Estrategias para la mejoría de la implementación de políticas o prácticas escolares dirigidas a los factores de riesgo de enfermedades crónicas
Referencias
References to studies included in this review
References to studies excluded from this review
References to ongoing studies
Additional references
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Trial name: School Nutrition Advances Kids (SNAK). Study design: Non‐randomised. Intervention duration: The study involved two overlapping cohorts: 1 year 9 month per cohort, 2 years 9 months both cohorts: Cohort 1: 2007‐2009. Cohort 2: 2008‐2010. Length of follow‐up from baseline: Follow‐up occurred in the next school year. Students in cohort 1 completed the baseline survey between November 2007 and March 2008 and the follow‐up survey between October and December 2008. Cohort 2 students completed baseline surveys between November 2008 and February 2009 and the follow‐up survey between October 2009 and January 2010. Differences in baseline characteristics: There were no significant differences among intervention groups with regard to school characteristics at baseline. There were some significant differences at baseline with regard to student dietary intake (all subsequent analyses adjusted for baseline dietary values). Table 2 reports difference at baseline in school characteristics. Some differences were apparent in school location and kitchen type but no P values were reported. Unit of allocation: School. Unit of analysis: School. | |
| Participants | School type: Middle Schools (7th and 8th grades). Region: Michigan, USA. Demographic/socioeconomic characteristics: Low‐income middle schools (the mean percentage of students eligible for free/reduced‐price meals for schools in the SNAK project was 68% (range, 50% to 98%), which was similar to all Michigan low‐income middle schools in 2007 (72%; n = 514). Inclusion/exclusion criteria: Inclusion: ‐ Having 50% or more of the students eligible for free or reduced‐price meals and having seventh and eighth grades within the same building (for follow‐up purposes). ‐ Having 50% or more of students eligible for free or reduced‐price meals. ‐ Having seventh and eighth grades within the same building. Number of schools allocated: Schools: 75 (54 intervention, 21 control). Student: 1777 Seventh Graders (completed baseline). 65 (3 intervention groups, 1 control group stated, but result reported according to 2 groups: intervention and control). Numbers by trial group: The study contained one control and three intervention groups. The intervention groups consisted of three different programs (or program combinations) 1) the Healthy Schools Action Team (HSAT), 2) the HSAT plus the School Nutrition Advances Kids Team (SNAK) and 3) the HSAT plus the Michigan State Board of Education (MSBE) nutrition policy. The sample sizes by trial group follow: n (controls baseline) = 21 n (controls follow‐up) = 20 completed some aspect of the project.17 completed FFQ. n (interventions baseline) = 54. n (HSAT baseline) = 24. n (HSAT + SNAK baseline) = 5. n (HSAT + MSBE POLICY baseline) = 25. n (interventions follow‐up) = 45 completed some aspect of the project. 38 completed the FFQ. n (HSAT follow‐up) = 18 completing some aspect and 16 with FFQ. n (HSAT + SNAK follow‐up) = 5 completing some aspect and 4 with FFQ. n (HSAT + MSBE POLICY follow‐up) = 22 completing some aspect and 18 with FFQ. Recruitment: Schools: Were recruited through an application for small grant funding with award values ranging from $2,000 to $4,600 with recruitment methods included direct mailings, e‐mails, and phone calls to eligible schools, as well as a posting on the Michigan Team Nutrition website. Students: Written parental consent and student assent were obtained. Recruitment rate: Schools: denominator unknown. Student: 20.6%. | |
| Interventions | Number of experimental conditions: 4 (3 intervention, 1 control, but reported according to 2 groups: intervention and control) Policies, practices or programs targeted by the intervention: The three policies, practices or programs implemented in this study were the HSAT program, the SNAK program and the MSBE nutrition policy. ‐ Schools completed the (HSAT) concerning healthy eating and nutrition and developed an action plan to improve school‐nutrition practices. ‐ Seventh‐grade student teams were formed (SNAK) wherein the students implemented nutrition education and marketing. ‐ The MSBE is a nutrition policy recommending that schools offer and promote healthy foods and beverages in all competitive venues. Implementation strategies: EPOC: Tailored interventions. ‐ The HSAT consisted of a tailored intervention (online assessment and action planning process). EPOC: Educational outreach visits. ‐ Provision of a facilitator (1 time to complete HSAT action plan). ‐ SNAK intervention group also received: facilitator/student meetings to assess student nutrition environment and policies. EPOC: External funding. ‐ Incentives ($1,000 to implement nutrition education or implement aspects of their action plan). ‐ SNAK intervention group also received: incentives: $1000 for students to implement student nutrition action plan Standardised ‐ Curriculum developed for facilitator/student meetings. ‐ MSBE nutrition policy intervention schools were also received: $1500 to compensate for any loss to food service revenue. EPOC: Local consensus processes. ‐ Coordinated School Health Team. MSBE nutrition policy intervention schools were also asked to: EPOC: Clinical practice guidelines. ‐ Implementation of policy (2003 MSBE Healthy Food and Beverage Policy) in cafeteria à la carte lines (during 2nd year). EPOC: Educational materials. ‐ Guidance documents and assistance were provided to schools, food service staff. Theoretical underpinning: Not reported. Description of control: Control group schools participated only in data collection during the study period and were offered the HSAT intervention after the last data collection point. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ Mean Nutrition Policy Change Score (Range: 0‐6) ‐ Mean Nutrition Education and/or Practice Change Score (Range: 0‐14) Data collection method: Survey: The Middle‐School School Environment and Policy Survey (SEPS) was completed either online or by paper (took approx. 30 minutes to complete). There were 2 versions of the survey: one for administrators/principals and one for food service directors/kitchen managers. Validity of measures used: Not reported/self‐report methods. The authors comment that the tool was trialled to establish face and content validity however, the tool was not subjective to rigorous validity testing. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Student‐level dietary intake. Data collection method: The Block Kids Food Frequency Questionnaire 2004 (ages 8‐17 years) at baseline and follow‐up. Validity of measures used: Not reported. | |
| Notes | Research funding: Supported by funding from the Robert Wood Johnson Foundation’s Healthy Eating Research Program, the Michigan Department of Community Health, and the USDA Supplemental Nutrition Assistance Program–Nutrition Education, supported by the Michigan Department of Human Services under contract numbers ADMIN‐07‐99010, ADMIN‐08‐99010, and ADMIN 09‐99010. Conflicts of interest: Authors report no competing financial interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomised. The schools were allocated based on preference and were not randomly assigned to group resulting in high risk of selection bias. |
| Allocation concealment (selection bias) | High risk | Non‐randomised trial and no indication that allocation was concealed resulting in high risk of selection bias. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All. No blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: Number of school‐initiated nutrition policy and practice changes. No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding; self‐report considered high risk. Outcome group: Mean nutrition policy change/nutrition education or practice change (SEP). No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding; self‐report considered high risk. Outcome group: Cafeteria à la carte and vending offerings. Self‐reported data from food service directors/other food service personnel and school administrators/principals. No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding; self‐report considered high risk. Outcome group: Process data. Unclear if personnel conducting analysis of various process data sources blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: Practice and Policy. Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. Outcome group: Changes in à la carte/vending during lunch. 18% missing/unreliable data overall, however relatively balanced across groups. Outcome group: Number of school‐initiated nutrition practice changes; and Number of school‐initiated nutrition policy changes. 5% missing data overall (n = 3), relatively balanced across groups but 2 schools missing from HSAT‐only group. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Potential confounding | Unclear risk | There is insufficient information to determine the risk of potential confounders. |
| Methods | Trial name: Pathways. Study design: Randomised controlled trial (not a cluster design). Food service component: 22 months. Health Behaviour and Anthropometric outcomes: 3 years (Spring 1997 – Spring 2000). Differences in baseline characteristics: Not reported. | |
| Participants | School type: Primary schools. Demographic/socioeconomic characteristics: Not reported. Inclusion/exclusion criteria: Inclusion: ‐ A projected 3rd grader enrolment of >15 children. ‐ > 90% of 3rd grade children of American Indian ethnicity. ‐ Retention from 3rd to 5th grade over the past 3 years of >70%. ‐ School meals prepared and administered on‐site. ‐ Availability of minimum facilities to deliver a physical activity program at the school. ‐ Approval of the study by school, community, and tribal authorities. Exclusion criteria: ‐ Schools that were considering closing or merging in the next 3 years. Number of schools allocated: ‐ 41 schools (Lunch program) ‐ 21 Intervention, 20 control. ‐ 39 schools (Breakfast program) ‐ 19 intervention, 20 control. Numbers by trial group: n (controls baseline) = 20/20. n (controls follow‐up) = 20/20. n (interventions baseline) = 19/21. n (interventions follow‐up) = 19/19. Recruitment: Students: Not reported. | |
| Interventions | Number of experimental conditions: 2 (1 Intervention, 1 Control). Policies, practices or programs targeted by the intervention: The practices targeted by the implementation intervention strategies were: ‐ To lower the fat in school breakfast and lunch: to reduce the fat contribution in meals to 30% or less of calories over five consecutive days. Implementation strategies: EPOC: Clinical practice guidelines: ‐ The food service intervention included the development of nutrient guidelines operationalised as behavioural guidelines. These behavioural guidelines included specific steps and skill‐building techniques for lowering the fat content of menu items. EPOC: Educational outreach visits: ‐ To support the behavioural guidelines, training sessions were conducted twice each school year with all food service staff. These training sessions were reinforced by at least five kitchen visits in the first year and eight or more visits to each school in the second and third years. EPOC: Educational materials: ‐ Materials and activities for the training sessions and kitchen visits were developed to reinforce the behavioural guidelines, and included posters, a videotape, food demonstrations, taste‐testing lower‐fat food items, and food quantity estimation activities. EPOC: Educational meetings: ‐ The food service working group, made up of nutrition research staff, some of whom were from the tribal communities involved in the study, met annually and held monthly conference calls to establish and carry out the intervention. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ % calories total fat breakfast (%) ‐ % energy from total fat Lunch (%) Data collection method: Data collection included information on all school breakfast and lunch meal items. Data on all foods offered were recorded on data forms completed by the school food service manager. Data included menus, recipes, vendor products with labels, and nutrient information on all prepared, processed, and packaged foods. All schools had a Pathways notebook with forms to be completed for each meal per day. On the form each food item was listed with a complete description of the food (e.g. raw carrots, canned whole kernel corn, etc.), the serving size, and the number of students served the food. Separate forms were completed for breakfast and lunch. The lead Pathways nutritionist at each of the four sites had overall responsibility for the data collection at their site. School breakfast menus and recipes were entered into the NUTRITION DATA SYSTEM. The nutrient composition was computed by taking the weighted nutrient average of all food items offered and served within each meal component category (milk, breads, fruits, vegetables, entrees, desserts (if served), and condiments) and summing the nutrient averages for all meal components to generate a nutrient total for a single school breakfast and for a single school lunch. Five‐day school breakfast averages were then calculated as well as five‐day school lunch averages. Validity of measures used: Not reported/self‐report methods. While the authors report that the data collector and cook/manager reviewed all data forms together for accuracy and completeness and that an individual with an advanced degree in nutrition or related area and/or a registered dietitian cross‐checked all forms for completeness and clarity, it is not explicitly reported that the tool/measurement methods have been validated or that a validated nutrition collection tool was used. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Adverse effects of the intervention on growth. Data collection method: Weight and height were measured annually. Validity of measures used: Not reported. Outcome relating to child diet, physical activity or weight status: Anthropometric data and dietary intake of total energy intake, percentage energy from fat. Data collection method: Anthropometric data : Height, weight, BMI and percentage body fat: ‐ Weight was measured with the use of self‐calibrating precision digital scales (Seca 770; Vogel and Halke GmbH, Hamburg, Germany) ‐ Height was measured with a fixed Shorr measuring board (Shorr Productions, Olney, MD). ‐ Two measurements were obtained and the average was recorded. ‐ Percentage body fat: estimated from bioelectrical impedance and anthropometry with the use of an equation developed and validated specifically for this study. Bioelectrical impedance was measured in duplicate with a single‐frequency tetrapolar plethysmograph (Valhalla Scientific, Valhalla, NY). Dietary Intake: 24 dietary recall and direct observation Validity of measures used: Anthropometric data: Percentage body fat equation was validated specifically for this study. Dietary Intake: Not reported. | |
| Notes | Other intervention components included: 1. Classroom curriculum: Two 45‐minute lessons were delivered by teachers each week for 12 weeks during the 3rd and 4th grades. This component was decreased to 8 weeks during 5th grade to allow for the follow‐up measurements during the final 2 months of the school year. 2. Physical activity was also a component of the intervention however, it is not reported on as Pathways research staff delivered some of this component to the school students. Consequently, this trial is reported as nutrition only trial. 3. Family involvement: Consisted of 1) family action packs, which were take‐home materials related to the Pathways intervention, including snack packs with samples of low‐fat foods and tips for preparing healthful snacks at home; and 2) family events at schools, which included cooking demonstrations and activities for healthier lifestyle, with the direct involvement of children. Research funding: Supported by funding grants HL‐50867, HL‐50869, HL50905, HL50885, and HL‐50907 from the National Heart, Lung, and Blood Institute. Conflicts of interest: Authors report no competing financial interests exist. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All/menu and recipes (nutrient and food groups) and school menu data collection. Given the nature of the intervention, participants and study personnel are likely to have been aware of study allocation and therefore high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: All/menu and recipe (nutrient and food groups) and school menu data collection. No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding; self‐report considered high risk. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: Low risk of attrition bias given that 39 of 41 schools that included breakfast were included in analysis. |
| Selective reporting (reporting bias) | Low risk | Design paper available and outcomes reported are consistent. http://ajcn.nutrition.org/content/69/4/760S.full.pdf+html |
| Methods | Trial name: HealthKick. Study design: Randomised controlled trial for implementation outcome. Intervention duration: 3 years. Differences in baseline characteristics: Not reported. | |
| Participants | School type: Elementary. Region: Cape Town, South Africa. Demographic/socioeconomic characteristics: Historically disadvantaged, low‐income communities from an urban area close to the city of Cape Town and from two rural areas outside of Cape Town, South Africa. Inclusion/exclusion criteria: Inclusion: ‐ Whether the principal expressed the need for a health promotion program to be implemented in the school. ‐ The presence of a shop or vendor selling food items at the school. ‐ Unhealthy diet and lack of physical activity among learners and teachers selected as a top health priority by the school principal. ‐ The view of the education district level managers of the potential of schools to effect changes, subjectively taking into account functionality (i.e. functional school‐based support team; school management team), ethos (co‐operation, will, inclination) and viability of school (e.g. results/performance of schools). ‐ Distance from the research office (not more than 105 minutes drive). Exclusion: ‐ School size (schools with less than 50 grade 4 learners were excluded). Number of schools allocated: 16. Numbers by trial group: n (controls baseline) = 8. n (controls follow‐up) = 8. n (interventions baseline) = 8. n (interventions follow‐up) = 8. Recruitment: Schools: The HealthKick study comprised sixteen eligible schools selected from the representative sample of 100 primary schools surveyed in two conveniently selected educations districts (one urban and one rural) in the Western Cape Province of South Africa during the formative phase of the study. Students: Not reported. Recruitment rate : Not clear. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The HealthKick Program which was an adaptation of the National School Health Policy and Implementation Guidelines (since replaced by the Integrated School Health Policy [ISHP]). The specific objectives were to: ‐ Promote healthy eating habits. ‐ To develop an environment within the school and community that promotes and facilitates these objectives through an action planning process (APP). Implementation strategies: EPOC: Local opinion leaders: ‐ To facilitate and drive the formal implementation of the APP, a champion (teacher) was identified at each school and they were encouraged to liaise with the project team whenever they required assistance. EPOC: Educational materials: ‐ An “educator’s manual” which contained an APP guide, a booklet for each action area containing guidelines for prioritising action as well as strategies to address identified priorities; the South African food‐based dietary guidelines; a poster listing the behaviour outcomes desired for the children; a poster for listing planned actions; and in 2011 a healthy lifestyle guide for teachers was included. ‐ A resource box with printed materials relating to a healthy lifestyle and its role in the school curriculum. ‐ A curriculum support manual integrating the HK goals with the existing Life Orientation curriculum, developed by an expert in a format familiar to educators. EPOC: Educational outreach visits: ‐ Optional intervention support was offered to the intervention schools in all four action areas during the three years of the intervention. The support took the form of structured activities by the research team to broaden the staff’s knowledge and skills around actions to support a healthy lifestyle. Furthermore, the research team kept in regular contact with the schools who were encouraged to call for assistance/support from the research team at any time. EPOC: Education meetings: ‐ Implementation and nutrition training workshop. Theoretical underpinning: Social Ecological model. Description of control: Principals at schools in the control arm received a booklet with “tips” for healthy schools and a guide to resources that could be accessed to assist in creating a healthier school environment. No further engagement took place between the research team and these schools except for the annual learner and environmental survey. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ School with shops selling fruit salad ‐ Vegetable gardens at schools ‐ Schools having nutrition‐related policies Data collection method: ‐ Data from the situational analysis were used as baseline information and an adapted version of the principal questionnaire and observational schedule used during the formative assessment which was completed annually at all 16 schools. ‐ Principals and school staff involved with the school nutrition program, tuck shops and vegetable gardens were interviewed using semi‐structured questionnaires. The interviews were conducted by members of the research team. As above and project officers acted as both implementers and outcome assessors. Interviews were recorded and transcribed, and the data managed with ATLAS.ti Qualitative Data Analysis. Initial data analysis involved coding the focus group data as group interviews (i.e. similar responses coded only once per group). Validity of measures used: Not reported/self‐report methods. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Student level dietary intake. Data collection method: 24‐hour recall. Validity of measures used: Not reported. | |
| Notes | Notes: Physical activity was also a goal of the HealthKick Program however, an implementation outcome was unavailable. Consequently, this trial is reported as a nutrition trial, with corresponding implementation strategies, and behavioural outcomes extracted. Research funding: Supported by funding from the World Diabetes Foundation. Conflicts of interest: Authors report no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The random sequence was generated by drawing the names of schools typed on folded white paper of exactly the same shape and size from a container. |
| Allocation concealment (selection bias) | Unclear risk | Although the authors' state that the allocation sequence was decided on by the project coordinator before the selection took place, there is no description of whether or not this was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: There is no mention that participants and personnel were blinded. Team members served as both implementers and researchers due to limited resources and therefore a high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: Self‐reported records were kept of all activities/events planned by the schools and the numbers that were carried out. Observation was not undertaken by an independent observer blind to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: No schools dropped out over the three years. |
| Selective reporting (reporting bias) | Low risk | There were no unreported process evaluation outcomes according to those planned in the published protocol. |
| Methods | Trial name: The trial was a brief intervention conducted as part of the Central Texas CATCH. The larger scope of the Central Texas CATCH program (reported by Hoelscher and colleagues 2001 and Springer and colleagues 2012) was excluded as the program did not report implementation outcomes appropriate for this review. Study design: Cluster‐randomised controlled trial. Intervention duration: 2009 to 2012. Length of follow‐up from baseline: Assessment occurred at 2 measurement periods, once in March and April of 2011, and again in March and April of 2012, during the second and third years of CATCH implementation, respectively. Differences in baseline characteristics: Schools were matched on size and composition of student ethnicity and economic disadvantage. Baseline demographic characteristics were reported to be similar between groups. Unit of allocation: Schools. Unit of analysis: School teachers. | |
| Participants | School type: Middle School (grades 6 – 8) Region: Central Texas Demographic/socioeconomic characteristics: Multi‐ethnic sample. Inclusion criteria: ‐ Grades (6‐ 8) Number of services allocated: 30. Numbers by trial group: Thirty central Texas middle schools were assigned to 1 of 3 conditions: training‐only (Basic), training plus facilitator support (Basic Plus), and training/facilitator support and a social marketing campaign (Basic Plus SM). There was 10 schools in each condition. Recruitment: Schools: Middle schools were selected to participate in the evaluation of the CATCH Middle School program. Recruitment rate: Schools: 30/32 = 94%. | |
| Interventions | Number of experimental conditions: 3 (3 intervention groups). Policies, practices or programs targeted by the intervention: To promote the adoption of activity breaks (Abs) by classroom teachers. Implementation strategies: Training‐only (Basic) received: EPOC: Local consensus process and clinical practice guidelines: ‐ A CATCH Middle School Abs guide was developed wherein PE and classroom teachers assisted in developing the guide by reviewing ABs from a variety of sources for ease of use and potential to generate PA and reinforce academic content. The guide included 55 Abs. Each school received 10 hard copies of the ABs and an electronic version to upload on the school’s shared drive so that all teachers could access them. EPOC: Local consensus process and educational meetings: ‐ A CATCH Team was developed at each school. The CATCH Team comprised faculty and staff members, parents, and community members, with one member designated the CATCH Champion. The team was charged with overseeing the implementation of the CATCH Program at their school, which included encouraging teachers to conduct ABs. CATCH program training's took place to promote the adoption of ABs by classroom teachers. Schools were required to send representatives from their CATCH Team to 8 CATCH training's conducted at regular intervals from September 2009 to January 2012. At these training's, CATCH Team members were introduced to the concept of ABs and were provided with research that supports the use of ABs to enhance academic performance. Basic Plus In addition to the aforementioned EPOC strategies this groups also received: EPOC: Educational outreach visits and tailored interventions: ‐ A CATCH facilitator was assigned and conducted monthly visits at these schools. During these visits they helped CATCH Teams devise strategies to promote ABs on their campus. These strategies included faculty meeting presentations explaining the benefits of ABs and regular teacher‐led demonstrations of ABs to faculty; placement of ABs on the school’s shared drive so teachers could access them easily; periodic e‐mail reminders to teachers; and scheduling of a school‐wide time to conduct ABs. Basic Plus SM In addition to all the aforementioned implementation strategies, this group also received: EPOC: Other: ‐ Social marketing campaigns to promote PA. Theoretical underpinning: Not reported. Description of control: There was no control group. All groups received varying amounts of implementation support (strategies). | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: Teacher reported frequency of AB implementation including: ‐ Have you conducted at least one AB this year? ‐ Percentage of teachers that conducted activity breaks weekly (%, N) ‐ Last week, did you conduct an activity break on at least 1 day? (%, N) Data collection method: Survey. The survey is a 15‐item, self‐administered questionnaire that includes items on teacher implementation of ABs, encouragement of specific health behaviours, and other process evaluation measures for the CATCH program. Validity of measures used: Not reported/self‐report methods. Outcome relating to staff knowledge, skills or attitudes: Teacher self‐efficacy to implement ABs Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Not reported. | |
| Notes | Research funding: This study was funded by the Michael & Susan Dell Foundation. Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools were matched on size and composition of student ethnicity and economic disadvantage and then randomly assigned to one of the 3 study conditions – no other information. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding of participants and personnel (performance bias) | High risk | Little information. Unclear if blinding of key study participants and personnel attempted, but likely that the blinding could have been broken, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) | High risk | Blinding of outcome assessment unclear, but likely that the blinding could have been broken, or the outcome measurement is likely to be influenced by lack of blinding. The CATCH Teacher Survey was created to assess the implementation of the CATCH program, including ABs, by classroom teachers. The survey is a 15‐item, self‐administered questionnaire that includes items on teacher implementation of ABs, encouragement of specific health behaviours, and other process evaluation measures for the CATCH program. |
| Incomplete outcome data (attrition bias) | High risk | Response rates varied among the conditions (Basic = 56.2%, Basic Plus = 69.7%, and Basic Plus SM = 83.2%, in measurement period 1 and Basic = 59.1%, Basic Plus = 48.9%, and Basic Plus SM = 75.4% in measurement period 2). All surveys from one Basic condition school, 15 surveys in total, were excluded from analysis at both measurement periods due to a low response rate (9%, N = 6) at measurement period 1. Additionally, 54 surveys from measurement period 1 and 58 surveys from measurement period 2 were excluded from analysis because the teacher only taught PE and/or athletics. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Recruitment to cluster | Unclear risk | Insufficient information provided. |
| Baseline imbalance | Low risk | The demographic characteristics of students and schools across the 3 conditions were similar at baseline. |
| Loss of cluster | High risk | All surveys from one Basic condition school, 15 surveys in total, were excluded from analysis at both measurement periods due to a low response rate (9%, N = 6) at measurement period 1. |
| Incorrect analysis | High risk | No account of clustering. Significant differences across conditions within each measurement period, and by conditions across measurement periods, were assessed by Chi2 for categorical outcomes and by analysis of variance (ANOVA) with a Scheffe post hoc test for continuous outcomes. |
| Contamination | Low risk | Contamination: Schools were randomised to study condition. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Methods | Trial name: Trying Alternative Cafeteria Options in Schools (TACOS). Study design: Cluster‐randomised controlled trial. Intervention duration: 2 years. Length of follow‐up from baseline: 2 years. Differences in baseline characteristics: Similar. Unit of allocation: Schools. Unit of analysis: Schools and students. | |
| Participants | School type: Schools (secondary). Region: St Paul metropolitan, Minneapolis, USA. Demographic/socioeconomic characteristics: Schools were predominantly urban. On average, 14% of students were non‐white (range 3% to 77%), and 9% were eligible for free lunch (range 1% to 57%). Two schools’ food services were run by food service management companies, 18 schools’ services were run by the school district food services, 19 schools prepared meals on‐site, and 20 schools participated in the National School Lunch Program. Inclusion criteria: ‐ The presence of an à la carte area in the school cafeteria operated by the school food service. ‐ A food service director and principal willing to take part in the study for 2 school years. ‐ A willingness to be randomly assigned to intervention or control group. ‐ Computerised à la carte sales data. ‐ A willingness to share these data with researchers, allow a mail‐based administration of student evaluation surveys, and allow student groups to collaborate with research staff on the development and implementation of school‐wide promotional activities involving foods offered in the à la carte area. Number of schools allocated: 20. Numbers by trial group: n (controls baseline) = 10. n (controls follow‐up) = 10. n (interventions baseline) = 10. n (interventions follow‐up) = 10. Recruitment: Not reported. Recruitment rate: 80%. Of the 25 eligible secondary schools invited to participate, 5 declined, primarily because of the respective food service directors’ concern about the additional food service staff burden related to compliance with research protocols. To avoid contamination caused by schools sharing the same food service director, only 1 school per district was included in the study. For student survey mean response rates for the 3 surveys were 75%, 75%, and 77%, respectively, and did not differ significantly between intervention and control schools. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: Intervention consisted of increasing the availability of lower‐fat foods in cafeteria à la carte areas and implementing school‐wide, student‐based promotions of these lower‐fat foods. The goal was to increase lower‐fat à la carte food availability by 30% relative to baseline. The ultimate goal was to have 50% of products be lower fat. Implementation strategies: EPOC: Local consensus processes: ‐ Quarterly meetings between research and food service staff were held to review progress toward goals. EPOC: Tailored intervention: ‐ Development of tailored lists of higher‐ and lower‐fat foods for schools. EPOC: Education meetings: ‐ TACOS staff worked with the student groups and their faculty advisors to train the students for specific promotional activities and to act as liaisons between students and the food service staff. EPOC: Pay for performance: ‐ Student groups were offered financial incentives for completing each promotion (from $100 to $300, depending on the complexity of the promotion). Theoretical underpinning: Not reported. Description of control: No intervention control. | |
| Outcomes | Outcome relating to the implementation of school service policies, practices or programs: ‐ Students seen any posters in school about cafeteria food choices? ‐ Students heard any messages over public address system, in school? ‐ Students heard about any contests or events at school about cafeteria food choices? ‐ Students took part in any taste tests, food samplings, or contests in the school cafeteria? ‐ Percentage low‐fat à la carte foods Data collection method: To monitor the extent to which intervention schools implemented their lower‐fat à la carte food availability goals, trained research staff visited each intervention school every 3 weeks to record all foods offered at lunchtime in the à la carte areas. In addition, complete à la carte inventories in intervention and control schools were conducted by trained research staff at baseline and after the second intervention year. Student exposure to the TACOS intervention activities was assessed with a series of 4 questions on a mailed student survey. Validity of measures: Not reported. Both self‐reports and objective measures were used. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: School food service revenue was reported. Data collection method: Data on school food service revenues were collected at the end of each school semester from a same point‐of sales software program including revenues from student reimbursable lunches, student à la carte foods, total à la carte foods, and total school food service revenues. Validity of measures: Not reported. Outcome relating to child diet, physical activity or weight status: Nutritional food choices two outcome measures assessing nutrition intake: 1) The percentage of lower‐fat à la carte foods sold and 2) students’ self‐reported food choices. Data collection method: 1) Students’ self‐reported food choices: Student food choices were measured via a mailed survey to a random sample of 75 students per school, according to the Dillman method, during the Fall of 2000, the Spring of 2001, and the Spring of 2002. Surveys comprised 48 questions related to students’ food choices. 2) Sales data were collected on a weekly basis in electronic format from school food service staff in each of the 20 schools Validity of measures used: Sales data: objective. | |
| Notes | Research funding: Supported by the National Institutes of Health (grant R18 HL61305). Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools were randomly allocated to experimental group. The random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: Student data and observations: No mention that students or TACOS staff were blinded. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: Student data and observations: No mention that students or TACOS staff were blinded. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: All 20 secondary schools participated. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Recruitment to cluster | Low risk | Schools were randomised to condition and those within each school participated. |
| Baseline imbalance | Low risk | Schools were randomised to condition. |
| Loss of cluster | Low risk | There were no losses of clusters. |
| Incorrect analysis | Unclear risk | Graphs of data by school showed that the first 3 weeks and last 3 weeks of each 40‐week academic year demonstrated excessive variation attributable to start‐up and termination process. Therefore, data from these weeks were excluded from the analysis. Unclear how the full analysis was performed. |
| Contamination | Low risk | To avoid contamination caused by schools sharing the same food service director, only one school per district was included in the study. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Methods | Trial name: Texas Tobacco Prevention Initiative. Study design: Non‐randomised control (comparison group). Intervention duration: 2 years. | |
| Participants | School type: Schools (middle and high). Region: East Texas, USA. Demographic/socioeconomic characteristics: Not reported. Inclusion/exclusion criteria: Not reported. Number of schools allocated: 134. Numbers by trial group: n (controls baseline) = Not reported. n (controls follow‐up) = Not reported. n (interventions baseline) = Not reported. n (interventions follow‐up) = Not reported. Recruitment: School: The baseline sample of schools was randomly selected by Texas Department of State Health Services (TDSHS) in school year (SY) SY2000from schools serving students in grades 6 through 12 in the East Texas study area. A representative sample of schools was selected. Participating schools were located in 69 districts in a 7‐county study area. The original SY2000 sample of 171 schools was drawn with probability proportional to study‐area size and school condition (intervention or comparison). Among these schools, 134 participated in the baseline study. This sample was retained and used in this SY2002 follow‐up. Student: Not reported Recruitment rate: 134/171 = 78.4% | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control) Policies, practices or programs targeted by the intervention: 1) Conduct tobacco‐use prevention education (TUPE) with the designated curriculums of Project Towards No Tobacco (TNT) at the middle school level and Not On Tobacco (NOT) at the high school level. 2) Conduct at least 1 tobacco prevention event. 3) Provide education and training for parents and staff regarding local policies and ordinances as well as state tobacco laws. 4) establish STARS, PALS, or Teens Against Tobacco Use (TATU) groups or other peer mentor programs at the high school level. EPOC: Local consensus processes: Contractual agreements were issued to intervention schools to: ‐ Participate in training organised by their Education Service Centres (ESC) on tobacco issues and curricula. ‐ Conduct TUPE with the designated curriculums of Project TNT at the middle school level and NOT at the high school level. EPOC: Educational outreach visits: ‐ The Texas Tobacco Prevention Initiative placed a Tobacco Specialist at each of four regional ESC serving the East Texas study area. Their responsibilities included coordination, distribution and management of funding, training, and technical assistance for intervention schools in respective service areas. EPOC: Educational meetings: ‐ Training to encourage planning and implementing the above activities based on the Guidelines for school health programs to prevent tobacco use and addiction. EPOC: External funding: ‐ Each school received an allocation of approximately $2000 per year to be used for materials, supplies and small equipment, in‐service release time, training, and travel to tobacco‐related meetings. Theoretical underpinning: Not reported. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ Enforcement of school policy on tobacco use ‐ Instruction on tobacco prevention education ‐ Assessment of prevention programs ‐ Student cessation support ‐ Teacher training for tobacco prevention education ‐ Establish or change school policy on tobacco use ‐ Faculty and staff cessation support ‐ Family involvement in student tobacco programs ‐ Parental involvement in policy ‐ Greater than 10 lessons Data collection method: Self‐report surveys were mailed to the schools for both principals and health coordinators. Validity of measures: Not reported/self‐report methods. Outcome relating to staff knowledge, skills or attitudes: At follow‐up, intervention schools were more likely than comparison schools to be extremely/moderately active in teacher training, using recommended curricula, offering more tobacco‐related lessons, and using more recommended teaching methods. More interest in staff development was reported at intervention schools. Data collection method: Self‐report surveys were mailed to the schools for both principals and health coordinators. Validity of measures: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Not reported. | |
| Notes | Research funding: Supported by funding from Texas Department of State Health Services. Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomised control (comparison group). It appears that schools were not randomly assigned to the intervention or the comparison group and therefore high risk of selection bias. |
| Allocation concealment (selection bias) | High risk | Non‐randomised trial and there is no indication that allocation was concealed and therefore at high risk of selection bias. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: There is no mention that participants or personnel were blinded to experimental group and therefore at high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: There is no blinding of principals or health coordinators described and the outcomes are likely to be influenced by the use of self‐reported questionnaires. |
| Incomplete outcome data (attrition bias) | High risk | Outcome group: High attrition as 25 (19%) schools were lost for the principal survey and 50 (37%) schools for the health coordinator survey. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Potential confounding | High risk | There is no mention of measurement of potential confounders, or any attempt to adjust for confounders. |
| Methods | Trial name: El Paso Coordinated Approach to Child Health (El Paso CATCH). Study design: Non‐randomised. Intervention duration: 1997 ‐ 2000. Length of follow‐up from baseline: 3 years. Differences in baseline characteristics: Not reported. Unit of allocation: Schools. Unit of analysis: Schools. | |
| Participants | School type: Elementary schools. Region: Participants were 24 elementary schools from five school districts in West Texas and Eastern New Mexico. Demographic/socioeconomic characteristics: El Paso, Texas, a region dominated by the Mexican culture and low‐income families. Inclusion/exclusion criteria: Not reported. Number of schools allocated: 24 (20 intervention, 4 control). Four schools served as controls, with the remaining 20 schools enrolled in the El Paso CATCH program. Most of the schools had baseline physical activity measures (n = 16) and 12 had baseline school meal assessments. Physical activity behaviour during PE classes was assessed in third, fourth, and fifth grades for 16 intervention schools and in third grade only for 4 intervention and the 4 control schools. Grades three, four, and five are reflected in school meal assessments for all schools. All but two schools (1 control and 1 intervention school) had PE with certified PE instructors. In these two schools, classroom teachers conducted PE for third grade only. Numbers by trial group: n (controls baseline) = 4. n (controls follow‐up) = 4. n (interventions baseline) = 20. n (interventions follow‐up) = 20. Recruitment: Not reported. Recruitment rate: Not reported. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: CATCH intervention was delivered at school level to: Food service: ‐ To reduce the total fat content of food served to 30%. ‐ To reduce the total sodium content to 600 mg ‐ 1000 mg per serving. Implementation strategies: EPOC: Educational meetings: ‐ Staff received training sessions to deliver CATCH. EPOC: Educational outreach visits: ‐ Staff received ongoing support visits to implement EATSMART/CATCH PE. EPOC: Educational materials: ‐ Educational materials were provided to staff/schools. Smart choices manual was provided to all schools. Theoretical underpinning: Social Learning Theory and Organisational Change. Description of control: Not reported but assume usual practice. | |
| Outcomes | Outcome relating to the implementation of school service policies, practices or programs: ‐ % fat in breakfast ‐ Sodium (mg) in breakfast ‐ % fat in lunch ‐ Sodium (mg) in lunch Data collection method: For both control and CATCH schools, school breakfast and lunch menus and their recipes were collected for 5 consecutive days during each semester in every year of the study. Recipes for these menus were obtained by interviewing cooks and kitchen managers in school cafeterias and by reviewing the cafeteria production sheets for each meal. Foods from the menus, production sheets, and recipes were entered into a nutritional database that is especially useful for ethnic foods (ESHA Research Inc, Salem, Ore). Once the nutrient content of the meals was analysed, averages of breakfast and lunch values across the 5 days of data collection were obtained. Validity of measures used: Not reported/self‐report methods. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: BMI, waist‐to‐hip ratio and weight. Data collection method: Anthropometry was conducted in the late Fall or early Spring semester (November, December, January, or February) of each year of the project. At least 3 people were trained to collect these measurements. Validity of measures used: Anthropometry is valid. Each person’s measurements were compared with an experienced technician’s values (the trainer), and reliability was established at a minimum of r = 0.90 for all measures before data collection. | |
| Notes | Note: This trial also contained a PA component as part of their policy, practice or programs implemented however, the trial was downgraded to a nutrition trial only as it did not report implementation outcomes for PA or in some instances, the direction and magnitude of effect was not known. Research funding: Supported by funding from the Patient Care and Outcomes Research Award program from the American Heart Association (9970182N) and the Paso del Norte Health Foundation, El Paso, Texas. Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomised. Four schools that were beginning the CATCH program in 1999 were randomly selected and then four control schools that were not in the CATCH program were selected by matching them to the intervention schools for district, relative location, number of PE teachers, number of cafeteria staff, size of third‐grade classes and size of school overall. |
| Allocation concealment (selection bias) | High risk | Non‐randomised. Intervention schools were in the CATCH program while control schools were not in the CATCH program. High risk of bias as no concealment of allocation. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: There was no blinding of participants or personnel described and performance is likely to be influenced by knowledge of group allocation. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: Questionnaires were used to survey PE teachers, cafeteria staff and classroom teachers about the implementation of CATCH. There is no blinding of participants described and the outcome is likely to be influenced by the use of self‐reported questionnaires. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: No schools appeared to drop out. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Potential confounding | Unclear risk | Matched intervention and control schools for district, relative location, number of PE teachers, number of cafeteria staff, size of third‐grade classes and size of school overall. However it is unknown whether all potential confounders were measured. |
| Methods | Trial name: Travis County Coordinated Approach To Child Health (CATCH) Trial. Study design: Non‐randomised. Intervention duration: 4 years. Length of follow‐up from baseline: 1 year. Differences in baseline characteristics: Not reported. Unit of allocation: Schools (elementary). Unit of analysis: Classroom and students (elementary). | |
| Participants | School type: Schools (elementary). Region: Four school districts in Travis County, Texas, USA. Demographic/socioeconomic characteristics: 53% female; 61% Hispanic, and 14% African American; and mean age of 9.9 years. Inclusion/exclusion criteria: ‐ Schools that include 4th grade classes. ‐ ≥ 60% of school composition of economically disadvantaged students. Number of schools allocated: 30. Numbers by trial group: n (controls baseline) = 15 (CATCH BasicPlus (BP) Group). n (controls follow‐up) = 15 (CATCH BP group). n (interventions baseline) = 15 (CATCH BasicPlus and Community (BPC) group). n (interventions follow‐up) = 15 (CATCH BPC group). Recruitment: Not reported. Recruitment rate: Not reported. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The objective of this CATCH program was to target multiple aspects of the school environment, including the classroom, nutrition services and the cafeteria environment, physical education (PE) activities, family and home environment, and, via school health promotion messages and events, the broader school community. This trial compared two versions of the CATCH program, the CATCH BP and the CATCH BPC. The CATCH BPC included all components of the BP program however schools were provided with additional support for building school and community partnerships and local decision making and capacity building related to physical activity (PA) and healthy eating promotion. Implementation strategies: CATCH BP: EPOC: Educational meetings: ‐ Coordinated school health CATCH training and booster training sessions. EPOC: Educational materials: ‐ CATCH program materials, CATCH component coordination kit and supplemental health promotion resources. EPOC: Local consensus process: ‐ CATCH Committee Meetings. EPOC: Pay for performance: ‐ CATCH Awards Program (recognition and funds for CATCH). EPOC: The use of information and communication technology: ‐ School social marketing efforts. EPOC: Educational outreach visits: ‐ CATCH facilitator support visits (1 visit/4–6 weeks). EPOC: Other: ‐ Family Fun night activities/events. CATCH BPC: All the above strategies plus: EPOC: Educational outreach visits: ‐ Additional CATCH facilitator visits (2–3 visits/4–6 weeks). EPOC: Educational meetings: ‐ CATCH Community “Best Practices” workshops (3/year). EPOC: Local consensus process: ‐ Community member required on CATCH Committee and CATCH Community “Best Practices” workshops (3/year). EPOC: Other: ‐ CDC School Health Index used as planning tool. EPOC: Educational materials: ‐ School program and community health promotion activity guide. Theoretical underpinning: Elements of Social Ecological Theory and Social Cognitive Theory. Description of control: Low‐income schools. They received the CATCH BP intervention. Alternate active implementation strategy. | |
| Outcomes | Outcome relating to the implementation of school service policies, practices or programs: Continuous ‐ CATCH parent and extracurricular activities ‐ CATCH coordinated healthy eating–related activities ‐ CATCH coordinated physical activity–related activities ‐ Number of CATCH lessons taught ‐ Number of health lessons taught Dichotomous ‐ % Reporting CATCH lessons in schoolroom ‐ % Reporting that fruit usually served at lunch Data collection method: Structured interview with CATCH Champion, self‐administered questionnaire for 4th grade classroom teachers and CATCH SPAN student questionnaire. Validity of measures: Not reported/self‐report methods. However the authors comment that the teacher and Champion measurement tools were based on previous instruments used to measure the dissemination of the CATCH program. The student survey used was modified from the SPAN study. The dietary intake, activity, and process measures were self‐reported, all of the measures were adopted from previous work by the study investigators and have demonstrated face validity, and have been evaluated for reproducibility. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Height, weight and BMI measurements along with student‐level dietary intake concerning their unhealthy food intake, food index score, fruit and vegetable intake and sweetened beverage consumption, sedentary behaviour and physical activity. Data collection method: Weight status: Weight measurements were collected using a Tanita BWB‐800S scale; a Perspectives Enterprise stadiometer was used to measure height. BMI was calculated using the standard formula, and BMI percentiles were calculated using the CDC 2000 growth charts. Dietary intake: Student questionnaire. Activity behaviours: Student questionnaire. Physical Activity: SOFIT. Validity of measures used: Weight Status: Validated: Standard protocols were followed by trained and certified research staff. Dietary Intake: The student survey used was modified from the SPAN study. Activity Behaviours: The student survey used was modified from the SPAN study. Physical Activity: Valid. | |
| Notes | Research funding: Supported by funding from Michael & Susan Dell Foundation. Conflicts of interest: Some authors received funding from Flaghouse, Inc. and the Michael & Susan Dell Foundation for development, dissemination and evaluation of the CATCH program. The University of Texas School of Public Health receives royalties based on sale of CATCH curriculum, of which 100% goes back into further research and development. The University of Minnesota receives royalties from Flaghouse, Inc. based on sale of CATCH curriculum materials, of which a portion is paid as royalties to the investigators. The remaining authors declared no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomised trial as it does not appear that the schools were randomised to experimental group. 15 CATCH BPC schools were matched to 15 similar low‐income CATCH BP schools by ethnicity and percentage economic disadvantaged. |
| Allocation concealment (selection bias) | High risk | Non‐randomised trial and there is no mention that allocation was concealed and therefore at high risk of selection bias. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: There is no mention that participants or personnel were blinded to experimental group allocation and therefore risk of performance bias is high. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: School‐level observations and teacher and student surveys provided process measures. It is not reported that observers or participants were blinded to group allocation and therefore the risk of detection bias is high. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: There was no school dropout reported. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Potential confounding | Unclear risk | CATCH BP and CATCH BPC schools were matched by ethnicity and percentage economic disadvantaged but it is unknown if there were other potential confounders that were not measured. |
| Methods | Trial name: Teens Eating for Energy and Nutrition at School (TEENS). Study design: Randomised controlled trial for implementation outcome. Intervention duration: 2 years. Length of follow‐up from baseline: 2.5 years (Fall 1998‐Spring 2000). Differences in baseline characteristics: Reported as none: “Participation did not differ significantly by treatment condition or by student‐level dietary variables”. Lytle 2004 reports significant differences between intervention and control students completing diet recall (race/ethnicity and parents’ highest education) and completing the student survey (race/ethnicity, parents’ full‐time employment, parents’ highest education). Unit of allocation: Schools. Unit of analysis: Schools. | |
| Participants | School type: Schools (middle). Region: Minneapolis/St. Paul Minnesota USA (lower‐income population). Demographic/socioeconomic characteristics: white (72.9%); and 19.8% were categorised as lower‐socioeconomic status. Inclusion/exclusion criteria: Inclusion: ‐ Schools required to have at least 20% of students in their district qualify for free or reduced‐price school lunch. ‐ Schools required to have both seventh and eighth graders attend their school and have at least 30 students in each of those grades. Number of schools allocated: 16 (8 intervention, 8 control). Numbers by trial group: n (controls baseline) = 8. n (controls follow‐up) = 5. n (interventions baseline) = 8. n (interventions follow‐up) = 8. Recruitment: Schools: Schools agreeing to be in the study committed to the measurement protocol, randomisation to condition, and if randomised to the intervention condition, to the following intervention protocol: 1) Offer all 10 sessions of the TEENS curriculum in each of the seventh and eighth grades, 2) allow the designated teacher to attend a full day of training each year, 3) allow for provision of a family education component, and 4) allow school food service staff to be trained on modifying the school food environment.” Parents: A sub‐sample of parents was randomly selected to complete parent survey. Students: All students who were in seventh grade during the baseline data collection period were considered eligible to participate in TEENS. Recruitment rate: Schools: 20 of 33 = 61%. Parents: 67% of families completed the parents survey (n = 343; 526 families sent the survey) Students: 3,878 (95.8%) students completed the baseline survey, 3,503 (90.3%) completed the interim survey, 3,010 (77.6%) completed the follow‐up survey, sample for analysis of survey data was 2833 students who had survey data at baseline and follow‐up. | |
| Interventions | Number of experimental conditions: 2 (1 TEENS intervention, 2 control). Policies, practices or programs targeted by the intervention: ‐ Teens Eating for Energy and Nutrition at School (TEENS) was a school‐based intervention trial conducted in middle schools with a goal of developing and evaluating school and family‐linked intervention strategies to promote students' consumption of fruit, vegetable, and lower fat snacks (FVLFS). ‐The TEENS intervention included classroom, family, school policy, and food service components. Implementation strategies: EPOC: Local opinion leaders and local consensus processes: ‐ School Nutrition Advisory Councils (SNACs) was established to convene school and parental stakeholders to discuss and propose school‐level policy to improve the school food environment. The composition of SNACs differed on a school‐to‐school basis but included as a minimum, a school administrator, food service staff, teacher, student, and university staff member. EPOC: Educational meetings and educational materials: ‐ School food service intervention: The emphasis of the school food service intervention was on increasing the offerings and sales of FVLFS in the lunchroom and on the à la carte lines. District food service directors and workers from intervention schools attended training that emphasised the importance of offering more FVLFS, gave them new tools for promoting FVLFS, exposed food service workers to snacks and beverages that could be offered on the à la carte line that met the TEENS fat criteria of less than 5 g of fat per serving, including taste testing of lower fat products, and offered a forum for sharing ideas between schools. TEENS interventionists also conducted on‐site training to help workers problem‐solve. Theoretical underpinning: Social Cognitive Theory (SCT) was used to inform the intervention plans. Description of control: Delayed intervention. | |
| Outcomes | Outcome relating to the implementation of service policies, practices or programs: ‐ Food offered: Foods to limit ‐ Foods offered: Foods to promote ‐ Foods sold: Foods to limit ‐ Food sold: Foods to promote Data collection method: School food environment/fruits, vegetables and salads: Data on the fruits, vegetables, and salads available on school cafeteria lunch lines were collected at eight time points: baseline (Fall 1998), six interim time points; and at follow‐up (Spring 2000). Each data point included 5 consecutive days of meal information. Data collected included the total number of students served the meal pattern lunch, the types and amounts of fruit and vegetable choices offered and sold, and the number of vegetable salads sold. With a few exceptions, these data were extracted from schools' food production records. Periodic observations of school meals were conducted to confirm production records. School food environment/à la carte: A daily data collection form for à la carte items that categorised à la carte items and documented the number of items offered and sold in each category was developed based on their earlier work conducted on à la carte in schools and intervention goals. At baseline and follow‐up, TEENS evaluation staff observed and recorded all the foods and beverages that were offered and sold on à la carte lines for a 5‐day period. Two evaluation staff conducted independent reviews of the data categorisation and abstraction for data quality assurance. Data were summarised into categories of “Foods to Promote” and “Foods to Limit”. “Foods to Promote” included snacks that were 5 or less g of fat, 100% fruit juice, water and low‐fat milk, fruits or vegetables offered, and other lower‐fat versions of popular entrees such as pizza or pretzels and cheese. “Foods to Limit” included all snacks that were more than 5 g of fat, fruit drinks, and higher fat popular entrees such as regular pizza or nachos. Validity of measures used: School food environment/fruits, vegetables and salads: Not reported however objective measures for implementation outcome assessment were used. School food environment/à la carte: Not reported however objective measures for implementation outcome assessment were used. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Student‐level fruit and vegetable intake and food choices. Data collection method: Student self‐report survey and 24‐hour recalls. Validity of measures: 24‐hour recalls – not reported. Student survey: Fruit and vegetable component of survey has been validated. Provides a reference to where the psychometric properties of the measure have been described: Survey development for assessing correlates of young adolescents’ eating. | |
| Notes | Research funding: Supported by funding from the National Cancer Institute (5R01 CA71943‐03) and from the Minnesota Obesity Center. Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools were randomly allocated to experimental group. The random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All Given the nature of the intervention, participants and study personnel are likely to have been aware of study allocation and therefore high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcome group: School food environment/fruits, vegetables, and salads Unclear if evaluation staff conducting data abstractions, observations and recording were blind to group allocation. Outcome group: School food environment/à la carte Unclear if evaluation staff conducting data abstractions, observations and recording were blind to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: School food environment/fruits, vegetables, and salads There was no attrition (16/16) and therefore risk of attrition bias is low. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Methods | Trial name: Bihar School Teachers Study (BSTS). Study design: Cluster‐randomised controlled trial. Intervention duration: 7 months. Differences in baseline characteristics: The sociodemographic characteristics and tobacco use patterns were comparable among participants in the intervention and control groups. | |
| Participants | School type: Government rural and urban schools representing grade levels 8‐10 were selected. The assumption is made that this reflects high schools. Demographic/socioeconomic characteristics: The authors report the study was conducted in an area with fewer social and financial resources than much of India at the time of the study. In 2001, only 4% of Bihar households had tap drinking water (national average = 37%), and 10% had electricity as a source of lighting (56% nationwide). Inclusion/exclusion criteria: Inclusion ‐ At least 8 teachers. Exclusion ‐ School districts located in flood zones (because school closures would make intervention delivery unfeasible). Number of services allocated: 72 Numbers by trial group: n (controls baseline) = 36 n (controls follow‐up) = 36 n (interventions baseline) = 36 n (interventions follow‐up) = 36 Recruitment: 72/86 schools Note. no sample sizes for children in enrolled schools given. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The BSTS was initiated to test the efficacy of a comprehensive tobacco control program (known as the ‘Tobacco‐Free Teachers/Tobacco‐Free Society’ program (TFT/TFS)) in increasing tobacco use cessation among teachers and promoting the adoption and implementation of school tobacco policies. The TFT/TFS targeted teachers as they have been identified as a high‐priority audience for tobacco control efforts in India, because they serve as role models for students. Implementation strategies: EPOC: Local opinion leader ‐ Each Health educator was assigned a set of five to six schools in which to deliver the intervention, with assistance from a designated teacher at each school, termed as Lead Teacher (LT). The LT played the role of a liaison between the HE and other school personnel at his/her school and was nominated by their school principal according to guidelines provided (being a non‐user/quitter of tobacco, being respected among teachers, possessing good leadership qualities and having willingness to give personal time for the program). EPOC: Continuous quality improvement ‐ Health educators offered ongoing technical support for the lead teachers through monthly school visits, phone support, and a mid‐year meeting with lead teachers from other intervention schools. The intervention protocol specified that health educators would conduct 1 visit per month to each school, for a total of 6 visits over the 7 months of intervention delivery. During each visit, health educators met with the principal and lead teacher and conducted a group discussion with the teachers and other school personnel. The lead teacher also conducted 6 to 8 group discussions with the other teachers in the school, addressing the topic defined for that month. EPOC: Education materials ‐ Program materials. Schools were provided with supporting educational and programmatic materials including: (i) posters (one per theme); (ii) a calendar (displaying the monthly theme); (iii) a notice board to display materials; (iv) a suggestion box for the HE/LT to receive feedback/questions; and (v) self‐help quit booklets (a step‐by‐step guide to quitting, available for each teacher). EPOC: Education meeting ‐ Each school appointed a lead teacher, who was trained to facilitate the program on‐site during a 2‐day training provided by wave in a centralised location. Mid‐year refresher training was also provided Health education sessions. Health education sessions were conducted twice per month at each school in the format of group discussions and were centred on six topics (themes): (i) teachers as role models for tobacco control; (ii) health effects of tobacco; (iii) motivations to quit tobacco; (iv) skills to quit tobacco; (v) dealing with withdrawal symptoms; and (vi) maintaining abstinence from tobacco. The first session of each month was facilitated by the HE and the second session was facilitated by the LT 2 weeks later, with the HE present as an observer. These sessions were usually conducted during lunch‐breaks (to avoid interference with teaching schedules) and engaged both tobacco users as well as non‐users. In‐depth protocols were created to ensure standardisation of intervention delivery of both HE and LT sessions. Twelve sessions total were offered to each school. EPOC: Local consensus process ‐ A tobacco policy workgroup was also formed in every school, with the responsibility of regularly announcing the policy and monitoring its implementation in each school as a way to build organisational support for quitters by creating a tobacco‐free school campus. Theoretical underpinning: Social Contextual Model of Health Behavior Change. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ Are any signs posted in your school warning that tobacco use is not allowed? ‐ The policy or rule is completely enforced Data collection method: School personnel survey. Validity of measures used: Not reported/self‐report methods. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to child diet, physical activity or weight status: Tobacco use. Data collection method: Policy observation checklist. Validity of measures used: Objective. | |
| Notes | Research funding: Supported by the National Cancer Institute at the National Institutes of Health (5R01CA120958, 5K05 A108663). Conflicts of interest: None declared. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Cluster‐RCT. The random sequence generation is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: Policy observation checklist Due to the nature of the intervention, unlikely that schools would have been blinded and therefore at high risk of performance bias. Outcome group: School personnel survey Unlikely that school personnel would have been blinded and therefore at high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: Policy observation checklist There is no mention that project staff who made the observations were blinded to group allocation. Outcome group: School personnel survey School personnel reported data and therefore at high risk of detection bias. |
| Incomplete outcome data (attrition bias) | Low risk | “756 of 947 eligible participants completed the baseline survey (80% response rate) and 684 completed the post intervention survey (72% response rate)". Attrition was relatively equal across experimental arms for the survey. |
| Selective reporting (reporting bias) | Low risk | There were no unreported implementation outcomes according to those planned in the published protocol. |
| Recruitment to cluster | Low risk | Recruitment bias: Individuals within each randomised cluster participated. |
| Baseline imbalance | Unclear risk | Baseline imbalance: Not reported |
| Loss of cluster | Low risk | Loss of clusters: There were no loss of clusters. |
| Incorrect analysis | High risk | Incorrect analysis: No adjustment for clustering within schools appears to have occurred. |
| Contamination | Low risk | Contamination: Unlikely due to a waiting‐list intervention design. |
| Compatibility with individually randomised RCTs | Unclear risk | Compatibility with individually randomised RCTs (cluster‐RCTs): Unable to determine. |
| Methods | Trial name: The North Carolina School Health and Tobacco Education Project (SHTEP)/Skills Management and Resistance Training (SMART). Study design: Cluster‐randomised controlled trial. Intervention duration: 4 years. Differences in baseline characteristics: Not reported. | |
| Participants | School type: Schools (junior or middle high schools). Demographic/socioeconomic characteristics: Not reported. Inclusion/exclusion criteria: In order to be eligible for participation, a school district had to have at least two junior high or middle schools (51 of 140 school districts in North Carolina met this criteria). All teachers who were eligible to teach health. Number of schools allocated: ‐ 21 districts (11 intervention, 10 control). ‐ 69 teachers (51 intervention, 18 control). ‐ 42 schools. Numbers by trial group: n (controls baseline) = 10. n (controls follow‐up) = 10. n (interventions baseline) = 11. n (interventions follow‐up) = 11. Recruitment: Schools: In both experimental and control school districts, two or more schools and two or more classrooms per school participated in the study. Teachers: All teachers in study districts identified by their schools as “eligible to teach health” were included in the sample. Students: Not reported. School districts: 21 school districts of 28 identified, therefore 75%. Schools: approximately 50 schools. Teachers at baseline 69/115 = 60%. Teachers at follow‐up 136/175 = 78%. Classrooms: approximately 100 classrooms. Students: Approximately 3000 students exposed to one of the tobacco prevention curricula. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: School health/tobacco prevention curricula (schools districts offered choice of three: Growing Healthy, Teenage Health Teaching Modules, Project SMART). EPOC: Educational meetings: ‐ Implementation intervention: In‐depth training for teachers and administrators on the use of the specific curriculum that had been adopted. EPOC: Educational materials: ‐ Schools were provided with curricular materials (schools chose the most suited of three options). EPOC: Local consensus processes: ‐ Signing of a Memorandum of Understanding: A Memorandum of Understanding, specifying which curriculum was adopted, how many lessons were to be taught, and how many classes would receive instruction, was signed by each district. Adoption intervention: Process consultation for adoption. A consultation workshop was conducted with each experimental district to inform school personnel about the 3 health curricula that were being disseminated Theoretical underpinning: Diffusion of innovation. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ % later implementation of curriculum for school district. ‐ Extent later implementation mean for school district (% of total curriculum activities taught). Data collection method: Each teacher who was eligible to teach health received an implementation check‐sheet and was asked to indicate which activities were taught. Data were also aggregated at school district level. Assessed at Year 4 follow‐up “later implementation”. A dichotomous measure of implementation (i.e., yes/no) necessary but not sufficient to assess the implementation of a school health curriculum. Therefore, Implementation checksheets were also used to assess implementation as the percentage of total curriculum activities that were taught (extent of implementation). Validity of measures used: Not reported/self‐report methods. Outcome relating to staff knowledge, skills or attitudes: Yes. Data collection method: 13‐item measure of awareness and concern among teachers and administrators about tobacco use among students. Validity of measure: Validity is not reported although the authors report the instrument is described elsewhere. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Not reported. | |
| Notes | Research funding: Supported by funding from the National Cancer Institute (#5 R01 CA 459907‐02). Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All Given the nature of the intervention, participants and study personnel are likely to have been aware of study allocation and therefore high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: All All outcomes subjective, self‐report. There is no mention of blinding of participants and personnel. Teachers completed check sheets that assessed their delivery of curricula activities and researchers conducted site visits at implementing schools. High risk of performance bias as the implementation outcomes likely to be influenced by knowledge of group allocation. |
| Incomplete outcome data (attrition bias) | High risk | Outcome group: Organisational climate The implementation measures represent cross‐sectional assessments. There was low attrition as only one experimental and one control district dropped out of the study. (Low risk of bias). Outcome group: Organisational size Organisational size represented the total student enrolment for each school district and was obtained from North Carolina Department of Public Instruction records. The smallest district had 4134 students and the largest district had 29,532 students.” Intervention = 9 districts (82%) Control = 7 districts (70%) Imbalance across intervention and control district response. (High risk of bias). Outcome group: Time of adoption Time of adoption ranged from 9.57 to 19.86 weeks. Intervention = 8 districts (73%) Control = 7 districts (70%) (High risk of bias). Outcome group: Awareness ‐ concern ‐ interest The response rate for teacher’s Awareness and interest was 69% (n = 432), and for concern was 52% (n = 324). Insufficient reporting of attrition/exclusions to permit judgement of 'Low risk' or 'High risk' (e.g. no reasons for missing data provided). (Unclear risk of bias). Outcome group: Level of Use ‐ District Of the 570 Level of Use instruments sent to teachers, 252 were returned and completed, for a response rate of 44% (n = 252). Only the Level of Use instruments for School Health and Tobacco Education Project curricula were analysed (n = 71). Intervention = 9 districts (82%) Control = 7 districts (70%) Imbalance across intervention and control district response. (High risk of bias). Outcome group: Level of Use ‐ Teacher Of the 570 Level of Use instruments sent to teachers, 252 were returned and completed, for a response rate of 44% (n = 252). Only the Level of Use instruments for School Health and Tobacco Education Project curricula were analysed (n = 71).” Intervention = 52 teachers Control = 20 teachers Insufficient reporting of attrition/exclusions to permit judgement of 'Low risk' or 'High risk' (e.g. no reasons for missing data provided). (Unclear risk of bias). Outcome group: Implementation Checklist ‐ District Initial Implementation Intervention = 8 districts (73%) Control = 6 districts (60%) Later Implementation Intervention = 8 districts (73%) Control = 6 districts (60%) Imbalance across intervention and control district response. (High risk of bias). Outcome group: Implementation Checklist ‐Teachers During year three 115 Implementation Checksheets were sent to teachers and 69 were returned (60%). Later implementation was measured in year four of the project. During this year, 136 of 175 (78%) Implementation Checksheets were returned. Insufficient reporting of attrition/exclusions to permit judgement of 'Low risk' or 'High risk' (no reasons for missing data provided). (Unclear risk of bias). |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Recruitment to cluster | Unclear risk | District selected which two middle or junior high schools participated. |
| Baseline imbalance | Low risk | Districts randomised to condition. |
| Loss of cluster | Low risk | Small loss of clusters (1 experimental, 1 control) and equal drop out across conditions. |
| Incorrect analysis | High risk | No adjustment for clustering reported in analysis. |
| Contamination | Low risk | Low risk of contamination as districts randomised to condition. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Methods | Trial name: HEALTHY. Study design: Randomised controlled trial for implementation outcome. Intervention duration: Approx. 3 ½ years (Fall 2006 ‐ Spring 2009). Length of follow‐up from baseline: Approx. 3 ½ years. Differences in baseline characteristics: Stated as similar but not shown. Unit of allocation: Schools. Unit of analysis: Schools. | |
| Participants | School type: Schools (middle). Region: 10 school districts located at 7 sites across the USA. Demographic/socioeconomic characteristics: Schools were serving largely minority and lower income populations. Inclusion criteria: ‐ The student body is representative of the adolescent population at risk for type 2 diabetes, defined as either at least 50% minority (African American, Hispanic/Latino and/or American Indian) and/or greater than 50% eligible for free or reduced lunch. ‐ Annual student attrition from all causes is ≤ 25%. ‐ Expected cohort size at end of study is at least 50 per school. ‐ School authorities are willing to accept randomisation of an individual school to intervention or control. If a school is assigned to the intervention program, this means that the school must arrange tasks/requirements needed to comply with the trial protocol. ‐ School authorities permit grade‐wide collection of height, weight, gender, age and race/ethnicity at baseline. ‐ The school assists with mass mailings of study materials to students’ homes. ‐ The school district possesses or obtains Federal Wide Assurance (FWA) to conduct research. ‐ Appropriate school authorities agree to adhere to the protocol. Number of schools allocated: 42 (21 intervention, 21 control). Numbers by trial group: n (controls baseline) = 21. n (controls follow‐up) = 21. n (interventions baseline) = 21. n (interventions follow‐up) = 21. Recruitment: ‐ Each site recruited 6 middle schools that were randomised into intervention or control. ‐ Students provided parental informed consent. Recruitment rate: Not reported. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The following nutritional goals were set for the NSLP (National School Lunch Program), SBP (School Breakfast Program) and à la carte school food services: ‐ Lower the average fat content of food served in schools. ‐ Serve at least 2 servings of fruit and/or vegetables per student on NSLP (National School Lunch Program) and at least 1 serving per student on SBP (School Breakfast Program) each day. ‐ Serve all dessert and snack foods with ≤ 200 kcal per single size serving and/or package. ‐ Eliminate milk >1% fat, all other added sugar beverages, and 100% fruit juice (100% fruit juice may only be served as ≤ 6 ounces as part of SBP). ‐ Serve at least 2 servings of high fibre (≥2 g of fibre per serving) grain‐based foods and/or legumes per student on NSLP and at least 1 serving per student on SBP each day. Implementation strategies: EPOC: Educational meetings: ‐ Provision of staff training (Food Services Manager and staff). ‐ Educational events held during lunchtime in and around the cafeteria. EPOC: Educational games: ‐ Conducted 'taste tests' of new products and unfamiliar foods, including conducting comparison of available items. EPOC: External funding: ‐ Intervention schools received $3000 per year to defray expenses and potential loss of income and received $125 for cafeteria enhancements, and to attend training. EPOC: Tailored intervention: ‐ Research staff worked with food service managers to identify barriers and develop solutions for schools to achieve selected goals. EPOC: Educational materials: ‐ Curricula, posters, brief messages displayed near serving lines. EPOC: Educational outreach: ‐ Research staff met weekly with food service managers to observe the food environment and too plan and support goal achievement. EPOC: The use of information and communication technology: ‐ Engagement with social marketing experts to generate content and offer guidance on the school social marketing efforts. EPOC: Other: ‐ Intervention launch and finale; these events were designed to promote global awareness for the program at participating schools. Family outreach including delivery of newsletters and materials. ‐ Meetings with district level staff and buyers who procure food and with food distributors, to solicit support for change. Theoretical underpinning: Social‐ecological models Description of control: Control school followed existing school district standards and guidelines. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: 12 scores across the following variables: ‐ Lower than average fat content ‐ Serve 2 servings of fruit and vegetables ‐ Serve all desert and snack foods with < 200 kcal ‐ Eliminate milk >1% fat ‐ Serve at least 2 servings of high fibre Data collection method: ‐ Data collected by trained staff not involved in the intervention. ‐ Nutrition data were extracted from food service management source documents maintained by school food service personnel. ‐ Average food group servings and nutrient amounts served per day were calculated by the trained program staff using the food service staff records. Validity of measure: Not reported however the measures used were objective. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Yes. Data collection method: By income statements, federal meal records and sales data. Validity of measure: Not reported. Outcome relating to adverse consequences: Adverse impact on scholastic performance. Data collection method: State accountability tests and the total number and passing rates of students taking the test. Grade and school level data were recorded—no individual student data were collected. Validity of measures used: Not reported. Outcome relating to child diet, physical activity or weight status: Assessed self‐reported dietary intake (energy, macronutrient, and grams consumed of selected food groups). Height, waist circumference and BMI. Data collection method: Dietary intake: Block Kids Questionnaire Anthropometry: Height (Perspective Enterprises PE‐AIM‐101 stadiometer) and weight (SECA Alpha 882 and SECA Large Capacity 634 electronic scales) were measured without shoes. Waist circumference was taken using a tape measure on bare skin measured just above the iliac crest Validity of measure: Dietary intake: Not reported. Anthropometry: Valid. | |
| Notes | Notes: This trial also contained a PA component as part of their policy, practice or programs implemented however, the trial was downgraded to a nutrition trial only as it did not report implementation outcomes for PA. Research funding: Supported by funding from the National Institute of Diabetes and Digestive and Kidney Diseases and the National Institute of Health grant numbers U01‐DK61230, U01‐DK61249, U01‐DK61231, and U01‐DK61223 to the STOPP‐T2D collaborative group Conflicts of interest: One author received consulting fees from McDonald’s Global Advisory Committee and another received consulting fees from General Mills and ConAgra Foods. The remaining authors declared no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools were randomly allocated to experimental group. The random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All. Given the nature of the intervention, participants and study personnel are likely to have been aware of study allocation and therefore high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome group: à la carte, Nutrition goals, Food group servings. Data were collected at baseline and end of study by trained study staff not involved in implementing the intervention. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: All. All 42 schools were retained therefore risk of attrition bias is low. |
| Selective reporting (reporting bias) | Low risk | The protocol is available and the outcomes reported are consistent. |
| Methods | Trial name: Good for Kids. Good for Life. Study design: Non‐randomised. Intervention duration: 11‐15 months (duration of treatment). Length of follow‐up from baseline: Baseline; November 2006 ‐ April 2007, Follow‐up: October 2008 ‐ March 2009. Differences in baseline characteristics: No significant difference in the prevalence of vegetable and fruit breaks between intervention and comparison schools. Relative to comparison schools, intervention schools were more likely to be small, and located in rural and lower socioeconomic areas. Unit of allocation: Schools. Unit of analysis: Schools. | |
| Participants | School type: Schools (K‐6 and K‐12 central schools). Region: Hunter New England, New South Wales, Australia. Demographic/socioeconomic characteristics: Region: A demographically and socioeconomically diverse population of approximately 121 000 children aged 5–14 years (14% of the state population of 5–14 year olds). Sample: Schools were primarily government, urban and lower SES schools. Inclusion/exclusion criteria: Inclusion: ‐ All primary schools (children 5–12 years of age) and central schools (children 5–18 years of age) across the state were eligible for participation. Exclusion: ‐ Special purpose schools catering for students with special needs. ‐ Juvenile justice schools. ‐ Schools serving children who are hospitalised. Number of schools allocated: 828 (422 intervention, 406 control). Numbers by trial group: n (controls baseline) = 316. n (controls follow‐up) = 258. n (interventions baseline) = 407. n (interventions follow‐up) = 388. Recruitment: Principals of both groups of schools were sent a letter inviting them to participate in the study. Two weeks after receipt of the letter, Principals were telephoned by a trained research assistant who confirmed school eligibility, sought consent to participate and scheduled a time for a telephone interview. Recruitment rate: 96.4% of intervention schools and 77.8% of control schools consented to participate in the baseline data collection. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: ‐ The prevalence of vegetable and fruit breaks. Implementation strategies: EPOC: Local consensus processes: ‐ Consensus processes. EPOC: Local opinion leaders: ‐ Leadership support and endorsement. EPOC: Educational meetings: ‐ Staff training and professional development. EPOC: Educational materials: ‐ Program materials (curriculum resource and materials, information to parents) EPOC: Other: ‐ Incentives (material goods). EPOC: Tailored interventions: ‐ Follow‐up support. EPOC: Monitoring the performance of the delivery of the health care: ‐ Implementation feedback (performance monitoring and feedback). Theoretical underpinning: A structured multi‐strategy intervention was developed based on theoretical frameworks of practice change and recommendations from reviews and implementation studies conducted in schools and other settings. Description of control: Comparison schools were not offered the multi‐strategy intervention described above, but were offered access to information‐based support provided by a non‐government organization. Information regarding the program was provided to schools via a website, newsletters and events. If a school chose to register for the program, teaching resource materials were forwarded to the school, with schools able to receive e‐mail and telephone information‐based support if desired. If the school provided evidence of having adopted the program, they were eligible to be 'certified' as such and to receive additional resource materials and obtain access to ongoing e‐mail and telephone support. In some areas of the state, schools could access additional support provided at the discretion of local health promotion teams. | |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programs: ‐ Prevalence of fruit and vegetable breaks. Data collection method: Principal reported computer‐assisted telephone interviewing (CATI). Validity of measures used: Self‐report however method has been validated. The accuracy of Principal‐reported implementation of vegetable and fruit breaks in schools was assessed in a convenience sample of intervention schools (n = 42; 10%). Based on observations made in these schools over a 9‐week period, pre‐service teachers located in schools reported in a pen‐paper survey if classes at the school had specific breaks or if students had permission to eat vegetables and/or fruit during class time ('yes all classes', 'yes some classes', 'no classes', 'don’t know'). The pre‐service teacher surveys were completed within one month of the Principal telephone survey. Comparison of Principal and pre‐service teacher report of vegetable and fruit breaks revealed perfect agreement (Kappa = 1.0). Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Not reported. | |
| Notes | Research funding: Supported by funding from the New South Wales Health ASSIST program. The project also received infrastructure support from the Hunter Medical Research Institute (HMRI) and Hunter New England Population Health. Conflicts of interest: Authors report no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomised trial. High risk of selection bias as intervention services were recruited from a selected area and control services from a comparison region. |
| Allocation concealment (selection bias) | High risk | Non‐randomised trial. Intervention services were recruited from a selected area, therefore high risk of selection bias as no concealment of allocation. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All due to nature of the intervention, school staff and study personnel delivering the intervention were not blind to study allocation. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: Prevalence of vegetable and fruit breaks No blinding of outcome assessment and the outcome measurement is likely to be influenced by lack of blinding, self‐report considered high risk. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: Although differential response rate for intervention vs. comparison schools at baseline and follow‐up (96.4% vs. 77.8% and 95.3% and 81.6%, respectively) appropriate analyses to address this were conducted. All schools lost to follow‐up were included in the GEE model (using last value carried forward method). |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Potential confounding | High risk | Baseline differences in intervention and control schools not adjusted for in analysis. Relative to comparison schools, intervention schools were more likely to be small, and located in rural and lower socioeconomic areas. |
| Methods | Trial name: No trial name. Study design: Randomised controlled trial. Intervention duration: 9 months. Length of follow‐up from baseline: Outcome data were collected at baseline (May–July 2014) and follow‐up (May–July 2015) Differences in baseline characteristics: There were no significant differences between groups in school characteristics or menu composition at baseline. Unit of allocation: Schools. Unit of analysis: Schools. | |
| Participants | School type: Primary schools. Region: Government and Catholic schools located in the Hunter New England (HNE) Local Health District in New South Wales (NSW), Australia. Demographic/socioeconomic characteristics: The HNE region covers a large non‐metropolitan area (more than 130,000 km2); with a demographically and socioeconomically diverse population of children aged 5 to 12 years. Inclusion/exclusion criteria: Inclusion: ‐ Located within HNE region Australia ‐ Primary schools Exclusion: ‐ Independent schools ‐ Having secondary students (including central schools i.e. enrolling students from Kindergarten to Grade 12) ‐ Those exclusively catering for children requiring specialist care ‐ Not having a canteen that operated at least once per week ‐ Schools participating in another canteen intervention study ‐ Schools identified by the NSW government as a high performing health‐promoting school in terms of implementing nutrition (including canteens) and physical activity policies and practices Number of schools allocated: 53 Numbers by trial group: n (controls baseline) = 25 n (controls follow‐up) = 24 n (interventions baseline) = 28 n (interventions follow‐up) = 27 Recruitment: Sixty‐eight schools were randomised prior to baseline data collection and approached to participate in the study of which 61 schools agreed. Recruitment rate: 89.7 % however some schools were later found to be ineligible. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The NSW state government had introduced a healthy school canteen policy (“Fresh Tastes @ School”). Utilising a ‘traffic light’ food classification system, the policy classifies foods and beverages sold in school canteens (whether that be pre‐packaged foods or those made on site by canteen staff ) as either ‘red’, ‘amber’ or ‘green’ based on their nutritional content. For all foods sold in the canteen at recess and lunch the policy requires schools to remove all red foods from regular sale and to fill the menu (that is more than 50%) with green foods and to not let amber foods dominate the menu. This study was designed assess the effectiveness of a multi‐strategy implementation intervention in increasing the implementation of the healthy canteen policy in Australian primary schools. Implementation strategies: EPOC: Audit and feedback ‐ Performance monitoring and feedback. During the workshop, schools were provided with a written feedback report on their previously supplied canteen menu. The feedback report identified the included foods and beverages that were red/banned, amber or green and the proportion of the menu contributed by each category. Red/banned food items in the report were advised to be removed, with alternatives, where possible, identified. Where amber foods dominated the menu (> 50 %), green alternative food items were recommended. The feedback report included a sample ‘compliant’ menu, individually tailored using the schools baseline menu. EPOC: Continuous quality improvement ‐ Canteen managers were asked to send an updated version of the menu for review and a second feedback report was generated EPOC: Education materials ‐ Tools and resources Canteen managers were provided with a ‘Canteen Resource Kit’ containing various printed and electronic instructional materials, including electronic menu and pricing templates, and a poster‐sized checklist that prompted canteen managers to regularly review their canteen practices relating to Fresh Tastes @ School. EPOC: Education meeting ‐ Canteen manager/parent training‐ A 1 day (5 hour) group‐training workshop was offered to canteen managers and parent representatives providing education and skill development in the Fresh Tastes @ School policy, label reading, canteen stock and financial management, pricing and promotion, and change management. Dietitians, experienced in delivering training to canteen managers, conducted the training. If a school canteen manager was unable to attend the workshop, they were telephoned and offered a 30–45 minute teleconference call or a face‐to‐face meeting with a dietitian to discuss workshop content and resources. EPOC: Local consensus process ‐ The workshop provided opportunities for canteen managers to participate in consensus processes through the development of a canteen action plan identifying how they would implement Fresh Tastes @ School in their school. EPOC: Local opinion leader ‐ Executive support‐ School principals were telephoned to inform them of the training and resources available to their school canteen and asked to demonstrate their support for implementation of the Fresh Tastes @ School policy by encouraging the canteen manager and a parent representative to attend canteen manager training and for receipt of ongoing support. EPOC: Tailored intervention ‐ The feedback report included a sample ‘compliant’ menu, individually tailored using the schools EPOC: Other ‐ Following training, canteen managers received two support contacts per school term via text messages. Framed by the TDF these contacts provided targeted advice to overcome common barriers to policy implementation and encouraged canteen managers to review progress against their action plan. Canteen managers who requested additional support were contacted by a project officer after the workshop and provided tailored advice. ‐ Recognition: Schools with a menu assessed as adhering to the policy (i.e. greater than 50 % green items and no red or banned items) received a congratulatory letter from the research team, and provided a positive feedback article they could include in their school newsletter. ‐ Canteen managers who attended the workshop also received kitchen equipment to the value of AUD$100. Theoretical underpinning: Theoretical Domains Framework. Description of control: Comparison schools were not offered the multi‐strategy intervention described above. | |
| Outcomes | Outcome relating to the implementation of school service policies, practices or programs: ‐ The proportion of schools with a canteen menu that did not include red or banned foods and beverages. ‐ The proportion of schools where green items make up the majority of the menu defined as more than 50 % of listed menu items. Data collection method: Audits of canteen menus faxed or emailed to the project team by the school. Validity of method: Objective and reported as valid. Authors report the method has previously been validated with a cross‐sectional study in 38 schools that Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Not reported. | |
| Notes | Research funding: Supported by funding received from the New South Wales Healthy Children’s Initiative. The project also received infrastructure support from the Hunter Medical Research Institute (HMRI) and Hunter New England Population Health. Conflicts of interest: Authors report no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised controlled trial. The random sequence was generated using a computerised random number function in Microsoft Excel. |
| Allocation concealment (selection bias) | Unclear risk | Group allocation was concealed from staff involved in school recruitment, however there is no information about how allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: Schools were not blinded to group allocation and therefore at high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome group: Dietitians conducting menu assessments were blinded to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: Only one school was lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | The trial was prospectively registered with the Australian New Zealand Clinical Trials Registry (ACTRN12614001148662). All predetermined outcomes were reported. |
| Methods | Trial name: Action Schools! British Columbia (BC). Study design: Cluster‐randomised controlled trial. Intervention duration: 11 months. Differences in baseline characteristics: Not reported. | |
| Participants | Region: British Columbia, Canada. Demographic/socioeconomic characteristics: A broad socioeconomic and cultural spectrum. ‐ Elementary schools from two British Colombia school districts that were ranked 'low' in terms of current implementation of physical activity initiatives. Number of schools allocated: 10 randomised, stratified by size (< 300 or > 300 students) and geographic location to: 3 intervention (Champion schools (CS)), 4 intervention (Liaison schools (LS)), 3 controls (usual practice schools (UP)). Numbers by trial group: n (controls baseline) = 3 services. n (controls follow‐up) = 3 services. n (interventions baseline) = 7 services (4 LS, 3CS). n (interventions follow‐up) = 7 services (4LS, 3 CS). Teachers: 42 grade 3 and 4 teachers. 50 grade 5 and 6 teachers. Students: Not reported. Recruitment: Schools: We gave presentations at District principals’ meetings and from a pool of 103 schools, 20 schools (19%) volunteered to participate. To discriminate between schools who were already undertaking physical activity initiatives from those who were not, we used results from the 2002 BC Ministry of Education Satisfaction Survey which assessed parent and student satisfaction with current school PA on a 5‐point Likert scale (5 = very satisfied). From the pool of 20 volunteer schools, schools (n = 11) with satisfaction score that ranked 3 or lower were invited to participate. One principal withdrew his school (before randomisation) after determining there was a chance their school could be randomly selected as a control school. Students/Teacher: Grades 4—6 were included. Forty‐two (100%) Grades 4 and 5 teachers consented to participate in Phase I and 49 (98%) Grades 5 and 6 teachers consented to participate in Phase II (23 taught Grade 5 in both phases). We also recruited children in these grades to participate in an evaluation of multiple health outcomes. School districts: N/A. Schools: 19% of schools approached consented, 11/20 were eligible (55%), 10/11 consented. Classrooms: Forty‐two (100%) Grades 4 and 5 teachers consented to participate in Phase I and 49 (98%) Grades 5 and 6 teachers consented to participate in Phase II. Students: Not reported. | |
| Interventions | Number of experimental conditions: Three (2 intervention: LS and CS, 1 control: UP) Policies, practices or programs targeted by the intervention: The AS! BC model provided tools for schools and teachers to create individualised Action Plans that increased PA opportunities across Six Action Zones: ‐ School Environment ‐ Scheduled PE ‐ Classroom Action ‐ Family and Community ‐ Extra‐curricular ‐ School Spirit EPOC: Tailored interventions. ‐ The AS! BC model provided tools for schools and teachers to create individualised Action Plans that increased PA opportunities across six Action zones: 1) School Environment, 2) Scheduled PE, 3) Classroom action, 4) Family and Community, 5) Extra‐curricular and 6) School spirit. EPOC: Educational meetings. ‐ Teachers received teacher‐on‐call support to attend a Classroom Action training session (half‐day) from the AS! BC Support Team and School Facilitators and had access to further training on professional development days and by telephone consultation (on request). ‐ The AS! BC model provided generalist teachers with training and resources to operationalise their Action Plan with the ultimate goal of providing students with 150 minutes of moderate intensity PA per week. ‐ In the CS condition the School Facilitator for CS schools provided the initial training to the designated ‘champion’ teacher (a teacher willing to activate and support their colleagues). EPOC: Educational materials. ‐ Each teacher received a Planning Guide and a copy of the Action Pages ‐ The AS! BC model provided generalist teachers with training and resources to operationalise their Action Plan with the ultimate goal of providing students with 150 minutes of moderate intensity PA per week. EPOC: Other: ‐ Teachers received an Action Bin which remained in each teacher’s classroom and contained equipment and resources to facilitate Classroom Action activities. Resources were gender inclusive and designed for children at all skill levels. ‐ Also, Classroom Action Bins were enhanced with specific resources as requested. ‐ In the CS condition, Classroom Action Bins contained a basic set of resources. EPOC: Local consensus process: ‐ A school action team ‐ A committee of school stakeholders (e.g. interested intermediate grade teachers, administrators, parents, health, sport/recreation practitioners) that created and supported implementation of the Action Plan EPOC: Educational outreach meetings: ‐ In the LS condition, teachers had weekly contact with the School Facilitator who would come to the classroom to provide mentorship and demonstrate activities. ‐ In the CS condition the School Facilitator for CS schools provided support to the designated ‘champion’ teacher (a teacher willing to activate and support their colleagues). Support was not provided to each classroom in the CS group Theoretical underpinning: Socioecological. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ Minutes per week of physical activity Data collection method: Teachers at Intervention schools were asked to complete weekly activity Logs during Phases I and II. Teachers recorded daily, the type, frequency and duration (minutes) of PA implemented in the classroom, in PE or in the other Action Zones. Activity Logs were collected monthly by the School Facilitators. Teachers at UP schools completed a modified version of the Activity Log. Validity of measures used: Not reported/self‐report methods. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Physical activity of step count, fitness and physical activity score as well as anthropometry (BMI). Data collection method: Physical activity: All children wore a New Lifestyles Digiwalker SW‐200 pedometer and completed the physical activity questionnaire for children (PAQ‐C) Fitness: 20‐m shuttle run. Anthropometry: Standing height (without shoes) was measured to the nearest 1 mm (Seca stadiometer Model 242, Hanover, MD). Weight in light clothing was measured using an electronic scale (Seca Model 840, Hanover, MD) to the nearest 0.1 kg. Body mass index (BMI) was determined as weight (kg)/height (m)2. Validity of method: Physical activity: Paper reports pedometers are a valid objective measure of PA. Validity of PAQ‐C is not reported. Fitness: Objective. Anthropometry: Valid. | |
| Notes | Research funding: Supported by funding from the British Columbia Ministry of Health, 2010 Legacies Now, BC Ministry of Tourism, Sport and the Arts and the Provincial Health Services Authority. Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools were stratified by size and geographic location and randomly assigned to a Usual Practice or Intervention or Champion condition. The random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All. Given the nature of the intervention, participants and study personnel are likely to have been aware of study allocation and therefore high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: All. All self‐reported outcomes and no blinding of outcome assessment and the outcome measurement is likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) | Unclear risk | Outcome group: Physical activity delivered. There is insufficient information to determine missing data for teacher response rates and intervention fidelity. |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes appear to be covered. |
| Recruitment to cluster | Low risk | Randomisation post‐recruitment. |
| Baseline imbalance | Unclear risk | Baseline characteristics by group not reported. |
| Loss of cluster | Low risk | No loss of clusters. |
| Incorrect analysis | Low risk | Clustering has been taken into account. |
| Contamination | Low risk | Low risk due to design. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Methods | Trial name: Child and Adolescent Trial for Cardiovascular Health (CATCH). Study design: Cluster‐randomised controlled trial. Intervention duration: 3 years 1991‐1994. Differences in baseline characteristics: Schools: Among the 96 schools measured at baseline, there were no significant differences between the study conditions for all relevant variables, insuring equivalency between groups. All 96 schools maintained their participation in their allocated treatment condition over the 3‐year study period. Students: There were no significant differences by site, gender, or ethnic group between those who did and did not participate. | |
| Participants | School type: Schools (elementary). Demographic/socioeconomic characteristics: Students were from ethnically diverse backgrounds and from geographically diverse areas. Inclusion/exclusion criteria: Inclusion of schools: ‐ Distance from one of the four study centres. ‐ Ethnic diversity. ‐ Food service characteristics (potential for intervention). ‐ Commitment to offering at least 90 minutes of PE per week. ‐ Commitment to participating in a 3‐year study. ‐ Cooperation with random assignment. Inclusion of students: ‐ In 3rd grade at beginning of trial. ‐ Parents and students agreed to provide a blood sample at baseline. Number of schools allocated: 96 from 12 districts. Numbers by trial group: n (controls baseline) = 40. n (controls follow‐up) = 40. n (interventions baseline) = 56. n (interventions follow‐up) = 56. The intervention schools were further randomised into two equal subgroups: n School‐based only (baseline) = 28. n School‐ and family‐based (baseline) = 28. n School‐based only (follow‐up) = 28. n School‐ and family‐based (follow‐up) = 28. Recruitment: School district superintendents received a letter describing the project and inviting their school district to participate in the study beginning in Fall 1991. While the recruitment process differed somewhat among sites the next step usually involved a personal meeting between a school district representative (for example superintendent, curriculum specialist or other district level person) and the principal investigator and sit intervention coordinator. After the initial meeting the necessary decision‐making procedures were followed for each school district indicating interest in participating in CATCH. School districts: Of the 15 school districts initially contacted among the four sites, 12 chose to participate in the study. In Louisiana, two of six school districts declined due to teacher strikes. In Minnesota one district declined due to competing district‐wide commitments. Schools: Following recruitment of districts schools within districts were contacted. Students: Not reported. Recruitment rate: School districts: 12/15. Schools: Of the 162 schools contacted 96 agreed to participate (59.3%) recruitment rate. Student: Total baseline 5106 (60.4%). | |
| Interventions | Number of experimental conditions: 3 (2 intervention: 1 control) The schools were randomised to either intervention (56 schools; 14 per field centre) or control status (40 schools; 10 per field centre). Randomisation occurred after all baseline measurements were completed. The intervention schools were further randomised into two equal subgroups: one group received a school‐based program consisting of school food service modifications, physical education, and the CATCH curricula (28 schools; seven per field centre); the other group received the same school‐based program plus a family‐based program (28 schools; seven per field centre). Policies, practices or programs targeted by the intervention: School level: 1. EATSMART: ‐ To reduce the total fat content of food served to 30%. ‐ To reduce the total sodium content to 600 mg ‐ 1000 mg per serving. ‐ Recommendations to lower the total cholesterol in foods offered. 2. CATCH PE: ‐ increase the amount of PE time that students spent in MVPA to 40% of class time. EPOC: Educational meetings: ‐ Staff received training sessions to deliver EATSMART and CATCH PE. EPOC: Educational outreach visits: ‐ Staff received ongoing support visits to implement EATSMART/CATCH PE. EPOC: Educational materials: ‐ Educational materials were provided to staff/schools for EATSMART and CATCH PE. ‐ Smart choices manual was provided to all schools. EPOC: Other: ‐ Families were engaged by Family Fun Nights and home curricula Theoretical underpinning: Social Learning Theory and Organisational Change. | |
| Outcomes | Outcome relating to the implementation of school service policies, practices or programs: ‐ Mean % of kilocalories from fat in lunches ‐ Mean mg of sodium in lunches ‐ Cholesterol mg in lunches (mean) ‐ Quality of PE lesson % of 7 activities observed Data collection method: Nutrient content of school lunches: Nutrient content of school lunches: Five consecutive, non‐ randomly selected days of school menu, recipe, and vendor product information were collected from each intervention and control school. School food service managers were instructed by trained and certified CATCH evaluation staff to keep a written record of lunch menus as well as the portions served each day. At the end of the 5‐day, CATCH evaluation, staff conducted in‐person interviews with the managers and cooks about the menus and recipes using standardised probes for ingredients and preparation methods. Nutrient and ingredient information for vendor products (i.e. foods purchased pre‐prepared) were collected from the food companies. Data entry and nutrient calculations for school menu data at each interval were performed using the Minnesota Nutrition Data System (NDS) Version 2.2. Quality of PE lesson: Direct observation. Validity of measures used: Nutrient content of school lunches: Not reported (measures not objective). Quality of PE lesson: Not reported however the measure used is objective. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Growth and nutritional quality of the school meals. Data collection method: Measurements of height and nutrient intake as described in implementation outcomes were collected. Validity of measures used: Not reported. Outcome relating to child diet, physical activity or weight status: 1) child diet 2) physical activity 3) anthropometry. Data collection method: Child diet: A 24‐Hour Dietary Recall measured total daily food and nutrient intake in a random sub‐sample of 30 students per school at both baseline and follow‐up. A non‐quantified food record was completed by students on the previous day and was used as a prompt for the interviewer who conducted the 24‐hour recall. The data were directly entered into a laptop computer during the interview and the NCC database was used for evaluation. Self‐reported child physical activity: The Self‐Administered Physical Activity Checklist (SAPAC). Fitness: 9‐minute distance run. Fitness other: SOFIT. Height, weight, and triceps and subscapular skin‐folds: Were measured using the Stadiometer, a balance scale, and Lange callipers, respectively. Skinfold thickness was measured three times at each site, with intra‐class correlation coefficients exceeding 0.97. Height was measured to the nearest 0.1 cm, weight to the nearest 0.1 kg, and the skin‐folds to the nearest mm. Body mass index (BMI) is defined as weight (kg)/by height (m)2. Validity of measures used: Child diet: This method has previously been shown to be reliable and valid. Self‐reported child physical activity: Validated. Fitness: Objective. Fitness other: Objective. Child physical activity: Validated. Anthropometry: Objective. | |
| Notes | Note: This study targeted PA, nutrition and tobacco however, implementation outcomes for tobacco were unavailable and as such, this trial is reported as a nutrition and PA only trial, with their corresponding implementation outcomes and strategies only reported. Research funding: Supported by funding from the National Heart, Lung and Blood Institute (U01HL 33927, UOI HL 39852, UOI HL 39870, UOI HL 33906, UOI HL 39880). Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools were randomly allocated to experimental group. The random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: There is no blinding to group allocation of participants or personnel described and this is likely to influence performance. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: There is no mention that observers were blinded to group allocation and therefore the risk of detection bias is high. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: None of the schools dropped out or refused to participate in the intervention activities. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol, therefore it is unclear if there was selective outcome reporting. |
| Recruitment to cluster | Low risk | Individuals within each randomised cluster participated. |
| Baseline imbalance | Low risk | Schools were randomly allocated to condition and so risk of baseline imbalance is low. |
| Loss of cluster | Low risk | None of the schools dropped out or refused to participate in the intervention activities. |
| Incorrect analysis | Low risk | The analysis appeared appropriate. |
| Contamination | Low risk | The unit of randomisation was the school and so risk of contamination is low. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Methods | Trial name: Cafeteria Power Plus project. Study design: Cluster‐randomised controlled trial. Intervention duration: The intervention took place during 2 consecutive school years beginning in Fall 2000. Length of follow‐up from baseline: 2 years. Differences in baseline characteristics: Not reported. Unit of allocation: Schools. Unit of analysis: Lunchroom observations. | |
| Participants | School type: Schools (elementary). Region: Twin Cities metropolitan area of Minnesota USA. Demographic/socioeconomic characteristics: The 26 schools had an enrolment that was 90% white and 21% of the school meals served were free or reduced price. Inclusion/exclusion criteria: Not reported. Number of schools allocated: 26. Numbers by trial group: n (controls baseline) = 13. n (controls follow‐up) = 13. n (interventions baseline) = 13. n (interventions follow‐up) = 13. Recruitment: Not reported. Recruitment rate: Schools: Not reported. Children: 91.7%. Of the 1820 students who were eligible to be observed in Spring 2000, 1668 were observed and became the baseline sample. Of the 1820 students, 41 had moved, 7 parents and 44 students refused participation, and 60 students were absent. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: ‐ Increasing the availability, appeal, and encouragement of fruits and vegetables in the school lunch program; emphasizing changes in the lunch line; and, secondarily, the school snack cart. ‐ Increase the quality and quantity of fruits and vegetables served. ‐ Increase the choices of fruits and vegetables in the lunch line, to make them look more attractive (by putting them in small cups or arranging by colour), and to vary the type and preparation methods daily. ‐ Special events to promote fruits and vegetables. Implementation strategies: EPOC: Educational meetings: ‐ Monthly meetings were held with the cook managers from each of the 13 intervention schools to discuss and share implementation issues and new ideas during the 1st school year. EPOC: Educational outreach visits: ‐ Intervention staff visited schools weekly, on average, and supported the activities for the kick‐off. EPOC: Educational materials: ‐ The “High 5 Flyers” that were hung in posters around the school cafeteria. EPOC: Other: ‐ Special events: sampling of fruit and vegetables, class challenges (to eat 3 serves of fruit and vegetables per day at lunch). EPOC: Local consensus processes: ‐ Monthly meetings were held with the cook managers from each of the 13 intervention schools to discuss and share implementation issues and new ideas during the 1st school year. Theoretical underpinning: Social Cognitive Theory. Description of control: Received training and materials at the end of the active study phase in Fall 2002. | |
| Outcomes | Outcome relating to the implementation of school service policies, practices or programs: ‐ Verbal encouragement by food staff (mean % of observations). ‐ Number of fruits and vegetables on the snack cart (mean). ‐ Number of fruits and vegetables students can choose (mean). ‐ Fruit and vegetables rated as appealing (mean %). Data collection method: Process measures for the study, collected in both the intervention and control schools, included direct observations of the lunchroom, lunch line, food cart, and food service staff behaviour. Validity of measures used: Not reported however the measure is objective. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Fruit and vegetable intake. Data collection method: Trained observers watched the selected students from a distance in the cafeteria and recorded all items eaten at lunch and their portion. Validity of measures used: Reported to be valid. | |
| Notes | Research funding: Supported by funding grants provided by a grant from the National Cancer Institute (R01 CA59805). Conflicts of interest: Not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools were randomly allocated to experimental group. The random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: Observations: There is no blinding to group allocation of participants or personnel described and this is likely to influence performance. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: There is no mention that observers were blinded to group allocation and therefore the risk of detection bias is high. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: All 26 schools were retained in the study. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Recruitment to cluster | Low risk | Direct observations of school environment and food service staff. |
| Baseline imbalance | Low risk | There were no significant differences at baseline from the lunch observations for all the main outcome measures. |
| Loss of cluster | Low risk | All 26 schools were retained in the study. |
| Incorrect analysis | Unclear risk | Used mixed‐model regression procedures however it is unclear if adjusted for clustering. |
| Contamination | High risk | Given that schools rather than school districts were randomised to condition, there is potential for contamination because all the schools were in the same school district and so shared the same food sources and lunch menus, even though preparation was done at each school site. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Methods | Trial name: Sports, Play, and Active Recreation for Kids (SPARK). Study design: Non‐randomised. Intervention duration: 2.5 years – reported in paper as 3 academic years (1990‐1993) (intervention began in Fall 1990 and ended in Spring 1992 for fourth grade teachers and started in Fall 1991 and ended in Spring 1993 for fifth grade teachers. Follow‐up observations were made during Fall 1993 and Spring 1994)/8 months /2 years. Differences in baseline characteristics: Not reported (however matched by size and ethnic make‐up (% white))/significant difference in age by condition (9.49 vs. 9.62 years). | |
| Participants | School type: Schools (elementary) 7/12 schools in one school district. Region: Southern California, USA. Demographic/socioeconomic characteristics: The schools were situated in a middle class suburb of a large city containing 82% European American, 12% Asian/Pacific Islander, 4% Latino, 2% African American with 53% male. Inclusion/exclusion criteria: School level was not reported. Student level Inclusion: ‐ Students were required to complete baseline and final survey and fitness test. Number of schools allocated: Of the seven schools, there were four interventions and three controls. The four intervention groups were further sub‐divided into two groups; one teacher arm and one specialist arm. The specialist arm was excluded in this review as the in‐school program was delivered by certified PE specialist (PES). Conversly, the other intervention arm was delivered by school teachers. Consequently, we report five schools as allocated. Students : 2 consecutive cohort of 4th graders, followed to 5th grade) Numbers by trial group: n (controls baseline) = 3. n (controls follow‐up) = 3. n (intervention (teachers‐led) baseline) = 2. n (interventions (teachers‐led) follow‐up) = 2. Recruitment: Schools: Schools agreed to participation in an experimental program and be randomised to one of three study conditions. Schools were stratified by percentages of minority student and within those strata; two schools were randomly assigned to each condition (PE specialist, teacher‐led or control). The remaining school was added to the control condition. Teachers: Not reported. Students: Two consecutive cohorts of fourth grade students entered the study. All fourth grade students were invited to participate. Approximately 98% provided informed consent through a passive consent procedure. Recruitment rate: 12/16 Principals consented (consent rate = 75%). Resourcing constraints meant that only 7 of 12 schools were randomised. All 4th grade classes in the 7 schools participates. | |
| Interventions | Number of experimental conditions: 3 (2 intervention conditions (PES condition, TT condition) 1 control condition). PES: credentialed PE specialists were employed and trained by the investigators to ensure full implementation of the intervention. Teacher‐led: In the trained classroom teacher condition, classroom teachers were trained in the intervention methods. Note: This review only reports on the Teacher‐led and control conditions. Policies, practices or programs targeted by the intervention: Sports, Play and Active Recreation for Kids (SPARK) PE was designed to be a comprehensive program for upper elementary students to increase physical activity. It was deigned to influence the quantity and quality of elementary PE lessons and the amount of PE through: ‐ # Lessons per week ‐ Minutes of PE per week Implementation strategies: Intervention strategies provided to all 3 conditions EPOC: Educational materials: ‐ Written curriculum guide identified the program philosophy and goals and included a yearly plan which was divided into instruction units with activity progressions within each unit. A detailed plan was provided for each PE lesson, which typically had two parts: health‐fitness activities and skill‐fitness activities. EPOC: Length of consultation: ‐ An additional 30 minutes per week was allocated for classroom instruction and practices in self‐management activities and skills. EPOC: Other: ‐ To support implementation of the curricula, equivalent types of equipment were provided to all seven schools, including control schools, and replacement equipment was added each year. Trained classroom teacher condition EPOC: Educational meetings: ‐ Classroom teachers were trained to implement SPARK PE. EPOC: Educational outreach visits: ‐ On‐site support which was provided during the 3 years ensured the curriculum was followed. A PE specialist provided feedback, encouragement and direct assistance during schools visits. The specialist assisted teachers by leading grade‐level planning meetings, modelling lesson segments, coordinating space and equipment, and giving verbal and written feedback after observing lessons. Theoretical underpinning: Not reported. Description of control: Usual PE was implemented by untrained classroom teachers/usual care. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ Duration (minutes) per week of physical education lessons ‐ Frequency (per week) of physical education lessons Data collection method: Measured by direct observation by trained assessors for one full week twice a year in each school year. Validity of measures used: Not reported however the measure is objective. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Physical activity (MVPA of students in classrooms and out of school physical activity as well as a fitness test) as well as height and weight. Data collection method: MVPA of students in classrooms: SOFIT (System for observing fitness instruction time) was used to obtain student activity levels. Codes were used to estimate energy expenditure associated with physical activity, which have been calibrated using heart rate monitoring and the system has been validated using Caltrac accelerometers. Out of school physical activity: Accelerometer was the primary measure of physical activity for out of school. Fitness: mile‐run test. Anthropometric measures: Height and weight were measured in stocking feet. Calf and triceps skinfolds were assessed three times using calibrated Lange calipers. Validity of measures used: MVPA of students in classrooms: The system has been validated using Caltrac accelerometers. Out of school physical activity: Valid. Fitness: Objective. Anthropometric measures: The interobserver agreement (intraclass correlations) was .87 for triceps skinfold and .93 for calf skinfold (n = 47). Anthropometry is a valid tool. | |
| Notes | Research funding: This work was supported by NIH grant HL44467. Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation of all schools did not occur resulting in high risk of selection bias. Within each stratum, one school was randomly assigned to each of the three experimental conditions. To guard against loss of control schools, the remaining school was assigned to the control condition. |
| Allocation concealment (selection bias) | High risk | Randomisation of all schools did not occur and there is no indication that allocation was concealed and therefore at high risk of selection bias. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All. Given the nature of the intervention, participants and study personnel are likely to have been aware of study allocation and therefore high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcome group: Observations of physical education classes. Implementation of the school physical education program was assessed by direct observation by trained assessors not part of the intervention team. There is insufficient information about whether these assessors were blinded. |
| Incomplete outcome data (attrition bias) | Unclear risk | Outcome group: Observations of physical education classes. Insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (e.g. no reasons for missing data provided). |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Potential confounding | Unclear risk | There is insufficient information to determine the risk of potential confounders. |
| Methods | Trial name: No trial name. Study design: Cluster‐randomised controlled trial. Intervention duration: The intervention started in April 2009 and continued till Dec 2009. Differences in baseline characteristics: There were no significant differences between the intervention and the control group in the student population at baseline. | |
| Participants | School type: Middle. Recruitment: 40 schools were invited to participate. For the purpose of randomisation, all the villages predominantly on the left side of Mohna Road (the main road passing through all these villages) were considered one group and those on the right side another group. One group was allocated as intervention (IG), and the other as control (CG) based on draw of lots. Schools: At school level, verbal consent was taken from the school administrator. Students: At student level, written consent was taken from the parents by sending the consent form to the students before administering the questionnaire. Students present at the time of school visit with a written consent from parents were included and those absent on the day of visit were excluded from the study. There were 1026 students in the intervention and 1322 students in control group. Demographic/socioeconomic characteristics: The mean age of the study population was 12.5 years (±1.08) in the intervention group and 12.3 years (±1.11) in the control group (P = 0.08). There were 47 % girls in the intervention group and 46 % girls in the control group (P = 0.6). Inclusion/exclusion criteria: School level Inclusion: No criteria reported. Students level inclusion: Present at the time of school visit with a written consent from parents were included and those absent on the day of visit were excluded from the study. Number of schools allocated: 40 (19 intervention, 21 control). Numbers by trial group: n (controls baseline) = 21 n (controls follow‐up) = 21 n (interventions baseline) = 19 n (interventions follow‐up) = 19 | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The intervention consisted of a school component (policies), a classroom component (activities) and a family component [Information Education & Communication (IEC) material]. Implementation strategies: EPOC: Local consensus processes: ‐ Initially a sensitisation meeting was conducted to sensitise the school administrators; a short film on non‐communicable diseases (NCDs) and their risk factors was shown in addition to baseline results. The meeting aimed to conclude with assured support from the school administrators and formation of school health committee The intervention had three components: a school component, a classroom component, a family/community component. School component: This aimed to create enabling environments in the schools by: EPOC: Local opinion leaders: ‐ Formation of school health committee. EPOC: Tailored interventions: ‐ Formulation of school action plan. EPOC: Educational materials: ‐ Improving school environment by display of posters and bulletin. EPOC: Educational games: ‐ Improving school environment by conducting quiz competitions, sports competitions and cultural activities based on non‐communicable diseases (NCDs). Classroom component: to involve student in health‐promoting activities including: EPOC: Educational meetings: ‐ Health education lectures, flash film, peer group discussions, flip charts, physical training classes. Family/community component: To reach out to the families and community through schools, including: EPOC: Other: ‐ Families were engaged via holiday assignments, school rally, distribution of pamphlets, list of healthy foods, and family orientation about NDCs during parent/teacher meetings and annual functions. Theoretical underpinning: It is reported that the intervention was not based on any theoretical model. Description of control: Not reported but assume usual practice. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ Schools having tobacco policy ‐ Policy about PA ‐ School food policy ‐ Average of fried foods ‐ Average of salted snacks ‐ Average of healthy foods Data collection methods: Were measured using a school check list. The information was gathered from school authorities and by direct observation. Validity of measures used: Not reported however the methods contained objective and non‐objective components. Outcome relating to cost: Not reported. Outcome relating to child diet, physical activity or weight status: Students attending physical training classes > 5 days, Leisure time MVPA, time watching TV, consumption of fruit, vegetables, deep fried foods, salted snacks, purchasing ‘eatables’ from outside and smoking status. Data collection method: Student survey. Validity of measures used: Not reported. | |
| Notes | Research funding: India Institute of Medical Sciences, New Delhi. Conflicts of interest: Authors report no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | All the villages predominantly on the left side of the main road passing through all these villages were considered one group and those on the right side another group. One group was allocated as intervention, and the other as control based on draw of lots. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All. No blinding or incomplete blinding, and the outcome is likely to be influenced by lack of blinding. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: School check‐list. The information was gathered from school authorities and by direct observation. No blinding of outcome assessment, and the outcome measurement is likely to be influenced by lack of blinding; self‐report considered high risk. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: School check‐list. No missing outcome data at school‐level and therefore low risk of attrition bias. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Recruitment to cluster | Low risk | Randomisation post‐recruitment and baseline data collection. |
| Baseline imbalance | Unclear risk | School‐baseline characteristics not reported. Arbitrary zone boundary used to create groups and unclear if systematic differences exist between‐group areas although balance between government and private schools relatively even in both groups. |
| Loss of cluster | Low risk | No loss of clusters. |
| Incorrect analysis | High risk | Unit of analysis error for the primary trial implementation outcome. |
| Contamination | Unclear risk | Even after taking due precautions, it is unclear if cross‐contamination might have occurred in the index study as in any other community trial. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Methods | Trial name: Lifestyle Education for Activity Program (LEAP). Study design: Randomised controlled trial for implementation outcome. Intervention duration: 2 years. Differences in baseline characteristics: There were no baseline age or racial/ethnic differences between girls in the control and the intervention schools. | |
| Participants | School type: High‐schools in 14 South Carolina counties (1998–2000). Region: South Carolina. Demographic/socioeconomic characteristics: No details about participating schools. Of students, 48.7% were African American and 46.7% were White, which was comparable to the population of the participating schools. Number of schools allocated: 24. Numbers by trial group: n (controls baseline) = 12 schools and 1221 girls. n (controls follow‐up) = 12 schools and 741 girls. n (interventions baseline) = 12 schools and 1523 girls. n (interventions follow‐up) = 12 schools and 863 girls. Recruitment: Schools: Not reported. Students: All eighth‐grade girls (n = 8155) who attended 1 of the 31 middle schools that “fed” students to the 24 participating high schools were invited to complete the measures. These girls participated in a school assembly during which the measurement protocol was explained, incentives were described (gifts and promotional items valued at < $10), and all girls were invited to participate. Recruitment rate %: School districts: Not reported. Schools: 24 schools, does not report school recruitment rate. Students: 97% of those recruited completed the baseline measures. (2744/2841 eighth‐grade girls who volunteered to participate in the measurement protocol). | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The LEAP intervention focused on changing personal, social, and environmental factors related to physical activity and involved changes to the school environment and instructional programs. Instructional program components included changes in physical education and health instruction to enhance physical activity self‐efficacy and enjoyment. Schools were not required to implement a specific LEAP curriculum. Rather, to change instructional practice. The environmental strategy involved changing school practices that encouraged and supported physical activity and included changes to school health services, faculty staff health promotion, school environment, and school community linkages. The original six components of LEAP from the Coordinated School Health Program model were expanded to 16 ‘‘essential elements’’(including instructional and environmental). Of these, schools were expected to implement all instructional elements and three environmental elements (school administrator support, school physical activity team, and media messages promoting physical activity). Implementation strategies: EPOC: Educational outreach visits: ‐ Two full‐time program support staff provided. EPOC: Local opinion leaders: ‐ Each LEAP team was headed by a LEAP champion who was usually the teacher responsible for girls PE. The LEAP champion was either the person assigned to be the primary contact for the school or the person who evolved as the strongest supporter of the intervention effort. The LEAP champion, in coordination with the LEAP project staff, worked to involve school administrators, teachers and staff in the LEAP team. EPOC: Educational meetings: ‐ Schools received training and strong encouragement to implement the remaining environmental elements. Staff training consisted of formal workshops and one‐on‐one technical assistance for school personnel. Training was provided through in‐service days before and during the school year. EPOC: Educational materials: ‐ LEAP staff maintained a wide range of resources, including physical activity videotapes, books EPOC: Other: ‐ Equipment (hand weights, exercise bands, pedometers) for the intervention schools. EPOC: Local consensus processes: ‐ LEAP staff worked with the LEAP champion and the LEAP team in each school to identify opportunities to enhance the environment or change school policy in support of physical activity. Training was provided for developing and implementing strategic plans to promote physical activity in the school. LEAP staff provided ongoing consultation and support to LEAP schools through regular visits, phone calls, e‐mail and a listserv. Theoretical underpinning: An ecological model provided the organising framework for the LEAP intervention and drew primarily from social cognitive theory for the overall intervention. Nothing specific to the implementation strategy. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ (Active PA team) School physical activity team‐ A team that regularly plans, implements and evaluates student and faculty PA programs. ‐ (Admin support) School administrator supports physical activity promotion‐ Tangible support from the principal for physical activity (PA) promotion, such as providing time and resources physical education (PE) classes and PA programs; participates on PA team. ‐ (Emphasise lifelong PE) Emphasises lifelong physical activity‐ Classes emphasise a variety lifetime PAs girls enjoy, such as dance, aerobics, strength training, etc. ‐ (Co‐op options in PE) Includes cooperative activities‐ PE has cooperative games, activities, and team‐ building, along with the traditional, competitive sport activities. ‐ (Provide health services) School nurse counselling for physical activity (health services) ‐ School nurse regularly counsels students about PA and has materials related to PA in health room. ‐ (Health promotion for staff) Adult modelling of physical activity through faculty/staff health promotion‐ School has an active wellness program in place which sponsors PA programs for staff. ‐ (Provide health education) Health education reinforces messages and skills taught in physical education ‐ Instructional activities in health education complement and reinforce those taught in PE. ‐ (Co‐ordinate PA events with community) Community agency involvement‐ School collaborates with community agencies to provide PA programs and resources for students, faculty/staff, and families. ‐ (Family involvement) Family involvement‐ Families are provided information about PA, PA resources, and PA opportunities. Data collection method: The organisational assessment interview was a 22‐item interview (administered in 10–15 minute) conducted by the independent process evaluator in all intervention and control schools with a school administrator (usually assistant principal), to assess organisational‐level components (i.e., school environment and instruction practice consistent with the LEAP intervention). This tool assessed organisational‐level factors and, unlike the process tools described in the previous section, was not designed to measure implementation. The organisational assessment rated nine of the essential elements, including seven environmental factors and two instructional factors. Additional items assessed events and activities (secular events) that could affect project outcomes such as participation in physical education teacher training and receiving an award in school health, and organisational resources such as budget for physical education. Validity of measures used: Not reported/self‐report methods. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Physical activity and weight status. Data collection method: Physical activity: The 3‐Day Physical Activity Recall (3DPAR), a modification of the Previous Day Physical Activity Recall, was used to assess physical activity. Weight status: Height and weight were measured in a private setting while students were dressed in light clothing. Height was measured to the nearest 1.0 centimetre with a portable stadiometer (Shorr Productions, Olney, Md); weight was measured to the nearest 0.1 kilogram (kg) with a calibrated digital scale (model PS6600, BeFour, Inc, Saulville, Wis). Body mass index (BMI) was calculated as body weight in kg divided by height in metres squared (kg/m2). Validity of measures used: Physical activity: 3DPAR. Weight status: BMI classified in accordance with the Center for Disease Control and Prevention’s growth charts for BMI. | |
| Notes | Research funding: Supported by a grant from the National Heart, Lung and Blood Institute (R01 HL057775). Conflicts of interest: Authors report no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools were paired by school size, percentage of girls who were African American, urban/suburban or rural location, and class structure. Schools from each pair were randomly assigned to control or intervention groups. The random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All given the nature of the intervention, participants and study personnel are likely to have been aware of study allocation and therefore high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: Organisational assessment interview No blinding of outcome assessment and the outcome measurement is likely to be influenced by lack of blinding; self‐report considered high risk. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: Organisational assessment interview. There were no missing outcome data and therefore low risk of attrition bias. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Methods | Trial name: Go for Health. Study design: Non‐randomised. Intervention duration: 2 years. Differences in baseline characteristics The ethnic distributions were comparable between treatment and control conditions and were similar to the ethnic distribution in the community. Unit of allocation: Schools (elementary). | |
| Participants | School type: Schools (elementary) in Texas City Independent School District. Demographic/socioeconomic characteristics: For all schools combined, ethnic distributions were Anglo‐American (62.3%), Mexican‐American (20.9%), Black‐American (14.8%), and Asian and American Indian (2%). Inclusion/exclusion criteria: Not reported. Number of services allocated: 4 schools included. Numbers by trial group: n (controls baseline) = 2. n (controls follow‐up) = 2. n (interventions baseline) = 2. n (interventions follow‐up) = 2 (1293 third and fourth grade students were enrolled in the four study schools). Recruitment: Schools: All 4 schools in the Texas City Independent School District participated. Students: At baseline 1293 third and fourth grade students were enrolled in the four study schools. Schools: Not reported. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: Innovations introduced into the schools included: 1) the new school lunch,) and 2) health education for healthful diet. Implementation of each of the program components required organisational changes in school programs and in the roles and practices of school personnel. Implementation strategies: Commitment of school district administrators to adopt the program was obtained in writing before intervention was initiated. Principals at each experimental school adopted a statement of support for the goal of providing healthful diet. Planning groups, consisting of teachers and staff, were established to inform intervention staff and to foster program ownership EPOC: Other: ‐ Institutional Commitment: Principals adopted an official statement of support for the goal to provide healthy diet. Alterations in Policies and Practices: 1) Policies to change food purchasing and menu planning 2) policies to support formation of school health task force at each school to develop school wide learning activities. Alterations in roles and actions of staff: 1) Changes to food preparation, presentations, and addition of healthy alternatives, 2) school health task force and school staff plan social learning activities to provide social support for continuation and to assist students to learn targeted behaviours. Student Learning: Changes in behaviour to 1) Increase selection and consumption of low‐sodium, low‐fat foods, 2) Increase duration and frequency in aerobic activity and 3) Skill development, modelling, behaviour rehearsal, reinforcement. School lunch The objective was to reduce the content of sodium and fat served in school lunches by 25% over a two‐year period. EPOC: Monitoring of performance: ‐ Existing menu planning, food purchasing, recipe selection, and food preparation practices were examined by project staff. EPOC: Local consensus processes: ‐ Specific practice changes in four areas purchasing, menu planning, recipes, and food preparation were identified and negotiated with the food service director and with intervention school cafeteria managers. EPOC: Educational outreach visits: ‐ The dietitian worked with the cafeteria managers and cooks to adjust standard recipes to reflect 25% reductions in fat and sodium. To facilitate implementation, food handlers received six hours of summer in‐service training conducted by the project staff in cooperation with cafeteria managers. The food service director and cafeteria managers were actively involved in the development of the new school lunch. ‐ The staff dietitian continually solicited the input and impressions of the cooks both formally and informally. EPOC: Managerial supervision: During the school year, the staff dietitian served as a consultant and was present in the treatment schools on a regular basis, providing feedback on performance and assistance in resolving food viability, recipe preparation, cooking, and serving problems. Health education for healthful diet EPOC: Educational materials: ‐ The innovation consisted of six health education modules on diet. ‐ The modules were attractively packaged with visual aids and teaching materials ready to be handed out to the children. EPOC: Local opinion leaders: ‐ The classroom modules were developed by project staff with the aid of a classroom teacher who had recently retired from the school district. EPOC: Educational outreach visits: ‐ To foster adoption of the modules, teachers were provided with 1 hour of training prior to the start date for each module. EPOC: Other: ‐ Children were eligible to receive token incentives (stickers, T‐shirts, sweat bands) upon completion of the major learning activities. Theoretical underpinning: Charter and Jones framework four levels at which implementation of innovations may occur in a school: 1) institutional commitment, 2) structural context, 3) role performance, and 4) learning activities. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ Sodium content of school meals mg by schools ‐ Fat content of school lunches (g) Data collection method: The identical menu was repeated in March and April each year of the study. At baseline, 12 meals were selected randomly from the March and April menus and analysed for nutrient content. Recipe analyses, based on detailed interviews with each cook in the intervention schools at baseline and in all four schools at mid‐test and post‐test, were conducted by trained staff nutritionists and analysed by the Nutrition Coding Center (NCC). Validity of measures used: Not reported/self‐report methods. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to child diet, physical activity or weight status: Child sodium and fat intake. Data collection method: A 24‐hour dietary recall interview was administered. Each child was interviewed at home in the company of one parent, who was asked about ingredients, food preparation, and other items as needed. Validity of measures used: Not reported. | |
| Notes | Note: This trial also included a PA component in the program however did not report a corresponding implementation outcome measure. Consequently, this trial is reported as a nutrition trial only. Research funding: Supported by Grant HL33376 from National Heart, Lung, and Blood Institute, National Institute of Health. Conflicts of interest: Not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomised trial. Elementary schools were not randomly assigned to experimental condition and therefore high risk of selection bias. |
| Allocation concealment (selection bias) | High risk | Non‐randomised trial. There is no indication that allocation was concealed and therefore at high risk of selection bias. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: All Due to nature of the intervention, school staff and study personnel delivering the intervention were not blind to study allocation. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcome group: New school lunch Blinding of outcome assessment ensured, and unlikely that the blinding could have been broken. (Low risk of bias). Outcome group: Physical education Random, anonymous observations of children’s physical activity were made during physical education classes by trained observers. Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’, e.g. not reported in methods or register. (Unclear risk of bias). Outcome group: Classroom instruction No blinding of outcome assessment and the outcome measurement is likely to be influenced by lack of blinding; self‐report considered high risk. (High risk of bias). Outcome group: Nutrient analysis of school lunches Recipe analyses were conducted by trained staff nutritionists. Insufficient information to permit judgement of ‘Low risk’ or ‘High risk’; e.g. not reported in methods or register. (Unclear risk of bias). |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: New school lunch There were no missing outcome data. Outcome group: Physical education There were no missing outcome data. Outcome group: Classroom instruction Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. Outcome group: Nutrient analysis of school lunches There were no missing outcome data. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Potential confounding | High risk | Appears no adjustments were made in analysis for school‐based confounders. |
| Methods | Trial name: 5‐a‐Day Power Plus. Study design: Cluster‐randomised controlled trial. Intervention duration: Unclear (beginning in the fourth grade (1994‐1995) and throughout the fifth‐grade school year (1995‐1996). Length of follow‐up from baseline: approximately 12 months. Differences in baseline characteristics: Similar – schools were matched pairs that were then randomised. Unit of allocation: Schools. Unit of analysis: Cafeteria observations. | |
| Participants | School type: Elementary schools. Region: St. Paul, Minnesota, USA. Demographic/socioeconomic characteristics: Of the 1750 fourth‐grade students enrolled at baseline, 1.3% were Native American, 6.4% were Hispanic, 19.1% were African American, 25.2% were Asian American (largely Hmong), and 48% were white. Approximately 60% of the students were eligible for free or reduced‐price school meals. Inclusion/exclusion criteria: Not reported. Number of schools allocated: 20 inner‐city public elementary schools. Numbers by trial group: 10 intervention, 10 control. Recruitment: Recruitment strategy not reported. Recruitment rate: Not reported. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The intervention consisted of a parent, industry, curricula and classroom component. Only the food service and curricula components were subject to an implementation strategy. Only the food service component had an implementation outcome assessed between experimental groups and consequently, only food service implementation strategies were extracted. Regarding the food service intervention, the four food service intervention strategies were 1) point‐of‐purchase promotion of fruit and vegetable using characters and messages from the classroom curricula, 2) increasing the appeal of fruit and vegetable by enhancing their attractiveness, 3) increasing the variety and choice of fruit and vegetable served, and 4) offering an additional fruit choice on days when baked or frozen desserts were served. These four strategies involved eight guidelines on how to offer appealing fruit and vegetable choices and four promotion guidelines. Implementation strategies: EPOC: Educational meetings: ‐ Centralised training sessions were held for food service staff from the intervention schools. It was held during a regularly scheduled school day and was conducted by the 5‐a‐Day Power Plus staff. Food service staff attended the teacher training for 2 hours and also attended 2‐hour training after school each of the 2 intervention years. Food service staff members were paid for attending the training members were paid for attending the training. EPOC: Other: ‐ A local producer provided some fruit and vegetable for use in classroom taste testing, home snack packs, and to expand choice in school lunch. They also provided a 30‐minute presentation on fruit and vegetable to each of the fifth‐grade intervention classrooms. Service staff members were paid for attending the training. Theoretical underpinning: 5‐a‐Day Power Plus intervention program was guided by social cognitive theory and social learning theory. Description of control: Not reported but assume usual practice. | |
| Outcomes | Outcome relating to the implementation of school service policies, practices or programs: ‐ Mean number of fruit and vegetable choices available 4th grade ‐ Mean number of fruit and vegetable choices available 5th grade ‐ Mean % of eight guidelines on how to offer appealing fruit and vegetable met 4th grade ‐ Mean % of eight guidelines on how to offer appealing fruit and vegetable met 5th grade ‐ Mean % of four fruit and vegetable promotions met 4th grade ‐ Mean % of four fruit and vegetable promotions met 5th grade Data collection method: An observation‐based process evaluation method was also developed to assess the food service intervention implementation. Direct observations were conducted in each of the 10 intervention and 10 control schools on a monthly basis using trained observers and standardised protocols and instruments. Validity of measures: Not reported however, considered an objective measure of implementation. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Student dietary intake. Data collection method: 24‐hour quantified food record and recall and student lunchroom observations. Validity of measures used: Not stated although observations considered an objective measure. | |
| Notes | Research funding: Supported by Grant R01CA59805 from the National Institute of Health. Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Schools were matched in pairs and randomly allocated to experimental group. The random sequence generation procedure is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: Participants (teachers and cooks) were aware that they were being asked to implement an intervention. There was no blinding to group allocation and this is likely to influence performance. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: Trained evaluation staff visited each school to conduct observations using standardised protocols and measures. However, there is no information provided about whether these personnel were blinded to group allocation and teacher self‐reported measures were completed. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: There is no report of any schools dropping out of the study. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Recruitment to cluster | Low risk | Individuals within each randomised cluster participated. |
| Baseline imbalance | Low risk | Schools were randomly allocated to condition and so risk of baseline imbalance is low. |
| Loss of cluster | Low risk | There is no report of any schools dropping out of the study. |
| Incorrect analysis | High risk | There was no reporting of statistical techniques apart from simple t‐tests. |
| Contamination | Low risk | Schools were randomly allocated to condition and so the risk of contamination is low. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
| Methods | Trial name: No trial name. Study design: Cluster‐randomised controlled trial. Intervention duration: Two school terms. Differences in baseline characteristics: Assumed to be zero. | |
| Participants | School type: Primary school. Demographic/socioeconomic characteristics: Socioeconomically disadvantaged communities. Inclusion/exclusion criteria: Inclusion ‐ Government or Catholic schools. ‐ Located within HNE Local Health District. ‐ having a socioeconomic status score of 5 or less (lower 50% of NSW) based on school postcode. ‐ Not participating in other physical activity studies. Number of services allocated: 46 Numbers by trial group: n (controls baseline) = 21 n (controls follow‐up) = 21 n (interventions baseline) = 25 n (interventions follow‐up) = 25 Recruitment: Schools: 46 Students: 1139 Schools: 72% Students: 58% | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The evidence‐based school physical activity program known as SCORES (Supporting Children’s Outcomes using Rewards, Exercise and Skills) was rolled out in primary schools and the implementation intervention strategies facilitated its roll out. Implementation strategies: EPOC: Audit and feedback Schools were provided feedback on the implementation of the intervention on three occasions via email. Classroom teachers were given detailed feedback reports on PE lesson quality on two occasions. Feedback was based on the SAAFE teaching principles. EPOC: Education materials Teachers were provided with resources (lesson booklets, posters, whistles, lanyards and fundamental motor skills cards) to support delivery of high quality PE lessons, teach fundamental motor skills and increase MVPA within PE lessons. EPOC: Education meeting All classroom teachers were offered a 90‐minute professional learning workshop including theory and practical sessions. The workshop focused on delivery of fundamental motor skills to students, strategies to improve lesson quality through student engagement and increase students’ MVPA. The quality PE teaching principles were from the original SCORES program and known as the Supportive, Active, Autonomous, Fair and Enjoyable (SAAFE) teaching principles. In additional, teachers were required to team teach a PE lesson with experienced Health Promotion staff on one occasion. EPOC: Education outreach visits Peer teaching with experienced Health Promotion staff with a PE background was offered to classroom teachers in intervention schools. PE lessons were also observed, followed by written feedback and verbal encouragement. EPOC: Local opinion leader A meeting with school executive was held at the commencement of intervention and a school champion nominated for each school. School champions were responsible for embedding the physical activity practices within the school and leading policy development. Ongoing support was provided throughout the intervention from experienced Health Promotion staff. EPOC: Other Ongoing Support: was provided to school champions to embed the practices within their schools. Additional support was provided to classroom teachers via five short (five minute) video clips viewed in staff meetings, reinforcing the quality PE teaching principles (based on the SAAFE principles). Classroom teachers were provided with stickers to be used as prompts for quality PE and issued to students throughout practical PE. School champions provided prompts to classroom teachers to implement the strategies via email, electronic calendar reminders, and in meetings. School champion also received a polo shirt. Intervention schools also received equipment ($180) to support delivery of recess and lunchtime activities. Theoretical underpinning: Social‐ecological theory. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: ‐ School PA policy or plan (% of schools). ‐ Overall lesson quality score. ‐ Recess PA (mean % of days offered). ‐ Lunch PA (mean % of days offered). ‐ Provision of sports equipment at recess (mean % of days offered). ‐ Provision of sports equipment at lunch (mean % of days offered). ‐ Provision of parent newsletters regarding PA. Data collection method: Survey and observation. Validity of measures used: Not reported/contains both objective and self‐report measures. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to child diet, physical activity or weight status: Physical activity. Data collection method: Accelerometer Validity of measures used: Objective. | |
| Notes | Research funding: No financial disclosures were reported by the authors of this paper. Conflicts of interest: All authors declare no conflict of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Cluster‐RCT. The random sequence produced using computerised random number function in Microsoft Excel. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: Both the schools and the health promotion staff delivering the intervention were aware of the schools’ group allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome group: PE teaching quality Low: Lessons observed by trained research staff with experience in PE, blinded to group allocation. Outcome group: School physical activity practices High: Teacher reported practices and due to the nature of the intervention teachers could not be blinded and therefore at high risk of detection bias. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: School Physical Activity practice 2 Low: “69 lessons were observed (88% of eligible lessons)” Outcome group: School Physical Activity practice 1, 3 & 4 High: “141 (87 intervention, 54 control) of the 382 eligible school teachers (37%) completed an online survey across the 46 participating intervention and control schools.” High attrition and unequal across study arms. |
| Selective reporting (reporting bias) | Low risk | “The trial was registered with the Australian New Zealand Clinical Trials Registry (ACTRN12615000437561)” All predetermined outcomes are reported. |
| Recruitment to cluster | Low risk | Recruitment bias: Individuals within each randomised cluster participated/random allocation of schools to group occurred post‐recruitment. |
| Baseline imbalance | Low risk | Baseline imbalance: Schools were randomly allocated to condition and so risk of baseline imbalance is low. |
| Loss of cluster | High risk | Loss of clusters: High risk of loss of clusters based on teacher reported data. |
| Incorrect analysis | Unclear risk | Incorrect analysis: Unclear if clustering was taken into account for the teacher reported school physical activity practices. |
| Contamination | Low risk | Contamination: The unit of randomisation is the school and so risk of contamination is low. |
| Compatibility with individually randomised RCTs | Unclear risk | Compatibility with individually randomised RCTs (cluster‐RCTs): Unable to determine if a herd effect exists. |
| Methods | Trial name: No trial name. Study design: Non‐randomised. Intervention duration: 1 year. Length of follow‐up from baseline: Approximately 1 year between baseline and follow‐up data collection Spring 2004 (Baseline data collection) to Spring 2005 (follow‐up data collection). Recruitment date not provided. Differences in baseline characteristics: Intervention schools had more students eligible for free/reduced‐price meal (32.9%) compared to controls (20.0%). Unit of allocation: School. Unit of analysis: School. | |
| Participants | School type: Public Schools (High). Region: Maine, USA. Demographic/socioeconomic characteristics: % students eligible for free/reduced‐price meal: control = 20.0%, intervention = 32.9%. No further details of student demographics provided. Inclusion/exclusion criteria: Inclusion: ‐ Participation in National school Lunch Program (NSLP). ‐ Offered an à la carte program. ‐ Have at least 1 snack and 1 beverage vending machine accessible to students. Exclusion: Not Provided. Number of schools allocated: 7. Numbers by trial group: n (controls baseline) = 3. n (controls follow‐up) = 3. n (interventions baseline) = 4. n (interventions follow‐up) = 4. Recruitment: Electronic informational letter sent from The Maine Department of Education to all superintendents (n = 150). Interested schools (n = 50) were screened by telephone. Recruitment rate: 7 schools expressed interest and met inclusion criteria (denominator unknown). | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: Implementing low‐fat, low‐sugar and portion controlled guidelines in à la carte and vending (snack and beverage) programs. Implementation strategies: EPOC: Educational outreach visits: ‐ Visits by research staff to each schools food and beverage supplier to identify items that met the LFLS guidelines. EPOC: Educational materials: ‐ Suppliers who stocked vending machines were given lists of the available LFLS items (expected to stock from the Fall 2004) and letters sent home to parents and students informing them of changes incentives. Banners were also displayed to promote healthier foods and taste testing was conducted. EPOC: Clinical practice guidelines: ‐ Modification of recipes and preparation techniques by research and food service personnel. EPOC: Procurement and distribution of supplies: ‐ Food service directors were given lists of available products/vendors that met LFLS guidelines. EPOC: Educational meetings: ‐ Presentations describing LFLS guideline made to school administrations, faculty and/or staff EPOC: External funding: ‐ $1500 allocated annual to school liaison personnel. EPOC: Local consensus process: ‐ A committee at each school site was created. A liaison identified at each school was responsible for establishing a the committee to promote the healthy changes in the vending machines and à la carte menus at their schools. Expectations for the committees were discussed in detail with each school liaison; these expectations included recruitment of representatives from all stakeholder groups — school administration, faculty, students, parents, and food service personnel — and the completion of at least four activities over the course of the school year to promote the healthy changes EPOC: Other: ‐ Early communication between the project team and schools began in 2004 as a means to obtain the cooperation of school administration, and meet food service personnel. Theoretical underpinning: Not reported. Description of control: Made no changes to à la carte and vending machine programs for 1 school year. | |
| Outcomes | Outcome relating to the implementation of school service policies, practices or programs: ‐ % items meeting nutrient (LFLS) criteria in à la carte. ‐ % items meeting nutrient (LFLS) criteria in snack vending. ‐ % items meeting nutrient (LFLS) criteria in beverage vending. ‐ % items meeting nutrient (LFLS) AND proportion criteria in à la carte. ‐ % items meeting nutrient (LFLS) AND proportion criteria in snack vending. ‐ % items meeting nutrient (LFLS) AND proportion criteria in beverage vending. Data collection method: Trained personnel visited the school on 5 consecutive non‐randomised days at baseline and follow‐up. Observation and recording of items sold was taken at breakfast and lunch at cafeterias. Vending machine data included: number of machines, items and nutritional information completed on the same day as nutritional observation. Validity of method: Not reported however methods considered objective. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Consumption of sugar sweetened beverages. Data collection method: Food frequency Questionnaire: Subjects were asked to complete the youth food frequency questionnaire for what they ate and drank over the past 30 days. Validity of method: The youth food frequency questionnaire has been shown to be valid in youth (defined as 9 to 18 years of age) with mean correlation of r = 0.49 for food groups from the youth food frequency questionnaire compared with three 24‐ hour recalls. | |
| Notes | Research funding: Supported by a grant from the Centers for Disease Control and Prevention (03022). Conflicts of interest: Not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐randomised design. High risk of selection bias as high schools volunteered into the intervention or control group. |
| Allocation concealment (selection bias) | High risk | Non‐randomised design. High schools volunteered into an experimental group, therefore high risk of bias as no concealment of allocation. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: High schools volunteered as intervention or control, therefore participants and personnel were not blind to allocation and there is a high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | Unclear risk | Outcome group: Trained personnel visited each school to conduct observations. There is no information provided about whether these personnel were blinded to group allocation (i.e. may have conducted observations only and be unaware of the purpose of the study) and therefore the risk of detection bias is unclear. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: No schools dropped out and this study conducted observations of à la carte and vending programs in schools. |
| Selective reporting (reporting bias) | Unclear risk | There is no study protocol therefore it is unclear if there was selective outcome reporting. |
| Potential confounding | Unclear risk | The characteristics of the school and food environments are presented for the control and intervention groups (i.e. number of students, percentage of students eligible for free/reduced‐price meal, closed campus policy during lunch, offered à la carte breakfast). However, given this is a quasi‐experimental trial with no random allocation it is unclear if all potential confounders were measured. |
| Methods | Trial name: No trial name. Study design: Randomised controlled trial. Intervention duration: 12 to 14 months. Length of follow‐up from baseline: To assess the primary trial outcome, data were collected at baseline (April to September, 2013) and at the completion of the implementation period (November, 2014 to April, 2015). Differences in baseline characteristics: There were no significant differences in baseline characteristic among schools. Unit of allocation: Schools. Unit of analysis: Schools. | |
| Participants | School type: Primary schools. Region: Hunter region of NSW, Australia Demographic/socioeconomic characteristics: The trial region contained a socioeconomically diverse group. Inclusion/exclusion criteria: Schools from the study region were randomly selected and invited to participate. Inclusion: ‐ Schools were required to have an operational canteen ‐ Ethier one or more items on their canteen menu that was restricted for sale (‘red’ or ‘banned’) or less than 50% Exclusion: ‐ Nongovernment schools ‐ Schools with both primary and secondary students ‐ Schools catering exclusively for children requiring specialist care Number of schools allocated: 70 Numbers by trial group: n (controls baseline) = 35 n (controls follow‐up) = 30 n (interventions baseline) = 35 n (interventions follow‐up) = 27 Recruitment: Recruitment continued until 70 schools provided consent for study participation. Recruitment rate: 88% as 80 schools were assessed for eligibility. Note. no sample sizes for children in enrolled schools given. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The New South Wales (NSW) Government launched a Healthy School Canteen Strategy (also known as Fresh Tastes @ School) to help prevent childhood obesity. The strategy classified foods sold by schools as ‘red’, ‘amber’ or ‘green’ based on their nutritional content. The strategy was adopted as policy by the government education department, and all government schools were mandated to remove items classified as ‘red’ from regular sale. Furthermore, schools were encouraged to ‘fill the menu’ with items classified as ‘green’ and ensure items classified as ‘amber’ did not dominate the menu. The primary aim of this study was to assess the effectiveness of a multi‐strategic intervention to increase implementation of the state‐wide healthy canteen policy. Implementation strategies: EPOC: Audit and feedback ‐ Performance monitoring and feedback menu reviews were conducted quarterly (unless menus were unchanged), and the results were used to compile written feedback reports to the canteen manager and school principal. Verbal discussion of the reports occurred during academic detailing visits or via telephone support calls. EPOC: Continuous quality improvement ‐ Policy implementation support Schools were allocated a support officer with qualifications in nutrition and dietetics and experience in supporting schools to implement the policy. Support officers contacted canteen managers every 2 months (via email, telephone or in person) throughout the intervention and used a continuous quality improvement framework of repeated goal setting, action planning, self‐monitoring and problem‐solving with canteen managers. EPOC: External funding ‐ Schools were also offered a small reimbursement to cover the costs associated with canteen manager attendance at training. EPOC: Education materials ‐ Tools and resources‐ Printed instructional materials, sample policies/menus, planning templates, pricing guides, product lists of policy compliant menu items, supplier contacts and menu assessment feedback were provided to all school canteen managers during the workshop or mailed to non‐attenders of the workshop. EPOC: Education meeting ‐ Canteen managers, canteen staff and parent representatives were invited to attend a training workshop (5 hours) with the aim of providing education and skill development in the policy, nutrition and food label reading, canteen stock and financial management, pricing and promotion, and change management. Training combined didactic and interactive components including opportunities for self‐assessment, role play and facilitator provided feedback. Training was facilitated by a support officer. EPOC: Education outreach visits ‐ School canteen visits were conducted 1 and 3 months post‐canteen manager training to enable support officers to observe the operational canteen environment, provide feedback and assist with problem‐solving barriers to policy implementation EPOC: Local consensus process ‐ Meetings between support officers and canteen staff were held to discuss and reach consensus regarding the policy, how best to implement it and to develop local canteen action plans to co‐ordinate implementation tasks. EPOC: Local opinion leader ‐ Executive support school principals were asked to communicate support for policy implementation and maintenance to teachers, parents, students and canteen managers during staff meetings, in newsletters and assemblies. Support officers also sought meetings with the executive of parent representative groups to garner their support for and input on policy implementation. EPOC: Tailored intervention ‐ Individualised goal setting, action planning with canteen managers at different schools EPOC: Other ‐ Quarterly project newsletters communicated key messages, provided information and case studies of successful implementation approaches to common barriers. ‐ Recognition Schools with a menu assessed as adhering to the policy (i.e. greater than 50% ‘green’ items and no ‘red’ or ‘banned’ items) received a congratulatory letter and phone call from the research team and were publicly acknowledged via marketing strategies. ‐ Canteen managers also received kitchen equipment to the value of AUD$100. Theoretical underpinning: The selection of intervention components was guided by the Theoretical Domains Framework. Description of control: No contact was made, and no resources provided to control schools during the intervention period by the research team. | |
| Outcomes | Outcome relating to the implementation of school service policies, practices or programs: ‐ The proportion of schools with a canteen menu that did not contain foods or beverages restricted for sale (‘red’ and ‘banned’) under the policy. ‐ The proportion of schools where healthy canteen items (‘green items’) represented more than 50% of listed menu items. Data collection method: Copies of canteen menus were collected from all participating schools and audited by two dietitians independently. Validity of method: Not reported yet objective. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: As a measure of potential adverse effects yearly income and expenditure of canteen profitability were calculated. Data collection method: canteen’s financial records. Validity: Objective. Outcome relating to child diet, physical activity or weight status: Mean (95% CI) energy, total fat and sodium of student purchases. Data collection method: Direct observation. Validity of method: Objective. | |
| Notes | Research funding: This work was supported by the Australian Research Council who provided funding for the trial [LP130101008]. In‐kind support was provided by the Hunter New England Population Health and the Hunter Medical Research Institute. Conflicts of interest: Authors report grants from Australian Research Council Linkage Project Scheme (LP130101008) during the conduct of the study; (2) no financial relationships with any organisation that might have an interest in the submitted work in the previous 3 years; and (3) no other relationships or activities that could appear to have influenced the submitted work. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised controlled trial. The random sequence was generated using a random number function in Microsoft Excel. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: School staff (principals and canteen managers) were not blinded to group allocation. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome group: Data collectors were blinded to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: 13 of the 70 (19%) schools did not provide their menu for assessment at follow‐up. There were no significant differences in baseline characteristics among schools that did and did not provide follow‐up data. |
| Selective reporting (reporting bias) | Low risk | There were no unreported implementation outcomes according to those planned in the published protocol. |
| Methods | Trial name: CAFÉ Study design: Randomised controlled trial. Intervention duration: 12 months Length of follow‐up from baseline: To assess the primary trial outcome, data were collected at baseline (Feb–Oct 2013) and follow‐up (Sept 2014–Jan 2015). Differences in baseline characteristics: No differences in the baseline characteristics of participating schools in the intervention and control group were apparent Unit of allocation: Schools. Unit of analysis: Schools. | |
| Participants | School type: Primary schools. Region: The study was conducted in the Hunter New England Local Health District of New South Wales, Australia. Demographic/socioeconomic characteristics: The study region consisted of a socioeconomically and demographically diverse population of approximately 112,000 children aged 5–12 years. Inclusion/exclusion criteria: Inclusion: ‐ Rural or remote primary schools within areas within the study region. ‐ Having a canteen open at least one day per week. ‐ Were not compliant with the NSW Healthy School Canteen Policy, defined as either having at least one canteen menu item restricted for sale (‘red’ or ‘banned’ item) or having less than 50% of menu items classified as healthy (‘green’ items) (based on dietitian assessment of the supplied canteen menu). Exclusion: ‐ Schools enrolling both primary and secondary students. ‐ Schools catering exclusively for children requiring specialist care. Number of schools allocated: 72 Numbers by trial group: n (controls baseline) = 36 n (controls follow‐up) = 24 n (interventions baseline) = 36 n (interventions follow‐up) = 29 Recruitment: 72 schools Recruitment rate: 64% | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: As part of the New South Wales obesity prevention strategy in 2005 the State government introduced the NSW Healthy School Canteen Policy called ‘Fresh Tastes @ School’. The policy was based on the 2003 Australian Dietary Guidelines and utilises a traffic light system to classify menu items as ‘red’, ‘amber’ or ‘green’ based on their nutritional profile (including energy, saturated fat, and/or salt). ‘Red’ items are typically nutrient poor, high‐energy foods; ‘amber’ items are considered to have some nutritional value, however if consumed in large amounts can contribute to excess energy intake, and ‘green’ items are those that are considered to be good sources of nutrients, such as fruit, vegetables and lean meats. The ‘Fresh Tastes @ School’ policy requires that schools: i) provide primarily ‘green’ items (> 50% of the menu) and ii) restrict the sale of ‘red’ foods and remove ‘banned’ drinks. Government primary schools are mandated to implement the policy, while implementation amongst non‐government schools is strongly encouraged. The efficacy of the intervention (implementation) strategies to facilitate the implementation of the Fresh Tastes @ School policy were tested in this trial. Implementation strategies: EPOC: Audit and feedback ‐ Menu audit: A dietitian who was blind to group allocation and not involved in the delivery of the intervention undertook audits of the canteen menus using a standardised template based on the ‘Fresh Tastes @ School’ policy. Canteen managers were requested to provide a copy of their menu and additional information needed to assess menu compliance with the ‘Fresh Tastes @ School’ policy (as described above). Additional phone contact was made by the dietitian as needed to obtain all necessary information to classify menu items as ‘red’, ‘banned’, ‘amber’ and ‘green’ according to the policy. Subsequent menu audits were planned for each term (four over a 12‐month period) with verbal and written feedback (described below) provided after each audit. Feedback report Dietitians developed a standard feedback report template which summarised whether or not the school menu complied with the ‘Fresh Tastes @ School’ policy. The feedback report was delivered via email or mail by a member of the health promotion team, depending on individual school preference. The report graphically displayed the proportion of ‘red’, ‘banned’, ‘amber’ and ‘green’ items on the menu and outlined the school’s compliance with the ‘Fresh Tastes @ School’ policy. Specific suggestions on how to change canteen menus to meet the requirements of the ‘Fresh Tastes @ School’ policy were provided including: healthy recipes, ideas about how to increase the number of ‘green’ items on their menu, and alternative food options to replace specific ‘red’ foods or ‘banned’ drinks. The health promotion staff also provided other useful resources based on canteen managers’ reported requirements, as assessed during the feedback calls (described below in ‘Resources’). EPOC: Continuous quality improvement ‐ Feedback calls: During the initial feedback call, the Health Promotion Officer reiterated the purpose of the report, discussed the results, clarified any unclear components, supported the canteen manager to undertake a goal‐setting process to identify key areas for improvement in order to improve compliance with the ‘Fresh Tastes @ School’ policy, and developed an action plan to overcome existing barriers to policy compliance. In all subsequent calls (two to four), the Health Promotion Officer tailored the discussion to the needs of the Canteen Manager based on previous contact; and monitored their actions and progress toward their goals, set new goals where required, or monitored compliance. Where possible, the same Health Promotion Officer provided support to the same school throughout the intervention period. Two of the five Health Promotion Officers had qualifications in nutrition and dietetics, however all support officers received the same training in implementing strategies to support organisational change processes and intervention delivery. EPOC: Education materials ‐ All intervention schools were provided with ‘Fresh Tastes @ School’ resources (including a Canteen Menu Planning guide, recipes, and a manual on financial management and food safety), healthy food guidelines, a menu planning template, sample policies and menus, pricing guides and a local suppliers buyer’s guide which lists foods that meet the ‘amber’ and ‘green’ criteria, developed by a state nutrition agency which provides canteen support to their member schools (Healthy Kids Association). EPOC: Tailored intervention ‐ The specific number of menu audits, feedback reports and calls provided was tailored depending on each school’s compliance with the guidelines and whether menu changes had occurred between the previous and planned menu audit; and the responsiveness of the canteen manager to the feedback (e.g. whether they declined to take feedback calls). Theoretical underpinning: The selection of specific canteen manager behaviour change techniques was based on Control Theory, which has previously been applied to audit and feedback interventions Description of control: Usual practice: Schools in the control group received the standard offer of professional development opportunities provided through the NSW Government’s Live Life Well @ School initiative. No support to implement the Fresh Tastes @ School was specifically provided by the local health promotion unit. | |
| Outcomes | Outcome relating to the implementation of school service policies, practices or programs: ‐ Proportion of schools having a canteen menu that did not contain any ‘red’ foods or ‘banned’ drinks ‐ Proportion of schools having a canteen menu that contained > 50% ‘green’ items as specified by the ‘Fresh Tastes @ School’ policy Data collection method: ‐ Menu audits were used to assess the primary trial outcome. Canteen managers were asked to supply their current canteen menu and participate in follow‐up telephone calls from dietitians to collect additional information required to assess menu compliance. If additional information was required to classify a menu item according to the policy, dietitians collected additional product information from canteen managers via phone or email using a standard data collection template. Validity of measure: Not reported/contains both objective assessments and self‐reports. Outcome relating to staff knowledge, skills or attitudes: Not reported. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Not reported. | |
| Notes | Research funding: In‐kind funding was received by Hunter New England Population Health to support conduct of the trial. Some authors were Postdoctoral Research Fellows funded by the National Heart Foundation and the National Health and Medical Research Council Career Statistical support was funded by the Priority Research Centre for Health Behaviour. Conflicts of interest: The authors declare that they have no competing interests. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised controlled trial. The random sequence was produced using a computer‐generated randomisation schedule in Microsoft Excel. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: Due to the nature of the intervention schools could not be blinded to group allocation and therefore at high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | Low risk | Outcome group: Menu audits were undertaken by dietitians blinded to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: 19 of the 72 (26%) schools did not provide menus at follow‐up. There were no significant differences in baseline characteristics among schools that did and did not provide follow‐up data. |
| Selective reporting (reporting bias) | Low risk | There were no unreported implementation outcomes according to those planned in the published protocol. |
| Methods | Trial name: Trial of Activity for Adolescent Girls (TAAG). Study design: Cluster‐randomised controlled trial. Intervention duration: 2‐year study‐directed intervention (Fall 2003 to Spring 2005). A third‐year intervention used school and community personnel to direct intervention activities. Differences in baseline characteristics: The study population was diverse with the largest percentage of African‐American girls in Louisiana and South Carolina and the largest percentage of Hispanic girls in California and Arizona. Differences between groups at baseline were not presented. | |
| Participants | School type: Schools (Middle). Demographic/socioeconomic characteristics: Not reported. ‐ Public middle schools (grades 6–8) were eligible if the majority of children enrolled lived in the community served by the school, so that the community component of the intervention would be relevant to them. ‐ Schools were excluded if they were unwilling or unable to respond to and report medical emergencies during the trial; plan to close or merge within 3 years, fewer than 90 girls in the 8th Grade, expected transience of > 38% in any given year or 35% over 2 years; does not offer physical education each semester for all grades; Fewer than 2 (year‐round schools) or 3 (semester‐based schools) physical education classes per week; participation in pilot testing of the study materials. ‐ Student exclusions included unable to read or understand questions in English, been told not to participate in or avoid exercise for health reasons, or have an existing medical condition; parent unwilling or unable to give consent; girls unwilling to assessment measurement. Number of schools allocated: 36. Numbers by trial group: n (controls baseline) = 18. n (controls follow‐up) = 18. n (interventions baseline) = 18. n (interventions follow‐up) = 18. Note: All 36 schools participated in the 6th‐grade measurements during Spring 2003 and in the 8th grade measurements during Spring 2005; however, only 34 schools participated in the 8th grade measurements during Spring 2006. Recruitment: Students: In each of 36 schools (6 per field centre), 60 randomly selected sixth‐grade girls were invited at baseline to be measured with a goal of measuring at least 80% (48) of those girls. At the end of the 2‐year intervention (end point) and in the subsequent year (follow‐up), 120 randomly selected eighth‐grade girls per field centre will be invited to participate in the measurements. Recruitment rate: Schools: Of the 68 schools invited to participate, 41 agreed (60%) and the 36 most conveniently accessed from the university‐based research centres were selected. Students: During 2003 Spring, 60 girls per school were randomly chosen. A total of 1721 (79.7%) of the 2160 eligible girls consented and participated in the measurement. During 2005 Spring, 4123 girls were eligible for the student‐level measurements, and 3504 (85.0%) consented and participated in the measurements. During 2006 Spring, 3915 were eligible at the six study sites, and 3502 (89.5%) consented and participated in the measurements. The approximate doubling of the number of girls measured in each 8th‐grade survey compared to the 6th‐grade survey was purposeful and based on our determination that the smaller 6th‐grade sample would have little adverse effect on power. | |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: Adaptation of PE classes to meet TAAG objectives and implementation of health education lessons were assessed through structured observations throughout the academic year by TAAG staff and teacher surveys at the end of the school year (dose, fidelity and acceptability). Implementation strategies: EPOC: Education meetings: ‐ Health education, PE, science or homeroom teachers attended workshops to teach a series of six lessons that promoted development of behavioural skills associated with physical activity. Each health education lesson included an activity challenge (i.e. homework) in which students monitored a behaviour and set goals to increase their activity. EPOC: Education materials: ‐ PE teachers received instructional materials for PE lessons; social marketing efforts that included posters, flyers and special activities were launched to encourage overall physical activity and promote TAAG‐specific programs to students. EPOC: Educational outreach visits: ‐ PE teachers received regular on‐site support to conduct lessons that encouraged active participation of girls during PE classes and to promote out‐of‐class physical activity. EPOC: Inter‐professional education: ‐ Collaborations were created between schools, community agencies and TAAG university staff to increase girl‐focused physical activity programs outside of PE classes. EPOC: Local opinion leaders: ‐ Program champions were recruited and trained during the second intervention year, and they directed the intervention to enhance its sustainability in the third year. EPOC: Local consensus processes: ‐ Intervention goals were identified to indicate optimal intervention implementation. Goals varied by component, but essentially were set for 100% fidelity for delivery of the intervention by TAAG staff to teachers and 80% fidelity for delivery by teachers to the students. Theoretical underpinning: Social‐ecological model, operant learning theory, social cognitive theory, organisational change and diffusions of innovation. | |
| Outcomes | Outcome relating to the implementation of school policies, practices or programs: Continuous ‐ Average number of physical activity programs Dichotomous ‐ Students were encouraged for out‐of‐PE‐class physical activity (percentage of classes) ‐ Teacher used strategies to minimise management time (% classes) ‐ Students were provided with choices (percentage of classes) ‐ Students were encouraged for in‐class physical activity (% classes) ‐ Student equipment ratio was appropriate for activity (% classes) ‐ Group sizes were appropriate for activity (percentage of classes) ‐ Percentage of school reporting collaborations Data collection method: Implementation of TAAG PE: Fidelity: Measured by observation. Implementation variable was observed ‘some’, ‘most’ or ‘all’ of class. Intervention goal = observation of 50% for item 1, 80% for all other items. Collaboration: Interview with Principal. Average number PE programs: Measured by surveys of physical activity program leaders at intervention and control schools. Validity of measures used: Trial used a combination of objective and self‐report components to assess implementation outcome. The self‐report components are reported as validated. Outcome relating to staff knowledge, skills or attitudes: Non‐assessed between groups. Outcome relating to cost: Not reported. Outcome relating to adverse consequences: Not reported. Outcome relating to child diet, physical activity or weight status: Physical activity and body composition. Data collection method: Physical activity: Assessed by accelerometer (Daily MET weighted minutes of MVPA). Sedentary minutes were defined as the number of minutes with less than light activity. Anthropometry: BMI, height, weight and percentage body fat. Standing height was measured without shoes using a portable stadiometer (Shorr Productions) to the nearest 0.1 cm. Body weight was assessed using a digital scale (Seca 880) and measured to the nearest 0.1 kg while the girl was dressed in light clothing without shoes. Triceps skinfold thickness was measured in triplicate on the right side of the body to the nearest 0.1 mm. BMI was calculated as weight (kg)/height (m2). Percentage body fat was estimated from anthropometric measures using an equation that was developed for use in girls in this age range. Validity of measure: Physical activity: Not reported. Anthropometry: Valid. | |
| Notes | Research funding: National Heart, Lung and Blood Institute; National Institutes of Health (U01HL66858, U01HL66857, U01HL66845, U01HL66856, U01HL66855, U01HL66853 and U01HL66852). Conflicts of interest: Authors report no conflicts of interest. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was stratified by field centre and by school district. The random sequence generation is not described. |
| Allocation concealment (selection bias) | Unclear risk | There is no information provided about allocation concealment and therefore it is unclear if allocation was concealed. |
| Blinding of participants and personnel (performance bias) | High risk | Outcome group: There is no mention that participants or personnel were blinded to experimental group and therefore at high risk of performance bias. |
| Blinding of outcome assessment (detection bias) | High risk | Outcome group: It is not reported that observers or participants were blind to group allocation. |
| Incomplete outcome data (attrition bias) | Low risk | Outcome group: Low school attrition rate reported. All 36 schools participated in the measurements in 2003 and 2005 and 34 schools participated in 2006. |
| Selective reporting (reporting bias) | Low risk | There were no unreported implementation outcomes according to those planned in the published protocol. |
| Recruitment to cluster | Low risk | Individuals within each randomised cluster participated. |
| Baseline imbalance | Low risk | Schools were randomly allocated to condition and so risk of baseline imbalance is low. |
| Loss of cluster | Low risk | Two of the 36 schools in Louisiana were closed due to damage from Hurricane Katrina. There is no mention though to which condition these were assigned. |
| Incorrect analysis | Low risk | All analyses took into account the expected positive intraclass correlation among responses for students, teachers and classes in the same school and school‐ or community‐level responses within the same site. |
| Contamination | Low risk | The unit of randomisation is the school and so risk of contamination is low. |
| Compatibility with individually randomised RCTs | Unclear risk | Unable to determine if a herd effect exists. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Does not report results of a trial | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Does not report results of a trial | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Does not report results of a trial | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| No baseline data, non‐randomised | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate intervention | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| No baseline data, non‐randomised | |
| Does not report results of a trial | |
| Inappropriate outcomes | |
| Does not report results of a trial | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Does not report results of a trial | |
| No baseline data, non‐randomised | |
| No baseline data, non‐randomised | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate intervention | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| No baseline data, non‐randomised | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Does not report results of a trial | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate intervention | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Does not report results of a trial | |
| Inappropriate intervention | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate intervention | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Does not report results of a trial | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| No baseline data, non‐randomised | |
| Non‐controlled study/inappropriate comparator | |
| No baseline data, non‐randomised | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Does not report results of a trial | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Does not report results of a trial | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate intervention | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate intervention | |
| Inappropriate participants OR inappropriate setting | |
| Non‐controlled study/inappropriate comparator | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Non‐controlled study/inappropriate comparator | |
| Inappropriate outcomes | |
| Inappropriate participants OR inappropriate setting | |
| Inappropriate outcomes | |
| Inappropriate outcomes | |
| Inappropriate outcomes |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Scaling‐up an efficacious school‐based physical activity intervention: Study protocol for the ‘Internet‐based Professional Learning to help teachers support Activity in Youth’ (iPLAY) cluster randomized controlled trial and scale‐up implementation evaluation |
| Methods | Study design: Two complementary studies will be conducted and evaluated alongside each other. |
| Participants | School type: Primary. Region: New South Wales (NSW), Australia. |
| Interventions | Number of experimental conditions: 2 (1 intervention, 1 control). Policies, practices or programs targeted by the intervention: The program targeted by the intervention is a modified version of the SCORES program. SCORES was a comprehensive, multicomponent physical activity and fundamental movement skills program for primary schools. The modified intervention centres around online delivery of professional learning to teachers. The modified intervention will be known as iPLAY (Internet‐based Professional Learning to help teachers to support Activity in Youth) and will be facilitated by various implementation strategies/interventions. Implementation strategies: ‐ Professional learning ‐ Rewards for teachers ‐ Action plan ‐ Individualised mentoring to primary teachers and feedback ‐ Peer observations and group discussions ‐ Prompts and self‐reflection ‐ Online learning and resources ‐ Social marketing |
| Outcomes | Outcome relating to the implementation of childcare service policies, practices or programs: ‐ A range of implementation outcomes will be collected and may be appropriate for inclusion. |
| Starting date | Enrolments began: 13/06/2016 |
| Contact information | A/Prof Chris Lonsdale, Institute for Positive Psychology and Education, Australian Catholic University, Locked Bag 2002, Strathfield NSW 2135 |
| Notes | Trial registration: Australia and New Zealand Clinical Trials Registry ( ACTRN12616000731493 ). Date of registration: June 3, 2016. |

Study flow diagram.
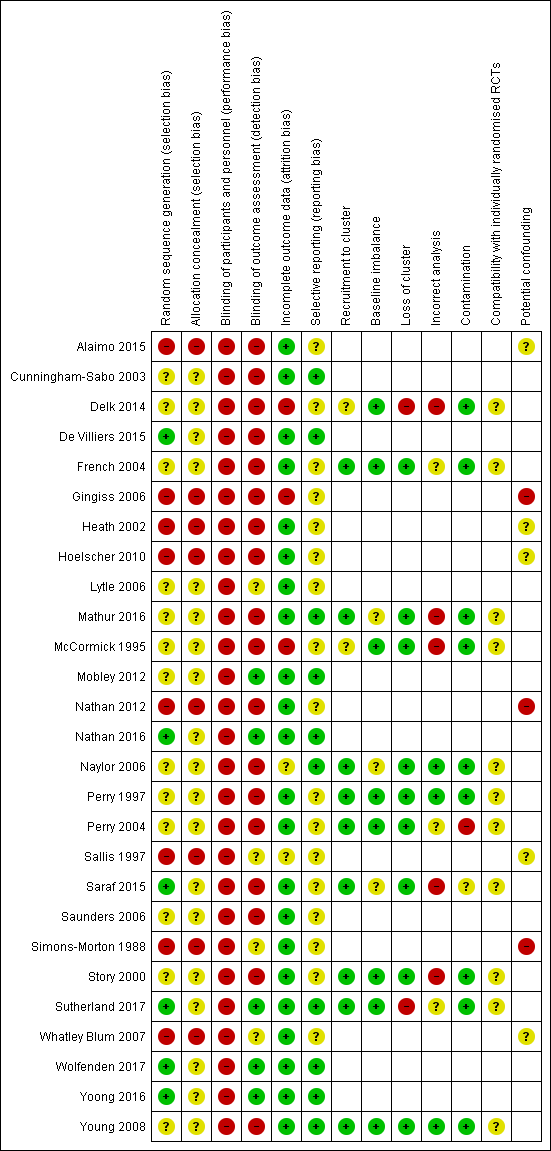
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
| Strategies for enhancing the implementation of school‐based policies or practices targeting risk factors for chronic disease | |||
| Patient or population: School aged children (5 ‐ <18 years) Settings: School Intervention: Any strategy (e.g. educational materials, educational meetings, audit and feedback, opinion leaders, education outreach visits) with the intention of improving the implementation of health promoting policies, programs or practices for physical activity, healthy eating, obesity prevention, tobacco use prevention or alcohol use prevention in schools Comparison: No intervention or usual practice (22 trials), alternate intervention (2 trials) or minimal support comparison group (3 trials) | |||
| Outcomes | Impact | Number of Participants | Quality of the evidence |
| Implementation of school‐based policies, practices or programs that aim to promote healthy or reduce unhealthy behaviours relating to child diet, physical activity, obesity, or tobacco or alcohol use | We are uncertain whether strategies improve the implementation of school‐based policies, practices or programs that aim to promote healthy or reduce unhealthy behaviours relating to child diet, physical activity, obesity, or tobacco or alcohol use. Among 13 trials reporting dichotomous implementation outcomes—the proportion of schools or school staff (e.g. classes) implementing a targeted policy or practice—the median unadjusted (improvement) effect sizes ranged from 8.5% to 66.6%. Of seven trials reporting the percentage of a practice, program or policy that had been implemented, the median unadjusted effect (improvement), relative to the control ranged from ‐8% to 43%. The effect, relative to control, reported in two trials assessing the impact of implementation strategies on the time per week teachers spent delivering targeted policies or practices ranged from 26.6 to 54.9 minutes per week. | 1599 schools (27 trials) | Very lowa,b |
| Measures of student physical activity, diet, weight status, tobacco or alcohol use | We are uncertain whether strategies to improve the implementation of school‐based policies, practices or programs targeting risk factors for chronic disease impact on measures of student physical activity, diet, weight status, tobacco or alcohol use | 29,181 studentsf (21 trials) | Very lowa,b,c |
| Knowledge, skills or attitudes of school staff involved regarding the implementation of health promoting policies, or practices | We are uncertain whether strategies to improve the implementation of school‐based policies, practices or programs targeting risk factors for chronic disease impact on the knowledge, skills or attitudes of school staff | 1347 stakeholders (3 trials) | Very lowa,b |
| Cost or cost‐effectiveness of strategies to improve the implementation | We are uncertain whether strategies to improve the implementation of school‐based policies, practices or programs targeting risk factors for chronic disease are cost‐effective | 42 schools (1 trial) 473 students (1 trial)g | Very lowa,b,d |
| Unintended adverse effects of strategies to improve implementation on schools, school staff or children | We are uncertain whether strategies to improve the implementation of school‐based policies, practices or programs targeting risk factors for chronic disease result in unintended adverse effects or consequences | 68 schools and 4603 studentsh (2 trials) | Very lowb,c |
| High quality: Further research is very unlikely to change our confidence in the estimate of effect. | |||
| aDowngraded one level due to limitations in the design. bDowngraded one level due to unexplained heterogeneity. cDowngraded one level due to indirectness. dDowngraded one level due to imprecision. eGRADE Working Group grades of evidence fTwo trials measured student behaviour through the use of non‐student data (e.g. purchases) and did not provide student sample sizes. gOne trial reported on the impact of an intervention on school level revenue. One trial reported on cost‐effectiveness. hOne trial measured adverse events through the use of non‐student data (i.e. canteen profits) and did not provide student sample sizes. | |||
| Trial | Audit and feedback | Clinical practice guidelines | Continuous quality improvements | Distribution of supplies | External funding | Education games | Education materials | Education meeting | Education outreach visits | Inter‐ professional education | Length of consultation | Local consensus process | Local opinion leader | Managerial supervision | Monitoring performance of delivery | Pay for performance | Tailored intervention | The use of communication technology | Other |
| X | X | X | X | X | X | ||||||||||||||
| X | X | X | X | ||||||||||||||||
| X | X | X | X | ||||||||||||||||
| X | X | X | X | X | X | ||||||||||||||
| X | X | X | X | ||||||||||||||||
| X | X | X | X | ||||||||||||||||
| X | X | X | |||||||||||||||||
| X | X | X | X | X | X | X | |||||||||||||
| X | X | X | X | ||||||||||||||||
| X | X | X | X | X | |||||||||||||||
| X | X | X | |||||||||||||||||
| X | X | X | X | X | X | X | X | ||||||||||||
| X | X | X | X | X | X | X | |||||||||||||
| X | X | X | X | X | X | X | |||||||||||||
| X | X | X | X | X | X | ||||||||||||||
| X | X | X | X | ||||||||||||||||
| X | X | X | X | X | |||||||||||||||
| X | X | X | X | X | |||||||||||||||
| X | X | X | X | X | X | X | |||||||||||||
| X | X | X | X | X | X | ||||||||||||||
| X | X | X | X | X | X | X | |||||||||||||
| X | X | ||||||||||||||||||
| X | X | X | X | X | X | ||||||||||||||
| X | X | X | X | X | X | X | X | ||||||||||||
| X | X | X | X | X | X | X | X | X | |||||||||||
| X | X | X | X | ||||||||||||||||
| X | X | X | X | X | X |
| EPOC subcategory | Definition |
| Audit and feedback | A summary of health workers’ performance over a specified period of time, given to them in a written, electronic or verbal format. The summary may include recommendations for clinical action. |
| Clinical practice guidelines | Clinical guidelines are systematically developed statements to assist healthcare providers and patients to decide on appropriate health care for specific clinical circumstances'(US IOM). |
| Educational materials | Distribution to individuals, or groups, of educational materials to support clinical care, i.e. any intervention in which knowledge is distributed. For example this may be facilitated by the Internet, learning critical appraisal skills; skills for electronic retrieval of information, diagnostic formulation; question formulation. |
| Educational meetings | Courses, workshops, conferences or other educational meetings. |
| Educational outreach visits, or academic detailing | Personal visits by a trained person to health workers in their own settings, to provide information with the aim of changing practice. |
| External funding | Financial contributions such as donations, loans, etc. from public or private entities from outside the national or local health financing system. |
| Inter‐professional education | Continuing education for health professionals that involves more than one profession in joint, interactive learning. |
| Length of consultation | Changes in the length of consultations. |
| Local consensus processes | Formal or informal local consensus processes, for example agreeing a clinical protocol to manage a patient group, adapting a guideline for a local health system or promoting the implementation of guidelines. |
| Local opinion leaders | The identification and use of identifiable local opinion leaders to promote good clinical practice. |
| Managerial supervision | Routine supervision visits by health staff. |
| Monitoring the performance of the delivery of healthcare | Monitoring of health services by individuals or healthcare organisations, for example by comparing with an external standard. |
| Other | Strategies were classified as other if they did not clearly fit within the standard subcategories. |
| Pay for performance – target payments | Transfer of money or material goods to healthcare providers conditional on taking a measurable action or achieving a predetermined performance target, for example incentives for lay health workers. |
| Procurement and distribution of supplies | Systems for procuring and distributing drugs or other supplies. |
| Tailored interventions | Interventions to change practice that are selected based on an assessment of barriers to change, for example through interviews or surveys. |
| The use of information and communication technology | Technology based methods to transfer healthcare information and support the delivery of care. |
| Trial | Trial name | Targeted risk factor | Implementation strategies | Comparison | Primary Implementation outcome and measures | Effect size | P < 0.05 |
| School Nutrition Advances Kids (SNAK) | Nutrition | Clinical practice guidelines, educational materials, educational outreach visits, external funding, local consensus processes, tailored interventions | Usual practice or waiting‐list control | Continuous: i) Nutrition policy score and ii) Nutrition education and/or practice score (2 measures) | Median (range) 0.65 (0.2 to 1.1) | 0/2 | |
| Pathways | Nutritionc | Clinical practice guidelines, educational materials, educational meetings, educational outreach visits | Usual practice | Continuous: Nutrient content of school meals % of calories from fat breakfast/lunch (2 measures) | Median (range) ‐3% (‐3.3% to ‐2.7%) | 1/2 | |
| HealthKick | Nutritionc | Local opinion leaders, educational materials, educational outreach visits, education meetings | Minimal support control | Dichotomous: % implementing a variety of policies and practices (3 measures) | Median (range) 25% (12.5% to 29.5%) | Not reported | |
| No trial name | Physical activity | Local consensus process, educational meetings, clinical practice guidelines, educational outreach visits, tailored interventions, other | Different implementation strategy | Continuous: % of teachers that conducted activity breaks weekly (1 measure 2 comparisons) Dichotomous: % implementing a variety of policies and practices (2 measures 4 comparisons) | Median (range) 13.3% (11.1% to 15.4%) Median (range) 26.5% (19.4% to 31.9%) | 6/6 | |
| Trying Alternative Cafeteria Options in Schools (TACOS) | Nutrition | Local consensus processes, tailored intervention, educational meetings, pay for performance | Usual practice or waiting‐list control | Continuous % of program implementation (5 measures) | Median (range) 33% (11% to 41%) | 5/5 | |
| Texas Tobacco Prevention Initiative | Tobacco | Educational meetings, educational outreach visits, external funding, local consensus processes | Usual practice | Dichotomous: % implementing a variety of policies and practices (10 measures) | Median (range) 18.5% (‐1% to 59%) | 7/10 | |
| El Paso Coordinated Approach to Child Health (El Paso CATCH) | Nutritionc | Educational materials, educational meetings, educational outreach visits | Usual practice | Continuous: % fat in school meal (2 measures) Sodium of school meals (2 measures) | Effect size Median (range) ‐1.7% (‐4.4% to 1%) Median (range) ‐29.5 (‐48 to ‐11) | 1/4 | |
| Travis County Coordinated Approach To Child Health (CATCH) Trial | Nutrition and physical activity | Educational materials, educational meetings, educational outreach visits, pay for performance, other, the use of information and communication technology, local consensus process | Different implementation strategy | Continuous: Mean number of lessons/or activities (5 measures) Dichotomous: % implementing a variety of policies and practices (2 measures) | Median (range) 0.8 (‐0.4 to 1.2) Median (range) 4.4% (3.6% to 5.2%) | 4/7 | |
| Teens Eating for Energy and Nutrition at School (TEENS) | Nutrition | Educational materials, educational meetings, local opinion leaders, local consensus processes | Usual practice or waitling‐list control | Dichotomous: % of schools offering or selling targeted foods (4 measures) | Median (range) 8.5% (4% to 12%) | 2/4 | |
| Bihar School Teachers Study (BSTS) | Tobacco | Local opinion leader, continuous quality improvement, education materials, education meeting, local consensus process | Usual practice or waiting‐list control | Dichotomous: % implementing a variety of policies and practices (2 measures) | Median (range) 56.9% (36.3% to 77.5%) | 2/2 | |
| The North Carolina School Health and Tobacco Education Project (SHTEP)/ Skills Management | Tobacco | Educational meetings, local consensus processes, educational materials | Minimal support control | Dichotomous: % later implementation of curriculum for school district (1 measure) Continuous: Mean extent later implementation for school district (% of total curriculum activities taught) (1 measure) | Effect Size (95%CI) 16.7% (‐37.7% to 64.1%) Mean differencea 0.56% | 0/2 | |
| HEALTHY study | Nutritionc | Educational games, educational meetings, external funding, tailored intervention, educational materials, educational outreach, other, the use of information and communication technology | Usual practice or waiting‐list control | Dichotomous: % schools meeting various nutrition goals (12 measures) | Median (range) 15.5% (0% to 88%) | Not reported | |
| Good for Kids. Good for Life | Nutrition | Educational materials, educational meetings, local consensus processes, local opinion leaders, other, monitoring the performance of the delivery of the healthcare, tailored interventions | Minimal support control | Dichotomous: % Schools implementing a vegetable and fruit break (1 measure) | Mean difference (95%CI) 16.2% (5.6% to 26.8%) | 1/1 | |
| No trial name | Nutrition | Audit and feedback, continuous quality improvement, education materials, education meeting, local consensus process, local opinion leader, tailored intervention, other | Usual practice | Dichotomous: % implementing a variety of policies and practices (2 measures) | Median (range) 35.5% (30.0% to 41.1%) | 2/2 | |
| Action Schools! British Columbia (BC) | Physical activity | Educational materials, educational meetings, educational outreach meetings, local consensus process, other, tailored Interventions | Usual practice or waiting‐list control | Continuous: Minutes per week of physical activity implemented in the classroom (1 measure 2 comparisons) | Median (range) 54.9 minutes (46.4 to 63.4) | 2/2 | |
| Child and Adolescent Trial for Cardiovascular Health (CATCH) | Nutrition and physical activityd | Educational materials, educational meetings, educational outreach visits, other | Usual practice or waiting‐list control | Continuous: % of kilocalories from fat in school lunch (1 measure) Mean milligrams of sodium in lunches (1 measure) Cholesterol milligrams in lunches (1 measure) Quality of PE lesson % of 7 activities observed (1 measure) | Effect size Mean difference (95%CI) ‐4.3% (‐5.8% to ‐2.8%) Mean difference (95%CI) ‐100.5 (‐167.6 to ‐33.4) Mean difference (95%CI) ‐8.3 (‐16.7 to 0.1) Mean difference (95%CI) 14.3% (11.6% to 17.0%) | 3/4 | |
| The Cafeteria Power Plus project | Nutrition | Educational meetings, educational outreach visits, educational materials, local consensus processes, other | Usual practice or waiting‐list control | Continuous: % of program implementation (2 measures) Mean number of fruit and vegetables available (2 measures) | Median (range) 14% (‐2% to 30%) Median (range) 0.64 (0.48 to 0.80) | 2/4 | |
| Sports, Play, and Active Recreation for Kids (SPARK) | Physical activity | Educational materials, educational meetings, educational outreach visits, length of consultation, other | Usual practice or waiting‐list control | Continuous: Duration (minutes) per week of physical education lessons (1 measure) Frequency (per week) of physical education lessons (1 measures) | Mean difference (95%CI) 26.6 (15.3 to 37.9) Mean difference (95%CI) 0.8 (0.3 to 1.3) | 2/2 | |
| No trial name | Nutrition, physical activity and tobacco | Educational games, educational materials, educational meetings, local consensus processes, local opinion leaders, tailored Interventions, other | Usual practice | Dichotomous: % implementing a variety of policies and practices (6 measures) | Median (range) 36.9% (‐5.3% to 79.5%) | 5/6 | |
| Lifestyle Education for Activity Program (LEAP) | Physical activity | Educational materials, educational meetings, educational outreach visits, local consensus processes, local opinion leaders, other | Usual practice or waiting‐list control | Continuous: School level policy and practice related to physical activity from the school administrators perspective (9 measures) | N/Ab | Not reported | |
| Go for Health | Nutritionc | Educational materials, educational outreach visits, local consensus processes, local opinion leaders, managerial supervision, monitoring of performance, other | Usual practice | Continuous: Macronutrient content of school meals (2 measures) | N/Ab | Not reported | |
| 5‐a‐Day Power Plus | Nutrition | Educational meetings, other | Usual practice | Continuous: Mean number of fruit and vegetables available (2 measures) % of guidelines implemented and % of promotions held (4 measures) | Median (range) 1.15 (1 to 1.3) Median (range) 38.4% (28.5% to 43.8%) | 6/6 | |
| Supporting Children’s Outcomes using Rewards, Exercise and Skills (SCORES) | Physical activity | Audit and feedback, education materials, education meeting, education outreach visits, local opinion leader, other | Usual practice or waiting‐list control | Dichotomous: % implementing a variety of policies and practices (2 measures) Continuous: Physical education lesson quality score (1 measures) % of program implementation (4 measures) | Median (range) 19% (16% to 22%) Mean difference 21.5a Median (range) ‐8% (‐18% to 2%) | 0/2 1/1 0/4 | |
| No trial name | Nutrition | Clinical practice guidelines, educational materials, educational meetings, educational outreach visits, external funding, distribution of supplies, local consensus process, other | Usual practice or waiting‐list control | Continuous: % of food and beverage items meeting guideline nutrient and portion criteria (6 measures) | Median (range) 42.95% (15.7% to 60.6%) | 5/6 | |
| No trial name | Nutrition | Audit and feedback, continuous quality improvement, external funding, education materials, education meeting, education outreach visits, local consensus process, local opinion leader, tailored intervention, other | Usual practice | Dichotomous: % implementing a variety of policies and practices (2 measures) | Median (range) 66.6% (60.5% to 72.6%) | 2/2 | |
| CAFÉ | Nutrition | Audit and feedback, continuous quality improvement, education materials, tailored intervention | Usual practice | Dichotomous: % implementing a variety of policies and practices (2 measures) | Median (range) 21.6% (15.6% to 27.5%) | 0/2 | |
| Trial of Activity for Adolescent Girls (TAAG) | Physical activity | Education materials, education meetings, educational outreach visits, inter‐professional education, local consensus processes, local opinion leaders | Usual practice | Dichotomous: % implementing a variety of policies and practices (7 measures) Continuous: Average number of physical activity programs taught (1 measure) | Median (range) 9.3% (‐6.8% to 55.5%) Effect Size (95%CI) 5.1 (‐0.4 to10.6) | 1/8 | |
| aNo measure of variability. bDid not report aggregate results by group. cPhysical activity was also a targeted risk factor however, this component did not meet our inclusion criteria (e.g. implementation outcomes unavailable, study staff implemented physical activity component etc.) and was therefore, not considered in our review. dTobacco use was also a targeted risk factor however, this component did not meet our inclusion criteria (e.g. implementation outcomes unavailable) and was therefore, not considered in our review. | |||||||

