clear who was blinded. There are subjective elements to the assessment of lower grades of oral mucositis using the WHO scale, requiring the patient's assessment of pain/soreness and their ability to swallow. Higher grades have more objective elements so may not be affected by potential lack of blinding of the assessor. This would be the same for other subjective and objective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Tehran University of Medical Sciences, Tehran, Iran Number of centres: 1 Study duration: February 2014 to March 2015 | |
| Participants | Inclusion criteria: aged 18 years or older with non‐Hodgkin's lymphoma, Hodgkin's disease or multiple myeloma; due to receive autologous HSCT; adequate cardiac, pulmonary, renal and hepatic function Exclusion criteria: Karnofsky performance score less than 70%; participation in another study using an unlicensed product Cancer type: haematologic: non‐Hodgkin's lymphoma (Group A: 25%; Group B: 25%); Hodgkin's disease (Group A: 23%; Group B: 23%); multiple myeloma (Group A: 53%; Group B: 53%) Cancer treatment: prior to receiving autologous HSCT, participants received the following conditioning regimens:
Age at baseline (years): Group A: mean 43 (SD 14); Group B: mean 45 (SD 16) Gender: Group A: 55% male; Group B: 48% male Number randomised: 80 (Group A: 40; Group B: 40) Number evaluated: 80 (Group A: 40; Group B: 40) | |
| Interventions | Comparison: Erythropoietin (recombinant human) versus placebo Group A: 50 IU/mL erythropoietin mouthwash in aqueous vehicle (sodium benzoate, sodium citrate, citric acid, sodium hydroxide, sugar and distilled water) supplied in glass bottle stored at 4°C, 15 mL 4 times daily, starting from the first day of conditioning chemotherapy until 14 days after HSCT or until discharge from hospital (i.e. neutrophil recovery), whichever occurred first, oral intake not permitted for 1 hour following mouthwashing Group B: same schedule with placebo (aqueous vehicle‐only) Compliance: "However, it was a limitation of our study that EPO mouthwash administration might be affected by patients' low compliance" (no data reported) Duration of treatment: variable and dependent on neutrophil recovery | |
| Outcomes |
| |
| Notes | Sample size calculation: 40 per group required assuming a 30% decrease in incidence of grade 2 to 4 mucositis at 5% significance and 80% power Funding: "There was no applicable funding source for the clinical trial" Declarations/conflicts of interest: "The authors have no conflict of interests to report" Data handling by review authors: there is a discrepancy in the incidence of grade 2 to 4 mucositis between Figure 2 and Table 2 (the latter has 1 extra event per group). However, this does not change the effect estimate. We have used the data in Table 2 as it reports numbers of participants along with percentages Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly allocated...in a blocked randomization schedule" and "Both patient randomization and drug preparation were performed in the pharmaceutical laboratory of Pharmacy Department" Comment: method of random sequence generation not described but done by university hospital pharmacy and therefore probably done adequately |
| Allocation concealment (selection bias) | Low risk | Quote: "Both patient randomization and drug preparation were performed in the pharmaceutical laboratory of Pharmacy Department" Comment: not explicitly described but pharmacy‐controlled randomisation should have ensured concealment of the random sequence from those recruiting participants |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, randomized, placebo‐controlled" and "The study participants, the attending physician and the outcome assessor were all blind to the treatment assignment" and "There were no differences in colour, flavour, taste or container of the study drug and the placebo" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, randomized, placebo‐controlled" and "The study participants, the attending physician and the outcome assessor were all blind to the treatment assignment" Comment: all parties were blinded |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: USA (16 sites) and Australia (4 sites) Number of centres: 20 Study duration: December 2005 to November 2008 | |
| Participants | Inclusion criteria: aged 18 years or older with haematologic malignancy (including myelodysplastic syndromes) and due to receive allogeneic SCT (marrow or PBPC) after a conditioning regimen; Karnofsky performance score of 70% or more; related donor or HLA‐matched unrelated donor identical at 6/6 HLA‐A, ‐B and ‐DRB1 loci (molecular typing of class I and class II for unrelated donors) Exclusion criteria: other malignancies; prior SCT; previous use of KGF; active infection or oral mucositis; congestive heart failure (NYHA class III or IV); use of a T‐cell depleted graft for GVHD prophylaxis; inadequate renal, liver or pulmonary function; pregnant or breastfeeding; refusal to use adequate contraception during study; participation in another investigational device or drug trial in previous 30 days Cancer type: haematologic: leukaemia (Group A: 71%; Group B: 79%); myelodysplastic syndrome (Group A: 16%; Group B: 12%); non‐Hodgkin's lymphoma (Group A: 12%; Group B: 8%); multiple myeloma (Group A: 0%; Group B: 1%); Hodgkin's disease (Group A: 1%; Group B: 0%) Cancer treatment: prior to receiving allogeneic SCT on day 0, participants received 1 of the following conditioning regimens from day ‐11 to ‐2:
Participants received methotrexate (with a calcineurin inhibitor ‐ either cyclosporine or tacrolimus) for GVHD prophylaxis on days 1, 3 and 6 (planned), and on day 11 (if toxicity allowed) at doses of 15 mg/m², 10 mg/m², 10 mg/m² and 10 mg/m² respectively Age at baseline (years): Group A: median 42 (range 18 to 62); Group B: median 44 (range 18 to 64) Gender: Group A: 52% male; Group B: 63% male Number randomised: 155 (Group A: 77; Group B: 78) Number evaluated: 155 (Group A: 77; Group B: 78) | |
| Interventions | Comparison: KGF (palifermin) versus placebo Group A: KGF (60 µg/kg) by IV bolus daily for 3 days prior to start of conditioning therapy, then a single 180 µg/kg dose after conditioning, but often 1 or 2 days before SCT (total dose = 360 µg/kg) Group B: same schedule with placebo Compliance: received at least 1 dose: Group A: 99%; Group B: 96%; received all doses: Group A: 92%; Group B: 88% Duration of treatment: 4 treatment days (over roughly 14 days) | |
| Outcomes |
| |
| Notes | Sample size calculation: based on GVHD (not met due to early stopping) Funding: "This study was supported by research funding from Amgen Inc. Jonathan Latham of PharmaScribe, LLC received funding from Amgen Inc. to provide assistance with the preparation of the manuscript. Xuesong Guan of Amgen Inc. provided assistance with statistical analyses" (pharmaceutical industry) Declarations/conflicts of interest: some authors were employees and stockholders of Amgen and some received compensation from Amgen for consultation Data handling by review authors: N/A Other information of note: planned sample size was 200 participants but the study was stopped due to slow recruitment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Subjects were randomly assigned..." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Subjects were randomly assigned..." |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, placebo‐controlled" |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Saga Medical School, Saga, Japan Number of centres: 1 Study duration: not reported | |
| Participants | Inclusion criteria: breast cancer patients Exclusion criteria: not reported Cancer type: breast: primary advanced (Group A: 2; Group B: 5); inflammatory (Group A: 4; Group B: 1); recurrent (Group A: 1; Group B: 1) Cancer treatment: preoperative IA high‐dose adriamycin (10 mg to 40 mg every 2 to 3 days to a total dose of 70 mg to 170 mg) Age at baseline (years): Group A: mean 53 (SD 11; range 38 to 69); Group B: mean 52 (SD 10; range 45 to 69) Gender: all female Number randomised: 14 (Group A: 7; Group B: 7) Number evaluated: 14 (Group A: 7; Group B: 7) | |
| Interventions | Comparison: G‐CSF versus no treatment Group A: G‐CSF (125 µg) by daily subcutaneous injection until leukocyte counts > 8000/mm³; timing in relation to chemotherapy not specifically reported, but the group was further divided into 2 subgroups where one (n = 4) received G‐CSF during/as an adjunct to the chemotherapy, and the other (n = 3) received G‐CSF afterwards (after the leukocyte counts were likely to drop below 2000/mm³) Group B: no treatment Compliance: not reported Duration of treatment: variable and dependent on leukocyte recovery (to > 8000/mm³) | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: "G‐CSF (Neutrogin) was provided by Chugai Pharmaceutical" Declarations/conflicts of interest: not reported Data handling by review authors: the data for incidence of mucositis were presented in subgroups of those receiving G‐CSF during or after chemotherapy but we used the overall data in our meta‐analyses Other information of note: both cases of mucositis were in the subgroup who received G‐CSF after chemotherapy. Oral mucositis may have already begun to develop in this subgroup | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomized into two groups" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "randomized into two groups" |
| Blinding of participants and personnel (performance bias) | High risk | Comparison with no treatment so blinding not possible |
| Blinding of outcome assessment (detection bias) | Unclear risk | It would be possible to blind the outcome assessor, as the data we used were assessed by an examiner looking for erythema and ulcers. However, it was not mentioned |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Seoul National University Hospital, Seoul, South Korea Number of centres: 1 Study duration: recruitment from March 2009 to August 2014 | |
| Participants | Inclusion criteria: aged 18 years or older with haematologic malignancy; due to receive intensive chemotherapy followed by autologous or allogeneic HSCT; normal oral cavity (grade 0 mucositis); ECOG score of 0 to 2 Exclusion criteria: received chemotherapy, radiotherapy or surgery within previous 3 weeks; history of allergy to the intervention or similar drugs; participation in other clinical trials within the previous 4 weeks with the potential to affect study results Cancer type: haematologic: multiple myeloma (Group A: 57%; Group B: 55%); lymphoma (Group A: 36%; Group B: 38%); other (Group A: 7%; Group B: 7%) Cancer treatment: prior to receiving autologous (Group A: 96%; Group B: 96%) or allogeneic HSCT, participants received the following conditioning regimens:
Age at baseline (years): Group A: median 53 (range 18 to 65); Group B: median 51 (range 19 to 65) Gender: Group A: 49% male; Group B: 54% male Number randomised: 138 (Group A: 69; Group B: 69) Number evaluated: 136 (Group A: 67; Group B: 69) | |
| Interventions | Comparison: EGF (recombinant human) versus placebo Group A: EGF (50 µg/mL) daily by oral spray, applied twice daily, sprayed (6 sprays per application) over the entire oral mucosa and then swallowed, no oral intake for 30 minutes afterwards; starting on first day of conditioning therapy and continuing until absolute neutrophil count recovered more than 1000 µL for 3 days and mucositis had resolved Group B: placebo as above Compliance: median patient compliance rate: Group A: 93% (range 35% to 100%); Group B: 92% (range 18% to 100%) Duration of treatment: variable and dependent on neutrophil recovery/resolution of mucositis | |
| Outcomes |
| |
| Notes | Sample size calculation: 62 participants per group required to detect 27% difference in incidence of grade 2 to 4 mucositis with 80% power and 5% significance Funding: multiple government grants; Daewoong Pharmaceutical Company (Seoul, Korea) only supplied interventions but provided no further funding and had no involvement with data collection, analysis or manuscript writing Declarations/conflicts of interest: none apparent Data handling by review authors: N/A Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly assigned...using a computer‐generated randomization protocol, by the Medical Research Collaborating Center, Seoul National University Hospital" Comment: adequate method used |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were randomly assigned...using a computer‐generated randomization protocol, by the Medical Research Collaborating Center, Seoul National University Hospital" Comment: although concealment not explicitly mentioned, use of centralised/third party randomisation ‐ likely to be done properly |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "placebo‐controlled, double‐blind" and "clinicians, patients, and investigators responsible for assessing outcomes and analyzing data were masked to treatment assignments" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "placebo‐controlled, double‐blind" and "clinicians, patients, and investigators responsible for assessing outcomes and analyzing data were masked to treatment assignments" Comment: all parties were blinded |
| Incomplete outcome data (attrition bias) | Low risk | Only 2 of 138 randomised participants were not included in the analysis |
| Selective reporting (reporting bias) | Low risk | Although most of the data were not usable in this review, this does not seem to be due to selective reporting |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Canada, USA and Europe (Hungary, Poland, Austria, Germany, Italy, Czech Republic) Number of centres: 46 Study duration: recruitment started August 2005, 4‐month follow‐up finished September 2007 | |
| Participants | Inclusion criteria: newly diagnosed, unresected stage 3 to 4B SCC of the oral cavity, oropharynx, nasopharynx, hypopharynx, or larynx; no evidence of secondary malignancy; at least 2 of 9 areas of the oral or oropharyngeal mucosa due to receive more than 50 Gy RT Exclusion criteria: not reported Cancer type: head and neck: oropharynx (Group A: 59%; Group B: 54%); oral cavity (Group A: 5%; Group B: 10%); larynx (Group A: 17%; Group B: 10%); hypopharynx (Group A: 15%; Group B: 23%); nasopharynx (Group A: 4%; Group B: 3%) Cancer treatment:
Age at baseline (years): Group A: mean 56 (SD 9); Group B: mean 55 (SD 8) Gender: Group A: 84% male; Group B: 85% male Number randomised: 188 (Group A: 94; Group B: 94) Number evaluated: 188 (Group A: 94; Group B: 94) | |
| Interventions | Comparison: KGF (palifermin) versus placebo Group A: KGF (180 µg/kg) by IV bolus over 30 to 60 seconds, 3 days prior to start of, and then once per week during radiochemotherapy, i.e. 8 doses (total dose = 1440 µg/kg) Group B: same schedule with placebo Compliance: 93% (SD 19%) of planned KGF doses were administered compared to 96% (SD 14%) in placebo group Duration of treatment: 8 treatment days (over 8 weeks) | |
| Outcomes |
| |
| Notes | Sample size calculation: assuming 60% of placebo group would develop grade 3 to 4 mucositis, 90 per group required to detect a reduction of at least 25% at 90% power and 5% significance Funding: "Supported by Amgen" (Swedish Orphan Biovitrum named as sponsor on trials registry, Amgen named as collaborator ‐ both pharmaceutical industry) Declarations/conflicts of interest: some authors had both employment or leadership positions and stock ownership within Amgen; some authors had received research funding from Amgen Data handling by review authors: N/A Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A centralized randomization system assigned patients to either palifermin or placebo in a 1:1 ratio" Comment: large multicentre trial using centralised randomisation method ‐ likely to be done properly |
| Allocation concealment (selection bias) | Low risk | Quote: "A centralized randomization system assigned patients to either palifermin or placebo in a 1:1 ratio" Comment: large multicentre trial using centralised randomisation method ‐ likely to be done properly |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "placebo‐controlled, double‐blind" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "placebo‐controlled, double‐blind" Comment: it is not clear who was blinded. There are subjective elements to the assessment of lower grades of oral mucositis using the WHO scale, requiring the patient's assessment of pain/soreness and their ability to swallow. Higher grades have more objective elements so may not be affected by potential lack of blinding of the assessor. This would be the same for other subjective and objective outcomes |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (5 arms) Location: UK Number of centres: 12 Study duration: recruitment from August 1989 to July 1990 | |
| Participants | Inclusion criteria: adults due to receive BMT after conditioning Exclusion criteria: myeloid malignancies Cancer type: mixed haematologic and solid (not reported by group): Hodgkin's disease (29%); non‐Hodgkin's lymphoma (33%); multiple myeloma (Group A: 20%); ALL (15%); solid (3%) Cancer treatment: prior to receiving BMT (autologous 84%; allogeneic 16%), participants received a conditioning regimen which consisted of chemotherapy only (71%) or with TBI (29%) Age at baseline (years): median 36 (range 17 to 64) (not reported by group) Gender: 69% male (not reported by group) Number randomised: 121 (Group A: 96; Group B: 25); Group A represents 4 arms with different dosages Number evaluated: 121 (Group A: 96; Group B: 25) | |
| Interventions | Comparison: G‐CSF versus placebo Group A: G‐CSF (2 µg/kg, 5 µg/kg, 10 µg/kg or 15 µg/kg) by 30‐minute IV daily starting from the day after BMT transplant and continuing until neutrophil count was > 1.0 x 10⁹/L for 3 consecutive days or until day 28, whichever occurred first Group B: as above but with placebo Compliance: not reported Duration of treatment: variable and dependent on neutrophil recovery | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: "Financial support for this trial was provided by Chugai Rhone Poulene" (pharmaceutical industry) Declarations/conflicts of interest: 1 author was employed by the funders Data handling by review authors: oral mucositis reported narratively in additional table Other information of note: G‐CSF administration only began after the conditioning and BMT transplant were completed, by which point oral mucositis may have already begun to develop (although time scale of conditioning/BMT transplant not reported) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised...in blocks of five by a computer‐generated randomisation schedule" Comment: adequate method used |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were randomised...in blocks of five by a computer‐generated randomisation schedule" Comment: insufficient information to determine whether or not the random sequence was adequately concealed |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "single blind...vehicle‐controlled" Comment: the use of a placebo (the 'vehicle') should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | High risk | Quote: "single blind...vehicle‐controlled" Comment: the quote implies that outcome assessment was not blinded |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | High risk | Oral mucositis not mentioned in the methods section as 1 of the study end points. It is only mentioned in the results narratively as there being no difference between any group, but with no data or P value |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Vita‐Salute San Raffaele University Hospital, Milan, Italy Number of centres: 1 Study duration: conducted from April 2009 to January 2015 | |
| Participants | Inclusion criteria: children aged 7 years or older with B‐cell lineage acute lymphoblastic leukaemia; scheduled to receive autologous HSCT after a conditioning regimen; Karnofsky performance score of 70 or more; were to have at least 1.5 x 10⁶ CD34+ cells reinfused per kilogram available for transplant; adequate cardiac, pulmonary, renal and hepatic function Exclusion criteria: not reported Cancer type: B‐cell lineage acute lymphoblastic leukaemia Cancer treatment: prior to receiving autologous HSCT (on day 0), participants received a conditioning regimen which consisted of TBI delivered in 8 fractions over 3 days (‐3 to ‐1) with at least 6 hours between fractions, followed by chemotherapy on day ‐1 (type and dose of radiotherapy and chemotherapy not reported) Age at baseline (years): Group A: median 11 (range 7 to 16); Group B: median 11 (range 7 to 16) Gender: Group A: 52% male; Group B: 44% male Number randomised: 60 (Group A: 30; Group B: 30) Number evaluated: 54 (Group A: 27; Group B: 27) | |
| Interventions | Comparison: KGF (palifermin) versus placebo Group A: KGF (60 µg/kg) by IV, on days ‐6 (3 days prior to start of conditioning regimen), ‐5 and ‐4, and on days 0 (the day of HSCT), 1, and 2 after transplant (total dose = 360 µg/kg) Group B: same schedule with placebo Compliance: not reported Duration of treatment: 6 treatment days (over 9 days) | |
| Outcomes |
| |
| Notes | Sample size calculation: numbers required not reported but was estimated at 80% power and 5% significance Funding: "This work was performed with Departmental funding only" Declarations/conflicts of interest: the authors report that they have no conflict of interest (supplemental material on journal website) Data handling by review authors: we emailed the lead author June 2017 for clarification of the oral mucositis data but, until we receive a response, we are unable to use those data Other information of note: unclear definitions of ulcerative (should be grade 2 to 4) and severe (should be grade 3 to 4): "...ulcerative OM (WHO grades | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A centralized randomization system assigned patients either to palifermin or conventional treatment in a 1:1 ratio......The statistician gave randomization list to the pharmacy, so the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment" |
| Allocation concealment (selection bias) | Low risk | Quote: "A centralized randomization system assigned patients either to palifermin or conventional treatment in a 1:1 ratio......The statistician gave randomization list to the pharmacy, so the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "The statistician gave randomization list to the pharmacy, so the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment. The pharmacy provided the research team with the blinded study medication" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The statistician gave randomization list to the pharmacy, so the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment. The pharmacy provided the research team with the blinded study medication" Comment: outcome assessors were clearly blinded |
| Incomplete outcome data (attrition bias) | Low risk | Overall attrition was same in both groups (10%) with the same reason given |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Vita‐Salute San Raffaele University Hospital, Milan, Italy Number of centres: 1 Study duration: conducted from April 2010 to January 2014 | |
| Participants | Inclusion criteria: children aged 9 to 15 years with B‐cell lineage acute lymphoblastic leukaemia; scheduled to receive allogeneic HSCT after a conditioning regimen Exclusion criteria: not reported Cancer type: B‐cell lineage acute lymphoblastic leukaemia Cancer treatment: prior to receiving allogeneic HSCT, participants received a conditioning regimen of a total of 12 Gy TBI delivered in 8 fractions of 1.5 Gy twice daily over 4 days Age at baseline (years): Group A: median 12 (range 8 to 15); Group B: median 12 (range 8 to 15) Gender: Group A: 50% male; Group B: 55% male Number randomised: 46 (Group A: 24; Group B: 22) Number evaluated: 46 (Group A: 24; Group B: 22) | |
| Interventions | Comparison: KGF (palifermin) versus placebo Group A: KGF (60 µg/kg) by IV, for 3 days prior to start of conditioning regimen and for 3 days after completion (total dose = 360 µg/kg) Group B: same schedule with placebo Compliance: not reported Duration of treatment: 6 treatment days (over unclear period of time ‐ not fully described) | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: "This work has been performed with departmental funding only" Declarations/conflicts of interest: "The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript" Data handling by review authors: we emailed the lead author June 2017 for clarification of the oral mucositis data but, until we receive a response, we are unable to use those data Other information of note: "Patients who had severe (grade 3 or 4) OM during blinded cycles received open‐label palifermin at the same dosages as in the other group. The research team assessed patients for OM at baseline before the cycle; at days 1, 2, 3 and at the end of the transplant cycle." ‐ nowhere else in the report suggests that there were multiple cycles of treatment; unclear definitions of ulcerative mucositis i.e. described correctly in one section as grades 2 to 4, but described in another section as grades 1 to 4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "No stratification was performed and two distinct computer‐generated a randomization lists. The statistician gave both randomization lists to the pharmacy, so the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment" |
| Allocation concealment (selection bias) | Low risk | Quote: "No stratification was performed and two distinct computer‐generated a randomization lists. The statistician gave both randomization lists to the pharmacy, so the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "The statistician gave both randomization lists to the pharmacy, so the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment. The pharmacy provided the research team with the blinded study medication" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "The statistician gave both randomization lists to the pharmacy, so the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment. The pharmacy provided the research team with the blinded study medication" Comment: outcome assessors were clearly blinded |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Turku University Central Hospital and Helsinki University Central Hospital, Finland Number of centres: 2 Study duration: recruitment from November 1994 to August 1996 | |
| Participants | Inclusion criteria: scheduled to receive total target dose of at least 56 Gy to the oropharyngeal mucosa Exclusion criteria: prior chemotherapy or radiotherapy; concurrent use of anticholinergic drugs; autoimmune thrombocytopenic purpura; WHO performance status higher than 2 Cancer type: head and neck: mobile tongue (Group A: 30%; Group B: 20%); oral cavity, other (Group A: 40%; Group B: 25%); oropharynx (Group A: 20%; Group B: 15%); nasopharynx (Group A: 5%; Group B: 10%); supraglottic larynx (Group A: 5%; Group B: 15%); hypopharynx (Group A: 0%; Group B: 15%) Cancer treatment:
Total target dose: Group A: median 65 Gy (range 56 to 68); Group B: median 66 Gy (range 58 to 73); oral surgery prior to RT: Group A: 20%; Group B: 30%; oral surgery after radiotherapy: 23 (not reported by group) Age at baseline (years): Group A: mean 63 (SD 10; range 47 to 87); Group B: mean 59 (SD 13; range 33 to 79) Gender: Group A: 60% male; Group B: 55% male Number randomised: 40 (Group A: 20; Group B: 20) Number evaluated: unclear; results presented as percentages | |
| Interventions | Comparison: GM‐CSF (molgramostim) plus sucralfate versus sucralfate alone Group A: after cumulative radiation dose of 10 Gy, GM‐CSF (150 µg to 300 µg ‐ dependent on body weight) by daily subcutaneous injection until the last day of RT; not given over weekends or during planned/unplanned treatment breaks; mean total dose = 3398 µg (range 300 µg to 7200 µg) Group B: no other treatment Compliance: not reported Duration of treatment: variable and dependent on duration of RT | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: GM‐CSF and sucralfate were both provided by pharmaceutical industry (Schering‐Plough Corporation and Orion‐Farmos Pharmaceuticals respectively) Declarations/conflicts of interest: not reported Data handling by review authors: no usable data Other information of note: GM‐CSF administration began after cumulative radiation dose of 10 Gy, by which point oral mucositis may have already begun to develop | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "assignment to the treatment groups was carried out via a phone call to the randomization center located at the Finnish Cancer Registry, Helsinki" |
| Allocation concealment (selection bias) | Low risk | Quote: "assignment to the treatment groups was carried out via a phone call to the randomization center located at the Finnish Cancer Registry, Helsinki" |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not possible as no placebo was used |
| Blinding of outcome assessment (detection bias) | Unclear risk | It would be possible to blind the outcome assessor for oral mucositis as the scale was fairly objective, but it was not mentioned. It would not be possible to blind oral pain assessment as this was done by the participant who was not blinded (however, we could not use the pain data so there was no bias for this outcome) |
| Incomplete outcome data (attrition bias) | Unclear risk | It is not clear how many participants were included in the analyses |
| Selective reporting (reporting bias) | High risk | Poor reporting of oral mucositis and oral pain |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Royal Marsden Hospital, London, UK Number of centres: 1 Study duration: recruitment from September 1997 to October 2000 | |
| Participants | Inclusion criteria: histologically proven T1 N0 or T2 N0 glottic carcinoma; due to receive RT with a 16‐fraction 3‐week regimen; WHO performance status 0 or 1 Exclusion criteria: renal or hepatic impairment; serious infections requiring antibiotics; taking corticosteroids or likely to require them; known allergy to GM‐CSF Cancer type: laryngeal Cancer treatment: accelerated radiotherapy: once‐daily fractions of 3.125 Gy, to a total dose of 50 Gy in 16 fractions over 21 days Age at baseline (years): Group A: median 60 (range 48 to 79); Group B: median 65 (range 32 to 70) Gender: Group A: 93% male; Group B: 86% male Number randomised: 29 (Group A: 15; Group B: 14) Number evaluated: 29 (Group A: 15; Group B: 14) | |
| Interventions | Comparison: GM‐CSF (molgramostim) versus no treatment Group A: GM‐CSF (150 µg) by daily subcutaneous injection, starting on day 14 of RT and continuing for 14 days i.e. for the last week of RT and for 1 week after completion of RT (total dose = 2100 µg) Group B: no treatment Compliance: 2 participants did not complete their course of GM‐CSF Duration of treatment: 14 days | |
| Outcomes |
| |
| Notes | Sample size calculation: 17 per group needed at 90% power and 5% significance to detect reduction from an anticipated 60% incidence of severe mucositis to 10% Funding: not reported Declarations/conflicts of interest: not reported Data handling by review authors: N/A Other information of note: imbalance in stage distribution, with more T2 patients in the GM‐CSF group. Consequently more of this group were treated with larger fields | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomly assigned to the active or control arms" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "were randomly assigned to the active or control arms" |
| Blinding of participants and personnel (performance bias) | High risk | Blinding not possible as no placebo was used |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "At each visit one of two independent observers, blinded to group allocation, scored mucositis..." |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Analgesic use reported as "No differences" with no data, however mucositis fully reported |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (7 arms) Location: USA Number of centres: 10 Study duration: not reported | |
| Participants | Inclusion criteria: 18 years or older; metastatic colon or rectal adenocarcinoma; scheduled to receive palliative 5FU and leucovorin chemotherapy; ECOG performance status 0 to 2 (ambulatory at least 50% of waking hours); life expectancy of at least 4 months; free of lesions and no recent history (within 30 days before baseline examination) of oral ulceration, herpes simplex, oral candidiasis, severe gingivitis, or the presence of active or chronic mucositis, xerostomia, or diarrhoea; absolute neutrophil count ≥ 1.5 x 109/L; platelet count ≥ 100 x 109/L; serum creatinine ≤ 2.0 mg/dL; serum bilirubin ≤ 2.0 mg/dL; serum aspartate amino transferase less than 5 times the upper limit of normal; absence of other serious concurrent medical illness Exclusion criteria: received chemotherapy, radiotherapy, or other investigational drugs within 4 weeks of enrolment (6 weeks for chemotherapy with mitomycin or nitrosoureas); any unresolved adverse event from previous therapy; major surgery within 2 weeks before study entry; history of insulin‐dependent diabetes mellitus; pregnant or breastfeeding; of child‐bearing potential and not using adequate contraceptive precautions; previous hypersensitivity reaction to leucovorin calcium or Escherichia coli‐derived material Cancer type: metastatic colorectal Cancer treatment: (palliative) leucovorin 20 mg/m² by rapid IV injection, followed immediately by 5FU 425 mg/m² by rapid IV injection for 5 consecutive days on days 4 to 8 of each 28‐day cycle Age at baseline (years): Group A: mean 62 (SD 10; range 44 to 84); Group B: mean 66 (SD 13; range 41 to 86) Gender: Group A: 57% male; Group B: 59% male Number randomised: 81 (Group A: 54; Group B: 27) Number evaluated: 81 (Group A: 54; Group B: 27) | |
| Interventions | Comparison: KGF (recombinant human) versus placebo Group A: KGF
Group B: placebo as above Compliance: 3 participants stopped KGF treatment due to adverse reactions involving the skin (1 in 60 and 2 in 80 µg/kg group) Duration of treatment: 3 days | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: "Supported by a grant from Amgen, Inc" (pharmaceutical industry) Declarations/conflicts of interest: not reported Data handling by review authors: we combined the 6 KGF groups to make a single pairwise comparison against placebo; in order to make a head‐to‐head comparison of doses we grouped the 3 lower doses (1 µg/kg, 10 µg/kg and 20 µg/kg) together and grouped the 3 higher doses (40 µg/kg, 60 µg/kg and 80 µg/kg) together to make pairwise groups for comparison Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "This study was a multicenter, randomized, double‐blinded, placebo‐controlled, phase I study" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "This study was a multicenter, randomized, double‐blinded, placebo‐controlled, phase I study" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blinded, placebo‐controlled" Comment: the use of a placebo should have ensured that blinding was successful; incidence of adverse events does not appear to differ enough between groups to cause unblinding |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blinded, placebo‐controlled" Comment: it is not clear who was blinded but the outcome is grade 2 to 4 WHO‐scale mucositis and it is unlikely that this would be affected by any lack of blinding |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: USA and Canada Number of centres: 7 Study duration: 1 November 1990 to 1 July 1993 | |
| Participants | Inclusion criteria: any age; undergoing allogeneic BMT (from HLA‐identical sibling) for haematological malignancy Exclusion criteria: due to receive methotrexate as part of GVHD prophylaxis; chronic lymphocytic leukaemia; chronic myelogenous leukaemia in blast crisis; acute lymphoblastic leukaemia or acute myelogenous leukaemia with failure at first induction or progressed beyond a second relapse; previously received cytokines; HIV; life expectancy less than 7 days Cancer type: haematologic malignancy: lymphoid malignancy (Group A: 21%; Group B: 16%); acute myeloid malignancy (Group A: 34%; Group B: 27%); chronic myeloid malignancy (Group A: 32%; Group B: 30%); multiple myeloma (Group A: 6%; Group B: 5%); myelodysplastic syndrome (Group A: 6%; Group B: 11%); aplastic anaemia (Group A: 2%; Group B: 11%) Cancer treatment: prior to receiving allogeneic BMT (from HLA‐identical sibling), participants received the following conditioning regimens: busulfan and cyclophosphamide with TBI (Group A: 9%; Group B: 16%) or without TBI (Group A: 32%; Group B: 34%); busulfan, cyclophosphamide, cytosine arabinoside, and methotrexate with TBI (Group A: 23%; Group B: 13%) or without TBI (Group A: 8%; Group B: 11%); cyclophosphamide and steroid with TBI (Group A: 0%; Group B: 2%); cyclophosphamide, cytosine arabinoside, and steroid with TBI (Group A: 23%; Group B: 18%); etoposide with TBI (Group A: 0%; Group B: 2%); etoposide, cytosine arabinoside, and cyclophosphamide with TBI (Group A: 2%; Group B: 0%); etoposide, cytosine arabinoside, cyclophosphamide, and asparaginase with TBI (Group A: 0%; Group B: 2%); etoposide, methotrexate, cytosine arabinoside, and steroid with TBI (Group A: 4%; Group B: 4%) Age at baseline (years): Group A: mean 32; Group B: mean 34 Gender: Group A: 60% male; Group B: 54% male Number randomised: 109 (Group A: 53; Group B: 56) Number evaluated: 109 (Group A: 53; Group B: 56) | |
| Interventions | Comparison: GM‐CSF (yeast‐derived recombinant human) versus placebo Group A: GM‐CSF (250 µg/m²) by 4‐hour IV infusion starting on day 0 (the day of BMT) to day 20 (total dose = 5250 µg/m²) Group B: as above with placebo Compliance: Group A: 13 participants (25%) stopped their intervention early: 11 due to adverse events (1 rash, 7 bone pain, 2 acute dyspnoea, 1 seizure); 2 (with no apparent toxicity) due to participant or physician request; Group B: 9 participants (16%) stopped their intervention early: 6 due to adverse events (2 rash, 2 bone pain, 1 elevated liver enzymes, 1 infections); 2 (on day 19) due to miscalculation of the number of days to receive the intervention; 1 (on day 9) due to severe mucositis and veno‐occlusive disease of the liver Duration of treatment: 21 days | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: "..product provided by Immunex" (pharmaceutical). Also mention of "sponsoring company" which is likely to be Immunex Declarations/conflicts of interest: not reported but 4 authors employed by Immunex Data handling by review authors: N/A Other information of note: GM‐CSF administration only began after the conditioning regimen, by which point oral mucositis may have already begun to develop | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Assignment to treatment was made via a randomization schema prepared by Almedica Corporation" Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Blinded numbered vials containing placebo or rhGM‐CSF were provided to each participating centre. The pharmacists, principal investigators, patients, support care personnel and sponsoring company were blinded to the study medication for the entire course of the study" Comment: probably done |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind placebo‐controlled" and "The pharmacists, principal investigators, patients, support care personnel and sponsoring company were blinded to the study medication for the entire course of the study" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind placebo‐controlled" and "The pharmacists, principal investigators, patients, support care personnel and sponsoring company were blinded to the study medication for the entire course of the study" Comment: everyone involved in the study was blinded |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | 5 participants in the placebo group received cytokines off study during the first 42 days after BMT but unlikely to bias the results in a meaningful way |
| Methods | Trial design: parallel (3 arms) Location: Russia Number of centres: 9 Study duration: recruitment from August 2006 to May 2007 | |
| Participants | Inclusion criteria: 18 years or older with colorectal cancer (stage I to IV); undergoing chemotherapy as primary cancer therapy; experienced WHO grade 2 or higher oral mucositis during first cycle of chemotherapy, but recovered prior to enrolment (i.e. grade 0); ECOG score of 0 to 2 Exclusion criteria: pregnant (or risk of pregnancy) or lactating; scheduled to receive RT to the head and neck; received other investigational drugs within 14 days of the start of the study; evidence of alcohol and drug abuse; pre‐existing conditions such as active fungal or herpetic infection Cancer type: colorectal (stage I to IV) Cancer treatment: all participants received 5FU (97% with leucovorin) but 1 received capecitabine; 6 participants (3 in low‐dose ITF, 3 in placebo) also received oxaliplatin; doses or regimens comparable between groups Age at baseline (years): Group A: median 62 ; Group B: median 56 ; Group C: median 59 Gender: Group A: 42% male; Group B: 33% male; Group C: 48% male Number randomised: 99 (Group A: 33; Group B: 33; Group C: 33) Number evaluated: 99 (Group A: 33; Group B: 33; Group C: 33) | |
| Interventions | Comparison: ITF (recombinant human) versus placebo Group A: ITF (10 mg/mL) oral spray, 300 µL (3 sprays) to the oral mucosa 8 times daily, starting on the first day (day 1) of the second chemotherapy cycle for total 14 days (total dose = 336 mg) Group B: ITF (80 mg/mL) oral spray as above (total dose = 2688 mg) Compliance: patient‐reported compliance was 97% Duration of treatment: 14 days | |
| Outcomes |
| |
| Notes | Sample size calculation: based on previous study, 80% power to detect 40% difference in incidence of WHO grade 2 or above Funding: The GI Company (pharmaceutical) Declarations/conflicts of interest: some authors had roles with the funding pharmaceutical company (and other companies) both compensated and uncompensated Data handling by review authors: we combined the 2 ITF groups to make a single pairwise comparison against placebo; we also made a separate comparison of the 2 ITF dosages Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly assigned" Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The patients were randomly assigned" |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, placebo‐controlled" Comment: it is not clear who was blinded. There are subjective elements to the assessment of oral mucositis using this scale, requiring the patient's assessment of pain/soreness and their ability to swallow but, as the participants were unaware of their group allocation, the assessment of oral mucositis can be considered to be blinded |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: USA and Australia Number of centres: 15 Study duration: not reported | |
| Participants | Inclusion criteria: 18 years or older with advanced (Duke's D) colon or rectal adenocarcinoma; scheduled to receive bolus 5FU and low‐dose leucovorin (Mayo regimen) as first‐line or subsequent therapy; normal oral cavity examination (no ulceration, herpes simplex, candidiasis, or severe gingivitis); ECOG score of 0 to 2; life expectancy of 4 months or more; absolute neutrophil count of 1.5 x 10⁹/L or higher; platelet count of 100 x 10⁹/L or higher; normal renal and hepatic function Exclusion criteria: previous radiotherapy or chemotherapy within 4 weeks or major surgery within 2 weeks of study day 1; insulin‐dependant diabetes; known allergy to leucovorin; known hypersensitivity to Escherichia coli‐derived material Cancer type: advanced colorectal (Duke's D) Cancer treatment: low‐dose leucovorin (20 mg/m²) by IV immediately followed by 5FU (425 mg/m²) by rapid IV once daily for 5 consecutive days on days 4 to 8 of each 28‐day cycle; 2 cycles (5FU dose could be decreased by 20% during cycle 2 if moderately severe toxicities occurred in cycle 1) Age at baseline (years): Group A: mean 65 (SD 11.2); Group B: mean 65 (SD 11.1) Gender: Group A: 57% male; Group B: 72% male Number randomised: 65 (not reported by group) Number evaluated: 64 (Group A: 28; Group B: 36) | |
| Interventions | Comparison: KGF (palifermin) versus placebo Group A: KGF (40 µg/kg) by IV for 3 consecutive days (days 1 to 3 of each 28‐day cycle) before the start of chemotherapy (total dose = 120 µg/kg) Group B: as above with placebo Compliance: not reported (only reports "palifermin was generally well tolerated") Duration of treatment: 3 days | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: "Supported by Amgen Inc" (pharmaceutical industry) Declarations/conflicts of interest: all authors were linked to the funding pharmaceutical company in terms of employment, consultancy, stock ownership, honoraria, and receipt of research funding Data handling by review authors: data were reported separately for the chemotherapy cycles 1 and 2 ‐ we used the data for cycle 1 Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly assigned (by center and prior chemotherapy)" Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Patients were randomly assigned (by center and prior chemotherapy)" Comment: insufficient information to determine method of random sequence generation |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, placebo‐controlled" Comment: it is not clear who was blinded. There are subjective elements to the assessment of oral mucositis using this scale, requiring the patient's assessment of pain/soreness and their ability to swallow but, as the participants were unaware of their group allocation, the assessment of oral mucositis can be considered to be blinded |
| Incomplete outcome data (attrition bias) | Low risk | Only 1 randomised participant was not included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: Helsinki University Central Hospital, Finland Number of centres: 1 Study duration: recruitment from October 1999 to April 2001 | |
| Participants | Inclusion criteria: undergone radical surgery for head and neck cancer and scheduled to receive postoperative RT to a total dose of 50 Gy or more to the oral and oropharyngeal mucosa Exclusion criteria: prior chemotherapy or RT; chronic autoimmune or inflammatory disease; WHO performance score > 2 Cancer type: head and neck: mobile tongue (Group A: 33%; Group B: 37%); floor of mouth (Group A: 19%; Group B: 16%); tonsil (Group A: 29%; Group B: 32%); oral cavity other (Group A: 19%; Group B: 16%) Cancer treatment: mean time from radical surgery to start of RT: Group A: 39 days (range 20 to 73); Group B: 38 days (range 20 to 56); conventionally fractionated RT to a total dose of 50 Gy to 60 Gy in 2‐Gy daily fractions, 5 times weekly (on weekdays) for 5 to 6 weeks, to the primary site and locoregional lymph nodes Age at baseline (years): Group A: median 56 (range 43 to 87); Group B: median 60 (range 24 to 72) Gender: Group A: 57% male; Group B: 79% male Number randomised: 40 (Group A: 21; Group B: 19) Number evaluated: 40 (Group A: 21; Group B: 19) | |
| Interventions | Comparison: GM‐CSF versus sucralfate Group A: starting after a cumulative RT dose of 10 Gy (after 1 week of RT); mouth was cleaned with water, then GM‐CSF (37.5 µg per 25 mL rinse) mouthwash rinsed around the mouth for 3 minutes then swallowed, 4 times daily after meals, on RT‐days (weekdays), until the end of RT (total dose dependent on duration of RT) Group B: as above but with sucralfate (1 g per 25 mL rinse) (total dose dependent on duration of RT) Compliance: not reported (only reports "both mouthwashes were well tolerated, and none of the patients reported any adverse effects related to the mouthwashes") Duration of treatment: 4 to 5 weeks (dependent on duration of RT) | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported Funding: not reported Declarations/conflicts of interest: not reported Data handling by review authors: we used oral mucositis incidence (maximum score experienced per patient) data provided by the authors; all participants experienced mucositis (grade 1 or above) as they had already received a week of RT before the intervention started, therefore we felt an analysis of incidence of any grade of mucositis should not be included Other information of note: GM‐CSF/sucralfate administration only began after 1 week of RT, by which point oral mucositis may have already begun to develop | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was done using computer‐generated random digits" Comment: adequate method used |
| Allocation concealment (selection bias) | Low risk | Quote: "they were assigned to a treatment group by way of a telephone call to the randomization office" Comment: third party/remote randomisation would have ensured concealment of the random sequence from those recruiting participants |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind" and "Both solutions looked alike, and neither the investigators nor the patients were aware of the contents of the solutions given. The drug vials were marked with a study code that prevented identification of the allocation group" Comment: adequate methods to ensure blinding |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blinded, placebo‐controlled" Comment: nobody involved in the study was aware of group allocation |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: USA Number of centres: not reported Study duration: recruitment from January 1995 to April 1996 | |
| Participants | Inclusion criteria: 18 years or older with histologically proven head and neck malignancy; mucosa of the oropharynx and/or oral cavity to be included in RT portal; Karnofsky performance score of 60 or more; no known hypersensitivity to E coli‐derived proteins; haemoglobin and platelet counts 100 x 10⁹/L or higher; absolute neutrophil count higher than 1.5 x 10⁹/L; normal blood pressure; agreement to bring dentition to acceptable level prior to RT (teeth with periapical abscesses or severe periodontal disease extracted, followed by a 10‐day healing period allowance) Exclusion criteria: lactating/pregnant/females not taking effective form of contraception; scheduled to receive chemotherapy or radiosensitising drugs during the planned RT; history of myeloid malignancy; underlying collagen vascular disease; active rheumatoid arthritis Cancer type: head and neck: nasopharynx (Group A: 0; Group B: 1); oropharynx (Group A: 2; Group B: 1); tongue (Group A: 2; Group B: 1); larynx (Group A: 2; Group B: 1); other/unknown (Group A: 2; Group B: 2) Cancer treatment: radiotherapy in 1.8 Gy to 2 Gy standard daily fractions from Monday to Friday, to total dose 50 Gy or more Age at baseline (years): not reported Gender: Group A: 100% male; Group B: 83% male Number randomised: 14 (Group A: 8; Group B: 6) Number evaluated: 14 (Group A: 8; Group B: 6) | |
| Interventions | Comparison: G‐CSF (r‐metHuG‐CSF) (filgrastim) versus placebo Group A: G‐CSF (starting at 3 µg/kg and titrated to keep neutrophil count between 10 x 10⁹/L and 30 x 10⁹/L) by daily subcutaneous injection, starting on the first day of RT (weekdays), until the end of RT (total dose dependent on duration of RT and neutrophil counts) Group B: placebo as above Compliance: not reported (only reports "Filgrastim was well tolerated") Duration of treatment: variable and dependent on duration of RT | |
| Outcomes |
| |
| Notes | Sample size calculation: 54 required to detect 30% decrease in incidence of grade 2 or 3 mucositis at 80% power at the 5% significance level Funding: "Financial support was provided through a grant from Amgen Inc" (pharmaceutical industry) Declarations/conflicts of interest: not reported Data handling by review authors: interruptions to cancer treatment outcome only reported narratively Other information of note: study was stopped after an interim analysis. Authors state that "owing to administrative obstacles, completion of the trial is not possible", rather than due to previously stated early stopping rules | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were randomized equally between the two treatment groups" and "The study material and randomization list were held by the UCLA Pharmacy for the duration of the study" Comment: method of random sequence generation not described but done by UCLA Pharmacy and therefore probably done adequately |
| Allocation concealment (selection bias) | Low risk | Quote: "Amgen Inc...prepared and packaged all drug and placebo in identical containers, with the only designator being the randomization number. The study material and randomization list were held by the UCLA Pharmacy for the duration of the study" Comment: pharmacy‐controlled randomisation would have ensured concealment of the random sequence from those recruiting participants |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "Amgen Inc...prepared and packaged all drug and placebo in identical containers, with the only designator being the randomization number" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "A single examiner...who was blinded to the patients' randomization status...scored mucositis on a weekly basis" Comment: both participants and outcome assessor were blinded |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | Although the study reports an interim analysis only, the study was stopped due to administrative reasons and is unlikely to introduce bias |
| Methods | Trial design: parallel (2 arms) Location: USA Number of centres: 13 Study duration: recruitment from March 2001 to October 2002 | |
| Participants | Inclusion criteria: 18 years or older; Karnofsky performance score of 70 or more; scheduled to undergo autologous HSCT after conditioning regimen of fractionated TBI plus etoposide and cyclophosphamide for haematological cancers; adequate cardiac, pulmonary, renal, and hepatic function Exclusion criteria: not reported Cancer type: haematologic: NHL (Group A: 68%; Group B: 65%); Hodgkins (Group A: 20%; Group B: 22%); multiple myeloma (Group A: 10%; Group B: 8%); leukaemia (Group A: 2%; Group B: 5%) Cancer treatment: prior to autologous HSCT, participants received the following conditioning regimen:
All participants received G‐CSF (filgrastim) 5 µg/kg per day from HSCT until neutrophil recovery Age at baseline (years): Group A: median 48 (range 18 to 69); Group B: median 49 (range 19 to 68) Gender: Group A: 56% male; Group B: 68% male Number randomised: 214 (Group A: 107; Group B: 107) Number evaluated: 212 (Group A: 106; Group B: 106) | |
| Interventions | Comparison: KGF (palifermin) versus placebo Group A: KGF (60 µg/kg) by IV for 3 consecutive days starting 3 days before RT, followed by 3 more doses after HSCT starting on the day of HSCT (total dose = 360 µg/kg) Group B: placebo as above Compliance: 212 participants received at least 1 dose of their allocated intervention and 205 participants (Group A: 103; Group B: 102) "completed the study" (it is not clear whether or not this means that they received all doses) Duration of treatment: 6 treatment days over 13 to 14 days | |
| Outcomes |
| |
| Notes | Sample size calculation: 210 participants required to detect a mean difference in duration of severe oral mucositis of at least 3 days (SD 6.6) at 90% power and 5% significance Funding: "Funded by Amgen" (pharmaceutical industry) Declarations/conflicts of interest: the majority of authors were linked to the funding pharmaceutical company in terms of employment, consulting fees, lecture fees, receipt of research funding, and ownership of equity Data handling by review authors: N/A Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients were randomly assigned in a 1:1 ratio" Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "patients were randomly assigned in a 1:1 ratio" Comment: insufficient information to determine method of random sequence generation |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "placebo‐controlled, double‐blind" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "placebo‐controlled, double‐blind" Comment: it is not clear who was blinded. There are subjective elements to the assessment of lower grades of oral mucositis using the WHO scale, requiring the patient's assessment of pain/soreness and their ability to swallow. Higher grades have more objective elements so may not be affected by potential lack of blinding of the assessor |
| Incomplete outcome data (attrition bias) | Low risk | Only 2 randomised participants (1 per group) were not included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: USA Number of centres: 1 Study duration: recruitment from January 1992 to December 1996 | |
| Participants | Inclusion criteria: 18 years or older with histologically proven AJCC stage II to IV squamous cell carcinoma of the head and neck; undergone gross complete resection with negative pathological surgical margins and medically fit to begin RT within 8 weeks of surgery; Karnofsky performance score of 80% or more; adequate haematologic and serum metabolic laboratory indices Exclusion criteria: nasopharyngeal cancer; concurrent active malignancy other than localised; nonmelanoma skin cancer; previous RT to head and neck; previous chemotherapy; positive serum β‐human chorionic gonadotropin in women of procreative potential; need for tube feeding at the start of RT Cancer type: stage II to IV squamous cell carcinoma of the head and neck: hypopharynx (Group A: 11%; Group B: 5%); larynx (Group A: 16%; Group B: 23%); oral cavity (Group A: 26%; Group B: 27%); oropharynx (Group A: 21%; Group B: 32%); unknown primary (Group A: 26%; Group B: 14%) Cancer treatment: postoperative external beam RT in once‐daily fractions of 1.8 Gy, 5 days per week, to total dose of 63 Gy at primary site and involved neck (54 Gy to regional lymphatics at risk for subclinical metastasis; spinal cord dose limited to 45 Gy) Age at baseline (years): Group A: median 67 (interquartile range 59 to 75); Group B: median 61 (interquartile range 54 to 67) Gender: Group A: 79% male; Group B: 73% male Number randomised: 41 (Group A: 19; Group B: 22) Number evaluated: 40 (Group A: 19; Group B: 21) | |
| Interventions | Comparison: G‐CSF versus placebo Group A: G‐CSF (3 µg/kg) by daily subcutaneous injection, 7 days per week, starting 3 days before the start of RT and continued to end of RT (total dose = dependent on duration of RT) Group B: placebo as above Compliance: not reported Duration of treatment: variable and dependent on duration of RT | |
| Outcomes |
| |
| Notes | Sample size calculation: planned sample sample size was 66 per group to detect absolute difference of 20% in PEG tube use (from 10% in one group to 30% in the other) at 80% power and 5% significance Funding: "This study was supported by NIH grant #CA69913" (government) Declarations/conflicts of interest: "No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this article" Data handling by review authors: although the scale for assessing oral mucositis does not completely match the 0 to 4 scales (such as WHO, etc), it was possible to dichotomise it for use in the 'any mucositis' meta‐analysis, and we also used grade 3 (confluent mucositis) as incidence of severe mucositis Other information of note: planned to enrol 132 participants but stopped due to slow recruitment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomized...by randomly permuted blocks...A randomization list was prepared by the Memorial Sloan‐Kettering Cancer Center Biostatistics Service and held by the pharmacy" Comment: specialist centre used |
| Allocation concealment (selection bias) | Low risk | Quote: "A randomization list was prepared by the Memorial Sloan‐Kettering Cancer Center Biostatistics Service and held by the pharmacy. Investigators did not have access to this list, ensuring that allocation could not be predicted before registration or changed afterwards" Comment: central/remote randomisation would have ensured concealment of the random sequence from those recruiting participants |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "All patients and treating physicians were blinded to treatment group assignment" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "All patients and treating physicians were blinded to treatment group assignment" Comment: the treating physician was the outcome assessor |
| Incomplete outcome data (attrition bias) | Low risk | Only 1 randomised participant was not included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: University of Texas MD Anderson Cancer Center, USA Number of centres: 1 Study duration: recruitment from December 2005 to February 2008; last follow‐up in May 2008 | |
| Participants | Inclusion criteria: aged 15 to 65 years with sarcoma; due to start chemotherapy at the centre; Karnofsky performance score of 80% or more; adequate bone marrow, renal, and hepatic function Exclusion criteria: history of pelvic RT; clinically significant cardiac disease; undergone surgery within the previous 2 weeks Cancer type: sarcoma Cancer treatment: doxorubicin (total dosage 90 mg/m²) administered by continuous IV infusion over 72 hours, and ifosfamide (total dosage 10 g/m²) administered by 3‐hour IV infusion for 4 days; participants with osteosarcoma (Group A: 2; Group B: 1) received the same dosage of doxorubicin but with intra‐arterial cisplatin (120 mg/m²); all participants received G‐CSF (pegfilgrastim) the day after chemotherapy; cycle repeated every 21 days; planned 6 cycles Age at baseline (years): Group A: median 42 (range 17 to 63); Group B: median 39 (range 15 to 64) Gender: Group A: 53% male; Group B: 50% male Number randomised: 48 (Group A: 32; Group B: 16) Number evaluated: 48 (Group A: 32; Group B: 16) | |
| Interventions | Comparison: KGF (palifermin) versus placebo Group A: KGF (180 µg/kg) by IV as single dose 3 days before the start of each chemotherapy cycle Group B: placebo as above Compliance: the proportion of participants that completed all 6 blinded cycles (i.e. they took their allocated intervention) was higher in Group A (63%) than Group B (31%) Duration of treatment: 1 day per 3‐week cycle; planned total 6 days of intervention over 18 weeks | |
| Outcomes |
| |
| Notes | Sample size calculation: 48 participants required to detect absolute difference of 50% (from 26% in Group A to 76% in Group B) in grade 2 to 4 mucositis at 88% power and 5% significance Funding: "Amgen provided the palifermin and partial funding for the study" (pharmaceutical industry) Declarations/conflicts of interest: principal investigator is a member of the Amgen board Data handling by review authors: we only report data from the first 2 cycles (blinded phase) as very few participants received placebo in the remaining cycles Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Two distinct computer‐generated randomization lists were prepared by the University of Texas M.D. Anderson Cancer Center, Department of Biostatistics, one for the 20 patients who consented to pharmacokinetic sampling and the other for the 28 patients who did not. For the pharmacokinetics cohort, the treatment allocation ratio was 4 patients receiving palifermin to 1 receiving placebo, in blocks of 5; for the other cohort, the ratio was 4 patients receiving palifermin to 3 receiving placebo, in blocks of 14" Comment: adequate method used |
| Allocation concealment (selection bias) | Low risk | Quote: "The statistician provided both randomization lists to the pharmacy, so the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment. At patient enrolment, the research team notified the pharmacy, which assigned the patient the next sequential slot and treatment from the appropriate randomization list on the basis of whether he or she had consented to pharmacokinetic sampling. The pharmacy provided the research team with the blinded study medication. Upon completion of the study, pharmacy provided the statistician with the 2 randomization lists, including individual patient treatment assignments, for analysis" Comment: pharmacy‐controlled randomisation would have ensured concealment of the random sequence from those recruiting participants |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment" and "Blinding might not have been maintained because of adverse effects of palifermin" Comment: some personnel may not have been blinded due to increased adverse effects, although adverse effects from palifermin may have been difficult to isolate from adverse effects of cancer treatment |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "the patient and the clinical research team (who assessed outcomes) were blinded to the study treatment" and "Blinding might not have been maintained because of adverse effects of palifermin" and "patients were assessed at each cycle by both research and clinical teams, including those without direct knowledge of the protocol" Comment: it seems unlikely that lack of blinding would affect outcomes as the higher grades of oral mucositis assessed in this study are more objective; also, some were assessed by personnel without knowledge of the protocol |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (2 arms) Location: the Netherlands Number of centres: 1 Study duration: recruitment from May 1997 to August 1999 | |
| Participants | Inclusion criteria: malignant disease and due to have myeloablative treatment followed by autologous or allogeneic BMT or PBSCT Exclusion criteria: not reported Cancer type: haematologic: lymphoma (Group A: 28%; Group B: 50%); acute leukaemia (Group A: 28%; Group B: 28%); CML (Group A: 22%; Group B: 6%); multiple myeloma (Group A: 22%; Group B: 17%) Cancer treatment: prior to autologous or allogeneic BMT or PBSCT, participants received the following conditioning regimens:
Lymphoma patients received BEAM; other patients received CYTBI or BUCY; nearly all participants received autologous or allogeneic PBSCT Age at baseline (years): Group A: median 47 (range 25 to 63); Group B: median 48 (range 18 to 62) Gender: Group A: 61% male; Group B: 39% male Number randomised: 36 (Group A: 18; Group B: 18) Number evaluated: 36 (Group A: 18; Group B: 18) | |
| Interventions | Comparison: GM‐CSF versus placebo Group A: GM‐CSF (300 µg daily dose) gel, 5 mL twice daily (early in the morning and before going to sleep) kept in the mouth for as long as possible and then swallowed; no oral intake for 1 hour afterwards; starting on day 1 (the day after the day of transplant) and continued until neutrophil recovery (typically up to 14 days after transplant) Group B: placebo as above Compliance: 8 participants (Group A: 4; Group B: 4) did not complete the study; they all cited the main reason being nausea and the taste of the gel Duration of treatment: variable and dependent on neutrophil recovery | |
| Outcomes |
| |
| Notes | Sample size calculation: not reported ("GM‐CSF was supplied by the sponsor for 18 patients so that 36 patients could be included in the study. This should be enough to demonstrate a clinically significant difference") Funding: "We thank Novartis and Schering‐Plough for supplying the GM‐CSF" (pharmaceutical industry) Declarations/conflicts of interest: not reported Data handling by review authors: N/A Other information of note: GM‐CSF administration only began after the conditioning treatment had been completed, by which point oral mucositis may have already begun to develop | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "the patients were randomized to receive GM‐CSF or placebo" Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "the patients were randomized to receive GM‐CSF or placebo" Comment: insufficient information to determine method of random sequence generation |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind placebo‐controlled" and "There was no difference in taste or appearance between the placebo and the GM‐CSF" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind placebo‐controlled" and "There was no difference in taste or appearance between the placebo and the GM‐CSF" Comment: it is not clear who was blinded. There are subjective elements to the assessment of lower grades of oral mucositis using the WHO scale, requiring the patient's assessment of pain/soreness and their ability to swallow. Higher grades have more objective elements so may not be affected by potential lack of blinding of the assessor |
| Incomplete outcome data (attrition bias) | Low risk | All randomised participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | Data for outcomes of this review were reported appropriately |
| Other bias | Low risk | No other sources of bias are apparent |
| Methods | Trial design: parallel (4 arms) Location: South Korea Number of centres: 6 Study duration: recruitment from January to August 2007 | |
| Participants | Inclusion criteria: 18 years or older with histological evidence of head and neck cancer; due to receive at least 5 weeks of primary RT, primary chemoradiotherapy, or postoperative RT; agreement to have complete medical history and physical examination; ECOG score of 0 to 2; white blood counts 3 x 10³/L or higher; platelet counts 100 x 10³/L or higher Exclusion criteria: oral ulcers; herpes simplex virus; severe periodontal disease; serum creatine levels greater than 2 mg/dL; ALT/AST values greater than 200 IU/L; cytotoxic chemotherapy or RT within 3 weeks of the start of the study; systemic or topical corticosteroids within 30 days of the start of the study; participated in another clinical study within 30 days of the start of the study Cancer type: head and neck: nasopharynx (Group A: 36%; Group B: 32%); oropharynx (Group A: 24%; Group B: 25%); oral cavity (Group A: 19%; Group B: 25%); hypopharynx (Group A: 2%; Group B: 4%); other (Group A: 19%; Group B: 14%) Cancer treatment:
Age at baseline (years): Group A: median 56 (range 18 to 75); Group B: median 51 (range 18 to 77) Gender: Group A: 69% male; Group B: 57% male Number randomised: 113 (Group A: 85; Group B: 28) Number evaluated: 103 (Group A: 76; Group B: 27) for incidence of moderate to severe mucositis; 94 (Group A: 70; Group B: 24) for incidence of severe mucositis | |
| Interventions | Comparison: EGF (recombinant human) versus placebo Group A: EGF
Group B: placebo as above Compliance: not reported Duration of treatment: 5 weeks | |
| Outcomes |
| |
| Notes | Sample size calculation: allowing for 10% attrition, 26 participants per group required Funding: "This study was supported by a grant from the National R&D Program for Cancer Central, Ministry of Health, Welfare and Family Affairs, Republic of Korea (0620270)" (government) and "The EGF and placebo treatments were supplied free of charge" (presumably pharmaceutical industry) Declarations/conflicts of interest: not reported Data handling by review authors: we combined the 3 EGF groups to make a single pairwise comparison against placebo; no formal statistical analysis was undertaken for the different EGF dosages Other information of note: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "We assigned patients randomly to 4 arms" Comment: insufficient information to determine method of random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "We assigned patients randomly to 4 arms" Comment: insufficient information to determine method of random sequence generation |
| Blinding of participants and personnel (performance bias) | Low risk | Quote: "double‐blind, placebo‐controlled" and "Three concentrations of EGF and a placebo containing the drug delivery vehicle were manufactured, packaged, and supplied in a double‐blind fashion" Comment: the use of a placebo should have ensured that blinding was successful |
| Blinding of outcome assessment (detection bias) | Low risk | Quote: "double‐blind, placebo‐controlled" Comment: it is not clear who was blinded. There are subjective elements to the assessment of most grades of oral mucositis using the RTOG scale, requiring the patient's assessment of pain. Grade 4 is more objective so may not be affected by potential lack of blinding of the assessor |
| Incomplete outcome data (attrition bias) | Low risk | Overall attrition was 9% (Group A: 11%; Group B: 4%). Slight differential between groups but the reasons were reported and mostly unrelated to interventions/outcomes. Unlikely to have biased the results |
| Selective reporting (reporting bias) | High risk | Several outcomes were assessed but not properly reported ("No secondary endpoint showed any difference between the placebo and study groups") |
| Other bias | Low risk | No other sources of bias are apparent |
5FU = fluorouracil; AJCC = American Joint Committee on Cancer; ALL = acute lymphoblastic leukaemia; allogeneic = cells from donor; AML = acute myelogenous leukaemia; AUC = area under the curve; autologous = patients' own cells; BMT = bone marrow transplantation; CALGB = Cancer and Leukaemia Group B; cGy = centigray; CML = chronic myelogenous leukaemia; CRT = chemoradiotherapy; CT = chemotherapy; ECOG = Eastern Co‐operative Oncology Group; EGF = epidermal growth factor; EQ‐5D = European Quality Of Life Utility Scale; FACT = Functional Assessment of Cancer Therapy; FDA = US Food and Drug Administration; G‐CSF = granulocyte‐colony stimulating factor; GM‐CSF = granulocyte‐macrophage colony‐stimulating factor; GVHD = graft‐versus‐host disease; Gy = gray; HLA = human leukocyte antigen; HSCT = haematopoietic stem cell transplantation; IA = intra‐arterial; ITF = intestinal trefoil factor; ITT = intention‐to‐treat; IV = intravenous; KGF = keratinocyte growth factor; MDS = myelodysplastic syndrome; N/A = not applicable; NCI‐CTC = National Cancer Institute common toxicity criteria; NHL = non‐Hodgkin's lymphoma; NIH = National Institutes of Health; OMAS = oral mucositis assessment scale; OMDQ = oral mucositis daily questionnaire; OMWQ‐HN = Oral Mucositis Weely Questionnaire ‐ Head and Neck cancer; PBPC = peripheral blood progenitor cell; PBSCT = peripheral blood stem cell transplantation; PEG = percutaneous endoscopic gastrostomy; PP = per protocol; RT = radiotherapy; RTOG = Radiation Therapy Oncology Group; SCC = squamous cell carcinoma; SCT = stem cell transplantation; SD = standard deviation; SMD = standardised mean difference; TBI = total‐body irradiation; TGF = transforming growth factor; TPN = total parenteral nutrition; VAS = visual analogue scale; WBC = white blood cell; WHO = World Health Organization; WCCNR = Western Consortium for Cancer Nursing Research.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Recombinant human interleukin‐11 versus placebo. Study stopped early due to adverse event triggering preset stopping rule ‐ data only for 10 patients in rhIL group and 3 placebo | |
| TGF‐beta(2) versus placebo. Cross‐over study with no first period data reported (see Types of studies) | |
| TGF‐beta(3) versus placebo. Participants assigned sequentially, not randomised | |
| G‐CSF versus thymopentin versus G‐CSF plus thymopentin versus placebo. Oral mucositis not mentioned (unknown if measured) | |
| G‐CSF (lipegfilgrastim) versus G‐CSF (pegfilgrastim). Oral mucositis not mentioned (unknown if measured). Insufficient information (abstract) | |
| GM‐CSF versus no treatment. Unclear if randomised or not. Only 13 participants. Insufficient information (abstract) | |
| KGF (palifermin) versus standard care. No random allocation | |
| ATL‐104 versus placebo. Not RCT ‐ this study combines patients who were in cohorts with increasing doses of mouthrinse to assess safety, with an RCT | |
| GM‐CSF versus placebo. Primary outcome was survival/cure, with mucositis as a toxicity. Unclear if mucositis was oral or gastrointestinal | |
| G‐CSF versus no treatment. No mention of randomisation and no description of when intervention given in relation to cancer treatment | |
| GM‐CSF versus placebo. Unclear if mucositis was oral or gastrointestinal | |
| G‐CSF versus placebo. Only 8 patients, 32 chemotherapy cycles and results presented assuming independent | |
| G‐CSF (pegfilgrastim) versus G‐CSF (filgrastim). Incidence of stomatitis reported in adverse events table | |
| G‐CSF (pegteograstim) versus G‐CSF (pegfilgrastim). Incidence of stomatitis reported in adverse events table | |
| GM‐CSF versus placebo. Unclear if mucositis was oral or gastrointestinal | |
| AG013 versus placebo. AG013 is composed of recombinant Lactococcus lactis engineered to secrete human Trefoil Factor 1. Randomised at first but participants not developing oral mucositis in chemotherapy cycle 1 were excluded from the next phase where oral mucositis was measured, so randomisation was lost | |
| G‐CSF (leridistim) versus G‐CSF (filgrastim). Incidence of stomatitis reported in adverse events table | |
| KGF (palifermin) versus placebo. Study terminated at 21 participants (298 planned) due to positive preliminary results from other palifermin studies | |
| KGF (palifermin) versus placebo. Study terminated at 5 participants due to departure of principal investigator and slow enrolment | |
| G‐CSF versus no treatment. Unclear if mucositis was oral or gastrointestinal | |
| GM‐CSF versus placebo. Some participants (6%) had oral mucositis at baseline | |
| GM‐CSF versus no treatment. Probably not RCT ‐ described as comparative study. Only 10 participants. Insufficient information (abstract) | |
| G‐CSF versus no treatment. Incidence of stomatitis reported in adverse events table | |
| KGF (palifermin) versus no treatment. From full text it is not RCT ‐ retrospective and allocation of KGF/no KGF based on doctor's decision |
G‐CSF = granulocyte‐colony stimulating factor; GM‐CSF = granulocyte‐macrophage colony‐stimulating factor; KGF = keratinocyte growth factor; RCT = randomised controlled trial; rhIL = recombinant human interleukin; TGF = transforming growth factor.
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Multicentre, double‐blind, randomised placebo‐controlled trial |
| Participants | 18 years or older with lymphoma and due to undergo high‐dose BEAM chemotherapy and autologous stem cell transplantation as inpatient |
| Interventions | Whey growth factor extract at 13.5 mg/mL in sterile saline versus placebo (sterile saline) |
| Outcomes |
|
| Notes | Funding: commercial sector/industry (TGR Biosciences, Australia) Contact: correspondence with pharmaceutical company suggests no benefit |
| Methods | Multicentre, randomised controlled trial (no placebo) |
| Participants | Head and neck cancer; receiving continuous course of radiotherapy for 6 to 7 weeks |
| Interventions | GM‐CSF (subcutaneous) versus no treatment |
| Outcomes | Signs and symptoms of oral mucositis: erythema, pain and dysphagia each measured on 0 to 3 scale |
| Notes | Abstract only (we were unable to link this abstract to a full‐text report) Some P values suggest benefit for GM‐CSF at some time points Quote: "GM‐CSF reduces the incidence and severity of radiation mucositis and allows the completion of the XRT treatment without protraction" |
| Methods | Randomised controlled trial (no placebo) |
| Participants | Anaemic participants with head and neck cancer receiving radiotherapy once daily (1.8 Gy or 2 Gy) to doses of 66 Gy to 70 Gy |
| Interventions | Recombinant human erythropoietin versus no treatment |
| Outcomes | Incidence of grade 3 mucositis and dermatitis |
| Notes | Abstract only (we were unable to link this abstract to a full‐text report) Higher rate of mucositis in the no‐treatment group (5.9% versus 0%) |
| Methods | Randomised placebo‐controlled trial |
| Participants | Adults (aged 19 to 68 years) undergoing haematopoietic stem cell transplantation |
| Interventions | G‐CSF versus placebo |
| Outcomes |
|
| Notes | Translation provided insufficient information. Discrepancy between graph legends and descriptions |
| Methods | Randomised controlled trial (no placebo) |
| Participants | Children with B‐cell non‐Hodgkin's lymphoma (B‐NHL) receiving chemotherapy |
| Interventions | G‐CSF versus no treatment |
| Outcomes |
|
| Notes | Abstract only (we were unable to link this abstract to a full‐text report) Quote: "G‐CSF+ patients showed a positive impact on the meantime to neutrophil recovery and hospital stay, but they had no impact in incidences of febrile neutropenia, infections, stomatitis, and total cost" |
| Methods | Double‐blind, randomised placebo‐controlled trial (1 of the 3 arms is a cross‐over) |
| Participants | 18 years or older with head and neck cancer due to receive conventional or hyperfractionated radiotherapy or intensity‐modulated radiotherapy (IMRT) with or without concurrent chemotherapy |
| Interventions | GM‐CSF mouthwash versus salt and soda mouthwash versus both (cross‐over arm) |
| Outcomes |
|
| Notes | Trials registry number: NCT00293462 Funding: University of California, San Francisco; National Cancer Institute (NCI) |
| Methods | Double‐blind, randomised placebo‐controlled trial |
| Participants | 18 years or older with resected colon cancer (American Joint Committee on Cancer Stage 2B or 3) and due to receive 5‐FU and leucovorin |
| Interventions | KGF versus placebo |
| Outcomes |
|
| Notes | Trials registry number: NCT00393822 Funding: Amgen (pharmaceutical industry) |
| Methods | Randomised controlled trial (no placebo) |
| Participants | Adults (aged 18 to 75 years) with head and neck cancer due to receive radiotherapy |
| Interventions | Recombinant human EGF versus Chining |
| Outcomes |
|
| Notes | Trials registry number: NCT02303197 Funding: Tianjin Medical University Cancer Institute and Hospital |
| Methods | Double‐blind, randomised placebo‐controlled trial |
| Participants | 16 years or older due to receive preparative cancer treatment regimen followed by autologous or allogeneic HSCT (cancer type not reported) |
| Interventions | KGF versus placebo |
| Outcomes |
|
| Notes | Trials registry number: NCT02313792 Funding: The Catholic University of Korea; Collaborator: "BLNH" (probably pharmaceutical industry) |
| Methods | Randomised controlled trial (no placebo) |
| Participants | Children with non‐Hodgkin's lymphoma due to receive 2 courses of COPAD induction chemotherapy |
| Interventions | G‐CSF versus no treatment |
| Outcomes |
|
| Notes | Quote: "The incidence of grade 3 and 4 mucositis was similar in both arms" |
| Methods | Multicentre, double‐blind, randomised placebo‐controlled trial |
| Participants | 18 years or older with multiple myeloma or lymphoma due to receive high‐dose chemotherapy (with or without TBI) followed by autologous HSCT |
| Interventions | Recombinant human FGF‐20 (velafermin) (3 arms with different dosages) versus placebo |
| Outcomes |
|
| Notes | Abstract only (we were unable to link this abstract to a full‐text report) Trials registry number: NCT00104065 |
| Methods | Multicentre, double‐blind, randomised placebo‐controlled trial |
| Participants | 18 years or older with multiple myeloma or lymphoma undergoing high‐dose chemotherapy (with or without TBI) followed by autologous HSCT |
| Interventions | Recombinant human FGF‐20 (velafermin) (3 arms with different dosages) versus placebo |
| Outcomes |
|
| Notes | Abstract only (we were unable to link this abstract to a full‐text report) Trials registry number: NCT00323518 |
| Methods | Randomised controlled trial (no placebo) |
| Participants | Aged 18 to 74 years with lymphoma, leukaemia or multiple myeloma; TBI plus high‐dose chemotherapy followed by autologous peripheral blood stem cell transplantation |
| Interventions | KGF (4 arms with different schedules) |
| Outcomes |
|
| Notes | Abstract only (we were unable to link this abstract to a full‐text report) Trials registry number: NCT00109031 |
| Methods | Multicentre, double‐blind, randomised placebo‐controlled trial |
| Participants | Haematologic malignancies; eligible for TBI plus high‐dose chemotherapy followed by autologous peripheral blood stem cell transplantation; aged 12 to 65 years |
| Interventions | KGF (7 doses) versus KGF (4 doses + 3 doses of placebo) versus placebo (7 doses) |
| Outcomes |
|
| Notes | Abstract only (we were unable to link this abstract to a full‐text report) Trials registry number: NCT00004132 |
5FU = fluorouracil; EGF = epidermal growth factor; EORTC QLQ‐H&N35 = European Organisation for Research and Treatment of Cancer, Quality of Life Questionnaire, Head and Neck Module; G‐CSF = granulocyte‐colony stimulating factor; GM‐CSF = granulocyte‐macrophage colony‐stimulating factor; HSCT = haematopoietic stem cell transplantation; IV = intravenous; KGF = keratinocyte growth factor; NCI‐CTC = National Cancer Institute common toxicity criteria; OMDQ = oral mucositis daily questionnaire; FGF‐20 = fibroblast growth factor‐20; TBI = total‐body irradiation; VAS = visual analogue scale; WHO = World Health Organization.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 KGF versus placebo, Outcome 1 Oral mucositis (any). | ||||
| 1.1 BMT/SCT after conditioning for haematological cancers | 4 | 655 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.88, 1.05] |
| 1.2 RT to head & neck with cisplatin | 2 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.90, 1.00] |
| 1.3 CT alone for mixed cancers | 2 | 215 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.60, 0.85] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 13 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 KGF versus placebo, Outcome 2 Oral mucositis (moderate + severe). | ||||
| 2.1 BMT/SCT after conditioning for haematological cancers | 6 | 852 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.80, 0.99] |
| 2.2 RT to head & neck with cisplatin/5FU | 3 | 471 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.83, 1.00] |
| 2.3 CT alone for mixed cancers | 4 | 344 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.45, 0.70] |
| 3 Oral mucositis (severe) Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.3  Comparison 1 KGF versus placebo, Outcome 3 Oral mucositis (severe). | ||||
| 3.1 BMT/SCT after conditioning for haematological cancers | 6 | 852 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.65, 1.11] |
| 3.2 RT to head & neck with cisplatin/5FU | 3 | 471 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.69, 0.90] |
| 3.3 CT alone for mixed cancers | 3 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.14, 0.65] |
| 4 Interruptions to cancer treatment (unscheduled RT breaks of 5 or more days) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.4  Comparison 1 KGF versus placebo, Outcome 4 Interruptions to cancer treatment (unscheduled RT breaks of 5 or more days). | ||||
| 4.1 RT to head & neck with cisplatin/5FU | 3 | 473 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.65, 1.59] |
| 5 Interruptions to cancer treatment (chemotherapy delays/discontinuations) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 KGF versus placebo, Outcome 5 Interruptions to cancer treatment (chemotherapy delays/discontinuations). | ||||
| 5.1 RT to head & neck with cisplatin | 2 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.62, 1.47] |
| 6 Oral pain Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.6  Comparison 1 KGF versus placebo, Outcome 6 Oral pain. | ||||
| 6.1 BMT/SCT after conditioning for haematological cancers | 1 | 42 | Mean Difference (IV, Random, 95% CI) | ‐0.85 [‐3.00, 1.30] |
| 6.2 RT to head & neck with cisplatin | 2 | 374 | Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.27, 0.02] |
| 7 Normalcy of diet (use of supplemental nutrition) Show forest plot | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.7  Comparison 1 KGF versus placebo, Outcome 7 Normalcy of diet (use of supplemental nutrition). | ||||
| 7.1 BMT/SCT after conditioning for haematological cancers | 4 | 714 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.58, 1.34] |
| 7.2 RT to head & neck with cisplatin/5FU | 3 | 473 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.77, 1.37] |
| 8 Normalcy of diet (worst ability to eat score ‐ 1 to 4 scale) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.8  Comparison 1 KGF versus placebo, Outcome 8 Normalcy of diet (worst ability to eat score ‐ 1 to 4 scale). | ||||
| 8.1 BMT/SCT after conditioning for haematological cancers | 1 | 42 | Mean Difference (IV, Random, 95% CI) | ‐0.5 [‐1.21, 0.21] |
| 9 Number of days in hospital Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.9  Comparison 1 KGF versus placebo, Outcome 9 Number of days in hospital. | ||||
| 9.1 BMT/SCT after conditioning for haematological cancers | 1 | 281 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐1.64, 1.64] |
| 10 Number of days of treatment with opioid analgesics Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.10  Comparison 1 KGF versus placebo, Outcome 10 Number of days of treatment with opioid analgesics. | ||||
| 10.1 BMT/SCT after conditioning for haematological cancers | 2 | 323 | Mean Difference (IV, Random, 95% CI) | ‐1.41 [‐3.33, 0.51] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 KGF (dose comparison), Outcome 1 Oral mucositis (any). | ||||
| 1.1 BMT/SCT after conditioning for haematological cancers | 1 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.75, 1.03] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 2.2  Comparison 2 KGF (dose comparison), Outcome 2 Oral mucositis (moderate + severe). | ||||
| 2.1 BMT/SCT after conditioning for haematological cancers | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 CT alone for metastatic colorectal cancer | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Oral mucositis (severe) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| Analysis 2.3  Comparison 2 KGF (dose comparison), Outcome 3 Oral mucositis (severe). | ||||
| 3.1 BMT/SCT after conditioning for haematological cancers | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Oral pain (maximum score on 0 to 10 VAS) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.4  Comparison 2 KGF (dose comparison), Outcome 4 Oral pain (maximum score on 0 to 10 VAS). | ||||
| 4.1 BMT/SCT after conditioning for haematological cancers | 1 | 28 | Mean Difference (IV, Random, 95% CI) | 0.70 [‐1.90, 3.30] |
| 5 Normalcy of diet (use of TPN) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 2.5  Comparison 2 KGF (dose comparison), Outcome 5 Normalcy of diet (use of TPN). | ||||
| 5.1 BMT/SCT after conditioning for haematological cancers | 1 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.63, 1.02] |
| 6 Normalcy of diet (worst ability to eat score ‐ 1 to 4 scale) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.6  Comparison 2 KGF (dose comparison), Outcome 6 Normalcy of diet (worst ability to eat score ‐ 1 to 4 scale). | ||||
| 6.1 BMT/SCT after conditioning for haematological cancers | 1 | 28 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.41, 1.21] |
| 7 Number of days in hospital Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.7  Comparison 2 KGF (dose comparison), Outcome 7 Number of days in hospital. | ||||
| 7.1 BMT/SCT after conditioning for haematological cancers | 1 | 224 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐1.78, 1.78] |
| 8 Number of days of treatment with opioid analgesics Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 2.8  Comparison 2 KGF (dose comparison), Outcome 8 Number of days of treatment with opioid analgesics. | ||||
| 8.1 BMT/SCT after conditioning for haematological cancers | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 3.1  Comparison 3 KGF versus chlorhexidine, Outcome 1 Oral mucositis (any). | ||||
| 1.1 CT alone for haematological cancer | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.54, 0.85] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 3.2  Comparison 3 KGF versus chlorhexidine, Outcome 2 Oral mucositis (moderate + severe). | ||||
| 2.1 CT alone for haematological cancer | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.05, 0.28] |
| 3 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 3.3  Comparison 3 KGF versus chlorhexidine, Outcome 3 Oral mucositis (severe). | ||||
| 3.1 CT alone for haematological cancer | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.01 [0.00, 0.19] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 4.1  Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 1 Oral mucositis (any). | ||||
| 1.1 BMT/SCT after conditioning for mixed cancers | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.80, 1.04] |
| 1.2 RT to head & neck | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.82, 1.23] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 4.2  Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 2 Oral mucositis (moderate + severe). | ||||
| 2.1 BMT/SCT after conditioning for haematological cancers | 1 | 109 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.79, 1.13] |
| 2.2 RT to head & neck | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.49, 1.06] |
| 3 Oral mucositis (severe) Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 4.3  Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 3 Oral mucositis (severe). | ||||
| 3.1 BMT/SCT after conditioning for mixed cancers | 3 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.33, 1.67] |
| 3.2 RT to head & neck | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.01, 7.09] |
| 3.3 CT alone for mixed cancers | 2 | 65 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.05, 7.11] |
| 4 Oral pain (maximum score on 0 to 10 VAS) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 4.4  Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 4 Oral pain (maximum score on 0 to 10 VAS). | ||||
| 4.1 BMT/SCT after conditioning for mixed cancers | 1 | 90 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.85, 2.05] |
| 5 Normalcy of diet (use of feeding tube/parenteral nutrition) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 4.5  Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 5 Normalcy of diet (use of feeding tube/parenteral nutrition). | ||||
| 5.1 BMT/SCT after conditioning for haematological cancers | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 1.1 [0.63, 1.91] |
| 5.2 RT to head & neck | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.01, 7.09] |
| 6 Number of days of treatment with opioid analgesics Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 4.6  Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 6 Number of days of treatment with opioid analgesics. | ||||
| 6.1 BMT/SCT after conditioning for mixed cancers | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐1.10 [‐1.91, ‐0.29] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 5.1  Comparison 5 GM‐CSF (dose comparison), Outcome 1 Oral mucositis (severe). | ||||
| 1.1 CT alone for breast cancer | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 2.75 [1.07, 7.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 6.1  Comparison 6 GM‐CSF versus sucralfate, Outcome 1 Oral mucositis (moderate + severe). | ||||
| 1.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.80, 1.14] |
| 2 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 6.2  Comparison 6 GM‐CSF versus sucralfate, Outcome 2 Oral mucositis (severe). | ||||
| 2.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.24, 1.21] |
| 3 Interruptions to cancer treatment Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 6.3  Comparison 6 GM‐CSF versus sucralfate, Outcome 3 Interruptions to cancer treatment. | ||||
| 3.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.13 [0.01, 2.36] |
| 4 Normalcy of diet (use of PEG tube) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 6.4  Comparison 6 GM‐CSF versus sucralfate, Outcome 4 Normalcy of diet (use of PEG tube). | ||||
| 4.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.01, 3.56] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 7.1  Comparison 7 G‐CSF versus placebo/no treatment, Outcome 1 Oral mucositis (any). | ||||
| 1.1 RT to head & neck | 2 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.86, 1.22] |
| 1.2 CT alone for lung cancer | 1 | 195 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.40, 0.87] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 7.2  Comparison 7 G‐CSF versus placebo/no treatment, Outcome 2 Oral mucositis (moderate + severe). | ||||
| 2.1 CT alone for breast cancer | 1 | 14 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.12, 0.95] |
| 3 Oral mucositis (severe) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 7.3  Comparison 7 G‐CSF versus placebo/no treatment, Outcome 3 Oral mucositis (severe). | ||||
| 3.1 RT to head & neck | 2 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.15, 0.87] |
| 4 Interruptions to cancer treatment (RT interruption) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 7.4  Comparison 7 G‐CSF versus placebo/no treatment, Outcome 4 Interruptions to cancer treatment (RT interruption). | ||||
| 4.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.01, 4.31] |
| 5 Normalcy of diet (use of PEG tube) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 7.5  Comparison 7 G‐CSF versus placebo/no treatment, Outcome 5 Normalcy of diet (use of PEG tube). | ||||
| 5.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.16 [0.01, 2.86] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 8.1  Comparison 8 G‐CSF (pegfilgrastim) versus G‐CSF (filgrastim), Outcome 1 Oral mucositis (any). | ||||
| 1.1 BMT/SCT after conditioning for mixed cancers | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.82, 1.27] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 8.2  Comparison 8 G‐CSF (pegfilgrastim) versus G‐CSF (filgrastim), Outcome 2 Oral mucositis (moderate + severe). | ||||
| 2.1 BMT/SCT after conditioning for mixed cancers | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.55, 1.11] |
| 3 Normalcy of diet (use of supplemental nutrition) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 8.3  Comparison 8 G‐CSF (pegfilgrastim) versus G‐CSF (filgrastim), Outcome 3 Normalcy of diet (use of supplemental nutrition). | ||||
| 3.1 BMT/SCT after conditioning for mixed cancers | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.94, 1.06] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (moderate + severe) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 9.1  Comparison 9 EGF versus placebo, Outcome 1 Oral mucositis (moderate + severe). | ||||
| 1.1 BMT/SCT after conditioning for haematological cancers | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.78, 1.43] |
| 1.2 RT to head & neck +/‐ cisplatin | 1 | 103 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.45, 0.99] |
| 2 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 9.2  Comparison 9 EGF versus placebo, Outcome 2 Oral mucositis (severe). | ||||
| 2.1 BMT/SCT after conditioning for haematological cancers | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.59, 1.80] |
| 3 Interruptions to cancer treatment (RT breaks > 2 consecutive days) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 9.3  Comparison 9 EGF versus placebo, Outcome 3 Interruptions to cancer treatment (RT breaks > 2 consecutive days). | ||||
| 3.1 RT to head & neck +/‐ cisplatin | 1 | 113 | Risk Ratio (M‐H, Random, 95% CI) | 4.38 [0.25, 75.44] |
| 4 Normalcy of diet (use of supplemental nutrition) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 9.4  Comparison 9 EGF versus placebo, Outcome 4 Normalcy of diet (use of supplemental nutrition). | ||||
| 4.1 BMT/SCT after conditioning for haematological cancers | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.55, 1.94] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 10.1  Comparison 10 ITF versus placebo, Outcome 1 Oral mucositis (any). | ||||
| 1.1 CT alone for colorectal cancer | 1 | 99 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.35, 0.79] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 10.2  Comparison 10 ITF versus placebo, Outcome 2 Oral mucositis (moderate + severe). | ||||
| 2.1 CT alone for colorectal cancer | 1 | 99 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.10, 0.48] |
| 3 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 10.3  Comparison 10 ITF versus placebo, Outcome 3 Oral mucositis (severe). | ||||
| 3.1 CT alone for colorectal cancer | 1 | 99 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.06, 36.39] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 11.1  Comparison 11 ITF (dose comparison), Outcome 1 Oral mucositis (any). | ||||
| 1.1 CT alone for colorectal cancer | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 1.3 [0.67, 2.54] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 11.2  Comparison 11 ITF (dose comparison), Outcome 2 Oral mucositis (moderate + severe). | ||||
| 2.1 CT alone for colorectal cancer | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.18, 3.09] |
| 3 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 11.3  Comparison 11 ITF (dose comparison), Outcome 3 Oral mucositis (severe). | ||||
| 3.1 CT alone for colorectal cancer | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.90] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 12.1  Comparison 12 Erythropoietin versus placebo, Outcome 1 Oral mucositis (any). | ||||
| 1.1 BMT/SCT after conditioning for haematological cancers | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.21, 0.60] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 12.2  Comparison 12 Erythropoietin versus placebo, Outcome 2 Oral mucositis (moderate + severe). | ||||
| 2.1 BMT/SCT after conditioning for haematological cancers | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.24, 0.79] |
| 3 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 12.3  Comparison 12 Erythropoietin versus placebo, Outcome 3 Oral mucositis (severe). | ||||
| 3.1 BMT/SCT after conditioning for haematological cancers | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.4 [0.14, 1.17] |
| 4 Number of days in hospital Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 12.4  Comparison 12 Erythropoietin versus placebo, Outcome 4 Number of days in hospital. | ||||
| 4.1 BMT/SCT after conditioning for haematological cancers | 1 | 80 | Mean Difference (IV, Random, 95% CI) | ‐2.95 [‐7.73, 1.83] |

Study flow diagram.
RCT = randomised controlled trial.
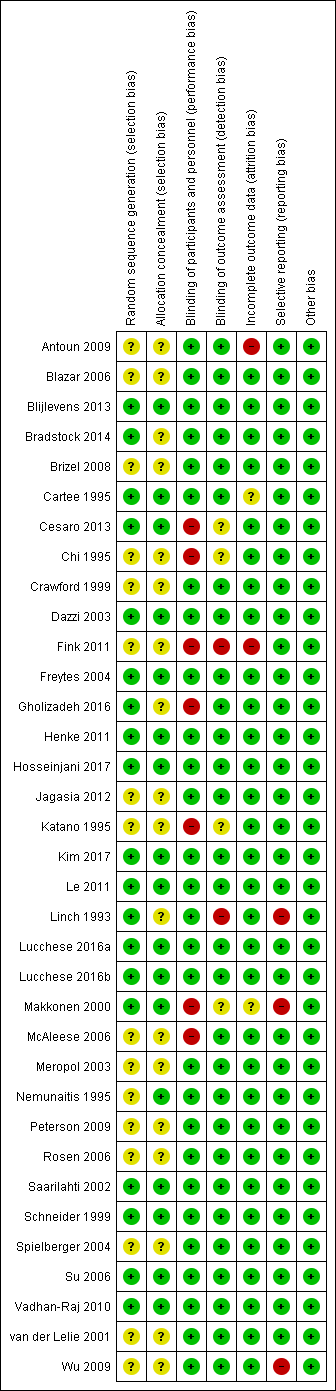
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Comparison 1 KGF versus placebo, Outcome 1 Oral mucositis (any).

Comparison 1 KGF versus placebo, Outcome 2 Oral mucositis (moderate + severe).
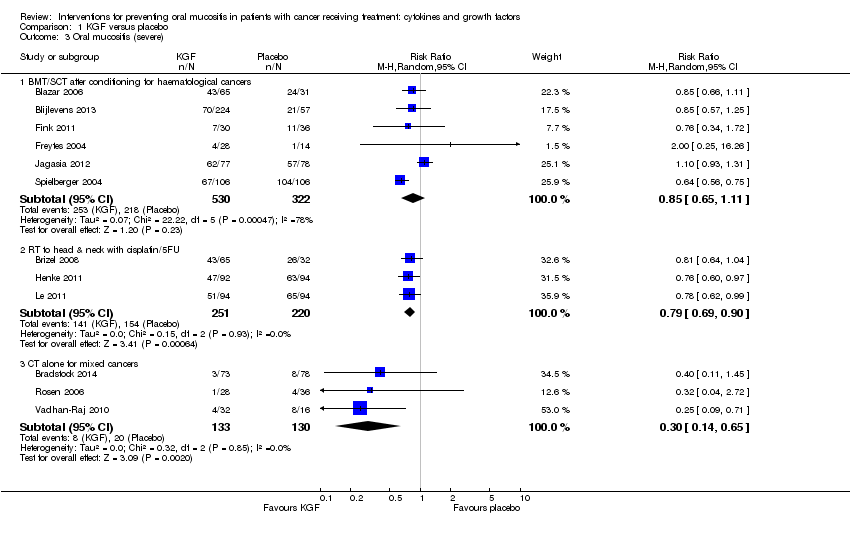
Comparison 1 KGF versus placebo, Outcome 3 Oral mucositis (severe).

Comparison 1 KGF versus placebo, Outcome 4 Interruptions to cancer treatment (unscheduled RT breaks of 5 or more days).

Comparison 1 KGF versus placebo, Outcome 5 Interruptions to cancer treatment (chemotherapy delays/discontinuations).
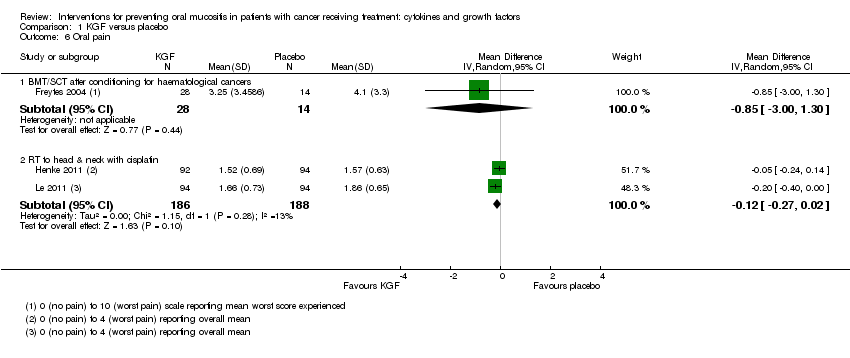
Comparison 1 KGF versus placebo, Outcome 6 Oral pain.
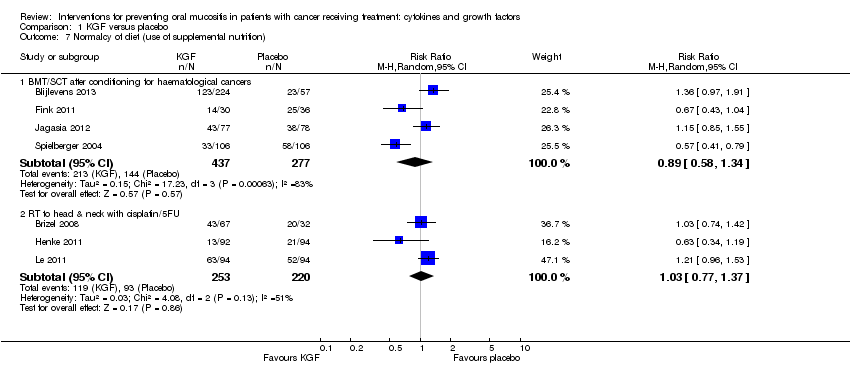
Comparison 1 KGF versus placebo, Outcome 7 Normalcy of diet (use of supplemental nutrition).
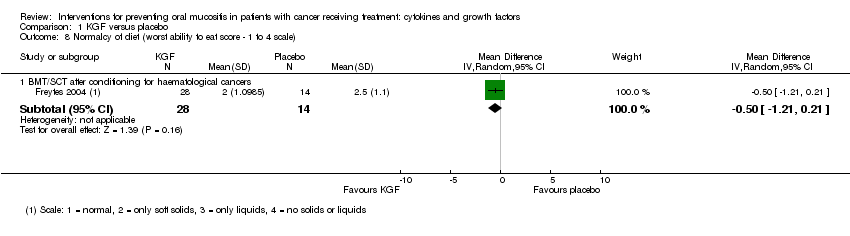
Comparison 1 KGF versus placebo, Outcome 8 Normalcy of diet (worst ability to eat score ‐ 1 to 4 scale).
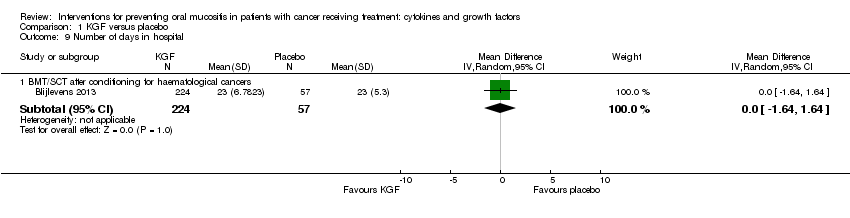
Comparison 1 KGF versus placebo, Outcome 9 Number of days in hospital.
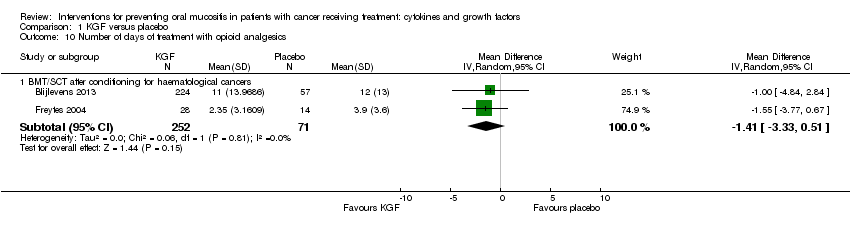
Comparison 1 KGF versus placebo, Outcome 10 Number of days of treatment with opioid analgesics.

Comparison 2 KGF (dose comparison), Outcome 1 Oral mucositis (any).
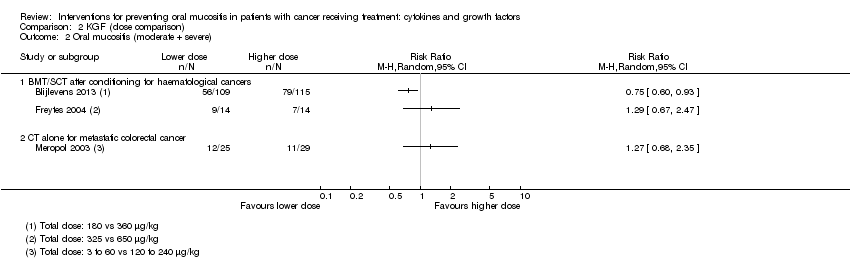
Comparison 2 KGF (dose comparison), Outcome 2 Oral mucositis (moderate + severe).

Comparison 2 KGF (dose comparison), Outcome 3 Oral mucositis (severe).
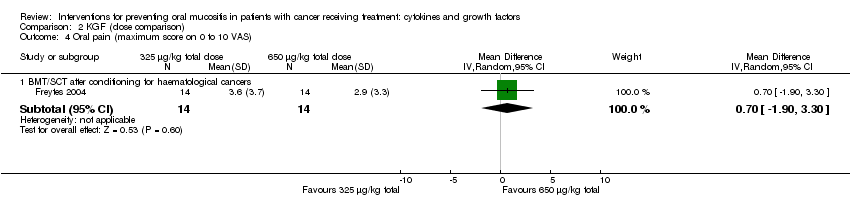
Comparison 2 KGF (dose comparison), Outcome 4 Oral pain (maximum score on 0 to 10 VAS).

Comparison 2 KGF (dose comparison), Outcome 5 Normalcy of diet (use of TPN).
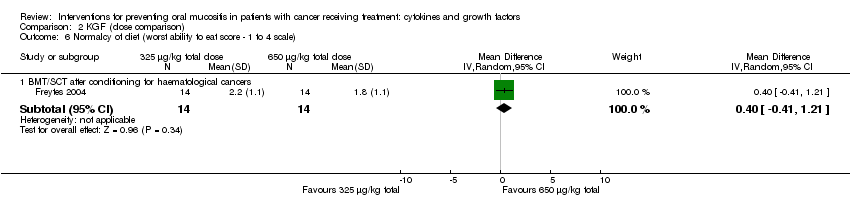
Comparison 2 KGF (dose comparison), Outcome 6 Normalcy of diet (worst ability to eat score ‐ 1 to 4 scale).
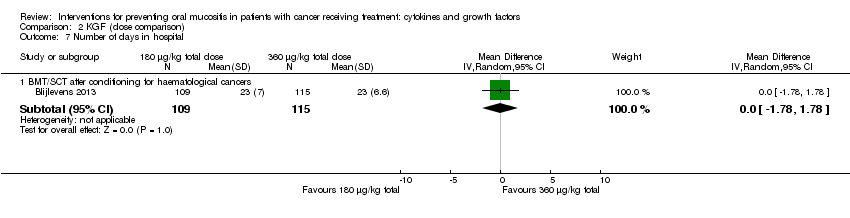
Comparison 2 KGF (dose comparison), Outcome 7 Number of days in hospital.
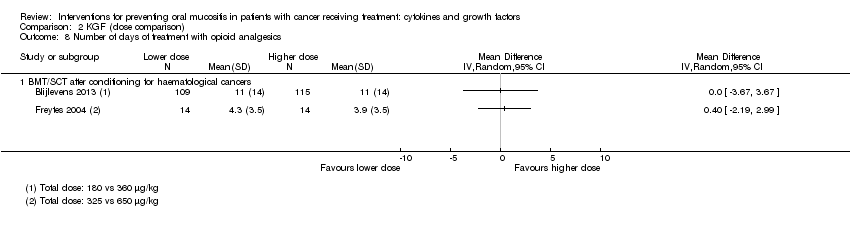
Comparison 2 KGF (dose comparison), Outcome 8 Number of days of treatment with opioid analgesics.
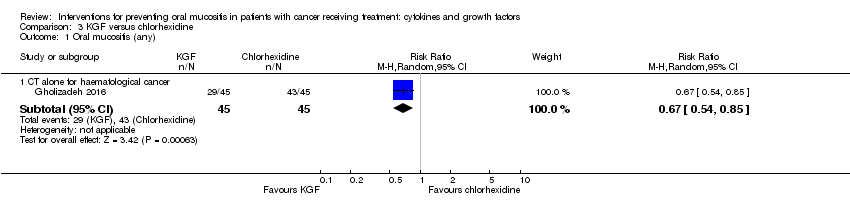
Comparison 3 KGF versus chlorhexidine, Outcome 1 Oral mucositis (any).
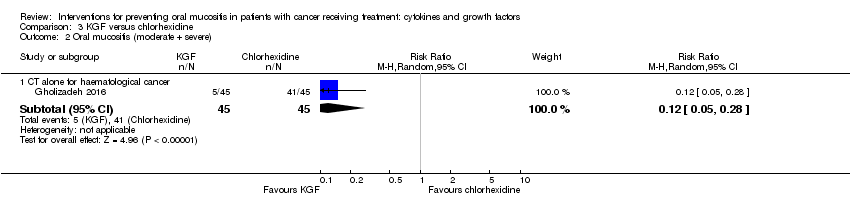
Comparison 3 KGF versus chlorhexidine, Outcome 2 Oral mucositis (moderate + severe).
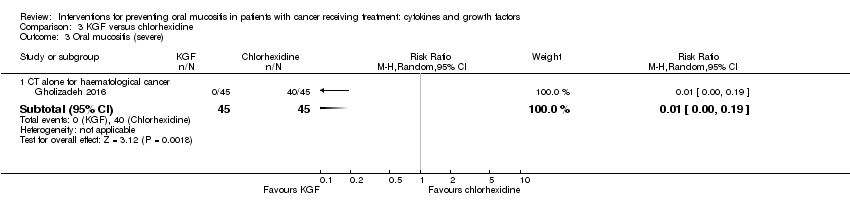
Comparison 3 KGF versus chlorhexidine, Outcome 3 Oral mucositis (severe).

Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 1 Oral mucositis (any).

Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 2 Oral mucositis (moderate + severe).

Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 3 Oral mucositis (severe).
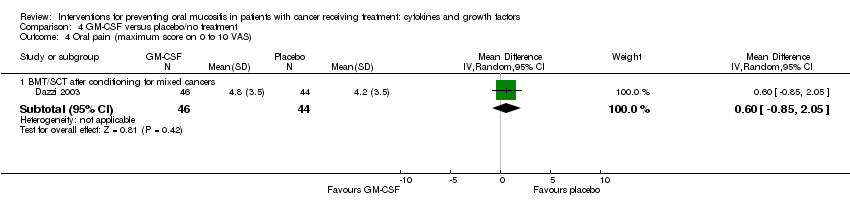
Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 4 Oral pain (maximum score on 0 to 10 VAS).

Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 5 Normalcy of diet (use of feeding tube/parenteral nutrition).

Comparison 4 GM‐CSF versus placebo/no treatment, Outcome 6 Number of days of treatment with opioid analgesics.
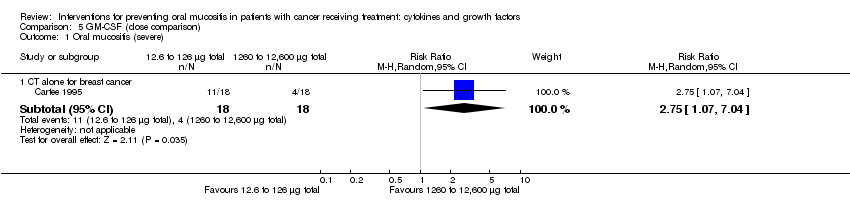
Comparison 5 GM‐CSF (dose comparison), Outcome 1 Oral mucositis (severe).

Comparison 6 GM‐CSF versus sucralfate, Outcome 1 Oral mucositis (moderate + severe).
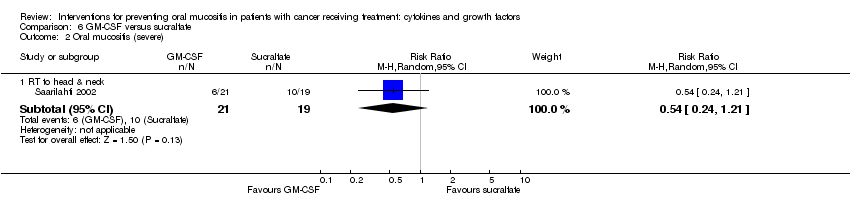
Comparison 6 GM‐CSF versus sucralfate, Outcome 2 Oral mucositis (severe).
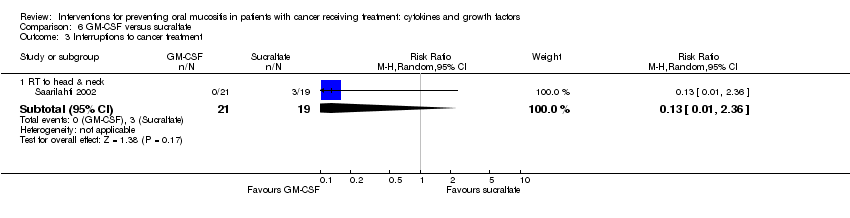
Comparison 6 GM‐CSF versus sucralfate, Outcome 3 Interruptions to cancer treatment.
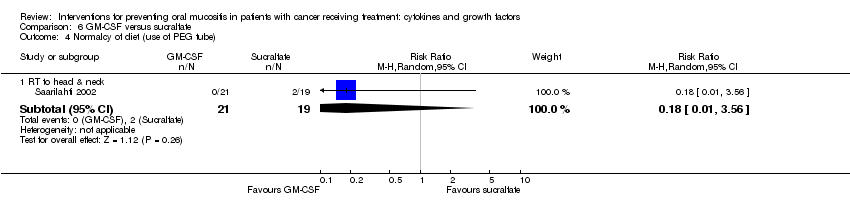
Comparison 6 GM‐CSF versus sucralfate, Outcome 4 Normalcy of diet (use of PEG tube).

Comparison 7 G‐CSF versus placebo/no treatment, Outcome 1 Oral mucositis (any).

Comparison 7 G‐CSF versus placebo/no treatment, Outcome 2 Oral mucositis (moderate + severe).

Comparison 7 G‐CSF versus placebo/no treatment, Outcome 3 Oral mucositis (severe).
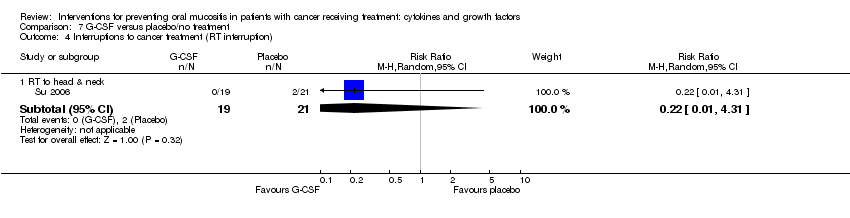
Comparison 7 G‐CSF versus placebo/no treatment, Outcome 4 Interruptions to cancer treatment (RT interruption).
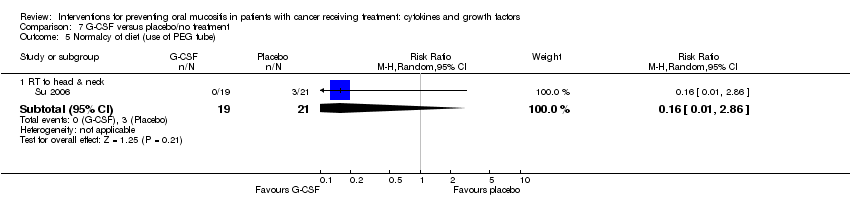
Comparison 7 G‐CSF versus placebo/no treatment, Outcome 5 Normalcy of diet (use of PEG tube).
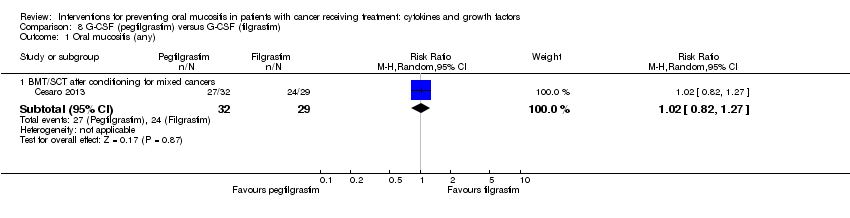
Comparison 8 G‐CSF (pegfilgrastim) versus G‐CSF (filgrastim), Outcome 1 Oral mucositis (any).
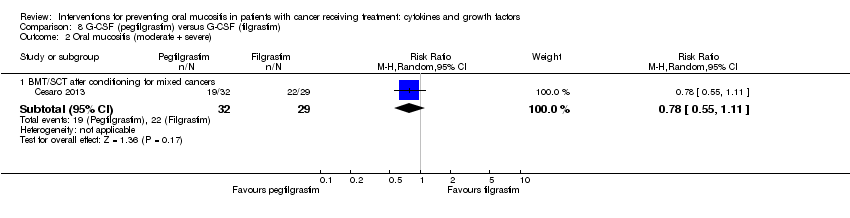
Comparison 8 G‐CSF (pegfilgrastim) versus G‐CSF (filgrastim), Outcome 2 Oral mucositis (moderate + severe).

Comparison 8 G‐CSF (pegfilgrastim) versus G‐CSF (filgrastim), Outcome 3 Normalcy of diet (use of supplemental nutrition).
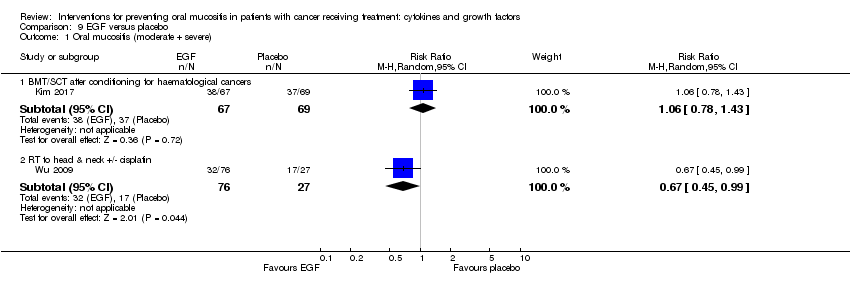
Comparison 9 EGF versus placebo, Outcome 1 Oral mucositis (moderate + severe).

Comparison 9 EGF versus placebo, Outcome 2 Oral mucositis (severe).
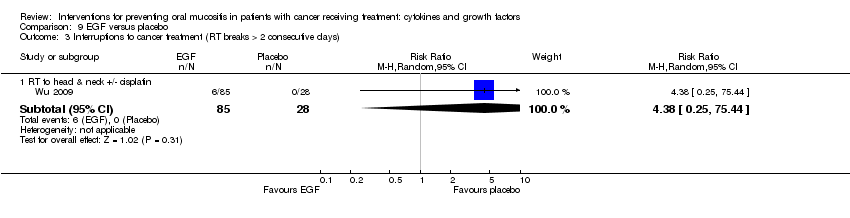
Comparison 9 EGF versus placebo, Outcome 3 Interruptions to cancer treatment (RT breaks > 2 consecutive days).
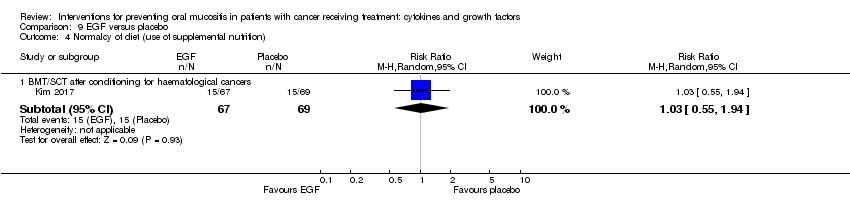
Comparison 9 EGF versus placebo, Outcome 4 Normalcy of diet (use of supplemental nutrition).

Comparison 10 ITF versus placebo, Outcome 1 Oral mucositis (any).

Comparison 10 ITF versus placebo, Outcome 2 Oral mucositis (moderate + severe).
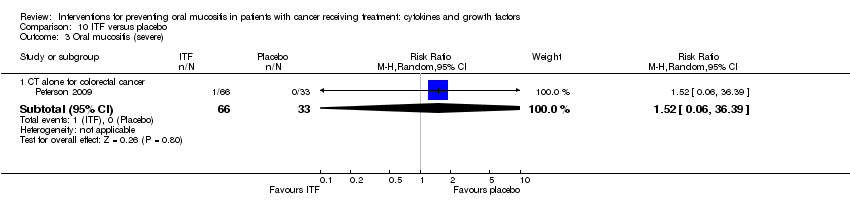
Comparison 10 ITF versus placebo, Outcome 3 Oral mucositis (severe).
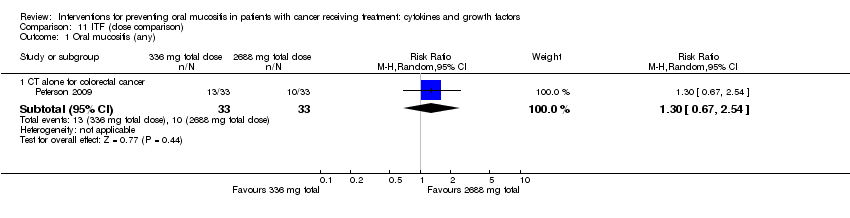
Comparison 11 ITF (dose comparison), Outcome 1 Oral mucositis (any).

Comparison 11 ITF (dose comparison), Outcome 2 Oral mucositis (moderate + severe).

Comparison 11 ITF (dose comparison), Outcome 3 Oral mucositis (severe).
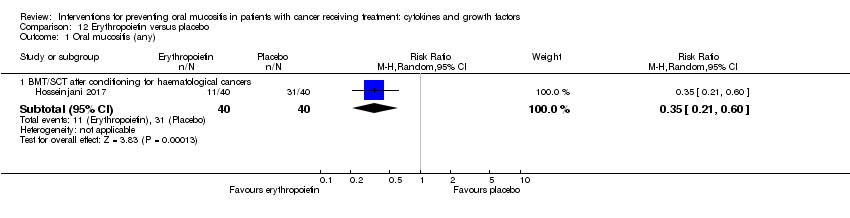
Comparison 12 Erythropoietin versus placebo, Outcome 1 Oral mucositis (any).
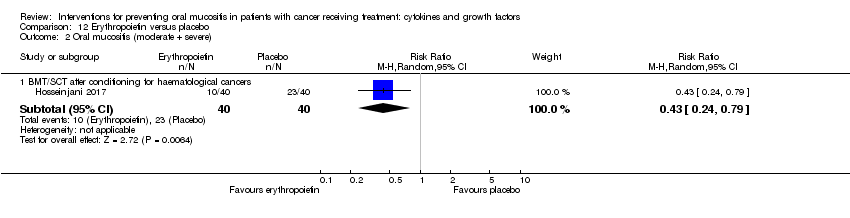
Comparison 12 Erythropoietin versus placebo, Outcome 2 Oral mucositis (moderate + severe).

Comparison 12 Erythropoietin versus placebo, Outcome 3 Oral mucositis (severe).
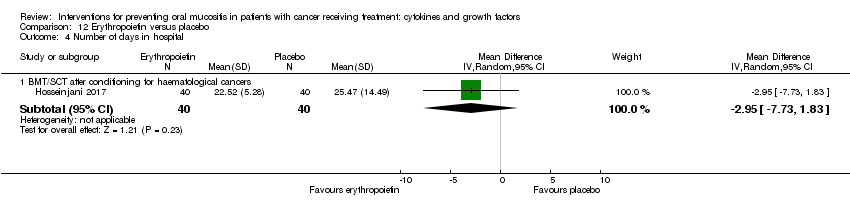
Comparison 12 Erythropoietin versus placebo, Outcome 4 Number of days in hospital.
| KGF compared to placebo for preventing oral mucositis in adults with cancer receiving treatment | ||||||
| Patient or population: adults** receiving treatment for cancer (see subgroup for treatment type) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with placebo | Risk with KGF | |||||
| Oral mucositis (moderate + severe) | BMT/SCT after conditioning for haematological cancers | RR 0.89 | 852 | ⊕⊕⊝⊝ | There might be a benefit for KGF in this population NNTB = 11 (95% CI 6 to 112) | |
| 848 per 1000 | 755 per 1000 | |||||
| RT to head and neck with cisplatin/5FU | RR 0.91 | 471 | ⊕⊕⊕⊝ | There is probably a benefit for KGF in this population NNTB = 12 (95% CI 7 to ∞) | ||
| 932 per 1000 | 848 per 1000 | |||||
| CT alone for mixed cancers | RR 0.56 | 344 | ⊕⊕⊕⊝ | It is likely that there is a benefit for KGF in this population NNTB = 4 (95% CI 3 to 6) | ||
| 631 per 1000 | 353 per 1000 | |||||
| Oral mucositis (severe) | BMT/SCT after conditioning for haematological cancers | RR 0.85 | 852 | ⊕⊕⊝⊝ | There might be a benefit for KGF in this population, but there is also some possibility of an increase in risk NNTB = 10 (95% CI 5 NNTB to 14 NNTH) | |
| 677 per 1000 | 575 per 1000 | |||||
| RT to head and neck with cisplatin/5FU | RR 0.79 | 471 | ⊕⊕⊕⊕ | It is very likely that there is a benefit for KGF in this population NNTB = 7 (95% CI 5 to 15) | ||
| 700 per 1000 | 553 per 1000 | |||||
| CT alone for mixed cancers | RR 0.30 | 263 | ⊕⊕⊝⊝ | There might be a benefit for KGF in this population NNTB = 10 (95% CI 8 to 19) | ||
| 154 per 1000 | 46 per 1000 | |||||
| Adverse events | Adverse events that were attributed to the study drugs rather than the cancer therapy were typically oral‐related or skin‐related. Events were mostly mild to moderate with very few incidences of serious events. However, reporting was poor and inconsistent, meaning that it was not appropriate to meta‐analyse data | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ***The number of people that would need to receive KGF in order to prevent 1 additional person from developing the outcome. Calculated as 1 divided by the absolute risk reduction (which is the control arm event rate minus the experimental arm event rate). NNTH means the number of people that would need to receive KGF to cause 1 additional person to develop the outcome. All decimal places have been rounded up to the nearest whole number (i.e. 6.1 = 7). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded by 1 level for inconsistency (substantial heterogeneity: I2 = 50% to 90%, P < 0.1); downgraded 1 further level for publication bias as there are 2 references in Studies awaiting classification that would be included in the conditioning/transplant subgroup, but the data are not available (NCT02313792; Spielberger 2001). | ||||||
| GM‐CSF compared to placebo/no treatment for preventing oral mucositis in adults with cancer receiving treatment | ||||||
| Patient or population: adults** receiving treatment for cancer (see subgroup for treatment type) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with placebo/no treatment | Risk with GM‐CSF | |||||
| Oral mucositis (moderate + severe) | BMT/SCT after conditioning for haematological cancers | RR 0.94 | 109 | ⊕⊝⊝⊝ | There is insufficient evidence to determine a benefit for GM‐CSF in this population NNTB = 20 (95% CI 6 NNTB to 10 NNTH) | |
| 839 per 1000 | 789 per 1000 | |||||
| RT to head and neck | RR 0.72 | 29 | ⊕⊝⊝⊝ | There is insufficient evidence to determine a benefit for GM‐CSF in this population NNTB = 4 (95% CI 3 NNTB to 14 NNTH) | ||
| 929 per 1000 | 669 per 1000 | |||||
| Oral mucositis (severe) | BMT/SCT after conditioning for mixed cancers | RR 0.74 | 235 | ⊕⊕⊝⊝ | There is insufficient evidence to determine a benefit for GM‐CSF in this population NNTB = 12 (95% CI 5 NNTB to 5 NNTH) | |
| 347 per 1000 | 257 per 1000 | |||||
| RT to head and neck | RR 0.31 | 29 | ⊕⊝⊝⊝ | There is insufficient evidence to determine a benefit for GM‐CSF in this population NNTB = 21 (95% CI 15 NNTB to 3 NNTH) | ||
| 71 per 1000 | 22 per 1000 | |||||
| CT alone for mixed cancers | RR 0.59 | 65 | ⊕⊝⊝⊝ | There is insufficient evidence to determine a benefit for GM‐CSF in this population NNTB = 5 (95% CI 3 NNTB to 2 NNTH) | ||
| 500 per 1000 | 295 per 1000 | |||||
| Adverse events | Adverse events that were attributed to the study drugs rather than the cancer therapy were typically bone pain, nausea, fever and headache. Events were not reported as being serious. Some studies did not report adverse events and 1 even reported that there were none. However, reporting was poor and inconsistent, meaning that it was not appropriate to meta‐analyse data | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ***The number of people that would need to receive GM‐CSF in order to prevent 1 additional person from developing the outcome. Calculated as 1 divided by the absolute risk reduction (which is the control arm event rate minus the experimental arm event rate). NNTH means the number of people that would need to receive GM‐CSF to cause 1 additional person to develop the outcome. All decimal places have been rounded up to the nearest whole number (i.e. 6.1 = 7). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded by 2 levels for imprecision (single study with a small sample size and the confidence interval includes a possible increase in risk that is of a similar magnitude to the possible reduction in risk); downgraded 1 further level for indirectness (single study so not widely generalisable). | ||||||
| G‐CSF compared to placebo/no treatment for preventing oral mucositis in patients with cancer receiving treatment | ||||||
| Patient or population: adults** receiving treatment for cancer (see subgroup for treatment type) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect | Number of participants | Quality of the evidence | Comments | |
| Risk with placebo/no treatment | Risk with G‐CSF | |||||
| Oral mucositis (moderate + severe) | CT alone for breast cancer | RR 0.33 | 14 | ⊕⊝⊝⊝ | There is very weak evidence that there might be a benefit for G‐CSF in this population NNTB = 2 (95% CI 2 to 20) | |
| 1000 per 1000 | 330 per 1000 | |||||
| Oral mucositis (severe) | RT to head and neck | RR 0.37 | 54 | ⊕⊕⊝⊝ | There is weak evidence that there might be a benefit for G‐CSF in this population NNTB = 3 (95% CI 3 to 15) | |
| 519 per 1000 | 192 per 1000 | |||||
| Adverse events | There was limited evidence of adverse events for G‐CSF. 2 of the 6 studies did not report adverse events. There were low rates of mild to moderate events, the most common of which appeared to be bone pain. However, reporting was poor and inconsistent, meaning that it was not appropriate to meta‐analyse data | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ***The number of people that would need to receive G‐CSF in order to prevent 1 additional person from developing the outcome. Calculated as 1 divided by the absolute risk reduction (which is the control arm event rate minus the experimental arm event rate). NNTH means the number of people that would need to receive G‐CSF to cause 1 additional person to develop the outcome. All decimal places have been rounded up to the nearest whole number (i.e. 6.1 = 7). | ||||||
| GRADE Working Group grades of evidence | ||||||
| 1Downgraded by 2 levels for imprecision (wide confidence interval and very small sample size); downgraded by 1 further level for high risk of performance bias; downgraded by 1 further level for indirectness (single study so not widely generalisable). | ||||||
| Study ID | Adverse events results |
|
| |
|
| |
| Insufficient evidence of a difference in infection or Grade 3 to 4 (NCI‐CTC 0 to 4 toxicity scale) skin rash/desquamation | |
| The study authors state that most adverse events were considered to be caused by the cancer treatment or the underlying cancer itself and not related to study treatment. 2 participants in the palifermin group had serious adverse events considered to be related to the intervention: 1 had increased sputum production; the other had dehydration, dysphagia, pain (including abdominal), pancreatitis, and subsequently had schistosomiasis | |
| Total of 28 side effects in palifermin group occurring in 11 of 22 patients (50%) who received at least 4 of the 6 doses. Most frequent (90.9%) were cases of erythema or exanthema, often associated with itching (54.5%). Often (54.5%) a swelling of the oral mucosa including the tongue occurred. In 4 out of 6 patients, this was accompanied by taste disturbance. The severity of side effects were classified as mild to moderate. The CTC Grade 3 occurred only once in the form of a strong heat sensation In 1 of the 11 cases, there was premature discontinuation of palifermin due to severe facial swelling with eyelid and laryngeal pain as well as painful swelling of the hands following the second injection | |
| 25 different adverse events were reported and were mostly not KGF‐related. There was insufficient evidence of a difference for diarrhoea, abdominal pain, infection or rash | |
| "..two patients reported knee joint pain, skin rash was observed in one patient, two patients had abnormal taste, and one showed lingual mucosal thickening" (control group was chlorhexidine mouthrinse. The authors do not report the events by treatment group) | |
|
| |
| KGF‐related AEs with incidence ≥ 5% in KGF group: higher rate of gastrointestinal disorders in KGF group (18/78 versus 2/73; RR 8.42, 95% CI 2.02 to 35.04; P = 0.003). Insufficient evidence of a difference in any AE, tongue coating, tongue disorder, skin and subcutaneous tissue disorders, rash, pruritus, or erythema | |
| "Study drug–related AEs were reported for 35% of palifermin and 11% of placebo patients. The most frequent study drug–related AEs (palifermin, placebo) were rash (9%, 2%), flushing (5%, 0%), dysgeusia (5%, 1%), nausea (4%, 1%),and vomiting (3%, 1%). None of these events led to study withdrawal. Serious AEs considered related to study treatment were reported for five palifermin patients (5%; one each with necrotic pancreatitis, hypersensitivity, tracheostomy malfunction, peritoneal carcinoma, and convulsion) and two placebo patients (2%; one each with hepatitis/hepatic enzyme increase and cryptogenic organizing pneumonia)" | |
| "The administration of palifermin was generally safe and without considerable complications. The only adverse reactions were rashes (lasting for 48–72 hours) localized to the face, upper neck and shoulders, erythema, and altered taste (consistent with the pharmacologic action of palifermin of oral epithelium and skin), most of which were of NCI grade 1 or 2 severity" | |
| "The administration of palifermin was mostly safe and without substantial complications. The mean duration of the OM and the number of adverse event was significant less in the palifermin group (Tables II, III, Figure 1). The main adverse episodes were erythema, cutaneous rashes and altered taste and three of the patients in the palifermin group showed a light thickness of the tongue, mouth and palate" | |
| "Although the predefined frequency of DLTs attributable to KGF was not reached with KGF doses between 1 and 80 µg/kg/d, there were three adverse reactions involving the skin that required discontinuation of KGF in the 18 patients treated with 60 or 80 µg/kg (Table 5). Overall, skin and oral adverse events (rash, flushing, pruritis, edema, hypoesthesia, paresthesia, tongue disorder [thickening], and alteration in taste sensation) attributed to KGF occurred in 13 of 18 patients treated with 60 and 80 µg/kg of KGF (eight patients, grade 1; four patients, grade 2; and one patient, grade 3) and in three of 11 patients treated with 40 µg/kg (all grade 1). These events were reported in 16 of 39 patients (41%) dosed with KGF at > 20 µg/kg/d, whereas these symptoms were reported in only two of 21 subjects (10%) treated with placebo. The skin and oral toxicities associated with KGF were generally mild to moderate in severity, with onset approximately 36 hours after the first dose of KGF and resolution 7 to 10 days thereafter" | |
|
| |
| "The incidence, frequency, and severity of adverse events were similar in the two groups, and most were attributable to the underlying cancer, cytotoxic chemotherapy, or total‐body irradiation. Those that occurred with an incidence that was at least 5 percentage points higher in the palifermin group than in the placebo group are listed in Table 3. Most of these adverse events were consistent with the pharmacologic action of palifermin on skin and oral epithelium (e.g., rash, pruritus, erythema, paresthesia, mouth and tongue disorders, and taste alteration). All these events were mild to moderate in severity, transient (occurring approximately three days after the third dose of palifermin and lasting approximately three days), and not a cause for the discontinuation of study drug. Serious adverse events considered to be related to treatment occurred in one palifermin recipient (rash) and one placebo recipient (hypotension)" | |
|
| |
| AE = adverse event; CI = confidence interval; KGF = keratinocyte growth factor; NCI‐CTC = National Cancer Institute common toxicity criteria; RR = risk ratio; WHO = World Health Organization. | |
| Study ID | Adverse events results |
| 2 participants (group allocation not reported) withdrew by day 3 due to intolerance to their mouthwash (dry mouth); 1 participant receiving GM‐CSF (1 µg/mL) had mouthwash withdrawn by day 3 due to possible allergic reaction (sensation of fullness in the posterior pharyngeal area) but resolved within 4 hours (the participant was withdrawn but appears to have been included in the analysis) | |
| "One patient had fever and chills, and two patients had general malaise and headache during GM‐CSF treatment. No patient had evidence of fluid retention after GM‐CSF" | |
| Not reported | |
| (Sucralfate given to both groups) "Only 2 of the 20 patients treated with GM‐CSF and sucralfate did not experience any side effects related to the drugs, but most side effects were mild (WHO Grade 1 or 2). The most common side effects were local skin reactions, fever, bone pain, and mild nausea...In the control group only 1 patient complained of nausea possibly related to the use of sucralfate, and another patient interrupted sucralfate treatment because of the same reason" | |
| "12 patients who received GM‐CSF had elevated white cell counts (WCC). The range of maximal WCC was 7.2–30.5 (median 19.7). All WCC had returned to normal within 3 weeks of completing injections (median 2 weeks). Three patients developed influenza‐like symptoms with the GM‐CSF and in one patient the injections were stopped because of this symptom. One patient developed an erythematous rash at his injection sites after completing his course of 14 injections (Figure 3). He had a past history of allergy to radiographic contrast medium" | |
|
| |
| (Comparator was sucralfate) "Both mouthwashes were well tolerated, and none of the patients reported any adverse effects related to the mouthwashes. Adverse effects commonly associated with subcutaneous GM‐CSF administration, such as nausea, vomiting, bone pain, headaches, and fever, were not observed" | |
| Not reported | |
| GM‐CSF = granulocyte‐macrophage colony‐stimulating factor. | |
| Study ID | Population | Outcome | GM‐CSF | Placebo | Result |
| BMT/SCT after conditioning for haematological cancers | Oral mucositis: no scale described | No data | No data | "There was no difference in the frequency of stomatitis (defined as a sore, infected or ulcerated mouth, lips or pharynx), the incidence being between 29 and 33% in all groups" | |
| BMT = bone marrow transplantation; G‐CSF: granulocyte‐colony stimulating factor; SCT = stem cell transplantation. | |||||
| Study ID | Adverse events results |
| "Both pegfilgrastim and filgrastim were well tolerated and no significant adverse effects were associated with their use" (G‐CSF versus G‐CSF) | |
| Approximately 20% of participants receiving G‐CSF experienced mild to moderate skeletal pain which was resolved by using oral analgesics; 6% of participants in both groups reported mild generalised rash/itching; 3 participants experienced an event thought to be G‐CSF‐related and which caused them to request withdrawal from the study: abdominal pain, diffuse aches and pains, and a flare‐up of pre‐existing eczema | |
| Not reported | |
| "There was no difference in the overall frequency of adverse clinical or laboratory events between the groups or in the frequency of adverse events thought by the clinicians to be possibly or probably due to study medication" | |
| Not reported | |
| "In general, toxicities typical of postoperative RT to the head and neck were observed. Additional toxicities attributable to G‐CSF and/or daily injections were as follows: elevated WBC requiring G‐CSF dose reduction by prospectively planned guidelines occurred in nine patients in the GCSF arm; grade 2–3 bone pain was observed in two patients in the G‐CSF arm; three patients refused injection (2 G‐CSF, 1 placebo)" | |
| G‐CSF = granulocyte‐colony stimulating factor. | |
| Study ID | Adverse events results |
| "Adverse events were similar in both groups (Table 3). The most common adverse event in the rhEGF group was nausea (n = 7, 10.4%). The incidence of other adverse events including oral pain, dry mouth, and taste alteration was low. All the adverse events were mild and transient. No grade 3 or 4 adverse events were noted during the study period" (there were no differences between groups in any adverse event) | |
| "The frequency of minor and serious adverse events was similar in all groups. Most adverse events were related to primary disease status and treatment modalities" | |
| EGF = epidermal growth factor. | |
| Study ID | Adverse events results |
| "Only a minority of patients (six [6.1%] of 99 patients) reported mild to moderate treatment‐emergent adverse events on the study. The symptoms included abdominal pain, diarrhea, oral pain, headache, and hypertension (Table 2). Of these, four were considered related to study drug: one (3%) was in the placebo group, two (6%) were in the low‐dose rhITF group, and one (3%) was in the high‐dose rhITF group. The events were isolated and resolved spontaneously without sequelae" | |
| ITF = intestinal trefoil factor. | |
| Study ID | Population | Outcome | TGF‐beta(2) | Placebo | Result |
| CT alone for colorectal cancer | Oral mucositis (WHO 0 to 4 scale): any oral mucositis | 0/9 | 2/4 | RR 0.10 (95% CI 0.01 to 1.71); P = 0.11 | |
| CI = confidence interval; CT = chemotherapy; RR = risk ratio; TGF = transforming growth factor; WHO = World Health Organization. | |||||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 BMT/SCT after conditioning for haematological cancers | 4 | 655 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.88, 1.05] |
| 1.2 RT to head & neck with cisplatin | 2 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.90, 1.00] |
| 1.3 CT alone for mixed cancers | 2 | 215 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.60, 0.85] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 13 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 BMT/SCT after conditioning for haematological cancers | 6 | 852 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.80, 0.99] |
| 2.2 RT to head & neck with cisplatin/5FU | 3 | 471 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.83, 1.00] |
| 2.3 CT alone for mixed cancers | 4 | 344 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.45, 0.70] |
| 3 Oral mucositis (severe) Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 BMT/SCT after conditioning for haematological cancers | 6 | 852 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.65, 1.11] |
| 3.2 RT to head & neck with cisplatin/5FU | 3 | 471 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.69, 0.90] |
| 3.3 CT alone for mixed cancers | 3 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.14, 0.65] |
| 4 Interruptions to cancer treatment (unscheduled RT breaks of 5 or more days) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 RT to head & neck with cisplatin/5FU | 3 | 473 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.65, 1.59] |
| 5 Interruptions to cancer treatment (chemotherapy delays/discontinuations) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 RT to head & neck with cisplatin | 2 | 374 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.62, 1.47] |
| 6 Oral pain Show forest plot | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 BMT/SCT after conditioning for haematological cancers | 1 | 42 | Mean Difference (IV, Random, 95% CI) | ‐0.85 [‐3.00, 1.30] |
| 6.2 RT to head & neck with cisplatin | 2 | 374 | Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.27, 0.02] |
| 7 Normalcy of diet (use of supplemental nutrition) Show forest plot | 7 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 BMT/SCT after conditioning for haematological cancers | 4 | 714 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.58, 1.34] |
| 7.2 RT to head & neck with cisplatin/5FU | 3 | 473 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.77, 1.37] |
| 8 Normalcy of diet (worst ability to eat score ‐ 1 to 4 scale) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 BMT/SCT after conditioning for haematological cancers | 1 | 42 | Mean Difference (IV, Random, 95% CI) | ‐0.5 [‐1.21, 0.21] |
| 9 Number of days in hospital Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 BMT/SCT after conditioning for haematological cancers | 1 | 281 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐1.64, 1.64] |
| 10 Number of days of treatment with opioid analgesics Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 BMT/SCT after conditioning for haematological cancers | 2 | 323 | Mean Difference (IV, Random, 95% CI) | ‐1.41 [‐3.33, 0.51] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 BMT/SCT after conditioning for haematological cancers | 1 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.75, 1.03] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 BMT/SCT after conditioning for haematological cancers | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 CT alone for metastatic colorectal cancer | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Oral mucositis (severe) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 3.1 BMT/SCT after conditioning for haematological cancers | 2 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Oral pain (maximum score on 0 to 10 VAS) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 BMT/SCT after conditioning for haematological cancers | 1 | 28 | Mean Difference (IV, Random, 95% CI) | 0.70 [‐1.90, 3.30] |
| 5 Normalcy of diet (use of TPN) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 BMT/SCT after conditioning for haematological cancers | 1 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.63, 1.02] |
| 6 Normalcy of diet (worst ability to eat score ‐ 1 to 4 scale) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 BMT/SCT after conditioning for haematological cancers | 1 | 28 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐0.41, 1.21] |
| 7 Number of days in hospital Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 BMT/SCT after conditioning for haematological cancers | 1 | 224 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐1.78, 1.78] |
| 8 Number of days of treatment with opioid analgesics Show forest plot | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 BMT/SCT after conditioning for haematological cancers | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 CT alone for haematological cancer | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.54, 0.85] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 CT alone for haematological cancer | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.12 [0.05, 0.28] |
| 3 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 CT alone for haematological cancer | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.01 [0.00, 0.19] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 BMT/SCT after conditioning for mixed cancers | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.80, 1.04] |
| 1.2 RT to head & neck | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.82, 1.23] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 BMT/SCT after conditioning for haematological cancers | 1 | 109 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.79, 1.13] |
| 2.2 RT to head & neck | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.49, 1.06] |
| 3 Oral mucositis (severe) Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 BMT/SCT after conditioning for mixed cancers | 3 | 235 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.33, 1.67] |
| 3.2 RT to head & neck | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.01, 7.09] |
| 3.3 CT alone for mixed cancers | 2 | 65 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.05, 7.11] |
| 4 Oral pain (maximum score on 0 to 10 VAS) Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 BMT/SCT after conditioning for mixed cancers | 1 | 90 | Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.85, 2.05] |
| 5 Normalcy of diet (use of feeding tube/parenteral nutrition) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 BMT/SCT after conditioning for haematological cancers | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 1.1 [0.63, 1.91] |
| 5.2 RT to head & neck | 1 | 29 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.01, 7.09] |
| 6 Number of days of treatment with opioid analgesics Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 BMT/SCT after conditioning for mixed cancers | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐1.10 [‐1.91, ‐0.29] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 CT alone for breast cancer | 1 | 36 | Risk Ratio (M‐H, Random, 95% CI) | 2.75 [1.07, 7.04] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.80, 1.14] |
| 2 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.24, 1.21] |
| 3 Interruptions to cancer treatment Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.13 [0.01, 2.36] |
| 4 Normalcy of diet (use of PEG tube) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.01, 3.56] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 RT to head & neck | 2 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.86, 1.22] |
| 1.2 CT alone for lung cancer | 1 | 195 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.40, 0.87] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 CT alone for breast cancer | 1 | 14 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.12, 0.95] |
| 3 Oral mucositis (severe) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 RT to head & neck | 2 | 54 | Risk Ratio (M‐H, Random, 95% CI) | 0.37 [0.15, 0.87] |
| 4 Interruptions to cancer treatment (RT interruption) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.01, 4.31] |
| 5 Normalcy of diet (use of PEG tube) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 RT to head & neck | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.16 [0.01, 2.86] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 BMT/SCT after conditioning for mixed cancers | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.82, 1.27] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 BMT/SCT after conditioning for mixed cancers | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.55, 1.11] |
| 3 Normalcy of diet (use of supplemental nutrition) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 BMT/SCT after conditioning for mixed cancers | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.94, 1.06] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (moderate + severe) Show forest plot | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 BMT/SCT after conditioning for haematological cancers | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.78, 1.43] |
| 1.2 RT to head & neck +/‐ cisplatin | 1 | 103 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.45, 0.99] |
| 2 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 BMT/SCT after conditioning for haematological cancers | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.59, 1.80] |
| 3 Interruptions to cancer treatment (RT breaks > 2 consecutive days) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 RT to head & neck +/‐ cisplatin | 1 | 113 | Risk Ratio (M‐H, Random, 95% CI) | 4.38 [0.25, 75.44] |
| 4 Normalcy of diet (use of supplemental nutrition) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 BMT/SCT after conditioning for haematological cancers | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.55, 1.94] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 CT alone for colorectal cancer | 1 | 99 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.35, 0.79] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 CT alone for colorectal cancer | 1 | 99 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.10, 0.48] |
| 3 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 CT alone for colorectal cancer | 1 | 99 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.06, 36.39] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 CT alone for colorectal cancer | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 1.3 [0.67, 2.54] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 CT alone for colorectal cancer | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.18, 3.09] |
| 3 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 CT alone for colorectal cancer | 1 | 66 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.01, 7.90] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Oral mucositis (any) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 BMT/SCT after conditioning for haematological cancers | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.35 [0.21, 0.60] |
| 2 Oral mucositis (moderate + severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 BMT/SCT after conditioning for haematological cancers | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.24, 0.79] |
| 3 Oral mucositis (severe) Show forest plot | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 BMT/SCT after conditioning for haematological cancers | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.4 [0.14, 1.17] |
| 4 Number of days in hospital Show forest plot | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 BMT/SCT after conditioning for haematological cancers | 1 | 80 | Mean Difference (IV, Random, 95% CI) | ‐2.95 [‐7.73, 1.83] |

