Resonancia magnética de perfusión para diferenciar gliomas de bajo y alto grado en la primera consulta
Resumen
Antecedentes
Los gliomas son el tumor cerebral primario más habitual. Se califican mediante el sistema de clasificación de la OMS en astrocitomas de grado II‐IV, oligodendrogliomas y oligoastrocitomas. Los gliomas de grado bajo (GGB) son tumores cerebrales infiltrativos de grado II de la OMS que habitualmente parecen sólidos y no realzados en la imagenología de resonancia magnética (IRM). Los pacientes con GGB a menudo tienen poco o ningún déficit neurológico, por lo cual pueden optar por un enfoque de vigilancia‐y‐espera sobre la resección quirúrgica, la radioterapia o ambas, debido a que la cirugía puede dar lugar a discapacidad neurológica temprana. Ocasionalmente, los gliomas de grado alto (GGA, grado III y IV de la OMS) pueden tener la misma apariencia que los GGB en la IRM. La adopción de un enfoque de vigilancia‐y‐espera podría ser perjudicial para el paciente si el tumor progresa rápidamente. Las técnicas de imagenología avanzadas se usan cada vez más en la práctica clínica para predecir el grado del tumor y ayudar en la decisión clínica de cuándo intervenir quirúrgicamente. Una de dichas técnicas de imagenología avanzada es la perfusión por resonancia magnética (RM), que detecta cambios hemodinámicos anormales relacionados con la mayor angiogénesis y la permeabilidad vascular, o "fugas" que ocurren con la histología tumoral agresiva. Las mismas son reflejadas por los cambios en el volumen sanguíneo cerebral (VSC) expresado como cVSC (cociente de VSC tumoral a VSC de la materia blanca de apariencia normal) y la permeabilidad, medida como Ktrans.
Objetivos
Determinar la exactitud diagnóstica de la prueba de la perfusión por RM para identificar a los pacientes con GGB primarios sólidos y no realzados (grado II de la OMS) en la primera consulta en niños y adultos. Al realizar el análisis cuantitativo para esta revisión, los pacientes con GGB se consideraron positivos para la enfermedad mientras que los pacientes con GGA se consideraron negativos para la enfermedad.
Determinar qué características clínicas y metodológicas afectan la exactitud de la perfusión por RM.
Métodos de búsqueda
La estrategia de búsqueda utilizó dos conceptos: (1) el glioma y las diversas histologías de interés, y (2) la perfusión por RM. Se utilizaron estrategias de búsqueda estructuradas apropiadas para cada base de datos consultada, que incluyeron: MEDLINE (Ovid SP), Embase (Ovid SP) y Web of Science Core Collection (Science Citation Index Expanded and Conference Proceedings Citation Index). La búsqueda más reciente para esta revisión se realizó el 9 noviembre 2016.
También se identificó "literatura gris" de los registros en línea de actas de congresos del American College of Radiology, de la European Society of Radiology, de la American Society of Neuroradiology y de la European Society of Neuroradiology en los últimos 20 años.
Criterios de selección
Los títulos y los resúmenes extraídos de los resultados de la búsqueda se seleccionaron para obtener los artículos de texto completo para la inclusión o la exclusión. Se estableció contacto con los autores para aclarar u obtener datos faltantes o no publicados.
Se incluyeron estudios transversales que realizaron la perfusión por RM de susceptibilidad dinámica (DSC, por sus siglas en inglés) o dinámica mejorada por contraste (DCE, por sus siglas en inglés) o ambas de los GGB y los GGA sin tratar y en los que se informaron los valores del cVSC o el Ktrans. Se seleccionaron los participantes con gliomas sólidos y no realzados sometidos a la perfusión por RM en el plazo de los dos meses antes de la confirmación histológica. Se excluyeron los estudios en participantes que recibieron radiación o quimioterapia antes de la perfusión por RM, o en pacientes sin confirmación histológica.
Obtención y análisis de los datos
Dos autores de la revisión extrajeron información sobre las características de estudio y los datos, y evaluaron la calidad metodológica mediante la herramienta Quality Assessment of Diagnostic Accuracy Studies (QUADAS‐2). Se presentó un resumen de las características de estudio y los resultados de QUADAS 2; y se calificaron los estudios como de buena calidad cuando presentaban un riesgo bajo de sesgo en los dominios del estándar de referencia del diagnóstico tisular y el flujo y el momento adecuado entre la perfusión por RM y el diagnóstico tisular.
En el análisis cuantitativo, los GGB se consideraron positivos para la enfermedad, mientras que los GGA fueron negativos para la enfermedad. La sensibilidad se refiere a la proporción de GGB detectados por la perfusión por RM, y la especificidad como la proporción de GGA detectados. Se elaboraron tablas de dos‐por‐dos con los positivos verdaderos y los negativos falsos como el número de GGB diagnosticados de forma correcta e incorrecta, respectivamente, mientras que los negativos verdaderos y los positivos falsos son el número de GGA diagnosticados de forma correcta e incorrecta, respectivamente.
El metanálisis se realizó en los estudios con tablas de dos‐por‐dos, con un análisis de sensibilidad adicional utilizando los estudios de buena calidad. Los datos limitados impidieron el análisis de regresión para explorar la heterogeneidad aunque se realizó el análisis de subgrupos en los grupos de histología tumoral.
Resultados principales
Siete estudios con tamaños de muestra pequeños (cuatro a 48) cumplieron con los criterios de inclusión. Los mismos se realizaron principalmente en hospitales universitarios y la mayoría incluyó a pacientes adultos. Todos los estudios realizaron la perfusión por RM con DSC y describieron métodos heterogéneos de adquisición y posprocesamiento. Sólo un estudio realizó la perfusión por RM con DCE, lo cual impidió el análisis cuantitativo.
El uso de los datos a nivel del paciente permitió la selección de los participantes individuales relevantes a la revisión, con riesgos generalmente bajos de sesgo para los dominios de la selección de los participantes, el estándar de referencia y el flujo y el momento adecuado. La mayoría de los estudios no usaron un umbral predeterminado, lo cual se consideró una fuente significativa de sesgo, sin embargo, este hecho no afectó el análisis cuantitativo debido a que se adoptó un umbral común del cVSC de 1,75 para la revisión. Las inquietudes con respecto a la aplicabilidad fueron escasas.
De los datos publicados y no publicados, 115 participantes fueron seleccionados e incluidos en el metanálisis. Los cVSC promedio (rango) de 83 GGB y 32 GGA fueron de 1,29 (0,01 a 5,10) y 1,89 (0,30 a 6,51), respectivamente. Mediante el umbral ampliamente aceptado del cVSC de <1,75 para diferenciar el GGB del GGA, los cálculos resumidos de la sensibilidad/especificidad fueron de 0,83 (IC del 95%: 0,66 a 0.93)/0,48 (IC del 95%: 0,09 a 0,90). El análisis de sensibilidad mediante cinco estudios de buena calidad produjo una sensibilidad/especificidad de 0,80 (IC del 95%: 0,61 a 0,91)/0,67 (IC del 95%: 0,07 a 0,98). El análisis de subgrupos para la histología tumoral demostró una sensibilidad/especificidad de 0,92 (IC del 95%: 0,55 a 0,99)/0,42 (IC del 95%: 0,02 a 0,95) en los astrocitomas (6 estudios, 55 participantes) y 0,77 (IC del 95%: 0,46 a 0,93)/0,53 (IC del 95%: 0,14 a 0,88) en los oligodendrogliomas+oligoastrocitomas (seis estudios, 56 participantes). Los datos fueron demasiado dispersos como para investigar cualquier diferencia entre los subgrupos.
Conclusiones de los autores
La evidencia limitada disponible impide la estimación fiable del rendimiento del cVSC derivado de la perfusión por RM con DSC para la identificación del grado en un GGB sólido sin tratar y no realzados en comparación con el GGA. Los datos agrupados produjeron una gama amplia de cálculos tanto para la sensibilidad (rango 66% a 93% para la detección del GGB) como para la especificidad (rango 9% a 90% para la detección del GGA). No fue posible determinar otras características clínicas y metodológicas que afectaron la exactitud de la técnica a partir de los datos limitados. Se necesita un tamaño de la muestra más grande tanto del GGB como del GGA, preferentemente mediante un enfoque de exploración estandarizado y con un estándar de referencia actualizado que incorpore los perfiles moleculares para establecer una conclusión definitiva.
PICOs
Resumen en términos sencillos
¿Cuán exacta es la perfusión por RM, un método de IRM avanzado, para diferenciar los gliomas de grado bajo de los gliomas de grado alto en niños y adultos?
¿Por qué es importante la diferenciación de los gliomas de grado bajo y de grado alto?
Los gliomas de grado bajo (GGB) son tumores cerebrales de crecimiento lento que tienen una apariencia característica en la IRM estándar. Los pacientes con GGB que tienen pocos o ningún síntoma pueden preferir retardar el tratamiento hasta el momento en que experimenten la progresión de los síntomas o la apariencia del tumor en la IRM; lo cual se denomina enfoque de vigilancia‐y‐espera. Sin embargo, ocasionalmente, los gliomas de grado alto (GGA), que son agresivos y requieren tratamiento inicial, pueden imitar la apariencia de los GGB. Sólo al examinar los tejidos obtenidos mediante la cirugía ‐ mediante el muestreo (biopsia) o la extracción del tumor (resección) ‐ es posible diferenciar el GGB y el GGA de forma definitiva. Sin embargo, un paciente con pocos o ningún síntoma puede desear evitar el riesgo de discapacidad neurológica temprana como resultado de la intervención quirúrgica. Por lo tanto, un método no invasivo y exacto para diferenciar los gliomas puede ayudar en la toma de decisiones de los pacientes de optar por un enfoque de vigilancia‐y‐espera o de recibir el tratamiento inicial.
¿Cuál era el objetivo de esta revisión?
La revisión está orientada a determinar cuán exacta es la perfusión por RM para diferenciar los GGB y los GGA, y qué factores afectan su exactitud. Los investigadores en Cochrane incluyeron siete estudios para responder esta pregunta.
¿Qué se estudió en esta revisión?
Se estudió una técnica de IRM avanzada denominada perfusión por RM. Este método detecta los vasos sanguíneos anormales que presentan un aumento de tamaño de los gliomas de grado bajo a los de grado alto. A diferencia de la intervención quirúrgica, la perfusión por RM es no invasiva y permite a los médicos determinar si los pacientes pueden adoptar un enfoque de vigilancia‐y‐espera, es decir, retardar el tratamiento incluida la revisión tisular inicial que requiere cirugía.
¿Cuáles son los principales resultados de la revisión?
El análisis incluyó resultados de 115 pacientes. Los resultados indican que en teoría, si la perfusión por RM fuera a usarse en 100 pacientes con tumores cerebrales con apariencia de GGB en la IRM estándar, de los cuales 72 en realidad presentan GGB, luego:
‐ se calcula que 74 tendrán un resultado de la perfusión por RM que indicará que tienen GGB, y de estos 15 tendrán GGA;
‐ se calcula que 26 tendrán un resultado de la perfusión por RM que indicará que tienen GGA, y de los mismos 13 tendrán GGB.
¿Cuán confiables son los resultados de los estudios en esta revisión?
En los estudios incluidos, el diagnóstico de GGB o GGA se realizó mediante la evaluación de todos los pacientes con una revisión tisular, y la mayoría fueron sometidos a la resección. El anterior se considera un método fiable para decidir si los pacientes en realidad presentan GGB o GGA.
El número pequeño de pacientes incluidos en esta revisión es una limitación principal para el análisis. Los cálculos de los estudios individuales y los datos agrupados fueron variables o presentaron una gama amplia. Los números informados en los resultados principales anteriormente son un promedio de los estudios de la revisión, aunque no se conoce si la perfusión por RM siempre producirá estos resultados. Además, los estudios incluidos difirieron en cómo se realizó la perfusión por RM, y el agrupamiento de los datos del análisis puede ser inapropiado.
¿Para quiénes son relevantes los resultados de esta revisión?
Los estudios incluidos se realizaron en Europa (Italia, Suecia, España, Francia), Asia (Japón) y América del Sur (Brasil) y la perfusión por RM se realizó principalmente en hospitales universitarios. La mayoría de los estudios incluyeron a adultos por lo cual los resultados pueden no ser representativos de los niños.
¿Cuáles son las implicaciones de esta revisión?
Los resultados basados en 115 pacientes mostraron que la perfusión por RM puede detectar un 66% a un 93% de los GGB, lo cual significa que un 7% a un 34% de los pacientes con GGB pueden ser clasificados de forma errónea como con GGA y por lo tanto ser sometidos a un tratamiento invasivo temprano con el riesgo consiguiente de eventos adversos. Mientras tanto, alrededor de la mitad de los pacientes con GGA pueden ser clasificados de forma errónea como con GGB, y por lo tanto ser sometidos a un tratamiento retardado. Debido a la incertidumbre en los cálculos las cifras pueden variar de un 9% a un 90% de los pacientes. Debido a la gama amplia de cálculos, actualmente, no puede determinarse cuán exacta es la perfusión por RM para diferenciar los GGB y los GGA. Los estudios futuros que informen la evidencia deberían incluir a un gran número de pacientes con GGB y GGA.
¿Cómo de actualizada está esta revisión?
Se buscaron y utilizaron estudios publicados desde 1990 hasta noviembre de 2016.
Authors' conclusions
Summary of findings
| Population | Almost all adults | |||||
| Setting | Mostly university hospitals, employing exclusively 1.5T or 3T MRI scanners | |||||
| Index test | Dynamic susceptibility contrast MR perfusion (commonly gradient echo rather than spin echo sequence acquisition), usually without contrast preload, typically using arterial input function or gamma variate function post‐processing algorithms, and preferentially using region‐of‐interest method to obtain Max rCBV values (CBV ratio of tumour: contralateral normal appearing white matter) | |||||
| Importance | For solid and non‐enhancing brain tumours with low rCBV, patients with no or little neurologic deficit may opt for conservative management over surgery to avoid early neurologic disability. Meanwhile, patients with high rCBV could favour early treatment for better tumour control. | |||||
| Reference standard | All with histologic examinations, majority with resection. | |||||
| Studies | Mostly prospective cross sectional studies (no case‐control studies) | |||||
| Positive Test | Summary accuracy | No. of study participants / selected patients | Prevalence | Implications | Quality of studies | Comments |
| rCBV threshold <1.75 indicates LGG | Sensitivity (proportion of LGG detected by MR perfusion) 0.83 (0.66, 0.93) (proportion of HGG detected by MR perfusion) 0.48 (0.09 to 0.90) | 392 patients / 115 with solid non‐enhancing Grade II‐IV gliomas who underwent tissue sampling within 2 months of MR perfusion (7 studies) | In a hypothetical population of solid and non‐enhancing Grade II‐IV gliomas, the prevalence of LGGs and HGGs is 72% and 28%, respectively. | Given 100 patients with solid and non‐enhancing infiltrative gliomas, 72 will have LGG and 28 with HGG. Of 72 patients with LGG, it is expected 12 patients will be misclassified to have HGG (but this could potentially be between 5 to 24 patients) and may undergo surgery, thus risking early neurologic deterioration. Meanwhile, of 28 patients with HGG, 15 will be misclassified to have LGG (but this could be between 3 to 25 patients), which may lead to a delay in treatment that can potentially adversely affect outcomes. | Generally low risk of bias in the patient selection domain, excepting 2 out of 7 studies with unclear patient sampling and inappropriate exclusion of small tumours. High risk of bias in the index test domain, mainly because 6 out of 7 studies did not use a pre‐specified threshold. However this did not affect meta‐analysis as we used a common rCBV threshold of 1.75. Low concerns of applicability for the patient selection, index test and reference standard domains by using patient‐level data. | Low numbers (4 to 48) with target and alternative conditions per study and only 2 studies had >20 patients. In general, individual studies had heterogeneous sensitivity and specificity, both with wide confidence intervals. Only 1 study had low risk of bias and low concern of applicability across all domains. Five studies were considered good quality (i.e., with low risk of bias in the domains of reference standard and flow & timing). Their sensitivity analysis yielded sensitivity 0.80 (95% CI 0.61 to 0.91) and specificity 0.67 (95% CI 0.07 to 0.98). Subgroup analysis showed sensitivity/specificity of [0.92 (95% CI 0.55 to 0.99)/ 0.42 (95% CI 0.02 to 0.95) in astrocytomas and 0.77 (95% CI 0.46 to 0.93)/0.53 (95% CI 0.14 to 0.88) in oligodendrogliomas + oligoastrocytomas. Data were too sparse to investigate any differences across subgroups. |
| HGG: high‐grade glioma, LGG: low‐grade glioma, rCBV: relative cerebral blood volume | ||||||
Background
Target condition being diagnosed
Epidemiology and pathology
Gliomas are tumours that arise from glial cells which form the supporting architecture of the brain. In the USA, around 18,000 gliomas are diagnosed each year, giving an incidence rate of 6.6 per 100,000. Over 90% of gliomas occur in adults (Dolecek 2012). The incidence rate is less in Europe (Crocetti 2012) and lesser still in Asia and Africa, although the rate is similar when comparing developed or industrialised countries (Ohgaki 2005). This variation may result from underestimate of case ascertainment rather than a different genetic predisposition (Crocetti 2012; Ohgaki 2005).
Using the World Health Organization (WHO) classification of brain tumours, gliomas are graded I‐IV to reflect increasing growth rate based on histology (Louis 2007). The recent 2016 WHO classification includes molecular information in addition (Louis 2016). Grade II gliomas (commonly known as 'low‐grade gliomas' (LGGs)) predominantly comprise astrocytomas, oligodendrogliomas and mixed oligoastrocytomas. LGGs tend to be diffuse and infiltrative tumours with a growth rate between that of grade I and grade III tumours. Despite growing slowly initially, they usually transform to high‐grade gliomas (HGGs) with time. The timing of this transition is highly variable and difficult to predict for an individual (Rees 2002). Approximately 50% of people with LGGs will experience malignant transformation usually within five years (Afra 1999; Piepmeier 1996), although more protracted growths of up to 20 years have been described (Claus 2006; Recht 1992). Once transformation occurs, the tumours are highly resistant to therapy. Prognostic factors for survival include age, presence of seizures alone, histology, and larger tumour size (Nicolato 1995; Pignatti 2002).
Clinical features and investigations
People with LGGs usually present with seizures, headaches or focal neurological features (for example, weakness). A classical presentation is a focal seizure in an otherwise healthy young adult. Other people may present with a LGG as an incidental finding after investigation for another condition (e.g. dizziness or blackouts) or after screening for employment purposes and be essentially asymptomatic. Regardless of presentation, the first‐line investigation is a contrast‐enhanced magnetic resonance imaging (MRI) scan. LGGs are solid tumours located within the brain itself and often have a characteristic appearance of poorly defined margins and little mass effect despite often large tumour volumes. Certain features strongly suggest a higher grade tumour, including contrast enhancement, signs of mass effect and significant peri‐tumoural vasogenic oedema. If any of these features is present, people often undergo early surgery (either biopsy or resection), followed by definitive oncological treatment (if appropriate).
Management
If a tumour appears to be an LGG (based on a contrast‐enhanced MRI scan), optimal management is debated (Whittle 2004) and varies between treating centres (Jakola 2012; Soffietti 2010; van den Bent 2005). Certain authorities would often recommend early surgical resection (Dolecek 2012). Case series of people undergoing surgical resection for LGG, often utilising advanced neurosurgical techniques such as awake craniotomy and brain mapping (Bello 2010), have demonstrated impressive outcomes (Duffau 2005). However, studies are limited by selection bias and other methodological issues. Other management options might be conservative management or observation in selected patients. This is often known as 'watch‐and‐wait' (NCCN Guidelines 2016). In particular, when people have no or few symptoms, have deep and inaccessible tumours located in/near 'eloquent' regions of the brain, or have significant co‐morbidity which can complicate the peri‐operative setting, conservative management becomes attractive because it decreases the risk of developing neurologic deficits from surgery (Reijneveld 2001).
Determining optimal management is complicated by tumours that appear to be LGGs on contrast‐enhanced MRI scans but turn out to be higher grade tumours (or non‐glial tumours) when subsequently biopsied. The accuracy of a standard contrast‐enhanced MRI scan in distinguishing a grade II from a grade III astrocytoma is only approximately 30% to 50% because morphologic features of LGGs and HGGs may overlap (Heiss 2011; Kondziolka 1993; Piepmeier 2009; Scott 2002). Although LGGs are typically solid and non‐enhancing, HGGs may mimic this appearance in the ultra‐early stage of development (Barker 1997; Bernstein 1994; Cohen‐Gadol 2004). Enhancement usually reflects a HGG but can be seen in some LGGs where it may indicate a more aggressive tumour (Pallud 2009). Histological analysis is the most reliable method of diagnosing LGGs but requires a surgical procedure, either taking a small tissue sample for diagnostic purposes only (biopsy), or a larger tissue sample when removal of the tumour is attempted (resection). Both of these procedures are invasive and have a risk of adverse events.
Index test(s)
Magnetic resonance (MR) perfusion
Advanced MRI techniques could provide additional information on the aggressiveness of the tumour. One such technique that is becoming routinely employed in clinical centres is magnetic resonance (MR) perfusion, which identifies tumour angiogenesis or the proliferation of abnormal vessels in tumours. Tumoural vessels are tortuous, immature and leaky, and result in abnormal blood flow (haemodynamics) in the brain. On MR perfusion, these are depicted in colour maps of cerebral blood volume (CBV) and vessel wall permeability, which are quantitatively expressed as the ratio of tumoural CBV to normal‐appearing white matter CBV (relative CBV or rCBV), and the volume transfer constant Ktrans (Provenzale 2006), respectively. High‐grade tumours show increased CBV and increased Ktrans on MR perfusion.
Most studies utilising MR perfusion have been in the context of suspected HGGs (Al‐Okaili 2006; Law 2003; Provenzale 2006). In this tumour group, MR perfusion can reliably demonstrate evidence of tumour angiogenesis, and an rCBV higher than 1.75 reliably associates with histological diagnosis (Law 2003). However, the role of MR perfusion for the identification of suspected LGGs has not been described. Specifically, it is not known if MR perfusion can differentiate between grade II gliomas and grade III/IVtumours that otherwise may appear the same on standard MRI scans.
Abnormalities on MR perfusion may also have a role in detecting grade transformation (increased malignancy) during follow‐up or as an independent biomarker of increased malignancy by itself, however neither of these roles were considered in this review.
Clinical pathway
Figure 1 summarises the pathway by which people with infiltrative gliomas are typically managed in the clinical setting. The role of imaging in the identification of primary disease as well as in surveillance for recurrence is incorporated.
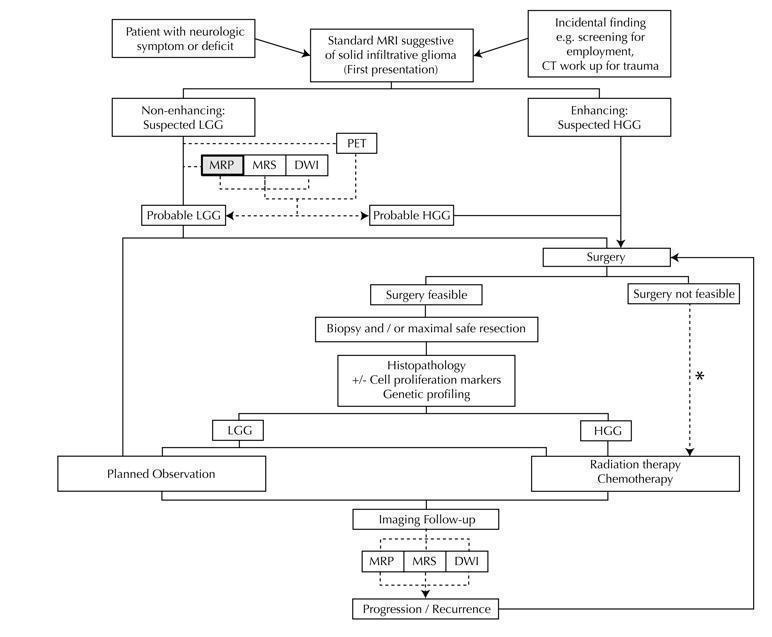
Diagram shows the clinical management algorithm for patients with infiltrative glioma. The role of the index test (MRP) for differentiating LGGs and HGGs at first presentation is shown with alternative tests (MRS, DWI, PET). These advanced MRI techniques are also used to identify progression or recurrence during interval scanning and are included, although they are outside the scope of this review. *May or may not be offered, depending on institutional/regional practice.
Abbreviations: LGG: Low‐grade glioma, HGG: High‐grade glioma,MRP: Magnetic resonance perfusion, MRS: magnetic resonance spectroscopy, DWI: Diffusion‐weighted imaging, PET: Positron emission tomography
This review focuses on primary tumours, determining the accuracy of MR perfusion in differentiating LGGs from HGGs. Such characterisation may improve decision‐making towards conservative management or active treatment (surgery or chemotherapy/radiotherapy).
Prior test(s)
People, whether symptomatic or asymptomatic, are identified as having primary infiltrative gliomas on a standard contrast‐enhanced MRI scan as baseline imaging investigation. However MR alone is insufficient for definite classification into low grade or high grade. Typically, tumours that appear solid, non‐enhancing and associated with little mass effect are suspected to be LGGs, however occasionally HGGs may have the same appearance.
Role of index test(s)
In addition to a standard contrast‐enhanced MRI scan, people with tumours may also undergo MR perfusion as part of their diagnostic work‐up, both of which are performed before surgery. The aim is to detect those tumours that are not LGGs but rather higher grade tumours on histology.
Alternative test(s)
Other imaging methods can be used to increase the accuracy of diagnosing LGGs. These include other MRI techniques such as diffusion weighted imaging and magnetic resonance spectroscopy, and positron emission tomography. These methods may also play a role in predicting tumour grading but they are not included in this review.
Rationale
Imaging features often play a major role in the initial management pathway of people with a brain tumour. There is interest in more accurate diagnosis and, in particular, in identifying when grade II tumours start to transform to grade III/IV tumours as early as possible in order to initiate treatment. If MR perfusion can reliably identify higher grade features in a tumour that otherwise appears like a grade II glioma on standard MRI scan, then possibly intervention would be more appropriate than a conservative 'watch‐and‐wait' approach. Conversely, if the MR perfusion findings reliably predict a grade II glioma, then a conservative 'watch‐and‐wait' approach could continue.
Experience with MR perfusion is relatively limited and only a few large centres publish their own small case series. Interpretation is limited by variability in the conditions assessed and technical details of the scanning. To our knowledge, no previous reviews have tried to systematically analyse all available imaging studies on magnetic resonance perfusion for the diagnosis of solid and non‐enhancing LGGs.
Objectives
To determine the diagnostic test accuracy of MR perfusion for identifying primary solid and non‐enhancing low‐grade (WHO Grade II) gliomas at first presentation in children and adults. In performing the quantitative analysis for this review, patients with LGGs were considered disease positive while patients with high‐grade (Grade III and IV) gliomas, being non‐LGGs, were considered as disease negative.
Secondary objectives
To determine what clinical features and methodological features affect the accuracy of MR perfusion.
Methods
Criteria for considering studies for this review
Types of studies
We included cross‐sectional studies with retrospective or prospective design, and excluded case‐control studies. Non‐English literature studies were eligible for inclusion.
Participants
We considered studies that enrolled paediatric and adult patients with solid and non‐enhancing infiltrative tumours on standard contrast enhanced MRI and who had subsequent WHO grade histologic classification following biopsy or resection. The interval period between MR perfusion and histologic diagnosis must be within two months, as LGGs can transform into HGGs over that period of time. As this review focused on primary and not recurrent disease, participants who had received previous surgery (either biopsy or resection) or oncological treatment (chemotherapy or radiotherapy) prior to the index test were excluded.
Index tests
Studies that employed dynamic susceptibility (DSC) and/or dynamic contrast‐enhanced (DCE) MR perfusion were considered for the review. They were included when data on rCBV and/or Ktrans were provided, regardless of the method of acquisition, imaging analysis or post‐processing performed. Studies that used arterial spin labelling MR perfusion were excluded, as this method has been largely utilised as a research tool.
For DSC MR perfusion, we adopted a common rCBV threshold of 1.75 following the landmark study of Law and colleagues (Law 2003). This value is widely accepted and is used and recommended in clinical practice (Al‐Okaili 2006). In this review, a positive test or rCBV < 1.75 implied an LGG diagnosis while a negative test or rCBV > 1.75 suggested an HGG diagnosis (Appendix 1). With reference to the seven studies included in this review, five studies did not report an rCBV threshold, while the other two studies used or reported various rCBV thresholds (1.29, 1.5, 5.66).
For DCE MR perfusion, there is no consensus in the field regarding a threshold. Only one out of seven included studies reported Ktrans and did not use a threshold.
The generation of MR perfusion data is a multistep process involving acquisition, post‐processing and imaging analysis. Technical differences may arise at each step, which can ultimately influence the perfusion value obtained. Thus it is acknowledged that there may not be an appropriate single threshold when using multicentre MR perfusion data.
Target conditions
The target condition is LGGs (disease positive in quantitative analysis), with the alternative condition being HGGs (i.e. non‐LGG or disease negative in quantitative analysis). Studies must have both conditions to be included in the review.
We included studies that enrolled WHO Grade II diffuse astrocytomas, oligodendrogliomas and oligoastrocytomas, their Grade III anaplastic counterparts and glioblastomas (see Table 1). Other WHO Grade II‐IV gliomas of different histologic type were excluded, because they are rare and usually have distinct clinical characteristics. Grade I tumours were also excluded because their distinct clinical and radiological features separate their management from that of grade II tumours. In this review, gliomas were included irrespective of patient age and tumour location, although it is recognised that paediatric and adult gliomas, and supratentorial and brainstem gliomas may be histologically similar but have biologic and molecular differences (Paugh 2010).
| WHO Grade | Tumour histology |
| I** | Pilocytic astrocytoma Subependymal giant cell astrocytoma Pleomorphic xanthoastrocytoma Ganglioglioma Ependymoma |
| II | Diffuse astrocytoma Oligodendroglioma Oligoastrocytoma |
| III | Anaplastic astrocytoma Anaplastic oligodendroglioma Anaplastic oligoastrocytoma |
| IV | Glioblastoma multiforme Gliomatosis cerebri |
* Partial listing and specific to the tumour histology types relevant to this review.
**These tumours are included in this table for reference only and are not part of the review.
Tumour histologies outside of these target conditions but having similar solid, non‐enhancing appearance as LGGs were recorded and excluded from the analysis.
Reference standards
The reference standard is histological diagnosis assessed according to the WHO 2007 criteria (Table 1). We recorded the method of tumour sampling (biopsy or resection) per study. Reference test failures were treated as no histologic confirmation, and excluded from the analysis.
There are two potential limitations with histology. First, histological diagnosis can be subjective and suffer from significant intra‐ and inter‐observer variability, even among neuropathologists (Brat 2008). Recently, the WHO classification (Louis 2016) has been substantially updated to incorporate molecular profiles in the diagnosis of diffuse gliomas, providing a layer of objectivity to tumour evaluation. However, these are not always available or reported, and were not used in this review. Second, tissue sampling is constrained by the surgical technique of tissue acquisition. Because gliomas are morphologically heterogeneous, they are susceptible to sampling errors, particularly in biopsies. Small volumes of tissue may not be representative of the most malignant component and are therefore less ideal compared with full tissue evaluation afforded by maximal resections. In fact, agreement in histological typing and grading between biopsies and resections has been found to be low (Muragaki 2008).
Search methods for identification of studies
No language or document‐type restrictions were applied.
Electronic searches
We performed a systematic search for literature with quantitative data. Articles were retrieved from the following electronic databases.
-
MEDLINE via OvidSP (Appendix 2, 1996 to 9 November 2016).
-
Embase via OvidSP (Appendix 3, 1996 to 9 November 2016).
-
Web of Science Core Collection, specifically Science Citation Index Expanded and Conference Proceedings Citation Index ‐ Science via Thomson Reuters Web of Science (Appendix 4 1990 to 9 November 2016).
The search was restricted to studies in humans, and was limited to studies in the last 20 years, since MR perfusion is a relatively recent MRI technique.
Searching other resources
Additional references were identified by manually searching the references of relevant review articles. We also used the 'related articles' feature in PubMed to identify articles similar in keywords and database subject headings to the original included studies.
We sought unpublished studies by searching the conference proceedings, available online, of the following radiologic and neuroradiologic societies (years accessed).
-
The Radiology Society of North America (2003 to 2016).
-
The American Society of Neuroradiology (1996 to 2016).
-
The European Society of Radiology (1999 to 2016).
-
The European Society of Neuroradiology (1995 to 2016).
Data collection and analysis
We followed the guidelines outlined in the Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy (Macaskill 2010).
Selection of studies
Prior to abstract review, two review authors (JMA, MGH) performed preliminary screening of titles to exclude irrelevant references. Subsequent screening was carried out by at least two authors (JMA, DMF, MGH, EKCL or JMP). Disagreements were resolved by consensus or third person.
During the abstract review, potentially eligible publications were selected based on the following criteria.
-
Did the study include participants suspected to have primary infiltrative gliomas (including LGG)?
-
Were brain tumours confirmed by histology?
-
Was MR perfusion performed?
An initial review of full‐text publications was then conducted to establish that they meet the following criteria.
-
Did the study enrol participants with solid non‐enhancing brain tumours on standard contrast‐enhanced MRI scan?
-
Were measurements on rCBV and/or Ktrans given?
-
Can a two‐by‐two table be extracted from the provided data?
When this information was not readily available from the published data, we contacted primary authors for clarification. In particular, information on the MRI appearance of the gliomas, i.e. if they were solid and non‐enhancing, and were not always explicitly reported in studies. We also requested for patient‐level data from authors to allow selection of tumours relevant to our review. The data included the individual perfusion values, the method of histologic confirmation, and interval period between the index test and histologic confirmation.
Detailed data extraction of full‐text paper or conference abstract was carried out to determine final eligibility based on the inclusion criteria (see Criteria for considering studies for this review).
Data extraction and management
Two review authors (JMA, DMF) independently completed a data extraction form on all included studies. The following data were retrieved.
-
General information: title, journal, year, publication status, and study design (prospective versus retrospective).
-
Sample size: number of participants included, those meeting the target and alternative conditions (i.e. other‐gliomas and non‐gliomas), and reference test failures.
-
Study setting: country and type of hospital.
-
Baseline characteristics: age, sex.
-
Clinical reference standard test: method of tissue sampling (biopsy or resection), blinding from MR perfusion results, interval period between MR perfusion and tissue diagnosis.
-
Histologic diagnosis and WHO grade of tumour. In this review, LGGs are considered disease positive, and HGGs are disease negative.
-
Details of the index test, including the strength of the MRI scanner, method of MR perfusion performed (DCE or DSC), pulse sequence, use of contrast preload, post‐processing algorithm, imaging analysis, blinding from histological analysis if retrospectively processed.
-
Quantitative results of the index tests, including but not limited to rCBV, Ktrans.
-
Authors' recommended threshold.
-
Number of true positive, false positive, true negative, false negative, and area under the receiver operating characteristic (ROC) curve, extracted based on authors' pre‐specified and recommended thresholds, and based on Law's threshold of 1.75. During the course of this review, we found that authors' pre‐specified and recommended thresholds were either missing or when available, heterogeneous, therefore we only used Law's threshold to construct the two‐by‐two contingency tables. A positive index test implied a diagnosis of LGG while a negative test suggested HGG. Thus, true positives are correctly diagnosed LGGs, false negatives are LGGs incorrectly labelled as HGG, true negatives are correctly diagnosed HGGs, while false positives are HGGs incorrectly labelled as LGG (Appendix 1).
We contacted primary authors via e‐mail for missing data and to obtain clarification on study methods.
Assessment of methodological quality
Each study was assessed for methodological quality using the revised Quality Assessment of Diagnostic Accuracy Studies tool (QUADAS 2) (Whiting 2011). QUADAS 2 assesses study quality through the use of signalling questions which facilitate assessment of risk of bias in four domains: patient sampling; index test; reference standard; and flow and timing. In addition, concerns regarding applicability were also rated in the first three domains. The QUADAS 2 tool for this review is described in Appendix 5 and was applied on study design and on the included patient data. To reduce uncertain risks, we sought clarification from authors when information was missing. e.g. blinding between MR perfusion and histology, details on the MRI acquisition and post‐processing.
Summative data from QUADAS 2 were used to describe the numbers of studies with high/low/unclear risk of bias as well as concerns regarding applicability. All studies with sufficient data were included in the general analysis, but studies with low risk of bias in the domains of reference standard and flow and timing were used in the sensitivity analysis.
Statistical analysis and data synthesis
The reported number of true positive, false positive, false negative and true negative cases were used to construct two‐by‐two tables based on the author's pre‐specified and recommended thresholds, and Law's threshold. When these counts could not be determined from published data, we contacted authors for individual patient‐level data.
Of the seven included studies, five studies did not report an rCBV threshold, while two studies pre‐specified or determined different rCBV thresholds (1.29, 1.5 and 5.66). One study used a pre‐specified threshold of 1.5, which was chosen as a mean between literature values (Law 2003; Zonari 2007). Thus, we used Law's threshold of 1.75 as a common threshold in the quantitative analysis for DSC perfusion, as this is more widely accepted in the field. Individual patient‐level data were classified using this common threshold to construct the two‐by‐two table per study.
Meanwhile, of the seven included studies, only one study reported Ktrans results, precluding quantitative analysis for DCE MR perfusion.
Coupled forest plots showing pairs of sensitivity and specificity, with their 95% confidence intervals (CI), were constructed for each study using RevMan 5.3 (Macaskill 2010; Review Manager 2014).
To estimate the summary sensitivity and specificity, we applied the bivariate model (Reitsma 2005), which accounts for between‐study variability in estimates of sensitivity and specificity through the inclusion of random effects for the logit sensitivity and logit specificity parameters of the bivariate model. To generate the bivariate model parameters required to construct the SROC plot in Revman 5.3 (Review Manager 2014), the model was fitted using the lme4 package of R (R Core team 2013) following Partlett 2016.
Investigations of heterogeneity
As part of the secondary objective, we planned to investigate heterogeneity potentially arising from differences in participant characteristics and study design:
-
tumour histology (subgroups for astrocytomas, oligodendrogliomas, and oligoastrocytomas);
-
MRI strength (1.5T versus 3T);
-
MR perfusion technique (DSC versus DCE);
-
use of contrast preload;
-
post‐processing technique (arterial input function versus gamma variate fitting; region of interest versus histogram analysis);
-
method of histological sampling (biopsy versus resection).
Due to the insufficient number of studies, we were unable to perform regression approach to explore heterogeneity.
Subgroup analysis was conducted for tumour histology (astrocytomas versus oligodendrogliomas plus oligoastrocytomas) based on the bivariate model. As the data are sparse, the bootstrap method was used to compute the 95% confidence intervals for the estimates through the boot package of R (R Core team 2013). Other subgroup analyses were not possible due to the small number of studies and participants.
Sensitivity analyses
To determine the robustness of the outcome of the meta‐analysis, we conducted sensitivity analysis on good quality studies, defined as those with low risk of bias in domains 3 (reference standard) and 4 (flow and timing) as specified in the QUADAS 2 criteria (Appendix 5).
We also initially intended to conduct sensitivity analysis based on tumour status outside the target and alternative conditions (i.e. including other‐gliomas and non‐gliomas), but no data were available to perform this.
Assessment of reporting bias
We did not assess reporting bias as there are no clear‐cut methods to perform this for studies of diagnostic accuracy (Brazzelli 2009). It is noted that the index test under review is a widely available MRI technique and could be routinely employed in clinical practice (NCCN Guidelines 2016). As such, it would be unlikely to have a record of all attempted evaluations using this technique and therefore positive results are more likely to be reported in the literature (Irwig 1995). To minimise this, we included radiology and neuroradiology conference proceedings in our literature search, where negative results could be documented which may not have been published. Further, the small number of included studies was also inadequate to assess reporting bias by funnel plot (Deeks 2005).
Results
Results of the search
The study selection process is summarised in a PRISMA flow chart (Figure 2). The literature search performed on 11 Nov 2016 identified 32,338 records, after de‐duplication and preliminary screening we identified 535 potentially relevant citations. After a further screening of titles and abstracts, we identified 19 studies for full‐text review. Of these, we excluded two which reported gliomas of mixed morphology that precluded selection of solid and non‐enhancing types (Law 2003; Sugahara 1998 ), two were excluded due to insufficient samples (no solid non‐enhancing HGGs) (Rollin 2006; Senturk 2009), seven excluded due to an unclear time interval between the index test and reference standard (protocol specified less than two months) (Fan 2006; Gaudino 2010; Lev 2004; Liu 2011; Romano 2011; Sahin 2013; Whitmore 2007), and one excluded as no two‐by‐two table could be derived (Morita 2010). Thus seven studies met all inclusion criteria.
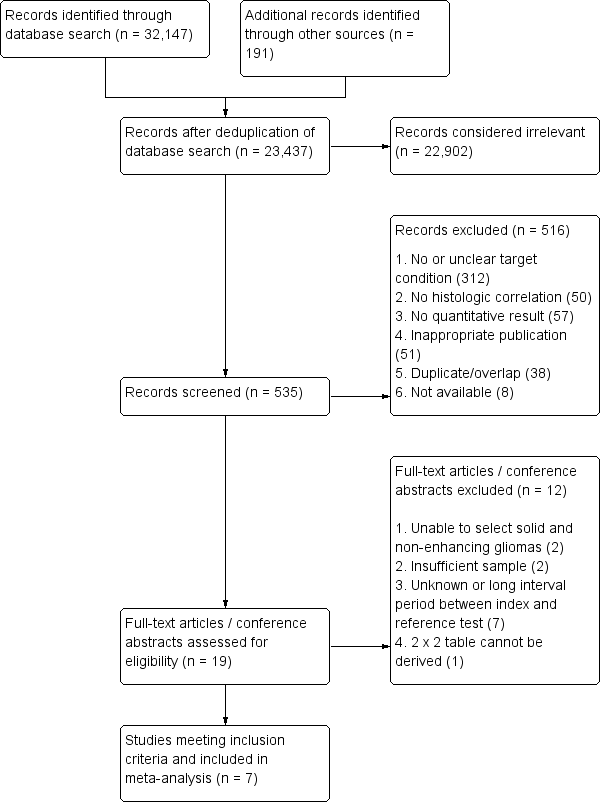
Flow diagram.
Methodological quality of included studies
We judged the methodological qualities of each of the seven included studies according to the modified QUADAS‐2 criteria (Appendix 5) and the results are presented in the respective sections below and summarised in Figure 3 and Figure 4. Often the research questions of the accepted studies did not match our review question, and we assessed studies for their risk of bias and concerns regarding applicability based on the study design and the extracted included patient data.

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study using QUADAS 2 tool, applied on study design and included patient data
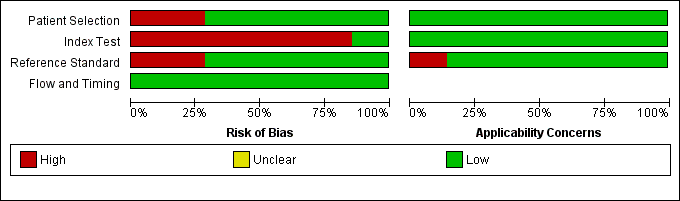
Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies
Only one study had low risk of bias and low concern for applicability across all domains (Cuccarini 2016). Five studies had low risk of bias in the domains of reference standard and flow & timing and were deemed of good quality (Cuccarini 2016; Falk 2014; Guzman de Villoria 2014; Kudo 2016; Maia 2004).
Participant Selection
Risk of bias for participant selection was low in five out of seven studies (Cuccarini 2016; Falk 2014; Guzman de Villoria 2014; Kudo 2016; Maia 2004). The other two studies had high risk due to unclear patient sampling (Yang 2002) and inappropriate exclusion of small tumours (Koob 2016). Although many studies had different objectives from our review and also reported contrast enhancing tumours and Grade 1 gliomas, by extracting patient‐level data from many authors, we were able to select participants with the target and alternative conditions only. Thus concerns of applicability with regard to participant selection were low.
Index test
The highest level of risk of bias was observed in the index test domain, with six studies lacking use of a pre‐specified threshold. Only one study used a pre‐specified rCBV threshold of 1.5 (Cuccarini 2016), which was chosen as a mean between literature values (Law 2003; Zonari 2007). However, this limitation in study design was overcome by using individual patient‐level data, which allowed use of a common rCBV threshold of 1.75 for the quantitative analyses. Meanwhile, in one study it was unclear if the index test was interpreted without knowledge of the results of the reference standard (Yang 2002). Concerns for applicability with regard to the index test were low, with good evidence in all included studies to suggest MR perfusion was performed in a way similar to clinical practice.
Reference standard
Reference standard issues were present in two studies, due to uncertainties regarding the blinding of interpretation (Koob 2016; Yang 2002). All studies based tumour grading on histopathological assessment. Concerns for applicability with regard to reference standard domains were generally low, with one study deemed high concern due to an unclear description of the proportions of patients undergoing a resection or biopsy (Koob 2016).
Flow and timing
There were no flow and timing issues. In all studies, patients underwent either biopsy or resection irrespective of the results of the index test. Only patients with an interval period of less than two months between the index test and reference standard were included in the analysis.
Findings
Seven studies were included; one study met inclusion criteria based on published data alone (Yang 2002), while the other six were confirmed to meet inclusion criteria after obtaining patient‐level data and/or clarification from authors (Cuccarini 2016; Falk 2014; Guzman de Villoria 2014; Koob 2016;Kudo 2016Maia 2004). Collectively, the seven studies reported 392 patients with brain tumours/gliomas, however only 124 were confirmed to be primary and untreated solid and non‐enhancing WHO grade II‐IV gliomas, and of these, only 115 underwent tissue sampling within 2 months of MR perfusion and were included in the review. The sample size per study was generally small and ranged from 4 to 48 cases, and only 2 studies had sample sizes of more than 20 (Cuccarini 2016; Maia 2004). The limited available evidence restricts the conclusions that can be drawn from the review.
All seven studies reported rCBV, which allowed quantitative analysis for DSC MR perfusion. Meanwhile, only one study reported Ktrans (Falk 2014,) which precluded quantitative analysis for DCE MR perfusion.
The included studies originated from Europe (Italy, Sweden, Spain and France), Asia (two studies from Japan) and South America (one from Brazil). All avoided case‐control design. One study was retrospective (Koob 2016), while the rest were prospectively performed. The studies were mostly conducted in university hospitals save for one study (Cuccarini 2016). The studies recruited mostly adults (only Koob 2016 specifically recruited paediatric participants).
Most patients underwent resection and only a small proportion underwent biopsy for tissue diagnosis. Histologic confirmation was via resection only in three studies (Cuccarini 2016; Kudo 2016; Maia 2004), mix of resection (predominant) and biopsy in three studies (Falk 2014; Guzman de Villoria 2014; Yang 2002), and was unspecified in one study (Koob 2016).
The majority of MRI scans were performed on a 1.5T scanner (Cuccarini 2016; Guzman de Villoria 2014; Koob 2016; Maia 2004; Yang 2002); two studies used a 3T scanner (Falk 2014; Kudo 2016). All studies performed DSC MR perfusion and provided rCBV results. Other DSC MR perfusion‐derived quantitative measures such as cerebral blood flow and apparent transfer constant were additionally reported by one study (Falk 2014), which was also the only study that performed DCE MR perfusion and provided Ktrans. Contrast preloading was used in two studies (Falk 2014; Kudo 2016), but not in four studies (Guzman de Villoria 2014;Koob 2016;Maia 2004;Yang 2002), while it was not reported in one study (Cuccarini 2016). The post‐processing algorithm was reported in all studies; four studies used arterial input function (Cuccarini 2016;Falk 2014; Koob 2016; Kudo 2016); two used gamma variate function (Guzman de Villoria 2014; Maia 2004), and one used area under the curve analysis (Yang 2002). All studies employed region of interest (ROI) method to obtain perfusion values in areas showing high perfusion, and one study (Falk 2014) provided histogram results from the ROI's drawn.
Individual perfusion values were published in two studies (Maia 2004; Yang 2002) and were provided by authors in the other five studies (Cuccarini 2016; Falk 2014; Guzman de Villoria 2014; Koob 2016; Kudo 2016). From these published and unpublished data, a total of 124 solid and non‐enhancing gliomas were identified, of which 115 (83 LGGs, 32 HGGs) met all inclusion criteria and were selected for the review.
The average rCBV per tumour grade and tumour histology in each included study are summarised in Table 2. Most studies recruited Grade II and III gliomas, with only one case of a solid and non‐enhancing Grade IV/glioblastoma with rCBV of 0.3 (Cuccarini 2016). All tumours were graded using the WHO classification, and in this review LGG was classified as disease positive, and HGG as disease negative for the quantitative analysis. Histology was available in all of them except for two of the four included cases from Koob 2016. Diffuse astrocytomas were reported in the remainder of the studies, and other tumour histology types were not always represented per study. Other tumours with solid and non‐enhancing appearance on MRI but with histology different from the target and alternative conditions were reported and excluded in two studies (Cuccarini 2016; Falk 2014).
| Included studies | LGG (Grade II) | HGG (Grade III+IV) | DA | OA | OG | AA | AOA | AOG |
| 1.15 ± 0.95 | 1.18 + 0.8 | 1.19 ± 0.76 | 1.12 ± 1.13 | 1.22 ± 0.57 | 1.15 ± 0.53 | 1.33 ± 0.98 | ||
| 1.30 + 0.48 | 1.76 + 0.93 | 1.48 + 0.69 | 1.20 + 0.21 | 1.19 + 0.32 | 2.22 + 1.18 | 0.86 | 1.76 | |
| 1.07 + 0.79 | 0.75 | 0.98 + 0.29 | 1.24 ±1.33 | 0.75 | ||||
| 0.8 + 0.04 | 0.8 + 0.6 | [0.77] | 0.82 | [0.41] | 1.28 | |||
| 3.1 ± 1.19 | 3.83 ± 2.34 | 2.31 ±1.23 | 3.88 ±.46 | 3.8 + 2.3 | ||||
| 1.16 ± 0.63 | 3.2 ± 0.35 | 0.9 ±.43 | 1.98 ± 0.57 | 1.27 | 3.24 ± 0.37 | 2.99 | ||
| 1.29 ± 0.17 | 1.76 ± 0.08 | 1.29 ± 0.17 | 1.81 | 1.7 |
LGG: Low‐grade glioma, HGG: high‐grade glioma, DA: diffuse astrocytoma, OA: oligoastrocytoma, OG: oligodendroglioma, AA: anaplastic astrocytoma, AOA: Anaplastic oligoastrocytoma, AOG: anaplastic oligodendroglioma.
Nearly all HGGs are Grade III, except for one case of Grade IV/glioblastoma from Cuccarini 2016, with rCBV of 0.3. Bracketed values in Koob 2016 are included for completion but represent unspecified gliomas, with no reported histology.
The average rCBV (range) per glioma grade and histology with their numbers are 1.29 (0.01 to 5.10) for LGGs (N = 83), 1.89 (0.30 to 6.51) for HGGs (N = 32). Average rCBV was 1.19 (0.34 to 3.72) for Grade II astrocytomas (N = 40), 1.63 (0.01 to 4.30) for Grade II oligodendrogliomas (N = 19), 1.22 (0.08 to 5.10) for Grade II oligoastrocytomas (N = 23). The rCBV for combined Grade II oligodendroglioma + oligoastrocytoma was 1.41 (0.01 to 5.10) (N = 42); 2.02 (0.65 to 3.79) for Grade III astrocytomas (N = 15), 2.99 (1.70 to 6.51) for Grade III oligodendrogliomas (N = 4); 1.44 (0.60 to 3.34) for Grade III oligoastrocytomas (N = 11) and 1.96 (0.60 to 6.51) for combined Grade III oligodendrogliomas+oligoastrocytomas (N = 15).
Only one study (Cuccarini 2016) used a pre‐specified rCBV threshold, and chose 1.5 as a mean between literature threshold values (Law 2003; Zonari 2007). Two studies determined rCBV thresholds for differentiating LGGs and HGGs: 1.29 (Cuccarini 2016) and 5.66 (Kudo 2016). The other five studies did not determine an rCBV threshold (Falk 2014;Guzman de Villoria 2014; Koob 2016; Maia 2004, Yang 2002). Because of the lack or variability of thresholds reported by studies, we adopted the widely accepted rCBV value of 1.75 as common threshold for the quantitative analysis of DSC MR perfusion. In this review, an rCBV < 1.75 was classified as test positive and implied a diagnosis of LGG, while an rCBV > 1.75 was classified as test negative and suggested a diagnosis of HGG. Thus in constructing the two‐by‐two contingency tables, true and false positives represented the number of LGGs correctly and incorrectly diagnosed, respectively, while true and false negatives represented the number of HGGs correctly and incorrectly diagnosed, respectively (Appendix 1).
The sensitivity and specificity of the seven included studies are presented in coupled forest plots in Figure 5. Sensitivity estimates were generally in the upper range and had wide confidence intervals. Mean sensitivities were > 0.70 in six out of seven studies (excepting Kudo 2016). Of these, two studies with a mean sensitivity of 1.00 had very wide confidence intervals, and were derived from studies with the smallest sample size of four each (Koob 2016, Yang 2002). In contrast, two studies with the largest sample sizes of 48 and 21 had mean sensitivities of 0.82 and 0.93 (Cuccarini 2016 and Maia 2004, respectively) with moderately wide confidence intervals. Meanwhile, mean specificities were quite heterogeneous and showed even wider confidence intervals. The two largest studies of Cuccarini 2016 and Maia 2004 had opposing mean specificity values of 0.21 and 1.00, respectively.
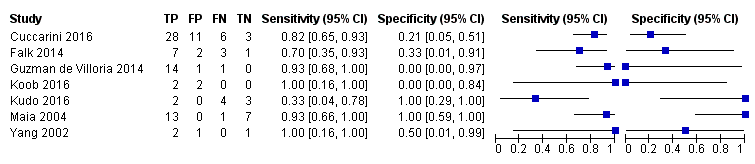
Coupled forest plots of included studies using rCBV threshold of < 1.75 for differentiating low grade gliomas from high‐grade gliomas.
Meta‐analysis of the seven studies using a bivariate model yielded a summary sensitivity and specificity of 0.83 (95% CI 0.66 to 0.93) and 0.48 (95% CI 0.09 to 0.90), respectively (Figure 6). The 95% confidence ellipse of the summary point is quite wide and spans the upper half of the range of sensitivity, and spans nearly the entire range of specificity.

Summary ROC Plot of DSC MR perfusion using rCBV threshold of 1.75 for differentiating low grade gliomas from high‐grade gliomas. In this review, a positive test or rCBV < 1.75 implied an LGG diagnosis, while a negative test or rCBV > 1.75 suggested an HGG diagnosis. In the SROC plot, each study is represented by an open circle with emanating lines, representing the sensitivity and specificity with their confidence intervals. The size of the open circle is proportional to the study sample size. The shaded circle represents the pooled sensitivity and specificity surrounded by a 95% confidence ellipse (dotted line), which in this case is 0.830 (95% CI 0.657, 0.926) and 0.479 (95% CI 0.086, 0.900), respectively.
Regression analysis to explore heterogeneity was not performed due to insufficient data.
Subroup analysis on tumour histology types showed summary sensitivities and specificities of 0.92 (95% CI 0.55 to 0.99) and 0.42 (95% CI 0.02 to 0.95) respectively, for astrocytomas using data from six studies (55 participants) (Cuccarini 2016; Falk 2014; Guzman de Villoria 2014; Kudo 2016; Maia 2004; Yang 2002), and 0.77 (95% CI 0.46 to 0.93) and 0.53 (95% CI 0.14 to 0.88), respectively, for combined oligodendrogliomas+oligoastrocytomas using data from six studies (56 participants) (Cuccarini 2016; Falk 2014; Guzman de Villoria 2014; Koob 2016; Kudo 2016; Maia 2004).
Additional subgroup analysis on other variables such as histologic confirmation method, MRI acquisition and post‐processing could not be performed due to limited data.
Sensitivity analysis using five good quality studies (107 participants: 79 LGG, 28 HGG) with low risk of bias in the domains of reference standard and flow and timing resulted in summary sensitivity of 0.80 (95% CI 0.61 to 0.91) and summary specificity of 0.67 (95% CI 0.07 to 0.98) (Cuccarini 2016; Falk 2014; Guzman de Villoria 2014; Kudo 2016; Maia 2004).
Overall, the individual studies and meta‐analysis yielded variable and/or wide‐ranging estimates which are attributed to the small sample sizes. Thus currently, the diagnostic accuracy of MR perfusion cannot be reliably determined based on the available data. Insufficient data also precluded determination of clinical and methodological factors affecting the accuracy of MR perfusion.
Discussion
In this review, we determined the accuracy of magnetic resonance (MR) perfusion for differentiating primary untreated low‐grade gliomas (LGGs) from high‐grade gliomas (HGGs), when they appear as solid and non‐enhancing on standard magnetic resonance imaging (MRI). While MR perfusion is becoming increasingly commonly used in clinical practice and regarded to be an integral technique in current brain tumour imaging (Welker 2015), we found limited evidence regarding its diagnostic performance for grading solid and non‐enhancing diffuse gliomas. There were insufficient data to determine the clinical and methodological features that affect the accuracy of this technique. The conclusions that can be drawn from the review are therefore restricted.
Summary of main results
Seven studies were included and all but one were prospectively carried out. All studies reported CBV ratio of tumour (rCBV) and only one reported Ktrans , limiting this review to DSC MR perfusion only. While most examined the diagnostic accuracy of MR perfusion, pre‐specified thresholds were not commonly used, and thresholds were either not determined or varied; thus we applied a common rCBV threshold of 1.75 for the quantitative analysis. The acquisition and post‐processing of MR perfusion were moderately heterogeneous, with different scanner magnetic field strengths employed (1.5 and 3T), different pulse sequences (spin echo and gradient echo), use and non‐use of contrast preload, and different post‐processing algorithms (arterial input function, gamma variate function and area under the curve). This may reflect the difficulties of implementing a single standard in clinical practice, or a lack of evidence for any given protocol, but may also make problematic the use of a single threshold when handling multicentre perfusion data. Subsequent analysis was similar, with predominant use of the region of interest (ROI) method to obtain rCBV, and targeting of tumour regions that show high perfusion. The majority of tumours were resected, allowing a more definitive reference standard.
From published data and unpublished results from authors, we were able to identify 115 solid and non‐enhancing gliomas that met all the inclusion criteria and allowed quantitative analysis for dynamic susceptibility (DSC) MR perfusion. The studies generally had small sample sizes (range of 4 to 48). Meta‐analysis identified that estimates for both mean sensitivity and specificity were very uncertain so evidence of diagnostic performance is unreliable. This is identified from the wide confidence intervals for the estimates of sensitivity and specificity: sensitivity 0.83 (95% CI 0.66 to 0.93) and specificity of 0.48 (95% CI 0.09 to 0.90). Sensitivity analysis using good quality studies and subgroup analysis on tumour histology produced consistent results; i.e. sensitivity and specificity cannot be reliably estimated based on small number of patients in the included studies. Regression analysis to explore heterogeneity also could not be performed due to insufficient data.
Thus, from the currently reviewed evidence, we cannot reliably estimate specificity from meta‐analysis as although the average estimate is 48%, from the 95% CI the value could be as low as 9% or as high as 90%. Sensitivity is also poorly estimated with an average of 83%, but with estimates potentially including values ranging from 66% to 93%.
A precis of these findings, together with the study quality assessment, are presented in the summary of findings Table.
Our meta‐analysis on 83 LGGs and 32 HGGs suggest that DSC MR perfusion performance cannot be reliably estimated based on current evidence for either sensitivity or specificity for the identification of primary and untreated, solid and non‐enhancing WHO grade II gliomas from higher grade gliomas. Additionally, the limited available data also preclude assessment on how other clinical and methodological features affect the accuracy of MR perfusion. Future research would need to include a much larger sample size of patients with both LGG and HGG, preferably using a standardised scanning protocol to reliably estimate performance of MR perfusion. A recent paper demonstrates that standardised acquisition and analysis for MR perfusion in a multicentre clinical setting is feasible, and derived an rCBV threshold of 3.33 to differentiate Grade II from III/IV gliomas (Anzalone 2017).
Strengths and weaknesses of the review
One study (Cuccarini 2016) closely mirrored the patient population and study design considered to be appropriate for studies of diagnostic accuracy. Also, most of the included studies were prospective in design and performed resection, which allowed a more definitive histologic diagnosis to serve as reference standard. The small number of included studies poses a limitation but this is a reflection of strict methodological standards required to remain faithful to the review question. During the screening process, we encountered many studies that performed MR perfusion for glioma grading, however they could not be included because often the MRI appearances of the tumour could not be ascertained or the perfusion values of such solid and non‐enhancing gliomas were not specifically reported. Many authors were contacted and invited to share their data by which we were able to include unpublished perfusion values from five studies in the meta‐analysis (Cuccarini 2016; Falk 2014; Guzman de Villoria 2014; Koob 2016; Kudo 2016). Overall, performing a meta‐analysis has allowed a thorough critique of the methodological quality of studies in the literature, and a substantially larger number of participants to base conclusions upon than any one single study. However, the included number of patients (115) remains small and limits the conclusions that can be drawn from this review.
Applicability of findings to the review question
Based on a small number of participants, the estimated sensitivity suggests that DSC MR perfusion may be able to detect up to 93% of patients with LGG, but sensitivity can be as low as 66%. Thus, between 7% and 34% of patients with LGG may have MR perfusion findings suggestive of HGG, and patients may feel compelled to undergo early intervention. In this instance one option could be to perform an early diagnostic biopsy, which can be performed with little morbidity (Kreth 2001), but risks undersampling and falsely undergrading the tumour (Muragaki 2008). Another option would be to consider aggressive surgical resection as is typically performed in HGG, for example with fluorescence or intra‐operative MRI guidance. This could potentially differ from the surgical approach offered in LGG where one might prefer awake craniotomy with functional brain mapping. A further option would be a further standard MRI scan with rCBV after a short time interval, as earlier intervention has not been widely shown yet to extend survival in LGG or asymptomatic transforming LGG and repeat scan may add further weight regarding whether or not to intervene.
Both surgical options will allow histologic confirmation but perhaps more importantly, provide a molecular profile of the tumour. The recent major restructuring of the WHO classification for brain tumours (Louis 2016) now establishes primacy of the incorporation of molecular genetic features with histology in tumour diagnosis, prognostication and therapy guidance. Following suit, the European Association for Neuro‐Oncology (EANO) have recently issued treatment guidelines based on this integrated phenotype‐genotype classification and recommends diagnostic biopsy at minimum, excepting high‐risk cases and those with unfavourable prognosis where treatment is unlikely to be successful (Weller 2017).
Meanwhile the estimated specificity of MR perfusion is more heterogeneous: 9% to 90%. This means that between 10% and 91% of cases of HGGs may be labelled as LGGs and patients may decide for a watch‐and‐wait approach. This would lead to delay in performing resection, when this would have been the strongly recommended initial treatment approach for people with surgically accessible HGG (Dietrich 2017).
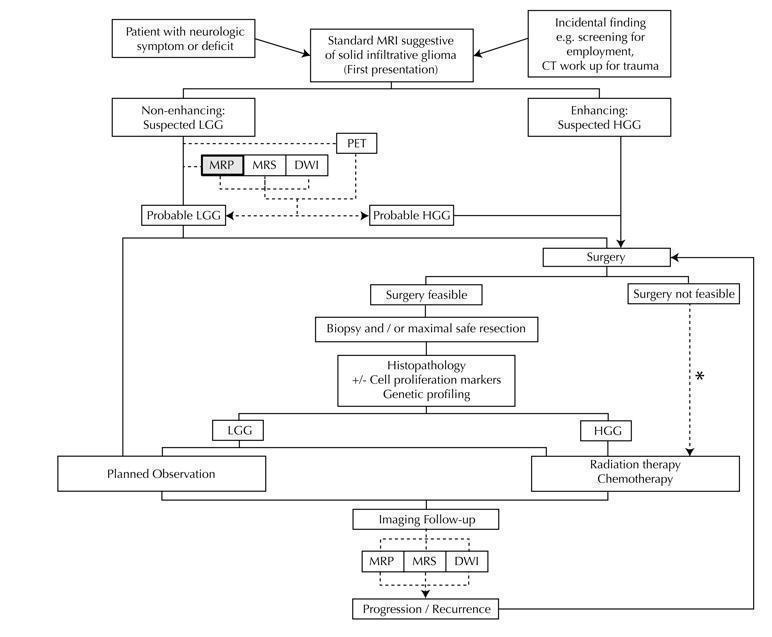
Diagram shows the clinical management algorithm for patients with infiltrative glioma. The role of the index test (MRP) for differentiating LGGs and HGGs at first presentation is shown with alternative tests (MRS, DWI, PET). These advanced MRI techniques are also used to identify progression or recurrence during interval scanning and are included, although they are outside the scope of this review. *May or may not be offered, depending on institutional/regional practice.
Abbreviations: LGG: Low‐grade glioma, HGG: High‐grade glioma,MRP: Magnetic resonance perfusion, MRS: magnetic resonance spectroscopy, DWI: Diffusion‐weighted imaging, PET: Positron emission tomography

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study using QUADAS 2 tool, applied on study design and included patient data
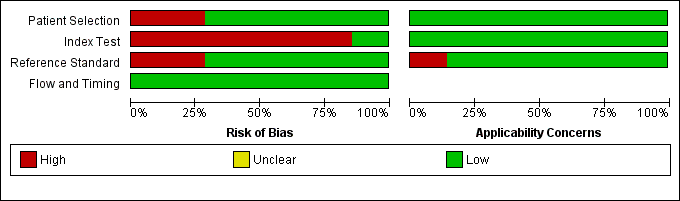
Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies
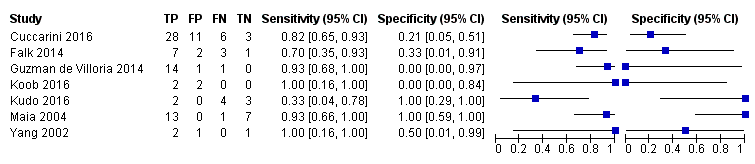
Coupled forest plots of included studies using rCBV threshold of < 1.75 for differentiating low grade gliomas from high‐grade gliomas.

Summary ROC Plot of DSC MR perfusion using rCBV threshold of 1.75 for differentiating low grade gliomas from high‐grade gliomas. In this review, a positive test or rCBV < 1.75 implied an LGG diagnosis, while a negative test or rCBV > 1.75 suggested an HGG diagnosis. In the SROC plot, each study is represented by an open circle with emanating lines, representing the sensitivity and specificity with their confidence intervals. The size of the open circle is proportional to the study sample size. The shaded circle represents the pooled sensitivity and specificity surrounded by a 95% confidence ellipse (dotted line), which in this case is 0.830 (95% CI 0.657, 0.926) and 0.479 (95% CI 0.086, 0.900), respectively.
| Population | Almost all adults | |||||
| Setting | Mostly university hospitals, employing exclusively 1.5T or 3T MRI scanners | |||||
| Index test | Dynamic susceptibility contrast MR perfusion (commonly gradient echo rather than spin echo sequence acquisition), usually without contrast preload, typically using arterial input function or gamma variate function post‐processing algorithms, and preferentially using region‐of‐interest method to obtain Max rCBV values (CBV ratio of tumour: contralateral normal appearing white matter) | |||||
| Importance | For solid and non‐enhancing brain tumours with low rCBV, patients with no or little neurologic deficit may opt for conservative management over surgery to avoid early neurologic disability. Meanwhile, patients with high rCBV could favour early treatment for better tumour control. | |||||
| Reference standard | All with histologic examinations, majority with resection. | |||||
| Studies | Mostly prospective cross sectional studies (no case‐control studies) | |||||
| Positive Test | Summary accuracy | No. of study participants / selected patients | Prevalence | Implications | Quality of studies | Comments |
| rCBV threshold <1.75 indicates LGG | Sensitivity (proportion of LGG detected by MR perfusion) 0.83 (0.66, 0.93) (proportion of HGG detected by MR perfusion) 0.48 (0.09 to 0.90) | 392 patients / 115 with solid non‐enhancing Grade II‐IV gliomas who underwent tissue sampling within 2 months of MR perfusion (7 studies) | In a hypothetical population of solid and non‐enhancing Grade II‐IV gliomas, the prevalence of LGGs and HGGs is 72% and 28%, respectively. | Given 100 patients with solid and non‐enhancing infiltrative gliomas, 72 will have LGG and 28 with HGG. Of 72 patients with LGG, it is expected 12 patients will be misclassified to have HGG (but this could potentially be between 5 to 24 patients) and may undergo surgery, thus risking early neurologic deterioration. Meanwhile, of 28 patients with HGG, 15 will be misclassified to have LGG (but this could be between 3 to 25 patients), which may lead to a delay in treatment that can potentially adversely affect outcomes. | Generally low risk of bias in the patient selection domain, excepting 2 out of 7 studies with unclear patient sampling and inappropriate exclusion of small tumours. High risk of bias in the index test domain, mainly because 6 out of 7 studies did not use a pre‐specified threshold. However this did not affect meta‐analysis as we used a common rCBV threshold of 1.75. Low concerns of applicability for the patient selection, index test and reference standard domains by using patient‐level data. | Low numbers (4 to 48) with target and alternative conditions per study and only 2 studies had >20 patients. In general, individual studies had heterogeneous sensitivity and specificity, both with wide confidence intervals. Only 1 study had low risk of bias and low concern of applicability across all domains. Five studies were considered good quality (i.e., with low risk of bias in the domains of reference standard and flow & timing). Their sensitivity analysis yielded sensitivity 0.80 (95% CI 0.61 to 0.91) and specificity 0.67 (95% CI 0.07 to 0.98). Subgroup analysis showed sensitivity/specificity of [0.92 (95% CI 0.55 to 0.99)/ 0.42 (95% CI 0.02 to 0.95) in astrocytomas and 0.77 (95% CI 0.46 to 0.93)/0.53 (95% CI 0.14 to 0.88) in oligodendrogliomas + oligoastrocytomas. Data were too sparse to investigate any differences across subgroups. |
| HGG: high‐grade glioma, LGG: low‐grade glioma, rCBV: relative cerebral blood volume | ||||||
| WHO Grade | Tumour histology |
| I** | Pilocytic astrocytoma Subependymal giant cell astrocytoma Pleomorphic xanthoastrocytoma Ganglioglioma Ependymoma |
| II | Diffuse astrocytoma Oligodendroglioma Oligoastrocytoma |
| III | Anaplastic astrocytoma Anaplastic oligodendroglioma Anaplastic oligoastrocytoma |
| IV | Glioblastoma multiforme Gliomatosis cerebri |
| * Partial listing and specific to the tumour histology types relevant to this review. **These tumours are included in this table for reference only and are not part of the review. | |
| Included studies | LGG (Grade II) | HGG (Grade III+IV) | DA | OA | OG | AA | AOA | AOG |
| 1.15 ± 0.95 | 1.18 + 0.8 | 1.19 ± 0.76 | 1.12 ± 1.13 | 1.22 ± 0.57 | 1.15 ± 0.53 | 1.33 ± 0.98 | ||
| 1.30 + 0.48 | 1.76 + 0.93 | 1.48 + 0.69 | 1.20 + 0.21 | 1.19 + 0.32 | 2.22 + 1.18 | 0.86 | 1.76 | |
| 1.07 + 0.79 | 0.75 | 0.98 + 0.29 | 1.24 ±1.33 | 0.75 | ||||
| 0.8 + 0.04 | 0.8 + 0.6 | [0.77] | 0.82 | [0.41] | 1.28 | |||
| 3.1 ± 1.19 | 3.83 ± 2.34 | 2.31 ±1.23 | 3.88 ±.46 | 3.8 + 2.3 | ||||
| 1.16 ± 0.63 | 3.2 ± 0.35 | 0.9 ±.43 | 1.98 ± 0.57 | 1.27 | 3.24 ± 0.37 | 2.99 | ||
| 1.29 ± 0.17 | 1.76 ± 0.08 | 1.29 ± 0.17 | 1.81 | 1.7 | ||||
| LGG: Low‐grade glioma, HGG: high‐grade glioma, DA: diffuse astrocytoma, OA: oligoastrocytoma, OG: oligodendroglioma, AA: anaplastic astrocytoma, AOA: Anaplastic oligoastrocytoma, AOG: anaplastic oligodendroglioma. Nearly all HGGs are Grade III, except for one case of Grade IV/glioblastoma from Cuccarini 2016, with rCBV of 0.3. Bracketed values in Koob 2016 are included for completion but represent unspecified gliomas, with no reported histology. | ||||||||
| Test | No. of studies | No. of participants |
| 1 rCBV ‐ Law Threshold Show forest plot | 7 | 115 |


