مقیاس ارزیابی رفتاری نوزادان (NBAS) و سیستم مشاهدات رفتاری نوزاد تازه متولد شده (NBO) در حمایت از مراقبان و بهبود پیامدها در مراقبان و نوزادان آنها
Referencias
منابع مطالعات واردشده در این مرور
منابع مطالعات خارجشده از این مرور
منابع مطالعات در حال انجام
منابع اضافی
منابع دیگر نسخههای منتشرشده این مرور
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 30 Mother‐infant pairs assigned to 1 of the 3 treatment groups: control (group I), explanation only (group II), demonstration only (group III) Number randomised to each group: 10 Participant mothers:
Participant infants:
| |
| Interventions | Control group: while the NBAS was performed on infants of mothers in this group, the mothers received no immediate feedback on their infants. Instead they received a class on infant furnishings. Explanation only: NBAS was performed on the infants, and following each assessment the investigator met with mother and explained the performance of the infant. Demonstration group: mothers observed the investigator performing NBAS on their infants and saw both stimuli and responses.The explanations were ongoing rather than at the end of session. | |
| Outcomes | Study outcomes: Price Adaptation Scale (PAS). A 21‐item instrument designed to measure the quality of reciprocity in mother‐infant interaction. Timing of outcome assessment: 10 days postpartum Outcome observer: a graduate student had been trained with the PAS rating system; this observer was unaware of treatment group to which the mothers were assigned. First assessment was 24‐48 h following delivery (pre‐test) and second observation was made at 10 days postpartum. Assessment was done between groups I vs III, groups I vs II, and group II vs III to find out whether instructions received about their neonate's capacities and behaviours influence the caregiver‐infant interaction at 10 to 12 days postpartum. | |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Eligible mother‐infant pairs were randomly assigned to 1 of 3 treatment groups; however, the method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment was not described. |
| Blinding of participants and personnel (performance bias) | High risk | No information was provided about whether the mothers in the study knew about their own or other treatment conditions. |
| Blinding of outcome assessment (detection bias) | Low risk | The raters were unaware of the treatment group to which the mothers were assigned. |
| Incomplete outcome data (attrition bias) | Low risk | No missing data |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes reported |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 44 Fathers were assigned to 1 of the 2 groups: experimental, control Number randomised to each group: 22 Participant fathers:
Analysis of variance revealed no significant socioeconomic differences between the control and experimental groups. Participant infants: not specified | |
| Interventions | Experimental group: the researcher demonstrated the NBAS to father and mother together. Immediate and continuing feedback as well as a terminal summary statement was given to the parents during the examination. Control group: NBAS was performed on the infants by the researcher, and a summary statement was given to the parents. No actual demonstration was provided. | |
| Outcomes | Study instruments:
Timing of outcome assessment: 8 weeks postpartum (as a home visit). Outcome observer: first demonstration of NBAS was carried out 2 to 3 days following delivery (pre‐test), and second observation was made at 8 weeks postpartum. Assessment was undertaken to identify whether demonstrating NBAS would affect quality and frequency of father‐infant interaction, paternal attitude towards caretaking, paternal involvement in caretaking, perception of infant difficultness and quality of interaction. | |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Eligible fathers were randomly assigned to experimental or control group using alternating allocation |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | Blinding of outcome assessors was not undertaken. NBAS demonstrations and postpartum home visits were both undertaken by the principal investigator. |
| Incomplete outcome data (attrition bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 125 Mothers were assigned to 1 of 2 groups: experimental (infant‐centred, NBAS‐based), control (mother‐centred; interview‐based) Number randomised to each group: 59 experimental, 66 control Participant mothers:
Participant infants:
| |
| Interventions | Experimental group: at day 3 in the hospital, and again at days 14 and 30 at home, the mother was invited to become a "participant observer" as the infant was examined with the NBAS by an experienced clinician with established reliability in using the NBAS as preventive intervention in the newborn period. After the administration of the NBAS, the examiner provided a narrative summary of the assessment, encouraging the parent to ask or discuss any questions, concerns or related issues. Control group: an experienced clinician interviewed the mother at days 3, 14 and 30, while a second, trained, reliable examiner administered and scored the NBAS with the infant in a separate room. After the interview, the mother was given a general summary of her infant's performance on the NBAS by the examiner, excluding specific guidelines for caregiving based on the observations of the infant during the NBAS. | |
| Outcomes | Study instruments:
Timing of outcome assessment: at 4 months age of the infant (at a laboratory). Outcome observer: Intervention protocols were administered on 3 successive days during the first month postpartum; at 3 days in the hospital and at 14 and 30 days at home. 3 touch points during the first month were implemented to allow 3 successive NBAS administration. Final outcome assessed at 4 months in the laboratory. | |
| Notes | Conflicts of interests: not mentioned Source of funding: grant R01 MH37234 from the National Institute of Mental Health, grant from the William Randolph Hearst Foundation and grant from the Mailman Family Foundation to TB Brazelton (PI) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Eligible mothers were randomly assigned to 1 of the 2 intervention groups; method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | Blinding was undertaken; coders were blind to infant IUGR and maternal intervention status. |
| Incomplete outcome data (attrition bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 67 Participants assigned to 1 of 4 groups: mother and father (experimental group I); only mother (experimental group II), mother and father (control group I); only mother (control group II) Number randomised to each group: 15 in each experimental group; 15 in each control group (after attrition) Participant both parents or mothers only:
Participant infants: not described | |
| Interventions | On 2nd, 3rd or 4th day of the infant's life and following the assessment of each newborn on the NBAS by a certified examiner, families participating in the project were allocated to 1 of 4 treatment groups. Experimental groups: actively elicited from their newborns a series of reflexes and behaviours culled from the NBAS under the guidance of the experimenter, now serving as facilitator – the same individual who had previously administered the NBAS to the infant. The facilitator neither touched nor held the infant during these sessions; rather she guided the parent through the procedure, describing what the parents were to do, alerting them as to what to look for, asking them what they observed, and discussing the significance of the behavioural phenomena under examination. Control group: received a detailed verbal report of the exam and their babies' performance from the examiner/facilitator. More specifically, the examiner described in step‐by‐step fashion exactly what she did during the exam, how the baby behaved, and the meaning of the infant's responses. | |
| Outcomes | Study instruments used
Timing of outcome assessment: during the prenatal phase of the project (preintervention) and again at 1, 3 and 9 months postpartum Outcome observer: Intervention protocols were administered on second, third or fourth day and outcomes observed at 1, 3 and 9 months postpartum to find out whether NBAS performed under the guidance of the experimenter yielded better results than control condition. | |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Eligible families were randomly assigned to 1 of 4 intervention groups; method of sequence generation was not described. |
| Allocation concealment (selection bias) | Low risk | The individual scheduling the prenatal visit was unaware of the group to which each family was assigned. |
| Blinding of participants and personnel (performance bias) | High risk | Blinding was achieved by providing the scheduler with a packet of manila folders in a specified order. Each time a prenatal visit was scheduled, the top folder in the stack was selected and the family's name and address were placed on the folder. The folders had been pre‐coded for treatment condition. |
| Blinding of outcome assessment (detection bias) | Low risk | The only people with knowledge of group assignment were: the author, who did not collect any of the data in the investigation, and the prenatal visitor, who also administered the Brazelton exam and the intervention. |
| Incomplete outcome data (attrition bias) | High risk | Attrition: 7 out of 67 participants. Participant attrition was not selective, either as a function of group assignment or background factors. No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Tota number randomised: 54 Participants assigned to 1 of 4 groups: experimental group I (used only NBAS), experimental group II (MABI), experimental group III (NBAS plus MABI), control group (NBAS not used on babies). Experimental groups II and III were not taken for calculation purposes. Number randomised to each group: 13 experimental, 13 control Participant mothers: all drug‐using mothers Characteristics of the participant both parents/mothers only:
Participant infants: no information | |
| Interventions | Experimental group: Brazelton only; mothers were taught how to elicit items from the Brazelton exam on their own infants. Control group: the experimenter talked with the mother about the conditions of the study and about her baby. | |
| Outcomes | Study instruments used:
Timing of outcome assessment: at 4 weeks (during a home visit) Outcome observer: a blind observer scored a feeding session and rated various aspects using the study instruments | |
| Notes | Conflicts of interests: not mentioned Source of funding: Virginia Commonwealth University (VCU) Faculty Grant‐in‐Aid awarded to the second author, and National Insitute on Drug Abuse (NIDA) Grant DA‐06094 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Eligible families were randomly assigned to 1 of the 4 intervention groups; no information provided about sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | A blinded observer scored feeding sessions and carried out the rating. |
| Incomplete outcome data (attrition bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 40 Participants assigned to 1 of 4 groups: maternal orientation to newborn behaviour using Infant Behaviour Assessment Record (IBAR) adapted from NBAS (intervention‐ group III); feeding observation and maternal orientation to newborn behaviour using IBAR adapted from NBAS (group I); only feeding observation (group II); no action (group IV) Number randomised to each group: 10 in each group Participant mothers:
Participant infants:
| |
| Interventions | Experimental (group III): used IBAR adapted from NBAS, as a guideline for orienting the mothers to their newborn behaviour on third day. Group I: instructed to feed baby as if no one were present at day 2 and on day 3 maternal orientation as for group III. Group II: only feeding observation on day 2 Group IV: no action | |
| Outcomes | Study instruments used:
Timing of outcome assessment: at 2 weeks (during a home visit) Outcome observer: each mother was asked to breastfeed her baby. Scoring of NCAFS was completed following each observation | |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participant mothers were assigned a group number from a cyclic rotating table of numbers. |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | High risk | Investigator singularly involved in all phases of data collection ‐ random allocation, pre‐testing, behavioural orientation and post‐testing |
| Incomplete outcome data (attrition bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 40 Participants were assigned to 1 of the 2 groups: experimental (used NBAS on babies), control (NBAS not used on babies) Number randomised to each group: 20 experimental, 20 control Participant mothers:
Participant infants:
| |
| Interventions | Experimental group: NBAS session was conducted on babies in the presence of the mother Control group: NBAS was not conducted | |
| Outcomes | Study instruments used:
Timing of outcome assessment: within 2 days of delivery, at 3 to 4 weeks after delivery and finally at 4 months after delivery Outcome observer: a researcher blind to the status of the family in the research assessed the final outcome at 4 months after delivery. | |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Eligible mother‐infant dyads were randomly assigned to 1 of the 4 intervention groups; sequence generation was not described |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | A blinded researcher assessed the final session and carried out the rating. |
| Incomplete outcome data (attrition bias) | High risk | 3 control dyads and 1 experimental dyad completed participation through time 2 but not time 3. Therefore, follow‐up sample size comprised of 17 participant dyads in the control group and 19 participant dyads in the experimental group. No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 75 Mother‐infant pairs assigned to 1 of 3 treatment groups: experimental, control group I, control group II Number randomised to each group: 25 Participant mothers:
Participant infants:
| |
| Interventions | Experimental group: parents received NBAS; parts of this examination were demonstrated to the mothers on the morning of their discharge, approximately 30 minutes following a feeding. A semi‐structured discussion modified for the individuality of each child was held with mothers and included an assessment of the child's strengths, individual differences and the importance of mutual interaction. Control group I: infants received standard newborn care. Physical examinations were performed in the absence of parents. Mothers were visited by one of the authors every day during stay, and any concerns raised by the mothers were addressed. Control group II: infants received standard care + complete physical examinations in front of the mothers on the morning of discharge. During the examination the physician discussed the normal physical findings and emphasised the robustness of the infants. | |
| Outcomes | Study instruments used:
Timing of outcome assessment: at 1 and 3 months of age; for 35 minutes at 1 month and for 45 minutes at 3 months Outcome observer: an observer blind to the group status assessed the outcome. | |
| Notes | Conflicts of interests: not mentioned Source of funding: supported by a biomedical research support grant from the University of Rochester and by a grant from the Commonwealth Fund (No. 74‐26) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Eligible newborns were randomly assigned to 1 of the 3 groups; method of sequence generation was not described |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | An observer blind to the group status assessed the outcome. |
| Incomplete outcome data (attrition bias) | Low risk | Out of the 75 who agreed to participate, 3 families dropped out of the study (2 before the first home visit, and 1 after the first home visit). No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: recruitment of infants January‐August 2004 | |
| Participants | Total number randomised: 41 Mother‐infant pairs assigned to 1 of 2 treatment groups: intervention, control Number randomised to each group: 25 intervention, 13 control (after attrition) Participant mothers: fluent in English Participant infants:
| |
| Interventions | Experimental group: received 7 home visits from an early‐intervention provider certified in the NBO system, who administered the NBO with the parents and discussed characteristics of the infant. The final visit took place no later than the end of 12th week of the infant's life. Control group: received traditional, early intervention, home‐based delivery; 7 home visits from an early‐intervention provider not certified in the NBO | |
| Outcomes | Study instruments used: Home Visiting Index (HVI). A 25‐item scale, which requests the parents to rate, on a 4‐point scale, their degree of agreement with statements about the quality of early intervention service delivery Timing of outcome assessment: at the end of the third month Outcome observer: the same early intervention service provider who gave the HVI to the parents at the end of the third month | |
| Notes | Conflicts of interests: both authors disclose their affiliation with the Brazelton Institute, Department of Newborn Medicine, Children's Hospital Boston. The second author is Director of the Brazelton Institute and assisted in the design of the neurobehavioural intervention under study. Source of funding: Robert Wood Johnson Health & Society Scholars Program at University of Wisconsin‐Madison and the Noonan Family Foundation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned to either NBO or usual care group using "simple randomisation procedures" – sequence generation was not provided. |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | Of the 41 infants recruited, 3 were not followed due to inability to contact the family after initial referral. No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | High risk | Both authors disclose their affiliation with the Brazelton Institute, Department of Newborn Medicine, Children's Hospital Boston. The second author is Director of the Brazelton Institute and assisted in the design of the neurobehavioural intervention under study. |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 42 Mother‐infant pairs assigned to 1 of the 3 treatment groups: father treatment (group 1), mother treatment (group II), control (group III) Number randomised to each group: father treatment, 14; mother treatment, 14; control group, 12 (after attrition) Participant parents:
Participant infants:
| |
| Interventions | Experimental groups: a training session based on the NBAS with either the mother (mother treatment) or the father (father treatment) actively learning to administer the items and to observe her or his own infant's behaviour. Parents were told that these were some "games and exercises" to get to know their baby better. The treatment was given no sooner than the second day. The sessions were held in the mother's room for mothers and in a small room off the nursery for fathers. Control group: parents did not receive the training session or know that it existed. | |
| Outcomes | Study instruments used:
Timing of outcome assessment: in the hospital, at least 6 hours after the treatment, and at home at 4 weeks Outcome observer: the hospital measures were collected by 3 female assistants who were blind to group membership. The 4‐week measures consisted of questionnaires that were mailed to the participant's homes. Except for the assessment of father's caretaking, all measures were performed on both parents. | |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | All parents who met the criteria were randomly assigned to a treatment group by the throw of a die and did not differ in terms of parents' age and education or infant birth weight. |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | Parents unaware of other treatment groups |
| Blinding of outcome assessment (detection bias) | Low risk | Measures were collected by assistants who were blind to group membership. 4‐week measure included a mailed questionnaire |
| Incomplete outcome data (attrition bias) | Low risk | 2 members in the control group were lost to follow‐up at assessment at 4 weeks postpartum. No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: participants recruited between December and January 2001 | |
| Participants | Total number randomised: 112 Mother‐infant pairs assigned to 1 of the 2 groups: intervention, control Number randomised to each group: 57 (final stage 55) intervention, 55 (final stage 51) control Participant mothers: first‐time parent cohabiting with the father of the baby Participant infants:
| |
| Interventions | Intervention group: mothers received routine care plus NBO in the hospital at mothers' bedside and again at 1 month, postpartum home visit Control group: mothers received routine hospital care and a short‐attention, control home visit | |
| Outcomes | Study instruments used: Edinburgh Postnatal Depression Scale (EPDS) – a 10‐item, self‐report questionnaire to assess symptoms of postnatal depression during the previous week Timing of outcome assessment: at 1 month postpartum Outcome observer: EPDS was a self‐administered questionnaire at 1 month postpartum; not mentioned whether it was administered by an investigator blind to the group status or not | |
| Notes | No conflict of interest: author is director of the Brazelton Institute Source of funding: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A coin toss was used to randomly allocate eligible mothers to intervention and control groups. |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | 112 mothers had enrolled for the study, but at 1 month postpartum, there were only 106 mothers. No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | High risk | Author is director of the Brazelton Institute |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 40 Mother‐infant pairs assigned to 1 of the 2 groups: intervention, control Number randomised to each group: 20 (final stage 18) intervention, 20 (final stage 17) control Participant mothers: first‐time parent living with the father of the baby Participant infants:
| |
| Interventions | Intervention group: mothers received routine hospital care plus NBO in the hospital and again at 1 month, postpartum home visit plus NBO (for second time). Home visit at 4 months postpartum. Control group: mothers received routine hospital care and home visit at 1 month and 4 months. | |
| Outcomes | Study instruments used: the CARE‐Index Timing of outcome assessment: at 4 months postpartum Outcome observer: CARE‐Index was administered in the home by an examiner who had been trained in its administration and coding and who was blind to the status of the dyad. | |
| Notes | Conclict of interest: author is director of the Brazelton Institute Source of funding: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Mothers who consented to participate were randomly assigned either to intervention or control group. Method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | Final outcome was assessed by an examiner who was blind to the status of the dyad |
| Incomplete outcome data (attrition bias) | High risk | 40 mothers were initially allocated to the study, but at 4 months postpartum only 35 mother‐infant dyads remained. |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | High risk | Author is director of the Brazelton Institute |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 48 Father‐infant pairs assigned to 1 of the 3 groups: experimental (group I), hospital control (group II), office control (group III) Number randomised to each group: 16 Participant fathers: married, older, white and college educated; they were skilled or professionally employed. These fathers were well prepared for childbirth, since most couples had attended the Lamaze childbirth education classes, and all couples had attended some form of prenatal classes. Participant infants:
| |
| Interventions | Experimental group: 2 × 30‐minute sessions were held with each father during the postpartum hospitalisation. The first when the infant was 12‐36 hours old and the second approximately 24 hours after the first session. These sessions were expressly for fathers, and mothers were not included. At the first session, a number of physical characteristics of the infant were pointed out. Some exercises were demonstrated and the father was given time to hold and interact with his infant. At the second session, the father was given an opportunity to hold and interact with his infant after demonstration of a standard number of behavioural items from NBAS. Hospital control group: these fathers spent the same amount of time with the investigator at the same postnatal time points and discussed the same information, but with a major difference. All information was presented through a prepared videotape of a typical normal newborn. Office control group: these fathers had no prior contact with the experiment except for the recruiting visit in the hospital. No educational information and no extra contact with their infants. | |
| Outcomes | Study instruments used: direct observations of behaviours made during infant's physical examination and subsequent ratings of behaviours made from videotape segments – these were sensitive measures of father‐infant interaction. Timing of outcome assessment: at 4 weeks of age of the infant. Outcome observer: infant was examined by the paediatric nurse practitioner while the baby was with the father. Selected father and infant behaviours were observed during the physical examination by an observer blind to the group status. | |
| Notes | Conflicts of interests: not mentioned Source of funding: supported in part by a Nurse‐Scientist pre‐doctoral fellowship (US Public Health Service (USPHS), Division of Nursing, Grant NU‐5008‐05) and a grant from the Developmental Psychobiology Endowment Fund, Department of Psychiatry, University of Colorado Medical Center. Dr Emde is supported by Research Scientist Award. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | First 2 groups (I and II) were randomly assigned to an experimental group or a hospital control group; method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome assessed by an observer unaware of the groups to which the participants belonged |
| Incomplete outcome data (attrition bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 20 Mother‐infant pairs assigned to 1 of 2 groups: experimental, control Number randomised to each group: 10 Participant mothers:
Participant infants:
| |
| Interventions | Experimental group: the intervention involved a teaching modelling session in which the investigator explained and demonstrated the infant's behavioural cues and responses to the mother using NBAS. The teaching plan was structured around 4 areas: interactive processes, motoric processes, organisation processes‐state control, and organisation processes‐response to stress. All of the interventions were scheduled around 1 of the infant's feeding times so that the infant would be awake and could be used in modelling the behaviours being discussed. Control group: NBAS was not used | |
| Outcomes | Study instruments used: assessment of Mother‐Infant Sensitivity. Mother‐infant interaction was measured using this instrument. Timing of outcome assessment: 10 to 14 days following delivery Outcome observer: study intervention was carried out 1 to 3 days after discharge from hospital in the first instance. An appointment was made with all mothers for a home visit 10‐14 days following delivery to observe another feeding session with the infant and obtain the post‐test data. The NBAS was also administered. | |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned to the control or the experimental group; no information provided about sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | Low risk | An observer unaware of the assignment of the mother to a group observed the feeding for the mother‐infant interaction. |
| Incomplete outcome data (attrition bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Number randomised: 25 Mother‐infant pairs assigned to 1 of 2 groups: intervention, control Number randomised to each group: 12 intervention, 13 control Participant mothers: not described Participant infants:
| |
| Interventions | Intervention group: at 34 weeks of age, intervention group mothers were invited to observe NBAS performed on their infants by a trained examiner with a second observer/recorder. Mothers were invited to ask questions during and after the examination. Control group: mothers were invited to observe a standard complete physical performed by an attending neonatologist and a second observer/recorder. Mothers were invited to ask questions during and after the examination. | |
| Outcomes | Study instruments:
Timing of outcome assessment: at 6 months corrected age of the baby Outcome observer: at 6 months corrected age. Mothers were interviewed using a semi‐structured format. | |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Mother‐infant pairs were randomly assigned to control and intervention groups; no information provided about sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | No information provided |
| Blinding of outcome assessment (detection bias) | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) | High risk | One control group participant refused follow‐up, and 4 were lost to follow‐up. They did not differ in income, demographic or medical characteristics. No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
| Methods | Design: parallel‐group, randomised trial Unit of allocation: participant Study dates: not reported | |
| Participants | Total number randomised: 48 Mother‐infant pairs assigned to 1 of 3 groups: experimental treatment (group I), control group (group II), or contrast treatment (group III) Number randomised to each group: 16 Participant mothers: white, middle‐class Participant infants: healthy, full‐term newborns | |
| Interventions | All infants were assessed using NBAS initially. Experiment treatment: active information through auditory, visual and tactile interaction. Mothers individually observed a 45‐minute demonstration of the NBAS conducted on their newborns, on second or third day of life after the examiner had assessed the newborn on NBAS before discharge from the hospital. The examiner, serving as facilitator, neither touched nor held the infant during these sessions; rather he talked the mother through the procedures and guided and encouraged her in eliciting infant responses. Control treatment: minimal information through auditory feedback. Immediately after the behavioural assessment of the newborn, the mother received a verbal summary of her infant's performance. The examiner described the baby's performance on the 4 categories of the profile, according to the priori cluster, and discussed the baby's performance with the new mother. This procedure allowed the investigator to alert the mother to characteristics of her newborn, based on its behavioural display, and provided the mother with the opportunity to talk about what she heard. Contrast treatment: passive observation with auditory and visual feedback. Mothers observed a 45‐minute demonstration of the NBAS conducted on their newborns. This procedure allowed the investigator to alert the mother to the characteristics of her newborn, based on its behavioural display, and also drew attention to specific infant behaviours and provided the mother with an opportunity to talk about what she was seeing. These mothers received a 1‐page summary of the demonstration 2 days later. | |
| Outcomes | Study instruments: pre‐coded checklist to assess mother‐infant interaction. Timing of outcome assessment: 4 and 6 weeks of age for the infant. Outcome observer: mother‐infant dyads were observed for 60 minutes on 1 occasion in the family's home, by 1 of the observers blind not only to experimental design but also to the purpose of the study. | |
| Notes | Conflicts of interests: not mentioned Source of funding: grant from the Penn State Division of Continuing Education | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomly assigned to 1 of the 3 treatment conditions; no information provided about sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) | High risk | The experimenter explicitly avoided telling mothers that the service provided would affect their parenting or their baby. However, one investigator administered all 3 treatments and thus was cognisant of group assignments. |
| Blinding of outcome assessment (detection bias) | Low risk | Observers were blind not only to the experimental design but also to the purpose of the study. |
| Incomplete outcome data (attrition bias) | Unclear risk | No information provided |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes were reported. |
| Other bias | Low risk | None |
APGAR: appearance, pulse, grimace, activity and respiration;IUGR: intrauterine growth retardation;MABI: Mother's Assessment of the Behaviour of her Infant; NBAS: Neonatal Behavioural Assessment Scale; NBO: Newborn Behavioural Observations system; PI: principal investigator; SD: standard deviation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| A derived "specialized application of NBAS" | |
| NBAS used as part of a wider intervention | |
| Used a variation of NBAS | |
| Not a randomised controlled trial | |
| Not a randomised controlled trial | |
| NBAS used as part of intervention with the Amazing Newborn DVD | |
| Intervention 'based on' NBAS | |
| NBAS part of broader package of care | |
| NBAS used in conjunction with MABI. | |
| Non‐randomised controlled trial; both control and intervention groups given NBAS | |
| Non‐randomised controlled trial | |
| Non‐randomised controlled trial | |
| Qualitative report of outcomes only (i.e. no date) | |
| NBAS used as part of intervention package – MITP. | |
| Intervention 'based on' NBAS; non‐randomised | |
| NBAS used as part of wider package of care | |
| Uses Newborn Individualized Developmental Care and Assessment Programme (NIDCAP) and Assessment of Preterm Infants' Behaviour (APIB) rather than NBAS | |
| Does not appear to be the NBAS | |
| Not a randomised controlled trial | |
| No information about how NBAS was used. | |
| NBAS used as part of wider intervention | |
| NBAS demonstrated on video | |
| NBAS as part of package with the MABI. | |
| NBAS as part of wider intervention package. |
MABI: Mother's Assessment of the Behaviour of her Infant; MITP: Mother Infant Transaction Program; NBAS: Neonatal Behavioural Assessment Scale.
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | What are the effects of supporting early parenting by increasing the understanding of the infant? A randomized community‐based trial |
| Methods | Design: cluster‐randomised trial |
| Participants | Study population: new families.
Exclusion criteria: parents or infants affiliated to special treatment elsewhere |
| Interventions | Intervention group: will receive NBO at 3 weeks after birth and in following visits up to 3 months Control group: will receive care as usual at 3 weeks after birth and in following visits up to 3 months |
| Outcomes |
|
| Starting date | 1 January 2017 |
| Contact information | Hanne Kronborg, Aarhus University, Denmark. E‐mail: [email protected] |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned Trials register number:NCT03070652 |
| Trial name or title | Understanding your newborn and adapting to parenthood (UNA): a randomised clinical effectiveness trial of the Newborn Behavioural Observations (NBO) for new families with maternal antenatal risk factors for postnatal depression (PND) |
| Methods | Design: randomised controlled trial |
| Participants | Study population: expectant first time single mothers and couples from the Royal Women’s Hospital and Bendigo Hospital in Australia. Target recuitment: this project aims to randomise n=150 expectant first time mothers screening positive for antenatal risk factors of PND. The study has so far screened n=218 first time mothers during pregnancy and of these women n=84 have screened positive for antenatal risk factors of PND and have been randomised into either the G1 comparison group or G2 intervention group. The project has also recruited n=80 first time fathers and of these participants, n=35 have been included in the randomised sample as above. |
| Interventions |
|
| Outcomes | G1 and G2 participants will complete the EPDS at 6 weeks and all three groups will complete an endpoint psychosocial questionnaire (including the EPDS and the PASS) at infant age 4 months. Additional endpoint data for G1 and G2 group participants will be collected on mother‐infant interaction, maternal depression diagnosis and infant development, using the Emotional Availability Scales, the SCID‐5 diagnostic interview depression module and the Bayley Scales of Infant Development respectively. |
| Starting date | 10 August 2017 |
| Contact information | Dr Susan Nicolson, Centre for Women’s Mental Health, [email protected] |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned Trials register number: not registered |
| Trial name or title | The effect of a Newborn Behavioral Observation System‐Early Intervention (NBO‐EI) model of care |
| Methods | Design: this is a pragmatic trial where infants from 5 early intervention programs in one state were randomized to receive an NBO‐EI model of care or usual care for the first 12 weeks corrected gestational age. Infants were followed up to 6 months corrected gestational age and a number of maternal and infant outcomes were measured. |
| Participants | Thirty‐two EI‐eligible infants participated. Of the total sample, 17 received the NBO‐EI model and 22 received usual EI care. |
| Interventions | Intervention group: received an NBO‐EI model of care. The NBO is an 18‐item neurobehavioral relationship‐based intervention that involves a shared observation of the infant with the parent and includes elicited maneuvers with the purpose of 1) identifying infant neurobehaviors, 2) interpreting these neurobehaviors in the context of the parent‐infant interaction and infant self‐regulation and intentions, with the goal of enhancing the parent‐infant relationship, the cornerstone of optimal infant neurodevelopment and function. Specifically, the NBO‐EI group received weekly home visits from an EI provider certified in the Newborn Observational (NBO) System up to 12 weeks corrected gestational age. Content of NBO‐EI home visits consisted of intervention strategies guided by the NBO. Specifically, at each home visit the EI service provider administered the NBO with the parents and discussed 1) the infant’s attempts and successes at self‐regulation and requests for support, 2) how the infant’s neurobehaviors contribute to the parent‐infant social interactional encounter and caregiver bonding. The intervention group received the NBO‐EI during their weekly home visit for up to twelve successive weeks. The final intervention visit took place no later than the end of the twelfth week of the infant’s life, when the infant was three months of age, adjusted for prematurity. After the final study visit, in accordance with federal mandates governing EI service delivery, EI families chose to continue with weekly home visits or modified their home visit schedule. Usual care group: the usual care (UC) group received traditional EI home‐based service delivery. The UC group received weekly home visits from an EI provider not certified in the NBO. The content of UC group home visits consisted of therapeutic and developmental activities deemed appropriate for the infant’s adjusted age and typically included visual tracking, reaching and grasping toys of a variety of textures, and tolerance of developmental play. The final study visit took place no later than the end of the twelfth week of the infant’s life, when the infant was three months of age, adjusted for prematurity. After the final study visit, in accordance with federal mandates governing EI service delivery, EI families chose to continue with weekly home visits or modified their home visit schedule. |
| Outcomes | Maternal depressive symptoms was collected using the Center for Epidemiologic Studies Depression Scale (CES‐D). The CES‐D asks mothers to report, on a 4‐point scale (0=rarely/none of the time to 3=all of the time), their frequency of symptoms for 20 scale items. Scores of 16 or greater indicate clinically significant depressive symptoms. The CES‐D was collected, via phone interview at the 3‐month and 6‐month follow‐up time, by an independent member of the study team who is blinded to the infant’s intervention group assignment. Parent‐infant interaction was collected using the Parent‐Child Early Relational Assessment (PCERA) . The PCERA measures parent’s and child’s affect and behavioral characteristics during a 5‐minute play observation using 29 parent items across 3 sub‐scales of parenting quality (positive affective involvement and verbalization; negative affect and behavior; and intrusiveness, insensitivity, and inconsistency) and 28 child items across 3 sub‐scales of infant emotional/behavioral regulation (positive affect, communicative, and social skills; quality of play, interest, and attentional skills; and dysregulation and irritability). For the this study, we utilized scores for the 3 parent and 3 child sub‐scales. Sub‐scale scores range from 1 (negative relational quality) to 5 (positive relational quality). PCERA scores were ascertained from a 5‐minute video clip taken by the EI home visitor (NBO‐EI and usual care groups) at 3 months and 6 months corrected gestational age. The 3‐month video will occur at the final study home visit. The 6‐month video coincided with the 6‐month eligibility / follow‐up evaluation that routinely occurs in MA EI programs. All videotapes will be reviewed and coded by an independent researcher trained in the PCERA. Parent’s perceptions of the quality of their interaction with their infant and the extent to which their home visitor facilitated optimal interaction was measured using the Home Visiting Index.[i] Home Visiting index (HVI) is a 25‐item scale that asks parents to rate, on a 4‐point scale (1=strongly agree and 4=strongly disagree) their degree of agreement with statements about the quality of EI service delivery. At the final study visit, parents were asked to complete the HVI and return it in a self‐addressed stamped envelope to the study team. Infant self‐regulation was collected using the Bayley Scales of Infants Development (BSID), Adaptive scale. The BSID, Adaptive Scale was collected, via phone interview at the 3‐month and 6‐month follow‐up time, by an independent member of the study team who is blinded to the infant’s intervention group assignment. Cognitive and personal‐social, function was collected using the Battelle Developmental Inventory (BDI‐2) cognitive and personal‐social sub‐scales. Batelle scores were collected via videotaped EI eligibility evaluation (at 6 months postterm) by an independent member of the study team who is blinded to the infant’s intervention group assignment. [i] NugentJK. Home visiting index. Brazelton Institute, Children’s Hospital, Boston; 2003 |
| Starting date | 1 November 2016 |
| Contact information | Beth M McManus, PT, MPH, ScD, [email protected], Mobile: 617‐529‐8138 |
| Notes | Conflicts of interests: not mentioned Source of funding: not mentioned Trials register number: nor registered |
EPDS: Edinburgh Postnatal Depression Scale; NBO: Newborn Behavioral Observations system.
Data and analyses
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quality of caregiver‐infant interaction: postintervention Show forest plot | 7 | 304 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.90, ‐0.17] |
| Analysis 1.1  Comparison 1 NBAS or NBO versus control, Outcome 1 Quality of caregiver‐infant interaction: postintervention. | ||||
| 2 Caregiver mental health (maternal depression): EPDS postintervention score Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.2  Comparison 1 NBAS or NBO versus control, Outcome 2 Caregiver mental health (maternal depression): EPDS postintervention score. | ||||
| 3 Caregiver mental health (maternal depression): EPDS postintervention score (dichotomous data) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| Analysis 1.3  Comparison 1 NBAS or NBO versus control, Outcome 3 Caregiver mental health (maternal depression): EPDS postintervention score (dichotomous data). | ||||
| 4 Infant social, emotional, cognitive and motor development Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.4  Comparison 1 NBAS or NBO versus control, Outcome 4 Infant social, emotional, cognitive and motor development. | ||||
| 4.1 BSID: mental development | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 BSID: psychomotor development | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Caregiver perception of infant Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| Analysis 1.5  Comparison 1 NBAS or NBO versus control, Outcome 5 Caregiver perception of infant. | ||||
| 6 Caregiver knowledge of infant behaviour (multiple choice factual questions) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.6  Comparison 1 NBAS or NBO versus control, Outcome 6 Caregiver knowledge of infant behaviour (multiple choice factual questions). | ||||
| 7 Caregiver stress Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| Analysis 1.7  Comparison 1 NBAS or NBO versus control, Outcome 7 Caregiver stress. | ||||
| 7.1 PSI: parent‐related sources of stress | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 PSI: child‐related sources of stress | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quality of caregiver‐infant interaction Show forest plot | 7 | 304 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.90, ‐0.17] |
| Analysis 2.1 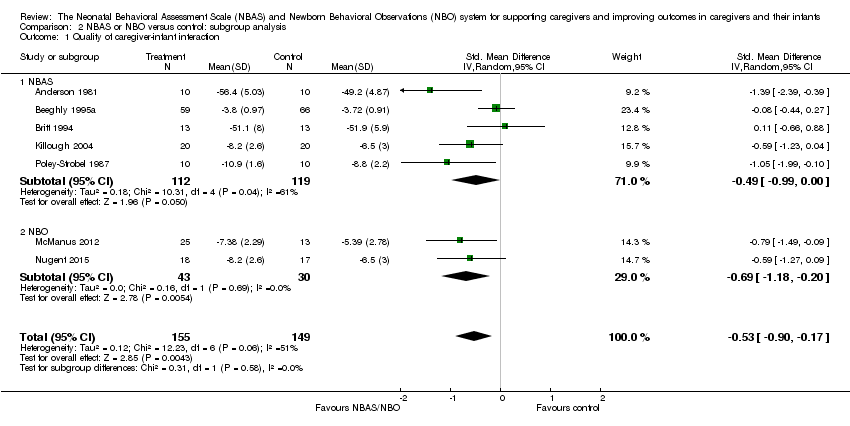 Comparison 2 NBAS or NBO versus control: subgroup analysis, Outcome 1 Quality of caregiver‐infant interaction. | ||||
| 1.1 NBAS | 5 | 231 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.99, ‐0.00] |
| 1.2 NBO | 2 | 73 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.18, ‐0.20] |
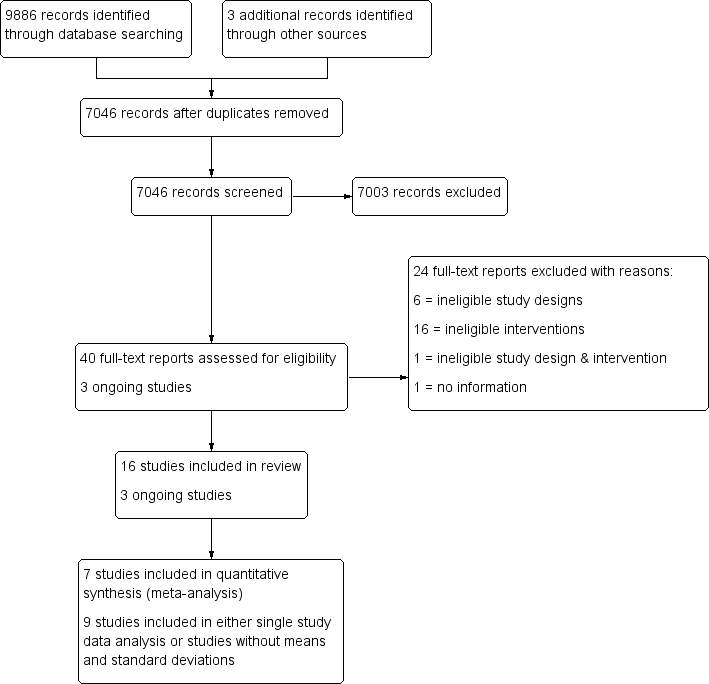
Study flow diagram.

Risk of bias summary: review authors' judgments about each risk of bias item for each included study.

Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.

Comparison 1 NBAS or NBO versus control, Outcome 1 Quality of caregiver‐infant interaction: postintervention.

Comparison 1 NBAS or NBO versus control, Outcome 2 Caregiver mental health (maternal depression): EPDS postintervention score.
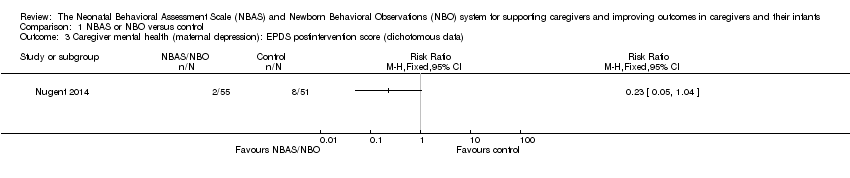
Comparison 1 NBAS or NBO versus control, Outcome 3 Caregiver mental health (maternal depression): EPDS postintervention score (dichotomous data).

Comparison 1 NBAS or NBO versus control, Outcome 4 Infant social, emotional, cognitive and motor development.

Comparison 1 NBAS or NBO versus control, Outcome 5 Caregiver perception of infant.
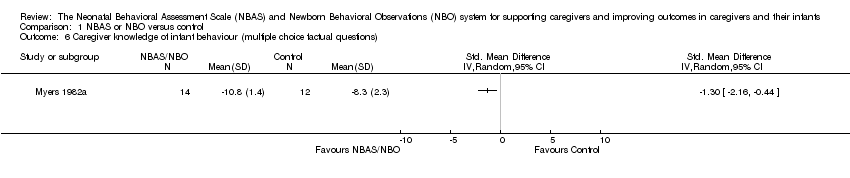
Comparison 1 NBAS or NBO versus control, Outcome 6 Caregiver knowledge of infant behaviour (multiple choice factual questions).

Comparison 1 NBAS or NBO versus control, Outcome 7 Caregiver stress.

Comparison 2 NBAS or NBO versus control: subgroup analysis, Outcome 1 Quality of caregiver‐infant interaction.
| NBAS or NBO versus control for caregiver‐infant interaction, caregiver mental health, and caregiver functioning | |||||
| Patient or population: caregiver‐infant dyads Settings: hospitals, clinics, home Intervention: NBAS or NBO Comparison: NBAS or NBO administered with no interaction | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect | Number of participants | Quality of the evidence | |
| Assumed risk | Corresponding risk | ||||
| Control group | NBAS or NBO | ||||
| Quality of caregiver‐infant interaction (parental sensitivity, attunement, etc.); continuous data Assessed at postintervention using validated assessment scales for caregiver‐infant interaction: higher scores indicate better outcome | The mean score for quality of caregiver‐infant interaction ranged across control groups from 3.72 to 51.90 | The mean caregiver‐infant interaction score in the intervention groups was 0.53 lower (0.90 lower to 0.17 lower) | — | 304 | ⊕⊕⊝⊝ |
| Caregiver mental health (depression), dichotomous data Assessed at postintervention using the EPDS; lower scores indicate less depression | Low‐risk population | RR 0.23 (0.05 to 1.04) | 106 (1 study) | ⊕⊕⊝⊝ | |
| 157 per 1000 | 36 per 1000 (8 to 163) | ||||
| Medium‐risk population | |||||
| NA | NA | ||||
| High‐risk population | |||||
| NA | NA | ||||
| Infant social, emotional, cognitive and motor development Assessed when infant aged 4 months, using the BSID; higher scores indicate better development | The mean score for infant mental development in the control group was 107.83 | The mean score for infant mental development in the intervention groups was0.13 lower (0.48 lower to 0.22 higher) | — | 125 (1 study) | ⊕⊕⊝⊝ |
| Caregiver perception of infant (parents' perception of the degree of difficult temperament of the infant) Assessed at postintervention, 8 weeks after delivery; higher score indicates better outcome | The mean score for caregiver perception of infant in the control group was 18.90 | The mean score for caregiver perception of the infant in the intervention group was 0.36 lower (0.95 lower to 0.24 higher) | — | 44 (1 study) | ⊕⊕⊝⊝ |
| Caregiver stress (maternal perceptions of her adjustment to the parenting role) Assessed when infant aged 4 months, using the PSI | The mean score for parent‐related caregiver stress in the control group was 2.19 | The mean score for parent‐related caregiver stress in the intervention groups was0.00 (0.35 lower to 0.35 higher) | — | 125 (1 study) | ⊕⊕⊝⊝ |
| Caregiver knowledge (related to infants' physical capacities, including reflexes and senses) Assessed at postintervention, using multiple choice factual questions; higher scores indicate better outcome | The mean score for caregiver knowledge in the control groups was8.30 | The mean score for caregiver knowledge in the intervention groups was 1.30 higher (0.44 to 2.16 higher) | — | 26 (1 study) | ⊕⊕⊝⊝ |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). | |||||
| GRADE Working Group grades of evidence | |||||
| 1Downgraded due to risk of bias due to poor quality research (e.g. limitations in design, including inadequate randomisation or allocation procedures, together with attrition, which ranged from 4% to 20% in seven studies – none of which conducted an intention‐to‐treat analysis), inconsistency for the main outcome due to high levels of heterogeneity for the NBAS; and indirectness in terms of the low levels of generalisability to wider risk groups within the population. 2Downgraded due to risk of bias due to poor quality research (e.g. limitations in design, including inadequate randomisation or allocation procedures, together with attrition, which ranged from 4% to 20% in seven studies – none of which conducted an intention‐to‐treat analysis), and indirectness in terms of the low levels of generalisability to wider risk groups within the population. | |||||
| Unit of analysis issues | Cluster‐randomised trials The randomisation of clusters can result in an overestimate of the precision of the results (with a higher risk of a type I error) when their use has not been compensated for in the analysis. Had we included a cluster‐RCT, we planned to explore whether the authors had adequately controlled for the effects of clustering in the study. When they had, and when there was little difference between the study designs, and when there was unlikely to be an interaction between the effect of the intervention and the choice of randomisation method, we planned to combine the data from the cluster‐RCT with data from individual RCTs. When the effects of clustering had not been controlled for properly, we planned to derive an estimate of the intracluster correlation coefficient (ICC) from the study or that of a similar population, and to report whether an ICC had been used and conduct sensitivity analyses to determine the effect of using an ICC. We also planned to assess the impact of including data from a cluster‐RCT on the inclusion of the study in the meta‐analyses using a sensitivity analysis to explore the effects of the randomisation method. However, no cluster RCTs were identified or included. |
| Trials with multiple treatments groups In the event that we had identified a multi‐arm study in which the NBAS and NBO had been compared with an alternative treatment and a control group, we planned to only extract data from two arms (e.g. NBAS and control group). In the event that we had identified a multi‐arm study in which the NBAS had been compared with the NBO and involved only one control group, we planned to combine the data from the NBAS and NBO arms for primary analyses and to conduct secondary, subgroup analyses and split the control group data. However, we identified no multiple treatment groups. | |
| Cross‐over trials Cross‐over trials are not possible with this type of intervention, and none were identified. | |
| Assessment of reporting bias | We planned to draw funnel plots (estimated differences in treatment effects against their standard error) if there was a sufficient number of included studies (e.g. more than 10), to identify asymmetry due to publication bias and other small study effects. We also planned to assess whether there had been selective reporting of outcomes and to assess the impact of this using a sensitivity analysis. However, there were insufficient studies to undertake this analysis. |
| Subgroup analysis and investigation of heterogeneity | We planned to explore possible reasons for heterogeneity by undertaking the following, additional subgroup analyses, scrutinising studies to determine the extent of between‐trial differences.
However, it was only possible to undertake subgroup analysis for NBAS versus NBO, due to the small number of studies. |
| Sensitivity analysis | We planned to conduct sensitivity analyses on the basis of method of sequence generation only, to assess the robustness of the results, but this was not possible due to the small number of studies. |
| NBAS: Neonatal Behavioral Assessment Scale; NBO: Newborn Behavioral Observations system; RCT: randomised controlled trial. | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quality of caregiver‐infant interaction: postintervention Show forest plot | 7 | 304 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.90, ‐0.17] |
| 2 Caregiver mental health (maternal depression): EPDS postintervention score Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3 Caregiver mental health (maternal depression): EPDS postintervention score (dichotomous data) Show forest plot | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Infant social, emotional, cognitive and motor development Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 BSID: mental development | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 BSID: psychomotor development | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Caregiver perception of infant Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6 Caregiver knowledge of infant behaviour (multiple choice factual questions) Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7 Caregiver stress Show forest plot | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 PSI: parent‐related sources of stress | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 PSI: child‐related sources of stress | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
| 1 Quality of caregiver‐infant interaction Show forest plot | 7 | 304 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.90, ‐0.17] |
| 1.1 NBAS | 5 | 231 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.99, ‐0.00] |
| 1.2 NBO | 2 | 73 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.18, ‐0.20] |

