Intervenciones para conseguir y mantener un empleo en pacientes adultos con enfermedades mentales graves: un metanálisis en red
Referencias
References to studies included in this review
References to studies excluded from this review
References to studies awaiting assessment
References to ongoing studies
Additional references
References to other published versions of this review
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Allocation: randomised Design: multi centre Duration: 11 months Country: Hong Kong, China | |
| Participants | N = 90 Diagnosis: schizophrenia or schizoaffective disorder as confirmed by the Chinese Version Structural Clinical Interview for the DSM IV. Included: 58% schizophrenia, 42% schizoaffective disorder Setting: recruitment of patients from two local psychiatric outpatient clinics or day hospitals Age: ≥ 18 years, mean 36.1 years Gender: 63% male Ethnicity: "Chinese people" Substance abuse: ‐ Living situation: ‐ Marital status: 88% single Employment status: unemployed Working history: 97% employment history Motivation: competitive employment as their current vocational goal Education: mean 15 years Disability benefit: ‐ Excluded: moderate or greater cognitive impairment. Excluded participants that had a score of > 18 on the 30‐item Mini‐Mental State Examination and/or were not mentally capable of giving informed consent | |
| Interventions | Integrated supported employment (N = 45) 6/7 core features of the IPS were incorporated with the exception of the rapid job search. Instead, ten WSST sessions (1.5–2 h/week) were conducted in group format prior to job search. Individualised ongoing support was given on an unlimited time basis within the study period after participants obtained employment. Integrated supported employment + cognitive remediation training (N = 45) Participants in the ISE + CRT programme received 6 h/week of individualised, visual‐based computer‐assisted cognitive exercises by 2 cognitive remediation software systems (Strong arm system and Captain's Log). A TV‐watching session was added on top of the ISE group as a control to neutralise the effect of additional time and therapist contact due to CRT in the ISE + CRT group. | |
| Outcomes | Percentage of participants who obtained competitive employment Weeks in competitive employment Mental health (BPRS) Quality of life (PWI) Drop outs | |
| Notes | Success in competitive employment was defined as having continuously worked in a job for ≥ 2 months for at least 20h/week No IPS/SE fidelity measurements reported Not included in the network meta‐analysis and direct comparison meta‐analysis because this is the only study about this intervention (comparison) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomly assigned by a blinded research assistant based on random assignment generated by SPSS" |
| Allocation concealment (selection bias) | Low risk | Assignment by a blinded research assistant |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by contents of programme |
| Blinding of outcome assessment (detection bias) | Low risk | "Blinded assessments on outcomes were conducted by independent assessors" |
| Incomplete outcome data (attrition bias) | Low risk | The programme attrition rate was 11%, with 9% for the intervention group and 13% for the control group. All participants were included in analyses following the ‘Intent‐to‐treat’ principle, with the last observation carried forward to replace any missing data. |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | Low risk | This study was funded by a grant from the Health and Medical Research Fund Committee (formally Health and Health Services Research Fund; HHSRF Project No.: 08091201). The content is solely the responsibility of the study authors and does not necessarily represent the official views of the funding agencies |
| Methods | Allocation: randomised Design: single centre Duration: 2 years (preliminary data for participants who had completed at least 1 year of study) Country: New York City, USA | |
| Participants | N = 212 (total sample N = 352) Diagnosis: in the community for < four months and previous hospitalisation of ≥ 2 months. Included: 75% schizophrenia, 7% other psychotic disorders, 11% psychoneurosis or depressive reaction Setting: Fountain House Foundation, a psychiatric rehabilitation centre Age: 68% under 35 years Gender: 60% male Ethnicity: 88% white Substance abuse: ‐ Living situation: ‐ Marital status: 70% never married Employment status: 92% unemployed Working history: ‐ Motivation: ‐ Education: 14% graduated from college, 30% attended college and 60% high school graduates Disability benefit: ‐ Excluded: out of hospital and in the community for ≥ 2 years, hospitalised primarily for drug addiction, alcoholism, overt homosexuality, uncontrolled epilepsy and criminal behaviour | |
| Interventions | Fountain House (N = 163) A programme of social and recreational activities to rebuild confidence, self‐esteem and social skills. In addition, there were day activities focused on work‐ordered activities in work crews in and around the Fountain House. Also, participants took part in supported employment for 4 months, after completing the programme of social and recreational activities and participating in work crews. After having completed those 4 months successfully participants would go on to obtain regular jobs. Control (N = 49) The control group represented those individuals who would not otherwise have received services, due to lack of facilities and personnel. They continued to receive community care from other services. | |
| Outcomes | Percentage of participants in competitive employment Hospital admissions | |
| Notes | A person was considered "gainfully employed", regardless of the number of h/week he worked Employment outcomes after 12 months (4 quarters) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | To achieve random assignment of research participants to the control and experimental groups, a method of "rotation at application," based on the time and date of the participant's application, was used. For every participant assigned to the control group, the next 3 were consecutively assigned to the experimental condition |
| Allocation concealment (selection bias) | High risk | Allocation was not concealed due to method of rotation at application |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | No details |
| Incomplete outcome data (attrition bias) | High risk | Follow‐up information on participants was secured on approximately 80% of control participants and 88% of experimental participants. Not all participants were followed up for a full 2 years. Participants continued to enter the study until the last 3 months. Thus numbers followed up are different at different time points. |
| Selective reporting (reporting bias) | High risk | Employment outcomes are only available in preliminary report |
| Other bias | Low risk | National Institute of Mental Health Project Grant OM‐29 1(RI)(C1) |
| Methods | Allocation: randomised Design: single centre Duration: 8 months Country: Fort Worth, Texas, USA | |
| Participants | N = 50 Diagnosis: chronically hospitalised psychiatric patients. Included: 78% schizophrenia, 14% chronic brain syndrome, 8% severe neurosis or character disorder Setting: Public Health Service Hospital, a federal hospital specialising in the treatment of narcotic addicts. The hospital also treats general psychiatric patients on a separate 500 bed service. Age: mean 46 years Gender: ‐ Ethnicity: ‐ Substance abuse: ‐ Living situation: hospitalised Marital status: ‐ Employment status: ‐ Working history: the majority of participants had been employed before hospitalisation as unskilled labourers Motivation: ‐ Education: very few had a high school diploma, 1/3 less than 7th grade Disability benefit: ‐ Excluded: > 62 years, hospitalised < 2 years in last 4 years, physically disabled‐bedridden, discharge plans completed, unpredictable physical violence, disabling organicity, hospital general psychiatric census | |
| Interventions | Experimental rehabilitation (N = 25) This was a specialised rehabilitation ward, where intensive multi‐disciplinary input, social skills groups, and group and individual vocational assignments were given. In addition, tours of local industrial facilities, sheltered workshop, and transitional work experience in local community enterprises were arranged. The most important aspect of this service was organised interagency co‐operative management of participants in community sheltered employment. Traditional continued treatment programmes (N= 25) Continuation of inpatient treatment on rehabilitation wards, option of referral to external VR services | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Hospital admissions Dropouts | |
| Notes | We will only use data from phase I: after phase I all participants became a new intervention group in phase II, in phase III all participants were randomised again Competitive employment was not specified | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Two groups were selected by lot. No further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by content of program |
| Blinding of outcome assessment (detection bias) | High risk | No details |
| Incomplete outcome data (attrition bias) | Low risk | 1 of 50 participants lost to follow‐up (suicide) |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | Unclear risk | No details about funding source |
| Methods | Allocation: randomised Design: multicentre Duration: 18 months Country: Malmo, Sweden | |
| Participants | N = 120 Diagnosis: SMI, which refers to having a psychosis diagnosis or a psychiatric diagnosis where the psychiatric disabilities significantly impact on everyday life functioning on a long‐term basis (2 years) Included: 64% psychotic disorder, 8% bipolar, 28% other Setting: participants were recruited from all 6 mental health teams in a southern Swedish city. Age: 18‐63, mean 38 years Gender: 56% male Ethnicity: 64% native, 36% immigrant Substance abuse:‐ Living situation:‐ Marital status: 82% single Employment status: had not worked in the preceding year Working history: 56% worked in the last 5 years Motivation: desire to work in the near future Education: ‐ Disability benefit: figures from a region close to where the present RCT took place showed that 9/10 participants were relying on sick leave benefits for their income Excluded: a somatic comorbidity causing reduced work ability | |
| Interventions | IPS (N = 60) The 8 principles of IPS were administrated by the employment specialist, and were adhered to 3 employment specialists were recruited. Their caseload for working full time was 20 participants. The IPS service was integrated with the mental healthcare service sharing the same facilities as the teams. Continuous information and discussion meetings were held 8 months before the start and throughout the study together with 6 mental healthcare teams, both national and private, the Social Insurance Agency (SIA), the Public Employment Service (PES), and FINSAM, a state‐funded organisation to facilitate co‐ordination across the healthcare system, municipality, SIA and PES. Furthermore, workshops were arranged in relation to the IPS fidelity evaluations. The fidelity score at 6 months was 110 (good fidelity), at 12 months 115 (excellent fidelity) and at 18 months 117 points (excellent fidelity) TVR (N = 60) 'Train‐place' vocational services located in the four welfare organisations, the healthcare, municipality, SIA and the PES. Typically, these nationally‐run services provide PVT in sheltered settings in a stepwise manner. The allocation of participants was dependent on the individuals’ care needs and symptom severity, as estimated by professionals in the mental healthcare team. The services ranged from individual rehabilitation support from a team member in the mental healthcare service, most often occupational therapists (50% of the participants), municipality‐run sheltered or day centre activities and PVT, joint co‐operation of vocational service in the SIA/PES, and support from either the PES or the SIA. Some participants also enrolled themselves in Fountain House (clubhouse) activities. | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Weeks in competitive employment Days to first competitive employment Dropouts Quality of life (MANSA) | |
| Notes | All competitively employed worked for at least 1 week in employment that paid at least minimum wage, available to any citizen and located in mainstream settings | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The randomisation was done centrally at the Swedish Institute of Health Sciences. The software programme in use produced a randomisation plan covering a block size of 8 random group allocation numbers at a time" |
| Allocation concealment (selection bias) | Low risk | Central allocation |
| Blinding of participants and personnel (performance bias) | High risk | "It was not possible to mask the participants’ allocation status for the study participants and the professionals involved after randomisation" |
| Blinding of outcome assessment (detection bias) | Low risk | "The researchers had no previous knowledge of the identity of any participant and coded data." "The allocation status was assessor‐blinded" |
| Incomplete outcome data (attrition bias) | High risk | 73% follow up. They performed a power analysis prior to the study and an ITT data analysis. ITT data are presented for best case or worst case of the primary outcome (obtaining competitive employment) scenario with imputation. Reasons for dropouts are reported |
| Selective reporting (reporting bias) | Low risk | All listed outcomes are reported |
| Other bias | Low risk | Financial support for this study was provided by a grant from the Swedish Research Council for Health, Working life and Welfare, and FINSAM. The Medical Faculty of Lund University and Vårdal Institutet contributed with the funding of researchers’ and research assistants’ wages |
| Methods | Allocation: randomised Design: single centre Duration: 9 months Country: Philadelphia, Pennsylvenia, USA | |
| Participants | N = 122 Diagnosis: severe mental illness. Included: 72% schizophrenia, 25% major affective disorder Setting: community mental health centre operating partial hospital programmes and outpatient programmes Age: mean 36 years Gender: 64% male Ethnicity: 80% white Substance abuse: 60% reported use of alcohol or street drugs Living situation: ‐ Marital status: 84% never married Employment status: unemployed, mean duration 9 years Working history: 82%, the positions included dishwasher, labourer, janitor, retail salesperson, mean length of employment 1 year Motivation: ‐ Education: mean years 12, 59% high school diploma, 17% some type of college degree Disability benefit:‐ Excluded: ‐ | |
| Interventions | Work focused programme (N = 61) A variety of rehabilitation intervention techniques, including one‐on‐one meetings, group sessions, individual advocacy, and long‐term supports, were used. While participating in the work‐focused programme, regular services from the CMH centre were provided, including partial hospital or outpatient services, case management, therapy, and medication monitoring. Programme interventions were based on techniques compatible with social learning theory, such as helping the client set attainable subgoals based on skill attainment and providing positive reinforcement for reaching these goals, and expectancy theory, in which motivation to work is seen as a function of positive valuation of work, the possession of necessary skills, and self‐efficacy. Control (N =61) Standard services offered, including partial hospitalisation, outpatient services, case management if needed, individual therapy, without specific vocational focus. Therapist typically provided little support to clients who were applying to participate in the system | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Drop outs | |
| Notes | Competitive employment was not specified | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | No details |
| Incomplete outcome data (attrition bias) | Unclear risk | The authors suggested that outpatient clients assigned to the experimental group tended to drop out in the first week after randomisation. However, they did not report the exact numbers. They only mentioned that 2 clients had left the experimental group after the first week and none in the control group. It is possible that this is not an ITT analysis. |
| Selective reporting (reporting bias) | High risk | Preliminary data, we did not find other reports |
| Other bias | Unclear risk | It was funded as a research and demonstration project by the National Institute on Disability and Rehabilitation Research. Those in the experimental group were significantly more likely to attend the partial hospital programme than those in the control group. Outpatient clients did not want to participate in the experimental group because they felt they were at a different functioning level, that is they felt that clients in the partial programme needed more structured programming and were less likely to have the skills needed for independent living. The group also differed in employment history. |
| Methods | Allocation: randomised Design: 2 x 2 factorial design Duration: 15 months Country: Chicago, Illinois, USA | |
| Participants | N = 131 Diagnosis: 55% schizophrenia, 19% affective disorder and 26% personality disorder Setting: a private psychosocial rehabilitation agency in the inner‐city area of a large Midwestern city Age: ≥ 18 years, mean 24.5 years Gender: 69% male Ethnicity: 75% white Substance abuse: ‐ Living situation: 25% living in hospital at the time of admission, 47% lived with parents or relatives, 14% lived in halfway houses, 2% lived sheltered, 14% lived alone Marital status: ‐ Employment status: unemployed Working history: 54% < 1 year work experience, 46% ≥ 1 year, 18% never worked for a period of > 3 months Motivation: stated goal of future employment Education: 80% high school graduates Disability benefit: 61% used government assistance Excluded: primary diagnosis of substance abuse or developmental disability, no prior participation in the programme of more than 30 days | |
| Interventions | Accelerated programme (N = 64) Participants in this programme immediately began a paid group placement for a minimum of 2 d/week. Thereafter, they were not to be returned to their prevocational crew, only if a strong justification was given by their caseworkers. Gradual programme ( N = 67) A series of graded work experiences intended to prepare members for competitive employment. Members began in prevocational crew, moved on to the group placement after 3‐6 months, them moved on to individual placement and finally moved to their own jobs. Participants in the gradual condition remained in the work crews for a minimum of 4 months. They were also discouraged from seeking community employment. | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Hospital admissions Dropouts | |
| Notes | Definition of competitive employment: employed at end of interval minimal 6 h/week Not included in the network meta‐analyses and direct comparison meta‐analyses, because we could not classify these interventions in different groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This study employed a 2 x 2 factorial design. Members were classified as work‐experienced or work inexperienced. They were then randomly assigned to 1 of 2 vocational conditions |
| Allocation concealment (selection bias) | Low risk | "After randomisation the research assistant contacted the caseworker who in turn met with the client to explain the assignment" |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by contents of programme |
| Blinding of outcome assessment (detection bias) | High risk | No details about blinding. Participants were interviewed, computerised hospital records based on information provided by caseworkers were used |
| Incomplete outcome data (attrition bias) | High risk | Data were collected on 82% at 15‐month follow‐up (N = 57 vs N = 50). N = 22 in the intervention group and N = 13 in the control group failed on placements or dropped out. 61% of the intervention group and 52% of the control group terminated from the agency during 15 months' follow‐up |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Unclear risk | This research was supported by a grant from the Field Foundation and by Grant No. 8103 from the Illinois Department of Mental Health and Developmental Disabilities. Portion of this research was completed when Gary Bond was Director of Research at Thresholds |
| Methods | Allocation: randomised Design: multicentre Duration: 4 years Country: Indianapolis, Indiana, USA | |
| Participants | N = 86 Diagnosis: serious mental illness according to Indiana Department of Mental Health criteria (major mental disorder and demonstrated disability and duration) Included: 66% schizophrenia or schizoaffective disorder, 14% personality disorder, 11% affective disorder, 17% secondary diagnosis of developmental disability Setting: 2 rehabilitation agencies of which one was a CMHC distributed over 4 centres located in an urban‐rural distribution and the other was a private not‐for‐profit agency located in Indianapolis. Age: 18 ‐60 years, mean 53.1 years Gender: 51% male Ethnicity: 80% white Substance abuse: 22% substance abuse problems Living situation: ‐ Marital status: 84% never married Employment status: unemployed for past 3 months, mean time since last job 38 months Working history: 70% had been employed continuously for a year or longer in a competitive job Motivation: expressing a desire to obtain competitive employment Education: 59% high school degree Disability benefit: being a recipient of or judged eligible for SSDI or SSI: 57% SSDI or combination, 28% SSI only Excluded: no formal vocational training in past 6 months | |
| Interventions | Accelerated entry into supported employment (N = 43) An immediate start in the SE programme after study admission, consisting of focusing on immediate competitive employment, without PVT. No screening of participants who were assumed suitable for employment. The clients’ strengths and preferences were evaluated to find jobs matching the client. In addition, the programme helped locating jobs through systematic contact with employers and occasionally negotiated with the employer to make reasonable accommodation. In addition, clients were given extensive job coaching after placement and follow‐along support was continued indefinitely. Non‐vocational aspects of their rehabilitation and treatment were also available. Gradual entry intro SE (N = 43) A minimum of 4 months’ preparation in prevocational work readiness training, before being eligible for the SE programme, consisting of vocational readiness classes, which taught skills such as resume writing, job interviewing and job keeping. After this the SE programme was started. | |
| Outcomes | Percentage of participants who obtained competitive employment Weeks in competitive employment Days to first competitive employment Dropouts | |
| Notes | Definition competitive employment: whether or not a client was competitively employed during follow‐up We used data after 1 year for this review, because employment outcomes after 2 and 4 years were only those who were currently employed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Clients were randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | "The employment specialists were responsible for providing all research data to the research team" |
| Incomplete outcome data (attrition bias) | High risk | Outcome data at 1 year follow‐up available for 86% of the participants (N = 39 and N = 35). Reasons for missing data reported. Final sample excluding 4‐month dropouts N = 65 (N = 34 and N = 31). No further details. They did not perform an ITT analysis |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | Support for this study was provided by Social Security Administration Grant 12‐D‐70299‐5‐01. The first author was supported by the Research Scientist Development Award K02 MH 00842 from the National Institute of Mental Health |
| Methods | Allocation: randomised Design: multisite Duration: 24 months Country: Chicago, Illinois, USA | |
| Participants | N = 200 Diagnosis: severe mental illness according to State of Illinois criteria, i.e. DSM IV criteria of schizophrenia spectrum disorder, bipolar disorder, obsessive‐compulsive disorder or other psychotic disorder and either significant treatment history or significant functional impairments (39% schizophrenia, 17% schizoaffective disorder, 24% bipolar disorder, 17% depression) Setting: Thresholds, psychiatric rehabilitation service Substance use: 32% used alcohol and 21% used drugs during study Living situation: 35% independent, 28% with family, 13% semi‐independent, 21% institutional, 3% homeless Marital status: 74% single, 21% divorced, 4% married Employment status: unemployed, no competitive employment in past 30 days Motivation: expressed goal of paid employment Work history: 40% ≥ 1 year work experience Education: 45% some college or associate's, 26% high school graduate or GED, 18% did not graduate high school Disability benefit: 76% | |
| Interventions | IPS (N = 100) The IPS programme was newly implemented. The programme model followed closely that described in the IPS manual. The implementation went poorly during the first 6 months. Programme fidelity (IPS fidelity scale) scores were low in the first 6 months but after personnel changes, the fidelity equalled or exceeded 70 during the rest of the study. All ratings were made by a single assessor (one of the authors) DPA (N = 100) DPA was a Thresholds vocational programme, that adhered to Clubhouse values concerning client empowerment but departed from the Cubhouse vocational programme standards. It is a stepwise approach to competitive employment in which clients are assessed on work readiness during PVT, then typically are initially placed in protected jobs for and indefinite period of time. DPA offers a range of job options from an existing pool of placements available through agency‐run businesses and standing relationships with employers. DPA emphasises peer support by maximising the clubhouse environment, group placements and employment groups. | |
| Outcomes | Percentage of participants who obtained competitive employment Number of weeks in competitive employment Number of days to first competitive employment Percentage of participants who obtained non‐competitive employment Mental health (PANNS) Quality of life (QOLI) Dropouts | |
| Notes | Competitive employment was defined as a job with a community employer in an integrated community setting, paying at least minimum wage. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was achieved by means of a computerised randomisation list in lots of 20 at each site" |
| Allocation concealment (selection bias) | Low risk | "After the baseline interview was completed, the interviewer called the offsite project director to report the identification number, programme location, and work history (experienced/inexperienced). The project director responded with study condition as determined by an a priori computerised randomisation list prepared for each work history level within site" |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | "Interviewers were not blind to vocational programme assignment" |
| Incomplete outcome data (attrition bias) | High risk | Number of lost to follow‐up reported, but no reasons for missing data provided. Of the 200 participants 171 (85.5%) completed the 24‐month interview. From 16 other participants employment data were obtained, yielding 187 participants (93.5%) in the final sample (IPS N = 92, DPA N = 95). Treatment exposure sample IPS n = 78 and DPA n = 64 |
| Selective reporting (reporting bias) | Low risk | All listed outcome of interest were reported |
| Other bias | Low risk | Funding: supported by Grant R01MH59987 from the National Institute of Mental Health. No details. No evidence of other bias. |
| Methods | Allocation: randomised Design: multi‐site Duration: 12 months Country: Chicago, Illinois, USA | |
| Participants | N = 90 Diagnosis: severe mental illness according to state criteria that is, diagnosis of schizophrenia spectrum disorder, bipolar disorder, or other psychotic disorder and either significant treatment history or significant functional impairments (53% schizophrenia, 18% depressive disorder, 25% bipolar disorder) Setting: Thresholds, a large psychiatric rehabilitation agency Age: ≥ 18 years, mean 43.8 years Gender: 79% male Ethnicity: 59% African American, 30% white Substance use: 22% alcohol dependence or abuse, 30% drug dependence or abuse. Living situation: 57% own apartment, 22% group home Marital status: 69% never married, 18% divorced Employment status: no competitive employment in past 3 months Work history: 49% worked in past 5 years, 95% held a competitive job in the past Motivation: expressed interest in a competitive job Education: 40% less than high school, 24% high school graduate, 32% some college, 3% college graduate. Criminal justice involvement: 98% arrested in the past, 76% incarcerated, 50% drug offence 44% theft, 37% violence, 62% felony, 67% misdemeanour, 20% arrested during study Disablity benefit: 89% Excluded: no legal, physical or other restriction that would prevent participating over the 12 months' follow‐up period, including pending criminal charges | |
| Interventions | IPS (N = 45) The IPS condition followed the principles of IPS SE, enhanced with a day‐long training for IPS employment specialists on criminal justice issues. The fidelity was assessed with the Revised Individual Placement and Support Fidelity Scale (IPS‐25). All fidelity reviews met the criteria for good fidelity. Work Choice (N = 45) Work Choice was based on the empirically validated job club model, tailored for people with psychiatric disabilities. It facilitated a self‐directed job search, helping clients with resume preparation, interview skills, and job leads. Classes were scheduled weekly at two conveniently located sites. The curriculum included training in application procedures, job search strategies, and linkage services. The classes were held in a room with computer workstations for applying online for jobs. A 14‐item Work Choice fidelity scale was developed for the study. The total score was 4.6, indicating adequate fidelity. | |
| Outcomes | Percentage participants who obtained competitive employment Percentage of participants in non‐competitive employment Hospital admissions Dropouts | |
| Notes | Competitive employment defined as jobs in integrated work settings in the competitive job market at prevailing wages, with supervision provided by personnel employed by the business | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A biostatistician prepared a randomised list based on an urn randomisation technique with block size equal to four" |
| Allocation concealment (selection bias) | Low risk | "Each participant opened the next consecutively numbered, sealed envelope, which revealed the assigned study condition" |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | Participants were interviewed and employment outcomes were corroborated through the agency's management information system and employment specialist logs. Blinding is not described, but it is unlikely. |
| Incomplete outcome data (attrition bias) | Low risk | Main outcome data were available for 85 participants (94%) |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | Baseline difference has been taken into account This study was supported by grant H133G100110 from the National Institute of Disability and Rehabilitation Research. |
| Methods | Allocation: randomised | |
| Participants | N = 312 Diagnosis: severe mental illness (80% schizophrenia or schizoaffective disorder, 17% bipolar disorder), had been ill and had major role dysfunction for at least 2 years Setting: 6 European mental health centres Age: between 18 years and local retirement age, mean 37.8 years Gender: 60% male Ethnicity: 90% born in country of residence Substance abuse: ‐ Living situation: 52% with friends/relatives, 34% alone, 14% sheltered Marital status: not reported Employment status: had not been in competitive employment in the preceding year Work history: 56% worked more than 1 month in past 5 years Motivation: wished to enter competitive employment Education: mean number of years 11.9 Disability benefit: ‐ Excluded: ‐ | |
| Interventions | IPS (N = 156) The IPS model consists of identification of patients who want to work in the competitive labour market, and helps them develop realistic goals and seek appropriate employment directly; there is no training phase. The IPS worker builds up a network of employers willing to accept patients, with whom the IPS worker continues contact, supporting both patient and employer. This support is open ended (in our study until the end of the 18‐month follow‐up), and the IPS worker had a maximum caseload of 25 patients. When the local services operated a CMH team system, all IPS workers were located within such a team. All IPS workers maintained good or fair levels of IPS fidelity throughout the study (median 65, min–max 61–70 of 75, IPS Fidelity Scale). Vocational Services (N = 156) The vocational service at every centre was chosen on the basis that it was the best alternative VR service available locally, and it was the typical and dominant service in the area. This rehabilitation consisted of an assessment of the patient’s rehabilitation needs, and the provision of a structured training programme aimed at combating deficits related to illness and training in appropriate work skills. The structured programme usually occupied most of the week and was generally at a day centre, although in Ulm it involved mostly residential care. | |
| Outcomes | Percentage of participants who obtained competitive employment Days in competitive employment Hospital admissions Mental health (PANNS, HADS) Quality of life (QOLP) Dropouts | |
| Notes | The primary outcome was the difference in proportions of people entering competitive employment (working for at least 1 day). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was done centrally with MINIM (version 1.5)" |
| Allocation concealment (selection bias) | Low risk | "The allocation sequence was concealed until the services had been assigned" |
| Blinding of participants and personnel (performance bias) | High risk | Participants and professionals were not blinded to service allocation |
| Blinding of outcome assessment (detection bias) | High risk | Researchers were not blinded to service allocation |
| Incomplete outcome data (attrition bias) | High risk | Total of 60 (19%) lost to follow‐up. N = 24 dropped out of IPS group (N = 21 refused interview, N = 3 died). N = 36 dropped‐out of vocational services group (N = 36 dropped out of service of which 27 were still included in study, N = 25 dropped out of study, N = 2 died of natural causes), no reasons provided; N = 2 died). All follow‐up participants receiving IPS were treated; in follow‐up participants in vocational services group, N = 93 were treated and N = 27 were not treated. The study conducted ITT analysis for primary outcome |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | Low risk | This study was funded by a grant from the European Union Quality of Life and Management of Living Resources Programme QLRT 2001‐00683. The sponsor of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication. |
| Methods | Allocation: randomised Design: single centre Duration: 18 months Country: Oxford, UK | |
| Participants | N = 123 Diagnosis: 58% psychotic disorder, ill for an average of 10 years Setting: a nonstatutory mental health service in Oxford (RESTORE) funded by local commissioners and which offered a range of programmes for individuals with mental health problems Age: 18‐65 years, mean 38 years Gender: 59% male Ethnicity: 85% white, 83% born in UK Substance abuse: ‐ Living situation: 89% independent accommodation Marital status: 21% married/cohabiting Employment status: unemployed for a minimum of 6 months, median of 24 months Working history: 97% worked previously Motivation: seeking employment in the open market, referred patients were assessed by the IPS worker for their motivation for obtaining employment before being offered the service Education: median 13 years of general education, 40% entered tertiary education Disability benefit: ‐ Excluded: main reason: duration of unemployment of less than 6 months | |
| Interventions | IPS LITE (N = 62) A shortened form of IPS in which job‐seeking support was limited to 9 months and support to those who acquired employment to 4 months. Those failing to obtain employment were referred back to their mental health team with an open invitation for re‐referral. A similar offer of re‐referral was made to those employed. IPS (N= 61) IPS is a form of VR based on eight principles: (a) focus on competitive employment; (b) no exclusion criteria; (c) rapid job search; (d) integration with mental health team; (e) attention to client’s job preferences; (f) time‐unlimited support; (g) benefits counselling; and (h) active job development. No IPS fidelity measurements reported | |
| Outcomes | Percentage of participants who obtained competitive employment Weeks in competitive employment Days to first competitive employment Mental health (BPRS, HADS) Quality of life (MANSA) Hospital admissions Dropouts | |
| Notes | Definition of competitive employment: employment in the open market for at least 1 day | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent statistician conducted the randomisation. "A non‐deterministic minimisation algorithm was used to produce treatment groups balanced for 5 factors: age, gender, diagnosis, duration of illness and previous employment. The first 2 participants were allocated using simple randomisation to avoid predictability. Subsequently, the minimisation algorithm was applied with an allocation ratio that was not fully deterministic: there was an 80% bias in favour of allocations that minimised the imbalance. If the marginal totals for the groups were the same at a given point, simple randomisation was then used" |
| Allocation concealment (selection bias) | Unclear risk | No further details |
| Blinding of participants and personnel (performance bias) | High risk | "Blinding was not possible for the participant, the IPS worker or the independent researcher" |
| Blinding of outcome assessment (detection bias) | High risk | "Blinding was not possible for the participant, the IPS worker or the independent researcher" |
| Incomplete outcome data (attrition bias) | High risk | 74% follow‐up (N = 48 in intervention group and N = 43 in control group), reasons for missing data described, analyses were conducted according to the ITT principle |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | Funding sources: Oxfordshire and Buckinghamshire Mental Health NHS Foundation Trust, National Institute for Health Research (NIHR), Research for Patient Benefit (RfPB) Programme funding (ref: PB‐PG‐0909‐20029) |
| Methods | Allocation: randomised Design: 2 centres, 1 included in this review* Duration: 3 years Country: Long Beach, California, USA | |
| Participants | N = 526 (Long Beach: N = 256) Diagnosis: a serious and persistent mental illness as demonstrated by a DSM III‐R diagnosis, a substantial functional impairment due to the mental disorder and eligible for public assistance as a result of the functional impairment. Included (Long Beach): 55% schizophrenia, 14% bipolar disorder Setting: The ISA (integrated service agency) the Village in Long Beach. The Village management and clinical leadership have wide experience in psychosocial rehabilitation programmes Age: 30% > 45 years Gender: 43% male Ethnicity: 68% white Substance abuse: ‐ Living situation: ‐ Marital status: 47% ever married Employment status: 11%‐12% earned some wages in baseline year (fiscal year before study) Working history: 19% worked at any time in past year Motivation: interest in work was not an eligibility requirement Education: ‐ Disability benefit: 74% received SSI in past year Excluded: primary substance abuse disorder Other: 4% arrested in past year and 2% convicted of a crime past year | |
| Interventions | ISA programme (N = 127) The Village ISA model uses interdisciplinary teams similar to those used in the PACT. The staff‐to‐client ratio is 1:10. Like newer PACT models it integrates services provided by the team with the services of programme specialists in employment, substance abuse and socialisation. There is staff to develop competitive jobs and support clients, where finding employment was a key value of the programme. The Village provided all employment services with its own staff, committing itself to operating a number of businesses at the programme site. These included a cafe and a small store (both open to the public), a catering service, a client bank, and a janitorial service. Besides staffing these transitional employment opportunities, the Village had at least two staff members working to develop competitive jobs and support clients in them. These specialised employment staff and the on‐site job supervisors have worked increasingly closely with the service teams. The integration of transitional employment with supported employment and a core service team is unique. Service as usual (N = 129) Usual mental health services with limited case management and limited amount of other rehabilitative services *Stanislaus ISA The SISA approach varied over time but constant involved outside contract. SISA did not have any in‐house transitional job opportunities nor did it have its own job developers. The core service team rather than specialist staff provided on‐the‐job support. | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Quality of life (QOLI) Hospital admissions Dropouts | |
| Notes | Competitive employment was not defined but they distinguished completive and transitional employment outcomes *For this review we only used data from one site: village, Long Beach, because we were not able to classify the intervention at SISA in Modesta, and no competitive employment data were available. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Clients were randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | No details about blinding, data collected from statewide data bases and client interviews |
| Incomplete outcome data (attrition bias) | High risk | Attrition before the study (Long Beach) began reduced the numbers to N = 102 in intervention group and N = 108 in control group (93%). In the 3rd study year service utilisation data were available for N = 95 and N = 86 participants (80%). N = 83 and N = 69 participants were interviewed (67%). In the analyses they used the N = 102 and N = 108 |
| Selective reporting (reporting bias) | Low risk | All listed outcomes are reported |
| Other bias | Low risk | The study was supported by the California Department of Mental Health and Grant 1R01 MH47063‐03 from the National Institute of Mental Health to Dr Hu |
| Methods | Allocation: cluster‐randomised Design: multicentre: 4 Duration: 12 months Country: London and Midlands, UK | |
| Participants | N = 159 Diagnosis: 1st episode psychosis Setting: expected to remain under the care of the early intervention service for at least the subsequent 12 months Age: 18‐35 years, mean 24 years Gender: 73% male Ethnicity: 57% white, 30% black, 14% Asian Substance abuse:‐ Living situation:‐ Marital status:‐ Employment status: not currently in mainstream employment or full‐time education Working history: 73% ever worked, 34% worked since unwell Motivation: all participants had a wish to work Education:‐ Disability benefit:‐ Excluded: organic disease | |
| Interventions | IPS + motivational interviewing (N = 81) Care coordinators were provided with a motivational interview training by recognised experts: 3‐day course, followed by 2 further sessions over the next 3 months and a 2‐day ‘refresher’ course in the second year. The training aimed to provide clinicians with a clear understanding of issues such as intrinsic motivation, ambivalence and readiness to change, as well as how to influence conversations, recognize appropriate times to use motivational interviewing and feel confident in the use of motivational interviewing in everyday practice. Training days consisted of brief didactic work, discussion, role‐play and recorded demonstrations. IPS (N = 78) The vocational specialists in the teams were trained to deliver IPS with fidelity. Scores on this measure for the 4 teams ranged from ‘good’ (both London teams and the intervention team in the Midlands had scores of 111‐114/125) to ‘exemplary’ (the control team in the Midlands with a score of 116). All 4 teams were rated as having IPS fully integrated with the mental health team. However, two teams – one in the intervention arm and one in the control arm – experienced gaps in the availability of IPS specialists when staff moved on or were absent through illness in both instances over comparable 6‐month periods. | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Weeks in competitive employment Dropouts | |
| Notes | Definition open employment: having a job paying at least minimum wage in a mainstream setting and not specifically for people with disabilities. "A cluster design was chosen to avoid ‘seepage’ from experimental conditions into the control arms" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Teams were randomised. in Both clusters 1 team was located in urban setting and 1 team in suburban/rural Design effect |
| Allocation concealment (selection bias) | High risk | Teams were recruited and baseline motivational training completed before recruitment of participants |
| Blinding of participants and personnel (performance bias) | High risk | "It was not possible to maintain masking to team allocation" |
| Blinding of outcome assessment (detection bias) | High risk | Information on occupational activity was obtained from the participants, from the clinical record and in two instances from family source |
| Incomplete outcome data (attrition bias) | Low risk | No loss of clusters. Occupational outcomes were obtained for 135 participants (85%) at 12‐month follow‐up (N = 68 in intervention group and N = 67 in control group). Sensitivity analyses were carried out. |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | The study was funded by a grant from the National Institute for Health Research (NIHR) under its Research for Patient Benefit programme. The views expressed are those of the study authors and not necessarily those of the National Health Service, the NIHR or the Department of Health Significant baseline differences in ethnicity: th the majority of black African and black Caribbean participants in the London teams, the majority of Asian participants in one Midlands team and very few from ethnic minority populations in the second Midlands team Random‐effects logistic regression models used taking account of clustering |
| Methods | Allocation: randomised Design: single centre Duration: 9 months Country: Chicago, Illinois, USA | |
| Participants | N = 132 Diagnosis: severely disturbed people. Included: 75% schizophrenia, 11% other psychosis, 11% major affective disorder,10% personality disorder Setting: Thresholds, a privately operated psychiatric rehabilitation centre. Thresholds offers a full range of programmes to foster improved client functioning in several important areas Age: ≥ 19 years, mean 25.4 years Gender: 53% male Ethnicity: ‐ Substance abuse: ‐ Living situation:‐ Marital status: ‐ Employment status: unclear, but unemployment seems likely because of low (re)employment rates Working history:‐ Motivation:‐ Education: ‐ Disability benefit: ‐ Excluded: not primarily alcohol‐ or drug‐dependent or mentally retarded | |
| Interventions | Comprehensive treatment (N = 66) This treatment consisted of individual casework, VR (i.e. gradual preparation for employment by participation in work crews, and thereafter, in voluntary or paid part‐time positions) and entry‐level jobs in the competitive market place, after having performed adequately in the transitional environments. In addition, social rehabilitation (i.e. problem‐solving and activity groups), linked residential facilities (where suitable), an academic programme (focused on passing the high school equivalency examination), and a medication and relapse discussion group was organised. Incoming clients were assigned to a work crew at Thresholds. After they demonstrated readiness for more demanding tasks they were placed in voluntary or paid part‐time positions in the community. Supportive treatment (N = 66) Supportive treatment programme relied almost exclusively on rehabilitative services and facilities available in the surrounding community. This resulted in referral to existing community services where appropriate. In addition, 6 h/week supportive treatment, which was widely used by practitioners who treat severely disturbed clients, discussion and peer‐support group, and visits fortnightly by a consulting psychiatrist (prescribed and discussed medication) were arranged | |
| Outcomes | Percentage of participants who obtained competitive employment Hospital admissions Dropouts | |
| Notes | Competitive employment, minimum wage was assumed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random assignment at intake |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given programme by contents |
| Blinding of outcome assessment (detection bias) | High risk | No details about blinding. Participants were interviewed. Admission data were corroborated by hospital records. |
| Incomplete outcome data (attrition bias) | High risk | Of the 132 clients who consented to participate (15 in each treatment) were eliminated because they attended fewer than 3 days during the 1st month after intake. At follow‐up they were unable to contact 5 participants of the comprehensive treatment and 14 from the supportive treatment. In the majority of these cases we reconstructed re‐hospitalisation data by talking to reliable informants and hospital records. We were able to obtain verified outcome data for 50 and 43 participants (76%) |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | Research was supported by grant 518 from the Illinois department of Mental Health and Developmental Disabilities At the time this work was done Dr. Bond was director of research at Thresholds in Chicago |
| Methods | Allocation: randomised Method: multicentre Duration: 18 months Country: New Hampshire, USA | |
| Participants | N = 143 Diagnosis: a major mental illness with major role dysfunction of at least 2 years and clinical stability (i.e. out of the hospital) for at least 1 month 47% schizophrenia and related psychotic disorders, 43% bipolar and other severe mood disorders Setting: CMH centres Age: 20‐65 years, mean 37.0 years Gender: 48% male Ethnicity: 95% white Substance abuse: 20% alcohol use/dependence, 11% drug abuse/dependence Living situation: 84% independent, 9% community residence Marital status: 50% never married, 38% separated/divorced, 10% married, 2.1% widowed Employment status: unemployment for at least 1 month, 36% currently working in non competitive employment (22% sheltered workshop), 0% in competitive employment Motivation: interest in competitive employment Work history: good employment histories Education: 40% > high school, 34% high school, 26% < high school Disability benefit: not reported Excluded: significant memory impairment, medical illness or substance dependence that would preclude participating in a training programme | |
| Interventions | IPS (N = 74) IPS used a team approach to integrate mental health and vocational services. Employment specialists were hired by mental health centres and attached directly to clinical teams to ensure coordinated services. Rather than providing pre‐employment assessment and training in job‐related activities, IPS employment specialists began helping clients to find jobs immediately and, after securing employment, provided training and follow‐along supports as needed. Implementation of IPS differed in the two cities. Both IPS programmes assisted some clients in obtaining volunteer work and sheltered jobs. In one site, these jobs were used as a means of transitioning clients to competitive work. In the second site, however, employment specialists placed more emphasis on sheltered jobs and used them for assessment and long‐term placement, contrary to the IPS model. Despite feedback to supervisors from the project director, this pattern persisted throughout the study, and this site was considered to have a weaker implementation of IPS. The research director monitored implementation through visits and reviewed computerised data. Data generally supported fidelity. Group skills training (GST) (N = 69) The programme offered individualised intake, pre‐employment training in a group format, individualised placement and support on the job, liaison with mental health providers, and follow‐along supports. The pre‐employment training was designed to develop awareness and skills in the three areas of choosing, getting, and keeping a job. In addition to discussing and practicing the skills needed for these tasks, clients were encouraged to explore work‐related values and to understand realistically their strengths and weaknesses as workers. Following the initial skills training, clients met with staff in a group twice each week to continue building interview skills and to discuss potential job leads and interviews. Once employed, clients continued to receive individual support services from GST staff. | |
| Outcomes | Percentage of participants who obtained competitive employment Dropouts Mental health (BPRS, no data available) Quality of life (QOLI, no data available) | |
| Notes | Competitive employment was defined as work in the competitive job market at prevailing wages supervised by personnel employed by the business | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Clients were stratified on the extent of previous employment and randomly assigned within site |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | Employment was assessed weekly by employment specialists and by direct interviews with clients. No details about blinding, but unlikely |
| Incomplete outcome data (attrition bias) | Low risk | Data were obtained for 140 of 143 participants. Two dropped out of the study, and one participant died (IPS lost 2, GST lost 1) |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | Low risk | This work was supported by US Public Health Services Grant MH‐00839 from the National Institute of Mental Health and Grant MH‐47650 from the National Institute of Mental Health and the Substance Abuse and Mental Health Services Administration and by the New Hampshire Divisions of Mental Health and Vocational Rehabilitation, the Mental Health Center of Greater Manchester, the Central New Hampshire Community Mental Health Services, and the Employment Connection Specialists. Group equivalence upon study entry was tested for 78 variables. Significant differences were found for two variables. IPS participants were less likely to report that they were not working because of mental disability, and they had more favourable scores on the Rosenberg Self‐Esteem Scale than did GST enrollees |
| Methods | Allocation: randomised Design: single centre Duration: 18 months Country: Washington DC, USA | |
| Participants | N = 152 Diagnosis: criteria SMD of District of Columbia Commission on Mental Health Services: major mental illness, defined as schizophrenia, schizoaffective disorder, bipolar disorder, recurrent major depression or borderline personality disorder, and at least 2 years of major role dysfunction (67% schizophrenia spectrum, 14% bipolar disorder, 16% depressive disorder) Setting: Community Connections, an agency in southeast Washington, DC that serves people with SMD who need intensive case management usually because their psychiatric disorders are complicated by homelessness, comorbid substance use disorder or HIV infection Age: mean 39.4 years Gender: 39% male Ethnicity: 82% African American Substance abuse: 9% current alcohol use disorder, 15% current drug use disorder Living situation: mean 23 days homeless in past year Marital status: 66% never married Employment status: unemployed Motivation: interest in competitive employment Work history: mean 7.7 months paid work in past 5 years Education: 65% high school or higher Disability benefit: not reported Excluded: memory impairment or medical illness that would preclude working or participating in research interviews | |
| Interventions | IPS (N =76) The IPS programme integrated mental health and vocational services by having an employment specialist join multidisciplinary case management teams. IPS employment specialists assisted clients in searching for jobs rapidly and, after securing employment, provided individualised, follow‐along supports as needed without time limits. 3 employment specialist were hired to implement IPS, each had a caseload of 25 clients and carried out all phases of the vocational process. Fidelity rating made regularly throughout the project by the research team indicated that the IPS programme consistently scored within high‐fidelity range of the IPS fidelity scale EVR (Enhanced VR) (N = 76) This approach was considered "enhanced" because an extra vocational counsellor was placed in the Rehabilitation Services Administration office to ensure that participants assigned to this condition were referred to appropriate rehabilitation agencies expeditiously. The vocational counsellor monitored participants monthly, and if a client was dissatisfied with the programme to which he or she was assigned or dropped out of vocational services, the counsellor attempted to link that participant with another agency. All of the EVR agencies endorsed competitive employment as their goal but used stepwise approaches that involved prevocational experiences, primarily paid work adjustment training in a sheltered workshop | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Days to first competitive employment Quality of life (QOLI) Mental health (BPRS) Dropouts | |
| Notes | Definition of competitive employment: work in competitive job market at prevailing wages with supervision provided by personnel employed by the business and in integrated work settings | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random assignment was stratified according to work history (> 1 year of employment in a previous job) |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | "A limitation was the inability to maintain the blindedness of interviewers" |
| Incomplete outcome data (attrition bias) | Low risk | 2/152 lost to follow‐up, no reasons provided |
| Selective reporting (reporting bias) | Low risk | All listed outcomes of interest reported |
| Other bias | Low risk | This work was supported by grant MH51346 from the Substance Abuse and Mental Health Services Administration and the National Institute of Mental Health, Washington, DC, and grant MH00839 from the National Institute of Mental Health |
| Methods | Allocation: randomised Design: multicentre Duration: 2 years Country: USA | |
| Participants | N = 2238 Diagnosis: a primary diagnosis of schizophrenia or a mood disorder. Included: 70% affective disorder, 30% schizophrenia Setting: 23 community‐based sites dispersed throughout the USA. All sites had demonstrated the ability to provide high‐fidelity IPS supported employment and integrated behavioural health interventions. Eligible participants were recruited from Social Security Administration lists of SSDI beneficiaries. Age: 18‐55 years, mean 43.5 years Gender: 47% male Ethnicity: 60% white, 26% black, 11% Hispanic Substance abuse: ‐ Living situation: ‐ Marital status: 46% never married Employment status: unemployed Working history: 30% worked in past 2 years Motivation: being interested in gaining employment Education: 12% < high school, 26% high school, 35% some college or technical, 11% bachelor degree Disability benefit: eligibility criteria, 76% on SSDI for > 24 months Excluded: residing in a custodial setting (such as a nursing home), having a legal guardian, having a life‐threatening physical illness that would preclude participating in the study, being currently competitively employed, and already receiving supported employment from the study site | |
| Interventions | Multifaceted intervention (N = 1121) Team‐based SE, systematic medication management, and other behavioural health services, along with elimination of barriers by providing complete health insurance coverage (with no out‐of‐pocket expenses) and suspending disability reviews. The Social Security Administration paid for all of these services and cost‐sharing reimbursements. Other behavioural health interventions were also offered and tailored to participants according to need and preference, e.g. case management, integrated substance abuse treatment, and family psycho‐education. The majority of sites achieved high‐fidelity IPS: 77% in the 1st year, 86% in the 2nd year, and 86% in the 3rd year; 98% of the annual fidelity ratings were fair or high. Usual services (N = 1117) The control group received the same services they had been receiving prior to enrolling. Usual care typically included the services covered by Medicare, such as outpatient physician visits, medications, and hospital care | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non/competitive employment (paid employment) Mental health (SFHS) Quality of life (QOLI) Drop outs | |
| Notes | Definition competitive employment: mainstream jobs in integrated work settings at usual wages with regular supervision | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation at each site |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by contents of programme |
| Blinding of outcome assessment (detection bias) | High risk | No details about blinding. Research interviewers assessed employment status using a computer‐assisted timeline follow‐back calendar |
| Incomplete outcome data (attrition bias) | Low risk | 84.6% followed up, N = 11 in intervention group and N = 13 in control group died and N = 50 and N = 58 < 2 interviews. They used 2 methods to address attrition and missing data. First they considered participants who did not complete at least 2 interviews as non‐responders and adjusted weights to zero. Second, they used imputation procedures to address other participants with missing data |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported, design article published |
| Other bias | Unclear risk | This study extends work that was conducted under contract SS00‐05‐60072 between the Social Security Administration and Westat. This analysis was conducted for the benefit of the Social Security Administration. The opinions expressed in this article are those of the authors and not necessarily those of the Social Security Administration |
| Methods | Allocation: randomised Design: single centre Duration: 16 weeks Country: Bedford, Massachussetts, USA | |
| Participants | N = 19 Diagnosis: dually diagnosed veterans, defined as those with a current psychiatric diagnosis of schizophrenia, bipolar disorder, major depression, ,PTSD or other anxiety disorder, and current drug or alcohol dependence. Included: 74% affective disorder, 58% anxiety disorder, 11% psychosis Setting: Bedford VA Medical Center Age: mean: 46.0 years Gender: 95% male Ethnicity: 79% white, 21% African American Substance abuse: limited to those with substance dependence for alcohol, cocaine, or opiates with active substance abuse in the prior 90 days. Included: 100% alcohol abuse or dependence, 73% drug abuse or dependence Living situation:‐ Marital status:‐ Employment status: unemployed, mean duration: 4.3 months Working history: potential for return to competitive supported employment within 6 months, as evidenced by a history of participation in competitive employment during the previous 3 years, and acceptance of the stated goal of returning to competitive employment within 8 months Motivation:stated goal of returning to competitive employment Education: mean: 13 years Disability benefit: 32% disability income Excluded: over the age of 55, chronic medical problems that would make it unlikely that they would be able to obtain and sustain a competitive job within 8 months, no intention to stay in the programme for at least 4 months or live in the local region for 12 months, < 10 years of formal education and those with a history of significant head trauma or other disorder resulting in significant cognitive impairment were also excluded | |
| Interventions | CWT only (N = 8) This was a multi‐component work‐for‐pay VR programme. Veterans were placed in structured work settings, usually in private companies, and were compensated for their work. They were typically paid by the CWT programme, which contracts with the company for their labour. While the veterans were working, CWT staff helped them negotiate and resolve difficulties on the job and prepare for obtaining their own competitive jobs. It also included a SE component designed to assist participants in maintaining employment in their own competitive jobs through structured support and management. The Bedford CWT SE services were consistent with published guidelines and treatment fidelity criteria for SE services. CTW + enhanced incentives (N = 13) CWT with enhanced incentives included the benefits available to those who participated in the basic CWT programme, and additional cash awards. Payment of these cash payments or bonuses was contingent on the completion of specified steps leading to obtaining and maintaining employment, maintaining abstinence from substance abuse, and indirectly to more prolonged retention in CWT. | |
| Outcomes | Number of participants who obtained competitive employment Weeks in competitive employment Dropouts | |
| Notes | Pilot study Return to competitive employment, definition was not described The results were not included in the network meta‐analyses and direct comparison meta‐analyses, because we could not classify these interventions in separate groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | No details about blinding of outcome assessment but unlikely: data regarding participation and wages were available from CWT clinical and financial records. |
| Incomplete outcome data (attrition bias) | High risk | Two participants assigned to the payment condition withdrew from participation several days after assignment because of changes in residence, data for these 2 participants were not available for analysis. Only 1 participant, assigned to the incentives condition, failed to complete the 16‐week follow‐up, stopping all participation in Week 15, resulting in no data about competitive employment income for weeks 15 and 16. Missing income and employment data were assumed to reflect no income and no employment. Total lost to follow‐up 3/21 = 14%, but all in intervention groups |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported. |
| Other bias | Low risk | This study was supported by the New England Mental Illness Research Education and Clinical Center. |
| Methods | Allocation: randomised Design: single centre Duration: 9 months Country: Bedford, Massachussetts, USA | |
| Participants | N = 100 Diagnosis: dually diagnosed veterans, defined as those meeting DSM‐IV criteria for a current diagnosis of (1) schizophrenia, bipolar disorder, major depression, ,PTSD or other anxiety disorder and (2) current drug or alcohol dependence or abuse, as well as active substance use within 90 days of enrolment. They had to be clinically stable, defined as having no suicidal or homicidal ideation in the prior 12 weeks and abstaining from drugs or alcohol for at least 1 week. Setting: Bedford VA Medical Center. Included: 79% major depression, 53% PTSD, 50% other anxiety disorder, 21% bipolar disorder, 9% psychotic disorder. Age: mean: 46.3 years Gender: 99% male Ethnicity: 78% white, 20% African American Substance abuse: all met criteria of dependence of at least 1 substance, 63% poly substance‐dependent. Alcohol 88%, cocaine 43%, cannabis 29%, opiates 26%. Living situation: ‐ Marital status:‐ Employment status: unemployed, mean months unemployed: 16 Working history: potential for return to competitive SE within 6 months, as evidenced by a history of at least some participation in competitive employment during the prior 3 years and acceptance of the stated goal of returning to competitive employment within 8 months Motivation: stated goal of returning to competitive employment Education: mean: 13 years. Disability benefit: 26% disability income, 61% any public support Excluded: older than 55, chronic medical problem that would make obtaining and sustaining a competitive job within 8 months unlikely, no intention to stay in VR for at least 4 months or live in the local region for 12 months, enrolment in other research studies that would affect their participation or difficulty understanding the contingency management programme (< 10 years of formal education, a history of significant head trauma or another disorder resulting in significant cognitive impairment or failed to pass a 10‐item quiz about the incentives) | |
| Interventions | VR (CWT) (N = 50) The CWT is a multi‐component work‐for‐pay VR programme. Veterans were placed in structured work settings, usually in private companies, and were compensated for their work. They were typically paid by the CWT programme, which contracted with the company for their labour. While the veterans were working, CWT staff helped them negotiate and resolve difficulties on the job and prepare for obtaining their own competitive jobs. It also included a SE component designed to assist participants in maintaining employment in their own competitive jobs through structured support and management. The Bedford CWT SE services were consistent with published guidelines and treatment fidelity criteria for SE services. VR (CWT) + contingency management (N = 50) The CWT programme combined with additional incentives for taking steps toward obtaining and maintaining competitive employment and for abstinence from substance use. A series of increasing cash incentives was offered for negative drug and alcohol screens. Employment incentives were available in two phases. Phase I incentives targeted job‐search tasks and were available for the first 16 weeks of the intervention. Phase II incentives targeted employment itself and were available for the first 32 weeks. In total, participants could earn up to USD 610 if they successfully completed all work‐related activities. Over the 36 weeks of the intervention, participants could earn incentives up to USD 1170. | |
| Outcomes | Number of participants who obtained competitive employment | |
| Notes | The current study built on the initial pilot study (Drebing 2005) to determine whether a revised version of this CM intervention applied to a larger sample of VR participants could improve treatment outcomes in terms of the number of participants obtaining and maintaining their own jobs. Competitive employment was defined as the participant working at least 20 h/week in an ongoing community‐based job for which he or she was paid at least minimum wage. The results were not included in the network meta‐analyses and direct comparison meta‐analyses, because we could not classify these interventions in separate groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The participants were randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | No detail |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by content of programme |
| Blinding of outcome assessment (detection bias) | High risk | "The study is limited by its reliance on self‐report data for key outcome variables" |
| Incomplete outcome data (attrition bias) | Unclear risk | Two participants, both assigned to the VR‐only condition, dropped out of the study during week 7. The follow‐up rate was 94% for the 3‐month follow‐up, 90% for the 6‐month follow‐up, and 88% for the 9‐month follow‐up. Unclear how many participants dropped out in the intervention or control group. All analyses were based on an ITT approach |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | This material was based on work supported by the VA Rehabilitation Research and Development Service (grant D2944R) and with resources of the New England Mental Illness Research, Education, and Clinical Center |
| Methods | Allocation: randomised Design: single centre Duration: 2 years Country: Pittsburg, Pennsylvania, USA | |
| Participants | N = 58 Diagnosis: schizophrenia, schizoaffective, or schizophreniform disorder; stabilisation on antipsychotic medications, a time‐span of no greater than 8 years since the onset of first psychotic symptoms and the presence of significant social and cognitive disability, as assessed using the Cognitive Style and Social Cognition Eligibility Interview. Included: 66% schizophrenia, 34% schizoaffective disorder, mean illness duration 3 years Setting: a specialty outpatient clinic in the comprehensive care service at the University of Pittsburgh Western Psychiatric Institute and Clinic, which serves the CMH needs of the majority of schizophrenia population. Age: mean 25.9 years Gender: 69% male Ethnicity: 69% white Substance abuse: ‐ Living situation: ‐ Marital status: ‐ Employment status: 26% employed at baseline Working history: ‐ Motivation: ‐ Education: 67% completed at least some college education, 33% attended college Disability benefit: ‐ Excluded: IQ < 80; significant substance use problems for at least 2 months prior to study enrolment | |
| Interventions | Cognitive enhancement therapy (N = 31) An integrated approach to the remediation of social‐cognitive and neurocognitive deficits in schizophrenia, where participants completed approximately 60 h of computer training in attention, memory, and problem‐solving, and participated in a newly revised, 45‐session, weekly social‐cognitive group that focuses on learning how to take the perspective of others, read non‐verbal cues, manage emotions, and appraise the social context. Enriched supportive therapy (N = 27) An illness management and psycho‐education approach that draws upon components of the basic and intermediate phases of the demonstrably effective personal therapy. Participants were seen on an individual basis. The treatment was divided into 2 phases. Phase I focused on basic psycho‐education about schizophrenia, the role of stress in the disorder, and ways to avoid/minimise stress. Phase II involved a personalised approach to the identification and management of life stressors that pose particular challenges to adequate social and role functioning | |
| Outcomes | Percentage of participants who obtained competitive employment Mental health (BPRS) Dropouts | |
| Notes | Paid competitive employment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised using a 1:1 ratio by way of computer‐generated random numbers |
| Allocation concealment (selection bias) | Low risk | "Computer‐generated random numbers" |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by content of programme |
| Blinding of outcome assessment (detection bias) | High risk | Raters were not blind to treatment assignment |
| Incomplete outcome data (attrition bias) | High risk | N = 67 participants were randomised, 9 excluded, reasons described, unclear intervention allocation of those participants. Analyses were conducted with 58 participants who were randomised and received any exposure, regardless of how limited, to their respective treatment conditions. N = 46 participants completed 2 years of treatment (69% of N =67) |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | Supported by NIMH grants MH 79537 and MH 60902. The NIMH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report and in the decision to submit the paper for publication. |
| Methods | Allocation: randomised Design: Duration: 1 year Country: New York, USA | |
| Participants | N = 34 Diagnosis: psychiatric disabilities including schizophrenia, major effective disorder, attention deficit disorder, paranoid personality disorder and oppositional defiant disorder Setting: no details Age: 16‐25 years, average 19 years Gender: 67% Ethnicity: 50% African American, 33% Hispanic Substance abuse:‐ Living situation:‐ Marital status:‐ Employment status:‐ Working history: 20% had any work experience Motivation:‐ Education: 80% special education Disability benefit:‐ Excluded:‐ | |
| Interventions | SE using job coaching (N = 14) Immediate placement in SE: job placement and job coaching services with weekly individual family and peer group therapy SE using natural support (N = 8) Immediate placement in SE: job placement services with weekly individual, family and peer group therapy Sheltered employment training (N = 12) Employment training in sheltered workshop setting with weekly individual, family and peer group therapy | |
| Outcomes | Percentage of participants who obtained competitive employment Weeks in competitive employment | |
| Notes | We used data of both SE groups as 1 intervention group Before randomisation all participants received vocational and social skills training Competitive employment: minimum wage and at least 20 h/week | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | Data were obtained via records maintained by job developers and interviews. No details about blinding |
| Incomplete outcome data (attrition bias) | High risk | No details about attrition rate. Preliminary results |
| Selective reporting (reporting bias) | High risk | No full report published |
| Other bias | Unclear risk | Funding source unclear |
| Methods | Allocation: randomised Design: single centre Duration: 24 months Country: Sumter County, South Carolina, USA | |
| Participants | N = 177 (N = 143 relevant) Diagnosis: meeting both the Federal Center for Mental Health Services’ criteria for severe and persistent mental illness, based upon diagnosis, illness duration, and level of disability 69% schizophrenia spectrum, 31% mood spectrum Setting: The South Carolina Department of Mental Health operated Santee‐Wateree Community Mental Health Center (SWCMHC) Age: ≥ 18 years, 71% between 26‐45 years Gender: 38% male Ethnicity: 77% African American, 19% white Substance abuse: 9% current alcohol abuse/dependence, 8% current drug abuse/dependence Living situation: not reported Marital status: 82.5% not married/not cohabiting Employment status: unemployed Motivation: current and/or future interest in competitive employment Work history: 60% > 6 months paid work in past 5 years Education: 52% high school or higher Disability benefit: 61% Excluded: not reported | |
| Interventions | ACT‐IPS (N = 66) The original study plan was a 3‐group trial comparing 2 newly implemented SE programmes, ACT‐IVR and IPS, to a traditional VR programme. 3 partially implemented and incompletely staffed ACT‐IVR and IPS programmes were integrated into a single ACT‐IPS programme, operating with ACT and IPS subteams composed of the ACT‐IVR and IPS staff members, respectively. To tightly integrate vocational and mental health services, the ACT‐IPS subteams met daily together as a full programme to allocate tasks to each IPS specialist and ACT staff member. Independent ACT and IPS consultants conducted fidelity assessment. IPS Fidelity Scale Yearly averaged total scores rose steadily over the project period, indicating very high IPS model fidelity in years 2–4. ACT fidelity checklist: yearly averaged checklist scores rose steadily over the project period: for years 1–4, indicating high‐fidelity in years 3 and 4. TVR (N = 77) SWCMHC and a local independent nonprofit VR agency specialising in the employment of adults with SMI, signed a formal agreement creating the comparison programme, which they named the Supported Employment Programme (SEP), despite its traditional VR philosophy. SWCMHC provided mental health and brokered case management services in parallel to vocational services. They introduced participants first to graduated work adjustment experiences as preparation for handling competitive job demands. After assessing each participant’s job skills and interests, employment specialists placed participants into 1 of its temporary, staff‐supervised, set‐aside jobs, which differed from competitive jobs in several ways. | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Weeks in competitive employment Days to first competitive employment Mental health (PANNS) (no data available) Quality of life (QOLI) (no data available) Dropouts Hospital admissions | |
| Notes | Definition competitive employment: the employer (a) paid competitive wages above the federal minimum to participants and workers without disabilities alike, (b) did not set aside the job for adults with disabilities, and (c) located the job in a typical community setting and if (d) the participant contracted for the job Part of Employment Intervention Demonstration Project (EIDP) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "SAS‐generated restricted random assignment sequence (permuted blocks of 3)" (SAS is a software programme) |
| Allocation concealment (selection bias) | Low risk | No investigator was permitted access the assignment sequence |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of programme |
| Blinding of outcome assessment (detection bias) | High risk | Unblinded study |
| Incomplete outcome data (attrition bias) | High risk | N = 108 (61%) completed the study. Voluntary withdrawal accounted for most attrition, followed by relocation outside the service area 34 participants were eliminated from the project due to project redesign |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | High risk | Project redesign and deviation from a prespecified random assignment process may have compromised study internal validity and programme construct validity. This study was supported by co‐operative agreement SM51823 from the Center for Mental Health Services (CMHS), SAMHSA, and US Department of Health and Human Services (DHHS), Rockville, Maryland, as part of the Employment Intervention Demonstration programme (EIDP), a multi‐site collaboration among 8 research demonstration sites, a co‐ordinating center, and CMHS/SAMHSA. Additional support was provided by grant SM53542 from CMHS/SAMHSA and grant MH01903 from the National Institute of Mental Health (NIMH) |
| Methods | Allocation: randomised Design: single centre Duration: 5 years Country: Bern, Switzerland | |
| Participants | N = 100 Diagnosis: stabilised mental disorder in accordance to ICD 10 combined with persistent impairment in the areas of role functioning, social functioning or independent living/self‐care skills. Included: 38% schizophrenia spectrum, 41% affective disorder, mean duration of illness 5.7 years Setting: participants recruited by the Swiss Insurance State Office. Job coach project of the Bern University Hospital of Psychiatry, staffed by employment specialists JCP is part of the CMH division of the Bern University Hospital of Psychiatry Age: 18‐64 years, mean 33.8 years Gender: 65% male Ethnicity: ‐ Substance abuse: 12% concomitant substance abuse Living situation: ‐ Marital status: 74% never married Employment status: out of competitive employment, 18% in sheltered work Working history: mean 24 months of unemployment before intake, employment rate (= ratio between employed/not employed) since age 20: 0.55 Motivation: interest in competitive employment Education: 62% completed vocational training, 25% unskilled or uncompleted, vocational training, 13% university degree Disability benefit: all participants had received the authorisation for VR from the Swiss invalidity insurance Excluded: learning disability (IQ < 70), primary substance abuse disorder, physical or organic handicap that seriously impeded work, unwillingness to attend regular outpatient therapy, performance < 50% of normal work performance as evidenced during the assessment phase; and/or attendance in the programme of < 15 h/week | |
| Interventions | Supported employment (N = 46) The Job Coach Project (JCP) was derived from the IPS model. Some modifications were made in order to meet the standards of the Swiss social insurance system and the needs of the Swiss labour market but also to enhance the sustainability. The JCP was staffed by employment specialists who assisted each participant in the programme in seeking competitive employment. Once employed, on‐the‐job training and follow‐along support was provided. If employment was terminated for any reason, the employment specialist assisted the individual in dealing with job loss and helped to secure another place. The maximum caseload was 12 participants. Several incentives were given to employers. As the JCP was part of the CMH division, the employment specialists were in close contact with the attending therapists from the outset. Repeated IPS fidelity ratings scored between 66 and 68 of 75, i.e. all score sets ranged from equivalent to consistent with the IPS. The sole exception to this was the organisation sub scale, which was not fully consistent, as the law on Swiss Invalidity Insurance requires that an assessment prior to all vocational reintegration programmes be carried out in the form of intake selection. TVR (N = 54) All control interventions had to be verified as high‐quality, train‐place VR programmes and be deemed by the Federal Social Insurance Office to be the best locally available alternative for each prospective participant. Participants in a TVR require a period of preparation before entering into regular employment. They are typically placed in sheltered workshops for 6‐12 months, after which a 3‐6‐month training stint in a companion open market may be feasible. The accompanying support by employment specialists terminated at the end of the TVR. | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Weeks in competitive employment Days to first competitive employment Mental health (PANNS) Quality of life (W‐QLI) Dropouts Hospital admissions | |
| Notes | Competitive employment was defined as a job on the open labour market that anyone could hold, not only individuals with disabilities. To be counted as competitively employed, the participant had to hold the job for at least 5 days and earn at least a minimum wage. All fidelity ratings were performed by the research team We used data after 2 years for this review (to be comparable to other study follow‐up data) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomisation was performed based on a random list generated by a computer algorithm. This list was randomly chosen from a choice of 10 lists and was then transformed in a stack of sequentially numbered and sealed envelopes containing individual assignments. These steps were performed by an administrative office outside the research team." |
| Allocation concealment (selection bias) | Low risk | "The randomisation procedure guaranteed that the research team was always fully blinded regarding to assignment." Sealed envelopes were used. |
| Blinding of participants and personnel (performance bias) | High risk | "Group assignment was only revealed once all initial assignments had been completed." |
| Blinding of outcome assessment (detection bias) | High risk | "Interviewer was not blind to programme assignments, thereby giving rise to possible rater bias. However, key employment measures were objective and duly corroborated by multiple sources." |
| Incomplete outcome data (attrition bias) | Low risk | Lost to follow‐up: 7/100. Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. ITT analysis performed |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Unclear risk | Swiss National Science Foundation, Grand 3200‐064032, unconditioned grants of the Federal Social Insurance Office, the Stanley Thomas Johnson Foundation, the Gottfired and Julia Bangerter‐Rhyner Foundation, the Bank Vontobel Foundation, the Dosenbach‐Waser Foundation and the Karl Mayer Foundation. Funder is also recruiter of participants and the income resource |
| Methods | Allocation: randomised Design: multicentre Duration: 24 months Country: London, UK | |
| Participants | N = 219 Diagnosis: severe mental illness: duration of illness over 2 years, global assessment of functioning (GAF) 60 or less and a SCAN diagnosis of a psychotic or chronic affective disorder 73% psychotic disorder, 27% mood disorder Setting: CMH teams in 2 boroughs of South London Age: between 18‐65 years, mean 38.5 years Gender: 67% male Ethnicity: 43% black, 38% white Substance abuse: not reported Living situation: 54% living alone Marital status: not reported Employment status: unemployed for at least 3 months Work history: 54% worked in the past 5 years Motivation: wanting to obtain competitive employment Education: not reported Disablity benefit: not reported Excluded: IPS in the previous 6 months | |
| Interventions | IPS (N = 109) 4 experienced employment specialists were linked with CMH teams. They focused on rapid placement with continued follow‐up support and sought to find employment opportunities that were consistent with participants’ preferences, skills and abilities. However, the integration of the IPS programme was not structural or managerial. IPS fidelity was found to be high; the IPS programme in the two boroughs received a good IPS rating; the IPS programme scored less well on the organisation dimension (specifically, integration of rehabilitation with mental health treatment) and, for Borough A, the services dimension (specifically, for the rapid search for a competitive job) compared with other dimensions. Treatment as usual ( N = 110) Treatment as usual consisted of existing psychosocial rehabilitation and day care programmes available in the local area. A range of courses were offered, most commonly pre‐employment preparation (e.g. interview skills, curriculum vitae coaching and application form practice), computers/information technology and confidence building/motivation | |
| Outcomes | Percentage of participants in competitive employment Mental Health (BPRS) Quality of life (MANSA, QOLP) Hospital admissions Dropouts | |
| Notes | Definition of competitive employment: a job paying at least the minimum wage, located in a mainstream socially integrated setting not set aside for persons with disabilities, held independently (i.e. not agency owned), with the participant in continuous employment for at least 30 days | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Treatment allocation was stratified by gender and age (10‐year bands). Randomisation with minimisation was used." |
| Allocation concealment (selection bias) | Low risk | Randomisation with minimisation was used, performed by the Institute of Psychiatry Mental Health and Neuroscience Clinical Trials Unit, a unit independent of the study to maintain concealment. |
| Blinding of participants and personnel (performance bias) | High risk | "It was not possible for participants or those administering the intervention to be masked to the participants’ allocation status" |
| Blinding of outcome assessment (detection bias) | High risk | "The researchers who conducted the 1‐year follow‐up interviews were masked to allocation status, but guessed 119 correctly out of the 197 (60%) clients assessed compared with a hypothesised 50% (with random guesses); this is significant at P = 0.005." |
| Incomplete outcome data (attrition bias) | Low risk | N = 15 (14%) in each group lost to follow‐up after 2 years: 20 withdrawn, 2 out of the country, 2 missing, 2 too ill to follow up, 3 unable to find. Furthermore, In the intervention group 1 participant was excluded from analysis because the researchers were unable to ascertain job status. No significant differences in sociodemographic or clinical variables between those who were and those who were not lost to follow‐up. All data were analysed in groups as randomised, whether or not receiving an intervention (i.e. ITT). |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | Low risk | This study was supported by the Wellcome Trust (GR071272MA); the supported employment programme was funded partly by the King’s Fund and the South London and Maudsley Charitable Trust |
| Methods | Allocation: randomised Design: single centre Duration: 6 months Country: Melbourne, Australia | |
| Participants | N = 41 Diagnosis: first episode psychosis. All participants received clinical diagnoses of schizophrenia‐spectrum disorders. Mean (SD) length of illness: intervention 12.25 (12.98) and control 15.68 (14.17) Setting: Early Psychosis Prevention and Intervention Centre (EPPIC) Age: between 15‐25 years, mean 21.4 years Gender: 80% male Ethnicity: ‐ Substance abuse: N = 23 had substance use diagnoses Living situation: 61% lived with family of origin, 36% rented a house/flat Marital status: 81% never married Employment status: 8% employed at baseline (N = 1 in intervention group and N = 2 in control group had a job) Work history: N = 34 reported a work history Motivation: wanted to find work, including a different job if they currently held one Education: 44% completed trade/technical training, 28% completed secondary education or partially completed tertiary training Disability benefit: 78% welfare benefits Excluded: lack of fluency in English Other: 92% absence of medical illness | |
| Interventions | IPS (N = 20) IPS is comprised of seven key principles: (1) a focus on competitive employment; (2) open to any person with a mental illness; (3) utilises a rapid job search approach; (4) integrated with mental health treatment team; (5) potential jobs are chosen based on people’s preferences; (6) time unlimited and provides individualised support; and (7) welfare benefits counselling is provided as monetary disincentives often need to be negotiated in the transition from a welfare benefit to paid employment. Additionally, the IPS model is extended to integrate supported education, given that vocational goals of this population frequently include completion of schooling or further training prior to job placement. An employment consultant was employed to deliver the vocational intervention which was carried out with high‐fidelity according to the Supported Employment Fidelity Scale. The fidelity was assessed by the project leader and reviewed with an interstate colleague independent of the project. Treatment as usual (N = 21) Treatment as usual consisted of participants continuing to receive EPPIC care. This involves individual case management and medical review, referral to external vocational agencies, as well as involvement with the group programme at EPPIC, which may involve participation in the vocationally oriented groups within the group programme. Treatment as usual was delivered primarily by EPPIC case managers. | |
| Outcomes | Percentage of participants who obtained competitive employment Number of weeks in competitive employment Drop outs | |
| Notes | Definition competitive employment: jobs which are not set aside but open to applications from anyone with the appropriate skills or qualifications | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomised by a statistician independent of the study using computer‐generated random numbers to carry out blocked randomisation to one of the two conditions" |
| Allocation concealment (selection bias) | Low risk | "The statistician was contacted by the leader of the project when a new participant enrolled and the statistician informed the leader of the group allocation. This information would then be given to the participant, the case manager of the participant and also the employment consultant if allocation was to the intervention group." |
| Blinding of participants and personnel (performance bias) | High risk | Information about allocation was given to leader of the project, participant, case manager and employment consultant |
| Blinding of outcome assessment (detection bias) | High risk | Assessments were conducted by a research assistant. The research assistant was not informed about allocation, but there were no formal tests of her masking to allocation. |
| Incomplete outcome data (attrition bias) | Low risk | 1 participant dropped out from the intervention group and 5 from the control group. In the control group 4 dropped out because they had enrolled wanting help to find work and felt that as they were not getting it they no longer wished to continue in the project. The remaining 2 participants dropped out as they were sent to jail. However, all who dropped out gave their permission for their employment status at follow‐up |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | High risk | This research was supported by a National Health and Medical Research Council programme Grant (ID: 350241) and an unrestricted study grant from Bristol Myers Squibb. Orygen Research Centre is supported by the Colonial Foundation There was a significant baseline difference in marital status. As more people in the control were in marital or marital‐like relationships. In logistic regression analysis there was a 6.65 more chance to have worked if married (P = 0.044) |
| Methods | Allocation: randomised Design: single centre Duration: 18 months Country: Melbourne, Australia | |
| Participants | N = 146 Diagnosis: first episode psychosis Setting: Early Psychosis Prevention and Intervention Centre (EPPIC), which is a sub‐programme of Orygen Youth Health. Orygen Youth Health is a public mental health service for young people aged 15–25 years Age: 15‐25 years, mean 20.3 years Gender: 67% male Ethnicity: 75% country of birth was Australia Substance abuse: not reported Living situation: not reported Marital status: 97% never married Employment status: 16% employed at baseline Working history: not reported Motivation: expressed an interest in employment or education, whether that was to find a job or course or to receive support to stay in a current job or course Education: 42% completed year 12, 18% year 11 and 18% year 10, 22% year 7‐9 Disability benefit: not reported Excluded: having severe intellectual disability or having florid psychosis that prevented the determination of ability to provide informed consent. Lack of fluency in English | |
| Interventions | IPS (N = 73) In addition to receiving treatment as usual, those in the IPS group received service from an employment consultant working according to the IPS model located on site at EPPIC. The employment consultant's job was to meet with clients as soon as possible after randomisation and provide them with an employment service based on the eight principles of the IPS model described above. No details about fidelity, but this study was conducted at the same centre as Killackey 2008 with high‐fidelity scores. Treatment as usual (N =73) Those in the TAU group received all the services that they were eligible for as clients of EPPIC. This included medical review, clinical case management, group programmes (some of which were vocationally oriented) and referral by case managers to offsite agencies (e.g. housing, welfare or employment agencies). In addition, a local Department of Employment and Workplace Relations contracted employment service had an employment consultant on site at Orygen for one half‐day per week, to whom all clients were able to be referred by case managers if this was deemed appropriate | |
| Outcomes | Percentage of participants who obtained competitive employment (only preliminary data after 6 months follow‐up available) Dropouts | |
| Notes | No details about definition of competitive employment Outcome data derived from a systematic review (Bond 2015a) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The participants were allocated using a computer programme for blocked randomisation in random permutated blocks of 4 and 8" |
| Allocation concealment (selection bias) | Low risk | "Randomisation was conducted by the study statistician who was not associated with assessments and treatments. She was the only person aware of the allocation sequence. She provided the group allocation to the study lead who informed the employment consultant and the participant’s case manager of the group to which the participant had been allocated" |
| Blinding of participants and personnel (performance bias) | High risk | The employment consultant and the participant’s case manager were informed about group allocation. Participants could also identify allocation by contents of the programme |
| Blinding of outcome assessment (detection bias) | Low risk | "All effort was taken to keep research assistants (RAs) blinded to study condition. RAs had no contact with the employment consultant, and participants were reminded at the start of each assessment that they were not to let the RA know whether they had been working with the employment consultant or not." |
| Incomplete outcome data (attrition bias) | High risk | 86% follow‐up |
| Selective reporting (reporting bias) | Unclear risk | Only preliminary data were available. Not all outcomes as listed in design article were reported |
| Other bias | Low risk | Supported by Australian Rotary Health; the Australian Research Council (LP0883273); Orygen Youth Health Research Centre; a National Health and Medical Research Council Clinical Research Fellowship (#628884); and University of Melbourne, Faculty of Medicine, Dentistry and Health Sciences Ronald Philip Griffiths Fellowships |
| Methods | Allocation: randomised Design: single centre Duration: 12 months Country: Montreal, Canada | |
| Participants | N = 150 Diagnosis: schizophrenia spectrum disorder (schizophrenia, schizoaffective disorder, schizophreniform disorder, psychosis not otherwise specified), bipolar disorder, or major depression. If their principal diagnosis was one of major depression, were classified as disabled due to mental illness by the provincial welfare system. Included: 59% schizophrenia spectrum and 20% bipolar disorder Setting: Douglas Hospital, a teaching psychiatric hospital with a VR centre Age: 18‐64 years, mean 40.3 years Gender: 62% male Ethnicity: 82% white Substance abuse: 4% alcohol misuse or dependence, 10% drug misuse or dependence Living situation: 22% residential services Marital status: 79% single/never married Employment status: unemployed Working history: 31% competitive employment in past 5 years, 42% paid non‐competitive work in past 5 years Motivation: express interest in competitive employment Education: 43% > 12 years Disability benefit: not reported Excluded: learning disability (IQ < 70), physical or organic handicap that seriously impeded work or did not have a case manager willing to see them at least once per month | |
| Interventions | Supported employment (N = 75) SE specialists helped the clients to (a) define a competitive job corresponding to his or her interests and capabilities; (b) obtain such a job; (c) continue in employment, once a job was obtained; (d) recover from job loss, identifying what went wrong and looking for a new employment opportunity. Fidelity was assessed on 2 occasions using the Supported Employment Fidelity Scale 11 months and 2.5 years after the programme was initiated. The two ratings were consensus ratings between two different pairs of investigators. Both ratings indicated good implementation of IPS. Usual vocational services (N = 75) Clients were given an opportunity to sign up for one of the many vocational services normally available. These included sheltered workshops, creative workshops, a client‐run boutique and horticultural programmes. Job‐finding skills training, as well as psychosocial interventions administered through two day‐treatment centres, were also available. None of these programmes had competitive employment as their immediate goal. In addition, clients could be offered a social integration measure, that is a Québec government programme that offers clients part‐time work in competitive settings, in exchange for a CAD 120 top‐up to their monthly welfare cheque and a free public transport pass. Finally, clients could also be referred to a non‐profit community agency that sought to place clients either in competitive jobs or in government subsidised adapted businesses, in which wages equal or exceed the legal minimum wage but where the majority of jobs are reserved for people who have disabilities. This agency was not integrated with clinical services, nor did it provide ongoing support to clients. | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment ("any paid jobs") Weeks in competitive employment Days to first competitive employment Dropouts | |
| Notes | Jobs were categorised as competitive if:
| |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Stratified randomisation was used, with two factors that were expected to influence vocational outcomes: previous work history (≥ 1 year of continuous work experience at some point in the past, or less) and clinical site. The biostatistician associated with the study generated 16 random assignment sequences" |
| Allocation concealment (selection bias) | Low risk | "The project co‐ordinator prepared an opaque envelope containing the assignment and gave it to the interviewer before the baseline interview" |
| Blinding of participants and personnel (performance bias) | High risk | "Assignment was revealed to both interviewer and participant at the conclusion of the baseline interview" |
| Blinding of outcome assessment (detection bias) | High risk | Interviewers were not masked to group assignment |
| Incomplete outcome data (attrition bias) | Low risk | 17% lost to follow‐up, N = 9 in control group and N = 16 in intervention group. Reasons seem to be similar in both groups. In total 5 moved, 17 refused, 3 had other reasons. ITT analysis used |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | This study was funded by the Canadian Institutes of Health Research, the Quebec Health Research Fund and AETMIS |
| Methods | Allocation: randomised Design: single centre Duration: 12 months Country: Montreal, Québec, Canada | |
| Participants | N = 24 (total sample 160) Diagnosis: severe mental illness. Included: 63% schizophrenia, 33% mood disorder Setting: participants enrolled in supported employment programmes in Montreal Age: mean 32.4 years Gender: 71% male Ethnicity: ‐ Substance abuse: ‐ Living situation: ‐ Marital status: ‐ Employment status: ‐ Working history: ‐ Motivation: wish to obtain a competitive job Education: 46% secondary education, 33% university, 17% Baccalauréat (academic qualification for entrance into university) Disability benefit: ‐ Excluded: zero exclusion | |
| Interventions | SE + CBT (N = 12) Group CBT intervention offered during 8 sessions over the course of 1 month, in order to respect the rapid job search principle of IPS, was developed. The content was tailored to facilitate the learning of skills specific to the work‐place, such as recognising and managing one’s stressors at work, determining and modifying dysfunctional thoughts,overcoming obstacles, improving one’s self‐esteem as a worker, dealing with criticism, using positive assertiveness, finding coping strategies to use at work, negotiating work accommodations and overcoming stigma. SE (N = 12) A SE following the 8 principles of IPS No fidelity measurements reported | |
| Outcomes | Number of participants who obtained competitive employment Number of participants who obtained non‐competitive employment Weeks in competitive employment | |
| Notes | Preliminary results of a subsample Definition of competitive employment: not reserved for people with disabilities, at least minimum wages and full time or part time | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Un essai randomisé contrôlé" (a randomised controlled trial) |
| Allocation concealment (selection bias) | Low risk | No details in article, low according to study author's information |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | Unclear if interviewers were blinded |
| Incomplete outcome data (attrition bias) | High risk | Preliminary results of a sub sample, no dropouts reported |
| Selective reporting (reporting bias) | Unclear risk | There was a slight bias in reporting since the preliminary analyses only focused on some of the measures, not all were analysed |
| Other bias | Low risk | No details about funding source, but they reported no conflicts of interest |
| Methods | Allocation: randomised Design: single centre Duration: 24 months Country: Baltimore, Maryland, USA | |
| Participants | N = 219 Diagnosis: criteria of severe mental illness based on diagnosis, duration of illness and level of disability. Patients were automatically eligible if they received SSI, SSDI or VA disability benefits because of a mental disorder (other than substance abuse only) or if they had a schizophrenia spectrum disorder using DSM IV criteria. Those not meeting these criteria were eligible if they had another axis I disorder (other psychotic, major affective or anxiety disorder) or an extensive prior hospitalisation history. Finally patients were included if they had had a history of a mental disorder for at least the past year, during which they were unable to spend 75% of their time in some gainful activity owing to the mental disorder. Included: 75% psychotic disorder, 25% mood disorders Setting: outpatient psychiatric care from 3 continuous care teams within a university‐run CMH agency serving inner‐city Baltimore Age: mean 41.5 years Gender: 57% male Ethnicity: 75% African American or other minority Substance abuse: 40% substance use diagnosis with current use, 50% with use in past 5 years, 75% with lifetime use Living situation: 52% independent, 24% supported or assisted, 18% with family, 6% homeless Marital status: 62% never married, 34% divorced/separated/widowed Employment status: at least 3 months unemployed Working history: 48% at least 1 job in past 5 years Motivation: not reported Education: 51% high school graduate or GED, 49% did not complete high school Disability benefit: 89% SSDI, SSI or combination Excluded: not reported | |
| Interventions | IPS (N =113) This model focuses on a rapid job search with continued follow‐along support. The IPS programme seeks employment opportunities that are consistent with participants’ preferences, skills, and abilities. Fidelity ratings, completed by the IPS programme developer who served as a consultant to the project, were made twice yearly using the IPS Fidelity Scale. The programme received high ratings of implementation fidelity across all review periods. Psychosocial rehabilitation (N =106) The comparison programme provided an array of services, including evaluation and skills training, socialisation, access to entitlements, transportation, housing supports, counselling and education. Vocational services included in‐house evaluation and training for individuals who staff believed were not yet fully prepared for competitive employment. Training focused on improving specific work readiness skills, such as work endurance, appropriate social interaction in the workplace, and acceptance of supervision. In‐house sheltered work and factory enclave projects were also available. For those ready for competitive employment, the psychosocial programme either provided in‐house assistance in securing employment or referred participants to city‐based rehabilitation or vocational service programmes | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Dropouts | |
| Notes | Definition competitive employment: a job in which the worker earned at least minimum wage and the worker had no contact with disabled workers and at least some contact with non‐disabled workers, and the job had not been set aside for a disabled person. Part of Employment Intervention Demonstration Project (EIDP) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Using pre‐prepared sealed envelopes participants were randomly assigned." No further details |
| Allocation concealment (selection bias) | Low risk | Randomised using pre‐prepared sealed envelopes |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | Employment data (primary outcome) were collected by using an employment form completed by case managers or vocational specialists |
| Incomplete outcome data (attrition bias) | High risk | N = 148 completed study, 26% lost to follow‐up in intervention group and 60% in control group |
| Selective reporting (reporting bias) | High risk | Not all listed outcomes were reported (e.g. quality of life, self‐esteem at follow‐up) |
| Other bias | Low risk | This study was supported by co‐operative grant UD7‐ SM51824 from the Center for Mental Health Services, Substance Abuse and Mental Health Services Administration, Department of Health and Human Services, Rockville, Md, as part of the Employment Intervention Demonstration Project; grant P50‐MH4370 from the National Institute of Mental Health, Rockville; and the Mental Illness Research Education and Clinical Center, Veterans Affairs Integrated Service Network 5, Baltimore. "The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the centre for mental health services, the substance abuse and mental health services administration, the department of health and human services or other employment intervention demonstration project collaborators" Participants received USD 20 for baseline interviews, USD 10 for each of next 2 follow‐up interviews and USD 15 for the 18‐ and 24‐month interviews |
| Methods | Allocation: randomised Design: multi centre Duration: 24 months Country: New York State, USA | |
| Participants | N = 68 Diagnosis: DSM‐III‐R criteria for schizophrenia, schizoaffective disorder or schizophreniform disorder with also one or more additional complicating factors. Setting: the study was conducted at 3 mental health centres, 1 each in an urban, suburban, and rural area of New York State. Participants were selected during an admission to an inpatient service or an acute partial hospital or when they were receiving crisis services for an acute psychotic episode. In total 28% of the participants was in hospital when they entered the study. Age: 18‐45 years, mean 29.8 years Gender: 65% male Ethnicity: 78% white Substance abuse: 80% no history of abuse Living situation: 47% lives with family, 25% supervised without family, 26% unsupervised without family, Marital status: 84%never married, 9% divorced/separated Employment status: 91.2% unemployed, 5.9% sheltered work, 2.9% competitive employed Working history:‐ Motivation:‐ Education: 30% high school graduate, 29% some college, 22% some high school Disability benefit: ‐ Excluded: acutely violent or suicidal people and those with major medical illness or physical addiction requiring immediate medical hospitalisation were excluded until they were stabilised or detoxified. | |
| Interventions | ACT + multifamily group (N = 37) After an initial psycho‐educational workshop for family members only, multifamily groups, each comprising 6 participants and their families, met with two ACT team members every other week for 2 years. The teams were guided by participants’ and family members’ preferences and intentions. One modification was made in the ACT approach: a more gradually paced recovery and rehabilitation concept was adopted from family psychoeducation to ensure the lowest risk of relapse and more consistent development of independent living skills ACT + crisis family intervention (N = 31) Co‐ordination between the team and family members occurred only during crises, without the input of other participants’ family members | |
| Outcomes | Number of participants who obtained competitive employment Number of participants who obtained non‐competitive employment Mental health (PANSS) | |
| Notes | We could not classify this comparison for the network meta‐analyses and direct comparison meta‐analyses No definition of competitive employment described, but they made a distinction between sheltered and competitive employment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants and their families were randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | "Post‐treatment interviews with the project staff failed to detect any bias in assigning participants to treatment conditions" |
| Blinding of participants and personnel (performance bias) | High risk | Personnel and participants were not blinded. They could identify assignment by contents of programme |
| Blinding of outcome assessment (detection bias) | Low risk | "Raters were independent and blind to the treatment condition" |
| Incomplete outcome data (attrition bias) | Low risk | No differences in attrition: three cases in each cohort (6/68) |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | High risk | New York State Alliance for the Mentally Ill, which sponsored the project, and the New York State Office of Mental Health, which provided funding Baseline differences were considered chance effects and were entered as control variables in subsequent analyses. Participants in the intervention condition received care from the same treatment teams that provided services to participants in the control condition. The possibility of clinician bias existed. |
| Methods | Allocation: randomised Design: multi centre Duration: 18 months Country: New York City, New York, USA | |
| Participants | N = 69 Diagnosis: a diagnosis in either the schizophrenia or the mood disorder spectrum. Included: 73% schizophrenia spectrum, 27% mood spectrum Setting: 2 New York state CMH centres , 1 of the 2 service sites was located in an increasingly urbanised suburb of New York City (New Rochelle, Westchester County) and the other in rural New York state (Kingston, Ulster County) Age: 18‐55 years, mean 33.0 years Gender: 70% male Ethnicity: 87% white Substance abuse: 91% none/rare alcohol use, 94% non/rare other substance use Living situation: 36% lived with family member, 64% non family Marital status: 74% never married, 13% separated/divorced Employment status: not employed competitively for the past 6 months Working history: mean months since last job 15, mean number of prior jobs: 6 Motivation: explicit wish to work Education: 34% high school graduate, 21% not high school graduate, 35% some college, 10% college grad Disability benefit: 64% SSI, 49% SSD, 4% SSA Excluded:‐ | |
| Interventions | FACT (N = 37) Family‐aided Assertive Community Treatment consisted of ACT, family intervention and vocational specialists. The vocational specialists were trained by Becker (one of the founders of IPS). Their specific tasks were to: I ) lead 9‐session goal‐setting groups; 2) work with each individual to identify and contact potential employers; 3) work on job development for the entire cohort, to find co‐operative potential employers; 4) coach participants on and off the job site in the initial month or two of employment; 5) provide technical assistance to their team‐mates in job‐coaching; and 6) develop methods for assessing work‐readiness, preparing resumes, and practicing interviewing skills TVR (N = 32) TVR with referral to state VR service often leading to placement in sheltered workshop. Case loads were heavier | |
| Outcomes | Number of participants who obtained competitive employment Weeks in competitive employment Number of participants who obtained non‐competitive employment | |
| Notes | No definition of competitive employment described, but they made a difference between type of employment (sheltered employment, supported employment, vocational training, competitive employment) No IPS fidelity measurements reported Part of Employment Intervention Demonstration Project (EIDP) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | Clinicians completed employment trackings form for each subject |
| Incomplete outcome data (attrition bias) | Unclear risk | No details about attrition rate |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | Supported by grant R18 SM 47642 from the National Institute of Mental Health |
| Methods | Allocation: randomised Design: multi centre Duration: 2‐3 years, average follow‐up was 26 months Country: New York City, New York, USA | |
| Participants | N = 48 Diagnosis: severe mental illness as determined by the State of New York Office of Mental Health. Included: 73% schizophrenia, 4% schizoaffective disorder, 23% mood disorder Setting: 2 CMH centres. Both agencies serve predominantly people from minority groups and provide a comprehensive range of services: housing, psychiatric, community support, day treatment, psychosocial, and integrated vocational services (including SE) Age: mean 37.6 years Gender: 55% male Ethnicity: 68% African American, 16% Hispanic Substance abuse: 9% current alcohol use, 30% lifetime alcohol use, 7% current drug use, 53% lifetime drug use Living situation: ‐ Marital status: 86% never married Employment status: not currently competitively employed Working history: all participants had at least one unsatisfactory job ending. Mean time since last job: 40 months Motivation: desire for competitive work Education: mean: 11 years of education Disability benefit:‐ Excluded:‐ | |
| Interventions | SE + cognitive training (N = 25) The Thinking Skills for Work Program was designed as an adjunct to SE. It was divided into 4 component parts and was delivered by a cognitive training specialist. Clients were engaged in 24 hours of computer‐based cognitive exercises (Cogpack v6) providing practice across the broad range of cognitive functions, including attention and concentration, psychomotor speed, learning and memory, and executive functions. Sessions required 45–60 minutes to complete, with clients usually completing 2–3 sessions per week for a total duration of about 12 weeks. Participants received performance scores in order to reinforce performance progress. The cognitive training specialist, the employment specialist, and the client met together to plan the job search, based on the client’s preferences. Then, a meeting was held to review the client’s job interests, to evaluate his or her cognitive strengths and gains made in the computer cognitive training exercises, and to consider possible support to compensate for cognitive impairments that could compromise work performance. The cognitive training specialist and the employment specialist met regularly to discuss job supports. Supported employment (N = 23) Both sites had SE programmes that broadly adhered to evidence‐based definitions of the practice. Both programmes had zero exclusion criteria, no PVT, minimal prevocational assessment, emphasis on rapid job search for competitive employment in integrated community settings, attention to consumer preferences with respect to jobs sought and disclosure of psychiatric disability, and provision of follow‐along supports to facilitate job retention Fidelity was rated with the Supported Employment Fidelity scale. The first 2 study authors conducted the fidelity assessments with sites receiving ratings of "fair" (score 60) and "good" (score 66) implementation | |
| Outcomes | Number of participants who obtained competitive employment Weeks in competitive employment Mental health (PANSS) Hospital admissions (no usable data) Dropouts | |
| Notes | Competitive work was defined as jobs paying minimum wage or higher, owned by the individual, not set aside for a person with a disability, and integrated in the community | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Assignment to the programmes was conducted on the basis of a computer‐generated randomisation list" |
| Allocation concealment (selection bias) | Unclear risk | "Individuals were randomly assigned within each centre." No further details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by content of programme |
| Blinding of outcome assessment (detection bias) | High risk | Vocational outcomes were assessed through regular contacts with clients and vocational staff members. No details about blinding but unlikely |
| Incomplete outcome data (attrition bias) | High risk | 48 clients were randomised (25 in intervention and 23 in control group). Soon after randomisation 2 clients (1 in intervention group, 1 in control group) withdrew consent from the study due to serious medical conditions, and 1 client (control) died. One client left vocational services and was lost to follow‐up within a month after randomisation. Twelve‐month employment data were available on 32 (67%) clients, rates of follow‐up were comparable between the 2 groups. No details about attrition rate after 2‐3 years |
| Selective reporting (reporting bias) | Low risk | All listed outcomes are reported |
| Other bias | Low risk | Supported by grant from the Center for Rehabilitation and Recovery, Coalition of Behavioral Health Agencies, Inc., New York Clients recruited for the project at CMHC A differed in a number of background and baseline characteristics from clients recruited from CMHC B. Because of these site differences, they included site as an independent variable. No significant differences between intervention and control group |
| Methods | Allocation: randomised Design: single centre Duration: 24 months Country: New York, New York, USA | |
| Participants | N = 34 Diagnosis: severe mental illness as defined by the New York Office of Mental Health. Included: 62% schizophrenia, 24% depression/anxiety, 6% bipolar disorder Setting: a VR programme affiliated with an urban medical centre (Mount Sinai Hospital). All study participants were in a combined vocational and day treatment programme that focused on work and accepted only consumers with work goals. Available services included case management, pharmacological treatment, day treatment activities, housing support services, volunteer work at the site, paid internships at the hospital, and supported employment. Age: ≥ 18 years, mean age 44.0 years Gender: 59% male Ethnicity: 62% African American, 15% Hispanic Substance abuse: 26% current alcohol use disorder, 26% current drug use disorder Living situation:‐ Marital status: 76% never married Employment status: unemployed Working history: history of unsatisfactory job ending, defined as either being fired from a job or quitting a job prior to securing another job. Mean months since last job: 65 Motivation: interest in obtaining work Education: mean years of education: 12 years Disability benefit: ‐ Excluded:‐ Other: 74% 1 or more medical co‐morbidities. Most frequent: hypertension (29%), diabetes (19%), high cholesterol (19%), hepatitis C (15%) | |
| Interventions | VR + cognitive training (N = 18) Participants were engaged in 24h of computer‐based cognitive exercises (Cogpack), which provided practice across the broad range of cognitive functions.Sessions required 45‐60 min, with consumers usually completing 2 sessions per week for about 16 weeks. Participants received performance scores to reinforce them. In addition, they participated in a weekly group. Topics in the group included the role of cognition in job performance and problem solving about compensatory strategies for dealing with common challenges on the job, such as remembering tasks, remaining focused, and improving work speed. Employment specialists were asked to attend the group if their consumer was having job performance difficulties. Plus VR: see below. VR only (N = 16) The vocational programme provided 2 types of services: internships and supported employment, each served by a separate team of vocational staff. The internship programme was an innovative VR model that provided work experience in time‐limited (up to 9 months), part‐time (up to 15 h), integrated (at the Mount Sinai Hospital) jobs, paying predominantly competitive wages or higher, depending on the participants’ ability to perform the job duties. Upon completing an internship work experience, consumers could choose another internship experience or SE SE was available to participants who had satisfactory performance in an internship job. The SE programme adhered to most of the principles, including integration of clinical and vocational services, matching jobs to consumers’ preferences, skills, and experiences, and ongoing, time‐unlimited support from employment specialists, who carried an average caseload of 25 consumers. The programme deviated from the zero exclusion and rapid job search principles of SE because consumers were encouraged to complete an internship job before enrolling in SE. In addition, job development and job support were provided by different vocational staff. No fidelity measurements described | |
| Outcomes | Number of participants in competitive employment Weeks in competitive employment Mental health (PANNS) | |
| Notes | SAMHSA definition of competitive employment used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomised by the project co‐ordinator using a computer‐generated randomisation programme" |
| Allocation concealment (selection bias) | Unclear risk | "Treatment assignment was not known in advance by study personnel" |
| Blinding of participants and personnel (performance bias) | Unclear risk | Participants and personnel could identify given intervention by content of programme |
| Blinding of outcome assessment (detection bias) | Unclear risk | Cognitive and Psychopathology assessments were conducted by an evaluator who was blind to treatment assignment. Employment activities were tracked weekly. No further details |
| Incomplete outcome data (attrition bias) | High risk | 32 (94%) completed the 3‐month assessment, and 25 (74%) were followed up for 24 months. No further details. No reasons of missing data described |
| Selective reporting (reporting bias) | Low risk | All listed outcomes are reported |
| Other bias | Low risk | Funder: New York State Office of Mental Health |
| Methods | Allocation: randomised Design: multi centre Duration: 30 months Country: the Netherlands | |
| Participants | N = 151 Diagnosis: severe mental illness. Included: 58% schizophrenia/psychotic disorder, 13% affective disorder, 22% personality disorder, 17% developmental disorder Setting: 4 regional CMH care divisions targeted at adult persons with severe mental illness Age: 18‐65 years, mean 34.9 years Gender: 74% male Ethnicity: 96% Dutch nationality Substance abuse: 11% drug (ab)use Living situation: 64% independent, 17% with family, 11% sheltered Marital status: 9% married Employment status: unemployed Working history: 61% paid employment in past 5 years, 53% competitive employment in past 5 years Motivation: explicit wish for competitive employment Education: 21% elementary school, 44% high school, 26% vocational education, 6% university degree Disability benefit: 58% disability benefit, 39% social benefit Excluded: paid work at study entrance, full‐time hospitalisation, engagement in another professional VR trajectory and participant in another study with conflicting interests | |
| Interventions | IPS (N = 71) IPS was implemented according to protocol, with employment specialists added to multidisciplinary CMH teams with a staff:client ratio varying from 1:20 to 1:30. The majority of mental health services and treatment offered by these outpatient teams were provided in the community, employing assertive outreach. Team staff consisted of psychiatrists, psychologists, community psychiatric nurses and other personnel, for example, rehabilitation workers. In all services IPS workers assisted people in getting regular jobs, offered follow‐along support, spent most of the time in the community and operated in close collaboration with the other CMH team members. Model fidelity of IPS was evaluated at 3 time points using the Quality of Supported Employment Implementation Scale. Several research team members were trained in IPS fidelity assessment at Dartmouth Center. Each assessment was done by two researchers according to protocol; all scores were based on consensus. Two of the four participating agencies scored “good‐high” on fidelity in every assessment, and two scored “moderate.” TVR (N = 80) In general these services offer a stepwise vocational trajectory, putting much stronger emphasis on lengthy assessment of individual competencies and on connecting to prevocational activities such as voluntary jobs before placement in regular jobs. The TVR staff did not participate in the mental health teams. | |
| Outcomes | Number of participants who obtained competitive employment Number of participants who obtained non‐competitive employment Days to first competitive employment Weeks in competitive employment Mental health (MHI‐5) Quality of life (MANSA) Hospital admissions Dropouts | |
| Notes | Definition competitive employment: a paid job in a company or organisation in the regular labour market, against prevailing wages, not set aside for persons with a disability, that is, in an integrated work setting (one day or more) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A stratified block randomisation procedure was used, with site and employment history (having had paid employment in the past 5 years yes or no) as stratification factors" |
| Allocation concealment (selection bias) | Low risk | "Randomisation was performed by an independent agency that sent the randomisation outcomes to the research team and the local research co‐ordinators at the same time" |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by content of programme |
| Blinding of outcome assessment (detection bias) | Low risk | "Interviewers were trained by the research team and were blind to the conditions" |
| Incomplete outcome data (attrition bias) | High risk | Response at 30 months was 57%. IPS and TVR arms did not differ in response/non‐response ratio nor in non‐response reasons. Reasons described. ITT analyses carried out. In case of the primary outcome they gathered data even for people who dropped out, so there was only one missing value on the primary outcome variable (employment) regarding the 30‐month period |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Unclear risk | Supported by grants from UWV (national authority on employee insurances) and ZonMw (national funding of health research and development). Other sponsors were Trimbos Institute, UMCG‐RGOc (University Medical Center Groningen) and Internal funding UMCG. Each participant received EUR 10 per completed interview |
| Methods | Allocation: randomised Design: single centre, multi‐arm Duration: 24 months Country: Hartford, Connecticut, USA | |
| Participants | N = 204 (N = 135 included in this review) Diagnosis: severe mental illness, as defined by the State of Connecticut Department of Mental Health and Addiction Services (DSM IV Axis I diagnosis or borderline personality disorder and severe impairment in psychosocial functioning or self‐care) Included: 52% schizophrenia, 22% schizoaffective disorder, 6% bipolar disorder, 18% major depression Setting: CMH centre Age: mean 41.4 years Gender: 61% male Ethnicity: 44% African American, 31% Hispanic, 23% white Substance abuse: 12% alcohol use disorder, 19% drug use disorder Living situation: not reported Marital status: 70% never married Employment status: lack of competitive employment Working history: 36% competitive employment in past 5 years, 22% non‐competitive or sheltered work in past 5 years Motivation: desire for competitive work Education: 54% less than high school Disability benefit: not reported Excluded: not reported | |
| Interventions | IPS (N = 68) Employment specialists serve on clients’ treatment teams alongside other members of the team. Each employment specialist provides the full range of vocational services to each client, including engagement in services, identifying job interests and vocational assessment, job finding, and job support. IPS uses assertive outreach, based on the ACT case‐management model for severe mental illness, to deliver most vocational services in clients’ natural settings in the community rather than at mental health or rehabilitation agencies. Fidelity to the IPS model was evaluated yearly by means of the IPS Fidelity Scale. Comparisons of the total fidelity score and the three sub scales indicated high fidelity (70/75). Psychosocial rehabilitation program (N = 67) The PSR program incorporated transitional employment into its vocational rehabilitation approach. Clients participated in a series of preparatory training activities, followed by transitional employment jobs and help them obtaining competitive work. In addition, the PSR program offered a drop‐in centre, skills training and support groups, recreational outings, and residential services. Overall, a survey suggested that the services and program philosophy of the PSR program in this study were typical of other PSR programs operating in the state of Connecticut during the time of the study. It should be noted that it was not certified by the International Center for Clubhouse Development. Standard services (N = 69)* Clients who were randomly assigned to standard services met with the vocational services coordinator and then were assigned to the program of their choice. This condition involved access to all other vocational services in Hartford for clients with severe mental illness, most of which were provided by one of two programs that contracted directly with the Connecticut Department of Mental Health and Addiction Services: a supported employment program located off‐site from the mental health centre (standard–supported), and a vocational program In which clients worked in jobs paying sub minimum wage or competitive wages in supervised janitorial enclaves in the community, fulfilling contracts obtained by that program (standard– enclave). Clients in standard services were also eligible to receive services from the Connecticut Bureau of Rehabilitation Services. * not included in this review because we could not classify this intervention | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Weeks in competitive employment Days to first competitive employment Mental health (PANNS) (no usable data) Dropouts | |
| Notes | Defintion of competitive employment: paid competitive wages, job in an integrated setting in the community (i.e. afforded regular contact with nonclients), contracted by the client (i.e. not filled at the discretion of the vocational programme). Part of Employment Intervention Demonstration Project (EIDP) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Clients were randomly assigned on the basis of a computer‐generated randomisation list, stratified by work history (competitive work in past 5 years or not), ethnicity, and gender" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | "Interviewers were not blind to vocational programme assignment" |
| Incomplete outcome data (attrition bias) | Low risk | Of the total sample 81% completed the 24‐month interview. Vocational data were missing for 6 participants; N = 3 IPS; N = 1 PSR and standard services N = 2. ITT analysis performed |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | Low risk | This project was one of eight controlled trials of VR programmes, supported by co‐operative #UD7 SM51818 from the US Department of Health and Human Services (DHHS) SAMHSA, Center for Mental Health Services (CMHS) as part of the Employment Intervention Demonstration programme (EIDP). Additional support was provided by National Institute of Mental Health (NIMH) Grants MH00842 and MH56147. |
| Methods | Allocation: randomised Design: single centre Duration: 18 months Country: Los Angeles, California, USA | |
| Participants | N = 69 Diagnosis: recent onset of psychotic illness with the beginning of the first major psychotic episode occurring within last 2 years, a diagnosis of schizophrenia or schizoaffective disorder mainly schizophrenic subtype. Included: 83% schizophrenia, 17% schizoaffective disorder. Mean total time ill 24.6 months Setting: recruited from a variety of local psychiatric hospitals and psychiatric clinics and through referrals from the UCLA outpatient service. All participants were receiving outpatient psychiatric treatment at UCLA aftercare Research Program Age: 18‐45 years, mean 25.2 years Gender: 67% male Ethnicity: 29% white, rest Asian/Pacific, black or Hispanic Substance abuse: no drug abuse or alcoholism in 6 months prior to hospitalisation, no evidence that substance abuse will be a prominent factor in course of disease Living situation: ‐ Marital status: 93% single Employment status: ‐ Working history: ‐ Motivation: interest in resume work or school Education: mean 13.2 years Disability benefit: 1/4 were receiving disability funds Excluded: substance abuse, neurological disorder, premorbid mental retardation, no contraindication for risperidone | |
| Interventions | IPS + Workplace Fundamentals Module (N = 46) The option of supported education was integrated with SE. IPS was combined with a group skills training approach, Workplace Fundamentals Module (WFM), to enhance return to regular school or competitive employment. The IPS worker facilitated a rapid search for schooling or employment, used assertive outreach, and gave ongoing vocational support. The same clinical team provided case management and psychiatric services for all participants. They adapted supported education to the IPS principles such that the whole programme met the standards for IPS fidelity. WFM is a group skills training approach that has the complementary goal of teaching social and problem solving skills necessary to keep a job. Each week for 6 months the participants were scheduled to attend two 75 min groups on the same day followed by 12 months of sessions on a fading frequency scale. The IPS worker would reinforce material from group WFM sessions by using it in the context of IPS meetings. Brokered VR (N = 23) Referrals to traditional VR services at separate agencies. The individual case manager discussed the range of options with each participant and agreed upon appropriate directions. They participated in skills training groups, but the groups did not focus on work settings and work skills. Their skills training included medication management training and communication skills training using methods that were similar to WFM | |
| Outcomes | Percentage of participants who obtained competitive employment Dropouts | |
| Notes | Outcome data derived from a systematic review (Bond 2015a) No IPS fidelity scores reported No further description of competitive employment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were randomly assigned in a 2/3 vs 1/3 ratio" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by contents of programme |
| Blinding of outcome assessment (detection bias) | High risk | No details |
| Incomplete outcome data (attrition bias) | High risk | 74% follow‐up 10 lost to follow‐up in intervention group and 8 in control group |
| Selective reporting (reporting bias) | Unclear risk | No full report available |
| Other bias | Unclear risk | Funding source not described |
| Methods | Allocation: cluster‐randomised Design: 10 clusters, 6 intervention and 4 control Duration: 1 year Country: London, UK | |
| Participants | N = 1037 Diagnosis: 54% psychosis, 21% depression/anxiety, 9% bipolar disorder Setting: 10 CMH teams of a large London Mental Health Trust Age: > 16 years, 72% ≥ 35 years Gender: 54% male Ethnicity: 63% white, 18% black Substance abuse:‐ Living situation: 90% living in the community Marital status: 57% single Employment status: unemployed Working history: 71% had been in open employment in the past Motivation:‐ Education:‐ Disability benefit:‐ Excluded: men > 65 years and women > 60 years (normal retirement age) were excluded | |
| Interventions | Vocational staff training (N = 645) Three structured 1‐h seminars by a Consultant Clinical Psychologist specialising in employment issues and a Work Placement co‐ordinator. The seminars supplemented by a written handbook, addressed vocational assessment, access to work and education and vocational planning/intervention for longer term, unemployed CMH team participants. The second covered the best ways to match individuals' needs and wishes with the opportunities available. The third was about incorporating work and education targets as a routine in the care plans. Team members were also supplied with a directory of work and educational opportunities and services in the local area. Seminars were held at weekly intervals and were completed for all teams within 6 weeks of randomisation date. Standard care (N = 392) High quality standard CMH team care | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Hospital admissions Dropouts | |
| Notes | Open/competitive employment, no definition but they distinguish sheltered work, voluntary work, education or training, work‐related activity and open employment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was at the level of the teams rather than the participant (cluster randomisation). Estimating an intra‐cluster co‐efficient of 0.02. Teams were randomised to control or intervention by an independent statistician. Recruitment before randomisation. They used 2 boroughs and teams were randomised within each borough to minimise geographical variations. Analyses without adjustment for cluster design, because the ICC was 0.00148, which leads to a design effect of 1.01. |
| Allocation concealment (selection bias) | Low risk | Randomisation was concealed |
| Blinding of participants and personnel (performance bias) | High risk | Personnel could identify given intervention by content of programme. Participants not described |
| Blinding of outcome assessment (detection bias) | High risk | The researchers could not be blinded to the intervention received because data had to be recorded from team case notes |
| Incomplete outcome data (attrition bias) | Low risk | Follow‐up data were obtained on 994 participants (95.8%). Records were inaccessible for 43 participants (27 intervention, 16 control). Of the 994 participants with follow‐up data, for 20 the keyworkers could not confirm vocational activity (15 intervention, 5 control). Vocational outcome data were obtained at 1 year on 974 participants (94% of the total sample). All analysis was carried out by the team and condition to which the subject was initially allocated. No loss of clusters reported |
| Selective reporting (reporting bias) | Low risk | All listed outcomes are reported |
| Other bias | Low risk | London Region Responsive Funding Programme At baseline the groups were comparable in terms of demographic and clinical characteristics. Only significant differences at baseline between individuals: ethnicity and patient status. These differences were controlled for in the final stratified analysis. Adjustment for baseline patient status and ethnicity showed that the initial differences did not effect outcome |
| Methods | Allocation: randomised Design: single centre Duration: 6 months Country: Tokyo, Japan | |
| Participants | N = 37 Diagnosis: primary diagnosis of either schizophrenia, mood disorder or neurotic disorder as defined by International Classification of Diseases (ICD)‐10. ≥ 5 contacts with the community support centre in the last year. High psychiatric service utilisation in last 2 years (≥ 2 or more hospitalisations, ≥ 100 inpatient days, ≥ 3 psychiatric emergency room visits, or ≥ 3 months no‐show to outpatient clinics). Low level of social functioning in the previous year as indicated by a score of ≤ 50 on the Global Assessment of Functioning Scale. Mean illness duration: 18 years Setting: a small community support centre administered by the city government in a suburban area near Tokyo. The centre staff provided broker‐style case management services. In close proximity to the centre were 2 other programmes: an ACT team funded through the national government and a Clubhouse operated by a private nonprofit organisation. These three organisations engaged in significant collaboration with each other Age: 18‐59 years, mean 40.6 years Gender: 49% male Ethnicity: ‐ Substance abuse: ‐ Living situation: 62% living with their family, 24% living alone Marital status: ‐ Employment status: not currently competitively employed Working history: 70% competitive employment before onset of illness, 35% after onset Motivation: ‐ Education:‐ Disability benefit:‐ Excluded: primary diagnosis of mental retardation, dementia, substance/alcohol abuse or personality disorder. No prior enrolment in supported employment | |
| Interventions | IPS (N = 18) IPS employment specialists received 4 months of training from a team of IPS trainers. The employment specialists also received on‐the‐job supervision from 2 senior psychiatrists. The IPS programme adhered to IPS model standards. Employment specialists assessed each participant’s work preferences, past work experiences, current skills, and tolerance for type and intensity of job demands. Together, participants and specialists searched for competitive jobs. Specialists provided time‐unlimited support before, during, and after periods of employment. The overall fidelity rating was 68 out of 75, which is considered good implementation. TVR (N = 19) TVR services at the community support centre. The programme consisted of PVT in various work groups in a simulated environment intended to help prepare participants for paid employment | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Weeks in competitive employment Dropouts | |
| Notes | The fidelity assessment was conducted by the first study author Competitive employment was operationally defined as a job paying at least minimum wage (as established in Japanese law), with ≥ five work h/week, for which anyone can apply, and not controlled by a service agency | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by content of programme |
| Blinding of outcome assessment (detection bias) | High risk | "The research interviewers were not blinded to study condition." The employment outcomes were assessed through self‐report and cross‐checked through chart records, which were maintained by support centre staff, who had day‐to‐day contact with participant |
| Incomplete outcome data (attrition bias) | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | Low risk | Supported by the Ministry of Health Labour and Welfare, Japan (Health and Labour Sciences Research Grant 200733005) |
| Methods | Allocation: randomised Design: single centre Duration: 12 months Country: Bedford, Massachussettes, USA | |
| Participants | N = 89 Diagnosis: clinically stable veterans with co‐morbid psychiatric and substance use disorders: 56% major depression, 33% bipolar disorder, 25% panic disorder, 26% other anxiety disorder Setting: VA healthcare Services Age: < 56 years, mean 45.2 years Gender: 100% male Ethnicity: 78% white Substance abuse: current or lifetime drug or alcohol abuse or dependence with active substance abuse in the prior 90 days. Included: 88% alcohol abuse, 56% drug abuse Living situation: homeless Marital status: 26% never married Employment status: Working history: history of at least 1 day of competitive employment within the last 3 years Included: 56% full‐time employment in prior 3 years Motivation: a stated goal of returning to competitive employment within 6 months Education: mean 13 years Disability benefit: 29% Excluded: an average of no more than 4 h of clinical appointments per week, any legally mandated treatment that would make employment impossible. Did not meet criteria for schizophrenia, schizoaffective disorder, or unspecified psychosis | |
| Interventions | Transitional work experience (N =50) The Bedford CWT programme offers TWE placements within companies in the community, as well as a few placements at the medical centre. Ninety percent of TWE placements exist in integrated, real‐work settings at which programme participants are doing the same work as non‐participants working alongside them. Job Placement services (N = 39) Participants assigned to job placement services were given contact numbers for 2 state VR specialists and were assisted in arranging the first appointment | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Weeks in competitive employment Days to first competitive employment Dropouts | |
| Notes | Participants who worked competitively at least 1 week | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify programme assignment |
| Blinding of outcome assessment (detection bias) | Unclear risk | All data were collected by research assistants who were independent of the intervention staff. No details about blinding |
| Incomplete outcome data (attrition bias) | High risk | 2 participants of the intervention group disappeared after the baseline evaluation. 10 of those assigned to the control condition subsequently entered the intervention services during the 12‐month follow‐up period. All stated that they entered the intervention services in order to obtain work because they felt that the control services were not helpful. Follow‐up data for participants assigned to intervention and who subsequently entered the intervention services were censored at the point of entry into intervention |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | Low risk | This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, and the VA New England Mental Illness Research Education and Clinical Center |
| Methods | Allocation: randomised Design: multi centre Duration: 30 months Country: Massachussetts, USA | |
| Participants | N = 177 Diagnosis: bipolar disorder, major depression, or schizophrenia and its related disorders as defined by the DSM‐IV, included: 52% schizophrenia Setting: Genesis Club, an ICCD‐certified clubhouse and The PACT at Community Healthlink Age: ≥ 18 years, mean 38.1 years Gender: 55% male Ethnicity: 79% white Substance abuse: 35% substance abuse disorder Living situation: not reported Marital status: not reported Employment status: not competitively employed at time of intake Working history: 57% had a standard job in 5 years before study Motivation: they did not screen on work interest, but 70% interested in work Education: 63% high school diploma Disability benefit: not reported Excluded: severe mental retardation (IQ > 60) or previously participated in either programme | |
| Interventions | Clubhouse (N = 89) A clubhouse run collaboratively by members and staff that emphasised mutual support, self‐determination, and therapeutic benefits of voluntary and paid work. Various rehabilitation services, including case management, a work‐ordered day, supported education, supported employment, transitional employment, and weekend social activities, were continuously available to clubhouse members, but attendance was not mandatory. The ICCD certified this programme and ensured fidelity to the standards for Clubhouse programmes PACT (N = 88) PACT was a mobile team that provided out‐of‐office clinical care, assistance with housing and daily living, substance abuse intervention, and help in finding meaningful activities or employment. Fidelity was verified annually. In both programmes, vocational staff who had training in SE worked closely with other staff to ensure rapid placement into mainstream jobs not reserved by employers for individuals with disabilities. On‐the‐job training and support were provided whenever needed. Clubhouse members could also work transitional employment jobs, which were above‐minimum‐wage jobs reserved for the clubhouse by a consortium of local employers. both programmes maintained acceptable fidelity over the 4‐year research period to SE model standards as assessed by a second SE expert | |
| Outcomes | Percentage of participants who obtained competitive employment Number of weeks in competitive employment Dropouts | |
| Notes | Part of Employment Intervention Demonstration Project (EIDP) Definition competitive employment: all jobs lasting at least 5 days that met the US Department of Labor’s definition of competitive employment: mainstream, integrated work paying at least minimum wage | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomly assigned to one of the two conditions by picking a card from a hat" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by content of programme |
| Blinding of outcome assessment (detection bias) | High risk | "Staff at each programme tracked all jobs acquired by their participants, many of which were obtained with assistance from the respective agencies. Other employment data were self‐reported to programme staff or the interviewers" |
| Incomplete outcome data (attrition bias) | High risk | N = 167 of 177 (94%) participants were followed up after 24 months: 83 Clubhouse and 84 PACT. After 127 weeks, 72 Clubhouse and 76 PACT participants remained active in the project (148 of 177 participants = 84%) Reasons mentioned |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Unclear risk | This study was made possible by co‐operative grant UD7‐SM‐51831 from the Center for Mental Health Services as part of the Employment Intervention Demonstration Program. The views expressed in this article are solely the responsibility of the authors and do not necessarily represent the official views of any agencies or collaborators. Editor’s Note (Psychiatric Services): The papers by Macias and colleagues and by Schonebaum and coworkers were submitted independently a year apart and reviewed separately. Neither set of authors knew of the others’ efforts. The two articles used different methods and a different choice of variables but came to the same overall conclusion. Macias present the independent assessment of evaluators, whereas Schonebaum offer the perspective of researchers connected to Fountain House, which created the Clubhouse model. Each validates findings of the other, turning this coincidence into what we think is an interesting lesson. |
| Methods | Allocation: cluster‐randomised Design: multi‐arm (3), multi centre (9) Duration: 3 months Country: Hong Kong, China | |
| Participants | N = 97 Diagnosis: schizophrenia, no less than 1 year cumulative hospitalisation Setting: 9 community‐based, staffed residential facilities for ex‐mentally ill people. Participants were recruited from halfway houses and sheltered workshops Age: between 18‐50 years, mean 35.7 years Gender: 62% male Ethnicity: Hong Kong Chinese, who spoke Cantonese, not English, 98% of Hong Kong residents are Chinese Substance abuse: ‐ Living situation: staffed residential facilities Marital status: ‐ Employment status: unemployed, mean duration of unemployment 41 months Working history: eligibility criteria: previous occupation: blue collar, low‐level clerical, or service industry Motivation: willingness to participate in a work‐related social skills programme Education: no less than 5 years of primary school and no more than 5 years of secondary school, 30% finished primary school, 29% F1‐F3 (grade 7‐9), 35% F4‐F5 (grade 10‐11) Disability benefit: ‐. Excluded: learning disability | |
| Interventions | Social skills training group (N = 26)* Hierarchical stages of learning were established based on a foundation of basic social skills and basic social survival skills followed by core work‐related skills, including those related to job securing and job retaining. The programme consisted of 10 weekly group sessions lasting 1.5‐2 h, with approximately 6‐8 members in each group. Each training group was facilitated by a trained occupational therapist assisted by an untrained welfare worker experienced in working with this client group. Social skills training group with follow‐up contacts (N = 30)* Received the social skills training plus follow‐up contact with group members and the trainer for 3 months gathered at a monthly meeting conducted by one of the occupational therapists who had run the training groups. These occasions were not as structured as the programme itself, and participants were encouraged to share their experiences of job hunting and job keeping. Control group (n = 41) Received standard psychiatric care on an outpatient basis | |
| Outcomes | Percentage of participants who obtained competitive employment | |
| Notes | *We merged the 2 social skills training groups together for the analyses 'Gainfully employed' seems to be competitive because of the job types reported: caretaker, security guard, waiter, junior clerk | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomisation was achieved by randomly assigning each of the 9 residential facilities to one of the three group conditions" Unclear if participants were recruited before or after randomisation. Design effect not reported |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | Low risk | "All participants were blind to research design. Participants did not know that there were groups with and without follow‐up." |
| Blinding of outcome assessment (detection bias) | Low risk | "The raters were blind to study design and the group status of the participants" |
| Incomplete outcome data (attrition bias) | Unclear risk | No details, but big numbers are unlikely because of short follow‐up |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Unclear risk | No details about study funding |
| Methods | Allocation: randomised Design: multi‐arm, multicentre Duration: 39 months for both intervention groups, 15 months for the control group Country: Hong Kong, China | |
| Participants | N = 189 Diagnosis: severe mental illness (operationally defined as schizophrenia, schizoaffective disorder, bipolar disorder, recurrent major depression, or borderline personality disorder); at least 2 years of major role dysfunction; medium–high functioning and free from serious role dysfunction for the past 3 months Included: 77% schizophrenia Setting: 2 non‐government organisations and 3 day hospitals in Hong Kong Age: mean 34.9 years Gender: 49% male Ethnicity: ‐ Substance abuse: ‐ Living situation: ‐ Marital status: ‐ Employment status: unemployed Working history: 91% employment history Motivation: desire to work Education: 77% secondary education Disability benefit: ‐ Excluded: memory impairment, learning disorder, and neurological or medical illness that would preclude their working or participation in assessments | |
| Interventions | IPS (N = 65) A single‐minded focus on competitive employment; eligibility for services based solely on client choice, with no exclusion on the basis of work readiness, substance use problems, lack of motivation, treatment non‐compliance and so on; rapid job search upon programme admission using the ‘place then train’ approach; attention to client preferences in the job search, rather than dependence on job availability; close integration between the employment services and the mental health treatment team; ongoing, individualised support and job training after clients obtained employment; systematic benefits counselling; and consultation with employer or job supervisor including advocacy accommodations. IPS fidelity scores ranged from 66‐68 out of 75 (88%–91%) Integrated SE (N = 58) The integrated SE programme combined IPS and WSST. The main difference with IPS is that it was enhanced by 10‐session WSST. The social skill training was provided to integrated SE participants before obtaining employment. A problem‐solving approach was used to help participants handle interpersonal conflicts throughout the follow‐up period. The IPS fidelity scores ranged from 65‐68 out of 75 (87%–91%). TVR (N = 66) TVR participants received comprehensive vocational assessments and pre‐vocational training conducted in the VR centres. Vocational assessments included work samples, vocational interest exploration, and situational vocational assessments. After the establishment of participants’ baseline work performance, pre‐vocational training on entry‐level job tasks were provided in order to help them develop specific job skills and work habits. The participants were placed in a sheltered environment in various work groups such as clerical training, computer training, and cleaning training. The aim of the workshop‐based training was to promote the participants to sheltered workshop or competitive employment. | |
| Outcomes | Percentage of participants who obtained competitive employment Weeks in competitive employment Quality of life (PWI) Dropouts | |
| Notes | Success in competitive employment was defined as having continuously worked in the job for at least 2 months for at least 20 h/week Data for the TVR group were available up to 15 months. They did not collect further follow‐up data due to the limited improvement in vocational and/or non‐vocational outcomes. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The participants were randomly assigned using SPSS |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | "The employment specialists were not blind to the treatment assignment of the participants." Participants could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | Low risk | "Assessments were conducted by an independent, trained, and blind assessor who was a registered occupational therapist" |
| Incomplete outcome data (attrition bias) | High risk | N = 85 (69%) completed the follow‐up assessment at 39 months N = 44/58 integrated SE participants and N =41/65 IPS participants. 54 TVR participants (81.8%) completed the 15‐month follow‐up assessment. ITT analyses were conducted on the entire randomised sample (N = 189) |
| Selective reporting (reporting bias) | Low risk | All listed outcomes are reported |
| Other bias | Low risk | This study was funded by a grant from the Health Services Research Committee (HHSRF Project No. 03040031) of the Hong Kong Government |
| Methods | Allocation: randomised Design: single centre Duration: 12 months Country: San Diego, USA | |
| Participants | N = 58 Diagnosis: 40% schizophrenia and 60% schizoaffective disorder Setting: CMH clinic Age: ≥ 45 years, mean 51.0 years Gender: 64% male Ethnicity: 60% white Substance abuse: 22% substance/alcohol use during study Living situation: ‐ Marital status: ‐ Employment status: unemployed Working history: 79% without significant paid work in 2 years, but 86% had once worked at least 12 months continuously, mean years since last job: 7 Motivation: stating a goal of working Education: mean 12.4 years Disability benefit: mean monthly disability entitlement income USD 830 Excluded: substance abuse/dependence within 30 days, history of head injury with loss of consciousness > 30 min, mental retardation, or neurological disorders | |
| Interventions | IPS (N= 30) Participants received manualised SE from an employment specialist whose maximum caseload was 25. IPS emphasises competitive work, integrated mental health and SE services, any client can participate, rapid job searching, service‐users' preferences, time‐unlimited follow‐along support, benefits counselling, and providing services in community settings. IPS fidelity ratings improved from “fair” to “good” over the study. “High” fidelity could not be achieved due to study design (only schizophrenia/schizoaffective clients included; study duration was 1 year; only 1 employment specialist) TVR (N = 28) Participants were referred to the Department of Rehabilitation for orientation, intake, and eligibility determination, then became clients of a brokered programme for individuals with mental illness. Vocational counsellors carried caseloads of 35 clients; additional staff provided job‐readiness and prevocational coaching/classes. To promote engagement and reduce attrition, study staff assisted participants with appointment‐setting, reminder calls, and transportation, if needed, to the first 3 appointments | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Weeks in competitive employment Days to first competitive employment Dropouts | |
| Notes | Competitive work was defined as employment paying at least minimum wage and not reserved for the disabled | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomised. No further details |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of programme |
| Blinding of outcome assessment (detection bias) | High risk | Raters were blinded. Employment outcomes (primary outcome) were collected via self‐report |
| Incomplete outcome data (attrition bias) | High risk | N = 46 were followed up (79%). 12 participants (IPS = 7; CVR = 5) dropped out, no significant difference between groups All analyses were ITT. Dropouts were assumed not to work, zeros were imputed for employment data following dropout |
| Selective reporting (reporting bias) | Low risk | All listed outcomes reported |
| Other bias | Low risk | This work was supported by the National Institute of Mental Health (MH066011 to EWT) and the National Alliance for Research on Schizophrenia and Depression; neither the NIMH nor NARSAD had any further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication |
| Methods | Allocation: randomised Design: single centre Duration: 24 months Country: Zürich, Switzerland | |
| Participants | N = 250 (183 unemployed at baseline) Diagnosis: mental disorder, all participants had to be in psychiatric and/or psycho‐therapeutical treatment during the whole study period. Included: 47% mood disorder, 16% schizophrenia/schizoaffective disorder, 17% personality disorder. Severity: > 50% 1‐5 admissions and mean age onset disease 10 years earlier than age at baseline Setting: University Hospital of Psychiatry Zurich (PUK) Age: 18‐60 years, mean 42.6 years Gender: 47% male Ethnicity: 78% born in country of residence Substance abuse: ‐ Living situation: lived in the canton of Zurich, 53% living alone, 36% with friends/relatives Marital status: ‐ Employment status: 73% unemployed Working history: 97% work history: 50% worked 1 month in past years, 47% < 1 month Motivation: wish to enter the competitive employment market or to remain there if they already had a job Education: 67% basic school, 15% high school, mean 10.2 years Disability benefit: IV‐pension due to a mental disorder (full or part time pension), < 1 year Excluded: organic mental disorder, mental retardation | |
| Interventions | IPS (N = 127, N = 92 unemployed at baseline) The intervention relied on the SE approach IPS. In total, there were 4 job coaches enrolled. 2 of them were full‐time employed, the other part time. All of them had a degree in psychology. The coaching frequency and the coaching duration of each session were determined individually by the job coach and the individual. No training of abilities or social skills nor any assessments of skills were administered beforehand. The job coach gave support during the application procedure (e.g. establishing realistic goals, writing applications, preparation of the job interview), and continued providing support according to the IPS principles during the participant employment (e.g. how to cope with workplace stressors including interpersonal conflicts with colleagues). The support was continued also in cases of job loss. The IPS fidelity scale was administered every 3 months. Moderate IPS fidelity was given throughout the whole study period (M = 61.2). Two items, item 4 (“cooperation with other institutions and other care team individuals”) and 14 (“community‐oriented services”), were rated low. Prevocational rehabilitation (N = 123, N = 91 unemployed at baseline) Participants of the control group were free to choose other vocational services including PVT, but were not supported by a job coach from ZhEPP | |
| Outcomes | Percentage of participants who obtained competitive employment Dropouts | |
| Notes | The primary outcome, obtaining competitive employment was scored as successfully fulfilled if the job was obtained by standard procedures (written application, CV, and job interview) and if the job was kept for at least 1 month We used the data of the participants who were unemployed at baseline (N = 183) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "For the purpose of randomisation, a list of numbers was created based on a Bernoulli distribution, a form of binomial probability distribution. Each participant was randomised according to that list" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by content of programme |
| Blinding of outcome assessment (detection bias) | High risk | No details about blinding. The participants were interviewed every 6 months by research workers |
| Incomplete outcome data (attrition bias) | High risk | The overall dropout rate was 32% (N = 79/250). The dropout rates in both groups were similar. 17 participants dropped out, from the participants who had a job in the beginning. In each group 31 participants who were unemployed at baseline dropped out: 62/183 = 34% Data for all participants were analysed as ITT. For that, the last observation carried forward (LOCF) method was used, meaning that in case of dropout, the last observation of a participant was used to replace the missing value. |
| Selective reporting (reporting bias) | Low risk | Study protocol was available, not all secondary outcomes were reported, it’s is possible that a separate publication will show those results |
| Other bias | Low risk | This study was funded by the Swiss Social Insurance Office (BSV). This funding was used for the salary of the job coaches and the scientific personnel and for the compensation of the interviews. No money was used to amplify participants’ income. The funding source had no influence on the design and the implementation of the study. |
| Methods | Allocation: randomised Design: multi centre Duration: 12 months Country: Brisbane, Townsville and Cairns, Australia | |
| Participants | N = 208 Diagnosis: psychotic disorder and a consumer of the mental health service at time of referral, not in an acute phase of illness and considered by the clinical team to be able to safely participate in the programme. Included: 81% psychotic disorder, 8% bipolar disorder, 6% major depressive disorder or anxiety disorder Setting: 4 CMH services Age: 18‐59 years, mean 32.4 years Gender: 69% male Ethnicity: Australian residents, 88% English spoken at home Substance abuse: ‐ Living situation: living in the mental health service catchment area with no immediate plans to move Marital status: 89% not partnered/single Employment status: not currently employed and not employed within the previous 3 months, currently available to work for ≥ 8 h/week Working history: 32% employed in prior year Motivation: interest in competitive employment as a goal Education: 68% completed year 12 Disability benefit: 68% disability support pension, 13% unemployment benefit Excluded: ‐ | |
| Interventions | IPS (N = 106) The intervention was governed by a standardised service level agreement between two agencies that enabled a full‐time employment specialist employed by the employment service, to be co‐located into the mental health team as the sole person delivering the employment service to volunteer consenting consumers of the mental health service. All four employment service partners in the intervention condition were contracted to the Australian Government and all received recurrent case‐based funding. The employment specialist was typically co‐located at the mental health service 4 of 5 d/week. Overall, the 4 interventions achieved good fidelity to IPS principles in the range 66–73 Disability employment services (N = 102) Non‐integrated forms of SE known as Disability Employment Services in Australia. Each site (intervention and control condition) received an initial training in evidence‐based practices in SE. Mental health case managers were given responsibility for delivering the control condition as part of enhanced routine mental health case management. They were provided assistance to engage with disability employment services in the local area. They were provided with a resource guide supported to select suitable employment services. Regular communication with the employment specialist was then encouraged. At 2 sites (Townsville and Cairns), there were no other disability employment services willing to accept referrals from the mental health teams, so staff of the same employment service but not co‐located with the mental health team, provided the control service. Employment services accepting these referrals had the same service contracts with the Australian Government. The four controls were estimated at fair IPS fidelity (range 56–65) | |
| Outcomes | Percentage of participants who obtained competitive employment Weeks in competitive employment Dropouts | |
| Notes | Competitive employment was defined as jobs in the open labour market at award wages or above, and not temporary jobs, piece work, voluntary work or unpaid work experience, and not jobs reserved for people with disabilities. The trial involved 4 other sites that did not use a randomised controlled design. One site did not succeed in implementation. Neither a full‐time co‐located employment specialist nor a local steering group, were established. Consequently, only fair fidelity was achieved with respect to IPS practices. Data collection was discontinued after 6 months because the arrangements resembled an informal collaboration more than a formal partnership. Data from this site were excluded from this analysis in the article. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sample randomisation was conducted centrally for all sites, at an individual level to a 1:1 allocation ratio, using a purpose‐designed MSAccess randomisation algorithm |
| Allocation concealment (selection bias) | Low risk | Central allocation |
| Blinding of participants and personnel (performance bias) | High risk | Due to the visible nature of the employment services being provided, it was not possible to mask the results of randomisation |
| Blinding of outcome assessment (detection bias) | Unclear risk | No details |
| Incomplete outcome data (attrition bias) | High risk | Early drop outs 28.4%. The majority of these continued in the vocational service but refused to take part in the data collection interviews. Attrition cases were more likely to speak a different language at home but otherwise did not differ from those that remained in the study. 56% completed follow‐up interview, N = 67 of intervention group and N = 49 in control group, reasons mentioned in flow chart |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | High risk | Implementation was based on a formal partnership approach that links a CMH service to an Australian Government‐funded disability employment service. Funding was offered in the form of a non‐recurrent AUD 75,000, per site, in the first year and AUD 50,000 in the second year. It was agreed that any participants who objected to their control condition randomisation would be offered the opportunity of transferring to the intervention after a minimum of 6 months’ assignment to the control service. Subsequently, 28 participants originally allocated to the control service opted to transfer to the IPS intervention after 6 months. The contaminated results were retained in the control group as originally allocated, but these results were also analysed separately. |
| Methods | Allocation: randomised Design: single centre Duration: 6 months Country: Brockton, Massachusetts, USA | |
| Participants | N = 28 Diagnosis: clearance by staff physician for off‐grounds rehabilitation. Included: 50% schizophrenia, 18% anxiety disorder, 14% depression Setting: VA hospital Age: ‐ Gender: 96% male Ethnicity:‐ Substance abuse: 7% alcohol, no further details Living situation: inpatient Marital status:‐ Employment status: unemployed Working history: minimal 2 weeks prior to study successful community hospital industrial rehabilitation placement, recommendation by rehabilitation therapist Motivation: willingness to volunteer for community CHIRP Education:‐ Disability benefit:‐ Excluded:‐ | |
| Interventions | Community‐based hospital industrial rehabilitation placement (CHIRP) (N = 14) Placements in a regular industrial setting off grounds (form of paid sheltered workshop), supervision by member of rehabilitation staff from hospital, transport, could continue to attend after leaving hospital, and standard hospital and community care. Standard care (N = 14) Standard hospital and community care | |
| Outcomes | Number of participants who obtained competitive employment Number of participants who obtained non‐competitive employment Hospital admissions | |
| Notes | Definition competitive employment: obtaining "regular competitive employment". Patients were free to secure regular employment or to continue in CHIRP during the study period | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Use of a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Participants were taken into the study in pairs (intervention and control) |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify given intervention by content of programme |
| Blinding of outcome assessment (detection bias) | High risk | No details about blinding |
| Incomplete outcome data (attrition bias) | Low risk | Data were obtained for all participants |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported |
| Other bias | Unclear risk | No details about funding source. Study authors were working at the hospital |
| Methods | Allocation: randomised Design: single centre Duration: 18 months Country: Hong Kong, China | |
| Participants | N = 92 Diagnosis: diagnosed at least 2 years previously as having a mental illness. Included: 70% schizophrenia spectrum, 18% affective disorder Setting: the Occupational Therapy Department, Kwai Chung Hospital Age: between 18‐55 years, mean 33.6 years Gender: 60% male Ethnicity: ‐ Substance abuse: ‐ Living situation: ‐ Marital status: 90% never married Employment status: unemployed Working history: mean months working at a paid job in the past 5 years: 17 months Motivation: expressed an interest in competitive employment Education: 68% grade 7‐11, 22% post secondary (grade 12 or above) Disability benefit: ‐ Excluded: serious medical illness that might affect their long‐term ability in competitive work | |
| Interventions | SE (N = 46) The SE programme of this study was based on the IPS model. The employment specialist was integrated into the participant’s clinical management team. The employment specialist assisted the participant to search for a competitive job on the basis of his or her educational background, work preference, and previous work experience. Once employed, on‐the‐job training and follow‐along support was provided. If employment was terminated for any reason, the employment specialist would assist the participant to recover from job loss and help him or her look for another job. The maximum caseload was limited to 20. The IPS programme developers were invited to conduct a 1‐week intensive training on the programme implementation as well as to rate the present programme by using the IPS Fidelity Scale. The local IPS programme received high ratings of implementation fidelity (scored 69 out of 75, which is equivalent to good implementation of SE). TVR (N = 46) The programme was implemented in the form of PVT in various work groups in a simulated environment. The primary objective of this programme was to equip participants with skills and knowledge related to choosing, obtaining, and keeping a competitive job in the community by using a stepwise train‐place approach. Although the participants were attending the programme, they were encouraged to seek open competitive employment by themselves by using the normal channels for job hunting, such as newspaper advertisements and Internet searches, as well as personal contacts with potential employers. | |
| Outcomes | Percentage of participants who obtained competitive employment Percentage of participants who obtained non‐competitive employment Weeks in competitive employment Days to first competitive employment Dropouts | |
| Notes | Definition competitive employment: a job paid at the market rate, for which anyone can apply, and not controlled by a service agency | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were individually randomly assigned by using random numbers generated by computer" |
| Allocation concealment (selection bias) | Unclear risk | No details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify the given intervention by contents of the programme |
| Blinding of outcome assessment (detection bias) | High risk | Measurements were conducted by the employment specialists |
| Incomplete outcome data (attrition bias) | Low risk | 1 participant in the control group was lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | This study was supported by grant 216033 from the Health Care and Promotion Fund, Food and Health Bureau, Hong Kong |
| Methods | Allocation: randomised Design: single centre Duration: 2 years Country: Bejing, China | |
| Participants | N = 103 Diagnosis: inpatients with a diagnosis of schizophrenia according to DSM–IV. They had been clinically stable for at least 1 month before recruitment and were about to begin their pre‐discharge home leave. Mean duration of illness 15 years Setting: the Chaoyang Mental Health Care Institute. As a district psychiatric hospital it has inpatient and outpatient service patients with schizophrenia. Age: 18‐60 years, mean 38.6 years Gender: 47% male Ethnicity: ‐ Substance abuse: excluded Living situation: at least one family member would be cohabiting with the participant after discharge Marital status: 54% never married Employment status: no employment immediately after discharge Working history: ‐ Motivation: ‐ Education: mean 10.7 years Disability benefit: ‐ Excluded: the presence of ongoing acute medical or neurological conditions, and current or a history of misuse of drugs and substances other than nicotine | |
| Interventions | Community re‐entry module (N = 53) A module of a standardised, structured social skills training programme devised at the University of California, Los Angeles. The community re‐entry module was primarily designed for inpatients, to foster seamless care in the transition between hospital and community. It consisted of 16 training sessions. Each of the sessions was taught using the 7 learning activities described in the trainer’s manual: introduction; videotape and questions/answers; role‐play; resource management; outcome problems; in vivo exercises; homework assignments. Each group comprised 6‐8 participants and the group sessions took place 4 times/week. Group psycho‐education (N = 50) An equally intensive programme of group psycho‐education, a standard psychosocial intervention in many parts of China. The opportunity to attend quarterly, community‐based workshops following discharge was offered to participants in both study groups as part of a routine intervention to reinforce the use in the community of skills acquired during admission. In addition, family members were encouraged to participate in these regular workshops. | |
| Outcomes | Percentage of participants who obtained competitive employment Mental health (PANNS) Hospital admissions Dropouts | |
| Notes | Re‐employment was defined as at least 3 consecutive months of salaried employment during study period | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly allocated |
| Allocation concealment (selection bias) | Unclear risk | No further details |
| Blinding of participants and personnel (performance bias) | High risk | Participants and personnel could identify intervention allocation by components of programme |
| Blinding of outcome assessment (detection bias) | Low risk | Two raters independently assessed all participants. The raters were not involved in the interventions and were also masked to the study protocol. Before commencing the study, participants were instructed by the research co‐ordinator not to disclose their group membership to the raters at any stage of study. In order to assess the effectiveness of the raters’ masking, we designed a 5‐point Likert scale. These results showed that the raters were not sure about the participants’ group membership, suggesting that masking was maintained relatively successfully throughout the study period |
| Incomplete outcome data (attrition bias) | Low risk | 94/103 (91%) participants completed all the research interviews. Missing post‐intervention and follow‐up data were calculated by using the ‘replace missing calculated by using the ‘replace missing values’ option of the SPSS |
| Selective reporting (reporting bias) | Low risk | All listed outcomes were reported |
| Other bias | Low risk | The study was funded by two grants, ZD199816 and TS199801, from the Bureau of Public Health, Beijing |
ACT: assertive community treatment; BPRS: Brief Psychiatric Rating Scale; CBT: cognitive behavioural therapy; CMH: community mental health; CWT: compensated work therapy; DPA: diversified placement approach DSM: Diagnostic and Statistical Manual of Mental Disorders; GED: General Education Diploma; HADS: Hamilton Depression and Anxiety Scale; IPS: individual placement and support; ITT: intention‐to‐treat; ISA: integrated service agency; IV: invalidity; MANSA: Manchester Short Assessment of Quality of Life; MHI: Mental Health Inventory; MMSE: Mini‐Mental State Examination; PACT: programme of ACT; PANNS: PTSD: post‐traumatic stress disorder; PVT: prevocational training; PWI: Personal Wellbeing Index; QOLI: The Quality of Life Interview; QOLP: Lancashire Quality of Life Profile; SAMHSA: Substance Abuse and Mental Health Services Administration; SE: supported employment; SFHS: Short‐Form Health Survey SMD: serious mental disorder; SMI: severe mental illness; SPSS: Statistical Package for the Social Sciences; SSA: Social Security Administration; SSDI; Social Security Disability Insurance; SSI; Supplemental Security Income; TVR: traditional vocational rehabilitation; TWE: transitional work experience; VA: Veterans Affairs; VR: vocational rehabilitation; WSST: work‐related social skills training
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Unclear employment outcome | |
| Wrong population: majority employed at baseline | |
| Large group of participants was already employment at baseline (43%) | |
| Wrong design: participants from 2 studies, not a RCT | |
| No competitive employment outcomes | |
| Paid work was part of the intervention | |
| No competitive employment outcomes | |
| Transitional funds were used | |
| Transitional funds were used, analysis of two trials | |
| No competitive employment outcomes | |
| Wrong design: secondary analysis on a pooled sample from four RCTs | |
| This is an aggregation of 8 independent RCTs from different cities in the USA. This project was named the Employment Intervention Demonstration Program (EIDP). We used the individual reports of these RCTs because of the heterogeneity of the interventions and control conditions. | |
| No competitive employment outcomes | |
| Wrong population: veterans with PTSD. Participants with schizophrenia, schizo‐affective disorder and bipolar disorder excluded because they were already eligible for IPS | |
| All participants were placed in jobs at baseline | |
| No competitive employment outcomes | |
| Employment was a combination of volunteer and paid employment | |
| Unclear definition of employment | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| Follow‐up of Zurich sample after termination of the EQOLISE trial (Burns 2007) | |
| No competitive employment outcomes | |
| Unclear definition of employment | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| Wrong design: not a RCT | |
| Wrong design: not a RCT | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| Unclear definition of employment | |
| Quasi experimental design, assignment based on clinical risk (severity of positive symptoms) | |
| Wrong design: a mixed randomised and quasi experimental design was used | |
| Wrong design: not randomised controlled | |
| All participants were employed at baseline | |
| Secondary analysis of results of 4 RCTs | |
| No competitive employment outcomes | |
| The definition of employment did not differentiate between competitive or transitional/sheltered employment | |
| Wrong design: cohort study | |
| Wrong design: matching procedure | |
| Unclear number of participants employed at baseline | |
| wrong population: majority employed or in military service at baseline | |
| No competitive employment outcomes | |
| Not randomised, the assignment was based on the order of entry | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| Wrong population: majority was employed at baseline | |
| No competitive employment outcomes | |
| Wrong design: not RCT. A big part of the participants (42%) was employed at baseline. No competitive employment outcomes | |
| No competitive employment outcomes | |
| Wrong design: includes data of a retrospective study | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| No competitive employment outcomes | |
| Wrong population: majority employed at baseline |
PTSD: post‐traumatic stress disorder; RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT |
| Participants | Adults, aged 18‐63 years, with a depressive episode, recurrent depression or bipolar disorder and interested in employment and not employed during the past year |
| Interventions | Individual Enabling and Support (IES) compared to TVR IES is guided by an employment specialist who works closely with the participant in relation to the outpatient team, family, Social Insurance Agency, Public Employment Service and employers. There are ten IES principles: 1) handling change and developing motivational and cognitive strategies, 2) having a time‐use pattern that supports work‐life balance. Principles 3–10 correspond to the IPS model. TVR was delivered by various professionals in several settings and organisations and was regulated by the social benefit and unemployment security system. The first step involved reducing symptoms and increasing work ability at a mental health service. Step 2 involved assessment of 50% work capacity and was performed by the SIA and PES. If work capacity was not met, participants could enter Step 3 with pre‐vocational activities at the municipality. The last step was vocational training during internship placements, and these could lead to employment positions through the Public Employment Service. |
| Outcomes | Number of participants, weeks and hours a week in competitive employment, internship, education, PVT. Depressive severity and quality of life |
| Notes |
| Methods | 2 x 2 RCT |
| Participants | People with serious mental illness |
| Interventions | Work skills training programme and IPS compared to IPS, and the participants were also randomly assigned to risperidon or olanzapine |
| Outcomes | Clinical and work outcomes |
| Notes |
| Methods | Cluster‐RCT |
| Participants | People, 15‐40 years, with first episode psychosis and ≤ 6 months on antipsychotic medication |
| Interventions | NAVIGATE compared to usual community treatment. NAVIGATE included 4 interventions: personalised medication management, family psycho education, resilience‐focused individual therapy and SE plus education. Usual community treatment was psychosis treatment determined by clinician choice and service availability |
| Outcomes | Days of paid employment or school attendance, employment rate, employment earnings, disability income, public support. Other outcomes published elsewhere: quality of life, mental health |
| Notes |
| Methods | RCT |
| Participants | People with severe mental illness (schizophrenia, bipolar disorder, major depression) who had not obtained or kept competitive work despite receiving high‐fidelity SE |
| Interventions | All participants continued to receive their usual mental health services, including a SE programme enhanced by training employment specialists in the management of cognitive impairments. Participants were randomly assigned to receive enhanced SE only or enhanced SE plus the Thinking Skills for Work program, which used three approaches: cognitive exercise practice (COGPACK), strategy coaching, and teaching coping/compensatory strategies |
| Outcomes | Cognitive outcomes, competitive work outcomes, symptoms and quality of life |
| Notes |
| Methods | RCT |
| Participants | Participants with SMI (83% schizophrenia) who had not benefited from vocational rehabilitation |
| Interventions | Vocational services enhanced by training vocational specialists in recognising cognitive difficulties and providing job‐relevant cognitive coping strategies (Enhanced Vocational Rehabilitation), or similarly enhanced vocational services and cognitive remediation (Thinking Skills for Work). Participants were recruited form 3 employment programmes: Project Moving On, MetroClub, and Adult Rehabilitation Services. Each of these programmes had a unique vocational rehabilitation model. |
| Outcomes | Employment outcomes including competitive employment, clinical symptoms |
| Notes |
| Methods | RCT |
| Participants | People aged 18–60 years, and on the caseload of the rehabilitation and recovery or early intervention in psychosis teams |
| Interventions | All participants received IPS. In the intervention group participants were offered 3‐6 sessions of work‐focused counselling delivered by a psychologist based on generic psychological practice, including goal‐based motivational procedures and CBT. |
| Outcomes | Hours in paid employment and other vocational activities such as education, training or volunteer work. Self‐esteem, costs, health and well‐being, self‐assessed barriers to work, perceived stigma, avoidance of social disapproval, social cognition and social problem solving |
| Notes |
CBT: cognitive behavioural therapy
IPS: individual placement and support
PVT: prevocational training
RCT: randomised controlled trial
SE: supported employment
SMI: serious mental illness
TVR: traditional vocational rehabilitation
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Cognitive training to enhance work program outcomes: preliminary findings |
| Methods | RCT |
| Participants | People with psychotic disorders participating in all types of work programmes including incentive therapy, CWT and SE |
| Interventions | Cognitive training PositScience or Nintento BrainAge. BrainAge employed engaging cognitive game software and PositScience used specially designed exercises that narrowly focus on discrete cognitive processes. Work services were provided as usual |
| Outcomes | Neurocognitive, vocational and quality of life outcomes |
| Starting date | Unknown |
| Contact information | Unknown |
| Notes | No data available yet |
| Trial name or title | Effectiveness of the Comprehensive Approach to Rehabilitation (CARe) methodology: design of a cluster randomized controlled trial |
| Methods | Cluster‐RCT |
| Participants | People with severe mental illness from participating organisation for sheltered and supported housing facilities |
| Interventions | Teams in the intervention group receive the CARe methodology training. The aims of this training are: training workers in the principles of rehabilitative and recovery‐supportive care and to support clients' rehabilitation process in a methodical way. The study will give special attention to the process of implementation. The CARe methodology consists of 6 steps: (1) building and maintaining a constructive relationship; (2) collecting information and making a personal profile with the client; (3) helping the client with formulating wishes, making choices and setting goals; (4) helping the client to making a Personal Plan; (5) helping the client execute the plan and (6) following the process, learn, evaluate and adjust. After the training programme the workers will be supported in working according to the CARe methodology by means of CARe coaching meetings (once every 4‐6 weeks). The teams in the control group do not receive the CARe methodology training. The workers in those teams will maintain work according to the (narrowly implemented) outdated CARe methodology. |
| Outcomes | Primary outcomes: recovery, social functioning (including employment status) and quality of life. Other outcomes are empowerment, hope, self‐efficacy beliefs and need for care. Model fidelity audit will be performed |
| Starting date | May 2012 |
| Contact information | |
| Notes | Unclear if competitive employment outcomes will be presented |
| Trial name or title | Individual placement and support supplemented with cognitive remediation and work‐related social skills training in Denmark: study protocol for a randomized controlled trial |
| Methods | Randomised, three‐arm, assessor‐blinded, multi centre trial |
| Participants | Adults diagnosed with schizophrenia, schizotypal or delusional disorders, bipolar disorder, or severe depression. Participants must reside in one of two major Danish cities: Copenhagen or Odense. They must be assigned to early intervention teams or community mental health services. They must express a clear desire for competitive employment or education. |
| Interventions | IPS and services as usual or IPS enhanced with cognitive remediation and work‐related social skills training and services as usual |
| Outcomes | The primary outcome is “hours in competitive employment or education”. Danish employment legislation provides opportunities for financial support when obtaining competitive employment. This could be subsidised employment. Secondary outcomes are work or education at some point during the follow‐up period (yes/no), days to first employment or beginning of education, cognitive impairment, functional level, self‐esteem, and self‐efficacy |
| Starting date | October 2012 |
| Contact information | |
| Notes |
| Trial name or title | Enhancing assertive community treatment with cognitive behavioral social skills training for schizophrenia: study protocol for a randomized controlled trial |
| Methods | RCT |
| Participants | People diagnosed with schizophrenia or schizoaffective disorder, receiving ACT services for at least 3 months, no prior social skills training or CBT in the past 3 years, and living in the community for at least the past month |
| Interventions | ACT alone or ACT + Adapted Cognitive Behavioral Social Skills Training (CBSST) The CBSST intervention is delivered in the context of the regular ACT visits. CBSST integrates CBT and social skills training techniques. |
| Outcomes | The primary outcome domain is psychosocial functioning: everyday living skills and activities related to employment, education, and housing. Additional outcome domains of interest include mediators of change in functioning, symptoms, quality of service and programme fidelity. |
| Starting date | February 2012 |
| Contact information | |
| Notes | This is also a mixed method implementation study |
| Trial name or title | Internet based cognitive remediation can assist people with severe mental illness to gain and retain employment‐the CogRem study |
| Methods | RCT |
| Participants | Unemployed people with severe mental illness who had joined a supported employment programme |
| Interventions | Internet‐based, cognitive remediation (CogRem) compared to internet‐based information control (WebInfo) |
| Outcomes | Paid working hours, earnings |
| Starting date | Unknown |
| Contact information | Unknown |
| Notes | Information based on conference abstract |
| Trial name or title | The effect of five years versus two years of specialised assertive intervention for first episode psychosis ‐ OPUS II: study protocol for a randomized controlled trial |
| Methods | RCT |
| Participants | People, aged 18‐37 years, with first episode psychosis in the schizophrenia spectrum |
| Interventions | A 2‐year specialised intensive assertive treatment programme (OPUS) or standard treatment. The integrated OPUS treatment consists of 3 core elements; ACT, family treatment and social skills training |
| Outcomes | Negative symptoms, simultaneous remission of psychotic and negative symptoms, substance abuse, user satisfaction, adherence to treatment, compliance with medication, suicidal behaviour, working alliance, self‐efficacy, use of bed days, ability to live independently, and labour‐market affiliation |
| Starting date | July 2009 |
| Contact information | |
| Notes | We excluded the previous study (OPUS I trial) because they did not report competitive employment outcomes |
| Trial name or title | 'Placement budgets' for supported employment‐‐improving competitive employment for people with mental illness: study protocol of a multicentre randomized controlled trial |
| Methods | Multicentre RCT |
| Participants | Current treatment in one of the 6 participating outpatient psychiatric clinics 12 months of unemployment and no programme of vocational integration over the last 3 months Motivation to work in competitive employment Being of working age (18–60 years) Resident in the Canton of Zurich Willing and capable of giving informed consent |
| Interventions | IPS with three different placement budgets of 25 h, 40 h, or 55 h working hours of job coaches. Support lasts 2 years for those who find a job. The intervention ends for those who fail to find competitive employment when the respective placement budgets run out. |
| Outcomes | Time between study inclusion and first competitive employment that lasted ≥ 3 months, motivation, stigmatisation, social network and social support, quality of life, job satisfaction, financial situation, and health conditions |
| Starting date | June 2010 |
| Contact information | |
| Notes |
| Trial name or title | Protocol for the effect evaluation of Individual Placement and Support (IPS): a randomised controlled multicenter trial of IPS versus treatment as usual for patients with moderate to severe mental illness in Norway |
| Methods | Multicentre RCT |
| Participants | People currently undergoing treatment for moderate to severe mental illness, who are currently out of the labour market but have an expressed desire to work |
| Interventions | IPS or high quality treatment as usual. Treatment as usual involves being offered a prioritised spot in a vocational rehabilitation scheme, primarily Work with assistance and/or traineeship in a sheltered business |
| Outcomes | The primary outcome of the study is increased labour market participation in ordinary paid employment or education. The secondary outcomes are mental health status, disability and quality of life |
| Starting date | Unknown |
| Contact information | |
| Notes | There will be a subgroup analysis for severe mental illness vs moderate mental illness |
ACT: assertive community treatment
CBT: cognitive behavioural therapy
CWT: compensated work therapy
IPS: individual placement and support
RCT: randomised controlled trial
SE: supported employment
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Obtaining competitive employment, short‐term follow‐up (≤ 1 year) Show forest plot | 18 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.1  Comparison 1 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Obtaining competitive employment, short‐term follow‐up (≤ 1 year). | ||||
| 1.1 SE vs psych care | 3 | 1087 | Risk Ratio (M‐H, Random, 95% CI) | 1.79 [0.94, 3.40] |
| 1.2 PVT vs psych care | 2 | 171 | Risk Ratio (M‐H, Random, 95% CI) | 8.96 [1.77, 45.51] |
| 1.3 TE vs psych care | 4 | 422 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.88, 1.45] |
| 1.4 SE vs TE | 3 | 231 | Risk Ratio (M‐H, Random, 95% CI) | 3.49 [1.77, 6.89] |
| 1.5 SE vs PVT | 2 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 2.52 [1.21, 5.24] |
| 1.6 TE vs PVT | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.59, 1.04] |
| 1.7 SE+ vs SE | 3 | 143 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.37, 2.25] |
| 2 Obtaining competitive employment, long‐term follow‐up (> 1 year) Show forest plot | 22 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Obtaining competitive employment, long‐term follow‐up (> 1 year). | ||||
| 2.1 SE+ vs psych care | 1 | 256 | Risk Ratio (M‐H, Random, 95% CI) | 4.32 [1.49, 12.48] |
| 2.2 SE vs psych care | 1 | 2238 | Risk Ratio (M‐H, Random, 95% CI) | 1.51 [1.36, 1.68] |
| 2.3 PVT vs psych care | 2 | 161 | Risk Ratio (M‐H, Random, 95% CI) | 2.19 [1.07, 4.46] |
| 2.4 SE+ vs TE | 2 | 212 | Risk Ratio (M‐H, Random, 95% CI) | 2.45 [1.69, 3.55] |
| 2.5 SE vs TE | 4 | 587 | Risk Ratio (M‐H, Random, 95% CI) | 3.28 [2.13, 5.04] |
| 2.6 SE+ vs PVT | 2 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 5.42 [1.08, 27.11] |
| 2.7 SE vs PVT | 9 | 1570 | Risk Ratio (M‐H, Random, 95% CI) | 2.31 [1.85, 2.89] |
| 2.8 SE+ vs SE | 3 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [1.03, 3.65] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Weeks in competitive employment, short‐term follow‐up (≤ 1 year) Show forest plot | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.1  Comparison 2 Any intervention to improve maintaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Weeks in competitive employment, short‐term follow‐up (≤ 1 year). | ||||
| 1.1 SE+ vs SE | 1 | 32 | Mean Difference (IV, Random, 95% CI) | ‐1.46 [‐3.38, 0.46] |
| 1.2 SE vs TE | 2 | 187 | Mean Difference (IV, Random, 95% CI) | 4.18 [1.27, 7.09] |
| 1.3 SE vs PVT | 1 | 58 | Mean Difference (IV, Random, 95% CI) | 6.89 [1.26, 12.52] |
| 1.4 SE vs psych care | 2 | 131 | Mean Difference (IV, Random, 95% CI) | 4.87 [0.37, 9.37] |
| 1.5 TE vs PVT | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 6.70 [‐1.76, 15.16] |
| 1.6 TE vs psych care | 1 | 10 | Mean Difference (IV, Random, 95% CI) | ‐4.39 [‐17.75, 8.97] |
| 2 Weeks in competitive employment, long‐term follow‐up (> 1 year) Show forest plot | 11 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 2.2  Comparison 2 Any intervention to improve maintaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Weeks in competitive employment, long‐term follow‐up (> 1 year). | ||||
| 2.1 SE+ vs SE | 3 | 154 | Mean Difference (IV, Random, 95% CI) | 10.09 [0.32, 19.85] |
| 2.2 SE+ vs PVT | 1 | 47 | Mean Difference (IV, Random, 95% CI) | 22.79 [15.96, 29.62] |
| 2.3 SE vs TE | 4 | 587 | Mean Difference (IV, Random, 95% CI) | 17.36 [11.53, 23.18] |
| 2.4 SE vs PVT | 5 | 390 | Mean Difference (IV, Random, 95% CI) | 11.56 [5.99, 17.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Days to first competitive employment, short‐term follow‐up (≤ 1 year) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.1 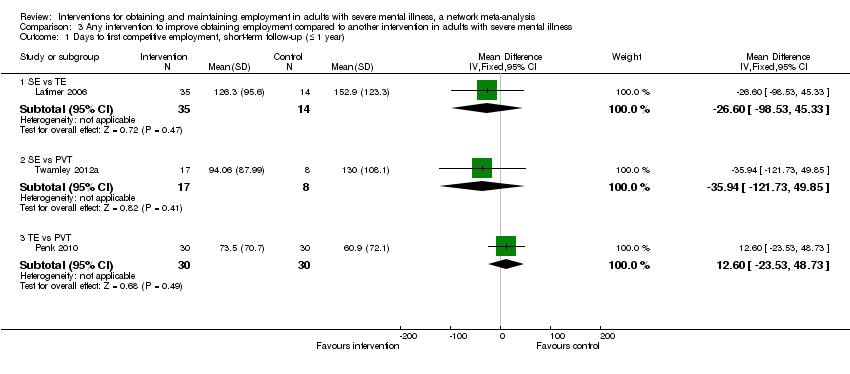 Comparison 3 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Days to first competitive employment, short‐term follow‐up (≤ 1 year). | ||||
| 1.1 SE vs TE | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐26.60 [‐98.53, 45.33] |
| 1.2 SE vs PVT | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | ‐35.94 [‐121.73, 49.85] |
| 1.3 TE vs PVT | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 12.60 [‐23.53, 48.73] |
| 2 Days to first competitive employment, long‐term follow‐up (> 1 year) Show forest plot | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 3.2  Comparison 3 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Days to first competitive employment, long‐term follow‐up (> 1 year). | ||||
| 2.1 SE+ vs TE | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐142.80 [‐238.70, ‐46.90] |
| 2.2 SE vs TE | 3 | 205 | Mean Difference (IV, Fixed, 95% CI) | ‐64.86 [‐115.95, ‐13.77] |
| 2.3 SE vs PVT | 2 | 96 | Mean Difference (IV, Fixed, 95% CI) | ‐35.01 [‐105.21, 35.19] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Obtaining non‐competitive employment, short‐term follow‐up (≤ 1 year) Show forest plot | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 4.1  Comparison 4 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Obtaining non‐competitive employment, short‐term follow‐up (≤ 1 year). | ||||
| 1.1 SE+ vs SE | 2 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.15, 17.22] |
| 1.2 SE vs TE | 2 | 187 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.18, 6.84] |
| 1.3 SE vs PVT | 2 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.39, 2.06] |
| 1.4 SE vs psych care | 1 | 900 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.61, 2.00] |
| 1.5 TE vs PVT | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 3.82 [2.24, 6.53] |
| 1.6 TE vs psych care | 2 | 78 | Risk Ratio (M‐H, Random, 95% CI) | 4.27 [0.00, 4883.69] |
| 1.7 PVT vs psych care | 1 | 122 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.12, 72.23] |
| 2 Obtaining non‐competitive employment, long‐term follow‐up (> 1 year) Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 4.2 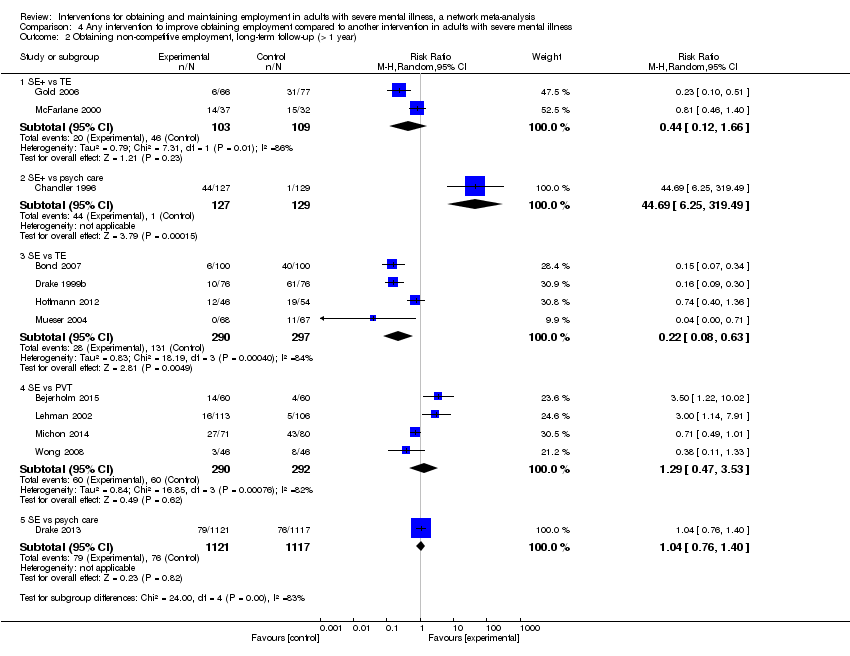 Comparison 4 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Obtaining non‐competitive employment, long‐term follow‐up (> 1 year). | ||||
| 2.1 SE+ vs TE | 2 | 212 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.12, 1.66] |
| 2.2 SE+ vs psych care | 1 | 256 | Risk Ratio (M‐H, Random, 95% CI) | 44.69 [6.25, 319.49] |
| 2.3 SE vs TE | 4 | 587 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.08, 0.63] |
| 2.4 SE vs PVT | 4 | 582 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.47, 3.53] |
| 2.5 SE vs psych care | 1 | 2238 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.76, 1.40] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quality of life, long‐term follow up (> 1 year) Show forest plot | 9 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| Analysis 5.1 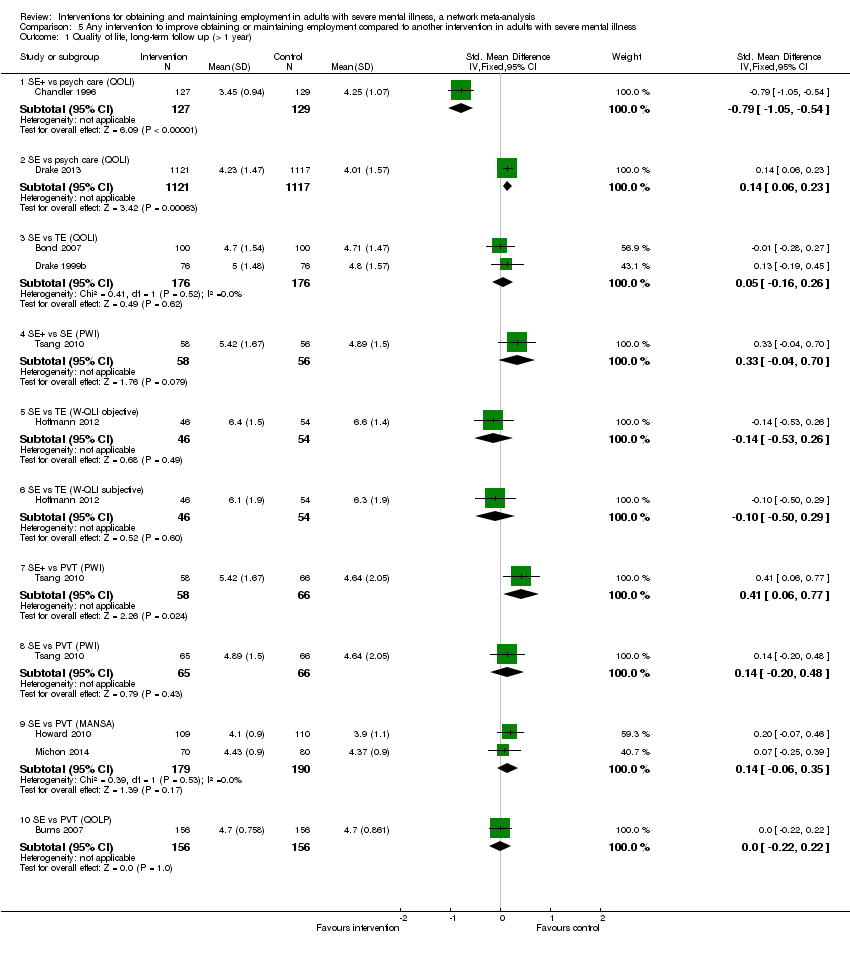 Comparison 5 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Quality of life, long‐term follow up (> 1 year). | ||||
| 1.1 SE+ vs psych care (QOLI) | 1 | 256 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.79 [‐1.05, ‐0.54] |
| 1.2 SE vs psych care (QOLI) | 1 | 2238 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [0.06, 0.23] |
| 1.3 SE vs TE (QOLI) | 2 | 352 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.16, 0.26] |
| 1.4 SE+ vs SE (PWI) | 1 | 114 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.33 [‐0.04, 0.70] |
| 1.5 SE vs TE (W‐QLI objective) | 1 | 100 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.53, 0.26] |
| 1.6 SE vs TE (W‐QLI subjective) | 1 | 100 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.50, 0.29] |
| 1.7 SE+ vs PVT (PWI) | 1 | 124 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.41 [0.06, 0.77] |
| 1.8 SE vs PVT (PWI) | 1 | 131 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.20, 0.48] |
| 1.9 SE vs PVT (MANSA) | 2 | 369 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.06, 0.35] |
| 1.10 SE vs PVT (QOLP) | 1 | 312 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.22, 0.22] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mental health long‐term follow‐up (> 1 year) Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 6.1  Comparison 6 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Mental health long‐term follow‐up (> 1 year). | ||||
| 1.1 SE vs psych care (SFHS) | 1 | 2238 | Mean Difference (IV, Random, 95% CI) | 2.88 [1.78, 3.98] |
| 1.2 PVT vs psych care (PANSS positive symptoms) | 1 | 103 | Mean Difference (IV, Random, 95% CI) | ‐2.48 [‐3.95, ‐1.01] |
| 1.3 PVT vs psych care (PANSS negative symptoms) | 1 | 103 | Mean Difference (IV, Random, 95% CI) | ‐1.61 [‐2.99, ‐0.23] |
| 1.4 PVT vs psych care (PANSS general symptoms) | 1 | 103 | Mean Difference (IV, Random, 95% CI) | ‐1.86 [‐3.09, ‐0.63] |
| 1.5 PVT vs psych care (composite index, multiple scales) | 1 | 58 | Mean Difference (IV, Random, 95% CI) | ‐7.09 [‐326.22, 312.04] |
| 1.6 SE vs TE (PANSS positive symptoms) | 1 | 200 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐1.71, 1.67] |
| 1.7 SE vs TE (PANSS negative symptoms) | 1 | 200 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐2.79, 1.19] |
| 1.8 SE vs TE (PANSS general psychopathology) | 1 | 200 | Mean Difference (IV, Random, 95% CI) | ‐2.69 [‐7.58, 2.20] |
| 1.9 SE vs TE (BPRS) | 1 | 152 | Mean Difference (IV, Random, 95% CI) | ‐1.90 [‐5.69, 1.89] |
| 1.10 SE vs PVT (HADS anxiety) | 1 | 312 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.88, 1.08] |
| 1.11 SE vs PVT (HADS depression) | 1 | 312 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐1.08, 0.88] |
| 1.12 SE vs PVT (MHI) | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐8.63, 2.63] |
| 1.13 SE vs PVT (PANSS positive symptoms) | 1 | 312 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.93, 1.13] |
| 1.14 SE vs PVT (PANSS negative symptoms) | 1 | 312 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.38, 0.98] |
| 1.15 SE vs PVT (PANSS general psychopathology) | 1 | 312 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐1.34, 2.14] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Dropouts, short‐term follow‐up (≤ 1 year) Show forest plot | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.1  Comparison 7 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Dropouts, short‐term follow‐up (≤ 1 year). | ||||
| 1.1 SE vs psych care | 3 | 1087 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.41, 1.10] |
| 1.2 PVT vs psych care | 1 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 102.04] |
| 1.3 TE vs psych care | 2 | 182 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.43, 1.06] |
| 1.4 SE vs TE | 2 | 187 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.78 [0.84, 3.77] |
| 1.5 SE vs PVT | 2 | 148 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.36 [0.56, 3.30] |
| 1.6 TE vs PVT | 1 | 89 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.92 [0.19, 79.40] |
| 1.7 SE+ vs SE | 2 | 119 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.43, 1.67] |
| 2 Dropouts, long‐term follow‐up (> 1 year) Show forest plot | 19 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| Analysis 7.2  Comparison 7 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Dropouts, long‐term follow‐up (> 1 year). | ||||
| 2.1 SE+ vs psych care | 1 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.50, 1.08] |
| 2.2 SE vs psych care | 1 | 2238 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.78, 1.52] |
| 2.3 PVT vs psych care | 2 | 161 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.45, 2.19] |
| 2.4 SE+ vs SE | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.37, 1.14] |
| 2.5 SE+ vs TE | 1 | 143 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.33, 1.13] |
| 2.6 SE vs TE | 4 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.89, 4.15] |
| 2.7 SE+ vs PVT | 2 | 193 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.59, 1.64] |
| 2.8 SE vs PVT | 9 | 1569 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.80, 1.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Hospital admissions, short‐term follow‐up (≤ 1 year) Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 8.1  Comparison 8 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Hospital admissions, short‐term follow‐up (≤ 1 year). | ||||
| 1.1 SE vs psych care | 1 | 900 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.74, 1.73] |
| 1.2 TE vs psych care | 4 | 422 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.30, 1.15] |
| 1.3 SE vs PVT | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.76, 2.01] |
| 2 Hospital admissions, long‐term follow‐up (> 1 year) Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| Analysis 8.2  Comparison 8 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Hospital admissions, long‐term follow‐up (> 1 year). | ||||
| 2.1 SE+ vs psych care | 1 | 256 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.73, 1.70] |
| 2.2 PVT vs psych care | 1 | 103 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.11, 0.65] |
| 2.3 SE+ vs TE | 1 | 143 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.55, 1.63] |
| 2.4 SE vs PVT | 3 | 681 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.60, 1.45] |

PRISMA Study flow diagram
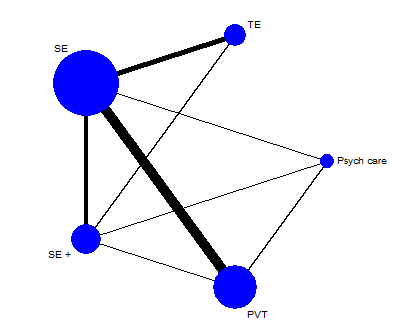
Network plot of direct comparisons of intervention main groups (long‐term follow‐up). Psych care: psychiatric care only; PVT: prevocational training; SE: supported employment; SE+: augmented supported employment; TE: transitional employment

Network plot of direct comparisons of intervention subgroups (long‐term follow‐up). CH: Clubhouse; CT: cognitive training; hf IPS: high‐fidelity Individual Placement and Support; job : job‐related skills training; lf IPS: low‐fidelity Individual Placement and Support; Psych care: psychiatric care only; SE + ACT: supported employment + assertive community treatment; SE + job: supported employment + job‐related skills training; SE + symp: supported employment + symptom‐related skills training; SE + TE: supported employment + transitional employment; SST: social skills training; SWS: sheltered workshops

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

Network meta‐analysis estimates of intervention benefit.
CI: confidence interval; Psych care: psychiatric care only; PVT: prevocational employment; RR: risk ratio; SE: supported employment; SE+: augmented supported employment; TE: transitional employment;

Plots of the surface under the cumulative ranking curves (SUCRAs) for the interventions included in the network (long‐term follow‐up).
PVT: prevocational training; Psych care: psychiatric care only; SE: supported employment; SE+: augmented supported employment; TE: transitional employment
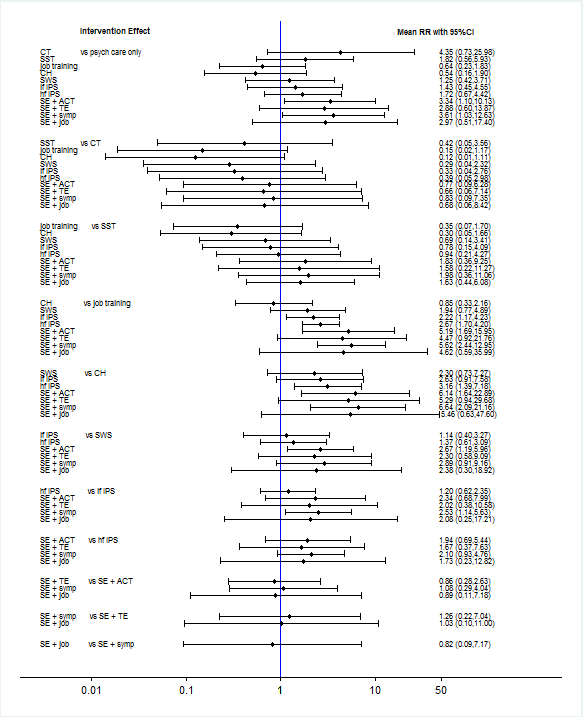
Effectiveness of intervention subgroups in obtaining competitive employment (long‐term follow‐up).
CH: Clubhouse; CI: confidence interval; CT: cognitive training; hf IPS: high‐fidelity Individual Placement and Support; job training: job‐related skills training; lf IPS: low‐fidelity Individual Placement and Support;Psych care only: psychiatric care only; RR: risk ratio; SE + ACT: supported employment + assertive community treatment; SE + job: supported employment + job‐related skills training; SE + symp: supported employment + symptom‐related skills training; SE + TE: supported employment + transitional employment; SST: social skills training; SWS: sheltered workshops

Plots of the surface under the cumulative ranking curves (SUCRAs) for the interventions subgroups included in the network (long‐term follow‐up)
CH: Clubhouse; CT: cognitive training; hf IPS: high‐fidelity Individual Placement and Support; job: job‐related skills training; lf IPS: low‐fidelity Individual Placement and Support;Psych care: psychiatric care only; SE + ACT: supported employment + assertive community treatment; SE + job: supported employment + job‐related skills training; SE + symp: supported employment + symptom‐related skills training; SE + TE: supported employment + transitional employment; SST: social skills training; SWS: sheltered workshops

Inconsistency plots for long‐term follow‐up and loop‐specific heterogeneity estimates.
PVT: prevocational training; Psych care: psychiatric care only; ROR: risk odds ratio; SE: supported employment; SE+: augmented supported employment; TE: transitional employment

Loop‐specific inconsistency in intervention subgroup network (long‐term follow‐up). hf IPS: high‐fidelity Individual Placement and Support; job: job‐related skills training; lf IPS: low‐fidelity Individual Placement and Support;Psych care: psychiatric care only; SE: supported employment;TE: transitional employment; SWS: sheltered workshops

Study limitations distribution for each network estimate for pairwise comparisons. Calculations are based on the contributions of direct evidence to the network estimates. The colours represent the risk of bias. PVT: prevocational training; Psych care: psychiatric care only; SE: supported employment; SE+: augmented supported employment; TE: transitional employment

Contribution matrix: Percentage contribution of each direct estimate to the NMA estimates. PVT: prevocational training; Psych care: psychiatric care only; SE: supported employment; SE+: augmented supported employment; TE: transitional employment

Comparison‐adjusted funnel plot for the network of intervention for obtaining competitive employment for people with severe mental illness (long‐term follow‐up). The black line represents the null hypothesis that the study‐specific effect sizes do not differ from the respective comparison‐specific pooled effect estimates. The blue line is the regression line. The interventions are ordered based on their focus on competitive job search. Missing small studies on the right side of the zero line (means ratio of RR > 1) suggests that small studies tend to exaggerate the effectiveness of interventions with more focus on competitive job search. PVT: prevocational training; Psych care: psychiatric care only; RR: risk ratio; SE: supported employment; SE+: augmented supported employment; TE: transitional employment

Comparison 1 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Obtaining competitive employment, short‐term follow‐up (≤ 1 year).
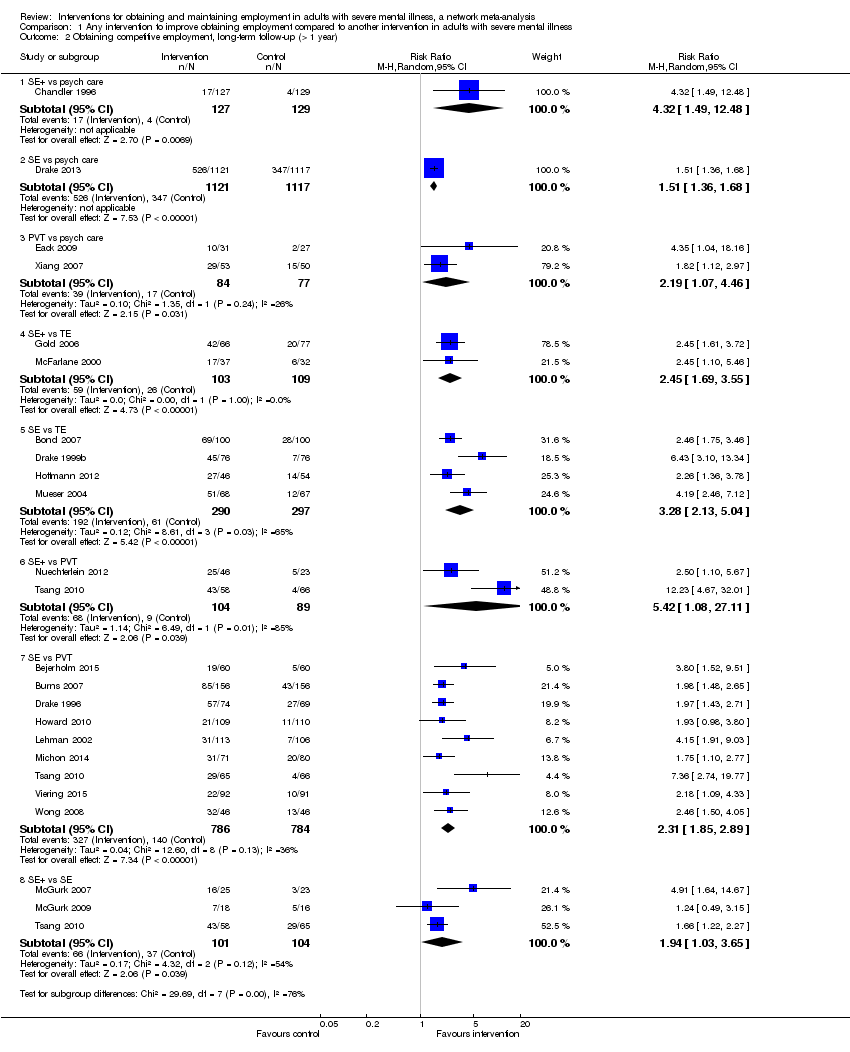
Comparison 1 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Obtaining competitive employment, long‐term follow‐up (> 1 year).

Comparison 2 Any intervention to improve maintaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Weeks in competitive employment, short‐term follow‐up (≤ 1 year).
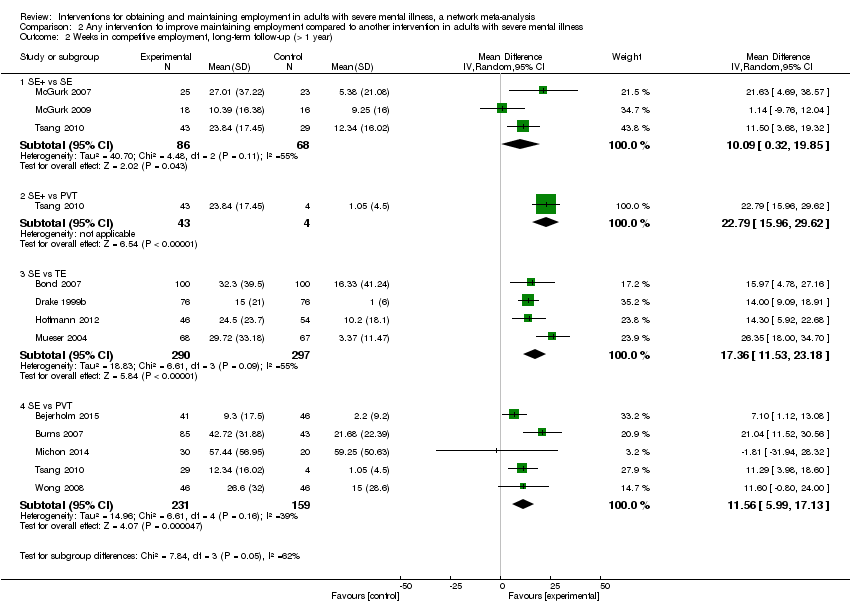
Comparison 2 Any intervention to improve maintaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Weeks in competitive employment, long‐term follow‐up (> 1 year).
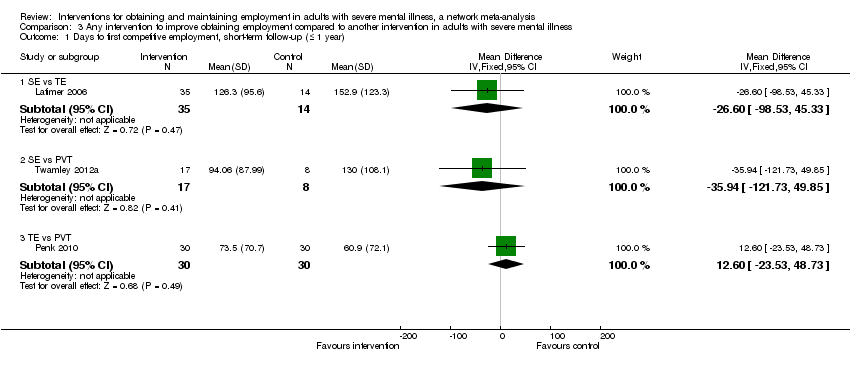
Comparison 3 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Days to first competitive employment, short‐term follow‐up (≤ 1 year).

Comparison 3 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Days to first competitive employment, long‐term follow‐up (> 1 year).
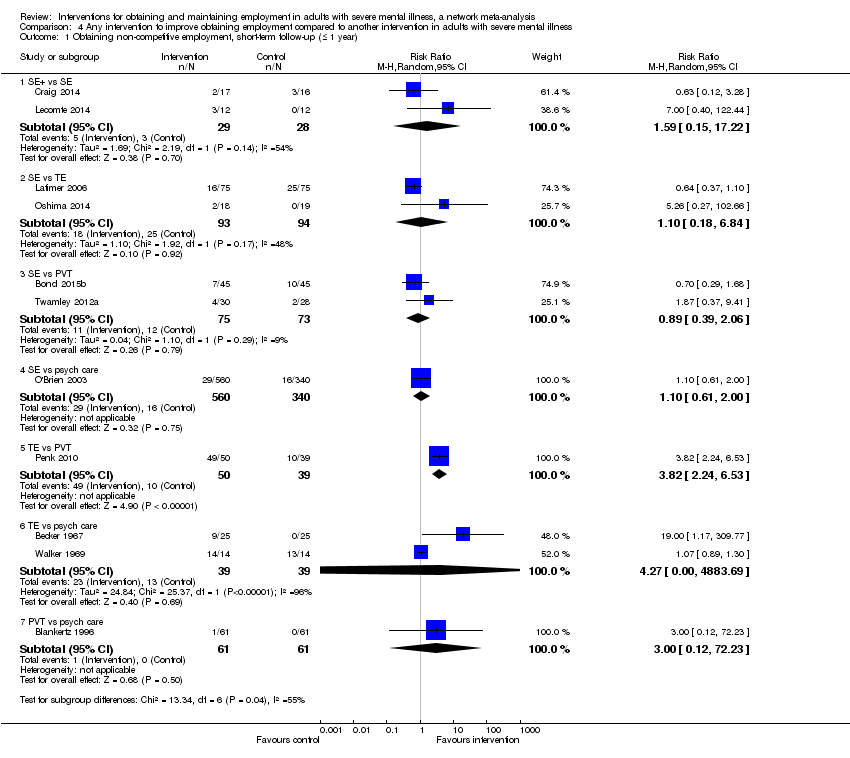
Comparison 4 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Obtaining non‐competitive employment, short‐term follow‐up (≤ 1 year).

Comparison 4 Any intervention to improve obtaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Obtaining non‐competitive employment, long‐term follow‐up (> 1 year).

Comparison 5 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Quality of life, long‐term follow up (> 1 year).

Comparison 6 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Mental health long‐term follow‐up (> 1 year).
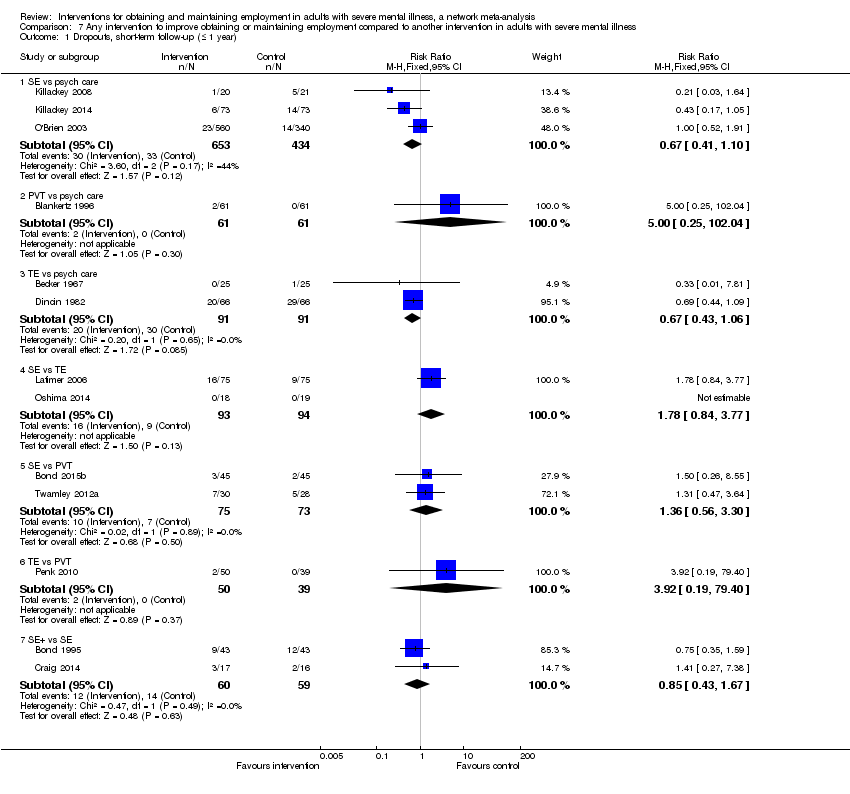
Comparison 7 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Dropouts, short‐term follow‐up (≤ 1 year).
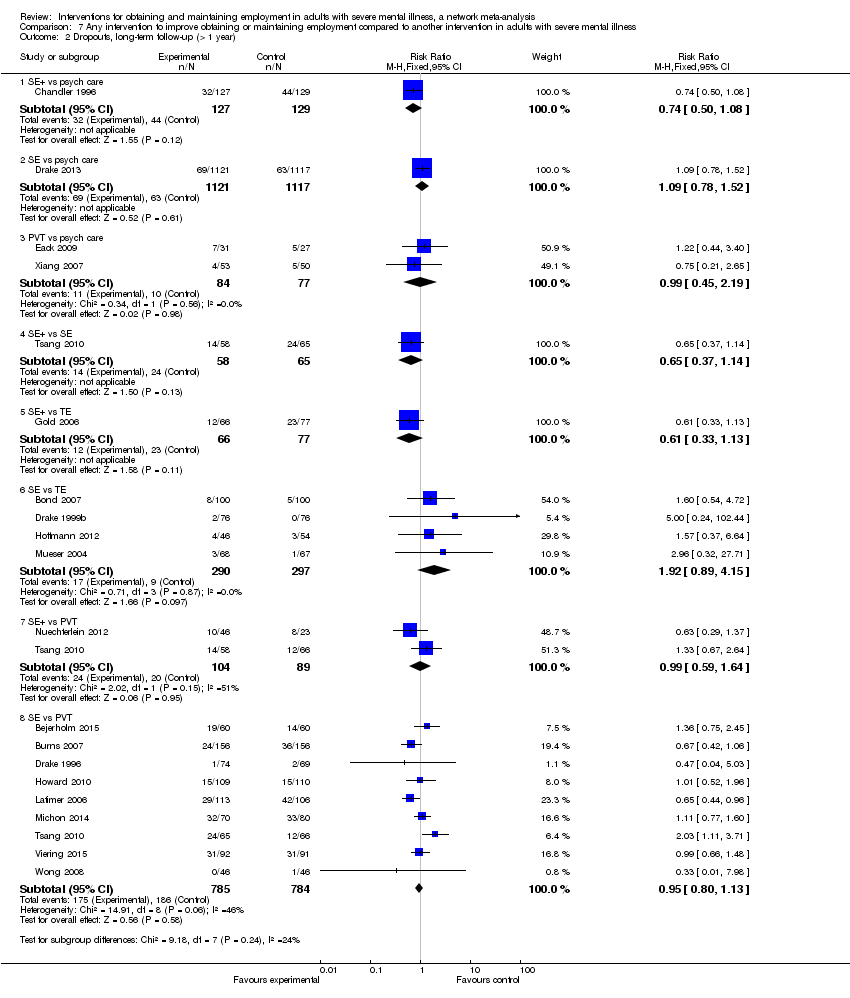
Comparison 7 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Dropouts, long‐term follow‐up (> 1 year).

Comparison 8 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 1 Hospital admissions, short‐term follow‐up (≤ 1 year).
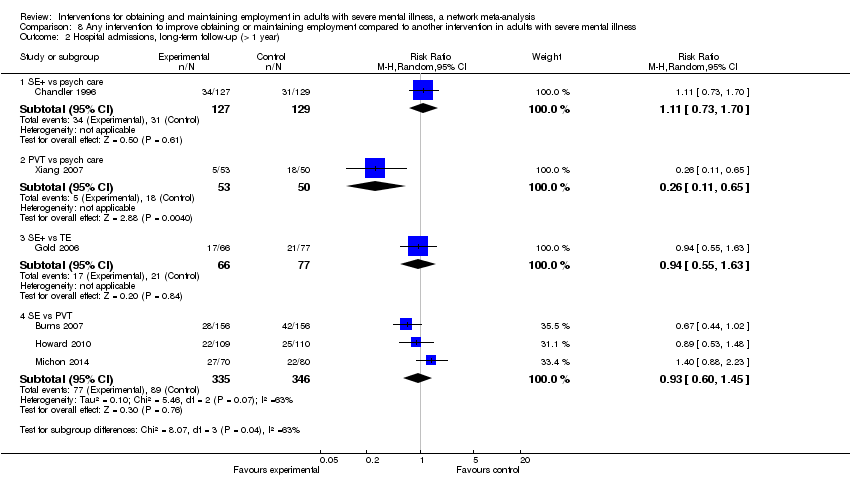
Comparison 8 Any intervention to improve obtaining or maintaining employment compared to another intervention in adults with severe mental illness, Outcome 2 Hospital admissions, long‐term follow‐up (> 1 year).
| Patient or population: adults with severe mental illness Settings: (community) psychiatric care/mental health services Interventions/comparisons: interventions for obtaining competitive employment: augmented supported employment, supported employment. pre‐vocational training, transitional employment, psychiatric care only | ||||||
| Comparison | Illustrative comparative risksa (95% CI) | Relative effect | SUCRA | No of participants | Quality of the evidence | |
| Assumed likelihood with control intervention | Corresponding likelihood with intervention | |||||
| Outcome: Number of participants who obtained competitive employment (follow up > 1 year) | ||||||
| Augmented supported employment vs. psychiatric care only | 187 per 1000 (18.7%) | 712 per 1000 (372 to 1366) | RR 3.81 (1.99 to 7.31) | 98.5% | 256 (1 study) | ⊕⊕⊕⊝ |
| Supported employment vs. psychiatric care only | 187 per 1000 (18.7%) | 509 per 1000 (290 to 890) | RR 2.72 (1.55 to 4.76) | 76.5% | 2238 (1 study) | ⊕⊕⊝⊝ |
| Pre‐vocational training vs. psychiatric care only | 187 per 1000 (18.7%) | 236 per 1000 (136 to 410) | RR 1.26 (0.73 to 2.19) | 40.3% | 161 (2 studies) | ⊕⊝⊝⊝ |
| Transitional employment vs. psychiatric care only | 187 per 1000 (18.7%) | 187 per 1000 (95 to 367) | RR 1.00 (0.51 to 1.96) | 17.2% | 0 | ⊕⊕⊝⊝ |
| Augmented supported employment vs. transitional employment | 223 per 1000 (22.3%) | 845 per 1000 (522 to 1369) | RR 3.79 (2.34 to 6.14) | 212 (2 studies) | ⊕⊕⊝⊝ | |
| Supported employment vs. transitional employment | 223 per 1000 (22.3%) | 604 per 1000 (401 to905) | RR 2.71 (1.80 to 4.06) | 87 (4 studies) | ⊕⊕⊕⊝ | |
| Pre‐vocational training vs. transitional employment | 223 per 1000 (22.3%) | 281 per 1000 172 to 457) | RR 1.26 (0.77 to 2.05) | 0 | ⊕⊕⊝⊝ | |
| Augmented supported employment vs. pre‐vocational training | 263 per 1000 (26.3%) | 794 per 1000 (494 to 1280) | RR 3.02 (1.88 to 4.87) | 193 (2 studies) | ⊕⊕⊝⊝ | |
| Supported employment vs prevocational training | 263 per 1000 (26.3%) | 568 per 1000 (419 to 771) | RR 2.16 (1.59 to 2.93) | 1569 (9 studies) | ⊕⊝⊝⊝ | |
| Augmented supported employment vs supported employment only | 457 per 1000 (45.7%) | 640 per 1000 420 to 978) | RR 1.40 (0.92 to 2.14) | 205 (3 studies) | ⊕⊕⊝⊝ | |
| GRADE Working Group grades of evidence | ||||||
| a The corresponding likelihood of obtaining employment with intervention (and its 95% CI) is based on the assumed likelihood with the control intervention (= median likelihood across studies) and the relative effect of the intervention (and its 95% CI). c We did not downgrade because of reporting bias as insufficient studies contributed to network treatment estimates to allow us to draw meaningful conclusions. 1 We downgraded one level due to study limitations (majority moderate risk of bias studies). 2 We downgraded one level due to study limitations (majority moderate risk of bias studies) and one level due to inconsistency (predictive interval for intervention effect includes effect that would have different interpretation and loop inconsistency). 3 We downgraded one level due to study limitations (majority moderate risk of bias studies), one level because of inconsistency (predictive interval for intervention effect includes effect that would have different interpretations) and one level for imprecision (CIs include values favouring either intervention). 4 We downgraded one level due to study limitations (majority moderate risk of bias studies) and one level because of imprecision (CIs include values favouring either intervention). 5 We downgraded two levels due to study limitations (majority high risk of bias studies). 6 We downgraded one level due to study limitations (majority moderate risk of bias studies). 7 We downgraded one level due to study limitations (majority moderate risk of bias studies) and one level because of imprecision (confidence intervals include values favouring either intervention). 8 We downgraded one level due to study limitations (majority moderate risk of bias studies) and one level because ofinconsistency (moderate level of heterogeneity). 9 We downgraded one level due to study limitations (majority moderate risk of bias studies), one level due to inconsistency (predictive interval for intervention effect includes effect that would have different interpretation and loop inconsistency) and one level because of detected publication bias (small study effects). 10 We downgraded one level due to study limitations (majority moderate risk of bias studies) and one level because of imprecision (confidence intervals include values favouring either intervention). | ||||||
| Study | Country | Follow‐upa | N | Mean age | Male participants | Diagnosis (majority) | Working history (majority) |
| China | short | 90 | 36 | 63% | Psychotic disorder | yes | |
| USA | short | 212 | N/A | 60% | Psychotic disorder | N/A | |
| USA | short | 50 | 46 | N/A | Psychotic disorder | yes | |
| Sweden | long | 120 | 38 | 56% | Psychotic disorder | yes | |
| USA | short | 122 | 36 | 64% | Psychotic disorder | yes | |
| USA | long | 131 | 25 | 69% | Psychotic disorder | yes | |
| USA | short | 86 | 35 | 51% | Psychotic disorder | yes | |
| USA | long | 200 | 39 | 64% | Psychotic disorder | no | |
| USA | short | 90 | 44 | 79% | Psychotic disorder | yes | |
| Europe (UK, Italy, Germany, Netherlands, Bulgaria, Switzerland) | long | 312 | 38 | 60% | Psychotic disorder | yes | |
| UK | long | 123 | 38 | 59% | Psychotic disorder | yes | |
| USA | long | 256 | N/A | 43% | Psychotic disorder | N/A | |
| UK | short | 159 | 24 | 73% | Psychotic disorder | yes | |
| USA | short | 132 | 25 | 53% | Psychotic disorder | N/A | |
| USA | long | 143 | 37 | 48% | Psychotic disorder | N/A | |
| USA | long | 152 | 39 | 39% | Psychotic disorder | N/A | |
| USA | long | 2238 | 44 | 47% | Affective disorder | N/A | |
| USA | short | 21 | 46 | 95% | Affective disorder + substance dependence | yes | |
| USA | short | 100 | 46 | 99% | Affective disorder + substance dependence | yes | |
| USA | long | 58 | 26 | 69% | Psychotic disorder | N/A | |
| USA | short | 34 | 19 | 67% | N/A | no | |
| USA | long | 143 | N/A | 38% | Psychotic disorder | yes | |
| Switzerland | long | 100 | 34 | 65% | Affective disorder | yes | |
| UK | long | 219 | 38 | 67% | Psychotic disorder | yes | |
| Australia | short | 41 | 21 | 81% | Psychotic disorder | yes | |
| Australia | short | 146 | 20 | 67% | Psychotic disorder | yes | |
| Canada | short | 150 | 40 | 62% | Psychotic disorder | yes | |
| Canada | short | 24 | 32 | 71% | Psychotic disorder | N/A | |
| USA | long | 219 | 42 | 57% | Psychotic disorder | yes | |
| USA | long | 68 | 30 | 65% | Psychotic disorder | N/A | |
| USA | long | 69 | 33 | 70% | Psychotic disorder | N/A | |
| USA | long | 48 | 38 | 55% | Psychotic disorder | yes | |
| USA | long | 34 | 44 | 59% | Psychotic disorder | yes | |
| Netherlands | long | 151 | 35 | 74% | Psychotic disorder | yes | |
| USA | long | 135 | 41 | 61% | Psychotic disorder | yes | |
| USA | long | 69 | 25 | 67% | Psychotic disorder | N/A | |
| UK | short | 1037 | N/A | 55% | Psychotic disorder | yes | |
| Japan | short | 37 | 41 | 49% | N/A | yes | |
| USA | short | 89 | 45 | 100% | Affective disorder +substance abuse/dependence | yes | |
| USA | long | 177 | 38 | 55% | Psychotic disorder | yes | |
| China | short | 97 | 36 | 62% | Psychotic disorder | yes | |
| China | long | 189 | 35 | 49% | Psychotic disorder | yes | |
| USA | short | 58 | 51 | 64% | Psychotic disorder | yes | |
| Switzerland | long | 183 | 43 | 47% | Affective disorder | yes | |
| Australia | short | 208 | 32 | 69% | Psychotic disorder | N/A | |
| USA | short | 28 | N/A | 96% | Psychotic disorder | N/A | |
| China | long | 92 | 34 | 60% | Psychotic disorder | N/A | |
| China | long | 103 | 38.6 | 47% | Psychotic disorder | N/A | |
| aFollow‐up: short ≤ 1 year; long > 1 year. bSecondary outcomes: 1 = maintaining employment | |||||||
| Study | Comparison intervention main group | Comparison intervention subgroups | Secondary outcomesb | Included in meta‐analysis | Included in network met‐analysis |
| SE+ vs SE+ | SE+ symp vs SE+ symp | 1, 4, 5, 6 | no | no | |
| TE vs psych care | CT vs psych care | 7 | yes | no | |
| TE vs psych care | SWS vs psych care | 2, 7, 6 | yes | no | |
| SE vs PVT | hf IPS vs job skills training | 1, 2, 3,5 6, | yes | yes | |
| PVT vs psych care | Job skills training vs psych care | 2, 6 | yes | no | |
| TE vs TE | Not classified CH accelerated vs gradual | 2, 6, 7 | no | no | |
| SE+ vs SE | SE+job skills training vs lfIPS | 1, 2, 7 | yes | no | |
| SE vs TE | hf IPS vs CH | 1,2,3,4,5,6 | yes | yes | |
| SE vs PVT | hf IPS vs job skills training | 1, 2,, 6, 7 | yes | no | |
| SE vs PVT | hf IPS vs job skills training | 1, 3, 4, 5, 6, 7 | yes | yes | |
| SE vs SE | hf IPS vs lf IPS | 1, 3, 4,5, 6, 7, | no | yes (sub) | |
| SE+ vs psych care | SE+ACT vs ACT | 2, 5, 6, 7 | yes | no | |
| SE+ vs SE | SE+motivational interviewing vs hf IPS | 1, 2, 6 | yes | no | |
| TE vs psych care | CH vs psych care care | , 6, 7 | yes | no | |
| SE vs PVT | lf IPS vs job skills training | 4, 5, 6 | yes | yes | |
| SE vs TE | hf IPS vs SWS | 2, 3, 4, 5, 6 | yes | yes | |
| SE vs psych | hf IPS vs psych | 1, 2, 4, 5, 6 | yes | yes | |
| SE+ vs SE+ | unclassified SE+TE+contingency management vs SE+TE | 1, 6 | no | no | |
| SE+ vs SE+ | unclassified SE+TE+contingency management vs SE+TE | 1 | no | no | |
| PVT vs psych care | CT vs psych care | 4, 6 | yes | yes | |
| SE vs TE | lf IPS vs SWS | 1 | yes | no | |
| SE vs TE | hf IPS vs SWS | 1,2,3,4,5,6 | yes | yes | |
| SE vs TE | hf IPS vs SWS | 1, 2, 3, 4, 5, 6 | yes | yes | |
| SE vs PVT | hf IPS vs job skills training | 4, , 5, 6, 7 | yes | yes | |
| SE vs psych | hf IPS vs psych | 1, 6 | yes | no | |
| SE vs psych | hf IPS vs psych | 6 | yes | no | |
| SE vs TE | hf IPS vs SWS | 1, 2, 3, 6 | yes | no | |
| SE+ vs SE | SE+symp vs hfIPS | 1, 2 | yes | no | |
| SE vs PVT | hf IPS vs job skills training | 2, 6 | yes | yes | |
| Psych care vs psych care | Not classified ACT+multifamily groups vs ACT+crisis family intervention | 2, 4 | no | no | |
| SE+ vs TE | ACT+SE vs SWS | 1, 2 | yes | yes | |
| SE+ vs SE | SE+symp vs lf IPS | 1, 4, 7, 6 | yes | yes | |
| SE+ vs SE | SE+symp vs lf IPS | 1, 4 | yes | yes | |
| SE vs PVT | hf IPS vs job skills training | 1, 2, 3, 4, 5, 6, 7 | yes | yes | |
| SE vs TE | hf IPS vs CH | 1, 2, 3, 4, 6 | yes | yes | |
| SE+ vs PVT | SE+job vs SST | 6 | yes | yes | |
| SE vs psych care | lf IPS vs psych care | 2, 6, 7 | yes | no | |
| SE vs PVT | hf IPS vs job skills training | 1, 2, 6 | yes | no | |
| TE vs PVT | SWS vs job skills training | 1, 2, 3, 6 | yes | no | |
| SE+ vs SE+ | ACT+SE vs SE+TE | 1, 6 | yes | yes(sub) | |
| PVT vs psych care | SST vs psych care | none | yes | no | |
| SE+ vs SE vs PVT | SE+symp vs hf IPS vs job skills training | 1, 5, 6 | yes | yes | |
| SE vs PVT | hf IPS vs job skills training | 1, 2, 3, 6 | yes | no | |
| SE vs PVT | lf IPS vs job skills training | 6 | yes | yes | |
| SE vs SE | lf IPS vs hfIPS | 1, 6 | no | no | |
| TE vs psych care | SWS vs psych care | 1, 2, 7 | yes | no | |
| SE vs PVT | hf IPS vs job skills training | 1, 2, 3, 6 | yes | yes | |
| PVT vs psych care | SST vs psych care | 4, 6, 7 | yes | yes | |
| (sub) = included in subgroup network meta‐analysis only. ACT: assertive community treatment | |||||
| SE+ | ||||
| 1.40 (0.92 to 2.14) | SE | |||
| 3.02 (1.88 to 4.87) | 2.16 (1.59 to 2.93) | PVT | ||
| 3.79 (2.34 to 6.14) | 2.71 (1.80 to 4.06) | 1.26 (0.77 to 2.05) | TE | |
| 3.81 (1.99 to 7.31) | 2.72 (1.55 to 4.76) | 1.26 (0.73 to 2.19) | 1.00 (0.51 to 1.96) | Psych care |
| Network meta‐analysis estimates of intervention effect (RR with 95% CI). The column intervention is compared with the row intervention. RR > 1 favours the column intervention. | ||||
| Psych care: psychiatric care only | ||||
| Intervention | SUCRA | mean rank |
| SE+ | 98.5 | 1.1 |
| SE | 76.5 | 1.9 |
| PVT | 40.3 | 3.4 |
| TE | 17.2 | 4.3 |
| Psychiatric care only | 17.5 | 4.3 |
| SUCRA = surface under the cumulative ranking curve | ||
| SE + job | |||||||||||
| 0.82 (0.09 to 7.17) | SE + symp | ||||||||||
| 1.03 (0.10 to 11.00) | 1.26 (0.22 to 7.04) | SE + TE | |||||||||
| 0.89 (0.11 to 7.18) | 1.08 (0.29 to 4.04) | 0.86 (0.28 to 2.63) | SE + ACT | ||||||||
| 1.73 (0.23 to 12.82) | 2.10 (0.93 to 4.76) | 1.67 (0.37 to 7.63) | 1.94 (0.69 to 5.44) | hf IPS | |||||||
| 2.08 (0.25 to 17.21) | 2.53 (1.14 to 5.63) | 2.02 (0.38 to 10.58) | 2.34 (0.68 to 7.99) | 1.20 (0.62 to 2.35) | lf IPS | ||||||
| 5.46 (0.63 to 47.60) | 6.64 (2.09 to 21.16) | 5.29 (0.94 to 29.68) | 6.14 (1.64 to 22.89) | 3.16 (1.39 to 7.18) | 2.63 (0.91 to 7.58) | CH | |||||
| 2.38 (0.30 to 18.92) | 2.89 (0.91 to 9.16) | 2.30 (0.58 to 9.09) | 2.67 (1.19 to 5.96) | 1.37 (0.61 to 3.09) | 1.14 (0.40 to 3.27) | 0.44 (0.14 to 1.38) | SWS | ||||
| 4.62 (0.59 to 35.99) | 5.62 (2.44 to 12.95) | 4.47 (0.92 to 21.76) | 5.19 (1.69 to 15.95) | 2.67 (1.70 to 4.20) | 2.22 (1.17 to 4.23) | 0.85 (0.33 to 2.16) | 1.94 (0.77 to 4.89) | Job | |||
| 1.63 (0.44 to 6.08) | 1.98 (0.36 to 11.06) | 1.58 (0.22 to 11.27) | 1.83 (0.36 to 9.25) | 0.94 (0.21 to 4.27) | 0.78 (0.15 to 4.09) | 0.30 (0.05 to 1.66) | 0.69 (0.14 to 3.41) | 0.35 (0.07 to 1.70) | SST | ||
| 0.68 (0.06 to 8.42) | 0.83 (0.09 to 7.35) | 0.66 (0.06 to 7.14) | 0.77 (0.09 to 6.28) | 0.39 (0.05 to 2.98) | 0.33 (0.04 to 2.76) | 0.12 (0.01 to 1.11) | 0.29 (0.04 to 2.32) | 0.15 (0.02 to 1.17) | 0.42 (0.05 to 3.56) | CT | |
| 2.97 (0.51 to 17.40) | 3.61 (1.03 to 12.63) | 2.88 (0.60 to 13.87) | 3.34 (1.10 to 10.13) | 1.72 (0.67 to 4.42) | 1.43 (0.45 to 4.55) | 0.54 (0.16 to 1.90) | 1.25 (0.42 to 3.71) | 0.64 (0.23 to 1.83) | 1.82 (0.56 to 5.93) | 4.35 (0.73 to 25.98) | Psych care |
| Network meta‐analysis estimates of intervention effect (RR, 95% CI). The column intervention is compared with the row intervention. RR > 1 favours the column intervention. | |||||||||||
| CH: Clubhouse | |||||||||||
| Intervention | SUCRA | mean rank |
| SE + symp | 80.3 | 3.2 |
| CT | 78.4 | 3.4 |
| SE + ACT | 77.8 | 3.4 |
| SE + TE | 69 | 4.4 |
| SE + job | 68.4 | 4.5 |
| Hf IPS | 51.9 | 6.3 |
| SST | 51.8 | 6.3 |
| lf IPS | 42.4 | 7.3 |
| SWS | 35.8 | 8.1 |
| Psychcare | 25.8 | 9.2 |
| Job | 10.6 | 10.8 |
| CH | 7.9 | 11.1 |
| SUCRA = surface under the cumulative ranking curve | ||
| Comparison | evidence | confidence | reasons for downgrading |
| SE + vs psych care | mixed | moderate | study limitationsa |
| SE vs psych care | indirect | low | study limitationsa;inconsistencyb,c |
| PVT vs psych care | mixed | very low | study limitationsa; inconsistencyb;imprecisiond |
| TE vs psych care | indirect | low | study limitationsa; imprecisiond |
| SE + vs TE | mixed | low | study limitationse |
| SE vs TE | mixed | moderate | study limitationsa |
| PVT vs TE | indirect | low | study limitationsa; imprecisiond |
| SE + vs PVT | mixed | low | study limitationsa inconsistencyf |
| SE vs PVT | mixed | very low | study limitationsa; inconsistencyb,c; publication biasg |
| SE + vs SE | mixed | low | study limitationsa; imprecisiond |
| Ranking | very low | study limitationsa; inconsistencyh; publication biasg | |
| a Dominated by evidence at high or moderate risk of bias. c Moderate level of heterogeneity. e Dominated by evidence at high risk of bias. f Loop inconsistency ROR 3.156 (95% CI 1.46 to 6.84). g Evidence for small study effects. h Evidence for inconsistency in the network (P = 0.001). psych care: psychiatric care only | |||
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Obtaining competitive employment, short‐term follow‐up (≤ 1 year) Show forest plot | 18 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 SE vs psych care | 3 | 1087 | Risk Ratio (M‐H, Random, 95% CI) | 1.79 [0.94, 3.40] |
| 1.2 PVT vs psych care | 2 | 171 | Risk Ratio (M‐H, Random, 95% CI) | 8.96 [1.77, 45.51] |
| 1.3 TE vs psych care | 4 | 422 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.88, 1.45] |
| 1.4 SE vs TE | 3 | 231 | Risk Ratio (M‐H, Random, 95% CI) | 3.49 [1.77, 6.89] |
| 1.5 SE vs PVT | 2 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 2.52 [1.21, 5.24] |
| 1.6 TE vs PVT | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.59, 1.04] |
| 1.7 SE+ vs SE | 3 | 143 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.37, 2.25] |
| 2 Obtaining competitive employment, long‐term follow‐up (> 1 year) Show forest plot | 22 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 SE+ vs psych care | 1 | 256 | Risk Ratio (M‐H, Random, 95% CI) | 4.32 [1.49, 12.48] |
| 2.2 SE vs psych care | 1 | 2238 | Risk Ratio (M‐H, Random, 95% CI) | 1.51 [1.36, 1.68] |
| 2.3 PVT vs psych care | 2 | 161 | Risk Ratio (M‐H, Random, 95% CI) | 2.19 [1.07, 4.46] |
| 2.4 SE+ vs TE | 2 | 212 | Risk Ratio (M‐H, Random, 95% CI) | 2.45 [1.69, 3.55] |
| 2.5 SE vs TE | 4 | 587 | Risk Ratio (M‐H, Random, 95% CI) | 3.28 [2.13, 5.04] |
| 2.6 SE+ vs PVT | 2 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 5.42 [1.08, 27.11] |
| 2.7 SE vs PVT | 9 | 1570 | Risk Ratio (M‐H, Random, 95% CI) | 2.31 [1.85, 2.89] |
| 2.8 SE+ vs SE | 3 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [1.03, 3.65] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Weeks in competitive employment, short‐term follow‐up (≤ 1 year) Show forest plot | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 SE+ vs SE | 1 | 32 | Mean Difference (IV, Random, 95% CI) | ‐1.46 [‐3.38, 0.46] |
| 1.2 SE vs TE | 2 | 187 | Mean Difference (IV, Random, 95% CI) | 4.18 [1.27, 7.09] |
| 1.3 SE vs PVT | 1 | 58 | Mean Difference (IV, Random, 95% CI) | 6.89 [1.26, 12.52] |
| 1.4 SE vs psych care | 2 | 131 | Mean Difference (IV, Random, 95% CI) | 4.87 [0.37, 9.37] |
| 1.5 TE vs PVT | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 6.70 [‐1.76, 15.16] |
| 1.6 TE vs psych care | 1 | 10 | Mean Difference (IV, Random, 95% CI) | ‐4.39 [‐17.75, 8.97] |
| 2 Weeks in competitive employment, long‐term follow‐up (> 1 year) Show forest plot | 11 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 SE+ vs SE | 3 | 154 | Mean Difference (IV, Random, 95% CI) | 10.09 [0.32, 19.85] |
| 2.2 SE+ vs PVT | 1 | 47 | Mean Difference (IV, Random, 95% CI) | 22.79 [15.96, 29.62] |
| 2.3 SE vs TE | 4 | 587 | Mean Difference (IV, Random, 95% CI) | 17.36 [11.53, 23.18] |
| 2.4 SE vs PVT | 5 | 390 | Mean Difference (IV, Random, 95% CI) | 11.56 [5.99, 17.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Days to first competitive employment, short‐term follow‐up (≤ 1 year) Show forest plot | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 SE vs TE | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐26.60 [‐98.53, 45.33] |
| 1.2 SE vs PVT | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | ‐35.94 [‐121.73, 49.85] |
| 1.3 TE vs PVT | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 12.60 [‐23.53, 48.73] |
| 2 Days to first competitive employment, long‐term follow‐up (> 1 year) Show forest plot | 6 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 SE+ vs TE | 1 | 62 | Mean Difference (IV, Fixed, 95% CI) | ‐142.80 [‐238.70, ‐46.90] |
| 2.2 SE vs TE | 3 | 205 | Mean Difference (IV, Fixed, 95% CI) | ‐64.86 [‐115.95, ‐13.77] |
| 2.3 SE vs PVT | 2 | 96 | Mean Difference (IV, Fixed, 95% CI) | ‐35.01 [‐105.21, 35.19] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Obtaining non‐competitive employment, short‐term follow‐up (≤ 1 year) Show forest plot | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 SE+ vs SE | 2 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.15, 17.22] |
| 1.2 SE vs TE | 2 | 187 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.18, 6.84] |
| 1.3 SE vs PVT | 2 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.39, 2.06] |
| 1.4 SE vs psych care | 1 | 900 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.61, 2.00] |
| 1.5 TE vs PVT | 1 | 89 | Risk Ratio (M‐H, Random, 95% CI) | 3.82 [2.24, 6.53] |
| 1.6 TE vs psych care | 2 | 78 | Risk Ratio (M‐H, Random, 95% CI) | 4.27 [0.00, 4883.69] |
| 1.7 PVT vs psych care | 1 | 122 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.12, 72.23] |
| 2 Obtaining non‐competitive employment, long‐term follow‐up (> 1 year) Show forest plot | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 SE+ vs TE | 2 | 212 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.12, 1.66] |
| 2.2 SE+ vs psych care | 1 | 256 | Risk Ratio (M‐H, Random, 95% CI) | 44.69 [6.25, 319.49] |
| 2.3 SE vs TE | 4 | 587 | Risk Ratio (M‐H, Random, 95% CI) | 0.22 [0.08, 0.63] |
| 2.4 SE vs PVT | 4 | 582 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.47, 3.53] |
| 2.5 SE vs psych care | 1 | 2238 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.76, 1.40] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quality of life, long‐term follow up (> 1 year) Show forest plot | 9 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.1 SE+ vs psych care (QOLI) | 1 | 256 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.79 [‐1.05, ‐0.54] |
| 1.2 SE vs psych care (QOLI) | 1 | 2238 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [0.06, 0.23] |
| 1.3 SE vs TE (QOLI) | 2 | 352 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.16, 0.26] |
| 1.4 SE+ vs SE (PWI) | 1 | 114 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.33 [‐0.04, 0.70] |
| 1.5 SE vs TE (W‐QLI objective) | 1 | 100 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.14 [‐0.53, 0.26] |
| 1.6 SE vs TE (W‐QLI subjective) | 1 | 100 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.50, 0.29] |
| 1.7 SE+ vs PVT (PWI) | 1 | 124 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.41 [0.06, 0.77] |
| 1.8 SE vs PVT (PWI) | 1 | 131 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.20, 0.48] |
| 1.9 SE vs PVT (MANSA) | 2 | 369 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.06, 0.35] |
| 1.10 SE vs PVT (QOLP) | 1 | 312 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.22, 0.22] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Mental health long‐term follow‐up (> 1 year) Show forest plot | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 SE vs psych care (SFHS) | 1 | 2238 | Mean Difference (IV, Random, 95% CI) | 2.88 [1.78, 3.98] |
| 1.2 PVT vs psych care (PANSS positive symptoms) | 1 | 103 | Mean Difference (IV, Random, 95% CI) | ‐2.48 [‐3.95, ‐1.01] |
| 1.3 PVT vs psych care (PANSS negative symptoms) | 1 | 103 | Mean Difference (IV, Random, 95% CI) | ‐1.61 [‐2.99, ‐0.23] |
| 1.4 PVT vs psych care (PANSS general symptoms) | 1 | 103 | Mean Difference (IV, Random, 95% CI) | ‐1.86 [‐3.09, ‐0.63] |
| 1.5 PVT vs psych care (composite index, multiple scales) | 1 | 58 | Mean Difference (IV, Random, 95% CI) | ‐7.09 [‐326.22, 312.04] |
| 1.6 SE vs TE (PANSS positive symptoms) | 1 | 200 | Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐1.71, 1.67] |
| 1.7 SE vs TE (PANSS negative symptoms) | 1 | 200 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐2.79, 1.19] |
| 1.8 SE vs TE (PANSS general psychopathology) | 1 | 200 | Mean Difference (IV, Random, 95% CI) | ‐2.69 [‐7.58, 2.20] |
| 1.9 SE vs TE (BPRS) | 1 | 152 | Mean Difference (IV, Random, 95% CI) | ‐1.90 [‐5.69, 1.89] |
| 1.10 SE vs PVT (HADS anxiety) | 1 | 312 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.88, 1.08] |
| 1.11 SE vs PVT (HADS depression) | 1 | 312 | Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐1.08, 0.88] |
| 1.12 SE vs PVT (MHI) | 1 | 150 | Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐8.63, 2.63] |
| 1.13 SE vs PVT (PANSS positive symptoms) | 1 | 312 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.93, 1.13] |
| 1.14 SE vs PVT (PANSS negative symptoms) | 1 | 312 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.38, 0.98] |
| 1.15 SE vs PVT (PANSS general psychopathology) | 1 | 312 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐1.34, 2.14] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Dropouts, short‐term follow‐up (≤ 1 year) Show forest plot | 13 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 SE vs psych care | 3 | 1087 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.41, 1.10] |
| 1.2 PVT vs psych care | 1 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 102.04] |
| 1.3 TE vs psych care | 2 | 182 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.43, 1.06] |
| 1.4 SE vs TE | 2 | 187 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.78 [0.84, 3.77] |
| 1.5 SE vs PVT | 2 | 148 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.36 [0.56, 3.30] |
| 1.6 TE vs PVT | 1 | 89 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.92 [0.19, 79.40] |
| 1.7 SE+ vs SE | 2 | 119 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.43, 1.67] |
| 2 Dropouts, long‐term follow‐up (> 1 year) Show forest plot | 19 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 SE+ vs psych care | 1 | 256 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.50, 1.08] |
| 2.2 SE vs psych care | 1 | 2238 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.78, 1.52] |
| 2.3 PVT vs psych care | 2 | 161 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.45, 2.19] |
| 2.4 SE+ vs SE | 1 | 123 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.37, 1.14] |
| 2.5 SE+ vs TE | 1 | 143 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.33, 1.13] |
| 2.6 SE vs TE | 4 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.89, 4.15] |
| 2.7 SE+ vs PVT | 2 | 193 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.59, 1.64] |
| 2.8 SE vs PVT | 9 | 1569 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.80, 1.13] |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Hospital admissions, short‐term follow‐up (≤ 1 year) Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 SE vs psych care | 1 | 900 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.74, 1.73] |
| 1.2 TE vs psych care | 4 | 422 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.30, 1.15] |
| 1.3 SE vs PVT | 1 | 90 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.76, 2.01] |
| 2 Hospital admissions, long‐term follow‐up (> 1 year) Show forest plot | 6 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 SE+ vs psych care | 1 | 256 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.73, 1.70] |
| 2.2 PVT vs psych care | 1 | 103 | Risk Ratio (M‐H, Random, 95% CI) | 0.26 [0.11, 0.65] |
| 2.3 SE+ vs TE | 1 | 143 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.55, 1.63] |
| 2.4 SE vs PVT | 3 | 681 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.60, 1.45] |

