拔牙后出血的干预措施
Referencias
References to studies excluded from this review
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Preventive trial | |
| Preventive trial | |
| Preventive trial | |
| Trial for management of bleeding immediately after deciduous teeth extraction | |
| Preventive trial | |
| Preventive trial | |
| Trial for pain management after removal of impacted third molar | |
| No treatment. It measured the amount of intraoperative and postoperative bleeding during and after the suspension of aspirin | |
| Preventive trial | |
| Preventive trial | |
| Preventive trial | |
| Preventive trial |
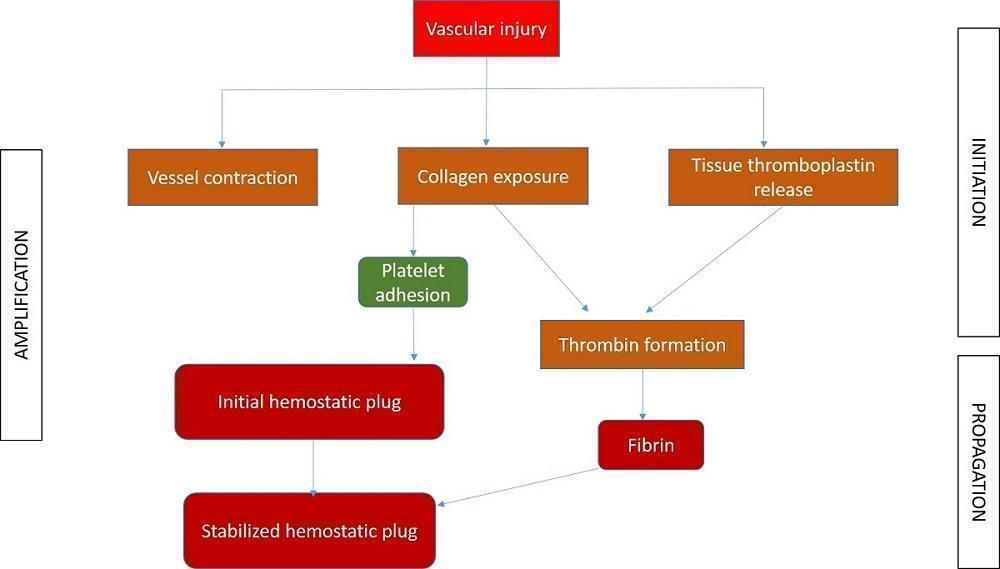
Different phases of coagulation

Study flow diagram
| Interventions for treating post‐extraction bleeding | ||||||
| Patient or population: people with post‐extraction bleeding Settings: hospital or dental practice | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | No of Participants | Quality of the evidence | Comments | |
| Assumed risk | Corresponding risk | |||||
| Bleeding, as measured by:
| No data are available as no RCTs have been conducted on interventions to treat post‐extraction bleeding | |||||
| Patient‐reported outcomes related to pain or discomfort during the procedure | ||||||
| Treatment‐associated average cost | ||||||
| Adverse events | ||||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | ||||||
| GRADE Working Group grades of evidence | ||||||
| Normal bleeding | Post‐extraction bleeding | ||
| Primary | Reactionary | Secondary | |
|
|
|
|
|
| Risk of bias | Interpretation | In outcome | In included studies |
| Low risk of bias | Plausible bias unlikely to seriously alter the results | Low risk of bias for all key domains | Most information is from studies at low risk of bias |
| Unclear risk of bias | Plausible bias that raises some doubt about the results | Unclear risk of bias for one or more key domains | Most information is from studies at low or unclear risk of bias |
| High risk of bias | Plausible bias that seriously weakens confidence in the results | High risk of bias for one or more key domains | The proportion of information from studies at high risk of bias is sufficient to affect the interpretation of results |

